Abstract
Background
Objective measures of community mobility are advantageous for capturing movement outside the home. Compared with subjective, self-reported techniques, global positioning system (GPS) technologies leverage passive, real-time location data to reduce recall bias and increase measurement precision. We developed methods to quantify community mobility among community-dwelling older adults and assessed how GPS-derived indicators relate to clinical measures of physical and cognitive performance.
Methods
Participants (n = 149; M ± standard deviation [SD] = 77.1 ± 6.5 years) from the program to improve mobility in aging (PRIMA) study, a physical therapy intervention to improve walking ability, carried a GPS device for 7 days. Community mobility was characterized by assessing activity space, shape, duration, and distance. Associations between GPS-derived indicators and cognition and physical function were evaluated using Spearman correlations.
Results
In adjusted models, a larger activity space, greater duration (eg, time out-of-home), and greater distance traveled from home were correlated with better 6-Minute Walk Test performance (ρ = 0.17–0.23, p’s < .05). A more circular activity shape was related to poorer performance on the Trail Making Test, Part A (ρ = 0.18, p < .05). More time out-of-home and a larger activity space were correlated with faster times on the Trail Making Test, Part B (ρ = −0.18 to −0.24, p’s < .05). Community mobility measures were not associated with global cognition, skilled walking, or usual gait speed.
Conclusion
GPS-derived community mobility indicators capture real-world activity among older adults and were correlated with clinical measures of executive function and walking endurance. These findings will guide the design of future interventions to promote community mobility.
Keywords: Cognition, Life-space activity, Physical performance, Public health
Community mobility is defined as an individual’s movement outside the home, including both active (eg, walking) and passive modes of transportation (eg, driving and public transportation) to navigate around the community (1,2). Community mobility is particularly important for the older adult population as it offers opportunities for promoting healthy aging and maintaining the quality of life, independence, and functional health through social engagement, physical and cognitive activity, and environmental enrichment at a time when mobility limitations are more likely to occur (3,4). Community mobility is important for independent living (5), social engagement (6), and completing many instrumental activities of daily living among older adults (2). Unlike traditional measures of mobility that occur in controlled, lab settings free of environmental demands (eg, curbs and stairs), community mobility better captures interactions between an individual and their real-world environment (2,7). Thus, it is important to examine older adults’ community mobility and assess performance in complex environments outside the traditional clinic-based setting.
Until recently, community mobility was measured using retrospective self-reported questionnaires, which are subject to recall bias; or travel diaries, which can be burdensome to participants. With recent advances in technology (eg, extended battery life, more affordable devices, decreased size, and easier to wear), novel methodologies utilizing global positioning system (GPS) technologies now allow for the passive and precise collection of objective data to characterize individuals’ movement throughout the community (8). Recent studies identified various cognitive, physical, social, or environmental factors associated with GPS-derived mobility indicators. For example, global cognition as measured by the Mini-Mental State Examination (MMSE) predicted the number of trips per week and the amount of time older adults spent outside of the home (9). Time out-of-home was also associated with better performance on physical tasks evaluating walking endurance and leg strength (9–11).
A recent review identified 29 studies published between 2008 and 2019 that used GPS technology to capture community mobility in older adults. A key finding from this review was the lack of standardized methods for processing GPS data (11). Most studies of community mobility take different approaches to process and clean GPS data, project the files into a geographic information system (eg, ArcGIS: Esri: Redlands, CA), and create metrics for activity space, shape, duration, or distance. This makes it challenging to generate inferences and compare estimates across studies. Also, GPS devices with battery-saving features often produce data with nonuniform sampling intervals, which require additional methods to ensure proper analysis and interpretation (eg, time-weighted approaches).
By applying the same methodological steps to processing and analyzing GPS data, harmonization and comparisons between studies can be made to advance our understanding of which community mobility indicators are related to older adults’ cognitive and physical performance. Here, we describe our methodology to capture multiple aspects of community mobility (eg, activity space, shape, duration, and distance) using GPS. This methodology was developed to address the unique needs and measures arising from the program to improve mobility in aging (PRIMA) study (eg, GPS devices with battery-saving features, time-weighted measures).
We had 2 objectives for this study: (a) outline the steps used to process and analyze GPS data to derive community mobility indicators and (b) compare real-world community mobility measures with clinic assessments of physical and cognitive performance among community-dwelling older adults. We hypothesized that increased community mobility would be related to better performance on lab-based cognitive and physical evaluations. We anticipated “moderate” correlations as community mobility is a complex measure influenced by numerous psychosocial, environmental, and functional factors (4).
Method
Participants and Protocol
This study used baseline data from the PRIMA study, a randomized single-blind 2-arm exercise intervention targeting walking speed in community-dwelling older adults. Inclusion criteria were (a) 65 years of age and older, (b) ambulatory without an assistive device or the assistance of another person, (c) 4-meter gait speed >0.60 m/s and <1.20 m/s, and (d) physician clearance to participate in a moderate intensity exercise program. Exclusion criteria were (a) inability to participate in the testing or exercise intervention or (b) safety concerns (eg, diagnosed dementia or cognitive impairment defined as a Modified Mini-Mental State Examination (3MS) score <79) (12). A detailed overview of the PRIMA study design is outlined elsewhere (13).
Participants were asked to carry one of two GPS devices (ie, iBlue 747: TSI: Hsinchu, Taiwan, Columbus V990: Columbus: Germany) for 7 consecutive days. In 2019, the iBlue devices malfunctioned. This led to a shift to the Columbus V990 GPS during the latter half of the study. Most participants carried the iBlue device at baseline. Participants were instructed to charge the device overnight and complete a paper-based activity log to record when they put the device on or off and if they removed the GPS device for more than 20 minutes during the course of the day. Baseline GPS data collection took place from July 2016 to October 2019.
Inclusion and Exclusion Criteria
Wear days
A total of 249 participants were enrolled in the PRIMA study. However, GPS data collection did not begin until after the PRIMA study started. Of the 249 participants, 209 were asked to carry a GPS device. After removing participants with data download errors (n = 23), complete equipment failure (n = 2), lost devices (n = 1), or noncompliance (n = 1), 182 participants had baseline GPS data. Upon reviewing the distributional characteristics of the GPS data, 16 participants with less than 5 days of wear were excluded over concerns of noncompliance, device malfunction, signal loss, or nonrepresentativeness of one’s movement throughout the community. Seventeen individuals with fewer than 5 wear days with at least 20% of time spent inside the home (eg, on vacation away from home) were also excluded to ensure the robustness of the data. Our final analytic sample included 149 participants. The demographic characteristics of the excluded participants were not statistically significantly different from the analytic sample (data not shown).
Clinic Measures
Participants completed several tests at the clinic to evaluate physical and cognitive performance (13). Clinic measures of physical function included: (a) mobility, as measured by usual gait speed on a 14-foot instrumented walkway system (Zeno Walkway, Protokinetics LLC, Havertown, PA) (13), (b) endurance, assessed by the distance traveled during a 6-Minute Walk Test (14), and (c) skilled walking, characterized by the time to complete the Figure of 8 Walk (15). The cognitive measures included: (a) global cognition, assessed with the Modified 3MS (12), (b) psychomotor speed, as measured by the time to complete the Trail Making Test, Part A (16), and (c) task switching, characterized by the time to complete the Trail Making Test, Part B (16).
GPS Battery-Saving Mode
The GPS devices went into an idle, battery-saver mode when movement, as measured by a built-in accelerometer, or satellite signals were not detected for a certain amount of time (ie, 2–5 minutes). Once the movement was detected, the devices would reinitialize and resume data collection. Thus, the sampling rate varied based on the participant’s movement patterns. When the device was in motion, the iBlue had a typical sampling rate ranging from 5 to 30 seconds, while the V990’s usual sampling rate was 1–3 seconds. While the power-saving features extended the device’s battery life by allowing for multiple days of wear time without recharging, it introduced the need for time-weighted approaches when obtaining activity space measures given the nonuniform sampling intervals.
Community Mobility Measures
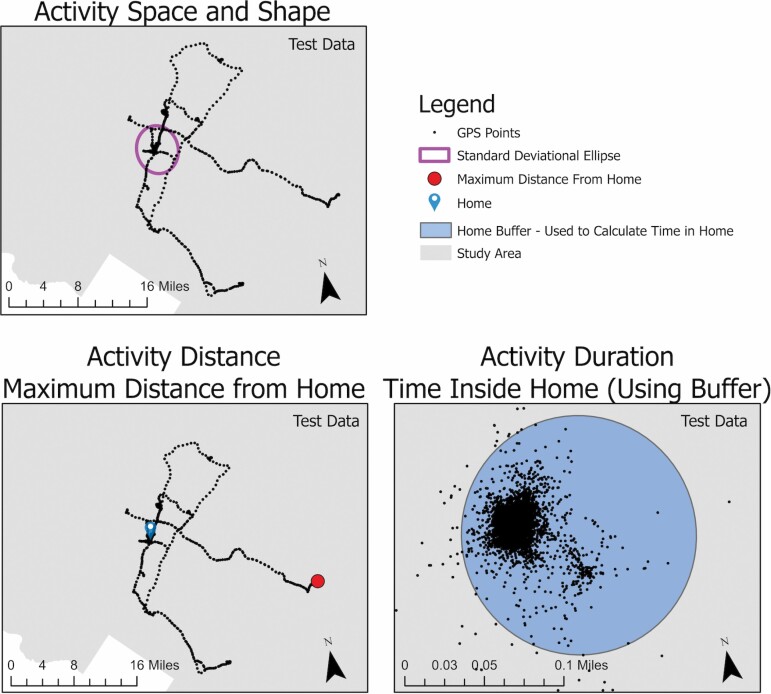
To capture community mobility, 4 components were measured and are described later: (a) activity space using the area of the standard deviational ellipse (SDE), (b) activity shape, as derived by the compactness (eg, circularity) of the SDE, (c) activity duration, from the time spent out-of-home, and (d) activity distance, from the maximum distance traveled from home. After reviewing the literature, these indicators were selected to capture all 4 characteristic aspects―space, time, movement scope, and attribute―that can be classified from GPS-derived measures of community mobility (17). We calculated daily measures and median measures during the week for each community mobility indicator to reduce the impact of outlier travel days and better estimate stable patterns of movement in the community throughout the week.
Activity space and shape
SDE area.—
The SDE is commonly used to illustrate the directional distribution of geospatial points and characterize one’s activity space (eg, the spatial extent of one’s travel to complete daily activities) (18–22). Similar to previous studies, we generated a one standard deviation SDE which contains approximately 68% of the participant’s GPS data to characterize activity space (21,22). Given the variable sampling intervals from the battery-saving features, the SDE was time-weighted such that each point was weighted by the time spent at each location (23).
SDE compactness.—
Compactness measures the shape of the activity space. It is calculated as the “ratio of the perimeter of a circle with the same area to the perimeter of the observed activity space.” (21) Values range from zero to one and represent how circular one’s activity space is (24). As one’s activity space becomes more circular, the compactness value gets closer to one.
Activity duration
Time out-of-home.—
Time spent outside of the home was characterized as both a median daily percentage and an overall total percentage. Overall percentage of time out-of-home represents the proportion of time spent outside of the 120 m home buffer out of the total time the device was worn across the entire wear period. Median daily percentage time out-of-home represents the median proportion of time spent outside of the 120 m home buffer out of the total time worn that day, provided at least some time was spent in home (ie, removing days on vacation).
While the median daily percentage captured participants’ typical time out of the home throughout the week, the overall percentage included total time spent outside of the home regardless of whether the time spent out-of-home took place primarily on a single day (ie, atypical travel). Percentages were used to assess the relative versus absolute amount of time spent outside of home and accounted for differences in total wear time between participants. In addition to a percentage measure, we also calculated the median and overall amount of time out-of-home (in hours) given that total wear time was not always 24 hours, and to investigate whether the magnitude of time spent outside was a stronger indicator than the percentage of time outside the home.
Activity distance
Maximum distance.—
We characterized activity distance by identifying the farthest distance (in kilometers) the participant traveled from their home. Similar to the activity duration measures, we calculated both median and overall measures to capture one’s typical distance traveled from home during the week as well as single days with large distances traveled.
Data Processing Pipeline
Preprocessing
GPS data were imported, and activity logs were examined to determine wear start and stop times (Figure 1). The GPS device was administered during the baseline visit and taken back to the clinic after carrying the device for 7 days. Therefore, we excluded the first day of data and truncated data collected after 7 wear days unless otherwise indicated in participants’ activity logs to reduce the impact of the clinic visit on the community mobility measures (eg, systematically upward bias in activity space, shape, duration, or distance)
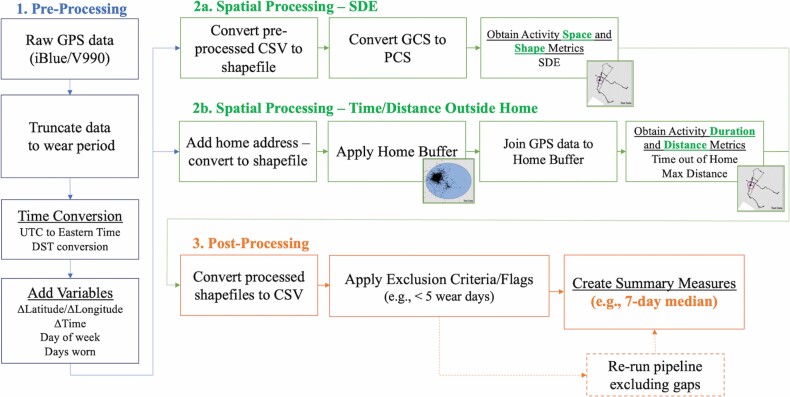
Figure 1.
GPS data processing pipeline. GPS = global positioning system; CSV = comma-separated values; UTC = Coordinated Universal Time; DST = daylight savings time; GCS = geographic coordinate system; PCS = projected coordinate system; SDE = standard deviational ellipse.
After truncating the data, an algorithm converted Universal Time Coordinated to Coordinated Universal Time and accounted for daylight savings time. Given the battery-saving features and nonuniform sampling intervals of the GPS devices, we created variables listing the change in time, latitude, and longitude between consecutive rows. We also generated an indicator for the day of the week and the number of days with GPS data present.
Spatial processing
Once preprocessing was complete, a shapefile was created in ArcGIS using ArcPy (25,26) to visualize the geographic features (Figure 2). Data were projected from the World Geodetic System 1984 (WGS84) geographic coordinate system to the USA Contiguous Albers Equal Area Conic projected coordinate system (27) to calculate the SDE area and compactness. This projection system was chosen because (a) it minimizes the distortion of area when transforming 3-dimensional, angular units to 2-dimensional, linear units and (b) it is commonly used by the United States Census Bureau (28), Environmental Protection Agency (29), and the United States Geological Survey (30).
Figure 2.
Community mobility measures derived from global positioning system (GPS) devices (test data).
For the activity space (eg, SDE area) and shape (eg, SDE compactness) measures, data were trimmed to exclude data points outside the continental United States. This approach is consistent with previous methodologies for calculating activity space and shape metrics (21). The SDE area was obtained using the Directional Distribution tool in ArcGIS. Compactness was calculated by dividing the perimeter of a circle with the same SDE area by the perimeter of the observed SDE (21).
Home addresses were geocoded based on participants’ reported addresses at baseline. Previous pilot testing of our GPS devices suggested that a 120-meter buffer around the participant’s residence was optimal for capturing in-home activity and accounted for any potential jitter that may arise in the GPS data (eg, being indoors, urban canyoning). Thus, we applied a 120-meter buffer around the participant’s home address prior to calculating time out-of-home. The Spatial Join tool in ArcGIS was used to capture location points lying within the participant’s 120-meter home buffer (23), and the different time out-of-home measures were calculated by dividing the time outside of the home buffer by the total wear time. Time out-of-home measures were characterized in hours and as a percentage.
The Proximity Analysis tool in ArcGIS (31) was used to assess the maximum straight-line distance traveled from the participant’s home, both overall and during each wear day.
Removal of Influential Time and Distance Gaps
As a result of the battery-saving features intrinsic to the GPS devices, which resulted in no data collection when the devices were not in motion, some data contained large time gaps of inactivity (eg, 8 hours). Given the time-weighted approach used to characterize community mobility, sizable time gaps not attributed to inactive time (eg, forgot device at home and battery death) could greatly influence activity space and duration indicators. To address this issue, we examined any GPS points with a time gap exceeding one hour and calculated the interpoint distance between the location of the large time gap and the subsequent location point. If the time gap exceeded 1 hour and the interpoint distance was greater than 120 meters (ie, buffer accounting for potential jitter in location acquisition), the data point was excluded from the time-weighted analyses. However, if the interpoint distance was less than 120 meters, the data points were not removed under the assumption that these time gaps were due to participants staying in the same location for an extended period.
Covariates
This study adjusted for factors thought to be associated with physical or cognitive performance and community mobility. Covariates included age, sex, GPS device used (iBlue vs. V990), season, and comorbidities. To capture comorbidities, the Duke Comorbidity Index was administered (32). This index asks participants to report whether they have been diagnosed with any of 18 common comorbidities (eg, diabetes, arthritis, and depression/anxiety). The comorbidities were then categorized into 8 domains (eg, respiratory, cardiovascular, and musculoskeletal) and summed to generate a comorbidity score ranging from 0 to 8 to reflect the number of comorbidity domains affected.
Statistical Analysis
Statistical analyses were performed using Stata, Version 14 (33). First, we generated descriptive statistics (eg, mean, median, and range) and visualized the distribution of each variable. Given the skewed distribution of some of the community mobility measures, a Spearman rank-order correlation assessed the relationship between the ranks of clinic-based and real-world community mobility measures. When examining correlations for the Trail Making Test, Part B, we also adjusted for performance on the Trail Making Test, Part A. We excluded 2 participants with invalid completion times when analyzing performance on the Trail Making Test, Part B.
Results
The average age of the analytic sample was 77.1 years (SD = 6.5; range: 65–97). Participants were mostly female (68%), White (86%), and highly educated (Table 1). The mean number of wear days was 6.8 (SD = 0.5; median = 7; range: 5–7), with a mean of 13 843 GPS points (SD = 26 944; median = 8 244; interquartile range [IQR] = 8 559) indicating high rates of compliance. Approximately 96% of the sample carried the iBlue GPS device at baseline, and 4% used the Columbus V990. The geographic distribution of participants’ residences spanned 110 census block groups, with an average of 1.35 (SD = 0.64, range = 1–4) people per block group.
Table 1.
PRIMA Analytic Sample Characteristics
| Characteristics | M ± SD or n (%) | Min. | Max. |
|---|---|---|---|
| Age | 77.1 ± 6.5 | 65 | 97 |
| Female sex | 101 (68) | ||
| White race | 128 (86) | ||
| >High school education | 123 (83) | ||
| Device: iBlue (vs V990) | 143 (96) | ||
| Season | |||
| Winter | 28 (19) | ||
| Spring | 30 (20) | ||
| Summer | 43 (29) | ||
| Fall | 48 (32) |
| Clinical measures | M ± SD or n (%) | Min. | Max. |
|---|---|---|---|
| Comorbidity domains affected | 2.8 ± 1.3 | 0 | 6 |
| 3MS | 96.3 ± 3.8 | 80 | 100 |
| Time on TMT-A (s) | 33.4 ± 12.9 | 15.3 | 90.0 |
| Time on TMT-B (s)* | 82.0 ± 42.2 | 33.2 | 300.0 |
| Distance on 6-Minute Walk Test (m) | 402.2 ± 88.2 | 187.8 | 617.1 |
| Time on Figure-of-8 Walk (s) | 9.9 ± 2.2 | 5.0 | 20.3 |
| Gait speed (14-feet, m/s) | 1.1 ± 0.2 | 0.7 | 1.4 |
| Depressive symptoms (GDS) | 1.0 ± 1.4 | 0 | 7 |
| Community mobility measures | Median (IQR) | Min. | Max. |
|---|---|---|---|
| Activity space (km2) | |||
| SDE area, median | 2.2 (0.4, 5.5) | 0.0 | 1 185.4 |
| Activity shape | |||
| SDE compactness, median | 0.7 (0.6, 0.8) | 0.4 | 1.0 |
| Activity duration | |||
| Total time out-of-home (hours) | 24.2 (16.1, 34.2) | 0.0 | 83.9 |
| Total time out-of-home (%) | 16.2 (11.6, 23.8) | 0.0 | 61.8 |
| Median time out-of-home (hours) | 3.3 (2.0, 4.8) | 0.0 | 10.5 |
| Median time out-of-home (%) | 15.2 (9.9, 22.8) | 0.0 | 57.6 |
| Activity distance (km) | |||
| Maximum distance, overall | 14.2 (9.4, 22.1) | 0.1 | 936.2 |
| Maximum distance, median | 5.1 (2.9, 8.1) | 0.0 | 137.6 |
| Daily GPS hours recorded, median | 24.0 (22.6, 24.0) | 8.3 | 24.0 |
Notes: n = 149; PRIMA = program to improve mobility in aging; SD = standard deviation; GDS = geriatric depression scale; TMT-A = Trail Making Test, Part A; TMT-B = Trail Making Test, Part B; 3MS = Modified Mini-Mental State examination; SDE = standard deviational ellipse; IQR = interquartile range; GPS = global positioning system.
*n = 147; excluded 2 participants with invalid completion times on TMT-B.
When exploring unadjusted relationships between GPS-derived community mobility measures and clinical assessments, a larger SDE area was significantly correlated with better performance on the Trail Making Test, Part B (ρ = −0.20, p = .02) and a greater distance traveled on the 6-Minute Walk Test (ρ = 0.24, p = .003). Higher SDE compactness (eg, a more circular activity space) was associated with slower times on the Trail Making Test, Part A (ρ = 0.20, p = .02). There were no significant associations between any community-mobility measures and global cognition (Table 2).
Table 2.
Spearman Correlations Between GPS-Derived Community Mobility and Clinical Measures of Cognitive and Physical Performance
| Unadjusted | Adjusted | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 3MS | TMT-A | TMT-B* | 6MWT | F8W | Gait | 3MS | TMT-A | TMT-B*,† | 6MWT | F8W | Gait | |
| Activity space (km2) | ||||||||||||
| SDE area, median | 0.10 | −0.10 | −0.20* | 0.24** | −0.13 | 0.13 | 0.08 | −0.08 | −0.18* | 0.19* | −0.08 | 0.10 |
| Activity shape | ||||||||||||
| SDE compactness, median | −0.03 | 0.20* | 0.13 | 0.02 | −0.01 | 0.09 | −0.03 | 0.18* | −0.01 | 0.04 | −0.03 | 0.11 |
| Activity duration | ||||||||||||
| Total time out-of-home (hours) | 0.11 | −0.18* | −0.29*** | 0.27*** | −0.23** | 0.18* | 0.09 | −0.14 | −0.24** | 0.21* | −0.16 | 0.13 |
| Total time out-of-home (%) | 0.07 | −0.17* | −0.27** | 0.22** | −0.20* | 0.15 | 0.05 | −0.15 | −0.22** | 0.17* | −0.15 | 0.12 |
| Median time out-of-home (hours) | 0.06 | −0.16 | −0.23** | 0.24** | −0.17* | 0.17* | 0.04 | −0.14 | −0.18* | 0.23** | −0.15 | 0.15 |
| Median time out-of-home (%) | 0.03 | −0.14 | −0.19* | 0.21** | −0.15 | 0.15 | 0.01 | −0.13 | −0.14 | 0.20* | −0.12 | 0.13 |
| Activity distance (km) | ||||||||||||
| Maximum distance, overall | 0.14 | −0.16 | −0.21* | 0.00 | 0.03 | −0.07 | 0.16 | −0.16 | −0.14 | 0.00 | 0.02 | −0.08 |
| Maximum distance, median | 0.12 | −0.11 | −0.18* | 0.24** | −0.16* | 0.13 | 0.11 | −0.08 | −0.14 | 0.19* | −0.12 | 0.09 |
Notes: n = 149; adjusted for age, sex, GPS device used, season, and comorbidities. 3MS = Modified Mini-Mental State examination; TMT-A = Trail Making Test, Part A; TMT-B = Trail Making Test, Part B; 6MWT = 6-Minute Walk Test; F8W = Figure-of-8 Walk; Gait = 14-feet gait speed; SDE = standard deviational ellipse. Bolded text represents significant coefficients at the p < .05 level.
*n = 147; excluded 2 participants with invalid completion times on TMT-B.
†Additionally adjusted for TMT-A.
*p < .05, **p < .01, ***p < .001.
A greater total time and percentage of total time out-of-home were related to better performance on the Trail Making Test, Part A (ρ = −0.17 to −0.18, p’s < .05) and Part B (ρ’s = −0.27 to −0.29, p’s < .01), a farther distance traveled on the 6-Minute Walk Test (ρ’s = 0.22–0.27, p’s < .01), and a faster time to complete the Figure of 8 Walk (ρ’s = −0.20 to −0.23, p’s < .05). More total time out-of-home was also linked to faster gait speeds (ρ = 0.18, p = .03). A higher median time out-of-home was correlated with better performance on the Trail Making Test, Part B (ρ = −0.23, p = .006) 6-Minute Walk Test (ρ = 0.24, p = .003), a faster Figure of 8 Walk (ρ = −0.17, p = .04), and faster gait speeds (ρ = 0.17, p = .04).
A greater median percentage of time out-of-home was significantly correlated with faster times on the Trail Making Test, Part B (ρ = −0.19, p = .02) and farther distances on the 6-Minute Walk Test (ρ = 0.21, p = .009). The overall maximum distance traveled from home was associated with better performance on the Trail Making Test, Part B (ρ = −0.21, p = .01), while the median maximum distance was related to faster times on the Trail Making Test, Part B (ρ = −0.18, p = .03), a greater distance traveled on the 6-Minute Walk Test (ρ = 0.24, p = .004), and faster times on the Figure of 8 Walk (ρ = −0.16, p = .047).
In adjusted models, a larger SDE area remained significantly associated with better performance on the 6-Minute Walk Test and Trail Making Test, Part B. SDE compactness was still significantly correlated with performance on the Trail Making Test, Part A. Associations between the time out-of-home measures and performance on the 6-Minute Walk Test and Trail Making Test, Part B persisted, except for the median percentage of time out-of-home. The median maximum distance traveled from home remained significantly associated with better performance on the 6-Minute Walk Test.
Discussion
Our objectives for this study were twofold. First, following the recommendations from Chung et al. (2021) to create a standardized processing protocol, we summarized the steps taken to process GPS data and obtain community mobility indicators among community-dwelling older adults who participated in a physical therapy intervention. The techniques outlined earlier can be used for GPS devices with battery-saving features. The use of GPS-derived measures to characterize community mobility is an emerging field, and this work will lead to further refinement and establishment of standard guidelines for GPS processing similar to wear time and sleep-wake time algorithms commonly employed with accelerometer-based data (34,35). Establishing a common data processing pipeline also aids in data harmonization and allows for comparisons of results across studies.
For the second objective, we explored associations between GPS-derived community mobility indicators and clinic-based cognitive and physical performance measures. The consistent associations between time out-of-home and in-clinic measures of cognitive and physical functions suggest that time spent outside of the home is sensitive to older adults’ functional status. Spending time outside the home may provide more opportunities for walking and other forms of physical activity to build functional reserves (36–38). Additionally, outdoor walking requires complex cognitive (eg, attention) and physical skills (eg, endurance and skilled walking) to adapt and navigate environmental challenges (eg, crosswalks, stairs, and uneven sidewalks) (2). Thus, a relatively simple measure like time out-of-home may be a helpful indicator to complement clinical measures of cognitive or physical capacity.
A larger SDE area was associated with a greater distance traveled on the 6-Minute Walk Test and faster times on the Trail Making Test, Part B. Unlike measures of activity duration (eg, time out-of-home), SDE area captures the spatial extent of travel (21). When looking at the maximum distance traveled throughout the wear period, a greater median distance from home was correlated with a greater distance on the 6-Minute Walk Test, a clinic-based measure of walking endurance. Our findings suggest that participants who traveled farther in the community performed better on clinical measures of task switching, a component of executive function, and walking endurance.
A more circular activity shape (eg, higher compactness) was significantly correlated with longer times to complete the Trail Making Test, Part A, a measure of psychomotor speed. This finding was unexpected as one might suppose a more circular activity space to be a proxy for the diversity of locations visited. These results may be explained by findings from a recent study showing that SDE compactness values were higher in regions with lower walkability, and individuals who reported walking outside also had lower compactness values (21).
The Trail Making Test, Part A measures psychomotor speed, but it also incorporates visual scanning processes that contribute to spatial navigation (39). Navigating trips farther away from home may place higher demands on visual scanning abilities while also resulting in a more elongated activity space (ie, lower compactness). Perhaps lower compactness may be expected in low walkability settings for those with better psychomotor speed, who are able to take trips farther from home to key destinations that are not accessible in their immediate neighborhoods. In comparison, those with lower psychomotor speed in low walkability settings may be less likely to make these trips and ultimately have more centralized activity around the home (ie, higher compactness).
Global cognition (eg, 3MS score) was not significantly correlated with any community mobility measures. However, the eligibility criteria required participants to have a 3MS score of at least 79. Therefore, associations may not have been apparent as this was a cognitively healthy sample. After adjusting for covariates, gait speed and performance on the skilled walking test were not significantly correlated with any community mobility indicators. Thus, other variables (eg, age and sex) may better explain older adults’ gait speed and skilled walking ability. These findings suggest that community mobility involves different elements of extended physical activity and cognitive performance (eg, navigating complex terrain) that extend beyond global cognition measures or functional capacity measured in a controlled, clinical setting (4,7).
While we found few associations with gait speed, many associations appeared with the 6-Minute Walk Test. Unlike gait speed, the 6-Minute Walk Test is thought to be a proxy for aerobic capacity (eg, physical fitness and endurance). This task is also much more demanding (~400 meters of walking vs 14 feet for gait speed), is likely more sensitive to functional differences (40), and may better characterize the level of mobility required for sustained free-living activity. This is particularly true for PRIMA participants, as they could still walk reasonably well but were at risk of mobility declines. These findings highlight the importance of capturing both real-world and clinic-based measures when exploring older adults’ physical and cognitive function.
Similar to previous studies, lab-based measures of physical and cognitive function were associated with real-world movement in the community (9–11). While the GPS-derived measures were significantly correlated to physical and cognitive performance tasks, it is important to note that the correlation coefficients are quite low, which suggests that several factors contributed to performance on clinic-based tests of cognitive and physical performance.
Community mobility is influenced by cross-cutting physical, cognitive, psychosocial, environmental, and personal factors (4,41,42). Future studies should incorporate additional psychosocial and environmental factors, such as neighborhood characteristics, street connectivity, weather, access to public transportation, and social cohesion, into the analysis to understand other variables associated with community mobility, cognitive performance, and physical function. Furthermore, GPS-derived community mobility research can be viewed through a healthy equity lens (43) to explore potential racial and poverty-related disparities that contribute to older adults’ community mobility. Overall, the results from this study suggest that objective GPS-derived measures of community mobility are feasible to collect, can be obtained using an automated processing pipeline, and were significantly correlated with performance on in-clinic measures.
Strengths and Limitations
The strengths of the present study include its large sample size of community-dwelling older adults and the objective method of data collection using GPS technologies. A recent scoping review of studies using GPS to measure community participation in older adults found that the typical sample size for similar studies is approximately 80, on average (44). The PRIMA study had GPS data on nearly twice as many participants, which affords us more power to detect differences in the data. Another strength includes PRIMA’s enrollment of participants with a wide range of physical functions as seen by the 6-Minute Walk Test, Figure-of-8 Walk, and gait speed measures. Thus, the sample is more likely to reflect the variability in functional performance typically seen among community-dwelling older adults. We also sought to establish a common approach or protocol to deriving community mobility characteristics, particularly for GPS devices with battery-saving features.
Some limitations should also be noted. First, we did not collect information on participants’ ability to drive, which can influence the size of one’s activity space (41). However, participants had to visit the clinic twice a week for their physical therapy sessions, which suggests they could drive themselves or arrange for regular and reliable transportation to the clinic. Thus, we may be underestimating the relationship between community mobility and lab-based measures as this sample may be more mobile than other community-dwelling older adults.
While the battery-saving features allowed more data to be collected, these features made it difficult to differentiate sedentary activity from device malfunctions (eg, battery death). Noncompliance or unreliable use should also be considered, as some participants did not carry the device for the entire wear period. We addressed this limitation by removing individuals with less than 5 days of wear time. Toward the end of baseline data collection, the iBlue 747 GPS devices began to malfunction, which led to a shift to the Columbus V990 logger. While the sampling frequency differed between devices, there is no indication that the data quality differed between these 2 devices. We were also unable to separate active (eg, walking, biking, and running) from passive travel (eg, riding in a car, bus, or an airplane) in the present study. For example, we may have not found associations between specific functional measures (eg, gait speed) and GPS measures due to the latter being predominantly driven by passive, vehicular transit. Analyses are currently underway to explore whether associations differ when stratified by older adults’ modality of travel.
Although GPS technologies have continued to improve in accuracy and precision, there is still a chance for signal dropout due to being indoors, urban canyoning (eg, degraded signal due to tall buildings), and measurement error (eg, outliers). We attempted to address this limitation by using median measures across the wear period to characterize community mobility and removing influential data points with a large time gap accompanied by large interpoint distances. Given our study looked at median weekly measures, outlier points may not be as influential when generating community mobility indicators. However, additional outlier removal procedures are likely warranted for studies using daily-level or minute-level community mobility data to generate inferences.
Our sample primarily consisted of White, female, and highly educated older adults; thus, the results may not generalize to other groups. Future studies should include a more representative sample of participants (eg, more racial/ethnic minorities, broader range of education, and socioeconomic status). Finally, although we followed precedent from previous studies by collecting GPS data for 7 days (44), 1 week may not be a sufficient wear period to accurately capture one’s typical movement throughout the community. Recent studies recommend a minimum of 8–14 days of valid GPS data to correctly measure community mobility (45,46).
Conclusion
GPS technologies are gaining in popularity to objectively capture community mobility. There are numerous ways to process the data and characterize movement throughout the community. This variability in processing makes it difficult to yield inferences across studies or harmonize data to advance our understanding of which factors (eg, cognitive performance and physical function) are associated with community mobility. This study aimed to establish a common approach and processing pipeline to analyze GPS data and derive community mobility indicators. After obtaining these indicators, we examined whether these GPS-derived features were related to lab-based measures of physical and cognitive function. A deeper understanding of which indicators (eg, activity space, shape, duration, and distance) are linked to older adults’ cognitive and physical function will inform future interventions and public policies targeting community mobility or seeking to promote independent living and aging in place.
Acknowledgments
We would like to thank the PRIMA participants for their time and contribution to the study. We would also like to thank Anisha Suri, MS; Dana Eldreth, PhD; Emily Richards, BA; Emma Baillargeon, PhD, DPT; Pamela Dunlap, DPT; and Patrick Donahue, MS for their helpful insights during our PRIMA GPS meetings.
Contributor Information
Breanna M Crane, Department of Mental Health, Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland, USA.
Kyle D Moored, Department of Epidemiology, University of Pittsburgh Graduate School of Public Health, Pittsburgh, Pennsylvania, USA.
Andrea L Rosso, Department of Epidemiology, University of Pittsburgh Graduate School of Public Health, Pittsburgh, Pennsylvania, USA.
Michelle C Carlson, Department of Mental Health, Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland, USA.
Funding
This work was supported by the National Institutes of Health (R01-AG045252 and K24-AG057728 to Jennifer S. Brach; R01-AG057671 to A.L.R.) and the Pittsburgh Pepper Center (P30-AG024827). This work was also supported by the National Institute on Aging Research Training in Age-Related Cognitive Disorders Training Grant (T32-AG027668 to B.M.C.) and the Johns Hopkins Epidemiology and Biostatistics of Aging Research Fellowship (T32-AG000247 to B.M.C.). This work was also supported by the National Institute on Aging Pittsburgh Epidemiology of Aging Training Program (T32-AG000181 to K.D.M.).
Conflict of Interest
None declared.
Author Contributions
B.M.C. was responsible for processing, analyzing, and interpreting the GPS data as well as drafting the article. K.D.M. contributed to the conception and design of the analysis, aided in analyzing and interpreting the data, and provided critical revisions to the article for intellectual content. A.L.R. and M.C.C. contributed to the conception and design of the analysis, aided in interpreting the data, and provided critical revisions to the manuscript. All authors read and approved the final manuscript.
Ethics Approval and Consent to Participate
The study was approved by the University of Pittsburgh and Johns Hopkins Bloomberg School of Public Health Institutional Review Board. All participants provided informed consent.
Availability of Data and Materials
The data generated and analyzed during the current study are not publicly available as they contain location information that could compromise the privacy of research participants.
Consent for Publication
Not applicable.
References
- 1. American Occupational Therapy Association. Occupational therapy practice framework: domain and process (3rd ed.). Am J Occup Ther. 2014;68(suppl 1):S1–S48. doi: 10.5014/ajot.2014.682006 [DOI] [Google Scholar]
- 2. Patla AE, Shumway-Cook A. Dimensions of mobility: defining the complexity and difficulty associated with community mobility. J Aging Phys Act. 1999;7(1):7–19. doi: 10.1123/japa.7.1.7 [DOI] [Google Scholar]
- 3. Okoro CA, Hollis ND, Cyrus AC, Griffin-Blake S. Prevalence of disabilities and health care access by disability status and type among adults―United States, 2016. MMWR Morb Mortal Wkly Rep. 2018;67(32):882–887. doi: 10.15585/mmwr.mm6732a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Webber SC, Porter MM, Menec VH. Mobility in older adults: a comprehensive framework. Gerontologist. 2010;50(4):443–450. doi: 10.1093/geront/gnq013 [DOI] [PubMed] [Google Scholar]
- 5. Sheppard KD, Sawyer P, Ritchie CS, Allman RM, Brown CJ. Life-space mobility predicts nursing home admission over 6 years. J Aging Health. 2013;25(6):907–920. doi: 10.1177/0898264313497507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Rosso AL, Taylor JA, Tabb LP, Michael YL. Mobility, disability, and social engagement in older adults. J Aging Health. 2013;25(4):617–637. doi: 10.1177/0898264313482489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Glass TA. Conjugating the “tenses” of function: discordance among hypothetical, experimental, and enacted function in older adults. Gerontologist. 1998;38(1):101–112. doi: 10.1093/geront/38.1.101 [DOI] [PubMed] [Google Scholar]
- 8. Fillekes MP, Röcke C, Katana M, Weibel R. Self-reported versus GPS-derived indicators of daily mobility in a sample of healthy older adults. Soc Sci Med. 2019;220:193–202. doi: 10.1016/j.socscimed.2018.11.010 [DOI] [PubMed] [Google Scholar]
- 9. McInnes L, Jones E, Rochester L, et al. Mobility in community dwelling older adults: predicting successful mobility using an instrumented battery of novel measures. J Frailty Aging. 2020;9(2):68–73. doi: 10.14283/jfa.2019.35 [DOI] [PubMed] [Google Scholar]
- 10. Harada K, Lee S, Lee S, Bae S, Harada K, Shimada H. Changes in objectively measured outdoor time and physical, psychological, and cognitive function among older adults with cognitive impairments. Arch Gerontol Geriatr. 2018;78:190–195. doi: 10.1016/j.archger.2018.06.003 [DOI] [PubMed] [Google Scholar]
- 11. Chung J, Sargent L, Brown R, Gendron T, Wheeler D. GPS tracking technologies to measure mobility-related behaviors in community-dwelling older adults: a systematic review. J Appl Gerontol. 2021;40(5):547–557. doi: 10.1177/0733464820979801 [DOI] [PubMed] [Google Scholar]
- 12. Teng EL, Chui HC. The Modified Mini-Mental State (3MS) examination. J Clin Psychiatry. 1987;48(8):314–318. [PubMed] [Google Scholar]
- 13. Brach JS, VanSwearingen JM, Gil A, et al. Program to improve mobility in aging (PRIMA) study: methods and rationale of a task-oriented motor learning exercise program. Contemp Clin Trials. 2020;89:105912. doi: 10.1016/j.cct.2019.105912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Butland RJ, Pang J, Gross ER, Woodcock AA, Geddes DM. Two-, six-, and 12-minute walking tests in respiratory disease. Br Med J (Clin Res ed). 1982;284(6329):1607. doi: 10.1136/bmj.284.6329.1607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hess RJ, Brach JS, Piva SR, VanSwearingen JM. Walking skill can be assessed in older adults: validity of the Figure-of-8 Walk Test. Phys Ther. 2010;90(1):89–99. doi: 10.2522/ptj.20080121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Army Individual Test Battery. Manual of Directions and Scoring. Washington, DC: War Department, Adjutant General’s Office; 1944. [Google Scholar]
- 17. Fillekes MP, Giannouli E, Kim E-K, Zijlstra W, Weibel R. Towards a comprehensive set of GPS-based indicators reflecting the multidimensional nature of daily mobility for applications in health and aging research. Int J Health Geogr. 2019;18(1):1–20. doi: 10.1186/s12942-019-0181-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Yuill RS. The standard deviational ellipse; an updated tool for spatial description. Geogr Ann Ser B. 1971;53(1):28–39. doi: 10.1080/04353684.1971.11879353 [DOI] [Google Scholar]
- 19. Lefever DW. Measuring geographic concentration by means of the standard deviational ellipse. AJS. 1926;32(1):88–94. doi: 10.1086/214027 [DOI] [Google Scholar]
- 20. Sherman JE, Spencer J, Preisser JS, Gesler WM, Arcury TA. A suite of methods for representing activity space in a healthcare accessibility study. Int J Health Geogr. 2005;4(1):24. doi: 10.1186/1476-072X-4-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hirsch JA, Winters M, Clarke P, McKay H. Generating GPS activity spaces that shed light upon the mobility habits of older adults: a descriptive analysis. Int J Health Geogr. 2014;13(1):1–14. doi: 10.1186/1476-072X-13-51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Zenk SN, Schulz AJ, Matthews SA, et al. Activity space environment and dietary and physical activity behaviors: a pilot study. Health Place. 2011;17(5):1150–1161. doi: 10.1016/j.healthplace.2011.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Esri Inc. Spatial Join (Analysis). 2021. https://pro.arcgis.com/en/pro-app/latest/tool-reference/analysis/spatial-join.htm
- 24. Manaugh K, El-Geneidy A. What makes travel “local”: defining and understanding local travel behaviour. J Transp Land Use. 2012;5(3):15–27. doi: 10.5198/jtlu.v5i3.300 [DOI] [Google Scholar]
- 25. ArcGIS Pro Python Reference (computer program).
- 26. ArcGIS Pro (Version 2.7; computer program). 2020.
- 27. Snyder JP. Map Projections: A Working Manual. Vol. 1395. Washington, DC: US Government Printing Office; 1987. [Google Scholar]
- 28. United States Census Bureau. OnTheMap: How to Import External Geography Data for Analysis. https://lehd.ces.census.gov/doc/help/onthemap/OnTheMapImportTools.pdf. Published 2011. Accessed.
- 29. Environmental Protection Agency. RSEI Grid and Locational Information. United States Environmental Protection Agency. https://www.epa.gov/rsei/rsei-grid-and-locational-information. Published 2020. Accessed. [Google Scholar]
- 30. Snyder JP. Map Projections Used by the US Geological Survey. US Government Printing Office;1982. [Google Scholar]
- 31. Esri Inc. An Overview of the Proximity Toolset. 2021. https://desktop.arcgis.com/en/arcmap/latest/tools/analysis-toolbox/an-overview-of-the-proximity-toolset.htm
- 32. Rigler SK, Studenski S, Wallace D, Reker DM, Duncan PW. Co-morbidity adjustment for functional outcomes in community-dwelling older adults. Clin Rehabil. 2002;16(4):420–428. doi: 10.1191/0269215502cr515oa [DOI] [PubMed] [Google Scholar]
- 33. Stata Statistical Software: Release 14. (computer program). College Station, TX: StataCorp LP; 2015. [Google Scholar]
- 34. Quante M, Kaplan ER, Cailler M, et al. Actigraphy-based sleep estimation in adolescents and adults: a comparison with polysomnography using two scoring algorithms. Nat Sci Sleep. 2018;10:13–20. doi: 10.2147/NSS.S151085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Syed S, Morseth B, Hopstock LA, Horsch A. Evaluating the performance of raw and epoch non-wear algorithms using multiple accelerometers and electrocardiogram recordings. Sci Rep. 2020;10(1):5866. doi: 10.1038/s41598-020-62821-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Carlson MC. Introduction: a life course perspective on activity and neurocognitive health. J Int Neuropsychol Soc. 2011;17(6):970–974. doi: 10.1017/S1355617711001366 [DOI] [PubMed] [Google Scholar]
- 37. Portegijs E, Tsai L-T, Rantanen T, Rantakokko M. Moving through life-space areas and objectively measured physical activity of older people. PLoS One. 2015;10(8):e0135308–e0135308. doi: 10.1371/journal.pone.0135308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Simonsick EM, Guralnik JM, Volpato S, Balfour J, Fried LP. Just get out the door! Importance of walking outside the home for maintaining mobility: findings from the Women’s Health and Aging Study. J Am Geriatr Soc. 2005;53(2):198–203. doi: 10.1111/j.1532-5415.2005.53103.x [DOI] [PubMed] [Google Scholar]
- 39. Lowry KA, Brach JS, Nebes RD, Studenski SA, VanSwearingen JM. Contributions of cognitive function to straight-and curved-path walking in older adults. Arch Phys Med Rehabil. 2012;93(5):802–807. doi: 10.1016/j.apmr.2011.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Newman AB, Simonsick EM, Naydeck BL, et al. Association of long-distance corridor walk performance with mortality, cardiovascular disease, mobility limitation, and disability. JAMA. 2006;295(17):2018–2026. doi: 10.1001/jama.295.17.2018 [DOI] [PubMed] [Google Scholar]
- 41. Kuspinar A, Verschoor CP, Beauchamp MK, et al. Modifiable factors related to life-space mobility in community-dwelling older adults: results from the Canadian Longitudinal Study on Aging. BMC Geriatr. 2020;20(1):35. doi: 10.1186/s12877-020-1431-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Dunlap PM, Rosso AL, Zhu X, Klatt BN, Brach JS. The association of mobility determinants and life space among older adults. J Gerontol A Biol Sci Med Sci 2021. 1–9. doi: 10.1093/gerona/glab268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Hill CV, Pérez-Stable EJ, Anderson NA, Bernard MA. The National Institute on Aging Health Disparities Research Framework. Ethn Dis. 2015;25(3):245–254. doi: 10.18865/ed.25.3.245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Gough C, Weber H, George S, Maeder A, Lewis L. Location monitoring of physical activity and participation in community dwelling older people: a scoping review. Disabil Rehabil. 2021;43(2):270–283. doi: 10.1080/09638288.2019.1618928 [DOI] [PubMed] [Google Scholar]
- 45. Zenk SN, Matthews SA, Kraft AN, Jones KK. How many days of global positioning system (GPS) monitoring do you need to measure activity space environments in health research? Health Place. 2018;51:52–60. doi: 10.1016/j.healthplace.2018.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Zhu L, Boissy P, Duval C, et al. How long should GPS recording lengths be to capture the community mobility of an older clinical population? A Parkinson’s example. Sensors. 2022;22(2):563–577. doi: 10.3390/s22020563 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data generated and analyzed during the current study are not publicly available as they contain location information that could compromise the privacy of research participants.