Abstract
This study examines trends in deaths from falls among adults aged 65 years or older by sex and by race and ethnicity between 1999 and 2020 in the US.
In 2020, 42 114 deaths in the US were related to falls, with 86% occurring among adults aged 65 years or older.1 Falls are the leading cause of injury and among the leading causes of death among older adults in the US.2,3 The increase in the number of older adults in the US and in the number of falls within this population underscore the need for population-level studies on this issue. Calls for such analyses date back to the 1990s,4 yet the majority of studies focus on injuries related to falls.3 More recent calls have also emphasized the need to study racial and ethnic differences in falls among older adults in the US.5 This study examined trends in deaths from falls among US adults aged 65 years or older by sex and by race and ethnicity between 1999 and 2020.
Methods
I analyzed data for all deaths recorded with falls (International Statistical Classification of Diseases and Related Health Problems, Tenth Revision codes W00-W19) as an underlying cause of death between 1999 and 2020 accessed through the Centers for Disease Control and Prevention’s WONDER platform.1 This platform combines death counts with population estimates produced by the US Census Bureau to calculate mortality rates. For each year, I extracted age-adjusted mortality rates (AAMRs) per 100 000 people for adults aged 65 years or older by sex and by race and ethnicity (Table). The AAMR accounts for differences due to age structures, allowing for direct comparisons across groups. Mortality rate ratios (MRRs) were calculated to evaluate the magnitude of the rates in 2020 compared with 1999. Annual percentage changes (APCs) in AAMRs were calculated using RStudio version 1.4.1717 (RStudio PBC). Significance was defined as P < .05 (2-sided). This study used deidentified aggregate data; thus, it was considered nonhuman research by US regulation (45 CFR §46.102[d]).
Table. Deaths Due to Falls Among Adults Aged 65 Years or Older in the US, 1999-2020.
| AAMR (95% CI) per 100 000 by year | Mortality rate ratioa | Total deaths, No. (%) | APC, % (95% CI) | P valueb | ||
|---|---|---|---|---|---|---|
| 1999 (n = 10 097) | 2020 (n = 36 508) | |||||
| Overall | 29.4 (28.8-30.0) | 69.4 (68.7-70.1) | 2.36 | 478 214 | 3.94 (3.56-4.33) | <.001 |
| By sex | ||||||
| Female | 24.3 (23.7-25.0) | 60.4 (59.5-61.2) | 2.49 | 256 296 (53.59) | 4.20 (3.77-4.61) | <.001 |
| Male | 38.3 (37.2-39.5) | 81.8 (80.6-83.1) | 2.14 | 221 918 (46.41) | 3.47 (3.12-3.82) | <.001 |
| By race and ethnicityc | ||||||
| African American | 16.5 (15.0-18.1) | 31.5 (29.9-33.2) | 1.91 | 16 956 (3.55) | 3.23 (2.58-3.88) | <.001 |
| American Indian or Alaska Native | 30.5 (20.8-43.0) | 53.6 (45.2-62.0) | 1.76 | 1901 (0.40) | 2.91 (1.84-3.97) | <.001 |
| Asian or Pacific Islander | 22.9 (19.1-26.7) | 38.0 (35.6-40.4) | 1.66 | 10 774 (2.25) | 2.31 (1.87-2.74) | <.001 |
| Hispanic | 23.4 (20.8-26.0) | 40.5 (38.6-42.4) | 1.73 | 19 779 (4.14) | 2.57 (2.05-3.08) | <.001 |
| White | 30.8 (30.2-31.4) | 78.4 (77.6-79.3) | 2.55 | 427 883 (89.48) | 4.29 (3.92-4.68) | <.001 |
Abbreviations: AAMR, age-adjusted mortality rate; APC, annual percentage change.
A mortality rate ratio greater than 1 represents an increase in the AAMR in 2020 when compared with 1999.
P values are based on a t test that the differences in the APC are 0 with 20 degrees of freedom.
Patterns by race and ethnicity were studied due to calls for such analyses found in existing literature.5 The Centers for Disease Control and Prevention provided information following 1977 Office of Management and Budget standards on race and ethnicity. All groups are composed of non-Hispanic individuals who died, and all Hispanic individuals who died are included as a separate group. Race and ethnicity were recorded in the death certificates. A total of 1384 deaths were excluded from the race and ethnicity analysis due to not having their ethnicity stated in the death certificate.
Results
Between 1999 and 2020, 478 214 deaths from falls occurred among adults aged 65 years or older, increasing from 10 097 in 1999 to 36 508 in 2020 (Table). The overall AAMR increased from 29.4 (95% CI, 28.8-30.0) to 69.4 (95% CI, 68.7-70.1) deaths per 100 000. By sex, the AAMR was highest for men across the period of analysis (rate per 100 000: for men, 38.3 in 1999 and 81.8 in 2020; for women, 24.3 in 1999 and 60.4 in 2020). By race and ethnicity, the AAMR per 100 000 was highest among White (30.8 in 1999; 78.4 in 2020) and American Indian or Alaska Native (30.5 in 1999; 53.6 in 2020) older adults, followed by Hispanic (23.4 in 1999; 40.5 in 2020), Asian or Pacific Islander (22.9 in 1999; 38.0 in 2020), and African American (16.5 in 1999; 31.5 in 2020) older adults. Increases over time within each sex and race and ethnicity subgroup were significant at P < .001.
The MRR increased for adults aged 65 years or older (MRR, 2.63) and all population subgroups, with the magnitude of the increase in AAMRs being highest among women and White older adults. The APCs indicate the rates increased significantly between 1999 and 2020 for the overall population (APC, 3.94% [95% CI, 3.56%-4.33%]) and all population subgroups, and the greatest increases occurred among women and White individuals. Visualizations for the trends for adults aged 65 years or older for the overall population, by sex, and by and race and ethnicity are shown in the Figure.
Figure. Age-Adjusted Mortality Rates for Falls Among Adults Aged 65 Years or Older, 1999-2020.
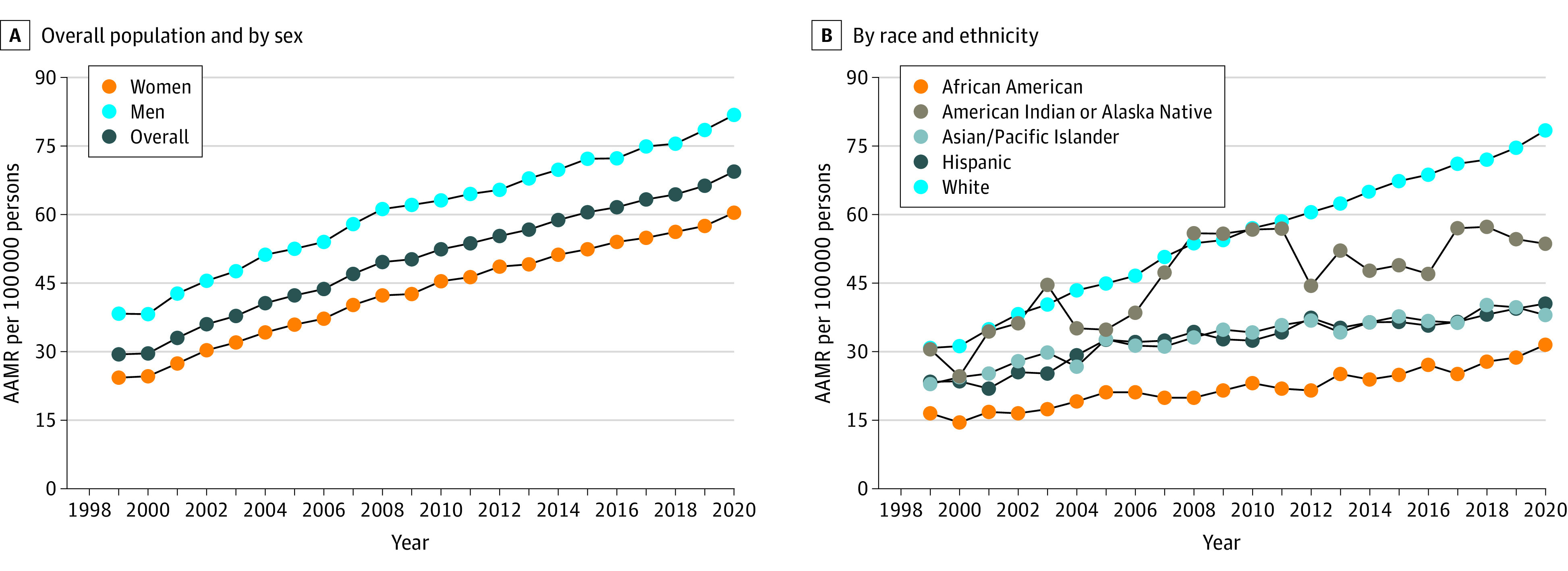
AAMR indicates age-adjusted mortality rate.
Discussion
Between 1999 and 2020, deaths coded as being caused by falls among adults aged 65 years or older increased in number and rates for the overall population and for every population subgroup, although the magnitude of the increase varied. However, the relative ranking of the different groups has not changed over time.
This study has several limitations. First, the study relied on the underlying cause of death as coded in the death certificate and deaths may be misclassified. Second, there were no significant changes in coding of deaths between 1999 and 2020, but improved reporting quality may partly explain the large increase in falls mortality. However, other studies combining national samples and vital records have produced estimates of increased incidence of fall injuries and fatalities,6 supporting these findings. Third, it is not known whether those who died had fallen before and/or where such falls occurred.
Given the increase in mortality due to falls among adults aged 65 years or older, continued work to prevent falls and reduce fall-related mortality is warranted.
Section Editors: Jody W. Zylke, MD, Deputy Editor; Kristin Walter, MD, Senior Editor.
Data Sharing Statement
References
- 1.Centers for Disease Control and Prevention . CDC WONDER: about underlying cause of death, 1999-2020. Accessed November 28, 2022. https://wonder.cdc.gov/ucd-icd10.html
- 2.Burns E, Kakara R. Deaths from falls among persons aged ≥65 years: United States, 2007-2016. MMWR Morb Mortal Wkly Rep. 2018;67(18):509-514. doi: 10.15585/mmwr.mm6718a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moreland B, Kakara R, Henry A. Trends in nonfatal falls and fall-related injuries among adults aged ≥65 years: United States, 2012-2018. MMWR Morb Mortal Wkly Rep. 2020;69(27):875-881. doi: 10.15585/mmwr.mm6927a5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sattin RW. Falls among older persons: a public health perspective. Annu Rev Public Health. 1992;13(79):489-508. doi: 10.1146/annurev.pu.13.050192.002421 [DOI] [PubMed] [Google Scholar]
- 5.Han BH, Ferris R, Blaum C. Exploring ethnic and racial differences in falls among older adults. J Community Health. 2014;39(6):1241-1247. doi: 10.1007/s10900-014-9852-8 [DOI] [PubMed] [Google Scholar]
- 6.Drew JAR, Xu D. Trends in fatal and nonfatal injuries among older Americans, 2004-2017. Am J Prev Med. 2020;59(1):3-11. doi: 10.1016/j.amepre.2020.01.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Sharing Statement


