Abstract
A substantial number of individuals who experience COVID-19 infection experience prolonged physical and mental symptoms after resolution of their initial infection, and among them, many individuals experience cognitive difficulties including memory lapses and executive function difficulties, often referred to as “brain fog.” The possible impact of COVID-19 infection on cognition in persons with HIV-related cognitive disorders is unknown. In this report, we describe post-COVID-19 cognitive and driving function in a 62-year-old man with HIV infection since the early 1990s.
Keywords: Human immunodeficiency virus-1 (HIV-1), SARS-COVID-19, Neurocognition, Driving, Psychomotor abilities
Introduction
Both HIV and COVID-19 infection are associated with cognitive dysfunction, even in patients with nondetectable viral loads (Heaton et al. 2010) and who have recovered from acute COVID-19 infection (Ceban et al. 2022). In this case history, we present a man with long-standing HIV infection who complained of difficulty in driving after COVID-19.
Case
The patient is a 62-year-old man with a history of HIV infection since 1991. He was treated with antiretroviral medications since that time, including multidrug combinations beginning in 1994. He reports a nadir CD4 count of 81 in 1993. At the time of his first contact with us in 2019, he had a nondetectable viral load (< 20 copies/mL) and a CD4 count of 712.
In May of 2019, the patient was recruited for a study of computer-based cognitive training (CCT) and transcranial direct current stimulation (tDCS) for HIV-associated mild neurocognitive disorder (MND). During telephone screening, he reported a history of HIV infection and current subjective cognitive difficulties including memory dysfunction. Testing confirmed objective deficits, and he met Frascati criteria for mild neurocognitive disorder (Antinori et al. 2007).
As part of this study, he completed a battery of neuropsychological tests before and after the study and at 1-month follow-up. Measures of psychomotor speed are most relevant to his post-COVID-19 function and are presented here. Baseline assessment was in May 2019, with follow-ups in August and September (Ownby and Kim 2021). As a follow-up, participants completed a driving simulator evaluation. He completed this evaluation in September 2019 and showed performance above average for persons 50 years and older with HIV-related cognitive disorders (Foley et al. 2013).
The patient was contacted in February 2022 as part of recruitment for a mixed-methods study of post-COVID-19 symptomatology (Thomas-Purcell et al. 2023). He completed a telephone screening, online self-report questionnaires, and a 45-min interview online by video conference as part of that study. The patient contracted COVID-19 in March of 2020 and met 2020 CDC case criteria for probable COVID-19. Symptoms reported by the patient during the acute phase included fever, rigors, myalgia, severe headache, fatigue, and coughing. Since recovering from the initial infection, he reports new symptoms of atrial fibrillation, shortness of breath, “brain fog,” fatigue, sleep disturbance, and difficulty in driving. He stated that he was fearful of driving, sometimes feeling confused and lost. He had limited his driving to daytime and in clear weather, relying on ride sharing services at other times.
Because of the previous assessments and his current complaints about driving, we undertook an assessment of his current functioning. The patient consented to re-assessment consisting of measures of psychomotor speed and attention, including the Trail Making Test (Reitan and Wolfson 1993); the Digit Span and Coding subtests of the Wechsler Adult Intelligence Scale, 4th ed. (Wechsler 2008); the Grooved Pegboard Test (Lafayette Instrument Company 2002); and the standard driving simulation.
Results
Cognitive testing
Results of testing during the training study and after COVID-19 infection are presented in Fig. 1. Although the patient’s psychomotor speed and attention were normal in 2019, clear decline was evident after COVID-19 on measures of psychomotor speed that are closely related to on-road driving performance.(Dawson et al. 2010; Papandonatos et al. 2015).
Fig. 1.
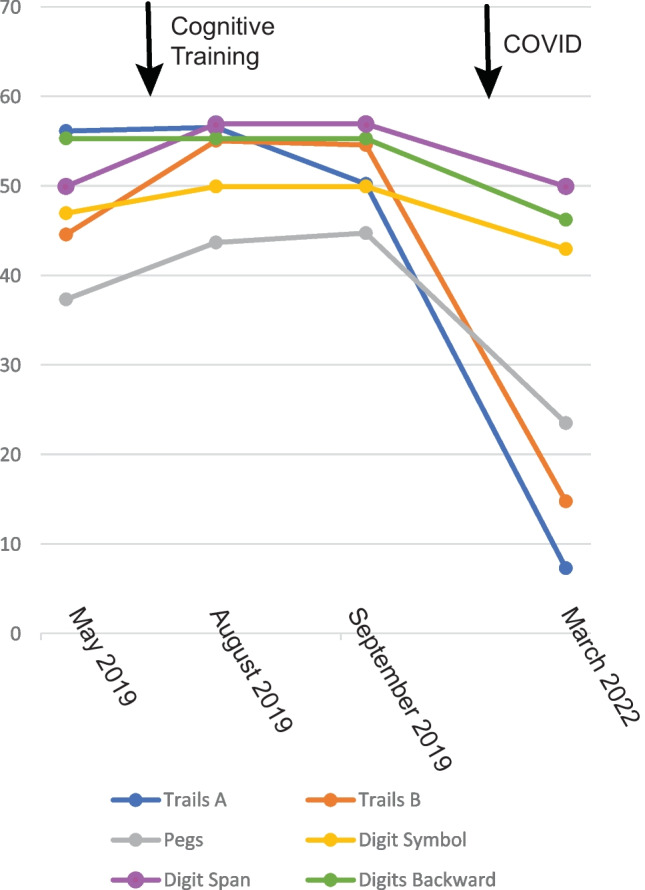
Neuropsychological testing in 2019 and 2022. Note: the horizontal (time) axis is not linear to enhance understandability
Olfaction
The patient did not complete a measure of olfactory function in 2019 but did so in 2022. His performance on the NIH Toolbox Odor Identification test was an age-corrected T score of 31, well below average.
Driving performance
We used the Advanced Routine and Emergency Driving (ARED) scenario available for the STSIM driving simulator software (Hawthorne CA: Systems Technology, Inc.). This requires the driver to complete typical and emergency driving tasks. Scores include the total number of mistakes (e.g., running off the road) and number of collisions. He also again completed a scenario testing braking reaction time. In 2019, the patient completed the ARED with 40 errors and 2 collisions; in 2022, he again completed the scenario with 40 errors and 2 collisions. His reaction time in 2019 was 733 ms and in 2022 was 544 ms.
Discussion
This case illustrates the potential negative impact of COVID-19 infection on the cognitive function of older persons with HIV-associated neurocognitive disorder. The patient had been well characterized with respect to cognitive function before infection, so that post-COVID-19 results are likely due to the infection, especially given the relatively brief period from 2019 to 2022 and stability of treatment for HIV, although continuing decline due to HIV and aging cannot be ruled out.
A limitation of this report is that the patient was judged to have probable COVID-19 based on the CDC case definition current at the time of the study before widespread testing was available but did not have definitive testing. It should be noted that his impaired odor identification is consistent with COVID-19, although it has also been linked to HIV infection (Vance et al. 2019).
Of interest is the patient’s concerns about his driving skills and the relation of these to cognition. His performance on the driving scenario was the same at both assessments, despite his concerns. Measures of psychomotor speed like the Grooved Pegboard and Trail Making Test can predict driving errors (Dawson et al. 2010; Roy and Molnar 2013), although our patient’s performance on them did not meet recommended test cut-off scores for impaired driving (Roy and Molnar 2013). By contrast, simulator performance, while correlated with on-road performance, may only be weakly related to it (Groeger and Murphy 2020). It is also possible that his performance on the simulator was better than on-road performance due to the lack of distractions in the laboratory and his increased attention to driving given his concerns.
This case illustrates the vulnerability of older persons with HIV infection to the effects of COVID-19 and the impact it can have on functional skills such as driving. Others have noted the potential negative impact of long COVID-19 symptoms on driving (Vingilis et al. 2021), and this case supports that observation.
Funding
The original study in which this patient participated, data from which are reported in this case, was supported by a grant from the US National Institute on Aging (R21AG056256) to Dr. Ownby.
Data availability
The data from the original study are available from the corresponding author on reasonable request.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Antinori A, Arendt G, Becker JT, Brew BJ, Byrd DA, Cherner M, Clifford DB, Cinque P, Epstein LG, Goodkin K, Gisslen M, Grant I, Heaton RK, Joseph J, Marder K, Marra CM, McArthur JC, Nunn M, Price RW, Pulliam L, Robertson KR, Sacktor N, Valcour V, Wojna VE. Updated research nosology for HIV-associated neurocognitive disorders. Neurology. 2007;69:1789–1799. doi: 10.1212/01.WNL.0000287431.88658.8b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ceban F, Ling S, Lui LMW, Lee Y, Gill H, Teopiz KM, Rodrigues NB, Subramaniapillai M, Di Vincenzo JD, Cao B, Lin K, Mansur RB, Ho RC, Rosenblat JD, Miskowiak KW, Vinberg M, Maletic V, McIntyre RS. Fatigue and cognitive impairment in post-COVID-19 syndrome: a systematic review and meta-analysis. Brain Behav Immun. 2022;101:93–135. doi: 10.1016/j.bbi.2021.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson JD, Uc EY, Anderson SW, Johnson AM, Rizzo M. Neuropsychological predictors of driving errors in older adults. J Am Geriatr Soc. 2010;58:1090–1096. doi: 10.1111/j.1532-5415.2010.02872.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foley JM, Gooding AL, Thames AD, Ettenhofer ML, Kim MS, Castellon SA, Marcotte TD, Sadek JR, Heaton RK, van Gorp WG, Hinkin CH. Visuospatial and attentional abilities predict driving simulator performance among older HIV-infected adults. Am J Alzheimers Dis Other Demen. 2013;28:185–194. doi: 10.1177/1533317512473192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groeger JA, Murphy G. Driver performance under simulated and actual driving conditions: validity and orthogonality. Accid Anal Prev. 2020;143:105593. doi: 10.1016/j.aap.2020.105593. [DOI] [PubMed] [Google Scholar]
- Heaton RK, Clifford DB, Franklin DR, Jr, Woods SP, Ake C, Vaida F, Ellis RJ, Letendre SL, Marcotte TD, Atkinson JH, Rivera-Mindt M, Vigil OR, Taylor MJ, Collier AC, Marra CM, Gelman BB, McArthur JC, Morgello S, Simpson DM, McCutchan JA, Abramson I, Gamst A, Fennema-Notestine C, Jernigan TL, Wong J, Grant I. HIV-associated neurocognitive disorders persist in the era of potent antiretroviral therapy: CHARTER Study. Neurology. 2010;75:2087–2096. doi: 10.1212/WNL.0b013e318200d727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lafayette Instrument Company (2002) Grooved Pegboard Test user instructions. Lafayette Instrument Company: Lafayette IN
- Ownby RL, Kim J (2021) Computer-delivered cognitive training and transcranial direct current stimulation in patients with HIV-associated neurocognitive disorder: a randomized trial. Front Aging Neurosci 13:766311 [DOI] [PMC free article] [PubMed]
- Papandonatos GD, Ott BR, Davis JD, Barco PP, Carr DB. Clinical utility of the Trail-Making Test as a predictor of driving performance in older adults. J Am Geriatr Soc. 2015;63:2358–2364. doi: 10.1111/jgs.13776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reitan RM, Wolfson D. The Halstead-Reitan neuropsychological test battery: theory and clinical interpretation. Tucson AZ: Neuropsychology Press; 1993. [Google Scholar]
- Roy M, Molnar F. Systematic review of the evidence for Trails B cut-off scores in assessing fitness-to-drive. Can Geriatr J. 2013;16:120–142. doi: 10.5770/cgj.16.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas-Purcell Kamilah. Chronic disease self-management of post-acute sequelae of COVID-19 among older adults: a mixed-methods analysis. Clinical Interventions in Aging. 2023;Volume 18:607–617. doi: 10.2147/CIA.S393732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vance DE, Cody SL, Nicholson WC, Cheatwood J, Morrison S, Fazeli PL. The association between olfactory function and cognition in aging African American and Caucasian men with HIV: a pilot study. J Assoc Nurses AIDS Care. 2019;30:e144–e155. doi: 10.1097/JNC.0000000000000086. [DOI] [PubMed] [Google Scholar]
- Vingilis E, Johnson J, Rapoport MJ, Beirness D, Boase P, Byrne PA, Jonah B, Mann RE, Seeley J, Wickens CM, Wiesenthal DL. Addendum - coronavirus disease 2019: what could be the effects on road safety? Accident; Analysis and Prevention. 2021;149:105712–105712. doi: 10.1016/j.aap.2020.105712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D (2008). Manual for the Wechsler Adult Intelligence Scale--IV. Pearson Assessment: San Antonio TX
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data from the original study are available from the corresponding author on reasonable request.


