ABSTRACT
The mediastinal teratomas can grow to a large size before becoming symptomatic. The symptoms are usually due to the compression of adjacent structures. A computed tomographic scan of the chest is the investigation of choice for making a provisional diagnosis and planning for further management. Removal of large mediastinal/thoracic teratoma can be associated with various intraoperative and postoperative complications, which can be life-threatening sometimes. We operated on a patient with a large mediastinal mass extending into the right thoracic cavity up to the costo-phrenic angle. The postoperative period was eventful and required judicious intensive care. The patient eventually recovered with conservative treatment. A literature search was done on PubMed using the keywords benign mediastinal teratoma. Case series/original articles published in the last two decades, that is, after the year 2000, were evaluated. As per the review of the literature, the prevalence of benign mediastinal teratoma may be higher in eastern countries. Thoracoscopic surgery is the preferred modality except for cases with adhesions or infiltration into surrounding structures.
KEY WORDS: Benign mediastinal teratoma, haemoptysis, mediastinal shift, postoperative complications, surgical excision
INTRODUCTION
Mediastinal mature cystic teratoma is a rare tumour that can grow to a large size and usually requires surgical intervention.[1] Mediastinal teratomas can be asymptomatic and diagnosed incidentally. However in symptomatic cases, chest pain, cough and breathlessness are the common presenting features and haemoptysis is rarely seen.[2] The tumour can attain a large size with compression of the underlying structures or can extend into the thoracic cavities unilaterally or bilaterally. Contrast-enhanced computed tomographic scan of the chest (CECT) is an important investigation and helps in making a provisional diagnosis. Magnetic resonance imaging (MRI) can also be helpful in cases where infiltration into surrounding structures is suspected because of superior tissue characterization. A positron emission tomographic (PET) scan is useful in differentiating benign from malignant lesions and is increasingly being used for mediastinal tumours.[3] A case of large benign mediastinal mature cystic teratoma is discussed along with a review of the literature. Informed consent was taken from the patient for the publication of images and clinical data.
Case summary
A 17-year-old female patient came with complaints of haemoptysis and breathlessness for 3 months. On examination, there was decreased air entry in the middle and lower zones of the right thorax. Chest X-ray revealed a large thoracic mass on the right side [Figure 1a]. CECT chest was done and it showed a large thoracic cystic mass extending from the mediastinum to the right thoracic cavity to the costo-phrenic recess posterior to the liver, although the diaphragm was intact. The mass was 15 cm × 12 cm and was dumbbell-shaped. CT appearance was suggestive of teratoma as there was fat density shadow along with calcifications and cystic areas also [Figure 1b, 1c and 1d]. As the mass was large and the patient was symptomatic, surgical excision was planned. Preoperative fine-needle aspiration cytology (FNAC) or core needle biopsy was not done as the radiological features were suggestive of teratoma, also her alpha-fetoprotein (AFP) levels, and beta-human chorionic gonadotropin (B-HCG) levels were within the normal range. General anaesthesia was given using a double-lumen endotracheal tube. Right posterolateral thoracotomy was done through the fifth intercostal space. There were dense pleural adhesions that were dissected with electrocautery. The mass was fixed, firm in consistency, immobile and had compressed the middle and lower lobes. The mass was densely adherent to the middle and lower lobes and the hilum of the right lung. The hilum of the right lung was inaccessible from the anterior side as the mass was covering it. Posteriorly also, the approach to the hilum was not possible due to the large size of the mass with significant compression on the surrounding structures. We tried to aspirate the cystic mass from the most prominent part anteriorly as well as from other sites but were unsuccessful. As the mass could not be separated from the middle and lower lobes, we planned for middle and lower lobe lobectomy along with excision of the mass. Dissection in the major fissure was started for lobectomy and during dissection, in the fissure, the cystic mass got opened up, and approximately 1 l of thick fluid was aspirated; hairs were also present in the aspirate. After decompression of the cystic mass, we could dissect the entire mass from the lung parenchyma [Figure 2a and 2b]. The whole of the mass was excised, except a small segment of the cyst wall was left over the pericardium in the area of the phrenic nerve and a small segment was left over the diaphragm. A frozen section study at this stage could also be helpful to differentiate benign from malignant pathology. Small air leaks from the lung parenchyma were closed with 5´0´ sutures. The specimen was sent for histopathologic examination (HPE). Standard thoracotomy closure was done after placing pleural drains. HPE report showed it to be a mature cystic teratoma [Figure 3a-c]. The patient was extubated on the first postoperative day. Approximately 6 h after extubation, patient complained of breathlessness. There was tachycardia with a heart rate of 140–150 beats/min and tachypnoea with a respiratory rate of 35–40 breaths/min with decreased air entry on the right side middle and lower zones. Chest X-ray revealed the collapse of the lower and middle lobes on the ipsilateral side with suspicion of a mediastinal shift to the contralateral side. The other possibility was pulmonary oedema. Initially, non-invasive positive pressure ventilation was started and diuretics were given with little improvement. However, there was immediate relief of dyspnoea on the application of the negative suction to the intercostal drain with the removal of the collected air probably causing the mediastinal shift. The patient gradually improved and her tachycardia and tachypnoea settled down. Repeat chest X-ray showed expansion of the lung with stabilization of mediastinum [Figure 2c]. Negative suction was continued on the next day along with intermittent non-invasive positive pressure ventilation support. Thereafter, continuous negative suction was gradually decreased and then shifted to intermittent negative suction and intermittent positive pressure ventilator support for the next 3 days. The intercostal tube was removed on the sixth postoperative day when the air leak had completely stopped. The patient recovered well and was discharged on the seventh postoperative day. The patient came for a follow-up after 1 month and then after 6 months and was doing well.
Figure 1.
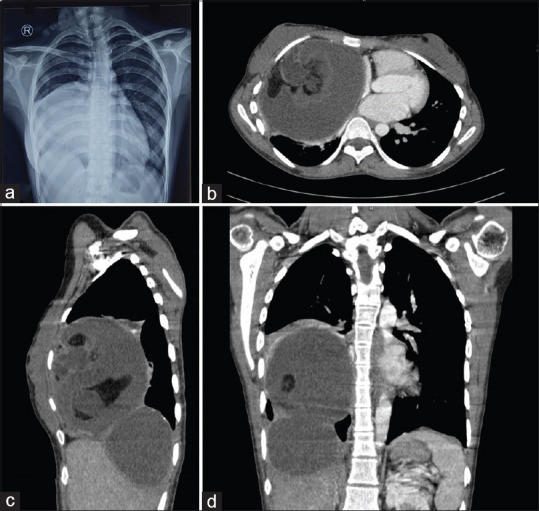
(a) Chest X-ray showing a large mediastinal mass extending into the right thoracic cavity in AP view; and (b–d) CT chest showing a large thoracic cystic mass in the axial, sagittal and coronal planes, respectively
Figure 2.

(a) Intraoperative image showing cyst wall adherent to the middle and lower lobes of the right lung, (b) intraoperative image after removal of the thoracic mass arising from the mediastinum and (c) postoperative chest X-ray in AP view
Figure 3.

(a) Gross photograph of the mass showing lobules of adipose tissue, hair tuffet, and areas of haemorrhage in the cyst wall. (b and c) Photomicrograph showing mature squamous epithelium with adnexa, salivary glands and islands of mature hyaline cartilage
DISCUSSION
Teratomas are germ cell tumours defined histologically as having components of all three germ cell layers, that is, ectoderm, endoderm and mesoderm. They can be mature and immature depending on the degree of differentiation of their components. Mature cystic teratomas are usually benign but they have malignant potential and long-term follow-up is required after complete excision. The characteristic histopathology features include the presence of mature tissue elements derived from three germ layers, including skin and appendageal structures, lobules of mature adipose tissue, respiratory epithelium, islands of hyaline cartilage and salivary gland tissue.[4] The presence of mature pancreatic tissue in mediastinal teratoma has also been documented.[5,6] Association has been noted between aberrations in the short arm of chromosome 12 with germ cell tumours.[7] The majority of mediastinal cystic teratomas are benign in young females and children, whereas in males, they can be malignant.
Clinical features
Benign mediastinal teratomas may be asymptomatic when small in size. Common symptoms associated with benign mediastinal teratoma are chest pain, cough and dyspnoea. Rarely haemoptysis can occur and trichoptysis is even rarer.[8,9] This case also had haemoptysis as the presenting symptom. Patients with mediastinal teratomas rarely can also present in respiratory distress, with pleural effusion due to rupture into the pleural cavity or cardiogenic shock with rupture into the pericardial cavity leading to cardiac tamponade.[10] Rupture into the mediastinum leading to mediastinitis has also been reported in the literature.[11] Rapid enlargement of the mass can lead to compression of the heart, great vessels and trachea with life-threatening complications.[12] Arrhythmias like paroxysmal atrial fibrillation can also occur due to the compressive effect.[13] Association with Klinefelter’s syndrome has been reported in germ cell tumours. Young patients of Klinefelter’s syndrome should be screened for extragonadal germ cell tumours.[14,15] Compression by large mediastinal mass may lead to murmur mimicking valvular heart disease.[16,17] Growing teratoma syndrome although rarely seen in mediastinal germ cell tumours requires a high degree of suspicion for early diagnosis and surgical treatment.[18]
Investigations
Chest X-ray in anteroposterior and lateral view is usually the initial investigation. The tumour is sometimes found incidentally, while investigating for some other problem. Chest CT with contrast is usually the investigation of choice. Characteristic features of benign teratoma on CT are the presence of soft tissue, cystic component, hairs, fat density and calcifications; sometimes bone fragments or teeth may also be seen. Malignant teratomas may reveal evidence of invasion, lymphadenopathy, or metastatic lesions in the lung or pleura. Suspicion of malignancy may need further studies like MRI of the chest or PET-CT.[19] Invasion of the neural tissue and vascular structures is better differentiated with MRI.[20] Tumour markers like AFP and beta-HCG are raised in malignant teratoma and normal levels are found in benign teratoma.[21] CT-guided FNAC or biopsy may be done where malignancy is suspected. For benign teratoma, the biopsy is not done and excision of the mass is the treatment of choice.
Surgical treatment
Surgery is the primary mode of treatment available. Surgical approaches can be median sternotomy, anterolateral thoracotomy, posterolateral thoracotomy, or video-assisted thoracoscopic surgery (VATS) depending upon the location, and size of the tumour, relation to the surrounding structures, and the presence or absence of adhesions. Robotic-assisted thoracoscopic surgery is also being performed at some centres.[22] Secure control of the airway during induction of anaesthesia is an important aspect that can prevent catastrophic events as the tumour can compress the trachea or the main-stem bronchus. Use of fibro-optic bronchoscopy, standby extracorporeal circulation (cardiopulmonary bypass through femoral access) or rapid sternotomy, and aspiration of the cystic mass are some of the methods described in the literature to manage the collapse of the airway and the haemodynamics.[23-25] Reverse Trendelenberg’s position may also be beneficial in relieving compression on the trachea or main-stem bronchus.
Surgical resection of a large mediastinal cystic mass without aspiration is very difficult as there is little access to the hilar structures and major vessels. Aspiration of the cystic mass improves exposure and makes dissection from the surrounding structures relatively easy. Resection of the tumour wall if adherent to the pericardium needs to be carefully done to prevent injury to the phrenic nerve. Some parts of the tumour wall (in case of benign teratoma) may need to be left in the area of the phrenic nerve; otherwise, injury to the phrenic nerve can lead to increased postoperative morbidity. If malignancy is suspected, a frozen section study intraoperatively can be helpful. In case the tumour is found to be malignant teratoma, then the unilateral phrenic nerve might need to be sacrificed to achieve curative resection albeit with increased morbidity. Intraoperative neural monitoring is useful while dissecting in close relation to nerves.[26] In the postoperative period after extubation, there are chances of mediastinal shift and lung collapse which can lead to haemodynamic changes. The use of non-invasive positive pressure ventilation and negative suction on the intercostal drain is helpful in such a situation.
Literature review
The literature on mediastinal/thoracic teratoma available on PubMed was reviewed. The search was done using the keywords ‘benign mediastinal teratoma’. Most of the literature on mediastinal teratomas is in the form of case reports and series with few large-volume studies available. Few reports are also available from India.[27,28] Although numerous case reports have been published from almost all over the world, however, the majority of large-volume studies are from eastern countries, especially Japan and China.[29-34] The prevalence of this pathology may be higher in their population. Original research articles published in the last two decades, that is, after the year 2000 available on PubMed, were evaluated [Table 1]. Only those studies with a focus on surgical treatment of benign mediastinal teratoma and having more than 10 cases were included.[29-34] Studies on other benign lesions of mediastinum like bronchogenic cysts, oesophageal cysts, neurogenic tumours, thymoma and malignant tumours like lymphoma, seminoma and choriocarcinoma were not included in the review. Tian et al.[29] in their large series on 108 cases reported partial resection of the pericardium in 12 cases, lobectomy in 5 cases and wedge resection in 9 patients apart from excision of the mediastinal mass. There was no recurrence of the tumour in their series. Pham et al.[30] advocated extraction of tumour contents to facilitate thoracoscopic surgery. In their series out of 28 cases operated by thoracoscopic surgery, 3 patients were converted to mini-thoracotomy. Hwang et al.[31] did a retrospective comparative evaluation between VATS and open surgery, 79 patients underwent VATS, 10 patients through thoracotomy technique and 43 patients through median sternotomy. Four patients in their study were converted to a thoracotomy approach from VATS. They reported VATS can be safely performed in selected cases. Tsubochi et al.[32] performed VATS in all their cases and recommended extraction/aspiration of cystic contents facilitated removal of the mass. Shintani et al.[33] found no recurrence after a mean follow-up of 4.6 years. They recommended VATS as a standard approach and open surgery for large tumours with preoperative symptoms. Chang et al.[34] reported an association between the presence of pancreatic tissue in the tumour and the occurrence of symptoms and complicated surgery. They recommended preoperative assessment for the presence of adhesions and increased incidence of complications in those with preoperative symptoms.
Table 1.
Analysis of studies on surgical treatment of benign mediastinal teratomas
| Reference Number of patients Male/Female | Size of the lesion (mean diameter in cm) | Procedures (TS/OS) | Complications Mortality | Conclusion/Remarks |
|---|---|---|---|---|
| Tian et al. (2020)[29] 108 42/66 | 8.45 | 22/86 | Chylothorax-1 Postoperative bleeding-1 RLNI-1 WI-2, PI Nil | Good prognosis, VATS is preferred, no recurrence occurred |
| Pham et al. (2020)[30] 28 14/14 | NA | 28/(~3) | ~Conversion to mini-thoracotomy due to adhesions—3 Nil | Large tumour size, adhesions may require mini-thoracotomy |
| Hwang et al. (2016)[31] 132 79/53 | 6.53±2.20 (TS group) 8.58±3.45 (OS group) | 79/53 | Chylothorax-1 WI-1 Nil | VATS is recommended in large cystic teratomas without infiltration of adjacent structure |
| Tsubochi et al. (2015)[32] 13 9/4 | 8 | 13/0 | Nil Nil | Aspiration of cystic contents facilitated VATS |
| Shintani et al. (2013)[33] 15 6/9 | 5.3 | 12/3 | Chylothorax-1 Nil | Open approach for large tumours |
| Chang et al. (2010)[34] 57 18/39 | 8.5±2.9 (TS group) 10.4±4.7 (OS group) | 14/43 | DE-2, HS-1, BAT-1, LA-1, WD-1 (conversion from VATS to mini-thoracotomy due to adhesions—3) Nil | Thoracoscopic technique feasible option, if adhesions are not found |
RLNI: Recurrent laryngeal nerve injury; WI: wound infection; PI: pulmonary infection; VATS: video-assisted thoracoscopic surgery; NA: not available; DE: diaphragmatic eventration; HS: Horner’s syndrome; BAT: brachiocephalic artery tear; LA: lung atelectasis; WD: wound dehiscence. Procedures. TS: Thoracoscopic surgery. OS: Open surgery
As per these studies, thoracoscopic surgery is preferred for most cases, whereas open surgery may be required in cases with large tumour size, infiltration into surrounding structures, and or the presence of adhesions. Complications reported in these studies include chylothorax, recurrent laryngeal nerve injury, Horner’s syndrome, diaphragmatic eventration, bleeding and wound infection.
CONCLUSION
Stabilization of the mediastinum after excision of a large mediastinal/thoracic mass is important postoperatively. Conservative measures with continuous or intermittent negative suction of the intercostal drain along with non-invasive positive pressure ventilation help in the stabilization of the mediastinum and re-expansion of the chronically collapsed lung. As per the literature review, the prognosis of surgical treatment of mediastinal teratoma is excellent with minimal morbidity and morbidity. Long-term follow-up is needed to detect recurrence, although the incidence is low. The prevalence of benign mediastinal teratoma may be higher in eastern countries, Japan and China, than in the rest of the world. This needs to be further investigated by large-volume studies. As per the evaluated series/studies, the thoracoscopic approach gives good results and is the preferred approach unless adhesions are present or infiltration into surrounding structures is present.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Yalagachin GH. Anterior mediastinal teratoma- A case report with review of literature. Indian J Surg. 2013;75((Suppl 1)):182–4. doi: 10.1007/s12262-012-0569-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hammen I, Lal Yadav A. Teratoma as unusual cause of chest pain, hemoptysis and dyspnea in a young patient. Respir Med Case Rep. 2017;23:77–9. doi: 10.1016/j.rmcr.2017.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yabuuchi H, Matsuo Y, Abe K, Baba S, Sunami S, Kamitani T, et al. Anterior mediastinal solid tumours in adults:Characterisation using dynamic contrast-enhanced MRI, diffusion-weighted MRI, and FDG-PET/CT. Clin Radiol. 2015;70:1289–98. doi: 10.1016/j.crad.2015.07.004. [DOI] [PubMed] [Google Scholar]
- 4.Kao CS, Bangs CD, Aldrete G, Cherry AM, Ulbright TM. A Clinicopathologic and Molecular Analysis of 34 Mediastinal Germ Cell Tumors Suggesting Different Modes of Teratoma Development. Am J Surg Pathol. 2018;42:1662–73. doi: 10.1097/PAS.0000000000001164. [DOI] [PubMed] [Google Scholar]
- 5.Agrawal T, Blau AJ, Chwals WJ, Tischler AS. A unique case of mediastinal teratoma with mature pancreatic tissue, nesidioblastosis, and aberrant islet differentiation:A case report and literature review. Endocr Pathol. 2016;27:21–4. doi: 10.1007/s12022-015-9393-4. [DOI] [PubMed] [Google Scholar]
- 6.Stella F, Davoli F. Giant mediastinal mature teratoma with increased exocrine pancreatic activity presenting in a young woman:A case report. J Med Case Rep. 2011;5:238. doi: 10.1186/1752-1947-5-238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee T, Seo Y, Han J, Kwon GY. Analysis of chromosome 12p over-representation and clinicopathological features in mediastinal teratomas. Pathology. 2019;51:62–6. doi: 10.1016/j.pathol.2018.10.002. [DOI] [PubMed] [Google Scholar]
- 8.Madhusudhan KS, Sharma R, Gadodia A, Kumar A. Spontaneous rupture of benign mediastinal teratoma:A report of two cases. Indian J Med Paediatr Oncol. 2012;33:123–5. doi: 10.4103/0971-5851.99750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guibert N, Attias D, Pontier S, Berjaud J, Lavialle-Guillautreau V, Didier A, et al. Mediastinal teratoma and trichoptysis. Ann Thorac Surg. 2011;92:351–3. doi: 10.1016/j.athoracsur.2011.01.036. [DOI] [PubMed] [Google Scholar]
- 10.Kang DK, Kang MK, Heo W, Hwang YH. Cardiac tamponade due to ruptured cystic teratoma:report of two cases. Oxf Med Case Reports. 2021;2021:omab044. doi: 10.1093/omcr/omab044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nakajima E, Kudo Y, Maehara S, Furumoto H, Matsubayashi J, Shimada Y, et al. Ruptured mediastinal mature teratoma causing severe mediastinitis:Report of a surgically resected case and a literature review. Surg Case Rep. 2021;7:48. doi: 10.1186/s40792-021-01132-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Omachi N, Kawaguchi T, Shimizu S, Okuma T, Kitaichi M, Atagi S, et al. Life-threatening and rapidly growing teratoma in the anterior mediastinum. Intern Med. 2015;54:2487–9. doi: 10.2169/internalmedicine.54.4622. [DOI] [PubMed] [Google Scholar]
- 13.Asteriou C, Barbetakis N, Kleontas A, Konstantinou D. Giant mediastinal teratoma presenting with paroxysmal atrial fibrillation. Interact Cardiovasc Thorac Surg. 2011;12:308–10. doi: 10.1510/icvts.2010.253039. [DOI] [PubMed] [Google Scholar]
- 14.Bonouvrie K, van der Werff Ten Bosch J, van den Akker M. Klinefelter syndrome and germ cell tumors:Review of the literature. Int J Pediatr Endocrinol. 2020;2020:18. doi: 10.1186/s13633-020-00088-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Völkl TM, Langer T, Aigner T, Greess H, Beck JD, Rauch, et al. Klinefelter syndrome and mediastinal germ cell tumors. Am J Med Genet A. 2006;140:471–81. doi: 10.1002/ajmg.a.31103. [DOI] [PubMed] [Google Scholar]
- 16.Lip HTC, Huei TJ, Wahid AA, Vendargon SJ. A rare presentation of anterior mediastinal teratoma mimicking valvular heart disease with a systolic murmur. Eurasian J Med. 2018;50:134–6. doi: 10.5152/eurasianjmed.2018.17388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Koçinaj D, Krasniqi X, Bakalli A. Immature teratoma mimicking pulmonary stenosis:A case report. J Med Case Rep. 2018;12:125. doi: 10.1186/s13256-018-1651-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sachdeva AK, Penumadu P, Kohli P, Dubashi B, Munuswamy H. Growing teratoma syndrome in primary mediastinal germ cell tumor:Our experience. Asian Cardiovasc Thorac Ann. 2019;27:98–104. doi: 10.1177/0218492318823345. [DOI] [PubMed] [Google Scholar]
- 19.Kitami A, Sano F, Ohashi S, Suzuki K, Uematsu S, Suzuki T, et al. The usefulness of positron-emission tomography findings in the management of anterior mediastinal tumors. Ann Thorac Cardiovasc Surg. 2017;23:26–30. doi: 10.5761/atcs.oa.16-00205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gaubert JY, Cohen F, Vidal V, Louis G, Moulin G, Bartoli JM, et al. Imagerie des tumeurs du médiastin [Imaging of mediastinal tumors. Rev Pneumol Clin. 2010;66:17–27. doi: 10.1016/j.pneumo.2009.12.011. [DOI] [PubMed] [Google Scholar]
- 21.Rivera C, Arame A, Jougon J, Velly JF, Begueret H, Dahan M, et al. Prognostic factors in patients with primary mediastinal germ cell tumors, a surgical multicenter retrospective study. Interact Cardiovasc Thorac Surg. 2010;11:585–9. doi: 10.1510/icvts.2010.238717. [DOI] [PubMed] [Google Scholar]
- 22.Ramcharran H, Wallen J. Robotic-assisted thoracoscopic resection of anterior mediastinal cystic teratoma:A case report and literature review. J Cardiothorac Surg. 2022;17:67. doi: 10.1186/s13019-022-01806-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Acharya MN, De Robertis F, Popov AF, Anastasiou N. Surgical resection of a huge ruptured mature mediastinal teratoma. Asian Cardiovasc Thorac Ann. 2016;24:726–8. doi: 10.1177/0218492316658847. [DOI] [PubMed] [Google Scholar]
- 24.Maeyama R, Uchiyama A, Tominaga R, Ichimiya H, Kuroiwa K, Tanaka M. Benign mediastinal teratoma complicated by cardiac tamponade:Report of a case. Surg Today. 1999;29:1206–8. doi: 10.1007/BF02482274. [DOI] [PubMed] [Google Scholar]
- 25.Kumar A, Persuad P, Shiwalkar N. Intraoperative catastrophe during benign mediastinal tumor mass excision:A case report. Cureus. 2019;11:e4941. doi: 10.7759/cureus.4941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mikai M, Sano A, Otsuka H, Koezuka S, Azuma Y, Makino T, et al. Resection of a superior mediastinal mature teratoma using intraoperative neural monitoring. Ann Thorac Surg. 2019;108:e287–8. doi: 10.1016/j.athoracsur.2019.03.035. [DOI] [PubMed] [Google Scholar]
- 27.Lakhotia S, Dewan RK. Benign cystic teratoma of mediastinum. Indian J Surg. 2008;70:244–6. doi: 10.1007/s12262-008-0070-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Oomman A, Santhosham R, Vijayakumar C, Jayaraman S, Ramachandran P, Kumar S. Anterior mediastinal teratoma presenting as cardiac tamponade. Indian Heart J. 2004;56:64–6. [PubMed] [Google Scholar]
- 29.Tian Z, Liu H, Li S, Chen Y, Ma D, Han Z, et al. Surgical treatment of benign mediastinal teratoma:Summary of experience of 108 cases. J Cardiothorac Surg. 2020;15:36. doi: 10.1186/s13019-020-1075-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pham LH, Trinh DK, Nguyen AV, Nguyen LS, Le DT, Nguyen DH, et al. Thoracoscopic surgery approach to mediastinal mature teratomas:A single-center experience. J Cardiothorac Surg. 2020;15:35. doi: 10.1186/s13019-020-1076-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hwang SK, Park SI, Kim YH, Kim HR, Choi SH, Kim DK. Clinical results of surgical resection of mediastinal teratoma:Efficacy of video-assisted thoracic surgery. Surg Endosc. 2016;30:4065–8. doi: 10.1007/s00464-015-4721-9. [DOI] [PubMed] [Google Scholar]
- 32.Tsubochi H, Endo S, Nakano T, Minegishi K, Tetsuka K, Hasegawa T. Extraction of mediastinal teratoma contents for complete thoracoscopic resection. Asian Cardiovasc Thorac Ann. 2015;23:42–5. doi: 10.1177/0218492314536173. [DOI] [PubMed] [Google Scholar]
- 33.Shintani Y, Funaki S, Nakagiri T, Inoue M, Sawabata N, Minami M, et al. Experience with thoracoscopic resection for mediastinal mature teratoma:A retrospective analysis of 15 patients. Interact Cardiovasc Thorac Surg. 2013;16:441–4. doi: 10.1093/icvts/ivs543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chang CC, Chang YL, Lee JM, Chen JS, Hsu HH, Huang PM, et al. 18 years surgical experience with mediastinal mature teratoma. J Formos Med Assoc. 2010;109:287–92. doi: 10.1016/S0929-6646(10)60054-X. [DOI] [PubMed] [Google Scholar]


