Abstract
BACKGROUND
Current guidelines for brace management of adolescent idiopathic scoliosis (AIS) are mostly recommended for curves between 25° to 40°. For AIS patients with curves >40°, surgery is often considered since bracing may be less effective; however, there are still some patients and families who refuse operation. Therefore, further research is necessary to determine optimal bracing management in this group. To date, few protocols for such have been reported in literature.
AIM
The aim of this study was to introduce and evaluate the effectiveness of the treatment protocol comprising of intensive bracing management and physiotherapeutic scoliosis-specific exercises (PSSE) in AIS patients with a major curve of 40-60° who refuse surgery.
DESIGN
This is a prospective cohort study.
SETTING
The study was carried out in an outpatient clinic.
POPULATION
10-18-year-old AIS patients having 40-60°curves and a Risser grade of 0-3, but firmly refusing surgery were eligible. Patients who had a proximal thoracic curve or had undergone any other form of treatment previously were excluded from the study.
METHODS
A total of 82 patients were recruited and received the treatment. The primary outcome was defined as “success” when the main curve was below 50° upon reaching skeletal maturity, and “failure” if otherwise. The secondary outcome was defined as improved (>5° reduction), unchanged (≤5° change) or progressed (>5° increase) based on the evolution of the main curve. The per protocol (PP) and intent to treat (ITT) analyses were performed to quantify success rates, while the dropouts were considered as failures. Risk factors associated with bracing failure were identified and a receiver operating characteristic (ROC) curve was used to determine the cut-off value.
RESULTS
A total of 77 patients completed the treatment, while 5 dropped out. The average main curve was 47.40±5.93° at baseline and 38.56±11.85° at last follow-up (P<0.001). Our management was successful in 83% and 78% of patients based on the PP and ITT analyses, respectively. When compared with the curve magnitude at baseline, 65% patients improved, 30% remained unchanged, and 5% progressed when using a 5° threshold. Univariate comparison and logistic regression analysis demonstrated that patients with successful outcomes had a significantly smaller baseline curve, larger Risser Stage, and larger in-brace correction (IBC) rate.
CONCLUSIONS
For AIS patients with 40-60° curves who refused surgery, our intensive bracing management along with PSSE was practical and effective, achieving success in 78% of patients based on an ITT analysis. A larger baseline curve, smaller Risser Stage, and smaller IBC rate were associated with treatment failure.
CLINICAL REHABILITATION IMPACT
Our intensive management provides new insights into improving the effectiveness of bracing in patients with AIS who refuse surgery. This is a promising option for patients with 40-60° curves, since their scoliosis may be treated using a non-surgical technique instead of surgery in the future.
Key words: Adolescent, Scoliosis, Physical therapy modalities
Adolescent idiopathic scoliosis (AIS) is one of the most common spinal deformities in school-age children and teenagers, with a total prevalence of 1-3%.1 The torsion of the spine occurs in three dimensions, with morphologically lordotic vertebrae translating and rotating to the same side.2 Fast progression of scoliosis during the adolescent growth spurt may lead to various cosmetic concerns, back pain, psychological problems, cardiopulmonary compromise, and a reduced health-related quality of life.3, 4 Therefore, appropriate treatment, including surgical and non-surgical approaches, is warranted to halt the progression of AIS. One of the main approaches in conservative treatment is bracing; it has been proven effective in the prevention of scoliosis progression with a high level of evidence in the recent Bracing in Adolescent Idiopathic Scoliosis Trial (BrAIST).5 The eligibility criteria for this type of treatment included skeletally immature AIS patients with 20-40° curves.6, 7 Treatment failure is often considered curve progression to 50 degrees or more prior to skeletal maturity. This endpoint is chosen because surgery becomes an option at this point in many practices around the world. Despite the widespread use of fusion and instrumentation, many families remain greatly concerned about its safety, invasiveness, high cost, restricted movement post-surgery, long recovery time, and a lifetime risk of complications.8, 9 Even if some patients are eligible for surgery, some remain firmly opposed to operative interventions and prefer to push through with non-invasive treatment instead. This remains to be a dilemma in clinical practice, since bracing management has only been proven to be effective for AIS patients with curves <40° in BrAIST.5 To enhance the effectiveness of bracing, various types of braces are fabricated and utilized worldwide. Many different kinds of modifications have been individually applied and personalized to improve patient fit and compliance.10 However, ways or methods by which brace management may be reinforced and be made more effective in patients with greater curves (>40°) have never been explored. The current concept of brace management, which targets patients with moderate curves (25-40°), includes a regular assessment of effectiveness every six months until skeletal maturity is reached. Besides, the assessment was mainly focused on the patients’ adherence to bracing during follow-up,11, 12 while it is uncommon to document increasing bracing force in the research literature. In this study, we reported on an intensive method, which emphasizes achieving incremental in-brace correction (IBC), in immature AIS patients with large curves (40-60°) who refused operation. This study aimed to evaluate the effectiveness of intensive bracing management combined with adjuvant scoliosis-specific exercises in replacing the need for surgery in AIS patients.
Materials and methods
Cohort
This was a prospective cohort study that was approved by the Institutional Review Board of our institution. The study was conducted in accordance with the principles of the Helsinki Declaration. All patients provided their consent about the management of clinical data by signing an informed consent form. All patients visited our clinic to consult with a physician with expertise in non-operative treatment of AIS, between January 2014 and December 2018. The inclusion criteria were as follows: 1) AIS patients with main curves ranging between 40-60°; 2) a Risser Stage of 0-3; 3) those who refuse any form of surgical intervention; and 4) receiving our treatment with a minimum follow-up of two years. Patients who had a proximal thoracic curve (with apex above T6) or had undergone other previous treatments were excluded from the study. Based on the criteria above, 82 patients were recruited and enrolled in our study. Two analyses, namely the intention to treat (ITT) and per protocol (PP) analyses, were performed and drop-outs were considered as the failure in the analysis.13
Bracing and exercising protocol
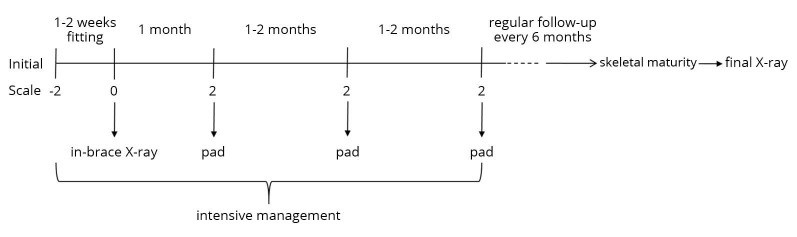
The prescribed braces were modified Gensingen braces, which were derived from Chêneau braces and are thoroughly described and utilized in existing literature.14 It opened on the ventral side and was fastened by two straps, whose tightness could be adjusted by patients themselves. Five scales (-2, -1, 0, 1, 2) were marked on the straps to record the tightness by an experienced orthotist. The marking “0” was determined firstly according to the maximum tightness that a patient could initially tolerate. After the benchmark “0” was set, adjacent scale was marked sequentially with a distance of 2 cm: first “1” or “-1,” then “2” or “-2.” Thus, from “-2” to “2,” the tightness of the straps gradually enhanced. Patients started wearing brace with the initial tightness of “-2.” In the first 1-2 weeks of fitting, the tightness was required to increase from “-2” to “0” and then in-brace radiographs were taken. After one month, the straps should be tightened to “2,” offering the maximum force, and patients visited the clinic for adding a pad. When the pad was added, patients could not maintain the current tightness due to the increased pressure inside the brace and need to lose the straps to the previous degree. It usually took 1-2 months for them to get the maximum tightness “2” again and another pad was prescribed after that. In this way, we routinely added 3-4 pads to gradually elevate the corrective force. The schematic diagram of this process is presented in Figure 1.
Figure 1.
—The schematic diagram of the intensive bracing management.
Intensive management was performed in the early follow-up period (usually the first six months) to offer the maximum bracing corrective force. During this period, patients were encouraged to visit the clinic at a frequent interval of 1-2 months to adjust the corrective force, closely monitor their compliance, and examine if any skin problems arose due to the high pressure. Photos of the patients’ backs were taken monthly to assess the aesthetic changes. After this period, a regular follow-up every 6 months was recommended for each patient. Upon reaching skeletal maturity, patients took the final radiographs and discontinued bracing through a weaning process. The weaning process was performed during a period of 2-3 months by two hours less bracing time every week.15 All patients were required to wear braces at least 20 hours per day. The objective monitoring, such as a temperature sensor, was not routinely used in these patients. During each visit, the actual time of daily bracing was recorded according to the patients’ recall memory and was confirmed by their parents. The average wearing time per day was calculated. The physiotherapeutic scoliosis-specific exercises (PSSE) used in this study was a unique approach from the Xinmiao treatment system (XTS).16 It consisted of daily corrective postures and intensive corrective exercises, including muscle strengthening and curve stretching movements.16 The physiotherapists trained every patient and their parents by enrolling them in several training courses and instructing them to perform exercises regularly at home. Patients were required to exercise for at least one hour per day. A multidisciplinary team at our center, including a physician, orthotist, and physiotherapist, worked together to ensure the appropriate implementation of bracing and exercising techniques.
Clinical and radiological assessment
Patients’ demographics, including age, sex, menstrual status and Risser sign, were recorded at baseline. Patients were required to take the posteroanterior and lateral spinal X-rays every six months. The radiographs were collected at the baseline and during follow-up for radiological assessment. Risser stages and curve magnitudes (using Cobb’s method) were determined on spinal radiographs. The thoracic curve and lumbar curve were measured for each patient. The larger one was defined as the main curve and the smaller one as the minor curve. Skeletal maturity was defined as having a 5 Risser sign for boys and 4 Risser sign (or two-years post-menarche) for girls. The IBC rates were calculated using the following formula: (Cobb angle at baseline – in-brace Cobb angle)/Cobb angle at baseline ×100%. According to the Scoliosis Research Society (SRS) guidelines, curves reaching 50° are at a high risk for continued progression throughout adulthood and are usually recommended for spinal fusion surgery.17 Therefore, the primary outcome in this study was defined as “success” when the main curve was achieved below 50° upon reaching skeletal maturity, and “failure” if otherwise. The secondary outcome was classified as follows, based on the evolution of the main curve: 1) improved (>5° reduction in the main curve); 2) unchanged (≤5° change in the main curve); and 3) progressed (>5° increase in the main curve).
Statistical analysis
Data analysis was performed using the SPSS 26.0 software (IBM Corp., Armonk, NY, USA). Successful rates were calculated in the PP and ITT analyses. The univariate comparison included the independent t-test for comparing continuous variables and the χ2 test or Fisher’s Exact Test for comparing categorical parameters. With potential related variables entered, factors that significantly associated with treatment success were identified by multivariable logistic regression in forward stepwise methods. The resulting model coefficients were applied to calculate predicted values of probability from the logistic equation. Receiver operating characteristic (ROC) curve was used to determine threshold ability for treatment success of this composite model, and of other individual parameters recruited. A P value of <0.05 was considered statistically significant.
Results
A total of 82 patients were enrolled but five patients dropped out of our study due to the skin problems that the braces caused. The dropouts were all female with a mean age of 12.2±0.8 years and an average main curve of 50.2±4.1°. Eventually, there were 77 patients (68 females and 9 males) who completed our treatment regimen. The mean age of patients was 12.7±1.4 years (range: 10-16 years). During the first visit, 17 girls were premenarche and 51 were post-menarche. Risser stages were distributed as follows: grade 0 in 18 patients (23%), grade 1 in 18 (23%), grade 2 in 13 (17%), and grade 3 in 28 (36%). According to the location of main curve, two subgroups were formed: main thoracic curve (44 cases) and main lumbar curve (33 cases). Statistical analysis of the baseline characteristics between the two groups showed no significant difference (Table I) (P>0.05). The average baseline primary curve and secondary curve were 47.40±5.93° and 31.19±7.54°, respectively (Table II).
Table I. —Baseline characteristics of patients.
| Parameters | Total | Thoracic | Lumbar | P value |
|---|---|---|---|---|
| Numbers | 77 | 44 | 33 | |
| Age (years) | 12.70±1.41 | 12.52±1.46 | 12.94±1.32 | 0.200 |
| Sex | 0.486 | |||
| Male | 9 (11.7%) | 4 (5.2%) | 5 (6.5%) | |
| Female | 68 (88.3%) | 40 (51.9%) | 28 (36.4%) | |
| Menstrual status | 0.569 | |||
| Premenstruation | 17 (22.1%) | 11 (14.3%) | 6 (7.8%) | |
| Post-menstruation | 51 (66.2%) | 29 (37.7%) | 22 (28.6%) | |
| Riser Stage | 0.898 | |||
| 0 | 18 (23.4%) | 11 (14.3%) | 7 (9.1%) | |
| 1 | 18 (23.4%) | 9 (11.7%) | 9 (11.7%) | |
| 2 | 13 (16.9%) | 8 (10.4%) | 5 (6.5%) | |
| 3 | 28 (36.4%) | 16 (20.8%) | 12 (15.6%) | |
| Follow-up time (years) | 3.26±0.83 | 3.19±0.76 | 3.35±0.92 | 0.420 |
Table II. —Comparison of main and minor curves at baseline and during the last follow-up.
| Curve | Baseline (°) | Last follow-up (°) | MD | 95% CI | P value |
|---|---|---|---|---|---|
| Main curve | 47.40±5.93 | 38.56±11.85 | 8.84 | 6.44, 11.24 | <0.001 |
| Minor curve | 31.19±7.54 | 27.17±10.84 | 4.03 | 2.26, 5.79 | <0.001 |
MD: mean difference; CI: confidence interval.
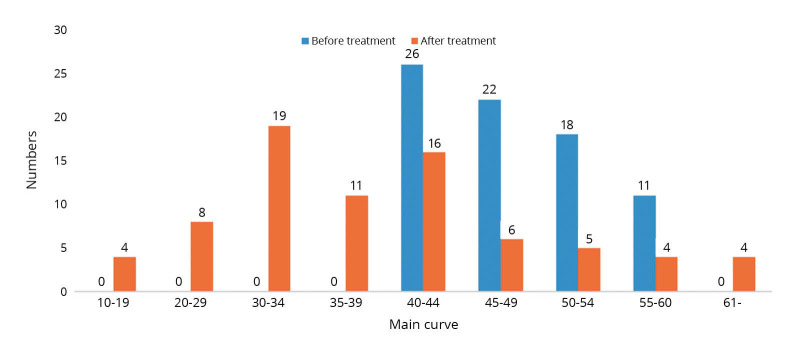
The immediate in-brace radiographs showed that the average of the main curve was 22.16±9.17° and IBC rates were calculated as 53.51±17.97%. Patients with a main lumbar curve had significantly larger IBC percentage than those with a main thoracic curve (59.36±18.29% vs. 49.12±16.60%, P=0.012). All patients were followed up until skeletal maturity with a mean duration of 3.26±0.83 years. The final X-rays at skeletal maturity demonstrated that the main curve was 38.56±11.85° and minor curve was 27.17±10.84° on average, both showing a statistically significant difference (P<0.001) (Table II). The distribution of the main curve magnitudes before and after the treatment was demonstrated in Figure 2.
Figure 2.
—The distribution of major curves before and after treatment.
Based on the endpoint of curve progression to 50°, the primary outcome was divided into success and failure. In general, the treatment was successful in 83% and 78% of patients based on the PP and ITT analyses, respectively; the latter included the number of drop-outs as failures (Table III).
Table III. —Treatment outcomes based on the PP and ITT analyses.
| Analysis | Total population |
Primary outcome | Secondary outcome | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Success | Failure | Improved | Unchanged | Progressed | ||||||||
| N. | % | N. | % | N. | % | N. | % | N. | % | N. | % | |
| ITT analysis | 82 | 100 | 64 | 78.0 | 18 | 22.0 | 50 | 61.0 | 23 | 28.0 | 9 | 11.0 |
| PP analysis | 77 | 100 | 64 | 83.1 | 13 | 16.9 | 50 | 64.9 | 23 | 29.9 | 4 | 5.2 |
The primary outcome was defined as “success” when main curve was below 50° upon reaching skeletal maturity, and “failure” otherwise. The secondary outcome was classified as follow: 1) improved – reduction of main curve >5°; 2) unchanged – change of main curve ≤5°; 3) progressed – increase of main curve >5°. PP: per protocol; ITT: intention to treat.
As for the secondary outcome, 65% patients improved, 30% remained unchanged, and 5% progressed based on the PP analysis, while 61% improved, 28% remained unchanged, and 11% progressed based on the ITT analysis. Further univariate comparison indicated that the IBC rates, Risser stages, and curve magnitudes at baseline were significantly different between the success and failure groups (P=0.002, 0.030, and 0.002, respectively), while age, sex, curve types, bracing time, and follow-up time showed no statistically significant difference (Table IV) (P>0.05).
Table IV. —Comparison of clinical and radiographic parameters between success and failure groups.
| Parameters | Success group | Failure group | P value | OR/MD | 95% CI |
|---|---|---|---|---|---|
| Number | 64 | 13 | - | ||
| Age (years) | 12.77±1.43 | 12.38±1.26 | 0.376 | 0.381 | (-0.472, 1.234) |
| Sex | 0.643 | 0.675 | (0.124, 3.693) | ||
| Male | 7 (9.1%) | 2 (2.6%) | |||
| Female | 57 (74.0%) | 11 (14.3%) | |||
| Risser Stage | 0.030* | 0.205 | (0.051, 0.819) | ||
| 0-1 | 26 (33.8%) | 10 (13.0%) | |||
| 2-3 | 38 (49.4%) | 3 (3.9%) | |||
| Curve type | 0.376 | 0.536 | (0.150, 1.922) | ||
| MT | 35 (45.5%) | 9 (11.7%) | |||
| ML | 29 (37.7%) | 4 (5.2%) | |||
| Baseline curve (°) | 46.3±5.4 | 52.8±5.7 | 0.002* | -6.46 | (-10.066, -2.848) |
| IBC rates (%) | 56.36±16.85 | 39.50±17.27 | 0.002* | 16.857 | (6.606, 27.109) |
| Bracing time (hours) | 18.8±3.2 | 16.8±5.3 | 0.205 | 2.012 | (-1.235, 5.259) |
| Follow-up (years) | 3.27±0.73 | 3.19±1.25 | 0.824 | 0.081 | (-0.690, 0.852) |
Dropouts were not included in the failure group. *Statistically significant. MT: main thoracic; ML: main lumbar; MD: mean difference; OR: Odds Ratio; CI: confidence interval.
With all these parameters included, the multivariable logistic regression analysis demonstrated that patients in the success group had a significantly smaller curve magnitude, higher Risser Stage, and higher IBC rate (Table V) (P=0.002, 0.016, and 0.004, respectively).
Table V. —Multivariable logistic regression results for treatment outcomes.
| Parameters | Risser group (sign) | IBC rates | Curve magnitude | Constant | |
|---|---|---|---|---|---|
| 1 (0-1) | 2 (2-3)* | ||||
| β | -2.701 | 0.105 | -0.279 | 12.233 | |
| SE | 1.117 | 0.036 | 0.090 | 4.245 | |
| Wald | 5.845 | 8.408 | 9.508 | 8.303 | |
| OR | 0.067 | 1.111 | 0.757 | - | |
| 95% CI | (0.008, 0.600) | (1.0.35, 1.192) | (0.634, 0.903) | - | |
| P value | 0.016 | 0.004 | 0.002 | 0.004 | |
Hosmer-Lemeshow Test: P=0.869. *Means the reference group. IBC: in-brace correction; OR: Odds Ratio; CI: confidence interval; SE: standard error.
The Hosmer-Lemeshow Test showed that the model performance of the multivariate logistic regression analysis was well calibrated (P=0.869). Based on the results of the logistic regression analysis, the predicted probability was calculated by the following formula: Probability of treatment success= (1+e2.701*Risser group+0.279*Curve magnitude-0.105*IBC rates-12.233)-1. ROC curve analysis was performed for the curve magnitude, IBC rate and the composite model. Composite model had the highest area under the curve (AUC) value of 0.919 (95% CI: 0.836 to1.000), indicating the increased accuracy of the composite model when compared with other individual factors (Figure 3).
Figure 3.
—A) The receiver operating characteristic curve of the composite prediction model; B) in-brace correction rate; and C) curve magnitude. AUC: area under the curve.
Discussion
Our results demonstrated that for AIS patients having 40-60° curves who refused surgery, the intensive management protocol, including bracing and PSSE, achieved success in 83% and 78% of patients based on the PP and ITT analyses, respectively. The average main curve decreased from 47.40±5.93° at baseline to 38.56±11.85° during the last follow-up, with more than 60% of patients showing a curve improvement. These findings suggest intensive bracing management may be an alternative method to avoid spinal fusion surgery in these patients (Figure 4).
Figure 4.
—A-I) A 13-year-old girl presented 50° lumbar curve and 34° thoracic curve but firmly refusing surgery. The initial Risser Stage was 0. The immediate in-brace X-ray showed an in-brace correction rate of 70%. After 4 years treatment, she reached skeletal maturity. The lumbar curve decreased to 19° and thoracic curve decreased to 16° (A-E). The cosmetic presentation also showed excellent improvement (F-I).
It is worth mentioning that high compliance rate of patients was another critical factor for treatment success; and this can be attributed to their strong desire and will to avoid surgery at all costs. The daily wearing time averaged up to 18.4±3.6 hours, which was much higher than the mean 12.1±6.5 hours in the BrAIST.5 Besides, skin problems caused by too much pressure inside the braces usually occurred within the first six months. These patients had to quit the treatment and operation may be a last solution. It is a potential complication of our treatment that we should be warning in the future. Several researchers also explored the effectiveness of brace treatment in AIS patients with large curves (>40°), but the success rates differed, ranging from 35.2% to 93% (Table VI).18-23
Table VI. —Literature review about brace treatment for adolescent idiopathic scoliosis patients with large curves (>40°).
| Authors | N. (Female/male) |
Age (years) | Risser stages | Curve magnitude (range) | Successful rates* | Curve change | |
|---|---|---|---|---|---|---|---|
| Baseline (°) | Follow-up (°) | ||||||
| Negrini et al.18 | 28 (24, 4) | 14.2 | 0-4 | 49.4 (45-58) | 40.15 | 93% | 1 (4%) progress 7 (25%) stabilize 20 (71%) improve |
| Lusini et al.19 | 34 | 15.25 | 0-4 | 52.5 (45-93) | 42.1 | 82.4% | 8 (24%) progress 5 (15%) stabilize 21 (62%) improve |
| Zhu et al.20 | 54 (45, 9) | 13.7 | 0-3 | 43.4 (40-50) | 43.7 | 35.2% | 35 (65%) progress 12 (22%) stabilize 7 (13%) improve |
| Verhofste et al.21 | 100 (85, 15) | 11.8 | 0-4 | 45 (40-59) | 53 | 42% | 57 (57%) progress 32 (32%) stabilize 11 (11%) improve |
| Aulisa et al.22 | 104 (96, 8) | 12.88 | 0-4 | 47.02 (>40) | 34.19 | 84.6% | 9 (9%) progress 14 (13%) stabilize 81 (78%) improve |
| Razeghinezhad et al.23 | 60 (53, 7) | 12.63 | 0-2 | 44.93 (40-55) | 47.29 | 48.3% | 34 (57%) progress 15 (25%) stabilize 11 (18%) improve |
| This study | 77 (68, 9) | 12.70 | 0-3 | 47.40 (40-60) | 38.56 | 83% | 4 (5%) progress 23 (30%) stabilize 50 (65%) improve |
*Drop-outs were excluded. Successful outcome means avoiding surgery or curve <50° at last.
The heterogeneity of samples and utilization of different types of braces and PSSE were proposed as reasons for the widely varied results.24 In a prospective controlled study, Lusini et al.19 compared outcomes of brace treatment with observation. In the efficacy analysis, they found that 23.5% of the patients in the brace group progressed >5° (or needed surgery), while 100% of the patients in the control group failed and required surgery. Negrini et al.18 reported the highest success rate in literature where 93% of the patients had curves below the threshold of 50° and could avoid spinal fusion surgery after non-surgical treatment. More recently, Zaina et al.24 reviewed nine papers, including 563 AIS with surgical indication but choosing bracing interventions, and found that a total of 32% of the patients improved, 26% were stable, and 42% worsened. This indicated that it was possible to obtain good results, including improvements, in the case of larger curves. Our study is the first to successfully propose an intensive management protocol and achieve impressive outcomes, especially when compared to previously published reports. In addition, we utilized stricter standards and excluded patients with a Risser grade of 4, which account for skeletally mature individuals. Although our management did follow general guidelines for bracing and PSSE, we did not follow any specific, data-driven benchmarks to gradually increase the corrective forces applied by the brace (through increasing strap tension or adding pads), instead we mainly performed management based on individual patient response and tolerance. Biomechanical studies showed that strap tension varied greatly in different positions and brace interface forces tended to increase with increasing strap tension, but no standard tension was set up in the clinic.25, 26 To simplify the problem, we marked five scales on the strap to gradually increase the corrective force without greatly affecting the patients’ comfort and compliance. Additionally, we usually added pads at the level of the curve apex for lumbar curves and at the level of the rib corresponding to the curve apex, which was about 2 levels below the apical vertebra, for the thoracic curves. However, the question of optimal placement remains unsettled and finite element analysis had found varied results.27, 28 Recently, Karam et al.29 drew a different conclusion that a lateral force applied at the apical vertebra was significantly more efficient in reducing thoracic curves than that applied at the apical rib. The inconsistency would lead to further investigation on the optimal modifications of braces. At present, the adjustment steps still relied on the extensive experience and skills of the physician and orthotist. In this study, binary logistic regression indicated that the curve magnitude at the baseline, Risser Stage, and IBC rate were significantly associated with treatment outcome. For 40-49° curves, nearly 95% (46/48) may possibly avoid surgery; but for 50-60° curves, only 60% (18/29) of our participants can achieve success. A larger Risser Stage and IBC rate also increased the possibility of success. Karol et al.30 found that while no difference existed in the initial curve magnitude, more patients at Risser Stage 0 had progression requiring surgery than patients at Risser Stage 1 or 2, despite bracing management. Clin et al.31 confirmed the importance of IBC to predict long-term outcome of brace treatment by finite element analysis. Razeghinezhad et al.23 also found that IBC had a significant correlation with treatment outcomes for large AIS curves (>40°) during the final follow-up, but their average IBC rates were only 15.73%. Several authors discovered that the low value of IBC was a risk factor for bracing failure.21, 32-34 Goodbody et al.34 reported a cut-off rate of 45% IBC, below which brace treatment tends to be less successful. Based on the results of logistic regression analysis, we developed a composite model and calculated the predicted probability of treatment success. The composite model had the highest AUC value of 0.919, indicating the increased accuracy of the composite model when compared with other individual factors. Exercising, as an adjuvant treatment to bracing, was another important part for our management. Previously, we had demonstrated that our exercise therapy (Xinmiao treatment system) could effectively control curve progression in 10-25° idiopathic scoliosis patients.16 Zheng et al.35 performed a randomized controlled trial in Mainland China and concluded that both bracing and exercising showed significant effectiveness on 20-40° AIS. Basically, PSSE showed many benefits, such as enhanced muscle strength, improved erector spinae activation, corrected postural defects, slowed curve progression, reduced curve severity, and pain relief.36-38
Limitations of the study
Our study had several limitations. First, several long-term studies with decades of follow-up showed that large curves after skeletal maturity still had potential risks of slow progression but was substantially slower compared with the fast progression that is observed during the adolescent growth spurt.39-41 Therefore, although all patients reached the end of growth in this article, long-time observation into adulthood is needed to check curve’s evolution in the success group. However, a study published by Weinstein et al. concluded that a natural history of adult idiopathic scoliosis with slow progression caused little physical impairment, including mostly back pain and cosmetic concerns, and these patients were productive and functional at a high level during the 50-year follow-up.4 Second, compliance was not measured objectively. Considering that this cohort had stronger motivations than normal subjects to avoid surgery and were under close surveillance by physicians, the potential bias could be eliminated to some extent. Furthermore, modifications of bracing management were largely empirical, and no quantitative standards existed for reference. More efforts are needed to determine the optimal management in the future. At last, although we constructed a predictive model, the formula was theoretical and relatively complex. More practicable methods still awaited further investigation to facilitate the prediction of prognosis.
Conclusions
In conclusion, for AIS patients with 40-60° curves who refuse surgery, our intensive bracing management along with PSSE demonstrated to be practical and effective, achieving success in 78% of patients based on the ITT analysis. A larger baseline curve, lower Risser Stage, and smaller IBC rate were associated with treatment failure. Our concept of intensive management may provide new insights into improving the effectiveness of bracing in AIS patients.
References
- 1.Weinstein SL, Dolan LA, Cheng JC, Danielsson A, Morcuende JA. Adolescent idiopathic scoliosis. Lancet 2008;371:1527–37. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=18456103&dopt=Abstract 10.1016/S0140-6736(08)60658-3 [DOI] [PubMed] [Google Scholar]
- 2.Negrini S, Donzelli S, Aulisa AG, Czaprowski D, Schreiber S, de Mauroy JC, et al. 2016 SOSORT guidelines: orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis Spinal Disord 2018;13:3. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29435499&dopt=Abstract 10.1186/s13013-017-0145-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Altaf F, Gibson A, Dannawi Z, Noordeen H. Adolescent idiopathic scoliosis. BMJ 2013;346:f2508. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=23633006&dopt=Abstract 10.1136/bmj.f2508 [DOI] [PubMed] [Google Scholar]
- 4.Weinstein SL, Dolan LA, Spratt KF, Peterson KK, Spoonamore MJ, Ponseti IV. Health and function of patients with untreated idiopathic scoliosis: a 50-year natural history study. JAMA 2003;289:559–67. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=12578488&dopt=Abstract 10.1001/jama.289.5.559 [DOI] [PubMed] [Google Scholar]
- 5.Weinstein SL, Dolan LA, Wright JG, Dobbs MB. Effects of bracing in adolescents with idiopathic scoliosis. N Engl J Med 2013;369:1512–21. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=24047455&dopt=Abstract 10.1056/NEJMoa1307337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Richards BS, Bernstein RM, D’Amato CR, Thompson GH. Standardization of criteria for adolescent idiopathic scoliosis brace studies: SRS Committee on Bracing and Nonoperative Management. Spine 2005;30:2068–75, discussion 2076–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=16166897&dopt=Abstract 10.1097/01.brs.0000178819.90239.d0 [DOI] [PubMed] [Google Scholar]
- 7.Negrini S, Grivas TB, Kotwicki T, Rigo M, Zaina F; international Society on Scoliosis Orthopaedic and Rehabilitation Treatment (SOSORT). Guidelines on “Standards of management of idiopathic scoliosis with corrective braces in everyday clinics and in clinical research”: SOSORT Consensus 2008. Scoliosis 2009;4:2. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=19149877&dopt=Abstract 10.1186/1748-7161-4-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gallant JN, Morgan CD, Stoklosa JB, Gannon SR, Shannon CN, Bonfield CM. Psychosocial Difficulties in Adolescent Idiopathic Scoliosis: Body Image, Eating Behaviors, and Mood Disorders. World Neurosurg 2018;116:421–432.e1. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29803063&dopt=Abstract 10.1016/j.wneu.2018.05.104 [DOI] [PubMed] [Google Scholar]
- 9.Negrini S, De Mauroy JC, Grivas TB, Knott P, Kotwicki T, Maruyama T, et al. Actual evidence in the medical approach to adolescents with idiopathic scoliosis. Eur J Phys Rehabil Med 2014;50:87–92. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=24622050&dopt=Abstract [PubMed] [Google Scholar]
- 10.Wood G. Brace modifications that can result in improved curve correction in idiopathic scoliosis. Scoliosis 2014;9:2. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=24593984&dopt=Abstract 10.1186/1748-7161-9-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schiller JR, Thakur NA, Eberson CP. Brace management in adolescent idiopathic scoliosis. Clin Orthop Relat Res 2010;468:670–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=19484317&dopt=Abstract 10.1007/s11999-009-0884-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zaina F, De Mauroy JC, Grivas T, Hresko MT, Kotwizki T, Maruyama T, et al. Bracing for scoliosis in 2014: state of the art. Eur J Phys Rehabil Med 2014;50:93–110. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=24622051&dopt=Abstract [PubMed] [Google Scholar]
- 13.Smith VA, Coffman CJ, Hudgens MG. Interpreting the Results of Intention-to-Treat, Per-Protocol, and As-Treated Analyses of Clinical Trials. JAMA 2021;326:433–4. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34342631&dopt=Abstract 10.1001/jama.2021.2825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weiss HR. “Brace technology” thematic series - the Gensingen brace™ in the treatment of scoliosis. Scoliosis 2010;5:22. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=20942970&dopt=Abstract 10.1186/1748-7161-5-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Steen H, Pripp AH, Lange JE, Brox JI. Predictors for long-term curve progression after Boston brace treatment of idiopathic scoliosis. Eur J Phys Rehabil Med 2021;57:101–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33016064&dopt=Abstract 10.23736/S1973-9087.20.06190-0 [DOI] [PubMed] [Google Scholar]
- 16.Liu D, Yang Y, Yu X, Yang J, Xuan X, Yang J, et al. Effects of Specific Exercise Therapy on Adolescent Patients With Idiopathic Scoliosis: A Prospective Controlled Cohort Study. Spine 2020;45:1039–46. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32675606&dopt=Abstract https://doi.org/ 10.1097/BRS.0000000000003451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weinstein SL, Dolan LA, Wright JG, Dobbs MB. Design of the Bracing in Adolescent Idiopathic Scoliosis Trial (BrAIST). Spine 2013;38:1832–41. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=24026162&dopt=Abstract 10.1097/01.brs.0000435048.23726.3e [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Negrini S, Negrini F, Fusco C, Zaina F. Idiopathic scoliosis patients with curves more than 45 Cobb degrees refusing surgery can be effectively treated through bracing with curve improvements. Spine J 2011;11:369–80. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=21292562&dopt=Abstract 10.1016/j.spinee.2010.12.001 [DOI] [PubMed] [Google Scholar]
- 19.Lusini M, Donzelli S, Minnella S, Zaina F, Negrini S. Brace treatment is effective in idiopathic scoliosis over 45°: an observational prospective cohort controlled study. Spine J 2014;14:1951–6. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=24295798&dopt=Abstract 10.1016/j.spinee.2013.11.040 [DOI] [PubMed] [Google Scholar]
- 20.Zhu Z, Xu L, Jiang L, Sun X, Qiao J, Qian BP, et al. Is Brace Treatment Appropriate for Adolescent Idiopathic Scoliosis Patients Refusing Surgery With Cobb Angle Between 40 and 50 Degrees. Clin Spine Surg 2017;30:85–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28207617&dopt=Abstract 10.1097/BSD.0b013e3182a1de29 [DOI] [PubMed] [Google Scholar]
- 21.Verhofste BP, Whitaker AT, Glotzbecker MP, Miller PE, Karlin LI, Hedequist DJ, et al. Efficacy of bracing in skeletally immature patients with moderate-severe idiopathic scoliosis curves between 40° and 60°. Spine Deform 2020;8:911–20. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32394324&dopt=Abstract 10.1007/s43390-020-00131-3 [DOI] [PubMed] [Google Scholar]
- 22.Aulisa AG, Guzzanti V, Falciglia F, Giordano M, Galli M, Aulisa L. Brace treatment of Idiopathic Scoliosis is effective for a curve over 40 degrees, but is the evaluation of Cobb angle the only parameter for the indication of treatment? Eur J Phys Rehabil Med 2019;55:231–40. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29517186&dopt=Abstract 10.23736/S1973-9087.18.04782-2 [DOI] [PubMed] [Google Scholar]
- 23.Razeghinezhad R, Kamyab M, Babaee T, Ganjavian MS, Bidari S. The Effect of Brace Treatment on Large Curves of 40° to 55° in Adolescents With Idiopathic Scoliosis Who Have Avoided Surgery: A Retrospective Cohort Study. Neurospine 2021;18:437–44. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34634198&dopt=Abstract 10.14245/ns.2040654.327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zaina F, Cordani C, Donzelli S, Lazzarini SG, Arienti C, Del Furia MJ, et al. Bracing Interventions Can Help Adolescents with Idiopathic Scoliosis with Surgical Indication: A Systematic Review. Children (Basel) 2022;9:1672. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=36360400&dopt=Abstract 10.3390/children9111672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Aubin CE, Labelle H, Ruszkowski A, Petit Y, Gignac D, Joncas J, et al. Variability of strap tension in brace treatment for adolescent idiopathic scoliosis. Spine 1999;24:349–54. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=10065519&dopt=Abstract 10.1097/00007632-199902150-00010 [DOI] [PubMed] [Google Scholar]
- 26.Mac-Thiong JM, Petit Y, Aubin CE, Delorme S, Dansereau J, Labelle H. Biomechanical evaluation of the Boston brace system for the treatment of adolescent idiopathic scoliosis: relationship between strap tension and brace interface forces. Spine 2004;29:26–32. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=14699272&dopt=Abstract 10.1097/01.BRS.0000103943.25412.E9 [DOI] [PubMed] [Google Scholar]
- 27.Rigo M, Negrini S, Weiss HR, Grivas TB, Maruyama T, Kotwicki T; SOSORT. ‘SOSORT consensus paper on brace action: TLSO biomechanics of correction (investigating the rationale for force vector selection)’. Scoliosis 2006;1:11. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=16857045&dopt=Abstract 10.1186/1748-7161-1-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Clin J, Aubin CE, Parent S, Sangole A, Labelle H. Comparison of the biomechanical 3D efficiency of different brace designs for the treatment of scoliosis using a finite element model. Eur Spine J 2010;19:1169–78. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=20094736&dopt=Abstract 10.1007/s00586-009-1268-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Karam JA, Eid R, Kreichati G, Abiad R, Kharrat K, Ghanem IB. Optimizing the vertical position of the brace thoracic pad: apical rib or apical vertebra? Orthop Traumatol Surg Res 2019;105:727–31. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30956156&dopt=Abstract 10.1016/j.otsr.2019.03.004 [DOI] [PubMed] [Google Scholar]
- 30.Karol LA, Virostek D, Felton K, Jo C, Butler L. The Effect of the Risser Stage on Bracing Outcome in Adolescent Idiopathic Scoliosis. J Bone Joint Surg Am 2016;98:1253–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27489315&dopt=Abstract 10.2106/JBJS.15.01313 [DOI] [PubMed] [Google Scholar]
- 31.Clin J, Aubin CÉ, Sangole A, Labelle H, Parent S. Correlation between immediate in-brace correction and biomechanical effectiveness of brace treatment in adolescent idiopathic scoliosis. Spine 2010;35:1706–13. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=21330954&dopt=Abstract 10.1097/BRS.0b013e3181cb46f6 [DOI] [PubMed] [Google Scholar]
- 32.Hawary RE, Zaaroor-Regev D, Floman Y, Lonner BS, Alkhalife YI, Betz RR. Brace treatment in adolescent idiopathic scoliosis: risk factors for failure-a literature review. Spine J 2019;19:1917–25. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31325626&dopt=Abstract 10.1016/j.spinee.2019.07.008 [DOI] [PubMed] [Google Scholar]
- 33.Xu L, Qin X, Qiu Y, Zhu Z. Initial Correction Rate Can be Predictive of the Outcome of Brace Treatment in Patients With Adolescent Idiopathic Scoliosis. Clin Spine Surg 2017;30:E475–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28437355&dopt=Abstract 10.1097/BSD.0000000000000343 [DOI] [PubMed] [Google Scholar]
- 34.Goodbody CM, Asztalos IB, Sankar WN, Flynn JM. It’s not just the big kids: both high and low BMI impact bracing success for adolescent idiopathic scoliosis. J Child Orthop 2016;10:395–404. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=27501808&dopt=Abstract 10.1007/s11832-016-0763-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zheng Y, Dang Y, Yang Y, Li H, Zhang L, Lou EH, et al. Whether Orthotic Management and Exercise are Equally Effective to the Patients With Adolescent Idiopathic Scoliosis in Mainland China?: A Randomized Controlled Trial Study. Spine 2018;43:E494–503. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28885287&dopt=Abstract 10.1097/BRS.0000000000002412 [DOI] [PubMed] [Google Scholar]
- 36.Negrini S, Donzelli S, Negrini A, Parzini S, Romano M, Zaina F. Specific exercises reduce the need for bracing in adolescents with idiopathic scoliosis: A practical clinical trial. Ann Phys Rehabil Med 2019;62:69–76. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30145241&dopt=Abstract 10.1016/j.rehab.2018.07.010 [DOI] [PubMed] [Google Scholar]
- 37.Monticone M, Ambrosini E, Cazzaniga D, Rocca B, Ferrante S. Active self-correction and task-oriented exercises reduce spinal deformity and improve quality of life in subjects with mild adolescent idiopathic scoliosis. Results of a randomised controlled trial. Eur Spine J 2014;23:1204–14. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=24682356&dopt=Abstract https://doi.org/ 10.1007/s00586-014-3241-y [DOI] [PubMed] [Google Scholar]
- 38.Schreiber S, Parent EC, Hedden DM, Moreau M, Hill D, Lou E. Effect of Schroth exercises on curve characteristics and clinical outcomes in adolescent idiopathic scoliosis: protocol for a multicentre randomised controlled trial. J Physiother 2014;60:234, discussion 234. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=25439713&dopt=Abstract 10.1016/j.jphys.2014.08.005 [DOI] [PubMed] [Google Scholar]
- 39.Weinstein SL, Zavala DC, Ponseti IV. Idiopathic scoliosis: long-term follow-up and prognosis in untreated patients. J Bone Joint Surg Am 1981;63:702–12. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=6453874&dopt=Abstract 10.2106/00004623-198163050-00003 [DOI] [PubMed] [Google Scholar]
- 40.Ascani E, Bartolozzi P, Logroscino CA, Marchetti PG, Ponte A, Savini R, et al. Natural history of untreated idiopathic scoliosis after skeletal maturity. Spine 1986;11:784–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=3810293&dopt=Abstract 10.1097/00007632-198610000-00007 [DOI] [PubMed] [Google Scholar]
- 41.Weinstein SL, Ponseti IV. Curve progression in idiopathic scoliosis. J Bone Joint Surg Am 1983;65:447–55. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=6833318&dopt=Abstract 10.2106/00004623-198365040-00004 [DOI] [PubMed] [Google Scholar]