ABSTRACT
A large proportion of patients who completely recovered from acute coronavirus disease 2019 (COVID-19) infection later continued to experience symptoms even after recovery, irrespective of the severity of the disease. Various terms with varying duration were used for those who had persistent symptoms, of which cough was the most common. We systematically searched the published literature concerning post-COVID-19 cough, its prevalence, and the potential ways to reduce it in clinical practice. The aim of this review was to provide an overview of existing literature concerning post-COVID-19 cough. Literature shows that augmented cough reflex sensitivity is responsible for persistent cough after acute viral upper respiratory infection (URI). Overall, the heightened cough reflex associated with SARSCoV2 induces neurotropism, neuroinflammation, and neuroimmunomodulation via the vagal sensory nerves. Therapies for post-COVID-19 cough aim at the suppression of cough reflex. For a patient who does not respond to early symptomatic treatment, Inhaled corticosteroids can be given a trial to suppress airway inflammation. More trials of novel cough therapies in patients with post-COVID-19 cough using various outcome measures need to be studied in future research. Several agents are currently available for symptomatic relief. However, non-response or refractory cough continues to preclude adequate symptom relief.
KEY WORDS: Cough, inhaled steroids, post-COVID
INTRODUCTION
A large proportion of patients acute coronavirus disease 2019 (COVID-19) infection later continued to experience symptoms even after recovery, irrespective of the severity of the disease. All the symptoms that occur during acute or follow-up and persist beyond four weeks of COVID-19 diagnosis were labelled by many authors as ‘long COVID’.[1] This term has been used in multiple ways in literature and is further classified according to National Institute for Health and Care Excellence (NICE) guidelines as ‘Ongoing symptomatic COVID-19’ with signs and symptoms persisting from four weeks to twelve weeks and ‘Post-COVID-19 syndrome’ with signs and symptoms developing during or after acute COVID-19 infection persisting more than 12 weeks and not explained by any alternative diagnosis.[2] Greenhalgh et al.[3] used the terms ‘post-acute COVID-19’ (from 3 to 12 weeks) and ‘chronic COVID-19’ for symptoms extending beyond 12 weeks. However, one of the most common persisting symptoms after COVID-19 infection is cough.[4] Over time, this cough can develop into a vicious cycle, where excessive coughing leads to irritation and inflammation and further worsens the cough. Here, we systematically searched the published literature concerning post-COVID-19 cough, its prevalence and the potential ways to reduce it in clinical practice.
MATERIALS AND METHODS
Due to the rapidity of the new research during the COVID-19 pandemic, many systematic reviews conducted in the earlier phase soon became redundant.
Here, we did a literature search on the PubMed database using the following keywords (POST SARS-CoV-2 or POST COVID-19 or LONG COVID) and (COUGH), and included all the studies published in 2021. Peer-reviewed studies were considered eligible if the sample size of at least 100 with laboratory-confirmed and/or clinically diagnosed COVID-19. A total of 209 articles were searched, and 176 free full texts were retrieved by our search strategy. We screened the titles and abstracts to identify relevant studies, and all the references that did not fit into the inclusion criteria were eliminated. A few more articles were identified through manual searching, bringing the total number of included articles to 22.
PREVALENCE
The aim of this review was to provide an overview of existing literature concerning post-COVID-19 cough. Previously published long COVID disability 2020 reports showed that 10%–20% of COVID-19 patients do experience some symptoms, including cough, for months.[5] Further, cough categorisation has been done as acute (lasting less than three weeks), subacute (lasting between three and eight weeks) and chronic (persisting for more than eight weeks).[6] The prevalence of chronic cough after SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus-2) varies across studies found in literature ranging from 2.1%[7] to as high as 73%[8] [Table 1].
Table 1.
Follow-up studies looked on prevalence of cough after recovery from COVID-19
| Author | Country | Sample | Mean/Median age (years) | Age Male % | Severe COVID (%) | Follow-up Period (month) | Prevalence of Cough |
|---|---|---|---|---|---|---|---|
| Reaz Mahmud et al.[9] | Dhaka, Bangladesh | 355 | 39.8 | 58.3% | 11 | 1 | 18.3% |
| Melina Michael et al.[10] | Metanalysis study (BMJ) 12 countries | 5031 | Not Applicable | 52% | NOT REPORTED | >3 | 8.17% |
| Angelo Carfi et al.[11] | Rome, Italy | 143 | 56.5 | 63% | 53.8 | 2 | 16% |
| Destin Groff et al.[12] | Systematic Review of 57 studies | 250351 | 54.4 | 56% | 79 | 6 | 13.1% [5.3-22.6%] |
| Menges et al.[13] | Zurich, Switzerland | 431 | 47 | 50% | NOT REPORTED | 8 | 39% |
| Qu Guangbo et al.[14] | Multicentric, Anhui Province and Hubei Province | 540 | 47.5 | 50% | 9.4 | 3 | 11% |
| Fabio Anastasio et al.[15] | Italy | 379 | 45.9 | 56% | 60.8 | 4 | 6.1% |
| Rebecca F. D’Cruz et al.[16] | King’s College Hospital, UK | 119 | 58.7 | 62% | 100% | 2 | 7% |
| Taquet M et al.[17] | Oxford University Hospitals, UK | 273618 | 46.3 | 44.4% | NOT REPORTED | 6 | 12.6% |
| Xiong et al.[18] | Wuhan, China | 538 | 52 | 45.5% | 38.4% | 3 | 7.1% |
| Arnold et al.[19] | Bristol, UK | 110 | 60 | 56% | 16.4% | 3 | 11% |
| Bellan M et al.[20] | Northern Italy | 238 | 61 | 59.7% | 72% | 4 | 6% |
| Dennis A et al.[21] | London, UK | 201 | 44 | 29% | 18.4% | 4 | 73.6% |
| Han X et al.[22] | Wuhan, China | 114 | 54 | 70% | 21% | 6 | 6.1% |
| Stavem K et al.[23] | Lorenskog, Norway | 434 | 49.8 | 44% | Not reported, All OPD patients included | 4 | 6% |
| Karaarslan et al.[24] | Ankara, Turkey | 300 | 52.5 | 59.7% | Not mentioned | 1 | 14 |
| Huang et al.[25] | China | 1733 | 57 | 52% | 68% | 6 | 4% |
| Moreno-Perez O et al.[26] | Spain | 277 | 56 | 52.7% | 65.7% | 3.5 | 21.3% |
| Rosales Castillo et al.[27] | Spain | 118 | 60.16 | 55.9% | 7.6% | 2 | 65.3% |
| Fernández-de-Las-Peñas et al.[28] | Multicentre study @ Spain | 1950 | 61 | 53% | 6.6% | 11.2 | 2.5% |
| Naik S et al.[29] | Northern India | 1234 | 41.6 | 69.4% | 33% | 3 | 2.1% |
| Sathyamurthi et al.[30] | Armonk, New York | 279 | 71.1 | 63.8% | 41.6% | 3 | 4.3% |
PATHOPHYSIOLOGY
Literature shows that augmented cough reflex sensitivity is responsible for persistent cough after acute viral upper respiratory infection (URI).[31,32] However, the major question is whether SARS-CoV-2 induces a cough similar to other viral URI or has some other pathophysiology. Different hypotheses explaining the emergence of coughing due to SARS-CoV-2 infection can be found in the literature. The respiratory epithelium is the primary site of entrance for SARS-CoV-2 and the vagal sensory nerves, which tend to terminate in the epithelium and sub-epithelial mucosa of the human airways, play a key role in regulating cough.[33] For cellular entry on mucosal surfaces, SARS-CoV-2 uses the cell surface protein angiotensin-converting enzyme type 2 (ACE2),[34] which is richly expressed in upper and lower airway epithelial cells. Although this enzyme has numerous functions, one of the functions is to regulate mucosal concentrations of bradykinin (a pro-inflammatory cytokine) and hence evoke coughing.[35,36] Pneumonia and acute lung injury caused by COVID-19 infection mainly involve the most peripheral conducting airways and alveoli, compared to other viral pneumonia. Eventually, SARS-CoV-2 impacts the large conducting airways (larynx, trachea and mainstem bronchi), peripheral airways and alveoli.[37,38] There is another controversy about the low incidence of persistent cough in COVID-19, especially in severe cases as compared to mild to moderate cases due to preferential involvement of lower airway and pneumonia, although more studies are required in this field. The variant of SARS-CoV-2 also has a variable prediction of the airway, as the delta variant predominantly involves the lower airway while the omicron involves the upper airway. Studies also show that C-fibre terminating in the upper and lower airways is responsible for transducing cough and causing the sensation of dyspnoea, respectively. Overall, the heightened cough reflex associated with SARS-CoV-2 induces neurotropism, neuroinflammation and neuroimmunomodulation via the vagal sensory nerves.[39]
DIAGNOSTIC APPROACH
The cough lasting for more than three weeks (subacute to chronic) from diagnosis of COVID-19 needs to be evaluated. A persistent cough (defined here as cough persisting for >3 weeks) in COVID-19 can be due to enhanced cough reflex due to SARS-CoV-2, COVID-19 pulmonary sequelae, aggravation of pre-existing lung disease or secondary infection, like bacterial, fungal or tuberculosis. Other common causes of chronic cough like a history of ACE inhibitors, cough variant asthma, GERD, etc., should also be considered as non-COVID conditions. Post-COVID-19 fungal complications shall also be considered as one of the differentials of cough in a subset of patients. A case series of seven post-COVID-19 patients showed pulmonary cavitation attributed to COVID-19-associated pulmonary aspergillosis (CAPA) in 5, mucormycosis in 1 and mycobacterium tuberculosis infection in another.[40] The history and clinical examination are always vital in the evaluation of any symptoms. Patients with a persistent cough should be evaluated with a chest X-ray PA view and a comparison with previous imaging must be done. In suspected cases, CT chest may be performed for further characterisation of opacity seen on chest X-ray. If chest X-ray is normal or consists of post-COVID-19 residual changes without any new opacity then consider the possibility of a post-viral enhanced cough reflex, which would subside during follow-up. SARS-CoV-2 infection may be a cause for the worsening of pre-existing lung diseases that need to be optimised with treatment. COVID-19 patients may develop tuberculosis, fungal (COVID-associated pulmonary mycosis) and bacterial infection in patients with new opacity on chest X-rays. The diagnostic approach is summarised in Figure 1.
Figure 1.
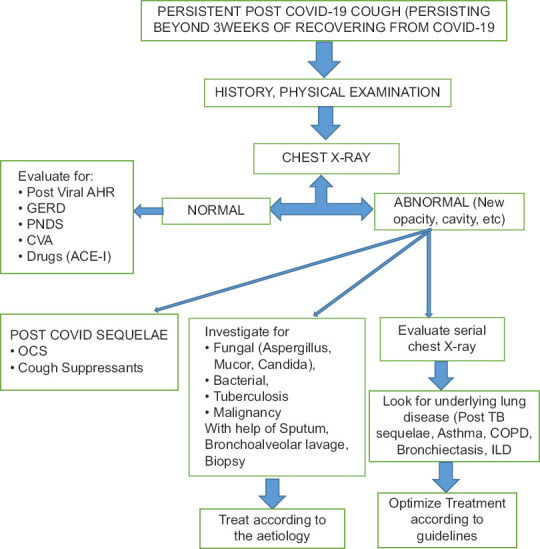
Overview of the evaluation of Persistent post-COVID-19 cough. ACE-I: angiotensin converting enzyme inhibitor; AHR: Airway Hyperreactivity; CVA: Cough Variant Asthma; PNDS: post-nasal drip syndrome; GERD: gastro-oesophageal reflux disease; COPD: Chronic Obstructive Pulmonary Disease; ILD: Interstitial lung disease
TREATMENT
Therapies for post-COVID-19 cough aim at the suppression of cough reflex. In such patients, several potential causes of chronic cough must be excluded before chronic cough may be considered directly linked to COVID-19. So aiming at suppression of the cough reflex, we have drugs that suppress the central cough reflex (dextromethorphan, gabapentin, amitriptyline and opioids),[8,41] drugs that suppress sensory neurons (lidocaine, benzonatate)[42] and those that are believed to act on airways to reduce inflammation, smooth muscle contraction and mucus secretion (beta-agonists, leukotriene antagonists, macrolide antibiotics).[43] Patients with chronic cough also often seek antitussive therapies, but it is unknown to a larger extent whether such approaches are effective in post-COVID-19 cough patients. Inhaled tiotropium also elucidates antitussive action in studies by inhibiting cough reflex sensitivity to capsaicin apart from bronchodilation.[44]
For a dry cough, we have cough syrups with the main ingredient being dextromethorphan, butamirate, dropropizine and levodropropizine. For cough with expectoration, we have medications that help to modify the character of mucus and reduce its viscosity, thereby easing expectoration (ambroxol, bromhexine, acetylcysteine, carbocysteine) that can be used in post-COVID-19 patients. Antihistaminics[45] and CystLT1 receptor antagonists (Montelukast)[46] have shown promising results in post-COVID-19 cough as evidenced by various clinical trials.
Several agents have been evaluated for long COVID cough that can be considered in daily practice [Table 2]. A role for inhaled steroids is not established but is possible.[47,48] According to Swiss recommendations, it is recommended to give empiric inhaled topical steroids in patients with long COVID cough.[49] Drugs like pregabalin[50] and gabapentin[51] have been shown to improve cough severity, cough frequency and QoL of patients with chronic cough. These neuromodulators can be considered for the post-COVID-19 syndrome for other symptoms accompanying cough, such as pain, but beware of their potential to worsen any cognitive dysfunction.[41] Newer investigational drug AF-219 (Gefapixant),[52] a P2X3 receptor antagonist, showed very promising phase two results in chronic cough, and its use in COVID-19-associated cough can be supported by the evidence that ACE2 is frequently co-expressed with P2X3 in dorsal root ganglion sensory neurons.[53] The endogenous receptor for substance P is neurokinin 1 receptor (NK1R) might also be a potential target for intervention, hence NK1R antagonists (aprepitant/orvepitant) can be tested in COVID-19 cough because TRPV1 in sensory neurons is upregulated by various viral infections (human rhinovirus).[7,54] TRPV-1 antagonist (SB-705498) showed a significant improvement in cough reflex sensitivity to capsaicin at 2 hours and a borderline significant improvement at 24 hours.[55]
Table 2.
Pharmacological treatment for post-COVID cough
| Drug Class | Examples | Citing studies | Sample size | Dose and Duration | Remarks |
|---|---|---|---|---|---|
| Antihistaminics | Levocetirizine Dextromethorphan | Sepiashvili R et al. (2021)[45] | 56 | 80% of patients had sooth in cough as a symptom. | |
| Centrally acting antitussive drugs/Neuro-modulating drugs | Gabapentin | Ryan et al. (2012)[41] | 32 | 1800 mg od | Improved cough specific QoL |
| Soltani Rasool et al. (2022)[51] | 76 | 300 mg tds ×5 days | Improved cough frequency and severity | ||
| Pregabalin | Vertigan AE et al. (2016)[50] | 40 | 300 mg od ×4 weeks along with SPT$ | Reduces cough symptoms and improves QOL | |
| Leukotriene receptor antagonist (LTRA) | Monteleukast | Mohamed Hussein A.A.R. et al. (2022)[46] | 32 | 10 mg/day ×14 days | Decrease number of cough paroxysm/day, cough severity index, cough QoL, cough duration |
| P2X3 Antagonist | Gefapixant (AF-219/MK-7264) | McGarvey L P et al (2022)[52] | 244 | 45 mg bid ×12 wks (COUGH 1) | Reduction in 24 hour cough frequency and Improvement in cough questionnaire score |
| 440 | 45 mg bid ×24 wks (COUGH 2) | ||||
| Charged sodium channel blocker | NTX-1175 (Nebulised) | Ongoing trial (EuraCT 2020-004715-27)[56] | |||
| NK#-1 Receptor antagonist | Aprepitant Orvepitant | Smith J et al.[54] | 13 | 30 mg od ×4 weeks (VOLCANO 1) | Improvement in objective daytime cough frequency, cough VAS and QoL. |
| Muscarinic antagonist | Inhaled Tiotropium | Dicpinigaitis PV et al. (2008)[44] | 11 | 18 mcg od ×7 days | Inhibits cough reflex sensitivity to capsaicin |
| Inhaled steroids | Glycopyrronium/Formoterol/Budesonide | Yamaya M et al. (2020)[48] | Inhibit CoV replication partly and modulate infection-induced inflammation in the airway. | ||
| TRPV 1 antagonist* | SB-705498 | Khalid S et al. (2014)[55] | 21 | 600 mg single dose | Improvement in cough reflex sensitivity to capsaicin |
| Immunomodulatory drugs | Thalidomide | ClinicalTrials.gov Identifier: NCT04273529[57] | 100 mg od× 14 days (results not posted yet) | ||
| Mast cell stabilizer | Inhaled Sodium Cromoglycate | ClinicalTrials.gov Identifier: NCT05077917[58] | 2 ml of 1% cromolyn sodium solution delivered via nebulizer 4 times a day for 4 days followed by 4% cromolyn solution administered intranasally 4 times per day for 14 days | ||
*TRPV 1 - Transient receptor potential vanilloid 1. #NK-1 - Neurokinin-1
Thalidomide has also shown promising results in controlling the disabling cough in ILD patients at a dose of 50–100 mg per day dosing. Thalidomide has been shown to reduce persistent cough and lung damage, improving patient life quality. It appears to be able to do this by blocking the inflammatory response.[59] Thus, thalidomide can also be further studied in research among the potential drugs for treating respiratory complications associated with COVID-19 based on its potent anti-inflammatory properties and its activity in attenuating exaggerated inflammation and cytokine storms. It is also known to be an upregulator for NK and T cells and thus can reverse the down-regulatory effect of COVID-19.[57]
Inhaled PA101 (Sodium Cromoglycate) 40 mg TDS could be a treatment option, and it has been studied for chronic cough in patients with IPF. Studies showed that it reduced daytime cough frequency by 31·1%, from a mean of 55 coughs per hour at baseline to 39 coughs per hour at day 14.[60] Mast cell activation in response to viral infection (COVID-19) may lead to protective function by directly fighting infection or helping the immune system. However, extensive mast cell activation leads to increased levels of inflammatory cytokine and chemokine release that further worsen inflammation and increase disease severity.[58] Few drugs like NTX-1175, a permanently charged sodium channel blocker, are yet under phase II clinical trials.[56]
Along with pharmacological treatment, other measures can be incorporated in patients recovering from a post-COVID-19 syndrome, including speech and language therapy along with physiotherapy, including slow, deep breath and gentle, relaxed breathing and huffing.[61]
Clinicians and researchers have focused on the acute phase of COVID-19, but continued monitoring after discharge for long-lasting effects is needed. In this review, we tried to focus on the epidemiology, pathophysiology and possible management of post-COVID-19 cough, which could help clinicians in their daily practice. More randomized control trials (RCTs) of novel cough therapies in patients with post-COVID-19 cough using various outcome measures need to be studied in future research.
CONCLUSION
The majority of patients with persistent cough following SARS-CoV-2 infection are due to residual airway inflammation leading to hyperreactivity airway. The symptomatic treatment in the form of a cough suppressant, cysteine leukotriene, may be an attempt for relief. It is important to remember that SARS–CoV-2 infection may be a cause for the overt manifestation of pre-existing subclinical allergic bronchitis. Chest X-ray, markers of allergic inflammation [blood eosinophil, Fractional exhalation of Nitric oxide (FeNO), Serum total IgE] and spirometry may help in identifying the underlying cause and accordingly treatment. For a patient who does not respond to early symptomatic treatment, Inhaled corticosteroids can be given a trial to suppress airway inflammation. There are many investigational drugs that are yet under evaluation for persistent cough due to non-COVID aetiology or idiopathic cause and can be attempted in refractory cases. However, there is a dire need at present to establish recommendations or guidelines from a major association.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Halpin SJ, McIvor C, Whyatt G, Adams A, Harvey O, McLean L, et al. Post discharge symptoms and rehabilitation needs in survivors of COVID-19 infection:A cross-sectional evaluation. J Med Virol. 2021;93:1013–22. doi: 10.1002/jmv.26368. [DOI] [PubMed] [Google Scholar]
- 2.COVID-19 rapid guideline: Managing the longterm effects of COVID-19-NICE, RCGP, and SIGN. version 1.20 [Google Scholar]
- 3.Greenhalgh T, Knight M, A’Court C, Buxton M, Husain L Management of post-acute covid-19 in primary care. BMJ. 2020;370:m3026. doi: 10.1136/bmj.m3026. doi: 10.1136/bmj.m3026. [DOI] [PubMed] [Google Scholar]
- 4.Post-COVID Conditions. CDC. [[Last accessed on 2022 Apr 09]]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html .
- 5.Wulf Hanson S, Abbafati C, Aerts JG, Al-Aly Z, Ashbaugh C, Ballouz T, et al. A global systematic analysis of the occurrence, severity, and recovery pattern of long COVID in 2020 and 2021. medRxiv [Preprint] 2022 2022.05.26.22275532. doi: 10.1101/2022.05.26.22275532. PMID: 35664995. PMCID: PMC9164454. [Google Scholar]
- 6.Irwin RS, Baumann MH, Bolser DC, Boulet LP, Braman SS, Brightling CE, et al. Diagnosis and management of cough executive summary:ACCP evidence-based clinical practice guidelines. Chest. 2006;129:1S. doi: 10.1378/chest.129.1_suppl.1S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abdullah H, Heaney LG, Cosby SL, McGarvey LP. Rhinovirus upregulates transient receptor potential channels in a human neuronal cell line:Implications for respiratory virus-induced cough reflex sensitivity. Thorax. 2014;69:46–54. doi: 10.1136/thoraxjnl-2013-203894. [DOI] [PubMed] [Google Scholar]
- 8.Morice AH, Fontana GA, Belvisi MG, Birring SS, Chung KF, Dicpinigaitis PV, et al. ERS guidelines on the assessment of cough. Eur Respir J. 2007;29:1256–76. doi: 10.1183/09031936.00101006. [DOI] [PubMed] [Google Scholar]
- 9.Mahmud R, Rahman MM, Rassel MA, Monayem FB, Sayeed SKJB, Islam MS, et al. Post-COVID-19 syndrome among symptomatic COVID-19 patients:A prospective cohort study in a tertiary care center of Bangladesh. PLoS One. 2021;16:e0249644. doi: 10.1371/journal.pone.0249644. doi:10.1371/journal.pone. 0249644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Michelen M, Manoharan L, Elkheir N, Cheng V, Dagens A, Hastie C, et al. Characterising long COVID:A living systematic review. BMJ Global Health. 2021;6:e005427. doi: 10.1136/bmjgh-2021-005427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carfì A, Bernabei R, Landi F Gemelli Against COVID-19 Post-Acute Care Study Group. Persistent symptoms in patients after acute COVID-19. JAMA. 2020;324:603–5. doi: 10.1001/jama.2020.12603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Groff D, Sun A, Ssentongo AE, Ba DM, Parsons N, Poudel GR, et al. Short-term and long-term rates of postacute sequelae of SARS-CoV-2 infection:A systematic review. JAMA Network Open. 2021;4:e2128568. doi: 10.1001/jamanetworkopen.2021.28568. doi:10.1001/jamanetworkopen. 2021.28568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Menges D, Ballouz T, Anagnostopoulos A, Aschmann HE, Domenghino A, Fehr JS, et al. Burden of post-COVID-19 syndrome and implications for healthcare service planning:A population-based cohort study. PLoS One. 2021;16:e0254523. doi: 10.1371/journal.pone.0254523. doi:10.1371/journal.pone. 0254523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Qu G, Zhen Q, Wang W, Fan S, Wu Q, Zhang C, et al. Health-related quality of life of COVID-19 patients after discharge:A multicenter follow-up study. J Clin Nurs. 2021;30:1742–50. doi: 10.1111/jocn.15733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Anastasio F, Barbuto S, Scarnecchia E, Cosma P, Fugagnoli P, Rossi G, et al. Medium-term impact of COVID-19 on pulmonary function, functional capacity and quality of life. Eur Respir J. 2021;58:2004015. doi: 10.1183/13993003.04015-2020. doi:10.1183/13993003.04015-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.D’Cruz RF, Waller MD, Perrin F, Periselneris J, Norton S, Smith LJ, et al. Chest radiography is a poor predictor of respiratory symptoms and functional impairment in survivors of severe COVID-19 pneumonia. ERJ Open Res. 2021;7:00655–2020. doi: 10.1183/23120541.00655-2020. doi:10.1183/23120541.00655-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Taquet M, Dercon Q, Luciano S, Geddes JR, Husain M, Harrison PJ. Incidence, co-occurrence, and evolution of long-COVID features:A 6-month retrospective cohort study of 273,618 survivors of COVID-19. PLoS Med. 2021;18:e1003773. doi: 10.1371/journal.pmed.1003773. doi:10.1371/journal.pmed. 1003773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Xiong Q, Xu M, Li J, Liu Y, Zhang J, Xu Y, et al. Clinical sequelae of COVID-19 survivors in Wuhan, China:A single-centre longitudinal study. Clin Microbiol Infect. 2021;27:89–95. doi: 10.1016/j.cmi.2020.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Arnold DT, Hamilton FW, Milne A, Morley AJ, Viner J, Attwood M, et al. Patient outcomes after hospitalisation with COVID-19 and implications for follow-up:Results from a prospective UK cohort. Thorax. 2021;76:399–401. doi: 10.1136/thoraxjnl-2020-216086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bellan M, Soddu D, Balbo PE, Baricich A, Zeppegno P, Avanzi GC, et al. Respiratory and psychophysical sequelae among patients with COVID-19 four months after hospital discharge. JAMA Network Open. 2021;4:e2036142. doi: 10.1001/jamanetworkopen.2020.36142. doi:10.1001/jamanetworkopen. 2020.36142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dennis A, Wamil M, Alberts J, Oben J, Cuthbertson DJ, Wootton D, et al. Multiorgan impairment in low-risk individuals with post-COVID-19 syndrome:A prospective, community-based study. BMJ Open. 2021;11:e048391. doi: 10.1136/bmjopen-2020-048391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Han X, Fan Y, Alwalid O, Li N, Jia X, Yuan M, et al. Six-month follow-up chest CT findings after severe COVID-19 pneumonia. Radiology. 2021;299:E177–86. doi: 10.1148/radiol.2021203153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stavem K, Ghanima W, Olsen MK, Gilboe HM, Einvik G. Persistent symptoms 1.5-6 months after COVID-19 in non-hospitalised subjects:A population-based cohort study. Thorax. 2021;76:405–7. doi: 10.1136/thoraxjnl-2020-216377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Karaarslan F, Demircioğlu Güneri F, Kardeş S. Postdischarge rheumatic and musculoskeletal symptoms following hospitalization for COVID-19:Prospective follow-up by phone interviews. Rheumatol Int. 2021;41:1263–71. doi: 10.1007/s00296-021-04882-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Huang C, Huang L, Wang Y, Li X, Ren L, Gu X, et al. 6-month consequences of COVID-19 in patients discharged from hospital:A cohort study. Lancet. 2021;397:220–32. doi: 10.1016/S0140-6736(20)32656-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moreno-Pérez O, Merino E, Leon-Ramirez JM, Andres M, Ramos JM, Arenas-Jiménez J, et al. Post-acute COVID-19 syndrome. Incidence and risk factors:A Mediterranean cohort study. J Infect. 2021;82:378–83. doi: 10.1016/j.jinf.2021.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rosales-Castillo A, de Los G, Ríos C, Mediavilla García JD. Persistent symptoms after acute COVID-19 infection:Importance of follow-up. Persistencia de manifestaciones clínicas tras la infección COVID-19:Importancia del seguimiento. Med Clin (Barc) 2021;156:35–6. doi: 10.1016/j.medcli.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fernández-de-Las-Peñas C, Guijarro C, Plaza-Canteli S, Hernández-Barrera V, Torres-Macho J. Prevalence of post-COVID-19 cough one year after SARS-CoV-2 infection:A multicenter study. Lung. 2021;199:249–53. doi: 10.1007/s00408-021-00450-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Naik S, Haldar SN, Soneja M, Mundadan NG, Garg P, Mittal A, et al. Post COVID-19 sequelae:A prospective observational study from Northern India. Drug Discov Ther. 2021;15:254–60. doi: 10.5582/ddt.2021.01093. [DOI] [PubMed] [Google Scholar]
- 30.Sathyamurthy P, Madhavan S, Pandurangan V. Prevalence, pattern and functional outcome of post COVID-19 syndrome in older adults. Cureus. 2021;13:e17189. doi: 10.7759/cureus.17189. doi:10.7759/cureus. 17189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dicpinigaitis PV, Bhat R, Rhoton WA, Tibb AS, Negassa A. Effect of viral upper respiratory tract infection on the urge-to-cough sensation. Respir Med. 2011;105:615–8. doi: 10.1016/j.rmed.2010.12.002. [DOI] [PubMed] [Google Scholar]
- 32.Dicpinigaitis PV, Tibb AS, Ramsey DL, Carr AN, Poore CL. Stability of cough reflex sensitivity during viral upper respiratory tract infection (common cold) Pulm Pharmacol Ther. 2014;28:154–57. doi: 10.1016/j.pupt.2014.05.004. [DOI] [PubMed] [Google Scholar]
- 33.West PW, Canning BJ, Merlo-Pich E, Woodcock AA, Smith JA. Morphologic characterization of nerves in whole-mount airway biopsies. Am J Respir Crit Care Med. 2015;192:30–9. doi: 10.1164/rccm.201412-2293OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Scialo F, Daniele A, Amato F, Pastore L, Matera MG, Cazzola M, et al. ACE2:The major cell entry receptor for SARS-CoV-2. Lung. 2020;198:867–88. doi: 10.1007/s00408-020-00408-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Colarusso C, Terlizzi M, Pinto A. Sorrentino Rt A lesson from a saboteur:High-MW kininogen impact in coronavirus-induced disease 2019. Br J Pharmacol. 2020;177:4866–72. doi: 10.1111/bph.15154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hewitt MM, Adams G, Jr, Mazzone SB, Mori N, Yu L, Canning BJ. Pharmacology of bradykinin-evoked coughing in guinea pigs. J Pharmacol Exp Ther. 2016;357:620–8. doi: 10.1124/jpet.115.230383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Undem BJ, Chuaychoo B, Lee MG, Weinreich D, Myers AC, Kollarik M. Subtypes of vagal aferent C-fbres in guinea-pig lungs. J Physiol. 2004;556:905–17. doi: 10.1113/jphysiol.2003.060079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chou YL, Scarupa MD, Mori N, Canning BJ. Differential efects of airway aferent nerve subtypes on cough and respiration in anesthetized guinea pigs. Am J Physiol Regul Integr Comp Physiol. 2008;295:R1572–84. doi: 10.1152/ajpregu.90382.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Song WJ, Hui C, Hull JH, Birring SS, McGarvey L, Mazzone SB, et al. Confronting COVID-19-associated cough and the post-COVID syndrome:Role of viral neurotropism, neuroinflammation, and neuroimmune responses. Lancet. Respiratory Med. 2021;9:533–44. doi: 10.1016/S2213-2600(21)00125-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rai DK, Priyadarshi RK, Karmakar S. Study to assess aetiology, clinical and imaging characteristics of post Covid-19 pulmonary cavitation. J Family Med Prim Care. 2022;11:739–43. doi: 10.4103/jfmpc.jfmpc_1425_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ryan NM, Birring SS, Gibson PG. Gabapentin for refractory chronic cough:A randomised, double-blind, placebo-controlled trial. Lancet. 2012;380:1583–9. doi: 10.1016/S0140-6736(12)60776-4. [DOI] [PubMed] [Google Scholar]
- 42.Lim KG, Rank MA, Hahn PY, Keogh KA, Morgenthaler TI, Olson EJ. Long-term safety of nebulized lidocaine for adults with difficult-to-control chronic cough:A case series. Chest. 2013;143:1060–5. doi: 10.1378/chest.12-1533. [DOI] [PubMed] [Google Scholar]
- 43.Spina D, McFadzean I, Bertram FK, Page CP. Peripheral mechanisms II:The pharmacology of peripherally active antitussive drugs. Handb Exp Pharmacol. 2009;187:155–86. doi: 10.1007/978-3-540-79842-2_8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dicpinigaitis PV, Spinner L, Santhyadka G, Negassa A. Effect of tiotropium on cough reflex sensitivity in acute viral cough. Lung. 2008;186:369–74. doi: 10.1007/s00408-008-9114-6. [DOI] [PubMed] [Google Scholar]
- 45.Sepiashvili R, Chikhladze M, Slavyanskaya T, Gamkredlidze S, Khachapuridze D. Role of antihistamines in the management of COVID-19 infection. Allergy: European Journal of Allergy and Clinical Immunology. 2021;76((SUPPL 110)):492. Article in English | EMBASE | ID: covidwho-1570415. [Google Scholar]
- 46.Mohamed Hussein AAR, Ibrahim MEAA, Makhlouf HA, Makhlouf NA, Abd-Elaal HK, Kholief K, et al. Value of montelukast as a potential treatment of post-COVID-19 persistent cough:A non-randomized controlled pilot study. Egypt J Bronchol. 2022;16:52. doi:10.1186/s43168-022-00154-6. [Google Scholar]
- 47.Tanaka H, Tsunematsu K, Nakamura N, Suzuki K, Tanaka N, Takeya I, et al. Successful treatment of hypersensitivity pneumonitis caused by grifola frondosa (Maitake) mushroom using a HFA-BDP extra-fine aerosol. Intern Med. 2004;432004 doi: 10.2169/internalmedicine.43.737. [DOI] [PubMed] [Google Scholar]
- 48.Yamaya M, Nishimura H, Deng X, Sugawara M, Watanabe O, Nomura K, et al. Inhibitory effects of glycopyrronium, formoterol, and budesonide on coronavirus HCoV-229E replication and cytokine production by primary cultures of human nasal and tracheal epithelial cells. Respir Investig. 2020;58:155–68. doi: 10.1016/j.resinv.2019.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Funke-Chambour M, Bridevaux PO, Clarenbach CF, Soccal PM, Nicod LP, von Garnier C, et al. Swiss recommendations for the follow-up and treatment of pulmonary long COVID. Respiration. 2021;100:826–41. doi: 10.1159/000517255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Vertigan AE, Kapela SL, Ryan NM, Birring SS, McElduff P, Gibson PG. Pregabalin and speech pathology combination therapy for refractory chronic cough:A randomized controlled trial. Chest. 2016;149:639–48. doi: 10.1378/chest.15-1271. [DOI] [PubMed] [Google Scholar]
- 51.Soltani R, Nasirharandi S, Khorvash F, Nasirian M, Dolatshahi K, Hakamifard A. The effectiveness of gabapentin and gabapentin/montelukast combination compared with dextromethorphan in the improvement of COVID-19- related cough:A randomized, controlled clinical trial. Clin Respir J. 2022;16:604–10. doi: 10.1111/crj.13529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.McGarvey LP, Birring SS, Morice AH, Dicpinigaitis PV, Pavord ID, Schelfhout J, et al. Efficacy and safety of gefapixant, a P2X3 receptor antagonist, in refractory chronic cough and unexplained chronic cough (COUGH-1 and COUGH-2):Results from two double-blind, randomised, parallel-group, placebo-controlled, phase 3 trials. Lancet. 2022;399:909–23. doi: 10.1016/S0140-6736(21)02348-5. [DOI] [PubMed] [Google Scholar]
- 53.Shiers S, Ray PR, Wangzhou A. ACE2 and SCARF expression in human dorsal root ganglion nociceptors:Implications for SARS-CoV-2 virus neurological effects. Pain. 2020;161:2494–501. doi: 10.1097/j.pain.0000000000002051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Smith J, Allman D, Badri H. The neurokinin-1 receptor antagonist orvepitant is a novel antitussive therapy for chronic refractory cough:Results from a phase 2 pilot study (VOLCANO-1) Chest. 2020;157:111–8. doi: 10.1016/j.chest.2019.08.001. [DOI] [PubMed] [Google Scholar]
- 55.Khalid S, Murdoch R, Newlands A, Smart K, Kelsall A, Holt K, et al. Transient receptor potential vanilloid 1 (TRPV1) antagonism in patients with refractory chronic cough:A double-blind randomized controlled trial. J Allergy Clin Immunol. 2014;134:56–62. doi: 10.1016/j.jaci.2014.01.038. [DOI] [PubMed] [Google Scholar]
- 56.Nocion Therapeutics. A Phase 2a, Randomised, Double-Blind, Placebo-Controlled, Two-Part Study to Assess the Efficacy, Safety, Tolerability, and Pharmacokinetic Profiles of Inhaled Doses of NOC-100 in Adult Participants with Chronic Cough or Acute Cough, including Cough due to Postinfectious COVID-19. EuraCT 2020-004715-27. [[Last accessed on 2022 Oct 28]]; [Google Scholar]
- 57.The Efficacy and Safety of Thalidomide in the Adjuvant Treatment of Moderate New Coronavirus (COVID-19) Pneumonia. ClinicalTrials.gov Identifier: NCT04273529. [[Last accessed on 2022 May 11]]; [Google Scholar]
- 58.Cromolyn Sodium for Treatment of COVID-19 Pneumonia. ClinicalTrials.gov Identifier: NCT05077917. [[Last accessed on 2022 May 11]]; [Google Scholar]
- 59.Horton MR, Santopietro V, Mathew L, Horton KM, Polito AJ, Liu MC, et al. Thalidomide for the treatment of cough in idiopathic pulmonary fibrosis:A randomized trial. Ann Intern Med. 2012;157:398–406. doi: 10.7326/0003-4819-157-6-201209180-00003. [DOI] [PubMed] [Google Scholar]
- 60.Birring SS, Wijsenbeek MS, Agrawal S, van den Berg JWK, Stone H, Maher TM, et al. A novel formulation of inhaled sodium cromoglicate (PA101) in idiopathic pulmonary fibrosis and chronic cough:A randomised, double-blind, proof-of-concept, phase 2 trial. Lancet Respir Med. 2017;5:806–15. doi: 10.1016/S2213-2600(17)30310-7. [DOI] [PubMed] [Google Scholar]
- 61.Chamberlain Mitchell SA, Garrod R, Clark L. Physiotherapy, and speech and language therapy intervention for patients with refractory chronic cough:A multicentre randomised control trial. Thorax. 2017;72:129–36. doi: 10.1136/thoraxjnl-2016-208843. [DOI] [PubMed] [Google Scholar]


