Abstract
Background
Although many studies have proven the harmful effects of smoking on human health, the associations between smoking status and infertility are limited in large epidemiologic studies. We aimed to investigate the associations between smoking status and infertility among child-bearing women in the United States of America (USA).
Methods
A total of 3,665 female participants (aged 18-45) from the National Health and Nutrition Examination Survey (NHANES) (2013-2018) were included in this analysis. All data were survey-weighted, and corresponding logistic regression models were performed to investigate the associations between smoking status and infertility.
Results
In a fully adjusted model, the risk of infertility was found to be increased by 41.8% among current smokers compared to never smokers (95% CI: 1.044-1.926, P=0.025). In the subgroup analysis, the odds ratios (95% CI) of the risk of infertility for current smokers were 2.352 (1.018-5.435) in the unadjusted model for Mexican American, 3.675 (1.531-8.820) in the unadjusted model but 2.162 (0.946-4.942) in fully adjusted model for people aged 25-31, 2.201 (1.097-4.418) in the unadjusted model but 0.837 (0.435-1.612) in fully adjusted model for people aged 32-38.
Conclusion
Current smokers was associated with a higher risk of infertility. The underlying mechanism of these correlations still needs more research. Our findings indicated that quitting smoking may serve as a simple index to reduce the risk of infertility.
Keywords: smoking status, infertility, NHANES, cross-sectional analysis, population-based study
1. Introduction
Infertility is a top public health concern which is defined as the failure to conceive within a year of unprotected sexual activity (1, 2). The United States’ Centers for Disease Control and Prevention (CDC) underlined that infertility was a serious public health concern with significant quality-of-life effects, such as psychological suffering, social stigma, financial strain, and marital discord (3). 15% of couples who are of childbearing age were struggling with infertility in the world (4). Although infertility is a widespread health problem, seldom are modifiable risk factors identified. Infertility has a complicated etiology that involves both male and female components, as well as a mixture of both. As of this writing, the CDC has designated infertility diagnosis and treatment as a national public health priority (5).
Cigarette smoking is a leading and preventable cause of morbidity and mortality worldwide (6–9). In the United States of America (USA), 34.1 million of individuals were reported to be smokers in 2019 (10). Smoking has so far been repeatedly shown to contribute to a wide range of human ailments, including reproductive abnormalities (11–13). About 4000 different chemicals, including alkaloids, heavy metals, and polycyclic aromatic hydrocarbons, all of which have reproductive toxicity are present in cigarette smoke (14, 15). Most research indicates that women who are current smokers and those who were exposed to parental smoking before conception had lower natural fertility (16).
By estimating an overall 60% increase in the probability of infertility, a meta-analysis highlighted a significant correlation between smoking and infertility (17). On the other hand, after controlling for relevant confounders, a prospective study was unable to find any discernible difference in fertility between smokers and non-smokers (18). In conclusion, there is conflicting evidence in the literature about the relationship between smoking and infertility. Other than that, the majority of earlier studies, however, used clinic-based samples, and only a few of them concentrated on sizable population-level samples. Considering the inconsistent and limited evidence on the associations between smoking status and infertility, based on a large national population-based representative survey, the objectives of this study were to evaluate the associations between smoking status and female infertility and determine which type of smoking status was linked with the highest infertility risk based on a population-based study. Age and race/ethnicity difference were further studied in the subgroup analysis because previous studies had demonstrated that they had an effect on the prevalence of infertility (19–22). The decision-making process by health authorities regarding programs for health promotion and intervention to avoid infertility in women of reproductive age may be aided by knowledge of the associations.
2. Methods
2.1. Data source and study population
NHANES, administered by the CDC and Prevention, is a nationally representative, cross-sectional survey conducted incessantly in 2-year cycles through questionnaire surveys, physical examinations, household interviews, and laboratory tests, designed to evaluate and assess the health and nutrition status of Americans. The included samples in this study have good representativeness because of the stratified multistage probability sampling approach used (23). The public can access all NHANES data at www.cdc.gov/nchs/nhanes/.
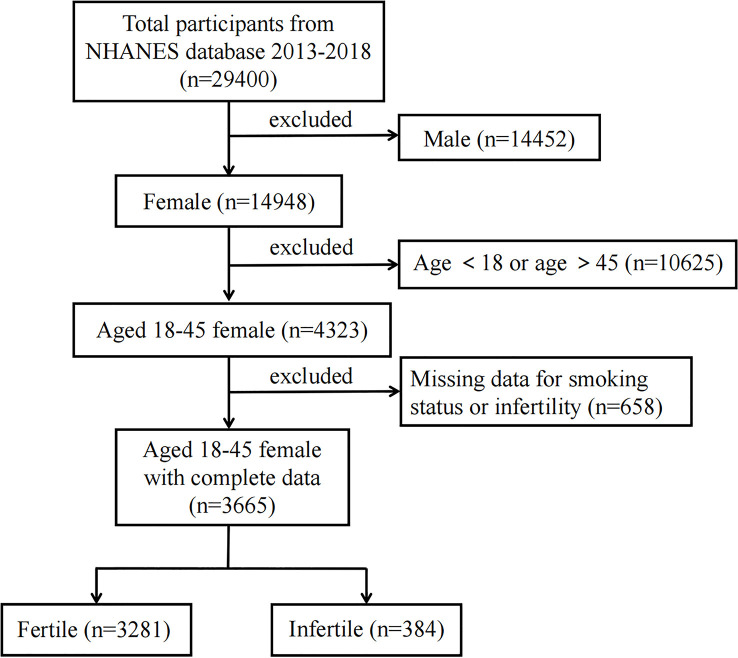
In the present study, NHANES data from 2013-2014, 2015-2016 and 2017-2018 were used. A total of 29,400 participants were incorporated at first; after the exclusion of males (n = 14,452), individuals aged <18 or >45 (n = 10,625) (24, 25), missing the smoking status or infertility data (n = 658), 3,665 participants were included in our final analysis ( Figure 1 ). The National Center for Health Statistics Ethics Review Board approved human subjects for the conduction of NHANES, and all participants provided their written informed consent.
Figure 1.
Flow chart of the study population. Describes how the sample of participants was composed. NHANES, National Health and Nutrition Examination Survey.
2.2. Study variables
In our analysis, the main exposure of interest is smoking status. Information on this exposure was obtained from relevant NHANES questionnaire items, which defined never smokers as having smoked fewer than 100 cigarettes in their lives, and former smokers as having smoked at least 100 cigarettes in their lives but not currently. These inquiries were made by trained interviewers using the Computer-Assisted Personal Interview (CAPI) technology at the mobile examination center (MEC). For these inquiries, both interpreters and proxy interviewers were accepted. Those who responded “Every day or certain days” to the question “Do you now smoke cigarettes?” were considered current smokers. Infertility is the key outcome of interest. These inquiries were made in the questionnaire on reproductive health using computer-assisted personal interviews conducted by qualified interviewers. Women who responded “yes” to the question “Have you ever attempted to become pregnant over a period of at least a year without becoming pregnant?” were labeled as experiencing infertility, with the answer “no” as the opposite category.
Our multivariable-adjusted models outlined relevant factors that might obscure the relationship between smoking status and infertility based on prior research (26). In our study, covariates including age (years), race/ethnicity (Mexican American/other Hispanic/non-Hispanic White/non-Hispanic Black/other races), education level (less than high school/high school/more than high school), marital status (married/living with partner, widowed/divorced/separated, never married) and ratio of family income to poverty (PIR), body mass index (BMI), diabetes, and physical activity were examined. According to Physical Activity Guidelines for Americans, 2nd edition of 75 min/week of vigorous or 150 min/week of moderate physical activity (27), participants were divided into three groups, including active, less active, and inactive. All detailed measurement procedures of the above variables are available on the NHANES website (www.cdc.gov/nchs/nhanes/).
2.3. Statistical analysis
For all statistical analyses, Stata (version 16.0), and EmpowerStats (version 2.0) were utilized with a determination of P < 0.05 for statistically significant. All estimates were computed using sample weights in accordance with National Center for Health Statistics’ analytical standards since NHANES seeks to create data that is representative of the civilian noninstitutionalized population in the USA. Continuous variables were characterized by mean ± SD if they were normally distributed and by median values and interquartile ranges otherwise. Percentages were used to characterize categorical variables which were compared by χ2 testing. To evaluate the relationship between smoking status and infertility, multivariable logistic regression was performed and the odds ratio (OR) values and 95% confidence intervals (95%CI) were calculated (28–32). Three models were built for the multivariate test. Model 1 had no variables adjusted. In Model 2, age and race/ethnicity were adjusted. Model 3 was adjusted for all covariates. Subgroup analysis stratified by age and race/ethnicity was carried out using stratified multivariate regression analysis.
3. Results
3.1. Baseline characteristics of participants
The weighted baseline characteristics of the included participants are displayed in Table 1 . A total of 3,665 female participants were incorporated, including 384 with infertility and 3665 without infertility, with an average age of 31.438 ± 8.122 years. Infertility was significantly more prevalent among women who were older at the time of the survey (35.367 years vs. 30.924 years, P < 0.001), had higher BMI (≥30 kg/m2: 55.061% vs 36.871%, P < 0.001) and higher family income (PIR >1.85: 65.737% vs 57.792%, P = 0.008), and they tended to be never married (Married/Living with partner: 77.152% vs. 57.500%, P <0.001). In addition, they were more inclined to suffer from diabetes (7.955% vs 7.955%, P <0.001) and more intend to be current smokers (23.859% vs 18.139%, P = 0.001).
Table 1.
Characteristics of the study population, National Health and Nutrition Examination Survey (NHANES) 2013–2018.
| Characteristic | Total (n=3665) |
No infertility (n=3281) |
Infertility (n=384) |
P value |
|---|---|---|---|---|
| Age (years) | 31.438 ± 8.122 | 30.924 ± 8.107 | 35.367 ± 7.099 | <0.001 |
| Race/Ethnicity (%) | 0.116 | |||
| Mexican American | 11.995 | 12.218 | 10.284 | |
| Other Hispanic | 7.908 | 8.075 | 6.631 | |
| Non-Hispanic White | 55.979 | 55.184 | 62.058 | |
| Non-Hispanic Black | 13.479 | 13.645 | 12.216 | |
| Other race | 10.639 | 10.878 | 8.810 | |
| Education (%) | 0.795 | |||
| Less than high school | 11.544 | 11.682 | 10.556 | |
| High school | 19.185 | 19.146 | 19.464 | |
| More than high school | 69.271 | 69.172 | 69.980 | |
| Marital status (%) | <0.001 | |||
| Married/Living with partner | 29.766 | 32.279 | 11.832 | |
| Widowed/Divorced/Separated | 10.319 | 10.222 | 11.016 | |
| Never Married | 59.915 | 57.500 | 77.152 | |
| PIR (%) | 0.008 | |||
| ≤ 1.30 | 29.636 | 30.210 | 25.369 | |
| 1.30- ≤ 1.85 | 11.630 | 11.998 | 8.894 | |
| > 1.85 | 58.734 | 57.792 | 65.737 | |
| BMI(%) | <0.001 | |||
| <25 | 36.806 | 38.036 | 27.382 | |
| 25≤-30 | 24.223 | 25.093 | 17.557 | |
| ≥30 | 38.971 | 36.871 | 55.061 | |
| Diabetes (%) | <0.001 | |||
| No | 96.502 | 97.085 | 92.045 | |
| Yes | 3.498 | 2.915 | 7.955 | |
| Physical activity (%) | 0.698 | |||
| Inactive | 54.379 | 54.159 | 56.055 | |
| Less active | 7.342 | 7.440 | 6.598 | |
| Active | 38.279 | 38.401 | 37.347 | |
| Smoking status(%) | 0.001 | |||
| Never smokers | 69.427 | 70.439 | 61.686 | |
| Former smokers | 11.773 | 11.422 | 14.456 | |
| Current smokers | 18.800 | 18.139 | 23.859 |
Mean ± SD for continuous variables: P value was calculated by one-way ANOVA; % for categorical variables: P value was calculated by χ2 test.
PIR, family income to poverty ratio; BMI, body mass index.
3.2. Associations between smoking status and infertility
Using binary logistic regression with single and multiple variables, we constructed three models to investigate relationships between smoking status and infertility. The pertinent effect size OR, 95%CI, and P-values are displayed in Table 2 . There was a substantial correlation between smoking status and infertility in Models 1, 2, and 3, which was positive regardless of the kind of adjusted covariates. In the initial model (Model 1), the risk of infertility among current smokers increased by 54.9% than that among never smokers (OR=1.549; 95% CI: 1.189-2.017, P=0.001), 33.6% in Model 2 (OR: 1.336, 95% CI: 1.013-1.763, P=0.040) and 41.8% in Model 3 (OR: 1.418, 95% CI: 1.044-1.926, P=0.025).
Table 2.
Association between smoking status and infertility.
| Model 1: OR (95%CI) P | Model 2: OR (95%CI) P | Model 3: OR (95%CI) P | |
|---|---|---|---|
| Smoking status | |||
| Never smokers | reference | reference | reference |
| Former smokers | 1.629 (1.179, 2.252) 0.003 | 1.312 (0.939, 1.832) 0.112 | 1.152 (0.806, 1.646) 0.437 |
| Current smokers | 1.549 (1.189, 2.017) 0.001 | 1.336 (1.013, 1.763) 0.040 | 1.418 (1.044, 1.926) 0.025 |
| P for trend | <0.001 | <0.001 | <0.001 |
Model 1 adjusted for none.
Model 2 adjusted for age and race/ethnicity.
Model 3 adjusted for age, race/ethnicity, education level, marital status, PIR, BMI, diabetes, and physical activity.
3.3. Subgroup analysis
Subgroup analysis revealed that the connection between smoking status and infertility was mostly present in Mexican Americans and participants aged 25 to 38 after controlling for variables. Tables 3 , 4 provide comprehensive information on the subgroup analysis. For Mexican American, the association is similar in Model 2 (OR: 2.304, 95% CI: 0.971-5.470, P=0.058) and Model 3 (OR: 1.883, 95% CI: 0.829-4.278, P=0.13), but not in Model 1 (OR: 2.352, 95% CI: 1.018-5.435, P=0.045) ( Table 3 ). For people aged 25-31, there is a significant positive association between smoking status and infertility in Model 1 (OR: 3.675, 95% CI: 1.531-8.820, P=0.004), Model 2 (OR: 2.501, 95% CI: 1.225-5.105, P=0.012) but not in Model 3 (OR: 2.162, 95% CI: 0.946-4.942, P=0.067). For people aged 32-38, there is a significant positive association in Model 1 (OR: 2.201, 95% CI: 1.097-4.418, P=0.026), but not in Model 2 (OR: 0.659, 95% CI: 0.363-1.195, P=0.169) and Model3 (OR: 0.837, 95% CI: 0.435-1.612, P=0.595) ( Table 4 ).
Table 3.
Association between smoking status and infertility stratified by race/ethnicity.
| Race/Ethnicity (%) | Model 1 OR (95%CI) P | Model 2 OR (95%CI) P | Model 3 OR (95%CI) P |
|---|---|---|---|
| Mexican American | |||
| Never smokers | reference | reference | reference |
| Former smokers | 2.146 (0.860,5.356) 0.102 | 2.081 (0.824,5.254) 0.121 | 1.673 (0.579,4.831) 0.342 |
| Current smokers | 2.352 (1.018,5.435) 0.045 | 2.304 (0.971,5.470) 0.058 | 1.883 (0.829,4.278) 0.130 |
| Other Hispanic | |||
| Never smokers | reference | reference | reference |
| Former smokers | 2.269 (0.813,6.338) 0.118 | 2.008 (0.699,5.768) 0.196 | 2.065 (0.673,6.342) 0.205 |
| Current smokers | 1.030 (0.316,3.362) 0.960 | 1.133 (0.343,3.748) 0.838 | 1.130 (0.284,4.496) 0.862 |
| Non-Hispanic White | |||
| Never smokers | reference | reference | reference |
| Former smokers | 1.204 (0.690,2.100) 0.514 | 0.908 (0.503,1.639) 0.749 | 0.821 (0.445,1.513) 0.527 |
| Current smokers | 1.310 (0.837,2.049) 0.238 | 1.180 (0.743,1.874) 0.482 | 1.231 (0.723,2.098) 0.444 |
| Non-Hispanic Black | |||
| Never smokers | reference | reference | reference |
| Former smokers | 1.405 (0.557,3.546) 0.471 | 1.239 (0.482,3.184) 0.656 | 1.112 (0.446,2.772) 0.820 |
| Current smokers | 1.726 (0.987,3.020) 0.056 | 1.608 (0.910,2.84) 0.1020 | 1.495 (0.786,2.843) 0.221 |
| Other Race | |||
| Never smokers | reference | reference | reference |
| Former smokers | 1.652 (0.672,4.063) 0.274 | 1.523 (0.612,3.788) 0.365 | 1.305 (0.445,3.829) 0.627 |
| Current smokers | 1.696 (0.593,4.851) 0.324 | 1.787 (0.577,5.539) 0.314 | 1.921 (0.472,7.823) 0.362 |
Model 1 adjusted for none.
Model 2 adjusted for age and race/ethnicity.
Model 3 adjusted for age, race/ethnicity, education level, marital status, PIR, BMI, diabetes, and physical activity.
Table 4.
Association between smoking status and infertility stratified by age.
| Age | Model 1 OR (95%CI) P | Model 2 OR (95%CI) P | Model 3 OR (95%CI) P |
|---|---|---|---|
| Age (25-31) | |||
| Never smokers | reference | reference | reference |
| Former smokers | 2.587 (0.864,7.751) 0.089 | 1.620 (0.647,4.058) 0.303 | 1.225 (0.448,3.351) 0.693 |
| Current smokers | 3.675 (1.531,8.820) 0.004 | 2.501 (1.225,5.105) 0.012 | 2.162 (0.946,4.942) 0.067 |
| Age (32-38) | |||
| Never smokers | reference | reference | reference |
| Former smokers | 1.523 (0.609,3.808) 0.368 | 1.404 (0.745,2.646) 0.293 | 1.511 (0.775,2.946) 0.226 |
| Current smokers | 2.201 (1.097,4.418) 0.026 | 0.659 (0.363,1.195) 0.169 | 0.837 (0.435,1.612) 0.595 |
| Age (39-45) | |||
| Never smokers | reference | reference | reference |
| Former smokers | 1.488 (0.801,2.764) 0.208 | 0.636 (0.302,1.338) 0.233 | 0.633 (0.301,1.331) 0.228 |
| Current smokers | 0.711 (0.398,1.269) 0.248 | 1.266 (0.706,2.268) 0.429 | 1.619 (0.843,3.109) 0.148 |
Model 1 adjusted for none.
Model 2 adjusted for age and race/ethnicity.
Model 3 adjusted for age, race/ethnicity, education level, marital status, PIR, BMI, diabetes, and physical activity.
4. Discussion
In this cross-sectional study, which included 3,665 people, we found that current smokers had a higher risk of infertility. An examination of subgroups revealed that populations with Mexican American heritage and those between the ages of 25 and 38 shared this connection. Our findings imply that smoking status should be taken into account while treating infertile individuals in therapeutic settings.
Clinical investigations on the connection between smoking status and infertility in females are still limited and controversial. Three studies indicated a substantial link between smoking and infertility, with the risk being 1.85 (95% CI: 1.08-3.14) times greater for smokers than for non-smokers (33–35). The relevant literature from 1966 through late 1997 was found by a meta-analysis, which revealed an OR of 1.60 for infertility among female smokers compared to non-smokers across all research designs (23). Since the publication of this meta-analysis, more extensive population-based studies have shown that smoking has a detrimental effect on fecundity, regardless of other factors. The largest of these studies found that active smoking was linked to an increased failure to conceive within both the 6- and 12-month trial periods (36). However, this study divided smoking into active, passive, or both and the number of cigarettes smoked instead of different status and we are unclear about the difference between the relationship of past and current smoking and infertility. An Ontario, Canada, retrospective cohort study of farm couples found no difference in the risk of infertility between current smokers and non-smokers (37). Additionally, based on data from a North American internet-based preconception cohort study that enrolled participants from 2013 to 2018, a prospective analysis of cigarette smoking and fecundability found both female current smoking and previous smoking were related to slight declines in fecundity (38). Both of the above studies are consistent with the findings of Model 3 in our study, indicating that the relationship between smoking and infertility varies from current smoking status. In our study, the relationship between former smokers and infertility in Table 2 was significant in Model 1 but not in Models 2 and 3 after adjusting for the covariate. The effect of former smokers on the outcome event infertility reflected not only the pure effect of exposure factor but also the effect of confounding factors. By constructing a multiple regression model in Model 2 and Model 3, i.e., “adjusting” for the effects of other confounding factors, the effect of the confounding factor was actually separated from the effect of the exposure factor. After eliminating the effect of the confounding factors, the spurious association between former smokers and the dependent variable disappeared, and there was no significant correlation between former smokers and infertility in Model 2 and Model 3. However, the population included in those studies did not distinguish between race and age. Thus, both age and race were the limitations of their study. In our study, the relationship between smoking status and infertility was found to be different across race and age groups by performing subgroup analysis.
Age and race/ethnicity have been proven in prior research to have an impact on the prevalence of infertility (19–22). Fecundity reportedly decreased for females in their late thirties and early forties. The likelihood of infertility rose from 10%-20% after age 35 to 45% in the early forties among women with previously confirmed fertility. Women who had never given birth were more likely to experience infertility at any age (19). Additionally, a study found that American Indians and Alaska Natives had a 1.30 times higher prevalence of decreased fecundity than white people (95% CI: 1.04 -1.62) (22). Thus, we conducted stratified analyses by age and race/ethnicity in the subgroup analysis.
Although the mechanisms underlying smoking and the risk of infertility have not been entirely understood, some evidence can support the negative association between them. Strong evidence suggested that smoking might impact natural female fertility by affecting several female reproductive function elements such as the ovary, oviduct, and uterus (39–41). In addition to clinical observational research in people, experiments on human tissues and cells as well as animal models have been used to study how smoking affects female reproductive function and fertility (42). But there is still debate over the outcomes. According to several research, smoking lowered the number of oocytes that may be obtained for assisted reproductive technology (ART) (43, 44). Those that are collected have a lower chance of becoming fertile, which lowers the quality of the resulting embryos (44, 45). However, when smokers are compared to age-matched controls, other studies have not discovered any differences in oocyte number, fertilization, embryo quality, clinical pregnancy, or birth rates (46, 47). The precise mechanism of the association between smoking status and infertility in our study remains unclear.
This study has a number of advantages. First, this study was based on data from NHANES, which are population-based sampling data collected across the country following a set procedure. The study samples were more representative since all analyses took into account the proper NHANES sampling weights. To make the results from the current study more trustworthy, the authors additionally made adjustments for confounding factors. However, it is impossible to disregard the study’s limitations. First, a clear causal association cannot be established by the authors because of the cross-sectional study methodology. Second, we were constrained in our secondary analysis due to our inability to gather fresh data. Therefore, there is a chance that unmeasured factors will cause residual confounding. For instance, because these data were not obtained, we were unable to control for the family history of infertility, a potentially significant confounder. To learn more about the harmful effects of smoking, it is crucial to investigate the relationship between smoking status and female infertility. More studies are still required to produce definitive pieces of data.
5. Conclusion
This study demonstrated that current smoking was associated with elevated infertility risk. In subgroup analyses, the associations of smoking status with infertility were only found in women aged 25-38 and in Mexican Americans. Further studies are still needed to validate our findings.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: https://www.cdc.gov/nchs/nhanes/index.htm.
Author contributions
SH designed the research, analyzed the data, and wrote the paper. LW assisted in manuscript preparation. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1. Warner L, Jamieson DJ, Barfield WD. Cdc releases a national public health action plan for the detection, prevention, and management of infertility. J Womens Health (Larchmt) (2015) 24(7):548–9. doi: 10.1089/jwh.2015.5355 [DOI] [PubMed] [Google Scholar]
- 2. Carson SA, Kallen AN. Diagnosis and management of infertility: a review. Jama (2021) 326(1):65–76. doi: 10.1001/jama.2021.4788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sun H, Gong TT, Jiang YT, Zhang S, Zhao YH, Wu QJ. Global, regional, and national prevalence and disability-adjusted life-years for infertility in 195 countries and territories, 1990-2017: results from a global burden of disease study, 2017. Aging (Albany NY) (2019) 11(23):10952–91. doi: 10.18632/aging.102497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gerrits T, Van Rooij F, Esho T, Ndegwa W, Goossens J, Bilajbegovic A, et al. Infertility in the global south: raising awareness and generating insights for policy and practice. Facts Views Vis Obgyn (2017) 9(1):39–44. [PMC free article] [PubMed] [Google Scholar]
- 5. Macaluso M, Wright-Schnapp TJ, Chandra A, Johnson R, Satterwhite CL, Pulver A, et al. A public health focus on infertility prevention, detection, and management. Fertil Steril (2010) 93(1):16 e1–0. doi: 10.1016/j.fertnstert.2008.09.046 [DOI] [PubMed] [Google Scholar]
- 6. Li G, Wang H, Wang K, Wang W, Dong F, Qian Y, et al. The association between smoking and blood pressure in men: a cross-sectional study. BMC Public Health (2017) 17(1):797. doi: 10.1186/s12889-017-4802-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cui M, Cui R, Liu K, Dong JY, Imano H, Hayama-Terada M, et al. Associations of tobacco smoking with impaired endothelial function: the circulatory risk in communities study (Circs). J Atheroscler Thromb (2018) 25(9):836–45. doi: 10.5551/jat.42150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Nam DJ, Oh CM, Ha E, Kim MH, Yang EH, Lee HC, et al. The association of pancreatic cancer incidence with smoking status and smoking amount in Korean men. Epidemiol Health (2022) 44:e2022040. doi: 10.4178/epih.e2022040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kojima G, Iliffe S, Jivraj S, Liljas A, Walters K. Does current smoking predict future frailty? the English longitudinal study of ageing. Age Ageing (2018) 47(1):126–31. doi: 10.1093/ageing/afx136 [DOI] [PubMed] [Google Scholar]
- 10. Cornelius ME, Wang TW, Jamal A, Loretan CG, Neff LJ. Tobacco product use among adults - United States, 2019. MMWR Morb Mortal Wkly Rep (2020) 69(46):1736–42. doi: 10.15585/mmwr.mm6946a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sansone A, Di Dato C, de Angelis C, Menafra D, Pozza C, Pivonello R, et al. Smoke, alcohol and drug addiction and Male fertility. Reprod Biol Endocrinol RB&E (2018) 16(1):3. doi: 10.1186/s12958-018-0320-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. National Collaborating Centre for Ws, Children’s H . National institute for health and clinical excellence: guidance. In: Fertility: assessment and treatment for people with fertility problems. London: Royal College of Obstetricians & Gynaecologists Copyright © 2013, National Collaborating Centre for Women’s and Children’s Health; (2013). [Google Scholar]
- 13. Hyland A, Piazza K, Hovey KM, Tindle HA, Manson JE, Messina C, et al. Associations between lifetime tobacco exposure with infertility and age at natural menopause: the women's health initiative observational study. Tob Control (2016) 25(6):706–14. doi: 10.1136/tobaccocontrol-2015-052510 [DOI] [PubMed] [Google Scholar]
- 14. de Angelis C, Galdiero M, Pivonello C, Salzano C, Gianfrilli D, Piscitelli P, et al. The environment and Male reproduction: the effect of cadmium exposure on reproductive function and its implication in fertility. Reprod Toxicol (2017) 73:105–27. doi: 10.1016/j.reprotox.2017.07.021 [DOI] [PubMed] [Google Scholar]
- 15. Alviggi C, Guadagni R, Conforti A, Coppola G, Picarelli S, De Rosa P, et al. Association between intrafollicular concentration of benzene and outcome of controlled ovarian stimulation in Ivf/Icsi cycles: a pilot study. J Ovarian Res (2014) 7:67. doi: 10.1186/1757-2215-7-67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. de Angelis C, Nardone A, Garifalos F, Pivonello C, Sansone A, Conforti A, et al. Smoke, alcohol and drug addiction and female fertility. Reprod Biol Endocrinol RB&E (2020) 18(1):21. doi: 10.1186/s12958-020-0567-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Augood C, Duckitt K, Templeton AA. Smoking and female infertility: a systematic review and meta-analysis. Hum Reprod (1998) 13(6):1532–9. doi: 10.1093/humrep/13.6.1532 [DOI] [PubMed] [Google Scholar]
- 18. de Mouzon J, Spira A, Schwartz D. A prospective study of the relation between smoking and fertility. Int J Epidemiol (1988) 17(2):378–84. doi: 10.1093/ije/17.2.378 [DOI] [PubMed] [Google Scholar]
- 19. Steiner AZ, Jukic AM. Impact of female age and nulligravidity on fecundity in an older reproductive age cohort. Fertil Steril (2016) 105(6):1584–8.e1. doi: 10.1016/j.fertnstert.2016.02.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gnoth C, Godehardt D, Godehardt E, Frank-Herrmann P, Freundl G. Time to pregnancy: results of the German prospective study and impact on the management of infertility. Hum Reprod (2003) 18(9):1959–66. doi: 10.1093/humrep/deg366 [DOI] [PubMed] [Google Scholar]
- 21. Rothman KJ, Wise LA, Sorensen HT, Riis AH, Mikkelsen EM, Hatch EE. Volitional determinants and age-related decline in fecundability: a general population prospective cohort study in Denmark. Fertil Steril (2013) 99(7):1958–64. doi: 10.1016/j.fertnstert.2013.02.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Craig LB, Peck JD, Janitz AE. The prevalence of infertility in American Indian/Alaska natives and other Racial/Ethnic groups: national survey of family growth. Paediatr Perinat Epidemiol (2019) 33(2):119–25. doi: 10.1111/ppe.12538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Zipf G, Chiappa M, Porter KS, Ostchega Y, Lewis BG, Dostal J. National health and nutrition examination survey: plan and operations, 1999-2010. Vital Health Stat 1 (2013) 56):1–37. [PubMed] [Google Scholar]
- 24. Arya S, Dwivedi AK, Alvarado L, Kupesic-Plavsic S. Exposure of U.S. population to endocrine disruptive chemicals (Parabens, benzophenone-3, bisphenol-a and triclosan) and their associations with female infertility. Environ pollut (2020) 265(Pt A):114763. doi: 10.1016/j.envpol.2020.114763 [DOI] [PubMed] [Google Scholar]
- 25. Zhu F, Chen C, Zhang Y, Chen S, Huang X, Li J, et al. Elevated blood mercury level has a non-linear association with infertility in U.S. women: data from the nhanes 2013-2016. Reprod Toxicol (2020) 91:53–8. doi: 10.1016/j.reprotox.2019.11.005 [DOI] [PubMed] [Google Scholar]
- 26. Liang Z, Liu J. Sleep behavior and self-reported infertility: a cross-sectional analysis among U.S. women. Front Endocrinol (2022) 13:818567. doi: 10.3389/fendo.2022.818567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. US Department of Health and Human Services . Physical activity guidelines for americans. 2nd ed. Wasington, DC: US Dept of Health and Human Services; (2018). [Google Scholar]
- 28. Xie R, Zhang Y. Index-based calculation or transient elastography to assess the degree of hepatic steatosis and fibrosis. J Nutr (2023) 153(3):909. doi: 10.1016/j.tjnut.2022.10.015 [DOI] [PubMed] [Google Scholar]
- 29. Xie R, Zhang Y. Association between 19 dietary fatty acids intake and rheumatoid arthritis: results of a nationwide survey. Prostaglandins leukotrienes essential Fatty Acids (2023) 188:102530. doi: 10.1016/j.plefa.2022.102530 [DOI] [PubMed] [Google Scholar]
- 30. Xie R, Zhang Y. Is assessing the degree of hepatic steatosis and fibrosis based on index calculations the best choice for epidemiological studies? Environ pollut (2023) 317:120783. doi: 10.1016/j.envpol.2022.120783 [DOI] [PubMed] [Google Scholar]
- 31. Xie R, Liu Y, Wang J, Zhang C, Xiao M, Liu M, et al. Race and gender differences in the associations between cadmium exposure and bone mineral density in us adults. Biol Trace Elem Res (2022). doi: 10.1007/s12011-022-03521-y [DOI] [PubMed] [Google Scholar]
- 32. Zhang Y, Xie R, Ou J. A U-shaped association between serum albumin with total triiodothyronine in adults. J Clin Lab Anal (2022) 36(6):e24473. doi: 10.1002/jcla.24473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Klemetti R, Raitanen J, Sihvo S, Saarni S, Koponen P. Infertility, mental disorders and Well-Being–a nationwide survey. Acta Obstet Gynecol Scand (2010) 89(5):677–82. doi: 10.3109/00016341003623746 [DOI] [PubMed] [Google Scholar]
- 34. Biringer E, Howard LM, Kessler U, Stewart R, Mykletun A. Is infertility really associated with higher levels of mental distress in the female population? results from the north-trondelag health study and the medical birth registry of Norway. J Psychosom Obstet Gynaecol (2015) 36(2):38–45. doi: 10.3109/0167482X.2014.992411 [DOI] [PubMed] [Google Scholar]
- 35. Salih Joelsson L, Tyden T, Wanggren K, Georgakis MK, Stern J, Berglund A, et al. Anxiety and depression symptoms among Sub-fertile women, women pregnant after infertility treatment, and naturally pregnant women. Eur Psychiatry (2017) 45:212–9. doi: 10.1016/j.eurpsy.2017.07.004 [DOI] [PubMed] [Google Scholar]
- 36. Hull MG, North K, Taylor H, Farrow A, Ford WC. Delayed conception and active and passive smoking. the Avon longitudinal study of pregnancy and childhood study team. Fertil Steril (2000) 74(4):725–33. doi: 10.1016/s0015-0282(00)01501-6 [DOI] [PubMed] [Google Scholar]
- 37. Curtis KM, Savitz DA, Arbuckle TE. Effects of cigarette smoking, caffeine consumption, and alcohol intake on fecundability. Am J Epidemiol (1997) 146(1):32–41. doi: 10.1093/oxfordjournals.aje.a009189 [DOI] [PubMed] [Google Scholar]
- 38. Wesselink AK, Hatch EE, Rothman KJ, Mikkelsen EM, Aschengrau A, Wise LA. Prospective study of cigarette smoking and fecundability. Hum Reprod (2019) 34(3):558–67. doi: 10.1093/humrep/dey372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Dechanet C, Anahory T, Mathieu Daude JC, Quantin X, Reyftmann L, Hamamah S, et al. Effects of cigarette smoking on reproduction. Hum Reprod Update (2011) 17(1):76–95. doi: 10.1093/humupd/dmq033 [DOI] [PubMed] [Google Scholar]
- 40. Talbot P, Riveles K. Smoking and reproduction: the oviduct as a target of cigarette smoke. Reprod Biol Endocrinol RB&E (2005) 3:52. doi: 10.1186/1477-7827-3-52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Budani MC, Tiboni GM. Ovotoxicity of cigarette smoke: a systematic review of the literature. Reprod Toxicol (2017) 72:164–81. doi: 10.1016/j.reprotox.2017.06.184 [DOI] [PubMed] [Google Scholar]
- 42. Camlin NJ, McLaughlin EA, Holt JE. Through the smoke: use of in vivo and in vitro cigarette smoking models to elucidate its effect on female fertility. Toxicol Appl Pharmacol (2014) 281(3):266–75. doi: 10.1016/j.taap.2014.10.010 [DOI] [PubMed] [Google Scholar]
- 43. Fuentes A, Munoz A, Barnhart K, Arguello B, Diaz M, Pommer R. Recent cigarette smoking and assisted reproductive technologies outcome. Fertil Steril (2010) 93(1):89–95. doi: 10.1016/j.fertnstert.2008.09.073 [DOI] [PubMed] [Google Scholar]
- 44. El-Nemr A, Al-Shawaf T, Sabatini L, Wilson C, Lower AM, Grudzinskas JG. Effect of smoking on ovarian reserve and ovarian stimulation in in-vitro fertilization and embryo transfer. Hum Reprod (1998) 13(8):2192–8. doi: 10.1093/humrep/13.8.2192 [DOI] [PubMed] [Google Scholar]
- 45. Gruber I, Just A, Birner M, Losch A. Effect of a woman's smoking status on oocyte, zygote, and day 3 pre-embryo quality in in vitro fertilization and embryo transfer program. Fertil Steril (2008) 90(4):1249–52. doi: 10.1016/j.fertnstert.2007.06.108 [DOI] [PubMed] [Google Scholar]
- 46. Cinar O, Dilbaz S, Terzioglu F, Karahalil B, Yucel C, Turk R, et al. Does cigarette smoking really have detrimental effects on outcomes of ivf? Eur J Obstet Gynecol Reprod Biol (2014) 174:106–10. doi: 10.1016/j.ejogrb.2013.12.026 [DOI] [PubMed] [Google Scholar]
- 47. Wright KP, Trimarchi JR, Allsworth J, Keefe D. The effect of female tobacco smoking on ivf outcomes. Hum Reprod (2006) 21(11):2930–4. doi: 10.1093/humrep/del269 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Publicly available datasets were analyzed in this study. This data can be found here: https://www.cdc.gov/nchs/nhanes/index.htm.