Abstract
Purpose:
Naturalistic developmental behavioral interventions (NDBIs) have demonstrated initial promise in facilitating social communication development for autistic toddlers, but their highly structured protocols may be a barrier toward their use by early intervention (EI) providers who must individualize intervention according to family-centered principles. This study aimed to characterize the extent to which EI speech-language pathologists (SLPs) use NDBI strategies, and the range of skills and behaviors addressed during their EI sessions, to contextualize the role of NDBIs within the scope of needs of families with autistic children in EI.
Method:
This observational study included 25 families with an autistic toddler and their EI SLP. One home-based session was recorded for each family, and an observational measure was used to describe SLPs' NDBI strategy use. Qualitative content analyses were also used to characterize the strategies SLPs recommended to families, and the child skills and behaviors they discussed.
Results:
SLPs did not implement NDBI strategies with high quality, but they implemented developmental NDBI strategies with significantly higher quality than behavioral NDBI strategies. SLPs discussed many strategies and skills across disciplines within the session.
Conclusions:
SLPs may require further training to implement NDBI strategies, but given the breadth and depth of skills addressed during sessions, researchers should investigate and report on the impact of NDBIs on a wider range of communication skills and developmental domains. This will facilitate clinical decision making and make these interventions better aligned with family-centered EI principles.
Supplemental Material:
Intervention programs in the naturalistic developmental behavioral intervention (NDBI; Schreibman et al., 2015) framework demonstrate promising outcomes in improving social communication outcomes for autistic toddlers in clinical trials (Sandbank et al., 2020; Tiede & Walton, 2019), but these interventions have not been widely disseminated in clinical practice. NDBIs combine strategies from intervention paradigms that have long been within the scope of practice of speech-language pathologists (SLPs; (American Speech-Language-Hearing Association, n.d.), raising the possibility that components of NDBIs are already in widespread use by SLPs serving autistic toddlers in community early intervention (EI) settings. However, EI providers report that some common procedures of manualized and highly structured NDBIs may be incompatible with their clinical obligation to individualize goals and strategies for the families they serve in EI (Pickard et al., 2021). Understanding how community-based EI SLPs utilize NDBI components and address the unique, varied needs of individual families is critical to optimizing both the design and dissemination of NDBI programs. This study will take a first step toward that goal by characterizing (a) the level of fidelity with which NDBI strategies are implemented by untrained community-based EI SLPs, (b) the activities and strategies they recommend to caregivers, and (c) the specific skills and behaviors discussed by caregivers and SLPs during their EI sessions.
NDBIs fuse principles from developmental and behavioral intervention paradigms within naturalistic contexts to facilitate the development of social communication skills along expected developmental trajectories (Schreibman et al., 2015). Developmental strategies are based on constructivist and social-interactionist theories of development (Piaget, 1952; Vygotsky, 1962, 1978) and focus on creating engaging, child-led, language-rich interactions from which children may learn new skills (e.g., modeling salient language, following the child's lead). Behavioral communication strategies in NDBIs derive from behaviorism, with clinicians using adult-led teaching episodes with three-part contingencies (antecedent-response-consequence) to elicit child communication skills and reinforce the child based on their response to the elicitation episode (e.g., communication temptations, prompting hierarchies), for example, prompting the child to “say ball” (antecedent) and waiting for them to say “ball” (response) before giving them the ball (consequence). Individual NDBI programs integrate these strategies in different ways, but common to all NDBI programs is that intervention procedures are manualized, with strategies to be implemented in the prescribed order and with a high level of fidelity (e.g., at the specified level of quality and quantity) when implemented by clinicians and/or caregivers (Schreibman et al., 2015). Despite the robust theoretical foundation and empirical support for NDBIs, clinician beliefs about the effectiveness of developmental and behavioral strategies and their need to provide family-centered intervention may prevent NDBIs from being utilized as designed.
Clinicians across disciplines working with autistic toddlers report that they value and use developmental strategies more frequently than behavioral strategies, suggesting that the intentional integration of strategies critical to NDBI programs may not occur in clinical practice. When asked to rank NDBI-aligned strategies by their perceived effectiveness, early childhood educators ranked many behavioral strategies lower than developmental strategies (Maye et al., 2020), and EI providers have also reported more frequent use of many developmental strategies than behavioral strategies (Pickard et al., 2021), suggesting that behavioral strategies may not be used frequently in clinical practice. However, only EI provider report of behavioral strategies was associated with increased self-competence in using NDBI programs (Pickard et al., 2021), indicating that the use of behavioral strategies may be critical to proper implementation of NDBI programs by community-based EI providers. Because high-quality strategy use may be critical for improving child outcomes (Wainer & Ingersoll, 2013), there is a great need for objective measures to characterize the quality of individual NDBI strategy implementation, and the extent to which behavioral and developmental strategies are used in an integrated manner by community-based EI providers.
Discrepancies between the outcomes targeted by NDBI programs as reported in clinical trials and by EI SLPs in clinical practice may present a barrier toward NDBI implementation in community settings. Although SLPs are trained to use expected developmental trajectories to facilitate goal-setting, as is the case in manualized NDBIs, EI clinicians must integrate family-centered practices in which they choose intervention strategies and goals based on family preferences and existing parenting practices (Dunst & Espe-Sherwindt, 2016; Individuals with Disabilities Education Improvement Act, 2004). Thus, EI SLPs should collaborate with caregivers to create functional, participation-based goals that target the child's communication in natural contexts of importance to the family. Research studies for young children with communication difficulties often report activity-based outcomes (Kwok et al., 2022), such as change on a standardized communication measure collected in a research setting. This difference in the nature of the targets in clinical practice (i.e., participation in life routines) and the outcomes reported in research (i.e., performance on standardized measures) raises the possibility that NDBIs do not adequately address communication during functional, family-centered goals. Furthermore, autistic children often experience difficulties in many domains of development and functioning (e.g., sleep, emotional and sensory regulation; Aranbarri et al., 2021), and EI providers may need to help families gain access to information to best support children in these domains. A greater understanding of the skills, behaviors, and developmental domains discussed by caregivers and EI SLPs will elucidate the role of NDBIs in addressing the wide range of needs EI providers must address with their autistic clients and their families, and may facilitate the use of more clinically relevant outcome measures to be used in future studies.
Lastly, the attenuated communication outcomes for autistic toddlers receiving intervention in community settings as opposed to clinical trials (Nahmias et al., 2019) highlight the need to disseminate evidence-based interventions to community-based providers. However, it is possible that the outcomes measured in research settings do not adequately address the goals EI SLPs are expected to target and that the intervention procedures are not always feasible to implement in current clinical practice. This study uses qualitative content analyses to identify the strategies and outcomes discussed by community-based SLPs and caregivers during their EI sessions to better understand both the structure of these sessions and the scope of skills targeted by EI SLPs. Such knowledge is essential for understanding how to practically translate the procedures of tightly controlled NDBI efficacy trials into clinical practice. Additionally, this study will be the first to use observational measures to characterize NDBI strategy usage by community-based EI providers, building upon prior work of self-reported frequency of strategy use. Such an approach will characterize the skillfulness (i.e., quality and quantity) with which these strategies are implemented as intended by manualized NDBIs in the community, which is essential for understanding the effectiveness of community-based services and ways that these services may be improved. Together, this information will help bridge the gap between research and clinical practice and facilitate the optimal design of NDBIs for widespread implementation and dissemination. The following questions guided this study:
Research Question 1: To what extent are SLPs observed to use NDBI strategies with the degree of skillfulness (i.e., quality and quantity) considered ideal in manualized NDBIs, and with what frequency do they report using NDBI strategies?
Research Question 2: To what extent do SLPs differ in their observed degree of skillfulness (i.e., quality and quantity) in implementing developmental and behavioral NDBI strategies as intended in manualized NDBIs?
Research Question 3: What strategies and activities do SLPs advise caregivers to use during their EI sessions?
Research Question 4: What child behaviors, skills, and developmental domains are discussed by SLPs and caregivers during their sessions?
Method
Procedure
Video recordings of home-based EI speech-language therapy sessions were collected for 25 families with an autistic toddler enrolled in Illinois EI speech-language therapy services and their EI SLP. Families were recruited from a clinical trial of a caregiver-implemented intervention for autistic toddlers (NCT02632773) and provided the contact information for their EI SLP who was then approached by a member of the research team about participation in this study. Informed consent for all participants was obtained online or over the phone and verified in writing, and one EI session was recorded for each SLP–family dyad. Caregivers and SLPs also completed surveys via Research Electronic Data Capture (Harris et al., 2009, 2019); only SLP surveys were utilized in this study (see Lee et al., 2022, for additional study details). All procedures were approved by Northwestern University's institutional review board.
Participants
A total of 22 SLPs and 25 families participated in this study (three SLPs worked with two participating families); surveys about demographics and therapeutic approach were completed by 21 SLPs. Most SLPs were White (17 SLPs; 77.3%) and female (19; 86.3%), and worked primarily in the EI setting (18; 81.8%). SLPs had worked with the family participants for an average of 6.6 months (SD = 4.2) at the time of study participation. SLPs reported working with an average of 5.1 autistic toddlers (SD = 2.6) and 13.7 toddlers with language disorders and no co-occurring diagnosis (SD = 8.7) at the time of study participation. No SLPs reported receiving training in any manualized NDBI (i.e., Joint Attention, Symbolic Play, Engagement, and Regulation [JASPER; Kasari et al., 2015]; Early Start Denver Model [Dawson et al., 2010; Pivotal Response Training [Koegel et al., 1999]; Social Communication, Emotional Regulation, and Transactional Support/Early Social Interaction [Prizant et al., 2003; Wetherby et al., 2014], Enhanced Milieu Teaching [Kaiser et al., 2000]; or other NDBIs). Child participants included 18 boys and seven girls and had a mean age of 31.6 months (SD = 4.0). Many family participants spoke a language other than English in the home (11; 52.4%), and most caregivers had a college or graduate degree (mothers: 15, 60%; fathers: 11, 44%). See Table 1 for additional demographic information.
Table 1.
Participant demographics.
| Family characteristics (n = 25) | |||
|---|---|---|---|
| Child | Mother | Father | |
| Gender n [%] | |||
| Female | 7 (28%) | ||
| Male | 18 (72%) | ||
| Race n [%] | |||
| Asian | 3 (12%) | 3 (12%) | 3 (12%) |
| Black | 2 (8%) | 1 (4%) | 2 (8%) |
| Native Hawaiian/Pacific Islander | 0 (0%) | 1 (4%) | 0 (0%) |
| White | 16 (64%) | 17 (68%) | 18 (72%) |
| More than one race | 2 (8%) | 1 (4%) | 0 (0%) |
| Prefer not to answer | 2 (8%) | 2 (8%) | 2 (8%) |
| Ethnicity n [%] | |||
| Hispanic or Latino | 8 (32%) | 5 (20%) | 7 (28%) |
| Not Hispanic or Latino | 16 (64%) | 19 (76%) | 16 (64%) |
| Prefer not to answer/unknown |
1 (4%) |
1 (4%) |
2 (8%) |
|
Speech-language pathologist characteristics (n = 21)
| |||
| Gender n [%] | |||
| Female | 19 (90.5%) | ||
| Male | 2 (9.5%) | ||
| Race n [%] | |||
| Asian | 2 (9.5%) | ||
| Black | 1 (4.8%) | ||
| White | 17 (81.0%) | ||
| More than one race | 1 (4.8%) | ||
| Years employed in early intervention n [%] | |||
| < 2 | 5 (23.8%) | ||
| 3–5 | 5 (23.8%) | ||
| 6–10 | 6 (28.6%) | ||
| More than 10 | 5 (23.8%) | ||
| Primary work setting n [%] | |||
| Early intervention | 19 (90.5%) | ||
| Preschool, elementary to high school | 1 (4.8%) | ||
| Private clinic | 1 (4.8%) | ||
Measures
Naturalistic Developmental Behavioral Intervention-Fidelity Rating Scale
The Naturalistic Developmental Behavioral Intervention–Fidelity Rating Scale (NDBI-Fi; Frost et al., 2020; Sone et al., 2021) was used to characterize the extent to which SLPs implemented individual NDBI strategies, as intended by manualized NDBI programs, during the recorded sessions. Although individual NDBI programs may vary in their use of specific strategies, the NDBI-Fi was designed to measure the common characteristics of these programs as operationally defined via consensus with NDBI researchers. It has demonstrated positive correlations with multiple NDBI programs (r = 0.60; Frost et al., 2020), indicating strong construct validity, and has also demonstrated high interrater reliability (interclass correlation coefficient [ICC] = .80; Frost et al., 2020). The authors of the NDBI-Fi use the term fidelity to describe the quality and quantity of clinician strategy use, but because “fidelity” is often used to describe the implementation of an entire intervention program (including total dosage, social validity, and other intervention components; Edmunds et al., 2022), here we use the term skillfulness to refer to the extent to which SLPs implement NDBI strategies with the quality and quantity considered “ideal” according to manualized NDBIs.
The NDBI-Fi is an observational rating scale consisting of nine items rated on a 5-point ordinal scale, with six items measuring developmental strategies (e.g., modeling appropriate language) and three items related to behavioral strategies (e.g., communication temptations; see Table 2 for a full list of strategies included on the NDBI-Fi, and Supplemental Material S3 for the full measure including quality and quantity indicators for the ratings). The NDBI-Fi has been validated to measure NDBI strategy use during interactions between caregivers and their autistic child (Frost et al., 2020; Sone et al., 2021) and was slightly adapted to capture SLP strategy use during EI sessions (i.e., accounting for the sometimes-triadic nature of EI sessions, such as when caregivers and SLPs jointly interacted with the child).
Table 2.
Strategies included on the NDBI-Fi.
| Strategy | Description |
|---|---|
| Behavioral strategoes | |
| Communication temptations | The SLP elicits child communication by arranging the environment, such as violating their expectations in a familiar routine, putting desired objects out of reach, or giving them toys that require assistance to operate. They should wait for the child to respond to the elicitation episode and may initiate a direct teaching episode if the child does not respond with the targeted skill. |
| Frequency of direct teaching | The SLP encourages the child to use a targeted skill using some sort of verbal prompt (e.g., say prompts, open questions, choice questions). Prompts must include instruction from the SLP, a child response, and reinforcement from the SLP to be considered a direct teaching episode. |
| Quality of direct teaching | Direct teaching episodes (a) are clear, (b) elicit a communication skill at or just above the child's developmental level, (c) are used when the child is motivated and interested in the object/action for which the SLP is prompting, (d) include scaffolding to support a correct response if the child does not initially respond with the prompted skill, and (e) end with the provision of reinforcement that is natural and appropriate to the activity. |
| Developmental strategies | |
| Face-to-face and on the child's level | The SLP is facing the child at a similar level within the child's line of sight. Toys and objects should be between the SLP and the child when possible. |
| Follow the child's lead | The child chooses activities, how long to stay in each activity, and how to play during each activity, with the SLP having an active role and honoring the child's interests and disinterests. The SLP may provide options for new activities/play actions but does not force the child to follow along. |
| Positive affect and animation | The SLP uses an upbeat and encouraging tone, facial expressions, and overall affect matched to the child's sensory and engagement needs. |
| Modeling appropriate language | The SLP uses utterances at or just above the child's developmental level and limits their use of questions and directions. Language should be topically contingent to the child's focus of attention. |
| Responding to child communication | The SLP responds to the child's communication attempts in a timely manner. They should respond to all forms of communication (e.g., vocalizations, words, gestures, eye gaze) and treat this communication as meaningful. If the child is not communicating, the SLP should imitate the child's actions and label them with topically contingent comments. |
| Pace of verbal models a | The SLP pauses between conversational turns to allow the child an opportunity to communicate, waiting at least 3 s before taking another verbal turn. |
Note. NDBI-Fi = Naturalistic Developmental Behavioral Intervention–Fidelity Rating Scale (Frost et al., 2020); SLP = speech-language pathologist.
Item added in Sone et al. (2021).
Guidelines were also created to isolate segments of the entire recorded session (mean session length: 60.0 min, SD = 7.6) that were appropriate for coding (i.e., when the SLP actively interacted with the child). Coders watched the entire session video, marking time stamps of continuous 5-min segments of active SLP–child interaction to extract for coding. Portions of the video were not included in a rated segment if (a) the SLP and caregiver spoke for a consecutive 30 s, (b) the caregiver and SLP spoke for a cumulative 1.5 min throughout a 5-min period, (c) the SLP only observed the parent and/or child, or (d) the SLP was not actively interacting with the child (e.g., passively handed them toys while focusing on a conversation with the caregiver or writing their session note). Therefore, an average of 7.28, 5-min segments (SD = 3.09) were rated with the NDBI-Fi for each SLP (range: 1–11). See Supplemental Material S3 for more information about the application of segmenting guidelines.
Coders included two doctoral student SLPs and one clinical master's student in speech-language pathology. Training consisted of reviewing the coding manual and rating a standard set of videos to reliability criteria established in previous studies (Sone et al., 2021). These criteria included rating three consecutive segments with (a) seven items rated within 1 point of the primary codes, (b) no items rated greater than 2 points apart, and (c) overall mean scores within 0.5 points. Ongoing reliability was also conducted on all rated segments in six session videos (24% of recorded sessions, 26.3% of total segments), with coders reaching acceptable to excellent levels of reliability (item-level ICC: .736–.99). Reliability coders also verified appropriate segmenting of the recorded sessions; there were no disagreements in the accuracy of segmenting guidelines across videos.
Therapeutic Approach Survey
SLPs completed a survey created by the research team to gather information about the strategies used during the recorded session. SLP participants selected the strategies they used during the session from a list of 27 strategies that are commonly used in EI and autism-specific interventions. Two members of the research team who are licensed EI SLPs reviewed websites and materials that SLPs commonly consult for intervention advice to identify commonly used strategies and terminology to use on the survey. SLPs were also given the option to write in strategies that were not represented on the checklist, but no SLPs wrote in other strategy options. Twelve strategies on this list were in line with developmental strategies that may be used in NDBIs (e.g., mirroring and mapping, matched turns), seven aligned with behavioral strategies that are often used in NDBIs (e.g., prompting, sabotage), and eight strategies are commonly used by SLPs in EI populations but are not specifically part of NDBI programs; many of these strategies may be used within the context of developmental or behavioral communication strategies (e.g., visual supports, speech-generating devices). Surveys were completed by SLPs following 23 of the 25 recorded sessions (92%).
Qualitative Coding
Qualitative content analyses were conducted on all recorded sessions to characterize the strategies and activities that SLPs advised caregivers to use (Research Question 3) as well as the skills and behaviors discussed by caregivers and SLPs (Research Question 4). All caregiver–SLP conversations were transcribed and imported into NVivo (QSR International Pty Ltd., 2020) for analysis. Qualitative coding was conducted by Authors 1, 2, and 3, all of whom are licensed SLPs with experience working in EI (see Acknowledgments for more information on authors' positionality). An inductive approach was used to create the coding manual for each research question, with coders reviewing all transcripts and videos to create initial codes using the session's manifest content (i.e., the words and actions observed in the video, as opposed to the coders' interpretation of the underlying intention of these observed behaviors). The coding manuals were iteratively updated following review of the codes with the transcripts until a final list of 28 unique strategies/activities were identified for Research Question 3, and 30 skills/domains were observed for Research Question 4. All transcripts were coded by Author 1 and either Author 2 or 3, with coders reaching high levels of reliability; percent agreement for each code in Research Question 3 ranged from 96.3% to 100% and 93.9% to 100% for Research Question 4. All discrepancies were resolved via consensus discussions by the two coders, resulting in 100% final agreement. The authors then categorized the final codes into categories to facilitate interpretation of the results.
Analysis
To characterize SLPs' observed use of NDBI strategies, mean scores for each item on the NDBI-Fi were calculated across segments in the recorded session to create an average score for each SLP. Segment scores were combined across sessions for the three SLPs who worked with two families in the study. If an SLP did not use a communication temptation or teaching episode (behavioral NDBI strategies) in a rated segment, they were rated “N/A” on the NDBI-Fi, and all N/As were converted to zeros for analysis; thus, the lowest possible score for behavioral strategies is a 0 and, for developmental strategies, a 1 (maximum scores for both strategy types was a 5). Mean scores were calculated for the six developmental strategies and the three behavioral strategies for each SLP, and a one-sample t test was used to explore the difference in SLPs' observed use of developmental and behavioral strategies. The total number of strategies reported to be used by SLPs during the recorded session was also summarized based on the therapeutic approach survey to identify common strategies; self-reported use of developmental and behavioral strategies was not directly compared due to differences in the number of developmental and behavioral strategies included on the therapeutic approach survey. For the qualitative analyses, the number of sessions in which each code was present was reported. Qualitative codes were not combined across sessions for the SLPs serving two families in the study to reflect the family-specific nature of these discussions, and therefore, the total number of sessions for qualitative analyses was 25.
Results
Research Question 1: SLPs' Observed and Reported Use of NDBI Strategies
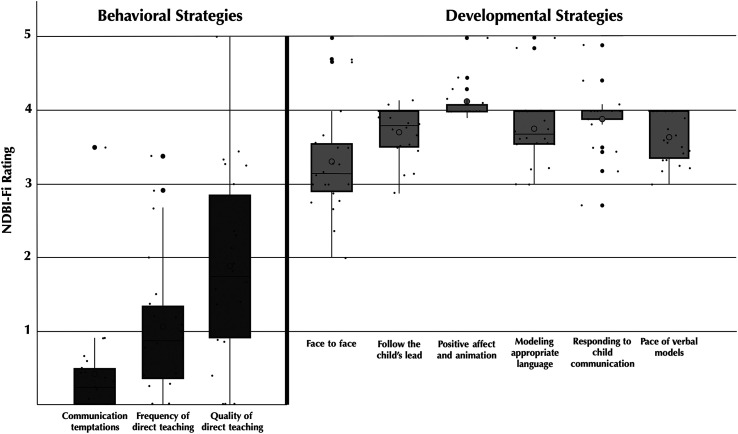
Overall NDBI-Fi scores across SLPs in the recorded session did not reach common standards of high-level skillfulness of strategy implementation (often conceptualized as 80% accuracy, or at least 4 out of 5 points on the NDBI-Fi; Perepletchikova & Kazdin, 2005), but there was great variation in the average skillfulness of individual strategies measured on the NDBI-Fi. Overall average NDBI-Fi scores were 2.9 out of a possible 5 points (SD = 0.4, range: 2.2–3.8). SLPs scored highest on the strategy “positive affect and animation” (M = 4.1, SD = 0.3), followed by “responding to child communication” (M = 3.9, SD = 0.4), “modeling appropriate language” (M = 3.8, SD = 0.5), “follow the child's lead” (M = 3.7, SD = 0.3), “pace of verbal models” (M = 3.6, SD = 0.3), “face to face” (M = 3.3, SD = 0.7), “quality of direct teaching” (M = 1.9, SD = 1.3), “frequency of direct teaching” (M = 1.1, SD = 0.9), and “communication temptations” (M = 0.4, SD = 0.8). Figure 1 displays NDBI-Fi scores for individual NDBI-Fi strategies.
Figure 1.
Observed levels of skillfulness of individual naturalistic developmental behavioral intervention (NDBI) strategies by speech-language pathologists (SLPs). SLPs implemented developmental strategies at significantly higher levels of skillfulness than behavioral strategies, according to ideal NDBI strategy standards as defined on the NDBI-Fi. Average scores across SLPs did not reach high levels of skillfulness traditionally used in clinical trials (i.e., 4 out of 5 points on the NDBI-Fi), although many SLPs did reach this threshold on individual developmental strategies. NDBI-Fi = Naturalistic Developmental Behavioral Intervention–Fidelity Rating Scale (Frost et al., 2020).
On the therapeutic approach survey, SLPs across the sample reported using a total of 24 different language facilitation strategies, with an average of 9.4 strategies reported in a single session (SD = 4.2). All SLPs reported using at least one NDBI strategy, and SLPs in 16 sessions (69.6%) used at least one strategy that did not fall under the NDBI framework, with the most common non-NDBI strategy used being sign language (12 out of 23 sessions, 52.2%). The most frequently reported strategies were following the child's lead (20 sessions, 87.0%), modeling target language (17 sessions, 73.9%), prompting (16 sessions, 69.6%), and language expansions (16 sessions, 69.6%). See Table 3 for the reported frequency of each strategy included on the therapeutic approach survey.
Table 3.
Self-reported strategy use.
| Strategy | Number of sessions (%) |
|---|---|
| Following the child's lead a | 20 (87.0%) |
| Modeling target language a | 17 (73.9%) |
| Prompting b | 16 (69.6%) |
| Language expansions a | 16 (69.6%) |
| Reduced length of utterance a | 14 (60.9%) |
| Verbal imitation a | 14 (60.9%) |
| Communication temptation b | 14 (60.9%) |
| Parallel talk a | 13 (56.5%) |
| Sign language | 12 (52.2%) |
| Notice and respond a | 12 (52.2%) |
| Self-talk a | 11 (47.8%) |
| Observe, wait, listen a | 10 (43.5%) |
| Sabotage b | 7 (30.4%) |
| Mirroring and mapping a | 7 (30.4%) |
| Verbal imitation hierarchy b | 6 (26.1%) |
| Visual supports | 5 (21.7%) |
| Auditory bombardment | 5 (21.7%) |
| Matched turns a | 4 (17.4%) |
| Recasting a | 4 (17.4%) |
| Environmental arrangement b | 3 (13.0%) |
| Functional communication training | 2 (8.7%) |
| Word affect action | 2 (8.7%) |
| Build up, break down | 1 (4.3%) |
| Speech-generating device | 1 (4.3%) |
| Pacing boards | 0 (0%) |
| Oral motor exercises | 0 (0%) |
| Drill work | 0 (0%) |
| Other | 0 (0%) |
Note. Surveys were completed following 23 out of 25 sessions (92%).
A developmental naturalistic developmental behavioral intervention (NDBI) strategy.
A behavioral NDBI strategy.
Research Question 2: Differences Between Developmentally and Behaviorally Derived NDBI Strategies
Developmental strategies were used with greater degrees of skillfulness than behavioral strategies during the recorded sessions. NDBI-Fi ratings for developmental strategies (M = 3.7, SD = 0.3) were significantly higher than ratings for behavioral strategies (M = 1.1, SD = 0.9; t = 12.5, p < .00; t = 12.5, p < .00), with a large effect (Cohen's d = 4.1). Of note, four SLPs (19%) were never observed to use any behavioral strategy in the recorded session.
Research Question 3: Strategies and Activities SLPs Advise Caregivers to Use
The results of the qualitative content analysis for Research Question 3 are reported in Table 4 (see Supplemental Material S1 for a codebook with full definitions of each code). A total of 28 unique strategies and activities were identified in the recorded sessions, with strategies falling into six primary categories. SLPs most frequently recommended strategies and activities that are intended to support communication and interactions (“communication supports,” 13 sessions, 52%), followed by developmental strategies (12 sessions, 48%), behavioral strategies (10 sessions, 40%), strategies targeting emotional/sensory regulation and challenging behaviors (eight sessions, 32%), other activities (seven sessions, 28%), and strategies to support sibling interactions (three sessions, 12%). Notably, SLPs in eight sessions (32%) did not recommend or coach caregivers to use any strategies or activities during the recorded session. Of the sessions in which SLPs did recommend or coach caregivers to use strategies (17 sessions, 68%), SLPs recommended an average of 5.76 strategies (SD = 3.88) from 3.11 categories (SD = 1.32) during a single session.
Table 4.
What strategies and activities do speech-language pathologists advise caregivers to use during their early intervention sessions?
| Code | Number of sessions (%) |
|---|---|
| Developmental strategies | 12 (48%) |
| Model salient language | 8 (32%) |
| Follow the child's lead | 7 (28%) |
| Play expansions | 5 (20%) |
| Take conversational turns | 3 (12%) |
| Label own action | 3 (12%) |
| Mirroring and mapping | 3 (12%) |
| Reduced length of utterance | 2 (8%) |
| Reduce questions | 2 (8%) |
| Notice and respond to communication | 1 (4%) |
| Behavioral strategies | 10 (40%) |
| Time delay | 7 (28%) |
| Prompt | 5 (20%) |
| Environmental arrangement | 3 (12%) |
| Offer choices | 1 (4%) |
| Communication supports | 13 (52%) |
| Visual/tactile/nonverbal cues | 8 (32%) |
| Model specific word/word types | 7 (28%) |
| Use sign language | 3 (12%) |
| Pause to give child processing time | 2 (8%) |
| Use PECS | 2 (8%) |
| Emotional/sensory regulation, challenging behavior | 8 (32%) |
| Use sensory activities | 6 (24%) |
| Small, contained spaces | 3 (12%) |
| Give child space/time alone | 2 (8%) |
| Use specific toys/activities of interest | 1 (4%) |
| Identify antecedents of behavior | 1 (4%) |
| Sibling interaction strategies | 3 (12%) |
| Find activities both siblings enjoy | 2 (8%) |
| Model language for target child | 2 (8%) |
| Model language for sibling | 2 (8%) |
| Other sibling strategy | 2 (8%) |
| Other strategies | 7 (28%) |
Note. N = 25 sessions. PECS = Picture Exchange Communication System.
Research Question 4: Child Skills, Behaviors, and Developmental Domains Discussed by SLPs and Caregivers
A total of 30 specific behaviors, skills, and developmental domains were identified during caregiver–SLP conversations in the recorded sessions across five broader categories (see Table 5 for full results and Supplemental Material S1 for a codebook with full definitions of each code). The most frequently discussed areas were spoken language (20 sessions, 80%), play (20 sessions, 80%), EI/preschool logistics (19 sessions, 76%), and emotional regulation/challenging behavior (19 sessions, 76%). Additionally, SLPs and caregivers discussed an average of 11.16 skills (SD = 4.82) in each session. Please see Supplemental Material S2 to see each SLP's observed NDBI-Fi scores alongside the strategies and goals they discussed during recorded sessions.
Table 5.
Child behaviors, skills, and developmental domains discussed by speech-language pathologists and caregivers.
| Code | Number of sessions (%) |
|---|---|
| Language and communication | 24 (96%) |
| Spoken language | 20 (80%) |
| Requesting | 16 (64%) |
| Gestures | 12 (48%) |
| Initiating interactions | 10 (40%) |
| Joint engagement | 10 (40%) |
| Eye contact | 9 (36%) |
| Questions | 9 (36%) |
| Articulation | 7 (28%) |
| Receptive language | 7 (28%) |
| Following directions | 7 (28%) |
| Echolalia | 7 (28%) |
| Sign language | 6 (24%) |
| Turn taking | 6 (24%) |
| Commenting | 3 (12%) |
| Other social communication | 6 (24%) |
| Play and cognitive skills | 20 (80%) |
| Play | 20 (80%) |
| Attention | 8 (32%) |
| Problem solving | 5 (20%) |
| Family values/routines | 21 (84%) |
| EI/preschool logistics | 19 (76%) |
| Daily routines | 8 (32%) |
| Sibling interactions | 6 (24%) |
| Potty training | 3 (12%) |
| Other family values | 5 (20%) |
| Autism-related domains | 22 (88%) |
| Emotional regulation/challenging behavior | 19 (76%) |
| Sensory needs | 14 (56%) |
| Restricted/repetitive behaviors | 3 (12%) |
| Other domains | 19 (76%) |
| Preacademic skills | 10 (40%) |
| Sleep | 5 (20%) |
| Diet | 3 (12%) |
| Other | 17 (68%) |
Note. The skills included in “autism-related domains” are very frequently discussed within the context of autism but are also common in other developmental disabilities. EI = early intervention.
N = 25 sessions.
Discussion
This study aimed to characterize EI SLPs' use of NDBI strategies; the strategies and activities they recommend to families; and the skills, behaviors, and developmental domains targeted and discussed by SLPs and caregivers during home-based sessions with autistic toddlers. SLPs were not observed to use individual NDBI strategies with high degrees of skillfulness (i.e., quality and quantity) but used developmental strategies with significantly higher skillfulness than behavioral strategies. All SLPs reported using multiple strategies within a session, most of which were aligned with NDBI strategies. SLPs advised caregivers to use multiple strategies and activities within a single session and discussed many skills and behaviors across developmental domains and functional outcomes. These results illustrate the current use of NDBI strategies by EI SLPs and also contextualize the role of NDBIs within the scope of services provided by SLPs to families with an autistic toddler.
The observed levels of overall NDBI strategy use as well as the discrepancies in the skillfulness of developmental and behavioral strategy implementation are consistent with previous findings. Just as EI providers across disciplines have reported that they more frequently use and value developmental strategies (Maye et al., 2020; Pickard et al., 2021), EI SLPs in this study were observed to use developmental strategies with greater skillfulness than behavioral strategies on the NDBI-Fi. Although developmental strategies were used with relatively higher skillfulness than behavioral strategies, they were still not implemented at the level of skillfulness observed in clinical trials and considered necessary to improve child outcomes in efficacy trials of NDBIs using trained research staff. No SLPs reached the high skillfulness threshold (4 out of 5 points on the NDBI-Fi; Perepletchikova & Kazdin, 2005) in their overall NDBI-Fi scores or behavioral scores, and only five SLPs reached this threshold in their developmental strategy scores. This may explain why communication outcomes for autistic toddlers participating in clinical trials are greater than those for autistic toddlers receiving community-based interventions (Nahmias et al., 2019). The level of quality and quantity with which strategies must be implemented to impact specific child outcomes remains unclear, and it is likely that different children may require more or less support based on their specific communication profiles (Schreibman et al., 2015; Wainer & Ingersoll, 2013). However, these results suggest that SLPs and other EI providers may require further professional development to appropriately implement NDBI intervention strategies at high levels of fidelity with their autistic clients.
Because EI providers should choose intervention strategies based on caregivers' preferences and existing capacities, it is possible that SLPs avoided or adapted their use of some individual strategies to better suit family needs, contributing to low observed levels of skillfulness compared with NDBI standards and differences in the observed use of developmental and behavioral strategies. Behavioral strategies were rarely observed in this study, and emotional regulation was discussed in the majority of sessions. Latino/a caregivers, for example, have reported that some behavioral communication strategies contribute to child frustration (Cycyk & Huerta, 2020), raising the possibility that SLPs avoided using such strategies to better support child emotional regulation and to account for family preferences. Autistic adults and other supporters of the neurodiversity movement have also objected to the use of many behavioral strategies due to negative impacts on autistic individuals' autonomy and mental health (Sandoval-Norton & Shkedy, 2019), and it is therefore possible that SLPs avoided using behavioral strategies due to their personal beliefs or those of the family, contributing to the differences in observed developmental and behavioral strategy skillfulness (according to the NDBI-Fi) in this study.
Furthermore, SLPs in this study may have adapted their use of NDBI strategies to better address families' desired goals. For example, the strategy “modeling appropriate language,” as defined through expert consensus on the NDBI-Fi, requires that interventionists limit their use of questions and directions in favor of using comments. However, adult–child interaction norms vary across cultures (Tamis-LeMonda et al., 2012), and the use of certain question types has been associated with higher levels of specific communication skills (Rowe et al., 2017). Thus, SLPs may have intentionally used questions or directions to address caregiver-desired goals and match their interactional preferences, which resulted in lower scores on the NDBI-Fi. As a global rating scale, the NDBI-Fi combines quality and quantity indicators to rate the skillfulness of each item, and therefore, observations about the specific ways in which SLPs could improve their quality or quantity of individual strategies were not formally captured. Future studies should investigate caregiver acceptability of individual strategies, adaptations to quality and quantity that may be made to account for these preferences, and the impact this has on a wider range of intervention outcomes than those prioritized in current NDBI research.
SLPs advised caregivers to use a variety of strategies used to support communication development and discussed many discrete communicative skills and functions. SLPs also discussed many child skills and behaviors related to functional outcomes (e.g., sibling interactions) and other domains of development (e.g., sensory and emotional regulation, sleep). SLPs recommended many developmental and behavioral strategies aligned with NDBIs and discussed many skills that are targeted in NDBIs (e.g., spoken language, joint engagement), indicating the value that widespread training in NDBIs may have for EI SLPs. Additionally, the discussion of skills, behaviors, and strategies that are not traditionally thought to fall within the scope of practice of SLPs is not surprising given the clinical importance of coordinating care across disciplines in family-centered EI (Individuals with Disabilities Education Improvement Act, 2004; Sandall et al., 2000). Autistic toddlers often receive services from clinicians across disciplines (e.g., special educators, occupational therapists), and therefore, SLPs may implement strategies from other domains that support their communication-related intervention (e.g., using sensory strategies recommended by an occupational therapist to support the child's regulation as they use communication facilitation strategies). Furthermore, caregivers report difficulties supporting their child's development and functioning in many non–communication-related domains. For example, in a recent study of caregiver and provider needs in EI, over 80% of caregivers of autistic children reported concerns about their child's sleep, behavior, and sensory patterns (Aranbarri et al., 2021). Therefore, it is likely that SLPs in the current sample discussed such domains in order to best build caregiver capacities to support their child's needs.
Taken together, these results suggest that NDBIs are aligned with many components of clinical practice for EI SLPs, but there is a great need to consider how NDBIs may best complement existing intervention approaches and how clinicians may adjust their practice to achieve positive child outcomes observed in NDBI efficacy studies. SLPs advised caregivers to use multiple strategies and activities within a single session, in contrast to caregiver-implemented NDBIs that often teach caregivers individual strategies in predetermined sequences (e.g., Project ImPACT, Stadnick et al., 2015; JASPER, Kasari et al., 2015). SLPs in this study had worked with the participating family for an average of 6.4 months (SD = 4.2), raising the possibility that they had used a more targeted approach in earlier sessions. Given that these SLPs rarely used active teaching strategies when coaching caregivers (see Lee et al., 2022, for additional information about coaching practices used by SLPs in the current sample), it is likely that the focused training used in NDBIs did not occur with caregivers before the recorded session. EI providers in community settings infrequently use coaching strategies to actively teach caregivers (Sawyer & Campbell, 2017), and it is possible that more focused training, as that used in NDBIs, may facilitate provider use of such coaching strategies.
Additionally, whereas interventionists in clinical trials must focus on the outcomes of interest to the individual study and follow highly structured protocols to maintain high fidelity of overall intervention implementation, EI clinicians must be prepared to offer a wider range of support and guidance individualized to the needs and priorities of each family. This may reduce the session time used for direct child intervention, potentially limiting the effectiveness of intervention on child-related outcomes. However, using session time to address additional skills or areas of concern with caregivers may better support caregiver-related outcomes, which also have a downstream impact on child development and well-being (Trivette et al., 2010). Intentional investigation of the impact of communication-related NDBI strategies on multiple domains of development is critical to understanding the balance of caregiver and child outcomes of NDBIs in clinical practice.
Limitations
There are a few notable limitations in this study. First, the relatively small sample limits generalizability of these findings to other providers. However, consistencies between observed use of individual NDBI strategies and provider report in previous studies strengthen the validity of these observations, and these results point to specific areas that may be investigated on a larger scale as researchers prepare to disseminate NDBIs to community settings. Second, the study's focus on NDBIs limited observation of other language facilitation strategies that SLPs may have used during the session. For example, many SLPs in this study reported and recommended that caregivers use non-NDBI strategies to support the child's communication (e.g., sign language, nonverbal cues), but the quality with which they implemented such strategies was not observed in this study. It is possible that SLPs' use of other strategies may support or impede the effectiveness of developmental and behavioral NDBI strategies, which may be investigated more robustly in the future, particularly given that many of these strategies could be used with both developmental and behavioral NDBI strategies. Inconsistencies in the names of strategies between intervention programs may limit the accuracy of findings about self-reported strategy use. EI providers have reported that they use many strategies for which they do not have a specific name (Pickard et al., 2021), suggesting that SLPs may conceptualize the strategies included in the survey in different ways.
Furthermore, SLPs reported using some strategies they were not observed to use on the NDBI-Fi, pointing to differences in researcher and clinician strategy definitions that limited the observational measure's sensitivity to SLP strategy use. For example, coders observed SLPs using instructional cues without the expectation of a child response with a follow-up reward or instructional cue in many sessions (e.g., pointing to a picture in a book and not reprompting when the child fails to respond to the point). The NDBI-Fi requires a follow-up cue or reward based on the child response to the initial instruction for it to be considered instructional (i.e., a “direct teaching episode”), thus precluding actions that SLPs may consider to be prompts from being counted on the NDBI-Fi. Furthermore, SLPs advised caregivers to use some strategies they were not observed to use according to the NDBI-Fi, such as communication temptations. This may be similarly due to different conceptualizations of these strategies and may also be explained by the manner in which SLPs advised caregivers to use strategies; SLPs were observed to advise caregivers to use strategies by providing tips or “homework” at the end of the intervention, and they may have therefore advised caregivers to use strategies they themselves did not use with the child during the session. This may explain why differences in developmental and behavioral strategy use was larger for observational measures than on self-reported or qualitative measures.
Future Directions
These results highlight ways that researchers may make NDBIs more valuable and feasible, thereby optimizing the design of these interventions to support greater dissemination in community settings. The focused nature of manualized NDBIs contrasts with the multidisciplinary nature of EI sessions in this study, suggesting a mismatch between ideal NDBI use and the procedures and goals of family-centered EI. In fact, previous studies have found that preservice education opportunities about EI and autism are rare (Campbell et al., 2009; Stronach & Schmedding-Bartley, 2019), continuing education and professional development are often costly and time-intensive (Thome et al., 2020), and the autism-specific nature of NDBIs may limit their use by EI providers, who see children with and without autism diagnoses (Pickard et al., 2021). Given the intensive methods that may be optimal for teaching clinicians (e.g., mentorship, in-vivo coaching; Kyzar et al., 2014; Marturana & Woods, 2012), it may be unreasonable to expect a single training to cover all the needs of autistic children and their families in EI; however, further investigation of the impact of NDBIs across developmental domains and on discrete skills commonly targeted by SLPs may facilitate clinical decision making around using NDBIs to meet specific family/child needs.
Furthermore, because individual NDBI strategies are commonly used in language interventions for other diagnostic populations, it may be possible that NDBIs are effective in improving communication skills for other populations. In fact, preschool teachers reported that many NDBI-aligned strategies are more effective for their other students compared with their autistic students (Maye et al., 2020). Thus, testing the effectiveness of NDBIs in other populations may also increase the perceived importance of NDBI professional development opportunities for EI providers. Widespread dissemination of NDBI programs has been slow despite promising therapist learning in effectiveness trials of NDBIs (Shire et al., 2017; Vismara et al., 2009), and therefore, efforts to make NDBI trainings more acceptable may motivate more EI clinicians to invest their time and resources to these professional development opportunities. Although this study included a small sample, that no SLP had received training in using NDBI interventions indicates that there is a great need for increased dissemination efforts.
Finally, researchers may benefit from the clinical expertise of community-based SLPs to develop future NDBI intervention studies. Differences between the goals discussed in this study and those targeted by NDBI trials suggest that SLPs may have intentionally used communication facilitation strategies considered “low quality” on the NDBI-Fi (e.g., questions and directions, as previously discussed). Future studies should use qualitative or mixed methods research to identify potential adaptations to NDBI strategies and measure their effectiveness in influencing specific goals of importance to EI providers and researchers. Researchers may also partner with clinicians to choose or design outcome measures to ensure their goals are represented by NDBI research. Efforts such as these will ensure that NDBIs are effective, relevant, and acceptable to clinicians in community settings, facilitating their widespread uptake.
Conclusions
EI SLPs did not implement individual NDBI strategies with the level of skillfulness considered to be ideal in research, which have been observed to optimize child outcomes. Nevertheless, SLPs spent a significant portion of their intervention sessions addressing related developmental domains and skills that may support caregiver needs, demonstrating the need for community-based clinicians to balance competing priorities to provide family-centered care. Outcomes of NDBIs are based on the overall use of packaged, manualized interventions, but connecting individual NDBI strategies with the specific skills they address may facilitate clinician decision making when individualizing intervention based on family needs. Furthermore, understanding the impact of NDBIs on other domains will better address the considerations that clinicians must take into account when providing coordinated, interdisciplinary care. EI SLPs may benefit from training in using NDBIs, and further investigation of these questions will make such trainings more effective for EI clinicians in the future.
Data Availability Statement
Data used in this study may be made available upon request from the corresponding author.
Supplementary Material
Acknowledgments
This study was supported by a grant awarded to Megan Roberts by the National Institutes of Health (R01DC014709). The authors would like to thank Katie Zanzinger, Marie Bloem, Amy Bahr, and the other staff and clinicians at the Early Intervention Research Group for their assistance with data collection and coding. They would also like to thank the participating families and speech-language pathologists for their time and commitment. All authors are White women and licensed speech-language pathologists with experience in early intervention and have been formally trained to implement and/or evaluate the fidelity of naturalistic developmental behavioral interventions programs. At the time of publication, Authors 1 and 2 are research doctoral students in communication sciences and disorders, Author 3 has a clinical doctorate in speech-language pathology and works in an academic medical center, and Author 4 has a PhD in Special Education and is the principal investigator of a lab investigating early interventions for children with communication disorders.
Funding Statement
This study was supported by a grant awarded to Megan Roberts by the National Institutes of Health (R01DC014709). All authors are White women and licensed speech-language pathologists with experience in early intervention and have been formally trained to implement and/or evaluate the fidelity of naturalistic developmental behavioral interventions programs. At the time of publication, Authors 1 and 2 are research doctoral students in communication sciences and disorders, Author 3 has a clinical doctorate in speech-language pathology and works in an academic medical center, and Author 4 has a PhD in Special Education and is the principal investigator of a lab investigating early interventions for children with communication disorders.
References
- American Speech-Language-Hearing Association. (n.d.). Autism [Practice Portal] . Retrieved April 26, 2022, from https://www.asha.org/practice-portal/clinical-topics/autism/
- Aranbarri, A. , Stahmer, A. C. , Talbott, M. R. , Miller, M. E. , Drahota, A. , Pellecchia, M. , Barber, A. B. , Griffith, E. M. , Morgan, E. H. , & Rogers, S. J. (2021). Examining US public early intervention for toddlers with autism: Characterizing services and readiness for evidence-based practice implementation. Frontiers in Psychiatry, 12, 786138. https://doi.org/10.3389/fpsyt.2021.786138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell, P. H. , Chiarello, L. , Wilcox, M. J. , & Milbourne, S. (2009). Preparing therapists as effective practitioners in early intervention. Infants and Young Children, 22(1), 21–31. https://doi.org/10.1097/01.IYC.0000343334.26904.92 [Google Scholar]
- Cycyk, L. M. , & Huerta, L. (2020). Exploring the cultural validity of parent-implemented naturalistic language intervention procedures for families from Spanish-speaking Latinx homes. American Journal of Speech-Language Pathology, 29(3), 1241–1259. https://doi.org/10.1044/2020_AJSLP-19-00038 [DOI] [PubMed] [Google Scholar]
- Dawson, G. , Rogers, S. , Munson, J. , Smith, M. , Winter, J. , Greenson, J. , Donaldson, A. , & Varley, J. (2010). Randomized, controlled trial of an intervention for toddlers with autism: The Early Start Denver model. Pediatrics, 125(1), e17–e23. https://doi.org/10.1542/peds.2009-0958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunst, C. J. , & Espe-Sherwindt, M. (2016). Family-centered practices in early childhood intervention. In Reichow B., Boyd B. A., Barton E. E., & Odom S. L. (Eds.), Handbook of Early Childhood Special Education (pp. 37–55). Springer. https://doi.org/10.1007/978-3-319-28492-7_3 [Google Scholar]
- Edmunds, S. R. , Frost, K. M. , Sheldrick, R. C. , Bravo, A. , Straiton, D. , Pickard, K. , Grim, V. , Drahota, A. , Kuhn, J. , Azad, G. , Pomales Ramos, A. , Ingersoll, B. , Wainer, A. , Ibanez, L. V. , Stone, W. L. , Carter, A. , & Broder-Fingert, S. (2022). A method for defining the CORE of a psychosocial intervention to guide adaptation in practice: Reciprocal imitation teaching as a case example. Autism, 26(3), 601–614. https://doi.org/10.1177/13623613211064431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frost, K. M. , Brian, J. , Gengoux, G. W. , Hardan, A. , Rieth, S. R. , Stahmer, A. , & Ingersoll, B. (2020). Identifying and measuring the common elements of naturalistic developmental behavioral interventions for autism spectrum disorder: Development of the NDBI-Fi. Autism, 24(8), 2285–2297. https://doi.org/10.1177/1362361320944011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris, P. A. , Taylor, R. , Minor, B. L. , Elliott, V. , Fernandez, M. , O'Neal, L. , McLeod, L. , Delacqua, G. , Delacqua, F. , Kirby, J. , Duda, S. N. , & on behalf of the REDCap Consortium. (2019). The REDCap Consortium: Building an international community of software platform partners. Journal of Biomedical Informatics, 95, 103208. https://doi.org/10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris, P. A. , Taylor, R. , Thielke, R. , Payne, J. , Gonzalez, N. , & Conde, J. G. (2009). Research Electronic Data Capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–381. https://doi.org/10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Individuals with Disabilities Education Improvement Act. (2004). Public Law 108–446, 20 U.S.C. 1400 et seq.
- Kaiser, A. P. , Hancock, T. B. , & Nietfeld, J. P. (2000). The effects of parent-implemented enhanced milieu teaching on the social communication of children who have autism. Early Education and Development, 11(4), 423–446. https://doi.org/10.1207/s15566935eed1104_4 [Google Scholar]
- Kasari, C. , Gulsrud, A. , Paparella, T. , Hellemann, G. , & Berry, K. (2015). Randomized comparative efficacy study of parent-mediated interventions for toddlers with autism. Journal of Consulting and Clinical Psychology, 83(3), 554–563. https://doi.org/10.1037/a0039080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koegel, L. K. , Koegel, R. L. , Harrower, J. K. , & Carter, C. M. (1999). Pivotal response intervention I: Overview of approach. Journal of the Association for Persons with Severe Handicaps, 24(3), 174–185. https://doi.org/10.2511/rpsd.24.3.174 [Google Scholar]
- Kwok, E. , Cermak, C. A. , Hatherly, K. , & Cunningham, B. J. (2022). Intervention goals for preschoolers with language difficulties and disorders: A scoping review using the International Classification of Functioning, Disability and Health Framework. American Journal of Speech-Language Pathology, 31(3), 1–70. https://doi.org/10.1044/2021_AJSLP-21-00226 [DOI] [PubMed] [Google Scholar]
- Kyzar, K. B. , Chiu, C. , Kemp, P. , Aldersey, H. M. , Turnbull, A. P. , & Lindeman, D. P. (2014). Feasibility of an online professional development program for early intervention practitioners. Infants and Young Children, 27(2), 174–191. https://doi.org/10.1097/IYC.0000000000000007 [Google Scholar]
- Lee, J. , Kaat, A. J. , & Roberts, M. Y. (2022). Involving caregivers of autistic toddlers in early intervention: Common practice or exception to the norm? American Journal of Speech-Language Pathology, 31(4), 1755–1770. https://doi.org/10.1044/2022_AJSLP-21-00246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marturana, E. R. , & Woods, J. J. (2012). Technology-supported performance-based feedback for early intervention home visiting. Topics in Early Childhood Special Education, 32(1), 14–23. https://doi.org/10.1177/0271121411434935 [Google Scholar]
- Maye, M. , Sanchez, V. E. , Stone-MacDonald, A. , & Carter, A. S. (2020). Early interventionists' appraisals of intervention strategies for toddlers with autism spectrum disorder and their peers in inclusive childcare classrooms. Journal of Autism and Developmental Disorders, 50(11), 4199–4208. https://doi.org/10.1007/s10803-020-04456-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nahmias, A. S. , Pellecchia, M. , Stahmer, A. C. , & Mandell, D. S. (2019). Effectiveness of community-based early intervention for children with autism spectrum disorder: A meta-analysis. Journal of Child Psychology and Psychiatry and Allied Disciplines, 60(11), 1200–1209. https://doi.org/10.1111/jcpp.13073 [DOI] [PubMed] [Google Scholar]
- Perepletchikova, F. , & Kazdin, A. E. (2005). Treatment integrity and therapeutic change: Issues and research recommendations. Clinical Psychology: Science and Practice, 12(4), 365–383. https://doi.org/10.1093/clipsy.bpi045 [Google Scholar]
- Piaget, J. , & Cook, M. (1952). The origins of intelligence in children. W. W. Norton & Co. https://doi.org/10.1037/11494-000 [Google Scholar]
- Pickard, K. , Mellman, H. , Frost, K. , Reaven, J. , & Ingersoll, B. (2021). Balancing fidelity and flexibility: Usual care for young children with an increased likelihood of having autism spectrum disorder within an early intervention system. Journal of Autism and Developmental Disorders, 1–13. https://doi.org/10.1007/s10803-021-04882-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prizant, B. M. , Wetherby, A. M. , Rubin, E. , & Laurent, A. C. (2003). The SCERTS model: A transactional, family-centered approach to enhancing communication and socioemotional abilities of children with autism spectrum disorder. Infants and Young Children, 16(4), 296–316. https://doi.org/10.1097/00001163-200310000-00004 [Google Scholar]
- QSR International Pty Ltd. (2020). NVivo. https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home
- Rowe, M. L. , Leech, K. A. , & Cabrera, N. (2017). Going beyond input quantity: Wh-questions matter for toddlers' language and cognitive development. Cognitive Science, 41(Suppl. 1), 162–179. https://doi.org/10.1111/cogs.12349 [DOI] [PubMed] [Google Scholar]
- Sandall, S. R. , McLean, M. E. , & Smith, B. J. (2000). DEC recommended practices in early intervention early childhood special education. ERIC Clearinghouse. [Google Scholar]
- Sandbank, M. , Bottema-Beutel, K. , Crowley, S. , Cassidy, M. , Feldman, J. I. , Canihuante, M. , & Woynaroski, T. (2020). Intervention effects on language in children with autism: A Project AIM meta-analysis. Journal of Speech, Language, and Hearing Research, 63(5), 1537–1560. https://doi.org/10.1044/2020_JSLHR-19-00167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandoval-Norton, A. H. , & Shkedy, G. (2019). How much compliance is too much compliance: Is long-term ABA therapy abuse? Cogent Psychology, 6, Article 1641258. https://doi.org/10.1080/23311908.2019.1641258 [Google Scholar]
- Sawyer, B. E. , & Campbell, P. H. (2017). Teaching caregivers in early intervention. Infants and Young Children, 30(3), 175–189. https://doi.org/10.1097/IYC.0000000000000094 [Google Scholar]
- Schreibman, L. , Dawson, G. , Stahmer, A. C. , Landa, R. , Rogers, S. J. , McGee, G. G. , Kasari, C. , Ingersoll, B. , Kaiser, A. P. , Bruinsma, Y. , McNerney, E. , Wetherby, A. , & Halladay, A. (2015). Naturalistic developmental behavioral interventions: Empirically validated treatments for autism spectrum disorder. Journal of Autism and Developmental Disorders, 45(8), 2411–2428. https://doi.org/10.1007/s10803-015-2407-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shire, S. Y. , Chang, Y.-C. , Shih, W. , Bracaglia, S. , Kodjoe, M. , & Kasari, C. (2017). Hybrid implementation model of community-partnered early intervention for toddlers with autism: A randomized trial. Journal of Child Psychology and Psychiatry and Allied Disciplines, 58(5), 612–622. https://doi.org/10.1111/jcpp.12672 [DOI] [PubMed] [Google Scholar]
- Sone, B. J. , Kaat, A. J. , & Roberts, M. Y. (2021). Measuring parent strategy use in early intervention: Reliability and validity of the Naturalistic Developmental Behavioral Intervention Fidelity Rating Scale across strategy types. Autism, 25(7), 2101–2111. https://doi.org/10.1177/13623613211015003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stadnick, N. A. , Stahmer, A. , & Brookman-Frazee, L. (2015). Preliminary effectiveness of Project ImPACT: A parent-mediated intervention for children with autism spectrum disorder delivered in a community program. Journal of Autism and Developmental Disorders, 45(7), 2092–2104. https://doi.org/10.1007/s10803-015-2376-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stronach, S. T. , & Schmedding-Bartley, J. L. (2019). Clinical decision making in speech-language intervention for toddlers with autism and other social communication delays. Perspectives of the ASHA Special Interest Groups, 4(2), 228–239. https://doi.org/10.1044/2019_PERS-SIG1-2018-0010 [Google Scholar]
- Tamis-LeMonda, C. S. , Song, L. , Leavell, A. S. , Kahana-Kalman, R. , & Yoshikawa, H. (2012). Ethnic differences in mother–infant language and gestural communications are associated with specific skills in infants. Developmental Science, 15(3), 384–397. https://doi.org/10.1111/j.1467-7687.2012.01136.x [DOI] [PubMed] [Google Scholar]
- Thome, E. K. , Loveall, S. J. , & Henderson, D. E. (2020). A survey of speech-language pathologists' understanding and reported use of evidence-based practice. Perspectives of the ASHA Special Interest Groups, 5(4), 984–999. https://doi.org/10.1044/2020_PERSP-20-00008 [Google Scholar]
- Tiede, G. , & Walton, K. M. (2019). Meta-analysis of naturalistic developmental behavioral interventions for young children with autism spectrum disorder. Autism, 23(8), 2080–2095. https://doi.org/10.1177/1362361319836371 [DOI] [PubMed] [Google Scholar]
- Trivette, C. M. , Dunst, C. J. , & Hamby, D. W. (2010). Influences of family-systems intervention practices on parent–child interactions and child development. Topics in Early Childhood Special Education, 30(1), 3–19. https://doi.org/10.1177/0271121410364250 [Google Scholar]
- Vismara, L. A. , Young, G. S. , Stahmer, A. C. , Griffith, E. M. , & Rogers, S. J. (2009). Dissemination of evidence-based practice: Can we train therapists from a distance? Journal of Autism and Developmental Disorders, 39(12), 1636–1651. https://doi.org/10.1007/s10803-009-0796-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vygotsky, L. (1962). Thought and language. MIT Press. https://doi.org/10.1037/11193-000 [Google Scholar]
- Vygotsky, L. (1978). Mind in society: Development of higher psychological processes. Harvard University Press. [Google Scholar]
- Wainer, A. , & Ingersoll, B. (2013). Intervention fidelity: An essential component for understanding ASD parent training research and practice. Clinical Psychology: Science and Practice, 20(3), 335–357. https://doi.org/10.1111/cpsp.12045 [Google Scholar]
- Wetherby, A. M. , Guthrie, W. , Woods, J. , Schatschneider, C. , Holland, R. D. , Morgan, L. , & Lord, C. (2014). Parent-implemented social intervention for toddlers with autism: An RCT. Pediatrics, 134(6), 1084–1093. https://doi.org/10.1542/peds.2014-0757 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data used in this study may be made available upon request from the corresponding author.