Abstract
This cross-sectional study examines the prevalence of hypertension among children and adolescents with low, very low, normal, or high birth weight.
Children and adolescents with low birth weight (LBW) have a higher risk for hypertension and cardiovascular disease later in life.1,2 Due to their lower number of nephrons and associated glomerular hyperfiltration, this population may be more sensitive to the adverse association of obesity with blood pressure (BP).1 We aimed to determine the extent to which the association between overweight or obesity and hypertension in US children and adolescents is modified by birth weight (BW).
Methods
Data were obtained from the National Health and Nutrition Examination Survey (NHANES) for 2-year cycles from 1999 to 2000 and 2017 to 2018. We included participants aged 8 to 15 years because BP measurement started at age 8 years in NHANES, and BW was reported by parent or proxy recall until age 15 years. The Yale Institutional Review Board deemed this cross-sectional study exempt from review. Parents and participants 12 years or older provided written consent; children younger than 12 years provided assent. We followed the STROBE reporting guideline.
Overweight or obesity was defined as body mass index (BMI) at or above the 85th percentile.3 Birth weight was categorized as very low BW (VLBW; <1500 g), LBW (1500-2499 g), normal BW (2500-3999 g), and high BW (HBW; ≥4000 g). Three consecutive BP measurements were obtained per protocol. The mean of all BP measurements determined hypertension status based on American Academy of Pediatrics guidelines.4
Hypertension prevalence was compared between overweight or obesity and BW categories using the χ2 test. We used modified Poisson regression5 to estimate prevalence ratio (PR) for the association of overweight or obesity with hypertension adjusted for age, sex, BW, and interaction between overweight or obesity and BW. The interaction was significant; thus, we investigated effect measure modification6 by estimating the PR of hypertension (1) for each combination of overweight or obesity and BW vs healthy BMI and normal BW as the reference and (2) for overweight or obesity within BW strata. We calculated the proportion of disease attributable to interaction among persons with both exposures.6 Additive interaction was present when the attributable proportion was more than 0.6
P < .05 indicated significance. Analyses accounted for the sampling design and were performed from June 2022 to January 2023 using Stata/SE 17.0 (StataCorp LLC).
Results
Of 14 615 participants (median [IQR] age, 12 [10-14] years; 49.1% girls and 50.9% boys [weighted percentages]) with BW, BMI, and BP data, 1.1% had VLBW, 7.2% had LBW, 80.6% had normal BW, and 11.1% had HBW. Overweight or obesity occurred in 35.2% of participants with VLBW, 36.1% with LBW, 38.1% with normal BW, and 43.8% with HBW.
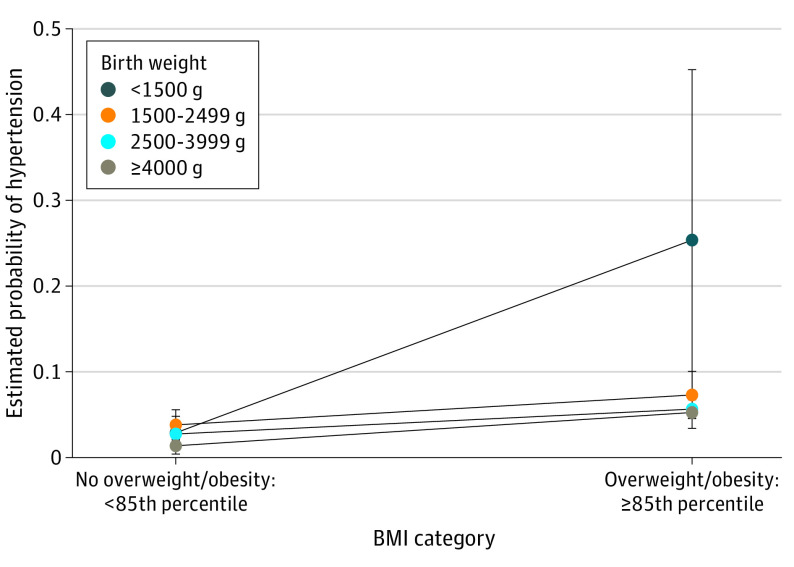
Hypertension prevalence was higher in participants with overweight or obesity vs healthy BMI (7.1% [95% CI, 6.3%-8.1%] vs 3.3% [95% CI, 2.7%-4.0%]) and in participants with lower BW (VLBW: 12.1% [95% CI, 5.7%-24.0%]; LBW: 6.1% [95% CI, 4.6%-8.2%]; normal BW: 4.7% [95% CI, 4.1%-5.3%]; HBW 3.8% [95% CI, 2.7%-5.4%]). The association between overweight or obesity and hypertension was modified by BW (P for interaction = .02). Participants with overweight or obesity in the VLBW vs normal BW category had higher hypertension risk (PR, 7.73 [95% CI, 2.80-21.33] vs 2.06 [95% CI, 1.59-2.67]; P = .005). Compared with participants with healthy BMI and normal BW, those with overweight or obesity and VLBW had over a 9-fold higher hypertension risk (PR, 9.23; 95% CI, 4.11-20.72) (Table; Figure). The proportion attributable to interaction among children with overweight or obesity and VLBW was 77.2% (95% CI, 57.9%-96.5%; P < .001).
Table. Effect Measure Modification by Birth Weight (BW) on the Association Between Overweight or Obesity and Hypertension (N = 14 615).
| BW categorya | No. of participants | Overweight or obesity | Hypertension prevalence (95% CI), % | PR (95% CI) | PR (95% CI), within BW strata | P value for interactionb |
|---|---|---|---|---|---|---|
| Normal BW | 11 707 | No | 3.4 (2.7-4.2) | 1 [Reference] | 2.06 (1.59-2.67) | NA |
| Yes | 6.8 (5.9-7.9) | 2.06 (1.59-2.67) | ||||
| HBW | 1493 | No | 1.7 (0.8-3.5) | 0.50 (0.23-1.08) | 3.85 (1.88-7.86) | .11 |
| Yes | 6.6 (4.7-9.0) | 1.92 (1.28-2.87) | ||||
| LBW | 1204 | No | 4.7 (3.0-7.3) | 1.39 (0.88-2.18) | 1.94 (1.04-3.60) | .83 |
| Yes | 8.7 (5.9-12.7) | 2.66 (1.75-4.04) | ||||
| VLBW | 211 | No | 3.5 (1.8-6.7) | 1.06 (0.55-2.02) | 7.73 (2.80-21.33) | .005 |
| Yes | 28.0 (12.1-52.3) | 9.23 (4.11-20.72) |
Abbreviations: HBW, high birth weight; LBW, low birth weight; NA, not applicable; PR, prevalence ratio; VLBW, very low birth weight.
Weight was categorized as normal BW (2500-3999 g), HBW (≥4000 g), LBW (1500-2499 g), and VLBW (<1500 g).
P values are shown for the partial interaction term comparing the association between overweight or obesity and hypertension in each BW category with the association in the reference category of normal BW.
Figure. Estimated Probability of Hypertension by Overweight or Obesity Body Mass Index (BMI) and Birth Weight.
Estimated margins with 95% CIs were calculated using the modified Poisson regression model with the covariates set at female sex aged 12 years.
Discussion
We found modification of the association between overweight or obesity and hypertension by BW. This study provided evidence that the interaction of lower BW and obesity with cardiovascular outcomes reported in adults2 may exist in childhood.
Study limitations included the reliance on BW recall, lack of additional pregnancy-related data, and hypertension diagnosis based on BP at 1 visit. Nevertheless, the results highlight the public health importance of preventing obesity in children and adolescents, especially those with VLBW.
Data Sharing Statement
References
- 1.Luyckx VA, Bertram JF, Brenner BM, et al. Effect of fetal and child health on kidney development and long-term risk of hypertension and kidney disease. Lancet. 2013;382(9888):273-283. doi: 10.1016/S0140-6736(13)60311-6 [DOI] [PubMed] [Google Scholar]
- 2.Frankel S, Elwood P, Sweetnam P, Yarnell J, Smith GD. Birthweight, body-mass index in middle age, and incident coronary heart disease. Lancet. 1996;348(9040):1478-1480. doi: 10.1016/S0140-6736(96)03482-4 [DOI] [PubMed] [Google Scholar]
- 3.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC growth charts for the United States: methods and development. Vital Health Stat 11. 2002;(246):1-190. [PubMed] [Google Scholar]
- 4.Flynn JT, Kaelber DC, Baker-Smith CM, et al. ; Subcommittee on Screening and Management of High Blood Pressure in Children . Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017;140(3):e20171904. doi: 10.1542/peds.2017-1904 [DOI] [PubMed] [Google Scholar]
- 5.Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702-706. doi: 10.1093/aje/kwh090 [DOI] [PubMed] [Google Scholar]
- 6.VanderWeele TJ, Knol MJ. A tutorial on interaction. Epidemiol Methods. 2014;3(1):33-72. doi: 10.1515/em-2013-0005 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Sharing Statement