Dear Editor,
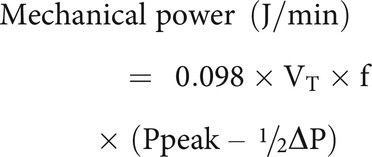
We would like to thank Dr Bruitman-Kruizinga and Dr Schultz for their interest in our study 1 and their important comments. The authors postulate that measuring mechanical power from continuous recordings in our study yielded a higher mechanical power when compared to previous studies, and they propose using the more widely applied simplified formula: 2
We would like to emphasize that this mathematical approximation has only been validated during volume controlled mechanical ventilation, 3 , 4 and some authors have suggested alternative formulas. 3 -6 Most importantly, the above formula has not been validated in patients receiving adaptive support ventilation (ASV) or other pressure-regulated modes of ventilation such as adaptive pressure ventilation (APV) (which were the 2 ventilator modes utilized in the initial study). In response to the comments by Dr Bruitman-Kruizinga and Dr Schultz, we calculated mechanical power using this formula, which was 21.8 [interquartile range [IQR] 18.9–31.8] J/min in ASV and 22.3 [IQR 19.2–29.8] J/min in APV in comparison to 28.2 [22.2–36.4] J/min and 26.9 [23.8–37.9] J/min for ASV and APV, respectively, calculated in our manuscript. We would like to take this opportunity to discuss the use of simplified formulae when estimating mechanical power.
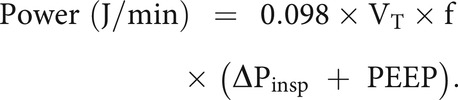
Any simplified formula makes assumptions about the shape of the pressure-volume curve during inspiration. During volume controlled ventilation, the pressure and volume change will occur in a roughly linear manner (when in a square flow pattern), approximating a triangular shape for the driving pressure component of mechanical power (which is favorable for the proposed formula). By contrast, with a pressure controlled breath, the driving pressure component of mechanical power on the pressure-volume curve approximates a rectangular shape. 6 Therefore, a separate formula has been proposed for pressure controlled ventilation, which might be more appropriate when using ASV and APV. 4 - 6
(Where Pinsp is the change in Paw during inspiration, the pressure control level while in pressure control or the inspiratory applied pressure in ASV or APV.)
Utilizing this surrogate formula for pressure control ventilation instead of the initial proposed formula by Dr Bruitman-Kruizinga and Dr Schultz resulted in a higher estimated mechanical power for the patients while on ASV (28.5 [IQR 21.5–37.7] J/min) and on APV (28.2 [IQR 24.7–33.4] J/min). Notably, this mechanical power estimate provided values very similar to those measured in our study directly via waveforms. Due to the limitations and approximations implied in these formulas, calculation of mechanical power from continuous recordings has been the accepted standard to which abbreviated formulas have been compared. 7 Whereas these formulas can be very helpful in epidemiological research, we believe in utilizing the highest available data granularity when continuous recordings are available.
Other factors may have contributed to a higher mechanical power in our study. One important and much-discussed factor included into mechanical power calculations is PEEP. In our study, PEEP was titrated using esophageal manometry as per routine clinical care at our institution. 8 This often results in higher PEEP levels 9 compared to standard PEEP tables. 10 Indeed, approximately 50% of the measured mechanical power in our cohort was due to the PEEP component. There is extensive debate regarding inclusion of the PEEP component into mechanical power, with many advocating for removal of this from the measurement. 11 - 14 Suffice to say, with widely different PEEP strategies between studies, it is challenging to compare mechanical power between different studies.
Another limitation of the commonly used calculation of mechanical power is the inclusion of the chest wall component. Due to the availability of esophageal pressure recordings, we calculated “lung-directed power” (total mechanical power delivered to the lung and excluding the chest wall). These values in ASV were 12.3 [9.8–17.6] J/min and 12.5 [9.6–17.0] J/min in APV. Currently there is not an agreed upon method for calculation of lung directed power, 12 nor a simplified formula to estimate this value. As such, we did not include it into the initial manuscript.
We agree with Dr Bruitman-Kruizinga and Dr Schultz about modulation of mechanical power by permissive hypercapnia, which can be an effective way to decrease the energy delivered to the respiratory system. In our study, the protocol dictated that minute ventilation during day 1 crossover measurements would remain unchanged from the baseline values established by the clinical team, so we cannot analyze the impact of clinical variation in breathing frequency as well as permissive hypercapnia on mechanical power in this study. Using permissive hypercapnia to lower mechanical power, however, will be an important tool for future investigations.
In conclusion, the letter by Dr Bruitman-Kruizinga and Dr Schultz, as well as the discussion above, highlights the urgent need for standardization of the methods of calculating mechanical power before this concept can become clinically useful at the bedside.
Footnotes
Drs Baedorf-Kassis and Talmor disclose a relationship with Hamilton Medical. The remaining authors have disclosed no conflicts of interest.
REFERENCES
- 1. Baedorf-Kassis EN, Bastos AB, Schaefer MS, Capers K, Hoenig B, Banner-Goodspeed V, et al. Adaptive support ventilation and lung-protective ventilation in ARDS. Respir Care 2022;67(12):1542-1550. [DOI] [PubMed] [Google Scholar]
- 2. Serpa Neto A, Deliberato RO, Johnson AEW, Bos LD, Amorim P, Pereira SM, et al. ; PROVE Network Investigators. Mechanical power of ventilation is associated with mortality in critically ill patients: an analysis of patients in two observational cohorts. Intensive Care Med 2018;44(11):1914-1922. [DOI] [PubMed] [Google Scholar]
- 3. Zhao Z, Frerichs I, He H, Long Y, Möller K, Serpa Neto A, et al. The calculation of mechanical power is not suitable for intra-patient monitoring under pressure controlled ventilation. Intensive Care Med 2019;45(5):749-750. [DOI] [PubMed] [Google Scholar]
- 4. Chiumello D, Gotti M, Guanziroli M, Formenti P, Umbrello M, Pasticci I, et al. Bedside calculation of mechanical power during volume and pressure controlled mechanical ventilation. Crit Care 2020;24(1):417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Trinkle CA, Broaddus RN, Sturgill JL, Waters CM, Morris PE. Simple, accurate calculation of mechanical power in pressure controlled ventilation (PCV). Intensive Care Med Exp 2022;10(22). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Becher T, van der Staay M, Schädler D, Frerichs I, Weiler N. Calculation of mechanical power for pressure controlled ventilation. Intensive Care Med 2019;45(9):1321-1323. [DOI] [PubMed] [Google Scholar]
- 7. Giosa L, Busana M, Pasticci I, Bonifazi M, Macrì MM, Romitti F, et al. Mechanical power at a glance: a simple surrogate for volume controlled ventilation. Intensive Care Med Exp 2019;7:61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Baedorf-Kassis E, Talmor D. Clinical application of esophageal manometry: how I do it. Crit Care 2021;25(1):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Beitler JR, Sarge T, Banner-Goodspeed VM, Gong MN, Cook D, Novack V, et al. Effect of titrating positive end-expiratory pressure (PEEP) with an esophageal pressure–guided strategy vs an empirical high PEEP-FIO2 strategy on death and days free from mechanical ventilation among patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA 2019;321(9):846-857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bellani G, Laffey JG, Pham T, Fan E, Brochard L, Esteban A, et al. ; ESICM Trials Group. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA 2016;315(8):788-800. [DOI] [PubMed] [Google Scholar]
- 11. Rocco PRM, Silva PL, Samary CS, Hayat Syed MK, Marini JJ. Elastic power but not driving power is the key promoter of ventilator-induced lung injury in experimental acute respiratory distress syndrome. Crit Care 2020;24(1):284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Schaefer MS, Loring SH, Talmor D, Baedorf-Kassis EN. Comparison of mechanical power estimations in mechanically ventilated patients with ARDS: a secondary data analysis from the EPVent study. Intensive Care Med 2021;47(1):130-132. [DOI] [PubMed] [Google Scholar]
- 13. Tonna JE, Peltan I, Brown SM, Herrick JS, Keenan HT, Grissom CK, et al. ; University of Utah Mechanical Power Study Group. Mechanical power and driving pressure as predictors of mortality among patients with ARDS. Intensive Care Med 2020;46(10):1941-1943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Santer P, Wachtendorf LJ, Suleiman A, Houle TT, Fassbender P, Costa EL, et al. Mechanical power during general anesthesia and postoperative respiratory failure: a multi-center retrospective cohort study. Anesthesiology 2022;137(1):41-54. [DOI] [PubMed] [Google Scholar]


