Abstract
Background: Migraine surgery at 1 of 6 identified “trigger sites” of a target cranial sensory nerve has rapidly grown in popularity since 2000. This study summarizes the effect of migraine surgery on headache severity, headache frequency, and the migraine headache index score which is derived by multiplying migraine severity, frequency, and duration. Materials and Methods: This is a PRISMA-compliant systematic review of 5 databases searched from inception through May 2020 and is registered under the PROSPERO ID: CRD42020197085. Clinical trials treating headaches with surgery were included. Risk of bias was assessed in randomized controlled trials. Meta-analyses were performed on outcomes using a random effects model to determine the pooled mean change from baseline and when possible, to compare treatment to control. Results: 18 studies met criteria including 6 randomized controlled trials, 1 controlled clinical trial, and 11 uncontrolled clinical trials treated 1143 patients with pathologies including migraine, occipital migraine, frontal migraine, occipital nerve triggered headache, frontal headache, occipital neuralgia, and cervicogenic headache. Migraine surgery reduced headache frequency at 1 year postoperative by 13.0 days per month as compared to baseline (I2 = 0%), reduced headache severity at 8 weeks to 5 years postoperative by 4.16 points on a 0 to 10 scale as compared to baseline (I2 = 53%), and reduced migraine headache index at 1 to 5 years postoperative by 83.1 points as compared to baseline (I2 = 2%). These meta-analyses are limited by a small number of studies that could be analyzed, including studies with high risk of bias. Conclusion: Migraine surgery provided a clinically and statistically significant reduction in headache frequency, severity, and migraine headache index scores. Additional studies, including randomized controlled trials with low risk-of-bias should be performed to improve the precision of the outcome improvements.
Keywords: headache, migraine disorders, migraine surgery, neuralgia, reconstructive surgical procedures, treatment outcome
Résumé
Historique: Le traitement de la migraine à l’une des six « zones gâchettes » établies d’un nerf crânien sensoriel cible ont rapidement gagné en popularité depuis 2000. La présente étude résume l’effet du traitement chirurgical de la migraine sur la gravité et la fréquence des céphalées et sur le score de migraine obtenu par la multiplication de la gravité, de la fréquence et de la durée des migraines. Matériel et méthodologie: La présente analyse systématique de cinq bases de données fouillées depuis leur création jusqu’à mai 2020 respecte la liste PRISMA et est enregistrée sous le numéro d’identification CRD42020197085 de PROSPERO. Les chercheurs ont retenu les études cliniques sur le traitement des céphalées par des interventions chirurgicales. Ils ont évalué le risque de biais des études aléatoires et contrôlées. Ils ont également effectué des méta-analyses des résultats au moyen d’un modèle à effets aléatoires pour déterminer le changement moyen regroupé par rapport à l’état de référence et, dans la mesure du possible, pour comparer des sujets traités à des sujets témoins. Résultats: Au total, 18 études respectaient les critères, y compris six études aléatoires et contrôlées, une étude clinique contrôlée, et 11 études non contrôlées auprès de 1 143 patients ayant des pathologies incluant la migraine, la migraine occipitale, la migraine frontale, la céphalée occipitale, la céphalée frontale, la névralgie occipitale et la céphalée cervicogénique. Par rapport à l’état de départ, le traitement chirurgical de la migraine avait réduit la fréquence des céphalées de 13,0 jours par mois (I2 = 0%) un an après l’opération, la gravité des céphalées de 4,16 points sur une échelle de 0 à 10 de huit semaines à cinq ans après l’opération (I2 = 53%) et le score de migraine de 83,1 points de un à cinq ans après l’opération (I2 = 2%). Ces méta-analyses sont limitées par le petit nombre d’études pouvant être analysées, y compris des études comportant de forts risques de biais. Conclusion: Le traitement chirurgical de la migraine assure une diminution cliniquement et statistiquement significative de la fréquence et de la gravité des céphalées, ainsi que des scores de migraine. D’autres études, y compris des études aléatoires et contrôlées comportant un faible risque de biais, devront être exécutées pour mieux préciser les améliorations aux résultats cliniques.
Mots-clés : céphalées, interventions chirurgicales reconstructives, névralgie, neuralgia, résultats du traitement, traitement chirurgical de la migraine, troubles migraineux
Introduction
An estimated 1 billion individuals worldwide have migraines.1,2 Affecting more women than men, migraines rank fifth for Disability-Adjusted Life Years in women and 20th in men. 1 Migraines may be accompanied by nausea, vomiting, photophobia, phonophobia, and typically last between 4 and 72 h. Many migraineurs also meet diagnostic criteria for chronic daily headache, defined as having 15 days with a headache per month for longer than 3 months.1–6
In 2000, Guyuron et al 7 reported that patient's migraines were resolved after forehead rejuvenation surgery. A surgical approach for peripherally triggered migraine has since been developed and includes 6 extracranial sites for peripheral sensory nerve decompression. Termed trigger sites, these sites are Site I: Frontal (supraorbital and supratrochlear nerves), Site II: Temporal (zygomaticotemporal branch of the trigeminal nerve), Site III: Endonasal or Rhinogenic (trigeminal end branches), Site IV: Occipital (greater occipital nerve), Site V: Temporal (auriculotemporal nerve), and Site VI: Occipital (lesser occipital nerve).8–12 While lifestyle changes and medical management remain the mainstay of headache treatment, patients with peripherally triggered migraines refractory to conservative management are often suitable candidates for surgical decompression.13–17
Several recent systematic reviews and meta-analyses have concluded that nerve decompression is effective in treating certain populations of individuals with headaches.15–18 1 review assessed surgical methods, finding that nerve decompression provided greater success rates than nerve stimulation which was in turn greater than radiofrequency ablation. 18 Other meta-analyses have summarized the outcome of headache elimination, reporting that the % of individuals with headache elimination ranges from 8.3% to 76% 16 and 8.3% to 83%. 17 A third meta-analysis which also assessed the proportion of individuals with headache elimination reported a pooled proportion of 38% of individuals experience migraine elimination, although when assessing only randomized controlled trials the proportion was 21.46%. 15 Additionally, the proportion of individuals who experienced no relief of symptoms following surgery ranged from 3.9% to 33.3%. 16 A meta-analysis has found that headache intensity improves by 3.97 on a 0 to 10 point scale, and headache frequency improves by 9.52 days per month, although high heterogeneity (I2 = 94%) in the meta-analyses of headache intensity and headache frequency limit the interpretation of those meta-analyses. This study systematically reviews all literature for peripheral nerve surgery performed on individuals with nerve compression-induced headaches. Meta-analyses were performed to establish how migraine surgery affects the outcomes of migraine intensity, migraine frequency, and the migraine headache index score.
Methods
This study complies with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines 19 and is registered on the International Prospective Register of Systematic Reviews under the ID: CRD42020197085.
Search Strategy
Two reviewers (DSH and AEG) independently performed literature searches of the following: Cochrane Library, Ovid MEDLINE, Ovid EMBASE, Web of Science, ClinicalTrials.gov. Searches were performed from inception of the database through June 28, 2020, using free text and MeSH term searches including the words “neuralgia,” “occipital nerve,” “nerve pain,” “neuropathy,” “migraine,” “tension-type headache,” “post-traumatic headache,” “cephalalgia,” “cervicogenic headache,” as well as word variations and similar words combined with the Boolean operators “OR” and “AND.” The search strategy was altered as necessary for each database. The full search strategy is included in Supplemental Appendix 1. Bibliographies of included studies were searched. Disagreement on article inclusion was resolved with a discussion with an additional reviewer (AGE). Data extraction was performed using a piloted form excel spreadsheet by 1 author (DSH) with over 90% of the data being checked by an additional reviewer (AGE). If multiple publications described the same cohort, then the study with the longer duration of follow-up was included.
Inclusion and Exclusion Criteria
Included were: (1) peer-reviewed original research articles, (2) prospective studies, (3) studies in English only, and (4) studies including patients over the age of 18 years, (5) studies treating causes of head pain including migraine, occipital neuralgia, cervicogenic headache, (6) studies of peripheral nerve surgery, and (7) studies reporting data on at least 8 patients.
Excluded were: (1) duplicate studies or cohorts, (2) incomplete trials, (3) abstracts or conference proceedings, (4) letters to the editor, (5) therapeutic nerve stimulation or non-denervating radiofrequency procedures, (6) retrospective studies, reviews, meta-analyses, case reports, animal studies, non-peer-reviewed “grey” literature, (7) studies with data on fewer than 8 patients, (8) studies not in English, and (9) studies treating vestibular migraine.
Risk of Bias
Risk of bias assessment was performed for randomized controlled clinical trials (RCTs) at study and outcome levels according to the Cochrane Collaboration Handbook Version 6.1. 20 Non-randomized clinical trials, or observational studies, all meet criteria for having high risk-of-bias according to this assessment and did not have a formal classification of risk-of-bias.
Outcome Measures
The primary outcome measure assessed by our study was the frequency of migraines experienced by patients. Secondary outcome measures were the severity of migraine, migraine headache index (MHI), and adverse effects. The MHI is a score that multiplies the migraine severity from 0 to 10, headache frequency in days per month, and the number of hours that the migraine is present. 21
Statistical Analysis
All statistical analyses were performed using RevMan 5.4.1 (Cochrane Collaboration). Only prospective studies were included in the meta-analyses. To incorporate the heterogeneity between studies, I2 was calculated to reflect the extent of variation that is primarily due to the different trials rather than sampling error. I2 values over 75% were considered highly heterogeneous and warranted investigation of study details that may contribute to heterogeneity. 22 All meta-analyses were performed using a random-effects model to account for increased variability between studies. 23 Continuous data were presented as mean differences and standard deviations. Data on headache frequency were converted to headache days per month for meta-analysis if a study reported data as headache days per week. Pain scores were converted to a 0 to 10 scale for meta-analyses if a study reported pain data on a 1 to 100 scale. Data used in analysis of studies reporting on multiple types of pain were overall, migraine pain, and pain in the operative trigger site. For analyses of score change from baseline, only studies reporting preoperative and postoperative outcome values were included. One study reported data only in subgroups of % improvement, and so the overall cohort's means and standard deviations were algebraically derived by combining the subgroups. 10 Standard error of the mean were calculated from standard deviation as follows: “SD = SEM * √(sample size).” A P-value <.05 was considered statistically significant. To establish a clinical context for the change in outcomes, a minimum clinically important difference (MCID) for pain severity was set as being between the range of 0.8 and 4 on a 0 to 10 scale, 24 and the MCID for headache frequency was set as 1 day per month. 25
Results
Article Selection
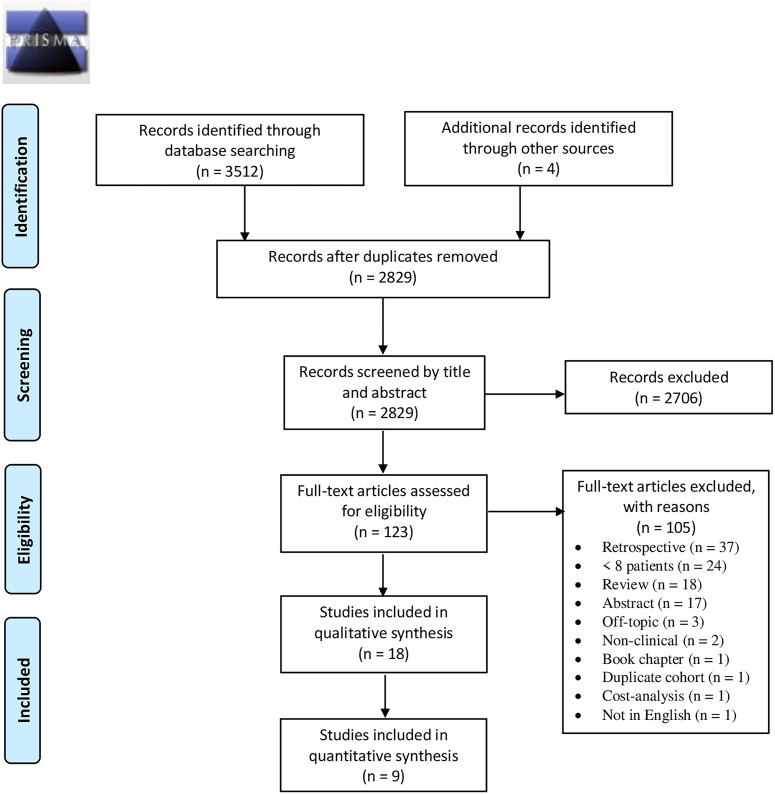
Application of the search strategy produced 3512 records, and 4 other studies were identified from review of bibliographies. After de-duplication, a title and abstract screen of 2829 unique records led to the exclusion of 2706 records. A full-text screen of the remaining 122 records led to the exclusion of 103 studies for the following reasons: retrospective study (n = 36), fewer than 8 patients (n = 24), abstract only (n = 17), review (n = 19), off-topic (n = 2), nonclinical study (n = 2), book chapter (n = 1), duplicate cohort (n = 1), not in English (n = 1), and radiofrequency treatment (n = 1). Therefore, 18 studies met criteria for qualitative synthesis and 9 studies had comparable data to allow for use in quantitative synthesis (Figure 1).
Figure 1.
Application of our search strategy identified 3516 records. After removal of duplicates, 2829 records were screened by title and abstract, leading to the exclusion of 2706 records. Full-text screen of 123 records led to the exclusion of 105 articles for reasons. Therefore, 18 articles were included in the systematic review and 9 articles in the meta-analyses.
Study Characteristics and Treatment Protocols
Study details and demographics are summarized in Table 1. Included were 6 RCTs,26–31 1 controlled clinical trial (CCT), 32 and 11 uncontrolled clinical trials (UCT).8,10,33–41 Studies treated 1143 patients with pathologies including migraine,10,26,27,30,40 occipital migraine, 41 frontal migraine, 31 occipital nerve triggered headache, 8 frontal headache, 39 occipital neuralgia,32–35,37,38 and cervicogenic headache.28,29,36 In the 13 studies reporting on patient gender, 141 patients were male and 319 were female. Seven studies were in North America,10,26,27,31,34,35,38 6 were in Europe,8,28,29,36,39,40 and 5 were in Asia.30,32,33,37,41
Table 1.
Summarizes the Study Details and Patient Demographic Information.
| Authors, year | Country | Study design, pathology | # of treated: control | # of females, males | Patient age (years) | Maximum follow-up | Outcomes tracked |
|---|---|---|---|---|---|---|---|
| Guyuron et al 26 | The United States of America | RCT Migraine | 100:25 | 73, 6 | 43.6 (range: 21-63) | 5 years | Headache frequency, headache severity, headache duration, MHI, MIDAS, MSQEM, MSQPRE, MSQRES, SFMEN, SFPH |
| Guyuron et al 27 | The United States of America | RCT Migraine | 49:26 | NR | Treatment: 45.1 ± 9.5 Control: 44.6 ± 8.3 | 1 year | % of patients with elimination or improvement, Headache frequency, headache severity, headache duration, MHI, MIDAS, MSQEM, MSQPRE, MSQRES, SFMEN, SFPH |
| Haspeslagh et al 28 | The Netherlands | RCT CEH | 15:15 | 22, 8 | Treatment: 47.5 ± 11.0 Control: 49.1 ± 12.8 | 1 year | Net changes in headache frequency, headache VAS severity, headache % VAS severity, RAND-36, MPI-DLV, and patient reported global perceived effect |
| Kvarstein et al 29 | Norway | RCT CEH | 31:21 | 25, 27 | Treatment: 45.8 ± 10.8 Control: 55.8 ± 8.3 | 18 week | Worst pain intensity, # of patients with pain reduction by 30% and 50%, procedural pain, health related quality of life, neck function, psychological distress, side effects |
| Filipović et al 39 | The Netherlands | UCT a Frontal headache | 22 | 15, 7 | Treatment: 42 ± 15.3 | 12 months | Headache intensity |
| Omranifard et al 30 | Iran | RCT Migraine | 25:25 | 42, 8 | Treatment: 42.2 ± 6.9 Control: 44.00 ± 7.6 | 1 year | Headache frequency, headache duration, headache intensity, MHI, headache cessation, treatment success (>50% improvement) |
| Yeom et al 32 | Korea | CCT Occipital neuralgia | 15:8 | 16, 7 | Treatment: 61 ± 6 Control: 62 ± 9 | Treatment: 21 (12-48) months Control: 33 (12-72) months | VAS pain, neck disability index, Japanese Orthopedic Association score |
| Gfrerer et al 10 | The United States of America | UCT Migraine | 85:NA | 71, 12 | Treatment: 45 ± 13 | 12.3 (minimum 3) months | Migraine frequency, migraine duration, migraine pain, MHI, # of trigger sites, and # who improved by either <5%, 5% to 80%, or >80% in MHI |
| Jose et al 33 | India | UCT Occipital neuralgia | 11:NA | 9, 2 | Treatment: 37.8 ± 7.6 | 10 to 14 months | Headache severity, headache frequency |
| Lin et al 41 | Taiwan | UCT Occipital migraine | 9 | 8, 1 | Treatment: 51.3 ± 10.7 | 8 weeks | Migraine severity |
| Blume et al 34 | The United States of America | UCT Occipital neuralgia | NR | NR | NR | 2 to 10 years | Recorded as excellent, good, fair, unchanged |
| Gatherwright et al 31 | The United States of America | RCT Frontal migraine | 13:0 | 13, 0 | Treatment: 41.8 (33-55) Control: NR | 22 (8-34) weeks | Headache frequency, headache severity, headache duration, MHI, migraine-free days, revision surgery prevalence |
| Dubuisson 35 | The United States of America | UCT Occipital neuralgia | 11:0 | 6, 5 | Treatment: 49 | 33 (3-66) months | Recorded as excellent (complete pain elimination without analgesics or therapy), good (>50% pain reduction with residual pain relieved by analgesics), or poor |
| Jansen 36 | Germany | UCT b CEH | 32:28 | 46, 14 | NR | Unilateral: 19.8 (2-100) months Bilateral: 25.5 (2-100) months | Recorded as pain free, improvement, recurrence |
| Li et al 37 | China | UCT Occipital neuralgia | 76 | 30, 46 | Treatment: 58 (47-78) | 20 (7-52) months | VAS pain severity |
| Raposio and Caruana 8 | Italy | UCT Occipital nerve triggered headache | 13 | NR | NR | 15 (6-36) months | % reduction in headache frequency, duration, and pain intensity |
| Ducic et al 38 | The United States of America | UCT Occipital neuralgia | 25 | NR | NR | None | Histologic investigation of the occipital artery |
| Caruana et al 40 | Italy | UCT Migraine, tension-type headache, and new daily persistent headache | 20 | 16, 4 | Treatment: 27 to 72 | 6 months | Validated questionnaires |
Abbreviations: UCT, uncontrolled clinical trial; CCT, controlled clinical trial; RCT, randomized controlled clinical trial; CEH, cervicogenic headache; MHI, migraine headache index; MIDAS, migraine disability assessment; MSQEM, migraine-specific questionnaire; MSQPRE, migraine-specific questionnaire, preventive; MSQRES, migraine-specific questionnaire, restrictive; SFMEN, 36-item short-form mental medical outcomes survey; SFPH, 36-item short-form physical medical outcomes survey; RAND-36, 36-item short-form survey; MPI-DLV, multidimentional pain inventory; VAS, visual analog scale.
This study included control comparisons of migraine medication and injected botulinum toxin type A by using the preoperative assessments of the patients who underwent these treatments.
This study also utilized a retrospective control cohort who saw no benefit from a surgery performed for an unrelated reason.
Data are reported as mean ± standard deviation.
Outcomes
Headache frequency was reported as episodes of pain per month10,26,27,30,33 or per week. 28 Headache severity was recorded on a visual analog scale from 0 to 1026,27,30,32,33,37,39,42 or 0 to 100,28,29 numeric rating scale from 0 to 10,10,31,41 Likert scale, 34 or by reporting symptom resolution or recurrence.36,37 Study outcomes are summarized in Table 2.
Table 2.
Summarizes the Surgical Outcomes of the Studies.
| Author, year | Treatment groups | Results |
|---|---|---|
| Guyuron et al 26 | Treatment: Occipital trigger site surgery (Trigger site IV), frontal trigger site surgery (Trigger site I), temporal trigger site surgery (Trigger site II), and/or intranasal trigger site surgery (Trigger site III). Control: occipital saline injection. | Treatment: All outcomes were significantly improved as compared to baseline (P < .0001) Control: Data is not present in this article due to receiving treatment at 1 year |
| Guyuron et al 27 | Treatment: Occipital trigger site surgery (Trigger site IV), frontal trigger site surgery (Trigger site I), and temporal trigger site surgery (Trigger site II). Control: Occipital trigger site surgery without semispinalis capitis myectomy, frontal trigger site surgery without myectomy, and temporal trigger site surgery without neurectomy. | Treatment: 57% had elimination and 84% had improvement; all other outcomes had statistically significant improvement. Control: 4% had elimination and 58% had improvement; statistically significant improvement occurred in all outcomes except headache duration, MSQEM, and SFPH |
| Haspeslagh et al 28 | Treatment: C3-C6 radiofrequency facet denervation followed by adjacent level diagnostic nerve blocks prior to additional denervation Control: Greater occipital nerve block with lack of improvement indicating transcutaneous electrical nerve stimulation therapy | Significant differences between treatment and control groups were not found |
| Kvarstein et al 29 | Treatment: Nerve-stimulator-guided percutaneous nitrous oxide cryoneurolysis for 90 s Control: Nerve-stimulator-guided methylprednisolone, bupivacaine injection | Treatment and control provided statistically significant decreases in pain intensity at all weeks. Treatment provided a statistically significant superior reduction compared to control in pain intensity at week 7 (P < .02) and 17 (P < .04) |
| Filipović et al 39 | Frontal trigger site surgery (Trigger site I) by endoscopic approach without glabellar muscle group resection | Headache intensity was significantly reduced at 3 and 12 months, with no statistical difference between 3 and 12 months, and the improvements were superior to patient self-controls of medication or botulinum toxin type A |
| Omranifard et al 30 | Treatment: Occipital trigger site surgery (Trigger site IV), frontal trigger site surgery (Trigger site I), temporal trigger site surgery (Trigger site II), and/or intranasal trigger site surgery (Trigger site III) Control: Medical therapy (inderal and amitriptyline) | Treatment had statistically significant superior improvements to control in headache frequency, headache duration, headache intensity, MHI, headache cessation, and treatment success (all P = or < .001) |
| Yeom et al 32 | Treatment: C1-C2 facet joint distraction, bone block insertion, and C1 posterior arch screw fixation with C2 root preservation Control: C2 root transection with C1-C2 segmental screw fixation via lateral mass screws | Treatment and control groups provided statistically significant improvements in VAS pain at 1, 3, 6, and 12 month follow-ups, but not in neck disability index or Japanese Orthopedic Association scores |
| Gfrerer et al 10 | Occipital trigger site (Trigger site IV) and lesser occipital trigger site surgery (Trigger site VI) performed with nerve excision | 57 patients improved by >80%, 14 by 5% to 80%, and 12 by <5%. 32 patients had 1 trigger site, 25 patients had 2 trigger sites, 15 had 3 trigger sites, 8 had 4 trigger sites, 2 had 5 trigger sites, and 1 had 6 trigger sites |
| Jose et al 33 | Treatment: Occipital trigger site surgery (Trigger site IV) | Surgery improved headache severity (P < .0033) and headache frequency (P < .0036) |
| Lin et al 41 | Occipital trigger site surgery (Trigger site IV) with triamcinolone injection and without subcutaneous flap | Migraine severity was significantly reduced as compared to baseline (P = .0067), and 8 of the 9 patients improved following surgery |
| Blume et al 34 | Occipital nerve territory radiofrequency electrocoagulation lesioning with a hand-held thermoelectrode | Excellent n = 351 (78%), good n = 32 (7%), fair n = 22 (5%); unchanged n = 45 (10%) |
| Gatherwright et al 31 | Frontal trigger site surgery (Trigger site I) Group 1: myectomy and arterectomy Group 2: myectomy and fasciotomy/foraminotomy Group 3: myectomy, fasciotomy/foraminotomy, and arterectomy The majority of patients also underwent sites II, III, V, or VI surgery. | Analysis for arterectomy subgroup: notable, but nonstatistically significant baseline differences. Revision surgeries were only performed if nonarterectomy. Only procedures with arterectomy provided statistically significant improvements to pain frequency and MHI. Both arterectomy and nonarterectomy groups saw statistically significant increases in migraine-free days. |
| Dubuisson 35 | C1 to 3 posterior rhizotomy | The 11 patients underwent 14 procedures and unilateral results were excellent (n = 7) or good (n = 3) or poor (n = 4) |
| Jansen 36 | Anterior cervical discectomy and fusion including removal of thickened dorsal ligament and dorsal osteophytes and insertion of anterior iliac crest into the intervertebral space | 100% were pain free postoperative initially, however, 37% of unilateral patients had recurrence or a new headache, and 36% of bilateral patients had recurrence or a new headache. A control retrospective cohort of patients with an unrelated (eg, for cancer) spine surgery saw no improvements in headache pain. |
| Li et al 37 | Occipital trigger site surgery (Trigger site IV) without myectomy or subcutaneous flap | 89.4% completely resolution, 6.6% had a 75% reduction, 3.9% recurrence |
| Raposio and Caruana 8 | Greater occipital nerve decompression with occipital artery ligation when in close proximity to the nerve (11 patients) or neurolysis at the trapezius or semispinalis muscle (2 patients) | 9 (92%) had complete relief, 3 (23%) had a >50% reduction in duration, frequency, and intensity, and 1 (8%) did not see benefits |
| Ducic et al 38 | Occipital trigger site surgery (Trigger site IV) without myectomy or subcutaneous flap | None of 15 arteries had evidence of vasculitis |
| Caruana et al 40 | Frontal trigger site surgery (Trigger site I) by endoscopic approach with glabellar muscle group resection Occipital trigger site surgery (Trigger site IV) without subcutaneous flap | 8 (40%) had migraine elimination, 9 had migraine alleviation (45%), and 3 (15%) did not see benefits |
Abbreviations: MHI, migraine headache index; MSQEM, migraine-specific questionnaire; SFPH, 36-item short-form physical medical outcomes survey.
Risk of Bias Assessment
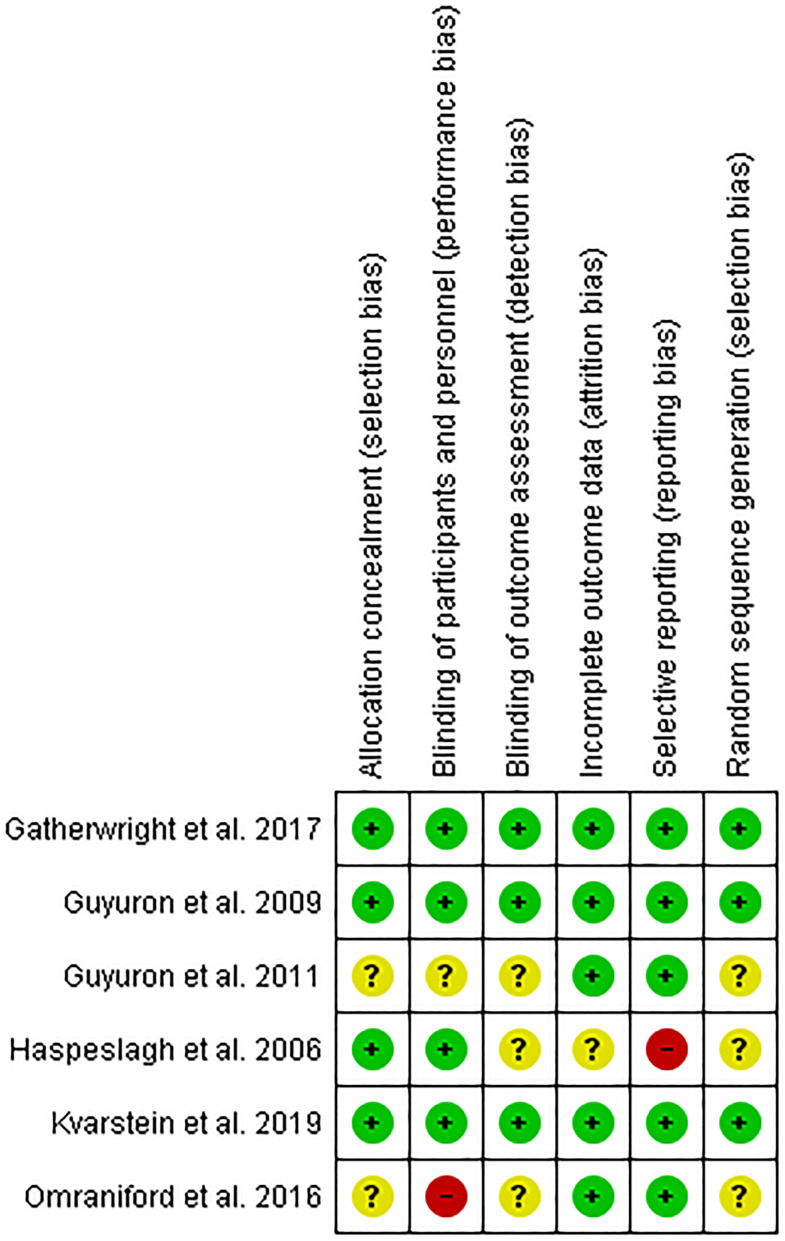
Cochrane risk of bias for the 6 RCTs is included in Figure 2. Three RCTs had a low risk of bias, 2 had a high risk of bias, and 1 study had an unclear risk of bias. The 11 UCTs and 1 CCT have a risk of bias due to their study designs not having randomized controls.
Figure 2.
Risk of bias assessment for randomized controlled trials resulted in 3 studies having low risk-of-bias, 1 study having unclear risk-of-bias, and 2 studies having high risk-of-bias. Red = high risk-of-bias. Yellow = unclear risk-of-bias. Green = low risk-of-bias.
Meta-Analyses
Meta-analyses were performed included only clinical trials (ie, RCTs, CCTs, UCTs).
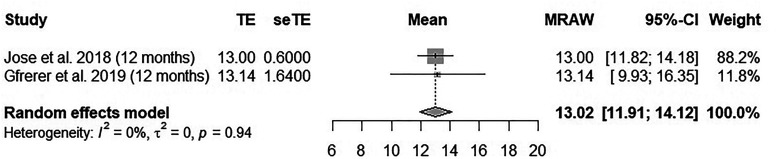
Meta-Analysis of Headache Frequency
Two UCTs10,33 had comparable data for analysis of the change in headache frequency from baseline to 12 months postoperative follow-up. Patients who underwent surgery had a pooled mean reduction of 13.02 headache days per month (I2 = 0%), as shown in Figure 3.
Figure 3.
Meta-analysis shows that following migraine surgery, the pooled mean reduction in migraine frequency at 1-year postoperative follow-up compared to baseline was 13.02 headache days per month.
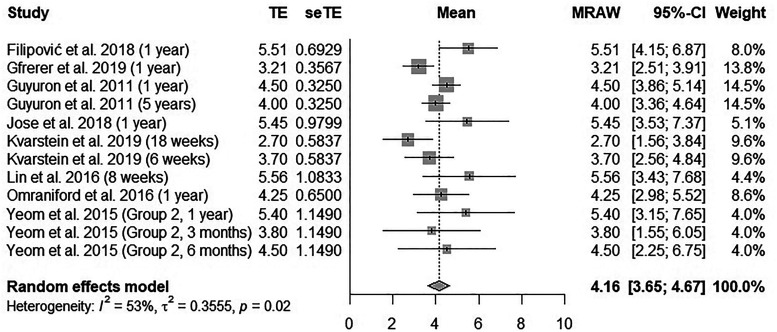
Meta-Analysis of Headache Pain Severity
Comparable data were present in 8 studies including 3 RCTs,26,29,30 1 CCT, 32 and 4 UCTs10,33,39,41 for analysis of the change in headache severity from baseline to postsurgical follow-ups from 8 weeks to 5 years. As shown in Figure 4, surgery provided a 4.16 pooled mean reduction in headache pain severity on a 0 to 10 scale as compared to baseline (I2 = 53%).
Figure 4.
Meta-analysis shows that following migraine surgery, the pooled mean reduction in migraine pain severity at 8 weeks to 5 years postoperative follow-ups compared to baseline was 4.16 points on a scale from 0 to 10.
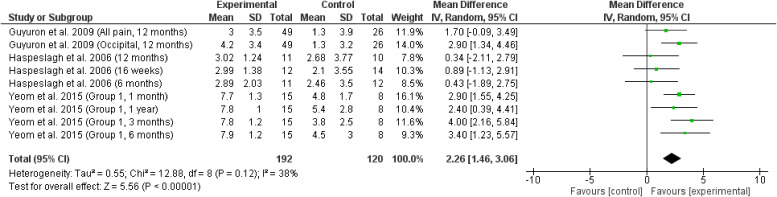
Comparable data were present in 2 RCTs27,28 and 1 CCT 32 for analysis of the net change in headache severity between treatment and control groups at 1 to 12 month follow-ups. Compared to control groups, headache severity in the treatment groups was significantly lower (P < .00001, I2 = 39%), as shown in Figure 5.
Figure 5.
Meta-analysis shows that at 1 month to 1 year, the treatment groups provided a greater reduction to headache intensity than the control groups.
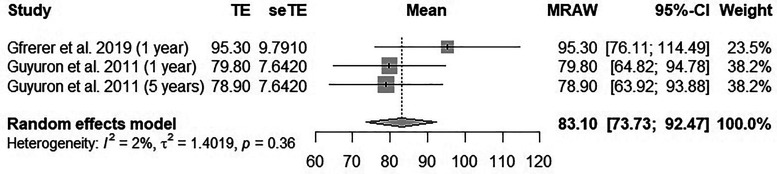
Meta-Analysis of Migraine Headache Index
Comparable data were present in 1 RCT 26 and 1 UCT 10 for analysis of the change from baseline to 1 to 5 year postoperative follow-ups. As shown in Figure 6, patients who underwent surgery had a pooled mean reduction in of 83.1 points (I2 = 2%).
Figure 6.
Meta-analysis shows that following migraine surgery, the pooled mean reduction in migraine headache index score at 1 to 5 years postoperative follow-ups compared to baseline was 83.10 points.
Discussion
Surgical Procedures and Outcomes
The meta-analyses for pain severity, headache frequency, and MHI each support migraine surgery as a method of treating individuals with migraine headaches. Each meta-analysis resulted in low or moderate heterogeneity between the included studies, despite including all types of migraine surgeries and postoperative follow-up times ranging from 1 month to 5 years. This suggests that the outcomes were comparable at short and long-term duration, and that surgery at the spinal nerve root and peripheral cranial nerve are also comparable.
The meta-analyses show that patients improved by a pooled mean of 4.16 points out of 10 in headache severity from a mean baseline severity of 7.86, a 53% improvement. This change is greater than the range of MCIDs that have been proposed for changes in pain severity, suggesting that migraine surgery produces clinically significant changes in the pain severity. 24 For headache frequency, patients improved by a pooled mean of 13.02 headache days per month, a 71% improvement from their baseline mean of 18.3. The change in headache frequency is also much greater than the previously described 1 day MCID of headache frequency which produces an improvement in a patient's quality of life. 25 Similarly, the 83.1 point pooled mean reduction in a patient's MHI represented a 77% reduction from their baseline mean 107.8 point MHI. An MCID for MHI has yet to be described in literature, however, because the MHI components of headache severity and frequency were both significantly improved, it can be assumed that this MHI improvement represents a clinically significant improvement.
Future studies may seek to investigate whether surgical decompression provides superior outcomes to nerve transections or other axonotmetic or neurotmetic therapies. Suboptimal outcomes are well documented in the bodies of literature on therapeutic nerve transections for amputations and neuromas even with protection or coaptation of the transected nerve ending to muscular, vascular, or adjacent nerve structures.43–47 However, for migraine surgery, a ubiquitous fit of all trigger sites to either decompression or neurolysis may not be feasible. The well-characterized sites of nerve compression in Site IV coincide with widespread decompression surgery being performed at this site. Alternatively, Site II does not have characterized areas of nerve compression and is often treated with nerve transection. In 2014, Ducic et al 48 surveyed Site IV patients who did not improve following nerve decompression. These patients were offered a second surgery to excise the nerve, which was reportedly more helpful than decompression in 68% of these patients, although adverse effects of nerve transection such as numbness and hypersensitivity were reported by 31%.
Importance of Trigger Site Identification
In a retrospective review by Forootan et al 49 of a Guyuron cohort, it was reported that patients often underwent simultaneous surgery at several trigger sites, for an average of 2.6 trigger sites per patient. Gfrerer et al 10 in a 2019 UCT, also operated on an average of 2 trigger sites, and reported that their outcomes followed an “all or nothing” pattern of response. A total of 57 of their 83 patients (69%) showed over an 80% improvement in MHI, while 17% of the patients showed less than 5% improvement in MHI. We believe that this highlights the importance of identifying and treating the trigger sites contributing to the migraine, whether by patient history stating the origin of the pain, physical exam eliciting tenderness in a trigger site, or injected botulinum toxin or anesthetic providing a temporary resolution to their headaches.
Occipital (Including Sites IV and VI) Surgery
In 1986, Blume and Ungar-Sargon 34 described percutaneous radiofrequency denaturation near the greater occipital nerve which produced good to excellent results in 85% of patients who had preoperative neuralgia responsive to GON block. Surgery at this area was later described as Site IV surgery by Guyuron et al 50 in 2005 and includes release of 6 recognized sites of occipital nerve compression: (1) between semispinalis capitis and obliques capitis inferior muscles, (2) as the nerve enters and (3) exits the semispinalis capitis muscle, (4) as the nerve enters the trapezius muscle, and (5) exits the trapezius fascia, and (6) by the occipital artery when it courses adjacent to the GON.51,52
In a 2009 RCT by Guyuron et al 27 a semispinalis capitis myectomy and subcutaneous flap procedure to protect the nerve were superior to nerve exposure alone. Most studies have reported using Guyuron's surgical method to Site IV surgery,27,30,50,52–54 which has been previously described, 55 although GON excision or neurolysis have also been reported as surgical options such as in patients who fail initial GON decompression.10,48,54
The role of occipital artery excision remains a topic of debate. Occipital artery resection has yet to show superiority to nonremoval, 56 but is believed by Guyuron and co-authors 31 to be a critical procedural component based on importance demonstrated from site I surgery. Whether routine removal of the arteries affects patient outcomes should be investigated in future studies. Despite being thought of as a compressive neuropathy, 55 adjunctive use of triamcinolone injections during surgery has also been described 41 and follows the trend of including corticosteroids in anesthetic injections.29,57–60 Excised occipital arteries did not have histologic evidence of vasculitis. 38
Occipital migraines are hypothesized to arise on occasion from the lesser occipital nerve (LON),8–12 located in the Site VI surgical area, or the third occipital nerve (TON) which may be treated using the same incision as Site IV surgery. 55 Patient outcomes are thought to be the same whether the TON is excised or decompressed. 9 The LON has had 3 possible points of compression identified by Peled et al 61 in 2016: (1) as the LON emerges from deep fascia to be behind the sternocleidomastoid, (2) as the LON ascends along with the SCM, (3) and at the branch point of the LON. The LON may be approached through an incision on the posterior sternocleidomastoid,41,52 although Ducic et al in 2009 and Afifi et al52,62 in 2019 reported a transversely oriented incision for occipital surgery, 2.5 cm caudal to the occipital protuberance, which allows access to both Sites IV and VI.
Surgery for Non-Occipital Headaches
The auriculotemporal nerve courses alongside the superficial temporal artery and has since been characterized as the target in Site V surgery. In 2019, Gfrerer et al 10 reported that a Site V surgery, which consists of nerve excision, 55 was undergone by only 6% of their patients who underwent migraine surgery.
Site I is a common operative site for migraine surgery 50 performed in 57% of the migraine surgery patients of Gfrerer et al. 10 Both endoscopic and open techniques have been described to decompress the supratrochlear and supraorbital nerve branches of the ophthalmic division of the trigeminal nerve. 55 In a 2012 retrospective matched analysis of a Guyuron cohort by Chepla et al 42 patients who underwent foraminectomy with depressor supercilii and corrugator myectomy were found to have statistically significant superior improvements in forehead pain (P < .05), forehead frequency (P < .05), and MHI (P < .01) compared myectomy alone. Arterectomy was shown to be vital to patient outcomes in a 2017 RCT by Gatherwright et al 31 although the total study size of 13 limits the finding that all 4 patients who underwent surgery without arterectomy required reoperation whereas none of the patients who initially underwent arterectomy required revision surgery.
Gfrerer et al 10 operated on the zygomaticotemporal nerve of Site II in 43% of their patients who underwent migraine surgery, for which excision is the standard procedure. 55 In a 2017 retrospective review, Janis et al 11 found surgical nerve decompression had greater improvements in MHI, headache frequency, severity, and duration than those who continued long-term botulinum injections.
Limitations
This review is limited by a low number of high-quality randomized controlled trials. Likewise, the meta-analyses are limited by having a small number of studies which increases the risk of type I error and may result in confidence intervals being too narrow. 23 The meta-analyses included patients with varied surgical procedures and operative sites as well as criteria for patient selection. Additionally, the meta-analytic method of pooling a change score is limited in its ability to account for baseline differences between studies. 63 As a relatively new field, migraine surgery publications may be at risk for publication bias whereby negative results are less prevalent, although the literature currently provides strong support toward the efficacy of migraine surgery in treating migraines.
Conclusion
Our meta-analyses indicate migraine surgery reduces headache frequency, headache severity, and the migraine headache index. The reductions in headache frequency and severity are clinically significant, although based on a small number of studies. The reviewed literature includes many studies that have high risk-of-bias, so additional RCTs with low risk-of-bias should be performed to improve the precision of the outcome improvements. Future research should focus on improving migraine surgery outcomes and investigating patient factors that predict surgical outcomes.
Supplemental Material
Supplemental material, sj-docx-1-psg-10.1177_22925503211036701 for Outcomes of Surgical Treatment of Migraines: A Systematic Review & Meta-Analysis by Adam G. Evans, Dorian S. Hill, Andrew E. Grush, Mauricio A. Downer, Maryo M. Ibrahim, Patrick E. Assi, Jeremy T. Joseph and Salam H. Kassis in Plastic Surgery
Footnotes
Ethics Statement: This article does not contain any studies with human or animal subjects.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Adam G. Evans https://orcid.org/0000-0001-8535-7583
Supplemental Material: Supplemental material for this article is available online.
References
- 1.Stovner LJ, Nichols E, Steiner TJ, et al. Global, regional, and national burden of migraine and tension-type headache, 1990-2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol. 2018;17(11):954-976. doi: 10.1016/S1474-4422(18)30322-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Migraine is an extraordinarily prevalent neurological disease, affecting 39 million men, women and children in the U.S. and 1 billion worldwide. Migraine Research Foundation. https://migraineresearchfoundation.org/about-migraine/migraine-facts/. Accessed 11/26/2020.
- 3.Jensen R, Stovner LJ. Epidemiology and comorbidity of headache. Lancet Neurol. 2008;7(4):354-361. doi: 10.1016/s1474-4422(08)70062-0 [DOI] [PubMed] [Google Scholar]
- 4.Ahmed F, Parthasarathy R, Khalil M. Chronic daily headaches. Ann Indian Acad Neurol. 2012;15(Suppl 1):S40-S50. doi: 10.4103/0972-2327.100002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Headache classification committee of the international headache society (IHS) The international classification of headache disorders, 3rd edition. Cephalalgia. 2018;38(1):1-211. doi: 10.1177/0333102417738202 [DOI] [PubMed] [Google Scholar]
- 6.Charles A. The migraine aura. Continuum (Minneap Minn). 2018;24(4, Headache):1009-1022. doi: 10.1212/con.0000000000000627 [DOI] [PubMed] [Google Scholar]
- 7.Guyuron B, Varghai A, Michelow BJ, Thomas T, Davis J. Corrugator supercilii muscle resection and migraine headaches. Plast Reconstr Surg. 2000;106(2):429-434; discussion 435-427. doi: 10.1097/00006534-200008000-00030 [DOI] [PubMed] [Google Scholar]
- 8.Raposio E, Caruana G. Tips for the surgical treatment of occipital nerve-triggered headaches. Eur J Plast Surg. 2017;40(3):177-182. doi: 10.1007/s00238-016-1249-8 [DOI] [Google Scholar]
- 9.Lee M, Lineberry K, Reed D, Guyuron B. The role of the third occipital nerve in surgical treatment of occipital migraine headaches. J Plast Reconstr Aesthet Surg. 2013;66(10):1335-1339. doi: 10.1016/j.bjps.2013.05.023 [DOI] [PubMed] [Google Scholar]
- 10.Gfrerer L, Hulsen JH, McLeod MD, Wright EJ, Austen WG. Migraine surgery: an all or nothing phenomenon? Prospective evaluation of surgical outcomes. Ann Surg. 2019;269(5):994-999. doi: 10.1097/sla.0000000000002697 [DOI] [PubMed] [Google Scholar]
- 11.Janis JE, Barker JC, Palettas M. Targeted peripheral nerve-directed onabotulinumtoxin A injection for effective long-term therapy for migraine headache. Plastic Reconstruct Surg – Global Open. 2017;5(3):e1270. doi: 10.1097/GOX.0000000000001270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Behin F, Behin B, Bigal ME, Lipton RB. Surgical treatment of patients with refractory migraine headaches and intranasal contact points. Cephalalgia. 2005;25(6):439-443. doi: 10.1111/j.1468-2982.2004.00877.x [DOI] [PubMed] [Google Scholar]
- 13.Demaagd G. The pharmacological management of migraine, part 1: overview and abortive therapy. Pharmacy Therapeutics. 2008;33(7):404-416. [PMC free article] [PubMed] [Google Scholar]
- 14.Wormald JCR, Luck J, Athwal B, Muelhberger T, Mosahebi A. Surgical intervention for chronic migraine headache: a systematic review. JPRAS Open. 2019;20:1-18. doi: 10.1016/j.jpra.2019.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vincent AJPE, van Hoogstraten WS, Maassen Van Den Brink A, van Rosmalen J, Bouwen BLJ. Extracranial trigger site surgery for migraine: a systematic review with meta-analysis on elimination of headache symptoms. Front Neurol. 2019;10:89-89. doi: 10.3389/fneur.2019.00089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nagori SA, Jose A, Roychoudhury A. Surgical management of migraine headaches: a systematic review and meta-analysis. Ann Plast Surg. 2019;83(2):232-240. doi: 10.1097/sap.0000000000001743 [DOI] [PubMed] [Google Scholar]
- 17.Bink T, Duraku LS, Ter Louw RP, Zuidam JM, Mathijssen IMJ, Driessen C. The cutting edge of headache surgery: a systematic review on the value of extracranial surgery in the treatment of chronic headache. Plast Reconstr Surg. 2019;144(6):1431-1448. doi: 10.1097/prs.0000000000006270 [DOI] [PubMed] [Google Scholar]
- 18.Ducic I, Felder JM, 3rd, Fantus SA. A systematic review of peripheral nerve interventional treatments for chronic headaches. Ann Plast Surg. 2014;72(4):439-445. doi: 10.1097/sap.0000000000000063 [DOI] [PubMed] [Google Scholar]
- 19.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Br Med J. 2009;339:b2535. doi: 10.1136/bmj.b2535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Higgins J, Thomas J, Chandler J, (eds.) et al. Cochrane Handbook for Systematic Reviews of Interventions version 6.2 (updated February 2021). Cochrane, 2021. Available from www.training.cochrane.org/handbook. [Google Scholar]
- 21.Schade AJ. Quantitative assessment of the tension-type headache and migraine severity continuum. Headache. 1997;37(10):646-653. doi: 10.1046/j.1526-4610.1997.3710646.x [DOI] [PubMed] [Google Scholar]
- 22.Lee YH. An overview of meta-analysis for clinicians. Korean J Intern Med. 2018;33(2):277-283. doi: 10.3904/kjim.2016.195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McKenzie JE, Herbison GP, Deeks JJ. Impact of analysing continuous outcomes using final values, change scores and analysis of covariance on the performance of meta-analytic methods: a simulation study. Res Synth Methods. 2016;7(4):371-386. doi: 10.1002/jrsm.1196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Olsen MF, Bjerre E, Hansen MD, et al. Pain relief that matters to patients: systematic review of empirical studies assessing the minimum clinically important difference in acute pain. BMC Med. 2017;15(1):35. doi: 10.1186/s12916-016-0775-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Silberstein SD, Marmura MJ, Shaw J, Yu S. Headache prophylaxis with BoNTA: patient characteristics. Headache: J Head Face Pain. 2010;50(1):63-70. 10.1111/j.1526-4610.2009.01481.x [DOI] [PubMed] [Google Scholar]
- 26.Guyuron B, Kriegler JS, Davis J, Amini SB. Five-year outcome of surgical treatment of migraine headaches. Plast Reconstr Surg. 2011;127(2):603-608. doi: 10.1097/PRS.0b013e3181fed456 [DOI] [PubMed] [Google Scholar]
- 27.Guyuron B, Reed D, Kriegler JS, Davis J, Pashmini N, Amini S. A placebo-controlled surgical trial of the treatment of migraine headaches. Plast Reconstr Surg. 2009;124(2):461-468. doi: 10.1097/PRS.0b013e3181adcf6a [DOI] [PubMed] [Google Scholar]
- 28.Haspeslagh SRS, Van Suijlekom HA, Lamé IE, Kessels AGH, van Kleef M, Weber WEJ. Randomised controlled trial of cervical radiofrequency lesions as a treatment for cervicogenic headache [ISRCTN07444684]. BMC Anesthesiol. 2006;6(1):1. doi: 10.1186/1471-2253-6-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kvarstein G, Högström H, Allen SM, Rosland JH. Cryoneurolysis for cervicogenic headache – a double blinded randomized controlled study. Scand J Pain. 2019;20(1):39-50. doi: 10.1515/sjpain-2019-0086 [DOI] [PubMed] [Google Scholar]
- 30.Omranifard M, Abdali H, Ardakani M, Talebianfar M. A comparison of outcome of medical and surgical treatment of migraine headache: in 1 year follow-up. Adv Biomed Res. 2016;5(1):121-121. doi: 10.4103/2277-9175.186994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gatherwright JR, Wu-Fienberg Y, Guyuron B. The importance of surgical maneuvers during treatment of frontal migraines (site I): a prospective, randomized cohort study evaluating foraminotomy/fasciotomy, myectomy, and arterectomy. J Plast Reconstr Aesthet Surg. 2018;71(4):478-483. doi: 10.1016/j.bjps.2017.09.015 [DOI] [PubMed] [Google Scholar]
- 32.Yeom JS, Riew KD, Kang SS, et al. Distraction arthrodesis of the C1–C2 facet joint with preservation of the C2 root for the management of intractable occipital neuralgia caused by C2 root compression. Spine. 2015;40(20):e1093-e1102. doi: 10.1097/BRS.0000000000001031 [DOI] [PubMed] [Google Scholar]
- 33.Jose A, Nagori SA, Chattopadhyay PK, Roychoudhury A. Greater occipital nerve decompression for occipital neuralgia. J Craniofac Surg. 2018;29(5):e518-e521. doi: 10.1097/scs.0000000000004549 [DOI] [PubMed] [Google Scholar]
- 34.Blume HG, Ungar-Sargon J. Neurosurgical treatment of persistent occipital myalgia-neuralgia syndrome. CRANIO®. 1986;4(1):65-73. doi: 10.1080/08869634.1986.11678132 [DOI] [Google Scholar]
- 35.Dubuisson D. Treatment of occipital neuralgia by partial posterior rhizotomy at C1–3. J Neurosurg. 1995;82(4):581. doi: 10.3171/jns.1995.82.4.0581 [DOI] [PubMed] [Google Scholar]
- 36.Jansen J. Surgical treatment of cervicogenic headache. Cephalalgia. 2008;28(Suppl 1):41-44. doi: 10.1111/j.1468-2982.2008.01620.x [DOI] [PubMed] [Google Scholar]
- 37.Li F, Ma Y, Zou J, et al. Micro-surgical decompression for greater occipital neuralgia. Turk Neurosurg. 2012;22(4):427-429. doi: 10.5137/1019-5149.Jtn.5234-11.1 [DOI] [PubMed] [Google Scholar]
- 38.Ducic I, Felder JM, 3rd, Janis JE. Occipital artery vasculitis not identified as a mechanism of occipital neuralgia-related chronic migraine headaches. Plast Reconstr Surg. 2011;128(4):908-912. doi: 10.1097/PRS.0b013e3182174229 [DOI] [PubMed] [Google Scholar]
- 39.Filipović B, de Ru JA, Hakim S, van de Langenberg R, Borggreven PA, Lohuis PJFM. Treatment of frontal secondary headache attributed to supratrochlear and supraorbital nerve entrapment with oral medication or Botulinum toxin type A versus endoscopic decompression surgery. JAMA Facial Plast Surg. 2018;20(5):394-400. doi: 10.1001/jamafacial.2018.0268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Caruana G, Bertozzi N, Boschi E, Pio Grieco M, Grignaffini E, Raposio E. Endoscopic forehead surgery for migraine therapy personal technique. Ann Ital Chir. 2014;85(6):583-586. Published 2015/02/26. [PubMed] [Google Scholar]
- 41.Lin SH, Lin HC, Jeng CH, Hsieh CH, Lin YH, Chen CC. Experience of surgical treatment for occipital migraine in Taiwan. Ann Plast Surg. 2016;76(Suppl 1):S80-S84. doi: 10.1097/sap.0000000000000697 [DOI] [PubMed] [Google Scholar]
- 42.Chepla KJ, Oh E, Guyuron B. Clinical outcomes following supraorbital foraminotomy for treatment of frontal migraine headache. Plast Reconstr Surg. 2012;129(4):656e-662e. doi: 10.1097/PRS.0b013e3182450b64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Economides JM, DeFazio MV, Attinger CE, Barbour JR. Prevention of painful neuroma and phantom limb pain after transfemoral amputations through concomitant nerve coaptation and collagen nerve wrapping. Neurosurgery. 2016;79(3):508-513. doi: 10.1227/neu.0000000000001313 [DOI] [PubMed] [Google Scholar]
- 44.Clarke C, Lindsay DR, Pyati S, Buchheit T. Residual limb pain is not a diagnosis: a proposed algorithm to classify postamputation pain. Clin J Pain. 2013;29(6):551-562. doi: 10.1097/AJP.0b013e318261c9f9 [DOI] [PubMed] [Google Scholar]
- 45.Dumanian GA, Potter BK, Mioton LM, et al. Targeted muscle reinnervation treats neuroma and phantom pain in major limb amputees: a randomized clinical trial. Ann Surg. 2019;270(2):238-246. doi: 10.1097/sla.0000000000003088 [DOI] [PubMed] [Google Scholar]
- 46.Toia F, Giesen T, Giovanoli P, Calcagni M. A systematic review of animal models for experimental neuroma. J Plast Reconstr Aesthet Surg. 2015;68(10):1447-1463. doi: 10.1016/j.bjps.2015.05.013 [DOI] [PubMed] [Google Scholar]
- 47.Leuzzi S, Armenio A, Leone L, et al. Repair of peripheral nerve with vein wrapping. G Chir. 2014;35(3-4):101-106. https://pubmed.ncbi.nlm.nih.gov/24841688, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4321586/. [PMC free article] [PubMed] [Google Scholar]
- 48.Ducic I, Felder JM III, Khan N, Youn S. Greater occipital nerve excision for occipital neuralgia refractory to nerve decompression. Ann Plast Surg. 2014;72(2):184-187. doi: 10.1097/SAP.0b013e3182898736 [DOI] [PubMed] [Google Scholar]
- 49.Forootan NS S, Lee M, Guyuron B. Migraine headache trigger site prevalence analysis of 2590 sites in 1010 patients. J Plast Reconstr Aesthet Surg. 2017;70(2):152-158. 10.1016/j.bjps.2016.11.004 [DOI] [PubMed] [Google Scholar]
- 50.Guyuron B, Kriegler J, Davis J, Amini S. Comprehensive surgical treatment of migraine headaches. Plast Reconstr Surg. 2005;115(1):1-9. [PubMed] [Google Scholar]
- 51.Ascha M, Kurlander DE, Sattar A, Gatherwright J, Guyuron B. In-depth review of symptoms, triggers, and treatment of occipital migraine headaches (site IV). Plast Reconstr Surg. 2017;139(6):e1333-e1342. doi: 10.1097/PRS.0000000000003395 [DOI] [PubMed] [Google Scholar]
- 52.Afifi AM, Carbullido MK, Israel JS, Sanchez RJ, Albano NJ. Alternative approach for occipital headache surgery: the use of a transverse incision and “W” flaps. Plast Reconstruct Surg – Global Open. 2019;7(4):e2176. doi: 10.1097/GOX.0000000000002176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gfrerer L, Maman DY, Tessler O, Austen WG, Jr. Nonendoscopic deactivation of nerve triggers in migraine headache patients: surgical technique and outcomes. Plast Reconstr Surg. 2014;134(4):771-778. doi: 10.1097/prs.0000000000000507 [DOI] [PubMed] [Google Scholar]
- 54.Ducic I, Hartmann EC, Larson EE. Indications and outcomes for surgical treatment of patients with chronic migraine headaches caused by occipital neuralgia. Plast Reconstr Surg. 2009;123(5):1453-1461. doi: 10.1097/PRS.0b013e3181a0720e [DOI] [PubMed] [Google Scholar]
- 55.Janis JE, Barker JC, Javadi C, Ducic I, Hagan R, Guyuron B. A review of current evidence in the surgical treatment of migraine headaches. Plast Reconstr Surg. 2014;134(4 Suppl 2):131S-141S. doi: 10.1097/prs.0000000000000661. [DOI] [PubMed] [Google Scholar]
- 56.Chmielewski L, Liu MT, Guyuron B. The role of occipital artery resection in the surgical treatment of occipital migraine headaches. Plast Reconstr Surg. 2013;131(3):351e-356e. doi: 10.1097/PRS.0b013e31827c6f71 [DOI] [PubMed] [Google Scholar]
- 57.Ryu JH, Shim JH, Yeom JH, Shin WJ, Cho SY, Jeon WJ. Ultrasound-guided greater occipital nerve block with botulinum toxin for patients with chronic headache in the occipital area: a randomized controlled trial. Korean J Anesthesiol. 2019;72(5):479-485. doi: 10.4097/kja.19145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Dilli E, Halker R, Vargas B, et al. Occipital nerve block for the short-term preventive treatment of migraine: a randomized, double-blinded, placebo-controlled study. Cephalalgia. 2014;35(11):959-968. doi: 10.1177/0333102414561872 [DOI] [PubMed] [Google Scholar]
- 59.Ashkenazi A, Matro R, Shaw JW, Abbas MA, Silberstein SD. Greater occipital nerve block using local anaesthetics alone or with triamcinolone for transformed migraine: a randomised comparative study. J Neurol, Neurosurg. Psychiatry. 2008;79(4):415-417. doi: 10.1136/jnnp.2007.124420 [DOI] [PubMed] [Google Scholar]
- 60.Cohen SP, Peterlin BL, Fulton L, et al. Randomized, double-blind, comparative-effectiveness study comparing pulsed radiofrequency to steroid injections for occipital neuralgia or migraine with occipital nerve tenderness. Pain. 2015;156(12):2585-2594. doi: 10.1097/j.pain.0000000000000373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Peled ZM, Pietramaggiori G, Scherer S. Anatomic and compression topography of the lesser occipital nerve. Plast Reconstruct Surg Global Open. 2016;4(3):e639-e639. doi: 10.1097/GOX.0000000000000654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Afifi AM, Carbullido MK, Israel JS, Sanchez RJ, Albano NJ. Alternative approach for occipital headache surgery: the use of a transverse incision and “W” flaps. Plast Reconstruct Surg – Global Open. 2019;7(4): e2176. doi: 10.1097/GOX.0000000000002176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kebede MM, Peters M, Heise TL, Pischke CR. Comparison of three meta-analytic methods using data from digital interventions on type 2 diabetes. Diabetes Metab Syndr Obes. 2018;12:59-73. doi: 10.2147/DMSO.S180106 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-psg-10.1177_22925503211036701 for Outcomes of Surgical Treatment of Migraines: A Systematic Review & Meta-Analysis by Adam G. Evans, Dorian S. Hill, Andrew E. Grush, Mauricio A. Downer, Maryo M. Ibrahim, Patrick E. Assi, Jeremy T. Joseph and Salam H. Kassis in Plastic Surgery