Take Home Message
Our review shows that magnetic stents are superior to traditional stents in terms of removal efficiency and comfort, despite the relatively high risk of some complications after removal.
Keywords: Magnetic stent, Ureteral stent, Meta-analysis, Ureteral Stent Symptom Questionnaire, Visual Analog Scale
Abstract
Context
The incidence of urolithiasis is increasing year by year. Ureteral stents are a popular treatment option for this condition. Efforts to improve the material and structure of stents to increase comfort and reduce complications have led to the introduction of magnetic stents.
Objective
To evaluate differences in removal efficiency and safety for magnetic and conventional stents.
Evidence acquisition
This study was conducted and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). Data were extracted according to the PRISMA principles. We collected and combined data from randomized controlled trials on magnetic versus conventional stents to evaluate the efficiency of their removal and the associated effects. Data synthesis was performed using RevMan 5.4.1 and heterogeneity was evaluated using I2 tests. A sensitivity analysis was also performed. Key metrics included the stent removal time, Visual Analog Scale (VAS) pain scores, and Ureteral Stent Symptom Questionnaire (USSQ) scores for various domains.
Evidence synthesis
Seven studies were included in the review. We found that magnetic stents had a shorter removal time (mean difference [MD] −8.28 min, 95% confidence interval [CI] −15.6 to −0.95; p = 0.03) and their removal was associated with less pain (MD −3.01 points, 95% CI −3.83 to −2.19; p < 0.01) in comparison to conventional stents. USSQ scores for urinary symptoms and sexual matters were higher for magnetic than for conventional stents. There were no other differences between the stent types.
Conclusions
Magnetic ureteral stents have the advantages of a shorter removal time, less pain during removal, and low cost in comparison to conventional stents.
Patient summary
For patients undergoing treatment of urinary stones, a thin tube called a stent is often temporarily inserted in the tube between the kidney and the bladder to allow stones to pass. Magnetic stents can be removed without any need for a second surgical procedure. Our review of studies comparing two types of stents suggests that magnetic stents are superior to conventional stents in terms of efficiency and comfort during removal.
1. Introduction
Clinicians had used a range of treatment methods for different kidney stone conditions until the ureteral stent was introduced by Finney [1]. Since then, stents have become hugely popular in urological surgery. Stents allow urine to pass through sites of stenosis while the ureter and anastomosis are healing, and facilitate unobstructed flow through the ureter in cases involving edema [2]. Silicone and polyurethane excelled in many material tests and became the most commonly used materials [3]. Given technological advances, there are many aspects of stent technology that are still improving, including materials used and stent coating [4]. However, when the stent is removed, pain and adverse events, such as hematuria and incomplete bladder emptying, are common [2], [5]. Stents have an important impact on quality of life, so stent modifications and improvements to optimize quality of life after treatment are ongoing [6]. The method for stent insertion is standard, but the method for removal is an area of active research; for example, magnets can be placed on the tail of the stent, referred to as a magnetic stent, to facilitate removal [7].
The first magnetic stent was invented in 1989 to reduce the difficulty and pain associated with stent removal, but its poor performance prevented widespread use in surgery [8]. A magnetic cylinder is attached to the distal end of a standard ureteral stent with a string, which should perfectly connect to the retrieval device [9]. Widespread unfamiliarity with their operation and uncertainty regarding their efficacy have hindered the application of and improvements in magnetic stents [10].
The aim of our study was to review the literature on comparisons of magnetic and traditional stents in terms of their removal and the incidence of postoperative symptoms.
2. Data acquisition
This study is reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).
2.1. Study selection
To identify relevant studies, we searched the PubMed, Embase, and other databases using “magnetic ureteral stent” and “magnetic double J” as keywords. During the screening process, we used the Patient/Population, Intervention, Comparator, Outcome, and Study design (PICOS) principles to select studies [11]. Our criteria were as follows: (1) Population (P): adult patients with kidney stones; (2) Intervention (I): magnetic double-J stent; (3) Comparator (C): conventional double-J stent; (4) Outcome (O): operative and postoperative results for stent removal; and (5) Study design (S): comparative studies.
The review included studies comparing data for magnetic and conventional ureteral stents for kidney stone conditions. The following publications were excluded: (1) studies not related to magnetic ureteral stents; and (2) studies with no specific data comparisons. We also excluded conference papers, comments, and letters. Figure 1 provides more details on the study selection process.
Fig. 1.
Flowchart of study selection for inclusion in the review.
2.2. Screening of publications
Two authors screened the publications according to the above criteria according to the title, abstract, and full text of each article to decide whether the study should be included.
2.3. Quality assessment
The methodological quality of all randomized controlled trials (RCTs) was assessed using Jadad scores, and that of the non-RCTs was assessed using the Newcastle Ottawa Scale.
2.4. Outcome measures
The aim of this meta-analysis was to assess differences in the efficiency and safety of stent removal between magnetic and conventional stents. We chose removal time and pain during removal, assessed using the Visual Analog Scale (VAS), as outcome measures. We also measured postoperative symptoms related to the two stent types in terms of Ureteral Stent Symptom Questionnaire (USSQ) scores for various domains.
2.5. Data pooling and analysis
RevMan 5.4.1 software (Cochrane Collaboration, London, UK) was used for data synthesis. Differences were considered statistically significant at p < 0.05, and 95% confidence intervals (CIs) are reported for the pooled results. The mean differences (MD) for relevant data were combined and analyzed. The I2 test was used to test for heterogeneity; if I2 was >50%, heterogeneity was considered significant, and a random-effects model was used. Sensitivity analyses in which studies were excluded in turn were used to determine whether each meta-analysis was stable. Forest plots are used to illustrate the results.
3. Evidence synthesis
3.1. Study selection
Table 1 lists the seven studies included in the final sample [12], [13], [14], [15], [16], [17], [18], of which five were RCTs and two were observational case-control studies. Six studies used Black-Star (Urotech, Achenmuehle, Germany) magnetic stents and one used a new type of magnetic stent made in China (Chinese patent number ZL201730073344.X). The brand of the conventional stents varied by and included Urotech, OptiMed, and Cook Universa devices; some studies did not even mention the brand name. Conventional stent materials in the studies included polyurethane, Percuflex, and unspecified materials. The stent size, whether magnetic or conventional, ranged from 4.8 Fr to 7 Fr.
Table 1.
Characteristics of studies included in the review
| Study, publication year, and country |
Design | Mean age (yr) | Sample size (n) | Condition | Intervention | Control | Outcome assessment |
|---|---|---|---|---|---|---|---|
| Rassweiler [12] 2017, Germany |
RCT | 48 | 35 | Urolithiasis | Magnetic DJS | Standard DJS | Removal time VAS on removal |
| Diranzo-Garcia [13] 2021, Spain |
RCT | 55 | 46 | Urolithiasis | Magnetic DJS | Standard DJS | USSQ score Removal time VAS on removal |
| Kapoor [14] 2020, Canada |
RCT | 60 | 41 | Urolithiasis | Magnetic DJS | Standard DJS | USSQ score Removal time |
| Farouk [15] 2019, Egypt |
RCT | 31 | 50 | Urolithiasis | Magnetic DJS | Standard DJS | USSQ score |
| O’Kelly [16] 2019, Ireland |
OCC | 48 | 100 | Urolithiasis | Magnetic DJS | Standard DJS | USSQ score VAS on removal |
| Sevcenco [17] 2017, Germany |
OCC | 50 | 163 | Urolithiasis | Magnetic DJS | Standard DJS | VAS on removal |
| Zeng [18] 2022, China |
RCT | 45 | 333 | Urolithiasis | Magnetic DJS | Standard DJS | USSQ score VAS on removal |
DJS = double-J stent; OCC = observational case-control study; RCT = randomized controlled trial; USSQ = Ureteral Stent Symptom Questionnaire; VAS = Visual Analog Scale for pain.
Supplementary Figure 1 shows the results for the risk-of-bias assessment.
3.2. Time to remove magnetic versus conventional stents
Data on the time taken to remove the magnetic versus the conventional stents were available for 147 patients. Synthesis revealed a significant difference between the stent types (MD −8.28 min, 95% CI −15.6 to −0.95; p = 0.03), but heterogeneity was evident (I2 = 96%; p < 0.001). The sensitivity analysis showed that there was no significant heterogeneity if the study by Kapoor et al. [14] was excluded (I2 = 0%, p = 0.35). On the basis of these results, we decided not to include the data from this study, leaving data for 106 patients in the final data set. This led to stable results without significant heterogeneity (MD −11.19 min, 95% CI −13.55 to −8.84; p < 0.01; Fig. 2A).
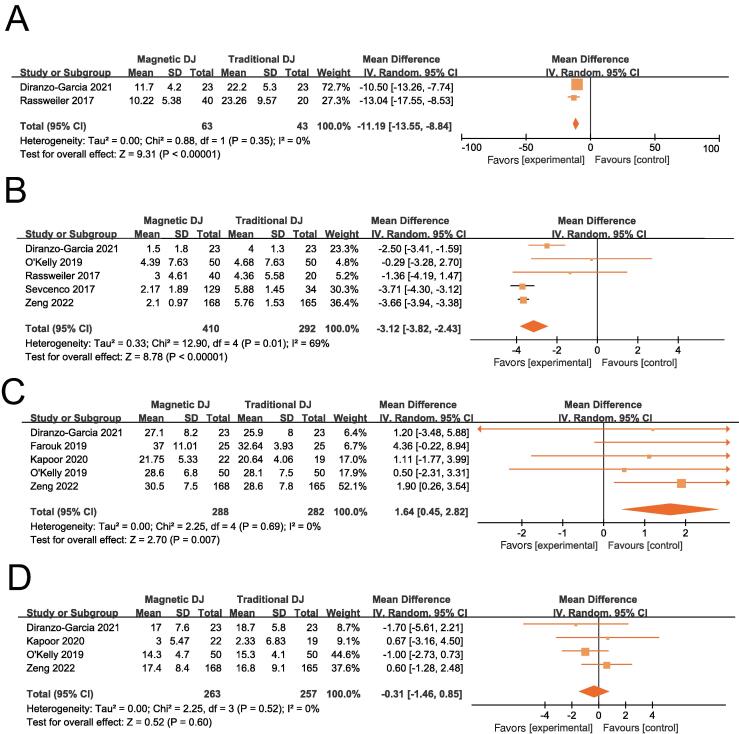
Fig. 2.
Forest plots for (A) the stent removal time after excluding the study by Kapoor et al. [14]; (B) the VAS pain score during stent removal; (C) the USSQ urinary symptoms score; and (D) the USSQ pain score after excluding the study by Farouk et al. [15]. CI = confidence interval; df = degrees of freedom; DJ = double-J stent; IV = inverse variance; SD = standard deviation; USSQ = Ureteral Stent Symptom Questionnaire; VAS = Visual Analog Scale.
3.3. VAS pain score for stent removal
Data on the pain associated with removal of magnetic versus conventional stents were available for 702 patients. Synthesis revealed a significant difference in score between the stent types (MD −3.12 points, 95% CI −3.82 to −2.43; p < 0.01), but heterogeneity was apparent (I2 = 69%, p = 0.01; Fig. 2B). Sensitivity analysis showed that although the results were stable after removing individual studies, significant heterogeneity still existed (Table 2). We also conducted subgroup analyses according to the magnetic stent brand and the material and size of conventional stents, as shown in Table 3.
Table 2.
Sensitivity analysis for the safety meta-analysis: estimates of the VAS pain score on stent removal
| Study omitted | VAS estimate (95% CI) |
|---|---|
| Diranzo-Garcia [13] | −3.23 (−4.12 to −2.34) |
| O’Kelly [16] | −3.25 (−3.96 to −2.54) |
| Rassweiler [12] | −3.15 (−3.96 to −2.34) |
| Sevcenco [17] | −2.56 (−3.79 to −1.33) |
| Zeng [18] | −2.53 (−3.75 to −1.31) |
CI = confidence interval; VAS = Visual Analog Scale.
Table 3.
Subgroup analyses for efficacy
| Variable | Heterogeneity | p value for difference | |||
|---|---|---|---|---|---|
| Studies (n) | I2 (%) | p value | OR (95% CI) | ||
| Efficacy | 5 | ||||
| Magnetic stent brand | |||||
| Black-Star | 4 | 71 | 0.02 | −2.55 (−3.79 to −1.31) | <0.00001 |
| New Chinese version | 1 | – | – | −3.66 (−3.94 to −3.38) | <0.00001 |
| Conventional stent material | |||||
| Polyurethane | 4 | 71 | 0.02 | −2.55 (−3.79 to −1.31) | <0.00001 |
| Unknown | 1 | – | – | −3.66 (−3.94 to −3.38) | <0.00001 |
| Conventional stent size | |||||
| 7 Fr | 2 | 61 | 0.11 | −2.96 (−5.11 to −0.81) | 0.007 |
| 6 Fr | 1 | – | – | −2.50 (−3.41 to −1.59) | <0.00001 |
| Unknown | 2 | 79 | 0.03 | −2.32 (−5.55 to 0.92) | 0.16 |
CI = confidence interval; OR = odds ratio.
3.4. USSQ scores for urinary symptoms
Data on urinary symptoms associated with removal of magnetic versus conventional stents were available for 570 patients. Synthesis revealed a statistically significant difference in score between the stent types (MD 1.64 points, 95% CI 0.45–2.82; p = 0.007). No heterogeneity was observed (I2 = 0%; p = 0.69; Fig. 2C).
3.5. USSQ scores for pain
Data on the pain associated with removal of magnetic versus conventional stents were available for 570 patients. Synthesis revealed no statistically significant difference in score (MD 1.17 points, 95% CI −1.59 to 3.93; p = 0.41), but heterogeneity was apparent (I2 = 81%; p = 0.0003). Sensitivity analysis showed that no significant heterogeneity was evident if the study by Farouk et al. [15] was removed (I2 = 0%; p = 0.52). Exclusion of data from this study left data for 520 patients in the final data set. This led to stable results without significant heterogeneity (MD −0.31 points, 95% CI −1.46 to −0.85; p = 0.60; Fig. 2D).
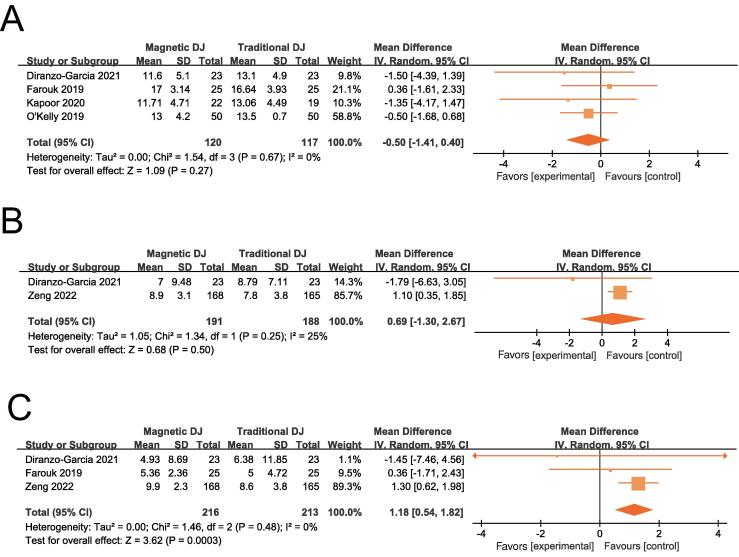
3.6. USSQ scores for general health
Data on general health associated with removal of magnetic versus conventional stents were available for 570 patients. Synthesis revealed no significant difference in score between the stent types (MD 0.41 points, 95% CI −1.79 to 2.62; p = 0.71), but heterogeneity was apparent (I2 = 84%; p < 0.0001). Sensitivity analysis showed that no significant heterogeneity was evident if the study by Zeng et al. [18] was removed (I2 = 0%; p = 0.67). Therefore, data from this study were excluded, leaving data for 237 patients in the final data set. This led to stable results without significant heterogeneity (MD −0.50 points, 95% CI −1.41 to −0.40; p = 0.27; Fig. 3A).
Fig. 3.
Forest plots for (A) the USSQ general health score after excluding the study by Zeng et al., 2022 [18]; (B) the USSQ work performance score after excluding the study by Farouk et al. [15]; and (C) the USSQ sexual matters score. CI = confidence interval; df = degrees of freedom; DJ = double-J stent; IV = inverse variance; SD = standard deviation; USSQ = Ureteral Stent Symptom Questionnaire.
3.7. USSQ scores for work performance
Data on work performance associated with removal of magnetic versus conventional stents were available for 429 patients. Synthesis revealed no significant difference in score between the stent types (MD 3.78 points, 95% CI −4.06 to 11.62; p = 0.35), but heterogeneity was apparent (I2 = 97%; p < 0.0001). Sensitivity analysis showed no significant heterogeneity if the study by Farouk et al. [15] was excluded (I2 = 25%; p = 0.25). Therefore, we decided to exclude data from this study, leaving data for 379 patients in the final data set. This led to stable results without significant heterogeneity (MD 0.69 points, 95% CI −1.30 to 2.67; p = 0.50; Fig. 3B).
3.8. USSQ scores for sexual matters
Data on scores for the sexual matters USSQ domain following removal of magnetic versus conventional stents were available for 429 patients. Synthesis revealed no significant difference in score between the stent types (MD 1.18 points, 95% CI 0.54–1.82; p = 0.003) and there was no heterogeneity (I2 = 0%, p = 0.48; Fig. 3C).
3.9. Discussion
Many international urological associations consider stent placement an indispensable step in urological surgery [19]. Even though conventional stents are widely used worldwide, there is no perfect solution for addressing the pain resulting from their placement and removal. Aside from removal with strings, the use of stent forceps during flexible cystoscopy is the most common procedure for removing stents; this procedure not only causes discomfort and pain for patients, but also requires high-level operator skill and high-quality surgical instruments [20]. Increasingly, nonendoscopic techniques for stent removal are attracting attention. Several studies have reported that magnetic stents prevent urinary symptoms after kidney transplantation and urolithiasis treatment [21], [22]. Taylor and McDougall [23] conducted the first study demonstrating the feasibility of nonendoscopic removal of magnetic stents. At present, the Black-Star stent is the magnetic stent most widely used in clinical practice [9]. Magnetic mounts also have advantages in terms of cost and operation. The magnetic option reduces the resources required for removal and thus the cost of the procedure [24], [25]. In addition, magnetic stent removal can be performed safely in an outpatient setting rather than in an operating room [9]. However, there are some cases for which it is difficult to remove a magnetic stent; flexible cystoscopy is very effective in these cases [9], [21].
The pain and postoperative symptoms caused by the two types of stent also require attention. It is well known that there is a high chance of symptoms such as nocturia, hematuria, and incontinence in patients with a stent [26], [27], [28], [29]. To this end, various improvements have been made, but their effects have been very limited [30].
Our study compared magnetic and conventional stents. We noted a shorter removal time and lower pain during removal for magnetic stents in comparison to conventional stents. For pain assessment, we used VAS scores (10-point scale). Multiple studies have reported no significant differences between magnetic and conventional stents in terms of USSQ scores for postoperative symptoms and quality of life [31], [32]. Although we found no differences in USSQ scores for pain, general health, and work performance, our results for USSQ domain scores for urinary symptoms and sexual matters were variable, with magnetic stents scoring higher than conventional stents. This may be one of the reasons why magnetic stents cannot completely replace conventional stents. Interestingly, no silicone stents were used in the studies included in our review, but Barghouthy et al. [33] and Wiseman et al. [34] considered that silicone-hydrocoated ureteral stents might be more tolerable than other stents, which can be regarded as a direction for future research and comparison and is worthy of further discussion.
The evidence suggesting a shorter removal time and less pain for magnetic stents would result in a better treatment experience for patients, which is also likely to reduce doctor-patient conflicts to some extent. The small difference in postoperative USSQ scores also dispels safety concerns.
The main limitation of our study is the small sample size, which is a shortcoming given the significant heterogeneity associated with syntheses of VAS scores for small sample sizes. In addition, the different stent brands, materials, and sizes used contribute a degree of variability to pooled results. Moreover, the different cutoffs for USSQ results in different countries add to the heterogeneity.
4. Conclusions
Magnetic stents have the advantages of a shorter removal time and less pain in comparison to conventional stents. However, postoperative urinary symptoms and side effect related sexually activity need to be considered.
Author contributions: Xi Jin had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Ma.
Acquisition of data: Cheng.
Analysis and interpretation of data: Cheng.
Drafting of the manuscript: Cheng.
Critical revision of the manuscript for important intellectual content: S. Jin, Wen.
Statistical analysis: Cheng.
Obtaining funding: X. Jin.
Administrative, technical, or material support: X. Jin.
Supervision: X. Jin.
Other: None.
Financial disclosures: Xi Jin certifies that all conflicts of interest, including specific financial interests and relationships and affiliations relevant to the subject matter or materials discussed in the manuscript (eg, employment/affiliation, grants or funding, consultancies, honoraria, stock ownership or options, expert testimony, royalties, or patents filed, received, or pending), are the following: None.
Funding/Support and role of the sponsor: This study was supported by the Foundation of Science & Technology of Sichuan Province (2022YFS0304); the 135 Project for Disciplines of Excellence, West China Hospital, Sichuan University (ZYGD18011); and a postdoctoral research project in West China Hospital, Sichuan University (2019HXBH087). The sponsors played no direct role in the study.
Ethics considerations: This study was in full compliance with internationally accepted standards for research practice and reporting and follows internationally recognized guidelines.
Associate Editor: Silvia Proietti
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.euros.2023.04.004.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Finney R.P. Experience with new double J ureteral catheter stent. J Urol. 1978;120:678–681. doi: 10.1016/s0022-5347(17)57326-7. [DOI] [PubMed] [Google Scholar]
- 2.Haleblian G., Kijvikai K., de la Rosette J., et al. Ureteral stenting and urinary stone management: a systematic review. J Urol. 2008;179:424–430. doi: 10.1016/j.juro.2007.09.026. [DOI] [PubMed] [Google Scholar]
- 3.Mardis H.K., Kroeger R.M., Morton J.J., et al. Comparative evaluation of materials used for internal ureteral stents. J Endourol. 1993;7:105–115. doi: 10.1089/end.1993.7.105. [DOI] [PubMed] [Google Scholar]
- 4.Mosayyebi A., Manes C., Carugo D., et al. Advances in ureteral stent design and materials. Curr Urol Rep. 2018;19:35. doi: 10.1007/s11934-018-0779-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Miyaoka R., Monga M. Ureteral stent discomfort: etiology and management. Indian J Urol. 2009;25:455–460. doi: 10.4103/0970-1591.57910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ramachandra M., Mosayyebi A., Carugo D., et al. Strategies to improve patient outcomes and QOL: current complications of the design and placements of ureteric stents. Res Rep Urol. 2020;12:303–314. doi: 10.2147/rru.S233981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mosayyebi A., Vijayakumar A., Yue Q.Y., et al. Engineering solutions to ureteral stents: material, coating and design. Cent Eur J Urol. 2017;70:270–274. doi: 10.5173/ceju.2017.1520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rassweiler M.C., Michel M.S., Ritter M. Black-Star®—magnetic DJ removal. J Urol. 2014;191:e949–e950. doi: 10.1016/j.juro.2014.02.2029. [DOI] [Google Scholar]
- 9.Rassweiler M.C., Michel M.S., Ritter M., et al. Magnetic ureteral stent removal without cystoscopy: a randomized controlled trial. J Endourol. 2017;31:762–766. doi: 10.1089/end.2017.0051. [DOI] [PubMed] [Google Scholar]
- 10.Macaluso J.N., Jr, Deutsch J.S., Goodman J.R., et al. The use of the Magnetip double-J ureteral stent in urological practice. J Urol. 1989;142:701–703. doi: 10.1016/s0022-5347(17)38858-4. [DOI] [PubMed] [Google Scholar]
- 11.Eriksen M.B., Frandsen T.F. The impact of patient, intervention, comparison, outcome (PICO) as a search strategy tool on literature search quality: a systematic review. J Med Library Assoc. 2018;106:420–431. doi: 10.5195/jmla.2018.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rassweiler M.C., Michel M.S., Ritter M., Honeck P. Magnetic ureteral stent removal without cystoscopy: a randomized controlled trial. J Endourol. 2017;31:762–766. doi: 10.1089/end.2017.0051. [DOI] [PubMed] [Google Scholar]
- 13.Diranzo-Garcia M., Pardo-Duarte P., Álvarez-Barrera A., et al. Magnetic double-J stent: evaluation of tolerance and impact on quality of life compared to traditional double-J stent. Actas Urol Esp. 2021;45:366–372. doi: 10.1016/j.acuroe.2021.04.004. [DOI] [PubMed] [Google Scholar]
- 14.Kapoor A., Akerman J., Wong E.C.L., et al. Comparison of a magnetic retrieval device vs. flexible cystoscopy for removal of ureteral stents in renal transplant patients: a randomized controlled trial. Can Urol Assoc J. 2020;15:E97–E. doi: 10.5489/cuaj.6684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Farouk A., Tawfick A., Hasan M., Abuftira A.A., Maged W.A. Can magnitip double-J stent serve as a substitute for a standard double-J stent? Turk J Urol. 2019;45:437–443. doi: 10.5152/tud.2019.19038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.O’Kelly J.A., Haroon U.M., Rauf A.J., et al. (2020) Ureteric stenting with magnetic retrieval: an alternative to traditional methods. Ir J Med Sci. 2020;189:289–293. doi: 10.1007/s11845-019-02075-8. [DOI] [PubMed] [Google Scholar]
- 17.Sevcenco S., Eredics K., Lusuardi L., Klingler H.C. Evaluation of pain perception associated with use of the magnetic-end ureteric double-J stent for short-term ureteric stenting. World J Urol. 2018;36:475–479. doi: 10.1007/s00345-017-2146-x. [DOI] [PubMed] [Google Scholar]
- 18.Zeng S., Liu B., Hu H., et al. The function improved of the newly designed magnetic-end ureteric stenting retrieval device: a clinical prospective randomized and control trial in a multicenter study. Contrast Media Mol Imaging. 2022;2022:4107491. doi: 10.1155/2022/4107491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Türk C., Petřík A., Sarica K., et al. EAU guidelines on interventional treatment for urolithiasis. Eur Urol. 2016;69:475–482. doi: 10.1016/j.eururo.2015.07.041. [DOI] [PubMed] [Google Scholar]
- 20.Raskolnikov D., Brown B., Holt S.K., et al. Reduction of pain during flexible cystoscopy: a systematic review and meta-analysis. J Urol. 2019;202:1136–1142. doi: 10.1097/ju.0000000000000399. [DOI] [PubMed] [Google Scholar]
- 21.Capocasale E., Cremaschi E., Valle R.D., et al. Implementing a ureteric magnetic stent in the kidney transplant setting: report of 100 consecutive cases. Transplantation. 2019;103:2654–2656. doi: 10.1097/tp.0000000000002855. [DOI] [PubMed] [Google Scholar]
- 22.Chalhoub M., Kohaut J., Vinit N., et al. Feasibility and safety of magnetic-end double-J ureteral stent insertion and removal in children. World J Urol. 2021;39:1649–1655. doi: 10.1007/s00345-020-03339-0. [DOI] [PubMed] [Google Scholar]
- 23.Taylor W.N., McDougall I.T. Minimally invasive ureteral stent retrieval. J Urol. 2002;168:2020–2023. doi: 10.1097/01.ju.0000033964.15384.e2. [DOI] [PubMed] [Google Scholar]
- 24.O’Connell L., Broe M.P., Rooney D., et al. Magnetic stent removal in a nurse led clinic; a nine month experience. Ir Med J. 2018;111:687. 2018/06/29. [PubMed] [Google Scholar]
- 25.Macario A. What does one minute of operating room time cost? J Clin Anesthesia. 2010;22:233–236. doi: 10.1016/j.jclinane.2010.02.003. 2010/06/05. [DOI] [PubMed] [Google Scholar]
- 26.Joshi H.B., Stainthorpe A., MacDonagh R.P., et al. Indwelling ureteral stents: evaluation of symptoms, quality of life and utility. J Urol. 2003;169:1065–1069. doi: 10.1097/01.ju.0000048980.33855.90. [DOI] [PubMed] [Google Scholar]
- 27.Leibovici D., Cooper A., Lindner A., et al. Ureteral stents: morbidity and impact on quality of life. Israel Med Assoc J. 2005;7:491–494. [PubMed] [Google Scholar]
- 28.Damiano R., Autorino R., Esposito C., et al. Stent positioning after ureteroscopy for urinary calculi: the question is still open. Eur Urol. 2004;46:381–387. doi: 10.1016/j.eururo.2004.04.004. [DOI] [PubMed] [Google Scholar]
- 29.Scarneciu I., Lupu S., Pricop C., et al. Morbidity and impact on quality of life in patients with indwelling ureteral stents: a 10-year clinical experience. Pak J Med Sci. 2015;31:522–526. doi: 10.12669/pjms.313.6759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chew B.H., Lange D. Advances in ureteral stent development. Curr Opin Urol. 2016;26:277–282. doi: 10.1097/mou.0000000000000275. [DOI] [PubMed] [Google Scholar]
- 31.Kim D.J., Son J.H., Jang S.H., et al. Rethinking of ureteral stent removal using an extraction string; what patients feel and what is patients’ preference?: a randomized controlled study. BMC Urol. 2015;15:121. doi: 10.1186/s12894-015-0114-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Barnes K.T., Bing M.T., Tracy C.R. Do ureteric stent extraction strings affect stent-related quality of life or complications after ureteroscopy for urolithiasis: a prospective randomised control trial. BJU Int. 2014;113:605–609. doi: 10.1111/bju.12541. [DOI] [PubMed] [Google Scholar]
- 33.Barghouthy Y., Wiseman O., Ventimiglia E., et al. Silicone-hydrocoated ureteral stents encrustation and biofilm formation after 3-week dwell time: results of a prospective randomized multicenter clinical study. World J Urol. 2021;39:3623–3629. doi: 10.1007/s00345-021-03646-0. [DOI] [PubMed] [Google Scholar]
- 34.Wiseman O., Ventimiglia E., Doizi S., et al. Effects of silicone hydrocoated double loop ureteral stent on symptoms and quality of life in patients undergoing flexible ureteroscopy for kidney stone: a randomized multicenter clinical study. J Urol. 2020;204:769–777. doi: 10.1097/ju.0000000000001098. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.