Abstract
Purpose of Review
Referral to nutrition care providers in the USA such as registered dietitian nutritionists (RDNs) for medical nutrition therapy (MNT) remains low. We summarize research on the effectiveness of MNT provided by dietitians versus usual care in the management of adults with dyslipidemia. Improvements in lipids/lipoproteins were examined. If reported, blood pressure (BP), fasting blood glucose (FBG) glycated hemoglobin (A1c), body mass index (BMI), and cost outcomes were also examined.
Recent Findings
The synthesis of three systematic reviews included thirty randomized controlled trials. Multiple MNT visits (3–6) provided by dietitians, compared with usual care, resulted in significant improvements in total cholesterol (mean range: − 4.64 to − 20.84 mg/dl), low-density lipoprotein cholesterol (mean range: − 1.55 to − 11.56 mg/dl), triglycerides (mean range: − 15.9 to − 32.55 mg/dl), SBP (mean range: − 4.7 to − 8.76 mm Hg), BMI (mean: − 0.4 kg/m2), and A1c (− 0.38%). Cost savings from MNT were attributed to a decrease in medication costs and improved quality of life years (QALY).
Summary
Multiple MNT visits provided by dietitians compared with usual care improved lipids/lipoproteins, BP, A1c, weight status, and QALY with significant cost savings in adults with dyslipidemia and justify a universal nutrition policy for equitable access to MNT.
Keywords: Medical nutrition therapy, Dietary counseling, Dyslipidemia, Hyperlipidemia, Hypertriglyceridemia, Cost savings
Introduction
Cardiovascular disease (CVD) is a leading cause of death in the USA and globally [1, 2]. Recent studies indicate an association between dyslipidemia and other cardiometabolic risk factors and atherosclerotic cardiovascular disease (ASCVD) [1, 2, 3••, 4•, 5•, 6, 7]. Risk factors associated with ASCVD, such as dyslipidemia, hyperglycemia, hypertension, and overweight/obesity, are modifiable with diet and other lifestyle interventions [3••, 4•, 5•, 6, 7]. Thus, multiple healthcare organizations in the USA recommend diet and lifestyle interventions, such as medical nutrition therapy (MNT) provided by dietitians, be the foundation of treatment to improve ASCVD risk factors [3••, 4•, 5•, 6, 7]. In 2015, the National Lipid Association (NLA) published strong evidence-based recommendations for patient referral to a dietitian for MNT to manage dyslipidemia [3••]. In the USA, national guidelines from the American Heart Association (AHA)/American College of Cardiology (ACC) [4•, 5•, 6], The Obesity Society (TOS) [7], and the American Diabetes Association (ADA) [8] recommend patients be referred to a nutrition care provider such as a dietitian for MNT for the treatment of dyslipidemia [3••, 4•, 5•], hypertension [4•, 5•], overweight/obesity [4•, 5•, 6, 7], hyperglycemia [8], and type 2 diabetes (T2D) [6, 8, 9].
Dietitians provide MNT in various practice settings in the USA, such as hospitals, physician offices, private practice, and other healthcare facilities in conjunction with a multidisciplinary healthcare team. However, there is a universal lack of consistency in access to nutrition care in the USA [10]. Apart from diabetes and kidney disease, Medicare beneficiaries in the USA do not have access to MNT to manage dyslipidemia and other cardiometabolic risk factors [11•]. Thus, the aim of this narrative review is to summarize the evidence that supports the clinical and cost benefit of MNT by a dietitian to manage dyslipidemia and associated conditions. These data will assist policy makers in the USA to justify universal access to MNT provided by dietitians to manage ASCVD risk factors in the clinical setting and in the health care system.
MNT Provided by Dietitians for Dyslipidemia and Cardiometabolic Risk Factors
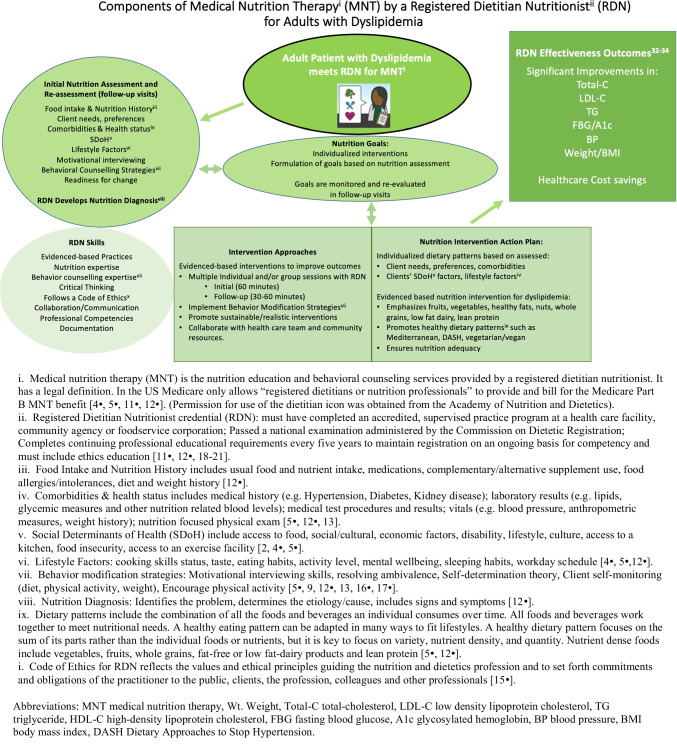
MNT is an evidence-based application of the Nutrition Care Process (NCP) by the dietitian [11•, 12•, 13–15, 16•, 17•, 18–20] [Fig. 1]. MNT in the management of dyslipidemia includes nutrition assessment, nutrition diagnosis, nutrition intervention, and monitoring and evaluation to affect lipids/lipoproteins, anthropometric measures (weight, BMI, waist circumference, body fat), BP, and glycemic status with the goal to ultimately prevent or delay its cardiometabolic consequences [11•, 13, 14, 21–23]. The NCP, as defined by the Academy of Nutrition and Dietetics, helps to determine the patient’s goals as they relate to adhering to a heart-healthy dietary pattern which helps to optimize positive outcomes [11•, 12•, 13, 14, 21, 24, 25]. The dietitian incorporates evidence-based expertise in behavioral counseling methods to facilitate sustainable and desirable behavior changes [23, 26]. Dietitians collaborate with various members of the multidisciplinary health care team including physicians, nurses/nurse practitioners, exercise physiologists, physical therapists, pharmacists, and mental health professionals to provide comprehensive care [3••, 4•, 11•, 27, 28]. A multidisciplinary team approach allows each team member to enhance and complement the efforts of each other while operating at the top of their expertise [3••, 4•, 5•].
Fig. 1.
Components of medical nutrition therapy (MNT) by a registered dietitian nutritionist (RDN) for adults with dyslipidemia
Healthcare Cost Burden of Cardiovascular Disease and Dyslipidemia
The economic cost of CVD attributed to dyslipidemia in the USA increased from $103.5 billion in 1996 to 1997 to $226.2 billion in 2017 to 2018 [2]. The average annual direct and indirect cost of CVD in the USA was estimated at $378 billion in 2017 to 2018. By event type, hospital inpatient stays accounted for the highest direct cost ($99.6 billion) in 2017–2018 in the USA [2]. In an observational cohort study [29] of 17,183 patients comparing patients with statin-controlled LDL-C with or without high TG, the overall difference in annual costs in the high TG cohort totaled over $2.6 million per year in excess annual costs and more than $13.5 million over the mean follow-up of 5.2 years suggesting significant potential healthcare savings (e.g., per person annual savings $964 in low TG group) [29]. In a retrospective study (n = 193,385) to examine healthcare costs related to cardiovascular events (CVE) in individuals with hyperlipidemia, costs were highest in the acute (first 30 days) post CVE and remained high over 3 years of follow-up as compared to those without a CVE [30]. In a systematic review of the cost of illness for hypercholesterolemia and mixed dyslipidemia, the direct costs estimate as an annual expenditure ranged from $17 to $259 million [31]. The clinical and economic impact of CVE events is a well-established public health issue [31]. It seems prudent to invest in access to MNT aimed at improving lipid levels to reduce residual CVD risk which can have an impact on healthcare cost savings [29].
Literature Review Methods
For this literature review, the population of interest was adults with dyslipidemia and the primary intervention of interest was MNT provided by dietitians. The outcomes of interest were improvements in circulating levels of lipids/lipoproteins [total-C (total cholesterol), LDL-C (low-density lipoprotein cholesterol), HDL-C (high-density lipoprotein cholesterol), TG (triglyceride)], blood pressure (BP), anthropometrics (weight, BMI), and glycemic control (fasting blood glucose (FBG) and glycated hemoglobin (A1c)]. A systematic search was performed to identify systematic reviews meeting eligibility criteria and published over the past 5 years using multiple databases (Medline (Bbsco), CINHAL (EBsco), Cochrane CENTRAL (Ebsco), and Cochrane Database of Systematic Reviews (Ebsco). Search terms included condition/population (e.g., hyperlipidemia, dyslipidemia, hypertriglyceridemia), intervention (diet therapy, medical nutrition therapy, behavior therapy, counseling, etc.), and study design (meta-analysis, systematic reviews (SR) etc.). A total of three SRs [32••, 33••, 34••] addressed the scope of this narrative review and were published within the past 5 years.
Summary of Evidence on the Effectiveness of MNT Provided by Dietitians in the Management of Adults with Dyslipidemia
Study and Population Characteristics
Three SRs were published in the last 5 years that evaluated the effectiveness of MNT in the management of adults with dyslipidemia [32••, 33••, 34••]. Study characteristics such as population, study designs of included studies, number and types of databases searched, sample size, risk of bias assessment, certainty of evidence, and outcomes were examined (Table 1). The three recent SRs examining the effectiveness of MNT in the management of dyslipidemia [32••, 33••, 34••] collectively included -30 unique RCTs [35–64]. Study participants also had additional ASCVD risk factors such as T2D [35, 36, 38, 39, 47, 51–53, 59, 62, 63], overweight or obesity [51, 53, 57, 60, 62], pre-diabetes [43, 53], hypertension [39, 42, 45, 47, 52, 58, 59, 61], CVD [39, 41, 59, 61], NAFLD [60], and MetS [48].
Table 1.
Recent systematic reviews examining the effect of medical nutrition therapy in the management of adults with dyslipidemia
| Systematic review | Population | Study designs included / | # of databases searched | Meta-analysis (yes/no) sample size | ROB tool | Certainty of evidence (yes/no) | Outcomes of interest reported |
|---|---|---|---|---|---|---|---|
| Mohr et al. 2022 [32••] | Adults with dyslipidemia (n = 838) | RCTs (n = 8) |
4 (MEDLINE, CINAHL, Cochrane CENTRAL, and Cochrane Database of Systematic Reviews) |
Yes | Cochrane’s ROB 2.0 | Yes | Total-C, LDL-C, HDL-C, TG, BP |
| Ross et al. 2019 [34••] |
Adults (≥ 18 years) at high-risk of cardiovascular disease (n = 1530) |
RCTs (n = 10) |
7 (ProQuest Family Health, Scopus, PubMed Central, MEDLINE, CINAHL and Cochrane) |
Yes | Cochrane’s ROB | Yes | Total-C, LDL-C, HDL-C, TG |
| Sikand et al. 2018 [33••] |
Adults with dyslipidemia and cardiovascular risk factors (n = 5704) |
RCTs(n = 11) Total studies (n = 34) • RCTs deemed observational per research question4 • Randomized cohort studies1 • Non-randomized controlled trials2 • Non-controlled trials2 • Prospective cohorts2 • Retrospective cohorts2 • Pre-Post studies10 |
3 (PubMed, Medline, Worldcat.org) |
Yes | Academy’s Quality Criteria Checklist | Yes | Total-C, LDL-C, HDL-C, TG, BP, FBG, A1c, BMI |
A1c, glycosylated hemoglobin; BMI, body mass index; BP, blood pressure; DBP, diastolic blood pressure; FBG, fasting blood glucose; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; RCTs, randomized controlled trials; ROB, risk of bias; SBP, systolic blood pressure; TG, triglyceride; Total-C, total cholesterol
All three systematic reviews (30 RCTs) [32••, 33••, 34••] examined the effect of MNT provided by dietitians or an international equivalent (for example, in the USA, the credential is Registered Dietitian Nutritionist (RDN); in Australia the nutrition care provider’s credential is referred to as an Accredited Practicing Dietitian (APD); and in Canada, it is Registered Dietitian (RD) [65, 66].
Fifteen RCTs describe providing individual-level interventions [35, 36, 38, 46–48, 51, 53, 55–58, 60, 63, 64], and seven RCTs included group-level interventions [39, 43, 47, 49, 56, 62, 64]. Although the number of MNT sessions by the dietitians varied, most interventions included three to six sessions over three to 6 months [35–37, 39–41, 44–47, 49, 53, 54, 56, 57, 64]. Session durations varied, but typically ranged from 30 to 120 min per session [43, 44, 50, 51, 53, 54, 57, 59]. Dietary approaches, when described, varied across studies and were often based on the target population. Dietary approaches targeted MNT for hyperlipidemia [58, 64], T2D [39], population-based dietary patterns [47, 62], reduced energy [51, 57, 63], reduced fat and/or cholesterol [51, 56, 57], Mediterranean diet [55], individualized diet [57], and low-carbohydrate diets [57, 63].
Summary of Effects on Outcomes of Interest: Circulating Levels of Lipids/Lipoproteins (Total-C, LDL-C, HDL-C, TG), BP, Anthropometrics (Weight, BMI) FBG and A1c
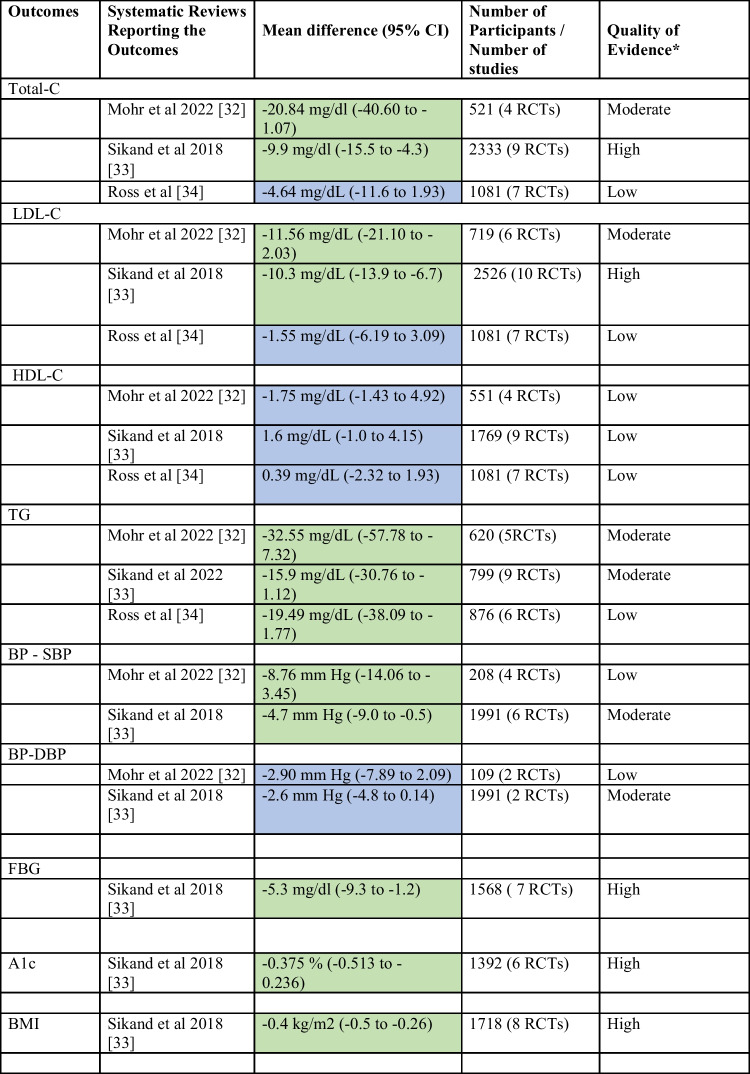
In the pooled analyses, all three systematic reviews (1) Mohr et al. 2022 (n = 838, seven RCTs)] [32••]; (2) Sikand et al. 2018 (n = 5704 in 34 studies/19 RCTs) [33••]; and (3) Ross et al. 2019 (n = 1530, 10 RCTs) [34••] reported significant improvements in lipids/lipoproteins (LDL-C, TG, total-C) with MNT provided by dietitians compared to usual care (Table 2). Furthermore, significant improvements were reported in BP [32••, 33••] and in anthropometrics (BMI), FBG, and A1c [33••]. Significant cost savings along with improved QALY and quality of life scores were also reported [33••].
Total-C: Total-C was reduced significantly (Table 2): Mohr et al. = − 20.84 mg/dL (n = 521, 4 RCTs) [32••], Sikand et al. = − 9.9 mg/dL (n = 2333, 9 RCTs) [33••], and Ross et al. = non-significant reduction [34••].
LDL-C: LDL-C was reduced significantly (Table 2): Mohr et al. = − 11.56 mg/dL (n = 719, 6 RCTs) [32••], Sikand et al. = LDL-C − 10.3 mg/dL (n = 2526, 10 RCTs) [33••], and Ross et al. = non-significant reduction [34••].
TG: TG was reduced significantly (Table 2): Mohr et al. = − 32.55 mg/dL, (n = 620, 5 RCTs) [32••], Sikand et al. = TG levels − 15.9 mg/dL (n = 799, 9 RCTs) [33••], and Ross et al. = − 19.5 mg/dL (n = 876, 6 RCTs) [34••].
HDL-C: Non-significant improvements (Table 2) were reported in HDL-C in all SRs [32••, 33••, 34••].
BP: BP improved significantly (Table 2): Mohr et al. SBP = − 8.76 mg/dL (n = 208, 4 RCTs) [32••], Sikand et al. = SBP − 4.7 mm Hg (n = 1991, 6 RCTs), and DBP − 2.6 mm Hg (n = 1991, 6 RCTs), (n = 2526, 10 RCTs) [33••]. Ross et al. did not evaluate BP [34••].
FBG: FBG improved significantly (Table 2): Sikand et al. = − 5.3 mg/dL (− 9.3 to − 1.2) [n = 1568, 7 RCTs) [34••]. Mohr et al. [33••] and Ross et al. [35] did not evaluate FBG.
A1c: A1c improved significantly (Table 2): Sikand et al. [23] = − 0.38%, (n = 1392, 6 RCTs) [33••]. Mohr et al. [32••] and Ross et al. [34••] did not evaluate A1c.
BMI: BMI was reduced significantly (Table 2): Sikand et al. = − 0.4 kg/m2 (n = 1718, 8 RCTs) [33••]. Mohr et al. [32••] and Ross et al. [34••] did not evaluate anthropometrics.
Cost savings: Cost savings of $638 to $1450 per patient per year were reported in SR 2 due to decreases in medications [33••]. Mohr et al. [33••] and Ross et al. [35] did not examine cost savings.
QALY: SR 2 reported an increase in QALY by 0.75 years [33••]. Mohr et al. [33••] and Ross et al. [35] did not evaluate the QALY saved.
Table 2.
Summary of findings of the systematic review focused on the effectiveness of MNT provided by RDN for dyslipidemia
A1c, glycosylated hemoglobin; BMI, body mass index; BP, blood pressure; DBP, diastolic blood pressure; FBG, fasting blood glucose; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; RCTs, randomized controlled trials; SBP, systolic blood pressure; TG, triglyceride; Total-C, total cholesterol
*Certainty of evidence information was reported as stated in the included systematic reviews. These systematic reviews used GRADE method to determine certainty of evidence for outcomes of interest and graded them as high, moderate, or low
Green shading indicates significant between group effect
Blue shading indicates non-significant between group effect
Discussion
Results from three systematic reviews consistently demonstrate the beneficial effects of MNT on dyslipidemia compared with usual care. Mohr et al. [32••] and Sikand et al. [33••] reported significant reductions in total-C, LDL-C, TG levels, and SBP and a similar non-significant increases in HDL-C, respectively. Ross et al. [34••] reported significant reductions in TG compared with usual care and reported no significant difference in total-C and LDL-C reduction between MNT and usual care (printed materials provided by a physician or nurse). This disparate finding could be attributed to its eligibility criteria [34••] which also included studies with only one face-to-face MNT visit, while Mohr et al. [32••] and Sikand et al. [33••] included studies that required at least two or more face-to-face MNT visits. Sikand et al. [33••] reported an average of three to six face-to-face MNT visits with a dietitian over 3–6 months led to significant improvements in lipids/lipoproteins, BP, FBG, A1c, and BMI suggesting that one face-to-face MNT visit is not adequate. Of note, there was little overlap between the systematic reviews due to different eligibility criteria. Out of thirty studies, only five studies (40, 43, 46, 49, 53) overlapped between the three systematic reviews. Four studies (40, 43, 46, 53) were common between Sikand et al. [33••] and Ross et al. [34••] and two studies [46, 49] between Sikand [33••] and Mohr et al. [32••].
Though the direction of findings was similar between the systematic reviews, those that had stricter inclusion criteria in relation to intervention rigor typically demonstrated greater effect sizes.
An earlier narrative review by Jacobson et al. [3••] reported significant improvements in lipids/lipoproteins (total-C, LDL-C, and TG), along with cardiometabolic risk factors (BP, A1c, and BMI) with multiple MNT visits. Another systematic review of eight studies by McCoin et al. [67] in 2008 also reported significant improvement in lipids/lipoproteins and cardiometabolic risk factors along with significant cost savings.
Although HDL-C is not considered a direct target of lifestyle therapy [3••], low HDL-C (< 35 mg/dL) levels are a strong predictor of CVD event risk. The clinical relevance of raising HDL-C with lifestyle remains uncertain and clinical trials involving medications that raise HDL-C (e.g., niacin and fibrates) have not been shown to improve CVD outcomes [3••, 4•, 68•]. The current targets of lifestyle and drug therapies are circulating levels of atherogenic cholesterol (LDL-C and non-HDL-C), and significant reductions in LDL-C were noted in all three systematic reviews [32••, 33••, 34••]. Non-HDL-C contains both LDL-C and very-low-density lipoprotein cholesterol (VLDL-C). Of note, TG levels (highly correlate with VLDL-C) were significantly improved with MNT intervention in all three systematic reviews [32••, 33••, 34••].
Use of Lipid Lowering Medications
Of note, some participants in included the RCTs were taking lipid-lowering medications [35, 39, 41, 47, 52, 53, 58–60]. Statins remain the primary evidence-based pharmacologic strategy for treating dyslipidemia [68•]. However, the additive effect of MNT could reduce the need and dosage of medications, augment the effect of pharmacologic treatment, reduce the cost of treatment (especially if branded non-statin therapy would otherwise be needed), and reduce the residual risk of CVD [32••, 33••, 34••, 68•]. For example, Orazio [52] noted that a multidisciplinary team inclusive of pharmacological treatment can lead to improvements in cardiovascular risk factors such as lipids/lipoproteins. In Adachi et al. [35] study, medication usage was controlled as the changes in medications were not significant between the Intervention group and control group. Furthermore, Sikand [33••] reported a significant reduction in LDL-C with combining MNT with lipid-lowering medications in two RCTs [n = 872] [59, 69] and concluded that although the effect of MNT by dietitians may not be discerned when combined with lipid-lowering medications, these studies demonstrate that treatment goals can be achieved when MNT provided by dietitians is combined with pharmacological approach [33••]. The use of statins and anti-diabetic and BP medications may also improve some lipids, blood glucose, and BP outcomes in conjunction with MNT [33••].
Cost Savings of MNT Provided by Dietitians for Dyslipidemia
Improving lifestyle factors, which includes nutrition, has been shown to improve outcomes for heart disease risk [3••, 4•, 5•, 6, 7, 68•, 70]. Dietitian-delivered MNT promotes changes in dietary intake of fat and saturated fat and positively impacts changes in serum lipid levels [32••, 34••, 67, 71]. When patients attended two to four MNT sessions over 6 to 12 weeks, they reduced daily dietary fat (5% to 8% saturated fat (2% to 4%) and energy intake (232–710 kcal per day). Total-C was lowered by 7% to 21%, and LDL-C was lowered by 7% to 22%. TGs were lowered from 11 to 31% [71]. Sikand et al. [33••] reported an annual cost savings of $638 to $1456 per patient from reduced medication use and a gain of 0.75 QALY per patient. In a study investigating behavioral economics to improve CVD health behaviors and outcomes, it was found that using a variety of platforms that encouraged more frequent interaction between patients and healthcare providers helped engage patients and improve their decision-making about their health [72]. Another approach using home-delivered healthy medically tailored meals (MTMs) prepared for individuals with chronic disease was associated with approximately 1.6 million averted hospitalizations and a net cost savings of about $13.6 billion annually [73]. Suboptimal diets are associated with heart disease, stroke, and T2D in the USA [74]. There is an increased interest in improving nutrition care and the availability of nutrition programs that also include medically tailored meals in the philosophy of “food is medicine” as potential tools to improve health outcomes and food security [73].
Why Are Dietitians Successful in Assisting Individuals with Making Nutrition and Lifestyle Behavioral Changes?
Beyond their nutrition expertise, another reason dietitians achieve significant lipid-lowering effects is that they arrange for help their patients need to make behavior changes. For dietitians, the 5A model (assess, advise, agree, assist, and arrange) serves as a clinical framework for helping patients’ lifestyle behavioral changes while ensuring the individual’s autonomy [16•, 17•, 23, 26]. Thus, dietitians focus on the common barriers to lifestyle change often attributed to SDoH [16•, 17•, 23, 26]. The 5 A framework helps patients resolve their ambivalence about making lifestyle behavior changes [16•, 17•, 23, 26]. Importantly, dietitians are skilled in helping patients deal with barriers to change including ambivalence to change and also helping patients address other barriers they have, so as to make healthy lifestyle changes (examples include support at home, work environment, financial) [8, 16•, 17•, 23, 26]. In fact, in terms of the 5 As a model of change, dietitians provide support to patients by assisting them to achieve their lifestyle goals and arranging for help they need to change their behaviors. Physicians are skilled at the first three components of the 5 As the model (i.e., assessment, agreeing, and advising), but are not trained (nor have time) to assist patients and arrange for the help they need to achieve their goals [8]. In contrast, dietitians have the knowledge and expertise to do this; the systematic reviews conducted to date clearly show the benefits of MNT in helping patients achieve their lifestyle (and clinical) goals [32••, 33••, 34••]. Thus, as integral members of the health care team because of their unique expertise, dietitians contribute importantly to optimizing patient care and improving patient outcomes [3••, 32••, 33••, 34••].
Policy Making in the USA for Universal Access to MNT Provided by Dietitians
MNT should be seamlessly integrated into clinical practice and into the USA healthcare system for equity in nutrition care to mitigate ASCVD risk factors. CVD remains the leading cause of mortality in the USA and globally [1, 2]. Dyslipidemia along with cardiometabolic risk factors, such as hyperglycemia, hypertension, and overweight/obesity, are modifiable with diet and other lifestyle interventions [32••, 33••, 34••]. MNT in the USA includes an evidence-based diet and lifestyle intervention typically provided by dietitians [11•, 13, 14, 21]. In the USA, despite strong evidence and recommendations from the NLA [3••], AHA/ACC [4•, 5•, 6], TOS [7] and ADA [8, 9], referral for MNT by dietitians remains low [10] due to a lack of universal access to nutrition care for patients with dyslipidemia, overweight/obesity, hypertension, and hyperglycemia. In addition, healthcare providers may be unaware of how to access the services of dietitians and other nutrition resources at the local, state, or national level. In the USA, healthcare providers can find dietitians by specialty and zip code through the Academy of Nutrition and Dietetics [75••]. In the USA, the policymakers of health systems should include dietitians in clinical practice and on the multidisciplinary health care teams. Improving access to nutrition care will allow healthcare providers to partner with dietitians for achieving successful outcomes in adults with dyslipidemia along with improving BP, FBG, A1c, and BMI, in conjunction with, and without lipid-lowering medications. Several resources are available for billing for nutrition services [76–79]. The expansion of MNT legislation for payment for services in the USA is a necessary step to provide nutrition care to seniors and to close the gaps in health disparities.
Conclusion
Multiple MNT visits provided by dietitians are effective and cost beneficial in improving dyslipidemia and cardiometabolic risk factors such as overweight/obesity, elevated BP, and A1c compared to usual care. High-quality evidence from three recent SRs offers strong justification for increasing access to MNT care for dyslipidemia, overweight/obesity, hypertension, and hyperglycemia to mitigate the risks of ASCVD in conjunction with and/or without lipid-lowering medications. Treatment goals can be achieved when MNT provided by a DIETITIAN is combined with a pharmacological approach with significant cost savings. MNT is an evidence-based, cost-effective component of treatment to help combat the most prevalent and costly chronic conditions, including conditions contributing to poor COVID-19 outcomes. Improvement of efforts to increase awareness among healthcare providers in the USA on how to access dietitians and other nutritional services and resources is needed. Access to MNT is critical for seniors and communities of color that suffer from chronic disease health disparities, driven by reduced access to medical and nutrition care, healthy foods, and safe places to be active.
In the USA, MNT by dietitians should be considered for reimbursement in the treatment of dyslipidemia, hyperglycemia, hypertension, and overweight/obesity as a standard of practice to optimize cardiovascular outcomes. The expansion of MNT legislation in the USA with advocacy from major influential medical societies is necessary to provide nutrition care to seniors and to close the gaps in health disparities. Further research is needed to include longer intervention periods.
Acknowledgements
The authors would like to gratefully acknowledge Dr Penny Kris-Etherton for providing guidance and valuable comments and feedback during the development of this manuscript.
Author Contribution
GS: conceptualize, design, and writing of the initial manuscript draft; GS, DH, MR, DDW: conception and design of the manuscript; GS, DH, MR, DDW: acquisition of data; GS, DH, MR, DDW, NDW: analysis and interpretation of data; GS, DH, MR, DDW, NDW: review/edit/supporting contributions to the manuscript; GS: supervision. All authors read and approved the final manuscript.
Declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Geeta Sikand, Email: gsikand@gmail.com, Email: gsikand@hs.uci.edu.
Deepa Handu, Email: dhandu@eatright.org.
Mary Rozga, Email: mrozga@eatright.org.
Desiree de Waal, Email: DesireedeWaal@msn.com.
Nathan D. Wong, Email: ndwong@hs.uci.edu
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Ahmad FB, Anderson RN. The leading causes of death in the US for 2020. JAMA. 2021;325(18):1829–1830. doi: 10.1001/jama.2021.5469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tsao CW, Aday AW, Almarzooq ZI, Alonso A, Beaton AZ, Bittencourt MS, et al. Heart disease and stroke statistics-2022 update: a report from the American Heart Association. Circulation. 2022;145(8):e153–e639. doi: 10.1161/cir.0000000000001052. [DOI] [PubMed] [Google Scholar]
- 3.••.Jacobson TA, Maki KC, Orringer CE, Jones PH, Kris-Etherton P, Sikand G, et al. National lipid association recommendations for patient-centered management of dyslipidemia: part 2. J Clin Lipidol. 2015;9(6 Suppl):S1–122.e1. 10.1016/j.jacl.2015.09.002. NLA narrative review of the effectiveness of medical nutrition therapy by RDNs. [DOI] [PubMed]
- 4.•.Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Circulation. 2019;140(11):e596-e646. 10.1161/cir.0000000000000678. Recent, comprehensive guideline to prevent cardiovascular disease. [DOI] [PMC free article] [PubMed]
- 5.•.Lichtenstein AH, Appel LJ, Vadiveloo M, Hu FB, Kris-Etherton PM, Rebholz CM, et al. 2021 Dietary guidance to improve cardiovascular health: a scientific statement from the American Heart Association. Circulation. 2021;144(23):e472-e87. 10.1161/cir.0000000000001031. American Heart Association dietary guidance for cardiovasular disease. [DOI] [PubMed]
- 6.Joseph JJ, Deedwania P, Acharya T, Aguilar D, Bhatt DL, Chyun DA, et al. Comprehensive management of cardiovascular risk factors for adults with type 2 diabetes: a scientific statement from the American Heart Association. Circulation. 2022;145(9):e722–e759. doi: 10.1161/cir.0000000000001040. [DOI] [PubMed] [Google Scholar]
- 7.Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association task force on practice guidelines and the obesity society. Circulation. 2014;129(25 Suppl 2):S102–S138. doi: 10.1161/01.cir.0000437739.71477.ee. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. 10. Cardiovascular disease and risk management: standards of care in diabetes-2023. Diabetes Care. 2023;46(Suppl 1):S158-s90. 10.2337/dc23-S010. [DOI] [PMC free article] [PubMed]
- 9.ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. 5. Facilitating positive health behaviors and well-being to improve health outcomes: standards of care in diabetes-2023. Diabetes Care. 2023;46(Supple 1):S68-s96. 10.2337/dc23-S005. [DOI] [PMC free article] [PubMed]
- 10.Devries S, Aggarwal M, Allen K, Kris-Etherton P, Theriot P, Freeman AM. Assessment of the low referral rate of cardiologists to dietitians/nutritionists. Int J Dis Reversal Prev. 2021;4(1):8.10.22230/ijdrp.2021v3n2a303.
- 11.•.Academy of nutrition and dietetics: revised 2017 scope of practice for the registered dietitian nutritionist. J Acad Nutr Diet. 2018;118(1):141–65. 10.1016/j.jand.2017.10.002. Describes the scope of practice for registered dietitian nutritionists, including those providing interventions for dyslipidemia. [DOI] [PubMed]
- 12.•.Academy of nutrition and dietetics: nutrition terminology reference manual (eNCPT): dietetics language for nutrition care. Nutrition Counseling. 2022. https://www.ncpro.org/pubs/encpt-en/page-059. Accessed 7 Nov 2022. Provides guidance to standardized practice for medical nutrition therapy provided by a dietitian.
- 13.Swan WI, Vivanti A, Hakel-Smith NA, Hotson B, Orrevall Y, Trostler N, et al. Nutrition care process and model update: toward realizing people-centered care and outcomes management. J Acad Nutr Diet. 2017;117(12):2003–2014. doi: 10.1016/j.jand.2017.07.015. [DOI] [PubMed] [Google Scholar]
- 14.Academy of nutrition and dietetics: definition of terms. 2021. https://www.eatrightpro.org/practice/quality-management/definition-of-terms. Accessed 21 Sept 2022.
- 15.Academy of nutrition and dietetics: what is code of ethics. 2018. https://www.eatrightpro.org/practice/code-of-ethics/what-is-the-code-of-ethics. Accessed 9 Nov 2022.
- 16.•.Kris-Etherton PM, Petersen KS, Després JP, Braun L, de Ferranti SD, Furie KL, et al. Special considerations for healthy lifestyle promotion across the life span in clinical settings: a science advisory from the American Heart Association. Circulation. 2021;144(24):e515-e32. 10.1161/cir.0000000000001014. Describes important considerations for implementing nutrition interventions across the life span. [DOI] [PubMed]
- 17.•.Kris-Etherton PM, Petersen KS, Després JP, Anderson CAM, Deedwania P, Furie KL, et al. Strategies for promotion of a healthy lifestyle in clinical settings: pillars of ideal cardiovascular health: a science advisory from the American Heart Association. Circulation. 2021;144(24):e495-e514. 10.1161/cir.0000000000001018. Discusses strategies to promote cardiovascular health. [DOI] [PubMed]
- 18.Academy of nutrition and dietetics: referring patients to an RDN. 2022. https://www.eatrightpro.org/about-us/what-is-an-rdn-and-dtr/work-with-an-rdn-or-dtr/referring-patients-to-an-rdn. Accessed 14 Nov 2022.
- 19.Academy of nutrition and dietetics: every registered dietitian is a nutritionist, but not every nutritionist is a registered dietitian. 2022. https://www.eatrightpro.org/about-us/what-is-an-rdn-and-dtr/what-is-a-registered-dietitian-nutritionist/every-registered-dietitian-is-a-nutritionist-but-not-every-nutritionist-is-a-registered-dietitian. Accessed 14 Nov 2022.
- 20.Academy of nutrition and dietetics: what is a registered dietitian nutritionist. 2022. https://www.eatrightpro.org/about-us/what-is-an-rdn-and-dtr/what-is-a-registered-dietitian-nutritionist. Accessed 14 Nov 2022.
- 21.Tewksbury C, Nwankwo R, Peterson J. Academy of nutrition and dietetics: revised 2022 standards of practice and standards of professional performance for registered dietitian nutritionists (competent, proficient, and expert) in adult weight management. J Acad Nutr Diet. 2022;122(10):1940–54.e45. doi: 10.1016/j.jand.2022.06.008. [DOI] [PubMed] [Google Scholar]
- 22.Skea ZC, Aceves-Martins M, Robertson C, De Bruin M, Avenell A. Acceptability and feasibility of weight management programmes for adults with severe obesity: a qualitative systematic review. BMJ Open. 2019;9(9):e029473. 10.1136/bmjopen-2019-029473. [DOI] [PMC free article] [PubMed]
- 23.Greaves C, Poltawski L, Garside R, Briscoe S. Understanding the challenge of weight loss maintenance: a systematic review and synthesis of qualitative research on weight loss maintenance. Health Psychol Rev. 2017;11(2):145–163. doi: 10.1080/17437199.2017.1299583. [DOI] [PubMed] [Google Scholar]
- 24.Filippou CD, Tsioufis CP, Thomopoulos CG, Mihas CC, Dimitriadis KS, Sotiropoulou LI, et al. Dietary approaches to stop hypertension (DASH) diet and blood pressure reduction in adults with and without hypertension: a systematic review and meta-analysis of randomized controlled trials. Adv Nutr. 2020;11(5):1150–1160. doi: 10.1093/advances/nmaa041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dos Reis Padilha G, Sanches Machado d'Almeida K, Ronchi Spillere S, Corrêa Souza G. Dietary patterns in secondary prevention of heart failure: a systematic review. Nutrients. 2018;10(7). 10.3390/nu10070828. [DOI] [PMC free article] [PubMed]
- 26.Cardel MI, Newsome FA, Pearl RL, Ross KM, Dillard JR, Miller DR, et al. Patient-centered care for obesity: how health care providers can treat obesity while actively addressing weight stigma and eating disorder risk. J Acad Nutr Diet. 2022;122(6):1089–1098. doi: 10.1016/j.jand.2022.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Academy of nutrition and dietetics' evidence analysis center: hypertension guideline. 2015. https://andeal.org/hf. Accessed 22 Sept 2022.
- 28.Academy of nutrition and dietetics evidence analysis center: adult weight management guideline. 2022. andeal.org/awm. Accessed 7 Nov 2022.
- 29.Nichols GA, Philip S, Reynolds K, Granowitz CB, O’Keeffe-Rosetti M, Fazio S. Comparison of medical care utilization and costs among patients with statin-controlled low-density lipoprotein cholesterol with versus without hypertriglyceridemia. Am J Cardiol. 2018;122(7):1128–1132. doi: 10.1016/j.amjcard.2018.06.029. [DOI] [PubMed] [Google Scholar]
- 30.Henk HJ, Paoli CJ, Gandra SR. A retrospective study to examine healthcare costs related to cardiovascular events in individuals with hyperlipidemia. Adv Ther. 2015;32(11):1104–1116. doi: 10.1007/s12325-015-0264-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ferrara P, Di Laura D, Cortesi PA, Mantovani LG. The economic impact of hypercholesterolemia and mixed dyslipidemia: a systematic review of cost of illness studies. PLoS One. 2021;16(7):e0254631. 10.1371/journal.pone.0254631. [DOI] [PMC free article] [PubMed]
- 32.••.Mohr AE, Hatem C, Sikand G, Rozga M, Moloney L, Sullivan J, et al. Effectiveness of medical nutrition therapy in the management of adult dyslipidemia: a systematic review and meta-analysis. J Clin Lipidol. 2022. 10.1016/j.jacl.2022.06.008. Recent systematic review that focused specifically of medical nutrition therapy provided by a dietitian for adults with dyslipidemia. [DOI] [PubMed]
- 33.••.Sikand G, Cole RE, Handu D, deWaal D, Christaldi J, Johnson EQ, et al. Clinical and cost benefits of medical nutrition therapy by registered dietitian nutritionists for management of dyslipidemia: a systematic review and meta-analysis. J Clin Lipidol. 2018;12(5):1113–22. 10.1016/j.jacl.2018.06.016. Systematic review that evaluates effect of medical nutrition therapy provided by a dietitian on lipid-related outcomes and cost-effectiveness of these intervention. [DOI] [PubMed]
- 34.••.Ross LJ, Barnes KA, Ball LE, Mitchell LJ, Sladdin I, Lee P, et al. Effectiveness of dietetic consultation for lowering blood lipid levels in the management of cardiovascular disease risk: a systematic review and meta-analysis of randomised controlled trials. Nutr Diet. 2019;76(2):199–210. 10.1111/1747-0080.12509. Systematic review that evaluates the effect of medical nutrition therapy provided by a dietitian on lipid-related outcomes. [DOI] [PMC free article] [PubMed]
- 35.Adachi M, Yamaoka K, Watanabe M, Nishikawa M, Kobayashi I, Hida E, et al. Effects of lifestyle education program for type 2 diabetes patients in clinics: a cluster randomized controlled trial. BMC Public Health. 2013;13:467. doi: 10.1186/1471-2458-13-467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Al-Shookri A, Khor GL, Chan YM, Loke SC, Al-Maskari M. Effectiveness of medical nutrition treatment delivered by dietitians on glycaemic outcomes and lipid profiles of Arab, Omani patients with Type 2 diabetes. Diabet Med. 2012;29(2):236–244. doi: 10.1111/j.1464-5491.2011.03405.x. [DOI] [PubMed] [Google Scholar]
- 37.Bray P, Cummings DM, Morrissey S, Thompson D, Holbert D, Wilson K, et al. Improved outcomes in diabetes care for rural African Americans. Ann Fam Med. 2013;11(2):145–150. doi: 10.1370/afm.1470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Brunerova L, Smejkalova V, Potockova J, Andel M. A comparison of the influence of a high-fat diet enriched in monounsaturated fatty acids and conventional diet on weight loss and metabolic parameters in obese non-diabetic and type 2 diabetic patients. Diabet Med. 2007;24(5):533–540. doi: 10.1111/j.1464-5491.2007.02104.x. [DOI] [PubMed] [Google Scholar]
- 39.Cohen LB, Taveira TH, Khatana SA, Dooley AG, Pirraglia PA, Wu WC. Pharmacist-led shared medical appointments for multiple cardiovascular risk reduction in patients with type 2 diabetes. Diabetes Educ. 2011;37(6):801–812. doi: 10.1177/0145721711423980. [DOI] [PubMed] [Google Scholar]
- 40.Delahanty LM, Sonnenberg LM, Hayden D, Nathan DM. Clinical and cost outcomes of medical nutrition therapy for hypercholesterolemia: a controlled trial. J Am Diet Assoc. 2001;101(9):1012–1023. doi: 10.1016/S0002-8223(01)00250-4. [DOI] [PubMed] [Google Scholar]
- 41.Haskell WL, Berra K, Arias E, Christopherson D, Clark A, George J, et al. Multifactor cardiovascular disease risk reduction in medically underserved, high-risk patients. Am J Cardiol. 2006;98(11):1472–1479. doi: 10.1016/j.amjcard.2006.06.049. [DOI] [PubMed] [Google Scholar]
- 42.Heller RF, Elliott H, Bray AE, Alabaster M. Reducing blood cholesterol levels in patients with peripheral vascular disease: dietitian or diet fact sheet? Med J Aust. 1989;151(10):566–568. doi: 10.5694/j.1326-5377.1989.tb101283.x. [DOI] [PubMed] [Google Scholar]
- 43.Imai S, Kozai H, Matsuda M, Hasegawa G, Obayashi H, Togawa C, et al. Intervention with delivery of diabetic meals improves glycemic control in patients with type 2 diabetes mellitus. J Clin Biochem Nutr. 2008;42(1):59–63. doi: 10.3164/jcbn.2008010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Johnston HJ, Jones M, Ridler-Dutton G, Spechler F, Stokes GS, Wyndham LE. Diet modification in lowering plasma cholesterol levels. A randomised trial of three types of intervention. Med J Aust. 1995;162(10):524–6. [PubMed]
- 45.Koopman H, Spreeuwenberg C, Westerman RF, Donker AJ. Dietary treatment of patients with mild to moderate hypertension in a general practice: a pilot intervention study (1). The first three months. J Hum Hypertens. 1990;4(4):368–71. [PubMed]
- 46.Lim HJ, Choi YM, Choue R. Dietary intervention with emphasis on folate intake reduces serum lipids but not plasma homocysteine levels in hyperlipidemic patients. Nutr Res. 2008;28(11):767–774. doi: 10.1016/j.nutres.2008.08.005. [DOI] [PubMed] [Google Scholar]
- 47.Ménard J, Payette H, Baillargeon JP, Maheux P, Lepage S, Tessier D, et al. Efficacy of intensive multitherapy for patients with type 2 diabetes mellitus: a randomized controlled trial. CMAJ. 2005;173(12):1457–1466. doi: 10.1503/cmaj.050054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Morita-Suzuki S, Fujioka Y, Mitsuoka H, Tashiro M, Harada M. Adding diet and exercise counseling to the health promotion plan alleviates anthropometric and metabolic complications in patients with metabolic syndrome. Nutr Metab Insights. 2012;5:49–58. doi: 10.4137/nmi.S9683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nasser R, Cook SL, Dorsch KD, Haennel RG. Comparison of two nutrition education approaches to reduce dietary fat intake and serum lipids reveals registered dietitians are effective at disseminating information regardless of the educational approach. J Am Diet Assoc. 2006;106(6):850–859. doi: 10.1016/j.jada.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 50.Neil HA, Roe L, Godlee RJ, Moore JW, Clark GM, Brown J, et al. Randomised trial of lipid lowering dietary advice in general practice: the effects on serum lipids, lipoproteins, and antioxidants. BMJ. 1995;310(6979):569–573. doi: 10.1136/bmj.310.6979.569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Olsen J, Willaing I, Ladelund S, Jørgensen T, Gundgaard J, Sørensen J. Cost-effectiveness of nutritional counseling for obese patients and patients at risk of ischemic heart disease. Int J Technol Assess Health Care. 2005;21(2):194–202. doi: 10.1017/S0266462305050269. [DOI] [PubMed] [Google Scholar]
- 52.Orazio LK, Isbel NM, Armstrong KA, Tarnarskyj J, Johnson DW, Hale RE, et al. Evaluation of dietetic advice for modification of cardiovascular disease risk factors in renal transplant recipients. J Ren Nutr. 2011;21(6):462–471. doi: 10.1053/j.jrn.2010.12.002. [DOI] [PubMed] [Google Scholar]
- 53.Parker AR, Byham-Gray L, Denmark R, Winkle PJ. The effect of medical nutrition therapy by a registered dietitian nutritionist in patients with prediabetes participating in a randomized controlled clinical research trial. J Acad Nutr Diet. 2014;114(11):1739–1748. doi: 10.1016/j.jand.2014.07.020. [DOI] [PubMed] [Google Scholar]
- 54.Rhodes KS, Bookstein LC, Aaronson LS, Mercer NM, Orringer CE. Intensive nutrition counseling enhances outcomes of National Cholesterol Education Program dietary therapy. J Am Diet Assoc. 1996;96(10):1003–10; quiz 11–2. 10.1016/s0002-8223(96)00268-4. [DOI] [PubMed]
- 55.Sialvera TE, Papadopoulou A, Efstathiou SP, Trautwein EA, Ras RT, Kollia N, et al. Structured advice provided by a dietitian increases adherence of consumers to diet and lifestyle changes and lowers blood low-density lipoprotein (LDL)-cholesterol: the increasing adherence of consumers to diet & lifestyle changes to lower (LDL) cholesterol (ACT) randomised controlled trial. J Hum Nutr Diet. 2018;31(2):197–208. doi: 10.1111/jhn.12508. [DOI] [PubMed] [Google Scholar]
- 56.Tonstad S, Sundfør T, Seljeflot I. Effect of lifestyle changes on atherogenic lipids and endothelial cell adhesion molecules in young adults with familial premature coronary heart disease. Am J Cardiol. 2005;95(10):1187–1191. doi: 10.1016/j.amjcard.2005.01.047. [DOI] [PubMed] [Google Scholar]
- 57.Thomson CA, Stopeck AT, Bea JW, Cussler E, Nardi E, Frey G, et al. Changes in body weight and metabolic indexes in overweight breast cancer survivors enrolled in a randomized trial of low-fat vs. reduced carbohydrate diets. Nutr Cancer. 2010;62(8):1142–52. 10.1080/01635581.2010.513803. [DOI] [PubMed]
- 58.Troyer JL, McAuley WJ, McCutcheon ME. Cost-effectiveness of medical nutrition therapy and therapeutically designed meals for older adults with cardiovascular disease. J Am Diet Assoc. 2010;110(12):1840–1851. doi: 10.1016/j.jada.2010.09.013. [DOI] [PubMed] [Google Scholar]
- 59.Vale MJ, Jelinek MV, Best JD, Dart AM, Grigg LE, Hare DL, et al. Coaching patients on achieving cardiovascular health (COACH): a multicenter randomized trial in patients with coronary heart disease. Arch Intern Med. 2003;163(22):2775–2783. doi: 10.1001/archinte.163.22.2775. [DOI] [PubMed] [Google Scholar]
- 60.Wong VW, Chan RS, Wong GL, Cheung BH, Chu WC, Yeung DK, et al. Community-based lifestyle modification programme for non-alcoholic fatty liver disease: a randomized controlled trial. J Hepatol. 2013;59(3):536–542. doi: 10.1016/j.jhep.2013.04.013. [DOI] [PubMed] [Google Scholar]
- 61.Wong MC, Wang HH, Kwan MW, Fong BC, Chan WM, Zhang DX, et al. Dietary counselling has no effect on cardiovascular risk factors among Chinese Grade 1 hypertensive patients: a randomized controlled trial. Eur Heart J. 2015;36(38):2598–2607. doi: 10.1093/eurheartj/ehv329. [DOI] [PubMed] [Google Scholar]
- 62.Woo J, Sea MM, Tong P, Ko GT, Lee Z, Chan J, et al. Effectiveness of a lifestyle modification programme in weight maintenance in obese subjects after cessation of treatment with Orlistat. J Eval Clin Pract. 2007;13(6):853–859. doi: 10.1111/j.1365-2753.2006.00758.x. [DOI] [PubMed] [Google Scholar]
- 63.Yamada Y, Uchida J, Izumi H, Tsukamoto Y, Inoue G, Watanabe Y, et al. A non-calorie-restricted low-carbohydrate diet is effective as an alternative therapy for patients with type 2 diabetes. Intern Med. 2014;53(1):13–19. doi: 10.2169/internalmedicine.53.0861. [DOI] [PubMed] [Google Scholar]
- 64.Zhao JY, Li H, Jin S, Chen XH, Chen LL. An integrated method of therapeutic lifestyle change for older adults with dyslipidaemia. Public Health. 2017;148:30–36. doi: 10.1016/j.puhe.2017.02.013. [DOI] [PubMed] [Google Scholar]
- 65.Dietitians Australia: credentialing of dietitians. 2022. https://dietitiansaustralia.org.au/working-dietetics/credentialing-dietitians. Accessed 14 Nov 2022.
- 66.Dietitians of Canada: registration to practice. 2022. https://www.dietitians.ca/Become-a-Dietitian/Education-and-Training/Regulatory-colleges-and-registration-to-practice. Accessed 14 Nov 2022.
- 67.McCoin M, Sikand G, Johnson EQ, Kris-Etherton PM, Burke F, Carson JA, et al. The effectiveness of medical nutrition therapy delivered by registered dietitians for disorders of lipid metabolism: a call for further research. J Am Diet Assoc. 2008;108(2):233–239. doi: 10.1016/j.jada.2007.10.041. [DOI] [PubMed] [Google Scholar]
- 68.•.Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the management of blood cholesterol: executive summary: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol. 2019;73(24):3168–209. 10.1016/j.jacc.2018.11.002. Recent, collaborative guideline describing current best practices for managing blood cholesterol. [DOI] [PubMed]
- 69.Welty FK, Nasca MM, Lew NS, Gregoire S, Ruan Y. Effect of onsite dietitian counseling on weight loss and lipid levels in an outpatient physician office. Am J Cardiol. 2007;100(1):73–75. doi: 10.1016/j.amjcard.2007.02.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Centers for disease control and prevention: prevent heart disease. 2022. https://www.cdc.gov/heartdisease/prevention.htm. Accessed 7 Nov 2022.
- 71.Academy of nutrition and dietetics evidence analysis center: medical nutrition therapy for dyslipidemia. 2022. https://www.andeal.org/topic.cfm?menu=5284. Accessed 7 Nov 2022.
- 72.Hare AJ, Patel MS, Volpp K, Adusumalli S. The role of behavioral economics in improving cardiovascular health behaviors and outcomes. Curr Cardiol Rep. 2021;23(11):153. doi: 10.1007/s11886-021-01584-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hager K, Cudhea FP, Wong JB, Berkowitz SA, Downer S, Lauren BN, et al. Association of national expansion of insurance coverage of medically tailored meals with estimated hospitalizations and health care expenditures in the US. JAMA Netw Open. 2022;5(10):e2236898. 10.1001/jamanetworkopen.2022.36898. [DOI] [PMC free article] [PubMed]
- 74.Micha R, Peñalvo JL, Cudhea F, Imamura F, Rehm CD, Mozaffarian D. Association between dietary factors and mortality from heart disease, stroke, and type 2 diabetes in the United States. JAMA. 2017;317(9):912–924. doi: 10.1001/jama.2017.0947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.••.Academy of nutrition and dietetics: find a nutrition expert. 2022. https://www.eatright.org/find-a-nutrition-expert/. Accessed 14 Nov 2022. Website to find and partner with a registered dietician nutritionist.
- 76.Academy of Nutrition and Dietetics: Medicare MNT. 2022. https://www.eatrightpro.org/payment/medicare/mnt/. Accessed 14 Nov 2022.
- 77.Academy of nutrition and dietetics: referrals to a registered dietitian nutritionist primary care provider toolkit. 2022. https://www.eatrightpro.org/payment/getting-started/referrals-and-primary-care-partnership/referrals-to-a-registered-dietitian-nutritionist-primary-care-provider-toolkit. Accessed 14 Nov 2022.
- 78.Academy of nutrition and dietetics: diagnosis and procedure codes. 2022. https://www.eatrightpro.org/payment/coding-and-billing/diagnosis-and-procedure-codes. Accessed 14 Nov 2022.
- 79.Academy of nutrition and dietetics: MNT business practice tools: common ICD-10-CM codes related to nutrition services. 2021. https://www.eatrightstore.org/product-subject/mnt-references/mnt-business-practice-tools-diagnosis-codes-for-medicare-mnt. Accessed 14 Nov 2022.