Abstract
Background
Access to reliable transportation is fundamental in the management of chronic disease. The purpose of this study was to investigate the association between vehicle ownership at the neighborhood-level and long-term mortality after myocardial infarction (MI).
Methods
This is a retrospective observational study evaluating adult patients admitted for MI between January 1st, 2006, and December 31st, 2016. Neighborhoods were defined by census tract and household vehicle ownership data was obtained from the American Community Survey courtesy of the University of California, Los Angeles Center for Neighborhood Knowledge. Patients were divided into 2 groups: those living in neighborhoods with higher vehicle ownership, and those living in neighborhoods with lower vehicle ownership. The cutoff of 4.34% of households reporting not owning a vehicle was used to define a neighborhood as one with “higher” vs “lower” vehicle ownership as this was the median value for the cohort. The association between vehicle ownership and all-cause mortality after MI was assessed using Cox proportional hazards regression models.
Results
A total of 30,126 patients were included (age 68.1 +/- 13.5 years, 63.2% male). After adjusting for age, sex, race/ethnicity, and medical comorbidities, lower vehicle ownership was associated with increased all-cause mortality after MI (hazard ratio [HR] 1.10; 95% confidence interval [CI] 1.06–1.14; p<0.001). This finding remained significant after adjusting for median household income (HR 1.06; 95% CI 1.02–1.10; p = 0.007). Upon comparison of White and Black patients living in neighborhoods with lower vehicle ownership; Black patients were found to have an increased all-cause mortality after MI (HR 1.21, 95% CI 1.13–1.30, p<0.001), a difference which remained significant after adjusting for income (HR 1.20; 95% CI 1.12–1.29; p<0.001). There was no significant difference in mortality between White and Black patients living in neighborhoods with higher vehicle ownership.
Conclusion
Lower vehicle ownership was associated with increased mortality after MI. Black patients living in neighborhoods with lower vehicle ownership had a higher mortality after MI than White patients living in similar neighborhoods but Black patients living in neighborhoods with higher vehicle ownership had no worse mortality than their White counterparts. This study highlights the importance of transportation in determining health status after MI.
1. Introduction
Living with ischemic heart disease requires careful attention to many aspects of daily life. Medications, doctor visits, diet, exercise, and managing stress are all vital components in treating this progressive disease [1]. The ability to incorporate these elements into one's lifestyle is heavily dependent upon the ability to access reliable transportation. Lack of transportation has been associated with lower adherence to medication use [2], [3], [4], [5], [6], inability to make it to medical appointments [2,7,8], and limitations in accessing nutritious foods [9].
The neighborhoods in which people live are instrumental in determining transportation accessibility as well as in determining the extent to which the lack of transportation will impact one's health. People who live in neighborhoods with limited access to transportation have fewer employment opportunities and are more likely to endure hardships related to poverty [10]. Beyond financial difficulties, individuals who live in these neighborhoods have less access to fresh fruits and vegetables [10] and less access to safe outdoor spaces for exercise and recreation [11]. These individuals may also be more reliant on active forms of transportation, such as walking or riding a bike, and are more likely to engage in these activities in dangerous conditions due to substandard infrastructure for active transport in these communities [10].
The association between the neighborhood in which a person lives and health outcomes has been described for a variety of disease states [12], [13], [14], including ischemic heart disease [15], [16], [17]. Previously validated indices for evaluating neighborhood socioeconomic status include metrics to evaluate transportation access because of the significant role transportation plays in determining health status [18,19]. Despite broad acknowledgement that transportation is one of the fundamental social determinants of health, the existing literature regarding the association between transportation disparities and outcomes after myocardial infarction is very limited. This study is intended to explore the association between disparities in household vehicle ownership and mortality after myocardial infarction (MI).
2. Methods
2.1. Study population
This is a retrospective observational study utilizing data from the Kaiser Permanente Southern California (KPSC) Health System. KPSC is an integrated health system that serves over 4.5 million members. KPSC members receive comprehensive healthcare insurance via enrollment through the Kaiser Foundation Health Plan. KPSC provides care to a population of members that represent the racial and ethnic diversity of the Southern California region. Member information is prospectively captured through a centralized electronic data warehouse and available electronic datasets contain information pertaining to demographics, pharmacy records, laboratory records, and healthcare utilization from both ambulatory visits and hospitalizations. The present study has been approved by the KPSC Institutional Review Board and given the observational nature of the study; a waiver of informed consent was obtained.
Adult patients (≥ 18 years old) admitted to the hospital with a principal diagnosis of acute MI between January 1st, 2006, and December 31st, 2016, were identified using International Classification of Diseases (ICD) 9 or 10 codes 412.x, 414.12, I21.x, I22.x, I23.x, or I25.42. Each patient was included in the study only once with the date of the first diagnosis of acute MI during the study period used as the index date. The one-year period prior to the index date was defined as the baseline window. Covariates were identified according to the following categories: demographics, medical comorbidities, cardiac risk factors, and use of cardiac medications. Medical comorbidities and cardiac risk factors were collected from the one-year prior to the index date. Use of cardiac medications was identified using outpatient pharmacy records.
Patients were excluded if they were not KPSC members and if they did not have continuous one-year membership prior to the index date to allow for adequate assessment of baseline covariates. Patients who died within 30 days of admission were excluded as the intent of the study was to examine the effect of transportation access on long-term outcomes. Patients without a permanent address on file that could be used to determine the census tract in which the patient lived were also excluded. Race and ethnicity were based on self-reported data and were categorized as White, Black, Hispanic (which included Hispanic people of any race), Asian (which included Pacific Islanders), and other (which included mixed race, Native American/Alaska Native, and unknown).
2.2. Vehicle ownership
Neighborhoods were defined by the census tract where each patient resided according to their address at the time of the index hospitalization. Household vehicle ownership data for each patient's neighborhood was obtained from the 2014–2018 American Community Survey courtesy of the University of California, Los Angeles Center for Neighborhood Knowledge [20]. The transportation metric utilized was the percentage of households in a neighborhood (census tract) that do not own a vehicle.
Patients were divided into 2 groups based on their neighborhood of residence: those living in neighborhoods with higher vehicle ownership, and those living in neighborhoods with lower vehicle ownership. Lower vehicle ownership is defined as neighborhoods with ≥ 4.34% of households reporting not owning a vehicle and higher vehicle ownership is defined as neighborhoods with < 4.34% of households reporting not owning a vehicle. The cutoff for determining if a neighborhood would be considered one with “higher” vs “lower” vehicle ownership was obtained by taking the median for the percentage of households with no vehicle for the entire cohort of patients included in the study.
2.3. Mortality
Mortality data was obtained from a mortality data file maintained at KPSC, with integrated death information derived from multiple sources including insurance enrollment records, hospital death records, and death master files from the State of California and the Social Security Administration.
2.4. Statistical analysis
All-cause mortality was analyzed according to the percentage of households without a vehicle in a neighborhood as well as race/ethnicity. Descriptive statistics were used to analyze covariate distribution. Continuous variables were reported as means with standard deviations and compared using the independent t-test. Categorical variables were reported as counts and percentages and were compared using the chi-square test.
Kaplan-Meier cumulative incidence plots were generated to show time to events for the primary endpoint of all-cause mortality. The association between living in a neighborhood with a higher percentage of households with no vehicle and all-cause mortality after myocardial infarction was assessed using Cox proportional hazards regression models. Multivariable models adjusted for age, sex, race/ethnicity, neighborhood median income, and medical comorbidities were used to estimate hazard ratios with 95% confidence intervals. P-values of less than 0.05 for association were used to indicate statistical significance. Statistical analyses were performed using Python 3.11 (Python Software Foundation, Wilmington, DE).
3. Results
3.1. Study population
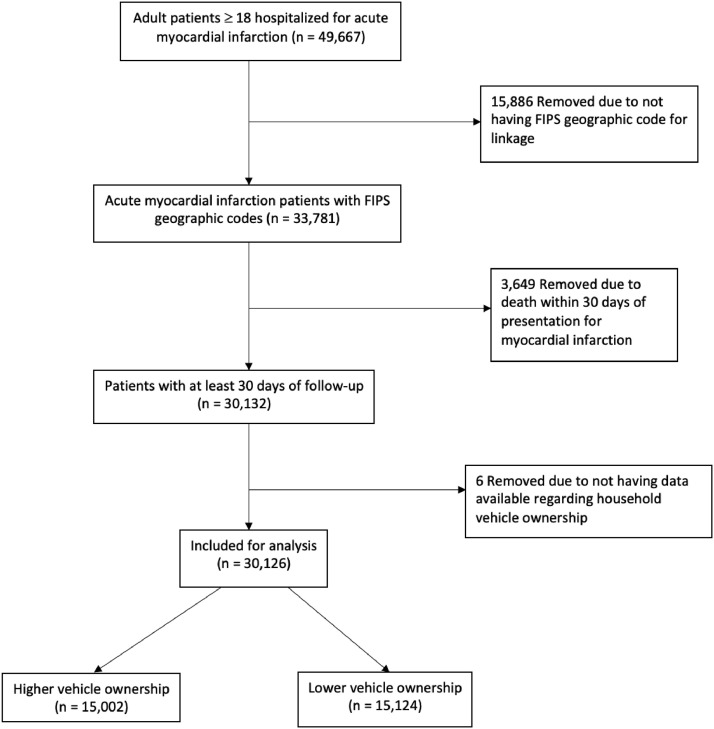
Between January 1, 2006, and December 31, 2016, a total of 49,667 patients were admitted to the hospital with a principal diagnosis of acute MI (Fig. 1). From this initial cohort, 33,781 had an address on file from which a Federal Information Processing Standard (FIPS) geographic code was available for determination of census tract, 30,132 survived beyond 30 days from the admission date of the index hospitalization, and 30,126 had data available regarding the percentage of households with no vehicle for their census tract and were ultimately included for analysis.
Fig. 1.
(page 21): flowchart of patient eligibility and inclusion.
Patients were separated into 2 groups based on percentage of households with no vehicle for their census tract: those living in neighborhoods with higher vehicle ownership (< 4.34% of households with no vehicle, n = 15,002 [49.8%]) and those living in neighborhoods with lower vehicle ownership (≥ 4.34% of households with no vehicle, n = 15,124 [50.2%]). White and Black patients were further separated into groups according to whether they lived in a neighborhood with higher or lower vehicle ownership: White patients living in neighborhoods with lower vehicle ownership (n = 7257), Black patients living in neighborhoods with lower vehicle ownership (n = 2305), White patients living in neighborhoods with higher vehicle ownership (n = 9267), and Black patients living in neighborhoods with higher vehicle ownership (n = 1069). Asian and Hispanic patients were also separated into groups according to neighborhood and descriptive statistics for these groupings can be found in Tables S1 and S2 of the supplemental appendix.
Compared to the higher vehicle ownership group, the lower vehicle ownership group had a higher percentage of women, Black, and Hispanic patients (Table 1). The lower vehicle ownership group had more patients living in neighborhoods with a median household income of < $45,000 per year and more patients insured through Medicaid. There were higher rates of hypertension, diabetes, congestive heart failure, stroke, lung disease, liver disease, kidney disease, and active smoking among patients in the lower vehicle ownership group.
Table 1.
: Baseline characteristics according to neighborhood vehicle ownership and race.
| Higher Vehicle Ownership |
Lower Vehicle Ownership |
White Patients Lower Vehicle Ownership |
Black Patients Lower Vehicle Ownership |
White Patients Higher Vehicle Ownership |
Black Patients Higher Vehicle Ownership |
||||
|---|---|---|---|---|---|---|---|---|---|
| (n = 15,002) | (n = 15,124) | P value | (n = 7257) | (n = 2305) | P value | (n = 9267) | (n = 1069) | P value | |
| Demographics | |||||||||
| Age | 67.8 (+/- 13.2) | 68.5 (+/- 13.7) | <0.01 | 71.2 (+/- 13.1) | 68.2 (+/- 13.5) | <0.01 | 69.6 (+/- 12.9) | 66.6 (+/- 13.2) | <0.01 |
| Male | 9857 (65.7) | 9197 (60.8) | <0.01 | 4435 (61.1) | 1131 (49.1) | <0.01 | 6017 (64.9) | 601 (56.2) | <0.01 |
| Race/Ethnicity | |||||||||
| Asian | 1263 (8.4) | 1145 (7.6) | <0.01 | ||||||
| Black | 1069 (7.1) | 2305 (15.2) | <0.01 | ||||||
| Hispanic | 2957 (19.7) | 3934 (26.0) | <0.01 | ||||||
| White | 9267 (61.8) | 7257 (48.0) | <0.01 | ||||||
| Other | 446 (3.0) | 483 (3.2) | 0.28 | ||||||
| Income | |||||||||
| < $45,000 | 1278 (8.5) | 6752 (44.6) | <0.01 | 2599 (35.8) | 1361 (59.0) | <0.01 | 659 (7.1) | 115 (10.8) | <0.01 |
| $45,000-$80,000 | 7886 (52.6) | 6775 (44.8) | <0.01 | 3619 (49.9) | 823 (35.7) | <0.01 | 4492 (48.5) | 654 (61.2) | <0.01 |
| >$80,000 | 5838 (38.9) | 1597 (10.6) | <0.01 | 1039 (14.3) | 121 (5.2) | <0.01 | 4116 (44.4) | 300 (28.1) | <0.01 |
| Insurance | |||||||||
| Commercial | 5953 (39.7) | 6035 (39.9) | 0.70 | 2420 (33.3) | 974 (42.3) | <0.01 | 3263 (35.2) | 478 (44.7) | <0.01 |
| Medicaid | 280 (1.9) | 522 (3.5) | <0.01 | 101 (1.4) | 101 (4.4) | <0.01 | 88 (0.9) | 33 (3.1) | <0.01 |
| Medicare | 5047 (33.6) | 5108 (33.8) | 0.82 | 2851 (39.3) | 743 (32.2) | <0.01 | 3475 (37.5) | 292 (27.3) | <0.01 |
| Other Insurance | 3722 (24.8) | 3459 (22.9) | <0.01 | 1885 (26.0) | 487 (21.1) | <0.01 | 2441 (26.3) | 266 (24.9) | 0.32 |
| Comorbidities | |||||||||
| Hypertension | 10,042 (66.9) | 10,659 (70.5) | <0.01 | 5123 (70.6) | 1850 (80.3) | <0.01 | 6197 (66.9) | 845 (79.0) | <0.01 |
| Hyperlipidemia | 9304 (62.0) | 9510 (62.9) | 0.12 | 4560 (62.8) | 1445 (62.7) | 0.92 | 5684 (61.3) | 680 (63.6) | 0.16 |
| Diabetes | 5099 (34.0) | 5756 (38.1) | <0.01 | 2332 (32.1) | 983 (42.6) | <0.01 | 2730 (29.5) | 414 (38.7) | <0.01 |
| Obesity | 2965 (19.8) | 3103 (20.5) | 0.11 | 1386 (19.1) | 602 (26.1) | <0.01 | 1795 (19.4) | 284 (26.6) | <0.01 |
| CAD | 2673 (17.8) | 2727 (18.0) | 0.64 | 1419 (19.6) | 425 (18.4) | 0.25 | 1784 (19.3) | 180 (16.8) | 0.06 |
| PVD | 4214 (28.1) | 4478 (29.6) | <0.01 | 2308 (31.8) | 767 (33.3) | 0.20 | 2771 (29.9) | 315 (29.5) | 0.80 |
| Atrial Fibrillation | 1571 (10.5) | 1609 (10.6) | 0.65 | 950 (13.1) | 231 (10.0) | <0.01 | 1148 (12.4) | 102 (9.5) | <0.01 |
| CHF | 2213 (14.8) | 2641 (17.5) | <0.01 | 1275 (17.6) | 539 (23.4) | <0.01 | 1405 (15.2) | 205 (19.2) | <0.01 |
| Stroke | 2404 (16.0) | 2591 (17.1) | 0.01 | 1347 (18.6) | 429 (18.6) | 0.98 | 1568 (16.9) | 210 (19.6) | 0.03 |
| Lung Disease | 3180 (21.2) | 3467 (22.9) | <0.01 | 1905 (26.3) | 571 (24.8) | 0.17 | 2129 (23.0) | 240 (22.5) | 0.73 |
| Liver Disease | 573 (3.8) | 664 (4.4) | 0.01 | 264 (3.6) | 117 (5.1) | <0.01 | 318 (3.4) | 38 (3.6) | 0.90 |
| Kidney Disease | 3989 (26.6) | 4642 (30.7) | <0.01 | 2142 (29.5) | 920 (39.9) | <0.01 | 2405 (26.0) | 342 (32.0) | <0.01 |
| Prior Medications | |||||||||
| Statin | 7751 (51.7) | 7968 (52.7) | 0.08 | 3891 (53.6) | 1223 (53.1) | 0.66 | 4781 (51.6) | 558 (52.2) | 0.73 |
| P2Y12 | 1419 (9.5) | 1431 (9.5) | 1.00 | 735 (10.1) | 223 (9.7) | 0.55 | 887 (9.6) | 115 (10.8) | 0.23 |
| Beta Blocker | 6338 (42.2) | 6589 (43.6) | 0.02 | 3277 (45.2) | 1126 (48.9) | <0.01 | 3991 (43.1) | 506 (47.3) | <0.01 |
| ACEi/ARB | 7692 (51.3) | 7964 (52.7) | 0.02 | 3790 (52.2) | 1308 (56.7) | <0.01 | 4676 (50.5) | 608 (56.9) | <0.01 |
| Nitrate | 1133 (7.6) | 1249 (8.3) | 0.02 | 590 (8.1) | 246 (10.7) | <0.01 | 664 (7.2) | 87 (8.1) | 0.27 |
| Smoking History | |||||||||
| Active | 1376 (9.2) | 1615 (10.7) | <0.01 | 789 (10.9) | 284 (12.3) | 0.06 | 892 (9.6) | 123 (11.5) | 0.06 |
| Passive | 56 (0.4) | 71 (0.5) | 0.23 | 31 (0.4) | 16 (0.7) | 0.15 | 28 (0.3) | 6 (0.6) | 0.16 |
| Quit | 4837 (32.2) | 4852 (32.1) | 0.77 | 2559 (35.3) | 771 (33.4) | 0.12 | 3173 (34.2) | 358 (33.5) | 0.65 |
| Never | 5650 (37.7) | 5559 (36.8) | 0.11 | 2372 (32.7) | 815 (35.4) | 0.02 | 3197 (34.5) | 408 (38.2) | 0.02 |
| Missing Information | 3083 (20.6) | 3027 (20.0) | 0.25 | 1506 (20.8) | 419 (18.2) | <0.01 | 1977 (21.3) | 174 (16.3) | <0.01 |
| Treatment for MI | |||||||||
| Medical Therapy | 8970 (59.8) | 9142 (60.4) | 0.25 | 4485 (61.8) | 1563 (67.8) | <0.01 | 5649 (61.0) | 742 (69.4) | <0.01 |
| PCI | 4804 (32.0) | 4754 (31.4) | 0.28 | 2210 (30.5) | 602 (26.1) | <0.01 | 2894 (31.2) | 265 (24.8) | <0.01 |
| CABG | 1562 (10.4) | 1528 (10.1) | 0.39 | 710 (9.8) | 169 (7.3) | <0.01 | 920 (9.9) | 78 (7.3) | <0.01 |
Abbreviations: CAD, coronary artery disease; PVD, peripheral vascular disease; CHF, congestive heart failure; P2Y12, P2Y12 inhibiting medications; ACEi, angiotensin converting enzyme inhibitor; ARB, angiotensin receptor blocker; MI, myocardial infarction; PCI, percutaneous coronary intervention; CABG, coronary artery bypass surgery.
White and Black patients had significantly different baseline demographics and comorbidity profiles, irrespective of whether they lived in a neighborhood with higher or lower vehicle ownership. Black patients were more likely to be younger, female, living in a neighborhood with a median household income of < $45,000 per year, and to be insured through commercial insurance or Medicaid. White patients were more likely to be insured through Medicare. Black patients had higher rates of hypertension, diabetes, obesity, congestive heart failure, and kidney disease. White patients had higher rates of atrial fibrillation. Black patients were more likely to have previously been prescribed beta blockers, angiotensin-converting enzyme inhibitors (ACEi) or angiotensin II receptor blockers (ARB). Black patients were more likely to have never smoked. Black patients were less likely to receive reperfusion therapy (percutaneous coronary intervention or coronary artery bypass surgery) compared to White patients.
Among White and Black patients living in neighborhoods with lower vehicle ownership; Black patients were more likely to have a prior history of liver disease and to have been prescribed nitrates. Among White and Black patients living in neighborhoods with higher vehicle ownership; Black patients were more likely to have a history of stroke.
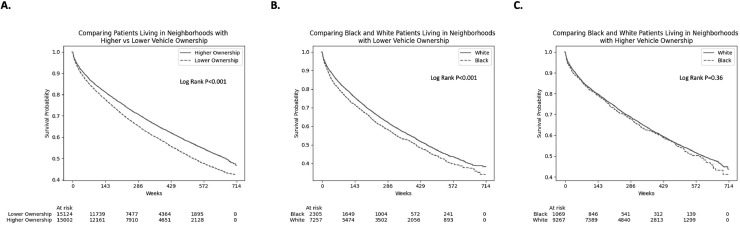
3.2. Association between vehicle ownership and mortality
Patients were followed for 6.2 +/- 3.8 years. Kaplan-Meier survival curves comparing all-cause mortality between patients living in neighborhoods with higher vs lower vehicle ownership demonstrate significantly higher mortality among patients living in neighborhoods with lower vehicle ownership (Fig. 2A, log rank p<0.001). Kaplan-Meier survival curves comparing all-cause mortality between White and Black patients living in neighborhoods with lower vehicle ownership demonstrate significantly higher mortality among Black patients (Fig. 2B, log rank p<0.001). Kaplan-Meier survival curves comparing all-cause mortality between White and Black patients living in neighborhoods with higher vehicle ownership demonstrate no significant mortality difference (Fig. 2C, log rank p = 0.36).
Fig. 2.
(page 22): Kaplan-Meier curves.
A. Comparing all-cause death according to neighborhood vehicle ownership.
B. Comparing all-cause death between White and Black patients living in neighborhoods with lower vehicle ownership.
C. Comparing all-cause death between White and Black patients living in neighborhoods with higher vehicle ownership.
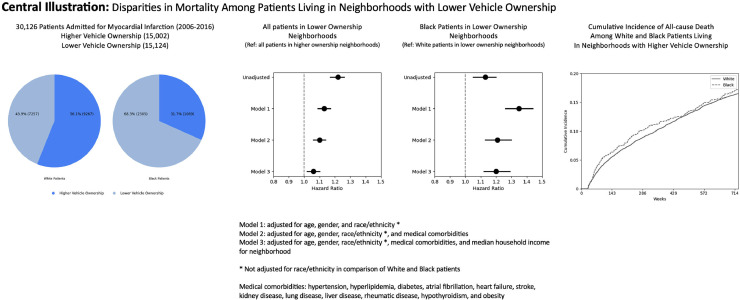
Central illustration (page 23): Mortality disparities according to neighborhood and race.
Table 2 shows the association between vehicle ownership and all-cause mortality. After adjusting for age, gender, race/ethnicity, and medical comorbidities, living in a neighborhood with lower vehicle ownership was associated with significantly higher all-cause mortality when compared to living in a neighborhood with higher vehicle ownership (hazard ratio [HR] 1.10; 95% confidence interval [CI] 1.06–1.14; p<0.001). This difference remained significant after adjusting for neighborhood median household income (HR 1.06; 95% CI 1.02–1.10; p = 0.007).
Table 2.
: Hazard ratios for all-cause death according to neighborhood vehicle ownership and race.
| Higher Vehicle Ownership | Lower Vehicle Ownership | P value | White Patients Lower Vehicle Ownership | Black Patients Lower Vehicle Ownership | P value | ||
|---|---|---|---|---|---|---|---|
| Unadjusted | Reference | 1.22 (1.17–1.26) | <0.001 | Reference | 1.13 (1.05–1.20) | <0.001 | |
| Model 1 | 1.13 (1.09–1.17) | <0.001 | 1.35 (1.26–1.44) | <0.001 | |||
| Model 2 | 1.10 (1.06–1.14) | <0.001 | 1.21 (1.13–1.30) | <0.001 | |||
| Model 3 | 1.06 (1.02–1.10) | 0.007 | 1.20 (1.12–1.29) | <0.001 | |||
Model 1: adjusted for age, gender, and race/ethnicity (not adjusted for race/ethnicity in comparison of White and Black patients).
Model 2: adjusted for age, gender, race/ethnicity (not adjusted for race/ethnicity in comparison of White and Black patients), and medical comorbidities (hypertension, hyperlipidemia, diabetes, atrial fibrillation, heart failure, stroke, kidney disease, lung disease, liver disease, rheumatic disease, hypothyroidism, and obesity.
Model 3: adjusted for age, gender, race/ethnicity (not adjusted for race/ethnicity in comparison of White and Black patients), medical comorbidities, and median household income for neighborhood.
Upon comparison between White and Black patients living in neighborhoods with lower vehicle ownership, after adjusting for age, gender, and medical comorbidities, being Black was associated with significantly higher all-cause mortality when compared to being White (HR 1.21; 95% CI 1.13–1.30; p<0.001). This difference remained significant after adjusting for neighborhood median household income (HR 1.20; 95% CI 1.12–1.29; p<0.001). Both the Asian and Hispanic cohorts were found to have lower mortality than White patients regardless of neighborhood, but this finding was not significant after adjusting for age and gender (see Figure S1 and Tables S3 and S4 for the survival analyses for these groups).
4. Discussion
Transportation is recognized as a fundamental social determinant of health but research investigating transportation disparities among patients with ischemic heart disease is lacking. The present study demonstrates that patients living in neighborhoods with lower vehicle ownership have a higher mortality after acute myocardial infarction compared to patients living in neighborhoods with higher vehicle ownership, even after accounting for median household income. Additionally, among those living in neighborhoods with lower vehicle ownership, Black patients had a higher mortality after acute myocardial infarction compared to White patients. There was no mortality difference between Black and White patients living in neighborhoods with higher vehicle ownership, suggesting that transportation serves as a key mediator in the disparities in health outcomes between Black and White patients after myocardial infarction.
Transportation inequities are increasingly recognized as significant contributors to disparities in healthcare access [21]. Despite this recognition, there is limited research into which patients are at the greatest risk for adverse health outcomes due to inadequate transportation [21] and this is especially true for patients with ischemic heart disease. This lack of research may explain why transportation intervention programs have failed to demonstrate a significant impact on medical outcomes [7,[21], [22], [23], [24]].
The one study that was found which specifically investigated the association between transportation barriers and outcomes in patients with ischemic heart disease is a 2018 paper by Erskine et al. This study utilized survey data of 2008 patients who suffered an acute MI to determine the association between transportation barriers, financial barriers, and lack of usual source of medical care with all-cause mortality. The authors found that patients who reported difficulty accessing healthcare due to transportation issues the year prior to MI had increased mortality at 2 -years post-MI. However, there were only 239 patients who reported transportation to be an issue with accessing medical care and the increased mortality among these patients appears to be due entirely to the 44 patients who reported having all three of the healthcare access barriers present: transportation barriers, financial barriers, and lack of usual source of medical care [25].
The study presented in this manuscript is unique in that the patients included were all well-insured, had equal access to primary and subspecialty care, and received their in-hospital and follow-up care in very similar medical centers because of their membership with the KPSC Health System. Even with these variables controlled for and after adjusting for median household income, there was still a significantly higher mortality among patients living in neighborhoods with lower vehicle ownership. The present study also included a very large and diverse patient cohort, which allowed for a thorough assessment of outcomes based on racial and ethnic differences. The fact that this study was able to control for treatment setting is particularly important in this regard as racial/ethnic differences in outcomes after MI have previously been demonstrated to be associated with racial and ethnic minorities being treated in lower performing medical centers compared to their White counterparts [26,27].
The utilization of an area-based metric of transportation disparities likely captures patients with additional socioeconomic risks but these risks cannot be ignored. On the contrary, the additional risk factors a patient has due to living in a neighborhood with lower vehicle ownership are likely magnified among those patients with unreliable transportation and an area-based transportation assessment helps to put these risks into context. It is notable that this study demonstrated increased mortality among patients living in neighborhoods with lower vehicle ownership even after adjusting for income. This is consistent with prior research demonstrating that living in a disadvantaged neighborhood can have detrimental health effects that are independent of a person's socioeconomic status [12,28,29] and the present findings suggest that transportation disparities may be a contributing factor.
Access to a motor vehicle is vitally important to chronic disease management and lack of adequate transportation has been associated with inability to make it to medical appointments [2,8,[30], [31], [32], [33]], delays in receiving medical therapy [2,[34], [35], [36]], increased reliance on emergency departments to receive care [2,37,38], and decreased likelihood to fill prescriptions [2], [3], [4], [5], [6]. Beyond difficulties in receiving medical care, lack of vehicle ownership has been associated with increased food insecurity [39], which itself is a risk for cardiovascular disease [40].
Socioeconomically deprived neighborhoods are less likely to have access to safe green outdoor spaces [11], which have been associated with increased physical activity, reduced levels of stress, and increased longevity [41]. Individuals who lack the transportation needed to escape to outdoor recreation areas may endure increased environmental stress in the form of neighborhood violence, noise, and pollution, all of which predispose these individuals to poor health outcomes [42,43]. These environmental stressors can also combine to diminish a person's ability to sustain health-promoting behaviors [44], which can be particularly harmful for patients with existing ischemic heart disease.
Decades of exclusionary housing practices, along with other forms of institutional racism, have created racially and ethnically segregated neighborhoods that persist throughout the United States [45]. Black Americans are more likely to live in neighborhoods with fewer employment opportunities, lower household income, worse access to quality education, and worse housing quality [46]. It has been well established that Black Americans are at increased risk for cardiovascular disease as well as for worse outcomes after MI [42,47,48]. This increased risk has been found to be largely attributable to the presence of greater cardiovascular disease risk factors [48,49] that are directly related to disparities in socioeconomic status [42,47,48]. The finding that Black patients living in neighborhoods with lower vehicle ownership had higher mortality than White patients living in similar neighborhoods but that there was no mortality difference between Black and White patients living in neighborhoods with higher vehicle ownership is consistent with these prior findings. This study suggests that providing certain high-risk patients with transportation after MI can have a meaningful impact on patient outcomes and additional research to identify these high-risk patients is certainly needed.
This study is inherently limited by the potential for confounding variables given its observational design. This study is also limited by needing to exclude patients who did not have a permanent address on file at the time of hospitalization. The inclusion of only KPSC members may reduce the overall generalizability of the study but it is reasonable to believe that these findings would be amplified in a less-well-insured cohort. Additionally, grouping patients into White, Black, Hispanic, and Asian subgroups does not account for the broad spectrum of ancestral diversity within each of these groups but limitations as to how data is captured within the electronic health record prevented a more thorough assessment of ancestry.
5. Conclusion
Living in a neighborhood with lower vehicle ownership was associated with increased mortality after myocardial infarction, even after adjusting for differences in household income. Black patients living in neighborhoods with lower vehicle ownership had a higher mortality after myocardial infarction than White patients living in neighborhoods with lower vehicle ownership. However, Black patients living in neighborhoods with higher vehicle ownership had no worse mortality than their White counterparts. These findings highlight the important role that transportation plays in determining health status among individuals with ischemic heart disease, particularly among Black individuals.
Statement of authorship
Jesse J Goitia Jr MD: Designed the study, performed statistical analysis, drafted the manuscript. James Onwuzurike MD: edited and revised the manuscript. Aiyu Chen MPH: performed statistical analysis. Yi-Lin Wu MS: performed statistical analysis. Albert Yuh-Jer Shen MD: edited and revised the manuscript. Ming-Sum Lee MD, PhD: collected data, performed statistical analysis, provided final review.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.ajpc.2023.100500.
Appendix. Supplementary materials
References
- 1.Fihn S.D., Gardin J.M., Abrams J., et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation. 2012;126(25):e354–e471. doi: 10.1161/CIR.0b013e318277d6a0. [DOI] [PubMed] [Google Scholar]
- 2.Syed S.T., Gerber B.S., Sharp L.K. Traveling towards disease: transportation barriers to health care access. J Community Health. 2013;38(5):976–993. doi: 10.1007/s10900-013-9681-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kripalani S., Henderson L.E., Jacobson T.A., Vaccarino V. Medication use among inner-city patients after hospital discharge: patient-reported barriers and solutions. Mayo Clin Proc. 2008;83(5):529–535. doi: 10.4065/83.5.529. [DOI] [PubMed] [Google Scholar]
- 4.Levine D.A., Kiefe C.I., Howard G., Howard V.J., Williams O.D., Allison J.J. Reduced medication access: a marker for vulnerability in US stroke survivors. Stroke. 2007;38(5):1557–1564. doi: 10.1161/STROKEAHA.106.478545. [DOI] [PubMed] [Google Scholar]
- 5.Musey V.C., Lee J.K., Crawford R., Klatka M.A., McAdams D., Phillips L.S. Diabetes in urban African-Americans. I. Cessation of insulin therapy is the major precipitating cause of diabetic ketoacidosis. Diabetes Care. 1995;18(4):483–489. doi: 10.2337/diacare.18.4.483. [DOI] [PubMed] [Google Scholar]
- 6.Welty T.E., Willis S.L., Welty E.A. Effect of limited transportation on medication adherence in patients with epilepsy. J Am Pharm Assoc. 2003;50(6):698–703. doi: 10.1331/JAPhA.2010.09081. [DOI] [PubMed] [Google Scholar]
- 7.Chaiyachati K.H., Hubbard R.A., Yeager A., et al. Association of Rideshare-Based Transportation Services and Missed Primary Care Appointments: a Clinical Trial. JAMA Intern Med. 2018;178(3):383–389. doi: 10.1001/jamainternmed.2017.8336. [DOI] [PubMed] [Google Scholar]
- 8.Silver D., Blustein J., Weitzman B.C. Transportation to clinic: findings from a pilot clinic-based survey of low-income suburbanites. J Immigr Minor Health. 2012;14(2):350–355. doi: 10.1007/s10903-010-9410-0. [DOI] [PubMed] [Google Scholar]
- 9.Wiig K., Smith C. The art of grocery shopping on a food stamp budget: factors influencing the food choices of low-income women as they try to make ends meet. Public Health Nutr. 2009;12(10):1726–1734. doi: 10.1017/S1368980008004102. [DOI] [PubMed] [Google Scholar]
- 10.Daniel H., Bornstein S.S., Kane G.C., et al. Addressing Social Determinants to Improve Patient Care and Promote Health Equity: an American College of Physicians Position Paper. Ann Intern Med. 2018;168(8):577–578. doi: 10.7326/M17-2441. [DOI] [PubMed] [Google Scholar]
- 11.Nesbitt L., Meitner M.J., Girling C., Sheppard S.R.J., Lu Y. Who has access to urban vegetation? A spatial analysis of distributional green equity in 10 US cities. Landsc Urban Plan. 2019;181:51–79. [Google Scholar]
- 12.Kind A.J.H., Buckingham W.R. Making Neighborhood-Disadvantage Metrics Accessible - The Neighborhood Atlas. N Engl J Med. 2018;378(26):2456–2458. doi: 10.1056/NEJMp1802313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fairfield K.M., Black A.W., Ziller E.C., et al. Area Deprivation Index and Rurality in Relation to Lung Cancer Prevalence and Mortality in a Rural State. JNCI Cancer Spectr. 2020;4(4):pkaa011. doi: 10.1093/jncics/pkaa011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sheets L.R., Henderson Kelley, Scheitler-Ring K., et al. An index of geospatial disadvantage predicts both obesity and unmeasured body weight. Prev Med Rep. 2020;18 doi: 10.1016/j.pmedr.2020.101067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Diez Roux A.V., Merkin S.S., Arnett D., et al. Neighborhood of residence and incidence of coronary heart disease. N Engl J Med. 2001;345(2):99–106. doi: 10.1056/NEJM200107123450205. [DOI] [PubMed] [Google Scholar]
- 16.Tonne C., Schwartz J., Mittleman M., Melly S., Suh H., Goldberg R. Long-term survival after acute myocardial infarction is lower in more deprived neighborhoods. Circulation. 2005;111(23):3063–3070. doi: 10.1161/CIRCULATIONAHA.104.496174. [DOI] [PubMed] [Google Scholar]
- 17.Goitia J.J., Jr., Phan D.Q., Schweis F., et al. Neighborhood Resources and Racial/Ethnic Differences in Survival After Myocardial Infarction. J Am Coll Cardiol. 2021;78(6):632–633. doi: 10.1016/j.jacc.2021.06.007. [DOI] [PubMed] [Google Scholar]
- 18.Singh G.K. Area deprivation and widening inequalities in US mortality, 1969-1998. Am J Public Health. 2003;93(7):1137–1143. doi: 10.2105/ajph.93.7.1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Butler D.C., Petterson S., Phillips R.L., Bazemore A.W. Measures of social deprivation that predict health care access and need within a rational area of primary care service delivery. Health Serv Res. 2013;48(2 Pt 1):539–559. doi: 10.1111/j.1475-6773.2012.01449.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.UCLA Center for Neighborhood Knowledge. California Disparities Mapping Tool. Downloaded from https://knowledge.luskin.ucla.edu/2541-2/August11, 2022. Accessed.
- 21.Razon N., Gottlieb L. Content Analysis of Transportation Screening Questions in Social Risk Assessment Tools: are We Capturing Transportation Insecurity? J Am Board Fam Med. 2022;35(2):400–405. doi: 10.3122/jabfm.2022.02.210256. [DOI] [PubMed] [Google Scholar]
- 22.Marcus A.C., Crane L.A., Kaplan C.P., et al. Improving adherence to screening follow-up among women with abnormal Pap smears: results from a large clinic-based trial of three intervention strategies. Med Care. 1992;30(3):216–230. doi: 10.1097/00005650-199203000-00004. [DOI] [PubMed] [Google Scholar]
- 23.Melnikow J., Paliescheskey M., Stewart G.K. Effect of a transportation incentive on compliance with the first prenatal appointment: a randomized trial. Obstet Gynecol. 1997;89(6):1023–1027. doi: 10.1016/s0029-7844(97)00147-6. [DOI] [PubMed] [Google Scholar]
- 24.Shekelle P.G., Begashaw M.M., Miake-Lye I.M., Booth M., Myers B., Renda A. Effect of interventions for non-emergent medical transportation: a systematic review and meta-analysis. BMC Public Health. 2022;22(1):799. doi: 10.1186/s12889-022-13149-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Erskine N.A., Waring M.E., McManus D.D., Lessard D., Kiefe C.I., Goldberg R.J. Barriers to Healthcare Access and Long-Term Survival After an Acute Coronary Syndrome. J Gen Intern Med. 2018;33(9):1543–1550. doi: 10.1007/s11606-018-4555-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lewey J., Choudhry N.K. The current state of ethnic and racial disparities in cardiovascular care: lessons from the past and opportunities for the future. Curr Cardiol Rep. 2014;16(10):530. doi: 10.1007/s11886-014-0530-3. [DOI] [PubMed] [Google Scholar]
- 27.Skinner J., Chandra A., Staiger D., Lee J., McClellan M. Mortality after acute myocardial infarction in hospitals that disproportionately treat black patients. Circulation. 2005;112(17):2634–2641. doi: 10.1161/CIRCULATIONAHA.105.543231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ludwig J., Sanbonmatsu L., Gennetian L., et al. Neighborhoods, obesity, and diabetes–a randomized social experiment. N Engl J Med. 2011;365(16):1509–1519. doi: 10.1056/NEJMsa1103216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hu J., Kind A.J.H., Nerenz D. Area Deprivation Index Predicts Readmission Risk at an Urban Teaching Hospital. Am J Med Qual. 2018;33(5):493–501. doi: 10.1177/1062860617753063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Branch L.G., Nemeth K.T. When elders fail to visit physicians. Med Care. 1985;23(11):1265–1275. doi: 10.1097/00005650-198511000-00005. [DOI] [PubMed] [Google Scholar]
- 31.Canupp K.C., Waites K.B., DeVivo M.J., Richards J.S. Predicting compliance with annual follow-up evaluations in persons with spinal cord injury. Spinal Cord. 1997;35(5):314–319. doi: 10.1038/sj.sc.3100367. [DOI] [PubMed] [Google Scholar]
- 32.Fitzpatrick A.L., Powe N.R., Cooper L.S., Ives D.G., Robbins J.A. Barriers to health care access among the elderly and who perceives them. Am J Public Health. 2004;94(10):1788–1794. doi: 10.2105/ajph.94.10.1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sarnquist C.C., Soni S., Hwang H., Topol B.B., Mutima S., Maldonado Y.A. Rural HIV-infected women's access to medical care: ongoing needs in California. AIDS Care. 2011;23(7):792–796. doi: 10.1080/09540121.2010.516345. [DOI] [PubMed] [Google Scholar]
- 34.Cunningham W.E., Andersen R.M., Katz M.H., et al. The impact of competing subsistence needs and barriers on access to medical care for persons with human immunodeficiency virus receiving care in the United States. Med Care. 1999;37(12):1270–1281. doi: 10.1097/00005650-199912000-00010. [DOI] [PubMed] [Google Scholar]
- 35.Guidry J.J., Aday L.A., Zhang D., Winn R.J. Transportation as a barrier to cancer treatment. Cancer Pract. 1997;5(6):361–366. [PubMed] [Google Scholar]
- 36.Salloum R.G., Smith T.J., Jensen G.A., Lafata J.E. Factors associated with adherence to chemotherapy guidelines in patients with non-small cell lung cancer. Lung Cancer. 2012;75(2):255–260. doi: 10.1016/j.lungcan.2011.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hoffmann R.L., Rohrer W.M., 3rd, South-Paul J.E., Burdett R., Watzlaf V.J. The effects of barriers on Health Related Quality of Life (HRQL) and compliance in adult asthmatics who are followed in an urban community health care facility. J Community Health. 2008;33(6):374–383. doi: 10.1007/s10900-008-9108-6. [DOI] [PubMed] [Google Scholar]
- 38.Rust G., Ye J., Baltrus P., Daniels E., Adesunloye B., Fryer G.E. Practical barriers to timely primary care access: impact on adult use of emergency department services. Arch Intern Med. 2008;168(15):1705–1710. doi: 10.1001/archinte.168.15.1705. [DOI] [PubMed] [Google Scholar]
- 39.Banks A.R., Bell B.A., Ngendahimana D., Embaye M., Freedman D.A., Chisolm D.J. Identification of factors related to food insecurity and the implications for social determinants of health screenings. BMC Public Health. 2021;21(1):1410. doi: 10.1186/s12889-021-11465-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liu Y., Eicher-Miller H.A. Food Insecurity and Cardiovascular Disease Risk. Curr Atheroscler Rep. 2021;23(6):24. doi: 10.1007/s11883-021-00923-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rojas-Rueda D., Nieuwenhuijsen M.J., Gascon M., Perez-Leon D., Mudu P. Green spaces and mortality: a systematic review and meta-analysis of cohort studies. Lancet Planet Health. 2019;3(11):e469–e477. doi: 10.1016/S2542-5196(19)30215-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Havranek E.P., Mujahid M.S., Barr D.A., et al. Social Determinants of Risk and Outcomes for Cardiovascular Disease: a Scientific Statement From the American Heart Association. Circulation. 2015;132(9):873–898. doi: 10.1161/CIR.0000000000000228. [DOI] [PubMed] [Google Scholar]
- 43.Akwo E.A., Kabagambe E.K., Harrell F.E., Jr, et al. Neighborhood Deprivation Predicts Heart Failure Risk in a Low-Income Population of Blacks and Whites in the Southeastern United States. Circ Cardiovasc Qual Outcomes. 2018;11(1) doi: 10.1161/CIRCOUTCOMES.117.004052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.August K.J., Billimek J. A theoretical model of how neighborhood factors contribute to medication nonadherence among disadvantaged chronically ill adults. J Health Psychol. 2016;21(12):2923–2933. doi: 10.1177/1359105315589391. [DOI] [PubMed] [Google Scholar]
- 45.Kershaw K.N., Osypuk T.L., Do D.P., De Chavez P.J., Diez Roux A.V. Neighborhood-level racial/ethnic residential segregation and incident cardiovascular disease: the multi-ethnic study of atherosclerosis. Circulation. 2015;131(2):141–148. doi: 10.1161/CIRCULATIONAHA.114.011345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kind A.J.H., Golden R.N. Social Determinants of Health: fundamental Drivers of Health Inequity. Wmj. 2018;117(5):231–232. [PubMed] [Google Scholar]
- 47.Bernheim S.M., Spertus J.A., Reid K.J., et al. Socioeconomic disparities in outcomes after acute myocardial infarction. Am Heart J. 2007;153(2):313–319. doi: 10.1016/j.ahj.2006.10.037. [DOI] [PubMed] [Google Scholar]
- 48.Graham G.N., Jones P.G., Chan P.S., Arnold S.V., Krumholz H.M., Spertus J.A. Racial Disparities in Patient Characteristics and Survival After Acute Myocardial Infarction. JAMA Netw Open. 2018;1(7) doi: 10.1001/jamanetworkopen.2018.4240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Graham G. Racial and Ethnic Differences in Acute Coronary Syndrome and Myocardial Infarction Within the United States: from Demographics to Outcomes. Clin Cardiol. 2016;39(5):299–306. doi: 10.1002/clc.22524. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.