This case-control study assesses disruptive life events of individuals with schizophrenia or bipolar I disorder using public consumer credit records in conjunction with electronic health record data.
Key Points
Question
Can novel, publicly available data aggregated by a consumer credit reporting agency support population-level studies on the occurrence of disruptive life events for patients with diagnoses of bipolar I disorder (BPI) or schizophrenia?
Findings
In this case-control study of 46 167 patients with a diagnosis of BPI or schizophrenia, electronic health records data and TransUnion data were used for arrests, bankruptcies, lien, and judgment filings and demonstrated differences in disruptive life events among patients with diagnoses of BPI or schizophrenia and 2 matched comparison cohorts.
Meaning
TransUnion data can support population-level studies on the occurrence of disruptive life events and may support effectiveness studies that assess disruptive life events in addition to clinical outcomes.
Abstract
Importance
There is a dearth of population-level data on major disruptive life events (defined here as arrests by a legal authority, address changes, bankruptcy, lien, and judgment filings) for patients with bipolar I disorder (BPI) or schizophrenia, which has limited studies on mental health and treatment outcomes.
Objective
To conduct a population-level study on disruptive life events by using publicly available data on disruptive life events, aggregated by a consumer credit reporting agency in conjunction with electronic health record (EHR) data.
Design, Setting, and Participants
This study used EHR data from 2 large, integrated health care systems, Kaiser Permanente Southern California and Henry Ford Health. Cohorts of patients diagnosed from 2007 to 2019 with BPI or schizophrenia were matched 1:1 by age at analysis, age at diagnosis (if applicable), sex, race and ethnicity, and Medicaid status to (1) an active comparison group with diagnoses of major depressive disorder (MDD) and (2) a general health (GH) cohort without diagnoses of BPI, schizophrenia, or MDD. Patients with diagnoses of BPI or schizophrenia and their respective comparison cohorts were matched to public records data aggregated by a consumer credit reporting agency (98% match rate). Analysis took place between November 2020 and December 2022.
Main Outcomes and Measures
The differences in the occurrence of disruptive life events among patients with BPI or schizophrenia and their comparison groups.
Results
Of 46 167 patients, 30 008 (65%) had BPI (mean [SD] age, 42.6 [14.2] years) and 16 159 (35%) had schizophrenia (mean [SD], 41.4 [15.1] years). The majoriy of patients were White (30 167 [65%]). In addition, 18 500 patients with BPI (62%) and 6552 patients with schizophrenia (41%) were female. Patients with BPI were more likely to change addresses than patients in either comparison cohort (with the incidence ratio being as high as 1.25 [95% CI, 1.23-1.28]) when compared with GH cohort. Patients with BPI were also more likely to experience any of the financial disruptive life events with odds ratio ranging from 1.15 [95% CI, 1.07-1.24] to 1.50 [95% CI, 1.42-1.58]). The largest differences in disruptive life events were seen in arrests of patients with either BPI or schizophrenia compared with GH peers (3.27 [95% CI, 2.84-3.78] and 3.04 [95% CI, 2.57-3.59], respectively). Patients with schizophrenia had fewer address changes and were less likely to experience a financial event than their matched comparison cohorts.
Conclusions and Relevance
This study demonstrated that data aggregated by a consumer credit reporting agency can support population-level studies on disruptive life events among patients with BPI or schizophrenia.
Introduction
Serious mental illnesses including bipolar I disorder (BPI) and schizophrenia have far-reaching consequences for patients, families, and society as a whole.1,2,3,4,5 Individuals diagnosed with schizophrenia or BPI are at higher risk for disability, premature mortality, and disruptive life events such as being involved with the justice system and becoming homeless or unemployed.6,7,8,9,10,11
Unfortunately, studies on disease exacerbation and efficacy of treatments focus almost exclusively on health care utilization outcomes such as psychiatric emergency department visits and hospitalizations.12,13,14 Existing studies on the occurrence of disruptive life events in US patients with BPI or schizophrenia have been limited by short observation periods, self-reported disruptive life events, or small sample sizes.2,8,15,16,17,18,19 Other studies have indirectly assessed disruptive life events among patients with schizophrenia or BPI by studying the prevalence of psychotic disorders in, for example, homeless or incarcerated populations.20 The lack of objectively measured, longitudinal data for large samples of patients with BPI or schizophrenia limits the ability to conduct population-level research on the timing and co-occurrence of disruptive life events along the course of a patient’s life and mental illness. Improving our understanding of the occurrence and timing of disruptive life events can help target interventions, assess the role of BPI or schizophrenia in patients’ socioeconomic standing, and eventually assess the effectiveness of treatments to improve patients’ life trajectories.
We use public records data aggregated by TransUnion, a consumer credit reporting agency, and electronic health record (EHR) data from 2 diverse health care systems to address this data scarcity issue for disruptive life events. EHR data come from Kaiser Permanente Southern California (KPSC) and Henry Ford Health (HFH) in Michigan from 2007 to 2019. TransUnion provided publicly available data on arrests by a legal authority, address changes (a proxy for residential instability), bankruptcy, lien, and judgment filings for patients 18 years and older.18,21 To demonstrate that these public records data can be used for population-level studies of patients with BPI or schizophrenia, we assessed differences in the occurrence of disruptive life events among patients with these illnesses, an active comparison group of patients with major depressive disorder (MDD) without a diagnosis of BPI or schizophrenia, and a general health (GH) cohort without a diagnosis of BPI, schizophrenia, or MDD. We sought to confirm and add to findings from prior research on less objectively measured data and smaller sample sizes and hypothesize that (1) disruptive life events differ between patients with schizophrenia or BPI and their active comparison cohort with MDD diagnosis and that (2) differences in the risk of disruptive life events are larger when compared with those in the GH cohort than the MDD cohort. To our knowledge, we are the first to demonstrate a population health approach for assessing and comparing the occurrence of disruptive life events among a large sample of US patients with BPI or schizophrenia.
Methods
In addition to a GH cohort, we chose an active comparison cohort of patients with MDD and no diagnoses of BPI or schizophrenia since MDD has some impact on functioning but in most cases is less severe than BPI or schizophrenia. Patients with diagnoses of BPI and schizophrenia and their respective comparison cohorts were identified using data from HFH and KSPC. Each health care system provides care to members in Michigan and Southern California, respectively. Membership has been found to be approximately representative of the respective underlying populations.22,23 Members obtain coverage through private and publicly sponsored plans. KPSC data include MediCal enrollees (Medicaid in California) while HFH data do not. Both health care systems maintain extensive EHRs on the care they provide. Claims data provide information on care provided outside of each health care system. HFH and KPSC are part of the Health Care Research Network, a nationwide consortium of research departments of not-for-profit health care systems.24 The Health Care Research Network has developed a distributed data collection model, the Virtual Data Warehouse, that uses a set of variable definitions to create local standardized data sets to facilitate cross–health care system research.25,26 This study was approved by the institutional review boards of both participating institutions and was determined exempt from obtaining informed consent because it was a retrospective observational study that presented minimal risk to participants.
Participants
We used the Virtual Data Warehouse to identify patients with a first diagnosis of schizophrenia (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] codes 295.0 through 295.9, 297.1, 297.3, 298.8, or 298.9; International Statistical Classification of Diseases, Tenth Revision, Clinical Modification [ICD-10-CM] codes F20.x, F22-25, F28-F29) and BPI (ICD-9-CM codes 296.0x, 296.1x, 296.4x, 296.5x, 296.6x, 296.7x, 296.8x, excluding 296.82; ICD-10-CM codes F30.x, F31.x, excluding F31.81). First diagnoses of nonaffective psychotic disorders were included in the schizophrenia category as they have been found to have a high likelihood of being revised and reclassified as schizophrenia over the course of a person’s illness.27,28 For the same reason, affective disorders not otherwise classified were included in the BPI category.29 We required a patient be given at least 1 inpatient or 2 mental health outpatient diagnoses. First diagnosis had to occur between 5 and 60 years of age. Sensitivity analyses assessed whether limiting our sample to patients receiving their first diagnosis after age 20 years would change results. We excluded patients who received a BPI or schizophrenia diagnosis after a diagnosis of dementia or other neurodegenerative disorder. Patients who had both a diagnosis of schizophrenia and BPI were included in the schizophrenia cohort as they meet criteria for schizoaffective disorder, classified in the DSM-5 as a psychotic disorder.30
We adjusted analyses for incident and prevalent diagnoses of schizophrenia, BPI, or MDD because patients with prevalent diagnoses were more likely to have an illness-related prior history of a disruptive life event before their first recorded diagnosis at KPSC or HFH. Incident diagnoses were defined as first diagnosis given to a patient aged 5 to 29 years with membership for at least 12 months in either health care system before their first diagnosis. The remainder of first documented diagnoses were considered prevalent. TransUnion data for financial disruptive life events and arrests were available up to December 31, 2019. We limited our sample to patients who were aged 18 years by December 31, 2018, to allow for at least 1 year of events to occur after their 18th birthday. Only events occurring after the first diagnosis were considered.
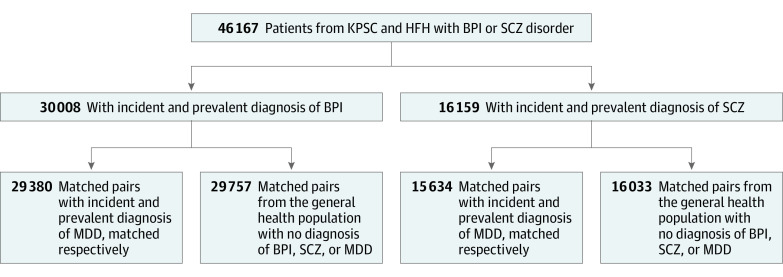
Each health care system performed 1:1 strata matching. Each patient with a schizophrenia or BPI diagnosis was matched to (1) a patient with MDD but no diagnosis of BPI or schizophrenia and (2) a patient without a diagnosis of BPI, schizophrenia, or MDD (GH cohort). We selected variables for matching based on known confounders in the occurrence of disruptive life events.31,32,33 Comparison groups were matched via SAS’s greedy matching algorithm, which matched control patients exactly on sex, race (African American, Asian, White, other/unknown), Medicaid status (KPSC only), and incident and prevalent diagnosis (in the case of the MDD comparison group). All data for matching came from the EHR. The year of diagnosis and calendar age (as of January 1, 2019) were matched within 2-year and 3-year bands, respectively. Of 16 159 patients with schizophrenia, 15 634 were matched to patients with MDD and 16 033 to patients in the GH cohort (Figure 1). For 30 008 patients with BPI, 29 380 were matched to patients with MDD and 29 757 to the GH cohort (Figure 1).
Figure 1. CONSORT Diagram for Building Matched Cohorts.
BPI indicates bipolar I disorder; HFH, Henry Ford Health; KPSC, Kaiser Permanente Southern California; MDD, major depressive disorder; SCZ, schizophrenia.
Outcome Data
Data obtained from TransUnion included (1) lien filings, (2) judgment filings, (3) bankruptcy filings, (4) number of address changes in the past 7 years, and (5) arrests. No information from credit reports or credit scores was used and no data on sex, race and ethnicity, or age were provided by TransUnion. Disruptive life events were available from January 1, 2007, to December 31, 2019. Data on address changes were available for the previous 7 years (as of October 2, 2020, the date of data acquisition) and were provided as counts by TransUnion. Data completeness was comparable across study sites. Lien filing data were incomplete for 2013 onward, thus analysis was limited to lien filings occurring during 2007 to 2013 only. More information on TransUnion outcomes and data sources are available in eAppendix 1 in Supplement 1. Using patients’ names, addresses, dates of birth, and social security numbers, TransUnion was able to link over 98% of patients to their database. Details regarding data safety and transfer can be found in eAppendix 2 and the eFigure in Supplement 1. The same safety procedures were followed for this analytic data set as for all individual-level EHR data. Descriptive information in this manuscript is only presented by broad diagnostic groups to assure patient confidentiality.
Statistical Analysis
We analyzed data of patients with schizophrenia or BPI matched to (1) the MDD active comparison cohort and (2) the GH cohort. To investigate the association between diagnosis and risk of experiencing disruptive life events, we constructed multivariable negative binomial models for count outcomes (address changes) and logistic models for binary outcomes (having a lien, bankruptcy, judgment filing, or arrest). Our models were based on the generalizing estimating equation framework to account for within-pairs correlation and to derive marginal (population-averaged) estimates for our parameters of interest. We assumed an unstructured correlation structure and used robust variance estimators. Models were adjusted for health care system, age at first diagnosis within each health care system (<18, 18-29, ≥30 years), current age (18-44, 45-64, ≥65 years), race and ethnicity, sex, and incident/prevalent diagnosis for patients with BPI/schizophrenia or MDD. Missing race was regrouped with other or multiple races (16.2%), 4 matched pairs that had sex missing were excluded from the analysis. No patient was missing age. We evaluated the impact of multiple testing on results using the Benjamini-Hochberg method (eTable 1 in Supplement 1).34 Statistical analysis was conducted using SAS statistical software version 9.4 (SAS Institute). Analysis took place between November 2020 and December 2022.
Results
Participant Demographics
The Table lists the demographic composition of patients with schizophrenia (n = 16 159) or BPI (n = 30 008) and their respective matched cohorts. KPSC patients comprised 94% of the sample of patients with schizophrenia or BPI. Patients with schizophrenia were more likely to be insured by Medicaid (1694 [10%] vs 2055 [6.8%]), less likely to be female (6552 [41%] vs 18 500 [62%]), less likely to be White (8812 [55%] vs 21 355 [71%]), and more likely to be African American or Black (3313 [21%] vs 3588 [12%]) compared with patients with BPI. The mean (SD) age as of December 31, 2019, of patients with schizophrenia or BPI was 41.4 (15.1) and 42.6 (14.2) years, respectively. The proportion of patients with BPI who experienced at least 1 of each disruptive life event ranged from 2.6% (n = 789) of patients with BPI having an arrest up to 12% (n = 3730) of patients with BPI having a bankruptcy filing. When compared with their respective matched cohorts, patients with schizophrenia were less likely to have a financial disruptive life event, while patients with BPI were more likely. Patients with schizophrenia had a higher rate of arrests than patients with BPI (3.4% [n = 542] vs 2.6% [n = 789]). The mean (SD) number of address changes was low across all cohorts (1.0 [1.6] and 1.6 [1.9] for patients with schizophrenia and BPI, respectively).
Table. Baseline Characteristics of Matched Cohorts.
| Characteristic | No. (%) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| SCZ and BPI | SCZ matched to MDD | SCZ matched to GH | BPI matched to MDD | BPI matched to GH | ||||||
| SCZ | BPI | SCZ | MDD | SCZ | GH | BPI | MDD | BPI | GH | |
| No. | 16 159 | 30 008 | 15 634 | 15 634 | 16 033 | 16 033 | 29 380 | 29 380 | 29 757 | 29 757 |
| Health care organization | ||||||||||
| HFH | 725 (4.5) | 2266 (7.6) | 600 (3.8) | 600 (3.8) | 658 (4.1) | 658 (4.1) | 1893 (6.4) | 1893 (6.4) | 2095 (7.0) | 2095 (7.0) |
| KPSC | 15 434 (95.5) | 27 742 (92.4) | 15 034 (96.2) | 15 034 (96.2) | 15 375 (95.9) | 15 375 (95.9) | 27 487 (93.6) | 27 487 (93.6) | 27 662 (93.0) | 27 662 (93.0) |
| Femalea | 6552 (40.5) | 18 500 (61.7) | 6460 (41.3) | 6460 (41.3) | 6498 (40.5) | 6498 (40.5) | 18 253 (62.1) | 18 253 (62.1) | 18 354 (61.7) | 18 354 (61.7) |
| Malea | 9607 (59.4) | 11 508 (38.3) | 9174 (58.7) | 9174 (58.7) | 9535 (59.5) | 9535 (59.5) | 11 127 (37.9) | 11 127 (37.9) | 11 403 (38.3) | 11 403 (38.3) |
| Age at first EHR-recorded diagnosis, mean (SD), y | 32.6 (13.3) | 33.5 (12.9) | 32.7 (13.4) | 32.7 (13.4) | 32.6 (13.3) | 32.6 (13.3) | 33.5 (12.8) | 33.5 (12.8) | 33.5 (12.8) | 33.5 (12.8) |
| Age on December 31, 2019, mean (SD), y | 41.4 (15.1) | 42.6 (14.2) | 41.3 (15.2) | 41.2 (15.2) | 41.5 (15.1) | 40.2 (14.2) | 42.6 (14.2) | 42.5 (14.2) | 42.7 (14.2) | 41.7 (13.5) |
| Race and ethnicity | ||||||||||
| Asian | 1357 (8.4) | 1294 (4.3) | 1306 (8.4) | 1306 (8.4) | 1350 (8.4) | 1350 (8.4) | 1255 (4.3) | 1255 (4.3) | 1289 (4.3) | 1289 (4.3) |
| Black | 3313 (20.5) | 3588 (12.0) | 3078 (19.7) | 3078 (19.7) | 3261 (20.3) | 3261 (20.3) | 3395 (12) | 3395 (12) | 3531 (11.9) | 3531 (11.9) |
| White | 8812 (54.5) | 21 355 (71.2) | 8650 (55.3) | 8650 (55.3) | 8759 (54.6) | 8759 (54.6) | 21 066 (72) | 21 066 (72) | 21 194 (71.2) | 21 194 (71.2) |
| Otherb/multiracial/unknown | 2677 (16.6) | 3771 (12.6) | 2600 (16.6) | 2600 (16.6) | 2663 (16.6) | 2663 (16.6) | 3664 (11.6) | 3664 (11.6) | 3743 (12.6) | 3743 (12.6) |
| Enrolled in Medicaid | 1694 (10.5) | 2055 (6.8) | 1580 (10.1) | 1580 (10) | 1675 (10.4) | 1675 (10.4) | 2000 (6.8) | 2000 (6.8) | 2046 (6.9) | 2046 (6.9) |
| Incident diagnosis | 4937 (30.6) | 6680 (22.3) | 4862 (31.1) | 4862 (31.1) | 4859 (30.3) | 0 | 6601 (22.5) | 6601 (22.5) | 6592 (22.2) | 0 |
| No. of address changes, mean (SD) | 1.0 (1.6) | 1.6 (1.9) | 1.0 (1.6) | 1.4 (1.8) | 1.0 (1.6) | 1.2 (1.6) | 1.6 (1.9) | 1.5 (1.8) | 1.6 (1.9) | 1.3 (1.7) |
| Had a previous arrestc | 542 (3.4) | 789 (2.6) | 526 (3.4) | 222 (1.4) | 540 (3.4) | 186 (1.2) | 775 (2.6) | 366 (1.2) | 787 (2.6) | 249 (0.8) |
| Had a lien filingd | 531 (3.8) | 1548 (5.7) | 769 (5.8) | 507 (3.8) | 611 (4.4) | 528 (3.8) | 1511 (5.7) | 1329 (5.0) | 1537 (5.8) | 1128 (4.2) |
| Had a judgment filingc | 1451 (9.0) | 3270 (10.9) | 1405 (9.0) | 1616 (10.3) | 1450 (9.0) | 1489 (9.3) | 3209 (10.9) | 2842 (9.7) | 3264 (11.0) | 2362 (7.9) |
| Bankruptcy filingc | 1153 (7.1) | 3730 (12.4) | 1115 (7.1) | 1650 (10.6) | 1148 (7.2) | 1299 (8.1) | 3626 (12.3) | 3593 (12.2) | 3700 (12.4) | 2632 (8.8) |
Abbreviations: BPI, bipolar I disorder; GH, general health; HFH, Henry Ford Health; KPSC, Kaiser Permanente Southern California; EHR, electronic health record; MDD, major depressive disorder; SCZ, schizophrenia.
Seven patients had sex missing (3 patients with SCZ, their 3 GH matches, and 1 patient with MDD that had been matched to one of the patients with SCZ and missing sex).
The other race and ethnicity group included American Indian, Alaskan Native, Native Hawaiian, and Pacific Islander.
For bankruptcy filings, judgment filings, and arrests, only data from 2007 to 2019 were used.
For lien filings, only data from 2007 to 2013 were used. All individuals had to be at least 18 years old on December 31, 2012, so the denominators for lien filings are 13 927 for SCZ and 27 049 for SCZ and BPI; 13 301 for SCZ matched to MDD; 13 789 for SCZ matched to GH; 26 372 for BPI matched to MDD; and 26 372 for BPI matched to GH.
Disruptive Life Events
Figure 2 displays the results of our analyses (full results available in eTable 3 in Supplement 1). Patients with schizophrenia were less likely to move than patients in either of the comparison groups. Patients with BPI had a higher risk of experiencing a move, particularly when compared with the GH cohort (n = 29 757; incidence rate ratio, 1.25 [95% CI, 1.23-1.28]). Patients with schizophrenia were throughout at significantly lower odds of a financial disruptive life event compared with either comparison group. The odds of a bankruptcy filing were, for example, 36% lower for patients with schizophrenia compared with the MDD cohort (n = 15 634; odds ratio, 0.64 [95% CI, 0.59-0.69]). In contrast, patients with BPI had higher odds of a financial disruptive life event than either comparison cohort. The odds of experiencing a bankruptcy filing, for instance, were up to 50% higher (odds ratio, 1.5 [95% CI, 1.42-1.58]) when compared with the GH cohort. The odds for arrests were high for both patients with schizophrenia and BPI and highest when compared with each respective GH cohort. Patients with schizophrenia had 3.04 times higher odds (95% CI, 2.57-3.59), and patients with BPI 3.27 times higher odds of arrests (95% CI, 2.84-3.78) than their GH cohort matches. Results of schizophrenia/BPI cohort comparisons with the MDD and GH cohort mirror findings from the descriptive tables that suggests patients with MDD struggle more than patients in the GH cohort when it comes to disruptive life events (eAppendix 3 in Supplement 1). Sensitivity analysis excluding patients diagnosed at age younger than 20 years and adjustment for multiple comparisons demonstrated stability of results (eTables 2 and 1 in Supplement 1, respectively).
Figure 2. Incidence Rate Ratios (IRRs)/Odds Ratios (ORs) and 95% CIs for Address Changes, Arrests, Lien Filings, Judgment Filings, and Bankruptcy Filings.
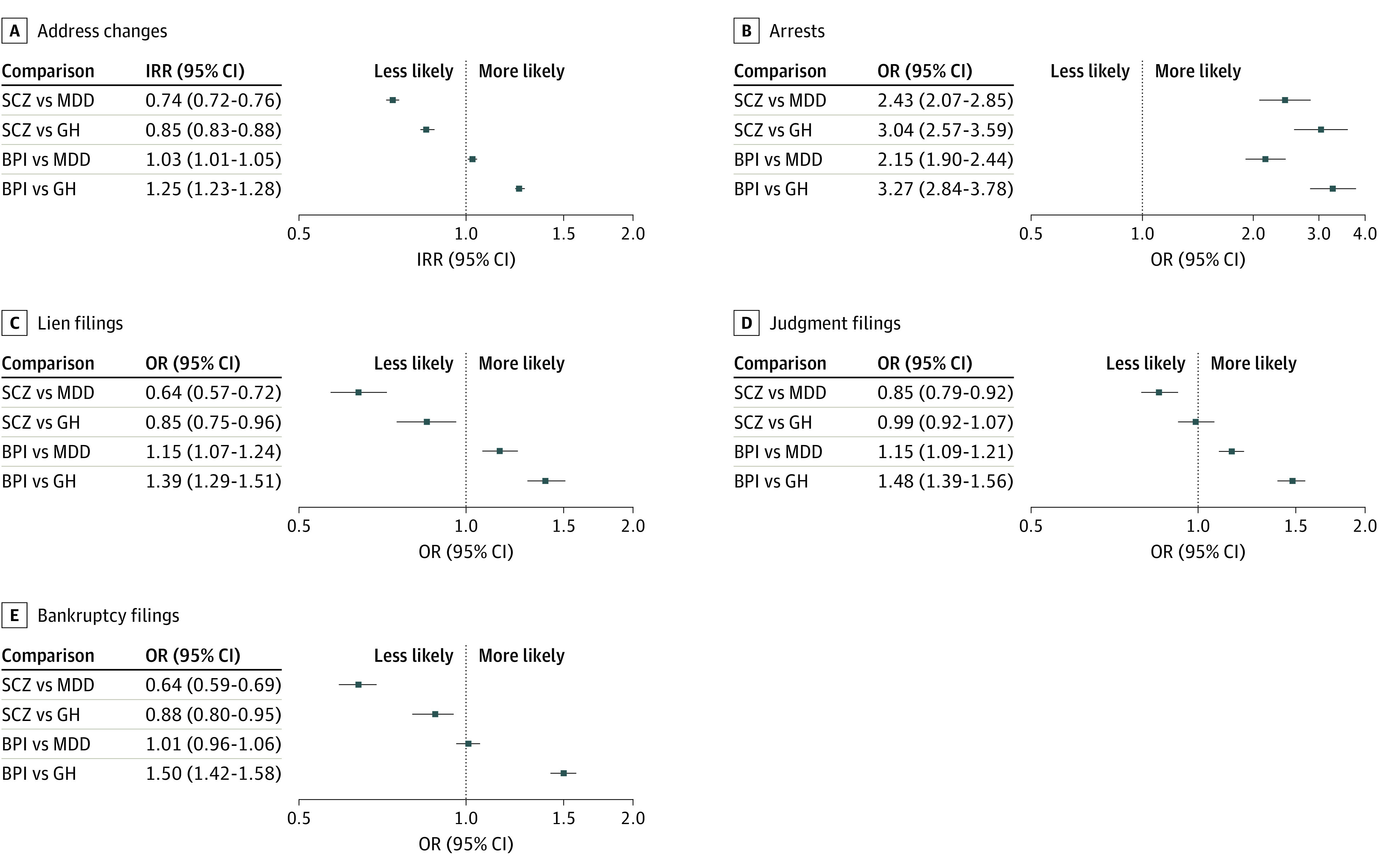
Disruptive life events among patients with diagnoses of schizophrenia (SCZ) or bipolar I disorder (BPI) compared with a major depressive disorder (MDD) cohort and a general health (GH) cohort. All models are adjusted for health care system, age at first diagnosis within each health care system, current age, race and ethnicity, sex, and incident/prevalent diagnosis. Outcome data were available from 2007-2019, except for lien filings, for which data were only available from 2007-2013.
Discussion
This study assessed the risk of disruptive life events among patients with schizophrenia or BPI by joining EHR records and novel public records data from TransUnion. Our findings align with and add to results from prior research using self-reported data or small sample sizes among US patients.2,9,15,35,36,37 We found that patients with BPI were more likely to experience a financial disruptive life event and change addresses compared with either comparison group. Patients with schizophrenia were less likely to have address changes and experience financial disruptive life events compared with the 2 comparison cohorts. Compared with each GH cohort, the odds of patients with schizophrenia or BPI being arrested were 3.04- and 3.27-times higher.
Numerous studies have investigated the effect of BPI and related disorders on perceived financial well-being.6,9,17,37,38 Patients with BPI have been found to have lower incomes, be more likely to report compulsive buying, to incur a financial crises, or to have lower self-perceived financial well-being.6,9 Our study mirrors these findings but better quantifies the phenomenon by analyzing a large sample, objectively reported outcomes, and matched comparison diagnostic groups. We found lower odds of these events for patients with schizophrenia. Bankruptcy, lien, and judgment filings require the ability to earn wages and accumulate wealth. Prior studies show that unemployment among patients with schizophrenia is high and that severity of mental illness affects lifetime employment and income.17,39,40,41 We hypothesize that because of the severity of schizophrenia, patients had lower odds of these events because they were less able to accumulate assets on which creditors could put a claim on.
BPI and schizophrenia are highly prevalent mental health diagnoses among the homeless population.8,20,42,43 Two studies assessing homelessness following a psychiatry encounter found that 7.6% experienced homelessness within 90 days and 15% of patients experienced homelessness within 12 months.8,18 We used the number of address changes as a proxy for residential instability, a common precursor to homelessness.44 Our findings provide additional evidence for higher residential instability for patients with BPI, while there were fewer address changes for patients with schizophrenia. Patients with schizophrenia may have lower odds of address changes because they may be persistently homeless or more likely to live in residential group homes or other supportive living environments.2,35,45
Prior studies have found high incidence of arrests among patients with BPI or schizophrenia.6,7,15,18 Fazel et al7 used Swedish public record data to calculate arrest rates among patients with psychotic disorders.7 Other US studies have asked patients to self-report arrests through surveys.6,15,18 To our knowledge, our study is among the first to link arrest records to EHR data for patients with BPI or schizophrenia and a comparison cohort.
Limitations
Despite using a large, diverse sample of patients with clinical diagnoses of schizophrenia and BPI, this research has important limitations. The patient populations were drawn from 2 large integrated health care systems; therefore, treatment patterns and care coordination of patients with mental health conditions may be different than in other care settings. The health care systems were in Southern California and in Michigan, and therefore results may not be generalizable to other areas of the US. We adjusted for incident or prevalent diagnosis; nevertheless, patients with incident diagnoses may have been struggling with their illness and disruptive life events for an unknown time before they received their first diagnosis at KPSC or HFH. While we matched our cohorts on major demographic confounders and Medicaid enrollment, EHR data do not provide us with information on other potential confounders such as employment or income. We also did not match patients on comorbidity burden, a task that goes beyond the scope of this project. Lien filings data were incomplete for 2013 onward and analyses were limited to lien filings occurring during 2007 to 2013 only. Also, TransUnion crime data do not currently include any reliable indicators for the seriousness of a person’s offense leading to an arrest. TransUnion public records data include public court data and other public data and web sources. We avoided the use of outcomes such as TransUnion’s public employment data, which heavily depends on a person’s internet presence and on self-reported sources, such as LinkedIn. The experience of living with a mental illness is likely to affect not just a person’s career trajectory but also its comprehensive documentation on a job-related webpage like Linkedin.46 We demonstrated concordant and discordant validity of disruptive life event outcomes; however, we were not able to confirm the completeness of data assembled by TransUnion by cross-checking the original data sources. Future research should investigate the timing of events as rates of disruptive life events are likely to vary across the course of a person’s illness.
Our team went to great lengths to protect patient data and confidentiality for this research study. TransUnion data have the potential to support clinical applications such as the prediction of suicide risk used in clinical decision support. Also, information from nonpublic financial records such as credit scores may provide more accurate information. However, important privacy concerns need to be explored; before these kind of data, even if limited to publicly available information, are used in the context of clinical care.47 Potential benefits of improving care and patient outcomes, and possibly even saving lives—as in the case of suicide prediction—need to be weighed with patient preferences around the use of such information.
Conclusions
Population health studies on the occurrence of disruptive life events, particularly those conducted in the US, have been hampered by the lack of reliable disruptive life events data. Public records data from TransUnion, as demonstrated here, can address this dearth. Currently, researchers conduct efficacy studies for treatment of schizophrenia and BPI using clinical outcomes such as changes in psychiatric hospitalizations and emergency department visits. Reliable longitudinal data on disruptive life events may allow assessment of the efficacy of treatments, not just on clinical outcomes, but on the course of patients’ lives.
eAppendix 1. Description of TransUnion Data
eReferences.
eAppendix 2. Multistep process to safeguard health data
eFigure. Process of merging clinical data from Kaiser Permanente Southern California (KPSC) and Henry Ford Health Systems (HFHS) and Transunion HealthCare (TUCH) disruptive life events data (DLE)
eAppendix 3. Analysis code for the study outcomes
eTable 1. P-values adjusted for multiple testing using the Benjamini-Hochberg
eTable 2. Sensitivity analysis restricting patients to those aged 20 or older at time of diagnosis
eTable 3. Coefficients and Confidence Intervals for the full models
Data sharing statement
References
- 1.Cloutier M, Greene M, Guerin A, Touya M, Wu E. The economic burden of bipolar I disorder in the United States in 2015. J Affect Disord. 2018;226:45-51. doi: 10.1016/j.jad.2017.09.011 [DOI] [PubMed] [Google Scholar]
- 2.Mausbach BT, Depp CA, Cardenas V, Jeste DV, Patterson TL. Relationship between functional capacity and community responsibility in patients with schizophrenia: differences between independent and assisted living settings. Community Ment Health J. 2008;44(5):385-391. doi: 10.1007/s10597-008-9141-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tsemberis S, McHugo G, Williams V, Hanrahan P, Stefancic A. Measuring homelessness and residential stability: the residential time-line follow-back inventory. J Community Psychology. 2007;35(1):29-42. doi: 10.1002/jcop.20132 [DOI] [Google Scholar]
- 4.Zhang W, Amos TB, Gutkin SW, Lodowski N, Giegerich E, Joshi K. A systematic literature review of the clinical and health economic burden of schizophrenia in privately insured patients in the United States. Clinicoecon Outcomes Res. 2018;10:309-320. doi: 10.2147/CEOR.S156308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Granek L, Danan D, Bersudsky Y, Osher Y. Living with bipolar disorder: the impact on patients, spouses, and their marital relationship. Bipolar Disord. 2016;18(2):192-199. doi: 10.1111/bdi.12370 [DOI] [PubMed] [Google Scholar]
- 6.Blanco C, Wall MM, Hoertel N, et al. Psychiatric disorders and risk for multiple adverse outcomes: a national prospective study. Mol Psychiatry. 2021;26(3):907-916. doi: 10.1038/s41380-019-0459-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fazel S, Wolf A, Palm C, Lichtenstein P. Violent crime, suicide, and premature mortality in patients with schizophrenia and related disorders: a 38-year total population study in Sweden. Lancet Psychiatry. 2014;1(1):44-54. doi: 10.1016/S2215-0366(14)70223-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Folsom DP, Hawthorne W, Lindamer L, et al. Prevalence and risk factors for homelessness and utilization of mental health services among 10,340 patients with serious mental illness in a large public mental health system. Am J Psychiatry. 2005;162(2):370-376. doi: 10.1176/appi.ajp.162.2.370 [DOI] [PubMed] [Google Scholar]
- 9.Hakulinen C, Musliner KL, Agerbo E. Bipolar disorder and depression in early adulthood and long-term employment, income, and educational attainment: a nationwide cohort study of 2,390,127 individuals. Depress Anxiety. 2019;36(11):1080-1088. doi: 10.1002/da.22956 [DOI] [PubMed] [Google Scholar]
- 10.Ko YS, Tsai HC, Chi MH, et al. Higher mortality and years of potential life lost of suicide in patients with schizophrenia. Psychiatry Res. 2018;270:531-537. doi: 10.1016/j.psychres.2018.09.038 [DOI] [PubMed] [Google Scholar]
- 11.Verdolini N, Pacchiarotti I, Köhler CA, et al. Violent criminal behavior in the context of bipolar disorder: systematic review and meta-analysis. J Affect Disord. 2018;239:161-170. doi: 10.1016/j.jad.2018.06.050 [DOI] [PubMed] [Google Scholar]
- 12.Hardy M, Jackson C, Byrne J. Antipsychotic adherence and emergency department utilization among patients with schizophrenia. Schizophr Res. 2018;201:347-351. doi: 10.1016/j.schres.2018.06.006 [DOI] [PubMed] [Google Scholar]
- 13.Luciano A, Metcalfe JD, Bond GR, et al. Hospitalization risk before and after employment among adults with schizophrenia, bipolar disorder, or major depression. Psychiatr Serv. 2016;67(10):1131-1138. doi: 10.1176/appi.ps.201500343 [DOI] [PubMed] [Google Scholar]
- 14.Sun SX, Liu GG, Christensen DB, Fu AZ. Review and analysis of hospitalization costs associated with antipsychotic nonadherence in the treatment of schizophrenia in the United States. Curr Med Res Opin. 2007;23(10):2305-2312. doi: 10.1185/030079907X226050 [DOI] [PubMed] [Google Scholar]
- 15.Hodgins S, Alderton J, Cree A, Aboud A, Mak T. Aggressive behaviour, victimization and crime among severely mentally ill patients requiring hospitalisation. Br J Psychiatry. 2007;191(4):343-350. doi: 10.1192/bjp.bp.106.06.029587 [DOI] [PubMed] [Google Scholar]
- 16.Khalsa HMK, Baldessarini RJ, Tohen M, Salvatore P. Aggression among 216 patients with a first-psychotic episode of bipolar I disorder. Int J Bipolar Disord. 2018;6(1):18. doi: 10.1186/s40345-018-0126-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nordt C, Müller B, Rössler W, Lauber C. Predictors and course of vocational status, income, and quality of life in people with severe mental illness: a naturalistic study. Soc Sci Med. 2007;65(7):1420-1429. doi: 10.1016/j.socscimed.2007.05.024 [DOI] [PubMed] [Google Scholar]
- 18.Olfson M, Mechanic D, Hansell S, Boyer CA, Walkup J. Prediction of homelessness within three months of discharge among inpatients with schizophrenia. Psychiatr Serv. 1999;50(5):667-673. doi: 10.1176/ps.50.5.667 [DOI] [PubMed] [Google Scholar]
- 19.Johnson SL. Life events in bipolar disorder: towards more specific models. Clin Psychol Rev. 2005;25(8):1008-1027. doi: 10.1016/j.cpr.2005.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Iwundu CN, Chen T-A, Edereka-Great K, Businelle MS, Kendzor DE, Reitzel LR. Mental illness and youth-onset homelessness: a retrospective study among adults experiencing homelessness. Int J Environ Res Public Health. 2020;17(22):8295. doi: 10.3390/ijerph17228295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Desmond M, Perkins KL. Housing and household instability. Urban Aff Rev. 2016;52(3):421-436. doi: 10.1177/1078087415589192 [DOI] [Google Scholar]
- 22.Koebnick C, Langer-Gould AM, Gould MK, et al. Sociodemographic characteristics of members of a large, integrated health care system: comparison with US Census Bureau data. Perm J. 2012;16(3):37-41. doi: 10.7812/TPP/12-031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rossom RC, Coleman KJ, Ahmedani BK, et al. Suicidal ideation reported on the PHQ9 and risk of suicidal behavior across age groups. J Affect Disord. 2017;215:77-84. doi: 10.1016/j.jad.2017.03.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Coleman KJ, Stewart C, Waitzfelder BE, et al. Racial-ethnic differences in psychiatric diagnoses and treatment across 11 health care systems in the mental health research network. Psychiatr Serv. 2016;67(7):749-757. doi: 10.1176/appi.ps.201500217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ross TR, Ng D, Brown JS, et al. The HMO research network virtual data warehouse: a public data model to support collaboration. EGEMS (Wash DC). 2014;2(1):1049. doi: 10.13063/2327-9214.1049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mental Health Research Network Projects. Accessed April 3, 2023. https://mhresearchnetwork.org/
- 27.Fusar-Poli P, Cappucciati M, Rutigliano G, et al. Diagnostic stability of ICD/DSM first episode psychosis diagnoses: meta-analysis. Schizophr Bull. 2016;42(6):1395-1406. doi: 10.1093/schbul/sbw020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Haahr U, Friis S, Larsen TK, et al. First-episode psychosis: diagnostic stability over one and two years. Psychopathology. 2008;41(5):322-329. doi: 10.1159/000146070 [DOI] [PubMed] [Google Scholar]
- 29.Saunders KEA, Goodwin GM. The course of bipolar disorder. Adv Psychiatr Treat. 2010;16(5):318-328. doi: 10.1192/apt.bp.107.004903 [DOI] [Google Scholar]
- 30.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013. [Google Scholar]
- 31.Diler RS, Merranko JA, Hafeman D, et al. Higher socioeconomic status and less parental psychopathology improve prognosis in youths with bipolar disorder. J Affect Disord. 2022;302:185-193. doi: 10.1016/j.jad.2022.01.058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Durbin A, Rudoler D, Durbin J, Laporte A, Callaghan RC. Examining patient race and area predictors of inpatient admission for schizophrenia among hospital users in California. J Immigr Minor Health. 2014;16(6):1025-1034. [DOI] [PubMed] [Google Scholar]
- 33.Holm M, Taipale H, Tanskanen A, Tiihonen J, Mitterdorfer-Rutz E. Employment among people with schizophrenia or bipolar disorder: a population-based study using nationwide registers. Acta Psychiatr Scand. 2021;143(1):61-71. doi: 10.1111/acps.13254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Series B Stat Methodol. 1995;57(1):289-300. doi: 10.1111/j.2517-6161.1995.tb02031.x [DOI] [Google Scholar]
- 35.De Girolamo G, Bassi M. Residential facilities as the new scenario of long-term psychiatric care. Curr Opin Psychiatry. 2004;17(4):275-281. [Google Scholar]
- 36.Downward P, Rasciute S, Kumar H. Health, subjective financial situation and well-being: a longitudinal observational study. Health Qual Life Outcomes. 2020;18(1):203. doi: 10.1186/s12955-020-01456-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Richardson T, Jansen M, Fitch C. Financial difficulties in bipolar disorder part 1: longitudinal relationships with mental health. J Ment Health. 2018;27(6):595-601. doi: 10.1080/09638237.2018.1521920 [DOI] [PubMed] [Google Scholar]
- 38.Zimmerman M, Balling C, Chelminski I, Dalrymple K. Patients with borderline personality disorder and bipolar disorder: a descriptive and comparative study. Psychol Med. 2021;51(9):1479-1490. doi: 10.1017/S0033291720000215 [DOI] [PubMed] [Google Scholar]
- 39.Baldwin ML, Marcus SC. Labor market outcomes of persons with mental disorders. Ind Relat. 2007;46(3):481-510. doi: 10.1111/j.1468-232X.2007.00478.x [DOI] [Google Scholar]
- 40.Marwaha S, Johnson S. Schizophrenia and employment: a review. Soc Psychiatry Psychiatr Epidemiol. 2004;39(5):337-349. doi: 10.1007/s00127-004-0762-4 [DOI] [PubMed] [Google Scholar]
- 41.Rosenheck R, Leslie D, Keefe R, et al. Barriers to employment for people with schizophrenia. Am J Psychiatry. 2006;163(3):411-417. doi: 10.1176/appi.ajp.163.3.411 [DOI] [PubMed] [Google Scholar]
- 42.Ayano G, Shumet S, Tesfaw G, Tsegay L. A systematic review and meta-analysis of the prevalence of bipolar disorder among homeless people. BMC Public Health. 2020;20(1):731. doi: 10.1186/s12889-020-08819-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Foster A, Gable J, Buckley J. Homelessness in schizophrenia. Psychiatr Clin North Am. 2012;35(3):717-734. doi: 10.1016/j.psc.2012.06.010 [DOI] [PubMed] [Google Scholar]
- 44.Giano Z, Williams A, Hankey C, Merrill R, Lisnic R, Herring A. Forty years of research on predictors of homelessness. Community Ment Health J. 2020;56(4):692-709. doi: 10.1007/s10597-019-00530-5 [DOI] [PubMed] [Google Scholar]
- 45.Trieman N, Smith HE, Kendal R, Leff J. The TAPS Project 41: homes for life? residential stability five years after hospital discharge. Community Ment Health J. 1998;34(4):407-417. doi: 10.1023/a:1018792108559 [DOI] [PubMed] [Google Scholar]
- 46.Spanakis P, Peckham E, Mathers A, Shiers D, Gilbody S. The digital divide: amplifying health inequalities for people with severe mental illness in the time of COVID-19. Br J Psychiatry. 2021;219(4):529-531. doi: 10.1192/bjp.2021.56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yarborough BJH, Stumbo SP. Patient perspectives on acceptability of, and implementation preferences for, use of electronic health records and machine learning to identify suicide risk. Gen Hosp Psychiatry. 2021;70:31-37. doi: 10.1016/j.genhosppsych.2021.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix 1. Description of TransUnion Data
eReferences.
eAppendix 2. Multistep process to safeguard health data
eFigure. Process of merging clinical data from Kaiser Permanente Southern California (KPSC) and Henry Ford Health Systems (HFHS) and Transunion HealthCare (TUCH) disruptive life events data (DLE)
eAppendix 3. Analysis code for the study outcomes
eTable 1. P-values adjusted for multiple testing using the Benjamini-Hochberg
eTable 2. Sensitivity analysis restricting patients to those aged 20 or older at time of diagnosis
eTable 3. Coefficients and Confidence Intervals for the full models
Data sharing statement