Abstract
COVID-19 has affected all aspects of human life so far. From the outset of the pandemic, preventing the spread of COVID-19 through the observance of health protocols, especially the use of sanitizers and disinfectants was given more attention. Despite the effectiveness of disinfection chemicals in controlling and preventing COVID-19, there are critical concerns about their adverse effects on human health. This study aims to assess the health effects of sanitizers and disinfectants on a global scale. A total of 91,056 participants from 154 countries participated in this cross-sectional study. Information on the use of sanitizers and disinfectants and health was collected using an electronic questionnaire, which was translated into 26 languages via web-based platforms. The findings of this study suggest that detergents, alcohol-based substances, and chlorinated compounds emerged as the most prevalent chemical agents compared to other sanitizers and disinfectants examined. Most frequently reported health issues include skin effects and respiratory effects. The Chi-square test showed a significant association between chlorinated compounds (sodium hypochlorite and per-chlorine) with all possible health effects under investigation (p-value <0.001). Examination of risk factors based on multivariate logistic regression analysis showed that alcohols and alcohols-based materials were associated with skin effects (OR, 1.98; 95%CI, 1.87–2.09), per-chlorine was associated with eye effects (OR, 1.83; 95%CI, 1.74–1.93), and highly likely with itching and throat irritation (OR, 2.00; 95%CI, 1.90–2.11). Furthermore, formaldehyde was associated with a higher prevalence of neurological effects (OR, 2.17; 95%CI, 1.92–2.44). Furthermore, formaldehyde was associated with a higher prevalence of neurological effects (OR, 2.17; 95%CI, 1.92–2.44). The use of sodium hypochlorite and per-chlorine also had a high chance of having respiratory effects. The findings of the current study suggest that health authorities need to implement more awareness programs about the side effects of using sanitizers and disinfectants during viral epidemics especially when they are used or overused.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11356-023-27197-6.
Keywords: COVID-19, Sanitizers and disinfectants, Side effects, Health protocols
Introduction
COVID-19 is one of the great challenges to human health. According to the report of the World Health Organization, by November 16, 2022, 548 million people were infected and more than 6 million deaths worldwide had occurred (WHO, 2022). The emergence of new and mutated strains of the virus over time and the production of less effective vaccines have exacerbated this catastrophic health challenge (Hashemi et al., 2022b; Viveiros-Rosa et al., 2022). From the beginning of the COVID-19 outbreak, simultaneously with treatment measures, health and preventive measures such as strict quarantine, social distancing, hand washing, disinfection of various surfaces, and wearing a mask among others, as health protocols to reduce and cut off the transmission chain were on the agenda of governments and health organizations (Alimohamadi et al., 2022a; Amanollahi et al., 2021; Hashemi et al., 2022b; Sharun et al., 2022). With the hypothesis of the persistence of the virus on different surfaces and its transmission through skin contact, personal and public hygiene by hand washing and disinfection of different surfaces became more important. Among the various surfaces with the most frequent contact were door handles, smartphones, remote controls, keyboards, tables and chairs, light switches, and elevator buttons, etc. (Al-Sayah, 2020; Ghafoor et al., 2021; Jin et al., 2020; Yari et al., 2020). The literature shows that SARS-CoV-2 can float in the air for 3 h, on smooth surfaces (glass, plastic, banknotes) for 4 to 7 days, on the outer layer of the surgical mask for up to 7 days, on copper surfaces, cardboard, and paper for less than 3 h and stainless steel up to 72 h (Chin et al., 2020; Dhama et al., 2021; Doremalen et al., 2020). The shelf life of the virus depends on various factors such as temperature, relative humidity, and pressure (Dindarloo et al., 2020; Gharehchahi et al., 2023; Kampf, 2020). To reduce the spread of the virus and disrupt the transmission chain, disinfection using sanitizers and disinfectants for living and non-living surfaces as an efficient method was recommended by the World Health Organization (WHO) and the US Environmental Protection Agency in accordance with the issued instructions (Chen et al., 2021; Dindarloo et al., 2020). Sanitizers and disinfectants used include alcohol-based materials, oxidizing agents, detergents, chlorine-releasing agents (sodium hypochlorite, per-chlorine), phenol-based disinfectants, iodine-releasing agents, aldehydes, hydrogen peroxide, and quaternary ammonium compounds, etc. (Al-Sayah, 2020; McDonnell and Russell, 1999; Rutala and Weber, 2019). Using sanitizers and disinfectants may have adverse effects on human health, mainly because of the harmful and corrosive compounds in the composition of most sanitizers and disinfectants, such as chlorine-releasing agents, quaternary ammonium cations, or oxidizing agents (Bonin et al., 2020; Dumas et al., 2019; Emmanuel et al., 2004; Nabi et al., 2020; Rafiee et al., 2022). The severity of these side effects may vary depending on the type of chemicals, their target objects (living or non-living surfaces), the frequency and volume of the chemicals, and the risk status of the exposed individual (Prajapati et al., 2022). Lack of knowledge and insufficient experience in sanitizer and disinfectant use increases the rate of side effects due to the use of these chemicals (Gharpure et al., 2020; Rai et al., 2020). Potential acute side effects of using sanitizers and disinfectants include skin effects, itching, sore throat, eyes, and nose irritation, and ailments of the respiratory system (cough, sneezing, shortness of breath). Neurological effects such as headache, dizziness, and vomiting have been also reported (ECDC, 2020; Goh et al., 2021; Lachenmeier, 2008). Regardless of the sanitizer and disinfectant safety information and application instructions prolonged use of these products may cause chronic side effects including disorders of the central nervous system (CNS), reproductive disorders, cancer, pulmonary obstruction, etc. (Choi et al., 2020). Although several studies have been conducted regionally in a variety of countries on some of the adverse health effects due to disinfectant use (Dawood et al., 2021; Dhama et al., 2021; Dindarloo et al., 2020; Ghafoor et al., 2021; Rosenman et al., 2021; Shah et al., 2021), the present study is a comprehensive survey aimed to estimate the health effects associated with the use of sanitizers and disinfectants among the general population on a global scale.
Methods
Design, participants, and sampling procedure
This study aims to assess the health effects of sanitizers and disinfectants on a global scale. There were no exclusion/inclusion criteria for participation in the study, and all individuals regardless of race, gender, occupation, and income level were included. The research project was approved by the ethics committee of Shiraz University of Medical Sciences (IR.SUMS.REC.1400.023). This study follows the principles of the Declaration of Helsinki. Survey design (non-interventional) is not considered a clinical trial under Directive 2001/20/EC and Regulation (Europe) No 536/2014. All participants provided online informed consent before the study.
Measurement tools
Questionnaire
The questionnaire was translated into 26 different languages by native language speakers. The questionnaire included three parts (including 26 items). The first part (7 questions) was referring to demographic information including age, gender, educational and occupational status, country, place of residence, and income level. The second part (6 questions) included the type, monthly usage volume, and the number of daily use of sanitizers and disinfectants for living and non-living surfaces. The chemicals which have been investigated included detergents (soap and toilet liquid, dishwashing liquid), alcohol or alcohol-based materials, hospital-grade sanitizers (savlon; antiseptic liquid), other commercial sanitizers (chlorhexidine gluconate, bronopol, triclosan), hospital disinfectants (quaternary ammonium, tetra-acetyl ethylenediamine), chlorine-based compounds (sodium hypochlorite, per-chlorine), hydrogen peroxide, and formaldehyde. The third part (13 questions) included health effects. Skin effects (itching and skin irritation, dryness, scaling, and urticaria), ocular (itching and eye irritation, and redness), irritation and itching of the throat, respiratory problems (itching and nasal irritation, runny nose, cough and sneezing, and shortness of breath), and neurological effects (headache, dizziness, and vomiting) were questioned. Questionnaire-related questions and options were reviewed by several specialists, including a dermatologist, otolaryngologist, ophthalmologist, pulmonologist, and chemist, as well as a biostatistics specialist.
Reliability and validity
The reliability of the questionnaire showed good internal consistency (Cronbach’s alpha = 0.90). The validity of the questionnaire for only seven living languages (Arabic, English, French, German, Persian, Russian, and Spanish) which are considered official or secondary languages of several countries, was reviewed by 5 to 7 experts in each of the 7 languages with research backgrounds related and faculty members. These experts assessed the validity in light of five components of necessity, relevance, transparency, simplicity, and ambiguity related to each question.
Data collection procedure
The questionnaire was designed using Google Form®. In some countries (e.g., China), lack of access to Google or due to poor bandwidth, other internal platforms (e.g., wenjuanxing) and sites (e.g.; https://www.wjx.cn/) were used to create online links to the questionnaire. The questionnaire was distributed via email or social networks such as Telegram, WhatsApp, Instagram, Twitter, LinkedIn, and WeChat. The questionnaire was available online for 9 months from August 1, 2021 to April 30, 2022 to achieve maximum participation.
Statistical analysis
The data were analyzed using IBM SPSS for Windows, version 28.0 (IBM Inc., Armonk, NY, USA). The Chi-square test was used to analyze descriptive statistics (n, %), and to evaluate the significance of the association between variables. To assess risk factors for health outcomes in participants, a multivariable logistic regression analysis was performed, and the relationship between risk factors and adverse effects of using sanitizers and disinfectants are presented as odds ratios (ORs) and 95%CIs, after adjustment for confounders, including age, gender, educational level, occupational status, place of residence (rural and urban areas), and income level. A p-value of <0.001 was considered statistically significant.
Result
Study design and participants
Demographic characteristics are shown in Table 1. A total of 91,056 participants [58,845 (64.60%) females and 32,211 (35.40%) males]. Respondents were well represented by ages 21 to 30 years (37,577, 41.30%), urban areas (76,122, 83.60%), bachelor’s degree (38,924, 42.70%), and median income (48,776, 53.60%). In this study, the income level was considered relative to the average income of each country. Therefore, the majority of participants had an average income in their country. Out of 193 United Nations (UN) members (and 2 countries that are non-member observer states: the Holy See and the State of Palestine), 154 countries participated in this study. The global participation rate was reported to be 79%. 41 countries (21%) from different continents did not participate in the study. According to Table 1, the number of participating countries from each continent includes Africa (48), America (19), Asia (44), Europe (39), and Oceania (4) countries correctly completed the questionnaire.
Table 1.
Demographic characteristics of the study (N = 91,056)
| Characteristics | N | Male | Female | ||
| Age | ≤20 | 9861(10.8) | 3502(3.8) | 6359(7.0) | |
| 21 to 30 | 37,577(41.3) | 12,637(13.9) | 24,940(27.4) | ||
| 31 to 40 | 22,250(24.4) | 8093(8.9) | 14,157(15.5) | ||
| 41 to 50 | 13,338(14.6) | 4744(5.2) | 8594(9.4) | ||
| 51 to 60 | 5746(6.3) | 2150(2.4) | 3596(3.9) | ||
| 60 and over | 2284(2.5) | 1085(1.2) | 1199(1.3) | ||
| Place of residence | Urban | 76,122(83.6) | 25,987(28.5) | 50,135(55.1) | |
| Rural | 14,934(16.4) | 6224(6.8) | 8710(9.6) | ||
| Level of education | School education | 14,784(16.2) | 5662(6.2) | 9122(10.0) | |
| Associate degree | 12,546(13.8) | 3673(4.0) | 8873(9.7) | ||
| Bachelor’s degree | 38,924(42.7) | 13,457(14.8) | 25,467(28.0) | ||
| Masters | 16,798(18.4) | 6348(7.0) | 10,450(11.5) | ||
| Ph.D. and postdoctoral | 8004(8.8) | 3071(3.4) | 4933(5.4) | ||
| Occupational status | Unemployed / housewife / student | 12,571(13.8) | 2443(2.7) | 10,128(11.1) | |
| University Student | 28,104(30.9) | 9489(10.4) | 18,615(20.4) | ||
| Government employee | 26,249(28.8) | 10,038(11.0) | 16,211(17.8) | ||
| Private office employee | 16,619(18.3) | 645(7.0) | 9974(11.0) | ||
| Freelance (self-employed) | 7513(8.3) | 3596(3.9) | 3917(4.3) | ||
| Income | Low | 8877(9.7) | 3004(3.3) | 5873(6.4) | |
| Lower-middle | 11,339(12.5) | 4325(4.7) | 7014(7.7) | ||
| Middle | 48,776(53.6) | 17,165(18.9) | 31,611(34.7) | ||
| Upper-middle | 18,308(20.1) | 6276(6.9) | 12,032(13.2) | ||
| High-income | 3756(4.1) | 1441(1.6) | 2315(2.5) | ||
| Number of participating countries by continent: N (RR*) | Africa | America | Asia | Europe | Oceania |
| 48 (24.6%) | 19 (9.7%) | 44 (22.5%) | 39 (20%) | 4(2%) | |
| No participation: N | 6 | 16 | 4 | 5 | 10 |
*Response Rate
Type and volume of sanitizers and disinfectants used
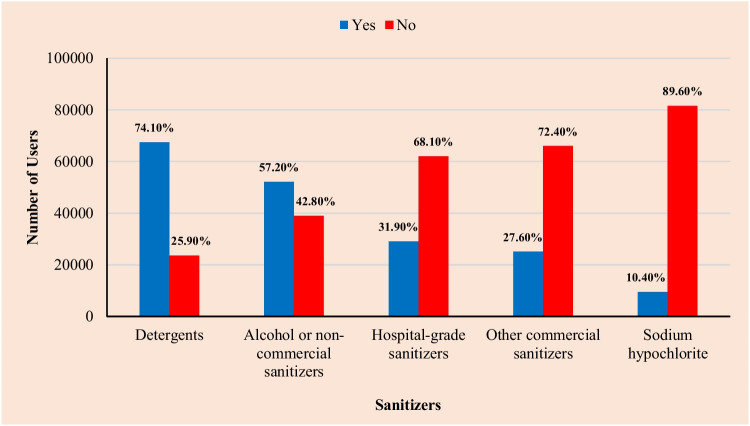
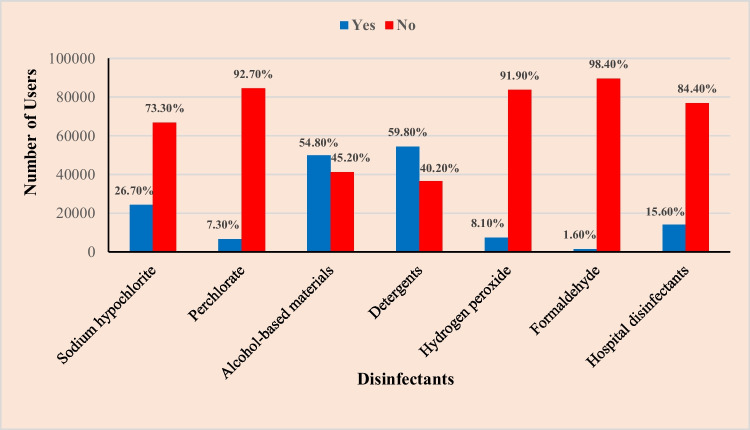
In the second part of the questionnaire, questions were asked about the type, volume, and number of times of daily use of 5 types of chemical compounds as sanitizers (Figure 1) and 7 types of substances as disinfectants (Figure 2). The status of the use of sanitizers and disinfectants is shown in Table 2 and Figures 1, 2, and 3. The usage status of the sanitizers for handwashing or other living surfaces is shown in Figure 1. Compared to other sanitizers, the highest use was detergents (soap and toilet liquid, dishwashing liquid) (67,445 users), and alcohol or non-commercial sanitizers (52,083 users). In contrast, chlorine compounds such as sodium hypochlorite (9490 users) were used less often as sanitizers. Additionally, the status of seven groups of disinfectants, which are used for the disinfection of various high-touch surfaces such as door handles, tables, chairs, remotes, keys, elevator buttons, etc., was explored (Figure 2). In this group, in addition to detergents (54,445 users) and alcohol-based products (49,879 users), which were most used compared to other disinfectants, the use of sodium hypochlorite was reported as a high-consumptive disinfectant (24,296 users). In contrast, formaldehyde (1441 users) and per-chlorine (6605 users) had the lowest usage as a disinfectant.
Fig. 1.
Usage status of five groups of sanitizers
Fig. 2.
Usage status of seven groups of disinfectants
Table 2.
Usage status of sanitizers and disinfectants
| Frequency of daily use | Monthly usage volume (CC**) | |||||||||
| Once a day | 1–3/d | 4–6/d | > 6/d | None | Low (≤100) | Average (101 to 300) |
High (301 to 500) |
Too much (≥500) | None | |
|
Sanitizers: N* (%) |
11,069 (12.2) |
29,778 (32.7) |
27,407 (30.1) |
21,608 (23.7) |
1140 (1.3) |
22,849 (25.1) |
45,091 (49.5) |
13,292 (14.6) |
8572 (9.4) |
1198 (1.3) |
| Monthly usage volume (L***) | ||||||||||
| Once a day | 1–3/d | 4–6/d | > 6/d | None |
Low (≤0.5) |
Average (0.5 to 1) |
High (1.1 to 2) |
Too much (>2) | None | |
| Disinfectants: N (%) |
35,959 (39.5) |
34,436 (37.8) |
11,158 (12.3) |
5159 (5.7) |
3990 (4.4) |
27,727 (30.5) |
44,686 (49.1) |
10,783 (11.8) |
4978 (5.5) |
2816 (3.1) |
*The users of sanitizers and disinfectants. **It is expressed in CC due to its use for living surfaces. ***It is expressed in liters due to its use for non-living surfaces
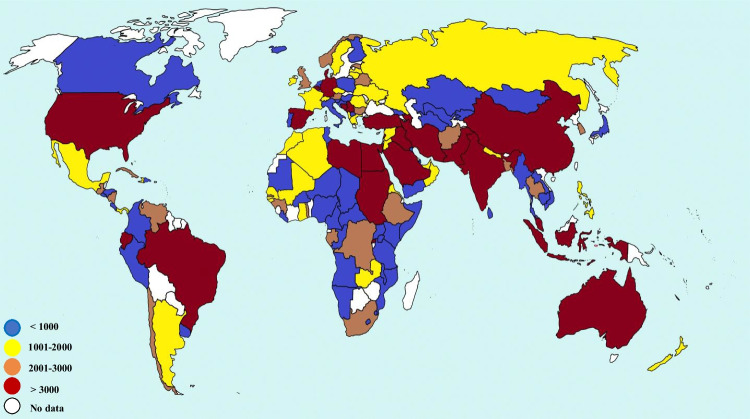
Fig. 3.
Distribution of the use of sanitizers and disinfectants in different countries
In terms of the frequency of daily use of sanitizers and disinfectants, the results showed that most participants tended to use sanitizers and disinfectants 1 to 3 times a day (29,778 users) and once a day (35,959 users), respectively. The volume of chemicals used was also one of the important factors in creating the scenarios of possible adverse effects and we found that most of the participants stated using the sanitizers and disinfectants at a volume of approximately 101–300 mL, and 0.5–1 L per month, respectively (Table 2).
The continental distribution of the inclination of users (individuals) to use sanitizers and disinfectants is shown in Figure 3. Four groups of countries were determined according to the sanitizers and disinfectant usage rate: countries with low usage (blue <1000), medium usage (yellow = 1001–2000), high usage (brown = 2001–3000), and countries that tend to consume too many sanitizers and disinfectants (red >3000). The number of countries that were less inclined to use sanitizers and disinfectants was in Africa, while the number of countries with the highest level of usage was in Asia. Similarly, the continental distribution shows that most countries with moderate usage of sanitizers and disinfectants were in continental Europe.
Adverse health outcomes of sanitizers and disinfectants
The distribution of the frequency of adverse events showed that the most common complaints reported by the participants were related to skin and respiratory system effects (Figure 4). The highest and lowest frequencies were related to skin dryness (65,680 cases) and neurological effects (headache, dizziness, and vomiting) (13,063 cases), respectively. Table 3 shows the possible adverse health outcomes as a result of the use of sanitizers and disinfectants based on the reports of the participants in this study. There was a significant relationship between the use of chlorine compounds such as sodium hypochlorite and per-chlorine with all the adverse effects (p < 0.001) (Table 3).
Fig. 4.
The frequency distribution of 12 health outcomes studied
Table 3.
Frequency table and the relationship between sanitizers/disinfectants and health outcomes (Chi-square test)
| Type of chemical | Itching and skin irritation | Skin dryness | Hand scaling | Skin urticaria (Hives) | |||||
| Yes | No | Yes | No | Yes | No | Yes | No | ||
| N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | ||
| Detergents (Soap and toilet liquid, dishwashing liquid) | Yes | 29,952(32.9) | 30,996(34.0) | 45,259(49.7) | 15,688(17.2) | 33,286(36.6) | 27,662(30.4) | 7037(7.7) | 48,320(53.1) |
| P-value | <0.001 | <0.001 | <0.001 | <0.001 | |||||
| Alcohol or alcohol-based materials | Yes | 24,786(27.2) | 27,300(30.0) | 39,573(43.5) | 12,513(13.7) | 27,979(30.7) | 24,107(26.5) | 10,614(11.7) | 41,472(45.5) |
| P-value | <0.001 | <0.001 | <0.025 | <0.001 | |||||
| Sodium hypochlorite (bleach) | Yes | 19,450(21.4) | 7443(8.2) | 33,453(36.7) | 3440(3.8) | 29,954(32.9) | 6940(7.6) | 4364(4.8) | 12,529(13.8) |
| P-value | <0.001 | <0.001 | <0.001 | <0.001 | |||||
| Hospital-grade sanitizers (savlon) | Yes | 14,322(15.7) | 14,698(16.1) | 21,417(23.5) | 7603(8.3) | 15,369(16.9) | 13,651(15.0) | 6134(6.7) | 22,886(25.1) |
| P-value | <0.001 | <0.001 | <0.001 | 0.022 | |||||
| Other commercial sanitizers | Yes | 11,719(12.9) | 13,372(14.7) | 17,880(19.6) | 7211(7.9) | 13,082(14.4) | 12,009(13.2) | 5018(5.5) | 20,073(22.0) |
| P-value | 0.592 | <0.001 | 0.847 | <0.001 | |||||
| Hospital disinfectants | Yes | 6501(7.1) | 7685(8.4) | 10,447(11.5) | 3739(4.1) | 6943(7.6) | 7243(8.0) | 3432(3.8) | 10,754(11.8) |
| P-value | 0.057 | <0.001 | <0.001 | <0.001 | |||||
| Per-chlorine | Yes | 4097(4.5) | 2511(2.8) | 5234(5.7) | 1374(1.5) | 4581(5.0) | 2027(2.2) | 1918(2.1) | 4690(5.2) |
| P-value | <0.001 | <0.001 | <0.001 | <0.001 | |||||
| Hydrogen peroxide | Yes | 3788(4.2) | 3592(3.9) | 5387(5.9) | 1993(2.2) | 3925(4.3) | 3455(3.8) | 1872(2.1) | 5508(6.0) |
| P-value | <0.001 | 0.088 | 0.049 | <0.001 | |||||
| Formaldehyde | Yes | 768(0.8) | 676(0.7) | 1000(1.1) | 444(0.5) | 923(1.0) | 521(0.6) | 436(0.5) | 1008(1.1) |
| P-value | <0.001 | 0.015 | <0.001 | <0.001 | |||||
| Type of chemical | Itching and eye irritation | Eye redness | Itching and throat irritation | Itching and nose irritation | |||||
| Yes | No | Yes | No | Yes | No | Yes | No | ||
| N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | ||
| Detergents (soap and toilet liquid, dishwashing liquid) | Yes | 6294(6.9) | 44,654(49.0) | 11,255(12.3) | 49,580(54.5) | 964(1) | 45,754(50.2) | 12,976(14.3) | 37,971(41.7) |
| P-value | 0.039 | <0.001 | <0.001 | 0.002 | |||||
| Alcohol or non-commercial alcohol-based sanitizers | Yes | 14,108(15.5) | 10,309(11.3) | 9289(10.2) | 8077(8.9) | 12,591(13.8) | 39,495(43.4) | 19,692(21.6) | 32,394(35.6) |
| P-value | 0.034 | <0.001 | <0.001 | 0.068 | |||||
| Sodium hypochlorite (bleach) | Yes | 15,407(16.9) | 11,487(12.6) | 11,302(12.4) | 12,592(13.8) | 5502(6.0) | 11,391(12.5) | 17,551(19.3) | 9342(10.3) |
| P-value | <0.001 | <0.001 | <0.001 | <0.001 | |||||
| Hospital-grade sanitizers | Yes | 7180 (7.9) | 21,840(24.0) | 5450(6.0) | 23,570(25.9) | 6671(7.3) | 22,349(24.5) | 10,359(11.4) | 18,661(20.5) |
| P-value | <0.001 | 0.126 | 0.321 | 0.210 | |||||
| Other commercial sanitizers | Yes | 6440(7.1) | 18,651(20.5) | 4482(4.9) | 20,609(22.6) | 6035(6.6) | 19,056(20.9) | 8911(9.8) | 16,180(17.8) |
| P-value | <0.001 | <0.001 | <0.001 | 0.055 | |||||
| Hospital disinfectants | Yes | 3310(3.6) | 10,876(11.9) | 2658(2.9) | 11,528(12.7) | 2978(3.3) | 11,208(12.3) | 4530(5.0) | 9656(10.6) |
| P-value | <0.001 | 0.274 | <0.001 | <0.001 | |||||
| Per-chlorine | Yes | 2614(2.9) | 3994(4.4) | 1922(2.1) | 4686(5.1) | 2624(2.9) | 3984(4.4) | 3484(3.8) | 3124(3.4) |
| P-value | <0.001 | <0.001 | <0.001 | <0.001 | |||||
| Hydrogen peroxide | Yes | 2084(2.3) | 5296(5.8) | 1750(1.9) | 5630(6.2) | 2049(2.3) | 5331(5.9) | 2579(2.8) | 4801(5.3) |
| P-value | <0.001 | <0.001 | <0.001 | 0.332 | |||||
| Formaldehyde | Yes | 525(0.6) | 919(1.0) | 410(0.5) | 1034(1.1) | 482(0.5) | 962(1.1) | 715(0.8) | 729(0.8) |
| P-value | <0.001 | <0.001 | <0.001 | <0.001 | |||||
| Type of chemical | Runny nose | Cough and Sneeze | Shortness of breath | Headaches, dizziness, and vomiting | |||||
| Yes | No | Yes | No | Yes | No | Yes | No | ||
| N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | ||
| Detergents (Soap and toilet liquid, dishwashing liquid) | Yes | 3296(3.6) | 45,653(50.1) | 5033(5.5) | 36,868(40.5) | 6248(6.9) | 49,700(54.6) | 4213(4.6) | 52,335(57.5) |
| P-value | 0.002 | 0.065 | 0.118 | ||||||
| Alcohol or alcohol-based materials | Yes | 12,601(13.8) | 39,485(43.4) | 20,148(22.1) | 13,773(15.1) | 9206(10.1) | 42,880(47.1) | 7114(7.8) | 44,972(49.4) |
| P-value | 0.068 | <0.001 | <0.001 | ||||||
| Sodium hypochlorite (bleach) | Yes | 5753(6.3) | 11,141(12.2) | 7833(8.6) | 9061(10.0) | 11,738(12.9) | 13,156(14.4) | 2929(3.2) | 13,965(15.3) |
| P-value | <0.001 | <0.001 | <0.001 | ||||||
| Hospital-grade sanitizers | Yes | 6473(7.1) | 22,547(24.8) | 10,172(11.2) | 18,848(20.7) | 5091(5.6) | 23,929(26.3) | 3682(4.0) | 25,338(27.8) |
| P-value | 0.210 | <0.001 | <0.001 | ||||||
| Other commercial sanitizers | Yes | 5845(6.4) | 19,246(21.1) | 8857(9.7) | 16,234(17.8) | 4223(4.6) | 20,868(22.9) | 3368(3.7) | 21,723(23.9) |
| P-value | 0.055 | <0.001 | <0.001 | ||||||
| Hospital disinfectants | Yes | 2784(3.1) | 11,402(12.5) | 4460(4.9) | 9726(10.7) | 2164(2.4) | 12,022(13.2) | 2005(2.2) | 12,181(13.4) |
| P-value | <0.001 | <0.001 | <0.001 | ||||||
| Per-chlorine | Yes | 2594(2.8) | 4014(4.4) | 3396(3.7) | 3212(3.5) | 1881(2.1) | 4727(5.2) | 1425(1.6) | 5183(5.7) |
| P-value | <0.001 | <0.001 | <0.001 | ||||||
| Hydrogen peroxide | Yes | 7380(8.1) | 5582(6.1) | 2677(2.9) | 4703(5.2) | 1593(1.7) | 5787(6.4) | 1254(1.4) | 6126(6.7) |
| P-value | 0.332 | <0.001 | <0.001 | ||||||
| Formaldehyde | Yes | 537(0.6) | 907(1.0) | 708(0.8) | 736(0.8) | 428(0.5) | 1016(1.1) | 419(0.5) | 1025(1.1) |
| P-value | <0.001 | <0.001 | <0.001 | ||||||
Skin effects
The use of detergents and alcohol or alcohol-based products resulted in a greater adverse effect on the skin than other chemicals (Table 3). Among the skin effects, the most commonly reported adverse effect was skin dryness. 45,259 and 39,573 of the participants complained of dry skin due to the use of detergents and alcohol or alcohol-based materials, respectively. There was a significant relationship between itching and skin irritation with all chemicals (except other commercial sanitizers and hospital disinfectants) (p < 0.001). Unlike other chemicals, there was no significant relationship between skin scaly with alcohols, commercial sanitizers, and hydrogen peroxide (p > 0.05).
Ocular effects
The contribution of sodium hypochlorite in causing ocular effects was greater than other chemicals. Participants reported itching and ocular irritation (15,407 cases) and ocular redness (11,302 cases) after using sodium hypochlorite. The data show a significant relationship between itching and ocular irritation with all sanitizers and disinfectants (except detergents and alcohol or alcohol-based materials) (p < 0.001) (Table 3).
Throat effects
Participants reported itching and irritation of the throat after using alcohol or alcohol-based products (12,591 cases), hospital-grade sanitizers such as savlon (6671 cases), and other commercial sanitizers (6035 cases). Itching and irritation of the throat as one of the possible side effects of sanitizers and disinfectants was significantly associated with some chemicals such as chlorine compounds (sodium hypochlorite and per-chlorine), hospital disinfectants, hydrogen peroxide, formaldehyde (p < 0.001) (Table 3).
Respiratory system effects
Respiratory effects including itching and nose irritation (19,692 cases), runny nose (12,601 cases), and cough and sneezing (20,148 cases) were reported after using alcohol or alcohol-based products. There was a significant relationship between shortness of breath with all chemicals except detergents (all p < 0.001). In contrast, except for chlorine compounds, there was no significant relationship between cough, sneezing, and runny nose with the majority of sanitizers and disinfectants (p > 0.05) (Table 3).
Neurological effects
The present findings showed that less than eight percent of the participants had self-reported neurological effects including headache, dizziness, and vomiting after using sanitizers and disinfectants. In total, 7114 and 419 of participants complained of headache, dizziness, and vomiting after using alcohol (the most) and formaldehyde (the least), respectively. The results indicated that a statistically significant relationship was found between possible neurological problems due to the use of analyzed sanitizers and disinfectants (except detergents) (all p < 0.001) (Table 3).
Multivariable logistic regression analysis
After controlling for confounders (demographic characteristics), a multivariable logistic regression analysis was performed to determine the risk factors associated with adverse health outcomes (Table 4). The use of some sanitizers and disinfectants was associated with skin adverse effects (e.g., Itching and skin irritation after using alcohol or alcohol-based materials: OR, 1.86; 95%CI, p > 0.05; or as a result of using sodium hypochlorite: OR, 1.43; 95%CI, p < 0.001). In contrast, the use of some other sanitizers and disinfectants was associated with a lower chance of itching and skin irritation (hospital disinfectants: OR, 0.91; 95%CI, p < 0.001). The use of Per-chlorine (OR, 1.47; 95%CI, p < 0.001), alcohol-based materials (OR, 1.98; 95%CI, p < 0.001), formaldehyde (OR, 1.40; 95%CI, p < 0.001) were associated with higher odds of skin dryness, scaling of the skin, skin urticaria respectively.
Table 4.
Risk factors for health effects by Multivariable Logistic Regression Analysis
| Type of chemical | Itching and skin irritation | Skin dryness | Skin scaling | Skin urticaria (Hives) | ||||||||
| Adjusted OR | CI (95%) | P | Adjusted OR | CI (95%) | P | Adjusted OR | CI (95%) | P | Adjusted OR | CI (95%) | P | |
| Detergents (Soap and toilet liquid, dishwashing liquid) | 1.15 | 1.09–1.21 | <0.001 | 1.06 | 1.02–1.10 | <0.001 | 1.15 | 1.11–1.19 | <0.001 | 0.94 | 0.90–0.97 | <0.001 |
| Alcohol or alcohol-based materials | 1.86 | 1.77–1.96 | 0.020 | 1.30 | 1.26–1.34 | <0.001 | 1.98 | 1.87–2.09 | <0.001 | 0.86 | 0.83–0.89 | <0.001 |
| Sodium hypochlorite (bleach) | 1.43 | 1.39–1.48 | <0.001 | 1.40 | 1.35–1.46 | <0.001 | 1.30 | 1.24–1.37 | <0.001 | 0.90 | 0.87–0.93 | <0.001 |
| Hospital-grade sanitizers | 1.08 | 1.05–1.12 | <0.001 | 0.82 | 0.79–0.93 | <0.001 | 1.01 | 0.98–1.04 | 0.394 | 0.86 | 0.83–0.89 | <0.001 |
| Other commercial sanitizers | 0.90 | 0.87–0.93 | <0.001 | 0.86 | 0.83–0.89 | <0.001 | 0.95 | 0.92–0.98 | 0.005 | 0.82 | 0.79–0.85 | <0.001 |
| Hospital disinfectants | 0.91 | 0.88–0.95 | <0.001 | 1.10 | 1.06–1.15 | <0.001 | 0.84 | 0.81–0.87 | <0.001 | 1.26 | 1.21–1.32 | <0.001 |
| Per-chlorine | 0.96 | 0.94–0.99 | <0.001 | 1.47 | 1.38–1.56 | <0.001 | 1.37 | 1.29–1.45 | <0.001 | 0.95 | 0.90–1.01 | 0.125 |
| Hydrogen peroxide | 1.15 | 1.09–1.21 | <0.001 | 0.95 | 0.90–1.01 | 0.125 | 0.96 | 0.91–1.01 | 0.136 | 1.37 | 1.29–1.45 | <0.001 |
| Formaldehyde | 1.20 | 1.07–1.34 | <0.001 | 0.85 | 0.76–0.96 | 0.011 | 1.46 | 1.31–1.64 | <0.001 | 1.40 | 1.24–1.57 | <0.001 |
| Type of chemical | Itching and Eye Irritation | Eye Redness | Itching and Throat Irritation | Itching and Nose Irritation | ||||||||
| Adjusted OR | CI (95%) | P | Adjusted OR | CI (95%) | P | Adjusted OR | CI (95%) | P | Adjusted OR | CI (95%) | P | |
| Detergents (Soap and toilet liquid, dishwashing liquid) | 0.95 | 0.92–0.98 | <0.001 | 0.85 | 0.82–0.88 | <0.001 | 0.69 | 0.62–0.76 | 0.063 | 1.21 | 1.17–1.24 | <0.001 |
| Alcohol or alcohol-based materials | 1.11 | 1.07–1.15 | 0.002 | 1.05 | 1.01–1.08 | <0.001 | 0.97 | 0.93–1.00 | 0.053 | 1.07 | 1.04–1.11 | <0.001 |
| Sodium hypochlorite (bleach) | 1.33 | 1.27–1.40 | <0.001 | 1.65 | 1.58–1.71 | <0.001 | 1.66 | 1.58–1.74 | <0.001 | 1.48 | 1.41–1.55 | <0.001 |
| Hospital-grade sanitizers | 0.83 | 0.80–0.86 | <0.001 | 0.90 | 0.86–0.93 | <0.001 | 0.84 | 0.81–0.87 | <0.001 | 0.87 | 0.84–0.89 | <0.001 |
| Other commercial sanitizers | 0.89 | 0.86–0.92 | <0.001 | 0.81 | 0.77–0.84 | <0.001 | 0.89 | 0.86–0.93 | <0.001 | 0.85 | 0.82–0.88 | <0.001 |
| Hospital disinfectants | 0.90 | 0.86–0.94 | <0.001 | - | - | - | 0.83 | 0.79–0.87 | <0.001 | 0.82 | 0.79–0.86 | <0.001 |
| Per-chlorine | 1.83 | 1.74–1.93 | <0.001 | 1.77 | 1.68–1.88 | <0.001 | 2.00 | 1.90–2.11 | <0.001 | 1.87 | 1.78–1.97 | <0.001 |
| Hydrogen peroxide | 1.15 | 1.09–1.22 | <0.001 | 1.49 | 1.40–1.58 | <0.001 | 1.19 | 1.13–1.26 | <0.001 | 0.92 | 0.87–0.97 | 0.003 |
| Formaldehyde | 1.40 | 1.26–1.57 | <0.001 | 1.34 | 1.19–1.52 | <0.001 | 1.29 | 1.15–1.45 | <0.001 | 1.56 | 1.40–1.73 | <0.001 |
| Type of chemical | Runny nose | Cough and Sneeze | Shortness of breath | Headaches, Dizziness, and Vomiting | ||||||||
| Adjusted OR | CI (95%) | P | Adjusted OR | CI (95%) | P | Adjusted OR | CI (95%) | P | Adjusted OR | CI (95%) | P | |
| Detergents (Soap and toilet liquid, dishwashing liquid) | 0.93 | 0.90–0.97 | <0.001 | 0.67 | 0.61–0.78 | <0.001 | 0.94 | 0.90–0.98 | 0.004 | 0.95 | 0.92–0.99 | 0.019 |
| Alcohol or alcohol-based materials | 0.76 | 0.73–0.79 | <0.001 | 1.05 | 1.02–1.08 | 0.005 | 0.91 | 0.87–0.94 | <0.001 | 1.06 | 1.02–1.10 | 0.002 |
| Sodium hypochlorite (bleach) | 1.76 | 1.6–1.8 | <0.001 | 1.74 | 1.65–1.83 | <0.001 | 1.78 | 1.68–1.88 | <0.001 | 1.32 | 1.27–1.38 | <0.001 |
| Hospital-grade sanitizers | 0.76 | 0.73–0.79 | <0.001 | 0.83 | 0.80–0.85 | <0.001 | 0.77 | 0.74–0.80 | <0.001 | 0.90 | 0.86–0.93 | <0.001 |
| Other commercial sanitizers | 0.82 | 0.79–0.85 | <0.001 | 0.83 | 0.81–0.86 | <0.001 | 0.84 | 0.81–0.88 | <0.001 | 0.81 | 0.78–0.84 | <0.001 |
| Hospital disinfectants | 0.76 | 0.73–0.80 | <0.001 | 0.81 | 0.77–0.84 | <0.001 | 1.10 | 1.04–1.15 | <0.001 | 0.80 | 0.76–0.84 | <0.001 |
| Per-chlorine | 1.91 | 1.81–2.02 | <0.001 | 1.47 | 1.42–1.52 | <0.001 | 1.67 | 1.56–1.77 | <0.001 | 1.72 | 1.62–1.81 | <0.001 |
| Hydrogen peroxide | 1.06 | 1.00–1.13 | 0.031 | 0.97 | 0.92–1.02 | <0.001 | 1.30 | 1.22–1.39 | <0.001 | 1.36 | 1.28–1.44 | <0.001 |
| Formaldehyde | 1.59 | 1.42–1.78 | <0.001 | 1.56 | 1.40–1.73 | <0.001 | 1.15 | 1.09–1.22 | <0.001 | 2.17 | 1.92–2.44 | <0.001 |
Adjusted for age, sex, educational level, occupational status, place of residence (rural and city), and income level
Itching and ocular irritation were reported after using per-chlorine: OR, 1.83; 95%CI, p < 0.001; and sodium hypochlorite: OR, 1.33; 95%CI, p < 0.001. Similarly, ocular redness was associated with the use of per-chlorine (OR, 1.77; 95%CI, p < 0.001), and hydrogen peroxide (OR, 1.49; 95%CI, p < 0.001).
The results showed that one of the important risk factors for throat-related effects is chlorine-based compounds. Per-chlorine resulted in double the risk for throat-related effects (OR, 2.00; 95%CI, p < 0.001), and sodium hypochlorite use is also a serious risk factor for itching and throat irritation (OR, 1.66; 95%CI, p < 0.001). Furthermore, the use of sodium hypochlorite (OR, 1.74; 95%CI, p < 0.001), and formaldehyde (OR, 1.56; 95%CI, p < 0.001) were accompanied by coughing and sneezing. Similarly, shortness of breath was associated with the use of sodium hypochlorite (OR, 1.78; 95%CI, p < 0.001), and per-chlorine (OR, 1.67; 95%CI, p < 0.001). There was a strong association between the use of formaldehyde and the occurrence of neurological effects (OR, 2.17; 95%CI, p < 0.001).
Discussion
Regarding the use of sanitizers and disinfectants in different continents, it was observed that in African countries, due to low-income levels, and lack of accessibility the tendency to use disinfectants was lower than in other continents. In contrast, in some less-resourced countries, such as Iran, and more-resourced countries, such as China, the USA, the UK, Germany, and Australia, etc., there was a greater tendency to use disinfectants. Adequate income levels, adequate education, and information, easy access to the types of sanitizers and disinfectants, and strict controlling measures by the governments have been effective in increasing the use of these chemicals (Becher et al., 2021; Bu et al., 2020; Tran et al., 2020; Unruh et al., 2022; Xu et al., 2020). Although our claim regarding some countries such as Venezuela, Iraq, Afghanistan, etc. was not correct. Contrary to the economic crisis prevailing in these countries, the use of sanitizers and disinfectants was high.
In addition to this more attention and the fear of contracting the disease, sometimes leads to the excessive usage of sanitizers and disinfectants, which leads to the occurrence of adverse effects due to the toxic nature of these chemicals on the population; finally, the body’s resistance to other infectious agents may decrease (Tachikawa, 2020; Vogel, 2011). On the other hand, the denial of the existential nature of the COVID-19 disease by people from different countries (Afolabi and Ilesanmi, 2021; Buguzi, 2021; Cabral et al., 2021; Thagard, 2021) can be one of the main reasons for not tending to use sanitizers and disinfectants as part of health protocols. We found that the disinfectants with the highest rate of causing different adverse health effects are chlorine compounds (sodium hypochlorite and per-chlorine). One of the reasons for this finding could be the widespread use of these compounds as bleaches, cleansers, and vegetable washes, for washing different surfaces, water disinfection as well as easy access and affordability. In addition to the inherent effects of using chemicals as sanitizers and disinfectants, there are other reasons such as misuse (mixing several chemicals without following the instructions), excessive use, and counterfeit and unauthorized products that can cause side effects (Alhouri et al., 2020; Cook and Brooke, 2021). However, some disinfectants (e.g., detergents) may not have serious adverse effects on human health, but prolonged exposure and overuse of any chemical increase their harmful potential (Baldeo et al., 2022). Similar studies have shown that most disinfectants, such as alcohols and proxygene compounds, can be considered potential irritants or skin allergens (Goh et al., 2021; Lachenmeier, 2008; Murphy and Friedman, 2019). The US centers for disease control and prevention (CDC) reported an increase in calls to the center because of overuse and frequent exposure to cleaning chemicals during the Covid-19 pandemic (CDC, 2020; Rosenman et al., 2021).
Various reports have claimed that long-term use of surfactants causes dryness and roughness of the skin (Goh et al., 2021; Paudel et al., 2022; Shibuya et al., 2022). Similarly, alcohol-based substances despite their low permeability to the skin had the most skin effects as a result of prolonged contact and regular and continuous use. Similar studies have reported increased exposure and frequency of alcohol use as a cause of skin irritation or dermatitis (Bouthoorn et al., 2011; Ghafoor et al., 2021; Lachenmeier, 2008). Unlike sanitizers and other disinfectants, alcohols were more effective in causing skin urticaria. In one study, skin urticaria was reported as a result of alcohol use (such as isopropanol) due to the combination of these alcohols with some solvents and organic matter (Berardi et al., 2020; Goh and Ahmed, 2020; Pecquet et al., 1992). The results obtained in this study regarding skin effects were in accordance with some scientific texts and similar studies (Bito et al., 2010; Chan and Maibach, 2008; Europe, 2017; Murphy and Friedman, 2019). The results of the multivariate regression analysis showed that detergents, alcohols or alcohol-based substances, and chlorine compounds have a higher potential of causing skin effects compared to other sanitizers and disinfectants.
Ocular effects (itching and irritation and eye redness) due to the use of sanitizers and disinfectants were less common than other effects. However, in terms of frequency, detergents and alcohol accounted for the largest share of ocular side effects. The results of some studies confirm our findings that itching and eye irritation are a result of the use of alcohol as a sanitizer/disinfectant (Ghafoor et al., 2021). Statistical results showed that among the chemicals studied, chlorine compounds had a higher chance of causing ocular effects compared to other disinfectants. This is probably due to the wide range of applications of chlorine compounds for different purposes as well as their ability to be mixed with other solvents. Studies have shown that the use of chlorine-based compounds in the form of sprays to disinfect surfaces will cause itching and eye irritation (Ghafoor et al., 2021; Schyllert et al., 2016; WHO, 2020). Since people used several types of chemicals separately or mixed to wash hands, face, and feet or to disinfect different surfaces, improper mixing of chemicals may release toxic gases and vapors that can affect the respiratory system. Studies have shown that mixing bleach with acidic cleaning agents leads to the release of highly irritating gases (PHE, 2015; Racioppi et al., 1994). Rosenman et al. claimed that not following hygienic instructions on how to use or mix cleansing products with other chemicals such as acid would create the conditions for chemical pneumonia or pulmonary edema (Rosenman et al., 2021). Our findings showed that chlorine compounds (sodium hypochlorite and per-chlorine) were involved in causing all effects related to the respiratory system. This claim was consistent with a list approved by the US Environmental Protection Agency (Alimohamadi et al., 2022b) that sodium hypochlorite is an irritant and allergen for the respiratory system (EPA, 2020). The results of multivariate regression analysis showed that formaldehyde had an immensely significant chance of causing neurological effects compared to other sanitizers and disinfectants. Formaldehyde, as a carcinogen by OSHA (Tarka et al., 2016), has an unpleasant odor and is an irritant that can cause many adverse effects on human health (Ghafoor et al., 2021).
Strengths and limitations
The present study holds significant value due to its comprehensive nature, covering 154 out of 192 United Nations member countries, indicating a truly global scope. The primary objective of this study was to achieve optimal participation across diverse segments of the general population. Regrettably, certain subgroups, namely villagers, individuals above the age of 60, non-academic individuals, and those employed in blue-collar occupations such as construction, manufacturing, and maintenance, exhibited lower levels of participation. This constraint constitutes a further limitation of the study. The main limitations of this study were the non-participation of individuals for personal reasons or lack of access to the internet, the drop-out of some countries (41 countries), and background effects such as exposure to various pollutants causing effects such as inflammation and respiratory effects, etc. (Hashemi et al., 2022a).
Conclusion
Our findings could serve as a useful source of information in reducing concerns related to the adverse health effects of sanitizers and disinfectant use through education and information by governments and health organizations during viral epidemics. Furthermore, the present results can be helpful for safety and health organizations overseeing the production of chemicals in updating instructions on how to use chemicals, as well as replacing low-risk, low-dose, high-impact chemicals in the production process if possible.
Supplementary information
COVID-19 Disease Questionnaire (PDF 122 kb)
Acknowledgements
We are sincerely thankful to the Research Center for Health Sciences, Department of Environmental Health, School of Health, Shiraz University of Medical Sciences, Shiraz, Iran. We also gratefully acknowledge the Kharkiv National Medical University and the esteemed president of that university, Dr. Valeriy Kapustnik, for their cooperation in uploading the electronic link of the questionnaire on the university’s website.
Author contribution
All authors contributed to the study’s conception and design. Data collection was performed by Fallah Hashemi, Lori Hoepner, Farahnaz Soleimani Hamidinejad,, Daniela Haluza, Sima Afrashteh, Alireza Abbasi, Elma Omeragić, Belma Imamović, Narin A. Rasheed,, Taqi Mohammed Jwad Taher, Fitri Kurniasari, Dhuha Youssef Wazqar, Özge Ceren Apalı, Ayca Demir Yildirim, Bo Zhao, Zaruhi Kalikyan, Cui Guo, Andrea Chong Valbuena, Magdalena Mititelu, Carolina Martínez Pando, Maria Saridi, Aikaterini Toska, Magalys Lopez Cuba, Precious Kwablah Kwadzokpui, Niguse Tadele, Tohfa Nasibova, Stefanie Harsch, Luvsan Munkh-Erdene, Wafaa Menawi, Efi Evangelou, Antoniya Dimova, Dimitar Marinov, Teodora Dimitrova, Anna Shalimova, Howieda Fouly, Anna Suraya,, Juliana Pereira da Silva Faquim, Bouadil Oumayma, Maria Antonieta Annunziato, Rezarta Lalo, Evridiki Papastavrou, Anju D. Ade, Susanna Caminada, Svetlana Stojkov, Carmen Gloria Narvaez, lutendo Sylvia Mudau, Ines Rassas, Daphnee Michel, Nur sema Kaynar, Sehar Iqbal, Halla Elshwekh, Irin Hossain, Sadeq AL-Fayyadh Aniuta Sydorchuk, Dua’a Mohammad Hasan Alnusairat Asli Mohamed Abdullahi, Neelam Iqbal, Apsara Pandey, Brenda Gómez-Gómez, Aysenur Gunaydin Akyildiz, Morosan Elena, Daniella Dwarica, Gantuya Dorj, Sumaya Yusuf Hasan, Noha M. Al-Shdayfat, Bojana Knezevic, Wendy Valladares, Cecilia Severi, Sofia Cuba Fuentes, Sofia Augusto, Elizaveta Sidorova, Anita Dewi Moelyaningrum, Tafaul Alawad, Atiqa Khalid,, Nafisa Mhna Kmbo Elehamer, Anna Mihaylova, Oxana Tsigengagel, Aziza Menouni, Agnieszka Wojtecka, Rozita Hod, Yusuf Banke Idayat, khadija Othman, Rim M. Harfouch, Tsonco Paunov, Meruyert Omar, Nana Christine Benderli,, Globila Nurika, Sana Amjad, Salma Elnoamany, Fatma Elesrigy, Marwa Mamdouh Shaban, Doménica Acevedo-López, Maria Kartashova, Atika Khalaf,, Sabah Abdullah Jaafar, Taisir A. Kadhim, Nada Ab. Hweissa, Yulong Teng, Fatima Elbasri Abuelgasim Mohammed Yagoub, Thayahlini Sasikumar, Christabel Nangandu Hikaambo, Aditi Kharat, Ulyana Lyamtseva, Maya Arfan Aldeeb,, Natalia Pawlas, Lkhagvasuren Khorolsuren, Roopeshwaree Pallavi Koonjul, Halima Boubacar Maïnassara, Priyanka Chahal, Rose Wangeci W, Ainur B. Kumar, Irina Zamora-Corrales, Stella Gracy, Maimouna Mahamat, Jakub Adamczyk, Haliza Abdul Rahman, Lolita Matiashova, Omneya Ezzat Elsherif, Nazdar Ezzaddin Rasheed Alkhateeb, Yamilé Aleaga, Shima Bahrami, Shaimaa Rahem Al-salihy, Paula Cabrera-Galeana, Mladena Lalic-Popovic, Eugenie Brown-Myrie, Divya Bhandari, Cinderella Akbar Mayaboti, Svetlana Stanišić, Sanda Kreitmayer Pestic, Muhammed Yunus Bektay, Haleama Al Sabbah, Saber Hashemi, Bouchetara Assia, Anne-Sophie Merritt, Zhian Ramzi, Himawatee Baboolal, Juman Isstaif, Rula Shami, Rahma Saad, Temwanani Nyirongo, Mohammad Hoseini.
Material preparation by Fallah Hashemi and Mohammad Hoseini, and data analysis by Lori Hoepner and Sima Afrashteh were performed. The first draft of the manuscript was written by Fallah Hashemi and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Data availability
There is no data to access online.
Declarations
Ethics approval
The study sampling protocol was approved by the Ethics Committee of the Shiraz University of Medical Science (IR.SUMS.REC.1400.023).
Consent to participate
All the people who participated in this study through an electronic questionnaire; Before answering the questions, they should have chosen the option of informed consent to participate in this research. It is necessary to explain that without choosing the option of informed consent, the participants were not able to enter the other sections of the questionnaire.
Consent for publication
All authors declare their consent to publish this article.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Fallah Hashemi, Email: info.foo@gmail.com.
Lori Hoepner, Email: Lori.Hoepner@downstate.edu.
Farahnaz Soleimani Hamidinejad, Email: solfarahnaz@gmail.com.
Daniela Haluza, Email: daniela.haluza@meduniwien.ac.at.
Sima Afrashteh, Email: sima.afrashte3@gmail.com.
Alireza Abbasi, Email: alireza.abasi1986@gmail.com.
Elma Omeragić, Email: elma.omeragic@ffsa.unsa.ba.
Belma Imamović, Email: belma.imamovic@ffsa.unsa.ba.
Narin A. Rasheed, Email: narin.rasheed@gmail.com
Taqi M. J. Taher, Email: ttahir@uowasit.edu.iq
Fitri Kurniasari, Email: fitri.kurniasari04@ui.ac.id.
Dhuha Youssef Wazqar, Email: dwazger@kau.edu.sa.
Özge Ceren Apalı, Email: oapali@hacettepe.edu.tr.
Ayca Demir Yildirim, Email: ayca.demiryildirim@uskudar.edu.tr.
Bo Zhao, Email: zhaobo@yonsei.ac.kr.
Zaruhi Kalikyan, Email: zkalikyan@yandex.ru.
Cui Guo, Email: guocuicui815@gmail.com.
Andrea Chong Valbuena, Email: chong.valbuena@gmail.com.
Magdalena Mititelu, Email: magdalena.mititelu@umfcd.ro.
Carolina Martínez Pando, Email: martinezpando_carolina@hotmail.com.
Maria Saridi, Email: sarmar32@windowslive.com.
Aikaterini Toska, Email: Ktoska07@yahoo.gr.
Magalys Lopez Cuba, Email: mlcuba@uhas.edu.gh.
Precious Kwablah Kwadzokpui, Email: kwadzokpuipreciousk@gmail.com, Email: 015pkwadzokpui@uhas.edu.gh.
Niguse Tadele, Email: niguse.tadele@aau.edu.et.
Tohfa Nasibova, Email: tnesibova@amu.edu.az.
Stefanie Harsch, Email: stefanie.harsch@ph-freiburg.de.
Luvsan Munkh-Erdene, Email: munkherdene@mnums.edu.mn.
Wafaa Menawi, Email: w.menawi@najah.edu.
Efi Evangelou, Email: evangeloue@hotmail.com.
Antoniya Dimova, Email: ant_dimova@abv.bg.
Dimitar Marinov, Email: dr.marinov.md@gmail.com.
Teodora Dimitrova, Email: tdimitrovatvd@gmail.com.
Anna Shalimova, Email: anna.shalimova83@gmail.com.
Howieda Fouly, Email: hoida.elfouly2@aun.edu.eg.
Anna Suraya, Email: Anna.suraya@binawan.ac.id.
Juliana Pereira da Silva Faquim, Email: julianafaquim@ufu.br.
Bouadil Oumayma, Email: Bouadiloumayma94@gmail.com.
Maria Antonieta Annunziato, Email: annunziato.maria@gmail.com.
Rezarta Lalo, Email: rezarta_lalo@yahoo.com.
Evridiki Papastavrou, Email: e.papastavrou@cut.ac.cy.
Anju D. Ade, Email: anju.ade@gmail.com
Susanna Caminada, Email: susanna.caminada@uniroma1.it.
Svetlana Stojkov, Email: svetlanastojkov22@gmail.com.
Carmen Gloria Narvaez, Email: cgnarvaez@udd.cl.
Lutendo Sylvia Mudau, Email: mudauls72@gmail.com.
Ines Rassas, Email: inesrassas@yahoo.fr.
Daphnee Michel, Email: daphnee.michel@uniq.edu.
Nur Sema Kaynar, Email: nursemakaynar1@gmail.com.
Sehar Iqbal, Email: Sehar.iqbal@aau.ac.ae.
Halla Elshwekh, Email: Halla.h.m@btc.org.ly.
Irin Hossain, Email: Irin.hossain@gmail.com.
Sadeq AL-Fayyadh, Email: s.al-fayyadh@conursing.uobaghdad.edu.iq.
Aniuta Sydorchuk, Email: sidorchuk@bsmu.edu.ua, Email: aniuta.sydorchuk@gmail.com.
Dua’a M. H. Alnusairat, Email: duaalnusairat@gmail.com
Asli Mohamed Abdullahi, Email: aslimaxamed10@gmail.com.
Apsara Pandey, Email: apsara.pandey@mnc.tu.edu.np.
Brenda Gómez-Gómez, Email: bred_gomez@hotmail.com.
Aysenur Gunaydin Akyildiz, Email: gunaydinaysenur@gmail.com.
Daniella Dwarica, Email: Danielladwarica@gmail.com.
Gantuya Dorj, Email: gantuya.d@mnums.edu.mn.
Sumaya Yusuf Hasan, Email: sumayayousif@agu.edu.bh.
Noha M. Al-Shdayfat, Email: dr.nuhash@aabu.edu.jo
Bojana Knezevic, Email: bojana.knezevic@kbc-zagreb.hr.
Wendy Valladares, Email: Wendy.valladares@unah.edu.hn.
Cecilia Severi, Email: severi.cecilia@gmail.com.
Sofia Cuba Fuentes, Email: maria.cuba@upch.pe.
Sofia Augusto, Email: s.augusto@fc.ul.pt.
Elizaveta Sidorova, Email: elizavsid@gmail.com.
Anita Dewi Moelyaningrum, Email: anitamoelyani@gmail.com, Email: anitadm@unej.ac.id.
Tafaul Alawad, Email: tafaulalawad@gmail.com.
Atiqa Khalid, Email: atiqakkhalid@gmail.com.
Nafisa M. K. Elehamer, Email: elehamer.nafisa@med.unideb.hu
Anna Mihaylova, Email: annamihaylova@abv.bg.
Oxana Tsigengagel, Email: tsigengagel.o@gmail.com.
Aziza Menouni, Email: aziza.menouni@kuleuven.be.
Agnieszka Wojtecka, Email: awojtecka@gumed.edu.pl.
Rozita Hod, Email: rozita.hod@ppukm.ukm.edu.my.
Yusuf Banke Idayat, Email: bitab19@yahoo.com.
Khadija Othman, Email: khadijaothman1993@gmail.com.
Rim M. Harfouch, Email: r.h.foph.LAT@aspu.edu.sy
Meruyert Omar, Email: Meruyertomar92@gmail.com.
Nana Christine Benderli, Email: christinenana@yahoo.fr.
Globila Nurika, Email: nurikaglobila@unej.ac.id.
Sana Amjad, Email: sana@ualberta.ca.
Salma Elnoamany, Email: salmaalnomany6@gmail.com.
Fatma Elesrigy, Email: Fatma.abdalgawad.12@med.menofia.edu.eg.
Marwa Mamdouh Shaban, Email: Marwamamdouh.mamdouh70@gmail.com.
Doménica Acevedo-López, Email: domeacevedo@gmail.com.
Maria Kartashova, Email: kmk8963@gmail.com.
Atika Khalaf, Email: atika.khalaf@hkr.se, Email: a.khalaf@squ.edu.om.
Sabah Abdullah Jaafar, Email: sabah.abd@mu.edu.iq.
Taisir A. Kadhim, Email: taisirak14@mu.edu.iq, Email: taiseer.alhussainy@gmail.com
Nada Ab Hweissa, Email: n.hweissa@zu.edu.ly.
Yulong Teng, Email: yulongteng@yonsei.ac.kr.
Fatima E. Mohammed, Email: fatima.abuelgasim12@gmail.com
Thayahlini Sasikumar, Email: thaya.viswa@gmail.com.
Christabel Nangandu Hikaambo, Email: xbellhikaambo@gmail.com, Email: Christabel.hikaambo@unza.zm.
Aditi Kharat, Email: aditi.kharat@utah.edu.
Ulyana Lyamtseva, Email: ulyamtseva@gmail.com.
Maya Arfan Aldeeb, Email: maldeeb@hamad.qa, Email: mayaldeeb@yahoo.com.
Natalia Pawlas, Email: natalia.pawlas@sum.edu.pl.
Lkhagvasuren Khorolsuren, Email: khorolsuren.l@mnums.edu.mn.
Roopeshwaree Pallavi Koonjul, Email: pallavikoonjul1234@gmail.com.
Halima Boubacar Maïnassara, Email: amhalima@gmail.com.
Priyanka Chahal, Email: drchahal10@gmail.com.
Rose W. Wangeci, Email: rwanjohi40@gmail.com
Ainur B. Kumar, Email: a.kumar@kaznmu.kz
Irina Zamora-Corrales, Email: irigaz87@gmail.com.
Stella Gracy, Email: gracystella1985@gmail.com.
Maimouna Mahamat, Email: m_mahamat@yahoo.fr.
Jakub Adamczyk, Email: j.adamczyk@ujd.edu.pl.
Haliza Abdul Rahman, Email: dr.haliza@upm.edu.my.
Lolita Matiashova, Email: lota94s@gmail.com.
Omneya Ezzat Elsherif, Email: oelsherif@hotmail.com.
Nazdar E. Alkhateeb, Email: nazdar.alkhateeb@hmu.edu.krd
Yamilé Aleaga, Email: Yamile.aleaga@ipk.sld.cu.
Shima Bahrami, Email: bahramishima31@gmail.com.
Shaimaa Rahem Al-salihy, Email: Sh.r802011@gmail.com.
Paula Cabrera-Galeana, Email: draPaulacabrera@gmail.com.
Mladena Lalic-Popovic, Email: mladena.lalic-popovic@mf.uns.ac.rs.
Eugenie Brown-Myrie, Email: ebrown@utech.edu.jm.
Divya Bhandari, Email: rayordeal3@gamil.com.
Cinderella Akbar Mayaboti, Email: cinderellamaya18@gmail.com.
Svetlana Stanišić, Email: sstanisic@singidunum.ac.rs.
Sanda Kreitmayer Pestic, Email: kreitmayersanda@gmail.com.
Muhammed Yunus Bektay, Email: yunusbektay@gmail.com.
Haleama Al Sabbah, Email: haleemah.alsabah@zu.ac.ae.
Saber Hashemi, Email: hashemisaber04@gmail.com.
Bouchetara Assia, Email: bouchetaraa@gmail.com.
Anne-Sophie Merritt, Email: anne-sophie.merritt@ki.se.
Zhian Ramzi, Email: zean.ramzi@univsul.edu.iq.
Himawatee Baboolal, Email: himawatee.baboolal475@we.utt.edu.tt.
Juman Isstaif, Email: j.isstaif@gmail.com.
Rula Shami, Email: ra1704753@qu.edu.qa.
Rahma Saad, Email: Rahmasaad63@gmail.com.
Temwanani Nyirongo, Email: temsnyirongo@gmail.com.
Mohammad Hoseini, Email: mohhoseini@sums.ac.ir.
References
- Afolabi AA, Ilesanmi OS (2021) Dealing with vaccine hesitancy in Africa: the prospective COVID-19 vaccine context. Pan Afr Med J:38. 10.11604/pamj.2021.38.3.27401 [DOI] [PMC free article] [PubMed]
- Alhouri A, Salloum A, Harfouch RM, Soumya G. Possible side effects of using detergents during the Covid19 pandemic in Syria. Ann Clin Cases. 2020;1:1023. [Google Scholar]
- Alimohamadi Y, Sepandi M, Rashti R, Nezhad HS, Afrashteh S. COVID-19: Clinical features, case fatality, and the effect of symptoms on mortality in hospitalized cases in Iran. J Taibah Univ Med Sci. 2022;17(5):725. doi: 10.1016/j.jtumed.2022.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alimohamadi Y, Sepandi M, Rashti R, Sedighinezhad H, Afrashteh S. COVID-19: clinical features, case fatality, and the effect of symptoms on mortality in hospitalized cases in Iran. J Taibah Univ Med Sci. 2022;17(5):725. doi: 10.1016/j.jtumed.2022.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Sayah MH. Chemical disinfectants of COVID-19: an overview. J Water Health. 2020;18:843–848. doi: 10.2166/wh.2020.108. [DOI] [PubMed] [Google Scholar]
- Amanollahi A, Ghorbani SS, Ghafouri HB, Afrashteh S, Nazari SSH. Which criteria were used to describe patients with COVID-19? A systematic review and meta analysis of clinical, laboratory, and imaging features. Med J Islam Repub Iran. 2021;35:112. doi: 10.47176/mjiri.35.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baldeo ARG, Castillo WV, Gegare RJD, Guiam-an LD, Ladaga JFE, Faller EM. The potential threat of excessive use of disinfectants: a review. J Homepage: www ijrpr com ISSN. 2022;2582:7421. [Google Scholar]
- Becher M, Stegmueller D, Brouard S, Kerrouche E. Ideology and compliance with health guidelines during the COVID-19 pandemic: a comparative perspective. Soc Sci Quart. 2021;102:2106–2123. doi: 10.1111/ssqu.13035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berardi A, Perinelli DR, Merchant HA, Bisharat L, Basheti IA, Bonacucina G, et al. Hand sanitisers amid CoViD-19: a critical review of alcohol-based products on the market and formulation approaches to respond to increasing demand. Int J Pharm. 2020;584:119431. doi: 10.1016/j.ijpharm.2020.119431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bito T, Izu K, Tokura Y. Evaluation of toxicity and Stat3 activation induced by hydrogen peroxide exposure to the skin in healthy individuals. J Dermatol Sci. 2010;58:157–159. doi: 10.1016/j.jdermsci.2010.03.013. [DOI] [PubMed] [Google Scholar]
- Bonin L, Vitry V, Olivier M-G, Bertolucci-Coelho L. Covid-19: effect of disinfection on corrosion of surfaces. Corros Eng Sci Technol. 2020;55:693–695. [Google Scholar]
- Bouthoorn SH, Van der Ploeg T, Van Erkel NE, Van der Lely N. Alcohol intoxication among Dutch adolescents: acute medical complications in the years 2000-2010. Clin Pediatr. 2011;50:244–251. doi: 10.1177/0009922810388509. [DOI] [PubMed] [Google Scholar]
- Bu F, Steptoe A, Mak HW, Fancourt D (2020) Time-use and mental health during the COVID-19 pandemic: a panel analysis of 55,204 adults followed across 11 weeks of lockdown in the UK. MedRxiv. 10.1101/2020.08.18.20177345
- Buguzi S (2021) Covid-19: counting the cost of denial in Tanzania. BMJ:373:n1052 [DOI] [PubMed]
- Cabral S, Ito N, Pongeluppe L (2021) The disastrous effects of leaders in denial: evidence from the COVID-19 crisis in Brazil. 10.2139/ssrn.3836147
- CDC. Reopening Guidance for cleaning and disinfecting public spaces, workplaces, businesses, schools, and homes. https://www.cdc.gov/coronavirus/2019-ncov/community/reopenguidance.html. Accessed 2020;7:16.
- Chan HP, Maibach HI. Hydrogen peroxide, blanching, and skin: an overview. Cutan Ocul Toxicol. 2008;27:307–309. doi: 10.1080/15569520802340396. [DOI] [PubMed] [Google Scholar]
- Chen Z, Guo J, Jiang Y, Shao Y. High concentration and high dose of disinfectants and antibiotics used during the COVID-19 pandemic threaten human health. Environ Sci Eu. 2021;33:1–4. doi: 10.1186/s12302-021-00456-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chin AW, Chu JT, Perera MR, Hui KP, Yen H-L, Chan MC, et al. Stability of SARS-CoV-2 in different environmental conditions. Lancet Mic. 2020;1:e10. doi: 10.1016/S2666-5247(20)30003-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi H-Y, Lee Y-H, Lim C-H, Kim Y-S, Lee I-S, Jo J-M, et al. Assessment of respiratory and systemic toxicity of Benzalkonium chloride following a 14-day inhalation study in rats. Part Fibre Toxicol. 2020;17:1–19. doi: 10.1186/s12989-020-0339-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook MA, Brooke N. Event-based surveillance of poisonings and potentially hazardous exposures over 12 months of the COVID-19 pandemic. Int J Environ Res Public Health. 2021;18:11133. doi: 10.3390/ijerph182111133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawood HN, Hwayyiz A, Alshemary IK, Rahman IA (2021) The clinical features of COVID-19 in a group of Iraqi patients: a record review. J Facult Med:63(1):8–12
- Dhama K, Patel SK, Kumar R, Masand R, Rana J, Yatoo M, et al. The role of disinfectants and sanitizers during COVID-19 pandemic: advantages and deleterious effects on humans and the environment. Environ Sci Pollut Res. 2021;28:34211–34228. doi: 10.1007/s11356-021-14429-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dindarloo K, Aghamolaei T, Ghanbarnejad A, Turki H, Hoseinvandtabar S, Pasalari H, et al. Pattern of disinfectants use and their adverse effects on the consumers after COVID-19 outbreak. J Environ Health Sci Eng. 2020;18:1301–1310. doi: 10.1007/s40201-020-00548-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dumas O, Varraso R, Boggs KM, Quinot C, Zock J-P, Henneberger PK, et al. Association of occupational exposure to disinfectants with incidence of chronic obstructive pulmonary disease among US female nurses. JAMA Netw Open. 2019;2:e1913563–e1913563. doi: 10.1001/jamanetworkopen.2019.13563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ECDC . European Centre for Disease Prevention and Control. Disinfection of environments in healthcare and nonhealthcare settings potentially contaminated with SARS-CoV-2. Stockholm: ECDC; 2020. [Google Scholar]
- Emmanuel E, Keck G, Blanchard J-M, Vermande P, Perrodin Y. Toxicological effects of disinfections using sodium hypochlorite on aquatic organisms and its contribution to AOX formation in hospital wastewater. Environ Int. 2004;30:891–900. doi: 10.1016/j.envint.2004.02.004. [DOI] [PubMed] [Google Scholar]
- EPA (2020) Environmental Protection Agency: pesticide registration: list N: disinfectants for use against SARS-CoV-2 (COVID-19)
- Europe . Assessment Report - active chlorine released from sodium hypochlorite. Regulation (EU) no 528/2012 concerning the making available on the market and use of biocidal products. Italy: Europe Commission; 2017. [Google Scholar]
- Ghafoor D, Khan Z, Khan A, Ualiyeva D, Zaman N. Excessive use of disinfectants against COVID-19 posing a potential threat to living beings. Curr Res Toxicol. 2021;2:159–168. doi: 10.1016/j.crtox.2021.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gharehchahi E, Dehghani F, Rafiee A, Jamalidoust M, Hoseini M. Investigating the presence of SARS-CoV-2 on the surfaces, fomites, and in indoor air of a referral COVID-19 Hospital, Shiraz Iran. J Health Sci Surveil Syst. 2023;11:241–251. [Google Scholar]
- Gharpure R, Hunter CM, Schnall AH, Barrett CE, Kirby AE, Kunz J, Berling K, Mercante JW, Murphy JL, Garcia‐Williams AG (2020) Knowledge and practices regarding safe household cleaning and disinfection for COVID-19 prevention—United States, American. J Transplant (10):2946–2950 [DOI] [PMC free article] [PubMed]
- Goh CF, Ahmed AHM. How to make hand sanitiser gel. Comm Eye Health. 2020;33:26. [PMC free article] [PubMed] [Google Scholar]
- Goh CF, Ming LC, Wong LC. Dermatologic reactions to disinfectant use during the COVID-19 pandemic. Clin Dermatol. 2021;39:314–322. doi: 10.1016/j.clindermatol.2020.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hashemi F, Hamidinejad FS, Hoepner L, Rafiee A, Abbasi A, Hoseini M. BTEX exposure of pregnant women and associations with pro-inflammatory cytokines (IL-6 and TNF-α) Air Quality, AtmosHealth. 2022;15:707–719. [Google Scholar]
- Hashemi F, Hoepner L, Hamidinejad FS, Abbasi A, Afrashteh S, Hoseini M. A survey on the correlation between PM(2.5) concentration and the incidence of suspected and positive cases of COVID-19 referred to medical centers: a case study of Tehran. Chemosphere. 2022;301:134650. doi: 10.1016/j.chemosphere.2022.134650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin Y-H, Cai L, Cheng Z-S, Cheng H, Deng T, Fan Y-P, et al. A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version) Mil Med Res. 2020;7:1–23. doi: 10.1186/s40779-020-0233-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kampf G. Potential role of inanimate surfaces for the spread of coronaviruses and their inactivation with disinfectant agents. Infect Prev Prac. 2020;2:100044. doi: 10.1016/j.infpip.2020.100044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lachenmeier DW. Safety evaluation of topical applications of ethanol on the skin and inside the oral cavity. J Occ Med Toxicol. 2008;3:1–16. doi: 10.1186/1745-6673-3-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonnell G, Russell AD. Antiseptics and disinfectants: activity, action, and resistance. Clin Microbiol Rev. 1999;12:147–179. doi: 10.1128/cmr.12.1.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy EC, Friedman AJ. Hydrogen peroxide and cutaneous biology: translational applications, benefits, and risks. J Am Acad Dermatol. 2019;81:1379–1386. doi: 10.1016/j.jaad.2019.05.030. [DOI] [PubMed] [Google Scholar]
- Nabi G, Wang Y, Hao Y, Khan S, Wu Y, Li D. Massive use of disinfectants against COVID-19 poses potential risks to urban wildlife. Environ Res. 2020;188:109916. doi: 10.1016/j.envres.2020.109916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, Tamin A, Harcourt JL, Thornburg NJ, Gerber SI, Lloyd-Smith JO (2020) Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 382(16):1564–1567 [DOI] [PMC free article] [PubMed]
- Paudel S, Shrestha R, Poudel P, Adhikari R. The influence of soap and alcohol-based cleanser on human skin. Spect Emerg Sci. 2022;2:56–65. [Google Scholar]
- Pecquet C, Pradalier A, Dry J. Allergic contact dermatitis from ethanol in a transdermal estradiol patch. Contact Dermatitis. 1992;27:275–275. doi: 10.1111/j.1600-0536.1992.tb03276.x. [DOI] [PubMed] [Google Scholar]
- PHE (2015) Compendium of chemical hazards: sodium hypochlorite In: Prajapati P, Desai H, Chandarana C (eds) Toxicological Overview. PHE publications gateway number, England
- Prajapati P, Desai H, Chandarana C. Hand sanitizers as a preventive measure in COVID-19 pandemic, its characteristics, and harmful effects: a review. J Egypt Public Health Ass. 2022;97:1–9. doi: 10.1186/s42506-021-00094-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Racioppi F, Daskaleros PA, Besbelli N, Borges A, Deraemaeker C, Magalini SI, et al. Household bleaches based on sodium hypochlorite: review of acute toxicology and poison control center experience. Food Chem Toxicol. 1994;32:845–861. doi: 10.1016/0278-6915(94)90162-7. [DOI] [PubMed] [Google Scholar]
- Rafiee A, Delgado-Saborit JM, Sly PD, Amiri H, Mosalaei S, Hoseini M. Health consequences of disinfection against SARS-CoV-2: exploring oxidative stress damage using a biomonitoring approach. Sci Total Environ. 2022;814:152832. doi: 10.1016/j.scitotenv.2021.152832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rai NK, Ashok A, Akondi BR. Consequences of chemical impact of disinfectants: safe preventive measures against COVID-19. Crit Rev Toxicol. 2020;50:513–520. doi: 10.1080/10408444.2020.1790499. [DOI] [PubMed] [Google Scholar]
- Rosenman KD, Reilly MJ, Wang L. Calls to a state poison center concerning cleaners and disinfectants from the onset of the COVID-19 pandemic through April 2020. Public Health Rep. 2021;136:27–31. doi: 10.1177/0033354920962437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutala WA, Weber DJ. Disinfection, sterilization, and antisepsis: an overview. Am J Infect Control. 2019;47:A3–A9. doi: 10.1016/j.ajic.2019.01.018. [DOI] [PubMed] [Google Scholar]
- Schyllert C, Rönmark E, Andersson M, Hedlund U, Lundbäck B, Hedman L, et al. Occupational exposure to chemicals drives the increased risk of asthma and rhinitis observed for exposure to vapours, gas, dust and fumes: a cross-sectional population-based study. Occup Environ Med. 2016;73:663–669. doi: 10.1136/oemed-2016-103595. [DOI] [PubMed] [Google Scholar]
- Shah K, Chhabra S, Chauhan NS. Disinfectants in the arena of COVID-19. Biomed Biotechnol Res J (BBRJ) 2021;5:121. [Google Scholar]
- Sharun K, Tiwari R, Yatoo MI, Natesan S, Megawati D, Singh KP, et al. A comprehensive review on pharmacologic agents, immunotherapies and supportive therapeutics for COVID-19. Narra J. 2022;2:e92–e92. doi: 10.52225/narra.v2i3.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shibuya R, Ishida Y, Hanakawa S, Kataoka TR, Takeuchi Y, Murata T, et al. CCL2–CCR2 signaling in the skin drives surfactant-induced irritant contact dermatitis through IL-1β–mediated neutrophil accumulation. J Invest Dermatol. 2022;142(571-582):e9. doi: 10.1016/j.jid.2021.07.182. [DOI] [PubMed] [Google Scholar]
- Tachikawa T. Overreliance on hand sanitizers may increase risk of coronavirus infection. Kyodo News; 2020. [Google Scholar]
- Tarka P, Kanecki K, Tomasiewicz K. Evaluation of chemical agents intended for surface disinfection with the use of carrier methods. Bactericidal, yeasticidal and sporocidal activity. Postepy Mikrobiologii. 2016;55:99–104. [Google Scholar]
- Tran TPT, Le TH, Nguyen TNP (2020) Rapid response to the COVID-19 pandemic: Vietnam government’s experience and preliminary success. J Glob Health:10. 10.7189/jogh.10.020502 [DOI] [PMC free article] [PubMed]
- Thagard P. The cognitive science of COVID-19: acceptance, denial, and belief change. Methods. 2021;195:92–102. doi: 10.1016/j.ymeth.2021.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unruh L, Allin S, Marchildon G, Burke S, Barry S, Siersbaek R, et al. A comparison of 2020 health policy responses to the COVID-19 pandemic in Canada, Ireland, the United Kingdom and the United States of America. Health Policy. 2022;126:427–437. doi: 10.1016/j.healthpol.2021.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viveiros-Rosa SG, Mendes CD, Farfán-Cano GG, El-Shazly M. The race for clinical trials on Omicron-based COVID-19 vaccine candidates: updates from global databases. Narra J. 2022;2:e88–e88. doi: 10.52225/narra.v2i3.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogel L. Hand sanitizers may increase norovirus risk. Can Med Assoc; 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . Cleaning and disinfection of environmental surfaces in the context of COVID-19: interim guidance. World Health Organization; 2020. [Google Scholar]
- World Health Organization (2022) WHO Coronavirus (COVID-19) Dashboard. https://covid19.who.int/
- Xu W, Wu J, Cao L. COVID-19 pandemic in China: context, experience and lessons. Health Pol Technol. 2020;9:639–648. doi: 10.1016/j.hlpt.2020.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yari S, Moshammer H, Asadi AF. Side effects of using disinfectants to fight COVID-19. As Pac J Environ Can. 2020;3:9–13. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
COVID-19 Disease Questionnaire (PDF 122 kb)
Data Availability Statement
There is no data to access online.