Abstract
Pulmonary infection due to Pseudomonas aeruginosa has emerged as a leading cause of mortality. A vigorous host response is required to effectively clear the organisms from the lungs. This host defense is dependent on the recruitment and activation of neutrophils and macrophages. A family of chemotactic cytokines (chemokines) has been shown to participate in this protective response. In this study, we assessed the role of the ELR+ (glutamic acid-leucine-arginine motif positive) CXC chemokines and their CXC chemokine receptor (CXCR2) in lung antibacterial host defense. The intratracheal administration of Pseudomonas to mice resulted in the time-dependent influx of neutrophils to the lung, peaking at 12 to 24 h after inoculation. The influx of neutrophils was associated with a similar time-dependent expression of the ELR+ CXC chemokines, KC, macrophage inflammatory protein 2 (MIP-2), and lipopolysaccharide-induced CXC chemokine (LIX). Selective neutralization of MIP-2 or KC resulted in modest changes in neutrophil influx but no change in bacterial clearance or survival. However, neutralization of CXCR2 resulted in a striking increase in mortality, which was associated with a marked decrease in neutrophil recruitment and bacterial clearance. Conversely, the site-specific transgenic expression of KC resulted in enhanced clearance of bacteria after Pseudomonas challenge. This study indicates that ELR+ CXC chemokines are critical mediators of neutrophil-mediated host defense in Pseudomonas pneumonia.
Pseudomonas aeruginosa has emerged as a common and serious pathogen of the lower respiratory tract. This organism is one of the leading causes of nosocomial pneumonia in adult and pediatric critical care units, as well as a major etiologic agent of pneumonia in neutropenic patients (1, 17, 20). In addition, its persistent colonization has been implicated in the chronic proinflammatory state and the progressive decline in pulmonary function in the airways of cystic fibrosis (CF) patients (7, 20, 21). Despite our clinical armamentarium, the morbidity and mortality from Pseudomonas pneumonia remain substantial. In the normal host, the inflammatory response that follows the introduction of P. aeruginosa into the alveolus is characterized by the intrapulmonary sequestration of neutrophils (6). The factors that regulate neutrophil recruitment and activation in Pseudomonas pneumonia have not been well characterized. Leukocyte recruitment is an integral component of the host defense cascade and is believed to be mediated, in part, by the production of chemotactic cytokines.
Four closely related families of chemotactic cytokines, referred to as chemokines, are now known to exist in humans, and most have murine homologues (27, 41). Their classification is based on the presence of four conserved cysteine residues at the N terminus, the first two of which are separated by variable numbers of nonconserved amino acids. The CXC chemokine family is further distinguished by the presence or absence of an amino acid sequence, glutamic acid-leucine-arginine (ELR motif), that precedes the CXC sequence. ELR+ CXC chemokines have been shown to induce neutrophil chemotaxis and stimulate neutrophil activation in pulmonary and extrapulmonary inflammatory responses (2, 10, 14, 30, 39, 48, 49). Several ELR+ CXC chemokines exist in humans, including interleukin-8 (IL-8), growth-related oncogene family (GRO-α,β) epithelial cell-derived neutrophil activating protein 78 (ENA-78), neutrophil activating peptide 2, and granulocyte chemotactic peptide 2 (GCP-2). Murine ELR+ CXC chemokines have also been identified; these include macrophage inflammatory protein 2 (MIP-2), KC, lipopolysaccharide-induced CXC chemokine (LIX), and Lungkine (35, 36, 50). ELR+ CXC chemokines have recently been shown to be induced in gram-negative bacterial pneumonia models. In vitro studies have shown that many virulent factors of P. aeruginosa induce robust IL-8 production from isolated neutrophils, alveolar macrophages, as well as respiratory bronchial and alveolar epithelia (4, 8, 9, 28, 31, 33, 37). Furthermore, a recent in vivo study of P. aeruginosa bronchopulmonary infection in CF mice demonstrated that retention of bacteria in the airways induced an excessive inflammatory response in CF mice above that of wild-type mice challenged with comparable bacterial inoculum (18). The proinflammatory response was due in part to a significant elevation of MIP-2 and KC in the lungs of CF mice, suggesting that these chemokines may be detrimental to the CF host in chronic P. aeruginosa bronchopulmonary infection. In our laboratory, we have shown that MIP-2 is expressed within the lungs, but not blood, of mice administered Klebsiella pneumoniae intratracheally (i.t.), and the neutralization of MIP-2 was shown to attenuate lung neutrophil influx without substantially altering survival (16). In contrast, the stable transgenic expression of KC in the lungs markedly increased neutrophil recruitment, resulting in significant increases in bacterial clearance and survival (47). The role of ELR+ chemokines in the host response of acute and chronic respiratory infection of P. aeruginosa remains unclear.
ELR+ CXC chemokine receptors have been characterized and found to be involved in neutrophil recruitment and activation responses (19, 26, 32, 45). Mice express only the CXCR2 receptor, which binds to all ELR+ CXC chemokines, whereas humans also possess a more selective receptor CXCR1 which binds specifically to IL-8 and GCP-2. In CXCR2 knockout mice, neutrophils were not recruited in vivo in response to MIP-2 or KC but did respond to other chemoattractants, suggesting that binding of ELR+ CXC chemokines to CXCR2 is essential for neutrophil recruitment and that CXCR2 is the exclusive receptor for these ligands (24). Studies evaluating the role of gram-negative ELR+ CXC chemokines and their receptor CXCR2 in models of bacterial pneumonia have not been described.
In this study, we examined the role of ELR+ CXC chemokines and their receptor in host defense following i.t. Pseudomonas challenge. We hypothesized that ELR+ CXC chemokines are important contributors in the innate host defense against Pseudomonas challenge by mediating neutrophil recruitment and bacterial clearance.
MATERIALS AND METHODS
Reagents.
Purified polyclonal rabbit anti-murine MIP-2 antibodies (Abs) used in neutralization studies and in the enzyme-linked immunosorbent assays (ELISAs) were produced by immunization of rabbits with carrier-free murine recombinant MIP-2 (R&D Systems, Minneapolis, Minn.) in multiple intradermal sites with complete Freund's adjuvant as previously described (12, 42). These Abs have been demonstrated to neutralize their target chemokine bioactivity in vitro and in vivo (16). Rat anti-murine KC monoclonal antibodies (MAbs) used in neutralization studies and in the ELISAs were purchased from R&D Systems. Fifteen to 30 μg of KC Ab per ml has been demonstrated to neutralize mouse KC bioactivity in the presence of 1 μg of murine KC per ml, using myeloperoxidase (MPO) release from human neutrophils as the bioassay. Purified polyclonal goat anti-murine CXCR2 antibodies were produced by intradermal immunization of goats with a 17-amino-acid peptide segment which comprises a portion of the seven-transmembrane receptor that resides on the cell surface of CXCR2 and has previously been shown to be the binding site for ligands. This antibody has been shown to detect CXCR2 by Western blot and fluorescence-activated cell sorting analysis of neutrophils (data not shown). We have demonstrated that this antibody is neutralizing both in vitro and in vivo and that its binding to CXCR2 on neutrophils does not alter peripheral blood neutrophil counts (29).
Preparation and use of MAb RB6-8C5 for in vivo neutrophils depletion.
RB6-8C5 is a rat anti-mouse monoclonal immunoglobulin G2b directed against Ly-6G, previously known as Gr-1, an antigen on the surface of murine granulocytes. Antigen expression increases with cell maturity and is absent from precursor cells. RB6-8C5, originally used for flow cytometry, is a complement-fixing isotype, well suited for in vivo cell depletion (13, 23, 25, 34, 44). The Ab was produced by TSD BioServices (Germantown, N.Y.) by intraperitoneal (i.p.) injection of hybridoma RB6-8C5 into nude mice and collection of ascites. One hundred micrograms of RB6-8C5 was administered i.p. 1 day prior to challenge i.t. with P. aeruginosa or vehicle. This resulted in peripheral blood neutropenia (absolute circulating neutrophil count of <50 cells/μl) by days 1 and 3 after Ab administration in both infected and control animals, with a return of peripheral counts to pretreatment levels by day 5.
Animals.
Specific-pathogen-free C57BL/6 mice (6- to 8-week-old females; Jackson Laboratory, Bar Harbor, Maine) were used in all experiments. All mice were housed in specific-pathogen-free conditions within the animal care facility at the University of Michigan (ULAM) until the day of sacrifice.
P. aeruginosa inoculation.
We chose to use P. aeruginosa strain UI-18 (PA-7; Parke-Davis, Ann Arbor, Mich.) in our studies, as this strain has been shown to induce an impressive intrapulmonary inflammatory response in mice (40). PA-7 was grown in tryptic soy broth (Difco, Detroit, Mich.) for 18 h at 37°C in a shaking incubator at 225 rpm. The concentration of bacteria in broth was determined by measuring the absorbance at 600 nm. A standard of absorbancies based on known CFU was used to calculate inoculum concentration. Dose of 105 to 106 organisms per mouse were chosen, as this range allowed for the development of substantial inflammation in normal mice by 36 to 48 h without significant mortality. Animals were anesthetized with approximately 1.8 to 2 mg of pentobarbital per animal i.p. The trachea was exposed, and 30 μl of inoculum or saline was administered via a sterile 26-gauge needle. The skin incision was closed with surgical staples.
MPO assay.
Lung MPO activity (as a measure of neutrophil quantity) was determined by a method described previously (15). Briefly, lungs were homogenized in 2 ml of a solution containing 50 mM potassium phosphate (pH 6.0) with 5% hexadecyltrimethylammonium bromide and 5 mM EDTA. The resultant homogenate was sonicated and centrifuged at 12,000 × g for 15 min. The supernatant was then mixed 1:15 with assay buffer and read at 490 nm. MPO units were calculated as the change in absorbancy (optical density [OD]) over time and expressed as mean mOD/time units ± standard error of the mean (SEM).
Lung inflammatory cell enumeration.
Lungs were harvested from euthanized mice, suspended in warm RPMI 1640 containing penicillin and streptomycin (both from Gibco), type I collagenase (150 U/ml), and DNase (0.03 mg/ml) (both from Worthington, Freehold, N.J.), minced with scissors to a fine slurry, and digested as previously described (3). After incubation in the above medium for 45 min, the tissue was forced through a nylon mesh using a glass pestle. The effluent cells were centrifuged at 400 × g for 40 min and washed once in 15 ml of cold phosphate-buffered saline (PBS). Cells were counted in a hemocytometer using trypan blue exclusion as an index of viability. Cell differentials were determined by Wright-Giemsa staining of cytospins. Total numbers of each cell type were determined by multiplying the percentage of each cell type by the total number of cells.
Lung histologic evaluation.
Mice were sacrificed with carbon dioxide inhalation. The pulmonary vasculature was perfused with 4% paraformaldehyde in PBS via the right ventricle. Lungs were then excised en bloc and inflation fixed in 4% paraformaldehyde in PBS. The lungs were then embedded in paraffin, and sections were cut and stained with hematoxylin and eosin under standard techniques.
Lung harvesting for cytokine analysis.
At designated time points, mice were sacrificed with carbon dioxide inhalation and blood was collected by orbital bleeding or direct cardiac puncture. Whole lungs were then harvested for assessment of the various cytokine protein levels. Prior to lung removal, the pulmonary vasculature was perfused via the right ventricle with 1 ml of PBS containing 5 mM EDTA. After removal, whole lungs were homogenized in 1.5 ml of complete protease inhibitor lysis buffer (Boehringer Mannheim, Indianapolis, Ind.). Homogenates were incubated on ice for 30 min and then centrifuged at 2,500 rpm for 10 min. Supernatants were collected, passed through a 0.45-μm-pore-size filter (Gelman Sciences, Ann Arbor, Mich.), and then stored at −20°C for assessment of cytokine levels.
Isolation and reverse transcription-PCR amplification of whole lung mRNA.
Whole lungs were harvested, immediately snap-frozen in liquid nitrogen, and stored at −70°C; then reverse transcription-PCR performed as previously described (16). Briefly, total cellular RNA from the frozen lungs were isolated, reversed transcribed into cDNA, and then amplified as previously described, using specific primers for KC, MIP-2, and LIX, with β-actin serving as a control. The primers had the sequences 5′-TGA-GCT-GCG-CTG-TCA-GTG-CCT-3′ and 5′-AGA-AGC-CAG-CGT-TCA-CCA-GGA-3′ for KC, 5′-TGC-CTG- AAG-ACC-CTG-CCA-AGG-3′ and 5′-GTT-AGC-CTT-GCC-TTT-GTT- CAG-3′ for MIP-2, 5′-CTC-AGT-CAT-AGC-CGC-AAC-CGA-GC-3′ and 5′-CCG-TTC-TTT-CCA-CTG-CGA-GTG-C-3′ for LIX, and 5′-ATG-GAT- GAC-GAT-ATC-GCT-C-3′ and 5′-GAT-TCC-ATA-CCC-AGG-AAG-G-3′ for β-actin. After amplification, the samples (20 μl) were separated on a 2% agarose gel containing ethidium bromide (0.3 mg/ml; 0.003%), and bands were visualized and photographed using UV transillumination.
Densitometric analysis of PCR gels.
After complete electrophoresis, the PCR gel image was captured and analyzed using the NIH Image software with a Macintosh computer. Data were expressed as a ratio of the measured calibrated mean pixel intensity of each cytokine band divided by the calibrated mean pixel intensity of the corresponding β-actin band at each time point.
Determination of plasma and lung P. aeruginosa CFU.
At the time of sacrifice, plasma was collected, the right ventricle was perfused with 1 ml of PBS, and then lungs were removed aseptically and placed in 3 ml of sterile saline. The tissues were then homogenized with a tissue homogenizer under a vented hood. The lung homogenates were placed on ice, and serial 1:10 dilutions were made. Ten microliters of each dilution was plated on soy base blood agar plates (Difco), the plates were incubated for 18 h at 37°C, and then colonies counted.
Murine cytokine ELISA.
Murine MIP-2 and KC protein levels were quantitated using a modification of a double-ligand method as previously described (16). Briefly, flat-bottomed 96-well microtiter plates (Nunc Immuno-Plate I 96-F; Nunc, Roskilde, Denmark) were coated at 50 μl/well with rabbit antibody against MIP-2 and KC (1 μg/ml in 0.6 M NaCl, 0.26 M H3BO4, and 0.08 M NaOH [pH 9.6]) for 16 h at 4°C and then washed with PBS (pH 7.5)–0.05% Tween 20 (wash buffer). Microtiter plate nonspecific binding sites were blocked with 2% bovine serum albumin in PBS and incubated for 90 min at 37°C. Plates were rinsed four times with wash buffer, neat or diluted (1:10) cell-free supernatants (50 μl) in duplicate were added, and the plates were incubated for 1 h at 37°C. Plates were washed four times, biotinylated rabbit antibodies against the specific cytokines (3.5 μg/ml in PBS [pH 7.5]–0.05% Tween 20–2% fetal calf serum) and plates were added at 50 μl/well, and plates were incubated for 30 min at 37°C. Plates were washed four times, streptavidin-peroxidase conjugate (Bio-Rad Laboratories, Richmond, Calif.) was added, and the plates were incubated for 30 min at 37°C. Plates were washed again four times and chromogen substrate (Bio-Rad) was added. The plates were incubated at room temperature to the desired extinction, and the reaction was terminated with 3 M H2SO4 solution (50 μl/well). Plates were read at 490 nm in an ELISA reader. Standards were 1/2-log dilutions of recombinant murine cytokines from 1 pg/ml to 100 ng/ml. This ELISA method consistently detected murine cytokine concentrations above 25 pg/ml. The ELISA did not cross-react with tumor necrosis factor, IL-1, IL-2, IL-4, or IL-6. In addition, the ELISA did not cross-react with other members of the murine chemokine family, including murine MIP-1α, RANTES, and ENA-78.
Statistical analysis.
Data were analyzed on a Power Macintosh 8600/300 computer using InStat version 2.01 and GraphPad Prizm version 2.0 statistical packages (GraphPad Software). Survival data were expressed as percent survival determined by the Kaplan-Meier method and compared using the Mantel-Haenszel logrank test. All other data were expressed as mean ± SEM and compared using an unpaired two-tail Mann-Whitney (nonparametric) test. P values were considered statistically significant if they were less than 0.05.
RESULTS
Influx of neutrophils into the lungs following intrapulmonary P. aeruginosa challenge.
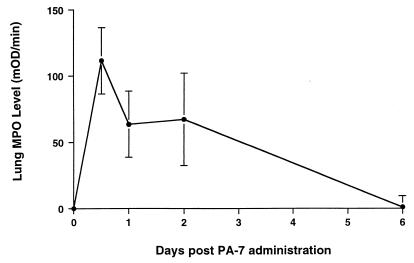
In initial experiments, we characterized the time course of lung neutrophil sequestration in C57BL/6 mice following intrapulmonary P. aeruginosa challenge. Lungs were harvested at 12 h and at days 1, 2, and 6; then whole lung homogenates were assessed for MPO content, a marker of neutrophil presence in the lung. Following P. aeruginosa inoculation, lung MPO levels increased over baseline, peaking maximally at 12 h and remaining elevated for 2 days before returning to baseline by 6 days after i.t. P. aeruginosa challenge (Fig. 1).
FIG. 1.
Whole lung MPO levels following i.t. administration of P. aeruginosa (106 CFU). Data represent mean + SEM (n = 5 animals per time point).
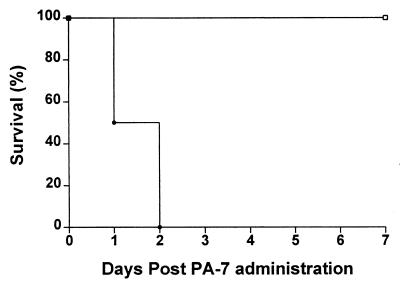
Effect of neutrophil depletion on survival following intrapulmonary P. aeruginosa challenge.
To determine the role of neutrophils in host defense in the setting of intrapulmonary P. aeruginosa challenge, survival was assessed in both mice depleted of neutrophils and non-neutrophil-depleted animals following intrapulmonary P. aeruginosa administration. C57BL/6 mice were administered 100 μg of MAb RB6-8C5 (anti-Ly-6G MAb) i.p. 18 h prior to P. aeruginosa i.t. inoculation. Preliminary studies have shown that this dose of MAb RB6-8C5 resulted in peripheral blood neutropenia (absolute circulating neutrophil count of <50 cells/μl) from 1 to 3 days after i.p. administration, with restoration of neutrophil counts by 5 days (data not shown). Following inoculation with 105 CFU of P. aeruginosa, 100% mortality was observed by 2 days in neutrophil-depleted mice, whereas no deaths were observed in control mice administered the same dose of P. aeruginosa (Fig. 2). This study indicates that neutrophils play a crucial role in the early host defense against intrapulmonary P. aeruginosa.
FIG. 2.
Effect of neutrophil depletion on survival of mice after i.t. administration of P. aeruginosa (105 CFU). Data are expressed as percent survival at each time point determined by the Kaplan-Meier method. Difference in survival between the two groups was compared using the Mantel-Haenszel logrank test (P < 0.001 compared to non-neutrophil-depleted mice; n = 10 mice per group). •, neutrophil-depleted mice; □, non-neutrophil-depleted control mice.
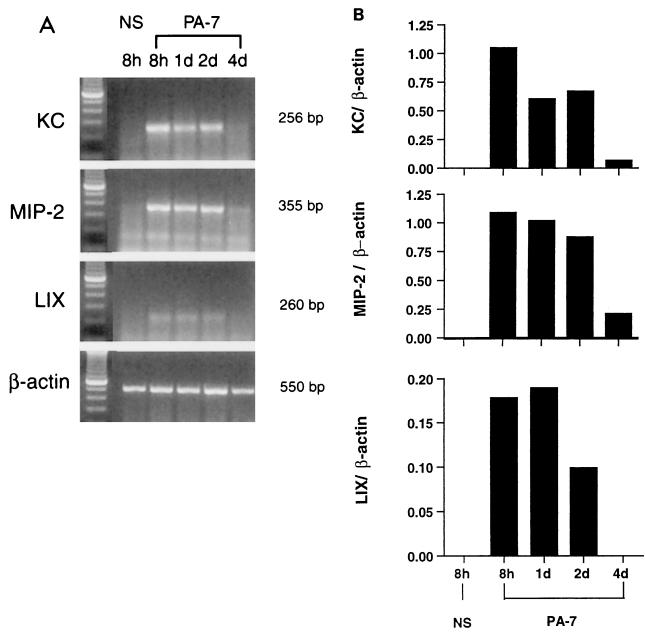
Time-dependent expression of ELR+ CXC chemokine mRNA after i.t. P. aeruginosa administration.
Given that ELR+ CXC chemokines possess potent neutrophil chemotactic effects in vivo and in vitro, we next determined whether ELR+ CXC chemokine message was induced in the setting of P. aeruginosa challenge. Mice were administered P. aeruginosa i.t., and lungs were harvested at 8 h and days 1, 2, and 4 after P. aeruginosa administration. The administration of P. aeruginosa (106 CFU) resulted in the time-dependent expression of KC, MIP-2, and LIX mRNA in the lungs of mice (Fig. 3). Expression of ELR+ CXC chemokine mRNA was noted by 8 h following bacterial inoculation, remained elevated at 2 days, and then decreased by 4 days postinoculation. In contrast, no ELR+ CXC chemokine mRNA expression was detected in the lungs of animals administered saline i.t. (Fig. 3A, NS lane).
FIG. 3.
(A) Time-dependent expression of ELR+ CXC chemokine mRNAs in lung homogenates following i.t. administration of P. aeruginosa (106 CFU). Positions of molecular weight markers are shown to the right. All cDNAs were amplified by 35 cycles of PCR, with the exception of β-actin, which required 25 cycles. Each lane represents the lungs of three animals combined. NS, noninfected saline control at 8-h time point; PA-7, infected animals at 8-h and day 1, 2, and 4 time points. (B) Time-dependent expression of ELR+ CXC chemokine mRNAs in lung homogenates following i.t. administration of P. aeruginosa (106 CFU). Values are expressed as relative intensity of each chemokine band divided by intensity of respective β-actin band in the same lane as determined by densitometry. NS, noninfected saline control at 8-h time point; PA-7, infected animals at 8-h and day 1, 2, and 4 time points.
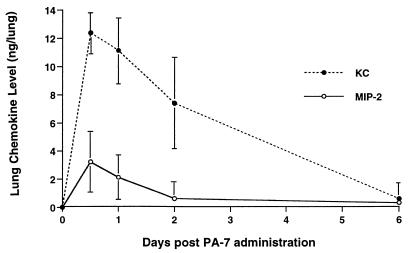
Time-dependent production of ELR+ CXC chemokines after i.t. P. aeruginosa administration.
We next determined whether specific ELR+ CXC chemokine proteins were induced in the setting of P. aeruginosa challenge. Mice were administered P. aeruginosa i.t.; then lungs were harvested at 12 h, and days 1, 2, and 6. The i.t. administration of P. aeruginosa (106 CFU) resulted in the time-dependent production of both KC and MIP-2 in the lungs of normal mice, as determined by specific ELISA. Maximal lung KC and MIP-2 levels peaked at 12 h following bacterial inoculation, remained elevated for 2 days, and then returned to baseline by 6 days postinoculation, compared to noninfected controls, where no KC or MIP-2 was detected in the lungs (Fig. 4). In this study, the time-dependent induction of both ELR+ CXC chemokines paralleled that of neutrophil influx into the lung. No KC or MIP-2 was detected in the blood of either infected mice or noninfected controls at any time point postchallenge (data not shown). LIX protein levels were not quantified due to the absence of an ELISA to specifically detect this chemokine.
FIG. 4.
Time-dependent production of ELR+ CXC chemokines (KC and MIP-2) following i.t. administration of P. aeruginosa (106 CFU). Data represent mean + SEM (n = 5 animals per time point).
Effect of selective neutralization of MIP-2 or KC on lung neutrophil influx after i.t. P. aeruginosa administration.
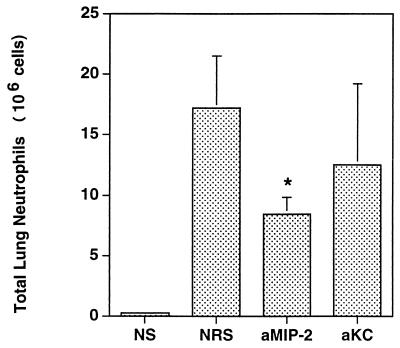
We next sought to determine whether selectively inhibiting an individual ELR+ CXC chemokine would affect outcome after intrapulmonary P. aeruginosa challenge. Mice were pretreated i.p. with 0.5 ml of rabbit anti-mouse polyclonal MIP-2 Ab or 100 μg of anti-KC MAb 2 h prior to i.t. administration of P. aeruginosa (106 CFU); lungs were harvested 24 h following i.t. challenge. Treatment with specific antichemokine antibodies reduced the amounts of chemokines to below levels detectable by ELISA (data not shown). Mice treated with anti-MIP-2 Ab showed a significant reduction in total number of lung neutrophils (49%; P < 0.003) compared to control animals administered normal rabbit serum (Fig. 5). Mice treated with anti-KC Ab also demonstrated a reduction in total number of lung neutrophils (30%), although this decrease did not reach the level of statistical significance. However, no differences were noted in survival or bacterial clearance between the anti-MIP-2 and anti-KC Ab-treated mice and animals receiving control serum (data not shown).
FIG. 5.
Effect of passive immunization with anti-MIP-2 Ab or anti-KC Ab on lung neutrophil influx 24 h following i.t. administration of P. aeruginosa (106 CFU; n = 5 animals per group). ∗, P < 0.01 compared to control serum-treated mice challenged with P. aeruginosa. NS, untreated mice challenged with noninfected saline; NRS, normal rabbit serum-treated control mice challenged with P. aeruginosa; aMIP-2, anti-MIP-2 Ab-treated mice challenged with P. aeruginosa; aKC, anti-KC Ab-treated mice challenged with P. aeruginosa.
Effect of CXCR2 neutralization on survival after i.t. P. aeruginosa administration.
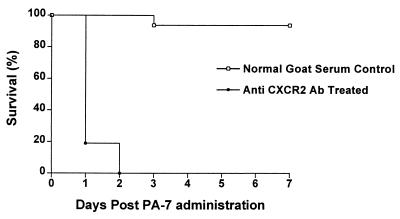
To evaluate the entire group of ELR+ CXC chemokines, we used a CXCR2 neutralizing Ab that inhibited the binding of all ligands to their common receptor, CXCR2. Mice were administered i.p. 0.5 ml of goat anti-mouse CXCR2 Ab 2 h prior to i.t. inoculation with P. aeruginosa 106 CFU, a nonlethal inoculum dose in normal mice. At 1 day after P. aeruginosa inoculation, both anti-CXCR2 Ab-treated and normal goat serum-treated control animals developed signs of pneumonia, including lethargy and ruffled fur. However, survival was substantially greater in control mice challenged with P. aeruginosa, with 90% long-term survival observed in this group (P < 0.01). In stark contrast, no animals survived beyond 2 days in the anti-CXCR2 Ab-treated infected mice (Fig. 6).
FIG. 6.
Effect of CXCR2 neutralization on survival of mice following i.t. administration of P. aeruginosa (106 CFU). Data are expressed as percent survival at each time point, determined by the Kaplan-Meier method. Difference in survival between the two groups (n = 20 animals per group) was compared using the Mantel-Haenszel logrank test (P < 0.001 as compared to control serum-treated mice).
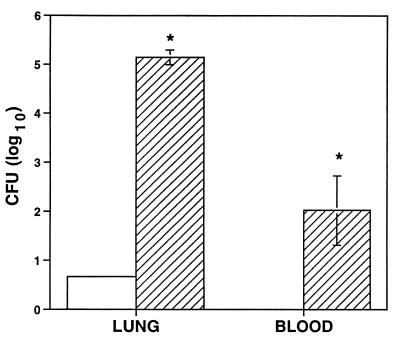
Effect of CXCR2 neutralization on bacterial clearance after i.t. P. aeruginosa administration.
To determine if the observed decrease in survival in anti-CXCR2 Ab-treated mice was due to impairment in bacterial clearance, anti-CXCR2 Ab-treated and normal goat serum-treated control mice were administered P. aeruginosa (106 CFU) i.t. The lungs and plasma were harvested 24 h after inoculation. At 24 h, anti-CXCR2 Ab-treated animals had a strikingly (4-log fold) greater number of P. aeruginosa CFU recovered from the lung compared to control animals challenged with P. aeruginosa (Fig. 7; P < 0.01). In addition, 50% (5 of 10) of anti-CXCR2 Ab-treated animals were bacteremic by 24 h, whereas no control mice were bacteremic at any time point after P. aeruginosa administration (data not shown). These results indicate that CXCR2 neutralization significantly impaired effective bacterial clearance in the lung and permitted dissemination of the organism to the bloodstream.
FIG. 7.
Effect of CXCR2 neutralization on lung and blood bacterial clearance 24 h following i.t. administration of P. aeruginosa (106 CFU). ∗, P < 0.01 compared to control serum-treated mice challenged with P. aeruginosa. Open bar, control serum-treated mice; hatched bar, anti-CXCR2 Ab-treated mice [n = 10 animals per group].
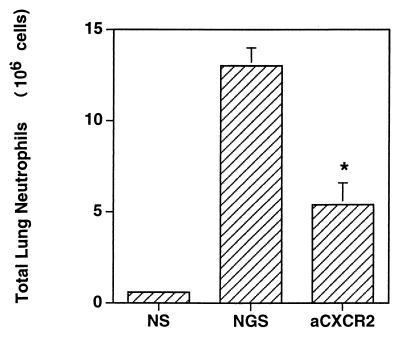
Effects of CXCR2 neutralization on lung inflammatory cell influx after i.t. P. aeruginosa administration.
To determine if the impairment in bacterial clearance in anti-CXCR2 Ab-treated animals was due to alterations in the recruitment of inflammatory cells to the airspace, anti-CXCR2 Ab-treated and serum control-treated mice were challenged with P. aeruginosa, and then lungs were enzymatically digested into single cell suspension to determine total cell counts 24 h following inoculation. This time point was chosen because maximum influx of neutrophils in response to the i.t. administration of P. aeruginosa occurred at 12 to 24 h postchallenge. Compared to control animals, anti-CXCR2 Ab-treated mice exhibited a significant reduction in both percentage (data not shown) and total numbers of neutrophils (P < 0.01) 24 h after P. aeruginosa administration (Fig. 8). Treatment with anti-CXCR2 Ab did not significantly alter the numbers of macrophages or lymphocytes after Pseudomonas challenge. To confirm the lung digest findings, lungs were harvested 24 h after inoculation with P. aeruginosa or saline and then assayed for lung MPO activity. In animals challenged with P. aeruginosa, a decrease in lung MPO activity similar in degree to that seen in total lung neutrophils was noted in the anti-CXCR2 Ab-treated mice compared to controls (data not shown). These results indicate that the impaired host response observed in CXCR2 neutralization was associated with a reduced influx of neutrophils into the lungs.
FIG. 8.
Effect of CXCR2 neutralization on lung neutrophil influx 24 h following i.t. administration of P. aeruginosa (106 CFU; n = 6 animals per group). ∗, P < 0.01 compared to control serum-treated mice challenged with P. aeruginosa. NS, untreated mice challenged with noninfected saline; NGS, normal goat serum-treated control mice challenged with P. aeruginosa; aCXCR2, anti-CXCR2 Ab-treated mice challenged with P. aeruginosa. Data are representative of two separate experiments.
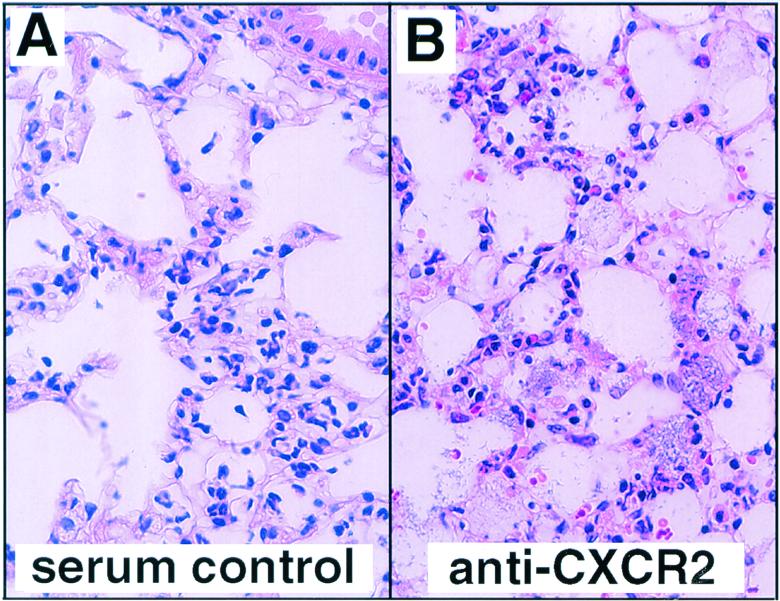
To further explore the effects of CXCR2 neutralization on pulmonary inflammation, lung histopathology was performed. Anti-CXCR2 Ab-treated and serum control-treated animals were challenged i.t. with 106 CFU of P. aeruginosa; then lungs were harvested for histologic examination 24 h later. Following bacterial administration, a prominent infiltration of neutrophils was observed in serum control-treated mice (Fig. 9). In contrast, fewer neutrophils were observed in the airspaces of anti-CXCR2 Ab-treated mice. In addition, an abundance of P. aeruginosa was observed in the airspaces of anti-CXCR2 Ab-treated mice, whereas no bacteria were seen in control animals.
FIG. 9.
Effect of CXCR2 neutralization on lung histopathology in normal goat serum-treated control and anti-CXCR2 Ab-treated mice 24 h following i.t. administration of P. aeruginosa (106 CFU; n = 2 animals per group). Hematoxylin-eosin stain; magnification, ×400.
DISCUSSION
Effective host defense against many bacterial pathogens of the respiratory tract is believed to require the recruitment and activation of neutrophils (46). Recent studies have suggested that ELR+ CXC chemokines are expressed in the setting of pneumonia (16, 18, 29, 47). In the setting of chronic Pseudomonas pneumonia in CF mice, persistent release of these chemokines (MIP-2 and KC) is implicated in the progressive neutrophil-dependent pathogenesis of airway destruction (18). In murine models of acute gram-negative bacterial and fungal pneumonia, these chemokines appear crucial to the innate host defense (16, 29, 47). The roles of this family or individual members of this family remain unclear. Mechanisms that mediate chronic inflammation in airways may be different from those that are involved in acute infection from Pseudomonas. In this study, we examined the contribution of multiple ELR+ CXC chemokine ligands and their shared chemokine receptor CXCR2 to neutrophil recruitment and bacterial clearance in a murine model of acute Pseudomonas pneumonia.
The two best-studied murine ELR+ CXC chemokines, MIP-2 and KC, are functional homologues of the human ELR+ CXC chemokines, IL-8 and GRO-α/β (36). MIP-2 and KC have been shown to contribute to neutrophil-dependent host defense in other models of pneumonia. Specifically, in a murine model of Pseudomonas pneumonia, MIP-2 and KC levels were associated with the presence of neutrophils in the lung (22); in murine Klebsiella pneumonia, MIP-2 was shown to be involved in the recruitment of neutrophils but had only modest effects on clearance of the pathogen and subsequent survival of animals (16). In our studies, we found that Ab-mediated depletion of a single ELR+ CXC chemokine (MIP-2 or KC) resulted in rather modest changes in lung neutrophil sequestration, but no changes in survival or bacterial clearance in animals challenged with Pseudomonas. Therefore, we investigated the importance of ELR+ CXC chemokines as a group in Pseudomonas pneumonia, by blocking their common receptor CXCR2. This approach allowed us to overcome the difficulties in simultaneous neutralization of multiple ligands, which may have redundant and overlapping functions. We used a goat anti-murine antibody, which did not deplete circulating neutrophils but prevented the in vivo influx of neutrophils into the peritoneum in response to exogenous KC (data not shown). Survival from the pneumonia that resulted from Pseudomonas inoculation in the setting of CXCR2 neutralization was indistinguishable from that caused by neutrophil depletion. Furthermore, impairment in bacterial clearance was dramatic in mice subjected to CXCR2 neutralization. While the residual lung accumulation of neutrophils in the setting of CXCR2 neutralization indicates that other mechanisms, such as other chemotactic factors or differential expression of adhesion molecules, may play a role in neutrophil influx in response to P. aeruginosa, the overall magnitude of effect of CXCR2 neutralization suggests that the interaction of ELR+ CXC chemokines with their receptor CXCR2 is a major, if not the most important, mechanism of neutrophil recruitment in host defense against P. aeruginosa.
The impressive effect of CXCR2 neutralization suggests that multiple ELR+ CXC chemokine ligands may be involved. Other candidate murine ELR+ CXC chemokines are less well characterized. The newly described murine chemokine LIX has been shown to share structural homology with the human chemokines ENA-78 and GCP-2 and is chemotactic for neutrophils in vitro (38). In a murine model of systemic endotoxemia, the expression of the ELR+ CXC chemokines was found to differ markedly in various organs (36), with prominent expression of MIP-2 in the lung, LIX in the heart, and equal expression of KC in lung, heart, and liver. Our studies suggest that LIX mRNA is expressed in the lung in a time course similar to that observed for MIP-2 or KC messages, albeit to a lesser degree. Unfortunately, neutralizing LIX Abs are not available to perform in vivo neutralization studies. Another recently described murine ELR+ CXC chemokine, Lungkine, has also been shown to be chemotactic for neutrophils in vitro; it is constitutively expressed by lung epithelial cells but not expressed in other organs (35). The preferential expression of chemokines in specific organs suggests that the various ELR+ CXC chemokines may have distinct biological roles. Studies are ongoing to evaluate the contribution of Lungkine in experimental Pseudomonas pneumonia.
This study has identified CXCR2 ligands as required components of host defense against P. aeruginosa. These results suggest that the augmentation of specific relevant members of the ELR+ CXC chemokine family may offer potential therapeutic avenues in the treatment of multiresistant and refractory nosocomial pneumonia due to P. aeruginosa. To this end, we have shown that the mice expressing the KC transgene in the lungs display enhanced resistance to intrapulmonary challenge with Klebsiella pneumoniae (47). Given the emergence of highly resistant bacterial pathogens and the increasing population of immunocompromised hosts (5, 11, 43), the treatment of bacterial infection has been and will continue to be quite difficult. Therefore, immunomodulation of host responses, especially if delivered in a site-directed fashion, may prove to be an attractive adjuvant to conventional antibiotic therapy. Furthermore, since CXC chemokines appear to occupy a distal position in the cytokine network, and exhibit more neutrophil chemotactic than activating effects, these favorable characteristics suggest that augmentation of chemokines may potentially improve the clinical outcome of patients with severe bacterial pneumonias while limiting the potentially serious adverse effects mediated by overzealous leukocyte activation and/or regulation of other potentially injurious cytokines. Future studies need to be performed to evaluate the effects of augmentation of ELR+ CXC chemokines on the outcome of Pseudomonas pneumonia.
ACKNOWLEDGMENTS
This research was supported in part by National Institutes of Health grants HL58200, HL57243, HL50057, HL31693, HL35276, 1KO8HL04220, 1KO8HL04421, and 1P50HL60289.
REFERENCES
- 1.Anonymous. National Nosocomial Infection Surveillance System. Atlanta, Ga: Centers for Disease Control and Prevention; October 1986–April 1998. [Google Scholar]
- 2.Antony V B, Godbey S W, Kunkel S L, Hott J W, Hartman D L, Burdick M D, Strieter R M. Recruitment of inflammatory cells to the pleural space. Chemotactic cytokines, IL-8, and monocyte chemotactic peptide-1 in human pleural fluids. J Immunol. 1993;151:7216–7223. [PubMed] [Google Scholar]
- 3.Birnboim H C, Doly J. A rapid alkaline extraction procedure for screening recombinant plasmid DNA. Nucleic Acids Res. 1979;7:1513–1523. doi: 10.1093/nar/7.6.1513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bryan R, Feldman M, Jawetz S C, Rajan S, DiMango E, Tang H B, Scheffler L, Speert D P, Prince A. The effects of aerosolized dextran in a mouse model of Pseudomonas aeruginosa pulmonary infection. J Infect Dis. 1999;179:1449–1458. doi: 10.1086/314755. [DOI] [PubMed] [Google Scholar]
- 5.Davies J. Inactivation of antibiotics and the dissemination of resistance genes. Science. 1994;264:375–382. doi: 10.1126/science.8153624. [DOI] [PubMed] [Google Scholar]
- 6.Davis P B, Drumm M, Konstan M W. Cystic fibrosis. Am J Respir Crit Care Med. 1996;154:1229–1256. doi: 10.1164/ajrccm.154.5.8912731. [DOI] [PubMed] [Google Scholar]
- 7.Demko C A, Byard P J, Davis P B. Gender differences in cystic fibrosis: Pseudomonas aeruginosa infection. J Clin Epidemiol. 1995;48:1041–1049. doi: 10.1016/0895-4356(94)00230-n. [DOI] [PubMed] [Google Scholar]
- 8.Denning G M, Wollenweber L A, Railsback M A, Cox C D, Stoll L L, Britigan B E. Pseudomonas pyocyanin increases interleukin-8 expression by human airway epithelial cells. Infect Immun. 1998;66:5777–5784. doi: 10.1128/iai.66.12.5777-5784.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.DiMango E, Ratner A J, Bryan R, Tabibi S, Prince A. Activation of NF-kappaB by adherent Pseudomonas aeruginosa in normal and cystic fibrosis respiratory epithelial cells. J Clin Investig. 1998;101:2598–2605. doi: 10.1172/JCI2865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Donnelly S C, Strieter R M, Kunkel S L, Walz A, Robertson C R, Carter D C, Grant I S, Pollok A J, Haslett C. Interleukin-8 and development of adult respiratory distress syndrome in at-risk patient groups. Lancet. 1993;341:643–647. doi: 10.1016/0140-6736(93)90416-e. [DOI] [PubMed] [Google Scholar]
- 11.Doyle R. U.S. deaths from pneumonia. Sci Am. 1997;276:29. doi: 10.1038/scientificamerican0297-29. [DOI] [PubMed] [Google Scholar]
- 12.Evanoff H L, Burdick M D, Moore S A, Kunkel S L, Strieter R M. A sensitive ELISA for the detection of human monocyte chemoattractant protein-1 (MCP-1) Immunol Investig. 1992;21:39–45. doi: 10.3109/08820139209069361. [DOI] [PubMed] [Google Scholar]
- 13.Fleming T J, Fleming M L, Malek T R. Selective expression of Ly-6G on myeloid lineage cells in mouse bone marrow. RB6-8C5 mAb to granulocyte-differentiation antigen (Gr-1) detects members of the Ly-6 family. J Immunol. 1993;151:2399–2408. [PubMed] [Google Scholar]
- 14.Goodman R B, Wood R G, Martin T R, Hanson-Painton O, Kinasewitz G T. Cytokine-stimulated human mesothelial cells produce chemotactic activity for neutrophils including NAP-1/IL-8. J Immunol. 1992;148:457–465. [PubMed] [Google Scholar]
- 15.Greenberger M J, Strieter R M, Kunkel S L, Danforth J M, Goodman R E, Standiford T J. Neutralization of IL-10 increases survival in a murine model of Klebsiella pneumonia. J Immunol. 1995;155:722–729. [PubMed] [Google Scholar]
- 16.Greenberger M J, Strieter R M, Kunkel S L, Danforth J M, Laichalk L L, McGillicuddy D C, Standiford T J. Neutralization of macrophage inflammatory protein-2 attenuates neutrophil recruitment and bacterial clearance in murine Klebsiella pneumonia. J Infect Dis. 1996;173:159–165. doi: 10.1093/infdis/173.1.159. [DOI] [PubMed] [Google Scholar]
- 17.Grogan J B. Altered neutrophil phagocytic function in burn patients. J Trauma. 1976;16:734–738. doi: 10.1097/00005373-197609000-00009. [DOI] [PubMed] [Google Scholar]
- 18.Heeckeren A, Walenga R, Konstan M W, Bonfield T, Davis P B, Ferkol T. Excessive inflammatory response of cystic fibrosis mice to bronchopulmonary infection with Pseudomonas aeruginosa. J Clin Investig. 1997;100:2810–2815. doi: 10.1172/JCI119828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Holmes W E, Lee J, Kuang W J, Rice G C, Wood W I. Structure and functional expression of a human interleukin-8 receptor. Science. 1991;253:1278–1280. [PubMed] [Google Scholar]
- 20.Konstan M W, Berger M. Current understanding of the inflammatory process in cystic fibrosis: onset and etiology. Pediatr Pulmonol. 1997;24:137–142. doi: 10.1002/(sici)1099-0496(199708)24:2<137::aid-ppul13>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 21.Konstan M W, Byard P J, Hoppel C L, Davis P B. Effect of high-dose ibuprofen in patients with cystic fibrosis. N Engl J Med. 1995;332:848–854. doi: 10.1056/NEJM199503303321303. [DOI] [PubMed] [Google Scholar]
- 22.Kooguchi K, Hashimoto S, Kobayashi A, Kitamura Y, Kudoh I, Wiener-Kronish J, Sawa T. Role of alveolar macrophages in initiation and regulation of inflammation in Pseudomonas aeruginosa pneumonia. Infect Immun. 1998;66:3164–3169. doi: 10.1128/iai.66.7.3164-3169.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lai L, Alaverdi N, Maltais L, Morse H C., III Mouse cell surface antigens: nomenclature and immunophenotyping. J Immunol. 1998;160:3861–3868. [PubMed] [Google Scholar]
- 24.Lee J, Cacalano G, Camerato T, Toy K, Moore M W, Wood W I. Chemokine binding and activities mediated by the mouse IL-8 receptor. J Immunol. 1995;155:2158–2164. [PubMed] [Google Scholar]
- 25.Lewinsohn D M, Bargatze R F, Butcher E C. Leukocyte-endothelial cell recognition: evidence of a common molecular mechanism shared by neutrophils, lymphocytes, and other leukocytes. J Immunol. 1987;138:4313–4321. [PubMed] [Google Scholar]
- 26.Loetscher P, Seitz M, Clark-Lewis I, Baggiolini M, Moser B. Both interleukin-8 receptors independently mediate chemotaxis. Jurkat cells transfected with IL-8R1 or IL-8R2 migrate in response to IL-8, GRO alpha and NAP-2. FEBS Lett. 1994;341:187–192. doi: 10.1016/0014-5793(94)80454-0. [DOI] [PubMed] [Google Scholar]
- 27.Luster A D. Chemokines—chemotactic cytokines that mediate inflammation. N Engl J Med. 1998;338:436–445. doi: 10.1056/NEJM199802123380706. [DOI] [PubMed] [Google Scholar]
- 28.Massion P P, Inoue H, Richman-Eisenstat J, Grunberger D, Jorens P G, Housset B, Pittet J F, Wiener-Kronish J P, Nadel J A. Novel Pseudomonas product stimulates interleukin-8 production in airway epithelial cells in vitro. J Clin Investig. 1994;93:26–32. doi: 10.1172/JCI116954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mehrad B, Strieter R M, Moore T A, Tsai W C, Lira S A, Standiford T J. CXC chemokine receptor-2 ligands are necessary components of neutrophil-mediated host defense in invasive pulmonary aspergillosis. J Immunol. 1999;163:6086–6094. [PubMed] [Google Scholar]
- 30.Miller E J, Cohen A B, Nagao S, Griffith D, Maunder R J, Martin T R, Weiner-Kronish J P, Sticherling M, Christophers E, Matthay M A. Elevated levels of NAP-1/interleukin-8 are present in the airspaces of patients with the adult respiratory distress syndrome and are associated with increased mortality. Am Rev Respir Dis. 1992;146:427–432. doi: 10.1164/ajrccm/146.2.427. [DOI] [PubMed] [Google Scholar]
- 31.Mori N, Oishi K, Sar B, Mukaida N, Nagatake T, Matsushima K, Yamamoto N. Essential role of transcription factor nuclear factor-κB in regulation of interleukin-8 gene expression by nitrite reductase from Pseudomonas aeruginosa in respiratory epithelial cells. Infect Immun. 1999;67:3872–3878. doi: 10.1128/iai.67.8.3872-3878.1999. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 32.Morohashi H, Miyawaki T, Nomura H, Kuno K, Murakami S, Matsushima K, Mukaida N. Expression of both types of human interleukin-8 receptors on mature neutrophils, monocytes, and natural killer cells. J Leukoc Biol. 1995;57:180–187. doi: 10.1002/jlb.57.1.180. [DOI] [PubMed] [Google Scholar]
- 33.Oishi K, Sar B, Wada A, Hidaka Y, Matsumoto S, Amano H, Sonoda F, Kobayashi S, Hirayama T, Nagatake T, Matsushima K. Nitrite reductase from Pseudomonas aeruginosa induces inflammatory cytokines in cultured respiratory cells. Infect Immun. 1997;65:2648–2655. doi: 10.1128/iai.65.7.2648-2655.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pennline K J, Pellerito F, DaFonseca M, Monahan P, Siegel M I, Smith S R. Flow cytometric analysis of recombinant murine GM-CSF (rmuGM-CSF) induced changes in the distribution of specific cell populations in vivo. Cytometry. 1990;11:283–291. doi: 10.1002/cyto.990110209. [DOI] [PubMed] [Google Scholar]
- 35.Rossi D L, Hurst S D, Xu Y, Wang W, Menon S, Coffman R L, Zlotnik A. Lungkine, a novel CXC chemokine, specifically expressed by lung bronchoepithelial cells. J Immunol. 1999;162:5490–5497. [PubMed] [Google Scholar]
- 36.Rovai L E, Herschman H R, Smith J B. The murine neutrophil-chemoattractant chemokines LIX, KC, and MIP-2 have distinct induction kinetics, tissue distributions, and tissue-specific sensitivities to glucocorticoid regulation in endotoxemia. J Leukoc Biol. 1998;64:494–502. doi: 10.1002/jlb.64.4.494. [DOI] [PubMed] [Google Scholar]
- 37.Sar B, Oishi K, Matsushima K, Nagatake T. Induction of interleukin 8 (IL-8) production by Pseudomonas nitrite reductase in human alveolar macrophages and epithelial cells. Microbiol Immunol. 1999;43:409–417. doi: 10.1111/j.1348-0421.1999.tb02424.x. [DOI] [PubMed] [Google Scholar]
- 38.Smith J B, Rovai L E, Herschman H R. Sequence similarities of a subgroup of CXC chemokines related to murine LIX: implications for the interpretation of evolutionary relationships among chemokines. J Leukoc Biol. 1997;62:598–603. doi: 10.1002/jlb.62.5.598. [DOI] [PubMed] [Google Scholar]
- 39.Standiford T J, Kunkel S L, Basha M A, Chensue S W, Lynch III J P, Toews G B, Westwick J, Strieter R M. Interleukin-8 gene expression by a pulmonary epithelial cell line. A model for cytokine networks in the lung. J Clin Investig. 1990;86:1945–1953. doi: 10.1172/JCI114928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Standiford T J, Strieter R M, Lukacs N W, Kunkel S L. Neutralization of IL-10 increases lethality in endotoxemia. Cooperative effects of macrophage inflammatory protein-2 and tumor necrosis factor. J Immunol. 1995;155:2222–2229. [PubMed] [Google Scholar]
- 41.Strieter R M, Kunkel S L. Chemokines. Vol. 1. 1996. Coordinating eds., R. G. Crystal, J. B. West, E. R. Weibel, and P. J. Barnes. Lippincott-Raven, Philadelphia, Pa. [Google Scholar]
- 42.Strieter R M, Kunkel S L, Burdick M D, Lincoln P M, Walz A. The detection of a novel neutrophil-activating peptide (ENA-78) using a sensitive ELISA. Immunol Investig. 1992;21:589–596. doi: 10.3109/08820139209069393. [DOI] [PubMed] [Google Scholar]
- 43.Svarva P L, Lyng R V, Maeland J A. Emergence of beta-lactam multiresistant variants of gram-negative bacilli in the presence of cefotaxime. Scand J Infect Dis. 1985;17:387–391. doi: 10.3109/13813458509058779. [DOI] [PubMed] [Google Scholar]
- 44.Tepper R I, Coffman R L, Leder P. An eosinophil-dependent mechanism for the antitumor effect of interleukin-4. Science. 1992;257:548–551. doi: 10.1126/science.1636093. [DOI] [PubMed] [Google Scholar]
- 45.Thomas K M, Taylor L, Navarro J. The interleukin-8 receptor is encoded by a neutrophil-specific cDNA clone, F3R. J Biol Chem. 1991;266:14839–14841. [PubMed] [Google Scholar]
- 46.Toews G B, Gross G N, Pierce A K. The relationship of inoculum size to lung bacterial clearance and phagocytic cell response in mice. Am Rev Respir Dis. 1979;120:559–566. doi: 10.1164/arrd.1979.120.3.559. [DOI] [PubMed] [Google Scholar]
- 47.Tsai W C, Strieter R M, Wilkowski J M, Bucknell K A, Burdick M D, Lira S A, Standiford T J. Lung-specific transgenic expression of KC enhances resistance to Klebsiella pneumoniae in mice. J Immunol. 1998;161:2435–2440. [PubMed] [Google Scholar]
- 48.Wolpe S D, Cerami A. Macrophage inflammatory proteins 1 and 2: members of a novel superfamily of cytokines. FASEB J. 1989;3:2565–2573. doi: 10.1096/fasebj.3.14.2687068. [DOI] [PubMed] [Google Scholar]
- 49.Wolpe S D, Davatelis G, Sherry B, Beutler B, Hesse D G, Nguyen H T, Moldawer L L, Nathan C F, Lowry S F, Cerami A. Macrophages secrete a novel heparin-binding protein with inflammatory and neutrophil chemokinetic properties. J Exp Med. 1988;167:570–581. doi: 10.1084/jem.167.2.570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yoshimura T, Johnson D G. cDNA cloning and expression of guinea pig neutrophil attractant protein-1 (NAP-1). NAP-1 is highly conserved in guinea pig. J Immunol. 1993;151:6225–6236. [PubMed] [Google Scholar]