Abstract
Background
Front-of-neck access (FONA) is an emergency procedure used as a last resort to achieve a patent airway in the prehospital environment. In this systematic review with meta-analysis, we aimed to evaluate the number and success rate of FONA procedures in the prehospital setting, including changes since 2017, when a surgical technique was outlined as the first-line prehospital method.
Methods
A systematic literature search (PROSPERO CRD42022348975) was performed from inception of databases to July 2022 to identify studies in patients of any age undergoing prehospital FONA, followed by data extraction. Meta-analysis was used to derive pooled success rates. Methodological quality of included studies was interpreted using the Cochrane risk of bias tool, and rated using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach.
Results
From 909 studies, 69 studies were included (33 low quality; 36 very low quality) with 3292 prehospital FONA attempts described (1229 available for analysis). The crude median success rate increased from 99.2% before 2017 to 100.0% after 2017. Meta-analysis revealed a pooled overall FONA success rate of 88.0% (95% confidence interval [CI], 85.0–91.0%). Surgical techniques had the highest success rate at a median of 100.0% (pooled rate=92.0%; 95% CI, 88.0–95.0%) vs 50.0% for needle techniques (pooled rate=52.0%; 95% CI, 28.0–76.0%).
Conclusions
Despite being a relatively rare procedure in the prehospital setting, the success rate for FONA is high. A surgical technique for FONA appears more successful than needle techniques, and supports existing UK prehospital guidelines.
Systematic review protocol
PROSPERO CRD42022348975.
Keywords: FONA, needle technique, prehospital, surgical technique, difficult airway
Editor's key points.
-
•
Since 2017, a surgical front-of-neck technique has been promoted as the recommended method for prehospital emergency airway access, but it is unclear whether this has improved success rates.
-
•
This systematic review shows a median success rate of 100.0% after 2017, with a pooled success rate of 88.0%.
-
•
Clinicians should be aware that despite it being a rare procedure in the prehospital setting, the surgical technique has a high success rate in adults. More research in paediatric patients is required.
In the prehospital setting, patients present with airway compromise for a variety of reasons, including cardiac arrest and traumatic injury. Prehospital teams and emergency services throughout the world are equipped to perform airway interventions, ranging from essential measures such as bag-valve-mask ventilation, to intubation, including prehospital emergency anaesthesia (PHEA).1,2 Front-of-neck access (FONA) is a technique used to achieve a patent airway in an emergency.2 It can be used as either a primary airway intervention (e.g. if a patient is trapped) or as a rescue technique in a failed intubation by rescue personnel who have been appropriately trained.2
There are a selection of techniques available for FONA.3 In the UK, the Difficult Airway Society (DAS) recommends a horizontal scalpel incision, followed by a bougie and then a size 6.0 tracheal tube using a twisting motion for adults in a ‘can't intubate, can't oxygenate’ (CICO) rescue scenario.4 The UK prehospital guidelines published in 2017 reflect the DAS guidance, recommending the same approach for all patients older than 8 yrs.4,5 However, other techniques are available, including needle cricothyroidotomy or formal tracheostomy procedures, often using the Seldinger technique.3 Two previous systematic reviews have looked at FONA in a prehospital setting.2,3 Hubble and colleagues2 included four needle cricothyroidotomy studies and eighteen surgical technique studies and showed a pooled success rate of 65.8% for the needle technique and 90.5% for the surgical technique.2 Langvad and colleagues3 also reviewed prehospital and in-hospital success rates using a variety of airway techniques. Success rates varied, with no technique shown to be superior. Studies were noted to be small, heterogenous, and often performed in laboratory or simulated conditions.3 The authors stated that, although no difference in success rate was found, a surgical technique did appear to be quicker than a Seldinger technique.3 These reviews predate more recent prehospital guidance and contemporaneous publications relating to success rates of FONA in this setting. Hence, there is limited up-to-date understanding of the success rates of FONA and how these have changed over time.5 It is also unclear if different prehospital team configurations and population groups influence the success rate of FONA.
The aim of this systematic review was to establish an estimate of the number of FONA attempts and success rate in patients requiring this airway intervention in the prehospital setting, incorporating both military, civilian, paediatric and adult data. In addition, comparisons were made between techniques, population groups, and prehospital team configurations to help guide future training and research.
Methods
We performed a systematic review of the literature reporting use of FONA for prehospital emergency airway management. Our primary outcome was the success rate of FONA attempts. Secondary outcomes were the success rates of individual FONA techniques, the success rate following the updated guidelines of 2017, the success rate for both adult and paediatric respectively, and the success rate of different prehospital providers.5 This systematic review was carried out in accordance with the Preferred Reporting Items for Meta-Analyses (PRISMA) guidelines and was prospectively entered onto the PROSPERO register (CRD42022348975).6,7
Electronic database searching was carried out in line with PRISMA guidelines. PubMed, Web of Science, Cochrane, OVID, Medline, and Embase were searched independently by two reviewers (PA and SM) using Medical Subject Headings (MESH) terms combined with the Boolean operator ‘AND’ (Table 1). The search dates start from the inception of each database to the date each search was performed (all on July 26, 2022). Non-English language papers, abstracts, and other non-published data were excluded; abstracts and non-published data were excluded to ensure the included literature had been peer-reviewed.
Table 1.
Electronic database search terms combined with Boolean operator ‘AND’. FONA, front-of-neck access.
| Terms for prehospital |
| Prehospital OR ‘pre-hospital’ OR ‘non hospital’ OR ‘non-hospital’ OR ‘out of hospital’ |
| Terms for FONA |
| ‘Surgical airway’ OR cricothyroidotomy OR cricotomy OR cricotracheotomy OR ‘FONA’ OR tracheotomy OR tracheostomy OR intercricothyrotomy OR ‘front of neck access’ |
| Terms for emergency |
| Emergency OR emergencies |
Titles and abstracts were uploaded to EndNote 20 (Clarivate Analytics, Boston, MA, USA), duplicates were removed, and relevant titles were selected by two independent reviewers (PA and SM). Where indicated, full-text papers were reviewed for inclusion or exclusion based on predefined criteria (Table 2). Reference lists were screened for relevant titles for completeness.
Table 2.
Inclusion and exclusion criteria. FONA, front-of-neck access.
| Inclusion criteria | Exclusion criteria | |
|---|---|---|
| Study design | Randomised controlled trials comparing the success rate of front of neck access (surgical airway) with control/alternative techniques. Prospective or retrospective observational cohort studies, case series, or case reports. | Unpublished material (PhD/MSc thesis), letters to the editor, reviews and conference abstracts. |
| Participants | Human subjects of any age undergoing prehospital emergency airway management with a tracheal tube through front of neck access (surgical airway/cricothyroidotomy). | Animal or cadaveric studies |
| Outcome | Reported FONA success rates | |
| Language | English language papers | Non-English language papers |
For studies deemed relevant by abstract, the full-text report was retrieved and examined further for compliance with the inclusion criteria. There were no relevant unpublished materials or conference abstracts excluded because they lacked a full report. There were no disagreements between the two independent reviewers about the inclusion of studies.
Records of each database search were kept, the date, total number of hits, number of duplicates removed, number excluded based on title, number excluded based on abstract and full text for each reviewer. All titles were stored on EndNote 20. The two reviewers (PA and SM) extracted data independently into Excel (Microsoft Corporation, Redmond, WA, USA). Extracted information included: authors, year, title, country, study design, study setting, time period, number of participants, study population, primary outcome measure, secondary outcome measures, inclusion and exclusion criteria, details of surgical technique used and indication for FONA (if reported), and study conclusions. Information collected for risk of bias assessment for individual study methodology and reporting included: participant selection, participant and allocation concealment, handling of incomplete outcome data, and outcome reporting.
After data extraction, results were compiled, and medians were calculated using Excel (Microsoft Corp., Redmond, WA, USA) for the various population groups (data are not normally distributed). Success rates were presented as median (range) to allow comparison with other studies.8 Meta-analysis was used to derive pooled success rates calculated assuming a random effects model using the inverse-variance method, with 95% confidence intervals (95% CIs) calculated using the Wilson method. Results of meta-analysis are presented as forest plots. Heterogeneity was established using I2 statistics. Analysis was performed using R4.2.1 (The R Foundation for Statistical Computing, Vienna, Austria) using the ‘meta’ package.9 Planned subgroup analysis included: (1) pre- and post-2017 data; (2) paediatric-only data, (3) FONA technique, and (4) type of prehospital team performing FONA.
The Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach was used to rate the reliability of evidence from each included study.10 As part of this, limitations of included study designs and execution were assessed using the Cochrane risk of bias tool.11 Quality appraisal was carried out by both reviewers (PA and SM) independently. There were no disagreements between the reviewers regarding the risk of bias and GRADE rating.
Results
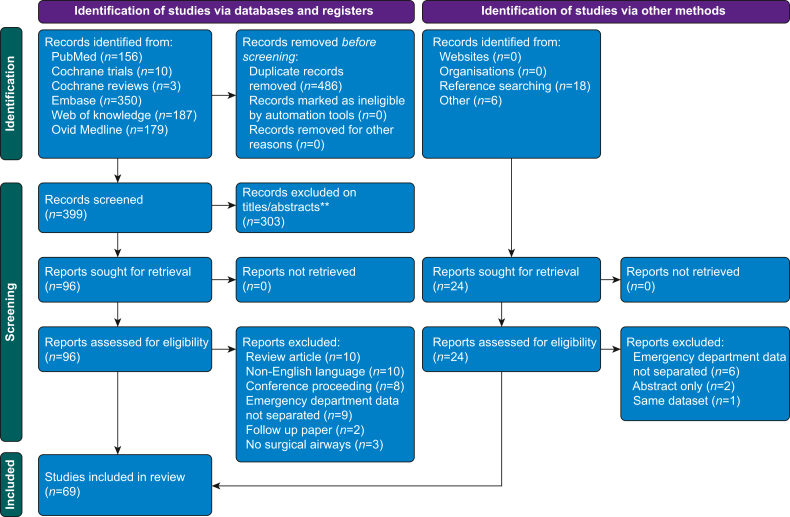
A total of 909 studies were identified. After duplicates were removed 423 studies were screened, with a total of 69 studies included (Fig 1). In total, 3292 prehospital FONA attempts are described (n = 1229 available for analysis). Success rates ranged from 0.0% to 100.0%, with a median of 100.0%. Supplementary Table S1 details the findings of each included study; the quality of evidence findings are available in Supplementary Table S2.12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52,56, 57, 58, 59, 60,62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74, 75, 76, 77, 78, 79, 80, 81, 82, 83, 84 Thirty-three studies were low quality and 36 were very low quality.
Fig 1.
PRISMA diagram summarising results of the systematic literature review. PRISMA, Preferred Reporting Items for Meta-Analyses.
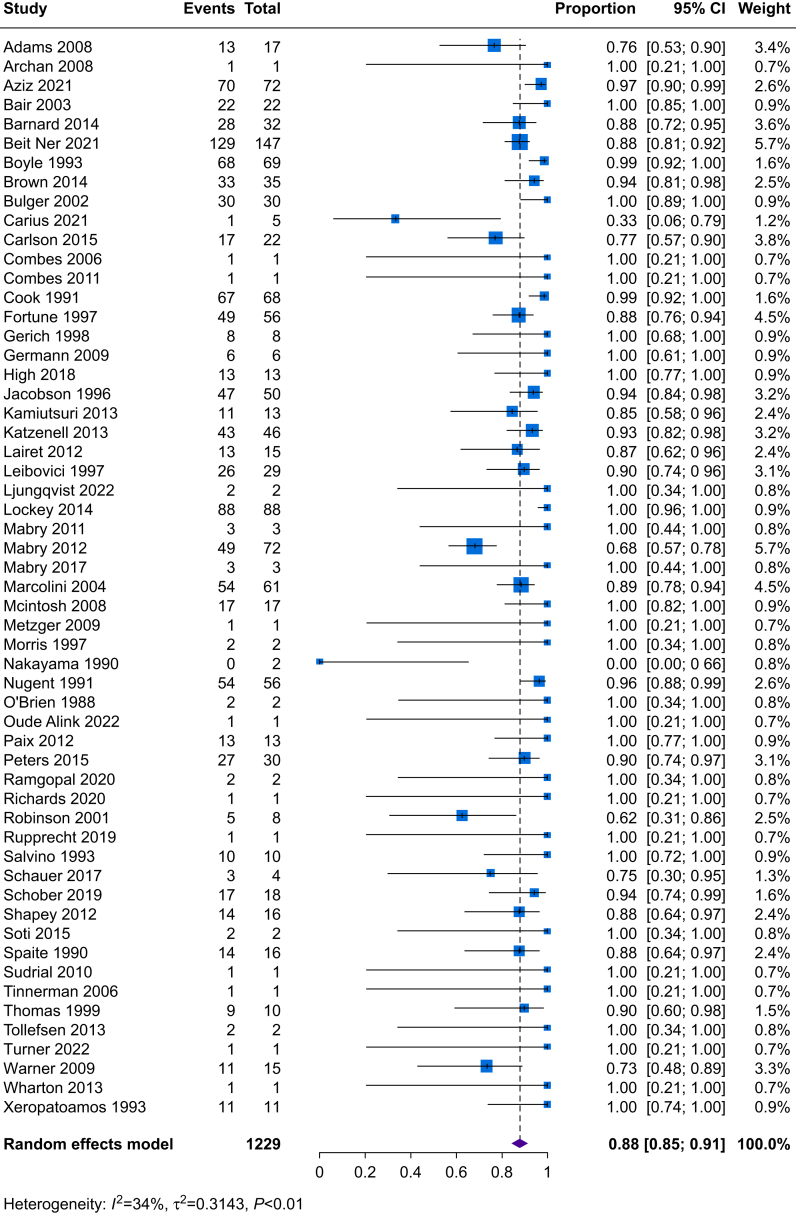
The crude median FONA success for data before 2017 (46 studies, 981 FONA attempts) was 99.2% (range, 0.0–100.0%). From 2017 onwards (10 studies, 248 FONA attempts), the median FONA success rate was 100.0% (range, 33.3–100.0%). Including all studies in a meta-analysis revealed a pooled success rate for FONA of 88.0% (95% CI, 85.0–91.0%; 1119 out of 1229 patients) (Fig 2). Pooled success rates for pre-2017 and post-2017 data remained relatively consistent at 88.0% (95% CI, 84.0–91.0%; 881 out of 968 patients) and 88.0% (95% CI, 77.0–94.0%; 238 out of 261 patients), respectively (Supplementary Fig. S1).
Fig 2.
Success rates for all studies. 95% CI, 95% confidence interval.
Table 3 shows the success rates for surgical vs needle vs tracheostomy kits (when success rates could be separated out into technique and when information on the technique used was available). The needle technique had the lowest median success rate at 50.0% (range, 0.0–100.0%) but only included 19 attempts. For tracheostomy kits, data from 219 patients were included with a median success rate of 93.0% (0.0–100.0%). Surgical FONA technique (n = 603) had the highest median success rate of 100.0% (range, 62.5–100.0%). Pooled success rates were: needle, 52.0% (95% CI, 28.0–76.0%); tracheostomy kit, 87.0% (95% CI, 82.0–91.0%); surgical technique, 92.0% (95% CI, 88.0–95.0%) (see Supplementary Fig. S2).
Table 3.
Success rates of various techniques used for FONA. FONA, front-of-neck access.
| Study | Number of patients | Success rate documented in manuscript (%) |
|---|---|---|
| Needle technique | ||
| Bulger and colleagues12 | 8 | 75.0 |
| Nakayama and colleagues13 | 2 | 0.0 |
| Shapey and colleagues14 | 4 | 50.0 |
| Tollefsen and colleagues15 | 1 | 100.0 |
| Warner and colleagues16 | 4 | 25.0 |
| Surgical technique | ||
| Adams and colleagues17 | 17 | 76.5 |
| Archan and colleagues18 | 1 | 100.0 |
| Aziz and colleagues19 | 72 | 97.2 |
| Bair and colleagues20 | 22 | 100.0 |
| Boyle and colleagues21 | 69 | 98.6 |
| Bulger and colleagues12 | 22 | 100.0 |
| Cook and colleagues22 | 68 | 98.5 |
| Germann and colleagues23 | 4 | 100.0 |
| High and colleagues24 | 7 | 100.0 |
| Jacobson and colleagues25 | 50 | 94.0 |
| Lairet and colleagues26 | 15 | 86.7 |
| Leibovici and colleagues27 | 16 | 93.8 |
| Ljungqvist and colleagues28 | 2 | 100.0 |
| Lockey and colleagues29 | 88 | 100.0 |
| Mabry and colleagues30 | 3 | 100.0 |
| Mabry and colleagues31 | 3 | 100.0 |
| Metzger and colleagues32 | 1 | 100.0 |
| Morris and colleagues33 | 2 | 100.0 |
| Nugent and colleagues34 | 56 | 96.4 |
| Paix and colleagues35 | 14 | 100.0 |
| Ramgopal and colleagues36 | 2 | 100.0 |
| Richards and colleagues37 | 1 | 100.0 |
| Robinson and colleagues38 | 8 | 62.5 |
| Rupprecht and colleagues39 | 1 | 100.0 |
| Salvino and colleagues40 | 10 | 100.0 |
| Schauer and colleagues41 | 2 | 100.0 |
| Shapey and colleagues14 | 12 | 100.0 |
| Soti and colleagues42 | 2 | 100.0 |
| Thomas and colleagues43 | 10 | 90.0 |
| Tollefsen and colleagues15 | 1 | 100.0 |
| Warner and colleagues16 | 11 | 91.0 |
| Wharton and Bennett44 | 1 | 100.0 |
| Xeropotamos and colleagues45 | 11 | 100.0 |
| Tracheostomy kit (including those using Seldinger technique) | ||
| Beit Ner and colleagues46 | 147 | 88.0 |
| Combes and colleagues47 | 1 | 100.0 |
| Germann and colleagues23 | 2 | 100.0 |
| High and colleagues24 | 6 | 83.3 |
| Katzenell and colleagues48 | 46 | 93.5 |
| Leibovici and colleagues27 | 13 | 84.6 |
| Schauer and colleagues41 | 2 | 0.0 |
| Sudrial and colleagues49 | 1 | 100.0 |
| Timmerman and colleagues50 | 1 | 100.0 |
In the five paediatric-only studies (29 patients undergoing FONA), the median FONA success rate was 100.0% (range, 0.0–100.0%) with a pooled success rate of 74.0% (95% CI, 56.0–87.0%; 22 out of 29 patients) (Supplementary Fig. S3a). One study detailed two attempts at needle FONA resulting in failure and complications including barotrauma.13 Another showed success with both the needle (patient aged 2) and surgical technique (patient aged 14).15 The study with the most paediatric patients (n = 22) did not detail further the FONA technique(s) used.51
In the 14 military-only studies (n = 192), median FONA success rate was 81.5% (range, 33.3–100.0%) with a pooled success rate of 81.0% (95% CI, 69.0–89.0%) (Supplementary Fig. S3b). The median success rate for emergency medical services team (n=85) was 93.8% with a pooled success rate of 81% (95% CI, 690–89.0%). The median success rate for a flight nurse led team (n=263) was 99.3% with a pooled success rate of 94.0% (95% CI, 86.0–98.0%). The median success rate of a paramedic led team (n=223) was 94.3% with a pooled success rate of 90.0% (95% CI, 86.0–94.0%). The median success rate of a physician led team (n=302) was 100.0% with a pooled success rate of 89.0% (95% CI, 83.0–93.0%) (Supplementary Table S3 and Supplementary Fig. S4).
Discussion
Overall, the success rate for FONA in the prehospital setting is high, with a crude median of 100.0% and a pooled success rate of 88.0%. This suggests that the procedure is safe, especially given that this represents the last-ditch attempt at securing an airway.
Since the introduction of the 2017 prehospital anaesthesia guidelines recommending a surgical technique for FONA, a small improvement of 0.8% has been seen in the median success rate.5 This is in keeping with the finding that a surgical FONA technique has the highest crude median success rate of 100.0%, although the pooled subgroup analysis results for pre- and post-2017 studies reveal a similar success rate of 88%. The study by Beit Ner and colleagues46 is likely to have had an impact on this lack of improvement, which used tracheostomies rather than the recommended surgical technique for FONA and also included military data.5
In terms of FONA technique, needle cricothyrotomy, although performed in a relatively small number of patients (n=19) compared with the surgical technique (n = 603), had a crude median success rate of half that of the surgical technique (50.0% vs 100.0%), which was echoed by the pooled success rates (52% for needle vs 92% for surgical). These findings are consistent with previous systematic reviews by Hubble and colleagues2 and Langvad and colleagues.3 Owing to the scarcity of patients having needle cricothyrotomy, it is difficult to draw any firm conclusions about which technique is best, although it would seem that surgical approaches are more preferred in real-world scenarios and are in keeping with the latest guidance.4,5
It is important to note that ‘success rate’ may be defined differently depending on the study. ‘Success’ is assumed to mean cannulation of the trachea via the front of the neck, but whether this results in successful ventilation and prevention of hypoxia is not always clear. In addition, if hypoxia has already occurred before the FONA attempt with corresponding poor long-term patient outcomes, it remains difficult to define the FONA as ‘successful’. Barnard and colleagues52 reported 28 out of 32 FONA attempts were successful, but also commented on significant complications amongst six patients (e.g. left main stem intubation). The significance of left main stem intubation, for example is unclear as, if recognised early, the harm to the patient is likely to be minimal. However, in the study by Bair and colleagues,20 although all FONA attempts were ultimately deemed successful, FONA attempts in nine out of 22 patients took more than 2 min to be performed. This time could have potentially resulted in a prolonged period of hypoxia, depending on attempts at oxygenation before FONA. Because of these discrepancies, future studies investigating FONA should carefully define ‘success’ and give more emphasis on long-term patient outcomes.
Overall, paediatric FONA had a median crude success rate of 100%, although this ranged from 0% to 100% with a pooled success rate of 74%. At present, DAS recommends percutaneous cannula cricothyroidotomy in situations of cannot intubate and cannot ventilate in children aged 1–8 yr.53 However, this approach is not risk-free. In an observational study amongst paediatric trauma patients by Nakayama and colleagues,13 of only two on-scene needle cricothyroidotomies performed because of the inability to place a tracheal tube, both were unsuccessful and led to massive subcutaneous emphysema, although both these children were older than 8 yr (age 12 and 15 yr, respectively). There was one successful attempt of a needle cricothyroidotomy described in a 2-yr-old child by Tollefsen and colleagues.15 The paediatric study with the most patients (n = 22) did not detail further the technique(s) used.51 Taken together with the overall lack of paediatric data, it is difficult to draw any conclusions about the most appropriate technique in the paediatric age groups. Difficulties with the needle technique have been shown in hospital. Cook and colleagues54 reported that 12 out of 19 narrow-bore cannula attempts failed and three out of seven wide-bore cannula attempts failed. In contrast, the three first choice surgical FONA attempts were successful.54 Given that data appear to support surgical technique being superior to needle-based approaches amongst adult patients, it may be that the same should be advocated amongst paediatric patients, although further research in this area is warranted to determine comparative success rates for each technique in the paediatric population.
High success rates were seen for both physician-led prehospital teams (highest crude median success rate at 100.0%) and flight nurse teams (highest pooled success rates at 94%). In contrast, military teams had the lowest crude median success rate at 76.5% (pooled success rate of 81%). The higher success rates seen amongst physician-led teams follow that of prehospital tracheal intubation.8 The lower FONA success rates observed in military teams may be attributable to team configuration (e.g. combat medic), type of injury pattern encountered in military patients (e.g. blast injuries), the need for FONA as the primary approach (which may increase the complexity of the procedure), and the environment which FONA is performed in. In contrast, physician-led teams are more likely to use FONA as a rescue technique for failed intubation attempts, rather than using it as the initial method for securing the airway; over the past 20 yr in London, only 17 out of 72 FONA performed were immediate primary airway interventions.19
This review incorporates several diverse population groups, including the military setting, which results in heterogeneity with an I2 of 34% (moderate heterogeneity).55 Particularly in the military studies, the training behind the medical team performing FONA is not always clear as they are referred to as ‘combat medics’ or ‘military medics’.26,30,52,56, 57, 58, 59, 60 There are also differences worldwide in the setup of prehospital teams and the standard FONA technique used; the 2017 guidelines were based on the UK DAS guidelines and may therefore not have been utilised outside of the UK.5,61 There is also difficulty in extracting success rates before and after 2017 in datasets that overlap this time period with different techniques still being used despite the update in guidance.46,62
Several of the studies included either did not report success rates or rates could not be reliably calculated (e.g. complication rates could not be separated from failure rates).56,58,60,63, 64, 65, 66, 67, 68, 69, 70, 71, 72 If these studies reported FONA success rates, it may have altered the findings of this systematic review, particularly within certain population groups. As an example, Diggs and colleagues63 would potentially add more than 1000 patients to the Emergency Medical Services group. Also, by choosing to include case reports, we are likely to have some systemic and publication bias to those that have a positive outcome and successful FONA; the small numbers of these case reports are unlikely to significantly impact on the results seen and instead give us some insight into unusual prehospital situations, such as FONA after failed intubation in a patient who developed facial and oropharyngeal oedema secondary to envenomation after a snakebite.37
It should also be noted that the studies are of low or very low quality. In time-critical settings, prehospital settings, or both, there are substantial practical and ethical difficulties in performing randomised controlled trials, which compare different FONA techniques. Therefore, data derived from observational studies are likely to be the best available evidence. Indeed, many of the studies incorporate very large data sets, particularly in the military setting, and review prolonged periods to help guide our understanding.
Overall, despite being a relatively rare procedure in the prehospital setting, the success rate for FONA is high. Surgical techniques for FONA appear to be more successful than needle techniques, and this supports the existing UK guidelines advocating the use of surgical FONA in the prehospital setting. More research is required in the paediatric population to determine the most successful FONA technique. We encourage other countries to review their guidelines and would support the development of an international database to which data relating to any FONA access attempt can contribute to further research of this rare event.
Authors’ contributions
Development of the study: SM, PA, MOM
Performed the systematic literature review: SM and PA
Performed the statistical analysis: JK
All authors were involved in the development, drafting, and final approval of the article.
Declaration of interest
No competing interests declared.
Handling editor: Jonathan Hardman
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.bja.2023.01.022.
Appendix A. Supplementary data
The following is the Supplementary data to this article.
References
- 1.Hubble M.W., Brown L., Wilfong D.A., Hertelendy A., Benner R.W., Richards M.E. A meta-analysis of prehospital airway control techniques: Part I. Orotracheal and nasotracheal intubation success rates. Prehosp Emerg Care. 2010;14:377–401. doi: 10.3109/10903121003790173. [DOI] [PubMed] [Google Scholar]
- 2.Hubble M.W., Wilfong D.A., Brown L.H., Hertelendy A., Benner R.W. A meta-analysis of prehospital airway control techniques: Part II. Alternative airway devices and cricothyrotomy success rates. Prehosp Emerg Care. 2010;14:515–530. doi: 10.3109/10903127.2010.497903. [DOI] [PubMed] [Google Scholar]
- 3.Langvad S., Hyldmo P.K., Nakstad A.R., Vist G.E., Sandberg M. Emergency cricothyrotomy—a systematic review. Scand J Trauma Resusc Emerg Med. 2013;21:43. doi: 10.1186/1757-7241-21-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Frerk C., Mitchell V.S., McNarry A.F., et al. Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth. 2015;115:827–848. doi: 10.1093/bja/aev371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lockey D.J., Crewdson K., Davies G., et al. AAGBI: safer pre-hospital anaesthesia 2017: association of anaesthetists of great britain and Ireland. Anaesthesia. 2017;72:379–390. doi: 10.1111/anae.13779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Page M.J., McKenzie J.E., Bossuyt P.M., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.University of York . 2022. PROSPERO: International Prospective Register of Systematic Reviews.www.crd.york.ac.uk/prospero Available from. [Google Scholar]
- 8.Crewdson K., Lockey D.J., Røislien J., Lossius H.M., Rehn M. The success of pre-hospital tracheal intubation by different pre-hospital providers: a systematic literature review and meta-analysis. Crit Care. 2017;21:31. doi: 10.1186/s13054-017-1603-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.R Development Core Team R . R Foundation for Statistical Computing; Vienna, Austria: 2008. A Language and Environment for Statistical Computing. [Google Scholar]
- 10.Schunemann H., Brozek J., Guyatt G., Oxman A. 2013. GRADE handbook.https://gdt.gradepro.org/app/handbook/handbook.html Available from. [Google Scholar]
- 11.Higgins J., Thomas J. 2019. Cochrane Handbook for Systematic Reviews of Interventions; p. 2022.https://training.cochrane.org/handbook/current Available from. [Google Scholar]
- 12.Bulger E.M., Copass M.K., Maier R.V., Larsen J., Knowles J., Jurkovich G.J. An analysis of advanced prehospital airway management. J Emerg Med. 2002;23:183–189. doi: 10.1016/s0736-4679(02)00490-0. [DOI] [PubMed] [Google Scholar]
- 13.Nakayama D.K., Gardner M.J., Rowe M.I. Emergency endotracheal intubation in pediatric trauma. Ann Surg. 1990;211:218–223. doi: 10.1097/00000658-199002000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shapey I.M., Kumar D.S., Roberts K. Invasive and surgical procedures in pre-hospital care: what is the need? Eur J Trauma Emerg Surg. 2012;38:633–639. doi: 10.1007/s00068-012-0207-9. [DOI] [PubMed] [Google Scholar]
- 15.Tollefsen W.W., Brown C.A., Cox K.L., Walls R.M. Two hundred sixty pediatric emergency airway encounters by air transport personnel: a report of the Air Transport Emergency Airway Management (NEAR VI: “A-TEAM”) project. Pediatr Emerg Care. 2013;29:963–968. doi: 10.1097/PEC.0b013e3182a219ea. [DOI] [PubMed] [Google Scholar]
- 16.Warner K.J., Sharar S.R., Copass M.K., Bulger E.M. Prehospital management of the difficult airway: a prospective cohort study. J Emerg Med. 2009;36:257–265. doi: 10.1016/j.jemermed.2007.10.058. [DOI] [PubMed] [Google Scholar]
- 17.Adams B.D., Cuniowski P.A., Muck A., De Lorenzo R.A. Registry of emergency airways arriving at combat hospitals. J Trauma. 2008;64:1548–1554. doi: 10.1097/TA.0b013e3181728c41. [DOI] [PubMed] [Google Scholar]
- 18.Archan S., Gumpert R., Kugler B., Seibert F.J., Prause G. Cricothyroidotomy on the scene in a patient with severe facial trauma and difficult neck anatomy. Am J Emerg Med. 2009;27:e1–e133. doi: 10.1016/j.ajem.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 19.Aziz S., Foster E., Lockey D.J., Christian M.D. Emergency scalpel cricothyroidotomy use in a prehospital trauma service: a 20-year review. Emerg Med J. 2021;38:349–354. doi: 10.1136/emermed-2020-210305. [DOI] [PubMed] [Google Scholar]
- 20.Bair A.E., Panacek E.A., Wisner D.H., Bales R., Sakles J.C. Cricothyrotomy: a 5-year experience at one institution. J Emerg Med. 2003;24:151–156. doi: 10.1016/s0736-4679(02)00715-1. [DOI] [PubMed] [Google Scholar]
- 21.Boyle M.F., Hatton D., Sheets C. Surgical cricothyrotomy performed by air ambulance flight nurses: a 5-year experience. J Emerg Med. 1993;11:41–45. doi: 10.1016/0736-4679(93)90008-u. [DOI] [PubMed] [Google Scholar]
- 22.Cook S., Dawson R., Falcone R.E. Prehospital cricothyrotomy in air medical transport: outcome. J Air Med Transp. 1991;10(7–9):12. [PubMed] [Google Scholar]
- 23.Germann C.A., Baumann M.R., Kendall K.M., Strout T.D., McGraw K. Performance of endotracheal intubation and rescue techniques by emergency services personnel in an air medical service. Prehosp Emerg Care. 2009;13:44–49. doi: 10.1080/10903120802474505. [DOI] [PubMed] [Google Scholar]
- 24.High K., Brywczynski J., Han J.H. Cricothyrotomy in helicopter emergency medical service transport. Air Med J. 2018;37:51–53. doi: 10.1016/j.amj.2017.10.004. [DOI] [PubMed] [Google Scholar]
- 25.Jacobson L.E., Gomez G.A., Sobieray R.J., Rodman G.H., Solotkin K.C., Misinski M.E. Surgical cricothyroidotomy in trauma patients: analysis of its use by paramedics in the field. J Trauma. 1996;41:15–20. doi: 10.1097/00005373-199607000-00004. [DOI] [PubMed] [Google Scholar]
- 26.Lairet J.R., Bebarta V.S., Burns C.J., et al. Prehospital interventions performed in a combat zone: a prospective multicenter study of 1,003 combat wounded. J Trauma Acute Care Surg. 2012;73:S38–S42. doi: 10.1097/TA.0b013e3182606022. [DOI] [PubMed] [Google Scholar]
- 27.Leibovici D., Fredman B., Gofrit O.N., Shemer J., Blumenfeld A., Shapira S.C. Prehospital cricothyroidotomy by physicians. Am J Emerg Med. 1997;15:91–93. doi: 10.1016/s0735-6757(97)90059-0. [DOI] [PubMed] [Google Scholar]
- 28.Ljungqvist H.E., Nurmi J.O. Reasons behind failed prehospital intubation attempts while combining C-MAC videolaryngoscope and Frova introducer. Acta Anaesthesiol Scand. 2022;66:132–140. doi: 10.1111/aas.13985. [DOI] [PubMed] [Google Scholar]
- 29.Lockey D., Crewdson K., Weaver A., Davies G. Observational study of the success rates of intubation and failed intubation airway rescue techniques in 7256 attempted intubations of trauma patients by pre-hospital physicians. Br J Anaesth. 2014;113:220–225. doi: 10.1093/bja/aeu227. [DOI] [PubMed] [Google Scholar]
- 30.Mabry R.L., Cuniowski P., Frankfurt A., Adams B.D. Advanced airway management in combat casualties by medics at the point of injury: a sub-group analysis of the reach study. J Spec Oper Med. 2011;11:16–19. doi: 10.55460/W35F-54HG. [DOI] [PubMed] [Google Scholar]
- 31.Mabry R.L., Kharod C.U., Bennett B.L. Awake cricothyrotomy: a novel approach to the surgical airway in the tactical setting. Wilderness Environ Med. 2017;28:S61–S68. doi: 10.1016/j.wem.2017.02.003. [DOI] [PubMed] [Google Scholar]
- 32.Metzger J.C., Eastman A.L., Benitez F.L., Pepe P.E. The lifesaving potential of specialized on-scene medical support for urban tactical operations. Prehosp Emerg Care. 2009;13:528–531. doi: 10.1080/10903120903144940. [DOI] [PubMed] [Google Scholar]
- 33.Morris A., Lockey D., Coats T. Fat necks: modification of a standard surgical airway protocol in the pre-hospital environmental. Resuscitation. 1997;35:253–254. doi: 10.1016/s0300-9572(97)00071-3. [DOI] [PubMed] [Google Scholar]
- 34.Nugent W.L., Rhee K.J., Wisner D.H. Can nurses perform surgical cricothyrotomy with acceptable success and complication rates? Ann Emerg Med. 1991;20:367–370. doi: 10.1016/s0196-0644(05)81656-7. [DOI] [PubMed] [Google Scholar]
- 35.Paix B.R., Griggs W.M. Emergency surgical cricothyroidotomy: 24 successful cases leading to a simple ‘scalpel-finger-tube’ method. Emerg Med Australas. 2012;24:23–30. doi: 10.1111/j.1742-6723.2011.01510.x. [DOI] [PubMed] [Google Scholar]
- 36.Ramgopal S., Button S.E., Owusu-Ansah S., et al. Success of pediatric intubations performed by a critical care transport service. Prehosp Emerg Care. 2020;24:683–692. doi: 10.1080/10903127.2019.1699212. [DOI] [PubMed] [Google Scholar]
- 37.Richards J.R., McKinney H.E., Shannon H.M., et al. Angioedema and dual nurse flight crew cricothyrotomy after envenomation by a severed rattlesnake head. Air Med J. 2020;39:417–420. doi: 10.1016/j.amj.2020.06.007. [DOI] [PubMed] [Google Scholar]
- 38.Robinson K.J., Katz R., Jacobs L.M. A 12-year experience with prehospital cricothyrotomies. Air Med J. 2001;20:27–30. [PubMed] [Google Scholar]
- 39.Rupprecht H., Gaab K. Prehospital tracheotomy in a case of avulsion of the larynx with a comminuted fracture of the jawbone. Clin Exp Emerg Med. 2019;6:173–176. doi: 10.15441/ceem.18.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Salvino C.K., Dries D., Gamelli R., Murphy-Macabobby M., Marshall W. Emergency cricothyroidotomy in trauma victims. J Trauma. 1993;34:503–505. doi: 10.1097/00005373-199304000-00006. [DOI] [PubMed] [Google Scholar]
- 41.Schauer S.G., April M.D., Cunningham C.W., Long A.N., Carter R. Prehospital cricothyrotomy kits used in combat. J Spec Oper Med. 2017;17:18–20. doi: 10.55460/MTTO-UKNJ. [DOI] [PubMed] [Google Scholar]
- 42.Soti A., Temesvari P., Hetzman L., Eross A., Petroczy A. Implementing new advanced airway management standards in the Hungarian physician staffed Helicopter Emergency Medical Service. Scand J Trauma Resusc Emerg Med. 2015;23:3. doi: 10.1186/s13049-014-0081-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Thomas S.H., Harrison T., Wedel S.K. Flight crew airway management in four settings: a six-year review. Prehosp Emerg Care. 1999;3:310–315. doi: 10.1080/10903129908958960. [DOI] [PubMed] [Google Scholar]
- 44.Wharton D.R., Bennett B.L. Surgical cricothyrotomy in the wilderness: a case report. Wilderness Environ Med. 2013;24:12–14. doi: 10.1016/j.wem.2012.06.007. [DOI] [PubMed] [Google Scholar]
- 45.Xeropotamos N.S., Coats T.J., Wilson A.W. Prehospital surgical airway management: 1 year’s experience from the Helicopter Emergency Medical Service. Injury. 1993;24:222–224. doi: 10.1016/0020-1383(93)90172-3. [DOI] [PubMed] [Google Scholar]
- 46.Beit Ner E., Tsur A.M., Nadler R., Glassberg E., Benov A., Chen J. High success rate of prehospital and en route cricothyroidotomy performed in the Israel Defense Forces: 20 years of experience. Prehosp Disaster Med. 2021;36:713–718. doi: 10.1017/S1049023X21001199. [DOI] [PubMed] [Google Scholar]
- 47.Combes X., Jabre P., Margenet A., et al. Unanticipated difficult airway management in the prehospital emergency setting: prospective validation of an algorithm. Anesthesiology. 2011;114:105–110. doi: 10.1097/ALN.0b013e318201c42e. [DOI] [PubMed] [Google Scholar]
- 48.Katzenell U., Lipsky A.M., Abramovich A., et al. Prehospital intubation success rates among Israel Defense Forces providers: epidemiologic analysis and effect on doctrine. J Trauma Acute Care Surg. 2013;75:S178–S183. doi: 10.1097/TA.0b013e318299d650. [DOI] [PubMed] [Google Scholar]
- 49.Sudrial J., Birlouez C., Guillerm A.-L., Sebbah J.-L., Amathieu R., Dhonneur G. Difficult airway management algorithm in emergency medicine: do not struggle against the patient, just skip to next step. Emerg Med Int. 2010;2010 doi: 10.1155/2010/826231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Timmermann A., Eich C., Russo S.G., et al. Prehospital airway management: a prospective evaluation of anaesthesia trained emergency physicians. Resuscitation. 2006;70:179–185. doi: 10.1016/j.resuscitation.2006.01.010. [DOI] [PubMed] [Google Scholar]
- 51.Carlson J.N., Gannon E., Clay Mann N., et al. Pediatric out-of-hospital critical procedures in the United States. Pediatr Crit Care Med. 2015;16:e260–e267. doi: 10.1097/PCC.0000000000000505. [DOI] [PubMed] [Google Scholar]
- 52.Barnard E.B., Ervin A.T., Mabry R.L., Bebarta V.S. Prehospital and en route cricothyrotomy performed in the combat setting: a prospective, multicenter, observational study. J Spec Oper Med. 2014;14:35–39. doi: 10.55460/62V1-UIZC. [DOI] [PubMed] [Google Scholar]
- 53.Difficult Airway Society . 2022. Cannot intubate and cannot ventilate (CICV) in a paralysed anaesthetised child aged 1 to 8 years.https://das.uk.com/files/APA3-CICV-FINAL.pdf Available from. [Google Scholar]
- 54.Cook T.M., Woodall N., Frerk C. Major complications of airway management in the UK: results of the fourth national audit project of the royal college of anaesthetists and the difficult airway society: Part 1. Anaesthesia. Br J Anaesth. 2011;106:617–631. doi: 10.1093/bja/aer058. [DOI] [PubMed] [Google Scholar]
- 55.Cochrane . 2015. Identifying and measuring heterogeneity.https://handbook-5-1.cochrane.org/chapter_9/9_5_2_identifying_and_measuring_heterogeneity.htm Available from. [Google Scholar]
- 56.Blackburn M.B., April M.D., Brown D.J., et al. Prehospital airway procedures performed in trauma patients by ground forces in Afghanistan. J Trauma Acute Care Surg. 2018;85:S154–S160. doi: 10.1097/TA.0000000000001866. [DOI] [PubMed] [Google Scholar]
- 57.Carius B.M., Dodge P.M., Hudson I.L., et al. An analysis of prehospital trauma registry: after-action reviews on airway interventions in Afghanistan. Med J (MEDCoE) 2021:32–37. [PubMed] [Google Scholar]
- 58.Hudson I.L., Blackburn M.B., Staudt A.M., Ryan K.L., Mann-Salinas E.A. Analysis of casualties that underwent airway management before reaching role 2 Facilities in the Afghanistan conflict 2008–2014. Mil Med. 2020;185:10–18. doi: 10.1093/milmed/usz383. [DOI] [PubMed] [Google Scholar]
- 59.Mabry R.L., Frankfurt A. An analysis of battlefield cricothyrotomy in Iraq and Afghanistan. J Spec Oper Med. 2012;12:17–23. doi: 10.55460/FYQG-8E49. [DOI] [PubMed] [Google Scholar]
- 60.Schauer S.G., Bellamy M.A., Mabry R.L., Bebarta V.S. A comparison of the incidence of cricothyrotomy in the deployed setting to the emergency department at a level 1 military trauma center: a descriptive analysis. Mil Med. 2015;180:60–63. doi: 10.7205/MILMED-D-14-00384. [DOI] [PubMed] [Google Scholar]
- 61.Price T.M., McCoy E.P. Emergency front of neck access in airway management. BJA Educ. 2019;19:246–253. doi: 10.1016/j.bjae.2019.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Schober P., Biesheuvel T., De Leeuw M.A., Loer S.A., Schwarte L.A. Prehospital cricothyrotomies in a helicopter emergency medical service: analysis of 19,382 dispatches. BMC Emerg Med. 2019;19:12. doi: 10.1186/s12873-019-0230-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Diggs L.A., Yusuf J.-E., De Leo G. An update on out-of-hospital airway management practices in the United States. Resuscitation. 2014;85:885–892. doi: 10.1016/j.resuscitation.2014.02.032. [DOI] [PubMed] [Google Scholar]
- 64.Gellerfors M., Fevang E., Bäckman A., et al. Pre-hospital advanced airway management by anaesthetist and nurse anaesthetist critical care teams: a prospective observational study of 2028 pre-hospital tracheal intubations. Br J Anaesth. 2018;120:1103–1109. doi: 10.1016/j.bja.2017.12.036. [DOI] [PubMed] [Google Scholar]
- 65.Meizoso J.P., Valle E.J., Allen C.J., et al. Decreased mortality after prehospital interventions in severely injured trauma patients. J Trauma Acute Care Surg. 2015;79:227–231. doi: 10.1097/TA.0000000000000748. [DOI] [PubMed] [Google Scholar]
- 66.Peters J., van Wageningen B., Hendriks I., et al. First-pass intubation success rate during rapid sequence induction of prehospital anaesthesia by physicians versus paramedics. Eur J Emerg Med. 2015;22:391–394. doi: 10.1097/MEJ.0000000000000161. [DOI] [PubMed] [Google Scholar]
- 67.Prekker M.E., Kwok H., Shin J., Carlbom D., Grabinsky A., Rea T.D. The process of prehospital airway management: challenges and solutions during paramedic endotracheal intubation. Crit Care Med. 2014;42:1372–1378. doi: 10.1097/CCM.0000000000000213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Pugh H.E., LeClerc S., McLennan J. A review of pre-admission advanced airway management in combat casualties, Helmand Province 2013. J R Army Med Corps. 2015;161:121–126. doi: 10.1136/jramc-2014-000271. [DOI] [PubMed] [Google Scholar]
- 69.Schauer S.G., Fernandez J.R.D., Roper J.L., et al. A randomized cross-over study comparing surgical cricothyrotomy techniques by combat medics using a synthetic cadaver model. Am J Emerg Med. 2018;36:651–656. doi: 10.1016/j.ajem.2017.11.062. [DOI] [PubMed] [Google Scholar]
- 70.Schauer S.G., Naylor J.F., Chow A.L., et al. Survival of casualties undergoing prehospital supraglottic airway placement versus cricothyrotomy. J Spec Oper Med. 2019;19:91–94. doi: 10.55460/D4C5-PVHK. [DOI] [PubMed] [Google Scholar]
- 71.Sunde G.A., Heltne J.-K., Lockey D., et al. Airway management by physician-staffed Helicopter Emergency Medical Services — a prospective, multicentre, observational study of 2,327 patients. Scand J Trauma Resusc Emerg Med. 2015;23:57. doi: 10.1186/s13049-015-0136-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wang H.E., Mann N.C., Mears G., Jacobson K., Yealy D.M. Out-of-hospital airway management in the United States. Resuscitation. 2011;82:378–385. doi: 10.1016/j.resuscitation.2010.12.014. [DOI] [PubMed] [Google Scholar]
- 73.Brown C.A., 3rd, Cox K., Hurwitz S., Walls R.M. 4,871 Emergency airway encounters by air medical providers: a report of the air transport emergency airway management (NEAR VI: “A-TEAM”) project. West J Emerg Med. 2014;15:188–193. doi: 10.5811/westjem.2013.11.18549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Combes X., Jabre P., Jbeili C., et al. Prehospital standardization of medical airway management: incidence and risk factors of difficult airway. Acad Emerg Med. 2006;13:828–834. doi: 10.1197/j.aem.2006.02.016. [DOI] [PubMed] [Google Scholar]
- 75.Fortune J.B., Judkins D.G., Scanzaroli D., McLeod K.B., Johnson S.B. Efficacy of prehospital surgical cricothyrotomy in trauma patients. J Trauma. 1997;42:832–836. doi: 10.1097/00005373-199705000-00013. [DOI] [PubMed] [Google Scholar]
- 76.Gerich T.G., Schmidt U., Hubrich V., Lobenhoffer H.P., Tscherne H. Prehospital airway management in the acutely injured patient: the role of surgical cricothyrotomy revisited. J Trauma. 1998;45:312–314. doi: 10.1097/00005373-199808000-00017. [DOI] [PubMed] [Google Scholar]
- 77.Kamiutsuri K., Okutani R., Kozawa S. Analysis of prehospital endotracheal intubation performed by emergency physicians: retrospective survey of a single emergency medical center in Japan. J Anesth. 2013;27:374–379. doi: 10.1007/s00540-012-1528-x. [DOI] [PubMed] [Google Scholar]
- 78.Marcolini E.G., Burton J.H., Bradshaw J.R., Baumann M.R. A standing-order protocol for cricothyrotomy in prehospital emergency patients. Prehosp Emerg Care. 2004;8:23–28. doi: 10.1080/312703002776. [DOI] [PubMed] [Google Scholar]
- 79.McIntosh S.E., Swanson E.R., Barton E.D. Cricothyrotomy in air medical transport. J Trauma. 2008;64:1543–1547. doi: 10.1097/TA.0b013e3181271b60. [DOI] [PubMed] [Google Scholar]
- 80.O’Brien D.J., Danzl D.F., Sowers M.B., Hooker E.A. Airway management of aeromedically transported trauma patients. J Emerg Med. 1988;6:49–54. doi: 10.1016/0736-4679(88)90251-x. [DOI] [PubMed] [Google Scholar]
- 81.Oude Alink M.B., Moors X.R.J., Karrar S., Houmes R.J., Hartog D.D., Stolker R.J. Characteristics, management and outcome of prehospital pediatric emergencies by a Dutch HEMS. Eur J Trauma Emerg Surg. 2022;48:989–998. doi: 10.1007/s00068-020-01579-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Peters J., Bruijstens L., van der Ploeg J., Tan E., Hoogerwerf N., Edwards M. Indications and results of emergency surgical airways performed by a physician-staffed helicopter emergency service. Injury. 2015;46:787–790. doi: 10.1016/j.injury.2014.11.024. [DOI] [PubMed] [Google Scholar]
- 83.Spaite D.W., Joseph M. Prehospital cricothyrotomy: an investigation of indications, technique, complications, and patient outcome. Ann Emerg Med. 1990;19:279–285. doi: 10.1016/s0196-0644(05)82045-1. [DOI] [PubMed] [Google Scholar]
- 84.Turner J., Brown A., Boldy R., Lumley-Holmes J., Rosser A., James A. Out-of-hospital cardiac arrest due to hanging: a retrospective analysis. Emerg Med J. 2022;39:106–110. doi: 10.1136/emermed-2020-210839. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.