Abstract
INTRODUCTION
One of the most common disabling complications in breast cancer (BC) patients is breast cancer-related lymphedema (BCRL), a pathological condition affecting both physical and psychological function, with detrimental consequences on health-related quality of life (HR-QoL). Rehabilitation has a key role in the comprehensive management of this condition with several studies reporting positive results after performing complex decongestive therapies (CDT) in these women. Kinesio taping (KT) is a rather recent therapeutic approach to treat BCRL, however, evidence in literature regarding its effectiveness is far from being fully characterized. Therefore, this systematic review aimed at assessing the role of KT among the CDT to treat BCRL.
EVIDENCE ACQUISITION
PubMed, Scopus, and Web of Science were systematically searched from inception until May 5th, 2022 to determine randomized control trials (RCTs) reporting patients with BCRL; KT as intervention; limb volume as outcome (PROSPERO number: CRD42022349720).
EVIDENCE SYNTHESIS
Out of the documents identified, 123 were eligible for data screening, and only 7 RCTs satisfied the eligibility criteria and were included. We found that KT might have a positive effect on limb volume reduction in patients with BCRL, albeit there is little evidence for low quality of the included studies.
CONCLUSIONS
Taken together, this systematic review showed that KT did not significantly reduce the upper limb volume in BCRL women, albeit it seemed to increase the flow rate during the passive exercise. Further high-quality-studies are mandatory to improve the knowledge in order to include the KT might into a multidisciplinary rehabilitative approach for the management of BC survivors affected by lymphedema.
Key words: Breast neoplasms, Lymphedema, Breast cancer lymphedema, Rehabilitation
Introduction
Breast cancer (BC) is the malignancy with the highest incidence in women, and its prevalence is continuously rising worldwide.1, 2 To date, recent advances in therapeutic interventions significantly reduced BC-related death rates with an increasing number of BC survivors, leading to a high prevalence of disabling sequelae of cancer and its treatments, including Breast Cancer-Related Lymphedema (BCRL).3, 4
BCRL is defined as arm oedema in BC patients induced by axillary lymphatic flow interruption, and it is an aggregation of protide-rich fluids that generate consistent swelling of the involved part of the body.5, 6 The progressive abnormal accumulation of fluid in the interstitial space, if left untreated, activates a damaging event cascade culminating in adipose deposit and fibrosis. Thus, chronic and disabling core of lymphedema might enclose a harmful impact on the physical and psychosocial well-being of BC survivors.4 Moreover, it has been widely established that lymphedema impacts body image, decreases self-esteem, provokes discomfort, functional impairment, pain, depression, anxiety, affecting family and social relations, with detrimental consequences on health-related quality of life (HR-QoL).7-9 To date, several risk factors have been identified to play a role in lymphedema onset, including extensive axillary disease, obesity, positive axillary lymph nodes, radiation therapy, and tumor-specific features.10, 11
In this scenario, a comprehensive rehabilitation approach is needed to target the multidimensional effects of lymphedema with physical therapy, weight management, and dietary supplements to reduce upper limb volume and improve overall well-being of patients with BCRL.12-16 Following the current guidelines,14 BCRL should be treated conservatively with a complete decongestive therapy (CDT), as well as physical exercise, manual lymphatic drainage, and multilayer compression bandages.17-20 Moreover, an early and appropriate intervention can lead to a diminishing complication incidence, improving the prognosis of the clinical status.21-23 On the other hand, surgical management should be taken into account in advanced stages, if conservative treatments are no more effective.12, 24, 25
In the recent years, new rehabilitation techniques have been proposed to alleviate edema, pain, and sensorial dysfunction of the upper limbs related to BCRL.6, 26 In particular, growing attention in scientific literature has been raised to kinesio taping (KT) which has been proposed as a safe and effective rehabilitation therapy for several diseases.27-31 This novel rehabilitation technique has been developed by Dr. Kenzo Kase and consists of elastic adhesive tape that might promote the activation of blood microcirculation and lymphatic drainage through the elevation of the skin and facilitating passage of lymph to the vascular system.32
KTs stretch the skin lightly, developing space between the dermis and fascia.33 In this scenario, it has been proposed that KT effects are quite comparable to compression treatment since it diminishes capillary filtration instead than enhancing. Moreover, KT might have overlapping features with manual lymphatic drainage, with therapeutic effects that can persist up to 24 hours.17
Therefore, KT would seem to increase lymphatic flow and could be used in the treatment of BCRL, relieving tissue fluid congestion, increasing blood and lymphatic microcirculation, but above all subcutaneous lymphatic drainage.34
Albeit KT has been proposed as a promising non-pharmacological intervention to manage BCRL, Smile et al.35 recently underlined a large gap of knowledge about the optimal therapeutic strategies for improving symptoms and reducing limb volume in patients with lymphedema.
Previous systematic reviews36-38 failed to demonstrate significant advantages of KT compared to other treatments. As a result, its role in a comprehensive rehabilitation approach is far from being fully characterized.
Therefore, this systematic review of randomized controlled trials (RCTs) aimed to update the state of the art about KT use in BCRL to describe the state-of-art of the evidence supporting KT to be part of the comprehensive rehabilitative management of BCRL patients.
Evidence acquisition
Search strategy
In this systematic review of RCTs, PubMed, Web of Science, and Scopus were systematically searched for articles published from the inception until September 30th, 2022, for distinctive databases, through the procedure described in Table I.
Table I. —Keyword search strategy for each database.
|
PubMed (“breast cancer” OR “breast neoplasm” OR “breast cancer related lymphedema”) AND (“edema” OR “oedema” OR “lymphedema” OR “lymphedema volume” OR “lymphoedema volume” OR “upper limb volume” OR “upper extremity volume” OR “cirtometry”) AND (“kinesiotaping” OR “kinesiotape” OR “tape” OR “taping” OR “kinesio tape” OR “kinesio taping” OR “physiotape”) |
|
Scopus TITLE-ABS-KEY(((“breast cancer” OR “breast neoplasm” OR “breast cancer related lymphedema”) AND (“edema” OR “oedema” OR “lymphedema” OR “lymphedema volume” OR “lymphoedema volume” OR “upper limb volume” OR “upper extremity volume” OR “cirtometry”) AND (“kinesiotaping” OR “kinesiotape” OR “tape” OR “taping” OR “kinesio tape” OR “kinesio taping” OR “physiotape”))) |
|
Web of Science ((“breast cancer” OR “breast neoplasm” OR “breast cancer related lymphedema”) AND (“edema” OR “oedema” OR “lymphedema” OR “lymphedema volume” OR “lymphoedema volume” OR “upper limb volume” OR “upper extremity volume” OR “cirtometry”) AND (“kinesiotaping” OR “kinesiotape” OR “tape” OR “taping” OR “kinesio tape” OR “kinesio taping” OR “physiotape”)) |
In addition, two reviewers performed a further manual search of the references of previous systematic reviews on analogous topics. All the methodological approaches of this systematic review respected the guidance of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines39 and the Cochrane Handbook for Systematic Reviews of Interventions.40 The study protocol has been registered to the International prospective register of systematic reviews (PROSPERO, registration number: CRD42022349720).
Selection criteria
All the potential articles were independently screened by two reviewers for eligibility after removing duplicates. Any disagreement has been settled with a third reviewer consultation. Through a PICO model, all papers were evaluated for eligibility. More in detail the PICO was:
-
participants involved patients with post-surgical BCRL diagnosis;
-
interventions involved rehabilitative approaches including KT for lymphatic drainage, administered in combination with other rehabilitation treatments or alone;
-
comparison will be conventional rehabilitation;
outcome measure consisted of upper limb volume changes, assessed with any quantification method.
-
-
We included only RCTs published in international peer-reviewed Journals. We excluded: 1) studies on children; 2) papers with a language other than English; 3) pilot study design; 4) full-text unavailability; 5) animal models manuscripts.
Data extraction and data synthesis
The data extraction was carried out independently by two reviewers through a customized sheet on Microsoft Excel. In case of extractive discrepancies, the agreement was reached through the involvement of a third auditor. Data extraction followed a descriptive approach: authors, nation, sample size, age (year), severity of lymphedema, intervention, control, outcome main findings. After the extraction, all data have been synthesized independently by two different authors from full-text documents. Any disagreement has been settled with a third reviewer consultation.
The results were provided as a descriptive summary through text and tables, to ensure a clear explanation of the characteristics and major findings of the included studies.
Risk of bias assessment
The estimation of the methodological quality of the included studies was conducted through the adoption of the risk of bias in version 2 of the Cochrane risk-of-bias tool for randomized trials (RoB 2). Two authors distinctly assessed each paper, and any divergences were resolved involving a third author. Bias degree was described RoB 2 domains: 1) randomization model; 2) allocation disguise; 3) participants and personnel blinding; 4) outcome valuation blinding; 5) outcome data report; 6) selective reporting of results; 7) other potential bias.
Evidence synthesis
Study characteristics
The applied research strategy found a total of 271 articles in the aforementioned databases. After the removal of the duplicate articles (N.=148), 123 manuscripts were reviewed and filtered by title and abstract, leading to the exclusion of 101 articles. Out of 22 full-text articles assessed for eligibility, 7 studies41-47 were included in this systematic review, as illustrated by the PRISMA 2020 Flow diagram (Figure 1).
Figure 1.
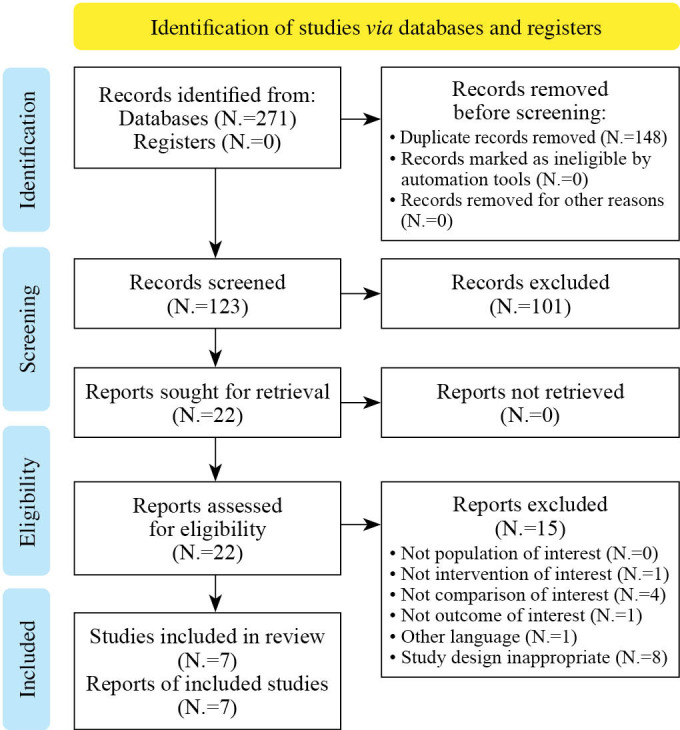
—PRISMA 2020 flow diagram for systematic review.
The main characteristics of the studies included in the present systematic review were reported by Table II.41-47
Table II. —Main characteristics of the studies included in the systematic review.
| Authors | Nation | Sample | Age (year) | Severity of lymphedema | Intervention | Control | Outcome | Main findings |
|---|---|---|---|---|---|---|---|---|
| Basoglu C. et al.41 | Türkiye | Total: N.=.40 Group 1: 20 Group 2: 20 |
Tot: NA Group 1: 53.7±8.6 Group 2: 53.4±8.3 |
Grade II | Group 1: 5-cm wide standard tapes (Kinesio® Tex Classic). A total of 6 tapes, 3 above the elbow and 3 below the elbow | Group 2: physiotherapist for the first week, 5 days a week. MLD, compression bandages, exercise, and skincare. MLD was applied to the side of the affected limb quadrant, starting at the base of the neck and then progressing to the limb. | Circumference difference (cm), volume difference (mL), Grip strength (kg), Q-DASH, Fact-B. Data were collected at T0 (baseline) and at T1 (4 weeks). | There was no significant difference between the two groups in terms of clinical improvements even with respect to the initial assessment of all outcomes (P>0.05). |
| Ozsoy-Unubol, T. et al.42 | Türkiye | Tot: N.=35 Group 1: 16 Group 2: 19 |
Tot: NA Group 1: 50.5±6.4 Group 2: 54.5±7.4 |
Grade I | Group 1: KT was applied at intervals in three-four days intervals for four weeks. KT was performed on the arms and forearms with a 4-fan type tape. The anchor started without tension and the tails of the 15% tension tape were applied to the medial, anterior, and posterior aspects of distal affected upper limb. | Group 2: patients were treated daily with CGs for 23 hours, preventive measures, education, and exercises. | Circumference measurements (cm). the shoulder range of motion (ROM) was measured with a goniometer, and pain, heaviness, and the sensation of tightness were assessed with a Visual Analog Scale (VAS). | Both groups had decreases in all classes of arm circumference differences at the end of the therapy and at three-month follow-up. Significant differences were detected early post treatment in the wrist, 15 cm distal from ME, and within the ME of the CG group. |
| Pajero Otero, V. et al.43 | Spain | Tot: N.=30 Group 1: 15 Group 2: 15 |
Tot: NA Group 1: Group 2: |
Grade II/III | Group 1 received KT (24 h/day during 4 weeks and replaced every week) followed by therapy with CGs. KT consisted of parallel strips, 1.25 cm wide, covering the distal affected upper limb in a spiral model, starting from the contralateral axilla, passing through the patient’s back. | Group 2 received compression garments which were followed by kinesio taping. | Relative change in volume and the relative change in volume of BRCL upper limb. shoulder ROM, and pain, heaviness, and the sensation of tightness were assessed with a 5-points Likert Scale. | Kinesio taping decreases BCRL lymphedema during its keeping phase compared to CGs. Moreover, upper limb ranges of motion improve significantly after KT application. |
| Pekyavaş, N.Ö. et al.44 | Türkiye | Tot: N.=45 Group 1: 15 Group 2: 15 Group 3: 15 |
Tot: NA Group 1: 56.5±9.4 Group 2: 49.6±10.5 Group 3: 58±8.5 |
Grade II/III | CDT consisting of skin care, MLD, compression application, and exercise program, with KT lymphatic correction application Each intervention underwent five sessions per week in the 2-week treatment program | The second group underwent CDT enclosing skin care, short-stretch multilayer compression application, MLD, and an exercise program. The third group likewise performed CDT consisting of skin care, MLD, compression application, and exercise program, but KT lymphatic correction application was applied under the bandage |
Lymphedema volume (mL). SF-36. VAS was used to assess stiffness, numbness, heaviness and discomfort. Assessment timepoints were set before and at the end of therapy (10th day) and a follow-up visit one month after the end of treatment. | The combination of KT with CDT (skincare, MLD and exercise) might have encouraging results on diminishing the BCRL symptoms |
| Tantawy, S.A. et al.45 | Egypt | Tot: N.=59 Group 1: 30 Group 2: 29 |
Tot: NA Group 1: 54.3±4.16 Group 2: 55.15±.27 |
Grade II/III | Group 1 underwent 2 KT sessions per 3 weeks. The KT involved one fan shape for the chest, 2 fan respectively for the arm, and the forearm, and lastly one fan for the wrist. | Group 2 underwent CGs (20-60 mmHg) daily for at least 15 hours for three weeks. | Circumference measurements (cm). SPADI, handgrip strength, and quality of life (EORTC QLQ-C30). pre and post 3 weeks of intervention | Significant reduction in limb circumference was demonstrated in the KT group. Moreover there was a significant impact in SPADI score, handgrip strength, and overall QoL at the end of the treatment (P<0.05) compared to PG group |
| Taradaj, J. et al.46 | Poland | Tot: N.=70 Group 1: 22 Group 2: 23 Group 3: 25 |
Tot: NA Group 1: 60.3±4.2 Group 2: 63.2±5.1 Group 3: 62.4±4.8 |
Grade II/III | Group 1 underwent KT (6 fans, up to 15% stretch) with MLD and intermittent pneumatic compression. KT included two fans from elbow to fingers, two fans from the axilla to the elbow, one fan from axillary nodes along the chest to the unaffected axillary side, and one from the inguinal region on the affected side along the trunk to the axillary contralateral side. | Group 2: sham KT combined with intermittent pneumatic compression and MLD. An adhesive had the same colour of KT, but without therapeutic characteristics. Methodology and application were the same as in group A. Group 3: Standard procedure (intermittent pneumatic compression and MLD and multilayered bandaging. |
Limb volume (cm3), handgrip strength, Range of motion was evaluated with standard goniometric measurement was performed (Baseline device; Technomex). The BCRL volume was assessed using an optoelectronic perometer. Timepoints were set at T0 (baseline) and at T1 (4 weeks). | After the treatment, KT reported a not significant reduction of grade II and III of BCRL. |
| Torres Lacomba, M. et al.47 | Spain | Tot: N.= 146 Group I: 29 Group 2: 28 Group 3: 30 Group 4: 29 Group 5: 30 |
Tot: NA Group 1: 59.6±10.6 Group 2: 58 11.4 Group 3: 56.2±11.5 Group 4: 58±13.8 Group 5: 59.8±9.4 |
Grade I/II | Group I underwent KT with 15-20% tension. KT included 2 fans (4 strap≠s) for shoulder, 2 fans (4 straps) for elbow, and 2 fans (4 straps) for wrist. | Group 2: Multilayer bandage group Group 3: simplified multilayer group Group 4: Cohesive group Group 5: Adhesive group |
Percentage excess volume change. Other outcomes measured were heaviness and tightness symptoms, and bandage or tape perceived comfort with a 10-point scale | Simplified multilayer seems more effective and more comfortable than multilayer bandage. Cohesive bandage seems as effective as simplified multilayer and multilayer bandage. Nevertheless, KT appeared to be the least effective |
M: male, F: female; KT: kinesio tape; MLD: manual lymphatic drainage; MMDC: moisture meter-D compact; CDT: complex decongestive therapy; CG: compression garment.
Kinesio taping
An overview with pictures of the different KT applications is depicted in Figure 2,41-47 to fully understand the procedures. Basoglu et al.41 administered one KT session per week for four weeks protocol. The authors used six tapes, three above and three below the elbow, with spiral and cross shapes along the arm, forearm, and anterior axillary-axillary anastomoses on the affected extremity (as depicted by Figure 2A).
Figure 2.
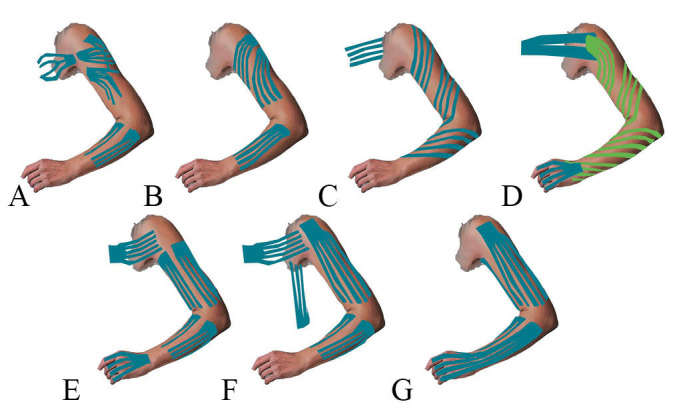
—Kinesio tape application methods (A: Basoglu et al.;41 B: Ozsoy-Unubol et al.;42 C: Pajero Otero et al.;43 D: Pekyavaş et al.;44 E: Tantawy et al.;45 F: Taradaj et al.;46 G: Torres Lacomba et al.47).
The tape length was adjusted according to the patient’s limb size. The tape preparation involved 4-lane (4 strip fan cut) and the 5 cm-section with the end left uncut. The uncut (anchor) end of the tape was placed near the unaffected lymph node and in accordance with the direction of the lymphatic flow. Ozsoy-Unubol et al.42 applied KT on the arms and forearms with a 4 fan strip type with a no tension anchor, while the 15% tension tails on the anterior, medial, and posterior facets of the forearms and arms (Figure 2B). Pajero Otero et al.43 used 1.25 cm wide strips starting from the contralateral axilla, along the patient’s back, and spiraling over the upper limb to the affected carpus (Figure 2C). No tension has been set on the already stretched skin to generate convolutions. Taping was maintained 24 hours per day for 4 weeks, eventually replaced every week. Pekyavaş et al.44 involved skin care education, self- lymphatic drainage instruction, exercise protocol, and a KT Lymphatic Correction Method administered with two fans on the chest, a 5-strip tape arranged in a spiral up to the wrist with a following fan on the carpus up to the 5 fingers of the hand affected by the disorder (Figure 2D). Tantawy et al.45 involved a KT application with one 5-strips fan shape through the thorax, two 4-strips fan for the upper limb, two 4-strips fan for the forearm, and one 2-strips fan shape for the wrist (Figure 2E). Taradaj et al.46 administered a KT (Nitto Denko, Osaka, Japan), for 4 days, once a week. The application consisted of 6 fans, up to 15% stretch, with MLD and intermittent pneumatic compression (Figure 2F). KT included two fans from elbow to fingers, two fans from the axilla to the elbow, one fan from axillary nodes along the chest to the unaffected axillary side, and one from the inguinal region on the affected side along the trunk to the axillary contralateral side. Torres-Lacomba et al.47 applied KT with 15-20% tension, applying 6 different fans (12 straps) for the upper limb with 2 fans for shoulder, 2 fans for elbow, and 2 fans for wrist (Figure 2G).
Outcome measures
Circumference differences between the upper limbs were measured by three authors42, 44, 47 with a nonelastic strip at five limb levels including metacarpophalangeal joint, the wrist, 15 cm distally from the medial epicondyle, the elbow, and 15 cm proximally from the medial epicondyle. In two trials,33, 41 limb circumference measurements were performed at four levels, the metacarpophalangeal joints, the wrists, 10 cm distal from lateral epicondyles, and 12 cm proximal from lateral epicondyles, as per the American Cancer Society’s treatment manual while the patient was sitting upright in a chair with the shoulder in 90-degree flexion. A 9-mm wide, bendable, and non-elastic tape with a sensitivity level 0.1 cm was used for in circumferential. Limb volumes were determined by using the circumferential measurements in the Frustum formula (truncated cone formula). Taradaj J et al.46 assessed the limb volume, using an optoelectronic Perometer 400 T (Pero-System Messgerate GmbH, Wuppertal, Germany). Tantawy SA et al.45 assessed circumference measurements at metacarpal bones,midhand, at 3 cm distally from the styloid process of the ulna and 45 cm proximally from the same reference point. The nonelastic strip measure was placed around the extremity to avoid any potential slacking.
Furthermore, Pajero Otero et al.43 assessed the relative volume variation of the BCRL through an algorithm (RVC = ((A2/U1)/(U2/A1)) − 1), where A1 and A2 are the volume of the affected upper limb at two diverse time points, and U1 and U2 are the volumes of the unaffected upper limb.
Basoglu et al.41 and Tantawy et al.45 assessed grip strength using a Jamar hydraulic hand dynamometer with readings in kilograms. Moreover, Taradaj et al.46 assessed hand grip strength using Hercules dynamometer (Technomex) with readings in Newton. Additionally, Ozsoy-Unubol et al.,42 Taradaj et al.,46 and Pajero Otero et al.43 measured the shoulder range of motion (ROM) with a goniometer. Three authors42, 44, 47 evaluated pain, heaviness, and the sensation of tightness with a Visual Analog Scale (VAS).
Regarding functioning, Basoglu et al.41 utilized the 11-item Quick-Disabilities of the Arm, Shoulder and Hand (Q-DASH) questionnaire to determine the upper limb functional level on a 5-point Likert scale (with 1= “no difficulty” and 5= “greatest difficulty”). Tantawy et al.45 used SPADI to measure shoulder pain and disability, incorporating 13 items calculating 2 domains: 5 items on pain and 8 items on disability.
Pekyavaş et al.44 assessed QoL with Short-Form 36 (SF-36), a multi-item score able to evaluate eight health domains each between 2 and 10 questions: physical functioning (PF), role limitations due to physical problems (RP), bodily pain (BP), general health perception (GH), vitality (VT), social functioning (SF), role limitations due to emotional problems (RE), and mental health (MH). Moreover, Basoglu et al.41 used the Functional Assessment of Cancer Therapy-Breast (FACT-B) for the assessment of quality of life. Lastly, Tantawy et al.45 used the quality of life by cancer-specific questionnaire (EORTC QLQ-C30), with 30 questions, including functional scores (physical, social, emotional, and cognitive aspects).
Qualitative syntheses of the study results
Physical effects
Torres-Lacomba et al.47 underlined that KT was the less effective treatment in reducing limb volume compared to other approaches (P<0.001). Similarly, Taradaj et al.46 demonstrated no significant limb volume reduction for grades II and III of BCRL after a comprehensive rehabilitation treatment including KT compared to comprehensive rehabilitation treatment including multilayer bandage. Nevertheless, Ozsoy-Unubol et al.42 assessed grades I of BCRL, highlighting that KT group and compression garments group significantly decreased (P<0.05) all classes of arm circumference differences at the end of the therapy and at three-month follow-up, without significant differences in limb measures between groups. Moreover, Pajero Otero et al.43 reported that KT with spiral application could reduce BCRL lymphedema volume compared to CGs, with a volume change of -5.7±2% of KT compared to -3.4±2.9% of CG. Tantawy et al.45 underlined a significant reduction in limb circumference with the KT and significant changes in terms of handgrip strength test. Similarly, Pajero Otero et al.43 reported significant functional improvement for upper limb ranges of motion in patients receiving KT application. On the other hand, Basoglu et al.41 did not report significant differences between the two groups in terms of limb circumferences, handgrip muscle strength, and Q-DASH.
Psychological effects
Pekyavaş et al.44 reported that the combination of a KT spiral pattern with CDT (skincare, MLD and exercise) might have encouraging results on diminishing the BCRL symptoms assessed with with SF-36 and VAS. In accordance, Tantawy et al.45 underlined a significant impact on SPADI score and overall QoL (P<0.05), with significant differences compared to CG. On the contrary, Basoglu et al.41 reported no significant difference between the two groups in terms of clinical improvements even with respect to the initial assessment of all clinical outcomes, including the FACT-B. Lastly, Torres-Lacomba et al.47 reported that KT was perceived as the most comfortable compression method compared to other treatments (P<0.001).
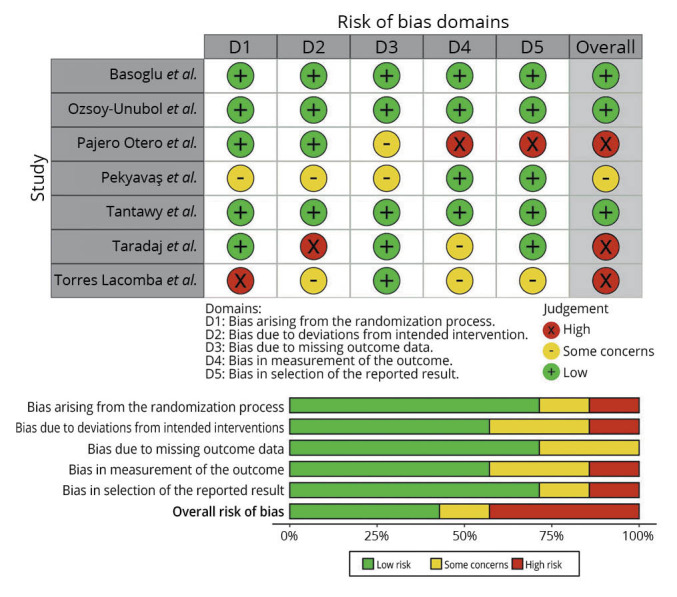
Risk of bias analysis
The risk of bias evaluation was assessed by RoB v.2, reporting that 3 studies (42.85%)43, 46, 47 were characterized by an overall high risk of bias. More in detail, only 1 study47 reported a high risk of bias in the randomization process, and only 1 paper43 showed a high risk in outcome measurement and result selection, as depicted in Figure 3.41-47
Figure 3.
Discussion
Lymphedema is one of the most frequent long-term sequelae after BC surgery approach with detrimental consequences on upper limb function and activities of daily living and account for a large percentage of the so called survivorship issues in BC women.48 To date, the gold standard treatment for BCRL is the CDT, a comprehensive rehabilitation program including skin care, MLD, multilayer compression bandaging, and lympho-kinetic exercises.32, 49, 50 On the other hand, KT has been recently proposed to have a role in BCRL management with growing literature supporting its advantages in BCRL care. To date, the impact of KT in the complex rehabilitation management of BCRL women is far from being fully characterized. Therefore, this systematic study aimed to update the state of the art of KT in the BC rehabilitation management to better address the critical issue of long terms management of BC survivors.
The results of the present systematic review suggested that KT might improve upper limb volume in patients with BCRL in the early phases, as a complement to conventional rehabilitative approaches. At the same time, it does not seem to be more effective than multilayer compressive bandaging and its practice also involves greater care. Nevertheless, it is a safe and well-tolerated technique for a multidisciplinary rehabilitative approach to cancer patients.45, 51, 52
It should be noted that to date few systematic reviews assessed the effects of KT in patients with BCRL,36-38 reporting no significant differences between KT and other treatments in terms of upper limb volume reduction. On the other hand, it should be noted that these systematic reviews included several reports with heterogeneous study designs, with significant implications for understanding comprehensive effects.36-38
Moreover, to the best of our knowledge, there are no good quality systematic reviews following relevant international guidelines and registered in an international registry. Lastly, most of the RCTs considered in our systematic review were published in the last few years and were not included in previous similar reviews,36-38 underlining that an up-to-date is necessary to clarify the role of KT in the rehabilitation approach to BCRL.
Our findings underlined that taping might be considered a complementary/alternative treatment that might improve the individualized management of BCRL patients. In this scenario, rehabilitation plays a pivotal role in improving HR-QoL of BC patients, with growing evidence supporting the effects of tailored rehabilitation programs improving symptoms in BC patients suffering from several disabling consequences, including BCRL, axillary web syndrome, cancer-related fatigue, osteoporosis, and hormone therapy related arthralgia.7, 53-55 In the recent years, growing efforts have been paid to the individualized management of BC survivors, targeting specific physical impairments related to cancers but also HR-QoL, frequently affected by physical and psychobiological consequences of cancer.7, 56, 57 BCRL is widely recognized as one of the most impactful conditions worsening HR-QoL in BC survivors; however, to date, the optimal rehabilitation approach includes several therapies aiming at reducing upper limb volume and improving HR-QoL, but the optimal combination of these treatments is still debated and the synergic effects between different rehabilitation modalities in terms of HR-QoL have to be clarified.
Interestingly, the results of our systematic review emphasized that there may be no standardized protocols for the application of KT in BCRL. In this scenario, it might partly explain the controversies in terms of effectiveness of KT intervention but might also underline that tailored strategies are needed to improve the clinical management of BC patients. On the other hand, it should be noted that, to date, there is no consensus about the optimal compression garment prescription or the optimal multilayer bandage, widely applied in clinical settings in the management of BCRL.53, 58
The positive effects of KT might be partly related to the improvement of the interstitial microcirculation, favoring the increase in blood and lymphatic flow and the absorption of liquid.4, 59 More in detail, the therapist generally adopts a level of tension generating an adequate level of traction on the skin. This traction stimulates an elevation of the epidermis and decreases the compression on the below the dermis, thus down-streaming nociceptive stimuli.60 Other suggested benefits seem to comprise enhanced blood and lymphatic circulation, declined pain perception, adjustment in the recruitment motion patterns of the treated muscles.61 Even though extensively practiced in clinical settings by many physiotherapists, our systematic review underlined conflicting results about its effectiveness in upper limb volume reduction.62 At the basis of these controversies, our data underlined several differences in application modalities, techniques, tension, location, duration, and frequency.41-47
Taken together, these data emphasized that standardized protocols are needed to improve knowledge about the optimal application method of KT in order to guide clinicians in a precise prescription of this promising component of CDT.14
Despite these considerations, several concerns about the optimal administration modalities still affect different well-consolidated components of CDT. Interestingly, the RCT by Torres-Lacomba et al.47 underlined significant advantages of multilayer compression garments compared to KT in terms of lymphedema volume. However, the authors underlined that KT might provide more comfort than CGs (P<0.001). Therefore, these findings suggested that KT should be considered in patients with low compliance to multilayer compression garments in order to optimize patient’s adherence to rehabilitation programs.
In line with previous reports underlining the key role of a holistic approach to cancer-related disability,63 it should be noted that most of the included studies compared KT with several other approaches (e.g.no treatment, sham taping, exercises, manual therapy, and garments). It has been proposed that KT and physical exercise might have a synergic role in BCRL management since lymphatic flow rate might increase during physical exercise due to thermal and mechanical processes. Interestingly, in this scenario, physical exercise might improve the overall well-being of cancer patients due to its positive effects on inflammation and oxidative stress.64 On the other hand, controversies are still open about its role in BCRL management and conflicting data are to date available on lymphedema volume effects.65-67 Taken together, the results of this systematic review might provide further evidence supporting the role of KT combined with physical exercise minimizing the negative effects of isometric muscle contraction in lymphatic flow and optimizing the role of muscle pump function during rhythmic muscle contraction and relaxation.68, 69 However, further trials are required to better describe the effects of physical exercise with or without KT in BC survivors suffering from BCRL.
Lastly, it should be noted that regardless of the comparative modality administrated or the outcome considered, the studies included in the present work generally reported an effect small enough not to be considered clinically valuable in favor of KT, or there were in outcome comparisons no significant differences between interventions. Nevertheless, Pajero-Otero et al. showed in a recent cross-over trial that KT was more satisfactory than multilayer bandaging, obtaining better DASH scores compared with CPT + IPC.70
In this scenario, most of the studies included measured upper limb volume with a centimetric method, calculating the volume of the limb indirectly with the truncated cone algorithm, providing only approximate results of the upper limb volume.46 Therefore, trials performing a precise volumetric assessment are still needed, implementing technological advances in the precise management of BCRL.71, 72 Furthermore, beyond the clinical efficacy of KT in terms of upper limb volume reduction, a multimodal patient assessment is needed to better characterize the functional implication of KT and its positive effects on HR-QoL.46 Lastly, the lack of meta-analysis is one of the main limitations of this systematic review. However, in accordance with the Cochrane Handbook for Systematic Review of Intervention (Ver, 6.1, 2020), the large heterogeneity of participants, intervention and outcomes did not allow to perform a meta-analysis, making it difficult to formulate a comprehensive evaluation.
Limitations of the study
Despite the intrinsic limitations of each study, it should be noted that the current systematic review is not free from limitations. First, the number of studies included is small, but only randomized controlled trials have been included providing specific data about the effectiveness of KT alone or combined with CDT. Second, the studies included assessed different application approaches of KT and different models of comparison. Therefore, it might be particularly difficult to draw a quantitative synthesis due to the heterogeneity of the study interventions.
Conclusions
KT showed to not have a significant efficacy in terms of upper limb volume reduction when compared to other rehabilitation treatments. However, this rehabilitative treatment (mostly with a spiral application of tape tail straps) seemed to increase the flow rate during a passive exercise, probably due to the thermal and mechanical processes in BCRL women.
In this context, KT could be taken into consideration for the multidisciplinary rehabilitative approach for BC survivors affected by lymphedema, albeit the low quality of the studies included might significantly affect the strength of these conclusions. Further trials assessing larger samples are needed to better characterize the efficacy of KT in BCRL patients.
References
- 1.Iacoviello L, Bonaccio M, de Gaetano G, Donati MB. Epidemiology of breast cancer, a paradigm of the “common soil” hypothesis. Semin Cancer Biol 2021;72:4–10. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32087245&dopt=Abstract 10.1016/j.semcancer.2020.02.010 [DOI] [PubMed] [Google Scholar]
- 2.Marcasciano M, Kaciulyte J, Mori FL, Lo Torto F, Barellini L, Loreti A, et al. Breast surgeons updating on the thresholds of COVID-19 era: results of a multicenter collaborative study evaluating the role of online videos and multimedia sources on breast surgeons education and training. Eur Rev Med Pharmacol Sci 2020;24:7845–54. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32744712&dopt=Abstract [DOI] [PubMed] [Google Scholar]
- 3.Drobot A, Bez M, Abu Shakra I, Merei F, Khatib K, Bickel A, et al. Microsurgery for management of primary and secondary lymphedema. J Vasc Surg Venous Lymphat Disord 2021;9:226–233.e1. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32446874&dopt=Abstract 10.1016/j.jvsv.2020.04.025 [DOI] [PubMed] [Google Scholar]
- 4.Abouelazayem M, Elkorety M, Monib S. Breast Lymphedema After Conservative Breast Surgery: An Up-to-date Systematic Review. Clin Breast Cancer 2021;21:156–61. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33358602&dopt=Abstract 10.1016/j.clbc.2020.11.017 [DOI] [PubMed] [Google Scholar]
- 5.Sharkey AR, King SW, Kuo RY, Bickerton SB, Ramsden AJ, Furniss D. Measuring Limb Volume: Accuracy and Reliability of Tape Measurement Versus Perometer Measurement. Lymphat Res Biol 2018;16:182–6. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28956715&dopt=Abstract 10.1089/lrb.2017.0039 [DOI] [PubMed] [Google Scholar]
- 6.Erdinç Gündüz N, Dilek B, Şahin E, Ellidokuz H, Akalın E. Diagnostic Contribution of Ultrasonography in Breast Cancer-Related Lymphedema. Lymphat Res Biol 2021;19:517–23. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33601960&dopt=Abstract 10.1089/lrb.2020.0068 [DOI] [PubMed] [Google Scholar]
- 7.Invernizzi M, Kim J, Fusco N. Editorial: Quality of Life in Breast Cancer Patients and Survivors. Front Oncol 2020;10:620574. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33312961&dopt=Abstract 10.3389/fonc.2020.620574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Paolucci T, Bernetti A, Bai AV, Segatori L, Monti M, Maggi G, et al. The sequelae of mastectomy and quadrantectomy with respect to the reaching movement in breast cancer survivors: evidence for an integrated rehabilitation protocol during oncological care. Support Care Cancer 2021;29:899–908. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32529493&dopt=Abstract 10.1007/s00520-020-05567-x [DOI] [PubMed] [Google Scholar]
- 9.Losco L, Bolletta A, de Sire A, Chen SH, Sert G, Aksoyler D, et al. The Combination of Lymph Node Transfer and Excisional Procedures in Bilateral Lower Extremity Lymphedema: Clinical Outcomes and Quality of Life Assessment with Long-Term Follow-Up. J Clin Med 2022;11:570. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=35160022&dopt=Abstract https://doi.org/ 10.3390/jcm11030570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ugur S, Arıcı C, Yaprak M, Mescı A, Arıcı GA, Dolay K, et al. Risk factors of breast cancer-related lymphedema. Lymphat Res Biol 2013;11:72–5. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=23772716&dopt=Abstract 10.1089/lrb.2013.0004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.de Sire A, Invernizzi M, Lippi L, Cisari C, Özçakar L, Franchignoni F. Blurred lines between axillary web syndrome and Mondor’s disease after breast cancer surgery: A case report. Ann Phys Rehabil Med 2020;63:365–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31121334&dopt=Abstract 10.1016/j.rehab.2019.04.007 [DOI] [PubMed] [Google Scholar]
- 12.de Sire A, Losco L, Lippi L, Spadoni D, Kaciulyte J, Sert G, et al. Surgical Treatment and Rehabilitation Strategies for Upper and Lower Extremity Lymphedema: A Comprehensive Review. Medicina (Kaunas) 2022;58:954. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=35888673&dopt=Abstract 10.3390/medicina58070954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Demark-Wahnefried W, Campbell KL, Hayes SC. Weight management and its role in breast cancer rehabilitation. Cancer 2012;118(Suppl):2277–87. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=22488702&dopt=Abstract 10.1002/cncr.27466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Executive Committee of the International Society of Lymphology . The diagnosis and treatment of peripheral lymphedema: 2020 Consensus Document of the International Society of Lymphology. Lymphology 2020;53:3–19. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32521126&dopt=Abstract [PubMed] [Google Scholar]
- 15.Paolucci T, Bernetti A, Bai AV, Capobianco SV, Bonifacino A, Maggi G, et al. The recovery of reaching movement in breast cancer survivors: two different rehabilitative protocols in comparison. Eur J Phys Rehabil Med 2021;57:137–47. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32406224&dopt=Abstract 10.23736/S1973-9087.20.06138-9 [DOI] [PubMed] [Google Scholar]
- 16.Paolucci T, Saggino A, Agostini F, Paoloni M, Bernetti A, Mangone M, et al. The influence of rehabilitation on quality of life in breast cancer survivors: A clinical study. Int J Environ Res Public Health 2021;18:8585. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34444332&dopt=Abstract 10.3390/ijerph18168585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Karafa M, Karafová A, Szuba A. The effect of different compression pressure in therapy of secondary upper extremity lymphedema in women after breast cancer surgery. Lymphology 2018;51:28–37. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30248729&dopt=Abstract [PubMed] [Google Scholar]
- 18.McLaughlin SA. Lymphedema: separating fact from fiction. Oncology (Williston Park) 2012;26:242–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=22545305&dopt=Abstract [PubMed] [Google Scholar]
- 19.Thompson B, Gaitatzis K, Janse de Jonge X, Blackwell R, Koelmeyer LA. Manual lymphatic drainage treatment for lymphedema: a systematic review of the literature. J Cancer Surviv 2021;15:244–58. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32803533&dopt=Abstract 10.1007/s11764-020-00928-1 [DOI] [PubMed] [Google Scholar]
- 20.Kilmartin L, Denham T, Fu MR, Yu G, Kuo TT, Axelrod D, et al. Complementary low-level laser therapy for breast cancer-related lymphedema: a pilot, double-blind, randomized, placebo-controlled study. Lasers Med Sci 2020;35:95–105. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31079232&dopt=Abstract 10.1007/s10103-019-02798-1 [DOI] [PubMed] [Google Scholar]
- 21.Muñoz-Alcaraz MN, Pérula-de-Torres LÁ, Serrano-Merino J, Jiménez-Vílchez AJ, Olmo-Carmona MV, Muñoz-García MT, et al. Efficacy and efficiency of a new therapeutic approach based on activity-oriented proprioceptive antiedema therapy (TAPA) for edema reduction and improved occupational performance in the rehabilitation of breast cancer-related arm lymphedema in women: a controlled, randomized clinical trial. BMC Cancer 2020;20:1074. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33167921&dopt=Abstract 10.1186/s12885-020-07558-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Naik M, Nayak P, Kumar KD. Effect of Physiotherapy in the Prevention and Relief of Secondary Lymphoedema in Subjects with Postoperative Breast Cancer- A Systematic Review of Randomised Controlled Trials. J Clin Diagn Res 2021. 10.7860/JCDR/2021/45745.14815 [DOI]
- 23.Lu SR, Hong RB, Chou W, Hsiao PC. Role of physiotherapy and patient education in lymphedema control following breast cancer surgery. Ther Clin Risk Manag 2015;11:319–27. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=25750536&dopt=Abstract [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bolletta A, di Taranto G, Losco L, Elia R, Sert G, Ribuffo D, et al. Combined lymph node transfer and suction-assisted lipectomy in lymphedema treatment: A prospective study. Microsurgery 2022;42:433–40. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34994481&dopt=Abstract 10.1002/micr.30855 [DOI] [PubMed] [Google Scholar]
- 25.Cigna E, Pierazzi DM, Sereni S, Marcasciano M, Losco L, Bolletta A. Lymphatico-venous anastomosis in chronic ulcer with venous insufficiency: A case report. Microsurgery 2021;41:574–8. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33991012&dopt=Abstract 10.1002/micr.30753 [DOI] [PubMed] [Google Scholar]
- 26.Marchica P, D’Arpa S, Magno S, Rossi C, Forcina L, Capizzi V, et al. Integrated treatment of breast cancer-related lymphedema: A descriptive review of the state of the art. Anticancer Res 2021;41:3233–46. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34230117&dopt=Abstract 10.21873/anticanres.15109 [DOI] [PubMed] [Google Scholar]
- 27.Vercelli S, Sartorio F, Foti C, Colletto L, Virton D, Ronconi G, et al. Immediate effects of kinesiotaping on quadriceps muscle strength: a single-blind, placebo-controlled crossover trial. Clin J Sport Med 2012;22:319–26. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=22450591&dopt=Abstract 10.1097/JSM.0b013e31824c835d [DOI] [PubMed] [Google Scholar]
- 28.Paoloni M, Bernetti A, Fratocchi G, Mangone M, Parrinello L, Del Pilar Cooper M, et al. Kinesio Taping applied to lumbar muscles influences clinical and electromyographic characteristics in chronic low back pain patients. Eur J Phys Rehabil Med 2011;47:237–44. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=21430611&dopt=Abstract [PubMed] [Google Scholar]
- 29.de Sire A, Curci C, Ferrara M, Losco L, Spalek R, Cisari C, et al. Efficacy of kinesio taping on hand functioning in patients with mild carpal tunnel syndrome. A double-blind randomized controlled trial. J Hand Ther 2021;S0894-1130(21)00058-2. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34256988&dopt=Abstract 10.1016/j.jht.2021.04.011 [DOI] [PubMed]
- 30.Arya KN, Pandian S, Puri V. Rehabilitation methods for reducing shoulder subluxation in post-stroke hemiparesis: a systematic review. Top Stroke Rehabil 2018;25:68–81. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29017429&dopt=Abstract 10.1080/10749357.2017.1383712 [DOI] [PubMed] [Google Scholar]
- 31.de Sire A, Moggio L, Demeco A, Fortunato F, Spanò R, Aiello V, et al. Efficacy of rehabilitative techniques in reducing hemiplegic shoulder pain in stroke: systematic review and meta-analysis. Ann Phys Rehabil Med 2022;65:101602. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34757009&dopt=Abstract 10.1016/j.rehab.2021.101602 [DOI] [PubMed] [Google Scholar]
- 32.Wang YX, Li HP, Jiang XX, Zhang MM, Wang HX, Ding XT. Overview of review on the prevention and treatment of breast cancer-related lymphedema. China J Cancer Prev Treat 2019;26:588–94. [Google Scholar]
- 33.Ergin G, Şahinoğlu E, Karadibak D, Yavuzşen T. Effectiveness of kinesio taping on anastomotic regions in patients with breast cancer-related lymphedema: A randomized controlled pilot study. Lymphat Res Biol 2019;17:655–60. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31329507&dopt=Abstract 10.1089/lrb.2019.0003 [DOI] [PubMed] [Google Scholar]
- 34.Malicka I, Rosseger A, Hanuszkiewicz J, Woźniewski M. Kinesiology Taping reduces lymphedema of the upper extremity in women after breast cancer treatment: a pilot study. Przegl Menopauz 2014;13:221–6. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=26327858&dopt=Abstract 10.5114/pm.2014.44997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Smile TD, Tendulkar R, Schwarz G, Arthur D, Grobmyer S, Valente S, et al. A Review of Treatment for Breast Cancer-Related Lymphedema: Paradigms for Clinical Practice. Am J Clin Oncol 2018;41:178–90. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28009597&dopt=Abstract 10.1097/COC.0000000000000355 [DOI] [PubMed] [Google Scholar]
- 36.Tremback-Ball A, Harding R, Heffner K, Zimmerman A. The Efficacy of Kinesiology Taping in the Treatment of Women With Post–Mastectomy Lymphedema: A Systematic Review. J Womens Health Phys Therap 2018;42:94–103. 10.1097/JWH.0000000000000098 [DOI] [Google Scholar]
- 37.Blanco EG, González MS. Efficacy of kinesio® taping in the treatment of lymphoedema after breast cancer: A systematic review. J Lymphoedema 2020;15:71–6. [Google Scholar]
- 38.Kasawara KT, Mapa JM, Ferreira V, Added MA, Shiwa SR, Carvas N, Jr, et al. Effects of Kinesio Taping on breast cancer-related lymphedema: A meta-analysis in clinical trials. Physiother Theory Pract 2018;34:337–45. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29308967&dopt=Abstract 10.1080/09593985.2017.1419522 [DOI] [PubMed] [Google Scholar]
- 39.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33782057&dopt=Abstract 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions. Second edition. Chichester, UK: John Wiley and Sons; 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Basoglu C, Sindel D, Corum M, Oral A. Comparison of complete decongestive therapy and kinesiology taping for unilateral upper limb breast cancer-related lymphedema: A randomized controlled trial. Lymphology 2021;54:41–51. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34506086&dopt=Abstract 10.2458/lymph.4680 [DOI] [PubMed] [Google Scholar]
- 42.Ozsoy-Unubol T, Sanal-Toprak C, Bahar-Ozdemir Y, Akyuz G. Efficacy of kinesio taping in early stage breast cancer associated lymphedema: A randomized single blinded study. Lymphology 2019;52:166–76. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32171183&dopt=Abstract [PubMed] [Google Scholar]
- 43.Pajero Otero V, García Delgado E, Martín Cortijo C, Romay Barrero HM, de Carlos Iriarte E, Avendaño-Coy J. Kinesio taping versus compression garments for treating breast cancer-related lymphedema: a randomized, cross-over, controlled trial. Clin Rehabil 2019;33:1887–97. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31495192&dopt=Abstract 10.1177/0269215519874107 [DOI] [PubMed] [Google Scholar]
- 44.Pekyavaş NÖ, Tunay VB, Akbayrak T, Kaya S, Karataş M. Complex decongestive therapy and taping for patients with postmastectomy lymphedema: a randomized controlled study. Eur J Oncol Nurs 2014;18:585–90. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=25066648&dopt=Abstract 10.1016/j.ejon.2014.06.010 [DOI] [PubMed] [Google Scholar]
- 45.Tantawy SA, Abdelbasset WK, Nambi G, Kamel DM. Comparative Study Between the Effects of Kinesio Taping and Pressure Garment on Secondary Upper Extremity Lymphedema and Quality of Life Following Mastectomy: A Randomized Controlled Trial. Integr Cancer Ther 2019;18:1534735419847276. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=31068019&dopt=Abstract 10.1177/1534735419847276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Taradaj J, Halski T, Rosinczuk J, Dymarek R, Laurowski A, Smykla A. The influence of Kinesiology Taping on the volume of lymphoedema and manual dexterity of the upper limb in women after breast cancer treatment. Eur J Cancer Care (Engl) 2016;25:647–60. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=25963332&dopt=Abstract 10.1111/ecc.12331 [DOI] [PubMed] [Google Scholar]
- 47.Torres-Lacomba M, Navarro-Brazález B, Prieto-Gómez V, Ferrandez JC, Bouchet JY, Romay-Barrero H. Effectiveness of four types of bandages and kinesio-tape for treating breast-cancer-related lymphoedema: a randomized, single-blind, clinical trial. Clin Rehabil 2020;34:1230–41. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32580577&dopt=Abstract 10.1177/0269215520935943 [DOI] [PubMed] [Google Scholar]
- 48.Thomaz JP, Dias TD, de Rezende LF. Effect of taping as treatment to reduce breast cancer lymphedema: literature review. J Vasc Bras 2018;17:136–40. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30377423&dopt=Abstract 10.1590/1677-5449.007217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pappalardo M, Starnoni M, Franceschini G, Baccarani A, De Santis G. Breast cancer-related lymphedema: recent updates on diagnosis, severity and available treatments. J Pers Med 2021;11:402. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=34065795&dopt=Abstract 10.3390/jpm11050402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hasenoehrl T, Keilani M, Palma S, Crevenna R. Resistance exercise and breast cancer related lymphedema - a systematic review update. Disabil Rehabil 2020;42:26–35. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30638093&dopt=Abstract 10.1080/09638288.2018.1514663 [DOI] [PubMed] [Google Scholar]
- 51.Taradaj J, Halski T, Zduńczyk M, Rajfur J, Pasternok M, Chmielewska D, et al. Evaluation of the effectiveness of kinesio taping application in a patient with secondary lymphedema in breast cancer: a case report. Przegl Menopauz 2014;13:73–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=26327833&dopt=Abstract 10.5114/pm.2014.41082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Moura HJ. Junior, Da Silva LV, Arca EA. Kinesio Taping Lymphatic in Breast Cancer Postoperative. J Health Sci 2019;21:153. 10.17921/2447-8938.2019v21n2p153-158 [DOI] [Google Scholar]
- 53.Armer JM, Hulett JM, Bernas M, Ostby P, Stewart BR, Cormier JN. Best Practice Guidelines in Assessment, Risk Reduction, Management, and Surveillance for Post-Breast Cancer Lymphedema. Curr Breast Cancer Rep 2013;5:134–44. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=26246870&dopt=Abstract 10.1007/s12609-013-0105-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.de Sire A, Lippi L, Venetis K, Morganti S, Sajjadi E, Curci C, et al. Efficacy of Antiresorptive Drugs on Bone Mineral Density in Post-Menopausal Women With Early Breast Cancer Receiving Adjuvant Aromatase Inhibitors: A Systematic Review of Randomized Controlled Trials. Front Oncol 2022;11:829875. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=35127539&dopt=Abstract 10.3389/fonc.2021.829875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Baglia ML, Lin IH, Cartmel B, Sanft T, Ligibel J, Hershman DL, et al. Endocrine-related quality of life in a randomized trial of exercise on aromatase inhibitor-induced arthralgias in breast cancer survivors. Cancer 2019;125:2262–71. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30840336&dopt=Abstract 10.1002/cncr.32051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kudre D, Chen Z, Richard A, Cabaset S, Dehler A, Schmid M, et al. Multidisciplinary Outpatient Cancer Rehabilitation Can Improve Cancer Patients’ Physical and Psychosocial Status-a Systematic Review. Curr Oncol Rep 2020;22:122. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=33001322&dopt=Abstract 10.1007/s11912-020-00979-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Reid-Arndt SA, Yee A, Perry MC, Hsieh C. Cognitive and psychological factors associated with early posttreatment functional outcomes in breast cancer survivors. J Psychosoc Oncol 2009;27:415–34. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=19813133&dopt=Abstract 10.1080/07347330903183117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.O’Donnell TF, Jr, Allison GM, Iafrati MD. A systematic review of guidelines for lymphedema and the need for contemporary intersocietal guidelines for the management of lymphedema. J Vasc Surg Venous Lymphat Disord 2020;8:676–84. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32444277&dopt=Abstract 10.1016/j.jvsv.2020.03.006 [DOI] [PubMed] [Google Scholar]
- 59.Lipińska A, Sliwiński Z, Kiebzak W, Senderek T, Kirenko J. [The influence of kinesiotaping applications on lymphoedema of an upper limb in women after mastectomy]. Fizjoterapia Pol 2007;7:258–69. [Polish]. [Google Scholar]
- 60.Kase K, Wallis J, Kase T. Clinical therapeutic application of the kinesio taping method. Third edition. Tokyo: Ken Ikai Co Ltd.; 2013. [Google Scholar]
- 61.Cai C, Au IP, An W, Cheung RT. Facilitatory and inhibitory effects of Kinesio tape: fact or fad? J Sci Med Sport 2016;19:109–12. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=25687484&dopt=Abstract 10.1016/j.jsams.2015.01.010 [DOI] [PubMed] [Google Scholar]
- 62.Parreira PC, Costa LC, Hespanhol LC, Jr, Lopes AD, Costa LO. Current evidence does not support the use of Kinesio Taping in clinical practice: a systematic review. J Physiother 2014;60:31–9. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=24856938&dopt=Abstract 10.1016/j.jphys.2013.12.008 [DOI] [PubMed] [Google Scholar]
- 63.Amatya B, Khan F, Galea MP. Optimizing post-acute care in breast cancer survivors: a rehabilitation perspective. J Multidiscip Healthc 2017;10:347–57. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=28919774&dopt=Abstract 10.2147/JMDH.S117362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Coughlin SS. Oxidative Stress, Antioxidants, Physical Activity, and the Prevention of Breast Cancer Initiation and Progression. J Environ Health Sci 2018;4:55–7. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=30957018&dopt=Abstract [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wang L, Shi YX, Wang TT, Chen KX, Shang SM. Breast cancer-related lymphoedema and resistance exercise: an evidence-based review of guidelines, consensus statements and systematic reviews. J Clin Nurs 2022. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=35894167&dopt=Abstract 10.1111/jocn.16437 [DOI] [PubMed]
- 66.Hayes SC, Singh B, Reul-Hirche H, Bloomquist K, Johansson K, Jönsson C, et al. The Effect of Exercise for the Prevention and Treatment of Cancer-Related Lymphedema: A Systematic Review with Meta-analysis. Med Sci Sports Exerc 2022;54:1389–99. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=35320145&dopt=Abstract 10.1249/MSS.0000000000002918 [DOI] [PubMed] [Google Scholar]
- 67.Montaño-Rojas LS, Romero-Pérez EM, Medina-Pérez C, Reguera-García MM, de Paz JA. Resistance training in breast cancer survivors: A systematic review of exercise programs. Int J Environ Res Public Health 2020;17:1–17. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32906761&dopt=Abstract 10.3390/ijerph17186511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ha KJ, Lee SY, Lee H, Choi SJ. Synergistic effects of proprioceptive neuromuscular facilitation and manual lymphatic drainage in patients with mastectomy-related lymphedema. Front Physiol 2017;8:959. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29234287&dopt=Abstract 10.3389/fphys.2017.00959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Cheville AL. Current and future trends in lymphedema management: implications for women’s health. Phys Med Rehabil Clin N Am 2007;18:539–53, x. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=17678766&dopt=Abstract 10.1016/j.pmr.2007.06.001 [DOI] [PubMed] [Google Scholar]
- 70.Pajero Otero V, García Delgado E, Martín Cortijo C, Rodríguez Ramos ML, De Carlos Iriarte E, Gil García A, et al. Intensive complex physical therapy combined with intermittent pneumatic compression versus Kinesio taping for treating breast cancer-related lymphedema of the upper limb: A randomised cross-over clinical trial. Eur J Cancer Care (Engl) 2022;31:e13625. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=35642305&dopt=Abstract 10.1111/ecc.13625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.de Sire A, Losco L, Cigna E, Lippi L, Gimigliano F, Gennari A, et al. Three-dimensional laser scanning as a reliable and reproducible diagnostic tool in breast cancer related lymphedema rehabilitation: a proof-of-principle study. Eur Rev Med Pharmacol Sci 2020;24:4476–85. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32373985&dopt=Abstract [DOI] [PubMed] [Google Scholar]
- 72.Invernizzi M, Runza L, de Sire A, Lippi L, Blundo C, Gambini D, et al. Integrating augmented reality tools in breast cancer related lymphedema prognostication and diagnosis. J Vis Exp 2020;2020. https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=32090996&dopt=Abstract [DOI] [PubMed]


