Abstract
Purpose: To describe a novel case of focal exudative retinal detachment, choroidal effusion, and acute angle closure in preeclampsia. Methods: A case report is presented. Results: A 37-year-old woman at 38 weeks gestation presented with 2 weeks of progressive blurred vision in the left eye. She had a visual acuity (VA) of 20/800 and an intraocular pressure (IOP) of 26 mm Hg in the left eye (compared with 17 mm Hg in the right eye). Examination showed subretinal fluid in the posterior pole, ciliochoroidal effusion, and angle closure in the left eye without pathology in the right eye. She was found to have hypertension and proteinuria consistent with preeclampsia. The visual symptoms resolved after delivery. At the 1-month follow-up, she had a VA of 20/60 OS, symmetric IOPs, and resolved subretinal and choroidal effusions. Conclusions: To our knowledge, this is the first reported case of ciliochoroidal effusion in the setting of preeclampsia. It may aid in the diagnosis of preeclampsia’s ocular manifestations and broaden pathophysiological understanding.
Keywords: preeclampsia, choroidal effusion, ciliochoroidal detachment, acute angle-closure glaucoma, angle closure, subretinal fluid, retinal detachment, pregnancy, hypertensive chorioretinopathy, hypertension
Introduction
Preeclampsia is a systemic vascular syndrome seen in peripartum patients. It is diagnosed based on the new onset of hypertension accompanied by proteinuria or other significant end-organ dysfunction after 20 weeks gestation or postpartum. 1 The etiology of preeclampsia is thought to involve antiangiogenic signaling in the maternal circulation and systemic endothelial dysfunction resulting from abnormal development of placental blood vessels, leading to placental hypoperfusion and ischemia. 1
Preeclampsia is associated with several ocular sequelae caused by microangiopathy, resembling processes in other organs, including the placenta, brain, liver, and kidney. Visual symptoms, most commonly blurred vision, have been reported in up to 25% of patients with preeclampsia with severe features. 2 The ocular manifestations of preeclampsia can mirror those of hypertensive retinopathy and include arteriolar narrowing, cotton-wool spots, flame hemorrhages, and serous retinal detachment (RD). 2 Serous RD in preeclampsia is often diagnosed postpartum and presents bilaterally, although prepartum and unilateral cases have been described. 3
We present a case of focal exudative detachment accompanied by novel findings of ciliochoroidal effusion leading to acute angle-closure glaucoma in a patient with preeclampsia.
Case Report
A 37-year-old G1P0 who was 38 weeks and 2 days pregnant presented with 2 weeks of gradually worsening blurred vision in the left eye. The pregnancy up to this point had been uneventful. She reported no eye pain or other ocular symptoms but did report worsening edema of her eyelids as well as her upper and lower extremities. She had no ocular history or other significant medical history.
On examination, the visual acuity was 20/20 OD and 20/800 OS. The intraocular pressure (IOP) measured with a tonometer (iCare) was 17 mm Hg in the right eye and 26 mm Hg in the left eye; on repeat assessment using a Tonopen (Reichert Technologies), the IOP in the left eye was 28 mm Hg. She had a possible trace afferent pupillary defect on the left side. No anterior segment abnormalities were noted on bilateral slitlamp examination. The fundus examination was normal in the right eye. The examination of the left eye was significant for subretinal fluid (SRF) in the macula extending beyond the arcades. There was also shallow peripheral choroidal effusion inferotemporally (Figure 1, A and B). No flame hemorrhages, vessel abnormalities, or other signs of retinal ischemia were visualized.
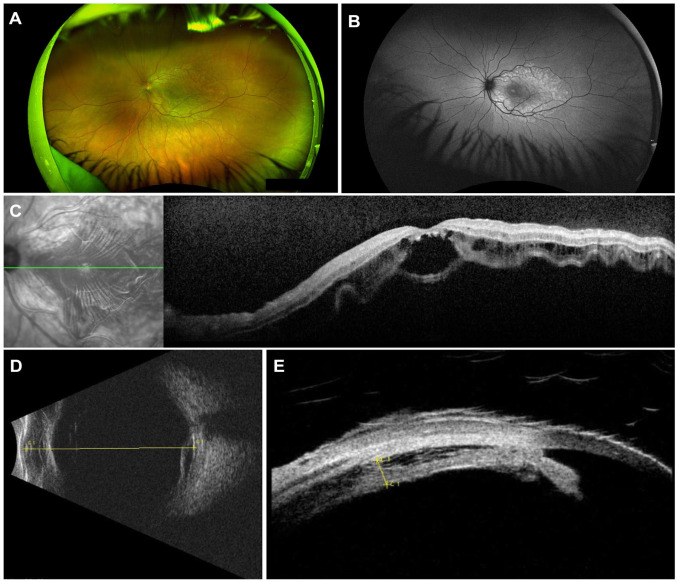
Figure 1.
Multimodal imaging of the left eye on initial presentation. Ultra-widefield fundus photograph (A) and fundus autofluorescence (B) show evidence of posterior pole subretinal fluid and shallow peripheral choroidal effusion, best appreciated in the inferotemporal periphery. (C) Optical coherence tomography shows subretinal fluid involving the entire macula. (D) B-scan ultrasonography shows retinal elevation involving the macula. (E) Ultrasound biomicroscopy shows shallow annular ciliochoroidal effusion with a maximum height of 1.3 mm (as marked) with shallowing of the anterior chamber and angle closure.
Fundus autofluorescence of the left eye showed decreased intensity over the fovea with a striated, vascular pattern of hypofluorescence and hyperfluorescence parafoveally (Figure 1B). Optical coherence tomography (OCT) of the same eye showed choroidal thickening, vessel dilation, and diffuse SRF throughout the macula (Figure 1C). B-scan ultrasonography of the left eye showed retinal elevation from 3 o’clock to 4:30 o’clock from the posterior pole to the equator, involving the macula (Figure 1D). No fundus thickening or mass lesion was detected. Annular serous ciliochoroidal effusion was detected on B-scan and ultrasound biomicroscopy, with associated angle closure and a central anterior chamber (AC) depth of 2.1 mm (Figure 1E).
Based on these ocular findings, the patient’s blood pressure was measured in the clinic and found to be 155/95 mm Hg. The previous measurement had been 110/75 mm Hg at an obstetric appointment 5 days previously.
The patient was sent to obstetric triage, where her systolic blood pressure remained elevated to the 140s and diastolic to the 90s. Urinalysis showed 3+ proteinuria. Based on these criteria, preeclampsia was diagnosed and deemed severe based on the presence of visual disturbance. 4 Labor was induced based on the diagnosis of preeclampsia, and the patient ultimately delivered via cesarean section. Her postpartum course was complicated by hemorrhage resulting from uterine atony and requiring a dilation and curettage. Her blood pressure normalized quickly after delivery.
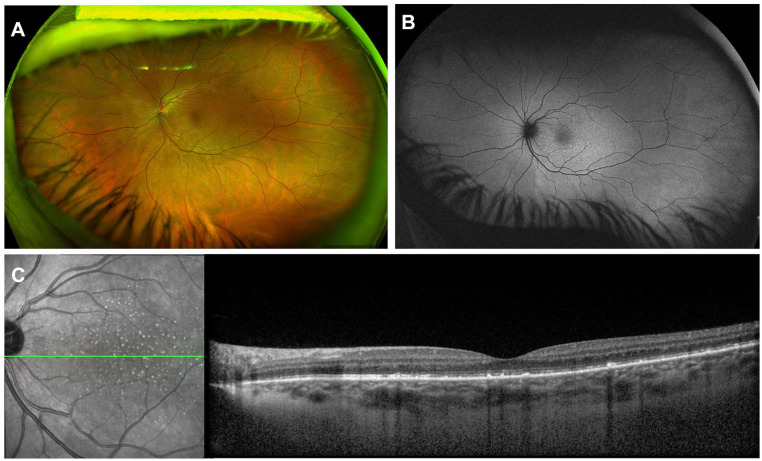
The patient returned to ophthalmology 1 month postpartum and reported visual improvement within days of delivery. The uncorrected VA in the left eye had improved to 20/100 with improvement to 20/60 with pinhole. The IOPs were symmetric. The ACs were deep bilaterally. Fundus examination of the left eye showed resolution of the posterior pole SRF and choroidal effusion, with new subtle hypopigmented pinpoint spots throughout the macula (Figure 2, A and B). The choroidal effusion had resolved. Repeat OCT confirmed resolution of the SRF with residual small, subretinal, hyperreflective deposits throughout the left macula as well as central ellipsoid zone attenuation (Figure 2C).
Figure 2.
Imaging of the left eye 1 month postpartum, Ultra-widefield fundus photograph (A) and fundus autofluorescence (B) show resolution of subretinal fluid and choroidal effusion with residual subtle punctate hyperautofluorescence in the macula. (C) Optical coherence tomography shows subretinal hyperreflective deposits in the area of previous subretinal fluid.
Conclusions
Preeclampsia and other causes of severe hypertension are known to cause choroid dysfunction. Endothelial dysfunction driven by antiangiogenic factors such as SFlt-1 (soluble Fms-like receptor tyrosine kinase-1) as well as generalized vasospasm have been shown to be part of the pathophysiology of preeclampsia. 1 These effects have been hypothesized to contribute to ischemia and the development of hypertensive choroidopathy. 5
Pathology studies have shown that the mechanism of hypertensive choroidopathy involves fibrinoid necrosis of choroidal vessels, and thus occlusion of the choriocapillaris, as well as necrosis of overlying retinal pigment epithelium (RPE). 6 In some cases, this compromise of the outer blood–retinal barrier leads to significant choroidal leakage, causing SRF or, if the volume of leakage is larger, serous RD. 7 Subretinal drusenoid deposits, as shown on postpartum imaging of our patient, are seen in approximately 30% of patients with serous RD resulting from preeclampsia, similar to serous RD from all causes. 8
There is evidence that choroidal changes occur in a large portion of preeclamptic patients. Increased choroidal thickness on OCT has been seen in cases of severe preeclampsia, and patients with preeclampsia have decreased perfusion of the choriocapillaris on OCT angiography compared with healthy pregnant women and nonpregnant women.9,10 A study comparing OCT and OCT angiography in patients who had had serous RD in the settings of preeclampsia and malignant hypertension found that features of hypertensive retinopathy, such as hemorrhages, exudates, cotton-wool spots, and optic disc edema, were more associated with the higher blood pressures observed in the malignant hypertension group. 5 Thus, choroidopathy was hypothesized to occur earlier in the course of hypertensive damage than retinopathy, consistent with our patient’s presentation with normal retinal vessels on examination and imaging. This could be the result of differential regulation of blood flow in retinal vessels compared with the choroid; the choroid is innervated by sympathetic and parasympathetic fibers, while retinal vascular flow is chiefly controlled by local autoregulation. 11
Although unilateral serous RD has been reported in preeclampsia, bilateral pathology is more common and more intuitive.3,12 It is possible that the unilateral choroidal pathology in our patient was simply the earliest manifestation of a process that might have affected the choroid in the fellow eye and potentially the retinal vasculature in either or both eyes if not for prompt delivery. It is also possible there are local differences in susceptibility of the choroid or RPE, perhaps as a result of a history of undiagnosed inflammation greater in 1 eye or a chance imbalance of ischemic and inflammatory signaling in the setting of preeclampsia.
Most notably, this patient had a choroidal effusion in addition to SRF, which to our knowledge has not been reported in the context of preeclampsia. Choroidal effusions are caused by transudation of serous fluid into the suprachoroidal potential space. 13 This shift of fluid into the interstitium can be driven by a hydrostatic pressure difference in the setting of decreased IOP or significant hypertension. 13 The latter mechanism is more likely in our patient, akin to her facial and lower extremity edema, which was also presumably caused by an imbalance in Starling forces. Although the studies of hypertensive choroidopathy discussed above posit choroidal ischemia as the underlying causative mechanism, they also suggest venous congestion that could predispose to interstitial fluid accumulation. Indeed, it is surprising that choroidal effusion has not been documented in previous case reports of ocular complications of preeclampsia. Additional imaging, such as ocular ultrasound, might be appropriate to evaluate for subtle choroidal fluid collections in future similar cases to predict and prevent complications.
To our knowledge, angle closure secondary to ciliochoroidal effusion with associated elevated IOP has not been reported as an ocular manifestation of preeclampsia. One study found no significant difference in IOP or ocular perfusion pressure between patients with severe preeclampsia and pregnant women with normal pressures. 14 However, secondary angle-closure glaucoma has been reported as a complication of choroidal effusion resulting from drug toxicity, glaucoma surgery, and idiopathic uveal effusion syndrome.15–17 Choroidal effusion, which has also been called ciliochoroidal detachment, causes angle closure via anterior displacement of the lens–iris diaphragm, 18 as was seen in our patient.
Fortunately, our patient’s acute pathology was reversible. The rapid improvement after delivery is typical of preeclampsia and its ocular manifestations. 2 Changes on the 1-month OCT are consistent with her 20/60 VA. Future monitoring is needed to determine whether her ellipsoid zone will reconstitute and her VA will improve further.
In conclusion, we report a case of unilateral SRF, choroidal effusion, and secondary angle closure in a prepartum patient with preeclampsia. Choroidal effusion and resulting angle closure leading to acutely elevated IOP have not previously been reported in the setting of preeclampsia. It is reasonable that in addition to SRF accumulation from hypertensive choroidopathy in the setting of preeclamptic endothelial dysfunction and vasospasm, pressure changes and venous congestion could lead to choroidal effusion and to anterior translation of the iris. Providers should monitor for choroidal effusion in cases of preeclampsia with ocular involvement. Preeclampsia is a relatively common cause of hypertensive crisis, and increased understanding of its ocular manifestations is key for diagnosis and treatment in the setting of peripartum pathology.
Footnotes
Ethical Approval: This case report was conducted in accordance with the Declaration of Helsinki. The collection and evaluation of all protected patient health information was performed in a US Health Insurance Portability and Accountability Act compliant manner.
Statement of Informed Consent: This report does not contain any personal identifying information and therefore written consent was not required.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Mary K. Munsell  https://orcid.org/0000-0003-4848-6786
https://orcid.org/0000-0003-4848-6786
Nicholas M. Carducci  https://orcid.org/0000-0002-6827-9664
https://orcid.org/0000-0002-6827-9664
References
- 1.Phipps EA, Thadhani R, Benzing T, Karumanchi SA.Pre-eclampsia: pathogenesis, novel diagnostics and therapies. Nature Rev Nephrol. 2019;15:275-289. doi: 10.1038/s41581-019-0119-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Samra KA.The eye and visual system in the preeclampsia/eclampsia syndrome: what to expect? Saudi J Ophthalmol. 2013;27(1):51-53. doi: 10.1016/j.sjopt.2012.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vigil-De Gracia P, Ortega-Paz L. Retinal detachment in association with pre-eclampsia, eclampsia, and HELLP syndrome. Int J Gynecol Obstet. 2011;114(3):223-225. doi: 10.1016/j.ijgo.2011.04.003 [DOI] [PubMed] [Google Scholar]
- 4.Espinoza J, Vidaeff A, Pettker CM, Simhan H; American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins. Gestational hypertension and preeclampsia. Obstet Gynecol. 2020;135(6):e237-e260. doi: 10.1097/AOG.0000000000003891 [DOI] [PubMed] [Google Scholar]
- 5.Lee CS, Choi EY, Lee M, Kim H, Chung H.Serous retinal detachment in preeclampsia and malignant hypertension. Eye (Lond). 2019;33:1707-1714. doi: 10.1038/s41433-019-0461-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kishi S, Tso MO, Hayreh SS.Fundus lesions in malignant hypertension: a pathologic study of experimental hypertensive choroidopathy. Arch Ophthalmol. 1985;103(8):1189-1197. doi: 10.1001/archopht.1985.01050080101029 [DOI] [PubMed] [Google Scholar]
- 7.He X, Ji Y, Yu M, Tong Y.Chorioretinal alterations induced by preeclampsia. J Ophthalmol. 2021;2021:8847001. doi: 10.1155/2021/8847001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Otero-Marquez O, Chung H, Lee CS, et al. Subretinal deposits in pre-eclampsia and malignant hypertension: implications for age-related macular degeneration. Ophthalmol Retina. 2021;5(8):750-760. doi: 10.1016/j.oret.2020.10.018 [DOI] [PubMed] [Google Scholar]
- 9.Garg A, Wapner RJ, Ananth CV, et al. Choroidal and retinal thickening in severe preeclampsia. Invest Ophthalmol Vis Sci. 2014;55:5723-5729. doi: 10.1167/iovs.14-14143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Urfalıoglu S, Bakacak M, Özdemir G, Güler M, Beyoglu A, Arslan G.Posterior ocular blood flow in preeclamptic patients evaluated with optical coherence tomography angiography. Pregnancy Hypertens. 2019;17:203-208. doi: 10.1016/j.preghy.2019.07.001 [DOI] [PubMed] [Google Scholar]
- 11.Bill A, Sperber GO.Control of retinal and choroidal blood flow. Eye. 1990;4:319-325. doi: 10.1038/eye.1990.43 [DOI] [PubMed] [Google Scholar]
- 12.Zatreanu L, Iyer NS.Unilateral chemosis, bullous serous retinal detachment, and presumed bacillary layer detachment in severe preeclampsia. Retin Cases Brief Rep. Published online March 4, 2021. doi: 10.1097/ICB.0000000000001141 [DOI] [PubMed] [Google Scholar]
- 13.Reddy AC, Salim S. Choroidal effusions. EyeNet Magazine. November2012:47-49. [Google Scholar]
- 14.Arpacı H, Koban Y, Tok A, Beyoğlu A.Ocular perfusion pressure and intraocular pressure in pregnant women with severe preeclampsia. Ginekol Pol. 2018;89(9):513-517. doi: 10.5603/GP.a2018.0087 [DOI] [PubMed] [Google Scholar]
- 15.Sankar PS, Pasquale LR, Grosskreutz CL.Uveal effusion and secondary angle-closure glaucoma associated with topiramate use. Arch Opthalmol. 2001;119(8):1210-1211. [PubMed] [Google Scholar]
- 16.Chira-Adisai T, Mori K, Ueno M, Sotozono C, Kinoshita S.Choroidal detachment-induced secondary angle-closure after trabeculectomy in patient with ocular venous congestion: a case report. Am J Ophthalmol Case Rep. 2020;19:100782. doi: 10.1016/j.ajoc.2020.100782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fourman S.Angle-closure glaucoma complicating ciliochoroidal detachment. Ophthalmol. 1989;96(5):646-653. doi: 10.1016/s0161-6420(89)32850-8 [DOI] [PubMed] [Google Scholar]
- 18.Lipa RKM, Sanchez MEG, Ordovas CAH, Aragües AR, Borque CG. Circumscribed ciliochoroidal effusion presenting as an acute angle closure attack. J Ophthalmol Vis Res. 2017;12(1):117-119. doi: 10.4103/jovr.jovr_99_14 [DOI] [PMC free article] [PubMed] [Google Scholar]