Abstract
Background
Fibromyalgia is a chronic pain syndrome characterized by persistent and widespread musculoskeletal pain. Telerehabilitation is a promising treatment for patients with fibromyalgia through long-term monitoring, intervention, supervision, consultation, and education.
Objective
This study aimed to perform a comprehensive systematic review and meta-analysis of the efficacy and safety of telerehabilitation in patients with fibromyalgia.
Methods
Randomized controlled trials (RCTs) related to fibromyalgia and telerehabilitation were systematically searched in the PubMed, PEDro, Cochrane Library, ScienceDirect, Ovid MEDLINE, Embase, and Web of Science databases from inception to November 13, 2022. Two independent researchers screened the literatures and evaluated the methodological quality using the Cochrane Risk of Bias Tool. The outcome measures included the Fibromyalgia Impact Questionnaire scale, pain intensity, depression, pain catastrophizing, quality of life (QoL), and adverse events. Pooled effect sizes were calculated by Stata SE 15.1; a fixed effects model was used when I2<50%, whereas a random effects model was used when I2≥50%.
Results
A total of 14 RCTs with 1242 participants were included in this meta-analysis. The pooled results indicated that the telerehabilitation improved the Fibromyalgia Impact Questionnaire score (weighted mean difference –8.32, 95% CI –11.72 to –4.91; P<.001), pain intensity (standardized mean difference [SMD] –0.62, 95% CI –0.76 to –0.47; P<.001), depression levels (SMD –0.42, 95% CI –0.62 to –0.22; P<.001), pain catastrophizing (weighted mean difference –5.81, 95% CI –9.40 to –2.23; P=.001), and QoL (SMD 0.32, 95% CI 0.18 to 0.47; P<.001) in patients with fibromyalgia compared to control interventions. Only 1 RCT reported a mild adverse event of telerehabilitation; the other 13 RCTs did not mention this.
Conclusions
Telerehabilitation can improve the symptoms and QoL of fibromyalgia. However, the safety of telerehabilitation remains uncertain due to the lack of sufficient evidence for the management of fibromyalgia. More rigorously designed trials are needed in the future to verify the safety and efficacy of telerehabilitation in fibromyalgia.
Trial Registration
PROSPERO CRD42022338200; https://tinyurl.com/322keukv
Keywords: telerehabilitation, fibromyalgia, systematic review, meta-analysis, rehabilitation, chronic pain, pain, musculoskeletal, monitoring, intervention, consultation, education, efficacy, safety
Introduction
Background
Fibromyalgia is a common chronic pain syndrome characterized by persistent and widespread musculoskeletal pain that is usually accompanied by sleep disruption, fatigue, cognitive dysfunctions, and depressed mood [1,2]. The persistent physical and psychological symptoms of fibromyalgia lead to a decrease in patients’ quality of life (QoL) and cause a huge economic burden on their families and society [3,4]. The main goals of fibromyalgia treatment are to reduce symptoms, maintain function, and improve QoL. Various treatments have been recommended for the management of fibromyalgia, such as medication, exercise, education, and psychotherapy [5-7]. However, patients with fibromyalgia require long-term clinical management and follow-up [8].
Telerehabilitation is defined as “the provision of rehabilitation services through information and telecommunications technology” [9,10], which can provide the assessment, intervention, supervision, education, monitoring, consultation, and prevention of disease [11]. Telerehabilitation can effectively facilitate real-time communication between patients and health care providers and increase patients’ access to medical help from specialized physicians and therapists [12,13]. Telerehabilitation also can tailor long-term and ongoing telerehabilitation services according to the needs of the patients [14]. Telerehabilitation has been widely used in the management of neurological [14], cardiorespiratory [15], and musculoskeletal disorder [16]. In particular, telerehabilitation has been recommended for managing chronic pain worldwide during the current COVID-19 pandemic situation [17].
With the rapid development of telecommunication technology, a number of randomized controlled trials (RCTs) on the application of telerehabilitation in patients with fibromyalgia have been published recently. For example, Hernando-Garijo et al [18] suggested that video-guided, aerobic exercise–based telerehabilitation could effectively reduce pain and improve psychological distress in patients with fibromyalgia. Lee et al [19] made remote real-time pain monitoring and rehabilitation interventions for fibromyalgia using wearable device. In addition, Molinari et al [20] and Yuan et al [21] found a positive effect of a mobile app or multimedia interactive system–based telerehabilitation intervention on individuals with fibromyalgia. However, few systematic reviews have summarized the characteristics, efficacy, and safety of telerehabilitation in fibromyalgia. According to our knowledge, only one review by Bernardy et al [22] has investigated the effects of internet-delivered psychotherapy in individuals with fibromyalgia. However, this study only focused on internet-delivered psychotherapy and ignored other types of telerehabilitation services, such as mobile apps, videoconferencing, web-based education, and wearable devices.
Objectives
Therefore, this study aimed to perform a comprehensive systematic review and meta-analysis of the efficacy and safety of telerehabilitation in patients with fibromyalgia.
Methods
This study was carried out by adhering to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines and was registered in the International Prospective Register of Systematic Reviews (PROSPERO; CRD42022338200).
Search Strategy
The PubMed, PEDro, Web of Science, ScienceDirect, Ovid MEDLINE, Cochrane Library, and Embase electronic databases were searched from inception to November 13, 2022. The following keywords and their combinations were used for the literature search: “Telerehabilitation,” “Telemedicine,” “eHealth,” “Videoconferencing,” “Wireless Technology,” “Mobile Health,” “Computer Communication Networks,” “Internet-Based Intervention,” “Fibromyalgia Syndrome,” and “Fibromyalgia.” The detailed search strategy is described in Multimedia Appendix 1. Furthermore, we manually searched the reference lists of eligible studies to identify additional studies.
Study Selection Criteria
Two independent researchers (YQW and Y Long) selected studies following the framework of Population, Intervention, Comparison, Outcomes, and Study Design. Any divergence during the screening process was resolved through consultation between the 2 researchers. If there was still no agreement, a third independent researcher (WJP) decided after group discussion.
All potentially eligible studies were screened following the pre-established criteria. The inclusion criteria were as follows: (1) RCTs; (2) patients were adults aged ≥18 years with a diagnosis of fibromyalgia according to the American College of Rheumatology criteria; (3) the intervention of the experiment group was telerehabilitation, with no restrictions on the specific modality of technology and the content of telerehabilitation; and (4) the control group received non-telerehabilitation including usual care, waiting list, no intervention, or conventional face-to-face treatment. The exclusion criteria were as follows: (1) the study was a case report, conference abstract, or review article; (2) the study was not published in English; and (3) the study only compared different types of telerehabilitation.
Data Extraction
Two investigators (YQW and XMP) independently completed the data extraction. The data included the first author, the year of publication, sample size, study design, characteristics of the participants (gender, age, diagnosis, duration of symptoms, etc), interventions, and outcome measures. When data were lacking, we tried to contact the corresponding author to obtain missing data. If there was a divergence between the reviewers, it was resolved by consultation with a third independent researcher (Y Luo).
Methodological Quality Assessment
Two independent reviewers (CG and YQL) assessed the methodological quality using the Cochrane Risk of Bias Tool [23]. The tool includes the following domains: (1) sequence generation (selection bias), (2) allocation concealment (selection bias), (3) blinding of participants and personal (performance bias), (4) blinding of outcome assessment (detection bias), (5) incomplete outcome data (attrition data), (6) selective reporting (reporting bias), and (7) other sources of bias.
Outcome Measures
Efficacy outcomes were evaluated using the Fibromyalgia Impact Questionnaire (FIQ) scale; pain intensity (eg, the Visual Analog Scale [VAS] and Brief Pain Inventory [BPI]); depression (eg, the Patient Health Questionnaire, the Beck Depression Inventory, the Center for Epidemiological Studies Depression Scale, and the Hospital Anxiety and Depression Scale-Depression); pain catastrophizing (Pain Catastrophizing Scale [PCS]); and QoL (Short Form Health Survey and the EQ-5D). Safety outcomes were evaluated based on adverse events.
Statistical Analysis
The statistical analysis was performed using the Stata software (version 15.1 SE; StataCorp). If outcomes were measured using different scales, we used the standardized mean difference (SMD) and 95% CI. Otherwise, when outcomes were measured using the same scales, we used the weighted mean difference (WMD) and 95% CI. Statistical heterogeneity was evaluated using the I2 statistic [24]. I2 values >75% indicated high levels of heterogeneity, I2 values ≥50% indicated medium levels of heterogeneity, and I2 values >25% indicated low levels of heterogeneity. If I2≥50%, we used the random effects model. Otherwise, we used the fixed effects model for data analysis. For the results of ≥10 included studies, publication bias in the meta-analysis was detected by performing Egger regression test and Begg rank correlation test [25,26].
Results
Study Inclusion
In total, 1382 records were identified from the 7 databases. After removing duplicates, screening the titles and abstracts, and reviewing the full-text, 1368 articles were excluded and 14 studies were considered eligible for this systematic review and meta-analysis [18-21,27-36] (Figure 1).
Figure 1.
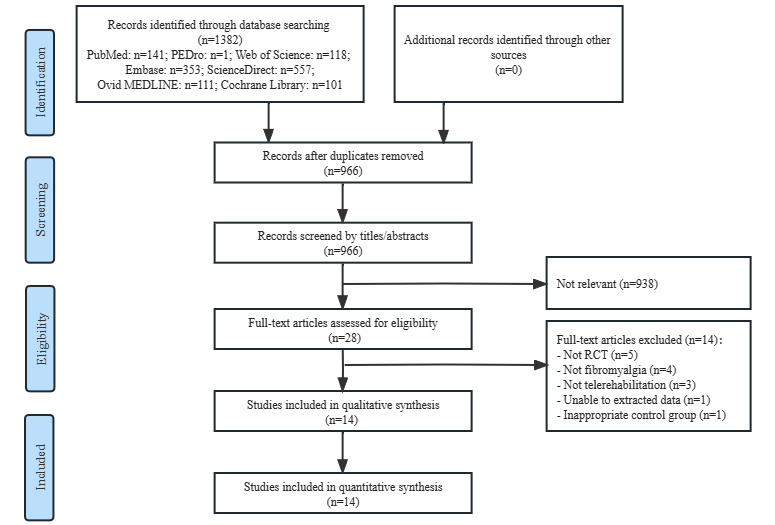
Flowchart of study selection. RCT: randomized controlled trial.
Study Characteristics
Table 1 summarizes the main clinical characteristics of the included studies. The 14 RCTs included 1242 participants diagnosed with fibromyalgia. The mean age of the participants ranged from 39.7 to 55.5 years. The duration of the symptoms ranged from 6.21 to 20 years. The control intervention of the included studies involved a waiting list [30-32], usual care or treatment [18,19,27,28,33,35,36], pharmacologic therapy [29], daily activity [20], standard follow-up [34], and paper-based instruction [21]. The 14 RCTs reported different outcomes: 12 studies measured the FIQ scale [18-21,29-36], 8 assessed pain intensity [18,19,21,27,28,31,32,36], 11 assessed depression [18-20,27,28,30-33,35,36], 3 assessed pain catastrophizing [18,20,33], and 6 assessed QoL [19,28,31,34-36] (Table 1).
Table 1.
Clinical characteristics of the included studies.
| Study | Sample size, n | Sex (male/female), n | Age (years), mean (SD) | Duration of symptoms (years) | Interventions | Duration of intervention | Outcome index | Adverse event |
| Williams et al [28], 2010 |
|
|
|
|
|
6 months | BPIe, SF-36f, CES-Dg, MFIh, MOSi, and STPIj | Not mention |
| Ang et al [27], 2010 |
|
|
|
|
|
6 weeks | NFRl threshold, FIQm-pain rating, and PHQ-8n | Not mention |
| Menga et al [29], 2014 |
|
|
|
|
|
6 and 12 months | FIQ and Number of Tender Points | Not mention |
| Vallejo, et al [30], 2015 |
|
|
|
|
|
10 weeks | FIQ, PCSp, HADSq, BDIr, and CPSSs | Not mention |
| Friesen, et al [31], 2017 |
|
|
|
|
|
8 weeks | FIQ-Rt, BPI, GAD-7u, HADS, SF-12, and PSEQv | Not mention |
| Hedman-Lagerlöf et al [32], 2018 |
|
|
|
|
|
10 weeks | FIQ, FIQ-pain, FFSx, WHO-DAS IIy, depressive symptoms using the PHQ-9, GAD-7, and ISIz | Increased pain |
| Molinari et al [20], 2018 |
|
|
|
|
|
4 weeks | Depression BDI-II, PANASab, GSES-12ac, FIQ-R, and PCS | Not mention |
| Simister et al [33], 2018 |
|
|
|
|
|
2 months | FIQ-R, CES-D, FFMQaf, CFQag, and SF-MPQah | Not mention |
| Lee et al [19], 2019 |
|
|
|
|
|
3 months | FIQ, VASaj, BDI, and EQ-5D | Not mention |
| García-Perea et al [34], 2021 |
|
|
|
|
|
6 and 12 months | FIQ and SF-36 | Not mention |
| Yuan et al [21], 2021 |
|
|
|
|
|
6 weeks | FIQ-R, VAS, WPIak, symptom severity, and self-care | Not mention |
| Serrat et al [35], 2021 |
|
|
|
|
|
12 weeks | FIQ-R, TSKal, HADS-Anxiety and HADS-Depression, and SF-36 | Not mention |
| Hernando-Garijo et al [18], 2021 |
|
|
|
|
|
15 weeks | FIQ, VAS, Algometer score, PCS, HADS, 6-min Walk Test, and Arm Curl Test | Not mention |
| Serrat et al [36], 2022 |
|
|
|
|
|
12 weeks | FIQ-R, VAS, HADS, and SF-36 | Not mention |
aEG: experimental group.
bCG: control group.
cWEB-SM: Web-Enhanced Behavioral Self-management.
dUC: usual care.
eBPI: Brief Pain Inventory.
fSF: Short Form Health Survey Questionnaire.
gCES-D: The Center for Epidemiological Studies Depression Scale.
hMFI: Multidimensional Fatigue Inventory.
iMOS: Medical Outcomes Study.
jSTPI: State-Trait Personality Inventory.
kCBT: cognitive behavioral therapy.
lNFR: Nociceptive Flexion Reflex.
mPHQ: Patient Health Questionnaire.
nFIQ: Fibromyalgia Impact Questionnaire.
oiCBT: internet-delivered cognitive behavioral therapy.
pPCS: Pain Catastrophizing Scale.
qHADS: Hospital Anxiety and Depression Scale.
rBDI: Beck Depression Inventory.
sCPSS: Chinese version of the Perceived Stress Scale.
tFIQ-R: Revised Fibromyalgia Impact Questionnaire
uGAD-7: Generalized Anxiety Disorder 7-Item.
vPSEQ: Pain Self-Efficacy Questionnaire.
wiEXP: internet-delivered exposure treatment.
xFFS: Fatigue Severity Scale.
yWHO-DAS II: the World Health Organization Disability Assessment Schedule II.
zISI: Insomnia Severity Index.
aaBPS: Best Possible Self.
abPANAS: The Positive and Negative Affect Scale.
acGSES-12: General Self Efficacy Scale.
adACT: acceptance and commitment therapy.
aeTAU: treatment as usual.
afFFMQ: The Five Facet Mindfulness Questionnaire.
agCFQ: The Cognitive Fusion Questionnaire.
ahSF-MPQ: The McGill Pain Questionnaire-short form.
aiPAAS: Pain Assessment and Analysis System.
ajVAS: Visual Analog Scale for Pain.
akWPI: Widespread Pain Index.
alTSK: The Tampa Scale for Kinesiophobia.
amMPP: Multicomponent Physiotherapy Program.
Table 2 summarizes the detailed protocols of telerehabilitation among the included studies. Regarding the medium of telerehabilitation, 8 studies used internet-based telerehabilitation [20,28,29,31-33,35,36], 5 used telephone- or mobile app–based telerehabilitation [18,21,27,30,34], and 1 used a wearable device to monitor and record real-time pain [19]. In terms of telerehabilitation programs, 6 studies used psychological interventions–based telerehabilitation [20,27,29,30,32,33], 2 used fibromyalgia self-management–based telerehabilitation [21,28], 3 used video-based guided exercise training telerehabilitation [18,35,36], 1 used a web-based pain course–based telerehabilitation [31], 1 provided real-time pain monitoring by a monitoring system [19], and 1 study provided web-based teleconsultation [34].
Table 2.
Specific protocol of telerehabilitation among the included studies.
| Study | Medium | Program |
| Williams et al [28], 2010 | Internet |
|
| Ang et al [27], 2010 | Telephone |
|
| Menga et al [29], 2014 | Internet |
|
| Vallejo et al [30], 2015 | Mobile app |
|
| Friesen et al [31], 2017 | Internet |
|
| Hedman-Lagerlöf et al [32], 2018 | Internet |
|
| Molinari et al [20], 2018 | Internet |
|
| Simister et al [33], 2018 | Internet |
|
| Lee et al [19], 2019 | Wearable device and mobile app |
|
| García-Perea et al [34], 2021 | Mobile app |
|
| Yuan et al [21], 2021 | Mobile app |
|
| Serrat et al [35], 2021 | Internet |
|
| Hernando-Garijo et al [18], 2021 | Telephone |
|
| Serrat et al [36], 2022 | Internet |
|
aCBT: cognitive behavioral therapy.
bMoodGYM: a free interactive web-based program [37].
cPAAS: Pain Assessment and Analysis System.
dFIQ: Fibromyalgia Impact Questionnaire.
ePNE: Pain Neuroscience Education.
Results From Quality Assessments
The risk of bias assessment according to the Cochrane criteria is shown in Figures 2 and 3. All trials reported a randomized method, providing a random sequence generation method, and one trial [36] reported an unclear allocation concealment method. One trial [33] was not blinded to the outcome assessment, and 5 trials [19,27,29,31,36] did not elaborate on whether the outcome assessment was blinded. Only three [20,29,32] of the 14 trials did not explicitly report whether they blinded the subjects. In addition, only 2 trials [27,33] mentioned dropout, but only 1 trial [27] did not elaborate on information processing.
Figure 2.
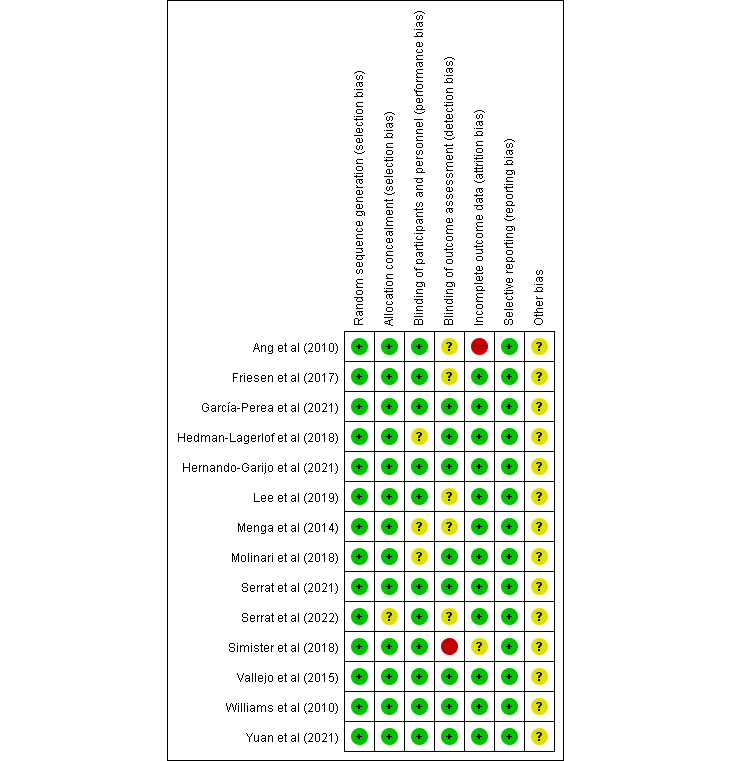
Risk of bias summary: review authors’ judgements about each risk of bias item for each included study [18-21,27-36].
Figure 3.
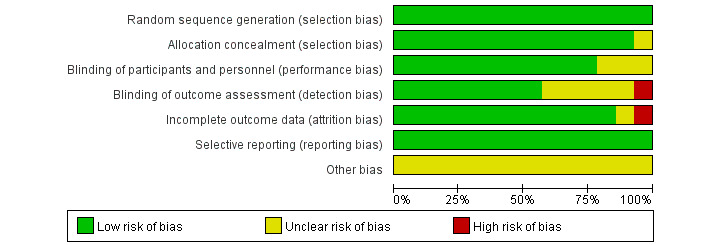
Risk of bias graph: review authors’ judgements about each risk of bias item presented as percentages across all included studies.
Effect of Telerehabilitation on the FIQ Scale
Twelve studies with 1076 participants [18-21,29-36] reported FIQ scale data. Owing to the existence of medium heterogeneity (I2=59.9%; P=.004), a random effects model was used. A meta-analysis showed that telerehabilitation had significantly reduced the FIQ scale score compared to the control group (WMD –8.32, 95% CI –11.72 to –4.91; P<.001; Figure 4).
Figure 4.
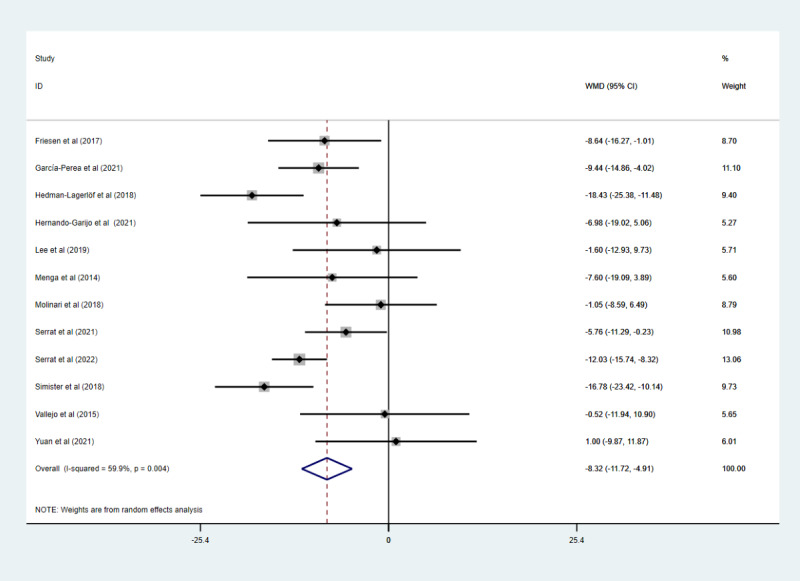
The effect of telerehabilitation on the Fibromyalgia Impact Questionnaire scale in fibromyalgia. WMD: weighted mean difference.
Effect of Telerehabilitation on Pain Intensity
Eight studies with 769 participants assessed pain intensity. Four studies used the VAS [18,19,21,36], 2 used FIQ-pain [27,32], and 2 used the BPI [28,31]. Due to the low heterogeneity (I2=0%; P=.61), a fixed effects model was used in the meta-analysis (Figure 5). The pooled results indicated that telerehabilitation had significantly improved pain intensity compared to the control group (SMD –0.62, 95% CI –0.76 to –0.47; P<.001).
Figure 5.
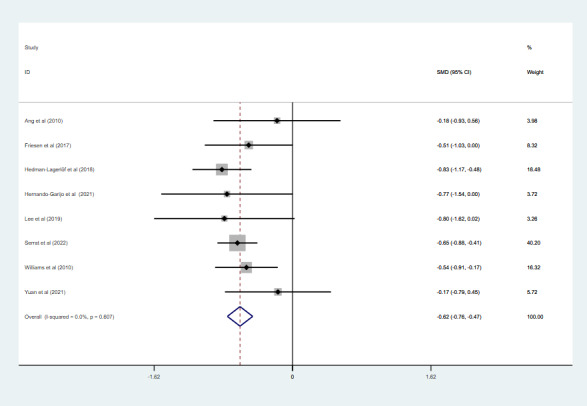
The effect of telerehabilitation on pain intensity in fibromyalgia. SMD: standardized mean difference.
Effect of Telerehabilitation on Depression
Eleven studies with 1058 participants assessed the depression levels. Two studies used the Patient Health Questionnaire [27,32], 2 used the Center for Epidemiological Studies Depression Scale [28,33], 3 used the Beck Depression Inventory [19,20,30], and 4 used the Hospital Anxiety and Depression Scale-Depression scale [18,31,35,36]. Due to the medium heterogeneity (I2=51.7%; P=.02), pooled results under a random effects model (Figure 6) indicated that telerehabilitation reduced the depression levels of patients with fibromyalgia (SMD –0.42, 95% CI –0.62 to –0.22; P<.001).
Figure 6.
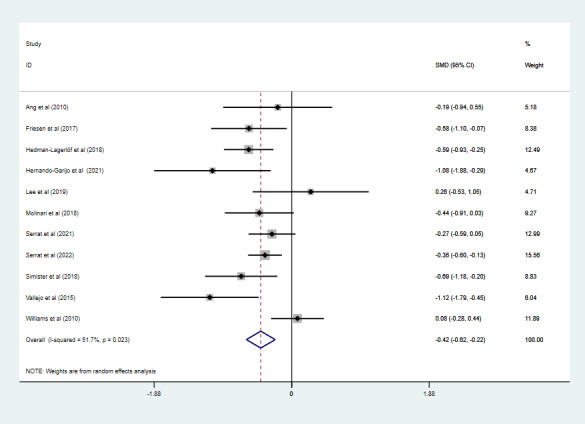
The effect of telerehabilitation on depression in fibromyalgia. SMD: standardized mean difference.
Effect of Telerehabilitation on Pain Catastrophizing
Pain catastrophizing was measured using the PCS. Three studies with 139 participants reported PCS data [18,20,30]. Because of the low heterogeneity (I2=40.2%; P=.19), a fixed effects model was used in the meta-analysis (Figure 7). The pooled results showed that telerehabilitation had significantly reduced PCS scores compared to the control group (WMD –5.81, 95% CI –9.40 to –2.23; P=.001).
Figure 7.
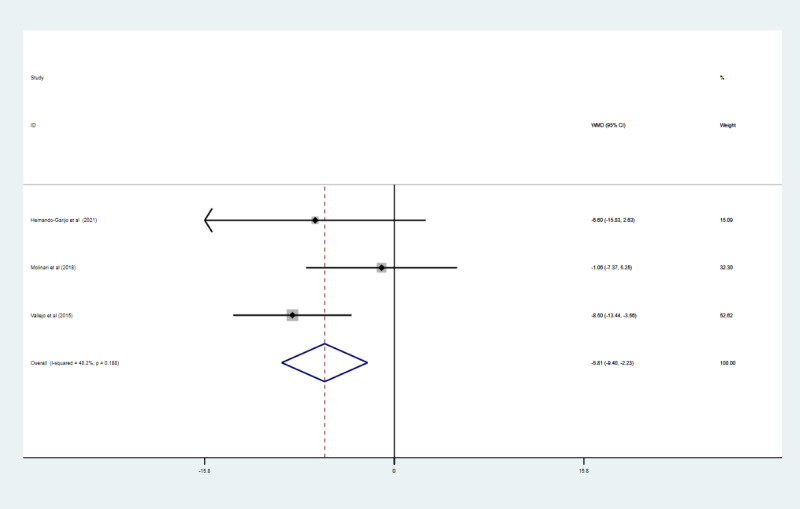
The effect of telerehabilitation on pain catastrophizing in fibromyalgia. WMD: weighted mean difference.
Effect of Telerehabilitation on QoL
Six studies with 764 participants assessed QoL. The QoL was assessed using the Short Form Health Survey in 5 studies [28,31,34-36] and the EQ-5D in 1 study [19]. In these studies, we found no significant heterogeneity in the QoL (I2=0%; P=.56). Pooled results under a fixed effects model (Figure 8) indicated that telerehabilitation had significantly improved the QoL compared with the control group (SMD 0.32, 95% CI 0.18 to 0.47; P<.001).
Figure 8.
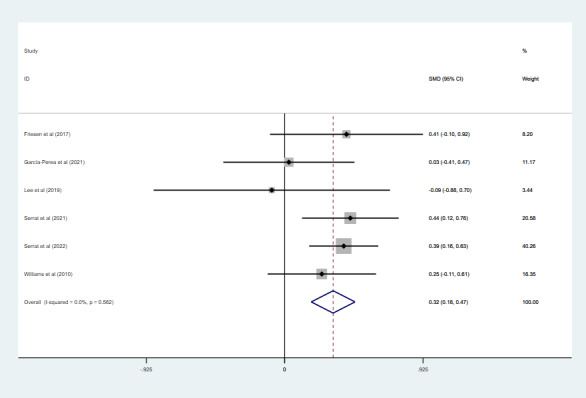
The effect of telerehabilitation on the quality of life in fibromyalgia. SMD: standardized mean difference.
Adverse Events
Only 1 RCT [32] reported an adverse event; the other 13 RCTs did not mention it. Hedman-Lagerlöf et al [32] reported that 34% of participants who received internet-based telerehabilitation experienced mild pain, but regression analysis showed no significant relationship between adverse events and telerehabilitation intervention.
Publication Bias
No publication bias was found for the FIQ (Egger: P=.11; Begg: P=.30) and depression (Egger: P=.44; Begg: P=.44) in the funnel plot (Multimedia Appendix 2).
Discussion
Principal Findings
The aim of this meta-analysis was to summarize the current evidence about the efficacy and safety of telerehabilitation for patients with fibromyalgia. The results of this meta-analysis indicated that telerehabilitation can improve the FIQ score, pain intensity, depression, and QoL in patients with fibromyalgia compared to control interventions (eg, waiting list, pharmacologic therapy, and other active nonpharmacological therapies). Importantly, we also considered another important factor applied to patients with fibromyalgia: the safety of telerehabilitation. Only 1 study of the included studies reported mild adverse events after telerehabilitation [32]. Therefore, the evidence is not yet sufficient to draw firm conclusions about the safety of telerehabilitation for patients with fibromyalgia.
The key to whether telerehabilitation can be applied in patients with fibromyalgia is considering the clinical significance and the economic and social benefits. Our results indicate that telerehabilitation can effectively alleviate the symptoms in patients with fibromyalgia. Meanwhile, there are a lot of potential advantages of telerehabilitation, such as improving the efficiency of health professionals and providing people with various health care resources (eg, knowledge, fibromyalgia education, and exercise guidance) about fibromyalgia and personalized rehabilitation recommendations [38]. More importantly, telerehabilitation can overcome geographical barriers and provide medical care services to people in rural and remote communities and patients with fibromyalgia who cannot attend traditional face-to-face rehabilitation services, which is especially essential during the COVID-19 pandemic [39]. In addition, although none of the included studies in this meta-analysis reported cost-effectiveness, several previous studies have demonstrated that telerehabilitation can reduce the monetary and time costs of rehabilitation services [40,41].
Comparison With Prior Work
In this meta-analysis, telerehabilitation was considered as a rehabilitation service of various telecommunication technology [42]. Currently, it is possible to apply telecommunication technology to rehabilitation service in clinical practice through cell phones, applications, virtual reality devices, and other electronic devices [43]. Telerehabilitation can deliver rehabilitation management services such as assessment, intervention, and patient consultation. The studies included in this meta-analysis primarily used the internet, telephone or mobile apps, and wearable devices to provide telerehabilitation services, including consultation, monitoring, education, and intervention. In addition, the conventional face-to-face management of fibromyalgia currently is mainly a nonpharmacological interventions tailored to individual symptoms, such as psychotherapy, exercise, and self-management strategies that involve active patient participation [44]. However, in this meta-analysis, the interventions of the included studies used 3 rehabilitation interventions, with psychological interventions being the mainstay, followed by video-guided exercise training and self-management.
Few systematic reviews have investigated the effects of telerehabilitation in patients with fibromyalgia. To the best of our knowledge, only 1 review by Bernardy et al [22] has investigated the effects of internet-delivered psychotherapy with fibromyalgia. They found that telerehabilitation reduced negative mood and improved QoL, which was consistent with our findings. However, in terms of pain intensity, there was no significant improvement in the telerehabilitation group compared to the control group, which is inconsistent with our results. This is because their study used an established dichotomous variable to assess pain, whereas our study used a continuous variable based on the VAS, BPI, and FIQ-pain to reflect pain improvement. Overall, this meta-analysis indicated that telerehabilitation has a positive effect on the FIQ score, pain intensity, depression, and QoL in patients with fibromyalgia.
Challenges of Telerehabilitation for the Management of Fibromyalgia
Furthermore, there are several challenges to consider when telerehabilitation is applied in clinical settings. First, since telerehabilitation requires patients to be proficient in telecommunication technology, it may be difficult for patients unfamiliar with modern technology (eg, individuals with low IT literacy). In addition, some studies have suggested that the protection of patients’ privacy and supervision of relevant laws and regulations are also important factors influencing their willingness to use telerehabilitation [45,46]. Finally, the safety of telerehabilitation treatment remains unclear in patients with fibromyalgia. More research is required in the future to investigate the safety of telerehabilitation for patients with fibromyalgia.
Limitations
This study had several limitations. First, the studies included in this meta-analysis were heterogeneous with respect to the medium and programs of telerehabilitation in the intervention group. Second, only 2 studies included a 6-month follow-up period, so this meta-analysis only examined the short-term effects of telerehabilitation. Therefore, the long-term effects are still unclear. Third, all eligible studies were published in English, and it is likely that relevant studies published in other languages have been omitted, resulting in a language bias.
Clinical Implications
Our study found that telerehabilitation is an effective treatment approach for patients with fibromyalgia. Telerehabilitation can provide accessible and continuous rehabilitation medical services for patients with fibromyalgia who cannot attend traditional face-to-face services or are geographically remote, and it could enable patients to manage their disease at any time and place in a timely and appropriate manner.
More high-quality studies are required in the future to determine the efficacy of different forms of telerehabilitation and to focus on longer follow-ups to assess long-term outcomes in patients with fibromyalgia.
Conclusion
Telerehabilitation can improve the FIQ score, pain intensity, depression level, pain catastrophizing, and QoL of patients with fibromyalgia. However, there was uncertainty about the safety of telerehabilitation, so rigorously designed trials are needed in the future to verify the safety and efficacy of telerehabilitation in fibromyalgia.
Acknowledgments
This work was supported by the Key Research and Development Project of Jiangxi Province (20203BBGL73127) and the Education Department Project of Jiangxi Province (GJJ190808) to MYW.
Abbreviations
- BPI
Brief Pain Inventory
- FIQ
Fibromyalgia Impact Questionnaire
- PCS
Pain Catastrophizing Scale
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses PROSPERO: International Prospective Register of Systematic Reviews
- QoL
quality of life
- RCT
randomized controlled trial
- SMD
standardized mean difference
- VAS
Visual Analogue Scale
- WMD
weighted mean difference
Search strategy.
Funnel plots.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) checklist.
Footnotes
Authors' Contributions: YQW and Y Long are the cofirst authors and have equal contributions. Y Luo (735083566@qq.com), YBZ (zhongyb2010@163.com), and MYW are joint corresponding authors. Y Luo, YBZ, and MYW contributed to the conception and design of the study. YQW, Y Long, WJP, CG, XMP, and YQL contributed to the literature search, data extraction, and methodological quality assessment. YQW and Y Long contributed to data analysis and interpretation. YQW and Y Long drafted the paper and completed the paper revision. All coauthors reviewed and approved the final manuscript.
Conflicts of Interest: None declared.
References
- 1.Giorgi V, Sirotti S, Romano ME, Marotto D, Ablin JN, Salaffi F, Sarzi-Puttini P. Fibromyalgia: one year in review 2022. Clin Exp Rheumatol. 2022 Jun;40(6):1065–1072. doi: 10.55563/clinexprheumatol/if9gk2. https://www.clinexprheumatol.org/pubmed/find-pii.asp?pii=35748720 .18644 [DOI] [PubMed] [Google Scholar]
- 2.Sarzi-Puttini P, Giorgi V, Marotto D, Atzeni F. Fibromyalgia: an update on clinical characteristics, aetiopathogenesis and treatment. Nat Rev Rheumatol. 2020 Nov 06;16(11):645–660. doi: 10.1038/s41584-020-00506-w.10.1038/s41584-020-00506-w [DOI] [PubMed] [Google Scholar]
- 3.Cabo-Meseguer A, Cerdá-Olmedo Germán, Trillo-Mata JL. Fibromyalgia: Prevalence, epidemiologic profiles and economic costs. Med Clin (Barc) 2017 Nov 22;149(10):441–448. doi: 10.1016/j.medcli.2017.06.008.S0025-7753(17)30477-3 [DOI] [PubMed] [Google Scholar]
- 4.D'Onghia M, Ciaffi J, Ruscitti P, Cipriani P, Giacomelli R, Ablin JN, Ursini F. The economic burden of fibromyalgia: a systematic literature review. Semin Arthritis Rheum. 2022 Oct;56:152060. doi: 10.1016/j.semarthrit.2022.152060.S0049-0172(22)00111-1 [DOI] [PubMed] [Google Scholar]
- 5.Kim SY, Busch AJ, Overend TJ, Schachter CL, van der Spuy I, Boden C, Góes Suelen M, Foulds HJ, Bidonde J. Flexibility exercise training for adults with fibromyalgia. Cochrane Database Syst Rev. 2019 Sep 02;9(9):CD013419. doi: 10.1002/14651858.CD013419. https://europepmc.org/abstract/MED/31476271 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cohen-Biton L, Buskila D, Nissanholtz-Gannot R. Review of fibromyalgia (FM) syndrome treatments. Int J Environ Res Public Health. 2022 Sep 24;19(19):12106. doi: 10.3390/ijerph191912106. https://www.mdpi.com/resolver?pii=ijerph191912106 .ijerph191912106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kundakci B, Kaur J, Goh SL, Hall M, Doherty M, Zhang W, Abhishek A. Efficacy of nonpharmacological interventions for individual features of fibromyalgia: a systematic review and meta-analysis of randomised controlled trials. Pain. 2022 Aug 01;163(8):1432–1445. doi: 10.1097/j.pain.0000000000002500.00006396-900000000-97874 [DOI] [PubMed] [Google Scholar]
- 8.Gota CE. What you can do for your fibromyalgia patient. Cleve Clin J Med. 2018 May 01;85(5):367–376. doi: 10.3949/ccjm.85gr.18002. https://www.ccjm.org/cgi/pmidlookup?view=long&pmid=29733785 . [DOI] [PubMed] [Google Scholar]
- 9.Pastora-Bernal J, Estebanez-Pérez María-José, Molina-Torres G, García-López Francisco-José, Sobrino-Sánchez Raquel, Martín-Valero Rocío. Telerehabilitation intervention in patients with COVID-19 after hospital discharge to improve functional capacity and quality of life. study protocol for a multicenter randomized clinical trial. Int J Environ Res Public Health. 2021 Mar 12;18(6):2924. doi: 10.3390/ijerph18062924. https://www.mdpi.com/resolver?pii=ijerph18062924 .ijerph18062924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Duruturk N. Telerehabilitation intervention for type 2 diabetes. World J Diabetes. 2020 Jun 15;11(6):218–226. doi: 10.4239/wjd.v11.i6.218. https://www.wjgnet.com/1948-9358/full/v11/i6/218.htm . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nizeyimana E, Joseph C, Plastow N, Dawood G, Louw QA. A scoping review of feasibility, cost, access to rehabilitation services and implementation of telerehabilitation: implications for low- and middle-income countries. Digit Health. 2022 Oct 11;8:20552076221131670. doi: 10.1177/20552076221131670. https://journals.sagepub.com/doi/10.1177/20552076221131670?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub0pubmed .10.1177_20552076221131670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rosen MJ. Telerehabilitation. Telemed J E Health. 2004;10(2):115–7. doi: 10.1089/tmj.2004.10.115. [DOI] [PubMed] [Google Scholar]
- 13.Xie SH, Wang Q, Wang LQ, Wang L, Song KP, He CQ. Effect of internet-based rehabilitation programs on improvement of pain and physical function in patients with knee osteoarthritis: systematic review and meta-analysis of randomized controlled trials. J Med Internet Res. 2021 Jan 05;23(1):e21542. doi: 10.2196/21542. https://www.jmir.org/2021/1/e21542/ v23i1e21542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cacciante L, Pietà Camilla Della, Rutkowski S, Cieślik B, Szczepańska-Gieracha J, Agostini M, Kiper P. Cognitive telerehabilitation in neurological patients: systematic review and meta-analysis. Neurol Sci. 2022 Feb 25;43(2):847–862. doi: 10.1007/s10072-021-05770-6. https://europepmc.org/abstract/MED/34822030 .10.1007/s10072-021-05770-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Suso-Martí Luis, La Touche R, Herranz-Gómez Aida, Angulo-Díaz-Parreño Santiago, Paris-Alemany A, Cuenca-Martínez Ferran. Effectiveness of telerehabilitation in physical therapist practice: an umbrella and mapping review with meta-meta-analysis. Phys Ther. 2021 May 04;101(5):pzab075. doi: 10.1093/ptj/pzab075. https://europepmc.org/abstract/MED/33611598 .6145901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cottrell MA, Galea OA, O'Leary SP, Hill AJ, Russell TG. Real-time telerehabilitation for the treatment of musculoskeletal conditions is effective and comparable to standard practice: a systematic review and meta-analysis. Clin Rehabil. 2017 May;31(5):625–638. doi: 10.1177/0269215516645148.0269215516645148 [DOI] [PubMed] [Google Scholar]
- 17.Eccleston C, Blyth FM, Dear BF, Fisher EA, Keefe FJ, Lynch ME, Palermo TM, Reid MC, Williams ACDC. Managing patients with chronic pain during the COVID-19 outbreak: considerations for the rapid introduction of remotely supported (eHealth) pain management services. Pain. 2020 May;161(5):889–893. doi: 10.1097/j.pain.0000000000001885. https://europepmc.org/abstract/MED/32251203 .00006396-202005000-00003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hernando-Garijo Ignacio, Ceballos-Laita Luis, Mingo-Gómez María Teresa, Medrano-de-la-Fuente Ricardo, Estébanez-de-Miguel Elena, Martínez-Pérez María Natividad, Jiménez-Del-Barrio Sandra. Immediate effects of a telerehabilitation program based on aerobic exercise in women with fibromyalgia. Int J Environ Res Public Health. 2021 Feb 20;18(4):622–626. doi: 10.3390/ijerph18042075. https://www.mdpi.com/resolver?pii=ijerph18042075 .ijerph18042075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee J, Park S, Ju JH, Cho JH. Application of a real-time pain monitoring system in Korean fibromyalgia patients: a pilot study. Int J Rheum Dis. 2019 May;22(5):934–939. doi: 10.1111/1756-185X.13472. [DOI] [PubMed] [Google Scholar]
- 20.Molinari G, García-Palacios Azucena, Enrique. Roca P, Fernández-Llanio Comella Nagore, Botella C. The power of visualization: back to the future for pain management in fibromyalgia syndrome. Pain Med. 2018 Jul 01;19(7):1451–1468. doi: 10.1093/pm/pnx298.4775212 [DOI] [PubMed] [Google Scholar]
- 21.Yuan Susan Lee King, Couto Letícia Assis, Marques Amélia Pasqual. Effects of a six-week mobile app versus paper book intervention on quality of life, symptoms, and self-care in patients with fibromyalgia: a randomized parallel trial. Braz J Phys Ther. 2021 Dec;25(4):428–436. doi: 10.1016/j.bjpt.2020.10.003. https://europepmc.org/abstract/MED/33248904 .S1413-3555(20)31118-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bernardy K, Klose P, Welsch P, Häuser W. Efficacy, acceptability and safety of Internet-delivered psychological therapies for fibromyalgia syndrome: a systematic review and meta-analysis of randomized controlled trials. Eur J Pain. 2019 Jan 06;23(1):3–14. doi: 10.1002/ejp.1284. https://pubmed.ncbi.nlm.nih.gov/29984490/ [DOI] [PubMed] [Google Scholar]
- 23.Higgins JPT, Altman DG, Gøtzsche Peter C, Jüni Peter, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JAC, Cochrane Bias Methods Group. Cochrane Statistical Methods Group The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011 Oct 18;343:d5928. doi: 10.1136/bmj.d5928. https://boris.unibe.ch/id/eprint/7356 .bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003 Sep 06;327(7414):557–60. doi: 10.1136/bmj.327.7414.557. https://europepmc.org/abstract/MED/12958120 .327/7414/557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Irwig L, Macaskill P, Berry G, Glasziou P. Bias in meta-analysis detected by a simple, graphical test. graphical test is itself biased. BMJ. 1998 Feb 07;316(7129):470; author reply 470–1. https://europepmc.org/abstract/MED/9492687 . [PMC free article] [PubMed] [Google Scholar]
- 26.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997 Sep 13;315(7109):629–34. doi: 10.1136/bmj.315.7109.629. https://europepmc.org/abstract/MED/9310563 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ang DC, Chakr R, Mazzuca S, France CR, Steiner J, Stump T. Cognitive-behavioral therapy attenuates nociceptive responding in patients with fibromyalgia: a pilot study. Arthritis Care Res (Hoboken) 2010 May 29;62(5):618–23. doi: 10.1002/acr.20119. https://onlinelibrary.wiley.com/doi/10.1002/acr.20119 . [DOI] [PubMed] [Google Scholar]
- 28.Williams David A, Kuper David, Segar Michelle, Mohan Niveditha, Sheth Manish, Clauw Daniel J. Internet-enhanced management of fibromyalgia: a randomized controlled trial. Pain. 2010 Dec;151(3):694–702. doi: 10.1016/j.pain.2010.08.034. https://europepmc.org/abstract/MED/20855168 .00006396-201012000-00022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Menga G, Ing S, Khan O, Dupre B, Dornelles AC, Alarakhia A, Davis W, Zakem J, Webb-Detiege T, Scopelitis E, Quinet R. Fibromyalgia: can online cognitive behavioral therapy help? Ochsner J. 2014;14(3):343–9. https://europepmc.org/abstract/MED/25249800 . [PMC free article] [PubMed] [Google Scholar]
- 30.Vallejo Miguel A, Ortega José, Rivera Javier, Comeche María I, Vallejo-Slocker Laura. Internet versus face-to-face group cognitive-behavioral therapy for fibromyalgia: a randomized control trial. J Psychiatr Res. 2015 Sep;68(6):106–13. doi: 10.1016/j.jpsychires.2015.06.006. https://europepmc.org/abstract/MED/25587207 .S0022-3956(15)00177-6 [DOI] [PubMed] [Google Scholar]
- 31.Friesen LN, Hadjistavropoulos HD, Schneider LH, Alberts NM, Titov N, Dear BF. Examination of an internet-delivered cognitive behavioural pain management course for adults with fibromyalgia: a randomized controlled trial. Pain. 2017 Apr 15;158(4):593–604. doi: 10.1097/j.pain.0000000000000802.00006396-201704000-00007 [DOI] [PubMed] [Google Scholar]
- 32.Hedman-Lagerlöf Maria, Hedman-Lagerlöf Erik, Axelsson Erland, Ljótsson Brjánn, Engelbrektsson Johanna, Hultkrantz Sofia, Lundbäck Karolina, Björkander Daniel, Wicksell Rikard K, Flink Ida, Andersson Erik. Internet-delivered exposure therapy for fibromyalgia: a randomized controlled trial. Clin J Pain. 2018 Jun;34(6):532–542. doi: 10.1097/AJP.0000000000000566. [DOI] [PubMed] [Google Scholar]
- 33.Simister Heather D, Tkachuk Gregg A, Shay Barbara L, Vincent Norah, Pear Joseph J, Skrabek Ryan Q. Randomized controlled trial of online acceptance and commitment therapy for fibromyalgia. J Pain. 2018 Jul;19(7):741–753. doi: 10.1016/j.jpain.2018.02.004. https://europepmc.org/abstract/MED/25587207 .S1526-5900(18)30084-1 [DOI] [PubMed] [Google Scholar]
- 34.García-Perea Eva, Pedraz-Marcos Azucena, Martínez-Rodríguez Sandra Helena, Otones-Reyes Pedro, Palmar-Santos Ana Maria. Effectiveness of a fibromyalgia online nursing consultation in the quality of life: a randomized controlled trial. Pain Manag Nurs. 2022 Aug;23(4):478–485. doi: 10.1016/j.pmn.2021.09.001. https://linkinghub.elsevier.com/retrieve/pii/S1524-9042(21)00210-1 .S1524-9042(21)00210-1 [DOI] [PubMed] [Google Scholar]
- 35.Serrat M, Coll-Omaña Mireia, Albajes K, Solé Sílvia, Almirall M, Luciano JV, Feliu-Soler A. Efficacy of the FIBROWALK multicomponent program moved to a virtual setting for patients with fibromyalgia during the COVID-19 pandemic: a proof-of-concept RCT performed alongside the state of alarm in Spain. Int J Environ Res Public Health. 2021 Sep 30;18(19):10300. doi: 10.3390/ijerph181910300. https://www.mdpi.com/resolver?pii=ijerph181910300 .ijerph181910300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Serrat M, Albajes K, Navarrete J, Almirall M, Lluch Girbés Enrique, Neblett R, Luciano JV, Moix J, Feliu-Soler A. Effectiveness of two video-based multicomponent treatments for fibromyalgia: The added value of cognitive restructuring and mindfulness in a three-arm randomised controlled trial. Behav Res Ther. 2022 Nov;158:104188. doi: 10.1016/j.brat.2022.104188. https://linkinghub.elsevier.com/retrieve/pii/S0005-7967(22)00159-0 .S0005-7967(22)00159-0 [DOI] [PubMed] [Google Scholar]
- 37.MoodGYM. [2023-03-27]. https://moodgym.com.au/
- 38.Chen T, Or CK, Chen J. Effects of technology-supported exercise programs on the knee pain, physical function, and quality of life of individuals with knee osteoarthritis and/or chronic knee pain: a systematic review and meta-analysis of randomized controlled trials. J Am Med Inform Assoc. 2021 Feb 15;28(2):414–423. doi: 10.1093/jamia/ocaa282. https://europepmc.org/abstract/MED/33236109 .6000401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chen M, Wu T, Lv M, Chen C, Fang Z, Zeng Z, Qian J, Jiang S, Chen W, Zhang J. Efficacy of mobile health in patients with low back pain: systematic review and meta-analysis of randomized controlled trials. JMIR mHealth uHealth. 2021 Jun 11;9(6):e26095. doi: 10.2196/26095. https://mhealth.jmir.org/2021/6/e26095/ v9i6e26095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tsang MP, Man GCW, Xin H, Chong YC, Ong MT, Yung PS. The effectiveness of telerehabilitation in patients after total knee replacement: A systematic review and meta-analysis of randomized controlled trials. J Telemed Telecare. 2022 May 12;:1357633X221097469. doi: 10.1177/1357633X221097469. [DOI] [PubMed] [Google Scholar]
- 41.Rennie K, Taylor C, Corriero AC, Chong C, Sewell E, Hadley J, Ardani S. The current accuracy, cost-effectiveness, and uses of musculoskeletal telehealth and telerehabilitation services. Curr Sports Med Rep. 2022 Jul 01;21(7):247–260. doi: 10.1249/JSR.0000000000000974.00149619-202207000-00007 [DOI] [PubMed] [Google Scholar]
- 42.Winters JM. Telerehabilitation research: emerging opportunities. Annu Rev Biomed Eng. 2002 Aug;4:287–320. doi: 10.1146/annurev.bioeng.4.112801.121923.112801.121923 [DOI] [PubMed] [Google Scholar]
- 43.Aragaki D, Luo J, Weiner E, Zhang G, Darvish B. Cardiopulmonary telerehabilitation. Phys Med Rehabil Clin N Am. 2021 May;32(2):263–276. doi: 10.1016/j.pmr.2021.01.004.S1047-9651(21)00004-8 [DOI] [PubMed] [Google Scholar]
- 44.Häuser Winfried, Ablin J, Perrot S, Fitzcharles M. Management of fibromyalgia: practical guides from recent evidence-based guidelines. Pol Arch Intern Med. 2017 Jan 04;127(1):47–56. doi: 10.20452/pamw.3877. https://pamw.pl/en/issue/article/28075425 . [DOI] [PubMed] [Google Scholar]
- 45.Redfern J. Can older adults benefit from smart devices, wearables, and other digital health options to enhance cardiac rehabilitation? Clin Geriatr Med. 2019 Nov;35(4):489–497. doi: 10.1016/j.cger.2019.07.004.S0749-0690(19)30052-7 [DOI] [PubMed] [Google Scholar]
- 46.Howard IM, Kaufman MS. Telehealth applications for outpatients with neuromuscular or musculoskeletal disorders. Muscle Nerve. 2018 Oct 17;58(4):475–485. doi: 10.1002/mus.26115. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Search strategy.
Funnel plots.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) checklist.


