Abstract
The Korean Society of Heart Failure guidelines aim to provide physicians with evidence-based recommendations for diagnosing and managing patients with heart failure (HF). In Korea, the prevalence of HF has been rapidly increasing in the last 10 years. HF has recently been classified into HF with reduced ejection fraction (HFrEF), HF with mildly reduced ejection fraction (EF), and HF with preserved EF (HFpEF). Moreover, the availability of newer therapeutic agents has led to an increased emphasis on the appropriate diagnosis of HFpEF. Accordingly, this part of the guidelines will mainly cover the definition, epidemiology, and diagnosis of HF.
Keywords: Heart failure; Ventricular ejection fraction; Heart failure, preserved ejection fraction; Cardiomyopathy; Biomarkers
INTRODUCTION
The Korean Society of Heart Failure (KSHF) had published treatment guidelines for chronic heart failure (HF) and acute HF in 2016 and 2017, respectively. Subsequently, the Guidelines Committee of the KSHF, established in 2018, reviewed the guidelines and published the 2019 Chronic Heart Failure Guidelines Update and the 2020 Acute Heart Failure Guidelines Update with support of the associated societies.1)
During the last 6 years—since the publication of Korea's first HF treatment guidelines—Korean researchers and patients have actively participated in numerous substantial and large-scale international multicenter clinical studies published worldwide. Several independent domestic studies have been published as well. Despite 2 revisions in 2018 and 2019, a complete revision of the HF guidelines was required to reflect the overall changes; hence, from 2021, relevant manuscripts were collected through the Guidelines Committee and after thorough discussion, 64 chapters were published in 2022.
An evidence-based method was employed for data analyses and providing recommendations for the guidelines; manuscripts received from expert clinicians in the country were reviewed by the Practice Guidelines Committee and edited after receiving a response from the authors. Prior to the publication of the revised guidelines, 2 workshops, several committee meetings, and 5 editorial board meetings were held with the Advisory and Review Committees to obtain substantive and reasonable opinions.
During the preparation of revised edition of the KSHF guidelines, the revised editions of the European and United States guidelines on HF were published in September 2021 and April 2022, respectively.2,3) The current version of the KSHF guidelines strives to reflect data pertaining to domestic realities beyond the acceptance of the modifications and is based on the results of recent studies conducted by Korean researchers and clinicians. Despite our efforts to include findings from domestic research, we were only able to provide distinct recommendations for the treatment of HF with mildly reduced ejection fraction (HFmrEF) and HF with preserved EF (HFpEF). Nonetheless, we have highlighted the unique epidemiological features of HF in Korea, including its prevalence and etiology, in the main manuscript.
The revised guidelines cover the diagnosis, medical treatment, surgical and device-based treatment, and specific etiology of HF. This part of the guidelines will mainly cover the definition, epidemiology, and diagnosis of HF. The main difference in this section compared to the previous guideline is the adoption of terminology for HF with EF 40–49% in accordance with Western guidelines, as well as the inclusion of a specific diagnostic method for HFpEF, which includes the diastolic stress test. Notably, this diagnostic method was developed by Korean researchers and has been added to the guidelines.
DIAGNOSIS AND CLASSIFICATION OF HF
Definition of HF
HF results from a functional or structural impairment of the heart due to low stroke volume or raised left ventricular (LV) filling pressure. The symptoms include dyspnea, swollen legs, and fatigue1); the signs include lung crackles and increased jugular venous pressure.
Classification of HF
LVEF, a parameter of LV contractility, is used to classify HF phenotypes. In general, LVEF ≤40% is defined as HF with reduced EF (HFrEF), whereas LVEF ≥50% is defined as HFpEF.4,5) In addition, if the LVEF was between 41–49%, the definition of HF with mid-range EF was used because it was considered close to HFpEF. However, recent studies reported similar effects of HFrEF medication in this group, leading to the newer classification of HFmrEF because of its proximity to HFrEF (Table 1).6,7,8,9)
Table 1. Classification of heart failure.
| Type of heart failure | Clinical evidence | LVEF | Additional evidence |
|---|---|---|---|
| HFrEF | Symptom*±Sign† | ≤40% | Not required |
| HFmrEF | Symptom*±Sign† | 41–49% | Not required |
| HFpEF | Symptom*±Sign† | ≥50% | Increase of NP levels or LV structural/functional abnormality suggesting LV diastolic dysfunction or increased LV filling pressure |
LVEF = left ventricular ejection fraction; HFrEF = heart failure with reduced ejection fraction; HFmrEF = heart failure with mildly reduced ejection fraction; HFpEF = heart failure with preserved ejection fraction; NP = natriuretic peptide; LV = left ventricular.
*Typical symptoms: exertional dyspnea, orthopnea, paroxysmal nocturnal dyspnea, fatigue, and pedal edema; Atypical symptoms: weight gain, weight loss, loss of appetite, and palpitation.
†Typical signs: jugular vein distension and S3 sound; Atypical signs: peripheral edema, rales, irregular heart beat, tachypnea, hepatomegaly, and ascites.
The proportion of patients with HF classified according to the LVEF status is as follows: in the Korean Heart Failure (KorHF) registry, the mean LVEF was 38.5±15.7%; 1,638 (57.6%), 491 (17.3%), and 714 (25.1%) patients had HFrEF, HFmrEF, and HFpEF, respectively; and in the Korean Acute Heart Failure (KorAHF) registry, 60.5%, 14.3%, and 25.2% were patients with HFrEF, HFmrEF, and HFpEF, respectively.10)
Different types of heart failure
In “chronic” HF, the disease course is stable and it gradually progresses. A sudden or gradual deterioration of chronic HF leads to “decompensated” HF. Such patients may require intravenous diuretics with or without hospitalization. In “compensated” HF, the symptoms are absent or improve after a period of time. In “acute” HF, the symptoms/signs worsen and require unplanned hospitalization or emergency room visits. “De novo” HF is the first occurrence of HF symptoms. When various causes lead to right ventricular (RV) dysfunction, resulting in symptoms and signs of HF, it is referred to as right-sided HF. The most common cause is secondary pulmonary hypertension (HTN) due to left-sided heart disease. Other possible causes include idiopathic pulmonary arterial HTN, chronic pulmonary thromboembolism, and chronic lung disease.11)
EPIDEMIOLOGY OF HEART FAILURE
Prevalence and incidence
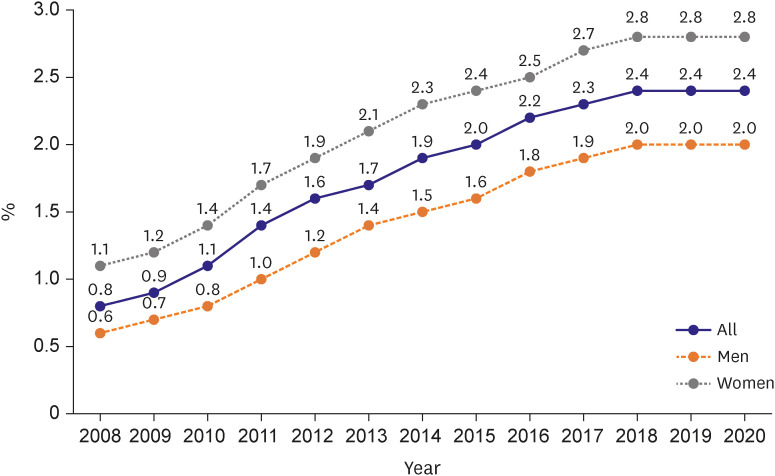
The global prevalence of HF is rapidly increasing and it is closely associated with a higher morbidity and mortality.12,13,14,15,16,17) HF is a leading cause of hospitalization and mortality, especially in the older adult population (>65 years).18) In the United States, the National Health and Nutrition Examination Survey estimates that more than 5.1 million people aged ≥20 years have HF,19) and this number is expected to increase by 46% to more than 8 million people by 2030.20) According to the 2020 Korean Heart Failure White Paper, the estimated prevalence of HF exhibited an increasing trend from 0.77% in 2002 to 2.24% in 2018. In 2018, 1,159,776 (2.24%) patients had HF.21) The prevalence of HF tends to rapidly increase with age. In 2018, the prevalence was 0.1–0.7% among people aged <50 years, and it sharply increased to 1.88% and 16.9% in those in their 50s and 80s, respectively. In particular, the prevalence in those aged ≥80 years was 15 times higher than the overall prevalence, indicating that age was the most important risk factor for HF. Additionally, the Guidelines Committee of the KSHF compiled the entire HF cohort using the Korea National Health Insurance Service database. The operational definition of HF required at least 3 claims for HF codes and the use of diuretics. In this cohort, the prevalence of HF showed an increasing trend from 0.81% in 2008 to 2.38% in 2020. In 2020, a total of 524,280 men and 733,695 women with HF were identified (Figure 1). Regarding the incidence of HF, the 2020 Korean Heart Failure White Paper shows a slight increasing trend from 2004 to 2014. However, the age-adjusted incidence rate, which is calculated using the Korean standard population in 2018, has been decreasing over time. The crude incidence rate of HF was 453 in 2004 and it increased to 579 per 100,000 persons in 2018 (an increase of 22%). The age-adjusted incidence was 693 in 2004 and 554 per 100,000 persons in 2018 (a decrease of 20%). This has been attributed to the improved treatment of ischemic heart (IHD) and valvular heart diseases, which are common causes of HF, to prevent progression to HF.
Figure 1. Temporal trends in heart failure from 2009 to 2020 in Korea using the Korean National Health Insurance Service claim data.
Mortality
The overall mortality and age-adjusted mortality rates for HF are increasing in Korea.21) The overall mortality of patients with HF rapidly increased from 39 per 100,000 persons in 2002 to 245 per 100,000 persons in 2018. The age-adjusted mortality increased from 75 per 100,000 persons in 2002 to 219 per 100,000 persons in 2018. The 1- and 5-year survival rate was 91% and 79%, respectively, in patients with HF, and 75% and 55%, respectively, in hospitalized patients with HF. Regarding longitudinal trend, the 1-year survival rate of hospitalized patients with HF significantly improved from 70% in 2004–2006 to 79% in 2016–2018, indicating improved survival rates of HF during the last 2 decades.22)
Etiology
The Framingham study found that HF incidence was as high as 10 per 1,000 persons in the older adult population (≥65 years), and that 75% of patients with HF had concomitant HTN.23) In 2013, an epidemiological data analysis using Korean Health Insurance Service sample data demonstrated that in HF, the prevalence of IHD and HTN were the highest at 45.4% and 43.6%, respectively, followed by valvular heart disease at 5.6% and cardiomyopathy at 3.1%.24) The Korean Heart Failure Registry (KorHF), which surveyed hospitalized patients with HF from 2004 to 2009, revealed that IHD, hypertensive heart disease, cardiomyopathy, and valvular heart disease accounted for 52.3%, 36.7%, 26.5%, and 12.7%, respectively.25) In addition, the KorAHF Registry, which examined 5,625 patients hospitalized for acute HF from 2011 to 2014, revealed that IHD, cardiomyopathy, valvular heart disease, tachycardia, and hypertensive heart disease accounted for 37.6%, 20.6%, 14.3%, 10%, and 4%, respectively. In Korea, IHD is the most common cause of HF.26,27)
DIAGNOSTIC ALGORITHM FOR HF
In patients with suspected HF, the following initial tests are recommended:
1. Twelve-lead electrocardiogram (ECG). (Class I, Level of Evidence C)
2. Assessment of B-type natriuretic peptide (BNP) or N-terminal (NT) pro BNP levels. (Class I, Level of Evidence B)
3. Diagnostic blood tests include complete blood count, lipid profile, and serum urea, electrolytes, and iron (transferrin saturation and ferritin), fasting blood glucose, glycated hemoglobin (HbA1c), and kidney (creatinine), liver, and thyroid function tests. (Class I, Level of Evidence C)
4. Echocardiography. (Class I, Level of Evidence C)
5. Chest radiography. (Class I, Level of Evidence C)
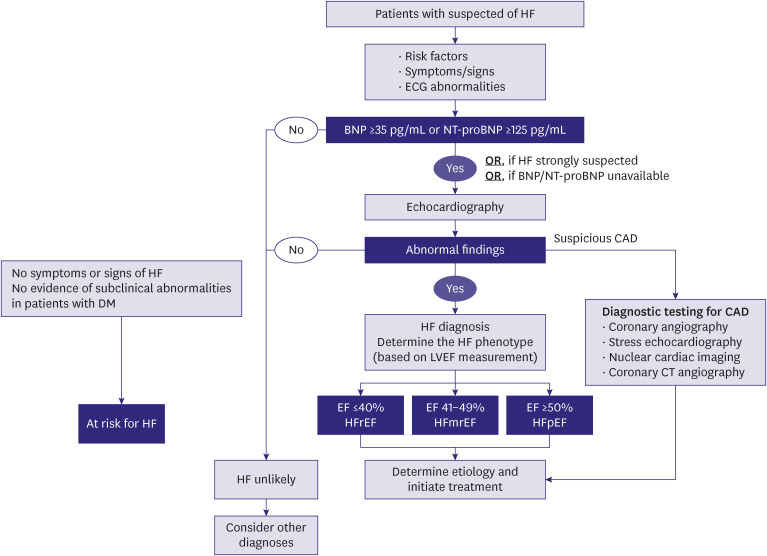
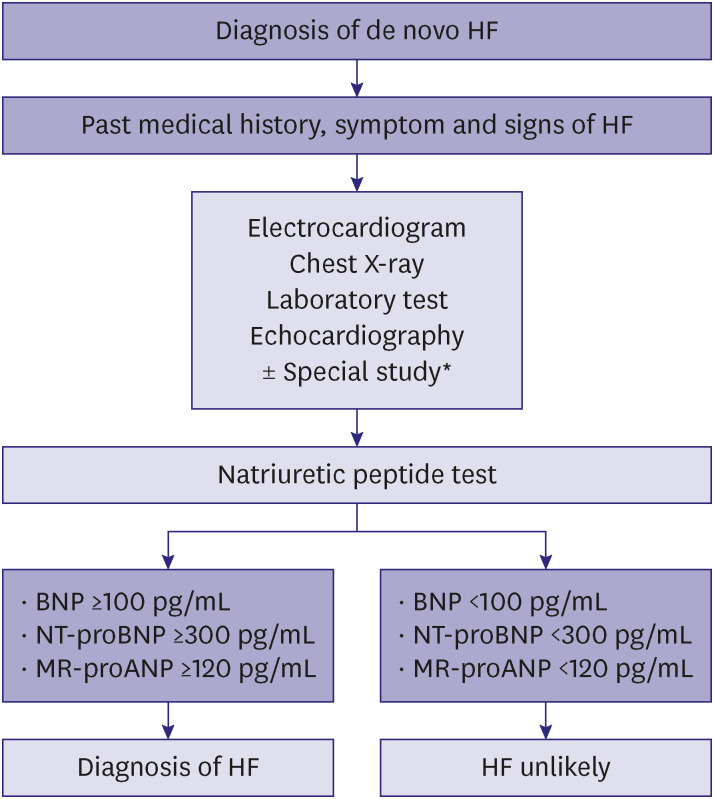
Careful history-taking and clinical examination are the cornerstones in the diagnosis of HF. Patients with HF may present with various symptoms (Table 1). Dyspnea is a common symptom of HF and it is usually exacerbated during exercise. However, these symptoms are non-specific; they appear in diseases of the airway, respiratory muscles, and chest wall as well, and healthy individuals do complain of dyspnea during exercise.28) When HF gradually becomes severe, patients develop orthopnea (they are more comfortable in a sitting rather than supine position) and paroxysmal nocturnal dyspnea. Orthopnea and paroxysmal nocturnal dyspnea are specific symptoms; however, the sensitivity is low because it is infrequent in mildly symptomatic patients. In addition, a decrease in cardiac output causes severe fatigue, and patients with arrhythmias, such as atrial fibrillation, often develop palpitations. Anorexia, indigestion, and bloating may occur in patients with RV dysfunction. Dyspnea is graded according to the activity necessary symptom manifestation (Table 2), which helps track the disease course or the response to HF treatment, though it is not proportional to the degree of ventricular function. To accurately diagnose HF, objective evidence suggesting cardiac dysfunction are needed in addition to the presence of suggestive symptoms and/or signs.29) The diagnostic algorithm for HF is illustrated in Figure 2.2,30) The diagnostic algorithm for acute HF is illustrated in Figure 3.2)
Table 2. New York Heart Association functional classification.
| Functional class | Symptoms |
|---|---|
| Class I | No symptoms with normal physical activity |
| Class II | Mild symptoms on exertion or with normal physical activity |
| Class III | Moderate symptoms with less than normal physical activity; however, no symptoms at rest |
| Class IV | Severe symptoms with minimal physical activity and even at rest |
Figure 2. The diagnostic algorithm for patients with suspected HF.
Adopted and modified from “Evaluation and management of patients with diabetes and heart failure: a Korean Diabetes Association and Korean Society of Heart Failure Consensus Statement. Int J Heart Fail 2023;5(1):1-20”.30)
HF = heart failure; ECG = electrocardiogram; BNP = B-type natriuretic peptide; NT-proBNP = N-terminal pro B-type natriuretic peptide; CAD = coronary artery disease; CT = computed tomography; DM = diabetes mellitus; LVEF = left ventricular ejection fraction; EF = ejection fraction; HFrEF = heart failure with reduced ejection fraction; HFmrEF = heart failure with mildly reduced ejection fraction; HFpEF = heart failure with preserved ejection fraction.
Figure 3. Diagnostic workup of new onset acute HF.
HF = heart failure; BNP = B-type natriuretic peptide; NT-proBNP = N-terminal pro B-type natriuretic peptide; MR-proANP = mid-regional pro-atrial natriuretic peptide.
*Coronary angiography, pulmonary embolism computed tomography, or lung sonography.
The following diagnostic tests are recommended for evaluation of patients with suspected HF.
(1) Electrocardiography
If the ECG is normal, the probability of HF is low.28) If abnormal ECG findings such as atrial fibrillation, Q wave, LV hypertrophy, and QRS widening are observed, the probability of HF is high.
(2) Natriuretic peptide
If possible, BNP levels should be measured; BNP <35 pg/mL, NT-pro hormone BNP (NT-proBNP) <125 pg/mL, or mid-regional pro atrial natriuretic peptide <40 pg/mL suggest extremely low probability of HF.31) (Further information is detailed in the chapter: Diagnostic blood tests).
(3) Essential blood tests
Diagnostic blood tests include complete blood count, lipid profile, and serum urea, electrolytes, and iron (transferrin saturation and ferritin), fasting blood glucose, HbA1c, and kidney (creatinine), liver, and thyroid function tests. These tests are necessary for the differential diagnosis of HF and for obtaining prognostic information on HF.
(4) Echocardiography
Echocardiography must be performed to assess heart function for diagnosing HF. The classification of HF is based on LVEF; therefore, LVEF assessment is essential. Thus, echocardiography evaluation should include chamber quantification, LV geometry, presence of regional wall motion abnormality (RWMA), pulmonary artery blood pressure, and RV, valvular, and diastolic functions.32)
(5) Chest radiography
Chest radiography is necessary to differentiate HF from other major causes of dyspnea (e.g., lung disease). Symptomatic pulmonary edema and cardiac hypertrophy, which suggest the high probability of HF, can be identified on chest radiographs.
DIAGNOSTIC TESTS FOR HEART FAILURE
1. Measurement of BNP or NT-proBNP levels may help prevent HF in patients at risk of HF without LV dysfunction. (Class IIa, Level of Evidence B)
2. In patients with suspected HF, measurement of BNP or NT-proBNP levels should be performed as the initial test, for the diagnosis and exclusion of HF. (Class I, Level of Evidence A)
3. In patients with acute or chronic HF, measurement of BNP or NT-proBNP levels is useful to assess the severity of HF and predict the prognosis. (Class I, Level of Evidence A)
4. In patients with acute HF, pre-discharge BNP or NT-proBNP levels may help predict post-discharge prognosis. (Class IIa, Level of Evidence B)
5. Measuring BNP or NT-proBNP levels for therapeutic drug dose change in patients with HF may not be helpful. (Class III, Level of Evidence B)
6. In patients with chronic HF, strategies to measure the multiple biomarkers that reflect myocardial injury, systemic inflammation, and myocardial fibrosis in addition to natriuretic peptides can be considered for risk stratification of HF. (Class IIb, Level of Evidence B)
As mentioned earlier, careful history taking and clinical examination are the initial steps in diagnosing HF. However, clinical symptoms and signs are neither highly sensitive nor specific for the diagnosis of HF; non-specific symptoms may delay accurate diagnosis or treatment, which eventually lead to poor prognosis and increased medical costs. Biomarkers enable rapid diagnosis or exclusion of HF at both a low cost and low risk; these help in setting a prognosis, and provide basic and practical information to understand the complex pathophysiology of HF.33) Various mechanisms such as myocardial stretching, matrix remodeling, myocardial damage, neurohormone activation, and inflammation are involved in the development and progression of HF through complex interactions. Natriuretic peptide is useful in diagnosing HF and assessing its severity, prognosis, and response to drug therapy. In addition, biomarkers such as troponin, soluble suppression of tumorigenicity-2 (sST2), galectin-3, high sensitivity C-reactive protein (hs-CRP), and growth-differentiation factor-15 (GDF-15) are attracting attention as adjunctive biomarkers.
Natriuretic peptide
(1) Types
Pressure or volume stress on the LV wall results in the secretion of natriuretic peptides. Biomarkers caused by LV wall stress consist of the physiologically active BNP and physiologically inactive NT-proBNP.34) Increased proBNP in HF breaks down into BNP and NT-proBNP. Both these substances have different biological and chemical characteristics; hence, each has its own advantages and disadvantages. Both are useful as diagnostic and prognostic markers for HF. However, owing to the different reference values or ranges, checking and interpreting each reference standard is vital (Table 3). Notably, BNP is degraded by neprilysin while NT-proBNP remains unaffected.35) Thus, angiotensin receptor-neprilysin inhibitors (ARNI) increase blood levels of BNP and not that of NT-proBNP. Therefore, when evaluating the dose-treatment response of ARNI, it may be preferable to measure changes in NT-proBNP levels. However, in the PARADIGM-HF study, in patients on ARNI, changes in BNP and NT-proBNP measured after 8–10 weeks were prognostically correlated, suggesting that both biomarkers were useful.36)
Table 3. Comparison of BNP and NT-proBNP.
| Characteristic | BNP | NT-proBNP |
|---|---|---|
| Diagnosis of HF in non-acute setting | ≥35 pg/mL | ≥125 pg/mL |
| Diagnosis of HF in acute setting | ≥100 pg/mL | ≥300 pg/mL |
| Half-life | Shorter, more rapid changes in response to treatment | Longer, a more stable measurement over time |
| Response to neprilysin | Degradable | Non-degradable |
| Specificity | More specific, less influenced by age and renal function | Less specific, influenced by age and renal function |
BNP = B-type natriuretic peptide; NT-proBNP = N-terminal-pro hormone B-type natriuretic peptide; HF = heart failure.
(2) Early screening of HF
The STOP-HF study demonstrated that echocardiography and cardiology consultation reduced the incidence of asymptomatic LV dysfunction in patients with a risk of HF (HTN, diabetes, and vascular disease [stage A HF]), if the BNP was >50 pg/mL.37) In addition, in patients with diabetes without cardiovascular disease who had elevated NT-proBNP levels, increased doses of renin-angiotensin-aldosterone system inhibitors and beta-blockers reduced cardiovascular events.38) Thus, natriuretic peptide-based screening tests and concomitant HF treatment are associated with a lower risk of LV dysfunction and HF.
(3) Diagnosis and differential diagnosis of HF
Measurement of natriuretic peptide levels is recommended as an initial test for diagnosing HF. In patients with non-acute suspected HF, if BNP <35 pg/mL or NT-proBNP <125 pg/mL, an extremely high negative prediction value of 0.94–0.98 possibly rules out HF.39,40) In patients with acute HF who visited the emergency room, a higher reference value can be applied to rule out HF (BNP <100 pg/mL or NT-proBNP <300 pg/mL).41,42) A study with 3,830 Korean patients at a single institution found that the sensitivity and specificity of BNP ≥108 pg/mL were 92.5% and 86.1%, respectively.43) However, natriuretic peptide values vary depending on the patient’s age and the presence of obesity and comorbidities. Clinicians should cautiously identify the non-HF and HF conditions that demonstrate high and low natriuretic peptide values, respectively (Table 4).44) Thus, HF should be ruled out or diagnosed using natriuretic peptide levels and the patient's symptoms, signs, and echocardiography findings.
Table 4. Clinical conditions with unusual natriuretic peptide level.
| Situations | Conditions |
|---|---|
| Conditions with high NP levels in patients without HF | Advanced age, anemia, stroke, chronic kidney disease, liver cirrhosis, acute coronary syndrome, chronic obstructive pulmonary disease, sepsis, and thyrotoxicosis |
| Conditions with low NP levels in patients with HF | Obesity, acute pulmonary edema, conditions with increased LA pressure and normal LV filling pressure (acute mitral regurgitation, mitral stenosis, and atrial fibrillation), and chronic compensated HF |
NP = natriuretic peptide; HF = heart failure; LA = left atrium; LV = left ventricular.
(4) Assessment of severity and prognosis of HF
Natriuretic peptide has a short half-life, which changes with hemodynamic stress or LV filling pressure, reflecting the severity of HF. A higher New York Heart Association functional classification or pulmonary congestion correlates with a higher concentration of natriuretic peptide.45) In the biomarker sub-study of the Val-HeFT study, HF-related readmissions and mortality increased significantly in the group with high BNP values. Mortality reportedly rose by 1.2% for every 10 pg/mL increase in BNP value.46) Natriuretic peptide concentrations measured at the beginning of hospitalization predicted in-hospital mortality, mortality within 30 days, and post-discharge mortality.47) Therefore, measuring natriuretic peptide concentrations is clinically useful for predicting severity and prognosis in patients with HF. Among BNP levels measured at various periods in hospitalized patients with HF, pre-discharge BNP measurement was the strongest predictor of readmission or mortality.48) Furthermore, the KorHF analysis in patients with acute HF revealed that NT-proBNP values predicted all-cause mortality.49) Therefore, pre-discharge BNP or NT-proBNP measurement helps predict post-discharge prognosis in patients with acute HF.
(5) Assessment of treatment response
Natriuretic peptide is an indicator of hemodynamic stimulation acting on the LV wall and is considered as a biochemical Swan-Ganz catheter; it has a role similar to that of HbA1c in diabetes or α-fetoprotein in hepatocellular carcinoma. Natriuretic peptide values decrease with guideline-directed medical therapy (GDMT) and these changes may associated with prognosis in patients with HF.46) In the PARADIGM-HF study, regardless of the treatment group, a decrease in natriuretic peptide values was associated with reduced HF-related cardiovascular mortality or readmissions.50) In addition, a post-drug treatment decrease in natriuretic peptide values was associated with reverse remodeling, such as increased cardiac output and decreased ventricular volume.51) However, the effectiveness of the strategy of modifying drug therapy in response to changes in natriuretic peptide values remains controversial.52) Therefore, further studies are needed to evaluate the cost-effectiveness of follow-up using natriuretic peptide levels to optimize drug dosages, ultimately aiming to improve the quality of life and mortality outcomes for patients with HF.
Other biomarkers
(1) Troponin
Troponin is a biomarker that indicates myocardial necrosis due to myocardial ischemia; however, it increases in other hemodynamically stressful conditions as well.53) Hemodynamic stress in HF causes myocardial damage and progressive myocardial necrosis. Troponin and BNP independently predicted in-hospitalization mortality in patients with HF.54) Recently, it has been indicated as a useful biomarker along with natriuretic peptides in the early detection of cardiotoxicity due to chemotherapy drugs.55)
(2) sST2
sST2 is a protein of the interleukin (IL)-1 receptor family that is secreted in response to mechanical strain of the myocardium or vessel. Soluble ST2 binds to IL-33 in the blood and interferes with the binding of IL-33 to ST2 ligands, which leads to myocardial cell death, fibrosis, and remodeling.56) Unlike natriuretic peptides, the concentration of sST2 does not vary according to obesity, age, atrial fibrillation, and renal diseases.57) Although sST2 is not helpful for the diagnosis of acute decompensated HF, it is a good predictor of the 1-year mortality and hospitalization in patients with HF.58)
(3) Galectin-3
Galectin-3, a beta-galactoside-binding lectin expressed by macrophages, is a regulator of tissue fibrosis. The combination of NT-proBNP and galectin-3 revealed an increased predictive value for HF-related mortality compared with NT-proBNP alone.59) In a meta-analyses, galectin-3 was associated with all-cause and cardiovascular mortalities, and revealed additional predictive power after adjusting for traditional risk factors.60)
(4) hs-CRP
A KorHF-registry analysis used hs-CRP as an indicator of systemic inflammation and reported that it was an independent predictor of mortality in patients with HF; increase in both NT-proBNP and hs-CRP levels was reportedly associated with a worse prognosis.61) Measurement of hs-CRP in addition to BNP and troponin revealed more accurate prediction of 30-day mortality compared with a single biomarker.62)
(5) GDF-15
GDF-15, a cytokine belonging to transforming growth factor-beta family, is a biomarker that increases in response to ventricular remodeling or myocardial inflammation.63) In the Val-HeFT study, after adjustment for BNP, hs-CRP, and troponin, GDF-15 predicted HF-related mortality and readmission.64) In addition, the PARADIGM-HF study revealed that baseline values of GDF-15 and its changes during treatment predicted HF-related mortality and hospitalization after adjusting for NT-proBNP levels, suggesting that natriuretic peptides do not reflect residual risk factors.65)
IMAGING TESTS FOR DIAGNOSING HF
1. During the process of diagnosing HF, transthoracic echocardiography is recommended to evaluate myocardial function. (Class I, Level of Evidence C)
2. Cardiac magnetic resonance (CMR) imaging is recommended to assess myocardial structure and function if a good quality image via transthoracic echocardiography cannot be obtained. (Class I, Level of Evidence C)
3. During the process of diagnosing HF, transthoracic echocardiography is recommended to assess the cause of HF. (Class I, Level of Evidence C)
4. Computed tomography coronary angiography may be beneficial in patients with low-to-intermediate pre-test probability or in cases where non-invasive stress test results are difficult to determine to rule out coronary artery disease, a cause of HF. (Class IIa, Level of Evidence C)
5. Invasive coronary angiography is recommended for patients with angina pectoris or symptomatic ventricular arrhythmias that persist even after drug treatment. (Class I, Level of Evidence B)
6. CMR imaging is recommended for characterization of myocardial tissue to identify the cause of HF. (Class I, Level of Evidence C)
7. CMR imaging using delayed gadolinium enhancement in dilated cardiomyopathy (DCM) may help distinguish between ischemic and non-ischemic myocardial injuries. (Class IIa, Level of Evidence C)
Assessment of cardiac function
Assessment of cardiac function is very important in diagnosing HF. The first recommended test is transthoracic echocardiography, and additional CMR imaging is sometimes performed.
(1) Echocardiography
The LVEF, assessed by echocardiography, is the most important diagnostic criteria for classifying HF. Moreover, accurate LVEF evaluation is important for indications for GDMT and non-pharmacological treatments such as implantable-cardioverter defibrillators and cardiac resynchronization therapy. LVEF is calculated as the difference between the volume of the LV at the end of diastolic and systolic phases divided by the volume at the end of diastolic phase.66) In addition to LVEF, LV global longitudinal strain (GLS), measured by speckle-tracking echocardiography, reflects subclinical myocardial systolic function. In Korean patients with HF, LV GLS exhibited incremental predictive value for long-term outcomes.67)
In addition, echocardiography helps assess the size of the ventricles and atria and wall thickness. Evaluation of diastolic function is essential in diagnosing HFpEF (elucidated in Chapter 7 of Part I). In patients with HF, RV dysfunction is often concomitant. Pressure or volume loads may affect RV function. The most common cause of chronic right HF is pulmonary HTN due to left-sided HF. Myocardial infarction, arrhythmogenic RV cardiomyopathy, or valvular disease may cause RV dysfunction as well. Echocardiographic parameters used to evaluate RV function include fractional area change, tricuspid annular plane systolic excursion, and tissue Doppler imaging of tricuspid annulus.66) The diagnosis of right-sided HF is elucidated in Part II, Chapter 26 (Diagnosis and treatment of right-sided heart failure).
(2) CMR imaging
CMR imaging may be performed to assess myocardial function. It has high accuracy and reproducibility; therefore, it is accepted as a gold standard for the assessment of volume, EF, and mass.68) Moreover, CMR imaging is recommended to assess the myocardial structure and function if echocardiographic imaging is of poor quality. In particular, CMR imaging is the most accurate method for measuring RV volume and EF.69)
Identifying the etiology of heart failure
Identifying the etiology of HF is essential for its treatment and prognosis prediction. The diverse causes of HF can be assessed through various imaging, blood, and genetic tests.
(1) Echocardiography
Echocardiography is the fundamental imaging test recommended to determine the cause of HF. It can assess RWMA, valvular structure and function, and myocardial thickness. If local RWMA is observed and it corresponds to a coronary artery territory, ischemic-origin HF may be suspected. If diffuse hypokinesia or non-coronary territory RWMA are observed, various cardiomyopathies (e.g., stress cardiomyopathy, sarcoidosis, and myocarditis among others) may be suspected (see Part II, Chapters 27–33). If structural and functional abnormalities of the valves are observed, HF caused by valvular heart disease may be suspected, and in such cases, surgery or percutaneous valve procedures should be considered (see Part II, Chapter 23: Treatment of valvular heart disease). Stress echocardiography with exercise or drugs such as dobutamine may be performed to evaluate the inducible myocardial ischemia or myocardial viability in patients considering coronary artery revascularization. It is also useful in evaluating changes in diastolic functional parameters during stress.70)
(2) Computed tomography coronary angiography and invasive coronary angiography
Computed tomography coronary angiography may help to rule out coronary artery disease in patients with low-to-intermediate pre-test probability, or in patients whose non-invasive stress test results are difficult to determine.71) Additionally, CT has the supplementary benefit of being able to investigate extracardiac structures such as the lung and thyroid. Invasive coronary angiography is recommended for patients with angina pectoris or refractory symptomatic ventricular arrhythmias that persist even after drug treatment.71)
(3) Cardiac magnetic resonance imaging
CMR imaging with myocardial perfusion and late gadolinium enhancement (LGE) help to identify the cause of HF by providing more information about the characteristics of myocardial tissue than echocardiography, and predict the prognosis.72) Therefore, CMR imaging is recommended for determining the cause of HF. LGE helps differentiate between ischemic and non-ischemic cardiomyopathies. The LGE pattern of ischemic cardiomyopathy is characterized by subendocardial or transmural involvement, and is consistent with coronary artery supply.73) Conversely, the LGE pattern of non-ischemic cardiomyopathy is characterized by subendocardial preservation and mid-wall or epicardial invasion; it does not coincide with the perfusion region of any coronary artery.74) Furthermore, it helps to differentiate non-ischemic cardiomyopathies. Hypertrophic cardiomyopathy (HCM) is characterized by the involvement of both the RV and interventricular septum, mainly in the mid-ventricular wall,75) and in the case of cardiac sarcoidosis, it is particularly characterized by the involvement of the mid or subepicardial basal septum.76) Cardiac amyloidosis has a characteristic LGE pattern of diffuse subendocardial ring enhancement. If the disease is considerably advanced, fibrosis may be increased in all cases of cardiomyopathy; thus, differential diagnoses with LGE may be difficult. Myocardial fibrosis provides a substrate for ventricular tachycardia in HF, and the presence of LGE and quantified values are predictors of increased occurrence of ventricular tachycardia.77)
In advanced diseases, fibrosis may increase in all cardiomyopathies, and differentiating the specific cardiomyopathy with the LGE pattern is challenging. Native T1 mapping and extracellular volume fraction (%) are helpful in such cases. Additionally, these values provide additional information as prognostic factors for HF.78) In myocarditis, LGE can be observed in various forms in an inflamed myocardium, and these can be confirmed by an increase in T2 value.79)
ROLE OF GENETIC TESTING IN DIAGNOSING HF (CARDIOMYOPATHY)
1. The family history of 3 or more generations of patients suspected of hereditary cardiomyopathy should be investigated. (Class I, Level of Evidence B)
2. Patients with suspected hereditary or familial cardiomyopathy should be advised genetic testing for identifying the cause of the disease. (Class I, Level of Evidence B)
3. All immediate family members (parents, siblings, and children) of patients with cardiomyopathy with a clear genetic mutation should undergo genetic testing. (Class I, Level of Evidence B)
Based on morphological characteristics, cardiomyopathy can be categorized as follows: congenital (hereditary/familial) and acquired (according to genetic mutations), DCM, HCM, and arrhythmogenic cardiomyopathy (AC). The incidence of DCM is 1:250–1:500, HCM is 1:500–1:5,000, and AC is 1:1,000–1:5,000.80,81) In Korea, cardiomyopathy is a leading cause of HF and accounts for the largest portion among diseases requiring heart transplantation.82) Direct causes of cardiomyopathy include gene mutations, toxins, autoimmunity, storage disease, infection, and tachycardia and disease modifiers that can aggravate the course of the disease include pregnancy and various cardiovascular comorbidities (HTN, diabetes, and hypothyroidism/hyperthyroidism among others). Gene mutations can be detected in approximately 40% of patients with DCM, 60% with HCM, and 15% with cardiomyopathy associated with chemotherapy, alcohol consumption, and childbirth (Table 5).2,83,84) However, genetic mutations can be detected in more than 10% of patients with DCM with unclear family history. Genetic testing can help predict the clinical prognosis of the disease and whether it will worsen. It may help decide the requirement of an implantable defibrillator and genetic consultation for families of patients with cardiomyopathy. All patients with DCM/HCM/AC should undergo genetic testing for determining a genetic cause. Moreover, all immediate family members (parents, siblings, and children) of patients with cardiomyopathy with clear genetic mutations should undergo genetic testing.2,85,86) The immediate family members of patients with DCM should undergo clinical examinations, including ECG and echocardiography, every 5 years, and more frequent examination is required if they are aged ≤50 years or if minor abnormalities are found (e.g., upper normal LV size, left ventricular hypertrophy [LVH] in ECG). The immediate family members of patients with HCM or AC should undergo clinical examinations, including ECG and echocardiography, every 2–5 years. They should be examined more frequently if minor abnormalities are found (e.g., mild LVH, mild RV enlargement, LVH or strain pattern in ECG).2,83,86)
Table 5. Causes, worsening factors, and phenotypes according to gene mutation in cardiomyopathy.
| Conditions | Cause | Worsening factor | Phenotype | |
|---|---|---|---|---|
| Gene mutation | ||||
| LMNA | × | × | DCM | |
| TTN* | × | DCM, (HCM) | ||
| RBM20 | × | DCM | ||
| MYH6* | × | DCM | ||
| MYH7* | × | DCM, HCM | ||
| MYPC | × | DCM, HCM | ||
| TNNT* | × | DCM, HCM | ||
| PLN | × | DCM, HCM, AC | ||
| DSP | × | × | AC, DCM, myocarditis | |
| TNNI3* | × | DCM | ||
| ABCC9* | × | DCM | ||
| TAZ* | × | DCM | ||
| SCN5a | × | × | AC, (DCM) | |
| Tropomyosin-1 | × | DCM | ||
| HFE, C282Y (hemochromatosis) | × | HCM, DCM | ||
| Galactosidase-A (fabry) | × | HCM | ||
| Neuromuscular disease | ||||
| Duchenne/becker muscular dystrophy, myotonic dystrophy syndrome | × | DCM | ||
| Mitochondria X-linked variant | × | DCM | ||
LMNA = lamin A/C; DCM = dilated cardiomyopathy; TTN = titin; HCM = hypertrophic cardiomyopathy; RBM20 = ribonucleic acid binding motif 20; MYH = myosin heavy chain; MYPC = myosin-binding protein C; TNNT = troponin-T; PLN = phospholamban; AC = arrhythmogenic cardiomyopathy; DSP = desmoplakin; TNNI = troponin I; SCN5a = sodium channel alpha unit 5; ABCC = ATP-binding cassette subfamily C; TAZ = tafazzin.
*Identified in a Korean study about gene mutation in patients with dilated cardiomyopathy.
DIAGNOSIS OF HEART FAILURE WITH PRESERVED EJECTION FRACTION
Diagnosis of HFpEF is challenging. Various diagnostic criteria have been proposed to date; however, the sensitivity and specificity of these criteria are unsatisfactory.87,88) Current diagnostic methods include score-based algorithms based on clinical characteristics, echocardiography, diastolic stress echocardiography, and invasive exercise stress catheterization for the differential diagnosis of HF and dyspnea due to other causes.5,89,90,91)
The following 3 diagnostic criteria for HFpEF must be met:
1) Symptoms and signs of HF
2) LV EF ≥50%
3) Objective evidence of structural or functional cardiac abnormalities consistent with LV diastolic dysfunction/increased LV filling pressure (including an increase in NT-proBNP or BNP levels)
Score-based diagnostic algorithms
The H2FPEF and HFA-PEFF scores are helpful in diagnosing HFpEF.92,93) Both scores classify a significant number of suspected patients as intermediate; hence, additional testing is needed for diagnosing HFpEF. Tables 6 and 7 presents 2 score-based algorithms that help diagnose HFpEF. However, although these algorithms are widely used, the diagnostic ambiguity of HFpEF remains. The H2FPEF score is a point-based algorithm that combines clinical risk factors and echocardiographic findings, whereas the HFA-PEFF score is a diagnostic algorithm based on objective results such as echocardiographic findings and biomarkers.
Table 6. Score-based diagnostic algorithm for heart failure with preserved ejection fraction: H2FPEF score92).
| Letter | Clinical variables | Values | Points |
|---|---|---|---|
| H2 | Heavy | Body mass index >30 kg/m2 | 2 |
| Hypertensive | Two or more anti-hypertensive agents | 1 | |
| F | Atrial fibrillation | Paroxysmal or persistent | 3 |
| P | Pulmonary hypertension | Doppler echocardiography measurement: pulmonary artery systolic pressure >35 mmHg | 1 |
| E | Elderly | Age >60 years | 1 |
| F | Filling pressure | Doppler echocardiography: E/e′ >9 | 1 |
| H2FPEF score | Total (0–9) |
Total score 
Probability of HFpEF 
HFpEF = heart failure with preserved ejection fraction.
Table 7. Score-based diagnostic algorithm for heart failure with preserved ejection fraction: HFA-PEFF score93).
| Criteria | Functional | Structural | Biomarker (sinus rhythm) | Biomarker (atrial fibrillation) |
|---|---|---|---|---|
| Major | Septal e′ <7 cm/s or lateral e′ <10 cm/s or average E/e′ ≥15 or TR velocity ≥2.8 m/s (PASP >35 mmHg) | LAVI >34 mL/m2 or LVMI >149/122 g/m2 (male/female) and RWT >0.42 | NT-proBNP >220 pg/mL or BNP >80 pg/mL | NT-proBNP >660 pg/mL or BNP >240 pg/mL |
| Minor | Average E/e′ 9–14 or GLS <16% | LAVI 29–34 mL/m2 or LVMI >115/95 g/m2 (male/female) or RWT >0.42 or LV wall thickness ≥12 mm | NT-proBNP 125–220 pg/mL or BNP 35–80 pg/mL | NT-proBNP 365–660 pg/mL or BNP 105–240 pg/mL |
| Major criteria: 2 points | ≥5 points: HFpEF | |||
| Minor criteria: 1 point | 2–4 points: diastolic stress test or invasive hemodynamic assessment | |||
TR = tricuspid regurgitation; PASP = pulmonary arterial systolic pressure; LAVI = left atrial volume index; LVMI = left ventricular mass index; RWT = relative wall thickness; NT-proBNP = N-terminal pro b-type natriuretic peptide; BNP = brain natriuretic peptide; GLS = global longitudinal strain; LV = left ventricle; HFpEF = heart failure with preserved ejection fraction.
Standard tests
The standard tests used to diagnose patients with HFpEF are NT-proBNP or BNP levels, chest radiography, ECG, and echocardiography. In particular, echocardiography should be used to confirm the evidence of left atrial enlargement (left atrial volume index >34 mL/m2 [sinus rhythm] and >40 mL/m2 [atrial fibrillation]) and evidence of LV hypertrophy (LV mass index ≥115 g/m2 [male], ≥95 g/m2 [female], relative wall thickness >0.42), which are indicators of chronic LV diastolic dysfunction. A resting tricuspid valve regurgitation velocity of >2.8 m/s (pulmonary artery systolic pressure >35 mmHg) is considered a major finding.
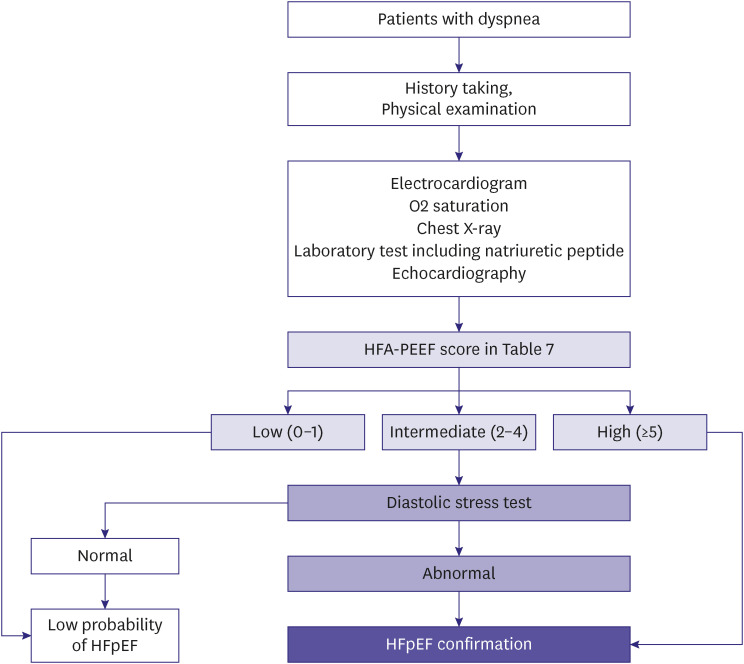
Diastolic stress test
If the diagnosis of HFpEF is inconclusive after standard tests, additional tests including cardiopulmonary exercise tests, exercise echocardiography, or invasive hemodynamic tests are recommended for a conclusive diagnosis. Figure 4 illustrates the recommended diagnostic algorithm for patients with dyspnea and suspected HFpEF.
Figure 4. Diagnostic algorithm of HFpEF.
BNP = B-type natriuretic peptide; ECG = electrocardiogram; HFpEF = heart failure with preserved ejection fraction.
If the HFA-PEFF score through echocardiography performed at rest and blood test is 2–4 points, diastolic stress test is recommended, in particular a non-invasive diastolic stress is preferred. However, if it is inconclusive, an invasive exercise hemodynamic test is recommended for evaluation. A diagnosis of HFpEF can be considered if diastolic stress echocardiography reveals E/e′ ≥15 and tricuspid regurgitation velocity >3.4 m/s, and invasive exercise hemodynamic measurements indicate a pulmonary capillary wedge pressure ≥15 mmHg at rest or >24 mmHg during exercise, or LV end-diastolic pressure ≥16 mmHg at rest. However, since such invasive exercise stress hemodynamic tests cannot be performed at several institutes, and because of the inherent risks of an invasive test, its clinical use remains limited.
CONCLUSION
In Part 1 of the guidelines, the definition, epidemiology, and diagnosis of HF have been discussed. The new definition of HF is crucial since patients with EF 40–49% are classified into HFmrEF, because the characteristics of this category are more similar to HFrEF than HFpEF. As the patient population with HF rapidly increases in Korea, HFpEF is frequently diagnosed. Furthermore, 2 score-based diagnostic algorithms for HFpEF have been covered in this part of the guidelines. Accurate diagnosis of HFpEF should be emphasized in this era of newer agents that help reduce HF-related cardiovascular mortality and hospitalization.
ACKNOWLEDGMENTS
This article has been published jointly, with consent, in both Korean Circulation Journal and International Journal of Heart Failure.
Also, the final version of this guideline was endorsed by Korean Society of Cardiology, Korean Society of Lipid and Atherosclerosis, Korean Association of Clinical Cardiology, Korean Society of Hypertension, Korean Society of Heart Failure, Korean Society of Echocardiography, Korean Society of Interventional Cardiology, Korean Heart Rhythm Society, and Korean Society of CardioMetabolic Syndrome.
Footnotes
Conflict of Interest: The authors have no financial conflicts of interest.
- Conceptualization: Cho HJ, Kang SM.
- Funding acquisition: Cho HJ, Yoo BS, Kang SM.
- Supervision: Cho HJ, Kang SM.
- Writing - original draft: Cho JY, Cho DH.
- Writing - review & editing: Youn JC, Kim D, Park SM, Jung MH, Hyun J, Choi J, Cho HJ, Park SM, Choi JO, Chung WJ, Yoo BS, Kang SM.
References
- 1.Kim KJ, Cho HJ, Kim MS, et al. Focused update of 2016 Korean Society of Heart Failure guidelines for the management of chronic heart failure. Int J Heart Fail. 2019;1:4–24. doi: 10.36628/ijhf.2019.0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McDonagh TA, Metra M, Adamo M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42:3599–3726. doi: 10.1093/eurheartj/ehab368. [DOI] [PubMed] [Google Scholar]
- 3.Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: Executive summary: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2022;79:1757–1780. doi: 10.1016/j.jacc.2021.12.011. [DOI] [PubMed] [Google Scholar]
- 4.Cho DH, Yoo BS. Current prevalence, incidence, and outcomes of heart failure with preserved ejection fraction. Heart Fail Clin. 2021;17:315–326. doi: 10.1016/j.hfc.2021.03.002. [DOI] [PubMed] [Google Scholar]
- 5.Shim CY. Heart failure with preserved ejection fraction: the major unmet need in cardiology. Korean Circ J. 2020;50:1051–1061. doi: 10.4070/kcj.2020.0338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Solomon SD, Claggett B, Lewis EF, et al. Influence of ejection fraction on outcomes and efficacy of spironolactone in patients with heart failure with preserved ejection fraction. Eur Heart J. 2016;37:455–462. doi: 10.1093/eurheartj/ehv464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Solomon SD, McMurray JJ, Anand IS, et al. Angiotensin-neprilysin inhibition in heart failure with preserved ejection fraction. N Engl J Med. 2019;381:1609–1620. doi: 10.1056/NEJMoa1908655. [DOI] [PubMed] [Google Scholar]
- 8.Lund LH, Claggett B, Liu J, et al. Heart failure with mid-range ejection fraction in CHARM: characteristics, outcomes and effect of candesartan across the entire ejection fraction spectrum. Eur J Heart Fail. 2018;20:1230–1239. doi: 10.1002/ejhf.1149. [DOI] [PubMed] [Google Scholar]
- 9.Lam CS, Solomon SD. Delivering therapeutic efficacy across the ejection fraction spectrum of heart failure. Circulation. 2022;146:1193–1195. doi: 10.1161/CIRCULATIONAHA.122.062022. [DOI] [PubMed] [Google Scholar]
- 10.Cho JH, Choe WS, Cho HJ, et al. Comparison of characteristics and 3-year outcomes in patients with acute heart failure with preserved, mid-range, and reduced ejection fraction. Circ J. 2019;83:347–356. doi: 10.1253/circj.CJ-18-0543. [DOI] [PubMed] [Google Scholar]
- 11.Arrigo M, Huber LC, Winnik S, et al. Right ventricular failure: pathophysiology, diagnosis and treatment. Card Fail Rev. 2019;5:140–146. doi: 10.15420/cfr.2019.15.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee HH, Cho SM, Lee H, et al. Korea heart disease fact sheet 2020: analysis of nationwide data. Korean Circ J. 2021;51:495–503. doi: 10.4070/kcj.2021.0097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kang SM. Key role of the Korean Society of Heart Failure: moving towards a global and individualized approach. Int J Heart Fail. 2022;4:136–138. doi: 10.36628/ijhf.2022.0014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yingchoncharoen T, Wu TC, Choi DJ, Ong TK, Liew HB, Cho MC. Economic burden of heart failure in Asian countries with different healthcare systems. Korean Circ J. 2021;51:681–693. doi: 10.4070/kcj.2021.0029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chung H, Sohn IS. Economic burden of heart failure in Asian countries based on real-world data. Korean Circ J. 2021;51:694–695. doi: 10.4070/kcj.2021.0197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cho SM, Lee H, Kim HC. Sex- and age-specific trends in cardiovascular health in Korea, 2007–2018. Korean Circ J. 2021;51:922–935. doi: 10.4070/kcj.2021.0211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cho DH, Lee CJ, Son JW, Choi J, Hwang J, Yoo BS. Temporal trends in heart failure over 11 years in the aging Korean population: a retrospective study using the national health insurance database. PLoS One. 2022;17:e0279541. doi: 10.1371/journal.pone.0279541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Krumholz HM, Chen YT, Wang Y, Vaccarino V, Radford MJ, Horwitz RI. Predictors of readmission among elderly survivors of admission with heart failure. Am Heart J. 2000;139:72–77. doi: 10.1016/s0002-8703(00)90311-9. [DOI] [PubMed] [Google Scholar]
- 19.Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics--2014 update: a report from the American Heart Association. Circulation. 2014;129:e28–292. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Heidenreich PA, Albert NM, Allen LA, et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6:606–619. doi: 10.1161/HHF.0b013e318291329a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Park JJ, Lee CJ, Park SJ, et al. Heart failure statistics in Korea, 2020: a report from the Korean Society of Heart Failure. Int J Heart Fail. 2021;3:224–236. doi: 10.36628/ijhf.2021.0023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim MS. The long journey to obtaining the epidemiological data of heart failure in Korea. Int J Heart Fail. 2021;3:221–223. doi: 10.36628/ijhf.2021.0036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lloyd-Jones DM, Larson MG, Leip EP, et al. Lifetime risk for developing congestive heart failure: the Framingham Heart Study. Circulation. 2002;106:3068–3072. doi: 10.1161/01.cir.0000039105.49749.6f. [DOI] [PubMed] [Google Scholar]
- 24.Lee JH, Lim NK, Cho MC, Park HY. Epidemiology of heart failure in Korea: present and future. Korean Circ J. 2016;46:658–664. doi: 10.4070/kcj.2016.46.5.658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Choi DJ, Han S, Jeon ES, et al. Characteristics, outcomes and predictors of long-term mortality for patients hospitalized for acute heart failure: a report from the Korean Heart Failure Registry. Korean Circ J. 2011;41:363–371. doi: 10.4070/kcj.2011.41.7.363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lee SE, Lee HY, Cho HJ, et al. Clinical characteristics and outcome of acute heart failure in Korea: results from the Korean Acute Heart Failure Registry (KorAHF) Korean Circ J. 2017;47:341–353. doi: 10.4070/kcj.2016.0419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee HY, Oh BH. Paradigm shifts of heart failure therapy: do we need another paradigm? Int J Heart Fail. 2020;2:145–156. doi: 10.36628/ijhf.2020.0010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mant J, Doust J, Roalfe A, et al. Systematic review and individual patient data meta-analysis of diagnosis of heart failure, with modelling of implications of different diagnostic strategies in primary care. Health Technol Assess. 2009;13:1–207. iii. doi: 10.3310/hta13320. [DOI] [PubMed] [Google Scholar]
- 29.Kelder JC, Cramer MJ, van Wijngaarden J, et al. The diagnostic value of physical examination and additional testing in primary care patients with suspected heart failure. Circulation. 2011;124:2865–2873. doi: 10.1161/CIRCULATIONAHA.111.019216. [DOI] [PubMed] [Google Scholar]
- 30.Lee KS, Noh J, Park SM, et al. Evaluation and management of patients with diabetes and heart failure: a Korean Diabetes Association and Korean Society of Heart Failure Consensus Statement. Int J Heart Fail. 2023;5:1–20. doi: 10.36628/ijhf.2022.0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gohar A, Rutten FH, den Ruijter H, et al. Mid-regional pro-atrial natriuretic peptide for the early detection of non-acute heart failure. Eur J Heart Fail. 2019;21:1219–1227. doi: 10.1002/ejhf.1495. [DOI] [PubMed] [Google Scholar]
- 32.Galderisi M, Cosyns B, Edvardsen T, et al. Standardization of adult transthoracic echocardiography reporting in agreement with recent chamber quantification, diastolic function, and heart valve disease recommendations: an expert consensus document of the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2017;18:1301–1310. doi: 10.1093/ehjci/jex244. [DOI] [PubMed] [Google Scholar]
- 33.Wettersten N. Biomarkers in acute heart failure: diagnosis, prognosis, and treatment. Int J Heart Fail. 2021;3:81–105. doi: 10.36628/ijhf.2020.0036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schellenberger U, O’Rear J, Guzzetta A, Jue RA, Protter AA, Pollitt NS. The precursor to B-type natriuretic peptide is an O-linked glycoprotein. Arch Biochem Biophys. 2006;451:160–166. doi: 10.1016/j.abb.2006.03.028. [DOI] [PubMed] [Google Scholar]
- 35.Langenickel TH, Dole WP. Angiotensin receptor-neprilysin inhibition with LCZ696: a novel approach for the treatment of heart failure. Drug Discov Today Ther Strateg. 2012;9:e131–e139. [Google Scholar]
- 36.Myhre PL, Vaduganathan M, Claggett B, et al. B-type natriuretic peptide during treatment with sacubitril/valsartan: the PARADIGM-HF trial. J Am Coll Cardiol. 2019;73:1264–1272. doi: 10.1016/j.jacc.2019.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ledwidge M, Gallagher J, Conlon C, et al. Natriuretic peptide-based screening and collaborative care for heart failure: the STOP-HF randomized trial. JAMA. 2013;310:66–74. doi: 10.1001/jama.2013.7588. [DOI] [PubMed] [Google Scholar]
- 38.Huelsmann M, Neuhold S, Resl M, et al. PONTIAC (NT-proBNP selected prevention of cardiac events in a population of diabetic patients without a history of cardiac disease): a prospective randomized controlled trial. J Am Coll Cardiol. 2013;62:1365–1372. doi: 10.1016/j.jacc.2013.05.069. [DOI] [PubMed] [Google Scholar]
- 39.Zaphiriou A, Robb S, Murray-Thomas T, et al. The diagnostic accuracy of plasma BNP and NTproBNP in patients referred from primary care with suspected heart failure: results of the UK natriuretic peptide study. Eur J Heart Fail. 2005;7:537–541. doi: 10.1016/j.ejheart.2005.01.022. [DOI] [PubMed] [Google Scholar]
- 40.Kelder JC, Cramer MJ, Verweij WM, Grobbee DE, Hoes AW. Clinical utility of three B-type natriuretic peptide assays for the initial diagnostic assessment of new slow-onset heart failure. J Card Fail. 2011;17:729–734. doi: 10.1016/j.cardfail.2011.04.013. [DOI] [PubMed] [Google Scholar]
- 41.Januzzi JL, Jr, Chen-Tournoux AA, Christenson RH, et al. N-terminal pro-B-type natriuretic peptide in the emergency department: the ICON-RELOADED study. J Am Coll Cardiol. 2018;71:1191–1200. doi: 10.1016/j.jacc.2018.01.021. [DOI] [PubMed] [Google Scholar]
- 42.Maisel A, Mueller C, Nowak R, et al. Mid-region pro-hormone markers for diagnosis and prognosis in acute dyspnea: results from the BACH (Biomarkers in Acute Heart Failure) trial. J Am Coll Cardiol. 2010;55:2062–2076. doi: 10.1016/j.jacc.2010.02.025. [DOI] [PubMed] [Google Scholar]
- 43.Yoo BS, Kim WJ, Jung HS, et al. The clinical experiences of B-type natriuretic peptide blood concentrations for diagnosis in congestive heart failure: the single hospital experience based on the large clinical database. Korean Circ J. 2004;34:684–692. [Google Scholar]
- 44.Maisel A, Mueller C, Adams K, Jr, et al. State of the art: using natriuretic peptide levels in clinical practice. Eur J Heart Fail. 2008;10:824–839. doi: 10.1016/j.ejheart.2008.07.014. [DOI] [PubMed] [Google Scholar]
- 45.Taub PR, Daniels LB, Maisel AS. Usefulness of B-type natriuretic peptide levels in predicting hemodynamic and clinical decompensation. Heart Fail Clin. 2009;5:169–175. doi: 10.1016/j.hfc.2008.11.009. [DOI] [PubMed] [Google Scholar]
- 46.Anand IS, Fisher LD, Chiang YT, et al. Changes in brain natriuretic peptide and norepinephrine over time and mortality and morbidity in the Valsartan Heart Failure Trial (Val-HeFT) Circulation. 2003;107:1278–1283. doi: 10.1161/01.cir.0000054164.99881.00. [DOI] [PubMed] [Google Scholar]
- 47.Lee DS, Stitt A, Austin PC, et al. Prediction of heart failure mortality in emergent care: a cohort study. Ann Intern Med. 2012;156:767–775. W-261, W-262. doi: 10.7326/0003-4819-156-11-201206050-00003. [DOI] [PubMed] [Google Scholar]
- 48.Logeart D, Thabut G, Jourdain P, et al. Predischarge B-type natriuretic peptide assay for identifying patients at high risk of re-admission after decompensated heart failure. J Am Coll Cardiol. 2004;43:635–641. doi: 10.1016/j.jacc.2003.09.044. [DOI] [PubMed] [Google Scholar]
- 49.Kang SH, Park JJ, Choi DJ, et al. Prognostic value of NT-proBNP in heart failure with preserved versus reduced EF. Heart. 2015;101:1881–1888. doi: 10.1136/heartjnl-2015-307782. [DOI] [PubMed] [Google Scholar]
- 50.Zile MR, Claggett BL, Prescott MF, et al. Prognostic implications of changes in N-terminal pro-B-type natriuretic peptide in patients with heart failure. J Am Coll Cardiol. 2016;68:2425–2436. doi: 10.1016/j.jacc.2016.09.931. [DOI] [PubMed] [Google Scholar]
- 51.Weiner RB, Baggish AL, Chen-Tournoux A, et al. Improvement in structural and functional echocardiographic parameters during chronic heart failure therapy guided by natriuretic peptides: mechanistic insights from the ProBNP Outpatient Tailored Chronic Heart Failure (PROTECT) study. Eur J Heart Fail. 2013;15:342–351. doi: 10.1093/eurjhf/hfs180. [DOI] [PubMed] [Google Scholar]
- 52.Felker GM, Anstrom KJ, Adams KF, et al. Effect of natriuretic peptide-guided therapy on hospitalization or cardiovascular mortality in high-risk patients with heart failure and reduced ejection fraction: a randomized clinical trial. JAMA. 2017;318:713–720. doi: 10.1001/jama.2017.10565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zanotti-Cavazzoni SL, Hollenberg SM. Cardiac dysfunction in severe sepsis and septic shock. Curr Opin Crit Care. 2009;15:392–397. doi: 10.1097/MCC.0b013e3283307a4e. [DOI] [PubMed] [Google Scholar]
- 54.Fonarow GC, Peacock WF, Horwich TB, et al. Usefulness of B-type natriuretic peptide and cardiac troponin levels to predict in-hospital mortality from ADHERE. Am J Cardiol. 2008;101:231–237. doi: 10.1016/j.amjcard.2007.07.066. [DOI] [PubMed] [Google Scholar]
- 55.Michel L, Mincu RI, Mahabadi AA, et al. Troponins and brain natriuretic peptides for the prediction of cardiotoxicity in cancer patients: a meta-analysis. Eur J Heart Fail. 2020;22:350–361. doi: 10.1002/ejhf.1631. [DOI] [PubMed] [Google Scholar]
- 56.Lee J, Kim EJ. ST2 as a biomarker to show the preventive effect of exercise in myocardial injury by doxorubicin? Int J Heart Fail. 2021;3:117–120. doi: 10.36628/ijhf.2021.0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hu SS, Kong LZ, Gao RL, et al. Outline of the report on cardiovascular disease in China, 2010. Biomed Environ Sci. 2012;25:251–256. doi: 10.3967/0895-3988.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 58.Aimo A, Vergaro G, Passino C, et al. Prognostic value of soluble suppression of tumorigenicity-2 in chronic heart failure: a meta-analysis. JACC Heart Fail. 2017;5:280–286. doi: 10.1016/j.jchf.2016.09.010. [DOI] [PubMed] [Google Scholar]
- 59.van Kimmenade RR, Januzzi JL, Jr, Ellinor PT, et al. Utility of amino-terminal pro-brain natriuretic peptide, galectin-3, and apelin for the evaluation of patients with acute heart failure. J Am Coll Cardiol. 2006;48:1217–1224. doi: 10.1016/j.jacc.2006.03.061. [DOI] [PubMed] [Google Scholar]
- 60.Imran TF, Shin HJ, Mathenge N, et al. Meta-analysis of the usefulness of plasma galectin-3 to predict the risk of mortality in patients with heart failure and in the general population. Am J Cardiol. 2017;119:57–64. doi: 10.1016/j.amjcard.2016.09.019. [DOI] [PubMed] [Google Scholar]
- 61.Park JJ, Choi DJ, Yoon CH, et al. Prognostic value of C-reactive protein as an inflammatory and N-terminal probrain natriuretic peptide as a neurohumoral marker in acute heart failure (from the Korean Heart Failure registry) Am J Cardiol. 2014;113:511–517. doi: 10.1016/j.amjcard.2013.10.022. [DOI] [PubMed] [Google Scholar]
- 62.Zairis MN, Tsiaousis GZ, Georgilas AT, et al. Multimarker strategy for the prediction of 31 days cardiac death in patients with acutely decompensated chronic heart failure. Int J Cardiol. 2010;141:284–290. doi: 10.1016/j.ijcard.2008.12.017. [DOI] [PubMed] [Google Scholar]
- 63.Cho DH, Son JW, Lee CJ, et al. Prognostic value of short-term follow-up of multiple biomarkers after discharge in hospitalized patients with acute heart failure (POSTBIO-HF): rationale and study design. Int J Heart Fail. 2022;4:110–116. doi: 10.36628/ijhf.2022.0005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Anand IS, Kempf T, Rector TS, et al. Serial measurement of growth-differentiation factor-15 in heart failure: relation to disease severity and prognosis in the Valsartan Heart Failure Trial. Circulation. 2010;122:1387–1395. doi: 10.1161/CIRCULATIONAHA.109.928846. [DOI] [PubMed] [Google Scholar]
- 65.Bouabdallaoui N, Claggett B, Zile MR, et al. Growth differentiation factor-15 is not modified by sacubitril/valsartan and is an independent marker of risk in patients with heart failure and reduced ejection fraction: the PARADIGM-HF trial. Eur J Heart Fail. 2018;20:1701–1709. doi: 10.1002/ejhf.1301. [DOI] [PubMed] [Google Scholar]
- 66.Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28:1–39.e14. doi: 10.1016/j.echo.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 67.Park JJ, Park JB, Park JH, Cho GY. Global longitudinal strain to predict mortality in patients with acute heart failure. J Am Coll Cardiol. 2018;71:1947–1957. doi: 10.1016/j.jacc.2018.02.064. [DOI] [PubMed] [Google Scholar]
- 68.Yoon YE, Hong YJ, Kim HK, et al. 2014 Korean guidelines for appropriate utilization of cardiovascular magnetic resonance imaging: a joint report of the Korean Society of Cardiology and the Korean Society of Radiology. Korean Circ J. 2014;44:359–385. doi: 10.4070/kcj.2014.44.6.359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sugeng L, Mor-Avi V, Weinert L, et al. Multimodality comparison of quantitative volumetric analysis of the right ventricle. JACC Cardiovasc Imaging. 2010;3:10–18. doi: 10.1016/j.jcmg.2009.09.017. [DOI] [PubMed] [Google Scholar]
- 70.Sicari R, Nihoyannopoulos P, Evangelista A, et al. Stress echocardiography expert consensus statement--executive summary: European Association of Echocardiography (EAE) (a registered branch of the ESC) Eur Heart J. 2009;30:278–289. doi: 10.1093/eurheartj/ehn492. [DOI] [PubMed] [Google Scholar]
- 71.Knuuti J, Wijns W, Saraste A, et al. 2019 ESC guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020;41:407–477. doi: 10.1093/eurheartj/ehz425. [DOI] [PubMed] [Google Scholar]
- 72.Valle-Muñoz A, Estornell-Erill J, Soriano-Navarro CJ, et al. Late gadolinium enhancement-cardiovascular magnetic resonance identifies coronary artery disease as the aetiology of left ventricular dysfunction in acute new-onset congestive heart failure. Eur J Echocardiogr. 2009;10:968–974. doi: 10.1093/ejechocard/jep115. [DOI] [PubMed] [Google Scholar]
- 73.Hamilton-Craig C, Strugnell WE, Raffel OC, Porto I, Walters DL, Slaughter RE. CT angiography with cardiac MRI: non-invasive functional and anatomical assessment for the etiology in newly diagnosed heart failure. Int J Cardiovasc Imaging. 2012;28:1111–1122. doi: 10.1007/s10554-011-9926-y. [DOI] [PubMed] [Google Scholar]
- 74.Mahrholdt H, Wagner A, Judd RM, Sechtem U, Kim RJ. Delayed enhancement cardiovascular magnetic resonance assessment of non-ischaemic cardiomyopathies. Eur Heart J. 2005;26:1461–1474. doi: 10.1093/eurheartj/ehi258. [DOI] [PubMed] [Google Scholar]
- 75.Choudhury L, Mahrholdt H, Wagner A, et al. Myocardial scarring in asymptomatic or mildly symptomatic patients with hypertrophic cardiomyopathy. J Am Coll Cardiol. 2002;40:2156–2164. doi: 10.1016/s0735-1097(02)02602-5. [DOI] [PubMed] [Google Scholar]
- 76.Patel MR, Cawley PJ, Heitner JF, et al. Detection of myocardial damage in patients with sarcoidosis. Circulation. 2009;120:1969–1977. doi: 10.1161/CIRCULATIONAHA.109.851352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Gao P, Yee R, Gula L, et al. Prediction of arrhythmic events in ischemic and dilated cardiomyopathy patients referred for implantable cardiac defibrillator: evaluation of multiple scar quantification measures for late gadolinium enhancement magnetic resonance imaging. Circ Cardiovasc Imaging. 2012;5:448–456. doi: 10.1161/CIRCIMAGING.111.971549. [DOI] [PubMed] [Google Scholar]
- 78.Puntmann VO, Carr-White G, Jabbour A, et al. T1-mapping and outcome in nonischemic cardiomyopathy: all-cause mortality and heart failure. JACC Cardiovasc Imaging. 2016;9:40–50. doi: 10.1016/j.jcmg.2015.12.001. [DOI] [PubMed] [Google Scholar]
- 79.Ferreira VM, Schulz-Menger J, Holmvang G, et al. Cardiovascular magnetic resonance in nonischemic myocardial inflammation: expert recommendations. J Am Coll Cardiol. 2018;72:3158–3176. doi: 10.1016/j.jacc.2018.09.072. [DOI] [PubMed] [Google Scholar]
- 80.Seferović PM, Polovina M, Bauersachs J, et al. Heart failure in cardiomyopathies: a position paper from the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2019;21:553–576. doi: 10.1002/ejhf.1461. [DOI] [PubMed] [Google Scholar]
- 81.Authors/Task Force members. Elliott PM, Anastasakis A, et al. 2014 ESC guidelines on diagnosis and management of hypertrophic cardiomyopathy. Eur Heart J. 2014;35:2733–2779. doi: 10.1093/eurheartj/ehu284. [DOI] [PubMed] [Google Scholar]
- 82.Lee HY, Jeon ES, Kang SM, Kim JJ. Initial report of the Korean Organ Transplant Registry (KOTRY): heart transplantation. Korean Circ J. 2017;47:868–876. doi: 10.4070/kcj.2016.0403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hershberger RE, Givertz MM, Ho CY, et al. Genetic evaluation of cardiomyopathy-a Heart Failure Society of America practice guideline. J Card Fail. 2018;24:281–302. doi: 10.1016/j.cardfail.2018.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Park HY. Hereditary dilated cardiomyopathy: recent advances in genetic diagnostics. Korean Circ J. 2017;47:291–298. doi: 10.4070/kcj.2016.0017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Tayal U, Ware JS, Lakdawala NK, Heymans S, Prasad SK. Understanding the genetics of adult-onset dilated cardiomyopathy: what a clinician needs to know. Eur Heart J. 2021;42:2384–2396. doi: 10.1093/eurheartj/ehab286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Yogasundaram H, Alhumaid W, Dzwiniel T, Christian S, Oudit GY. Cardiomyopathies and genetic testing in heart failure: role in defining phenotype-targeted approaches and management. Can J Cardiol. 2021;37:547–559. doi: 10.1016/j.cjca.2021.01.016. [DOI] [PubMed] [Google Scholar]
- 87.Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC): developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37:2129–2200. doi: 10.1093/eurheartj/ehw128. [DOI] [PubMed] [Google Scholar]
- 88.Yancy CW, Jessup M, Bozkurt B, et al. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation. 2017;136:e137–e161. doi: 10.1161/CIR.0000000000000509. [DOI] [PubMed] [Google Scholar]
- 89.Obokata M, Kane GC, Reddy YN, Olson TP, Melenovsky V, Borlaug BA. Role of diastolic stress testing in the evaluation for heart failure with preserved ejection fraction: a simultaneous invasive-echocardiographic study. Circulation. 2017;135:825–838. doi: 10.1161/CIRCULATIONAHA.116.024822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ha JW, Andersen OS, Smiseth OA. Diastolic stress test: invasive and noninvasive testing. JACC Cardiovasc Imaging. 2020;13:272–282. doi: 10.1016/j.jcmg.2019.01.037. [DOI] [PubMed] [Google Scholar]
- 91.Shim CY. Stress testing in heart failure with preserved ejection fraction. Heart Fail Clin. 2021;17:435–445. doi: 10.1016/j.hfc.2021.02.007. [DOI] [PubMed] [Google Scholar]
- 92.Reddy YN, Carter RE, Obokata M, Redfield MM, Borlaug BA. A simple, evidence-based approach to help guide diagnosis of heart failure with preserved ejection fraction. Circulation. 2018;138:861–870. doi: 10.1161/CIRCULATIONAHA.118.034646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Pieske B, Tschöpe C, de Boer RA, et al. How to diagnose heart failure with preserved ejection fraction: the HFA-PEFF diagnostic algorithm: a consensus recommendation from the Heart Failure Association (HFA) of the European Society of Cardiology (ESC) Eur J Heart Fail. 2020;22:391–412. doi: 10.1002/ejhf.1741. [DOI] [PubMed] [Google Scholar]