To the Editor,
Recently, in the Journal, Baedorf Kassis et al 1 compared adaptive support ventilation (ASV) with conventional invasive ventilation with respect to important ventilator settings in subjects with ARDS. The results of their randomized crossover clinical trial, confirm the results of another study that compared ASV with invasive ventilation. 2 Indeed, ASV keeps tidal volume (VT) within the broadly accepted safety limit. With automated ventilation modes like ASV, VT decreases especially in patients with a higher driving pressure (ΔP).
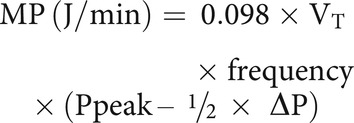
Mechanical power (MP) of ventilation is the amount of energy transferred from the ventilator to the respiratory system, a summary value that includes relevant components of lung-protective ventilation 3 that have been shown to have associations with patient-centered outcomes as well as mortality. 4 - 6 In the study of Baedorf Kassis et al, 1 the amount of MP was 28.2 [22.2–36.4] J/min and 26.9 [23.8–37.9] J/min, with ASV and with invasive ventilation, respectively, surprisingly higher than in other studies in subjects with ARDS. 4,5 This difference may be driven by disease severity: the sicker the lungs, the higher the MP. However, differences may also be caused by differences in the way MP was calculated. Baedorf Kassis et al determined the inspiratory work of breathing from the area under the inspiratory limb of the airway pressure/volume curve and multiplied it by the breathing frequency to calculate the MP. 7,8 This is somewhat different from the frequently used simple equation for MP, wherein VT is multiplied by frequency and the difference between peak pressure and ΔP: 3
We are aware that it is not certain yet what the correct method is to calculate MP, but to allow comparison with other studies, it would be helpful if Baedorf Kassis et al also provide MP calculated by using the simple equation. Besides, given that all of the subjects in this study received an esophageal balloon catheter as standard of care, it would be very interesting to also see the MP of the lung (ie, using the transpulmonary pressures with the equation mentioned above).
We also noticed in their study that permissive hypercapnia may not have been used in all subjects, since the reported median arterial pH was normal. This suggests that clinicians may have targeted a more “normal” arterial PaCO2 that corrects the arterial pH, than accepting a “high” arterial PaCO2 as part of permissive hypercapnia. Could this also explain the high MP in their study? In fact, permissive hypercapnia is an attractive way to reduce MP. Since each breath contains energy, decreasing the number of breaths, as part of permissive hypercapnia, lowers the total energy. It is uncertain how ASV will compare to traditional ventilation with regard to MP when permissive hypercapnia is used.
Footnotes
Ms Buiteman-Kruizinga and Dr Schultz disclose relationships with Hamilton Medical.
Dr Schultz is Director of Research for Hamilton Medical.
REFERENCES
- 1. Baedorf Kassis EN, Bastos AB, Schaefer MS, Capers K, Hoenig B, Banner-Goodspeed V, et al. Adaptive support ventilation and lung-protective ventilation in ARDS. Respir Care 2022. [DOI] [PubMed] [Google Scholar]
- 2. Buiteman-Kruizinga LA, Mkadmi HE, Schultz MJ, Tangkau PL, van der Heiden PLJ. Comparison of mechanical power during adaptive support ventilation versus nonautomated pressure controlled ventilation-a pilot study. Crit Care Explor 2021;3(2):e0335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gattinoni L, Tonetti T, Cressoni M, Cadringher P, Herrmann P, Moerer O, et al. Ventilator-related causes of lung injury: the mechanical power. Intensive Care Med 2016;42(10):1567-1575. [DOI] [PubMed] [Google Scholar]
- 4. Urner M, Jüni P, Hansen B, Wettstein MS, Ferguson ND, Fan E. Time-varying intensity of mechanical ventilation and mortality in patients with acute respiratory failure: a registry-based, prospective cohort study. Lancet Respir Med 2020;8(9):905-913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Serpa Neto A, Deliberato RO, Johnson AEW, Bos LD, Amorim P, Pereira SM, et al. ; PROVE Network Investigators. Mechanical power of ventilation is associated with mortality in critically ill patients: an analysis of patients in two observational cohorts. Intensive Care Med 2018;44(11):1914-1922. [DOI] [PubMed] [Google Scholar]
- 6. Costa ELV, Slutsky AS, Brochard LJ, Brower R, Serpa Neto A, Cavalcanti AB, et al. Ventilatory variables and mechanical power in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med 2021;204(3):303-311. [DOI] [PubMed] [Google Scholar]
- 7. Schaefer MS, Loring SH, Talmor D, Baedorf-Kassis EN. Comparison of mechanical power estimations in mechanically ventilated patients with ARDS: a secondary data analysis from the EPVent study. Intensive Care Med 2021;47(1):130-132. [DOI] [PubMed] [Google Scholar]
- 8. Chiumello D, Gotti M, Guanziroli M, Formenti P, Umbrello M, Pasticci I, et al. Bedside calculation of mechanical power during volume and pressure controlled mechanical ventilation. Crit Care 2020;24(1):417. [DOI] [PMC free article] [PubMed] [Google Scholar]


