To the Editor:
Shared decision making (SDM) facilitates collaborative treatment decisions based on patient and family values, goals, and preferences (1). In intensive care unit (ICU) settings, effective SDM results in goal-concordant treatment decisions, improved psychological outcomes among families and clinicians, and shorter ICU lengths of stay (1–7). Despite evidence of racial disparities in clinician communication and ICU outcomes, it is unknown if ICU clinicians equitably engage racially minoritized families in SDM (8–10). Thus, our objective was to compare ICU physicians’ SDM behaviors in audio-recorded meetings with Black versus White families.
Methods
We conducted a mixed-methods study using qualitative data from a randomized trial of a decision aid about prolonged mechanical ventilation (⩾10 d) (11). The trial was conducted in 13 medical and surgical ICUs at 5 hospitals in North Carolina, Pennsylvania, and Washington. Families randomized to the intervention viewed a decision aid about prolonged mechanical ventilation outcomes, then ICU physicians held unscripted, audio-recorded meetings with families from both trial arms. From 146 meetings, we purposively sampled 129 that had complete recordings, were in English, and included a primary surrogate decision maker (hereafter referred to as “family member”) who self-identified as Black or White.
We used summative content analysis to quantify SDM behaviors (12). An a priori coding schema was adapted from a validated SDM framework for ICU physicians (Table E1 in the data supplement) (5, 13). A research team consisting of an ICU nurse (H.Y.), a palliative care physician (J.E.M.), a communication studies scientist (M.C.H.), and an ICU physician (D.C.A.), all with qualitative or health equity research expertise, met biweekly throughout the analysis. Four audio-recorded family meetings were analyzed by all team members to ensure consistency in code application through discussion, then the remainder were coded independently (14). Fourteen codes were summed to calculate an SDM score for each meeting.
Results
The sample included meetings with 22 (17.1%) Black and 107 (82.9%) White family members. Family members had a median age of 53.0 years (interquartile range [IQR], 44.0, 62.0 yr) and were predominantly female (75.2%). They endorsed high health literacy (median, 5.0; IQR, 4.0, 6.0), hope (96.9%), and social support (96.1%). Compared with White families, Black families were more commonly randomized to the intervention (59.1% vs. 45.8%) and less commonly interacted with racially concordant physicians (0% vs. 80.4%). Patients’ age and race were similar to those of their family members, and 26.4% died in the hospital (Table 1). Ninety-six physicians participated in one to four family meetings each. They had a median age of 35.0 years (IQR, 32.0, 42.0 yr), and most were White (75.0%), male (64.6%), and preferred to engage families as equal partners in decision making (80.4%) (Table 2).
Table 1.
Family member and patient demographics
| White Family Member | Black Family Member | Total | |
|---|---|---|---|
| Number | 107 | 22 | 129 |
| Family member characteristics | |||
| Age, yr, median (IQR) | 54.0 (45.0, 62.0) | 48.5 (39.0, 56.0) | 53.0 (44.0, 62.0) |
| Female, % | 75.7 | 72.7 | 75.2 |
| Relationship to patient, % | |||
| Partner | 53.3 | 27.3 | 48.8 |
| Parent | 20.6 | 31.8 | 22.5 |
| Child | 14.0 | 27.3 | 16.3 |
| Other | 12.2 | 13.6 | 12.4 |
| Randomized to intervention, % | 45.8 | 59.1 | 48.1 |
| Health literacy, median (IQR)* | 5.0 (4.0, 6.0) | 5.0 (3.0, 7.0) | 5.0 (4.0, 6.0) |
| Endorses hope for future, %† | 96.3 | 100 | 96.9 |
| Endorses social support, %‡ | 98.1 | 86.4 | 96.1 |
| Family–physician sex concordance, % | |||
| Female–female | 25.2 | 18.2 | 24.0 |
| Male–male | 16.8 | 18.2 | 17.0 |
| Discordant | 58.0 | 63.6 | 58.9 |
| Family–physician race concordance, % | 80.4 | 0 | 66.7 |
| Patient characteristics | |||
| Age, yr, median (IQR) | 54.0 (41.0, 67.0) | 48.0 (35.0, 59.0) | 53.0 (40.0, 64.0) |
| Female, % | 32.7 | 40.9 | 34.1 |
| Race, % | |||
| White | 97.2 | 0 | 80.6 |
| Black | 0.9 | 100 | 17.8 |
| Other | 1.9 | 0 | 1.6 |
| Charlson comorbidity index score (29), median (IQR) | 3.0 (1.0, 6.0) | 3.0 (1.0,5.0) | 3.0 (1.0, 6.0) |
| APACHE II score (30) at enrollment, median (IQR) | 23.0 (18.0, 28.0) | 23.5 (17.0, 31.0) | 23.0 (18.0, 28.0) |
| In-hospital mortality, % | 26.2 | 27.3 | 26.4 |
Definition of abbreviations: APACHE = Acute Physiology and Chronic Health Evaluation; IQR = interquartile range.
Ranging from 3 to 15 in order of decreasing health literacy.
The statement assessing hope was, “I look forward to the future with hope.”
The statement assessing social support was, “I feel that I have someone I can turn to for advice about making important decisions (like medical decisions).”
Table 2.
Physician demographics
| Demographic Characteristic | Data |
|---|---|
| Number | 96 |
| Age, yr, median (IQR) | 35.0 (32.0, 42.0) |
| Female, % | 35.4 |
| Race, % | |
| White | 75.0 |
| Black | 4.2 |
| Asian | 10.4 |
| Other | 10.4 |
| Self-reported decision-making style, % | |
| Leads decision making | 10.9 |
| Engages patient or family as equal partner | 80.4 |
| Allows patient or family to make decision | 8.7 |
Definition of abbreviation: IQR = interquartile range.
Among 14 components of SDM, physicians addressed a median of 6.5 (IQR, 5.0, 8.0) with Black families and 6.0 (IQR, 4.0, 9.0) with White families. They most often discussed informational components, including discussing prognosis or the purpose of the visit (95.3% and 72.9%, respectively), in meetings with families of both races. Physicians less often engaged in preference-sensitive components, including eliciting preferences or linking decisions to preferences (51.9% and 43.4%, respectively), although no meaningful racial differences were evident. Regardless of family race, physicians least frequently broached difficult topics, including death or spirituality (17.1% and 7.8%, respectively). The only meaningful racial difference was that physicians provided less validation about medical decisions and family roles to Black than to White families (27.3% vs. 49.5%) (Figure 1).
Figure 1.
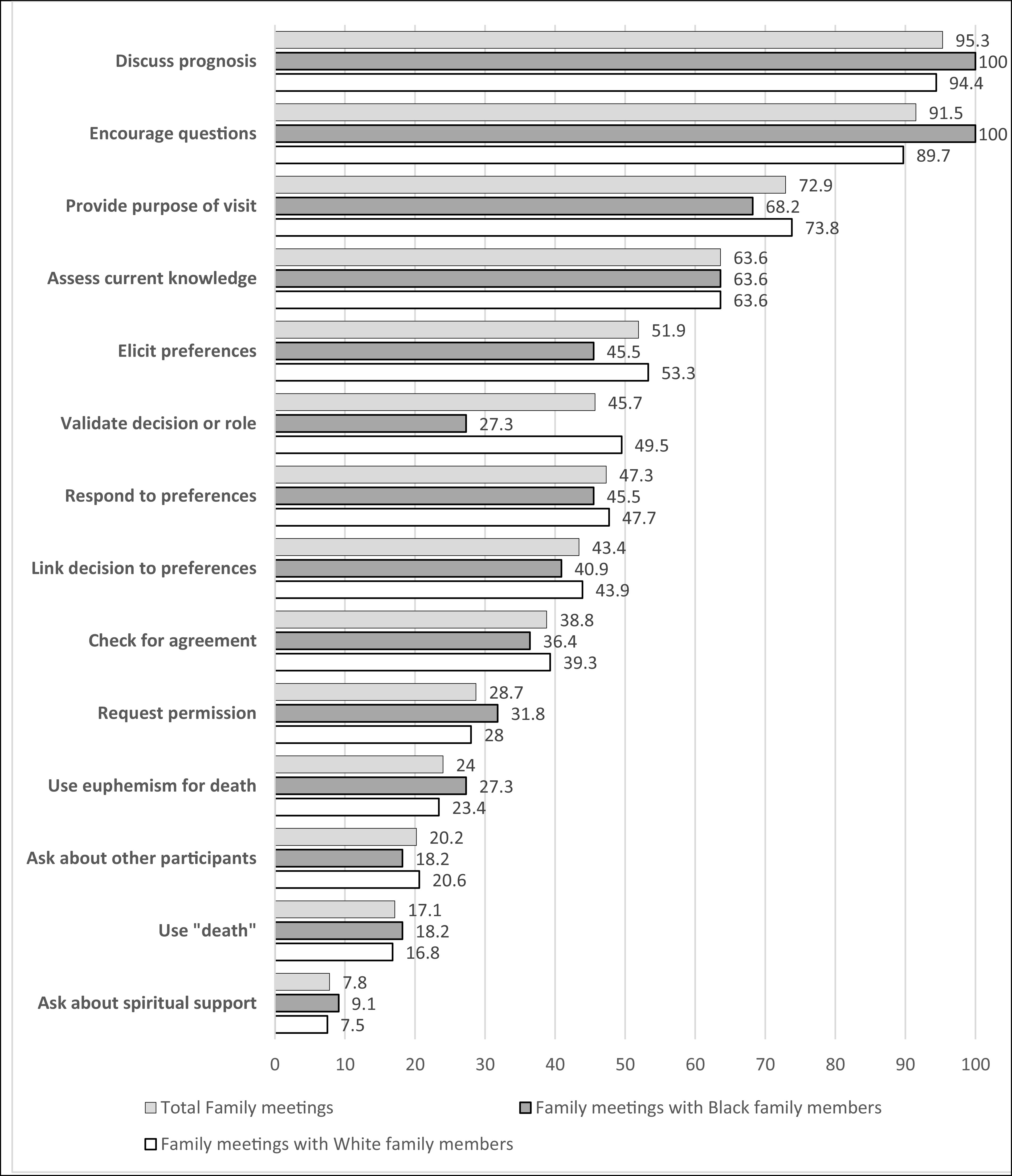
Frequency of shared decision-making components used by intensive care unit physicians in meetings with Black versus White family members, by order of frequency (percentage) among all family members.
Discussion
In this mixed-methods study, ICU physicians appeared to approach SDM similarly with Black and White families. However, they less frequently validated Black families’ medical decisions or involvement in care. Although ICU physicians commonly discussed informational components of SDM, they engaged in preference-sensitive communication in half of the meetings and discussed difficult topics in less than one-fourth of meetings.
That physicians addressed most components of SDM equally with Black and White families is encouraging. In particular, the high frequency of informational components, such as discussing prognosis, in both groups suggests that racially minoritized families have equal access to medical information about their critically ill loved ones. For other components of SDM, future studies should interrogate whether equality signals equity. For example, if Black families have greater spiritual needs than White families, an equitable approach may require more frequent discussion of spirituality with Black families (15).
We confirmed several findings from other studies. First, discussion of preferences did not occur in half of meetings, despite the need to make highly value-laden decisions (16–19). Second, physicians infrequently discussed death or spirituality, although we know that families want clinicians to do so (20, 21).
A notable finding was that physicians provided validation less commonly to Black than to White families. This is the only component of our coding schema that assessed an emotional rather than cognitive feature of SDM. Emotional support is increasingly recognized as necessary to promote high-quality decision making and psychological well-being among decision makers (11, 22, 23). Furthermore, validating families’ roles and decisions is critical to establishing trustworthiness, which is important for all families but is especially salient for those who are minoritized (24). Disparate empathic communication should be a focus of future study and may represent a novel mechanism of racial disparities in ICU outcomes (25). The effect of family–physician race concordance on communication should also be evaluated, although this may be challenging because of limited critical care workforce diversity (26, 27).
This study has several strengths, including a rich, multicenter qualitative database and an interdisciplinary analytic team. There are also limitations. First, the Hawthorne effect is possible (28). However, family meetings were unscripted, and racial bias was not a focus of the original trial; therefore, physicians are unlikely to have altered their approach to SDM as relevant to racially minoritized families. Second, in this hypothesis-generating study, we identified the presence of SDM components, but not how physicians communicated these to families (e.g., how prognosis was framed). Additional inductive qualitative analyses are needed. Third, we could not analyze nonverbal communication (13).
In conclusion, although ICU physicians appeared to approach SDM similarly with Black and White families, we identified a racial difference in their validation of Black families’ decisions and roles. We also confirmed opportunities to improve preference-sensitive communication and discussion of difficult topics with all families.
Footnotes
Supported by National Institutes of Health/National Heart, Lung, and Blood Institute grants R01HL109823 (C.E.C.) and K23HL164968 (D.C.A.).
This letter has a data supplement, which is accessible from this issue’s table of contents at www.atsjournals.org.
Author disclosures are available with the text of this letter at www.atsjournals.org.
References
- 1. Kon AA, Davidson JE, Morrison W, Danis M, White DB, American College of Critical Care Medicine, American Thoracic Society Shared decision making in ICUs: an American College of Critical Care Medicine and American Thoracic Society policy statement. Crit Care Med . 2016;44:188–201. doi: 10.1097/CCM.0000000000001396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gravel K, Légaré F, Graham ID. Barriers and facilitators to implementing shared decision-making in clinical practice: a systematic review of health professionals’ perceptions. Implement Sci . 2006;1:16. doi: 10.1186/1748-5908-1-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. White DB, Braddock CH, III, Bereknyei S, Curtis JR. Toward shared decision making at the end of life in intensive care units: opportunities for improvement. Arch Intern Med . 2007;167:461–467. doi: 10.1001/archinte.167.5.461. [DOI] [PubMed] [Google Scholar]
- 4. Curtis JR, White DB. Practical guidance for evidence-based ICU family conferences. Chest . 2008;134:835–843. doi: 10.1378/chest.08-0235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mohan D, Alexander SC, Garrigues SK, Arnold RM, Barnato AE. Communication practices in physician decision-making for an unstable critically ill patient with end-stage cancer. J Palliat Med . 2010;13:949–956. doi: 10.1089/jpm.2010.0053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bibas L, Peretz-Larochelle M, Adhikari NK, Goldfarb MJ, Luk A, Englesakis M, et al. Association of surrogate decision-making interventions for critically ill adults with patient, family, and resource use outcomes. JAMA Netw Open . 2019;2:e197229. doi: 10.1001/jamanetworkopen.2019.7229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wendlandt B, Ceppe A, Choudhury S, Cox CE, Hanson LC, Danis M, et al. Modifiable elements of ICU supportive care and communication are associated with surrogates’ PTSD symptoms. Intensive Care Med . 2019;45:619–626. doi: 10.1007/s00134-019-05550-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. van Ryn M. Research on the provider contribution to race/ethnicity disparities in medical care. Med Care . 2002;40:I140–I151. doi: 10.1097/00005650-200201001-00015. [DOI] [PubMed] [Google Scholar]
- 9. McGowan SK, Sarigiannis KA, Fox SC, Gottlieb MA, Chen E. Racial disparities in ICU outcomes: a systematic review. Crit Care Med . 2022;50:1–20. doi: 10.1097/CCM.0000000000005269. [DOI] [PubMed] [Google Scholar]
- 10.Cooper LA, Roter DL. Unequal treatment: confronting racial and ethnic disparities in health care. Washington, DC: National Academies Press; 2003. Patient-provider communication: the effect of race and ethnicity on process and outcomes of healthcare; pp. 552–593. [PubMed] [Google Scholar]
- 11. Cox CE, White DB, Hough CL, Jones DM, Kahn JM, Olsen MK, et al. Effects of a personalized web-based decision aid for surrogate decision makers of patients with prolonged mechanical ventilation: a randomized clinical trial. Ann Intern Med . 2019;170:285–297. doi: 10.7326/M18-2335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res . 2005;15:1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 13. Elliott AM, Alexander SC, Mescher CA, Mohan D, Barnato AE. Differences in physicians’ verbal and nonverbal communication with Black and White patients at the end of life. J Pain Symptom Manage . 2016;51:1–8. doi: 10.1016/j.jpainsymman.2015.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Shenton AK. Strategies for ensuring trustworthiness in qualitative research projects. Educ Inf . 2004;22:63–75. [Google Scholar]
- 15. Eaton TL, Scheunemann LP, Butcher BW, Donovan HS, Alexander S, Iwashyna TJ. The prevalence of spiritual and social support needs and their association with postintensive care syndrome symptoms among critical illness survivors seen in a post-ICU follow-up clinic. Crit Care Explor . 2022;4:e0676. doi: 10.1097/CCE.0000000000000676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Scheunemann LP, Ernecoff NC, Buddadhumaruk P, Carson SS, Hough CL, Curtis JR, et al. Clinician-family communication about patients’ values and preferences in intensive care units. JAMA Intern Med . 2019;179:676–684. doi: 10.1001/jamainternmed.2019.0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. DeKeyser Ganz F, Engelberg R, Torres N, Curtis JR. Development of a model of interprofessional shared clinical decision making in the ICU: a mixed-methods study. Crit Care Med . 2016;44:680–689. doi: 10.1097/CCM.0000000000001467. [DOI] [PubMed] [Google Scholar]
- 18. Ge C, Goss AL, Crawford S, Goostrey K, Buddadhumaruk P, Shields AM, et al. Variability of prognostic communication in critically ill neurologic patients: a pilot multicenter mixed-methods study. Crit Care Explor . 2022;4:e0640. doi: 10.1097/CCE.0000000000000640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Xu L, El-Jawahri AR, Rubin EB. Tracheostomy decision-making communication among patients receiving prolonged mechanical ventilation. Ann Am Thorac Soc . 2021;18:848–856. doi: 10.1513/AnnalsATS.202009-1217OC. [DOI] [PubMed] [Google Scholar]
- 20. Barlet MH, Barks MC, Ubel PA, Davis JK, Pollak KI, Kaye EC, et al. Characterizing the language used to discuss death in family meetings for critically ill infants. JAMA Netw Open . 2022;5:e2233722. doi: 10.1001/jamanetworkopen.2022.33722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Choi PJ, Curlin FA, Cox CE. Addressing religion and spirituality in the intensive care unit: a survey of clinicians. Palliat Support Care . 2019;17:159–164. doi: 10.1017/S147895151800010X. [DOI] [PubMed] [Google Scholar]
- 22. October TW, Dizon ZB, Arnold RM, Rosenberg AR. Characteristics of physician empathetic statements during pediatric intensive care conferences with family members. JAMA Netw Open . 2018;1:e180351. doi: 10.1001/jamanetworkopen.2018.0351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Selph RB, Shiang J, Engelberg R, Curtis JR, White DB. Empathy and life support decisions in intensive care units. J Gen Intern Med . 2008;23:1311–1317. doi: 10.1007/s11606-008-0643-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Peek ME, Gorawara-Bhat R, Quinn MT, Odoms-Young A, Wilson SC, Chin MH. Patient trust in physicians and shared decision-making among African-Americans with diabetes. Health Commun . 2013;28:616–623. doi: 10.1080/10410236.2012.710873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Park J, Beach MC, Han D, Moore RD, Korthuis PT, Saha S. Racial disparities in clinician responses to patient emotions. Patient Educ Couns . 2020;103:1736–1744. doi: 10.1016/j.pec.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lane-Fall MB, Miano TA, Aysola J, Augoustides JGT. Diversity in the emerging critical care workforce: analysis of demographic trends in critical care fellows from 2004–2014. Crit Care Med . 2017;45:822–827. doi: 10.1097/CCM.0000000000002322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Shen MJ, Peterson EB, Costas-Muñiz R, Hernandez MH, Jewell ST, Matsoukas K, et al. The effects of race and racial concordance on patient-physician communication: a systematic review of the literature. J Racial Ethn Health Disparities . 2018;5:117–140. doi: 10.1007/s40615-017-0350-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sidani S. Health intervention research: understanding research design & methods. Thousand Oaks, CA: Sage; 2015. [Google Scholar]
- 29. Quan H, Li B, Couris CM, Fushimi K, Graham P, Hider P, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol . 2011;173:676–682. doi: 10.1093/aje/kwq433. [DOI] [PubMed] [Google Scholar]
- 30. Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med . 1985;13:818–829. [PubMed] [Google Scholar]


