Abstract
Objectives.
(1) Identify anatomic contributions to chronic rhinosinusitis (CRS) necessitating revision endoscopic sinus surgery (RESS). (2) Create a clinical acronym to guide imaging review prior to RESS that addresses pertinent sites of disease and potential sites of surgical morbidity.
Data Sources.
Ovid MEDLINE, Embase and Medline via Embase.com, Web of Science Core Collection, Cochrane Central Register of Controlled Trials (CENTRAL), and Google Scholar.
Review Methods.
Systematic search was performed using a combination of standardized terms and keywords. Studies were included if they investigated anatomic contributions to persistent CRS requiring RESS or the relationship between anatomic landmarks and surgical morbidity. Identified studies were screened by title/abstract, followed by full-text review. Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines were strictly followed.
Results.
In total, 599 articles met screening criteria, 89 were eligible for full-text review, and 27 studies were included in the final review. The identified anatomic sites of interests are broad; the most frequently cited anatomic region was retained anterior ethmoid cells (22/27 studies), followed by posterior ethmoid cells (14/27 studies). Using the consolidated information, a clinical acronym, REVISIONS, was created: Residual uncinate, Ethmoid cells (agger, Haller, supraorbital), Vessels (anterior and posterior ethmoid), Infundibulum, Septal deviation, I (eye) compartment, Onodi cell, Natural os, and Skull base slope and integrity.
Conclusions.
The REVISIONS acronym was developed as a tool to distill the unique anatomic contributions of primary endoscopic sinus surgery failure into a format that can be easily incorporated in preoperative radiologic review and surgical planning to optimize outcomes and minimize complications.
Keywords: revision sinus surgery, chronic rhinosinusitis, endoscopic sinus surgery, preoperative imaging review
Chronic rhinosinusitis (CRS) is estimated to affect approximately 13% of the US population, with over 250,000 people undergoing endoscopic sinus surgery (ESS) per year in the country.1,2 While considered an effective surgery for those with unremitting symptoms despite maximal medical therapy, 7% to 15% of patients undergoing ESS will require revision endoscopic sinus surgery (RESS).3–5
The preoperative sinus computed tomography (CT) scan is a mainstay of endoscopic sinus surgery, demonstrating the extent of disease and revealing anatomic variants that may contribute to sinus disease burden or complicate successful sinus surgery. Various systematic approaches have been developed to assist in the otolaryngologist’s evaluation of the preoperative sinus CT scan, with the “Cribriform plate, Lamina papyracea, Onodi cell, Sphenoid sinus pneumatization, and (anterior) Ethmoidal artery (CLOSE)” mnemonic being the most widely used.6 Resident physicians find the CLOSE system a favorable approach to improve preoperative identification of critical anatomic structures.7,8
In patients undergoing RESS, the anatomy is typically complicated by residual air cells missed at the time of initial surgery, bony thickening, scar tissue, and other altered anatomic landmarks, often making the surgery more complicated than the primary ESS.9 While the implementation of the CLOSE mnemonic has significantly improved identification of potentially complicating anatomic sinus variants on preoperative CT for primary ESS, to our knowledge, no systematic, efficient approach to evaluate the preoperative CT scan for RESS exists. The objective of this study was to systematically review the RESS literature to determine which aspects of sinus anatomy contribute to the need for revision surgery and to identify altered landmarks that may preclude morbidity in RESS. From this information, a clinically and educationally useful acronym for the evaluation of preoperative sinus CT imaging for RESS was developed.
Methods
The systematic review was conducted and reported in accordance to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) of Observational Studies in Epidemiology guidelines. The study protocol was registered on PROSPERO (registration number: CRD42020222478). The protocol was published automatically without review by the PROSPERO team to enable PROSPERO to focus on COVID-19 registrations.
Eligibility Criteria
Eligible studies included those that investigated anatomic contributions to persistent CRS requiring RESS or the relationship between anatomic landmarks and surgical morbidity. Studies were excluded if they involved (1) pediatric populations, (2) nonendoscopic surgical techniques, (3) disease processes other than CRS, and (4) non-English studies. Studies that did not assess explicit anatomic contributions to persistent disease were also excluded.
Search Protocol and Study Selection
The published literature was searched using strategies created by a medical librarian for studies investigating anatomic causes of persistent CRS requiring RESS. The search strategies were established using a combination of standardized terms and keywords and were implemented in Ovid MEDLINE and Epub Ahead of Print, In-Process, In-Data-Review & Other Non-Indexed Citations, Daily and Versions, Embase and Medline via Embase.com, Web of Science Core Collection, Cochrane Central Register of Controlled Trials (CENTRAL), and Google Scholar. Searches were completed for all articles published up to November 2020. Full search strategies are provided in the appendix (in the online version of the article). All articles were screened by 2 authors independently in 2 phases. The first phase involved screening for relevance based on the title and abstract. After exclusion of the nonrelevant articles, the remaining articles were reviewed in full text by the 2 investigators to determine their final eligibility. Reviewers were blinded to each other’s results.
Data Collection Process
Data extraction was performed by two authors (O.A.K., A.M.P.) using a standardized Microsoft Excel spreadsheet. All disagreements were resolved through consensus, and expert opinion was sought as necessary. Data were collected for the key radiographic or intraoperative findings that were determined to be contributing to persistent CRS.
Data Analysis
Quality of included studies was captured using the Methodological Index for Non-Randomized Studies (MINORS) instrument for evaluation of methodologic quality of nonrandomized surgical studies.10 This instrument captures 12 key components of investigations, and the sum of the included components is used as a marker of quality, with a maximum score of 16 for noncomparative studies and 24 for comparative studies. Each radiographic or intraoperative finding was listed along with the number of articles mentioning each feature. From this list, a multistage iterative review process among all authors commenced, seeking to rank identified features by both number of mentions and surgical implications by consensus. Different acronyms were tried and tested by the primary author and evaluated by all authors to assess for strength, usability, and memorability.
Results
Study Selection
Our systematic search identified 1538 articles. There were 579 duplications that were removed, resulting in a total of 959 unique citations. These articles underwent title and abstract screening, which identified 89 studies that met the eligibility criteria for full-text review. The primary reason for exclusion following abstract review was that the study did not include the RESS population (n = 502), followed by case reports (n = 97). In total, 27 studies were included in the qualitative synthesis (Figure 1).4,11–36
Figure 1.
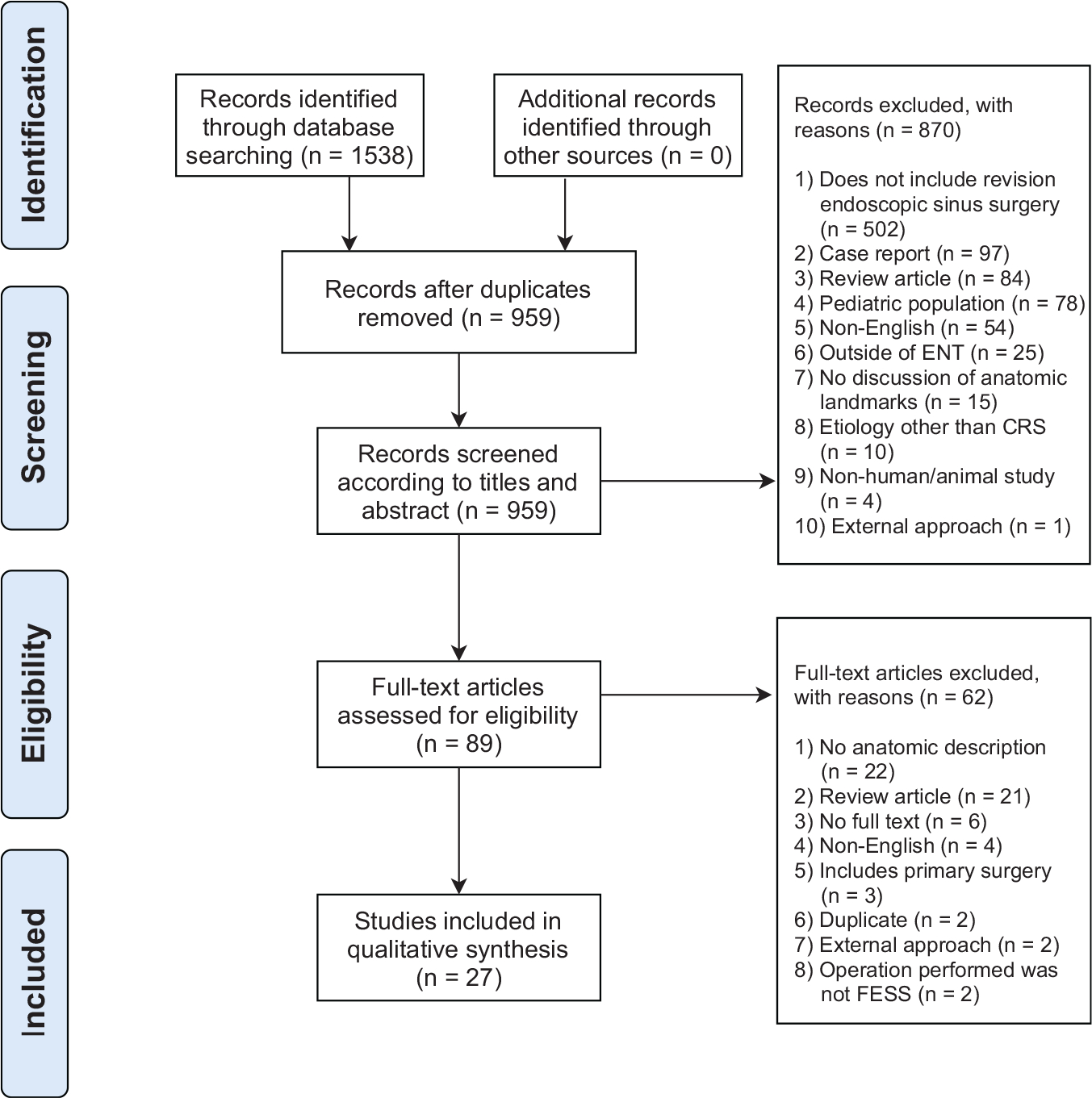
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flowchart. ENT, ear, nose, and throat; ESS, Endoscopic Sinus Surgery.
Study and Patient Characteristics of the Selected Studies
Twenty-seven studies met inclusion criteria. These studies either detailed the anatomic findings associated with recurrent or persistent disease in the CRS population or discussed anatomic considerations to prevent morbidity in RESS. These studies highlight the anatomic site(s) critical to address in the revision surgery. Most included studies were case series (25/27) and took place in a single institution (20/27). The number of revision surgeries included in these studies ranged from 5 to 246 (mean [SD], 73 [50]) for a total of 1973 revision surgeries. The MINORS score was calculated for each individual study, resulting in an average value of 11.7. More detailed description of included studies is found in Table 1.
Table 1.
Baseline Characteristics of the 27 Included Studies.
| Study, year | Study type | Single vs multi-institutional study | Total No. of revision surgeries | No. of revision surgeries with preoperative CT scan | Women, No. (%) | Age, mean (SD) or mediana (range), y | MINORS criteria score |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Parsons et al,31 1996 | Case series | Multi | 61 | 61 | — | 9 | |
| Chu et al,20 1997 | Case series | Single | 173 | 153 | — | — | 12 |
| Moses et al,29 1998 | Case series | Single | 90 | 65 | 54 (60) | 42a (20–77) | 13 |
| Ramadan,33 1999 | Case series | Single | 52 | 52 | 23 (44) | 42 | 12 |
| Richtsmeier,34 2001 | Case series | Single | 128 | 128 | — | — | 12 |
| Bradley and Kountakis,16 2004 | Case series | Multi | 80 | 80 | 35 (44) | 48 (16–76) | 14 |
| Chiu and Vaughan,19 2004 | Case series | Single | 67 | 67 | — | — | 13 |
| Musy and Kountakis,4 2004 | Case series | Single | 80 | 80 | — | — | 11 |
| Albu and Baciut,12 2010 | Case series | Single | 28 | 28 | — | 40b | 14 |
| Otto and DelGaudio,30 2010 | Case series | Single | 149 | 149 | 66 (52) | — | 11 |
| Khalil et al,26 2011 | Case series | Single | 63 | 63 | 18 (29) | 50 (12.1) | 11 |
| Gore et al,23 2013 | Case series | Single | 55 | 55 | — | — | 10 |
| Mansour,28 2013 | Case series | Single | 5 | 5 | 2 (40) | (17–54) | 9 |
| Valdes et al,36 2014 | Case series | Multi | 66 | 66 | 39 (59) | 52 | 11 |
| El-Shiekh,21 2015 | Case series | Single | 71 | 71 | 19 (27) | 45 (24–59) | 11 |
| Bewick et al,15 2016 | Case series | Multi | 75 | 75 | 19 (42) | 59 (12.7) | 13 |
| Chapurin et al,18 2016 | Case series | Single | 60 | 58 | 26 (45) | 52 (14–77) | 11 |
| Goyal et al,24 2016 | Case series | Single | 50 | 50 | — | — | 7 |
| Herzallah et al,25 2016 | Case series | Multi | 84 | 84 | 36 (43) | 34 (14.0) | 11 |
| Kuan et al,27 2016 | Case series | Multi | 69 | 69 | 33 (48) | 51a (21–79) | 11 |
| Cantillano et al,17 2017 | Case series | Single | 27 | 27 | 11 (41) | 46 (12–66) | 11 |
| Benkhatar et al,14 2018 | Case series | Single | 10 | 10 | 2 (20) | — | 13 |
| Rajwani et al,32 2018 | Cohort | Single | 246 | 246 | 111 (45) | 54 (12.8) | 19 |
| Socher et al,35 2018 | Case series | Single | 28 | 28 | 11 (39) | 37 (10.2) | 11 |
| Fu et al,22 2019 | Case control | Single | 72 | 72 | 42 (58) | No septoplasty: 55 (2), Septoplasty: 52 (2) | 19 |
| Al-Abdulwahid et al,11 2020 | Case series | Single | 60 | 60 | — | — | 9 |
| Baban et al,13 2020 | Case series | Multi | 24 | 24 | 12 (50) | 41 (20–62) | 9 |
Abbreviations: AFRS, allergic fungal rhinosinusitis; CRS, chronic rhinosinusitis; CT, computed tomography; MINORS, Methodological Index for Non-Randomized
Studies; —, missing.
Median.
Age of larger cohort (not solely revision endoscopic sinus surgery).
Identified Anatomic Landmarks
The unique anatomic sites contributing to recurrent or persistent CRS symptoms were consolidated (see Suppl. Table S1 in the online version of the article). The identified anatomic sites of interests are broad; the most frequently cited anatomic region was retained anterior ethmoid cells (22/27 studies), followed by posterior ethmoid cells (14/27 studies). Included studies are noted to be heterogenous in the primary purpose of the investigation. Often, studies focused specifically on the impact of a particular region on the need for RESS. Such studies could be focused on the frontal recess or causes of surgical failure of the frontal sinus,14,16,19,28,36 maxillary sinus,12,27,34 nasal septum,22 or others.18,25,31 Details of identified anatomic subsite by each study are displayed in the Supplemental Table 1 (in the online version of the article). Of note, no study explicitly explored the relationship of anatomic contributions to surgical morbidity in the RESS population.
REVISIONS Acronym
The next step of the study sought to consolidate the ascertained information, along with expert opinion and literature review, to create an acronym serving as a clinical tool to enhance otolaryngologist preoperative planning. Several iterations of the acronym were created, drawing upon important anatomic sites identified in this systematic review that led to recurrent or persistent CRS in greater than 9 individual studies (Table 2), potential complications of ESS, and expert opinion. The developed acronym, REVISIONS, was unanimously agreed upon to meet the aforementioned goals in the most succinct and memorable format. The components of REVISIONS include the following: Residual uncinate, Ethmoid cells (agger, Haller, supraorbital), Vessels (anterior and posterior ethmoid), Infundibulum, Septal deviation, I (eye) compartment, Onodi cell, Natural os, and Skull base slope and integrity.
Table 2.
REVISIONS Acronym With Anatomical Findings by Study.a
| Parsons et al,31 1996 | Chu et al,20 1997 | Moses et al,29 1998 | Ramadan,33 1999 | Richtsmeier,34 2001 | Bradley and Kountakis,16 2004 | Chiu and Vaughan,19 2004 | Musy and Kountakis,4 2004 | Albu and Baciut,12 2010 | Otto and DelGaudio,30 2010 | Khalil et al,26 2011 | Gore et al,23 2013 | Mansour,28 2013 | Valdes et al,36 2014 | El-Shiekh,21 2015 | Bewick et al,15 2016 | Chapurin et al,18 2016 | Goyal et al,24 2016 | Herzallah et al,25 2016 | Kuan et al,27 2016 | Cantillano et al,17 2017 | Benkhatar et al,14 2018 | Rajwani et al,32 2018 | Socher et al,35 2018 | Fu et al,22 2019 | Al-Abdulwahid et al,11 2020 | Baban et al,13 2020 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||||||||||||||||
| Residual uncinate | |||||||||||||||||||||||||||
| Ethmoid cells | |||||||||||||||||||||||||||
| Vessels | |||||||||||||||||||||||||||
| Infundibulum | |||||||||||||||||||||||||||
| Septal deviation | |||||||||||||||||||||||||||
| I (eye)—orbital walls | |||||||||||||||||||||||||||
| Onodi cell | |||||||||||||||||||||||||||
| Natural os | |||||||||||||||||||||||||||
| Skull base slope and integrity | |||||||||||||||||||||||||||
Shaded areas indicate anatomic site found in revision endoscopic sinus surgery cases.
Discussion
This systematic review identified 27 studies investigating anatomic findings associated with primary ESS failure. Key anatomic considerations for RESS were identified as critical for surgically recurrent or persistent CRS and to prevent surgical complications. The REVISIONS acronym—Residual uncinate, Ethmoid cells (agger, Haller, supraorbital), Vessels (anterior and posterior ethmoid), Infundibulum, Septal deviation, I (eye) compartment, Onodi cell, Natural os, and Skull base slope and integrity—highlights these common anatomic contributions. Issues can occur at 1 or several of these anatomic sites and contribute to continued disease.
Failure of primary ESS can be multifactorial. Host, environmental, or anatomic factors can all play a role.37 Medical management of inflammatory disease is crucial, and RESS should only be considered when anatomic contributions are felt to be the leading cause. Examination of the sinonasal anatomy through endoscopic and radiographic measures is needed to identify anatomic contributions to surgical failure.13,37 None of the reviewed studies directly investigated the relationship between altered anatomic landmarks and surgical morbidity.
RESS warrants special preoperative considerations. It is well established that RESS is more challenging; thereby, the potential for complications is higher. The main challenges associated with RESS include postoperative scarring and altered anatomy that distorts operative landmarks.18,29,37,38 Prior investigations have found that approximately 7% to 15% of patients who undergo ESS will undergo revision surgery.3–5 Reported rates of surgical complications following RESS vary. Wigand and Hosemann39 conducted a retrospective study of 90 patients undergoing ESS for CRS and found that revision surgery was found to be a significant risk factor for CSF leak. In a single-institution review of patients who underwent ESS for CRS over a 25-year period, Stankiewicz et al40 reported surgical complications in 105 of 3402 patients (3.09%). Patients undergoing revision surgery were reported to have greater risk of CSF leak and bleeding. Severity of bleeding was noted to be higher in the revision population. In contrast, Krings et al3 investigated risk of complications in RESS for CRS using a large all-payer database for Florida and California and found rates of complications between primary and revision surgeries to be statistically similar (0.36% vs 0.46%, respectively) with an odds ratio of 1.26 for complications in the revision population and 95% confidence interval of 0.79 to 2.00. Reported complications included skull base complications, orbital complications, and hemorrhagic complications requiring a transfusion.
Preoperative surgical checklists have increased in usage since the development of the World Health Organization (WHO) Surgical Safety Checklist, whose implementation has been shown in multiple randomized clinical trials to reduce perioperative morbidity and mortality and to improve interdisciplinary communication.41 The success of the WHO checklist has led to the development and adoption of numerous other checklists in medicine, including patient handover routines, medication prescription, and infection control precautions.42 Checklists or acronyms have also been developed to aid clinicians in preparation for sinus surgery, with the “CLOSE” acronym by O’Brien et al43 being the most well-known and heavily used tool in the clinical setting. This tool emphasizes anatomic landmarks that can be particularly variable but are critical to recognize to avoid complications of ESS.43 Many otolaryngology residents use the CLOSE system as a part of their preoperative surgical planning. However, this tool was established for the primary surgical population. The RESS population is complicated by scarring and altered operative landmarks. Therefore, preoperative planning for RESS requires additional considerations.29,37,38 No such tool has been developed as a standardized preoperative method to identify anatomic causes of primary surgical failure and to highlight important landmarks to avoid surgical complications in the RESS population. The REVISIONS acronym fulfills this void. This study builds on previous investigations into the RESS population by consolidating key anatomic areas of interest and developing a preoperative radiographic review acronym that serves as a clinical and educational tool. The components of the acronym are as follows:
Residual Uncinate Process
The uncinate process is often described as a “hook” that most commonly attaches superiorly to lamina papyracea extending inferiorly and posteriorly toward the infundibulum (Figure 2).4,13,19 The superior attachment of the uncinate can vary; it may attach to the lamina papyracea, the ethmoid roof, or the middle turbinate, thereby affecting the direction of frontal sinus drainage.19,44 The importance of adequate uncinate removal during endoscopic sinus surgery is heavily noted in the studies included in this systematic review,4, 11, 13, 15, 17, 19, 21, 23, 24, 26, 31, 32, 34, 35 as failure to do so prevents identification of the natural maxillary ostium and adequate medication delivery to the osteomeatal complex (OMC). Failure to identify and incorporate the natural maxillary ostium contributes to recirculation of mucus as mucociliary flow is directed to the obstructed natural os rather than the surgically created antrostomy.31 The mucosa and bone of the uncinate can also contribute to disease burden of CRS.15 Up to 64% of patients undergoing RESS may have a residual uncinate.15,26
Figure 2.
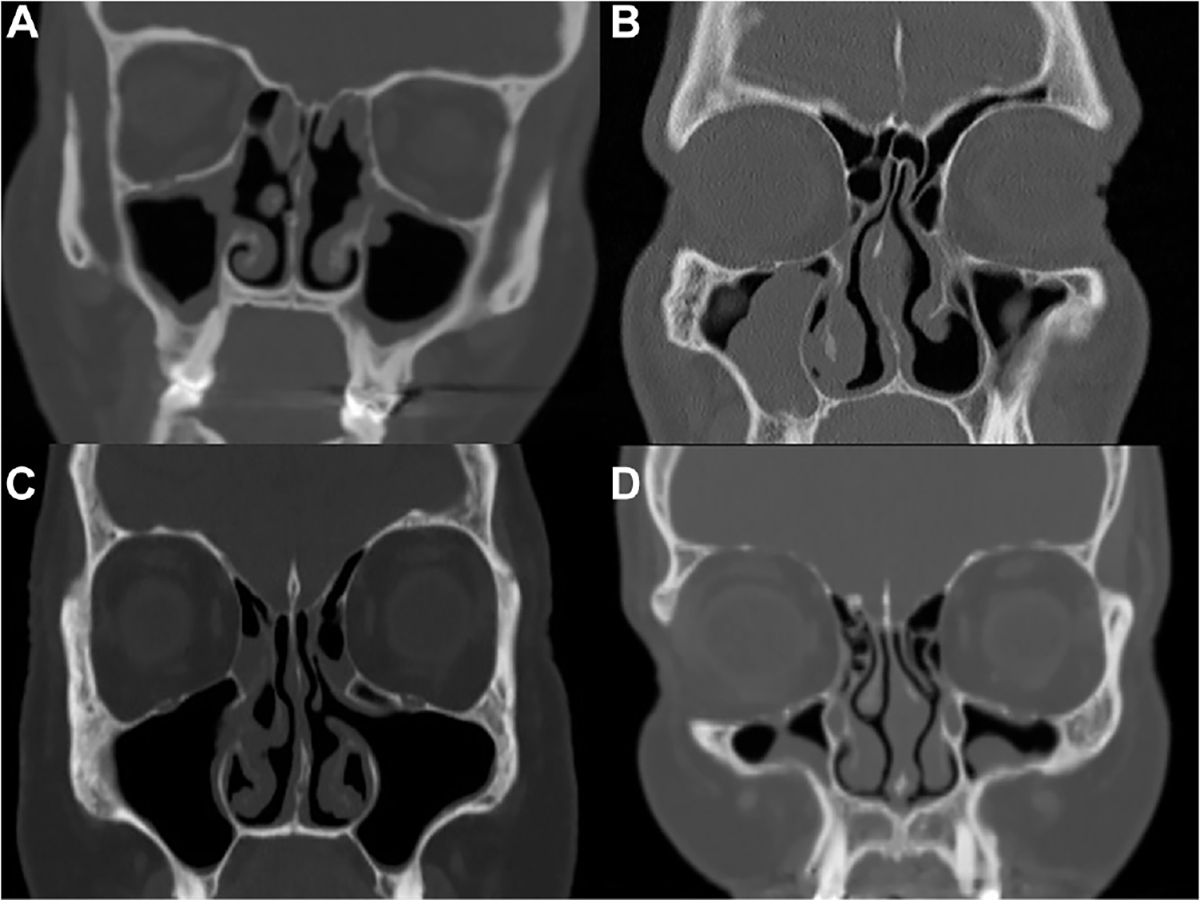
Four coronal images depicting anatomic features to recognize preoperatively to optimize outcomes. (A) Left-sided residual uncinate. (B) Depiction of agger nasi cells bilaterally. (C) A left-sided Haller cell. (D) Left-sided supraorbital cell.
Ethmoid Cells (Agger Nasi, Bulla Ethmoidalis, Supraorbital Ethmoid Cell)
Residual ethmoid air cells were the most commonly identified anatomic finding in this systematic review.4, 11–14, 16, 17, 19–21, 23–26, 28–30, 32–36 Up to 92% of patients undergoing RESS were found to have residual ethmoid air cells.26 Identifying remnant ethmoid air cells can be critical to ensuring a successful RESS (Figure 2). Several types of ethmoid air cells and ethmoid bony partitions along the medial orbital wall and skull base are addressed in RESS. While all cells and their residual partitions have been grouped into this category, identifying the specific types of ethmoid air cells is important.
The agger nasi is one such important cell. This cell is the most consistent and most anterior of the ethmoid air cells.16,19 The origin of the cell is at the infundibular groove, and this cell forms the anterior boundary of the frontal recess. As such, residual agger nasi cells are highly associated with RESS for frontal sinus rhinosinusitis.16,19 The ethmoid bulla and supraorbital cell are 2 additional cells worth considering. The ethmoid bulla is the posterior boundary of the frontal recess, and inadequate removal of the superior portion of this cell can further contribute to persistent or recurrent disease in the frontal sinus.20–23 In addition to being a potential obstruction to sinus outflow, remnant walls and mucosa can act as a nidus for scar formation, worsening obstruction.19 Removing bony partitions surrounding the supraorbital ethmoid air cell enlarges the frontal recess. Failing to address the supraorbital ethmoid cell can result in persistent frontal sinusitis.
Vessels (Anterior and Posterior Ethmoid Arteries)
Hemorrhagic complications from damage to the anterior or posterior ethmoid arteries, while not unique to the RESS population, are still important to consider. RESS often requires removal of residual ethmoid bony partitions along the skull base where the anterior and posterior ethmoid arteries travel. The vessels can be recognized radiographically through the anterior and posterior ethmoid notch along the medial orbital wall.43 The anterior ethmoid artery can lie inferior to the ethmoid roof either in a bony canal or within a mesentery.37 Radiographically, it can be identified 1 slope posterior to the globe or between the superior oblique and medial rectus (Figure 3). Classically, the posterior wall of the supraorbital ethmoid air cell marks the approximate location of the anterior ethmoid artery. For this reason, additional consideration is made when approaching this region in the revision setting as alteration of the supraorbital cell can distort the anatomy.19
Figure 3.
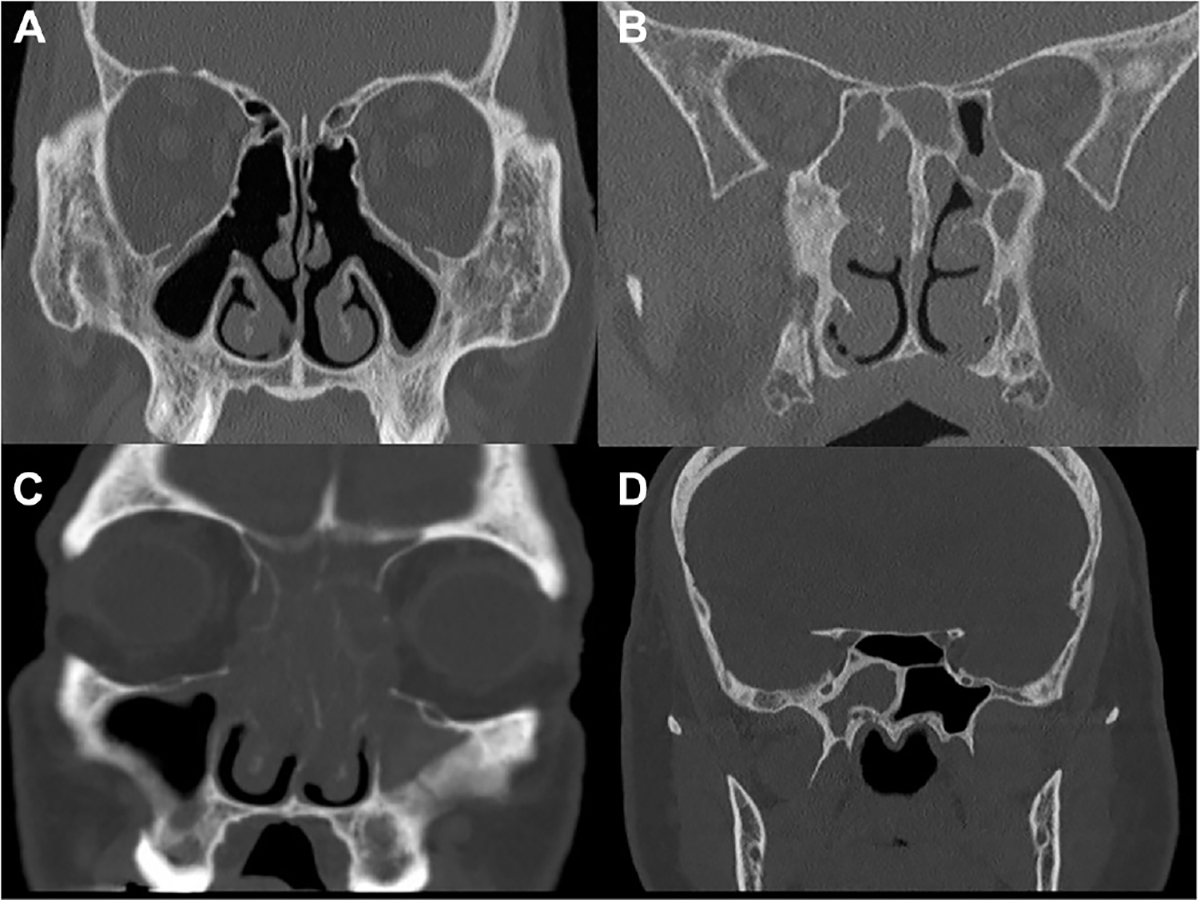
Further anatomic features to recognize preoperatively. (A) Left-sided anterior ethmoid artery. (B) Bilateral posterior ethmoid arteries. (C) Bilateral lamina papyracea erosion. (D) An Onodi cell identified by the transverse septation.
Infundibulum
This 3-dimensional space incorporates the spectrum of anatomic findings relating to the middle turbinate and posterior uncinate process. Key considerations relating to the middle turbinate include lateralization with scarring, pneumatization, or inflammatory disease involvement of the mucosa.4,15,20 There is a growing body of literature surrounding the management of the middle turbinate for its increasingly recognized impact on outcomes, including olfaction and need for revision surgery. A randomized control trial by Roy and Lade45 compared outcomes of preservation vs resection of the middle turbinate in the setting of CRS with nasal polyposis. The authors concluded that resection of the middle turbinate did demonstrate statistically significant symptomatic improvement. Other studies advocate for preserving the middle turbinate, finding more minimally invasive methods of addressing the middle turbinate to prevent loss of neuroepithelium correlated to loss of olfaction, or altering a critical skull base landmark.46–48 Another randomized control trial recently published by Khafagy et al49 found, in a head-to-head comparison of middle turbinate partial resection vs bolgerization, more favorable outcomes are noted with the partial resection group, including decreased incidence of lateralization. A certain conclusion from the literature is that neglecting to address the middle turbinate can lead to obstruction within the middle meatus that can require RESS.19,24,26
Septal Deviation
Several studies found septal deviation to contribute to persistent or recurrent CRS.13,17,21–24,26,29,32,35 The proposed mechanisms include contribution to OMC obstruction, synechiae formation within the infundibulum, and diminished access for postoperative debridement and medication penetration.22,23 In addition, Fu et al22 suggest that a deviated nasal septum can alter the nasal airflow, which can diminish mucociliary clearance. This mechanism is evidenced by computational fluid dynamic studies that have measured the aerodynamic difference due to a deviated nasal septum.50
I (Eye)—Orbital Walls
Preoperative assessment of the medial orbital wall is an important step prior to primary and revision sinus surgery. Bony dehiscence predisposes to injury to the medial rectus and other orbital contents (Figure 3).19,43 Intraoperatively, removing ethmoid air cell partitions to adequately expose the lamina papyracea is an important step to minimize the risk of inadvertent injury to the orbit.9,37
Onodi Cell
Residual posterior ethmoid air cells were the second most identified anatomic finding in the RESS population.4, 12, 13, 17, 18, 21, 23–27, 32, 33, 35 The Onodi cell deserves special recognition due to its relationship to the internal carotid artery and the optic nerve. Furthermore, an Onodi cell can be mistaken as the sphenoid sinus (Figure 3). It is important to recognize the presence of an Onodi cell and ensure that the sphenoid sinus proper is entered in addition to the posterior ethmoid cell.20–24 The clival recess is a useful landmark to ensure exposure to the sphenoid sinus.9,37,51
Natural Ostium
Sinus surgery for CRS involves enlargement of naturally existing sinus ostia, which are often apparent on preoperative radiographic examination (Figure 2).32 Creation of a surgical antrostomy that does not incorporate the natural ostium of a sinus can result in mucociliary recirculation, worsening sinus disease.15 This finding is often apparent on careful preoperative radiographic examination.34 In addition, scarring or osteitis of the bone surrounding the frontal or sphenoid ostia was identified as a contributor to CRS. The frontal sinus ostium and frontal recess are particularly susceptible to stenosis following primary surgery due to difficult postoperative access for debridement and potentially diminished topical medical penetrance.20,30,34
Skull Base Slope and Integrity
Adequate assessment of the skull base and anatomic variants such as a low-hanging cribriform plate is important to prevent surgical morbidity during primary ESS and RESS.19,43 Those performing RESS must be extra diligent in both their preoperative radiographic review and intraoperative assessment of the skull base due to potentially altered anatomic configuration.29
This systematic review is limited in several aspects. Primarily, results are reported in a heterogeneous manner. Some articles reported results by the number of patients included while some reported by side of surgery. This presents a limitation in determining the relative impact of each anatomic site onto causes of primary surgical failure. The quality of developed clinical tools can be enhanced if reporting is more consistent. An additional limitation during the development of the REVISIONS acronym comes from the trade-off between comprehensive and user-friendly acronyms. The development of a clinically friendly acronym is often restricted by the need to allow a memorable and simple design while also maximizing the impact. Several renditions of acronyms were attempted and determined to be too complicated. Discussions among all contributing authors compromised on REVISIONS as the simplest tool while maximizing value. Furthermore, an additional consideration not included in this study is the impact of inflammatory conditions of the nasal cavity and paranasal sinuses. Conditions such as polyposis, allergies, and odontogenic sinusitis were all noted to be contributing to need for RESS.11, 13, 17, 19, 29, 30, 32, 33, 36 However, this was not tangibly measured in many studies. Finally, a concept that is difficult to capture in this investigation is that despite the reporting of anatomic sites as mutually exclusive causes of surgical failure, the reality is that anatomic entities listed in Supplemental Table S1 (in the online version of the article) are often interrelated. Several of the anatomic areas that were identified interact to cause recurrent or persistent CRS.
Conclusion
This systematic review included 27 studies and was designed to identify the most common anatomic sites of obstruction that lead to recurrent or persistent CRS requiring a RESS. The REVISIONS acronym was developed as a tool to distill the unique anatomic contributions of primary ESS failure into a format that can be easily incorporated in preoperative radiologic review and surgical planning as well as intraoperatively to optimize outcomes and minimize complications. The future direction will be to implement our acronym into academic otolaryngology departments and compare both educational and clinical outcomes pre- and postimplementation as has been done with primary ESS.
Supplementary Material
Footnotes
Disclosures
Competing interests: None.
Supplemental Material
Additional supporting information is available in the online version of the article.
References
- 1.Bhattacharyya N Ambulatory sinus and nasal surgery in the United States: demographics and perioperative outcomes. Laryngoscope. 2010;120(3):635–638. [DOI] [PubMed] [Google Scholar]
- 2.Tan BK, Chandra RK, Pollak J, et al. Incidence and associated premorbid diagnoses of patients with chronic rhinosinusitis. J Allergy Clin Immunol. 2013;131(5):1350–1360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Krings JG, Kallogjeri D, Wineland A, Nepple KG, Piccirillo JF,Getz AE. Complications of primary and revision functional endoscopic sinus surgery for chronic rhinosinusitis. Laryngoscope. 2014;124(4):838–845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Musy PY, Kountakis SE. Anatomic findings in patients undergoing revision endoscopic sinus surgery. Am J Otolaryngol. 2004;25(6):418–422. [DOI] [PubMed] [Google Scholar]
- 5.Stein NR, Jafari A, DeConde AS. Revision rates and time to revision following endoscopic sinus surgery: a large database analysis. Laryngoscope. 2018;128(1):31–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.O’Brien WT Sr, Hamelin S, Weitzel EK. The preoperative sinus CT: avoiding a “CLOSE” call with surgical complications. Radiology. 2016;281(1):10–21. [DOI] [PubMed] [Google Scholar]
- 7.Yao CM, Fernandes VT, Palmer JN, Lee JM. Educational value of a preoperative CT sinus checklist: a resident’s perspective. J Surg Educ. 2013;70(5):585–587. [DOI] [PubMed] [Google Scholar]
- 8.Error M, Ashby S, Orlandi RR, Alt JA. Single-blinded prospective implementation of a preoperative imaging checklist for endoscopic sinus surgery. Otolaryngol Head Neck Surg. 2018;158(1):177–180. [DOI] [PubMed] [Google Scholar]
- 9.Cohen NA, Kennedy DW. Revision endoscopic sinus surgery. Otolaryngol Clin North Am. 2006;39(3):417–435, vii. [DOI] [PubMed] [Google Scholar]
- 10.Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological Index for Non-Randomized Studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. [DOI] [PubMed] [Google Scholar]
- 11.Al-Abdulwahid FA, Almomen A, Alshakhs A, et al. A review of the different intraoperative findings of revision endoscopic frontal surgery. Indian J Otolaryngol Head Neck Surg. 2020;1–6. 10.1007/s12070-020-02196-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Albu S, Baciut M. Failures in endoscopic surgery of the maxillary sinus. Otolaryngol Head Neck Surg. 2010;142(2):196–201. [DOI] [PubMed] [Google Scholar]
- 13.Baban MIA, Mirza B, Castelnuovo P. Radiological and endoscopic findings in patients undergoing revision endoscopic sinus surgery. Surg Radiol Anat. 2020;42(9):1003–1012. [DOI] [PubMed] [Google Scholar]
- 14.Benkhatar H, Khettab I, Sultanik P, Laccourreye O, Bonfils P.Frontal sinus revision rate after nasal polyposis surgery including frontal recess clearance and middle turbinectomy: a long-term analysis. Auris Nasus Larynx. 2018;45(4):740–746. [DOI] [PubMed] [Google Scholar]
- 15.Bewick J, Egro FM, Masterson L, Javer AR, Philpott CM. Anatomic findings in revision endoscopic sinus surgery: case series and review of contributory factors. Allergy Rhinol (Providence). 2016;7(3):151–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bradley DT, Kountakis SE. The role of agger nasi air cells inpatients requiring revision endoscopic frontal sinus surgery. Otolaryngol Head Neck Surg. 2004;131(4):525–527. [DOI] [PubMed] [Google Scholar]
- 17.Cantillano P, Rubio F, Naser A, Nazar R. Revision endoscopic sinonasal surgery. Acta Otorrinolaringol Esp. 2017;68(1):1–8. [DOI] [PubMed] [Google Scholar]
- 18.Chapurin N, Honeybrook A, Johnson S, Wang C, Jang DW. Radiographic characterization of the retroantral ethmoid cell. Int Forum Allergy Rhinol. 2016;6(12):1315–1318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chiu AG, Vaughan WC. Revision endoscopic frontal sinus surgery with surgical navigation. Otolaryngol Head Neck Surg. 2004;130(3):312–318. [DOI] [PubMed] [Google Scholar]
- 20.Chu CT, Lebowitz RA, Jacobs JB. An analysis of sites of disease in revision endoscopic sinus surgery. Am J Rhinol. 1997;11(4):287–291. [DOI] [PubMed] [Google Scholar]
- 21.El-Shiekh AM. Revision endoscopic sinus surgery: my experience. Al-Azhar Assiut Med J. 2015;13:1–6. [Google Scholar]
- 22.Fu T, Lee D, Yip J, Jamal A, Lee JM. Impact of septal deviation on recurrent chronic rhinosinusitis after primary surgery: a matched case-control study. Otolaryngol Head Neck Surg. 2019; 160(5):922–927. [DOI] [PubMed] [Google Scholar]
- 23.Gore MR, Ebert CS Jr., Zanation AM Senior BA. Beyond the “central sinus”: radiographic findings in patients undergoing revision functional endoscopic sinus surgery. Int Forum Allergy Rhinol. 2013;3(2):139–146. [DOI] [PubMed] [Google Scholar]
- 24.Goyal P, Gupta A, Kaur I. Radiological and endoscopic findings in 50 cases of recurrent sinusitis undergoing revision endoscopic sinus surgery. J Evolution Med Dent Sci. 2016;5(97):7101–7104. [Google Scholar]
- 25.Herzallah IR, Saati FA, Marglani OA, Simsim RF. Retromaxillary pneumatization of posterior ethmoid air cells: novel description and surgical implications. Otolaryngol Head Neck Surg. 2016;155(2):340–346. [DOI] [PubMed] [Google Scholar]
- 26.Khalil HS, Eweiss AZ, Clifton N. Radiological findings in patients undergoing revision endoscopic sinus surgery: a retrospective case series study. BMC Ear Nose Throat Disord. 2011;11:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kuan EC, Mallen-St Clair J, Frederick JW, et al. Significance of undissected retromaxillary air cells as a risk factor for revision endoscopic sinus surgery. AmJRhinolAllergy. 2016;30(6):448–452. [DOI] [PubMed] [Google Scholar]
- 28.Mansour HA. Double J stent of frontal sinus outflow tract in revision frontal sinus surgery. J Laryngol Otol. 2013;127(1):43–47. [DOI] [PubMed] [Google Scholar]
- 29.Moses RL, Cornetta A, Atkins JP Jr, Roth M, Rosen MR, Keane WM. Revision endoscopic sinus surgery: the Thomas Jefferson University experience. Ear Nose Throat J. 1998;77(3):190, 193–195, 199–202. [PubMed] [Google Scholar]
- 30.Otto KJ, DelGaudio JM. Operative findings in the frontal recess at time of revision surgery. AmJOtolaryngol. 2010;31(3):175–180. [DOI] [PubMed] [Google Scholar]
- 31.Parsons DS, Stivers FE, Talbot AR. The missed ostium sequence and the surgical approach to revision functional endoscopic sinus surgery. Otolaryngol Clin North Am. 1996;29(1):169–183. [PubMed] [Google Scholar]
- 32.Rajwani A, Manji J, Finkelstein-Kulka A, et al. A retrospective review of six hundred and nineteen cases to determine the prevalence and factors associated with revision endoscopic sinus surgery in AFRS vs NON-AFRS patients. Clin Otolaryngol. 2018; 43(2):700–705. [DOI] [PubMed] [Google Scholar]
- 33.Ramadan HH. Surgical causes of failure in endoscopic sinus surgery. Laryngoscope. 1999;109(1):27–29. [DOI] [PubMed] [Google Scholar]
- 34.Richtsmeier WJ. Top 10 reasons for endoscopic maxillary sinus surgery failure. Laryngoscope. 2001;111(11, pt 1):1952–1956. [DOI] [PubMed] [Google Scholar]
- 35.Socher JA, Mello J, Baltha BB. Tomographical findings in adult patients undergoing endoscopic sinus surgery revision. Int Arch Otorhinolaryngol. 2018;22(1):73–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Valdes CJ, Bogado M, Samaha M. Causes of failure in endoscopic frontal sinus surgery in chronic rhinosinusitis patients. Int Forum Allergy Rhinol. 2014;4(6):502–506. [DOI] [PubMed] [Google Scholar]
- 37.Govindaraj S, Agbetoba A, Becker S. Revision sinus surgery. Oral Maxillofac Surg Clin North Am. 2012;24(2):285–293, ix. [DOI] [PubMed] [Google Scholar]
- 38.Bhatti MT. Neuro-ophthalmic complications of endoscopic sinus surgery. Curr Opin Ophthalmol. 2007;18(6):450–458. [DOI] [PubMed] [Google Scholar]
- 39.Wigand ME, Hosemann WG. Results of endoscopic surgery of the paranasal sinuses and anterior skull base. J Otolaryngol. 1991;20(6):385–390. [PubMed] [Google Scholar]
- 40.Stankiewicz JA, Lal D, Connor M, Welch K. Complications in endoscopic sinus surgery for chronic rhinosinusitis: a 25-year experience. Laryngoscope. 2011;121(12):2684–2701. [DOI] [PubMed] [Google Scholar]
- 41.Fudickar A, Hörle K, Wiltfang J, Bein B. The effect of the WHO Surgical Safety Checklist on complication rate and communication. Dtsch Arztebl Int. 2012;109(42):695–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Boyd J, Wu G, Stelfox H. The impact of checklists on inpatient safety outcomes: a systematic review of randomized controlled trials. J Hosp Med. 2017;12(8):675–682. [DOI] [PubMed] [Google Scholar]
- 43.O’Brien WT, Hamelin S, Weitzel EK. The preoperative sinus CT: Avoiding a “CLOSE” call with surgical complications. Radiology. 2016;281(1):10–21. [DOI] [PubMed] [Google Scholar]
- 44.Huang BY, Lloyd KM, DelGaudio JM, Jablonowski E, Hudgins PA. Failed endoscopic sinus surgery: spectrum of CT findings in the frontal recess. Radiographics. 2009;29(1):177–195. [DOI] [PubMed] [Google Scholar]
- 45.Roy M, Lade H. Functional endoscopic sinus surgery of nasal polyposis: the vexing question of whether to resect or preserve middle turbinate. Indian J Otolaryngol Head Neck Surg. 2019; 71(suppl 3):2025–2030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dolci RLL, de Carvalho ACM, Rickli JCK, et al. Relationship between the bilateral removal of the middle nasal turbinate and the olfactory function in endoscopic skull base surgery. World Neurosurg. 2020;142:e337–e343. [DOI] [PubMed] [Google Scholar]
- 47.Hudon MA, Wright ED, Fortin-Pellerin E, Bussieres M. Resection versus preservation of the middle turbinate in surgery for chronic rhinosinusitis with nasal polyposis: a randomized controlled trial. J Otolaryngol Head Neck Surg. 2018;47(1):67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Alam S, Li C, Bradburn KH, Zhao K, Lee TS. Impact of middle turbinectomy on airflow to the olfactory cleft: a computational fluid dynamics study. Am J Rhinol Allergy. 2019;33(3):263–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Khafagy Y, Ghonim M, Elzayat S, Elgendy A. Comparison between the endoscopic scores of bolgerization versus partial resection of the middle turbinate for management of the postoperative lateralization in the early follow-up period after endoscopic frontal sinusotomy: a randomized controlled study. Am J Otolaryngol. 2021;42(5):102998. [DOI] [PubMed] [Google Scholar]
- 50.Li L, Han D, Zhang L, et al. Aerodynamic investigation of the correlation between nasal septal deviation and chronic rhinosinusitis. Laryngoscope. 2012;122(9):1915–1919. [DOI] [PubMed] [Google Scholar]
- 51.Chiu AG, Palmer JN, Adappa ND. Atlas of Endoscopic Sinus and Skull Base Surgery. Elsevier; 2019. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


