Abstract
Objective
Rabies is a neglected zoonotic disease that can infect all mammals, including humans. We aimed to summarise the current knowledge of the incidence, risk factors and mortality of rabies in Southeast Asia.
Design
Systematic review based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses 2020.
Data sources
Scopus, Web of Science and PubMed were searched from 1 January 2012 to 21 February 2023.
Eligibility criteria
Original English language articles published between 2012 and 2023 were included.
Data extraction and synthesis
Nine independent reviewers extracted data and assessed the risk of bias. The quality appraisal of included articles was carried out using the Mixed Methods Appraisal Tool.
Results
A total of eight articles were included in this analysis. In Vietnam, the incidence of rabies ranged from 1.7 to 117.2 per 100 000 population. The cumulative incidence in Sarawak was estimated at 1.7 per 100 000 population. In Indonesia, 104 human rabies cases were reported from 2008 to 2010, while in Thailand, a total of 46 rabies cases were reported in Thailand from 2010 to 2015. In the Philippines, the incidence of rabies ranged from 0.1 to 0.3 per 100 000 population. An increased risk of rabies virus infection was associated with a high population density, illiteracy, seasonal patterns and dog butchers. The case fatality rate was 100%.
Conclusion
This study included research from Southeast Asia, which may not represent rabies infection in other regions or continents. In addition, the role of publication bias should be acknowledged as grey literature was not included. The occurrence of rabies in Southeast Asia is due to the high number of unvaccinated stray and pet dogs, working hazards (dog butchers in Vietnam), the unavailability of the rabies vaccine in rural regions and misinformation about the significance of seeking treatment after dog bites.
PROSPERO registration number
CRD42022311654.
Keywords: epidemiology, epidemiology, public health, systematic review
STRENGTHS AND LIMITATIONS OF THIS STUDY.
This review only includes research from Southeast Asia, which may not represent rabies infection in other regions or continents.
We did not include grey literature or national guidelines, which could have been useful in this study.
The inclusion of studies that defined or diagnosed rabies based on clinical signs or laboratory tests increased the chances of identifying rabies cases in Southeast Asian countries.
Introduction
Rabies is a neglected zoonotic disease caused by an RNA virus from the family Rhabdoviridae, genus Lyssavirus.1 Once clinical symptoms appear, rabies is almost 100% fatal.2 All mammals can be infected with the rabies virus, including humans. More than 99% of human rabies cases are transmitted via dogs.3 With the necessary evidence and tools in place for the control and elimination of rabies, canine rabies can be eliminated, as demonstrated in Western Europe, Canada, the USA, Japan, a few Latin American countries and many parts of Asia. However, rabies is still widespread, occurring in more than 80 countries, particularly low/middle-income countries in Africa and Asia.3 4 Furthermore, half of the global population lives in canine rabies-endemic areas and hence is at risk of contracting rabies.3
Globally, canine rabies is estimated to cause approximately 59 000 human deaths annually. In Asia, rabies is clearly a major problem: the number of human deaths due to rabies in Asia is higher than in any other region in the world. Most human rabies deaths occur in Asia (59.6%), followed by Africa (36.4%), while only less than 0.05% of human rabies deaths occur in the Americas. In addition, India alone accounts for 35% of global human rabies deaths, higher than any other country.4 In Asia, canine rabies is estimated to cause a loss of 2.2 million disability-adjusted life-years per year, while the annual cost of postexposure prophylaxis (PEP) is highest in Asia, estimated at up to US$1.5 billion.5
In Southeast Asia, only Singapore has eradicated canine rabies through the implementation of robust national rabies control programmes, while other countries in this subregion are not considered rabies-free.6 Malaysia was declared rabies-free by the World Organisation for Animal Health in July 2013, but several rabies outbreaks since 2015 have caused Malaysia to lose its rabies-free status.7 Even though Thailand and Vietnam have not been able to eliminate rabies, there has been a substantial reduction in human rabies deaths through the implementation of dog mass vaccination, intensified PEP in humans and awareness education.8
Rabies is 100% preventable through vaccination in animals and humans.9 The WHO has recommended pre-exposure prophylaxis for those with continual, frequent or increased risk of exposure to rabies virus (eg, veterinarians and animal handlers). If exposed to a rabid animal, the WHO recommends PEP, which consists of immediate wound management, immediate vaccination and the administration of rabies immunoglobulin for high-risk exposures.10 Nevertheless, dog vaccination is considered the most cost-effective strategy for preventing rabies in humans.2
Despite the availability of evidence and guidelines for the control and management of rabies, countries in Southeast Asia face some constraints in controlling rabies, including inadequate resources, lack of political commitment, lack of consensus on strategy, weak intersectoral coordination, insensitive surveillance systems, limited accessibility to modern rabies vaccines and supply problems, as well as a lack of public awareness and cooperation.8 However, the high estimated burden of rabies more than justifies the need to prioritise rabies control, particularly in Asian countries.
Information on rabies epidemiology is a prerequisite for the effective planning of rabies control programmes. Previous systematic reviews focused on rabies epidemiology in India,11 Nepal1 and Arab countries,12 while literature synthesising data on rabies epidemiology in Southeast Asia is limited. Hence, this systematic review aims to provide an in-depth assessment of the incidence, risk factors and mortality of rabies in Southeast Asian countries, based on the published literature.
Materials and methods
This systematic review was registered with the PROSPERO database (CRD42022311654) and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 statement.13 A meta-analysis was not carried out as the included studies differed in terms of methodology, settings, participants, interventions and outcomes, suggesting heterogeneity. An internal protocol was developed to document the criteria for conducting this systematic review, but this is not published.
Patient and public involvement
There was no patient and/or public involvement in this study (none).
Research question formulation
The review question was developed based on the CoCoPop (condition, context, population) and PEO (population, exposure, outcome) concepts.14 The population, intervention, comparison intervention, outcome measures framework is commonly used to develop focused clinical questions for quantitative reviews,15 while the CoCoPop and PEO concepts are suitable for reviews related to prevalence and aetiology.14 Based on the CoCoPop concept, the condition refers to the incidence of rabies, the context refers to Southeast Asia and the population is the general population. Based on the PEO concept, the population refers to the general population in Southeast Asia, the exposure refers to rabies and the outcome is the mortality caused by rabies. Hence, the main research questions are (1) What is the incidence of rabies among the general population in Southeast Asian countries? (2) What are the risk factors of rabies among the general population in Southeast Asian countries? and (3) What is the mortality rate of rabies among the general population in Southeast Asian countries?
Data source and search strategy
PubMed, Web of Science and Scopus were searched from 1 January 2012 to 21 February 2023. The keywords used to search for related articles are provided in table 1.
Table 1.
Keywords search used in the screening process
| Database | Search string |
| Scopus |
|
| Web of Science |
|
| PubMed |
|
Study selection
The inclusion criteria were (1) publications from 2012 to 2023, (2) original articles and (3) publications in the English language. The following types of studies were included in this review: (1) reports on the incidence and risk factors of rabies in Southeast Asia and (2) reports on the mortality rate of rabies in Southeast Asia. Non-original articles such as conference proceedings, perspectives, commentaries, opinions, reports, systematic reviews and meta-analyses were excluded. The publication period was limited to 2012–2023 so that the systematic review could be built on recent literature.
Data extraction and synthesis
Duplicates were deleted, and at least two reviewers rescreened the remaining papers. Before their inclusion in the review, articles were screened in three stages. Any article that did not meet the inclusion criteria based on title screening was eliminated in the first phase. The abstracts of the remaining papers were reviewed in the second phase, and any publications that did not fit the inclusion criteria were eliminated from the review. The full-text articles were examined attentively in the last phase to eliminate any papers that did not fulfil the inclusion criteria. Before the data extraction process, both reviewers needed to agree that the entire publication should be reviewed. Any disagreements were worked out through discussion. All data extraction was conducted independently using a standardised data extraction form that was organised using Microsoft Excel. Information collected in the form included (1) author, (2) publication year, (3) reference, (4) country, (5) study design, (6) statistical analysis and (7) results, which included incidence, risk factors and mortality. Due to the heterogeneity of the included studies, narrative synthesis was performed.
Quality assessment
Quality assessment was conducted by the authors on all eight studies using the Mixed Methods Appraisal Tool (MMAT).16 The MMAT is a critical appraisal tool that was developed to appraise studies included in systematic mixed study reviews. The quality of the methodology of five categories of studies (qualitative studies, randomised controlled trials, non-randomised studies, quantitative descriptive studies and mixed methods studies) can be appraised using this tool. For each category, five criteria are used to assess the quality of the study. It is advised not to calculate an overall score from the rating of each criterion using the latest version of MMAT16. However, due to problems faced by researchers in reporting the MMAT results, a suggestion was provided for reporting an overall score (5*****/100% of the quality criteria met, 4****/80% of the quality criteria met; 3***/60% of the quality criteria met; 2**/40% of the quality criteria met; 1*/20% of the quality criteria met). The details of this assessment are reported in table 2.
Table 2.
The details of Mixed Methods Appraisal Tool assessment
| Author | Type of study | Score | 1.1 | 1.2 | 1.3 | 1.4 | 1.5 |
| Is the sampling strategy relevant to address the research question? | Is the sample representative of the target population? | Are the measurements appropriate? | Is the risk of non-response bias low? | Is the statistical analysis appropriate to answer the research question? | |||
| Nguyen et al31 | Quantitative | 40% | Can’t tell | Can’t tell | Yes | Can’t tell | Yes |
| Pham et al30 | Quantitative | 100% | Yes | Yes | Yes | Yes | Yes |
| Sim et al27 | Quantitative | 60% | Yes | Can’t tell | Yes | Can’t tell | Yes |
| Yurachai et al34 | Quantitative | 80% | Yes | Yes | Yes | Can’t tell | Yes |
| Phung et al29 | Quantitative | 80% | Yes | Yes | Yes | Can’t tell | Yes |
| Susilawati et al33 | Quantitative | 80% | Yes | Yes | Yes | Yes | No |
| Lee et al32 | Quantitative | 100% | Yes | Yes | Yes | Yes | Yes |
| Guzman et al28 | Quantitative | 80% | Yes | Yes | Yes | No | Yes |
Results
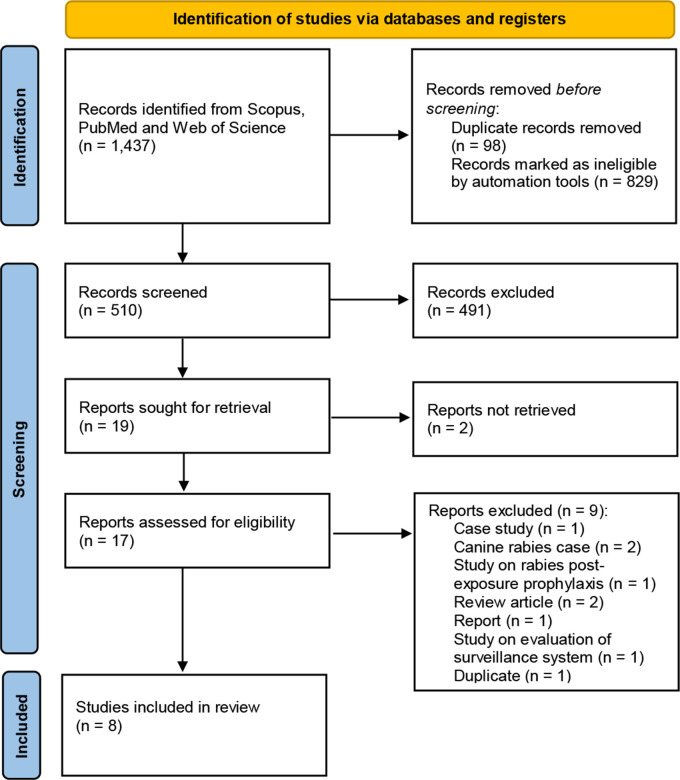
A total of 1437 records were identified from the 3 databases to evaluate the incidence, risk factors and mortality rate of rabies in Southeast Asia. Using automation tools, 829 records were excluded based on year, publication type and language. A total of 98 duplicate records were found and removed, leaving 510 records for title screening. The titles and abstracts were screened independently based on the review questions. A total of 491 articles were removed during the screening. For the remaining 19 articles, the full text was retrieved for assessment of eligibility. Disagreements were resolved through discussion to reach a consensus. Eleven articles were removed for the following reasons: they did not meet the objective (n=4),17–20 they were not primary/original research articles (n=4),21–24 the full article could not be retrieved (n=2)25 26 and they were duplicates (n=1),27 leaving a total of eight articles for proceeding with the quality appraisal. The PRISMA flow chart is presented in figure 1.
Figure 1.
PRISMA 2020 flow diagram for new systematic reviews that included searches of databases. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Quality appraisal
According to the MMAT evaluation criteria, 75% of the articles (n=6) met 75%–100% of the MMAT checklist, representing high quality. Of the articles, 12.5% (n=1) met 50%–75% of the evaluated criteria, representing moderate quality, while 12.5% of the articles (n=1) met less than 50% of the evaluated criteria, representing low quality.
Background of the eligible studies
A total of eight studies were included in this systematic review, of which four were conducted in Vietnam, and one each in Indonesia, Malaysia, Thailand and the Philippines (online supplemental table). The themes covered by all studies included incidence rates, case numbers and risk factors of rabies in Southeast Asia. Among the included studies, three studies particularly discussed rabies mortality.
bmjopen-2022-066587supp001.pdf (85.8KB, pdf)
Incidence and risk factors of rabies in Southeast Asian countries
Overall, the incidence of rabies ranged between 0.1 per 100 000 population in the Philippines28 and 117.2 per 100 000 population in Vietnam.18 The average monthly number of rabies cases in Vietnam was 429 during the period from 2011 to 2015, with the incidence ranging from 1.7 to 117.2 per 100 000, with higher incidences observed in the Red River, South Central Coast (SCC) and Mekong River Delta (MRD) regions.29 Specific to Southern Vietnam, a total of 94 human rabies cases were reported between 2009 and 2018, with an average of nine cases recorded annually, representing an incidence of 2.7 cases per 10 million population.30 The highest number was reported in 2018 (5.5 cases per 10 million population). Most cases were among men and individuals aged 50 years and above.
Dog butchers in Vietnam were at high risk of rabies virus infection.31 The study found that 28.3% of butchers were at risk of rabies exposure due to the slaughtering of sick dogs and getting bites, scratches or knife cuts. Of 406 participants, 8.6% had sufficient levels of rabies neutralising antibody for protection and only 8.1% were vaccinated. In terms of location, rabies cases were limited to specific areas. Hotspots were identified in southern Vietnam, particularly in the MRD and SCC.32 Seasonal patterns were observed, with a strong peak in February/July and a minor peak in October/December in the MRD region. However, a strong peak was detected in the middle of each year in the SCC. Temperature, humidity and cumulative rainfall are positively associated with an increased incidence of rabies in Vietnam. In terms of socioeconomic factors, increases in population density, as well as the percentage of illiteracy, elevated the risk of rabies.29
In Indonesia, 104 human rabies cases were reported in Bali from November 2008 to November 2010. Most of the cases were among men. Almost all (92%) cases had a history of a dog bite. Only 5.8% had their wounds treated and received an antirabies vaccine after the bite incident.33 Even worse, rabies cases in Sibu, Sarawak, also did not seek medical attention following a dog bite.27 The cumulative incidence in Sibu was estimated at 1.7 per 100 000 population. The incubation period varied from 17 days to 2 years.
A total of 46 confirmed and probable cases of human rabies were reported in Thailand from 2010 to 2015, of which 11 were reported in Eastern Thailand.34 Even though rabies can be prevented by vaccination, more than 90% of rabies death cases in Thailand did not receive or improperly stopped receiving PEP. In terms of suspected rabies exposures, 6204 exposures were reported from 8 provinces in Eastern Thailand, resulting in a crude exposure rate of 106 reported rabies exposures per 100 000 people. Dogs were the main source of exposure (77.8%), while children under the age of 15 and older persons over the age of 60 had the highest overall reported exposure rates (189.7 and 189.2/100 000, respectively).
In the Philippines, there were 575 rabies cases from 2006 to 2015, of which 70% were among men. Nearly 34% of the patients were aged 41–60 years. The incidence rate of human rabies per 100 000 population in 2007, 2010 and 2015 was 0.1305, 0.1356 and 0.1708 in the National Capital Region; 0.2890, 0.2965 and 0.1961 in Region III; and 0.1449, 0.1272 and 0.1041 in Region IV–A, respectively.28
Rabies mortality in Southeast Asian countries
The case fatality rate was 100% as mentioned in 2 studies.27 33 Of the six deaths reported in Sibu, five patients succumbed to the illness within 2 weeks of symptom onset, with five out of the six cases reporting a dog bite history.23 In Indonesia, Susilawati et al33 reported 104 fatalities due to rabies, of which 96 cases had a history of dog bites.22 In the Philippines, 463 people died from rabies infection.28
Discussion
Incidence and risk factors of rabies in Southeast Asian countries
Rabies in Asia and Africa contributes to over 99% of the human rabies deaths that occur in the world today. The vast majority (60%) of these deaths occur in Asia.35 Every year, an estimated 59 000 people die from rabies worldwide, with the majority (95%) of these deaths occurring in Africa and Asia due to a lack of PEP services for animal-bite patients and rabies surveillance personnel and facilities.36 These statistics support the results of our study, which shows the reporting of a high number of rabies cases in Vietnam, Indonesia and Thailand, which are endemic for rabies.37
Rabies is concentrated in Asia and Southeast Asia because it is frequently neglected when health and agriculture budgets are set, although the costs and economic benefits of implementing rabies prevention programmes have been successfully established in high-income countries.38 The high number of rabies cases in Southeast Asia can also be attributed to the high number of unowned, free-roaming dogs that cannot be controlled without considerable effort and thus are not vaccinated.39 Vaccination programmes for dogs can provide herd immunity and break the rabies transmission cycle in this reservoir species and have been successfully applied in several countries around the world.40
Another cause of the high incidence of rabies in Southeast Asia is the working hazards of dog butchers, especially in countries that have legalised dog consumption, such as Vietnam.41 The Centers for Disease Control and Prevention also reported the illegal trafficking of dogs for human consumption in Vietnam (https://www.cdc.gov/globalhealth/stories/rabies_southeast_asia.htm), which could possibly contribute to the high incidence of rabies in Vietnam. Professional dog butchers in northern Vietnam are at a high risk of rabies virus infection due to exposure during the slaughtering process from the handling of sick or dead dogs and getting bitten, scratched or cut with knives. A study reported that 91.9% of professional dog butchers in Vietnam were not vaccinated against rabies, which may be because of fear of the side effects of the rabies vaccine, inability to afford vaccination and incorrect knowledge of rabies prevention.31
The rabies incidence of 0.1 per 100 000 population in the Philippines is similar to that reported in China in 2016.42 The lower rabies incidence in the Philippines compared with other Southeast Asian countries may be due to the implementation of theAnti-Rabies Act of 2007 to prevent and control human rabies.43 In addition, the consumption of dog meat was banned in 1998 with the implementation of the Animal Welfare Act, which may contribute to the lower incidence of rabies in the Philippines.44
Men are more likely to contract rabies infection than women.19 Similar findings were reported in Iraq, where more than 89% of rabies cases were among men.45 This can be attributed to the fact that most women are housewives, while men are engaged in outdoor activities.46 Another study in Ethiopia also stated that men are more likely to perform nightly and outdoor activities, while women are more likely to remain indoors for cultural and religious reasons,47 which could explain the increased incidence of rabies in men.
According to study a by Yurachai et al,34 rabies infection affects children more compared with other age groups.24 This corresponds to a WHO report, stating that 40% of rabies victims are children ages 4–15 (https://www.who.int/news-room/fact-sheets/detail/rabies). Other studies in Yemen and Iran reported similar findings, with nearly 40% of the individuals exposed to rabies infection falling in this age group.45 48 Children in this age group are probably more likely to play with, annoy or approach biting animals, which contributes to the higher rate of bites in this age group.45 In contrast, according to a study by Pham et al,30 older people are more likely to become infected with rabies.19
In several studies included in this systematic review, the diagnosis of most rabies cases was based only on detailed history and clinical diagnosis.17 19 21 To diagnose rabies in humans, multiple samples such as saliva, serum, spinal fluid and skin biopsies of hair follicles from the nape of the neck are analysed. Viral isolation or reverse transcription-PCR can be used to analyse saliva. Serum and spinal fluid are tested for rabies virus antibodies. Skin biopsies can be used to detect rabies antigens in the cutaneous nerves at the base of the hair follicles (https://www.cdc.gov/rabies/diagnosis/animals-humans.html). In the future, low/middle-income countries need to standardise the diagnosis of rabies based on the laboratory tests mentioned above for the accuracy of the diagnosis and to enable comparison with other studies in developed countries.
Of the included studies, only one was conducted among butchers, who were at higher risk of contracting rabies.20 Apart from butchers, individuals working as veterinarians, veterinary technicians, animal control workers and wildlife rehabilitators were also considered to have a higher risk of contracting rabies than the general population.49 This calls for more studies incorporating individuals involved in occupations identified as high risk for rabies exposure and infection.
In this study, climate was postulated to be one of the risk factors for rabies infection. This was echoed by a study in China showing that the incidence of rabies increases with the ambient temperature. A warmer climate causes animals to be more active in their environment and to travel greater distances when tracking, which contributes to the spread of rabies. In addition, as temperatures rise, people tend to wear lighter clothing and expose more skin, which increases the likelihood of being bitten by a dog.50 In South Korea, the seasonality of wildlife rabies was attributed to behaviours such as searching for food during the winter or early spring. Dogs may thus have more opportunities to come into contact with rabid animals during this period due to greater animal movement, which could contribute to seasonal patterns in the occurrence of rabies in humans.51
Rabies mortality in Southeast Asian countries
In this study, rabies had a high fatality rate, with 100% of the infected cases dying. This is supported by a review in Africa by Nyasulu et al, who reported that Algeria, Namibia, Eswatini (formerly Swaziland), Tunisia, Uganda, Zambia and Zimbabwe had high morbidity and mortality due to rabies, with 563 cases (33.9% deaths), 269 cases (94% deaths), 62 cases (88.7% deaths), 91 cases (90% deaths), 466 cases (40.9% deaths), 207 cases (32.8% deaths) and 114 cases (80.7% deaths), respectively.52 Because of the large population of stray dogs in this area, the chances of being bitten by a dog are high. Not only are the chances of being bitten high in these areas, but access to treatment in a timely and adequate manner is also very limited. Rabies vaccines may not be routinely available in rural areas where most exposures occur, and rabies immunoglobulins, which are required for category III bites, are always in short supply.53
These factors significantly contribute to the high mortality rate, as the highly protective rabies vaccine is frequently unavailable in these poor areas. In addition, the public is often unconcerned and unaware of the need for early treatment after being bitten by dogs.54 According to recent studies, many rabies victims contracted the disease owing to neglect, ignorance or a lack of primary healthcare facilities.55 Thus, health promotion and education should be given to the public as knowledge regarding rabies is essential to reduce morbidity and mortality.5
In high-income countries such as the USA, the incidence of rabies and associated mortality is low. In the last decade, there have been only 25 cases of human rabies reported in the USA (2009–2018), with 23 deaths.6 The low number of cases of rabies infection is due to successful animal control and vaccination programmes, successful outreach programmes, public health capacity and laboratory diagnostics and the availability of modern rabies biologics.56 Even though rabies is preventable, the exorbitant cost of vaccinations, combined with a lack of education and knowledge about the disease, limits PEP use.55
Strengths and limitations
In this study, we only included research from Southeast Asia, which may not represent rabies infection in other regions or continents. We did not include grey literature or national guidelines, which could have been useful in this study. Nevertheless, the strength of this review lies in its inclusion of studies that defined or diagnosed rabies based on either clinical signs or laboratory testing. Given that rabies is often diagnosed clinically, especially in low/middle-income countries,57 this process increased the chances of identifying rabies cases in Southeast Asian countries.
Recommendations
A successful rabies prevention and control programme requires integrating and strengthening intersectoral and transdisciplinary collaboration and cooperation among various societal components.58 The Association of Southeast Asian Nations Rabies Elimination Strategy places great value on the organisational and One Health frameworks for rabies eradication. The single most significant way to deal with rabies concerns is to eliminate dog-mediated rabies. The requirement for PEP is considerably reduced when dog rabies is eradicated.59 To benefit from the synergy and maximisation of shared resources, comprehensive rabies control programmes should involve the combination of human, financial and material resources with other disease programmes.35
Mass canine vaccination campaigns will boost herd immunity and reduce the risk of human rabies exposure, but this will need strong governmental commitment and extensive social mobilisation. The veterinary authority’s active engagement in animal rabies control at the national level is critical, and it is their social responsibility to prevent human rabies through well-planned dog rabies control programmes.37 In 1983, the Pan American Health Organization initiated an elimination programme for human rabies transmitted by dogs that was mainly based on the mass immunisation of dogs; this has led to a 90% reduction in dog rabies in Chile and other Latin American countries.60
Rabies control and elimination in low endemic rabies countries such as Malaysia and Singapore have been made possible by the strict enforcement of dog registration, vaccination and population management measures. Malaysia shares a border with Thailand, and the notion of an immunological belt has been developed through dog licensing, required vaccination of dogs and the systematic extermination of unvaccinated dogs in a buffer zone to prevent rabies from entering the country.37 Perhaps other middle and high endemic rabies countries could follow this rabies control strategy implemented by their Southeast Asian neighbour.
Public information and education are important to increase awareness and enhance community participation and support in rabies prevention programmes. Dissemination of important information such as the high fatality rate of rabies, its epidemiology, its prevention and control, and the disease control programme, in general, is vital for programme implementation and responsible pet ownership. By recognising rabies’ influence on people’s daily lives and the fact that dogs can be a source of human infection, community and school-based rabies prevention initiatives will be easier to establish.61
The involvement of stakeholders is crucial, and by bringing together key stakeholders from the corporate and public sectors, health security and the need to form public–private partnerships, which are critical in rabies prevention programmes, can be addressed.62 National government agencies can maintain standardised approaches for rabies management and elimination and advocate on how to begin public–private cooperation to ensure long-term intervention. All stakeholders can benefit from such technical and administrative effort as they provide credibility and quality assurance to the prevention programme’s effectiveness.35 Various examples of public–private partnerships that aid in implementing public programmes, research and policy formation can be seen in Indonesia, India, Sri Lanka, the Philippines, Thailand and Vietnam.3
Conclusion
Rabies has often been neglected and not given priority in terms of funding for prevention programmes, resulting in the continued presence of rabies cases in Southeast Asia despite the endorsement of multiple programmes by the WHO. The high number of unvaccinated stray and pet dogs, working hazards (dog butchers in Vietnam), unavailability of the rabies vaccine in rural areas, as well as ignorance regarding the importance of seeking treatment after dog bites, are among the factors that contribute to rabies cases in Southeast Asia.
Supplementary Material
Acknowledgments
We would like to thank the Department of Community Health, Faculty of Medicine, National University of Malaysia, for their technical support.
Footnotes
Contributors: All authors, MYJL, AFNAH, DA, NR, MRH, SSSAR, MSJ, AO and AH, were involved in conceptualisation, methodology, extensive search of articles, critical review of articles, results synthesis and original draft write up. MRH supervised the manuscript preparation. All authors have read and agreed to the final draft of the manuscript. MRH is responsible for the overall content as the guarantor.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Not applicable.
References
- 1.Devleesschauwer B, Aryal A, Sharma BK, et al. Epidemiology, impact and control of rabies in Nepal: a systematic review. PLoS Negl Trop Dis 2016;10:e0004461. 10.1371/journal.pntd.0004461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization . WHO fact sheets: Rabies [Internet]. 2021. Available: https://www.who.int/news-room/fact-sheets/detail/rabies
- 3.World Health Organization . WHO expert consultation on rabies second report. World Health Organ Tech Rep Ser 2013:1–139. [PubMed] [Google Scholar]
- 4.Hampson K, Coudeville L, Lembo T, et al. Estimating the global burden of endemic canine rabies. PLoS Negl Trop Dis 2015;9:e0003709. 10.1371/journal.pntd.0003709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization . WHO expert consultation on rabies: third report. 2018. [Google Scholar]
- 6.Center for Disease Control and Prevention . Rabies status: assessment by country [Internet]. 2021. Available: https://www.cdc.gov/rabies/resources/countries-risk.html
- 7.Navanithakumar B, Sohayati A, Rohaiza Y, et al. An overview of rabies outbreaks in Malaysia, ordinances and laws. Malays J Vet Res (Putrajaya) 2019;10:148–58. [Google Scholar]
- 8.Ward MP. Review of rabies epidemiology and control in South, South East and East Asia: past, present and prospects for elimination. Zoonoses Public Health 2012;59:451–67. 10.1111/j.1863-2378.2012.01489.x [DOI] [PubMed] [Google Scholar]
- 9.Abela-Ridder B. Rabies: 100 per cent fatal, 100 per cent preventable. Vet Rec 2015;177:148–9. 10.1136/vr.h4196 [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization . Rabies vaccines: WHO position paper. Weekly Epidemiological Record = Relevé Épidémiologique Hebdomadaire 2010;85:309–20. [Google Scholar]
- 11.John D, Royal A, Bharti O. Burden of illness of dog-mediated rabies in India: a systematic review. Clinical Epidemiology and Global Health 2021;12:100804. 10.1016/j.cegh.2021.100804 [DOI] [Google Scholar]
- 12.Alaifan T, Altamimi A. A systematic review of epidemiology of rabies in Arab countries. J Health Inform Dev Ctries 2019;13. [Google Scholar]
- 13.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Munn Z, Stern C, Aromataris E, et al. What kind of systematic review should i conduct? A proposed typology and guidance for systematic reviewers in the medical and health sciences. BMC Med Res Methodol 2018;18:5. 10.1186/s12874-017-0468-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stern C, Al E, Sigurdson C, et al. Developing the review question and inclusion criteria tobacco and alcohol-relat ED Int ervent ions for people wit H mild/moderat E Int ellect ual disabilit ies: a SY. AJN The American Journal of Nursing 2014;114:53–6. 10.1097/01.NAJ.0000445689.67800.86 [DOI] [PubMed] [Google Scholar]
- 16.Hong QN, Fàbregues S, Bartlett G, et al. The mixed methods appraisal tool (MMAT) version 2018 for information professionals and researchers. EFI 2018;34:285–91. 10.3233/EFI-180221 [DOI] [Google Scholar]
- 17.Melyantono SE, Susetya H, Widayani P, et al. The rabies distribution pattern on dogs using average nearest neighbor analysis approach in the karangasem district, Bali, Indonesia, in 2019. Vet World 2021;14:614–24. 10.14202/vetworld.2021.614-624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lachica ZPT, Peralta JM, Diamante EO, et al. A cointegration analysis of rabies cases and weather components in davao City, Philippines from 2006 to 2017. PLoS ONE 2020;15:e0236278. 10.1371/journal.pone.0236278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tran CH, Afriyie DO, Pham TN, et al. Rabies post-exposure prophylaxis initiation and adherence among patients in Vietnam, 2014-2016. Vaccine 2019;37 Suppl 1:A54–63. 10.1016/j.vaccine.2019.01.030 [DOI] [PubMed] [Google Scholar]
- 20.Lawpoolsri S, Kaewkungwal J, Khamsiriwatchara A, et al. Data quality and timeliness of outbreak reporting system among countries in greater mekong subregion: challenges for international data sharing. PLoS Negl Trop Dis 2018;12:e0006425. 10.1371/journal.pntd.0006425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mu TT, Sein AA, Soe C, et al. Rabies in Myanmar: prevalent, preventable but not prioritized. Am J Trop Med Hyg 2017;97:989–91. 10.4269/ajtmh.17-0198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ward MP. Rabies in the Dutch East Indies a century ago – a spatio-temporal case study in disease emergence. Preventive Veterinary Medicine 2014;114:11–20. 10.1016/j.prevetmed.2014.01.009 [DOI] [PubMed] [Google Scholar]
- 23.Hemachudha P, Hemachudha T. Rabies: presentation, case management and therapy. J Neurol Sci 2021;424:117413. 10.1016/j.jns.2021.117413 [DOI] [PubMed] [Google Scholar]
- 24.Nguyen HTT, Tran CH, Dang AD, et al. Rabies vaccine hesitancy and deaths among pregnant and breastfeeding women-Vietnam, 2015-2016. MMWR Morb Mortal Wkly Rep 2018;67:250–2. 10.15585/mmwr.mm6708a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Purwo Suseno P, Rysava K, Brum E, et al. Lessons for rabies control and elimination programmes: a decade of one health experience from Bali, Indonesia. Rev Sci Tech 2019;38:213–24. 10.20506/rst.38.1.2954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nguyen HTT, Afriyie DO, Tran CH, et al. Progress towards rabies control and elimination in Vietnam. Rev Sci Tech 2019;38:199–212. 10.20506/rst.38.1.2953 [DOI] [PubMed] [Google Scholar]
- 27.Sim BNH, Liang BNW, Ning WS, et al. A retrospective analysis of emerging rabies: a neglected tropical disease in Sarawak, Malaysia. J R Coll Physicians Edinb 2021;51:133–9. 10.4997/JRCPE.2021.207 [DOI] [PubMed] [Google Scholar]
- 28.Guzman FD, Iwamoto Y, Saito N, et al. Clinical, epidemiological, and spatial features of human rabies cases in Metro Manila, the Philippines from 2006 to 2015. PLoS Negl Trop Dis 2022;16:e0010595. 10.1371/journal.pntd.0010595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Phung D, Nguyen HX, Nguyen HLT, et al. The effects of socioecological factors on variation of communicable diseases: a multiple-disease study at the National scale of Vietnam. PLoS ONE 2018;13:e0193246. 10.1371/journal.pone.0193246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pham QD, Phan LT, Nguyen TPT, et al. An evaluation of the rabies surveillance in southern Vietnam. Front Public Health 2021;9:610905. 10.3389/fpubh.2021.610905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nguyen AKT, Vu AH, Nguyen TT, et al. Risk factors and protective immunity against rabies in unvaccinated butchers working at dog slaughterhouses in northern Vietnam. Am J Trop Med Hyg 2021;105:788–93. 10.4269/ajtmh.20-1172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lee HS, Thiem VD, Anh DD, et al. Geographical and temporal patterns of rabies post exposure prophylaxis (pep) incidence in humans in the mekong river delta and southeast central coast regions in vietnam from 2005 to 2015. PLoS One 2018;13:e0194943. 10.1371/journal.pone.0194943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Susilawathi NM, Darwinata AE, Dwija IBNP, et al. Epidemiological and clinical features of human rabies cases in Bali 2008-2010. BMC Infect Dis 2012;12:81. 10.1186/1471-2334-12-81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yurachai O, Hinjoy S, Wallace RM. An epidemiological study of suspected rabies exposures and adherence to rabies post-exposure prophylaxis in eastern Thailand, 2015. PLoS Negl Trop Dis 2020;14:e0007248. 10.1371/journal.pntd.0007248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Miranda MEG, Miranda NLJ. Rabies prevention in Asia: institutionalizing implementation capacities. In: Rabies and rabies vaccines. Cham: Springer, 2020: 103–16. 10.1007/978-3-030-21084-7 [DOI] [Google Scholar]
- 36.Human rabies: 2016 updates and call for data. Wkly Epidemiol Rec 2017;92:77–86. [PubMed] [Google Scholar]
- 37.Gongal G, Wright AE. Human rabies in the who Southeast Asia region: forward steps for elimination. Adv Prev Med 2011;2011:383870. 10.4061/2011/383870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Knobel DL, Cleaveland S, Coleman PG, et al. Re-evaluating the burden of rabies in Africa and Asia. Bull World Health Organ 2005;83:360–8. [PMC free article] [PubMed] [Google Scholar]
- 39.Chanachai K, Wongphruksasoong V, Vos A, et al. Feasibility and effectiveness studies with oral vaccination of free-roaming dogs against rabies in Thailand. Viruses 2021;13:571. 10.3390/v13040571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schneider MC, Belotto A, Adé MP, et al. Current status of human rabies transmitted by dogs in Latin America. Cad Saude Publica 2007;23:2049–63. 10.1590/s0102-311x2007000900013 [DOI] [PubMed] [Google Scholar]
- 41.Nguyen TT, Hoang VT, Nguyen TH. Epidemiology of rabies in Vietnam, 2009–2011. J Prev Med (Wilmington) 2013;7:29–37. [Google Scholar]
- 42.Qi L, Su K, Shen T, et al. Epidemiological characteristics and post-exposure prophylaxis of human rabies in Chongqing, China, 2007-2016. BMC Infect Dis 2018;18:6. 10.1186/s12879-017-2830-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.San Jose R, Magsino PJ, Bundalian R. Pet owners’ awareness on RA 9482 (anti-rabies act of 2007) in Magalang, Pampanga Philippines. Heliyon 2019;5:e01759. 10.1016/j.heliyon.2019.e01759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Food and Agriculture Organization of the United nations . The animal welfare act of 1998. 1998.
- 45.Abdulmoghni RT, Al-Ward AH, Al-Moayed KA, et al. Incidence, trend, and mortality of human exposure to rabies in Yemen, 2011-2017: observational study (preprint). JMIR Public Health and Surveillance [Preprint]. 10.2196/preprints.27623 [DOI] [PMC free article] [PubMed]
- 46.Guadu T, Shite A, Chanie M, et al. Assessment of knowledge, attitude and practices about rabies and associated factors: in the case of Bahir Dar town. Glob Vet 2014;13:348–54. [Google Scholar]
- 47.Yibrah M, Damtie D. Incidence of human rabies exposure and associated factors at the gondar health center, Ethiopia: a three-year retrospective study. Infect Dis Poverty 2015;4:3. 10.1186/2049-9957-4-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Horton DL, Ismail MZ, Siryan ES, et al. Rabies in Iraq: trends in human cases 2001-2010 and characterisation of animal rabies strains from Baghdad. PLoS Negl Trop Dis 2013;7:e2075. 10.1371/journal.pntd.0002075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Blanton JD, Colwell E, Walden CL, et al. Rabies exposures and pre-exposure vaccination practices among individuals with an increased risk of rabies exposure in the United States. J Am Vet Med Assoc 2018;252:1491–502. 10.2460/javma.252.12.1491 [DOI] [PubMed] [Google Scholar]
- 50.Guo D, Yin W, Yu H, et al. The role of socioeconomic and climatic factors in the spatio-temporal variation of human rabies in China. BMC Infect Dis 2018;18:526. 10.1186/s12879-018-3427-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kim CH, Lee CG, Yoon HC, et al. Rabies, an emerging disease in Korea. J Vet Med B Infect Dis Vet Public Health 2006;53:111–5. 10.1111/j.1439-0450.2006.00928.x [DOI] [PubMed] [Google Scholar]
- 52.Nyasulu PS, Weyer J, Tschopp R, et al. Rabies mortality and morbidity associated with animal bites in africa: a case for integrated rabies disease surveillance, prevention and control: a scoping review. BMJ Open 2021;11:e048551. 10.1136/bmjopen-2020-048551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Acharya KP, Subedi D, Wilson RT. Rabies control in South Asia requires a one health approach. One Health 2021;12:100215. 10.1016/j.onehlt.2021.100215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Liu Q, Wang X, Liu B, et al. Improper wound treatment and delay of rabies post-exposure prophylaxis of animal bite victims in China: prevalence and determinants. PLoS Negl Trop Dis 2017;11:e0005663. 10.1371/journal.pntd.0005663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.World Health Organization . Rabies vaccines who position paper. Weekly Epidemiological Record = Relevé Épidémiologique Hebdomadaire 2007;82:425–36. [PubMed] [Google Scholar]
- 56.Center for Disease Control and Prevention . Human rabies [Internet]. 2021. Available: https://www.cdc.gov/rabies/location/usa/surveillance/human_rabies.html
- 57.Banyard AC, Horton DL, Freuling C, et al. Control and prevention of canine rabies: the need for building laboratory-based surveillance capacity. Antiviral Res 2013;98:357–64. 10.1016/j.antiviral.2013.04.004 [DOI] [PubMed] [Google Scholar]
- 58.Léchenne M, Miranda ME, Zinsstag J, et al. Integrated rabies control. In: One Health: the theory and practice of integrated health approaches. CAB International, 2015: 176–89. [Google Scholar]
- 59.OIE SRR-SEA . OIE World organisation for animal health, OIE sub-regional representation for South-East Asia (OIE SRR-SEA): ASEAN rabies elimination strategy. 2016. [Google Scholar]
- 60.Belotto A, Leanes LF, Schneider MC, et al. Overview of rabies in the Americas. Virus Res 2005;111:5–12. 10.1016/j.virusres.2005.03.006 [DOI] [PubMed] [Google Scholar]
- 61.Birhane MG, Miranda MEG, Dyer JL, et al. Willingness to pay for dog rabies vaccine and registration in Ilocos Norte, Philippines (2012). PLoS Negl Trop Dis 2012;10:e0004486. 10.1371/journal.pntd.0004486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lembo T, Attlan M, Bourhy H, et al. Renewed global partnerships and redesigned roadmaps for rabies prevention and control. Vet Med Int 2011;2011:923149. 10.4061/2011/923149 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-066587supp001.pdf (85.8KB, pdf)
Data Availability Statement
Data are available on reasonable request.