Abstract
Aims:
Adolescents and young adults at clinical high risk (CHR) for psychosis report few close friends. Social support has been linked to conversion to psychosis and psychosis relapse in CHR individuals. Expanding earlier research on loneliness and friendships at a single timepoint, this study described composition and changes in social network and its association with clinical and cognitive symptoms among CHR adolescents.
Methods:
95 individuals (46 CHR individuals, 49 healthy volunteers) completed baseline and one-year follow-up Social Network Index (SNI) evaluations and clinical interviews. Analyses first examined SNI size and composition across ten categories (e.g., family, close friends, coworkers, classmates) between groups. Then, the relationship between SNI size and baseline social symptoms (i.e., paranoia, social anhedonia, social anxiety, social cognition), social function, and changes in symptoms and social networks over 1-year were examined within the CHR group.
Results:
CHR individuals showed smaller social networks overall, driven by fewer friendships and family relationships. Social cognition and social anxiety significantly related to SNI size at baseline, but social anhedonia and paranoia did not. SNI size related to social function, but with a modest effect size (r’s=.45 and .56). Surprisingly, an increase in positive symptom severity related to an increase in familial but a decrease in coworker social network size.
Conclusions:
The social support deficits in the CHR group were specific to relatives and friendships, with social anxiety and social cognition as implicated symptoms. Social relationships may serve as a promising early intervention target in individuals at CHR for psychosis.
Keywords: psychosis risk, social networks, social support, social cognition, social anxiety
Introduction
Social deficits and decreased social support are significant predictors of conversion to psychosis in clinical high risk (CHR) individuals (Brucato et al., 2017; Fusar-Poli et al., 2010; Gayer-Anderson & Morgan, 2013), occurring prior to psychosis onset in individuals at CHR (Gee & Cannon, 2011; Pruessner, Iyer, Faridi, Joober, & Malla, 2011; Robustelli, Newberry, Whisman, & Mittal, 2017). As a result, social relationships may serve as a potential treatment target for CHR individuals with attenuated positive symptoms.
In an earlier study, Robustelli and colleagues (2017) indicated fewer close friendships (the only social category examined), lower diversity of social contacts, and less perceived support (Robustelli et al., 2017). It remains unclear, however, if this is specific to friendship (the only examined domain), related to clinical and cognitive symptoms, or reflected changes in symptoms.
CHR individuals show deficits in social cognition and increased symptoms of social anxiety, social anhedonia, and paranoia that may contribute to social deficits (Cornblatt et al., 2012; Kuhney et al., 2021; Lencz, Smith, Auther, Correll, & Cornblatt, 2004; Rietdijk et al., 2013). Yet, no study has examined how social deficits impact social network size for CHR adolescents. Additionally, the social network index measure has not been validated against traditional measures of social functioning for CHR adolescents. Lastly, a longitudinal component to describe social network size and composition change over time was not explored by Robustelli et al. (2017). Examining data from a single time point (Addington, Penn, Woods, Addington, & Perkins, 2008; Robustelli et al., 2017) limits insight into how networks change during a period marked by social development (Wrzus, Hänel, Wagner, & Neyer, 2013).
Identifying symptoms that impact social network size can guide early interventions during the psychosis risk period. Poor social support is associated with increased negative (Pruessner, Iyer, Faridi, Joober, & Malla, 2011) and positive (Robustelli et al., 2017) symptoms in CHR individuals. Although positive and negative symptoms may contribute to social deficits, paranoia and social anhedonia are particularly relevant because of their social nature (Blanchard, Mueser, & Bellack, 1998; Gee & Cannon, 2011; Robustelli et al., 2017). Negative social symptoms (e.g., social anhedonia) persist following effective treatment of positive symptoms (Cornblatt et al., 2003). Targeting positive symptoms alone may not be sufficient for improving social support. Additionally, social support deficits do not respond to typical psychosis treatment (Cornblatt et al., 2003). Identifying which symptoms are most relevant to social network size would allow for more targeted early interventions.
CHR individuals are also more likely to be socially anxious compared to their peers (Kuhney et al., 2021; Rietdijk et al., 2013), which may influence social network size through the initiation or maintenance of relationships. CHR individuals also experience declines in social cognition (Allott et al., 2014; Pelletier et al., 2013), impairing the comprehension of social information and theory of mind necessary for successful social interaction. Identifying which symptoms or deficits are most relevant to social network size would allow for more targeted early interventions. However, the relationship of symptoms and cognition to social network size has not been previously examined. Finally, a longitudinal perspective would also help identify how symptom changes during developmental course relate to changes in social network size or composition. These gaps in the current literature limit our understanding of the contributors to social network size necessary to identify potential treatment targets for CHR individuals.
The current study examined social networks, as assessed by the Social Network Index (SNI), in a sample of both CHR individuals and non-psychiatrically diagnosed young adults and late adolescents (HC). Robustelli et al. (2017) described the quality and number of friendships to investigate loneliness in CHR adolescents at a single timepoint. This study compared a larger sample of CHR and HC groups in terms social network size, clinical/cognitive symptom contributions to social network size, and changes in social network size with symptoms over 1-year. We predicted that the CHR group would on average have smaller social networks. Expanding on earlier findings that were restricted to the friendships domain, all the individual subdimensions (i.e., close friends, relatives, classmates) were examined to identify categories that contributed to differences in social network size. Second, this study examined the unique associations of social anxiety, social cognition, social anhedonia, and paranoia to social network size. We expected these symptoms to be associated with smaller social networks. Additionally, the study compared the SNI to other measures of social support as a means of describing its potential for use in the psychosis-risk period. Finally, a longitudinal analysis examined the relationship between changes in attenuated psychosis symptoms and changes in social network composition over a one-year period. We anticipated that increased symptom severity would relate to greater reliance on family members and less contact with secondary sources such as friends, classmates, or coworkers.
Methods
Study Settings and Sample.
Both non-psychiatric healthy control (HC) participants and those at CHR for psychosis were recruited through email, Craigslist, and newspaper advertisements. To specifically target CHR individuals, additional recruitment occurred in collaboration with psychiatrists, school counselors, psychiatric hospitals, and community mental health centers. Advertising methods incorporated in-person presentations at community mental health events, phone calls, regular mailing lists, and bus advertisements in Boulder, Aurora, and Denver, Colorado. Our initial sample included 107 participants (53% female; HC=52, CHR=55) completed a baseline visit and 37% of the sample completed a follow-up appointment (CHR Group; N=18; 17 at approximately 12 months; 1 at 24 months post-baseline). Thirteen individuals were missing data necessary to calculate the Social Network Size scale resulting in 95 individuals (HC=49, CHR=46) being included in those group analyses. A subsample of the baseline datapoints (85/95) for these participants were included in an earlier analysis (Robustelli et al., 2017). Between the CHR participants who only participated at baseline and the CHR participants who completed two annual visits, there were no significant differences in age, sex, race, income, student status, or any of the primary parameters of interest (p’s>.11). Participants within the longitudinal CHR subsample were more often employed than the rest of the CHR subsample, χ2(1, 18)=11.19, p=.01. For more sample descriptions, see Tables and Supplemental Information (SI).
Clinical Assessment.
Trained clinicians administered the Structured Interview for Psychosis-Risk Syndromes (SIPS; Miller et al., 1999) at baseline and follow-up to identify CHR participants. Among the attenuated positive and negative symptom measures, the SIPS included paranoia and social anhedonia. Structured Interview for Axis-I DSM-IV Disorders (SCID; First, Spitzer, Gibbon, & Williams, 1995) identified formal psychosis spectrum diagnosis in CHR participants or the presence of any Axis-I disorder in the healthy control participants for exclusionary purposes. Trained clinical staff made all diagnostic decisions under the direct supervision of VAM. Doctoral students conducted the interviews with an interrater reliability criterion of Kappa 0.80. For inclusion and APS diagnosis see SI.
Social Network Index.
Social Network Index (SNI) assessed the size of a participant’s social network at baseline and the follow-up visit. The SNI included 12 self-report questions that assessed a participant’s involvement in close relationships among 12 categories such as spouses, relatives, friends, religious groups, coworkers, or other groups (e.g., social clubs, arts). In each category, subjects could indicate a maximum amount of “7 or more” close relationships resulting in a maximum possible score of 67 in total network size (SNI-size; Cohen, Doyle, Skoner, Rabin, & Gwaltney, 1997). Select items, including marital-like relationships and children, were not included in the social network size score if less than 5% of the sample endorsed them (Robustelli et al., 2017). This modified measure assessed participant involvement in 10 types of relationships, excluding marital status and children, to better reflect our adolescent and young adult sample.
Social Function, Symptom, and Cognition Scales.
At baseline, participants completed numerous social function, symptom, and cognition scales, including the Global Functioning Scale, the Social Interaction Anxiety Scale, and the Mayer-Salovey-Caruso Emotional Intelligence Test. Global Social Functioning Scale is a semi-structured interview that assesses individuals’ success and independence in both social and role domains (GFS; Cornblatt et al., 2007). Social Interaction Anxiety Scale (SIAS; Mattick & Clarke, 1998) is a self-report assessment of fears during general social interaction. Mayer-Salovey-Caruso Emotional Intelligence Test is a subtest of the MATRICS Consensus Cognitive Battery (MCCB; Nuechterlein et al., 2008) that assesses social cognition across several abilities, including identifying emotion through facial expressions, the cause of emotions, and emotional regulation. More information on these scales is available in the SI.
Analytical Strategy.
A t-test examined potential differences in age by groups and chi-square analyses examined potential group differences in sex, race, income range, student status, and employment. Nuisance covariates were selected if they were related to the predictive or outcome variables (Miller & Chapman, 2001). T-tests examined group differences (between CHR and HC groups) in composite social network size, as well as in each subdimension assessed by the SNI. A multiple regression examined the contributions of clinical and cognitive symptoms (paranoia, social anhedonia, social anxiety, social cognition) to social network size within the CHR group. The results reflected the unique contribution of symptoms to social network size beyond the variance accounted for by other symptoms as all predictors in a single model. This approach preserved power by reducing the total number of comparisons and is consistent with recommendations for a sample of this size (Harris, 1985; Van Voorhis & Morgan, 2007). Additional models describing individual regression analyses and collinearity between social symptoms are available in the SI (Hair, Anderson, Tatham, & Black, 1995; Vanhove, 2020). A separate correlational analysis related baseline social network size to baseline global functioning to assess the conceptual link between these two measures. In an exploratory analysis, non-parametric spearman’s correlations examined the association between participants’ change in social network size and change in reported SIPS symptoms over a one-year period. To account for different potential types of changes, both changes in composite SNI size and changes in specific subdimensions (e.g., family, friends, classmates) were examined. All analyses were conducted in Rv1.3.959 and model code is available in SI.
Results
Participants.
95 individuals (56.8% female; HC=49, CHR=46), and 37% of the sample (CHR group; N=18) completed a follow-up appointment (See SI). There were no significant group differences in sex, χ2(1,95)=2.29, race, χ2(1,95)=9.29, or age, p’s>.22. There was also no significant difference in total income or employment status (p’s>.65). The HC subsample was more often enrolled in education compared to the CHR group, χ2(1,95)=4.15, p=.04.
Group Differences in Social Network Size.
An independent samples t-test examined whether SNI-size differed across CHR and HC groups. There was a significant group difference in SNI-size, t(93)=3.30, p=.001, such that the CHR group had significantly smaller social networks compared to HC. In follow-up analyses, t-tests were also conducted to examine which SNI-size subdimension scores differed across the two groups. CHR individuals talked to fewer close friends compared to HC participants, t(93)=2.04, p=.04. Additionally, CHR individuals talked to fewer relatives compared to HC participants, t(93)=4.51, p<.001.
Baseline Symptoms to Social Network Size.
A simultaneous general linear regression model examined the unique contribution of paranoia, social anhedonia, social anxiety, and social cognition to total SNI-size. The omnibus analyses suggested a significant overall model fit, F(4,39)=3.52, p=.02. Social anxiety symptoms severity significantly predicted social network size, t=2.13, =−.12, partial-r=−.32, p=.04. Social cognition performance significantly predicted social network size, t=2.33, =.22, partial-r=.35, p=.03. Attenuated psychosis symptoms (paranoia and social anhedonia) did not significantly contribute to the model (p’s>.22, Figure 1).
Fig.1.
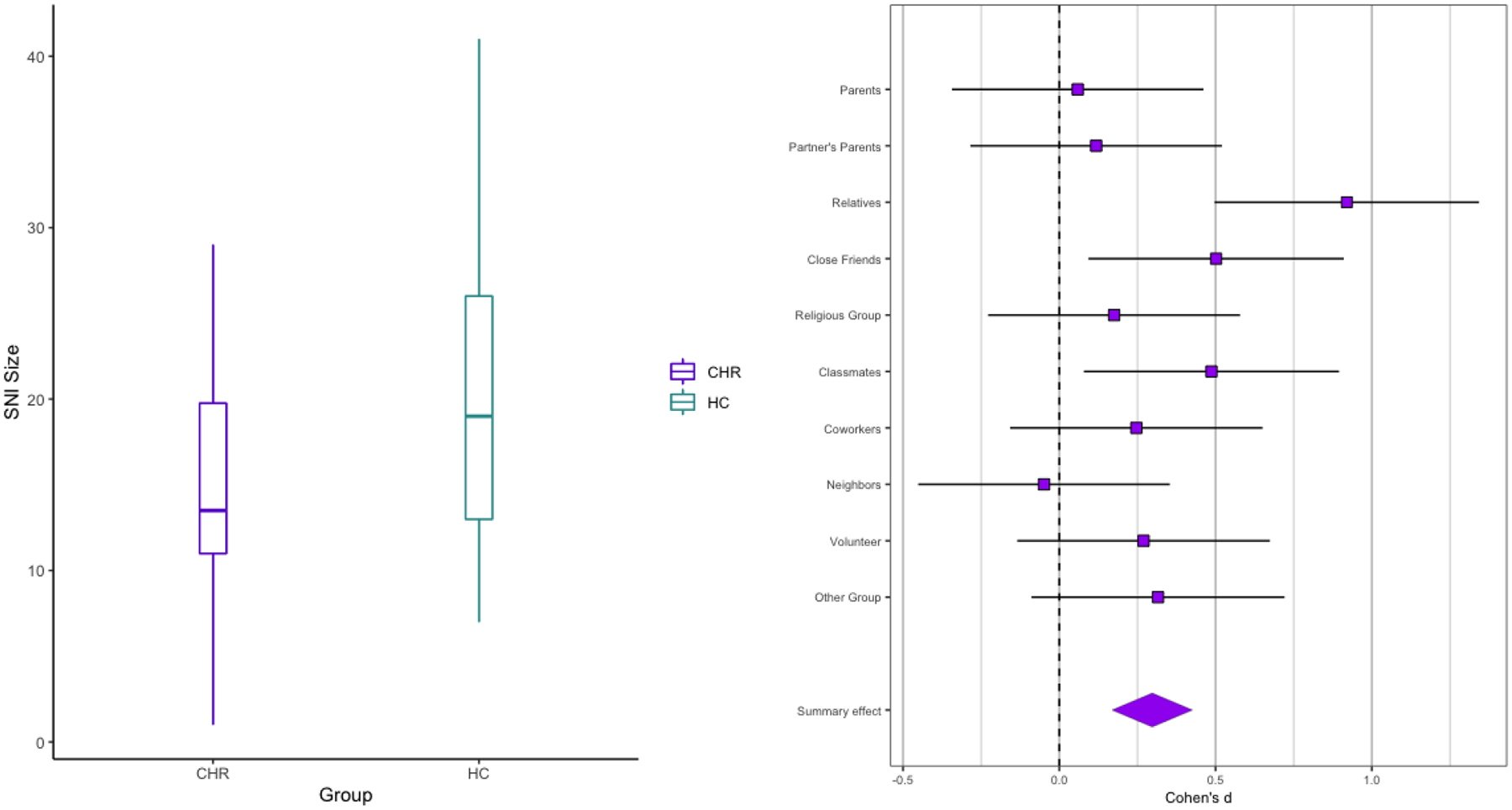
(A): Group Differences in Baseline Social Network Index Size Scores. (B): Cohen’s d and Standard Error of the Mean Values for Subdimensions of Social Network Index Assessment.
SNI – Social Network Index: Social Network Size
Validation of Social Network Size Against Global Functioning Scale.
In a general linear model, total SNI-size was related to Global Functioning Scale social, r(45)=.56, p<.001, and role, r(45)=.45 p=.002 and both subscales accounted for 32% of the variance in total SNI-size, F(2,45)=10.12, r=.29 p<.001.
Change in Social Network Size and Symptoms.
In a set of exploratory analyses, change in social network size was related to change in symptoms (follow up-baseline). There was no significant correlation between change in total SNI-size and either positive (r(17)=.25, p=.33) or negative symptoms (r(17)=−.13, p=.60). Among the subdomains, there was a significant positive relationship between change in positive symptoms and the family relationship, r(17)=.62, p=.01; increased positive symptoms related to increased number of relatives in close contact. The CHR group still had significantly smaller family SNI-size compared to their peers (See above for Baseline findings: Follow-Up: t(40)=2.77, p=.01; CHR: M=0.94, StD=1.06; HC: M=2.17, StD=1.63). The Other Social Network Category related to both positive (r(17)=.56, p=.02) and negative symptoms (r(17)=.54, p=.02), indicating that CHR individuals have larger non-traditional groupings as symptoms worsen. There was also a significant negative relationship between change in coworker interaction and negative symptoms (r(17)=−.58, p=.01), which showed a similar effect size relationship with positive symptoms, r(17)=−.37, p=.13), Figure 2. This demonstrated that increasing negative symptoms might coincide with declining coworker relationships.
Fig. 2.
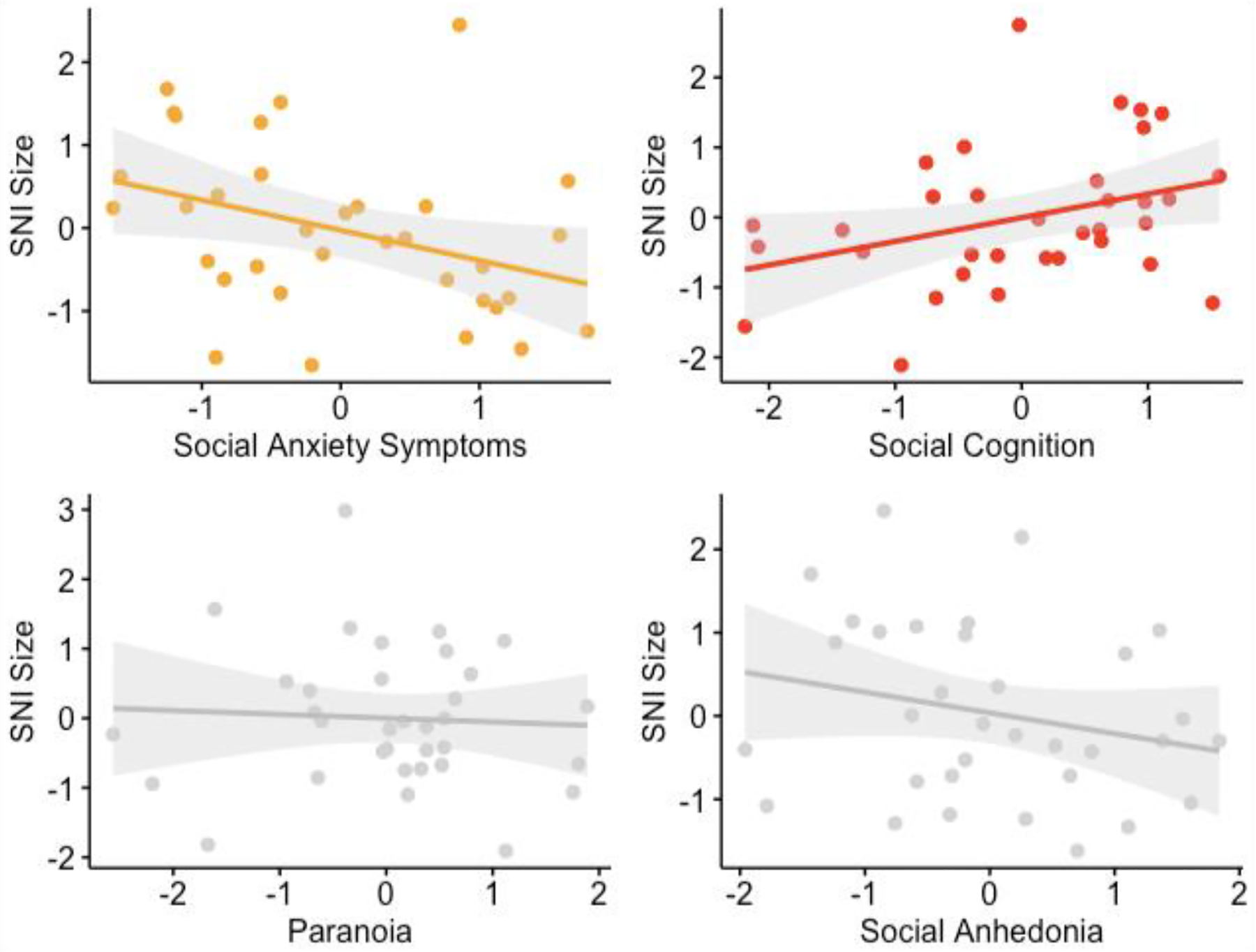
Model-Corrected Correlations Between Baseline Social Network Index and Baseline Social Symptoms (left to right, top to bottom): Social Anxiety, Social Cognition, Paranoia, and Social Anhedonia. The significant contributors to the model (social anxiety symptom and social cognition) appear at the top and non-significant contributors are in the bottom row.
SNI – Social Network Index: Social Network Size
Discussion
The CHR group had, on average, smaller social networks sizes compared to their peers. This paper expands on previous findings of fewer close friends, to demonstrate that CHR individuals also have reduced family SNI-size. Social network size uniquely associated with social anxiety and social cognition, but not social anhedonia and paranoia. SNI-size significantly related to the GFS subscales, a current gold standard in assessing social functioning in psychosis risk. However, these measures only accounted for around one-third of the variance in SNI-size (20.25% GFS-role; 31.36% GFS-social). SNI-size may provide novel insight into social relationships during the psychosis-risk period. Lastly, the exploratory analysis indicated changes in symptoms did not predict total SNI-size. Instead, symptoms related to both increases and decreases in SNI-size by specific domains. Increased positive symptoms related to increased contact with family and relatives but withdrawal from friends and coworkers. While the cause of these changes remains uncertain, they mark novel targets for future interventions to grow and maintain social support for CHR individuals.
Compared to their peers, the CHR group, on average, had smaller social networks across domains. Reduced SNI-size in CHR individuals is consistent with past findings of fewer friendships (Robustelli et al., 2017), but the current study extended these findings beyond friendship. Both friendships and relatives’ SNI subcategories were significantly smaller for CHR individuals compared to peers. Previous research has demonstrated that declines in social support are one of the most consistently reliable predictors of conversion to psychiatric disorders (Goldberg, Rollins, & Lehman, 2003); the current study suggested that both friendships and relatives are specific domains that may be useful treatment targets to improve sociality.
Social cognition and social anxiety at baseline contributed to baseline SNI-size over paranoia and social anhedonia symptoms. Previous analyses indicate that CHR individuals experience difficulties in social comprehension (Allott et al., 2014; Fusar-Poli et al., 2010; Green et al., 2012; Pelletier et al., 2013) and social anxiety (Kuhney et al., 2021; Rietdijk et al., 2013). The current findings demonstrated that these social features contribute to a smaller total SNI-size. Previous analyses demonstrated increased perceived social support related to decreased negative symptoms (Robustelli et al., 2017). In contrast, the current study found total SNI-size did not relate to social anhedonia nor paranoia when accounting for the variance related to social anxiety and social cognition. However, these findings are consistent with previous research suggesting that social deficits were not resolved following improvement in positive symptoms (Cornblatt et al., 2003). Further understanding of how social anxiety and social cognition relate to SNI-size over clinical course may inform potential treatment targets.
Global functioning related to total SNI-size, with moderate variance remaining. The current findings suggest that the SNI-size may contribute unique insight into the social deficits as well as provide information regarding specific domains. The GFS scales require a clinician to parse clinical symptoms from social deficits and aggregate across the frequency, quality, and the number of relationships. In contrast, the SNI provides complementary information with a detailed account of various social areas assessed as the participant’s number and frequency of social contacts.
The exploratory analyses suggested SNI-size and categories may be clinically informative on the nature of social network changes. Although these analyses should be interpreted with caution given the small sample size, findings suggest an increase in positive symptoms relates to an increase in the SNI-size among relatives and a shrinking of SNI-size in coworkers in a time where young adults may typically expand their networks. Engaging with social networks increased in frequency in the other less traditional social areas (e.g., extracurricular clubs), which related to worsening in positive and negative symptoms. Notably, despite the increases in relationships with relatives and other groups as positive symptoms progress, the CHR participants still maintained significantly fewer relationships than their non-clinical peers. It is possible that as symptoms intensify, relatives provide increased support and more regular contact. Alternatively, the relatives could be a source of stress, exacerbating symptoms through expressed emotion (Carol & Mittal, 2015; Miklowitz et al., 2014; O’Brien et al., 2014). In either case, these domain specific social relationships could be a target for expressed emotion interventions.
Although this study presents compelling results, there are important limitations to consider. The baseline CHR sample size is comparable to those of other longitudinal studies (35–50 individuals; Allott et al., 2014; Green et al., 2012; Mittal et al., 2011; Niendam et al., 2007). Yet future work would benefit from the increased power of larger samples. Follow-up analyses were conducted on smaller sample sizes (N=18) due to attrition, which is common in many longitudinal studies. CHR individuals who withdrew from the study did not significantly differ from the CHR group in the longitudinal subsample across many demographic factors except that they were more often employed. Future studies would benefit from a more robust longitudinal sample. Additionally, the CHR sample was receiving diverse care within the community that was not standardized, and it is unknown if this impacted the findings. Future analyses should incorporate qualitative assessments to measure participants’ satisfaction with social relationships and perceived support. Lastly, the current study depended on clinical interviews and self-report; future studies could benefit from including more direct behavioral measures of social interaction (e.g., social media activity).
Supplementary Material
Table 1.
Demographic Metrics by Group
| CHR (N=46) |
HC (N=49) |
||
|---|---|---|---|
| Variables | Mean (StD) | Mean (StD) | Group Difference |
| Age at Baseline (years) | 18.35 (1.84) | 18.84 (2.02) | NS |
| Sex (% female) | 47.8% | 65.3% | NS |
| Education (% student) | 80.4% | 95.9% | CHR < HC* |
| Employment (% employed) | 41.3% | 44.9% | NS |
| Social Network Size | 14.54 (6.64) | 19.76 (8.57) | CHR < HC** |
| Close friends | 2.98 (2.21) | 3.86 (1.97) | CHR < HC* |
| Relatives | 0.82 (1.04) | 2.06 (1.59) | CHR < HC *** |
| Classmates | 3.87 (3.08) | 5.02 (2.82) | NS |
| Coworkers | 1.89 (2.52) | 2.45 (2.75) | NS |
| Neighbors | 1.11 (1.84) | 1.04 (1.41) | NS |
| Parents | 1.70 (0.47) | 1.73 (0.49) | NS |
| Partners’ Parent(s) | 0.17 (0.53) | 0.22 (0.62) | NS |
| Religious Group Members | 0.43 (1.47) | 0.71 (1.88) | NS |
| Volunteer Group Members | 0.35 (0.97) | 0.71 (1.63) | NS |
| Other Group Members | 0.87 (2.04) | 1.59 (2.86) | NS |
| Social Anxiety | 28.90 (17.5) | 10.68 (9.38) | CHR > HC*** |
| Social Cognition (t score) | 41.38 (10.1) | 46.53 (9.35) | CHR < HC* |
| Paranoia | 3.32 (1.17) | 0.10 (0.37) | CHR > HC*** |
| Social Anhedonia | 1.91 (1.84) | 0.06 (0.24) | CHR > HC*** |
| Social Role Functioning | 6.76 (1.68) | 8.59 (0.70) | CHR < HC*** |
p < 0.05,
p < 0.01,
p < 0.001;
Clinical High Risk for Psychosis (CHR), Non-psychiatrically diagnosed individual (HC); Social network size measured through the Social Network Index (Cohen, Doyle, Skoner, Rabin, & Gwaltney, 1997), a 12 item questionnaire with composite scores ranging from 0 to 67, and subcategory scores ranging from 0 to 7; Social anxiety measured through Social Interaction Anxiety Scale (Mattick & Clarke, 1998), with scores ranging from 0 (no social anxiety) to 128 (highest social anxiety); Social cognition t scores obtained from the Mayer-Salovey-Caruso Emotional Intelligence Test (Nuechterlein et al., 2008), with raw scores ranging from 69 to 120; paranoia and social anhedonia measures through the Structured Interview for Prodromal Symptoms (First, Spitzer, Gibbon, & Williams, 1995), with scores ranging from 0 (absent) to 6 (severe and psychotic/extreme).
Acknowledgments
This work was supported by the National Institutes of Mental Health (Grant R01s. MH094650, MH112545-01, MH103231, MH112545, MH094650, R21/R33MH103231; T32MH126368 to KSFD). We have no conflicts to disclose. The study resulting in this publication was assisted by a grant from the Baker Program in Undergraduate Research, which is administered by Northwestern University’s Weinberg College of Arts and Sciences. However, the conclusions, opinions, and other statements in this publication are the authors and not necessarily those of the sponsoring institution.
Data Availability Statement
The de-identified data will be made available upon request for purposes consistent for the research described in the original consent, and model/analyses scripts are fully available in the supplemental materials.
References
- Addington J, Penn D, Woods SW, Addington D, & Perkins DO (2008). Social functioning in individuals at clinical high risk for psychosis. Schizophrenia Research, 99(1), 119–124. 10.1016/j.schres.2007.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allott KA, Schäfer MR, Thompson A, Nelson B, Bendall S, Bartholomeusz CF, … Amminger GP (2014). Emotion recognition as a predictor of transition to a psychotic disorder in ultra-high risk participants. Schizophrenia Research, 153(1), 25–31. 10.1016/j.schres.2014.01.037 [DOI] [PubMed] [Google Scholar]
- Ballon JS, Kaur T, Marks II, & Cadenhead KS (2007). Social functioning in young people at risk for schizophrenia. Psychiatry Research, 151(1), 29–35. 10.1016/j.psychres.2006.10.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanchard JJ, Mueser KT, & Bellack AS (1998). Anhedonia, Positive and Negative Affect, and Social Functioning in Schizophrenia. Schizophrenia Bulletin, 24(3), 413–424. 10.1093/oxfordjournals.schbul.a033336 [DOI] [PubMed] [Google Scholar]
- Brucato G, Masucci MD, Arndt LY, Ben-David S, Colibazzi T, Corcoran CM, … Girgis RR (2017). Baseline demographics, clinical features and predictors of conversion among 200 individuals in a longitudinal prospective psychosis-risk cohort. Psychological Medicine, 47(11), 1923–1935. 10.1017/S0033291717000319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carol EE, & Mittal VA (2015). Resting cortisol level, self-concept, and putative familial environment in adolescents at ultra high-risk for psychotic disorders. Psychoneuroendocrinology, 57, 26–36. 10.1016/j.psyneuen.2015.03.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Doyle WJ, Skoner DP, Rabin BS, & Gwaltney JM (1997). Social Ties and Susceptibility to the Common Cold. JAMA, 277(24), 1940–1944. 10.1001/jama.1997.03540480040036 [DOI] [PubMed] [Google Scholar]
- Cornblatt BA, Auther AM, Niendam T, Smith CW, Zinberg J, Bearden CE, & Cannon TD (2007). Preliminary Findings for Two New Measures of Social and Role Functioning in the Prodromal Phase of Schizophrenia. Schizophrenia Bulletin, 33(3), 688–702. 10.1093/schbul/sbm029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornblatt BA, Carrión RE, Addington J, Seidman L, Walker EF, Cannon TD, … Lencz T (2012). Risk Factors for Psychosis: Impaired Social and Role Functioning. Schizophrenia Bulletin, 38(6), 1247–1257. 10.1093/schbul/sbr136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornblatt BA, Lencz T, Smith CW, Correll CU, Auther AM, & Nakayama E (2003). The Schizophrenia Prodrome Revisited: A Neurodevelopmental Perspective. Schizophrenia Bulletin, 29(4), 633–651. 10.1093/oxfordjournals.schbul.a007036 [DOI] [PubMed] [Google Scholar]
- Erickson DH, Beiser M, Iacono WG, Fleming JA, & Lin T (1989). The role of social relationships in the course of first-episode schizophrenia and affective psychosis. The American Journal of Psychiatry, 146(11), 1456–1461. 10.1176/ajp.146.11.1456 [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, & Williams JBW (1995). The Structured Clinical Interview for DSM-III-R Personality Disorders (SCID-II). Part I: Description. Journal of Personality Disorders, 9(2), 83–91. 10.1521/pedi.1995.9.2.83 [DOI] [Google Scholar]
- Fusar-Poli P, Byrne M, Valmaggia L, Day F, Tabraham P, Johns L, & McGuire P (2010). Social dysfunction predicts two years clinical outcome in people at ultra high risk for psychosis. Journal of Psychiatric Research, 44(5), 294–301. 10.1016/j.jpsychires.2009.08.016 [DOI] [PubMed] [Google Scholar]
- Gayer-Anderson C, & Morgan C (2013). Social networks, support and early psychosis: A systematic review. Epidemiology and Psychiatric Sciences, 22(2), 131–146. 10.1017/S2045796012000406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee DG, & Cannon TD (2011). Prediction of conversion to psychosis: Review and future directions. Revista Brasileira de Psiquiatria, 33(suppl 2), s129–s142. 10.1590/S1516-44462011000600002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg RW, Rollins AL, & Lehman AF (2003). Social network correlates among people with psychiatric disabilities. Psychiatric Rehabilitation Journal, 26(4), 393–402. 10.2975/26.2003.393.402 [DOI] [PubMed] [Google Scholar]
- Green MF, Bearden CE, Cannon TD, Fiske AP, Hellemann GS, Horan WP, … Nuechterlein KH (2012). Social Cognition in Schizophrenia, Part 1: Performance Across Phase of Illness. Schizophrenia Bulletin, 38(4), 854–864. 10.1093/schbul/sbq171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hair JF, Anderson RE, Tatham RL, & Black WC (1995). Multivariate data analysis (3rd ed.). New York: Macmillan Publishing Company. [Google Scholar]
- Harris RJ (1985). A primer of multivariate statistics (2nd ed.). New York: Academic Press. [Google Scholar]
- Horan WP, Subotnik KL, Snyder KS, & Nuechterlein KH (2006). Do Recent-Onset Schizophrenia Patients Experience a “Social Network Crisis”? Psychiatry: Interpersonal and Biological Processes, 69(2), 115–129. 10.1521/psyc.2006.69.2.115 [DOI] [PubMed] [Google Scholar]
- Kuhney FS, Damme KSF, Pelletier-Baldelli A, Chun C, Ellman LM, Schiffman J, & Mittal VA (2021). Prevalence and Functional Consequences of Social Anxiety in Individuals at Clinical High-Risk for Psychosis: Perspective from a Community Sample Comparison. Schizophrenia Bulletin Open, sgab025. 10.1093/schizbullopen/sgab025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lencz T, Smith CW, Auther A, Correll CU, & Cornblatt B (2004). Nonspecific and attenuated negative symptoms in patients at clinical high-risk for schizophrenia. Schizophrenia Research, 68(1), 37–48. 10.1016/S0920-9964(03)00214-7 [DOI] [PubMed] [Google Scholar]
- Macdonald EM, Hayes RL, & Baglioni AJ (2000). The quantity and quality of the social networks of young people with early psychosis compared with closely matched controls. Schizophrenia Research, 46(1), 25–30. 10.1016/S0920-9964(00)00024-4 [DOI] [PubMed] [Google Scholar]
- Mattick RP, & Clarke JC (1998). Development and validation of measures of social phobia scrutiny fear and social interaction anxiety11Editor’s note: This article was written before the development of some contemporary measures of social phobia, such as the Social Phobia and Anxiety Inventory (Turner et al., 1989). We have invited this article for publication because of the growing interest in the scales described therein. S.T. Behaviour Research and Therapy, 36(4), 455–470. 10.1016/S0005-7967(97)10031-6 [DOI] [PubMed] [Google Scholar]
- Miklowitz DJ, O’Brien MP, Schlosser DA, Addington J, Candan KA, Marshall C, … Cannon TD (2014). Family-Focused Treatment for Adolescents and Young Adults at High Risk for Psychosis: Results of a Randomized Trial. Journal of the American Academy of Child & Adolescent Psychiatry, 53(8), 848–858. 10.1016/j.jaac.2014.04.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GA, & Chapman JP (2001). Misunderstanding analysis of covariance. Journal of Abnormal Psychology, 110(1), 40–48. 10.1037/0021-843X.110.1.40 [DOI] [PubMed] [Google Scholar]
- Miller TJ, McGlashan TH, Woods SW, Stein K, Driesen N, Corcoran CM, … Davidson L (1999). Symptom Assessment in Schizophrenic Prodromal States. Psychiatric Quarterly, 70(4), 273–287. 10.1023/A:1022034115078 [DOI] [PubMed] [Google Scholar]
- Mittal VA, Jalbrzikowski M, Daley M, Roman C, Bearden CE, & Cannon TD (2011). Abnormal movements are associated with poor psychosocial functioning in adolescents at high risk for psychosis. Schizophrenia Research, 130(1), 164–169. 10.1016/j.schres.2011.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niendam TA, Bearden CE, Zinberg J, Johnson JK, O’Brien M, & Cannon TD (2007). The Course of Neurocognition and Social Functioning in Individuals at Ultra High Risk for Psychosis. Schizophrenia Bulletin, 33(3), 772–781. 10.1093/schbul/sbm020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nuechterlein KH, Green MF, Kern RS, Baade LE, Barch DM, Cohen JD, … Marder SR (2008). The MATRICS Consensus Cognitive Battery, part 1: Test selection, reliability, and validity. The American Journal of Psychiatry, 165(2), 203–213. 10.1176/appi.ajp.2007.07010042 [DOI] [PubMed] [Google Scholar]
- O’Brien MP, Miklowitz DJ, Candan KA, Marshall C, Domingues I, Walsh BC, … Cannon TD (2014). A randomized trial of family focused therapy with populations at clinical high risk for psychosis: Effects on interactional behavior. Journal of Consulting and Clinical Psychology, 82(1), 90–101. 10.1037/a0034667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelletier AL, Dean DJ, Lunsford-Avery JR, Smith AK, Orr JM, Gupta T, … Mittal VA (2013). Emotion recognition and social/role dysfunction in non-clinical psychosis. Schizophrenia Research, 143(1), 70–73. 10.1016/j.schres.2012.10.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pruessner M, Iyer SN, Faridi K, Joober R, & Malla AK (2011). Stress and protective factors in individuals at ultra-high risk for psychosis, first episode psychosis and healthy controls. Schizophrenia Research, 129(1), 29–35. 10.1016/j.schres.2011.03.022 [DOI] [PubMed] [Google Scholar]
- Rietdijk J, Ising HK, Dragt S, Klaassen R, Nieman D, Wunderink L, … van der Gaag M (2013). Depression and social anxiety in help-seeking patients with an ultra-high risk for developing psychosis. Psychiatry Research, 209(3), 309–313. 10.1016/j.psychres.2013.01.012 [DOI] [PubMed] [Google Scholar]
- Robustelli BL, Newberry RE, Whisman MA, & Mittal VA (2017). Social relationships in young adults at ultra high risk for psychosis. Psychiatry Research, 247, 345–351. 10.1016/j.psychres.2016.12.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Voorhis CRW, & Morgan BL (2007). Understanding Power and Rules of Thumb for Determining Sample Sizes. Tutorials in Quantitative Methods for Psychology, 3(2), 43–50. 10.20982/tqmp.03.2.p043 [DOI] [Google Scholar]
- Vanhove J (2020). Collinearity isn’t a disease that needs curing [Preprint]. PsyArXiv. 10.31234/osf.io/mv2wx [DOI] [Google Scholar]
- Wrzus C, Hänel M, Wagner J, & Neyer FJ (2013). Social network changes and life events across the life span: A meta-analysis. Psychological Bulletin, 139(1), 53–80. 10.1037/a0028601 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The de-identified data will be made available upon request for purposes consistent for the research described in the original consent, and model/analyses scripts are fully available in the supplemental materials.


