Abstract
Background:
Lumbar multifidus muscle provides stability to the spine. The present study aimed to evaluate the reliability of ultrasound findings in patients with lumbar multifidus myofascial pain syndrome (MPS).
Methods:
A total of 24 cases (7 females, 17 males, mean age: 40.13± 5.69, BMI: 26.48±4.96) with multifidus MPS were assessed. The variables were muscle thickness in rest and contraction, thickness changes, and cross-sectional area (CSA) in rest and contraction. Two examiners performed the test and retest sessions.
Results:
The active trigger points of lumbar multifidus on the right and left side of the cases were 45.8 % and 54.2%, respectively. The intraclass correlation coefficient (ICC) values for muscle thickness and thickness changes showed moderate to very high reliability for both within and between intra-examiner measurements. (ICC, 1st examiner: 0.78-0.96; ICC, 2nd examiner: 0.86-0.95). In addition, the ICC values of within and between-session intra-examiner for CSA were high. (ICC, 1st examiner: 0.83-0.88; ICC, 2nd examiner: 0.84-0.89). The ICC and standard error of measurement (SEM) of inter-examiner reliability ranged between 0.75 to 0.93 and 0.19 to 0.88 for multifidus muscle thickness and thickness changes. The ICC and SEM of inter-examiner reliability ranged between 0.78 to 0.88 and 0.33 to 0.90 for CSA of the multifidus muscle.
Conclusion:
The within and between-session reliability of multifidus thickness, thickness changes, and CSA was moderate to very high in patients with lumbar MPS when taken by two examiners. Furthermore, the inter-examiner reliability of these sonographic findings was high.
Key Words: Low back pain, Myofascial pain syndrome, Multifidus thickness, Ultrasound, Trigger points
Introduction
Low back pain (LBP) is one of the most common musculoskeletal disorders that many experiences at least once in their lifetime.1,2 The prevalence of chronic LBP is about 27.18% in Iranian people.3 Lumbar disc protrusion, radiculopathy, trauma, and overuse are the leading causes of LBP.4 Myofascial pain syndrome (MPS) is also one of the main causes of back pain.5,6 An important feature of MPS is the presence of trigger points.7 A trigger point is a tender point within taut bands of the muscles that become painful due to pressure, traction, contraction, and loading.8 Trigger points may produce local or referred pain divided into active and latent types.9 Active trigger points elicit local and referral pain, so the patient reports the same familiar and permanent pain. In the case of latent trigger points, the localized and referred pain is unfamiliar to the patient and only increases with the palpation by the examiner.10 Active trigger points are the main cause of pain in 85% of patients with musculoskeletal pain.11 Meanwhile, according to recent studies, lumbar multifidus with a prevalence of 43% is one of the most muscles with trigger points in patients with chronic LBP.6
In recent years, the use of ultrasound (US) to record skeletal muscle thickness and cross-sectional area (CSA) has become a common practice.12 A point that makes clinical decisions is not only based on subjective information, but also on Obtaining objective data from the patients.13 The US has been used as a reliable and valid tool in musculoskeletal pain such as neck, shoulder, and knee pain.14-16 This tool has been widely used for back pain, and its reproducibility and validity have been studied.17,18 The US is a readily available imaging modality that plays a major role in diagnosing, disease monitoring, and intervening. The use of the US is expanding because of being a noninvasive, portable, and real-time data-capturing.19-21
The validity of the US in assessing muscle morphology has been studied by comparing the US with MRI, which is the gold standard of musculoskeletal imaging.18,22 Moreover, the validity of the US in assessing the thickness and activity of the lumbar multifidus muscle (correlation coefficient 0.51 to 0.61) has been studied by comparing it with electromyography and the gold standard for determining muscle activity.23
Despite extensive studies on the use of US for musculoskeletal disorders, this instrument has received less attention in the field of myofascial pain syndrome(MPS).20 Measuring thickness and muscle activity in patients with LBP due to MPS has been considered in recent years.20 Previous studies have not reported an increase or decrease in thickness and CSA. Recently, Ezzati et al. showed that muscle thickness in rest, fair, and normal contractions are the same between healthy people and MPS subjects. In the fair contraction, the patient lifts the head and neck opposite to gravity and looks up and in a normal contraction, the patient moves the head and neck in the range upward opposite to the maximum resistance. Muscle activity is also less in MPS patients than in healthy people.24 It should be noted that this study was performed on subjects with neck pain due to upper trapezius MPS.
Measurement of reliability is clinically important in patients with MPS. The location of the probe, the image of the trigger points, the measurement of muscle thickness, and CSA on separate days reveal the importance of US reliability which a clinician may consider for diagnosis or treatment methods in patients with MPS.25 To assess muscle thickness and CSA in different conditions, it is essential to ensure that the observed differences after treatment or between groups are related to actual changes rather than the random error in the measurement methods.26 Additionally, the determination of minimal detectable changes (MDCs) allows researchers and clinicians to evaluate actual alterations following treatment.27 Intra-examiner reliability is a value of the consistency in ratings given by the same person across different times, and inter-examiner reliability is the degree of agreement among examiners. However, reliability is dependent on examiners, subjects, and test conditions.28-30 Nevertheless, the intra-examiner and inter-examiner reliability of multifidus muscle US findings in patients with LBP due to MPS have not been studied.
The objectives of the present study were: 1) to evaluate within and between session intra-examiner reliability of US findings for assessment of lumbar multifidi thickness and CSA in rest and contracted states, 2) to evaluate inter-examiner reliability of US findings for assessment of lumbar multifidi thickness and CSA in rest and contracted states 3) to determine the standard error of measurement values (SEMs) and MDCs for multifidi thickness and CSA in patients with MPS.
Materials and Methods
Participants
A simplified guide by Bujang et al. was used to calculate the sample size needed for this study.31 According to the ICC value of 0.4, an alpha level of 0.05, and a power of 0.9, the sample size was 23 cases. Patients with chronic LBP due to multifidus MPS were eligible and met inclusion criteria if found to have active trigger points. An expert physiotherapist performed a screening examination to exclude other causes of LBP. The inclusion criteria were at least one active trigger point in multifidus muscle, age between 20 and 40 years, and pain duration ≥3 months. The exclusion criteria were: patients who have fibromyalgia based on the criteria of the American faculty of rheumatology which were: 1) widespread pain index≥ 7 and symptom severity score≥ 5. 2) generalized pain: pain in 4/5 regions, and 3) symptoms ≥3 months,32 rheumatoid diseases, degenerative diseases, fracture, dislocations, those with a history of lumbar surgery, patients who have cancer, individuals with psychosocial disorders who would be assessed using the Persian version of the stress- anxiety- depression questionnaire (DASS-21) due to the adverse effects of these disorders on muscle activity.33,34
Trigger Point Examination
The spinous process of L4 vertebrae was determined as a landmark in finding and palpating the lumbar multifidus muscle. At first, the patient was lying on his side. After seeing the spinous process, the examiner moved his finger about 1 cm and palpated medially and distally. The taut band, tenderness, and pain recognition were the three main clinical criteria for diagnosing multifidus muscle myofascial pain syndrome.9 One of the important steps in evaluating patients was to find the lumbar spinous process, which was done by palpating the upper point of the iliac crest so that the highest point of the iliac crest was equal to the space between the fourth and fifth disc. The spinous process of the upper vertebra was marked as L4 and the lower vertebra as L5.35
Lumbar Multifidus Muscle Thickness Measurement by Ultrasonography
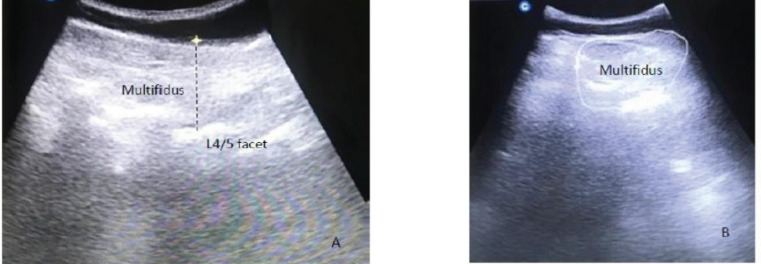
A diagnostic ultrasound (Chison, China) with a curved probe and 5-14 MHz frequency was used. The patient lies on the examination bed in a prone position to evaluate the multifidus muscle. To reduce lumbar lordosis, a small pillow was placed under the patient’s abdomen, and the patient was asked to relax his paraspinal muscles. According to the method mentioned above, the spinous process of the fifth lumbar vertebra is palpated and marked. The US probe was placed longitudinally in the middle to confirm the spinous process of the fifth vertebra. At first, a bilateral image of the lumbar multifidus muscle was observed, and then the measurement in the affected multifidus muscle was performed separately. The distance between the apex of the facet joint to the plane between thoracolumbar fascia and subcutaneous fat was recorded as longitudinal multifidus muscle thickness [Figure 1]. To measure the thickness of the muscle in the contraction position, the subject raises the opposite arm, which creates a moderate contraction in the multifidus muscle.36 For this purpose, the patient lifts a weight of 0.5 to 1.5 kg, adjusted based on the patient’s weight, about 5 cm from the bed by the opposite arm. In this case, the shoulder is 120 degrees in abduction, and the elbow is 90 degrees in flexion. The patient was asked to hold his breath at the end of the exhale to minimize the effects of breathing on muscle thickness and maintain this state for 3 seconds. All steps of this evaluation were explained to the patient once before performing US. 43, 70
Figure 1.
Ultrasonography Imaging: Image of the L4/5 multifidus thickness(A) and cross-sectional area(B) at rest
Lumbar Multifidus Muscle Cross-Sectional Area Measurement by Ultrasonography
To measure the CSA of the multifidus muscle, the probe was placed transversely in the target area: Muscle margins (inner margin: spinous process, lower margin: lamina, upper margin: thoracolumbar fascia, and outer margin: erector spine muscle) were drawn on the affected side [Figure 1]. Each measurement was performed three times, and its average will be used for statistical tests. Two examiners performed three trials during each session, and the retest session was 6 to 8 days later.
Statistical analysis
The three trials of muscle thickness and CSA measurement were averaged for within and betweensession intra- and inter-examiner reliability.
The two-way random intra-class correlation coefficient model was calculated with 95% confidence intervals (CIs) to report relative reliability. We selected a two-way random design, in which both the examiners and subjects were randomly assigned from a larger set. ICC 2,1 were used for within-session reliability because each examiner measured each subject, and the reliability was measured by a single measurement. Furthermore, ICC 2,3 were used for between-session and inter-examiner reliability because each examiner measured each subject, and the reliability was measured by taking an average of three measurements.37 The interpretations of reliability coefficients were based on Munro’s classification: 0.00-0.25-little, 0.26-0.49-low correlation, 0.50-0.69- moderate correlation, 0.70-0.89- high correlation, and 0.90-1.00 very high correlation.38
The SEM was computed to estimate measurement error and absolute reliability. This item was calculated as SEM=SD*SQRT (1-ICC), where “SD” was the standard deviation of the measurements.39
The MDC was used to compute the clinically significant changes between the two measurements. The MDC was analyzed as 95% CI of SEM (1.96 SEM) of the measures.39
Results
A total of 24 participants (7 females, 17 males, mean age: 40.13± 5.69, BMI: 26.48±4.96) were assessed in this study. The active trigger points on the right and left side of the patients were 45.8 % and 54.2%, respectively. [Table 1].
Table 1.
Demographic data for patients with lumbar multifidus myofascial pain syndrome
| Variables | Mean ± SD |
|---|---|
| Age(years) | [40.13] [5.69] |
| Weight(kg) | [74.81] [14.09] |
| Height(cm) | [168.33] [9.29] |
| Body Mass Index | [26.48] [4.96] |
| Pain duration(m) | [10.71] [8.54] |
| Gender Female Male |
[7] [29.2%] [17] [70.8%] |
| Side of pain Right Left |
[11] [45.8%] [13] [54.2%] |
SD, standard deviation
The average thickness and CSA of multifidus muscle in rest and contraction position in test and retest sessions are shown in table 2. In addition, the within and between-session intra-examiner reliability of thickness and CSA of multifidus muscle in rest and contraction positions are indicated in Table 2.
Table 2.
Within and between session reliability of the thickness and cross-sectional area in subjects with multifidus myofascial pain syndrome
| Examiner | Sonographic measures | Within –session intra-examiner | Between session intra-examiner | |||||
|---|---|---|---|---|---|---|---|---|
|
(Mean) (SD),
test |
ICC, Test |
(Mean) (SD),
Re-test |
ICC,
Re-test |
ICC | SEM | MDC | ||
| 1st Examiner | Thickness(rest,cm) | [3.51] [0.52] | [0.93] | [3.55] [0.63] | [0.96] | [0.88] [0.75,0.94] | [0.16] | [0.32] |
| Thickness(contraction,cm) | [3.77] [0.59] | [0.89] | [3.66] [0.61] | [0.92] | [0.78] [0.56,0.90] | [0.21] | [0.41] | |
| Thickness change% | [7.98] [10.31] | [0.87] | [7.45] [77.82] | [0.87] | [0.84] [0.80,0.88] | [0.58] | [1.16] | |
| CSA (rest, cm2) | [15.36] [1.34] | [0.84] | [16.16] [1.41] | [0.88] | [0.86] [0.84,0.88] | [0.32] | [0.64] | |
| CSA (contraction, cm2) | [16.32] [1.83] | [0.83] | [16.30] [1.96] | [0.87] | [0.88] [0.87,0.89] | [0.67] | [1.33] | |
| 2nd Examiner | Thickness(rest,cm) | [3.58] [0.62] | [0.94] | [3.61] [0.42] | [0.95] | [0.86] [0.83,0.88] | [0.22] | [0.44] |
| Thickness(contraction,cm) | [3.73] [0.68] | [0.92] | [3.74] [0.67] | [0.93] | [0.90] [0.85,0.93] | [0.25] | [0.61] | |
| Thickness change% | [4.56] [9.63] | [0.90] | [4.89] [7.87] | [0.88] | [0.88] [0.85,0.90] | [0.72] | [1.44] | |
| CSA (rest, cm2) | [15.17] [1.32] | [0.88] | [15.21] [1.27] | [0.90] | [0.87] [0.83,0.91] | [0.29] | [0.58] | |
| CSA (contraction, cm2) | [16.36] [2.05] | [0.88] | [17.32] [2.09] | [0.84] | [0.87] [0.83,0.91] | [0.71] | [1.42] | |
SD, Standard Deviation; ICC, Intra-class Correlation Coefficients; SEM, Standard Error of Measurement; MDC, Minimal Detectable Change; CSA, Cross-Sectional Area
The within-session intra-examiner reliability of all variables in different conditions was high to very high (ICC range: 0.83-0.98). The ICC values for muscle thickness in rest, contraction states, and thickness changes varied between 0.87 and 0.96. Furthermore, these values for CSA in rest and contraction states were 0.83-0.88.
The between-session intra-examiner reliability of all variables in different conditions was moderate to high (ICC range: 0.78-0.90). The ICC values for muscle thickness in rest, contraction states, and thickness changes varied between 0.78 and 0.90. Moreover, these values for CSA in rest and contraction states were 0.86-0.88. The SEM for between-session intra-examiner reliability was 0.16-0.72, and the MDC was 0.32-1.44 for all conditions.
Table 3 shows the ICC, SEM, and MDC values for inter-examiner reliability. The inter-examiner reliability of all variables in different conditions was high to very high (ICC range: 0.75-0.93). The ICC values for muscle thickness in rest, contraction states, and thickness changes were between 0.75 and 0.93. Also, The SEM for inter-examiner reliability was 0.19-0.88 for muscle thickness and 0.33-0.90 for CSA. Finally, the MDC was 0.44-1.80 for all conditions.
Table 3.
Inter-examiner reliability of the thickness and cross-sectional area in subjects with multifidus myofascial pain syndrome
| Reliability | Measures | ICC | SEM | MDC |
|---|---|---|---|---|
| Inter-examiner (test session) | Thickness (rest,cm) |
[0.91] | [0.58] | [1.15] |
| Thickness (contraction,cm) |
[0.89] | [0.22] | [0.44] | |
| Thickness change% | [0.86] | [0.61] | [1.22] | |
| CSA (rest, cm2) | [0.84] | [0.34] | [0.68] | |
| CSA (contraction, cm2) |
[0.81] | [0.88] | [1.76] | |
| Inter-examiner (re-test session) |
Thickness (rest,cm) |
[0.93] | [0.62] | [1.34] |
| Thickness (contraction,cm) |
[0.89] | [0.31] | [0.62] | |
| Thickness change% | [0.88] | [0.76] | [1.52] | |
| CSA (rest, cm2) | [0.81] | [0.44] | [0.88] | |
| CSA (contraction, cm2) |
[0.78] | [0.90] | [1.80] | |
| Inter-examiner (test and re-test sessions) |
Thickness(rest,cm) | [0.90] | [0.19] | [0.38] |
| Thickness (contraction,cm) |
[0.84] | [0.37] | [0.74] | |
| Thickness change% | [0.75] | [0.88] | [1.76] | |
| CSA (rest, cm2) | [0.88] | [0.33] | [0.66] | |
| CSA (contraction, cm2) |
[0.81] | [0.77] | [1.54] |
ICC, Intra-class Correlation Coefficients; SEM, Standard Error of Measurement; MDC, Minimal Detectable Change; CSA, Cross-Sectional Area
Discussion
The present study revealed moderate to very high within and between-session intra-examiner reliability for lumbar multifidus thickness and cross-sectional area in patients with MPS. Also, the inter-examiner reliability of the mentioned variables was high to very high.
US plays a more outstanding role in evaluating the functional activity of muscles than MRI and CT scans.40 MPS is a non-neurological disorder that alters muscle function. To our knowledge, there was no study to evaluate the reliability of multifidus muscle function in low back patients due to MPS.13
Previous studies showed high reliability of multifidus thickness and CSA in the US in subjects with LBP.26, 41-44 Skeie et al. (2015) investigated the reliability of the US in measuring multifidus muscles. For this purpose, two experienced examiners performed US measurements on 30 individuals with and without LBP. Measurements included the thickness of the lumbar multifidus muscle at rest, during contraction, on consecutive days, and before and after walking. The results showed that the reliability of contraction was high among the examiners and was lower in the maximum contraction state than in the minimum contraction.42
An objective diagnostic tool is one of the major demands in evaluating people with LPB. MRI and CT scans can not distinguish patients with LBP from healthy patients due to abnormalities. The US is performed in real-time and includes various conditions that measure thickness, blood flow, and stiffness. Using this tool, patients with LBP were differentiated from healthy subjects according to the thickness and stiffness of the transverse abdominal muscle, multifidus muscle, lumbar, and thoracic fascia.40
To date, the reliability of US for multifidus muscle in people with MPS has not been studied. Farragher et al. (2021) established the test–retest and inter-rater reliability of lumbar multifidus in healthy subjects. The results showed good to excellent test–retest and inter-rater reliability for lumbar multifidus thickness (ICC: 0.89-0.98).45 Furthermore, Cuellar et al. revealed excellent test–retest reliability (ICC3,1 = 0.83) for the lumbar multifidus thickness.46
Like the present study, they used the average of three measurements to calculate ICCs and SEM, which may improve reliability and SEMs up to 50%.46
Like the present study, some previous studies have shown that the value of reliability at rest is greater than muscle contraction. One of the reasons may be the change in tissue echogenicity and the inability to find the exact muscle fascia in the state of muscle contraction.47
On the other hand, the reliability in patients with LBP is lower than in healthy individuals. In addition, the position of the upper limb or lower limb in the contraction position of multifidus also affects reliability. In the present study, the contralateral upper limb method revealed high reliability like in some studies. However, in the study by Sion et al., the contralateral lower extremity method was used because elderly patients could not raise their arms for various reasons, including frozen shoulders. High reliability was also reported for this condition.47
Thickness changes in muscle evaluation with the US are equivalent to measuring electromyographic activity.48 The reproducibility of US imaging about thickness changes indicates its clinical value. In the present study, it was between 0.75 and 0.90. Interpreting the results based on muscle thickness changes should be cautious. Therefore, to have higher reliability, the physiotherapist should receive sufficient training in the basics of adjusting the US parameters, and the anatomy of the desired location. The physiotherapists in the present study had at least eight years of experience working with the US, which was probably one reason for the high reliability of the US.47, 48 Recently, the results of a review study showed that the reliability of US imaging for multifidus muscle was acceptable. The range of reported reliability values was similar to our findings.49
SEM is directly related to a test’s reliability: The larger the SEM, the lower the test’s reliability. The MDC is considered the minimum amount of change that is not likely due to chance variation in the measurement. In the present study, the largest SEM and MDC for CSA of multifidus muscle were shown in the contraction state. It seems that changing or disappearing fascial borders may occur after contraction.47 In contrast, the lowest SEM and MDC were reported for multifidus muscle thickness at rest.
The within and between-session reliability of multifidus thickness, thickness changes, and CSA was good to excellent in patients with lumbar MPS when taken by two examiners. Furthermore, the inter-examiner reliability of these sonographic findings was fair to excellent. The reliability of multifidus muscle thickness was higher than CSA. In both contraction states (thickness and CSA), the reliability of multifidus muscle was lower than rest positions in patients with lumbar MPS.
Limitations
Several limitations should be considered. First, we did not standardize our contralateral limb height by using an external apparatus for the muscle thickness and CSA in contraction states. Second, we did not assess pain during muscle contraction. It may cause lower reliability and larger SEM in contraction states.29 Third, the results of the present study may not be generalized to other test conditions. Fourth, we did not design a control group without LBP.
Conflict of interest:
The authors do NOT have any potential conflicts of interest with respect to this manuscript.
Disclosure:
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Acknowledgements
The authors would like to thank the Iran University of Medical Sciences for supporting this research.
References
- 1.Fatoye F, Gebrye T, Odeyemi I. Real-world incidence and prevalence of low back pain using routinely collected data. Rheumatol Int. 2019;39(4):619–626. doi: 10.1007/s00296-019-04273-0. [DOI] [PubMed] [Google Scholar]
- 2.Wu A, March L, Zheng X, et al. Global low back pain prevalence and years lived with disability from 1990 to 2017: estimates from the Global Burden of Disease Study 2017. Ann Transl Med. 2020;8(6):299. doi: 10.21037/atm.2020.02.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Noormohammadpour P, Mansournia MA, Koohpayeh-zadeh J, et al. Prevalence of chronic neck pain, low back pain, and knee pain and their related factors in community-dwelling adults in Iran. Clin J Pain. 2017 ;33(2):181–187. doi: 10.1097/AJP.0000000000000396. [DOI] [PubMed] [Google Scholar]
- 4.Hartvigsen J, Hancock MJ, Kongsted A, et al. What low back pain is and why we need to pay attention. Lancet. 2018;391(10137):2356–67. doi: 10.1016/S0140-6736(18)30480-X. [DOI] [PubMed] [Google Scholar]
- 5.Rozhkov D, Zinovyeva O, Barinov A, et al. Myofascial pain syndrome in female patients with chronic nonspecific back pain: diagnosis and treatment. Neurology, Neuropsychiatry, Psychosomatics. 2020;12(2):57–63. [Google Scholar]
- 6.Yousefzadeh Chabok S, Ezzati K, Saberi A, Hosein Zadeh J. Evaluating the Prevalence of Lumbar Myofascial Pain Syndrome in Patients with Non-specific Chronic Low Back Pain and a Normal MRI Study. Journal of Guilan University of Medical Sciences. 2020;29(1):43–50. [Google Scholar]
- 7.Bourgaize S, Newton G, Kumbhare D, Srbely J. A comparison of the clinical manifestation and pathophysiology of myofascial pain syndrome and fibromyalgia: implications for differential diagnosis and management. J Can Chiropr Assoc. 2018 ;62(1):26–41. [PMC free article] [PubMed] [Google Scholar]
- 8.Motaqi M, Ghanjal A. Trigger and Tender Points (Definitions, Similarities, Differences, Treatments) International Journal of Musculoskeletal Pain Prevention. 2020;5(4):393–5. [Google Scholar]
- 9.David G. Myofascial Pain and Dysfunction: The Trigger Point Manual, Vol. 1 - Upper Half of Body. 2nd Edition. Lippincott Williams & Wilkins; 2018. Simons, Janet G. [Google Scholar]
- 10.Ribeiro DC, Belgrave A, Naden A, Fang H, Matthews P, Parshottam S. The prevalence of myofascial trigger points in neck and shoulder-related disorders: a systematic review of the literature. BMC Musculoskelet Disord. 2018;19(1):252. doi: 10.1186/s12891-018-2157-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fernández-de-Las-Peñas C, Dommerholt J. International consensus on diagnostic criteria and clinical considerations of myofascial trigger points: a Delphi study. Pain Med. 2018;19(1):142–150. doi: 10.1093/pm/pnx207. [DOI] [PubMed] [Google Scholar]
- 12.Rahmani N, Kiani A, Mohseni-Bandpei MA, Abdollahi I. Multifidus muscle size in adolescents with and without back pain using ultrasonography. J Bodyw Mov Ther. 2018;22(1):147–151. doi: 10.1016/j.jbmt.2017.05.016. [DOI] [PubMed] [Google Scholar]
- 13.Ezzati K, Khani S, Moladoust H, Takamjani IE, Nasiri E, Ettehad H. Comparing muscle thickness and function in healthy people and subjects with upper trapezius myofascial pain syndrome using ultrasonography. J Bodyw Mov Ther. 2021: 253–256. doi: 10.1016/j.jbmt.2020.12.016. [DOI] [PubMed] [Google Scholar]
- 14.Winter J, Kimber A, Montenegro S, Gao J. Ultrasonography to assess the efficacy of osteopathic manipulative treatment for lumbar spine asymmetry. J Am Osteopath Assoc. 2020;120(11):761–769. doi: 10.7556/jaoa.2020.127. [DOI] [PubMed] [Google Scholar]
- 15.Arimi SA, Bandpei MAM, Rezasoltani A, Peolsson A, Mohammadi M. Multifidus muscle size changes at different directions of head and neck movements in females with unilateral chronic non-specific neck pain and healthy subjects using ultrasonography. J Bodyw Mov Ther. 2018;22(3):560–565. doi: 10.1016/j.jbmt.2017.09.011. [DOI] [PubMed] [Google Scholar]
- 16.Basha MAA, Eldib DB, Aly SA, et al. Diagnostic accuracy of ultrasonography in the assessment of anterior knee pain. Insights Imaging. 2020;11(1):107 . doi: 10.1186/s13244-020-00914-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.ShahAli S, Shanbehzadeh S, ShahAli S, Takamjani IE. Application of ultrasonography in the assessment of abdominal and lumbar trunk muscle activity in participants with and without low back pain: A systematic review. J Manipulative Physiol Ther. 2019;42(7):541–550. doi: 10.1016/j.jmpt.2019.05.003. [DOI] [PubMed] [Google Scholar]
- 18.Fortin M, Rizk A, Frenette S, Boily M, Rivaz H. Ultrasonography of multifidus muscle morphology and function in ice hockey players with and without low back pain. Phys Ther Sport. 2019:37:77–85. doi: 10.1016/j.ptsp.2019.03.004. [DOI] [PubMed] [Google Scholar]
- 19.Patil P, Dasgupta BJTaimd. Role of diagnostic ultrasound in the assessment of musculoskeletal diseases. Ther Adv Musculoskelet Dis. 2012;4(5):341–55. doi: 10.1177/1759720X12442112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Whittaker JL, Ellis R, Hodges PW, et al. Imaging with ultrasound in physical therapy: What is the PT’s scope of practice? A competency-based educational model and training recommendations. Br J Sports Med. 2019;53(23):1447–1453. doi: 10.1136/bjsports-2018-100193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Djordjevic O, Konstantinovic L, Miljkovic N, Bijelic G. Relationship between electromyographic signal amplitude and thickness change of the trunk muscles in patients with and without low back pain. Clin J Pain. 2015;31(10):893–902. doi: 10.1097/AJP.0000000000000179. [DOI] [PubMed] [Google Scholar]
- 22.Goubert D, De Pauw R, Meeus M, et al. Lumbar muscle structure and function in chronic versus recurrent low back pain: a cross-sectional study. Spine J. 2017;17(9):1285–1296. doi: 10.1016/j.spinee.2017.04.025. [DOI] [PubMed] [Google Scholar]
- 23.Kim CY, Choi JD, Kim SY, Oh DW, Kim JK, Park JW. Comparison between muscle activation measured by electromyography and muscle thickness measured using ultrasonography for effective muscle assessment. J Electromyogr Kinesiol. 2014 ;24(5):614–20. doi: 10.1016/j.jelekin.2014.07.002. [DOI] [PubMed] [Google Scholar]
- 24.Ezzati K, Khani S, Moladoust H, et al. Comparing muscle thickness and function in healthy people and subjects with upper trapezius myofascial pain syndrome using ultrasonography. J Bodyw Mov Ther. 2021;26:253–256. doi: 10.1016/j.jbmt.2020.12.016. [DOI] [PubMed] [Google Scholar]
- 25.Kumbhare DA, Elzibak AH, Noseworthy MDJAJoPM, Rehabilitation Assessment of myofascial trigger points using ultrasound. Am J Phys Med Rehabil. 2016;95(1):72–80. doi: 10.1097/PHM.0000000000000376. [DOI] [PubMed] [Google Scholar]
- 26.Taghipour M, Mohseni-Bandpei MA, Abdollahi I, Rajabzadeh F, Naghdi N, Pourahmadi MR. Reliability of B-mode ultrasonography to measure lumbar multifidus muscle dimensions in patients with unilateral lumbar disc herniation. J Bodyw Mov Ther. 2021;26:153–157. doi: 10.1016/j.jbmt.2020.06.042. [DOI] [PubMed] [Google Scholar]
- 27.Sions JM, Velasco TO, Teyhen DS, Hicks GE. Reliability of ultrasound imaging for the assessment of lumbar multifidi thickness in older adults with chronic low back pain. J Geriatr Phys Ther. 2015;38(1):33–9. doi: 10.1519/JPT.0000000000000021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Romero-Morales C, Calvo-Lobo C, Navarro-Flores E, et al. M-mode ultrasound examination of soleus muscle in healthy subjects: intra-and inter-rater reliability study. Healthcare (Basel) 2020;8(4):555. doi: 10.3390/healthcare8040555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Djordjevic O, Djordjevic A, Konstantinovic L. Interrater and intrarater reliability of transverse abdominal and lumbar multifidus muscle thickness in subjects with and without low back pain. J Orthop Sports Phys Ther. 2014;44(12):979–88. doi: 10.2519/jospt.2014.5141. [DOI] [PubMed] [Google Scholar]
- 30.Taghipour M, Mohseni-Bandpei MA, Abdollahi I, et al. Reliability of B-mode ultrasonography to measure lumbar multifidus muscle dimensions in patients with unilateral lumbar disc herniation. J Bodyw Mov Ther. 2021;26:153–157. doi: 10.1016/j.jbmt.2020.06.042. [DOI] [PubMed] [Google Scholar]
- 31.Bujang MA, Baharum N. A simplified guide to determination of sample size requirements for estimating the value of intraclass correlation coefficient: a review. Archives of Orofacial Science. 2017;12(1) [Google Scholar]
- 32.Ahmed S, Aggarwal A, Lawrence AJRI. Performance of the American College of Rheumatology 2016 criteria for fibromyalgia in a referral care setting. Rheumatol Int. 2019;39(8):1397–1403. doi: 10.1007/s00296-019-04323-7. [DOI] [PubMed] [Google Scholar]
- 33.Asghari A, Saed F, Dibajnia P. Psychometric properties of the Depression Anxiety Stress Scales-21 (DASS-21) in a non-clinical Iranian sample. Int J psychol. 2008;2(2):82–102. [Google Scholar]
- 34.Lo LC, Hatfield BD, Wu CT, Chang CC, Hung TM. Elevated state anxiety alters cerebral cortical dynamics and degrades precision cognitive-motor performance. Sport, Exercise, and Performance Psychology. 2019;8(1) [Google Scholar]
- 35.Magee DJ, Manske RC. Orthopedic physical assessment-E-Book. 1st ed. Elsevier Health Sciences; 2020. [Google Scholar]
- 36.Koppenhaver S, Kniss J, Lilley D, et al. Reliability of ultrasound shear-wave elastography in assessing low back musculature elasticity in asymptomatic individuals. J Electromyogr Kinesiol. 2018;39:49–57. doi: 10.1016/j.jelekin.2018.01.010. [DOI] [PubMed] [Google Scholar]
- 37.Mehta S, Bastero-Caballero RF, Sun Y, et al. Performance of intraclass correlation coefficient (ICC) as a reliability index under various distributions in scale reliability studies. Stat Med. 2018;37(18):2734–2752. doi: 10.1002/sim.7679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Carter R, Lubinsky J. Rehabilitation research: principles and applications. 5st ed. Elsevier Health Sciences; 2015. [Google Scholar]
- 39.Mohammadi-Rad S, Mohseni Bandpei M, Salavati M, et al. Reliability of Center of Pressure measures of Postural Stability in Anterior Cruciate Ligament Reconstructed Athletes: Effect of Vibration and Cognitive Load. Arch Bone Jt Surg. 2022;10(2):171–182. doi: 10.22038/ABJS.2021.54007.2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cheung WK, Cheung JPY, Lee W-N. Role of ultrasound in low back pain: a review. Ultrasound Med Biol. 2020;46(6):1344–1358. doi: 10.1016/j.ultrasmedbio.2020.02.004. [DOI] [PubMed] [Google Scholar]
- 41.Wong AY, Parent E, Kawchuk G. Reliability of 2 ultrasonic imaging analysis methods in quantifying lumbar multifidus thickness. J Orthop Sports Phys Ther. 2013;43(4):251–62. doi: 10.2519/jospt.2013.4478. [DOI] [PubMed] [Google Scholar]
- 42.Skeie EJ, Borge JA, Leboeuf-Yde C, Bolton J, Wedderkopp N. Reliability of diagnostic ultrasound in measuring the multifidus muscle. Chiropr Man Therap. 2015;23:15 . doi: 10.1186/s12998-015-0059-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Plaza-Manzano G, Navarro-Santana MJ, Valera-Calero JA, Fabero-Garrido R, Fernández-de-las-Peñas C, López-de-Uralde-Villanueva I. Reliability of lumbar multifidus ultrasound assessment during the active straight leg raise test. Eur J Clin Invest. 2022;52(5):e13728. doi: 10.1111/eci.13728. [DOI] [PubMed] [Google Scholar]
- 44.Sánchez Romero EA, Alonso Pérez JL, Muñoz Fernández AC, et al. Reliability of Sonography Measures of the Lumbar Multifidus and Transversus Abdominis during Static and Dynamic Activities in Subjects with Non-Specific Chronic Low Back Pain. Diagnostics (Basel) 2021;11(4):632. doi: 10.3390/diagnostics11040632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Farragher J, Pranata A, El-Ansary D, et al. Reliability of lumbar multifidus and iliocostalis lumborum thickness and echogenicity measurements using ultrasound imaging. Australas J Ultrasound Med. 2021;24(3):151–160. doi: 10.1002/ajum.12273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cuellar W, Blizzard L, Callisaya M, et al. Test-retest reliability of measurements of abdominal and multifidus muscles using ultrasound imaging in adults aged 50–79 years. Musculoskelet Sci Pract. 2017;28:79–84. doi: 10.1016/j.msksp.2016.11.013. [DOI] [PubMed] [Google Scholar]
- 47.Sions JM, Velasco TO, Teyhen DS, Hicks GE. Ultrasound imaging: intraexaminer and interexaminer reliability for multifidus muscle thickness assessment in adults aged 60 to 85 years versus younger adults. J Orthop Sports Phys Ther. 2014;44(6):425–34. doi: 10.2519/jospt.2014.4584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kiesel KB, Uhl TL, Underwood FB, Rodd DW, Nitz AJ. Measurement of lumbar multifidus muscle contraction with rehabilitative ultrasound imaging. Man Ther. 2007;12(2):161–6. doi: 10.1016/j.math.2006.06.011. [DOI] [PubMed] [Google Scholar]
- 49.Taghipour M, Mohseni-Bandpei MA, Behtash H, et al. Reliability of Real-time Ultrasound Imaging for the Assessment of Trunk Stabilizer Muscles: A Systematic Review of the Literature. J Ultrasound Med. 2019;38(1):15–26. doi: 10.1002/jum.14661. [DOI] [PubMed] [Google Scholar]