Abstract
Background
Healthcare workers can suffer from work‐related stress as a result of an imbalance of demands, skills and social support at work. This may lead to stress, burnout and psychosomatic problems, and deterioration of service provision. This is an update of a Cochrane Review that was last updated in 2015, which has been split into this review and a review on organisational‐level interventions.
Objectives
To evaluate the effectiveness of stress‐reduction interventions targeting individual healthcare workers compared to no intervention, wait list, placebo, no stress‐reduction intervention or another type of stress‐reduction intervention in reducing stress symptoms.
Search methods
We used the previous version of the review as one source of studies (search date: November 2013). We searched the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, Embase, PsycINFO, CINAHL, Web of Science and a trials register from 2013 up to February 2022.
Selection criteria
We included randomised controlled trials (RCT) evaluating the effectiveness of stress interventions directed at healthcare workers. We included only interventions targeted at individual healthcare workers aimed at reducing stress symptoms.
Data collection and analysis
Review authors independently selected trials for inclusion, assessed risk of bias and extracted data. We used standard methodological procedures expected by Cochrane. We categorised interventions into ones that:
1. focus one’s attention on the (modification of the) experience of stress (thoughts, feelings, behaviour);
2. focus one’s attention away from the experience of stress by various means of psychological disengagement (e.g. relaxing, exercise);
3. alter work‐related risk factors on an individual level; and ones that
4. combine two or more of the above.
The crucial outcome measure was stress symptoms measured with various self‐reported questionnaires such as the Maslach Burnout Inventory (MBI), measured at short term (up to and including three months after the intervention ended), medium term (> 3 to 12 months after the intervention ended), and long term follow‐up (> 12 months after the intervention ended).
Main results
This is the second update of the original Cochrane Review published in 2006, Issue 4. This review update includes 89 new studies, bringing the total number of studies in the current review to 117 with a total of 11,119 participants randomised.
The number of participants per study arm was ≥ 50 in 32 studies. The most important risk of bias was the lack of blinding of participants.
Focus on the experience of stress versus no intervention/wait list/placebo/no stress‐reduction intervention
Fifty‐two studies studied an intervention in which one's focus is on the experience of stress. Overall, such interventions may result in a reduction in stress symptoms in the short term (standardised mean difference (SMD) ‐0.37, 95% confidence interval (CI) ‐0.52 to ‐0.23; 41 RCTs; 3645 participants; low‐certainty evidence) and medium term (SMD ‐0.43, 95% CI ‐0.71 to ‐0.14; 19 RCTs; 1851 participants; low‐certainty evidence). The SMD of the short‐term result translates back to 4.6 points fewer on the MBI‐emotional exhaustion scale (MBI‐EE, a scale from 0 to 54). The evidence is very uncertain (one RCT; 68 participants, very low‐certainty evidence) about the long‐term effect on stress symptoms of focusing one's attention on the experience of stress.
Focus away from the experience of stress versus no intervention/wait list/placebo/no stress‐reduction intervention
Forty‐two studies studied an intervention in which one's focus is away from the experience of stress. Overall, such interventions may result in a reduction in stress symptoms in the short term (SMD ‐0.55, 95 CI ‐0.70 to ‐0.40; 35 RCTs; 2366 participants; low‐certainty evidence) and medium term (SMD ‐0.41 95% CI ‐0.79 to ‐0.03; 6 RCTs; 427 participants; low‐certainty evidence). The SMD on the short term translates back to 6.8 fewer points on the MBI‐EE. No studies reported the long‐term effect.
Focus on work‐related, individual‐level factors versus no intervention/no stress‐reduction intervention
Seven studies studied an intervention in which the focus is on altering work‐related factors. The evidence is very uncertain about the short‐term effects (no pooled effect estimate; three RCTs; 87 participants; very low‐certainty evidence) and medium‐term effects and long‐term effects (no pooled effect estimate; two RCTs; 152 participants, and one RCT; 161 participants, very low‐certainty evidence) of this type of stress management intervention.
A combination of individual‐level interventions versus no intervention/wait list/no stress‐reduction intervention
Seventeen studies studied a combination of interventions. In the short‐term, this type of intervention may result in a reduction in stress symptoms (SMD ‐0.67 95%, CI ‐0.95 to ‐0.39; 15 RCTs; 1003 participants; low‐certainty evidence). The SMD translates back to 8.2 fewer points on the MBI‐EE. On the medium term, a combination of individual‐level interventions may result in a reduction in stress symptoms, but the evidence does not exclude no effect (SMD ‐0.48, 95% CI ‐0.95 to 0.00; 6 RCTs; 574 participants; low‐certainty evidence). The evidence is very uncertain about the long term effects of a combination of interventions on stress symptoms (one RCT, 88 participants; very low‐certainty evidence).
Focus on stress versus other intervention type
Three studies compared focusing on stress versus focusing away from stress and one study a combination of interventions versus focusing on stress. The evidence is very uncertain about which type of intervention is better or if their effect is similar.
Authors' conclusions
Our review shows that there may be an effect on stress reduction in healthcare workers from individual‐level stress interventions, whether they focus one's attention on or away from the experience of stress. This effect may last up to a year after the end of the intervention. A combination of interventions may be beneficial as well, at least in the short term. Long‐term effects of individual‐level stress management interventions remain unknown. The same applies for interventions on (individual‐level) work‐related risk factors.
The bias assessment of the studies in this review showed the need for methodologically better‐designed and executed studies, as nearly all studies suffered from poor reporting of the randomisation procedures, lack of blinding of participants and lack of trial registration. Better‐designed trials with larger sample sizes are required to increase the certainty of the evidence. Last, there is a need for more studies on interventions which focus on work‐related risk factors.
Keywords: Humans, Anxiety, Anxiety/diagnosis, Emotions, Health Personnel, Health Personnel/psychology, Occupational Stress, Occupational Stress/prevention & control, Psychotherapy, Psychotherapy/methods
Plain language summary
The effect of individual‐level interventions for reducing stress in healthcare workers
Key messages
‐ Individual‐level interventions in which one’s attention is on the experience of stress (like focusing on thoughts, feelings, behaviour) or away from the experience of stress (like exercising, relaxing) may reduce stress among healthcare workers up to one year after the intervention.
‐ A combination of individual‐level interventions may reduce stress up to a couple of months after the intervention.
‐ We do not know if interventions that focus on work‐related risk factors on an individual level have any effect on stress.
What is stress?
There is currently no clear definition of (work‐related) stress. This review is about healthcare workers with low levels of stress to moderate distress and burnout, which might lead to depression and anxiety but does not have to. People with stress can experience physical symptoms like headaches, muscle tension or pain, but also mental symptoms, like impaired concentration. They can also have behavioural problems (like conflicts with other people) and emotional problems (like emotional instability).
What can be done about stress among healthcare workers?
Stress among healthcare workers can be tackled at an organisational level, but also at an individual level. Stress management interventions at the individual‐level aim to:
‐ focus one’s attention on the experience of stress (thoughts, feelings, behaviour), for example by cognitive‐behavioural therapy or coping skills training;
‐ focus one’s attention away from the experience of stress, for example by yoga, Tai Chi, drawing, or acupuncture;
‐ alter work‐related risk factors on an individual level, such as alterations in work demands.
What did we want to find out?
We wanted to find out if various types of individual‐level stress management interventions are better than no intervention (or another intervention) to reduce stress among healthcare workers currently working as such.
What did we do
We searched for studies that looked at stress management interventions in healthcare workers and reported on stress symptoms. The healthcare workforce comprises a wide variety of professions and occupations who provide some type of healthcare service, including direct care practitioners and allied professionals.
We compared and summarised the results of the studies and rated our confidence in the evidence, based on factors such as study methods and study size.
What did we find?
We found a total of 117 studies that involved a total of 11,119 healthcare workers. Most studies followed their participants up to three months and some up to 12 months, but only few longer than a year.
We found that there may be an effect on stress reduction in healthcare workers from stress management interventions, whether they focus one's attention on or away from the experience of stress. This effect may last up to a year after the end of the intervention. A combination of interventions may be beneficial as well, at least in the short term. The long‐term effects of stress management interventions, longer than a year after the intervention has ended, remain unknown. The same applies for interventions on (individual‐level) work‐related risk factors.
What are the limitations of the evidence?
The estimates of the effects of individual‐level stress management interventions may be biassed because of a lack of blinding of the participants in the included studies. Furthermore, many studies were relatively small. Taken together, our confidence in the effects we found is reduced.
How up to date is this evidence?
The evidence is up‐to‐date to February 2022.
Summary of findings
Summary of findings 1. An intervention in which one's attention is on the experience of stress (feelings, thoughts, behavior) compared to no intervention/wait list/placebo/no stress‐reduction intervention for stress reduction in healthcare workers.
| An intervention in which one's attention is on the experience of stress compared to no intervention/wait list/placebo/no stress‐reduction intervention for stress reduction in healthcare workers | ||||
| Patient or population: healthcare workers Setting: various healthcare settings Intervention: an intervention in which one's attention is on the experience of stress Comparison: no intervention/wait list/placebo/no stress‐reduction intervention | ||||
| Outcomes | Anticipated absolute effects* (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | What happens |
| Effect with an intervention in which one's attention is on the experience of stress | ||||
| Stress symptoms (follow‐up up to and including 3 months after end of intervention) | SMD 0.37 lower (0.52 lower to 0.23 lower) | 3645 (41 RCTs) | ⊕⊕⊝⊝ Low1 | On the short term, an intervention in which one's attention is on the experience of stress may result in a reduction in stress symptoms. The standardized mean difference translates back to 4.6 fewer (6.4 fewer to 2.8 fewer) points on the MBI‐emotional exhaustion scale2. |
| Stress symptoms (follow‐up > 3 to 12 months after end of intervention) | SMD 0.43 lower (0.71 lower to 0.14 lower) | 1851 (19 RCTs) | ⊕⊕⊝⊝ Low1 | On the medium term, focus one's attention on the experience of stress may result in a reduction in stress symptoms. The standardized mean difference translates back to 5.3 fewer (8.7 fewer to 1.7 fewer) points on the MBI‐emotional exhaustion scale3. |
| Stress symptoms (follow‐up >12 months after end of intervention) | no effect estimate | 68 (1 RCT) | ⊕⊝⊝⊝ Very low 2 | The evidence is very uncertain about the long‐term effect on stress symptoms of focusing one's attention on the experience of stress. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; SMD: standardized mean difference | ||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||
1 The certainty of the evidence was downgraded by two levels for very serious risk of bias (bias arising from the randomisation process and lack of blinding; i.e. performance bias) in combination with some inconsistency and suspicion of publication bias.
2 The certainty of the evidence was downgraded by three levels for very serious risk of bias (bias arising from the randomisation process and lack of blinding; i.e. performance bias) and very serious imprecision (small sample size, the confidence interval includes both a benefit and a harm).
3 The MBI‐Emotional exhaustion scale has a total score of 54 and we used the mean score (23.6) and standard deviation (12.2) of the control healthcare workers population in Fiol DeRoque 2021 as reference for interpreting the effect sizes. A score below 18 points is regarded as a low score on emotional exhaustion and a score above 36 as a high score on emotional exhaustion (Maslach 1996).
Summary of findings 2. An intervention in which one's attention is away from the experience of stress compared to no intervention/wait list/placebo/no stress‐reduction intervention for stress reduction in healthcare workers.
| An intervention in which one's attention is away from the experience of stress compared to no intervention/wait list/placebo/no stress‐reduction intervention for stress reduction in healthcare workers | ||||
| Patient or population: healthcare workers Setting: various healthcare settings Intervention: an intervention in which one's attention is away from the experience of stress Comparison: no intervention/wait list/placebo/no stress‐reduction intervention | ||||
| Outcomes | Anticipated absolute effects* (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | What happens |
| Risk with an intervention in which one's attention is away from the experience of stress | ||||
| Stress symptoms (follow‐up up to and including 3 months after end of intervention) | SMD 0.55 lower (0.70 lower to 0.40 lower) | 2366 (35 RCTs) | ⊕⊕⊝⊝ Low 1 | On the short term, an intervention in which one's attention is away from the experience of stress may result in a reduction in stress symptoms. The standardized mean difference translates back to 6.8 fewer (8.6 fewer to 4.9 fewer) points on the MBI‐emotional exhaustion scale2. |
| Stress symptoms (follow‐up > 3 to 12 months after end of intervention) | SMD 0.41 lower (0.79 lower to 0.03 lower) | 427 (6 RCTs) | ⊕⊕⊝⊝ Low 1 | On the medium term, an intervention in which one's attention is away from the experience of stress may result in a reduction in stress symptoms. The standardized mean difference translates back to 5.0 fewer (9.7 fewer to 0.4 fewer) points on the MBI‐emotional exhaustion scale2. |
| Stress symptoms (follow‐up >12 months after end of intervention) | ‐ | (0 RCTs) | ‐ | No studies reported the long‐term effect on stress symptoms of focusing one's attention away from the experience of stress. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; SMD: standardized mean difference | ||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||
1 The certainty of the evidence was downgraded by two levels for very serious risk of bias (bias arising from the randomisation process and lack of blinding; i.e. performance bias) in combination with some inconsistency and suspicion of publication bias.
3 The MBI‐emotional exhaustion scale has a total score of 54 and we used the mean score (23.6) and standard deviation (12.2) of the control healthcare workers population in Fiol DeRoque 2021 as reference for interpreting the effect sizes. A score below 18 points is regarded as a low score on emotional exhaustion and a score above 36 as a high score on emotional exhaustion (Maslach 1996).
Summary of findings 3. An intervention in which the focus is on work‐related risk factors on an individual level compared to no intervention/no stress‐reduction interventionfor stress reduction in healthcare workers.
| An intervention in which the focus is on work‐related risk factors on an individual level compared to no intervention/no stress‐reduction intervention for stress reduction in healthcare workers | ||||
| Patient or population: healthcare workers Setting: various healthcare settings Intervention: an intervention in which the focus is on work‐related risk factors on an individual level Comparison: No intervention/no stress‐reduction intervention | ||||
| Outcomes | Anticipated absolute effects* (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | What happens |
| Effect with an intervention in which the focus is on work‐related risk factors on an individual level | ||||
| Stress symptoms (follow‐up up to and including 3 months after end of intervention) | no effect estimate | 87 (3 RCTs) | ⊕⊝⊝⊝ Very low 1 | The evidence is very uncertain about the short‐term effect of an intervention in which the focus is on work‐related risk factors on stress symptoms. |
| Stress symptoms (follow‐up > 3 to 12 months after end of intervention) | no effect estimate | 152 (2 RCTs) | ⊕⊝⊝⊝ Very low 2 | The evidence is very uncertain about the medium‐term effect of an intervention in which the focus is on work‐related risk factors on stress symptoms. |
| Stress symptoms (follow‐up >12 months after end of intervention) | no effect estimate | 161 (1 RCT) | ⊕⊝⊝⊝ Very low 2 | The evidence is very uncertain about the long‐term effect of an intervention in which the focus is on work‐related risk factors on stress symptoms. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; SMD: standardized mean difference; MD: mean difference | ||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||
1 The certainty of the evidence was downgraded by three levels for very serious risk of bias (bias arising from the randomisation process and lack of blinding; i.e. performance bias), inconsistency and very serious imprecision (small sample size, the confidence interval includes both a benefit and a harm).
2 The certainty of the evidence was downgraded by three levels for very serious risk of bias (bias arising from the randomisation process and lack of blinding; i.e. performance bias) and very serious imprecision (small sample size, the confidence interval includes both a benefit and no effect).
Summary of findings 4. A combination of individual‐level interventions compared to no intervention/wait list/no stress‐reduction intervention for stress reduction in healthcare workers.
| A combination of individual‐level interventions compared to no intervention/wait list/no stress‐reduction intervention for stress reduction in healthcare workers | ||||
| Patient or population: healthcare workers Setting: various healthcare settings Intervention: a combination of individual‐level interventions Comparison: no intervention/wait list/no stress‐reduction intervention | ||||
| Outcomes | Anticipated absolute effects* (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | What happens |
| Effect with a combination of individual‐level interventions | ||||
| Stress symptoms (follow‐up up to and including 3 months after end of intervention) | SMD 0.67 lower (0.95 lower to 0.39 lower) | 1003 (15 RCTs) | ⊕⊕⊝⊝ Low 1 | On the short term, a combination of individual‐level interventions may result in a reduction in stress symptoms. The standardized mean difference translates back to 8.2 fewer (11.7 fewer to 4.8 fewer) points on the MBI‐Emotional exhaustion scale4. |
| Stress symptoms (follow‐up > 3 to 12 months after end of intervention) | SMD 0.48 lower (0.95 lower to 0.00) | 574 (6 RCTs) | ⊕⊕⊝⊝ Low 2 | On the medium term, a combination of individual‐level interventions may result in a reduction in stress symptoms, but the evidence does not exclude no effect. The standardized mean difference translates back to 5.9 fewer points (11.7 fewer to no difference) on the MBI‐Emotional exhaustion scale4. |
| Stress symptoms (follow‐up >12 months after end of intervention) | no effect estimate | 88 (1 RCT) | ⊕⊝⊝⊝ Very low 3 | The evidence is very uncertain about the long‐term effect of a combination of individual‐level interventions on stress symptoms. |
| CI: confidence interval; SMD: standardized mean difference | ||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||
1 The certainty of the evidence was downgraded by two levels for very serious risk of bias (bias arising from the randomisation process and lack of blinding; i.e. performance bias) in combination with some inconsistency and suspicion of publication bias.
2 The certainty of the evidence was downgraded by two levels for very serious risk of bias (lack of blinding; i.e. performance bias) and inconsistency. We did not downgrade for imprecision, as the wide confidence interval is due to the inconsistency between study results.
3 The certainty of the evidence was downgraded by three levels for very serious risk of bias (bias arising from the randomisation process and lack of blinding; i.e. performance bias) and very serious imprecision (small sample size, the confidence interval includes both a benefit and a harm).
4 The MBI‐emotional exhaustion scale has a total score of 54 and we used the mean score (23.6) and standard deviation (12.2) of the control HCW population in Fiol DeRoque 2021 as reference for interpreting the effect sizes. A score below 18 points is regarded as a low score on emotional exhaustion and a score above 36 as a high score on emotional exhaustion (Maslach 1996).
Background
This is the second update of the original Cochrane Review (Marine 2006) published in 2006, Issue 4. Healthcare workers can suffer from work‐related stress as a result of organisational factors and an imbalance of demands, skills, and social support at work. Prolonged exposure to these factors negatively impacts the service these workers are able to provide (Tawfik 2019). Frequently, this leads to severe distress, burnout, or psychosomatic disorders amongst healthcare works and subsequent deterioration in service quality (Tawfik 2019).
Description of the condition
Healthcare workers are at high risk of work‐related stress compared to the general working population. Prolonged exposure to work‐related stressors can overwhelm the coping capacities of healthcare workers leading to work‐related stress, which can gradually develop into a Stress‐Related Disorder (SRD) (van der Molen 2020). Symptoms of stress or SRDs, can manifest as physical (e.g. headaches, muscle tension or pain), mental (impaired concentration), behavioural (conflict with other people), and emotional (emotional instability) problems (van Dam 2021).
It is challenging to determine the prevalence of SRDs globally as there is little agreement on the case definition (De Hert 2020). However, multiple studies report high levels of stress and burnout in groups of healthcare workers representing various disciplines. For example, Bridgeman 2018 reported that 30% to 70% of physicians and nurses experience burnout symptoms, while another study reported that 56% of anaesthesiologists experience burnout symptoms (Bridgeman 2018; De Hert 2020; Sanfilippo 2017).
There are a variety of factors in the workplace that may contribute to SRDs, such as lack of role clarity, effort–reward imbalance, systemic inequities, lack of social support, high emotional demands, and lack of decision authority (Bridgeman 2018; van der Molen 2020). Besides, personal factors, such as perfectionism or high standards, may also add to stress suggesting a multifactorial contribution to the development of SRDs (De Hert 2020).
The consequences of SRDs in healthcare workers are more far‐reaching than in some other professions as they can adversely affect the quality of patient care (Shanafelt 2010). Furthermore, the negative health effects for the individual healthcare worker should also not be underestimated as SRDs have been associated with coronary health problems, but also with low job satisfaction and cynicism (Bridgeman 2018; Costello 2016). SRDs may also affect healthcare organisations due to increased turnover rates and absenteeism (Maunder 2006). SRDs also have a large economic impact (Hassard 2018) which makes identifying effective interventions to reduce this burden an urgent one.
Description of the intervention
Interventions at both the organisational level and the individual employee level are needed to prevent and reduce work‐related stress in healthcare workers. The scope of this review is limited to stress management interventions at the individual level. After the previous update of this review, we decided to modify our approach in describing individual‐level stress interventions. For this purpose, we looked at stress as a generic term that refers to two distinct concepts, namely ‘stressors’ (environmental characteristics, or thoughts which cause an adverse reaction in the individual) and ‘strain’ (the individual’s adverse reaction to the stressor) (Bamber 2006; Beehr 1987; Knapp 1988). Given these concepts of stress, one can differentiate three separate avenues of intervention: 1. factors in one’s environment (e.g. work) that cause stress (the focus of the Cochrane Review by Giga 2018), 2. one’s thoughts relating to stress, and 3. the adverse emotional experience resulting from the former two. Various cognitive‐behavioural approaches aim to alleviate the experience of stress and prevent it from becoming chronic (e.g. burnout, depression or somatic illness) by changing the ways in which an individual worker thinks about and manages the perception of stressors in his/her work and the resulting thoughts and feelings. The third approach springs from the idea that the emotional experience of stress is harmful in itself, especially when extended over a long period of time, and so the aim of intervention is to alleviate the emotional response directly by, for example, relaxation techniques. In effect, something else is brought in to take the place mostly occupied by stressful thoughts and feelings (Bamber 2006; Beehr 1987; Knapp 1988). In order to maximise usability and intuitiveness of the results of our review, we reframed the latter two approaches as interventions that focus at thoughts and feelings related to stress and as interventions in which the focus is turned away from thoughts and feelings related to stress.
We conceptualised four distinct approaches to addressing work‐related stress at the individual level:
focus one’s attention on the (modification of the) experience of stress (thoughts, feelings, behaviours);
focus one’s attention away from the experience of stress by various means of psychological disengagement;
alter work‐related risk factors on an individual level; and
combine two or more of the above.
The first approach consists of, but is not limited to, the following: cognitive‐behavioural techniques: assertiveness training, coping skills training, and communication skills training. The second approach includes approaches such as relaxation, massage, mindfulness meditation, exercise (e.g. yoga, tai chi, stretch‐release, drawing, acupuncture, etc.), and playing or listening to music.
Note that with regard to mindfulness it is sometimes difficult to judge whether the central element of the intervention is to focus on the experience of stress or away from it. For example, the general principles of mindfulness‐based stress reduction and cognitive‐behavioural therapy are similar such as increased awareness, regulation, cognitive flexibility and goals‐based behaviours. However, some studies such as mindfulness‐meditation solely used mindfulness techniques to shift focus away from the experience of stress by directing attention to the present moment (Hofmann 2017; Tang 2015). We therefore categorise interventions like mindfulness‐based stress reduction as type 1 and mindfulness‐based meditation as type 2.
The third approach focus' on work‐related risk factors and typically includes planning, scheduling, adjusting work demands on an individual level.
The last approach consists of a combination of two or more of the first three approaches. For instance, combining cognitive behavioural techniques with relaxation.
How the intervention might work
By focusing on the experience of stress and its possible causes, it may be possible to manage one's thoughts, feelings, behaviours and to change these by learning new techniques to do so (Beck 2005). For example, cognitive behavioural therapy (CBT) focus' on the thoughts and feelings that drive behaviours. The overarching goal of this approach is to manage stress at work is to help individuals control the automatic thoughts that exacerbate emotional difficulties such as severe distress, burnout, and depression (Beck 2005).
By diverting one's attention away from the experience of stress by means of relaxation, exercise, or something else, it may be possible to reduce the overall experience of stress (Creswell 2014). The goal is to induce a state of mental and bodily calm in order to counteract the agitation caused by stress. This can be achieved by, for example, being a passive recipient of a massage (Mahdizadeh 2019), or by actively performing various exercises such as yoga (Fang 2015). The focus is thus directed towards a specific relaxing activity and away from the unpleasant thoughts and feelings associated with stress (Borges 2021).
Modifying work‐related risk factors on an individual level may also influence stress levels. An example of this approach is that healthcare workers can have a say in their own work schedule or can make adjustments to their workloads or receive training to identify what may cause stress and think about alterations they could make to their job to discuss with their supervisor (Arrigoni 2015).
Why it is important to do this review
An extensive number of reviews have been published on the effectiveness of interventions to reduce stress in healthcare workers (Aryankhesal 2019; Busireddy 2016; Patel 2019; Sanfilippo 2017; Wiederhold 2018; Zhang 2020). However, some reviews are focused on one specific group of healthcare workers like nurses or physicians (Aryankhesal 2019) and other reviews have only focused on the effectiveness of one type of intervention such as mindfulness (Fendel 2021). To the best of our knowledge there are no up‐to‐date reviews that examine the effectiveness of various types of individual‐level interventions aimed at reducing stress in various healthcare workers to provide a more complete overview. Despite the fact that healthcare workers consist of a multitude of job tasks and titles they still form a reasonably homogeneous population such that it is reasonable to assume interventions directed to them would achieve roughly similar results regardless of specific job title.
It is important to offer healthcare workers interventions that are aimed at reducing the adverse effects of stress. When prevention is offered in a timely manner, it can reduce stress and prevent SRDs. It is therefore important to investigate which interventions are effective (Alberdi 2016). Prevention of SRDs has several advantages. Firstly, it can protect the health of the healthcare workers (Bridgeman 2018). Second, it is also better for the quality of patient care (De Hert 2020). And lastly, there is already a shortage of healthcare workers due to high turnover rates and effective prevention of SRDs may help reduce this. However, there is no consensus about which interventions are effective to prevent SRDs in healthcare workers. It is therefore important to publish an updated version of this review, also because healthcare workers have been affected more by SRDs than before the COVID‐19 pandemic (Blake 2020).
Because the characteristics of interventions designed for healthcare workers may be different from those of other occupations, the aim of this review is to determine the effectiveness of interventions to reduce SRDs specifically in healthcare workers. Given the large amount of included studies in the review evaluating all stress interventions in healthcare workers (Ruotsalainen 2015), the update was divided into this review on individual‐level interventions and another one by Giga 2018 which focus' solely on organisational interventions. These two reviews together supersede the review that was first published in 2006 (Marine 2006) and updated in 2015 (Ruotsalainen 2015). Since this review focus' on individual‐level interventions, studies that solely focused on organisational factors (i.e. quantitative demands, emotional tasks, variation of work, influence at work) are excluded.
Objectives
To evaluate the effectiveness of stress‐reduction interventions targeting individual healthcare workers compared to no intervention, wait list, placebo, no stress‐reduction intervention or another type of stress‐reduction intervention in reducing stress symptoms.
Methods
Criteria for considering studies for this review
Types of studies
Consistent with the previous versions of this review, we limited inclusion to randomised controlled trials (RCTs) to evaluate intervention effectiveness. We only included completed studies published in peer‐reviewed scientific journals; abstracts without accompanying full texts and dissertations were excluded.
Types of participants
We included studies in which the interventions were directed at healthcare workers who had not actively sought help for conditions such as burnout, depression, or anxiety disorder. This included all healthcare workers and trainees in any healthcare setting engaged in clinical work. We excluded studies in which any portion of participants were not doing clinical work, e.g. administrators, receptionists or when the outcomes were not reported separately for the participants who were doing clinical work. Personal caregivers who were family members or friends were excluded from this review.
Types of interventions
We included RCTs that evaluated the effectiveness of any type of intervention for individual healthcare workers aimed at preventing or reducing symptoms of stress. We excluded interventions targeting healthcare organisations because they are covered by the Giga 2018 review. Generally, four approaches to managing work‐related stress at the individual level can be distinguished:
1. focus one’s attention on the (modification of the) experience of stress (thoughts, feelings, behaviour);
2. focus one’s attention away from the experience of stress by various means of psychological disengagement;
3. alter work‐related risk factors on an individual level; and
4. combine two or more of the above.
Interventions such as mindfulness‐based stress reduction which focus on increasing awareness, regulation, cognitive flexibility and goals‐based behaviour directly related to stress were classified as type 1, whereas mindfulness ‐based meditation (Hofmann 2017; Tang 2015) that aim to shift attention away from the experience of stress and unpleasant thoughts was in type 2.
We included all trials that compared the effectiveness of an active intervention with no intervention (including usual care), wait list, a placebo intervention, no stress‐reduction intervention or to another type of stress‐reduction intervention.
The distinction between no intervention, wait list, placebo intervention, and no stress‐reduction intervention is not always apparent. We considered the comparison with a placebo intervention when participants were blinded to group assignment and both groups were told that they received a stress reduction intervention and the placebo intervention has no ‘active ingredient’. For instance when transcranial magnetic stimulation is compared to sham transcranial magnetic stimulation (Kim 2016). Trials with placebo arms were combined with those with no‐intervention controls, wait list controls and no stress‐reduction intervention controls in the meta‐analysis.
We considered the comparison with another type of stress‐reduction intervention when both groups received some kind of stress reduction intervention that was not part of regular care. In this comparison participants may or may not be blinded to group assignment. The comparison could include only different types of interventions, for instance, type 1 versus type 2 (psycho‐educational stress management (SMC) vs mindfulness‐based stress reduction (MSBR) (Errazuriz 2022).
Types of outcome measures
We included studies that evaluated the effectiveness of interventions using validated and standardised self‐report questionnaires measuring symptoms of work‐related stress or burnout. We deemed all other outcomes that do not measure stress or its effects on individuals beyond the scope of this review. Examples of excluded outcomes are: risk factors for stress (such as workload, conflicts, support), coping skills, knowledge or attitude change, work performance, patient satisfaction and claims from clients, employee absenteeism and turnover.
We considered the following follow‐up times for outcome measurement:
short term defined as up to and including three months after the intervention has been completed;
medium term defined as more than three months up to 12 months; and
long term defined as 12 months or longer.
Primary outcomes
Validated and standardised self‐report questionnaires measuring symptoms of work‐related stress or burnout examples of these measures include the following.
Perceived Stress Scale (PSS) (Cohen 1983).
Maslach Burnout Inventory (MBI) (comprised of three subscales: emotional exhaustion, depersonalisation, personal accomplishment) (Maslach 1982).
Depression Anxiety Stress Scale (DASS) (Lovibond 1995).
General Health Questionnaire (GHQ) (Goldberg 1991).
Oldenburg Burnout Inventory (OBI) (Demerouti 2003).
Visual Analogue Scale ‐ stress symptoms.
Copenhagen Burnout Inventory (CBI) (Kristensen 2005).
Secondary outcomes
For secondary outcomes we considered all outcome measures of the detrimental effects of stress or burnout. These included measures such as: (a) Psychological symptoms: anxiety and depression, such as the State‐Trait Anxiety Inventory (Spielberger 1970), Beck Depression Inventory (BDI) (Beck 1961) and Hospital Anxiety Depression Scale (HADS) (Zigmond 1983); (b) Measures of the cost‐effectiveness of interventions, such as incremental cost‐effectiveness ratios (ICERs), incremental cost‐per‐QALY (quality‐adjusted life year) and cost‐benefit ratios. Studies that reported only one or more of the secondary outcomes without any primary outcomes were excluded.
Search methods for identification of studies
We used a replacement approach and used the previous review (Ruotsalainen 2015) as one source of studies. Hence, two sources were used:
Included studies in the previous version of this review (Ruotsalainen 2015), search date up to November 2013.
Electronic searches (2013 to February 2022)
Electronic searches
Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library, 2013 to February 2022)
MEDLINE/PubMed (2013 to February 2022)
Embase (2013 to February 2022)
PsycINFO (2013 to February 2022)
CINAHL/EBSCO (2013 to February 2022)
Web of Science (2013 to February 2022)
Searching other resources
We examined the reference lists from included articles and reviews for any additional eligible studies.
Data collection and analysis
Selection of studies
We used Covidence (Covidence 2022) for screening. Six review authors (ST, LE, AL, AT, KN, HM) independently screened titles and abstracts followed by full‐texts against the inclusion criteria. If there was any disagreement, the two review authors involved discussed this until disagreement was resolved.
Data extraction and management
Three review authors conducted the extraction of data by using a made‐to‐measure data extraction form in Covidence (ST, LE, AL) (Covidence 2022). Data extraction of the outcomes was done independently by the three review authors or researchers and students from the medical faculty of the University of Amsterdam. One review author checked all data extraction and reached consensus in cases of conflict. All questions concerning data extraction processes were resolved by discussion with all review authors.
Assessment of risk of bias in included studies
We used the Cochrane risk of bias tool (Higgins 2011) to assess the risk of bias in included studies. The tool includes the following assessment items: adequate sequence generation, allocation concealment, blinding, incomplete outcome data addressed, selective outcome reporting, and other bias.
Measures of treatment effect
We plotted the results of each trial as means and standard deviations (SDs) for continuous outcomes. Because in many cases different instruments were used to measure stress, we transformed the means into standardised mean differences (SMDs).
In many cases multiple similar outcome measures were used, or an instrument had several subscales but no summary measure. In case of multiple similar outcomes, we chose the outcome which we deemed to best represent a measure of stress symptoms in healthcare workers, such as the PSS (Cohen 1983). When study authors used subscales such as with the MBI (Maslach 1996), we chose the subscale that in our view best represented stress, such as the emotional exhaustion scale of the MBI (Maslach 1996).
Unit of analysis issues
For studies that employed a cluster‐randomised design and that reported sufficient data to be included in the meta‐analysis and that did not make an allowance for the design effect, we calculated the design effect based on a fairly large assumed intra‐cluster correlation (ICC) of 0.10. Even though we did not find information for the ICC)for these types of studies we assumed that 0.10 would be a realistic estimate. We used studies from implementation research to support this assumption (Campbell 2001). We followed the methods stated in the Cochrane Handbook for Systematic Reviews of Interventions (Cochrane Handbook, Higgins 2022) for the calculations: design effect = 1+(M‐1)*ICC, where M is the average cluster size and ICC is the intra‐cluster correlation coefficient.
For studies with multiple study arms and one control condition, we combined groups to create a single pair‐wise comparison with the control condition.
For studies with multiple study arms and no control condition, we entered the first two study arms in the meta‐analysis.
Dealing with missing data
Where necessary, we sought missing data (means and standard deviations (SDs)) from authors. In total, 16 study authors either provided data that had not been published in their articles which enabled us to enter these studies into the meta‐analyses, provided clarification on their published article, or referred us to supplementary information (Barattucci 2019; Cohen‐Katz 2005; Dunne 2019; Dyrbye 2019; Errazuriz 2022; Gärtner 2013; Jensen 2006; Kline 2020; Moody 2013a; Oman 2006; Ozgundondu 2019; Pehlivan 2020; Sampson 2019; Sawyer 2021; West 2014; West 2021).
Where necessary and possible, we used WebPlotDigitizer (Rohatgi, 2022) to retrieve means and SDs from figures for the following studies: CezardaCosta 2019; Cheng 2015; Luthar 2017; Kline 2020 (control group only).
When SDs were not reported we calculated them from other reported values according to the methods stated in the Cochrane Handbook (Higgins 2022).
For West 1984 we took the means and SDs that resulted from the post‐hoc comparisons in the repeated measures analyses. For Norvell 1987, we took the post‐treatment values and calculated SDs based on the P value. We calculated a t‐value from this P value even though the authors used a Mann‐Whitney U test. For Shapiro 2005, we took the post‐treatment values and the F‐value reported by the authors. We calculated a t‐value and subsequent SDs by taking the square root of the F‐value as the t‐value. For Tsai 1993, we took the post‐treatment values from the figure reporting the results of the repeated measures' analysis. We took the reported P value belonging to the repeated measures' analysis as if it had resulted from a t‐test and calculated the SDs based on this t‐value. For Ewers 2002, we took the post‐treatment scores and the P values belonging to the independent t‐tests to calculate a t‐value and subsequently SDs.
For Dahlgren 2022 and Gunasingam 2015, we calculated SDs based on 95% confidence intervals (CIs). For CezardaCosta 2019, Mao 2021 and Riley 2017 we calculated SDs based on the standard error (SE.) For Seidel 2021, the N per group was not reported, we assumed that there were an equal number of participants in the two study groups, i.e. 41 and 42.
Lee 2021, Mealer 2014 and Ozgundondu 2019 reported their stress outcomes with a median and interquartile range (IQR). In accordance with the Cochrane Handbook (Higgins 2022) we requested mean and SDs. In the case we did not receive a response, we entered the median and IQR in the meta‐analysis, and we assumed that outcome data were normally distributed.
Participants are included in the groups to which they were originally randomised, but missing data for participants were not included in the denominator.
In the case missing SDs were either not provided by the study authors or could not be calculated, these missing data were not imputed.
Assessment of heterogeneity
We assessed heterogeneity in line with GRADE guidance (Schünemann 2013). We deemed an I² value of more than 50% to indicate considerable heterogeneity. When we identified heterogeneity, we tried to understand the reasons for the heterogeneity by exploring the options outlined in the Cochrane Handbook (Higgins 2022) and we investigated the presence of outlying studies. When the heterogeneity could not be explained, we downgraded the certainty of the evidence. In addition, we calculated the prediction intervals, to provide information about how much the true effect size varies across studies calculated with CMA Prediction Intervals.
Assessment of reporting biases
We avoided reporting bias by including studies and not articles. If multiple articles reported results from a single study, we consolidated all the data from all articles under one study ID only. We avoided language bias by including studies in any language. Because standardised mean differences (SMDs) are related to their standard error (SE) (Zwetsloot 2017), we did not use the SEs to generate a funnel plot instead we used the sample size as recommended by Zwetsloot 2017. The funnel plots were generated in STATA 17 (STATA 2022).
Data synthesis
We combined studies that we deemed sufficiently similar regarding participants, intervention, control, outcome and follow‐up time in one comparison.
We pooled the results statistically when the outcomes were similar concepts, such as perceived stress symptoms. Because many instruments were used, we used SMDs to combine the stress‐related outcomes using meta‐analysis. Not all instruments used one summary score, but presented the results of various subscales. In cases where there was no summary measure, we chose the subscale that best represented a measure of stress. For example, for this analysis, we used only the emotional exhaustion subscale of the Maslach Burnout Inventory (MBI). In this way, we considered the various stress symptoms scales to measure the same concept. We pooled the results using a random‐effects model.
To interpret the effect size, the mean (23.6) and SD (12.2) on the MBI of the control healthcare worker population in Fiol DeRoque 2021 was used. The MBI‐Emotional exhaustion scale has a total score of 54. A score below 18 points is regarded as a low score on emotional exhaustion and a score above 36 as a high score on emotional exhaustion (Maslach 1996).
Subgroup analysis and investigation of heterogeneity
We conducted the following subgroup analyses and incorporated them in all comparisons:
type of intervention (see Types of interventions for more details);
length of follow‐up (see Types of outcome measures for more details);
type of outcome (see Primary outcomes; Secondary outcomes for more details).
On top of those subgroups, we considered the subgroups mentioned in the original protocol, i.e. type of healthcare worker and duration and intensity of the intervention (Marine 2000). When considering those subgroups, we took into account that subgroup effects on top of the current subgroups in interventions and outcomes may prove spurious and may not explain all the variability in the extent of inconsistency, as most putative subgroup effects ultimately prove spurious (Schünemann 2013).
Type of healthcare worker
For the current update of the review that includes only individual‐level interventions, we considered a subgroup analysis by type of healthcare worker as redundant. The reason is that we think that the intervention types included in this review work the same way for various healthcare workers (e.g. physicians, nurses). The previous findings of this review and a recent publication on this topic (de Wijn 2022) supported this assumption. In the previous review update (Ruotsalainen 2015), it was concluded that a subgroup analyses based on type of healthcare worker did not explain heterogeneity (“Since working conditions differ considerable between various occupations in health care, we analysed if there were differences in the effects of CBT and relaxation between various occupations. We did so only for comparisons with sufficient studies: CBT versus no intervention and relaxation versus no intervention. We ignored the previous subgroups in the CBT and relaxation intervention categories and divided the studies according to the occupation of the participants into nurses, physicians, all staff and other healthcare professionals. There were no differences between these subgroups. Within the subgroups however, there was still considerable statistical heterogeneity. We therefore do not think that the occupation of the participants explains statistical heterogeneity between studies.") Therefore, we cancelled this subgroup analysis and reported this in the section "Differences between protocol and review".
Duration and intensity of the intervention
For this update, we discussed the proposed subgroup analyses based on the duration and intensity of the intervention as stated in the original protocol (Marine 2000). We discussed what a proper grouping would be and found that dividing the studies in short or longer and intense or less intense interventions would be an arbitrary approach as no definition was formulated a priori. Moreover, such a grouping would ideally be based on a mixture of the duration and intensity of the intervention (e.g. number of sessions, the length of the sessions, homework assignments) and the compliance with the intervention. However, we explored whether the arbitrary cut‐off for duration of the intervention of 12 weeks shows an effect in effect size. We added this in the "Differences between protocol and review".
Compliance
de Wijn 2022 found that stress management interventions for nurses in which the sample was exposed to the majority of the planned sessions reached greater effect sizes compared to interventions in which the compliance to the intervention/attendance to the planned sessions was lower. This finding should be interpreted with caution due to a lot of missing data (de Wijn 2022). However, we aimed to explore if the effect sizes based on studies in which participants attended 80% or more of the scheduled sessions would differ from the studies where participants attended less than 80% of the scheduled sessions. We added this in the "Differences between protocol and review".
Sensitivity analysis
To assess the effect of risk of bias on the pooled results, we performed a sensitivity analysis in which we excluded studies with a high risk of bias and assessed whether this changed the results appreciably. We defined a study having a high risk of bias overall when we judged it to have a high risk of bias in three or more domains.
Summary of findings and assessment of the certainty of the evidence
We used the GRADE approach to assess the certainty of the body of evidence for the intervention categories and comparisons most important for health decision‐making (Guyatt 2011). A priori, we decided that the comparisons of an intervention with no intervention are most important for decision‐making for the primary outcome of stress symptoms only for all three follow‐up times. Comparisons of one intervention versus another intervention were considered to be less informative. We downgraded the certainty of the evidence by one to three levels depending on the seriousness of the violations in each domain. We considered the risk of bias tables for each study in that intervention category to assess the risk of bias for an intervention category. We downgraded the certainty of the evidence if there were one or more limitations in the following domains: risk of bias, consistency, directness of the evidence, precision of the pooled estimate and the possibility of publication bias. All statements on the effects of interventions, such as in the summary of finding tables and the conclusion were worded in line with the recommendations on communicating findings when using the GRADE approach (Santesso 2020). Review authors ST and JB undertook GRADE, which was then also discussed with JR, RS, KN, LE and HM until consensus was reached.
Results
Description of studies
Results of the search
From the initial set of included articles for the earlier systematic review (Ruotsalainen 2015), we included 28 eligible articles. Furthermore, we included one previously excluded article (Gärtner 2013). The systematic searches updated in 2018 and February 2022 yielded altogether 4776 references, excluding duplicates. We assessed 254 full‐text articles for eligibility and excluded 160. This left 92 new articles. Put together, 120 articles describing 117 studies fulfilled our inclusion criteria (Figure 1).
1.

In addition, we located eight ongoing studies (Baker 2015; Bateman 2020; Bratt 2022; Kuribayashi 2019; Ng 2019; Pérula‐de Torres 2019; Rees 2018; Weiner 2020) for which we could not find published outcome data.
In addition, six studies were published in a language other than English or Dutch, for which we were currently unable to find professional translation (Ahmadi 2019; Ghods 2017; Lu 2020; Rogala 2016; Taft 2021; Xiao Yan 2019). In three studies (Fei 2019; Klatt 2012; Valipour 2020) no full‐text was available, and two (Imamura 2019; Sasaki 2021) did not report on stress symptoms despite being specified in the trial protocol. Details for these studies are provided in "Characteristics of studies awaiting classification".
We sought additional information regarding study details and statistical data or both from 26 included studies, and we received a response from 11 study authors (Barattucci 2019; Dunne 2019; Dyrbye 2019; Errazuriz 2022; Kline 2020; Ozgundondu 2019; Pehlivan 2020; Sampson 2019; Sawyer 2021; West 2014; West 2021). From the set of included studies from Ruotsalainen 2015, the previous author team received additional information from five study authors (Cohen‐Katz 2005; Gärtner 2013; Jensen 2006; Moody 2013a; Oman 2006).
Nine included studies could not be included in the meta‐analysis for various reasons. For Chen 2015, Duchemin 2015, Ghawadra 2020, Martins 2011, Novoa 2014, Palumbo 2012, Schrijnemaekers 2003 and Tonarelli 2018 it was due to missing data. Our efforts to reach these study authors were unsuccessful. Leao 2017 used a dichotomous outcome measure that we could not enter into the meta‐analysis.
One final update search was run on the 26th of September 2022, yielding 555 records excluding duplicates. We assessed 29 full‐text articles for eligibility and excluded 12. Seventeen articles were added to the "Studies awaiting classification" and will be considered in the next update of this review. We furthermore assessed 44 trial registration records and excluded 42. Two were added to the "Ongoing studies" (Al‐Hammouri 2022; Jeffers 2017).
Included studies
This second review update included 117 included studies (11,119 participants), this included an additional 89 studies (8691 participants) since the last update (Ruotsalainen 2015).
Study designs
Of the 117 included studies, 109 were individually randomised controlled trials (RCTs), and eight were cluster‐RCTs.
Seven of the cluster‐RCTs that we included in the meta‐analysis had a unit of analysis error. In other words, these studies ignored the clustering of the data in their analysis. To address this we used a formula (see "Unit of analysis issues") to calculate the design effect based on average cluster size (M) and an intra‐cluster correlation coefficient. We calculated the design effect as 2.4 for the Barbosa 2015 study (four clusters, M = 14.5), 1.5 for Gärtner 2013 (57 clusters, M = 5.4); 2.01 for the Jensen 2006 study (19 clusters, M = 11.05), 2.0 for Kesselheim 2020 (nine clusters, M = 11.1), 3.15 for Sampson 2019 (four clusters, M = 22.5); 3.7 for Verdes Montenegro Atalaya 2021 (six clusters, M = 27.5) and 3.5 for Sharif 2013 (two clusters, M = 26). We used the design effect to reduce the number of participants in both intervention and control groups if we were able to use quantitative outcome data in meta‐analyses.
Country and time period
Forty‐one studies had been carried out in North America, 35 in Europe, 19 in Asia, nine in the Middle East, nine in South America, three in Oceania and one on two continents.
Type of settings and participants
Altogether 94 of the included studies had been conducted in hospitals, four in residential care homes for the elderly or persons with disabilities, 14 in mixed or other healthcare settings, and five in a Medical Emergency service. Sixty studies included exclusively nurses, 23 included physicians, and 34 various or other healthcare staff. Almost all studies (N = 105) did not formulate inclusion or exclusion criteria based on stress symptom levels, while 12 studies (Behnammoghadam 2019; Chen 2015; Ghawadra 2020; Günüsen 2010; Kurebayashi 2012; Kurebayashi 2014; Montibeler 2018; Novoa 2014; Peterson 2008; Prado 2018; Saganha 2012; Stanton 1988) included healthcare workers with a medium and/or high level of stress symptoms only.
Sample sizes
The total number of participants randomised was 11,119. The number of participants per study arm was (Simmons 2018) < 50 in 85 studies (Alexander 2015; Amutio 2015; Aranda Ausern 2016; Axisa 2019; Bagheri 2019; Barbosa 2015; Behnammoghadam 2019; Bernburg 2019; Bernburg 2020; Brennan 2006; CezardaCosta 2019; Cheng 2015; Chesak 2020; Cho 2021; Cohen‐Katz 2005; Concilio 2021; Copeland 2021; deSouza 2021; Dincer 2021; Duchemin 2015; Dunne 2019; Dyrbye 2019; Emani 2020; Errazuriz 2022; Ewers 2002; Gollwitzer 2018; Gunasingam 2015; Günüsen 2010; Hilcove 2021; Ho 2021; Huang 2020a; Janzarik 2022; Kavurmaci 2022; Kharatzadeh 2020; Kim 2016; Kline 2020; Kurebayashi 2012; Leao 2017; Lebares 2021; Lee 1994; Lee 2021; Lin 2015; Lin 2019; Luthar 2017; Mache 2015; Mache 2016; Mache 2017; Mache 2018; Mackenzie 2006; Martins 2011; McGonagle 2020; Mealer 2014; Medisauskaite 2019; Moench 2021; Montibeler 2018; Moody 2013a; Norvell 1987; Novoa 2014; OBrien 2019; Oman 2006; Ozbas 2016; Ozgundondu 2019; Palumbo 2012; Pehlivan 2020; Prado 2018; Redhead 2011; Reynolds 1993; Riley 2017; Saganha 2012; Sampson 2019; Sawyer 2021; Schroeder 2018; Seidel 2021; Shapiro 2005; Sharif 2013; Shin 2020; Sood 2011; Stanton 1988; Tonarelli 2018; Verdes Montenegro Atalaya 2021; West 1984; West 2014; Yazdani 2010; Yung 2004; Zarvijani 2021) and ≥ 50 in 32 studies (Barattucci 2019; Brazier 2022; Chen 2015; Dahlgren 2022; Dyrbye 2016; ElKhamali 2018; Fendel 2021; Finnema 2005; Fiol DeRoque 2021; Foji 2020; Frogeli 2020; Gärtner 2013; Ghawadra 2020; Grabbe 2020; Hersch 2016; Huang 2020; Jensen 2006; Kesselheim 2020; Kurebayashi 2014; Lee 2020; Mandal 2021; Mao 2021; McConachie 2014; Melchior 1996; Montaner 2021; PelitAksu 2020; Peterson 2008; Schrijnemaekers 2003; Tsai 1993; Wei 2017; West 2021; Xie 2020).
Interventions
Fifty‐two studies examined the effectiveness of focusing on the experience of stress (Amutio 2015; Axisa 2019; Bagheri 2019; Barattucci 2019; Behnammoghadam 2019; Cheng 2015; Chesak 2020; Dyrbye 2016; Dyrbye 2019; Errazuriz 2022; Fendel 2021; Fiol DeRoque 2021; Foji 2020; Frogeli 2020; Gärtner 2013; Ghawadra 2020; Gollwitzer 2018; Grabbe 2020; Gunasingam 2015; Günüsen 2010; Huang 2020; Huang 2020a; Jensen 2006; Kesselheim 2020; Kharatzadeh 2020; Lee 1994; Lee 2020; Lin 2019; Mache 2015; Mache 2016; Mache 2017; Mache 2018; Mackenzie 2006; Mao 2021; Martins 2011; McConachie 2014; McGonagle 2020; Medisauskaite 2019; Moody 2013a; Pehlivan 2020; Riley 2017; Sampson 2019; Sawyer 2021; Schroeder 2018; Sharif 2013; Tonarelli 2018; Verdes Montenegro Atalaya 2021; Wei 2017; West 1984; West 2021; Xie 2020; Zarvijani 2021). The content of the interventions varies for instance from cognitive‐behavioral therapy to emotional skills training.
Forty‐two studies examined the effectiveness of focusing away of the experience of stress (Alexander 2015; Aranda Ausern 2016; Brennan 2006; CezardaCosta 2019; Chen 2015; Cho 2021; Cohen‐Katz 2005; Copeland 2021; Dahlgren 2022; deSouza 2021; Dincer 2021; Duchemin 2015; Dunne 2019; Emani 2020; Errazuriz 2022; Hilcove 2021; Ho 2021; Kavurmaci 2022; Kim 2016; Kline 2020; Kurebayashi 2012; Kurebayashi 2014; Leao 2017; Lebares 2021; Lee 2021; Lin 2015; Mandal 2021; Montibeler 2018; Novoa 2014; Oman 2006; Ozgundondu 2019; Palumbo 2012; PelitAksu 2020; Prado 2018; Saganha 2012; Seidel 2021; Shapiro 2005; Shin 2020; Stanton 1988; Tsai 1993; Yazdani 2010; Yung 2004). The content of the interventions varies from yoga to meditation to music listening.
Seven studies examined ways to alter work‐related risk factors on an individual level (Concilio 2021; Ewers 2002; Finnema 2005; Melchior 1996; Peterson 2008; Redhead 2011; Schrijnemaekers 2003).
Seventeen studies examined a combination of interventions (Barbosa 2015; Bernburg 2019; Bernburg 2020; Brazier 2022; ElKhamali 2018; Hersch 2016; Janzarik 2022; Luthar 2017; Mealer 2014; Moench 2021; Montaner 2021; Norvell 1987; OBrien 2019; Ozbas 2016; Reynolds 1993; Sood 2011; West 2014).
Three studies compared only two different types of stress prevention interventions with one another (Barbosa 2015; Riley 2017; Xie 2020).
The duration of the intervention ranged from one session (e.g. Axisa 2019) to 12 weeks (e.g. Chesak 2020) with most interventions lasting a few sessions only.
Type of control group
Most included studies used a no‐intervention control group (N = 72). Another 27 studies used a waiting‐list control group. Eight studies used a no stress‐reduction control group (Brennan 2006; Concilio 2021; Grabbe 2020; Jensen 2006; Mao 2021; Tsai 1993; West 2014; Tonarelli 2018) and another seven studies used a placebo control group (Chen 2015; Fiol DeRoque 2021; Kim 2016; Lee 2021; Prado 2018; Shin 2020; Novoa 2014).
Multiple intervention arms
Fifteen studies compared two or more active stress interventions with a control condition (Cheng 2015; Copeland 2021; Errazuriz 2022; Gärtner 2013; Gollwitzer 2018; Günüsen 2010; Kline 2020; Kurebayashi 2012; Kurebayashi 2014; Leao 2017; Lebares 2021; Pehlivan 2020; Verdes Montenegro Atalaya 2021; West 1984; Yung 2004).
With Cheng 2015; Copeland 2021; Gärtner 2013; Gollwitzer 2018; Günüsen 2010; Kline 2020; Kurebayashi 2012; Kurebayashi 2014; Pehlivan 2020; Verdes Montenegro Atalaya 2021; Yung 2004, we combined intervention arms to create a single pair‐wise comparison.
With Lebares 2021 we entered both interventions in the same comparison with the two control groups. We entered the intervention reported in Errazuriz 2022 in different comparisons. West 1984 had five study arms but finally reported data only on one study arm versus a no‐intervention or no‐effect condition. We used this as an intervention versus no‐intervention comparison. We did not enter Leao 2017 in the comparison as the outcomes were dichotomous.
Multiple control arms
Four studies included two control arms (Jensen 2006; Novoa 2014; Lebares 2021; Prado 2018). With Jensen 2006 we compared the intervention arm with the no stress‐reduction intervention arm. With Prado 2018 we used the placebo control arm instead of the wait list control group. We did not include Novoa 2014 in the meta‐analysis due to missing values. With Lebares 2021 we compared both control arms to the two intervention arms.
Outcomes
Altogether 43 studies used the Maslach Burnout Inventory (MBI) while 29 studies used the Perceived Stress Scale (PSS). The remaining studies used stress symptom questionnaires such as Perceived Stress Questionnaire (PSQ), Depression Anxiety Stress Scale (DASS‐stress), or General Health Questionnaire (GHQ). Twenty‐one studies reported a depression or anxiety outcome measure such as the State‐Trait Anxiety Inventory (STAI), DASS or Center for Epidemiologic Studies Depression Scale (CES‐D).
Only one study (Gärtner 2013) reported the cost‐effectiveness of their intervention.
Follow‐up
(i) Short term
There were 105 studies with an outcome measurement between the end of the intervention up to and including three months after the intervention.
(ii) Medium term
In 34 studies there was a follow‐up measurement between three and 12 months after intervention.
(iii) Long term
Only four studies had a follow‐up measurement more than 12 months after the intervention.
Excluded studies
The main reasons for excluding studies from this review were as follows (see the "Characteristics of excluded studies" for more detail).
1. Wrong outcomes
2. Wrong study design
3. Wrong publication type
4. Wrong population (not only healthcare workers)
5. Wrong intervention
Risk of bias in included studies
In general, we judged most included studies to suffer from methodological issues, with at least two items that we judged to put them at a high risk of bias (Figure 2). We judged only four studies to have no domain with a high risk of bias or to NOT have more than two domains with an uncertain risk of bias (Barbosa 2015; Cheng 2015; deSouza 2021; Fiol DeRoque 2021).
2.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Blinding was consistently problematic in almost all studies because study authors used self‐report to assess stress symptoms as the participants and the providers could not be blinded to the intervention. However, in 14 studies participants were (tried to be) blinded to group assignment (Barbosa 2015; Chen 2015; Cheng 2015; Concilio 2021; deSouza 2021; Fiol DeRoque 2021; Kim 2016; Lebares 2021; Lee 2021; Luthar 2017; Medisauskaite 2019; Novoa 2014; Prado 2018; Shin 2020).
Allocation
Half of the included studies did not clearly describe the method for generating random numbers or did not employ a truly random sequence. It is surprising to note that some of these studies provided only sparse details on the randomisation process. Details of allocation concealment were frequently lacking. In most of the included studies, we assumed that randomisation was applied blind to all eligible participants at the same time. If this assumption is correct then researchers and participants could not foresee assignment. We therefore rated this as unclear risk of bias.
Blinding
We considered the reporting of stress symptoms by questionnaires as an outcome assessment that could be biased by knowledge of the intervention. We judged that it could be possible that a participant in the intervention group, knowing that they have gone through a six‐week course of stress management, would rate their stress symptoms more favourably than a person in the control group. This would create an overestimation of the effect of the intervention. Most authors mentioned that blinding could be an issue, but also discussed that blinding was not possible in these circumstances. We rated these studies as having a high risk of bias. However, in 16 studies, participants were (tried to be) blinded to group assignment. These mainly came from the second category of interventions (focussing away from stress) such as aromatherapy, auriculotherapy or acupressure or studies in which two or more active interventions were compared with one another.
Incomplete outcome data
Twenty‐five percent of the included studies had attrition rates exceeding 20% of the initial sample. When explanations for loss‐to‐follow‐up were missing, when reasons were not entirely random, or when the responders differed from non‐responders on baseline characteristics, we judged these studies to be at high risk of attrition bias. In some studies, it was unclear whether participants dropped out and the studies were therefore labelled as being at unclear risk of bias.
Selective reporting
It is surprising to note that most studies lack a study protocol or trial registration. When studies lacked a protocol, it was difficult to judge if outcomes were reported as planned. If the authors mentioned a protocol, we reviewed the protocol for a priori outcomes. If there was no mention of a protocol we looked online to see whether there was a protocol published. If not, we judged reporting in the study based on the methods and results sections.”. In most studies there was no indication of selective outcome reporting. In one study (Jensen 2006) only significant differences were reported, which we took to be a sign of high risk of bias. In Finnema 2005 the results for nursing assistants consisted of covariance analyses that were not prespecified and because of this, we judged the study to be at high risk of bias. In four studies (Bagheri 2019; Dahlgren 2022; ElKhamali 2018; Errazuriz 2022) the trial protocol mentioned a stress symptom questionnaire that was not reported in the included studies, which we took to be a sign of high risk of bias. In Dincer 2021 participants randomised to the intervention group that did not attend the: Emotional Freedom Techniques (EFT) session (n = 5) were excluded, which we took to be a sign of high risk of bias. In Kurebayashi 2012 the authors present data separately for participants who had high SSL scores to begin with but not at all for participants with a moderate SSL score, which was also categorised as high risk of bias.
Other potential sources of bias
There were several risks of bias that came up in addition to the risks mentioned above, such as low or unclear compliance with the intervention or low or unclear response rate. If other biases were not apparent, we judged the other potential source of bias as low in the risk of bias tool.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4
See: Table 1; Table 2; Table 3; and Table 4 and GRADE assessment of the primary outcomes at the end of this section for full description of how we rated the certainty of the evidence.
1. Focus one's attention on the experience of stress vs. no intervention/wait list/placebo/no stress‐reduction intervention
1.1. Any symptoms of stress‐related outcome (Follow‐up to 3 months after the end of the intervention)
We combined the results of 41 studies. There was a standardised mean difference (SMD; of ‐0.37, 95% confidence interval (CI) ‐0.52 to ‐0.23) showing difference in stress symptoms between the interventions that focus one's attention on the experience of stress and no intervention/wait list/placebo/no stress‐reduction intervention up to and including three months after the end of the intervention (3645 participants; low‐certainty evidence; Analysis 1.1). We found considerable heterogeneity (I2 = 77%) and a 95% prediction interval from ‐1.19 to 0.45. When excluding three outlying SMDs, I2 reduced to 57%. The funnel plot revealed a lack of studies in the right part of the funnel where the negative studies would be expected, indicating that there could be publication bias (Figure 3).
1.1. Analysis.

Comparison 1: ‘Focus one’s attention on the experience of stress (thoughts, feelings, behaviour)’ vs No intervention/wait list/placebo/no stress‐reduction intervention (SMD), Outcome 1: Any symptoms of stress‐related outcome (follow‐up up to 3 months after the end of the intervention)
3.
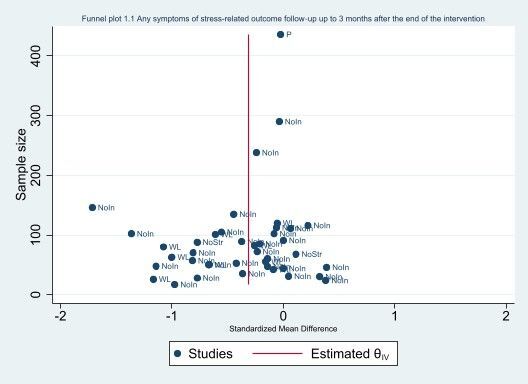
Funnel plot (1.1 Any symptoms of stress‐related outcome (follow‐up up to 3 months after the end of the intervention)
1.2 Any symptoms of stress‐related outcome (Follow‐up from > 3 to 12 months after the end of the intervention)
Results from 19 studies suggested that an intervention focusing on the experience of stress decreased stress symptoms more than no intervention/wait list/no stress‐reduction intervention (SMD ‐0.43, 95% CI ‐0.71 to ‐0.14; 1851 participants; low‐certainty evidence; Analysis 1.2) at > 3 to 12 months follow‐up. We found considerable heterogeneity (I2 = 88%) and a 95% prediction interval from ‐1.70 to 0.84. When excluding two outlying SMDs, I2 reduced to 42%. The funnel plot revealed a lack of studies in the right part of the funnel where the negative studies would be expected, indicating that there could be publication bias (Figure 4).
1.2. Analysis.

Comparison 1: ‘Focus one’s attention on the experience of stress (thoughts, feelings, behaviour)’ vs No intervention/wait list/placebo/no stress‐reduction intervention (SMD), Outcome 2: Any symptoms of stress‐related outcome (follow‐up > 3 to 12 months after the end of the intervention)
4.
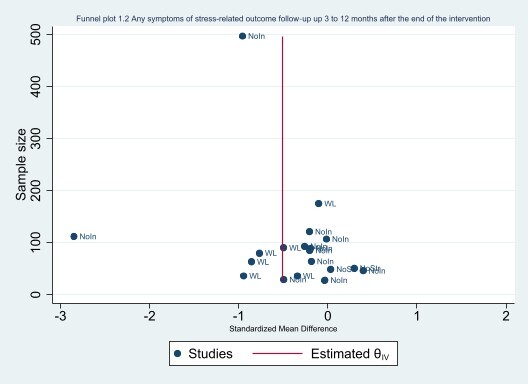
Funnel plot (1.2 Any symptoms of stress‐related outcome (follow‐up > 3 to 12 months after the end of the intervention))
1.3 Any symptoms of stress‐related outcome (Follow‐up > 12 months after the end of the intervention)
One study combining two intervention arms showed no differences (mean difference (MD) 0.40, 95% CI ‐1.50 to 2.30) in stress symptoms of an intervention focusing on the experience of stress compared to no intervention at >12 months of follow‐up (68 participants; very low‐certainty evidence; Analysis 1.3). It was not possible to study heterogeneity or publication bias.
1.3. Analysis.

Comparison 1: ‘Focus one’s attention on the experience of stress (thoughts, feelings, behaviour)’ vs No intervention/wait list/placebo/no stress‐reduction intervention (SMD), Outcome 3: Any symptoms of stress‐related outcome (follow‐up >12 months)
1.4 Psychological symptoms (Follow‐up to and including 3 months after the end of the intervention)
Eight studies showed no differences in psychological symptoms after interventions focusing on the experience of stress more than after no intervention/wait list up to and including three months after the intervention (SMD ‐0.27, 95% CI‐0.58 to 0.03; 742 participants; Analysis 1.4).
1.4. Analysis.

Comparison 1: ‘Focus one’s attention on the experience of stress (thoughts, feelings, behaviour)’ vs No intervention/wait list/placebo/no stress‐reduction intervention (SMD), Outcome 4: Psychological symptoms: anxiety and depression (follow‐up up to 3 months after the end of the intervention)
1.5 Psychological symptoms (Follow‐up from > 3 to 12 months after the end of the intervention)
Three studies showed no differences in psychological symptoms in the interventions focusing on the experience of stress compared to no intervention participants on psychological symptoms > 3 to 12 months after the intervention (no pooled effect estimate; 196 participants; Analysis 1.5).
1.5. Analysis.

Comparison 1: ‘Focus one’s attention on the experience of stress (thoughts, feelings, behaviour)’ vs No intervention/wait list/placebo/no stress‐reduction intervention (SMD), Outcome 5: Psychological symptoms: anxiety and depression (follow‐up > 3 to 12 months after the end of the intervention)
2. Focus one's attention away from the experience of stress vs. no intervention/wait list/placebo/no stress‐reduction intervention
2.1. Any symptoms of stress‐related outcome (Follow‐up to and including 3 months after the end of the intervention)
We combined the results of 35 studies. This resulted in a SMD of ‐0.55 (95% CI ‐0.70 to ‐0.40) showing that stress symptoms were reduced with interventions that focus one's attention away from the experience of stress when compared to no intervention/wait list/placebo/no stress‐reduction intervention and when measured up to and including three months after the end of the intervention (2366 participants; low certainty‐evidence; Analysis 2.1). We found considerable heterogeneity (I2 = 68%) and a 95% prediction interval from ‐1.33 to 0.23. When excluding one outlying SMD, I2 reduced to 33%. The funnel plot revealed a lack of studies in the right part of the funnel where the negative studies would be expected, indicating that there could be publication bias (Figure 5).
2.1. Analysis.

Comparison 2: ‘Focus one’s attention away from the experience of stress by means of relaxation, exercise or something else’ vs No intervention/wait list/placebo/no stress‐reduction intervention (SMD), Outcome 1: Any symptoms of stress‐related outcome (follow‐up up to 3 months after the end of the intervention)
5.
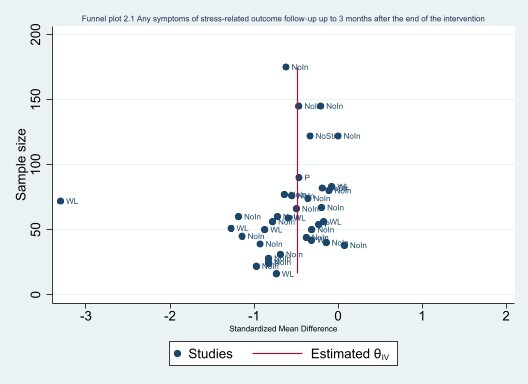
Funnel plot (2.1 Any symptoms of stress‐related outcome (follow‐up up to 3 months after the end of the intervention))
2.2 Any symptoms of stress‐related outcome (Follow‐up from >3 to 12 months after the end of the intervention)
Results from six studies indicated that an intervention focusing away from the experience of stress decreased stress symptoms more than no intervention/wait list (SMD ‐0.41, 95% CI ‐0.79 to ‐0.03; 427 participants; low‐certainty evidence; Analysis 2.2) at > 3 to 12 months follow‐up. We found considerable heterogeneity (I2 = 71%) and a 95% prediction interval from ‐1.71 to 0.89. When excluding one outlying SMD, I2 reduced to 0%. It was not possible to study publication bias with a funnel plot due to the low number of studies included in the analysis.
2.2. Analysis.

Comparison 2: ‘Focus one’s attention away from the experience of stress by means of relaxation, exercise or something else’ vs No intervention/wait list/placebo/no stress‐reduction intervention (SMD), Outcome 2: Any symptoms of stress‐related outcome (follow‐up > 3 to 12 months after the end of the intervention)
2.3 Any symptoms of stress‐related outcome (Follow‐up from > 12 months after the end of the intervention)
No data found for this outcome.
2.4 Psychological symptoms (Follow‐up to and including 3 months after the end of the intervention)
Seven studies found that an intervention focusing away from the experience of stress resulted in an SMD of ‐1.07 (95% CI ‐1.95 to ‐0.19) of psychological symptoms compared to no intervention/wait list/placebo up to and including three months after the end of the intervention (378 participants; Analysis 2.3). No data found for other follow‐up measurements of psychological symptoms.
2.3. Analysis.

Comparison 2: ‘Focus one’s attention away from the experience of stress by means of relaxation, exercise or something else’ vs No intervention/wait list/placebo/no stress‐reduction intervention (SMD), Outcome 3: Psychological symptoms: anxiety and depression (follow‐up up to 3 months after the end of the intervention)
3. Focus on work‐related risk factors on an individual level vs. no intervention/no stress‐reduction intervention
3.1. Any symptoms of stress‐related outcome (Follow‐up to and including 3 months after the end of the intervention)
One study showed that focusing on work‐related risk factors on an individual level decreased stress symptoms more than no intervention up to and including three months after the end of the intervention (SMD ‐1.23; 95% CI ‐2.21 to ‐0.26) while two others showed no difference in stress symptoms (no pooled effect estimate; 87 participants; very low‐certainty evidence; Analysis 3.1). We found considerable heterogeneity (I2 = 70%) and a 95% prediction interval from ‐10.12 to 9.68. It was not possible to study publication bias.
3.1. Analysis.

Comparison 3: ‘Focus on work‐related risk factors on an individual level such as work demands’ vs No intervention/no stress‐reduction intervention (SMD), Outcome 1: Any symptoms of stress‐related outcome (follow‐up up to 3 months after the end of the intervention)
3.2 Any symptoms of stress‐related outcome (Follow‐up from > 3 to 12 months after the end of the intervention)
One study showed that focusing on work‐related risk factors on an individual level decreased stress symptoms more than no intervention >3 to 12 months after the end of the intervention (SMD ‐0.38, 95% CI ‐0.73 to ‐0.03) while one study showed no difference in stress symptoms (SMD 0.09, 95% CI ‐0.78 to 0.95) (no pooled effect estimate; 152 participants; very low‐certainty evidence; Analysis 3.2). With two studies, no funnel plot could be made.
3.2. Analysis.

Comparison 3: ‘Focus on work‐related risk factors on an individual level such as work demands’ vs No intervention/no stress‐reduction intervention (SMD), Outcome 2: Any symptoms of stress‐related outcome (follow‐up > 3 to 12 months after the end of the intervention)
3.3 Any symptoms of stress‐related outcome (Follow‐up > 12 months after the end of the intervention)
One study showed no difference (MD ‐1.52, 95% CI ‐3.61 to 0.57) in stress symptoms of focusing on work‐related risk factors on an individual level > 12 months after the end of the intervention (161 participants; very low‐certainty evidence; Analysis 3.3).
3.3. Analysis.

Comparison 3: ‘Focus on work‐related risk factors on an individual level such as work demands’ vs No intervention/no stress‐reduction intervention (SMD), Outcome 3: Any symptoms of stress‐related outcome (follow‐up >12 months)
3.4 Psychological symptoms (Follow‐up from > 3 to 12 months after the end of the intervention)
One study showed no effect (MD ‐1.07, 95% CI ‐2.90 to 0.76) of focusing on work‐related risk factors on an individual level on psychological symptoms > 3 to 12 months after the end of the intervention (110 participants; Analysis 3.4).
3.4. Analysis.

Comparison 3: ‘Focus on work‐related risk factors on an individual level such as work demands’ vs No intervention/no stress‐reduction intervention (SMD), Outcome 4: Psychological symptoms: anxiety and depression (follow‐up > 3 to 12 months after the end of the intervention)
4. Combination of intervention types vs. No intervention/wait list/no stress‐reduction intervention
4.1. Any symptoms of stress‐related outcome (Follow‐up to and including 3 months after the end of the intervention)
We combined the results of 15 studies and found a SMD of ‐0.67 (95% CI ‐0.95 to ‐0.39) showing less stress symptoms after the combined interventions and no intervention/wait list/no stress‐reduction intervention up to and including three months (1003 participants; low‐certainty evidence; Analysis 4.1). We found considerable heterogeneity (I2 = 77%) and a 95% prediction interval from ‐1.75 to 0.41. When excluding three outlying SMDs, I2 reduced to 46%. The funnel plot revealed a lack of studies in the right part of the funnel where the negative studies would be expected, indicating that there could be publication bias (Figure 6).
4.1. Analysis.

Comparison 4: ‘Combination of interventions’ vs No intervention/wait list/no stress‐reduction intervention (SMD), Outcome 1: Any symptoms of stress‐related outcome (follow‐up up to 3 months after the end of the intervention)
6.
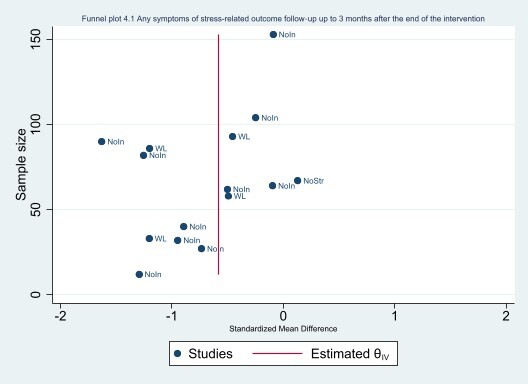
Funnel plot (4.1 Any symptoms of stress‐related outcome (follow‐up up to 3 months after the end of the intervention))
4.2 Any symptoms of stress‐related outcome (Follow‐up from > 3 to 12 months after the end of the intervention)
According to six studies, a combined intervention did not decrease stress symptoms more than no intervention/wait list/no stress‐reduction intervention at > 3 to 12 months follow‐up (SMD ‐0.48, 95% CI ‐0.95 to 0.00; 574 participants; low‐certainty evidence; Analysis 4.2). We found considerable heterogeneity (I2 = 87%) and a 95% prediction interval from ‐1.85 to 1.79. It was not possible to study heterogeneity or publication bias.
4.2. Analysis.

Comparison 4: ‘Combination of interventions’ vs No intervention/wait list/no stress‐reduction intervention (SMD), Outcome 2: Any symptoms of stress‐related outcome (follow‐up > 3 to 12 months after the end of the intervention)
4.3 Any symptoms of stress‐related outcome (Follow‐up > 12 months after the end of the intervention)
One study showed no difference (MD ‐1.80, 95% CI ‐5.74 to 2.14) in stress symptoms of a combined intervention on an individual level > 12 months after the end of the intervention (88 participants; very low‐certainty evidence; Analysis 4.3). It was not possible to study heterogeneity or publication bias.
4.3. Analysis.

Comparison 4: ‘Combination of interventions’ vs No intervention/wait list/no stress‐reduction intervention (SMD), Outcome 3: Any symptoms of stress‐related outcome (follow‐up > 12 months)
4.4 Psychological symptoms (Follow‐up to and including 3 months after the end of the intervention)
Four studies showed no differences in psychological symptoms of a combination of intervention types > 3 to 2 months after the end of the intervention (no pooled effect estimate, 192 participants; Analysis 4.4).
4.4. Analysis.

Comparison 4: ‘Combination of interventions’ vs No intervention/wait list/no stress‐reduction intervention (SMD), Outcome 4: Psychological symptoms: anxiety and depression (follow‐up up to 3 months after the end of the intervention)
4.5 Psychological symptoms (Follow‐up from > 3 to 12 months after the end of the intervention)
One study (MD ‐2.20, 95% CI ‐5.88 to 1.48) showed no differences in psychological symptoms of a combined intervention > 3 to 12 months after the end of the intervention on psychological symptoms (91 participants; Analysis 4.5).
4.5. Analysis.

Comparison 4: ‘Combination of interventions’ vs No intervention/wait list/no stress‐reduction intervention (SMD), Outcome 5: Psychological symptoms: anxiety and depression (follow‐up > 3 to 12 months after the end of the intervention)
4.6 Psychological symptoms (Follow‐up from > 12 months after the end of the intervention)
One study showed no differences (MD ‐2.10, 95% CI ‐5.43 to 1.23) in psychological symptoms of a combined intervention > 12 months after the end of the intervention on psychological symptoms (88 participants; Analysis 4.6).
4.6. Analysis.

Comparison 4: ‘Combination of interventions’ vs No intervention/wait list/no stress‐reduction intervention (SMD), Outcome 6: Psychological symptoms: anxiety and depression (follow‐up > 12 months after the end of the intervention)
5. Focus one's attention on the experience of stress vs. focus one's attention away from the experience of stress
5.1. Any symptoms of stress‐related outcome (Follow‐up to and including 3 months after the end of the intervention)
Three studies showed no differences in stress symptoms of focusing one's attention on the experience of stress versus focusing one's attention away from the experience of stress up to an including three months after the end of the intervention (no pooled effect estimate, 193 participants; Analysis 5.1).
5.1. Analysis.

Comparison 5: Focus one’s attention on the experience of stress vs focus one’s attention away from the experience of stress, Outcome 1: Any symptoms of stress‐related outcome (follow‐up up to 3 months)
5.2 Any symptoms of stress‐related outcome (Follow‐up from > 3 to 12 months after the end of the intervention)
Two studies showed no differences in stress symptoms of focusing one's attention on the experience of stress versus focusing one's attention away from the experience of stress > 3 to 12 months after the end of the intervention (no pooled effect estimate, 74 participants; Analysis 5.2) at > 3 to 12 months follow‐up.
5.2. Analysis.

Comparison 5: Focus one’s attention on the experience of stress vs focus one’s attention away from the experience of stress, Outcome 2: Any symptoms of stress‐related outcome (follow‐up > 3 to 12 months after the end of the intervention)
5.3 Any symptoms of stress‐related outcome (Follow‐up > 12 months after the end of the intervention)
One study showed no differences in stress symptoms of an intervention focusing on the experience of stress compared to focusing away from stress at > 12 months of follow‐up (38 participants; Analysis 5.3).
5.3. Analysis.

Comparison 5: Focus one’s attention on the experience of stress vs focus one’s attention away from the experience of stress, Outcome 3: Psychological symptoms: anxiety and depression (follow‐up up to 3 months)
5.4 Psychological symptoms (Follow‐up to and including 3 months after the end of the intervention)
One study showed no differences in on psychological symptoms of an intervention focusing on the experience of stress compared to focusing away from stress (38 participants; Analysis 5.4).
5.4. Analysis.

Comparison 5: Focus one’s attention on the experience of stress vs focus one’s attention away from the experience of stress, Outcome 4: Psychological symptoms: anxiety and depression (follow‐up > 3 to 12 months after the end of the intervention)
5.5 Psychological symptoms (Follow‐up from > 3 to 12 months after the end of the intervention)
No data found for this outcome.
6. Combination of interventions vs. focus one's attention on the experience of stress
6.1. Any symptoms of stress‐related outcome (Follow‐up to and including 3 months after the end of the intervention)
One study showed no differences in stress symptoms of a combined intervention versus focus one's attention on the experience of stress up to and including three months after the end of the intervention (no effect estimate; 24 participants; Analysis 6.1).
6.1. Analysis.

Comparison 6: ‘Combination of interventions’ vs focus one's attention on the experience of stress (SMD), Outcome 1: Any symptoms of stress‐related outcome (follow‐up up to 3 months)
6.2 Any symptoms of stress‐related outcome (Follow‐up from > 3 to 12 months after the end of the intervention)
One study showed no differences in stress symptoms of a combined intervention versus focus one's attention on the experience of stress > 3 to 12 months after the end of the intervention (no effect estimate; 24 participants; Analysis 6.2).
6.2. Analysis.

Comparison 6: ‘Combination of interventions’ vs focus one's attention on the experience of stress (SMD), Outcome 2: Any symptoms of stress‐related outcome (follow‐up > 3 to 12 months after the end of the intervention)
6.3 Psychological symptoms
No data found for this outcome.
GRADE assessment
1. Focus one's attention on the experience of stress vs. no intervention
The certainty of the evidence for Analysis 1.1 and Analysis 1.2 was downgraded by two levels for very serious risk of bias (bias arising from the randomisation process and lack of blinding; i.e. performance bias) in combination with some inconsistency and suspicion of publication bias. The certainty of the evidence for Analysis 1.3 was downgraded by three levels for very serious risk of bias (bias arising from the randomisation process and lack of blinding; i.e. performance bias) and very serious imprecision (small sample size, the confidence interval includes both a benefit and a harm).
2. Focus one's attention away from the experience of stress vs. no intervention
The certainty of the evidence for Analysis 2.1 and Analysis 2.2 was downgraded by two levels for very serious risk of bias (bias arising from the randomisation process and lack of blinding; i.e. performance bias) in combination with some inconsistency and suspicion of publication bias.
3. Focus on work‐related risk factors on an individual level vs. no intervention
The certainty of the evidence for Analysis 3.1 was downgraded by three levels for very serious risk of bias (bias arising from the randomisation process and lack of blinding; i.e. performance bias), inconsistency and very serious imprecision (small sample size, the confidence interval includes both a benefit and a harm). The certainty of the evidence for Analysis 3.2 and Analysis 3.3 was downgraded by three levels for very serious risk of bias (bias arising from the randomisation process and lack of blinding; i.e. performance bias) and very serious imprecision (small sample size, the confidence interval includes both a benefit and no effect).
4. Combination of intervention types vs. no intervention
The certainty of the evidence for Analysis 4.1 was downgraded by two levels for very serious risk of bias (bias arising from the randomisation process and lack of blinding; i.e. performance bias) in combination with some inconsistency and suspicion of publication bias. The certainty of the evidence for Analysis 4.2 was downgraded by two levels for very serious risk of bias (lack of blinding; i.e. performance bias) and inconsistency. We did not downgrade for imprecision, as the wide confidence interval is due to the inconsistency between study results. The certainty of the evidence for Analysis 4.3 was downgraded by three levels for very serious risk of bias (bias arising from the randomisation process and lack of blinding; i.e. performance bias) and very serious imprecision (small sample size, the confidence interval includes both a benefit and a harm).
Subgroup analysis
We considered duration of the intervention as a characteristic to analyse studies with short duration separately from studies with longer duration. Analysis 1.6 and Analysis 2.4 show an exploratory subgroup analysis based on duration. No differences were seen between these subgroups. Within the subgroups there was still considerable heterogeneity. We have no reason to assume that the duration of the intervention explains heterogeneity between studies, but we're very uncertain about the effect of duration of the intervention on stress symptoms.
1.6. Analysis.

Comparison 1: ‘Focus one’s attention on the experience of stress (thoughts, feelings, behaviour)’ vs No intervention/wait list/placebo/no stress‐reduction intervention (SMD), Outcome 6: Explanatory analysis ‐ subgroup (short vs long duration of intervention): any symptoms of stress‐related outcome (follow‐up up to 3 months after the end of the intervention)
2.4. Analysis.

Comparison 2: ‘Focus one’s attention away from the experience of stress by means of relaxation, exercise or something else’ vs No intervention/wait list/placebo/no stress‐reduction intervention (SMD), Outcome 4: Explanatory analysis ‐ subgroup (short vs long duration of intervention): any symptoms of stress‐related outcome (follow‐up up to 3 months after the end of the intervention)
We considered compliance as a characteristic to analyse studies with poor compliance separately from studies with better compliance. However, we found that compliance was not reported in about 50% of the studies. We decided that subgroup analysis in which half of the studies could not be included would not be of added value and no conclusions can be drawn from such analyses.
Sensitivity analysis
Most studies did not blind participants and therefore the overall certainty in the effect estimates is reduced. In order to provide an indication of the robustness of the overall conclusions we conducted the sensitivity analyses according to protocol for each comparison.
1. Focus one's attention on the experience of stress vs. no intervention
Removing low‐quality studies from the comparison of focusing one's attention on the experience of stress vs. no intervention on the short term left 31 studies. The SMD changed slightly from ‐0.37 (95% CI ‐0.52 to ‐0.23) to ‐0.49 (95% CI ‐0.67 to ‐0.31). For the same comparison for the medium term, removing low‐quality studies left eight studies. The SMD changed slightly from ‐0.43 (95% CI ‐0.71 to ‐0.14) to ‐0.41 (95% CI ‐0.65 to ‐0.17). The overall results and the direction of the effect for this comparison seem not to be affected by methodological quality of the included studies, and we considered the results of the analyses robust. For the same comparison for the long term, removing low‐quality studies left zero studies, so no sensitivity analysis was possible.
2. Focus one's attention away from the experience of stress vs. no intervention
Removing low‐quality studies from the comparison of focusing one's attention away from the experience of stress vs. no intervention on the short term left 24 studies. The SMD changed slightly from ‐0.55 (%95 CI ‐0.70 to ‐0.40) to ‐0.45 (95% CI ‐0.58 to ‐0.33). The overall results and the direction of the effect for this comparison seem not to be affected by methodological quality of the included studies, and we considered the results of the analyses robust. For the same comparison for the medium term, removing low‐quality studies left five studies, so no sensitivity analysis was possible.
3. Focus on work‐related risk factors on an individual level vs. no intervention
Removing low‐quality studies from the comparison of focusing one's attention on individual work‐related risk factors vs. no intervention on the short term left two studies, so no sensitivity analysis was possible. For the same comparison for the medium term, removing low‐quality studies left one study, so no sensitivity analysis was possible. For the same comparison for the long term, removing low‐quality studies left zero studies, so no sensitivity analysis was possible.
4. Combination of intervention types vs. no intervention
Removing low‐quality studies from the comparison of a combination of intervention types vs. no intervention in the short term left 13 studies in the comparison. The SMD changed slightly from ‐0.67 (95% CI ‐0.95 to ‐0.39) to ‐0.74 (95% CI ‐1.06 to ‐0.42). The overall results and the direction of the effect for this comparison seem not to be affected by methodological quality of the included studies, and we considered the results of the analyses robust. For the same comparison in the medium term, four studies were included and in the long term no studies were included precluding any analysis.
Discussion
Summary of main results
The primary objective of this review was to examine the effect of individual‐level stress management interventions on stress symptoms in healthcare workers. This review update includes an additional 89 studies, bringing the total number of studies to 117. Overall, the findings from the synthesis of randomised controlled trials (RCTs) indicate that there may be an effect on stress reduction in healthcare workers from individual‐level stress interventions, whether they focus one's attention on or away from the experience of stress. This effect may last up to a year after the end of the interventions. The evidence on the long‐term effect (more than a year after the end of the intervention) on stress symptoms for these two types of interventions is unclear.
In the short term, less than three months after the end of the intervention, a combination of individual‐level interventions may result in a reduction in stress symptoms. The evidence of effects thereafter or in the long term is inconclusive.
Only seven studies investigated interventions in which the focus is on work‐related risk factors, such as work demands. Due to this lack of evidence, we do not know if this type of intervention is effective.
Overall completeness and applicability of evidence
This systematic review includes the most recent evidence from studies published between 2013 and February 2022, which ensures that our findings are suitable for and applicable to current healthcare settings.
The majority of the included studies were conducted in hospitals (94), the remaining 23 were conducted in other healthcare contexts (14 in mixed or other healthcare settings, five in medical emergency, four in residential care homes for the elderly or disabled). We believe that the results are generalisable to most healthcare situations, but they are most applicable to the hospital setting. Half of the studies (60) included nurses only, 23 physicians and 34 various or other healthcare staff. This is a more diverse population, compared to earlier Cochrane Reviews on the same topic (Ruotsalainen 2015), enhancing the applicability of our findings.
About 64% of the studies were conducted in the Western industrialised world (North America and Europe) and 16% in Asia. The remaining 20% of the studies were spread over the Middle East, South America and Oceania and one study on two continents. Studies conducted in Africa are missing, just as in the former review (Ruotsalainen 2015). The findings are therefore not applicable to the large continent of Africa.
The outcome measurements were diverse, focusing on outcomes such as burnout (such as the Maslach Burnout Inventory (MBI)) or on the experience of stress symptoms (List of Stress symptoms). The lack of clarity on the definition of occupational stress is reflected in this wide range of outcome measurements.
With regard to the interventions, we note that a minority of the included studies focused on the root cause of occupational stress: altering work‐related risk factors. One might expect this type of intervention to yield the most long‐term, sustainable changes, so it is a shortcoming that not more studies took this approach. Almost half (44%) of the studies focused on the experience of stress in itself and 36% on focusing away from stress. A smaller percentage (15%) of the interventions focused on a combination of the above approaches. Furthermore, studies do not really seem to distinguish whether their intervention program is aimed at the prevention of occupational stress or aimed at the treatment of (early) stress symptoms which might also contribute to a lack of clarity on the definition of (occupational) stress.
Quality of the evidence
We assessed the methodological quality of the included RCTs using the Cochrane risk of bias tool (Higgins 2011). We assessed most included studies as having a high risk of bias arising from the randomisation process and lack of blinding; i.e. performance bias and to a lesser extent due to losses to follow‐up. The lack of blinding is problematic as the findings may be explained, at least in part, by a placebo effect. We tried to decrease the heterogeneity of the evidence generated by assessing intervention effects in four categories and with distinct follow‐up times (i.e. up to three months, three to 12 months, and more than one year after the intervention) and on distinct outcomes. We found some inconsistency. Inconsistency could also arise from the categorisation of interventions. The remaining variation within these categories could be due to dissimilar mechanisms of change.
We downgraded the certainty of evidence by two levels for interventions focusing attention on the experience of stress until one‐year follow‐up by two levels for very serious risk of bias (bias arising from the randomisation process and lack of blinding; i.e. performance bias) in combination with some inconsistency and suspicion of publication bias. We downgraded the certainty of evidence by two levels for interventions focusing attention on the experience of stress with three levels for longer follow‐up periods due to very serious risk of bias and very serious imprecision (intervention could be harmful or beneficial).
For interventions focusing attention away from the experience of stress until one‐year follow‐up, we downgraded the certainty of the evidence by two levels due to very serious risk of bias in combination with some inconsistency and suspicion of publication bias.
For interventions focusing on work‐related risk factors on an individual level, we downgraded three levels due to very serious risk of bias, imprecision and inconsistency.
For combined interventions, we downgraded the certainty of the evidence by two levels for the outcome until one‐year follow‐up and by three levels for longer follow‐up periods due to very serious risk of bias, inconsistency, imprecision, or suspicion of publication bias.
Potential biases in the review process
Potential biases could be caused by missing studies with our search strategy and because study authors did not always present the necessary information, sometimes even after we contacted them. However, we assess the effect of these possible biases to be very low because our search strategy was very extensive and the high number of studies we were able to include in the comparisons. Also, we checked relevant references of the included studies. By explicitly operationalising the types of individual targeted interventions that were eligible in each type of intervention and by focusing on stress symptoms only, we reduced bias due to differences in interpretation between the author team. We further substantiated this by adding explicitly that the operationalisation of the types of individual targeted interventions and focus on the effect of stress symptoms only.
We reduced bias due to differences in interpretation between the author team. Bias might have been introduced when multiple stress symptom questionnaires were measured other than the Perceived Stress Scale or the Maslach Burnout Inventory (MBI), and we had to decide which was "the best" to include in the meta‐analysis. Since, not all questionnaires have been validated very well this decision might sometimes be arbitrary and not based on high‐quality evidence (Shoman 2021). However, since all questionnaires have the same underlying construct i.e. measuring stress symptoms, we feel that the effect on the overall conclusion is small. Nonetheless, when more evidence on the psychometric properties of stress symptom questionnaires is available, these decisions might be reconsidered. We have made these decisions transparent by providing all stress symptom questionnaire that have been measured by the authors in the characteristic of included studies and providing with a footnote which stress symptom questionnaires was included in the meta‐analysis.
Potential bias might be introduced by the categorisation of interventions into focusing on stress, focusing away from stress, work‐related, and combination as variation remains within each category. In the previous version of this review, the main categorisation was in person‐ and work‐directed interventions. In this update, we further specified the person‐directed interventions based on the ideas of Bamber 2006. By doing this, we tackled the difficulties encountered with the previous categorisation (Ruotsalainen 2015). Future studies should focus on unravelling underlying stress mechanisms.
Agreements and disagreements with other studies or reviews
Our review aimed to assess the effect of all individual‐level stress interventions for all types of healthcare workers. This approach provided us with the opportunity to group interventions according to a general working mechanism (i.e. interventions that draw one's attention on the experience of stress and interventions in which one's attention is drawn away from the experience of stress or interventions that focus on work‐related risk factors) rather than according to one specific intervention type. As such, we categorised mindfulness‐based interventions into different comparisons, depending on whether yoga and relaxation was the main goal or whether mindfulness was embedded in a more cognitive‐behavioural approach, such as mindfulness‐based stress reduction.
Our review has a different conclusion than a systematic review focusing on hospital nurses (Jung 2021). That review looked at the effect of various mind‐body modalities on mental health and concluded that there was no difference in burnout symptoms between groups that received mindfulness as part of a stress‐reduction programme and those receiving no intervention. But one study comparing yoga to usual care did find a difference in burnout scores. Our review found that there may be an effect for interventions focusing one's attention away from the stress experience (such as yoga) as well as interventions focusing one's attention on the stress experience (mindfulness‐based stress reduction). Our review differs from the Jung 2021 review in that our objective was broader, including all healthcare workers and all stress‐related outcome measures. We reasoned that for individual‐level interventions, the intervention effect for different type of healthcare workers should be comparable. As a result, we were able to include more studies and calculate an effect estimate with more certainty.
The Spinelli 2019 review focused on mindfulness only but also took the approach of looking across healthcare occupations. As a result, they were able to include 38 RCTs. Overall, they found moderate effects on stress outcomes and a small effect on burnout specifically. They reported that the included mindfulness interventions all appeared to significantly affect overall outcomes. This is more in line with our findings, although we did look at non‐mindfulness individual‐level interventions as well. Another review (Zhang 2021) focusing on physical relaxation (such as yoga and massage therapy) in all healthcare workers included 15 RCTs. Their conclusion was that these methods reduce occupational stress compared to no intervention control groups. This is in line with our finding that focusing one's attention away from stress results in stress reduction. Their network analysis revealed yoga as the best method within these types of interventions.
Another Cochrane Review by Kunzler 2020 evaluated the evidence for resilience interventions in healthcare workers. As resilience building and stress reduction interventions often go hand in hand, their findings provide a valuable companion to our review. They concluded based on 17 RCTs that resilience training may lead to lower levels of stress, which was a secondary outcome in their review. Resilience training most often was based on mindfulness and cognitive‐behavioural therapy and was comparable to our category of interventions that draw one's attention to the experience of stress. However, their conclusion was based on very low‐certainty evidence, which is a problem of more reviews on healthcare workers on this topic, such as Clough 2017, while we graded the certainty of the evidence as low.
Our review focuses on healthcare workers, however it is relevant to compare our findings to other reviews examining different occupations. In the Richardson 2008 review of 55 interventions as tested in 36 experimental studies, a significant medium to large effect on occupational stress was found, and the effect was significantly and consistently larger for cognitive behavioural interventions. In contrast, in our review we found that there may be an effect for cognitive behavioural interventions as for relaxation techniques. This might be explained by the occupation of healthcare workers, we focused on, and the type of stressors these employees face. Healthcare workers often have to deal with inevitable situations like death of a patient or telling patients about their permanent loss of quality of life. In these stressful situations that cannot be influenced (any more), the active coping and practice of functional responses which is at the heart of cognitive behavioural approaches, might not be the most suitable way of coping. A more passive way of coping such as relaxation or mediation (refocus, away from the stress) might be a better fit to these types of stressors and this might explain why we did not find a bigger effect of the cognitive behavioural approaches compared to the relaxation techniques.
Authors' conclusions
Implications for practice.
Our review shows that there may be an effect on stress in healthcare workers from individual‐level stress interventions, whether they focus one's attention on or away from the experience of stress. This effect may last up to a year after the end of the intervention. A combination of interventions might be beneficial as well, at least in the short term. The long‐term effects, longer than a year after the intervention ended, of individual‐level stress interventions remain unknown. The same applies for interventions focussed on modifying work‐related risk factors.
The estimates of the effects of individual‐level stress interventions may be biased because of a lack of blinding of the participants in the studies. The true effect of interventions in which one's attention is directed on or away from the experience of stress is likely to be close to the estimate of the effect, but there is a possibility that the effect is substantially different (e.g. due to placebo effect). The effect could be potentially smaller than our synthesis of the available evidence indicated. Our confidence in the effect of combinations of interventions is limited, and the true effect may be substantially different from the estimate of the effect. We have very little confidence in the effect of individual‐level interventions in which the focus is on work‐related risk factors. Based on the included studies we cannot indicate whether or not there is any effect, even though this approach is often considered to be the most impactful and sustainable way to eliminate stress in the workplace. These interventions tend to be complex because they require changes in how the work is organised, designed and managed, which is often beyond the scope of the individual employee (Nielsen 2010). Also, difficulties in adequately measuring the effects might explain why this kind of intervention does not live up to the expectations researchers have of them based on theories.
Country‐specific policies and legislation can influence what types of interventions are implemented. In most countries, there is some legislation on health and safety at work, but the extent and quality varies between countries according to a report by the World Health Organization (Burton 2010). The minimum variant is protecting workers from injuries or illness, but more refined legislation is in place in many countries requiring aspects such as a risk assessment, and the implementation and monitoring of measures. However, examining whether such legislation is effective is beyond the scope of our review.
Implications for research.
The findings of this review show the need for methodologically better designed and executed studies. Trials of this type are required as nearly all included studies suffered from lack of blinding of participants and personnel. We acknowledge the difficulty of blinding in stress reduction interventions. Nevertheless, in 14 studies attempts were made to blind participants to group assignment, thus showing that blinding is not impossible. Better design and execution of studies also include providing details on the randomisation process and study protocol or trial registration.
Furthermore, there is a need for more studies on interventions in which the focus is on work‐related risk factors both at the individual and organisational level. With more participants the optimal information size can be reached and conclusions can be drawn.
We believe it would be helpful to investigate and identify unpublished data (potentially showing no effect or a harmful effect) of individual‐level stress management interventions. Large studies on this topic might also help resolve this small‐study issue.
The long‐term effects of individual‐level stress management interventions are unknown due to the total absence of studies or paucity of data. Studies following the participants for more than a year after the intervention has ended are needed to be able to draw conclusions about the long‐term benefits, if any, on stress reduction of interventions aimed at reducing stress in healthcare workers.
Designing interventions to reduce stress amongst high‐risk populations should be preferably based on working mechanisms or underlying biological or behavioural change models.
We found a preliminary indication for a higher standardised mean difference (SMD) when using a wait list control group compared to a non‐intervention control group, which has been corroborated by previous research (Faltinsen 2022). Further research is needed to determine how each control arm could affect the SMD.
When studying the effect of an intervention focusing on the experience of stress compared to no intervention, wait list control group, placebo, or no stress‐reduction intervention, we recommend future research to have at least 116 participants per study arm at follow‐up. This calculation is based on the SMD of analysis 1.1 (α 0.05, power 80%, difference between two independent means) (Faul 2017). When studying the effect of an intervention focusing away from the experience of stress compared to no intervention, wait list control group, placebo, or no stress‐reduction intervention, we recommend future research to have at least 53 participants per study arm at follow‐up. Again, this calculation is based on the SMD of analysis 1.2 (α 0.05, power 80%, difference between two independent means) (Faul 2017).
What's new
| Date | Event | Description |
|---|---|---|
| 22 May 2023 | Amended | Updated acknowledgements to include specifics on NIHR Incentive Award. |
History
Protocol first published: Issue 2, 2000 Review first published: Issue 4, 2006
| Date | Event | Description |
|---|---|---|
| 12 May 2023 | New search has been performed | This review has been updated to include the results of a new search on February 2022. The previous review (Ruotsalainen 2015) has been split into this review on individual‐level interventions and a review on organization‐level interventions (Giga 2018). We used a replacement approach and used the previous review (Ruotsalainen 2015) as one source of studies. |
| 12 May 2023 | New citation required and conclusions have changed | In this update, we added 89 studies on top of the 28 related titles identified from the studies in the previous review making 117 total included studies. For this update, we categorized stress‐interventions and outcomes in another way, resulting in new GRADE assessments that are not one‐to‐one comparable to the previous version |
Notes
2023 update: this review update was split from the original title (Ruotsalainen 2015) and now only included individual‐level interventions and added a further 89 studies including 11,119 participants. We implemented several improvements and described these in the section "Differences between protocol and review". For example, we excluded stressors as an outcome.
Acknowledgements
This study/project was funded by the National Institute for Health Research (NIHR) Evidence Synthesis Programme (NIHR150837) Incentive Award Scheme 2021. The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
We are grateful for the funding provided for this project by the National Institute for Health Research (NIHR), UK. The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care, UK.
We thank Jos Verbeek, Albert Mariné, and Mariné A, Serra C for their work on the previous version of this review. We thank Vittoria Lutje for updating the searches and running the updated searches.
We thank J Cohen‐Katz, S Ketelaar/K Nieuwenhuijsen, K Moody, D Oman, P Dunne, J Kline, M Barattucci, T Pehlivan, M Sampson 2019, E Smoktunowicz, C West, A Sawyer, A Errazuriz, Jensen, B Yüceer for providing further information or data from their study.
We thank our colleagues from Amsterdam UMC location Vrije Universiteit Amsterdam and University of Amsterdam, Public and Occupational health, Michiel Greidanus, Sanne Gommers, Donna Beerda, Donny Kreuger, Elmi Zwaan, Fenna van Ommen, Marije Hagendijk, and Judith Mollet for their help with extracting the outcomes as second data extractor.
We thank the following students of the faculty of Medicine of the University of Amsterdam for their help with extracting the outcomes as second data extractor: Anniek Nauta, Boris Brojović, Bram Millenaar, Charlie Sent, Chiel Klein, Danny Kroon, Frederique Wekker, Guus Kerkvliet, Ida Blokland, Jens Nijzink, Jesse Warmerdam, Loran Mul, Lotte Bos Mertcan Göç, Mirte Dekkers, Nina Bijl, Nisrine Aynaou, Sabine de Beer, Sam Rozemuller.
We thank the peer reviewers for their comments: Giuseppe La Torre, Department of Public Health and Infectious Diseases ‐ Sapienza University of Rome; Amit Abraham, Weill Cornell Medicine‐Qatar; and Afroditi Kanellopoulou, Statistician, Cochrane Central.
We thank the Cochrane Work Review Group for supporting the authors in the development of this review.
The following people conducted the editorial process for this article:
Sign‐off Editor (final editorial decision): Jan Hoving, Cochrane Work, Amsterdam UMC
Contact Editor: Jos Verbeek, Cochrane Work, Amsterdam UMC
Managing Editor (selected peer reviewers, collated peer‐reviewer comments, provided editorial guidance to authors, edited the article): Jessica Thomas, Cochrane Work, Amsterdam UMC
Information Specialist (searching support): Faridi van Etten, Amsterdam UMC
Methods and Statistician review: Afriditi Kanellopoulou, Statistician at Cochrane Central
Copy‐editing (initial copy‐edit and final proofread): Heather Maxwell, Copy‐edit Group at Cochrane Central
Appendices
Appendix 1. Search strategy
Ovid MEDLINE(R) and Epub Ahead of Print, In‐Process, In‐Data‐Review & Other Non‐Indexed Citations, Daily and Versions(R) <1946 to February 09, 2022>
1 exp Health Personnel/ or "health personnel".mp. or "health care personnel".mp. or "healthcare personnel".mp. or "health care worker*".mp. or "healthcare worker*".mp. or "health worker*".mp. or "health professional*".mp. or "health care professional*".mp. or "healthcare professional*".mp. or "medical care personnel".mp. or nurse?.mp. or physician?.mp. or anesthetist?.mp. or audiologist?.mp. or "dental staff".mp. or "dental personnel".mp. or dentist?.mp. or "medical staff".mp. or "nursing staff".mp. or "nursing personnel".mp. or nutritionist?.mp. or dietitian?.mp. or therapist?.mp. or pharmacist?.mp. or veterinarian?.mp. or "medical personnel".mp. or physiotherapist?.mp. 1469819
2 (care professional? or healthcare professional? or elderly care or nurse? or healthcare worker? or care worker? or physician? or doctor?).mp. 1085871
3 (hospital? or healthcare organi?ation or icu or picu or nursing homes or eol facilit* or "end of life facilit*").ab,kf,ti. 1349587
4 1 or 2 or 3 2647944
5 exp Stress, Psychological/ or "occupational stress".mp. or "occupational strain".mp. or "occupational burden".mp. or "work stress".mp. or "work strain?".mp. or "work burden?".mp. or "work‐related stress".mp. or "work‐related strain?".mp. or "work‐related burden?".mp. or "psychological load?".mp. 147646
6 ((health surveillance adj2 (employee? or worker?)) or (interview* adj5 (employee? or worker?))).ab,kf,ti. 3743
7 (prevent* adj2 (harm* or work or stress)).ab,kf,ti. 10691
8 (((job or work or occupation*) adj2 stress) or compassion fatigue or burnout or burn out or ((strain? or demand*) adj2 (work or job or profession?))).ab,kf,ti. 31680
9 (work abil* or work participa* or work functioning or "functioning at work").ab,kf,ti. 3326
10 ((mental or psych*) adj2 (stress or emotion*)).mp. 149113
11 (anxiety or depression or ((heart or coronary or cardio*) adj2 (disease? or disorder?))).mp. 1328494
12 (autonom* or bullying or bullied or cyberbullying).ab,hw,kf,ti. 202566
13 (decision latitude or decision authority or skill discretion or social support or effort reward).ab,kf,ti. 48057
14 organi?ational justice.ab,kf,ti. 388
15 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 1679887
16 4 and 15 246563
17 exp workplace/ or work*.mp. or job?.mp. or employee*.mp. or occupation*.mp. 2143173
18 (paid work or worker? or vocational or occupation* or presenteeism or employment or employee? or job? or work place or work related or work disabil* or work product* or work limit* or work instabili* or work performance or work capacit or work evaluat* or work direct* or working populat* or workplace).ab,kf,ti. 509144
19 17 or 18 2180713
20 16 and 19 56322
21 exp patients/ or patient*.mp. 7827241
22 20 not 21 28613
23 (randomized controlled trial or controlled clinical trial).pt. 648159
24 (randomized or placebo or randomly or trial or groups).ab. 3176534
25 23 or 24 3322226
26 exp animals/ not humans.sh. 4956807
27 25 not 26 2843767
28 22 and 27 4665
Scopus
( ( ( ( ( TITLE‐ABS‐KEY ( ( "health personnel" OR "health care personnel" OR "healthcare personnel" OR "health care worker*" OR "healthcare worker*" OR "health worker*" OR "health professional*" OR "health care professional*" OR "healthcare professional*" OR "medical care personnel" OR nurse? OR physician? OR anesthetist? OR audiologist? OR "dental staff" OR "dental personnel" OR dentist? OR "medical staff" OR "nursing staff" OR "nursing personnel" OR nutritionist? OR dietitian? OR therapist? OR pharmacist? OR veterinarian? OR "medical personnel" OR physiotherapist? ) ) ) OR ( TITLE‐ABS‐KEY ( ( care AND professional? OR healthcare AND professional? OR elderly AND care OR nurse? OR healthcare AND worker? OR care AND worker? OR physician? OR doctor? ) ) ) OR ( TITLE‐ABS‐KEY ( ( hospital? OR healthcare AND organi?ation OR icu OR picu OR nursing AND homes OR eol AND facilit* OR "end of life facilit*" ) ) ) ) AND ( ( TITLE‐ABS‐KEY ( ( stress OR "occupational stress" OR "occupational strain" OR "occupational burden" OR "work stress" OR "work strain?" OR "work burden?" OR "work‐related stress" OR "work‐related strain?" OR "work‐related burden?" OR "psychological load?" ) ) ) OR ( ( TITLE‐ABS‐KEY ( ( health AND surveillance ) AND ( employee? OR worker? ) OR interview* AND ( employee? OR worker? ) ) ) OR ( TITLE‐ABS‐KEY ( ( job OR work OR occupation* ) AND ( stress OR compassion AND fatigue OR burnout ) ) ) OR ( TITLE‐ABS‐KEY ( ( work AND abil* OR work AND participa* OR work AND functioning OR "functioning at work" ) ) ) OR ( TITLE‐ABS‐KEY ( ( autonom* OR bullying OR bullied OR cyberbullying ) ) ) OR ( TITLE‐ABS‐KEY ( ( bullying OR bullied OR cyberbullying ) ) ) OR ( TITLE‐ABS‐KEY ( ( decision AND latitude OR decision AND authority OR skill AND discretion OR effort AND reward OR organizational AND justice ) ) ) ) ) ) AND ( ( TITLE‐ABS‐KEY ( randomized AND controlled AND trial ) ) OR ( TITLE‐ABS‐KEY ( controlled AND clinical AND trial OR random* OR double‐blind OR single‐blind OR ( ( singl* OR doubl* OR trebl* OR tripl* ) AND ( mask* OR blind* ) ) ) ) ) ) AND NOT ( TITLE‐ABS‐KEY ( ( animal AND NOT human ) ) ) ) AND ( TITLE‐ABS‐KEY ( ( work* OR job* OR employee* OR occupation* ) ) )
1,619 results
Cinahl
Select / deselect all
| Search ID# | Search Terms | Actions | |
| S9 | s7 NOT s8 | View Results (1,521) View Details Edit |
|
| S8 | TI patient* | View Results (727,918) View Details Edit |
|
| S7 | S3 AND S6 | View Results (1,742) View Details Edit |
|
| S6 | AB ("randomized controlled trial*" OR "controlled clinical trial*" OR "controlled trial*" OR random* OR double‐blind OR "double blind") OR TI ("randomized controlled trial*" OR "controlled clinical trial*" OR "controlled trial*" OR random* OR double‐blind OR "double blind") | View Results (416,931) View Details Edit |
|
| S5 | S3 AND S4 | View Results (7,386) View Details Edit |
|
| S4 | TX "randomized controlled trial*" OR "controlled clinical trial*" OR "controlled trial*" OR random* OR double‐blind OR "double blind" OR single‐blind OR "single blind" OR "clinical trial*" OR ( ( singl* OR doubl* OR trebl* OR tripl* ) AND (mask* OR blind* ) ) | View Results (1,760,234) View Details Edit |
|
| S3 | S1 AND S2 | View Results (22,854) View Details Edit |
|
| S2 | AB "health care personnel" OR "healthcare personnel" OR "health care worker*" OR "healthcare worker*" OR "health worker*" OR "health professional*" OR "health care professional*" OR "healthcare professional*" OR "medical care personnel" OR nurse? OR physician? OR anesthetist? OR audiologist? OR "dental staff" OR "dental personnel" OR dentist? OR "medical staff" OR "nursing staff" OR "nursing personnel" OR nutritionist? OR dietitian? OR therapist? OR pharmacist? OR veterinarian? OR "medical perso ... | View Results (1,026,684) View Details Edit |
|
| S1 | AB stress OR "occupational stress" OR "occupational strain" OR "occupational burden" OR "work stress" OR "work strain?" OR "work burden?" OR "work‐related stress" OR "work‐related strain?" OR "work‐related burden?" OR "psychological load?" | View Results (146,198) View Details Edit |
PsycInfo
| Search ID# | Search Terms | Actions | |
| S9 | s7 NOT s8 | View Results (1,259) View Details Edit |
|
| S8 | TI patient* | View Results (183,016) View Details Edit |
|
| S7 | S3 AND S6 | View Results (1,377) View Details Edit |
|
| S6 | AB ("randomized controlled trial*" OR "controlled clinical trial*" OR "controlled trial*" OR random* OR double‐blind OR "double blind") OR TI ("randomized controlled trial*" OR "controlled clinical trial*" OR "controlled trial*" OR random* OR double‐blind OR "double blind") | View Results (235,145) View Details Edit |
|
| S5 | S3 AND S4 | View Results (1,515) View Details Edit |
|
| S4 | TX "randomized controlled trial*" OR "controlled clinical trial*" OR "controlled trial*" OR random* OR double‐blind OR "double blind" OR single‐blind OR "single blind" OR "clinical trial*" OR ( ( singl* OR doubl* OR trebl* OR tripl* ) AND (mask* OR blind* ) ) | View Results (287,667) View Details Edit |
|
| S3 | S1 AND S2 | View Results (20,128) View Details Edit |
|
| S2 | AB "health care personnel" OR "healthcare personnel" OR "health care worker*" OR "healthcare worker*" OR "health worker*" OR "health professional*" OR "health care professional*" OR "healthcare professional*" OR "medical care personnel" OR nurse? OR physician? OR anesthetist? OR audiologist? OR "dental staff" OR "dental personnel" OR dentist? OR "medical staff" OR "nursing staff" OR "nursing personnel" OR nutritionist? OR dietitian? OR therapist? OR pharmacist? OR veterinarian? OR "medical perso ... | View Results (323,949) View Details Edit |
|
| S1 | AB stress OR "occupational stress" OR "occupational strain" OR "occupational burden" OR "work stress" OR "work strain?" OR "work burden?" OR "work‐related stress" OR "work‐related strain?" OR "work‐related burden?" OR "psychological load?" | View Results (238,644) View Details Edit |
Cochrane Central Register of Controlled Trials
Issue 2 of 12, February 2022
#276 (health personnel or "health care personnel" or "healthcare personnel" or "health care worker*" or "healthcare worker*" or "health worker*" or "health professional*" or "health care professional*" or "healthcare professional*" or "medical care personnel" or nurse? or physician? or anesthetist? or audiologist? or "dental staff" or "dental personnel" or dentist? or "medical staff" or "nursing staff" or "nursing personnel" or nutritionist? or dietitian? or therapist? or pharmacist? or veterinarian? or "medical personnel" or physiotherapist?):ti,ab,kw 106189
#277 care worker* or nurse* or physician* 87712
#278 #276 or #277 119949
#279 (stress or "occupational stress" or "occupational strain" or "occupational burden" or "work stress" or "work strain?" or "work burden?" or "work‐related stress" or "work‐related strain?" or "work‐related burden?" or "psychological load?"):ti,ab,kw 65145
#280 ((job or work or occupation*) AND (stress or compassion fatigue or burnout )):ti,ab,kw 5695
#281 ((work abil* or work participa* or work functioning or "functioning at work")):ti,ab,kw 21757
#282 (bullying or bullied or cyberbullying):ti,ab,kw 463
#283 ((decision latitude or decision authority or skill discretion or social support or effort reward)):ti,ab,kw 16728
#284 (organizational justice):ti,ab,kw 37
#285 #279 or #280 or #281 or #282 or #283 or #284 97280
#286 #278 and #285 14233
#287 (work* or job? or employee* or occupation*):ti,ab,kw 99224
#288 #286 and #287 8424
#289 (patient*):ti 388757
#290 #288 not #289 7248 limit to Pubmed, Embase and Cinahl results = 4571
ClinicalTrial.gov
CONDITION| stress or occupational stress or occupational strain or occupational burden or work stress or work strain or work burden or work‐related stress or work‐related strain or work‐related burden or psychological load AND OTHER TERMS| health personnel or health care personnel or health care worker or healthcare worker or health worker or health professional or health care professional or healthcare professional or medical care personnel or nurse or physician or medical staff or nursing staff or nursing personnel or medical personnel
World Health Organization International Clinical Trials Registry Platform
Basic search: stress AND healthcare OR stress AND health worker OR stress AND nursing personnel OR stress AND medical personnel
Data and analyses
Comparison 1. ‘Focus one’s attention on the experience of stress (thoughts, feelings, behaviour)’ vs No intervention/wait list/placebo/no stress‐reduction intervention (SMD).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Any symptoms of stress‐related outcome (follow‐up up to 3 months after the end of the intervention) | 41 | 3645 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐0.52, ‐0.23] |
| 1.1.1 No intervention | 29 | 2434 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐0.53, ‐0.16] |
| 1.1.2 Wait list | 9 | 619 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.52 [‐0.80, ‐0.25] |
| 1.1.3 Placebo | 1 | 436 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.21, 0.16] |
| 1.1.4 No stress‐reduction intervention | 2 | 156 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.33 [‐1.19, 0.53] |
| 1.2 Any symptoms of stress‐related outcome (follow‐up > 3 to 12 months after the end of the intervention) | 19 | 1851 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.43 [‐0.71, ‐0.14] |
| 1.2.1 No intervention | 11 | 1271 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.46 [‐0.90, ‐0.02] |
| 1.2.2 Wait list | 6 | 480 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.53 [‐0.83, ‐0.24] |
| 1.2.3 No stress reduction intervention | 2 | 100 | Std. Mean Difference (IV, Random, 95% CI) | 0.16 [‐0.23, 0.56] |
| 1.3 Any symptoms of stress‐related outcome (follow‐up >12 months) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.4 Psychological symptoms: anxiety and depression (follow‐up up to 3 months after the end of the intervention) | 8 | 742 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.27 [‐0.58, 0.03] |
| 1.4.1 No intervention | 7 | 482 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.28 [‐0.68, 0.11] |
| 1.4.2 Wait list | 1 | 260 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.28 [‐0.53, ‐0.04] |
| 1.5 Psychological symptoms: anxiety and depression (follow‐up > 3 to 12 months after the end of the intervention) | 3 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.5.1 No intervention | 3 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.6 Explanatory analysis ‐ subgroup (short vs long duration of intervention): any symptoms of stress‐related outcome (follow‐up up to 3 months after the end of the intervention) | 41 | 3645 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐0.52, ‐0.23] |
| 1.6.1 Short (< 12weeks) | 29 | 2647 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.32 [‐0.49, ‐0.15] |
| 1.6.2 Long (≥ 12 weeks) | 12 | 998 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐0.78, ‐0.22] |
Comparison 2. ‘Focus one’s attention away from the experience of stress by means of relaxation, exercise or something else’ vs No intervention/wait list/placebo/no stress‐reduction intervention (SMD).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Any symptoms of stress‐related outcome (follow‐up up to 3 months after the end of the intervention) | 35 | 2366 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.55 [‐0.70, ‐0.40] |
| 2.1.1 No intervention | 22 | 1565 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.48 [‐0.61, ‐0.35] |
| 2.1.2 Wait list | 8 | 429 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.88 [‐1.53, ‐0.24] |
| 2.1.3 Placebo | 3 | 168 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.43 [‐0.74, ‐0.12] |
| 2.1.4 No stress‐reduction intervention | 2 | 204 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.27 [‐0.55, 0.00] |
| 2.2 Any symptoms of stress‐related outcome (follow‐up > 3 to 12 months after the end of the intervention) | 6 | 427 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.79, ‐0.03] |
| 2.2.1 No intervention | 4 | 312 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.43 [‐0.98, 0.12] |
| 2.2.2 Wait list | 2 | 115 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐0.77, ‐0.03] |
| 2.3 Psychological symptoms: anxiety and depression (follow‐up up to 3 months after the end of the intervention) | 7 | 378 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.07 [‐1.95, ‐0.19] |
| 2.3.1 No intervention | 2 | 127 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.67 [‐1.60, 0.25] |
| 2.3.2 Wait list | 3 | 173 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.89 [‐4.24, 0.46] |
| 2.3.3 Placebo | 2 | 78 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐0.79, 0.11] |
| 2.4 Explanatory analysis ‐ subgroup (short vs long duration of intervention): any symptoms of stress‐related outcome (follow‐up up to 3 months after the end of the intervention) | 35 | 2366 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.55 [‐0.70, ‐0.40] |
| 2.4.1 Short (<12 weeks) | 33 | 2255 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.52 [‐0.68, ‐0.37] |
| 2.4.2 Long (≥ 12 weeks) | 2 | 111 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.96 [‐1.48, ‐0.43] |
Comparison 3. ‘Focus on work‐related risk factors on an individual level such as work demands’ vs No intervention/no stress‐reduction intervention (SMD).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Any symptoms of stress‐related outcome (follow‐up up to 3 months after the end of the intervention) | 3 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1.1 No intervention | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1.2 No stress‐reduction intervention | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.2 Any symptoms of stress‐related outcome (follow‐up > 3 to 12 months after the end of the intervention) | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.3 Any symptoms of stress‐related outcome (follow‐up >12 months) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.4 Psychological symptoms: anxiety and depression (follow‐up > 3 to 12 months after the end of the intervention) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Comparison 4. ‘Combination of interventions’ vs No intervention/wait list/no stress‐reduction intervention (SMD).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Any symptoms of stress‐related outcome (follow‐up up to 3 months after the end of the intervention) | 15 | 1003 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.67 [‐0.95, ‐0.39] |
| 4.1.1 No intervention | 10 | 666 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.71 [‐1.08, ‐0.34] |
| 4.1.2 Wait list | 4 | 270 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.79 [‐1.21, ‐0.38] |
| 4.1.3 No stress‐reduction intervention | 1 | 67 | Std. Mean Difference (IV, Random, 95% CI) | 0.13 [‐0.35, 0.61] |
| 4.2 Any symptoms of stress‐related outcome (follow‐up > 3 to 12 months after the end of the intervention) | 6 | 574 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.48 [‐0.95, ‐0.00] |
| 4.2.1 No intervention | 3 | 330 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.70 [‐1.52, 0.12] |
| 4.2.2 Wait list | 2 | 177 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.36 [‐0.65, ‐0.06] |
| 4.2.3 No stress‐reduction intervention | 1 | 67 | Std. Mean Difference (IV, Random, 95% CI) | 0.00 [‐0.48, 0.48] |
| 4.3 Any symptoms of stress‐related outcome (follow‐up > 12 months) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.4 Psychological symptoms: anxiety and depression (follow‐up up to 3 months after the end of the intervention) | 4 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.4.1 No intervention | 3 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.4.2 Wait list | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.5 Psychological symptoms: anxiety and depression (follow‐up > 3 to 12 months after the end of the intervention) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.6 Psychological symptoms: anxiety and depression (follow‐up > 12 months after the end of the intervention) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Comparison 5. Focus one’s attention on the experience of stress vs focus one’s attention away from the experience of stress.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 Any symptoms of stress‐related outcome (follow‐up up to 3 months) | 3 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.2 Any symptoms of stress‐related outcome (follow‐up > 3 to 12 months after the end of the intervention) | 2 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.3 Psychological symptoms: anxiety and depression (follow‐up up to 3 months) | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.4 Psychological symptoms: anxiety and depression (follow‐up > 3 to 12 months after the end of the intervention) | 1 | 38 | Std. Mean Difference (IV, Random, 95% CI) | 0.24 [‐0.39, 0.88] |
Comparison 6. ‘Combination of interventions’ vs focus one's attention on the experience of stress (SMD).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 6.1 Any symptoms of stress‐related outcome (follow‐up up to 3 months) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.2 Any symptoms of stress‐related outcome (follow‐up > 3 to 12 months after the end of the intervention) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Alexander 2015.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Yoga
Control (No intervention)
Overall
Included criteria: no prior experience with yoga, willingness to complete eight weekly sessions and homework exercises, and willingness to be randomly assigned to the research or control group. Excluded criteria: serious illness or major orthopaedic diagnoses of the neck, back, pelvis, or lower extremities that could interfere with completion of the yoga intervention protocol. Pretreatment: NR Compliance rate: NR Response rate: NR Type of healthcare worker: exclusively nurses |
|
| Interventions |
Intervention characteristics Yoga
Control (no intervention)
|
|
| Outcomes | MBI
Health Promoting Lifestyle Profile II (HPLP II)
|
|
| Identification |
Sponsorship source: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by the Research and Creative Activities Fund of Texas Christian University. Country: USA Setting: Hospital Comments: NR Authors name: Gina K. Alexander Institution: Texas Christian University, Harris College of Nursing and Health Sciences Email: g.alexander@tcu.edu Address: TCU Box 298620, Fort Worth, TX 76129, USA Time period: NR |
|
| Notes | MBI‐EE included in analysis 2.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Questionnaire, and core study questionnaires. After individuals completed consent forms and baseline assessments, they were enroled in the study and randomized to the intervention (yoga) or usual care control group. A total of 54 individuals Sequence generation process not mentioned |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to understand whether intervention allocations could have been foreseen in advance of, during, enrolment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not reported. |
| Selective reporting (reporting bias) | Unclear risk | No trial registration or study protocol reported in the study and we did not find one online. No indication of selective reporting. |
| Other bias | Unclear risk | Compliance rate and response rate not reported. |
Amutio 2015.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Mindfulness training
Control (wait list)
Overall
Included criteria: willingness to complete the questionnaires and commitment to adhere to the programmes' attendance and dedication requirements. Excluded criteria: were being in psychiatric or psychological treatment, or not being actively practising at the time of the study. Pretreatment: no initial differences between groups were found for the main variables of our study (mindfulness, F = 2.51, P = 0.12; burnout, F = 1.11, P = 0.30; and emotional exhaustion, F = 2.87, P = 0.10), including demographic or professional characteristics (P > 0.05) Type of healthcare worker: exclusively physicians Response rate: NR Compliance rate: regarding acceptability of the intervention to participants, the attendance rates for the two phases of the program were 88% for weekly sessions and 72% for monthly sessions |
|
| Interventions |
Intervention characteristics Mindfulness training
Control (wait list)
|
|
| Outcomes |
Maslach Burnout Inventory ‐ Emotional Exhaustion
Maslach Burnout Inventory ‐ Depersonalisation
Maslach Burnout Inventory ‐ Personal accomplishment (lack of)
|
|
| Identification |
Sponsorship source: The authors report the University of the Basque Country (UPV/EHU)provided funding for the materials and travel expenses. The Official Medical College of Biscay in Spain provided the physical setting to conduct the sessions. Country: Spain Setting: all participants were actively used in public (42.9%) or private (52.4%) practice. Comments: NR Authors name: Alberto Amutio, PhD; Institution: Department of Social Psychology and Methodology of the BehavioralSciences, Faculty of Psychology, University of the Basque Country (UPV/EHU), Spain Email: Alberto.amutio@ehu.eus Address: Avda Tolosa, 70, Donostia‐San Sebastian, Gipuzko Time period: NR |
|
| Notes | MBI‐EE included in analysis 1.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants in the experimental group (n = 21) were randomly selected using the statistical program SPSS 20.0. The remaining subjects were included in the control group (n = 21)." |
| Allocation concealment (selection bias) | Unclear risk | Judgement Comment: Unable to judge whether participants and/or investigators could possibly foresee assignment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "Each participant in the experimental group committed to attending the sessions, doing the exercises assigned as home‐work, and answering the evaluation questions at the end of each of the phases of the study. The waitlist control group was told that a similar course would be offered again." Judgement Comment: Participants not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | not explicitly stated whether participants dropped out. |
| Selective reporting (reporting bias) | Unclear risk | No trial registration or no study protocol reported, nor did we find one online. |
| Other bias | Low risk | No indication of other sources of bias |
Aranda Ausern 2016.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Control (no intervention)
Mindfulness and self‐compassion program
Overall
Included criteria: informed consent, committing to completing the pre‐ and post‐intervention questionnaires, attending at least 75% of the sessions and practising mindfulness and self‐compassion for 45 minutes a day. Excluded criteria: having completed a mindfulness and/or compassion program in the previous 6 months; having a psychiatric illness that did not make participation in the study advisable. Pretreatment: they were not significant in any of the characteristics considered. Type of healthcare worker: various healthcare staff but 46.7% nurses and physicians 53.3% Response rate: NR Compliance rate: Intervention group 92% and control group 92% |
|
| Interventions |
Intervention characteristics Control (no intervention)
Mindfulness and self‐compassion program
|
|
| Outcomes |
Perceived Stress Questionnaire (PSQ)
|
|
| Identification |
Sponsorship source: This work has been partially financed by the Department of Health of the Government of Navarra, by obtaining the first prize in the II Contest of Ideas for Health Research in Primary Care. Country: Spain Setting: NR Comments: NR Authors name: Aranda Auserón Institution: Subdirección de Farmacia, Servicio Navarro de Salud‐Osasunbidea (SNS‐O), Pamplona, Spain Email: garandaa@navarra.es Address: NR |
|
| Notes | PSS included in analysis 2.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomization of the groups was carried out by assigning correlative numbers to the 48 participants and selecting a total of 25 from a balloon with 48 numbered balls; these numbers were part of the intervention group, with the rest remaining in the control group. |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to understand whether intervention allocations could have been foreseen in advance of, during, enrolment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants not blinded whereas outcomes are self‐reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 3 of the 48 (16%) randomised participants were lost to follow‐up, which is below our pre‐defined cut‐off point. |
| Selective reporting (reporting bias) | Unclear risk | No trial protocol or registration mentioned in the study nor did we find one online. |
| Other bias | Unclear risk | Low participation rate in the study (48 of 1281; 3.75%) |
Axisa 2019.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Evaluation of a well‐being workshop
Control (no intervention)
Overall
Included criteria: recruitment was restricted to physician trainees completing their RACP basic physician training in New South Wales (NSW) hospitals. Excluded criteria: NR Pretreatment: differences between groups at 3 and 6 months were assessed using linear regression models, with group as a covariate, and adjusted for the participants’ baseline value of the outcome measure. Compliance rate: not explicitly reported "Lack of control over work rosters, difficulty swapping shifts, being on call or studying for the RACP exams, were major factors influencing the intervention group participant attendance at workshops" Response rate: 88% Type of healthcare worker: exclusively physician trainees |
|
| Interventions |
Intervention characteristics Evaluation of a wellbeing workshop
Control (no intervention)
|
|
| Outcomes |
ProQOL ‐ Burnout
DASS ‐ stress
DASS ‐ Anxiety
DASS ‐ Depression
|
|
| Identification |
Sponsorship source: The authors received no financial support for the research, authorship, and/or publication of this article Country: Australian Setting: Several hospitals Comments: NR Authors name: Carmen Axisa Institution: University of Technology Sydney, Sydney, NSW, and; PhD Candidate, Sydney Medical School, The University of Sydney, Sydney, NSW, Australia Email: carmen.axisa@uts.edu.au Address: University of Technology Sydney, Building 10, Level 7, 235 Jones St, Ultimo, Sydney, NSW 2007, Australia. Time period: 2014‐105 |
|
| Notes | DASS‐stress included in analysis 1.1 and 1.2 DASS‐Anxiety included in analysis 1.4 and 1.5 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants were randomly assigned to the intervention or control group using a web‐based True Random Number Generator service." |
| Allocation concealment (selection bias) | Unclear risk | Unable to judge whether participants and/or investigators could possibly foresee assignment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 46 of the 59 (78%) randomised participants included in the analyses. Not reported whether lost to follow‐up was at random. |
| Selective reporting (reporting bias) | Low risk | No trial registration or no study protocol reported. No indication of selective reporting. |
| Other bias | Unclear risk | Compliance difficult to assess. |
Bagheri 2019.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Cognitive‐behavioural therapy + relaxation
Control (no intervention)
Overall
Included criteria: nurses of both sexes, undergraduate and postgraduate education, all age groups, more than one year experience of clinical work, and working in different wards. Excluded criteria: having a chronic physical and psychological illness, taking drugs that affected the mental system, and loss of a first‐degree relative (father, mother, spouse or child) less than six months beforehand. It was also announced that one of the admission requirements was the principle of confinement to educational materials and issues raised by the group members in each session. Pretreatment: age and the variable burnout and its subscales before intervention were not significantly different in the two groups. Compliance rate: NR Response rate: NR Type of healthcare worker: various healthcare professionals including nurses 44 (75%), head nurses 10 (17%) and supervisors 5 (9%) |
|
| Interventions |
Intervention characteristics Cognitive‐behavioural therapy + relaxation
Control (no intervention)
|
|
| Outcomes |
Maslach Burnout Inventory ‐ Emotional Exhaustion
Maslach Burnout Inventory ‐ Depersonalisation
Maslach Burnout Inventory ‐ Personal accomplishment (lack of)
|
|
| Identification |
Sponsorship source: NR Country: Iran Setting: Hospital Comments: NR Authors name: Bagheri T Institution: Burn Research Centre, Iran University of Medical Sciences, Tehran, Email: mahnoushmomeni@gmail.com, momeni.m@iums.ac.ir Address: Burn Research Centre, Motahari Hospital, Rashid Yasami St, Vali‐e‐asr Ave, Tehran, Iran Time period: 2014 |
|
| Notes | MBI‐EE included in analysis 1.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "They were assigned by the block randomization method to two groups of 30 subjects." Unclear how randomization took place. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Participants in the study included all nurses, head nurses and supervisors who met the inclusion criteria. They were assigned by the block randomization method to two groups of 30 subjects." Unable to judge whether participants or researchers could foresee the outcome of block randomization. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not described. |
| Selective reporting (reporting bias) | High risk | Quote: "their annual evaluation. Outcome measures: A demographic questionnaire was used to collect personal, social and occupational data including age, sex, marital status, educational level, work experience, overtime worked per month, work area, work shift, number of children and economic status. Burnout in all participants in the study was determined by the Maslach Burnout Questionnaire. Maslach Burnout Questionnaire (MBQ). The Maslach Burnout Questionnaire has 22 items which measure burnout in the three dimensions of emotional exhaustion (9 questions), personality depersonalization (5 questions), and individual performance (8 questions). In order to determine the total burnout score, questions 1, 2, 3, 5, 6, 9, 10, 12, 13, 14, 15, 19, 21 and 22 are considered (+) and questions 4, 7, 8, 11, 16, 17, 18 and 20 (‐), and then aggregated. Results for burnout frequency will be 35 to 84 (high), ‐15 to 34 (average), ‐16 to ‐66 (low) and for burnout severity 40 to 98 (high), ‐18 to 39 (average) and ‐19 to ‐77 (low). The validity of the questionnaire was verified by Maslach and Jackson and its reliability was calculated through Cronbach’s alpha, which was reported between ‐0.60 and 0.08. In Sedghi’s research, the reliability was determined to be 0.78. 20 The Cronbach’s alpha was reported as 0.8 in the present study. Data collection. In the second stage, the nurses in the intervention group received group cognitive therapy. In the third stage, immediately after and one month after training completion, the burnout level of all participants in the study was determined and evaluated by the Maslach burnout inventory. Data analysis. Data were extracted" In the trial register it is mentioned that the primary outcome is the Job Stress Questionnaire and the General Health questionnaire a secondary outcome while those have not been reported. https://en.irct.ir/trial/8633 |
| Other bias | Unclear risk | The response rate nor the compliance rate have been reported. |
Barattucci 2019.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Mindfulness‐Based IARA Model®
Control (no intervention)
Overall
Included criteria: NR Excluded criteria: NR Pretreatment: χ2 analyses revealed no differences between groups for any of the demographic and work characteristics: Gender, age education, marital state, and organisational seniority. t‐test analyses highlighted that training and control groups were almost overlapping at baseline on outcome measures. Compliance rate: NR Response rate: 98% Type of healthcare worker: various healthcare workers including doctors, nurses, and healthcare assistants |
|
| Interventions |
Intervention characteristics Mindfulness‐Based IARA Model®
Control (no intervention)
|
|
| Outcomes |
Zung Self‐Rating Anxiety Scale (SAS)
Perceived Stress Scale (PSS)
|
|
| Identification |
Sponsorship source: this research received no external funding. Country: Italy Setting: public hospitals Comments: NR Authors name: Massimiliano Barattucci Institution: eCampus University, 22060 Novedrate, Italy Email: massimiliano.barattucci@uniecampus.it Address: 22060 Novedrate, Italy Time period: 2018‐2019 |
|
| Notes | Author M.Barattucci kindly provided clarification on table 5. PSS included in analysis 1.2 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "All HCPs belonging to these wards—doctors, nurses, and healthcare assistants—were randomly assigned to a control group (N = 301) or to an IARA training program (N = 301)." Sequence generation process insufficiently described |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Material and Methods The research was configured as a randomized pre‐post evaluation with a comparison group, which included the completion of a questionnaire at the beginning (T0) and at the end of the training (T1). Baseline assessment was managed in November 2018, while Follow‐up in May 2019. All procedures performed in present study were in accordance with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. All participants gave their signed consent to participate in the study. The study was approved by the local ethics committee. From different Italian public hospitals, 602 HCP volunteer participants were recruited. The research involved many wards, such as oncology, general medicine, neurology, general surgery, gastroenterology, orthopedics, traumatology, urology, otolaryngology, pulmonology, and home care professionals. All HCPs belonging to these wards—doctors, nurses, and healthcare assistants—were randomly assigned to a control group (N = 301) or to an IARA training program (N = 301). Overall,</b> 497 workers participated in filling" Insufficient information to understand whether intervention allocations could have been foreseen in advance of, during, enrolment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "and of 202 HCPs for the control group (response rate = 68%; Figure 1)." High lost to follow‐up in the control group, reasons not provided. Unclear whether this was a random. |
| Selective reporting (reporting bias) | Unclear risk | No trial registration or study protocol reported nor did we find one online. |
| Other bias | Unclear risk | Compliance not reported. |
Barbosa 2015.
| Study characteristics | ||
| Methods |
‐Study design: cluster‐randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Psychoeducational intervention
Education‐only (active control)
Overall
Included criteria: to be included in the study, DCWs had to be employed for at least two months (so adjustments to the residents and facility had been achieved) and provide morning personal care (i.e. period of time between 7AM and 12AM that involved activities related to bathing, grooming, dressing and toileting) to people with a diagnosis of moderate to severe dementia. Excluded criteria: temporary DCWs and trainees were excluded as it was not possible to ensure their participation until the end of the study. Pretreatment: None of the measured socio‐demographic variables were statistically significantly different at baseline. At baseline, there were no significant differences between the groups in perceived stress, burnout, or job satisfaction. Compliance rate: NR Response rate: 100% Type of healthcare worker: Exclusively direct care workers (DCWs) |
|
| Interventions | Psychoeducational intervention Type of the intervention: Intervention type 4 ‐ Combination of two or more of the above Description of the intervention: the supportive component aimed to provide DCWs with coping strategies to manage work‐related stress and prevent burnout (e.g. time‐management, assertiveness, and problem‐solving). At the end of each supportive component, relaxation techniques, stretching, and strengthening exercises were practised. The number of sessions: 8 Duration of each session on average: 90 min Duration of the entire intervention: 8 weeks Duration of the entire intervention short vs long: short Intervention deliverer: by a gerontologist and a physical therapist with training and experience in PCC approaches and psycho‐educational groups Intervention form: group Education‐only (active control) Type of the intervention: education‐only Description of the intervention: the control facilities received an education‐only intervention.The coordination, length, order, and content of the sessions were the same as the educational component of the PE intervention. It was the absence of the supportive component that distinguished both interventions. Each participant was assisted during morning care by the same professionals who helped DCWs to deliver a more PCC and clarified doubts that emerged from sessions. The number of sessions: 8 Duration of each session on average: 90 min Duration of the entire intervention: 8 weeks Duration of the entire intervention short vs long: short Intervention deliverer: by a gerontologist and a physical therapist with training and experience in PCC approaches and psycho‐educational groups Intervention form: Group |
|
| Outcomes |
The Perceived Stress Scale (PSS)
Maslach Burnout Inventory ‐ Emotional exhaustion
Maslach Burnout Inventory ‐ Depersonalisation
Maslach Burnout Inventory ‐ Personal accomplishment
|
|
| Identification |
Sponsorship source: This work was supported by grants (grant numbers SFRH/BD/72460/2010 and RIPD/CIF/109464/2009) from the Foundation for Science and Technology (FCT) Country: Portugal Setting: 4 aged‐care facilities Comments: NR Authors name: Ana Barbosa Institution: Department of Health Sciences, University of Aveiro, Campus Universita ´rio de Santiago, Email: anabarbosa@ua.pt Address: Agra do Crastoedifıcio 30, Aveiro, Portugal. Time period: NR |
|
| Notes | PSS included in analysis 7.1 and 7.2 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | All four facilities agreed to participate and were randomly allocated to the experimental group—PE intervention—or control group— education‐only intervention, using a random number generator. |
| Allocation concealment (selection bias) | Low risk | After recruitment, the facilities within each pair were randomly assigned to the experimental group–PE intervention—or control group— education‐only intervention—using a random number generator. This decision was supported by the fact that education has become the most widely used approach with DCWs. Randomization occurred at the facility level because of possible contamination. No indication of allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants were blinded to the experimental or the control group. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Researchers were not blinded to the intervention or assessments, however outcomes were PROs. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Lost to follow‐up not at random (due to sick leave, dismissal, vacation) but relatively small (13%) |
| Selective reporting (reporting bias) | Unclear risk | No trial registration or study protocol reported, nor did we find one online. No indication of selective reporting. |
| Other bias | Unclear risk | Unit of analysis error (i.e. when a study ignored the clustering of the data in their analysis). Compliance not reported. |
Behnammoghadam 2019.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Eye movement desensitisation and reprocessing (EMDR)
Control (no intervention)
Overall
Included criteria: employed as one of the technician classes (rescuer, basic, middle, or senior technician) at pre‐hospital medical emergency services, age range 18–55 years, working at pre‐hospital medical emergency services as their main job, not employed in administrative departments or communication centre of pre‐hospital medical emergency services, no drug addiction, no hearing or vision impairment, and concurrently, getting scores above 19 in the Alken stress scale, and provided written informed consent to participate in the study. Excluded criteria: no motivation to cooperate, intolerance to the treatment, absent for more than one therapeutic session, imprecise completion of data collection instruments, transfer or death of the technician. Pretreatment: there were no significant differences between the two groups for age, years of experience and stress at baseline. Compliance rate: not able to assess as participants absent for more than one therapeutic session were excluded Response rate: not able to assess Type of healthcare worker: exclusively emergency medical technicians |
|
| Interventions |
Intervention characteristics Eye movement densensitization and reprocessing (EMDR)
Control (no intervention)
|
|
| Outcomes |
Elkin stress symptoms scale
|
|
| Identification |
Sponsorship source: NR Country: Iran Setting: Medical Emergency Services, urban and road stations Comments: NR Authors name: Sharif Shahini Institution: University of Medical Sciences, Next to Imam Sajad Hospital Email: sharif.shahini@yahoo.com Address: PO Box: 2591994 Yasuj, Iran Time period: 2017 |
|
| Notes | Elkin stress symptoms scale included in analysis 1.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A number was assigned to the subjects who concurrently got a score of above 19 in the SSS, and by matching that number with the block random allocation list, the technicians were assigned to the intervention or control group, and the process was continued until the completion of the estimated sample size." |
| Allocation concealment (selection bias) | Unclear risk | Quote: "25 people for each group. During random block assignment, the order of the participants in the intervention and control groups was determined as follows. By multiplying the number of study groups (two groups) by 2, the number of samples per block was calculated as 4; then, by calculating the factorial of each block sample size (4!=4×3×2×1=24), the number of blocks generated from all possible orders was obtained as 24; since the number of people in each block was 4 and the estimated sample size was 50 based on the following description, by matching 13 random numbers generated by Sample Randomizer with the mentioned block numbers, the order of 50 research subjects was determined, numbers 1–50 were allocated to the subject and control groups, and the random allocation list was edited." Difficult to judge whether participants and/or investigators could possibly foresee assignment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | Quote: "Iranian Clinical Trial Registry Website (code: IRCT20180102038191N1)." Trial registration in which the stress scale is not specified. No indication of selective reporting. |
| Other bias | Unclear risk | Not able to assess compliance/as participants absent for more than one therapeutic session were excluded. |
Bernburg 2019.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Mental Health Promotion Intervention
Control (wait list)
Overall
Included criteria: formal inclusion criteria were: (1) employment as a full time working nurse in a psychiatric hospital department, (2) time to take part in the study over the whole time period, (3) written consent to finish the surveys (baseline and three follow‐ups) Excluded criteria: not being on sick‐leave (Due to sickness absence, six nurses were excluded) Pretreatment: we found no significant differences between intervention and WCG with regard to gender, age, and working experience. Not recorded whether groups differed at baseline on the primary outcome perceived stress. Compliance rate: NR Response rate: not able to assess Type of healthcare worker: exclusively nurses working in psychiatry |
|
| Interventions |
Intervention characteristics Mental Health Promotion Intervention
Control (wait list)
|
|
| Outcomes |
Perceived Stress Questionnaire
|
|
| Identification |
Sponsorship source: NR Country: Germany Setting: Psychiatric Hospital Comments: NR Authors name: Monika Bernburg Institution: Institute of Occupational Medicine, Social Medicine and Environmental Medicine, Goethe‐University, Frankfurt am Main, Germany Email: mache@uke.de Address: CONTACT Stefanie Maches. Institute for Occupational and Maritime Medicine (ZfAM), University Medical Center Hamburg‐Eppendorf, Seewartenstrasse 10, 20459 Hamburg, Germany Time period: NR |
|
| Notes | PSQ included in analysis 4.1 and 4.2 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "generated algorithm." Quote: "participate in this intervention study. Afterwards, these nurses were randomised into two study groups through a computer‐generated algorithm." |
| Allocation concealment (selection bias) | Unclear risk | Quote: "The researchers invited 140 nurses via email and/or direct communication to participate in the intervention. In sum, 86 nurses confirmed and gave their consent to participate in this intervention study. Afterwards, these nurses were randomized into two study groups through a computer‐generated algorithm." Insufficient information to understand whether intervention allocations could have been foreseen in advance of, during, enrolment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "So in the end, 44 nurses were included in the intervention group (IG) and 42 nurses took part in waitlist control group (CG)." Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition was not reported. |
| Selective reporting (reporting bias) | Unclear risk | No trial registration or study protocol reported, nor did we find one online |
| Other bias | Unclear risk | Compliance rate not reported and response rate not able to assess. Not recorded whether groups differed at baseline on the primary outcome perceived stress. |
Bernburg 2020.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Psychosocial competence training combined with cognitive behavioural and solution‐focused counselling
Control (no intervention)
Overall
Included criteria: Inclusion criteria were: (1) regular access to the Internet, (2) full‐time employment in a clinic, (3) a maximum of two years of work experience (junior nurse), (4) availability and willingness to participate during the 36 weeks, (5) agree to complete the questionnaires, (6) no previous knowledge or experience with mental health promotion training. Excluded criteria: NR Pretreatment: Baseline data on socio‐demographic differences indicated only small, insignificant differences between intervention and control group (P > 0.05). Not recorded whether groups differed at baseline on the primary outcome perceived stress. Compliance rate: NR Response rate: difficult to assess as figure 1 is mentioned but not included in the article. Type of healthcare worker: exclusively junior nurses |
|
| Interventions |
Intervention characteristics Psychosocial competence training combined with cognitive behavioural and solution‐focused counselling
Control (no intervention)
|
|
| Outcomes |
Perceived Stress Questionnaire (PSQ)
Maslach Burnout Inventory ‐ Emotional Exhaustion
|
|
| Identification |
Sponsorship source: NR Country: Germany Setting: Hospitals Comments: NA Authors name: Monika Bernburg Institution: Institute of Occupational Medicine, Social Medicine and Environmental Medicine, Goethe University, Germany Email: s.mache@uke.de Address: Address for correspondence: Stefanie Mache, Institute for Occupational Medicine and Maritime Medicine (ZfAM), University Medical Center Hamburg‐Eppendorf, Martinistraße 52, 20251Hamburg, Germany. Time period: NR |
|
| Notes | MBI‐EE included in analysis 4.1 and 4.2 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "After answering the baseline questionnaire (t0) participants were randomized with the ratio 50%: 50% to the two study groups (IG or CG). The randomization process was accomplished with a computer generated list of numbers." |
| Allocation concealment (selection bias) | Low risk | Quote: "This list was created by an independent research assistant; another assistant was blinded to the list, securing covered distribution to research conditions." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "The CG group was asked to complete all surveys. The CG group received no intervention on mental health and did not undertake anything comparable to the intervention, e.g. any other training in psychosocial skills, counselling or therapy." Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Dropout attrition: There was an overall drop‐out rate (from randomization to analysis) of 12%. 10 participants decided to terminate the study (reasons included illness, non‐appearance of participants) and did not answer the questionnaires. Overall, four of the 94 participants at T1, 6/94 of participants at T2 and 4/94 of participants at T3 did not provide all follow‐up data on the results. The participants who did not provide all follow‐up data did not differ in any meaningful way, either in the primary outcome or in other baseline outcomes (P > 0.05), from those who provided data. " Low loss to follow‐up and follow‐up seems to be at random. |
| Selective reporting (reporting bias) | Unclear risk | No trial registration or no study protocol reported, nor did we find one online |
| Other bias | Unclear risk | Compliance rate not reported and response rate difficult to assess. Not recorded whether groups differed at baseline on the primary outcome perceived stress. |
Brazier 2022.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Dear Doctor
Control (no intervention)
Overall
Included criteria: trainees were invited to participate if they were registered as being in Core Training Year 2 (CT2), or Speciality Training Years 3 or 4 (ST3 or ST4) of the UK training programme at the time of recruitment. Excluded criteria: no exclusion criteria were applied. Pretreatment: randomisation was well‐balanced in the final sample: participants in the two trial groups did not differ in terms of profile or covariates. Compliance rate: 1 of the 139 opted out (99%) Response rate: 18% Type of healthcare worker: exclusively trainee anaesthetists |
|
| Interventions |
Intervention characteristics Dear Doctor
Control (no intervention)
|
|
| Outcomes |
Copenhagen Burnout Inventory ‐ work‐related subscale
|
|
| Identification |
Sponsorship source: The study was funded by the National Institute for Health Research Imperial Patient Safety Translational Research Centre and registered (ISRCTN11418903) Country: UK Setting: Royal College of Anaesthetists Comments: NR Authors name: A Brazier Institution: National Institute for Health Research Imperial Patient Safety Translational Research Centre, Faculty of Medicine, Imperial College London, London, UK Email: a.brazier19@imperial.ac.uk Address: NR Time period: 2019‐2020 |
|
| Notes | CBI included in analysis 4.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants were randomly assigned to intervention or control conditions with a 1:1 allocation ratio using a random number generator (Stata â, StataCorp, College Station, TX, USA). Randomisation was stratified by training year and across five broad training regions. " |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to understand whether intervention allocations could have been foreseen in advance of, during, enrolment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "Participants were not blinded to their condition assignment: intervention group participants received the intervention; control participants did not." Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Quote: "Despite the high attrition, there were no significant differences in participant characteristics (v 2 s < 3.80, ps > 0.15) or baseline outcomes measures (ts < 0.81, ps > 0.42) between those who did and did not complete the final survey (see also online Supporting Information Table S4)." High attrition, reasons other than did not complete survey not given. Lost to follow‐up appears to be at random. |
| Selective reporting (reporting bias) | Unclear risk | Quote: "The following exploratory findings should be regarded as indicative as they were not pre‐specified in the trial registry or protocol (the relevant outcomes were added after the start of the trial)." Trial registration number not provided, Difficult to assess whether there is selective outcome reporting. |
| Other bias | Unclear risk | Quote: "The RCoA identified and invited 1549 trainees to participate via email. Of the 647 (response rate 42%) who completed the baseline survey, 274 trainees (18% of the original cohort) consented to participate and remained in the trial throughout the trial period." Quote: "Female participants (v 2 = 8.07, p = 0.018), those with lower burnout (t = ‐2.42, p = 0.016), higher ‘meaningful’ score (t = 3.29, P = 0.001) and ‘valued’ score (t = 2.97, p = 0.003) were more likely to sign up for the trial after completing the baseline survey." Low selective response rate. |
Brennan 2006.
| Study characteristics | ||
| Methods | RCT, USA | |
| Participants | Nurses with at least 6 months full‐time bedside nursing in a hospital setting. Those who regularly receive massage therapy on their own as well as anyone with medical reasons for not being able to have chair massage were excluded. | |
| Interventions | 1) Experimental: massage: application to the back, neck, shoulders, arms and hands. Techniques used were effleurage, petrissage, friction, vibration and compression. One 30‐minute session per person over 4 days 2) Control: 10‐minute self‐directed break | |
| Outcomes | The Perceived Stress Scale | |
| Identification | ||
| Notes | PSS included in analysis 2.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported. |
| Allocation concealment (selection bias) | Low risk | "Sample size was 82 participants, randomly assigned to the massage group or the control group per a randomization schedule developed by a biostatistician who worked for the hospital but was not on the study team" (p. 337) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | "A total of 60 follow‐up surveys were completed, a 73% return rate" (p.339) |
| Selective reporting (reporting bias) | Low risk | There was only one outcome measured and reported. |
| Other bias | Unclear risk | We did not find any indications of other sources of bias. |
CezardaCosta 2019.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Stretching exercise
Control (no intervention)
Overall
Included criteria: to participate in the research, NPs could not present any medical impediment to performing physical exercises and not participating in any kind of physical activity oriented during the research. Those individuals who were absent from classes for three consecutive sessions for any reason were excluded. Excluded criteria: NR Pretreatment: NR Compliance rate: the frequency of the students was recorded in all classes. The participant who missed three or more consecutive classes was excluded from the investigation; however, the only person excluded from the study was even allowed participating in the classes Response rate: NR Type of healthcare worker: exclusively nurses |
|
| Interventions |
Intervention characteristics Stretching exercise
Control (no intervention)
|
|
| Outcomes |
Occupational Stress Scale (OSS)
|
|
| Identification |
Sponsorship source: Fundação Carlos Chagas Filho de Amparo à Pesquisa do Estado do Rio de Janeiro (FAPERJ Country: Brasil Setting: The State Institute of the Brain Paulo Niemeyer (IEC). Comments: NR Authors name: Flávia Porto Institution: Instituto de Educação Física e Desportos, Universidade do Estado do Rio de Janeiro Email: laviaporto30@gmail.com Address: Rua São Francisco Xavier, 524, Sala 9122F, Maracanã, CEP 20550‐900, Rio de Janeiro, RJ, Brasil Time period: NR |
|
| Notes | OSS included in analysis 2.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "They were chosen from a list of random numbers generated in software (Microsoft Excel 2010, São Paulo, Brazil)." |
| Allocation concealment (selection bias) | Unclear risk | Quote: "The volunteers were randomly assigned to the experimental group (EG: n = 20, 35.5 ± 9.5 years old, 69.9 ± 13.7 kg and 1.62±0.5m) and the control group (CG: n = 19, 37.8±8.9 years old, 81.8±15.4 kg and 1.68±0.9m). They were chosen from a list of random numbers generated in software (Microsoft Excel 2010, São Paulo, Brazil). The CG was submitted to the same evaluation as the EG. However, they did not participate in the classes of muscle stretching (MS). There was no blinding of participants and evaluators; however, it was considered that it did not influence the outcome of the study." Difficult to judge whether participants and/or investigators could possibly foresee assignment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "There was no blinding of participants and evaluators; however, it was considered that it did not influence the outcome of the study." Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote: "(MS). There was no blinding of participants and evaluators; however, it was considered that it did not influence the outcome of the study." Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "The participant who missed three or more consecutive classes was excluded from the investigation; however, the only person excluded from the study was even allowed participating in the classes." |
| Selective reporting (reporting bias) | Low risk | Trial registration. No indication of selective reporting. |
| Other bias | Unclear risk | Response rate not reported. |
Chen 2015.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Aromatherapy
Control (no intervention)
Overall
Included criteria: female nursing staff, participants were chosen by applying the following criteria: displaying more symptoms of stress than the average of 4.6, scheduled to work over seven consecutive days, ages and working years. The criteria possessed by the experimental group included: able to communicate with researchers, willing to participate in the project, not allergic to lavender, not suffering from any form of liver or kidney dysfunction, and with normal olfactory functions. Excluded criteria: NR Pretreatment: comparisons of control variables (ages, work experiences, working years, levels of education and promotion potentials) between the experimental and the control group showed no significant statistical distribution variance. Differences in the number of the stress symptoms on the pre‐test day between the experimental group and the control group did not have a statistical significance. Compliance rate: NR Response rate: not able to assess. Purposive sampling. Type of healthcare worker: exclusively female nurses. |
|
| Interventions |
Intervention characteristics Aromatherapy
Control (no intervention)
|
|
| Outcomes |
Number of Job stress‐related symptoms
|
|
| Identification |
Sponsorship source: NR Country: Taiwan Setting: Teaching hospital Comments: NR Authors name: Li Fang Institution: Department of Nursing, Meiho University, Email: fangli72@yahoo.edu.tw Address: 23 Pingguang Road, Neipu Shiang, Pingtung County 912, Taiwan. Time period: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Subsequently, the 110 nurses were randomly separated into two groups, one experimental group of 53 and one control group of 57." |
| Allocation concealment (selection bias) | Unclear risk | Difficult to judge whether participants and/or investigators could possibly foresee assignment, but the outcomes are not likely to be influenced. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Participants of the control group pinned small empty bottles on their clothes on the right chest. Some participants of the control group might note that the small bottle would not decrease stress because it had no odour. When participants in the experimental group received small bottles containing lavender oil and experienced the smells, they might know there was something in the bottle that might make differences." Placebo control group. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants were blinded and outcomes are PROs. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not mentioned explicitly, but it appears that there is no loss to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | No trial registration or study protocol reported, nor did we find one online No indication of selective reporting. |
| Other bias | Unclear risk | Compliance rate not reported. Response rate not able to assess.‘Loosely’ validated outcome measure. |
Cheng 2015.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Gratitude
Hassle
Control (no intervention)
Overall
Included criteria: full‐time Chinese professional workers Excluded criteria: exclusion criterion was scheduled long leave in the next 4 months. Pretreatment: age, education and years of experience differed statistically significant at baseline. Compliance rate: the compliance rate was excellent, with 99% of the diary days having valid returns. There were no significant differences between the two groups on number of diaries completed, as well as total number of events reported in the 4‐week period. Response rate: 82% Type of healthcare worker: various health care professionals including physicians (33%), nurses (55%) and physical/occupational therapists (12%). |
|
| Interventions |
Intervention characteristics Gratitude
Hassle
Control (no intervention)
|
|
| Outcomes |
Perceived Stress Scale
Center for Epidemiologic Studies‐Depression Scale (CES‐D)
|
|
| Identification |
Sponsorship source: This study was supported by Research Grants Council of Hong Kong Strategic Public Policy Research Grant No. HKIEd1001‐SPPR‐08 awarded to Sheung‐Tak Cheng. Country: Hong Kong Setting: 5 public hospitals Comments: NR Authors name: Sheung‐Tak Cheng Institution: Department of Health and Physical Education, Hong Kong Email: takcheng@ied.edu.hk Address: Institute of Education, 10 Lo Ping Road, Tai Po, N.T. Time period: NR |
|
| Notes | PSS included in analysis 1.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "control. Method Design and Randomization This was a double‐blind randomized controlled trial with follow‐up to 3 months posttreatment. Participants were randomly assigned into one of three experimental conditions— gratitude, hassle, and nil‐treatment control. 3 Block‐restricted randomization was performed by the second author using a true random number generator to create groups of" Quote: "generator to create groups of equal size (n = 34 per group). Participants were told that this was a study about the well‐being of health care workers, without further details about the research objective or hypothesis. Data collection consisted purely of self‐ administered questionnaires. The research assistants were blind to experimental assignment and were not involved in obtaining diaries or answers to the questionnaires. Participants were debriefed at the conclusion of the study." |
| Allocation concealment (selection bias) | Low risk | No indication of selection bias |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote: "All questionnaires and diaries were filled out by the participants themselves, who were told not to disclose details of the experiment to others." Although this was a double‐blind randomised‐controlled trial it is questionable whether the blinding was effective as participants randomised to the gratitude or hassle group were asked to keep a diary and could have informed colleagues. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Participants were blinded to group assignment and outcomes are PROs. It is questionable whether the blinding was effective as participants randomised to the gratitude or hassle group were asked to keep a diary and could have informed colleagues. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "One hassle and two gratitude participants did not have data at the 3‐month follow‐up (see Figure 1). Little’s (1988) missing completely at random test yielded a nonsignificant result, 2 (6) 7.14, p.308. Therefore, the data were missing completely at random, and all available data could be used. |
| Selective reporting (reporting bias) | Low risk | Quote: "The trial protocol is available from the first author." No public trial protocol nor trial registration. No identification of selective outcome reporting. |
| Other bias | Low risk | Quote: "Although age, years of experience, and education were significantly different among groups at baseline, and were related to perceived stress, only the latter two were included as covariates, as age and years of experience were highly correlated (r .89, p.001) and experience was theoretically more closely related to stress." Quote: "total of 125 practitioners were approached, and 102 physicians, nurses, physiotherapists, and occupational therapists provided consent to participate (success rate 82%)." Quote: "Owing partly to reminders sent by the research team, the compliance rate was excellent, with 99% of the diary days having valid returns. There were no significant differences between the two groups on number of diaries completed" |
Chesak 2020.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Authentic Connections Groups
Control (no intervention)
Overall
Included criteria: inclusion criteria included being: (a) a nursing education specialist or clinical nurse specialist, and (b) a mother to at least one child or adult child. Excluded criteria: exclusion criteria included: (a) being actively suicidal or (b) meeting criteria for psychoses. Pretreatment: NR Compliance rate: 1/18 allocated to the intervention group dropped out. Session attendance rates among the intervention group averaged 92% across the study (not including the participant who dropped out) Response rate: NR Type of healthcare worker: exclusively nurses |
|
| Interventions |
Intervention characteristics Authentic Connections Groups
Control (no intervention)
|
|
| Outcomes |
The Perceived Stress Scale
Maslach Burnout Inventory ‐ Emotional Exhaustion
Maslach Burnout Inventory ‐ Personal accomplishment (lack of)
Self‐Rating Depression Scale ‐ Depression
Self‐Rating Depression Scale ‐ Anxiety
|
|
| Identification |
Sponsorship source: Funding Sources: Elizabeth C. Bonner Endowment Fund; Authentic Connections Country: USA Setting: Hospital Comments: NA Authors name: Sherry S. Chesak Institution: Department of Nursing, Division of Nursing Research, Mayo Clinic Email: chesak.sherry@mayo.edu Address: 200 First St. SW, Rochester, MN 55905 Time period: NR |
|
| Notes | PSS included in analysis 1.1 and 1.2 Self‐Rating Depression Scale ‐ Depression included in analysis 1.4 and 1.5 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Participants who agreed and consented were randomly assigned to the intervention group (n = 18) or control group (n = 18)." Sequence generation process not mentioned |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Participants who agreed and consented were randomly assigned to the intervention group (n = 18) or control group (n = 18). " Unable to judge whether participants and/or investigators could possibly foresee assignment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 13/15 of the 18 participants (72%/83%) allocated to the intervention group completed respectively post‐intervention and 3‐month follow‐up assessment. 17/14 of the 18 participants (78%/94%) allocated to the intervention group completed respectively post‐intervention and 3‐month follow‐up assessment. Reasons not provided. Not mentioned whether lost to follow‐up at random. |
| Selective reporting (reporting bias) | Unclear risk | No trial registration or study protocol reported, nor did we find one online |
| Other bias | Unclear risk | Not able to assess response rate. Authors mention that they have corrected for baseline differences. However, the baseline characteristics have not been reported. |
Cho 2021.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Meridian acupressure
Control (wait list)
Overall
Included criteria: the inclusion criteria for participants were daytime shift work nurses who voluntarily agreed to participate, without cognitive disorder, with clear consciousness, ability to communicate in verbal and non‐verbal language, and ability to understand the objectives of the study. Three participants who reported a poor state of health state without a doctor’s diagnosis and prescription were included. Excluded criteria: the exclusion criteria were persons diagnosed with acute or chronic illness by a doctor, those who have taken a prescription with skin lesions at the intervention site, and pregnant and lactating women. Pretreatment: the analysis of the homogeneity between the intervention and control groups showed that they were homogeneous, with a significance level of P < 0.05 Compliance rate: NR Response rate: NR convenience sample Type of healthcare worker: exclusively nurses |
|
| Interventions |
Intervention characteristics Meridian acupressure
Control (wait list)
|
|
| Outcomes |
The stress scale ‐ psychological stress
The stress scale ‐ physical stress
The State Anxiety Inventory (SAI)
The stress scale ‐ total
|
|
| Identification |
Sponsorship source: The author(s) received no financial support for the research, authorship, and/or publication of this article Country: Korea Setting: Hospital Comments: NR Authors name: Youngmi Cho Institution: Department of Nursing, Sun Moon University Email: choyoung23@yahoo.com Address: Chungcheongnam‐do, Asan‐si 31460 Korea Time period: 2018 |
|
| Notes | The stress scale included in analysis 2.1 STAI included in analysis 2.3 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The participants were recruited through convenience sampling. During the coin toss, heads meant the subject became a participant in the intervention group in this study." |
| Allocation concealment (selection bias) | Unclear risk | Quote: "The participants were recruited through convenience sampling. During the coin toss, heads meant the subject became a participant in the intervention group in this study. " Insufficient information to understand whether intervention allocations could have been foreseen in advance of, during, enrolment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | No trial registration or no study protocol reported, nor did we find one. |
| Other bias | Unclear risk | Compliance and response rate not recorded. |
Cohen‐Katz 2005.
| Study characteristics | ||
| Methods | RCT, USA | |
| Participants | 25 nurses, pastoral care, respiratory therapy and social work personnel | |
| Interventions | 1) Experimental: mindfulness‐based stress reduction programme: 8‐week program with approximately 2.5 hours teaching per week and homework practice with audiotapes for six days a week. Group sessions included teaching on topics such as communication skills, stress reactivity and self‐compassion and experiential exercises to help participants integrate these concepts. 2) Control: no intervention | |
| Outcomes | MBI, Brief Symptom Inventory | |
| Identification | We kindly received data from the author. | |
| Notes | MBI‐EE included in analysis 2.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Participants were then randomly assigned to the treatment group or the wait‐list control group." (p.27) |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 2/14 (14%) in the treatment group did not return completed inventories and were not taken into consideration in the analyses, which is below our pre‐defined cut‐off value. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Unclear risk | We did not find any indications of other sources of bias. |
Concilio 2021.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Text messaging (Social Support Behavioral Code)
Control (text messaging ‐ medical facts)
Overall
Included criteria: eligibility criteria were: (a) NLGNs employed as RNs for the first time, (b) ages 19 to 37 years (millennials and post‐millennials) as the majority joining the workforce (NursingLicensure.org, 2020), (c) proficient in English, (d) working in an acute care facility as an RN during the first year of hire, (e) had a working personal smartphone, (f) had the ability to send and receive text messages, (g) had an active and working personal email account, (h) were willing to participate for 6 weeks, (i) completed survey instruments at baseline, week 3, and week 6, (j) agreed to not use or carry their smartphone while performing direct patient care, and (k) assumed any data charges for text messages Excluded criteria: exclusion criteria were NLGNs who had worked as an RN on another floor or at another organisation Pretreatment: NR Compliance rate: Response rate: 100% Type of healthcare worker: exclusively nurses who were in their first year of hire. |
|
| Interventions |
Intervention characteristics Text messaging (Social Support Behavioral Code)
Control (text messaging ‐ medical facts)
|
|
| Outcomes |
Perceived Sense of Stress (PSS)
|
|
| Identification |
Sponsorship source: NR Country: USA Setting: two urban health care systems located in western Pennsylvania and southern California. Comments: NR Authors name: Lisa Concil Institution: Lecturer and Clinical Instructor, San Diego State University Email: 10006 Maya Linda Road, #5207, San Diego, CA 92126 Address: lconcilio@sdsu.edu Time period: NR |
|
| Notes | PSS included in analysis 3.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was conducted using an online random sequence generator (Random.org, 2019)." |
| Allocation concealment (selection bias) | Unclear risk | Quote: "A $20 gift card was sent to participants who completed the study requirements. Additionally, the first four participants who completed the study at the end of week 6 were awarded another $50 gift card." We assume that consecutive nurses were randomised. Difficult to judge whether nurses or the investigator could possibly foresee assignment. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Unclear whether participants were blinded. The control group received 'placebo' text messages. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unclear whether participants were blinded whereas outcomes were self‐reported. The control group received 'placebo' text messages. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rate is low. (21/22 were included in the analysis). Reason provided. Not reported whether the participant that was lost to follow‐up differed from the other participants. |
| Selective reporting (reporting bias) | Unclear risk | No trial registration or no study protocol reported, nor did we find one online. No indication of selective reporting. |
| Other bias | Unclear risk | Not reported whether there were any baseline differences between groups on stress, gender, age. |
Copeland 2021.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Meditation
Journal
Outside
Gratitude
Control (no intervention)
Overall
Included criteria: Full and part‐time nurses and nurse aides working any shift at a suburban, 225 bed, Level 1 trauma centre were eligible to participate. Excluded criteria: NR Pretreatment: NR Compliance rate: 3 of the 18 nurses assigned to an intervention group did not complete the six‐week intervention (17%) Response rate: NR Type of healthcare worker: exclusively nurses |
|
| Interventions |
Intervention characteristics Meditation
Journal
Outside
Gratitude
Control (no intervention)
|
|
| Outcomes |
ProQOL ‐ Burnout
ProQOL ‐ Compassion Satisfaction
ProQOL ‐ Secondary Trauma
|
|
| Identification |
Sponsorship source: The author(s) received no financial support for the research, authorship, and/or publication of this article. Country: United States of America Setting: 1 trauma center Comments: NR Authors name: Darcy Copeland Institution: College of Natural and Health Sciences, University of Northern Colorado Email: darcy.copeland@unco.edu Address: Gunter Hall 3080, Campus Box 125, Greeley, CO 80639, USA Time period: NR |
|
| Notes | Pro_QOL_BO included in analysis 2.1.Intervention groups combined to create a single pair‐wise comparison | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "As participants were enrolled, they were randomized, using a list of random numbers generated from an online random number generator, into one of five groups: meditation, outside, gratitude, journal, or control." |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Upon receipt of IRB approval, nurses and nurse aids were invited to participate via organizational email. As interested participants contacted the PI, they were screened for eligibility and a time was arranged to complete informed written consent procedures, the pre‐intervention assessment, and receive intervention instructions. As participants were enroled, they were randomized, using a list of random numbers generated from an online random number generator, into one of five groups: meditation, outside, gratitude, journal, or control." As a list of random numbers was used it is assumed that the person who randomised patients could foresee allocation it is however unclear who performed randomisation. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not asked to change any other practise while at work; participants assigned to one intervention were not expressly discouraged from engaging in the other interventions. Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes were self‐reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 2 of the 22 participants were not included in the analysis (9%). Reasons were provided. Participants who did not complete the study were more often male however loss to follow‐up is below our pre‐defined cut‐off point. |
| Selective reporting (reporting bias) | Unclear risk | No trial registration or no study protocol reported, nor did we find one. |
| Other bias | Unclear risk | Not recorded whether there were differences at baseline between groups. |
Dahlgren 2022.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Proactive recovery programme
Control (no intervention)
Overall
Included criteria: RNs with less than 12 months’ work experience were eligible to participate. Excluded criteria: NR Pretreatment: no significant differences were observed between the two groups at baseline for any of the background variables or any of the outcome measures at baseline. Compliance rate: 36 of the 99 (36%) participants randomised to the intervention group participated in two of the three sessions. Response rate: 45% (207/461) Type of healthcare worker: exclusively nurses |
|
| Interventions |
Intervention characteristics Proactive recovery programme
Control (no intervention)
|
|
| Outcomes |
Perceived Stress Scale (PSS)
Shirom‐Melamed Burn‐out Questionnaire (SMBQ) ‐ Global
|
|
| Identification |
Sponsorship source: This study was funded by AFA Försäkring (150024) Country: Sweden Setting: Eight Swedish hospitals Comments: NR Authors name: Anna Dahlgren Institution: Department of Clinical Neuroscience, Karolinska Institute, Stockholm, Solna, Sweden Email: anna.dahlgren@ki.s Address: NR Time period: 2017‐2018 |
|
| Notes | PSS included in analysis 2.1 and 2.2 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Excel generator for random allocation to groups was used by the research team. Based on a previous feasibility study, adjustments to the process of random group allocation were made if many nurses from the same ward were initially allocated to one group. Twenty adjustments were also made for participants who were randomised to the intervention group but knew that they could not attend the group sessions. They were moved to the control group and replaced by a random participant from the control group. |
| Allocation concealment (selection bias) | High risk | Quote: "parallel randomised control trial was designed to include 100 participants in each group (intervention and wait list control) to detect moderate effect sizes (Cohen’s d = 0.5) resulting in a power of 0.94. Excel generator for random allocation to groups was used by the research team. Based on a previous feasibility study, adjustments to the process of random group allocation were made if many nurses from the same ward were initially allocated to one group. Twenty adjustments were also made for participants who were randomised to the intervention group but knew that they could not attend the group sessions. They were moved to the control group and replaced by a random participant from the control group. Adjustments were made for 24 participants. Masking was not applicable. After the follow‐up measure the control group received the intervention." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | 'Masking was not possible'. Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 130 of the 207 randomised participants (63%) completed 6 months follow‐up. Reasons not provided as well as whether it was at random. |
| Selective reporting (reporting bias) | High risk | Trial registration (https://clinicaltrials.gov/ct2/show/NCT04246736). In the trial registration many other stress outcomes were mentioned, which were not mentioned in this study, i.e.
|
| Other bias | Unclear risk | Judgement Comment: Low response rate 207/461 (45%) |
deSouza 2021.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Massage
Control (no intervention)
Overall
Included criteria: The inclusion criteria were the following: woman age 20 to 45; working in day‐time shift (morning, afternoon, 12‐hour shift), LSS score ≥ 40, time working in the hospital at least one year, a 30‐day interval between returning from vacation or medical level. Excluded criteria: The exclusion criteria were: smokers, hypertensive individuals, use of glucocorticoids, beta‐blockers, psychoactive drugs in the last three months, pregnant, or hysterectomised woman, use of integrative practises (acupuncture, massage, herbal therapy, Reiki, or floral therapy amongst others) for at least two months. Pretreatment: the groups were homogenous regarding the qualitative variables used to describe the population ‐ age, BMI, LSS, and BPI ‐ except for the pain interference component in enjoyment of life (P = 0.037). Compliance rate: two of the 30 missed a massage session (6.7%) Response rate: 60 of the 91 eligible patients participated (66%) Type of healthcare worker: exclusively nurses |
|
| Interventions |
Intervention Characteristics Massage
Control (no intervention)
|
|
| Outcomes |
The List of Stress Symptoms (LSS)
|
|
| Identification |
Sponsorship source: The study was funded by the Research Support Foundation of the State São Paulo (Process No 2017/19, 645‐2) Country: Brazil Setting: Two teaching cancer hospitals Comments: NR Authors name: Borges de Souza Institution: Nursing course of the Santa Casa de São Paulo school of medicine sciences Email: Talita.Paverni@fcmsantacasasp.edu.br Address: Rua dr. Cesario Motta 3r, 61, 01221‐020 Time period: 2017‐2018 |
|
| Notes | LSS included in analysis 2.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The volunteers who met the inclusion criteria were numbered for the two‐group simple randomization (http://www.randomizer.org). After this, one of the researchers created a sequential numerical list: the first participant was randomly chosen and the rest were included in the list as they met the eligibility criteria and according to the groups of the randomized list. |
| Allocation concealment (selection bias) | Unclear risk | The volunteers who met the inclusion criteria were numbered for the two‐group simple randomization (http://www.randomizer.org). After this, one of the researchers created a sequential numerical list: the first participant was randomly chosen and the rest were included in the list as they met the eligibility criteria and according to the groups of the randomized list. Insufficient information to understand whether intervention allocations could have been foreseen in advance of, during, enrolment. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants were blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The study was blinded to researchers, participants and statistician. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 12 of the initial 60 participants discontinued the study (20%), reasons provided but not whether they differed with responders. After that another 12 participants was randomized and included in the analysis. The baseline characteristics are provided for 30 participants, but it is unclear which participants are included here. |
| Selective reporting (reporting bias) | Low risk | In the trial protocol, the authors mention that salivary cortisol is, alongside the LSS, the primary outcome. Salivary not reported in this article. https://ensaiosclinicos.gov.br/rg/RBR-3bjjf4 but is not one our outcome measures so no selective reporting on outcomes that we are interested in. |
| Other bias | Low risk | Judgement Comment: No indication of other sources of bias. |
Dincer 2021.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Emotional Freedom Techniques
Control (wait list)
Overall
Included criteria: nurses caring for COVID‐19 patients. Inclusion criteria were: a) not having any psychiatric diagnoses, b) not taking any courses about coping with anxiety and stress, and c) volunteering to participate in the study Excluded criteria: NR Pretreatment: no statistically significant pre‐intervention differences were found between the groups on demographic variables. The pre‐test stress level, anxiety level and the burn‐out score did not differ significantly between the groups. Compliance rate: five of the 40 participants did not attend the EFT sessions (13%) Response rate: 100% Type of healthcare worker: exclusively nurses caring for COVID‐19 patients |
|
| Interventions |
Intervention characteristics Emotional Freedom Techniques
Control (wait list)
|
|
| Outcomes |
State Anxiety Scale
The Burnout Scale
Subjective Units of Distress Scale
|
|
| Identification |
Sponsorship source: This research was not funded. Country: Turkey Setting: A university hospital Comments: NR Authors name: Berna Dincer Institution: Department of Internal Medicine Nursing, Faculty of Health Science, Istanbul Medeniyet University, Istanbul, Turkey Email: berna.dincer@medeniyet.edu.tr Address: 38, Tıbbiye Street, Istanbul, Uskudar 34668, Istanbul, Turkey Time period: 2020 |
|
| Notes | Subjective Units of Distress Scale included in analysis 2.1 STAI included in analysis 2.3 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Eighty nurses who met the inclusion criteria were assigned to groups using an online random number generator. |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to understand whether intervention allocations could have been foreseen in advance of, during, enrolment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "After completing the Descriptive Characteristics Form online, a time for the meeting was determined in collaboration with the participants in each subgroup. They were also asked to stay comfortable in as calm and tranquil an environment as possible during the session. The EFT treatment was provided by the first author, who was certified in EFT. Each 5‐person group began by having the participants complete the pre‐test SUD, the STAI‐I, and the burnout scale via SurveyMonkey." Participants were not blinded. Baseline questionnaire filled in after randomisation. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote: "The analysis was conducted by a researcher who was blind to group assignment." Participants were not blinded whereas outcomes were self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 10% lost‐to‐follow‐up however unknown whether this was at random however loss to follow‐up is below our pre‐defined cut‐off point. |
| Selective reporting (reporting bias) | High risk | No intention to tread analysis. Participants randomised to the intervention group that did not attend the EFT session (n = 5) were excluded. |
| Other bias | Low risk | No indication of other sources of bias |
Duchemin 2015.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline Characteristics Mindfulness‐based intervention
Control (wait list)
Overall
Included criteria: participants were personnel, 18 or older, from the surgical intensive care unit (SICU) of a large academic medical center. Eligibility criteria included any personnel working in the SICU and having contact with the patients or their families. Excluded criteria: individuals practising mindfulness, yoga, or exercising more than 30 minutes a day were excluded, as were individuals with third trimester pregnancy or a history of recent surgery if it limited ability to perform the gentle yoga movement Pretreatment: there were no significant differences between the two groups for age (P = 0.9496, t = 0.0638), years of experience (P = 0.9485, t = 0.06512), or years working in the SICU (P = 0.8702, t = 0.1648). Compliance rate: NR Response rate: not able to assess as the exact number of eligible individuals is not reported. More than 200 individuals working in the SICU were eligible to participate and were informed about the study through flyers and information provided at staff meetings. Thirty‐two individuals were interested in participating and all were eligible to participate because of minimal exclusion criteria to reflect real workplace conditions. Type of healthcare worker: various healthcare staff but 69% nurses |
|
| Interventions |
Intervention characteristics Mindfulness‐based intervention
Control (wait list)
|
|
| Outcomes |
DASS ‐ stress
Perceived Stress Scale
Maslach Burnout Inventory ‐ emotional exhaustion
Maslach Burnout Inventory ‐ depersonalization
Maslach Burnout Inventory ‐ Personal accomplishment
Professional Quality of Life (ProQOF)
|
|
| Identification |
Sponsorship source: Funding: Funded in part by the OSU Harding Behavioral Health Stress, Trauma and Resilience program Country: Unites States Setting: A large academic medical center Comments: NR Authors name: Anne‐Marie Duchemin Institution: Department of Psychiatry, The Ohio State University, Email: anne‐marie.duchemin@osumc.edu Address: 1670 Upham Drive, Columbus, OH 43210, USA. Time period: NR |
|
| Notes | Not able to include in analysis due to missing data. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Eligible participants were randomized 1:1 using Graphpad software to intervention group or waiting list control group, with stratification by gender and type of work. Assessments were performed for all" |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Eligible participants were randomized 1:1 using Graphpad software to intervention group or waiting list control group, with stratification by gender and type of work. Assessments were performed for all participants," Difficult to judge whether participants and/or investigators could possibly foresee assignment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote: "Questionnaires and samples were coded." Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "There was no drop‐out and all participants completed the 2 sets of assessments." |
| Selective reporting (reporting bias) | Unclear risk | No trial registration or study protocol reported, nor did we find one online |
| Other bias | Unclear risk | Quote: "was considered statistically significant. RESULTS More than 200 individuals working in the SICU were eligible to participate and were informed about the study through flyers and information provided at staff meetings. Thirty‐two individuals were interested in participating and all were eligible to participate due to minimal exclusion criteria to reflect real workplace conditions. Participants (n = 32) were" Not able to assess the response rate as the exact number of eligible individuals is not reported. Compliance not reported. |
Dunne 2019.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Attention‐based training (ABT)
Control (wait list)
Overall
Included criteria: a current staff member of the emergency department of St. James’ Hospital; preference to participate in the study and to be over 18 years of age Excluded criteria: alcohol or substance abuse within the past 6 months; more than four consecutive classes of meditation or other mind–body practises (including yoga and Tai‐chi) in the past two years; a diagnosis of schizophrenia; currently using (at time of enrolment) anti‐psychotic medication or recently started on anti‐depressant meditation (less than three months at the time of enrolment). Participants on a stable dose of anti‐depressant medication (for more than three months) were permitted but advised to consult with their general practitioner or psychiatrist prior to enrolment. Pretreatment: NR Type of healthcare worker: exclusively emergency department healthcare worker Response rate: 100% Compliance rate: 16 of the 29 followed at least two sessions > 55% |
|
| Interventions |
Intervention characteristics Attention‐based training (ABT)
Control (wait list)
|
|
| Outcomes |
Maslach Burnout Inventory ‐ Emotional Exhaustion
Maslach Burnout Inventory ‐ Depersonalisation
Maslach Burnout Inventory ‐ Personal accomplishment
DASS ‐ stress
DASS ‐ anxiety
|
|
| Identification |
Sponsorship source: NR Country: Ireland Setting: Hospital Comments: NR Authors name: PJ Dunne Institution: Trinity Translational Medicine Institute, Trinity College Email: padraicdunne@rcsi.com Address: Dublin D08 W9RT, Ireland Time period: NR |
|
| Notes | The authors kindly referred to the supplementary file. MBI‐EE included in analysis 2.1 DASS anxiety included in analysis 2.3 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Emergency MDT participants were stratified by role and gender and allocated to intervention or no‐treatment control group using an online randomization tool [17]. Volunteers" |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Emergency MDT participants were stratified by role and gender and allocated to intervention or no‐treatment control group using an online randomization tool [17]." Insufficient information to understand whether intervention allocations could have been foreseen in advance of, during, enrolment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "There was no significant difference between study completers and withdrawers." 42 of the 58 participants were analysed. Response rate 72%. However, missing at random according to the authors. |
| Selective reporting (reporting bias) | Unclear risk | The authors report a trial registration, nor did we find one online |
| Other bias | Unclear risk | Unclear whether participants differ on baseline characteristics. |
Dyrbye 2016.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Intervention
Control (no intervention)
Overall
Included criteria: NR Excluded criteria: NR Pretreatment: Reported socio demographic baseline characteristics of participants randomised to the intervention group were similar to socio demographic baseline characteristics of participants randomised to the control group Compliance rate: We could not determine if participants in the intervention arm actually completed their chosen weekly micro‐tasks Response rate: NR Type of healthcare worker: physicians from various disciplines |
|
| Interventions |
Intervention characteristics Intervention
Control (no intervention)
|
|
| Outcomes |
Maslach Burnout Inventory ‐ Emotional exhaustion
Maslach Burnout Inventory ‐ Personal accomplishment (lack of)
Maslach Burnout Inventory ‐ Depersonalisation
|
|
| Identification |
Sponsorship source: NR Country: USA Setting: Mayo Clinic Departments of Medicine in Minnesota and Arizona and Mayo Clinic Department of Surgery in Minnesota Comments: NR Authors name: Dyrbye LN, West CP, Richards ML, Ross HJ, Satele D, Shanafelt TS Institution: Mayo Clinic Email: Dyrbye.liselotte@mayo.edu Address: 200 Second Street SW, Rochester, Minnesota, 55905, United States Time period: NR |
|
| Notes | MBI‐EE included in analysis 1.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants were randomized to an intervention group or a control group using a computer‐generated algorithm. Randomization was stratified by speciality (Internal Medicine or Surgery), campus (Rochester or Arizona), and baseline response to the single item, “The work I do is meaningful to me” (from the Empowerment at Work Scale (Spreitzer, 1995)). All participants were asked to complete baseline and end‐of‐study (three month) survey. For both surveys consented participants received an e‐mailed cover letter with a link to a web‐based survey." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to understand whether intervention allocations could have been foreseen in advance of, during, enrolment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Over 90% of participants in each arm completed both the baseline and end‐of‐study surveys. |
| Selective reporting (reporting bias) | Unclear risk | No protocol registration, nor did we find one online. |
| Other bias | Unclear risk | Response rate not reported. Quote: We could not determine if participants in the intervention arm actually completed their chosen weekly micro‐tasks |
Dyrbye 2019.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Coaching
Control (wait list)
Overall
Included criteria: Individuals who had been in practice for 5 to 30 years were eligible Excluded criteria: NR Pretreatment: no group differences reported Type of healthcare worker: exclusively physician Response rate: 12% Compliance rate: Participants randomised to the intervention group had a mean of 5.5 coaching sessions (range, 0‐6 coaching sessions). |
|
| Interventions |
Intervention characteristics Coaching
Control (wait list)
|
|
| Outcomes |
Maslach Burnout Inventory ‐ Emotional exhaustion
Maslach Burnout Inventory ‐ Depersonalization
Maslach Burnout Inventory ‐ Personal accomplishment
|
|
| Identification |
Sponsorship source: Funding for this study was provided by the Mayo Clinic Department ofMedicine Program on Physician Well‐Being and thePhysician Foundation Country: USA Setting: Mixed healthcare settings including the department of medicine, family medicine and pediatric Comments: NR Authors name: Liselotte N.Dyrbye Institution: Department of Medicine, Program on Physician Well‐Being, Mayo Clinic Email: dyrbye.liselotte@mayo.edu Address: 200 First StSW, Rochester, MN 55905 Time period: 2017‐2018 |
|
| Notes | We kindly received the mean and SD of the MBI‐EE for both groups from author C. West. MBI‐EE included in analysis 1.1 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "We used a computer‐generated dynamic allocation algorithm to randomize participants into a coaching group and a control group. Randomization" |
| Allocation concealment (selection bias) | Unclear risk | Quote: "We used a computer‐generated dynamic allocation algorithm to randomize participants into a coaching group and a control group. Randomization was stratified by years in practice, work site (Arizona, Florida, Minnesota, or Mayo Clinic Health System), and primary care (family medicine, general pediatrics, or general internal medicine) vs sub‐specialty practice." Insufficient information to understand whether intervention allocations could have been foreseen in advance of, during, enrolment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 82 of the 88 completed follow‐up >93% |
| Selective reporting (reporting bias) | Low risk | The authors report a trial register. For the outcomes that we are interested in, there is no selective outcome reporting. |
| Other bias | Unclear risk | Low participation rate (88 of the 764 eligible physicians participated) |
ElKhamali 2018.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Multimodel intervention
Control (no intervention)
Overall
Included criteria: (1) actively working in an adult ICU, (2) held a registered nurse license, and (3) had at least 6 months’ work experience in the current ICU. Excluded criteria: (1) current placement outside ICU, (2) on maternity or sick leave, (3) planning to leave ICU, or (4) already completed the simulation intervention prior to the beginning of the trial. Pretreatment: the only major between‐group difference was in marital status (46% were single in the intervention group vs 62% in the control group). Compliance rate: 100% Response rate: 100% Type of healthcare worker: nurses |
|
| Interventions |
Intervention characteristics Multi‐model intervention
Control (no intervention)
|
|
| Outcomes |
Job stress questionnaire (JSQ) ‐ psychological demand
Job stress questionnaire (JSQ) ‐ decision latitude
Job stress questionnaire (JSQ) ‐ Social support
The Copenhagen Psychosocial Questionnaire ‐ (COPSOQ) ‐ stress
The Copenhagen Psychosocial Questionnaire ‐ (COPSOQ) ‐ burnout
|
|
| Identification |
Sponsorship source: NR Country: France Setting: Hospital Comments: NR Authors name: Radia El Khamali Institution: Assistance Publique‐Hôpitaux de Marseille, Hôpital Nord, Réanimation des Détresses Respiratoires et des Infections Sévères, Marseille, Franc Email: laurent.papazian@ap‐hm.fr Address: Laurent Papazian, MD, PhD, Médecine Intensive‐Réanimation, Hôpital Nord, Chemin des Bourrely, 13015 Marseille, France Time period: 2016‐2019 |
|
| Notes | COPSOQ stress included in analysis 4.2 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Briefly, ICU nurses meeting the inclusion criteria were selected by lots drawn by the clinical research unit at the Assistance Publique‐Hôpitaux de Marseille, which was not involved with the ICU. At each planned session, the chief nurse provided the clinical research unit with a list of nurses to participate in the program (each nurse chose an identification number). The clinical research unit selected 2, 4, 6, 8, 10, or 12 nurses to participate in the trial. Half of the selected nurses (1, 2, 3, 4, 5, or 6) were randomized to the intervention group and the other half were randomized to the control group. |
| Allocation concealment (selection bias) | Unclear risk | Participants were randomly assigned using a computer‐generated randomization list (allocation ratio of 1:1) and a permuted block design (block size range, 4‐8). Participants from 1 to 3 ICUs were randomized to 1 of 2 equal‐sized groups: (1) the 5‐day intervention simulation training group or (2) the control group (nurses did not participate in simulation training but answered questionnaires). Insufficient information to understand whether intervention allocations could have been foreseen in advance of, during, enrolment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Almost no loss to follow‐up, those lost reasons were reported |
| Selective reporting (reporting bias) | High risk | Registration protocol: https://clinicaltrials.gov/ct2/show/NCT02672072 Did not report on the outcomes of Maslach Burnout inventory |
| Other bias | Low risk | No indication for other sources of bias. |
Emani 2020.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Chromotherapy‐based intervention
Control (no intervention)
Overall
Included criteria: inclusion criteria: interested in attending chromotherapy educational and consultation sessions at least three times per month for a period of 3 months, age range between 25 and 45 years Excluded criteria: exclusion criteria included existing comorbid clinical conditions that could have any effect on fatigue such as depression, thyroid disease or severe infection, surgery operation from three months ago, or participants who were suffering from malnutrition and iron deficiency anaemia, and participants who were unable for other reasons to continue their participation in this research. Pretreatment: there were no significant differences between the two groups for age, years of experience, or years working Compliance rate: of 96 nurses 80 participated in all sessions > 83% Response rate: NR Type of healthcare worker: nurses |
|
| Interventions |
Intervention characteristics Chromotherapy‐based intervention
Control (no intervention)
|
|
| Outcomes |
Professional Quality of Life (ProQol) ‐ Compassion satisfaction
Profesional Quality of Life (ProQol) ‐ Burn out
Professional Quality of Life (ProQOL) ‐ Secondary traumatic stress
|
|
| Identification |
Sponsorship source: NR Country: Iran Setting: Hospital Comments: NR Authors name: Roghiye Emani Institution: Nursing and Midwifery Faculty of Urmia University of Medical Sciences, Urmia, Iran; Email: haleh_ghavami@yahoo.co.uk Address: Nursing and Midwifery Faculty of Urmia University of Medical Sciences, Pardis–e‐Nazlou, 11 km of Nazlou Road, Urmia, Iran Time period: NR |
|
| Notes | PRO‐QOl_BO included in analysis 2.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A total of 96 ICU nurses assessed for eligibility; among them 80 nurses (according to inclusion and exclusion criteria of the study) were randomized to the experimental group or to the control group." "For randomization in this study, an independent researcher‐made random allocation cards using computer‐generated the random numbers. The allocator kept the original random allocation sequences in an inaccessible third place and worked with a copy. " |
| Allocation concealment (selection bias) | Low risk | Quote: "For randomization in this study, an independent researcher‐made random allocation cards using computer‐generated the random numbers. The allocator kept the original random allocation sequences in an inaccessible third place and worked with a copy." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Lost to follow‐up not reported. |
| Selective reporting (reporting bias) | Low risk | IRCT registration number: IRCT2017101431588N3. No indication of selective reporting. |
| Other bias | Unclear risk | Response rate not able to assess. Compliance not reported. |
Errazuriz 2022.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Mindfulness‐based stress reduction (MSBR)
Psychoeducational stress management (SMC)
Wait list
Overall
Included criteria: (i) non‐physician healthcare workers; (ii) aged ≥ 18 years; (iii) with a permanent work contract; and (iv) in direct contact with patients. Excluded criteria: participants were excluded if they reported suicidal ideation or problematic alcohol consumption at enrolment as measured in items 8 and 11 of the 45‐item Outcome Questionnaire Pretreatment: the three groups did not differ significantly in any of the collected baseline characteristics, except for levels of ’rewards’ at work and scores in the mindfulness ‘describing’ facet Compliance rate: NR Response rate: NR Type of healthcare worker: various healthcare workers |
|
| Interventions |
Intervention characteristics Mindfulness‐based stress reduction (MSBR)
Psychoeducational stress management (SMC)
Wait list
|
|
| Outcomes |
General Health Questionnaire (GHQ‐12)
45‐item Outcome Questionnaire (OQ‐45)
Perceived Stress Scale (PSS)
|
|
| Identification |
Sponsorship source: NR Country: Chile Setting: Mixed healthcare settings including: a tertiary hospital, a teaching hospital and an outpatient complex. Comments: NR Authors name: Antonia Errazuriz Institution: Department of Psychiatry, School of Medicine, Pontificia Universidad Catolica de Chile Email: anerrazuriz@uc.cl Address: School of Medicine, Pontificia Universidad Catolica de Chile, Diagonal Paraguay 362, Santiago, 8330077, Chile Time period: NR |
|
| Notes | We kindly received the mean and SD of the primary outcome from author A. Errazuriz. PSS included in analysis 1.1 and 1.2 and 2.1 and 2.2 and 5.1 and 5.2 and 6.1 and 6.2 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants were randomized into three groups (1:1:1 ratio) using computer‐generated random numbers, stratified by work position." |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Allocation was executed by ordering subjects according to the random number within strata and assigning the subjects within each stratum to groups 1, 2, and 3, consecutively, until exhausting the number of subjects within each stratum." Insufficient information to understand whether intervention allocations could have been foreseen in advance of, during, enrolment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 52 of the 105 (50%) randomised participants were included in the analysis. Reasons not provided. Not reported whether lost to follow‐up at random. |
| Selective reporting (reporting bias) | High risk | Trial registration: ISRCTN12039804. Did not report on Maslach Burnout Inventory and number of sick leaves in the previous three months |
| Other bias | Unclear risk | Compliance rate and response rate not reported. |
Ewers 2002.
| Study characteristics | ||
| Methods | RCT, UK | |
| Participants | 20 forensic mental health nurses | |
| Interventions | 1) Experimental: psychosocial Intervention Training: 20 days of training with the aim to improve nurses' knowledge about serious mental illness and attitude towards patients and thus decrease subjective burnout. Training duration 6 months. The training helps clinicians to conceptualise their patients' problems within a more empathic framework and trains them in the skills to intervene effectively. Thus, self‐efficacy may increase and jobs may be perceived as more rewarding. 2) Control: no intervention | |
| Outcomes | MBI directly after training | |
| Identification | ||
| Notes | MBI‐EE included in analysis 3.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The 20 staff who volunteered for the PSI training were randomly allocated to either the experimental PSI training group (n = 10) or a waiting list control group (n=10). The sample was stratified by ward, sex and day/night duty, thus subjects in each group represented all grades of staff and all wards." (p. 473) |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Presumably all participants completed all measurements as no data reported on dropouts. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Unclear risk | We did not find any indications of other sources of bias. |
Fendel 2021.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Mindfulness based program (MBP)
Control (no intervention)
Overall
Included criteria: Physicians younger than 45, with an ongoing position as a resident physician at base‐line, and minimum employment of 40% Excluded criteria: NR Pretreatment: at baseline, there were no statistically significant differences between groups with regard to demo‐graphics, meditation experience, distress and quality of care outcomes except for a difference in how attentive the resident physicians were, as judged by their colleagues Compliance rate: 198 eligible 147 participated in at least 50% of the intervention > 74% Response rate: 150 of the 181 eligible physicians participated (83%) Type of healthcare worker: resident physician |
|
| Interventions |
Intervention characteristics Mindfulness‐based program (MBP)
Control (no intervention)
|
|
| Outcomes |
Copenhagen Burnout Inventory (CBI)‐ burnout
Perceived Stress Scale (PSS)
General Health Questionnaire‐12 (GHQ‐12) Mental distress
Patient Health Questionnaire (PHQ4) ‐ depression
Patient Health Questionnaire (PHQ4) ‐ anxiety
|
|
| Identification |
Sponsorship source: NR Country: Germany Setting: University of Freiburg Comments: NR Authors name: Johannes Fendel Institution: Department of Occupational and Consumer Psychology, Institute of Psychology, University of Freiburg, Freiburg, Germany Email: NR Address: Department of Occupational and Consumer Psychology, Institute of Psychology, University of Freiburg, Freiburg, Germany Time period: 2018‐2020 |
|
| Notes | PSS included in analysis 1.1 and 1.2 PHQ included in analysis 1.4 and 1.5 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "email from the study team. We used minimisation to allocate participants into one of two groups using the software Qminim [64]. Through this approach, we minimised the imbalance between the groups with regard to gender (male, female) and baseline levels of personal burnout (CBI cut‐off values 0– 37.4 = low, 37.5–62.4 = medium, 62.5–100 = high burnout) [65]. We applied a weighted random". |
| Allocation concealment (selection bias) | Low risk | Quote: "A researcher with no contact with participants carried out minimisation and group assignment after the completion of baseline assessments." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "Due to the nature of the interventions, participants and trainers were aware of the allocated arm. To minimise bias, self‐report measures were administered online." |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | A low drop‐out rate of 18% at follow‐up for the primary outcome. 98% included in the intention to treat analysis. |
| Selective reporting (reporting bias) | Low risk | Trial registration DRKS00014015. No indication of selective reporting on stress/burnout assessment. |
| Other bias | Low risk | No indication of other sources of bias |
Finnema 2005.
| Study characteristics | ||
| Methods | RCT, the Netherlands | |
| Participants | 99 nursing assistants | |
| Interventions | 1) Experimental: Integrated emotion‐oriented care: Basic training course of two days with an intermediary period of two weeks for homework (for all staff members on intervention wards) addressing staff members' own experience, phases of ego‐experience of the demented residents and the application of (non‐)verbal empathic skills. Advanced course of seven days spread out over seven to eight months for five people from each intervention ward and an Adviser course of 10 days over nine months for one person from each intervention ward. 2) Control: Training and support in giving usual care |
|
| Outcomes | The Organization and Stress Scale | |
| Identification | ||
| Notes | OSS included in analysis 3.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "A pretest‐posttest control group design with matched groups (randomized clinical trial) was used" (p. 331) |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | "During the experimental period 25 nursing assistants dropped out due to: illness (11), pregnancy (2), and transfer (9). In three cases questionnaires were missing. Data analysis was carried out on 99 'complete' cases. Drop‐out did not differ between the groups..." (p. 333) |
| Selective reporting (reporting bias) | High risk | For nursing assistants results consist of covariance analyses that were not prespecified. |
| Other bias | Low risk | We did not identify any indications of other sources of bias. |
Fiol DeRoque 2021.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Mindfulness‐based mHealth intervention (PsyCovidApp Group)
Control (App) group
Overall
Included criteria: healthcare workers from any medical speciality (pneumology, internal medicine, emergency, primary care, etc) and role (physicians, nurses, nurse assistants, etc) with access to a smartphone. We included health care workers who had provided direct, face‐to‐face health care to patients with a diagnosis of infection with COVID‐19. Excluded criteria: healthcare workers who were not able to download and activate the app used to deliver the intervention during the next 10 days following the baseline assessment. Pretreatment: reported socio demographic baseline characteristics of participants randomised to the intervention group were similar to socio demographic baseline characteristics of participants randomised to the control group Compliance rate: 684 healthcare workers of which 482 participated in at least 50% of the intervention 482 > 74% Response rate: 482 of the 525 (92%) eligible participants participated Type of healthcare worker: various HCWs |
|
| Interventions |
Intervention characteristics Mindfulness‐based mHealth intervention (PsyCovidApp Group)
Control (App) group
|
|
| Outcomes |
DASS ‐ overall
Maslach Burnout Inventory ‐ Emotional exhaustion
Maslach Burnout Inventory ‐ Personal accomplishment
Maslach Burnout Inventory ‐ Depersonalisation
|
|
| Identification |
Sponsorship source: NR Country: Spain Setting: Hospital Comments: NR Authors name: Maria Antònia Fiol‐DeRoque Institution: Health Research Institute of the Balearic Islands, Palma de Mallorca, Spain Email: mariajesus.serranoripoll@ssib.es Address: Maria Jesús Serrano‐Ripoll, PhD Health Research Institute of the Balearic Islands Edificio S, Hospital Universitario Son Espases Carretera de Valldemossa Palma de Mallorca, 07120 Spain Time period: 2020 |
|
| Notes | MBI‐EE included in analysis 1.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants were randomly assigned (1:1) to receive the PsyCovidApp intervention or the control app over two weeks by a designated researcher" Using a computer‐generated sequence of random numbers create by Internet relay chat. |
| Allocation concealment (selection bias) | Low risk | Randomization done by a designated researcher who was not involved in data collection or analysis. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Health care workers were blinded to group allocation (as both groups received an app) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Participants, the outcome data collectors and trial statisticians were unaware of the treatment allocation." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Loss to follow‐up less than 20%. 436 of the 482 randomized participants had complete two‐week outcome data. |
| Selective reporting (reporting bias) | Low risk | https://clinicaltrials.gov/ct2/show/NCT04393818 No differences between study and registration of the protocol |
| Other bias | Low risk | No indication of other source of bias |
Foji 2020.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Emotional intelligence training
Control (no intervention)
Overall
Included criteria: NR Excluded criteria: people who have not already received any training on the topic of research. If a person has already been trained, the results of the study will be affected whether the score obtained from the study is present or not? Do not use anti‐anxiety and tranquilizers during the study period. Drug use could interfere with the outcome (due to sleepiness and lack of consciousness) (either at the training stage or the completion stage of the response). No night shift before the night before the tests. Fatigue caused by night shift could interfere with completing the questionnaire or understanding the training sessions. [4] To commit to attend all or more than half of the meetings. Pregnant nurses were excluded or nurses with underlying diseases (blood pressure, diabetes, etc.) were excluded. Pretreatment: NR Compliance rate: NR Response rate: NR Type of healthcare worker: exclusively nurses |
|
| Interventions |
Intervention characteristics Workplace Health Promotion Program
Control (no intervention)
|
|
| Outcomes |
General Health Questionnaire (GHQ)
|
|
| Identification |
Sponsorship source: NR Country: Iran Setting: Hospital Comments: NR Authors name: Dr. Razieh Khosrorad Institution: Department of Health Education, School of Health, Sabzevar University of Medical Sciences, Sabzevar, Iran. Educational Neuroscience Research Center, Sabzevar University of Medical Sciences, Sabzevar, Iran. Email: rkhosrorad@yahoo. com Address: NR Time period: NR |
|
| Notes | GHQ included in analysis 1.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Target population of this study consist of nurses in units of Mohammad Vasei, Shahid Beheshti, and Shahidan Mobini Hospitals in Sabzevar, randomly divided into two groups and a sample of 135 people were randomly selected based on the list of sample group names and random number table |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not reported |
| Selective reporting (reporting bias) | Unclear risk | Inaccessible plan number 94098 with the ethics code of IR.MEDSAB.REC.1394.51. No indication of selective reporting. |
| Other bias | Unclear risk | Response rate and compliance rate not reported. |
Frogeli 2020.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Engagement in proactive behaviours
Control (care as usual)
Overall
Included criteria: eligible participants were newly graduated nurses who worked at any clinical department of Uppsala University Hospital and participated in the transition‐to‐practice program Excluded criteria: NR Pretreatment: no group differences reported Type of healthcare worker: exclusively nurses Response rate: 86% Compliance rate: 95% |
|
| Interventions |
Intervention characteristics Engagement in proactive behaviours
Control (care as usual)
|
|
| Outcomes |
Items from the Stress and Energy Questionnaire
|
|
| Identification |
Sponsorship source: Funding: This study was supported by AFA insurance [Grant no 140007] Country: Sweden Setting: University hospital Comments: NR Authors name: Elin Frögéli Institution: Department of Clinical Neuroscience, Karolinska Institute Email: elin.frogeli@ki.se Address: NR Time period: 2016‐2017 |
|
| Notes | Included in analysis 1.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The participants were randomized to one of two groups of equal size at a 1:1 ratio, stratified by clinical ward. Specifically, person 1 that was registered for the program was allocated to group 1, person 2 was allocated to group 2, person 3 to group 3, and so on. However, if person 1 and person 3 came from the same clinical ward, person 3 was placed in group 2. Person 4 was then placed in group 1 and person 5 in group 2, and so on. The purpose of this design was to avoid having too many nurses from the same clinical ward being placed in the same study group, as this would cause problems of staffing on the clinical wards." Sequence generation process not mentioned. |
| Allocation concealment (selection bias) | High risk | Participants and/or investigators enroling participants could possibly foresee assignments and thus introduce selection bias. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "Finally, no measures were taken to assure that there was no diffusion of information between the groups, which may have affected the results." Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Quote: "Attrition Analysis: We investigated differences in the study variables at baseline between participants who responded at follow‐up and those who did not. These analyses revealed no differences." Randomized 239 ‐> lost to follow‐up ‐> 55 = 23% but no differences between responders and not responders. However, these analyses have not been reported. |
| Selective reporting (reporting bias) | Unclear risk | No mention of a protocol, nor did we find one |
| Other bias | Unclear risk | Quote: "The reliability of some of the measures in the present trial was questionable, which may have limited the ability to properly assess the outcomes." ‘Loosely’ validated outcome measure |
Ghawadra 2020.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Mindfulness‐based training
Control (no intervention)
Overall
Included criteria: nurses who work in wards who had mild to moderate levels of stress and depression (according to DASS‐21) in an earlier cross‐sectional survey. Excluded criteria: nurses who work in the outpatient clinic, or nursing managers, due to the different types of patient care, roles and responsibilities. Nurses who have a history of mental illness (n = 3) were excluded in the first study. The nurses who had severe and extremely severe levels of SAD (according to DASS‐21). They were advised to seek professional help at the psychiatric/psychology clinic in the hospital. Pretreatment: reported socio‐demographic baseline characteristics of participants randomised to the intervention group were similar to socio‐demographic baseline characteristics of participants randomized to the control group Compliance rate: the drop‐out rate was high, especially for the website intervention (48.3%). Response rate: it seems that all eligible participants actually participated Type of healthcare worker: nurses |
|
| Interventions |
Intervention characteristics Mindfulness‐based training
Control (no intervention)
|
|
| Outcomes |
DASS ‐ Depression
DASS ‐ Anxiety
DASS ‐ stress
|
|
| Identification |
Sponsorship source: NR Country: Malaysia Setting: Hospital Comments: NR Authors name: Sajed Faisal Ghawadra Institution: Department of Nursing Science, Faculty of Medicine, University of Malaya, Kuala Lumpur, Malaysi Email: katlim@um.edu.my Address: Khatijah Lim Abdullah, Department of Nursing Science, Faculty of Medicine, University of Malaya, 506030 Kuala Lumpur, Malaysia and Fakultas Keperawatan Universitas Airlangga, Surabaya, Indonesia Time period: NR |
|
| Notes | Not able to include in analysis due to missing data. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The participants were randomly assigned to the intervention and control groups using stratified blocked randomization." Sequence generation process insufficiently described. |
| Allocation concealment (selection bias) | Unclear risk | Unable to judge whether participants and/or investigators could possibly foresee assignment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 25 of the 249 (11%) participants were not analysed. Reasons provided. Not mentioned whether lost to follow‐up was at random however loss to follow‐up is below our pre‐defined cut‐off point. |
| Selective reporting (reporting bias) | Unclear risk | Trial registration, nor did we find one online |
| Other bias | Low risk | Low compliance but the per protocol analysis did not differ from the intention to treat analysis. Per‐protocol (PP) analysis was performed for (n = 136) participants who completed all the intervention (workshop and website), and for those who completed the three‐point questionnaires; the intervention and control group in PP analysis were n = 37 and 99, respectively. The results of the PP using GEE were similar to ITT, which strengthens the validity of the results |
Gollwitzer 2018.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline Characteristics Mental contrasting with implementation intentions‐ MCII
Mental contrasting with implementation intentions + further intervention groups ‐ IIMCII
Control
Overall
Included criteria: NR Excluded criteria: NR Pretreatment: There were no significant differences between the two groups for age, years of experience, or years working Compliance rate: NR Response rate: of 251 eligible participants 129 participated > 51% Type of healthcare worker: various healthcare workers |
|
| Interventions |
Intervention characteristics Mental contrasting with implementation intentions ‐ MCII
Mental contrasting with implementation intentions + further intervention groups ‐ IIMCII
Control (no intervention)
|
|
| Outcomes |
Perceived Stress Questionnaire‐ 20‐ PSQ‐20
|
|
| Identification |
Sponsorship source: NR Country: Germany Setting: Various health institutions Comments: NR Authors name: Peter M Gollwitzer Institution: Department of Psychology, New York University, New York, NY, United States Email: gabriele.oettingen@nyu.edu Address: NR Time period: NR |
|
| Notes | PSQ included in analysis 1.1. Intervention groups combined to create a single pair‐wise comparison | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The message also contained the email address of the experimenter whom the nurses should contact if they wanted to register for the study. Those who registered (N = 251 nurses) were contacted in return by the experimenter (again via email) and given access to the study website that had been created by using the soscisurvey.de data collection service. Participants who entered the website (N = 129) were randomly assigned to the three conditions of the study (MCII = 41, and IIMCII = 41, Control = 47)" |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 105 of the 129 (81%) randomized participants answered the final questionnaire. Reasons not provided nor whether missing was at random. |
| Selective reporting (reporting bias) | Unclear risk | No registration, nor did we find one. |
| Other bias | Unclear risk | Data on participants' adherence to the MCII instructions and the frequency and context of participants using MCII is not described. |
Grabbe 2020.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Community Resiliency Model
Control (Nutrition)
Overall
Included criteria: NR Excluded criteria: NR Pretreatment: no significant differences were noted between the two randomised groups by age, years in nursing, or on any of the base‐line measures. Compliance rate: 59 of the 99 (60%) participants allocated to the intervention group did not receive the intervention Response rate: of the 1600 invited nurses, 196 completed baseline and were randomised (12%) Type of healthcare worker: nurses |
|
| Interventions |
Intervention characteristics Community Resiliency Model
Control (Nutrition)
|
|
| Outcomes |
Secondary traumatic stress (STSS)
Copenhagen Burnout Inventory (CBI)
|
|
| Identification |
Sponsorship source: NR Country: USA Setting: Hospital Comments: NR Authors name: Linda Grabbe Institution: Nell Hodgson Woodruff School of Nursing, Emory University, Atlanta, GA Email: lgrabbe@emory.edu Address: Corresponding author: Linda Grabbe, Nell Hodgson Woodruff School of Nursing, Emory University, 1520 Clifton Rd, Atlanta, GA30322 Time period: 2017‐2018 |
|
| Notes | CBI included in analysis 1.1 and 1.2 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "These participants were then randomly placed in either the intervention or control group. The" |
| Allocation concealment (selection bias) | Unclear risk | Difficult to judge whether participants and/or investigators could possible foresee assignment. However, it is assumed that randomization was performed in one go and that participants and/or investigators could not foresee assignment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Not reported whether lost to follow‐up was at random. 40% lost. |
| Selective reporting (reporting bias) | Unclear risk | No protocol registration, nor did we find one. |
| Other bias | Unclear risk | Low response and compliance rate. |
Gunasingam 2015.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline Characteristics Debriefing intervention
Control (no intervention)
Overall
Included criteria: the sample of interns invited to participate were those who were based at the teaching hospital during term 3 of 2011 Excluded criteria: interns who were seconded to other hospitals were excluded Pretreatment: reported socio‐demographic baseline characteristics of participants randomised to the intervention group were similar to socio‐demographic baseline characteristics of participants randomised to the control group. Compliance rate: attendance at the debriefing sessions was not always 100%, leading to the potential argument that those who were regularly in attendance were experiencing more or less stress. Response rate: 31 of 52 invited interns entered this study (60%). Type of healthcare worker: physicians |
|
| Interventions |
Intervention characteristics Debriefing intervention
Control (no intervention)
|
|
| Outcomes |
Maslach Burnout Inventory ‐ Emotional Exhaustion
Maslach Burnout Inventory ‐ Cynicism
Maslach Burnout Inventory ‐ Professional efficacy
|
|
| Identification |
Sponsorship source: NR Country: Australia Setting: Hospital Comments: NR Authors name: Nishmi Gunasingam Institution: Royal Prince Alfred Hospital, Camperdown, New South Wales, Australia Email: nishmi@gmail.com Address: Dr Nishmi Gunasingam, Medical Training andAdministration Unit, RoyalPrince Alfred Hospital, Missenden Road, Camperdown, NSW 2050 Time period: 2011 |
|
| Notes | MBI‐EE included in analysis 1.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants were allocated a unique identifying number to maintain anonymity. A computer generated randomisation code" |
| Allocation concealment (selection bias) | Unclear risk | Quote: "allocated participants to the debriefing intervention or control group." Difficult to judge whether participants and/or investigators could possible foresee assignment. However, it is assumed that randomization was performed in one go and that participants and/or investigators could not foresee assignment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | No trial registration or no study protocol reported, nor did we find one online |
| Other bias | Unclear risk | Difficult to assess compliance rate ‐> Attendance at the debriefing sessions was not always 100%, leading to the potential argument that those who were regularly in attendance were experiencing more or less stress. |
Gärtner 2013.
| Study characteristics | ||
| Methods | Cluster‐RCT, the Netherlands | |
| Participants | Nurses on wards of an academic hospital were screened for work and health problems: Experimental: 29 wards, 591 participants of which 151 screened positive. Control: 28 wards, 561 participants of which 161 screened positive. Experimental: 17%, Control 22% men, > 45 years age ‐ Experimental 51% Control 46%, > 10 years of experience ‐ Experimental 51% Control 41% | |
| Interventions | 1) Experimental 1: all who screened positive were referred to Occupational Health Physician (OHP). Participants who were screened as positive were invited for a face‐to‐face preventive consultation with their occupational physician. The consultation was voluntary, and workers could reschedule or cancel it if they wished. Supervisors were not informed about the screening results or about the invitation for and content of the preventive consultation of any employee. The 7‐step protocol for OHPs closely followed occupational physicians’ care as usual for consultations initiated by the employee in contrast to the compulsory consultation in the context of absenteeism. Occupational physicians received 3 hours of training from the researchers on the use of the protocol. (CBT) 2) Experimental 2: participants received personalised feedback on their screening results immediately after filling out the baseline questionnaire, both onscreen and in an e‐mail. The personalised feedback was followed by an invitation for a tailored offer of self‐help EMH interventions, on the basis of an algorithm based on the specific symptoms and the work‐relatedness of the symptoms. participants were mostly offered a choice of 2 to 3 EMH interventions to leave room for personal preferences. Participants who screened negative on all mental health complaints were invited to follow an EMH intervention aimed at enhancing and retaining their mental fitness. The EMH interventions are self‐help interventions on the Internet aimed at reducing specific mental health complaints or enhancing well‐being. The interventions are mainly based on the principles of cognitive behavioural therapy and combine a variety of aspects, e.g. providing information and advice, weekly assignments, the option of keeping a diary and a forum to get in contact with others who have similar complaints. The EMH interventions were developed as stand‐alone interventions by the Trimbos Institute (CBT). 2) Control: waiting list: In the control arm. Participants filled out the baseline questionnaire; however, results of the screening‐questionnaires were not to be reported back to participants, and no further interventions were advised at baseline. As compensation, participants in the control arm received their personal screening results together with a tailored choice for a self‐help EMH intervention six months after baseline. |
|
| Outcomes | Gartner 2013: the study's primary outcome was help‐seeking behaviour; we used secondary outcomes: distress from the Dutch 4DKL, anxiety and depression from Brief Symptom Inventory Ketelaar 2013: the study used work‐functioning as the primary outcome: we used the distress part of the Dutch 4DKL as stress outcome; anxiety and depression were also measured but not reported Bolier 2014: Brief Symptom Inventory (BSI) ‐ Anxiety and Brief Symptom Inventory (BSI) ‐ depression Noben 2014: cost‐effectiveness |
|
| Identification | ||
| Notes | We got the following data for the distress scale of the 4DKL at 6 months follow‐up for the group who screened positive from author K Nieuwenhuijsen: Experimental: N = 86 6.24 ± 6.52 Control: N = 116 6.82 ± 6.57 We got the following data from author S. Ketelaar: Distress measure with 4DKL at 6 months follow‐up for the group who screened positive: Experimental: N = 52 6.06 ± 6.54; Control: N = 116 6.82 ± 6.5.7 4DKL included in analysis 1.2 Intervention groups combined to create a single pair‐wise comparison. BSI‐depression included in analysis 1.4 Experimental 2 vs control 4DKL included in analysis 5.2 Experimental 1 vs Experimental 2 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | " Randomization was performed at the ward level (n = 86). Randomization sequences with a block size of three were generated with Nquery Advisor (Statistical Solutions, Ltd, Cork, Ireland) by one researcher (K.N.) who was not involved in the recruitment" |
| Allocation concealment (selection bias) | Unclear risk | Not blinded |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | At 3 months lost to follow‐up: Experimental 37% / Control 30%; at 6 months Experimental 46% / Control 34% |
| Selective reporting (reporting bias) | Low risk | Gartner 2013: All outcomes reported that were announced in protocol Ketelaar 2013: Anxiety and Depression were not reported in Ketelaar 2013 but in Bolier 2014 |
| Other bias | Unclear risk | Compliance very low: 34% of those invited visited their OHP |
Günüsen 2010.
| Study characteristics | ||
| Methods | RCT, Turkey | |
| Participants | Quote: "All of the nurses (n = 227) were invited to complete the Maslach Burnout Inventory (MBI) developed by Maslach & Jackson (1981). Those who completed the questionnaire and received a score on emotional exhaustion higher than the median score for all nurses were invited to participate in the burnout reduction intervention." (p. 487) 108 nurses were randomised to one of three conditions. | |
| Interventions | 1) Coping training (N = 36) Quote: "The group that received coping training consisted of two groups, each group consisting of 18 people. In the first week, the concept of stress was explained to the nurses, and coping methods used by the nurses in stressful conditions were discussed. In the second session, basic communication skills on the stress level were discussed. In the third session, cognitive coping methods were presented theoretically. In the fourth session, cognitive distortions found among nurses and methods for coping with these distortions were discussed. In the fifth session, the problem‐solving method was theoretically explained to the nurses. In the sixth session, stressful situations that the nurses encountered were discussed and resolved by means of the problem‐solving method. In the seventh session, problems that the nurses had difficulty coping with were discussed by utilizing the skills learnt during the course of the programme." (p. 488) 2) Support group (N = 36) "...the support group consisted of three groups, each group consisting of 12 people. The nurses talked about the most frequently encountered stressors in the workplace and expressed their feelings towards their jobs. At the beginning of each session, the nurses expressed their feelings related to difficult situations at the workplace. Then, a problem chosen by the nurses was attempted to be solved by using reflective cycle steps. Researchers provided information when needed. Possible solution methods were discussed in the groups, and the nurses were advised to use these methods in their daily lives. The nurses shared their difficult and favourable times and also exchanged recommendations with each other." (p. 488) 3) Control: No intervention (N = 36) | |
| Outcomes | MBI | |
| Identification | ||
| Notes | MBI‐EE included in analysis 1.1 and 1.2. Intervention groups combined to create a single pair‐wise comparison. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Random allocation was concealed by using a system of sequentially numbered, opaque, sealed envelopes containing the computer‐generated random allocation, which had been drawn up by a statistician. During the randomization, the researchers and the participants did not know the groups to which they would be allocated." (p. 487) |
| Allocation concealment (selection bias) | Low risk | See above |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | "No blinding was applied to the participants and the researchers." (p. 487) |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "Intention‐to‐treat analysis was used because of sample loss." (p. 487) |
| Selective reporting (reporting bias) | Low risk | The authors only measured and adequately reported results of the MBI. |
| Other bias | Unclear risk | We did not find any indications of other sources of bias. |
Hersch 2016.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline Characteristics Web‐based BREATHE
Control (no intervention)
Overall
Included criteria: Nurses had to be 21 years of age or older and work at one of the participating hospitals Excluded criteria: NR Pretreatment: reported socio‐demographic baseline characteristics of participants randomised to the intervention group were similar to socio‐demographic baseline characteristics of participants randomised to the control group. Compliance rate: the majority of program group participants logged into the program 1 to 3 times. Ten participants in the experimental group never logged into the program. The average number of logins for those who logged in at least once was 2.5. The average amount of time spent in the BREATHE program was 43 minutes. Response rate: of 117 eligible participants 105 participated > 88% Type of healthcare worker: nurses |
|
| Interventions |
Intervention characteristics Web‐based BREATHE
Control (no intervention)
|
|
| Outcomes |
Nursing Stress Scale
Symptoms of distress
|
|
| Identification |
Sponsorship source: NR Country: USA Setting: Hospital Comments: NR Authors name: Rebekah K. Hersch Institution: ISA Associates, Inc. Email: rhersch@isagroup.com Address: SA Associates, Inc., 201 North Union Street, Suite 330, Alexandria, Virginia Time period: NR |
|
| Notes | Symptoms of distress included in analysis 4.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was conducted using a block randomized design with blocks of 4 and 6. The 0 and 1 within each block were random and the order of the group of 4 and the group of 6 was random. Randomization occurred after each participant completed the pretest question‐ naire. The online questionnaire site was checked every day to determine who completed the pretest each day and individuals were assigned to the next condition on the randomization table as they completed the questionnaire." |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Once randomization was complete, participants were notified of the condition to which they were assigned (no blinding procedures were employed) and were informed of next steps; experimental group participants were sent a link to the BREATHE program along with a randomly generated username and password and instructions for using the program." Insufficient information to understand whether intervention allocations could have been foreseen in advance of, during, enrolment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 14 of the 104 randomised participants were lost to follow‐up (1 control group vs 13 intervention group). Missing data were imputated. Missing not at random. We found that the following participants were less likely to respond to the posttest measure: those who reported greater number of days in which they had five or more drinks on the same occasion at pretest, those who reported more drinks per day at pretest, and those who had lower scores on the understanding of depression and anxiety measure at pretest |
| Selective reporting (reporting bias) | Unclear risk | No trial registration or no study protocol reported, nor did we find one online |
| Other bias | Low risk | No indication of other sources of bias |
Hilcove 2021.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: Parallel group |
|
| Participants |
Baseline characteristics Mindfulness‐based Yoga
Control (no intervention)
Overall
Included criteria: employees who provided direct patient care (including but not limited to nurses, nursing assistants, therapists, physicians, and social workers), older than 18 years. Excluded criteria: the presence of joint or muscle problems that limited mobility (e.g. advanced arthritis, herniated disk, or past injuries that prevent painless or safe movement), having routinely practised yoga or any other MB intervention in the past 6 months, or currently on medication that might interact with the results of salivary cortisol measures, including prednisone, cortisone, or steroid‐based medicine. Pretreatment: reported socio‐demographic baseline characteristics of participants randomised to the intervention group were similar to socio‐demographic baseline characteristics of participants randomised to the control group. Compliance rate: there was 98.7% attendance across all sessions for those in the MB yoga intervention group. Response rate: NR Type of healthcare worker: Nurses & other healthcare professionals |
|
| Interventions |
Intervention characteristics Mindfulness‐based Yoga
Control (no intervention)
|
|
| Outcomes |
Maslach Burnout Inventory ‐ Emotional Exhaustion
The Perceived Stress Scale (PSS)
|
|
| Identification |
Sponsorship source: NR Country: USA Setting: Hospital Comments: NR Authors name: Kelly Hilcove Institution: Honor Health Scottsdale Shea Medical Center Email: Kelly@KellyHilcove.com Address: BSN, RN, HNB‐BC, Board Certified Holistic Nurse, Honor Health Scottsdale Shea Medical Center, 9003 East Shea Boulevard, Scottsdale, AZ 85261, Time period: NR |
|
| Notes | PSS included in analysis 2.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Once identified as eligible, participants signed consent, completed subjective assessments, and were randomly assigned to the intervention or control group using a computerized randomization tool." |
| Allocation concealment (selection bias) | Unclear risk | Difficult to judge whether participants and/or investigators could possibly foresee assignment. However, it is assumed that randomization was performed in one go and that participants and/or investigators could not foresee the assignment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Two members of the control group were not able to participate in collection of post‐intervention data, due to personal time constraints, yielding an attrition rate of 2.5%." |
| Selective reporting (reporting bias) | Unclear risk | No trial registration or no study protocol reported, nor did we fine one online |
| Other bias | Unclear risk | Response rate not reported. |
Ho 2021.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Mindful‐Compassion Art‐based Therapy (MCAT)
Waitlist‐control
Overall
Included criteria: inclusion criteria included healthcare workers (i.e. physicians, nurse, medical social workers, and allied health professionals) whose primary job was caring for terminally ill patients, 21 years old and above, and fluent in both written and spoken English Excluded criteria: exclusion criteria included the inability to provide informed consent or major depression (or other mental health conditions) or both. Pretreatment: reported socio‐demographic baseline characteristics of participants randomised to the intervention group were similar to socio‐demographic baseline characteristics of participants randomised to the control group. Compliance rate: NR Response rate: NR Type of healthcare worker: physicians, nurse, medical social workers, and allied health professionals |
|
| Interventions |
Intervention characteristics Mindful‐Compassion Art‐based Therapy (MCAT)
Waitlist‐control
|
|
| Outcomes |
Maslach Burnout inventory general survey‐ burn‐out
Maslach Burnout inventory general survey‐ exhaustion
Maslach Burnout Inventory ‐ cynicism
Maslach Burnout Inventory ‐ professional efficacy
|
|
| Identification |
Sponsorship source: NR Country: Singapore Setting: Hospice Comments: NR Authors name: Andy Hau Yan Ho Institution: Action Research for Community Health Laboratory, Psychology Programme, School of Social Sciences, Nanyang Technological University, Singapore, Singapore Email: andyhyho@ntu.edu.sg Address: NR Time period: NR |
|
| Notes | MBI‐EE included in analysis 2.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Simple randomization for each recruitment round was conducted by using an allocation sequence based on a computer‐generated list of random numbers. Specifically, a random number sequence ranging from 1 to 18 or 20 (depending on the number of participants recruited in each recruitment round) was generated via Research Randomizer (Urbaniak and Plous, 2019). Thereafter, each participant was randomly assigned a unique number from the sequence. |
| Allocation concealment (selection bias) | Unclear risk | See above. Difficult to judge whether participants and/or investigators could possibly foresee assignment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No attrition throughout the entire research period. |
| Selective reporting (reporting bias) | Low risk | Trial registration NCT03440606. No indication of selective outcome reporting. |
| Other bias | Unclear risk | Response rate and compliance rate not reported. |
Huang 2020.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Balint group intervention
Control (no intervention)
Overall
Included criteria: The inclusion criteria encompassed (1) working in an ICU a licensed nurse for at least one year and working in hospitals with at least 1000 beds and 100 ICU nurses. Excluded criteria: the exclusion criteria were: (1) Participants who have neuropsychiatric disorders; (2) Participants in pregnancy or lactation; (3) Participants who incomplete or invalid questionnaire. Pretreatment: reported socio‐demographic baseline characteristics of participants randomised to the intervention group were similar to socio‐demographic baseline characteristics of participants randomised to the control group. Compliance rate: 100% Response rate: 100% Type of healthcare worker: nurses |
|
| Interventions |
Intervention characteristics Balint group intervention
Control (no intervention)
|
|
| Outcomes |
Maslach Burnout Inventory ‐ Emotional Exhaustion
Maslach Burnout Inventory ‐ Depersonalisation
Maslach Burnout Inventory ‐ Personal accomplishment
|
|
| Identification |
Sponsorship source: NR Country: China Setting: Hospital Comments: NR Authors name: Huigen Huang Institution: Guangdong Provincial People’s Hospital, Guangdong Academy of Medical Sciences, Guangzhou, Guangdong, China Email: gdpphhuanghuigen@163.com Address: No. 102 Zhongshan Er Road, Guangdong Provincial People’s Hospital, Guangdong Academy of Medical Sciences, Guangzhou, Guangdong, 510080, China. Time period: 2016 |
|
| Notes | MBI‐EE included in analysis 1.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "under the leadership of Guangdong General Hospital from May 2016 to November 2016. The participants were selected through random sampling first, then they were divided into two groups (i.e. the intervention group and the control group) with a random number generator." |
| Allocation concealment (selection bias) | Unclear risk | Then they were divided into two groups (i.e. the intervention group and the control group) with a random number generator Insufficient information to understand whether intervention allocations could have been foreseen in advance of, during, enrolment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 6 of the 152 randomised participants withdrew (4%). Reasons provided. Missing not at random however loss to follow‐up is below our pre‐defined cut‐off point. |
| Selective reporting (reporting bias) | Unclear risk | No trial registration or no study protocol reported, nor did we find one online. |
| Other bias | Low risk | No indication of other sources of bias |
Huang 2020a.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Balint intervention
Wait‐list control group
Overall
Included criteria: NR Excluded criteria: NR Pretreatment: there were no significant differences between the two groups for age and gender Compliance rate: 100% Response rate: all residents invited voluntarily participated (100% response rate). Type of healthcare worker: residents |
|
| Interventions |
Intervention characteristics Balint intervention
Wait‐list control group
|
|
| Outcomes |
Maslach Burnout Inventory human services survey ‐ Emotional Exhaustion
Maslach Burnout Inventory human services survey ‐ Depersonalisation
Maslach Burnout Inventory human services survey ‐ Personal accomplishment
|
|
| Identification |
Sponsorship source: NR Country: China Setting: Hospital Comments: NR Authors name: Lei Huang Institution: Department of Psychiatry, Tongji Hospital, Tongji University School of Medicine, Shanghai, China, Medical Education Division, Tongji Hospital, Tongji University School of Medicine, Shanghai, China Email: wuwy@tongji.edu.cn Address: NR Time period: 2016 |
|
| Notes | MBI‐EE Included in analysis 1.2 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Following consent and the completion of the first round of assessment completion, the 36 residents were randomly assigned to the intervention (n = 18) or the control group (n = 18)." Sequence generation process insufficiently described |
| Allocation concealment (selection bias) | Unclear risk | Difficult to judge whether participants and/or investigators could possible foresee assignment. However, it is assumed that randomization was performed in one go and that participants and/or investigators could not foresee assignment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up. |
| Selective reporting (reporting bias) | Low risk | No trial registration or no study protocol reported. No indication of selective reporting. |
| Other bias | Low risk | No indication of other sources of bias reported. |
Janzarik 2022.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Intervention (resilience)
Control (no intervention)
Overall
Included criteria: NR Excluded criteria: NR Pretreatment: there were no significant differences between intervention and control group regarding age, gender, marital status, weekly working hours, and stressor load before the intervention. Compliance rate: NR Response rate: NR Type of healthcare worker: nurses |
|
| Interventions |
Intervention characteristics Intervention (resilience)
Control (no intervention)
|
|
| Outcomes |
General Health Questionnaire‐28‐ (GHQ‐28)
Mainz Inventory of Microstressors (MIMI)
Perceived Stress Scale (PSS)
|
|
| Identification |
Sponsorship source: NR Country: Germany Setting: Hospital Comments: NR Authors name: Gesche Janzarik Institution: Leibniz Institute for Resilience Research Email: pt.janzarik@gmail.com Address: Leibniz Institute for Resilience Research (LIR) Mainz, 55122 Mainz, Germany Time period: NR |
|
| Notes | PSS included in analysis 4.1 and 4.2 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "This randomised controlled trial included three assessment points: pre‐test, post‐test, and three follow‐up measurements at three, six, and nine months." Not reported how randomisation took place (e.g. software) |
| Allocation concealment (selection bias) | Unclear risk | Difficult to judge whether participants and/or investigators could possible foresee assignment. However, it is assumed that randomization was performed in one go and that participants and/or investigators could not foresee assignment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 58 of the 72 (80%) randomised participants responded to the latest follow‐up time included in this review. Reasons provided. Not mentioned whether missing was at random. |
| Selective reporting (reporting bias) | Unclear risk | No trial registration or no study protocol reported, nor did we find one online. |
| Other bias | Unclear risk | Compliance rate and response rate not reported. |
Jensen 2006.
| Study characteristics | ||
| Methods | Cluster‐RCT, Denmark | |
| Participants | 210 eldercare workers | |
| Interventions | 1) Experimental 1: Stress Management Intervention: The SMI was developed to address the work stress in health care with particular attention to prevention of burnout and development of strategies for stress management. Training occurred over 20 weeks, with group sessions every 2 weeks, and each session lasting 2 hours. Between sessions, the participants were given assignments concerning implementation of the programme in daily practice. 2) Experimental 2: Transfer Technique Intervention: The TTI was based on the Stockholm training concept, which aims to reduce the biomechanical load on the back, minimise work in asymmetric postures, and prevent sudden unexpected loads. Training in the TTI arm was a combination of practical classroom education (24 hours for each worker) and instruction at the work site. There were 11 instructors who belonged to the 7 groups in the TTI arm, with 1 to 2 persons in each group who received 30 hours of education during the initial phase of the study. 3) Control: Reference Programme consisting of lessons of the participants' own choice in matters unrelated to the intervention programmes but of the same duration as the active intervention lessons (e.g. on skin care, proper treatment of a person with diabetes, etc.) | |
| Outcomes | MBI (results not reported in article but obtained directly from author) |
|
| Identification | MBI‐EE included in analysis 1.2 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Randomization was performed at group level because the intervention programs were meant to involve the employee as a group during education and implementation. The assignment to the different intervention programs was balanced to secure representation of all 3 programs in each of the wards." (p.1762) |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "Altogether, 163 members of the source population (79%) participated in both baseline and follow‐up investigation, and completed at least 2 sets of diaries during the study period. The proportion of dropouts from baseline to follow‐up did not differ significantly across intervention groups. We observed no differences in age and number of years occupied in health care and mean intensity of LBP during the past year between participants who remained in the study and participants who dropped out." (p.1762). |
| Selective reporting (reporting bias) | High risk | Results data for the MBI, Setterlind's Stress Scores and rating of social support were not reported because they were not statistically significantly different between groups. "...[N]o significant changes were found in either of the intervention arms in ... the Maslach Burnout Inventory, the Setterlind stress scores, or the rating of social support (data not shown)" (p. 1765) |
| Other bias | Low risk | We did not find any indications of other sources of bias. |
Kavurmaci 2022.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Yoga
Control (no intervention)
Overall
Included criteria: not participating in yoga and similar regular exercise program during the research, not having any health problems that will prevent yoga, to agree to participate in the study. Excluded criteria: NR Pretreatment: reported sociodemographic baseline characteristics of participants randomised to the intervention group were similar to sociodemographic baseline characteristics of participants randomised to the control group. Compliance rate: two of the 35 participants in the experimental group excluded from the study because they did not regularly participate in yoga practice. Response rate: Of 80 participants 67 participated > 84% Type of healthcare worker: nurses |
|
| Interventions |
Intervention characteristics Yoga
Control (no intervention)
|
|
| Outcomes |
Maslach Burnout Inventory ‐ Emotional Exhaustion
Maslach Burnout Inventory ‐ Depersonalisation
Maslach Burnout Inventory ‐ Personal accomplishment
|
|
| Identification |
Sponsorship source: NR Country: Turkey Setting: Nursing faculty Comments: NR Authors name: Mehtap Kavurmaci Institution: Department of Internal Medicine Nursing, Atatürk University, Erzurum, Turkey Email: m.curcani@hotmail.com Address: Mehtap Kavurmaci, PhD, Department of InternalMedicine Nursing, Atatürk University, Erzurum25080, Turkey Time period: 2019 |
|
| Notes | MBI‐EE included in analysis 2.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The individuals were selected for the sample by the probability sampling method of simple random sampling. These individuals were listed for the simple random sampling method, and it was select 70 individuals from the table of random numbers including 35 in the experiment group and 35 in the control group." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to understand whether intervention allocations could have been foreseen in advance of, during, enrolment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Two of the participants in the experimental group were excluded from the study because they did not regularly participate in yoga practice. One of the participants in the control group was excluded from the study because he did not complete his final test. Unknown whether non‐completers differed from completers however loss to follow‐up is below our pre‐defined cut‐off point. |
| Selective reporting (reporting bias) | Unclear risk | No trial registration or no study protocol reported, nor did we find one online. |
| Other bias | Low risk | No indication of other sources of bias. |
Kesselheim 2020.
| Study characteristics | ||
| Methods |
Study design: cluster‐randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Novel training (intervention group)
Usual training (control group)
Overall
Included criteria: NR Excluded criteria: NR Pretreatment: there were no significant differences between the UT and intervention arms with respect to age, gender, or additional professional degrees. At baseline, pretest data reveal that UT and intervention groups did not differ significantly in their scores on the PHOSAH, MBI, PPOS, or Empowerment at Work Scale (Table 2). Mean scores on the PHOSAH, the primary outcome measure, were 7.4 (SD 4.2) for fellows in the UT group and 8.2 (SD 3.3) for the intervention group (P = 0.35). However, baseline performance on the PHOSAH was somewhat lower than previously published, with mean score of 9 (SD 3.4) .15 Fellows in both groups had similar levels of satisfaction with their fellowship training in several domains of humanism and professionalism (Table 3). Compliance rate: NR Response rate: NR Type of healthcare worker: paediatric haematology‐oncology fellows |
|
| Interventions |
Intervention characteristics Novel training (intervention group)
Usual training (control group)
|
|
| Outcomes |
Maslach Burnout Inventory ‐ Emotional Exhaustion
Maslach Burnout Inventory ‐ Depersonalisation
Maslach Burnout Inventory ‐ Personal accomplishment (lack of)
|
|
| Identification |
Sponsorship source: NR Country: USA Setting: Hospital Comments: NR Authors name: Jennifer Kesselheim Institution: Department of Pediatric Oncology, Dana‐Farber/Boston Children’s Cancer and Blood Disorders Center, Boston, Massachusettes Email: Jennifer_kesselheim@dfci.harvard.edu Address: Jennifer Kesselheim, Dana‐Farber/Boston Children’s Cancer and Blood Disorders Center, Boston, Massachusettes 450 Brookline Avenue, D1107, Boston, MA02215 Time period: 2016‐2017 |
|
| Notes | MBI‐EE included in analysis 1.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: Program directors committed to study participation sought local approval from their Institutional Review Board after which their program was randomized to either the intervention or UT arm of the study. Sequence generation process insufficiently described. |
| Allocation concealment (selection bias) | Unclear risk | Unable to judge whether participants and/or investigators could possible foresee assignment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 89 of the 100 randomised participants included in the analysis (89%). Reasons not described nor whether missing was at random. However loss to follow‐up is below our pre‐defined cut‐off point. |
| Selective reporting (reporting bias) | Unclear risk | No trial registration or no study protocol reported, nor did we fine one online |
| Other bias | Unclear risk | Unit of analysis error (i.e. when a study ignored the clustering of the data in their analysis). Compliance not reported. |
Kharatzadeh 2020.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Emotion regulation training
Control (no intervention)
Overall
Included criteria: employment in intensive or critical care units, no previous participation in an ERT program and not currently taking psychotropic medication or other unprescribed substances. Excluded criteria: NR Pretreatment: at baseline, an independent sample t‐test showed no significant difference between the two groups in terms of age and working hours per month. The two groups also did not differ in sex, nor marital status. There were no between‐group differences in CERQ, DASS‐21, and ProQoL‐5 subscale scores at baseline. The statistical analysis controlled for baseline scores for CERQ, DASS‐21 and ProQoL‐5 scores as confounders. Compliance rate: four of the 30 (13%) participants randomised to the intervention group missed more than 2 sessions Response rate: nine of the 71 (13%) eligible participants did not want to participate Type of healthcare worker: nurses |
|
| Interventions |
Intervention characteristics Emotion regulation training
Control (no intervention)
|
|
| Outcomes |
Professional Quality of Life (ProQol) ‐ Burn out
DASS ‐ depression
DASS ‐ Anxiety
DASS‐ Stress
|
|
| Identification |
Sponsorship source: NR Country: Iran Setting: Hospital Comments: NR Authors name: Hamid Kharatzadeh BSc, MSc, PhD Candidate Institution: Department of Clinical Psychology, Faculty ofHuman Sciences, Shahed University, Tehran, Iran Email: m_alavi@nm.mui.ac.ir Address: Mousa Alavi, Nursing and Midwifery CareResearch Center, Faculty of Nursing andMidwifery, Isfahan University of MedicalSciences, Isfahan, Iran Time period: 2018‐2019 |
|
| Notes | DASS‐stress included in analysis 1.1 DASS ‐ depression included in analysis 1.4 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "randomly allocated to either the treatment group" Using a computer‐based randomization allocation |
| Allocation concealment (selection bias) | Unclear risk | Quote: "using a computer‐based randomiza‐ tion allocation (refer to the study CONSORT diagram, Figure 1)." Insufficient information to understand whether intervention allocations could have been foreseen in advance of, during, enrolment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Follow‐up lost less then 20% (53 of the 60 randomised participants included in the analysis). |
| Selective reporting (reporting bias) | Low risk | IRCT20171005036572N3. No indication of selective outcome reporting |
| Other bias | Low risk | No indication of other sources of bias |
Kim 2016.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline Characteristics Repetitive transcranial magnetic stimulation (rTMS)
Control (placebo)
Overall
Included criteria: NR Excluded criteria: individuals with 1) past or current diagnosis of any axis I psychiatric disorder based on the Structured Clinical Interview for DSM‐IV‐TR Axis I Disorders, Patient Edition (SCID‐I/P),19 2) severe medical illness, 3) organic mental disorder, seizure disorder, or mental retardation, 4) pregnancy, 5) current psychotropic medication use, 6) surgical treatment of intracranial lesions, or 7) a magnetic substance in their brain or orbital area. Pretreatment: at baseline, there were no significant differences between the intervention group and the control group with regard to age, duration of employment, working hours per week, marital status, occupation, socio‐economic status, all Compliance rate: among the 28 enroled participants, data from four participants were dropped because they did not complete the TMS sessions or QEEG assessment: one participant from the active‐TMS group and one participant from the sham‐TMS group discontinued the TMS sessions due to headache and one participant from the active‐TMS group and one participant from the sham‐TMS group missed their QEEG appointments without giving notification. Ultimately, 24 participants completed all TMS sessions and QEEG assessments Response rate: NR Type of healthcare worker: various HCWs |
|
| Interventions |
Intervention characteristics Repetitive transcranial magnetic stimulation (rTMS)
Control (sham TMS)
|
|
| Outcomes |
Psychological strain
Beck’s depression inventory
Beck’s anxiety inventory
|
|
| Identification |
Sponsorship source: NR Country: South‐Korea Setting: Hospital Comments: NR Authors name: Young In Kim Institution: Department of Psychiatry, Chung‐Ang University Hospital, Seoul, Republic of Korea Email: sunmikim706@gmail.com Address: Sun Mi Kim, MD, PhD Department of Psychiatry, Chung‐Ang University Hospital, 102 Heukseok‐ro, Dongjak‐gu, Seoul 06973, Republic of Korea Tel: +82‐2‐6299‐1519, Fax: +82‐2‐6298‐1508 Time period: NR |
|
| Notes | PSY included in analysis 2.1 Beck’s depression inventory included in analysis 2.3 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Participants were randomly divided into two groups: the active‐TMS group and the sham‐TMS group. " Sequence generation process insufficiently described |
| Allocation concealment (selection bias) | Unclear risk | Difficult to judge whether participants and/or investigators could possibly foresee assignment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants were randomly divided into two groups: the active‐TMS group and the sham‐TMS group. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants were blinded and outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No intention to treat analysis. Among the 28 enroled participants, data from four participants were dropped because they did not complete the TMS sessions or QEEG assessment (14%): one participant from the active‐TMS group and one participant from the sham‐TMS group discontinued the TMS sessions due to headache and one participant from the active‐TMS group and one participant from the sham‐TMS group missed their QEEG appointments without giving notification. Ultimately, 24 participants completed all TMS sessions and QEEG assessments. Missing not at random however below our pre‐defined cut‐off value. |
| Selective reporting (reporting bias) | Unclear risk | No trial registration or no study protocol reported, nor did we find one online. No indication of selective reporting. |
| Other bias | Unclear risk | Not able to assess response rate. |
Kline 2020.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Dog
Coloring
Control (no intervention)
Overall
Included criteria: emergency care providers, including nurses, residents, and physicians on duty in the ED of Eskenazi hospital Excluded criteria: provider statement of dislike, allergy, fear or other reason to not interact with a therapy dog, and prior enrolment Pretreatment: no significant differences in age and gender between the two experimental groups and the control group. Authors did not report any other results. Compliance rate: 127 eligible and 122 participated in at least 50% of the intervention thus > 96% Response rate: NR Type of healthcare worker: nurse, physician resident |
|
| Interventions |
Intervention characteristics Dog
Colouring
Control (no intervention)
|
|
| Outcomes |
Perceived Stress Scale (PSS)
Stress (VAS)
|
|
| Identification |
Sponsorship source: NR Country: USA Setting: Hospital Comments: NR Authors name: Jeffrey A Kline Institution: Indiana University School of Medicine, Indianapolis Email: jefkline@iupui.edu Address: Indiana University School of Medicine, Indianapolis Time period: 2018 |
|
| Notes | Author J Kline kindly provided the mean and SD of the primary outcome for the intervention groups. Modified PSS included in analysis 2.1. Intervention groups combined to create a single pair‐wise comparison |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "were randomized by preprinted random sequence to receive either exposure to a therapy dog or to coloring a mandala." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to understand whether intervention allocations could have been foreseen in advance of, during, enrolment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | Trial registration NCT03628820. No selective outcome reporting. |
| Other bias | Unclear risk | Response rate not reported. |
Kurebayashi 2012.
| Study characteristics | ||
| Methods | RCT, Brazil | |
| Participants | 75 nurses at the Teaching Hospital of the University of São Paulo. Quote: "In order to define the sample of participants, the authors used the Stress Inventory or Stress Symptoms List – SSL. This instrument was applied to all subjects who agreed to participate in the study (N = 109); however, only subjects who achieved mean (29 to 60 points), high (61 to 120 points) or very high (>120 points) scores were included in the sample; 75 of them completed the study. As for the distribution of the participants, 22 subjects were placed in the Control Group, 27 in the Needles Group and 26 in the Seeds Group." (p. 88) Quote: "The inclusion criteria were: belonging to the nursing team; voluntary participation in the study with availability to attend the sessions; obtaining a minimum SSL score at mean, high and very high stress level; not being pregnant. The authors excluded from the sample all the subjects who went on vacation or medical leave after the beginning of the study; did not show up to the session or gave up due to adverse effects, and those who had low SSL score." (p. 88) |
|
| Interventions | 1) Experimental 1: Auriculotherapy (form of acupuncture performed on the ears) with needles (n = 27) 2) Experimental 2: Auriculotherapy with seeds (n = 26) 3) Control: No intervention(n = 22) "The intervention groups received eight sessions (one session a week), with duration of 5 to 10 minutes each session, on the Shenmen, Kidney and Brainstem points. The first two points have calmative properties and the kidney point has energetic function. After the location of the reactive points with a point locator, the ear auricle was hygienized with cotton and ethyl alcohol 70% and, then, semi‐permanent needles were applied or seeds were fixed with adhesive plaster, according to the intervention group. In the group of auriculo therapy with seeds, mustard seeds were used, and the participants were instructed to stimulate them three times a day, for 15 times, with moderate pressure. The volunteers were instructed to remove the needles or seeds 24 hours before the session and, in case there was any discomfort, itching or signs of allergy, they should remove them before that." (p. 88) |
|
| Outcomes | Stress Symptoms List | |
| Identification | ||
| Notes | SSl included in analysis 2.1. Intervention groups combined to create a single pair‐wise comparison. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "This randomized controlled clinical experiment was performed with three groups..." (p. 88) |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | "...there was a loss of 34 subjects during the study. Seven professionals went on vacation after the beginning of the study and two on medical leave; 12 missed the session because they had forgotten it, due to traffic problems or the difficulty to reschedule it and seven did not show up for the first session. One participant gave up due to adverse effects, in this case, nightmares, and five exclusions were due to low score (1), not belonging to the nursing team (3), and not filling out properly the questionnaires (1)." (p. 89) The authors do not report how the dropouts were distributed among the study groups. |
| Selective reporting (reporting bias) | High risk | The authors present data separately for participants who had high SSL scores to begin with in table 2 but not at all for participants with a moderate SSL score. |
| Other bias | Low risk | We did not find any indications of other sources of bias. |
Kurebayashi 2014.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Auriculotherapy (protocol group)
Auriculotherapy (no protocol group)
Control (no intervention)
Overall
Included criteria: voluntary participation in the study with the availability of time to attend the sessions, and obtaining a score in the SSL indicating a medium or high level of stress. Excluded criteria: nephrolithiasis with surgical indication (the Kidney point can stimulate the expulsion of stones), performing another energy therapy, taking anxiolytic or anti‐depressant medication, or being pregnant. Pretreatment: NR Compliance rate: NR Response rate: 175 of the 213 (82%) eligible nurses participated Type of healthcare worker: nurses |
|
| Interventions |
Intervention characteristics Auriculotherapy (protocol group)
Auriculotherapy (no protocol group)
Control (no intervention)
|
|
| Outcomes |
Vasconcelos’ Stress Symptoms List (SSL)
|
|
| Identification |
Sponsorship source: NR Country: Brasil Setting: Hospital Comments: NR Authors name: Leonice Fumiko Sato Kurebayashi Institution: Doctoral student, Escola de Enfermagem, Universidade de São Paulo, São Paulo, SP, Brazil. Email: juliaps@usp.br Address: Maria Júlia Paes da Silva Universidade de São Paulo. Escola de Enfermagem Av. Dr. Enéas de Carvalho Aguiar, 409Bairro: Cerqueira César CEP: 05409‐000, São Paulo, SP, Brasil Time period: 2011 |
|
| Notes | SSL included in analysis 2.1. Intervention groups combined to create a single pair‐wise comparison | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "using numbers randomly generated by the site www.randomizer.org" |
| Allocation concealment (selection bias) | Unclear risk | Difficult to judge whether participants and/or investigators could possibly foresee assignment. However, it is assumed that randomisation was performed in one go and that participants and/or investigators could not foresee assignment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up. |
| Selective reporting (reporting bias) | Low risk | Protocol registration checked, no selective reporting. |
| Other bias | Unclear risk | 'Loosely' validated outcome measure. Compliance rate not reported. |
Leao 2017.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Mono‐sensory
Bisensory
Multisensory
Control (no intervention)
Overall
Included criteria: female health professionals aged between 18 and 60 years old who worked in healthcare or healthcare‐related areas Excluded criteria: relevant dermatological findings, women who worked at night or alternating shifts (due to the known chronobiological changes that could affect the outcomes in this study), as well as women who were pregnant or lactating. Pretreatment: reported socio‐demographic baseline characteristics of participants randomised to the intervention group were similar to socio‐demographic baseline characteristics of participants randomised to the control group. Compliance rate: we were surprised by the lack of time and availability of participants to take part in the study. Although many participants were interested in participating during the recruitment stage, they showed poor compliance and did not attend subsequent evaluations, especially those scheduled for 15 days and 30 days following the study (follow‐up). Response rate: of the 374 eligible participants 123 were randomised (33%) Type of healthcare worker: nurses |
|
| Interventions |
Intervention characteristics Mono‐sensory
Bisensory
Multisensory
Control (no intervention)
|
|
| Outcomes |
The ISS Inventory of Symptoms of Stress
|
|
| Identification |
Sponsorship source: Hospital Isrealita Albert Einstein Country: Brasil Setting: Private hospital Comments: NR Authors name: Eliseth Ribeiro Leão Institution: Research Institute, Hospital Israelita Albert Einstein. São Paulo, Brazil Email: eliseth.leao@einstein.b Address: NR Time period: 2014 |
|
| Notes | Dichotomous outcome measure that we could not enter into the meta‐analysis | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "signed an informed consent form. Then, we randomized participants and conducted a pilot test with seven volunteers to evaluate any necessary adjustments to the study (1 control participant, and two participants for each of the intervention groups). Participants were randomized using opaque, sealed and numbered envelopes and then ran‐ domly selected using a computer program with numbers generated by the Research Randomizer1 in order to distribute participants among the four arms of the study: |
| Allocation concealment (selection bias) | Unclear risk | Participants were randomized using opaque, sealed and numbered envelopes and then randomly selected using a computer program with numbers generated by the Research Randomizer in order to distribute participants among the four arms of the study. The enrolment occurred continuously from July to October, 2014. The follow‐up of each participant was always performed 30 days after the end of the intervention. The study was conducted at a single center. Data collection was completed in December 2014. Difficult to judge whether participants and/or investigators could possibly foresee assignment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes were self‐report. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 30 of the randomised participants were not included in the analysis (30/123 24%). Reasons provided. Not reported whether missing at random. |
| Selective reporting (reporting bias) | Low risk | Trial registration NCT02406755. No indication of selective reporting. |
| Other bias | Unclear risk | 251/374 (67%) did not want to participate. Low compliance ‐> We were surprised by the lack of time and availability of participants to take part in the study. Although a large number of participants were interested in participating during the recruitment stage, they showed poor compliance and did not attend subsequent evaluations, especially those scheduled for 15 days and 30 days following the study (follow‐up). |
Lebares 2021.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline Characteristics Enhanced stress resilience training‐1 (ESRT‐1)
Control‐1 (no intervention)
Enhanced stress resilience training‐2 (ESRT‐2)
Control‐2 (no intervention)
Overall
Included criteria: NR Excluded criteria: NR Pretreatment: reported socio‐demographic baseline characteristics of participants randomised to the intervention group were similar to socio‐demographic baseline characteristics of participants randomised to the control group Compliance rate: 89 assigned to intervention 50% actually participated Response rate: NR Type of healthcare worker: post‐graduate residents and surgeons |
|
| Interventions |
Intervention characteristics Enhanced stress resilience training‐1 (ESRT‐1)
Control‐1 (no intervention)
Enhanced stress resilience training‐2 (ESRT‐2)
Control‐2 (no intervention)
|
|
| Outcomes |
Cohen's Perceived Stress Scale (PSS‐10)
Maslach Burnout Inventory ‐ emotional exhaustion
Maslach Burnout Inventory ‐ Depersonalisation
|
|
| Identification |
Sponsorship source: NR Country: USA Setting: Hospital Comments: NR Authors name: Carter C. Lebares Institution: Department of Surgery, University of California, San Francisco Email: carter.Lebares@ucsf.edu Address: NR Time period: 2016‐2017 |
|
| Notes | PSS included in analysis 2.1 and 2.2 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "In 2016 and 2017, we conducted a partially‐blinded, pilot, parallel group randomized trial (NCT#03141190) with 1:1 allocation of PGY‐1 residents to ESRT‐1 (n ¼ 23) versus active Control‐1 (n ¼ 21). ESRT‐1 participants (100% surgical) were" Computer‐generated randomization |
| Allocation concealment (selection bias) | Unclear risk | One male control mistakenly attended the first week of ESRT‐2 and was allowed to continue in the intervention arm |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Although participants were blinded to assignment and asked not to discuss class content between arms, communication was certainly possible and should be considered in evaluating our results. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Although participants were blinded to the assignment and asked not to discuss class content between arms, communication was certainly possible and should be considered in evaluating our results. Outcomes are self‐report. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Total absences were minimal (10%) across all trials, populations, and conditions; 80% were attributable to scheduled vacations or emergent patient situations. The remainder were attributable to over‐sleeping. Attrition was limited to two female participants (both nonsurgical), who dropped from ESRT‐2 (intervention arm) due to disinterest in performing home practice and feeling ‘‘overloaded’’ by additional obligations.Participants who did not complete the study felt more overloaded however loss to follow‐up is below our pre‐defined cut‐off point. |
| Selective reporting (reporting bias) | Low risk | Trial registration NCT03141190NCT03518359. No indication of selective reporting. |
| Other bias | Low risk | No indication of other sources of bias. |
Lee 1994.
| Study characteristics | ||
| Methods | Randomised controlled trial, Taiwan | |
| Participants | 60 hospital nurses suffering from either: insomnia, headache or gastrointestinal discomfort. | |
| Interventions | 1) Experimental: assertiveness training: six 2‐hour sessions on Monday, Wednesday and Friday at 2pm to 4pm on two consecutive weeks. The contents of sessions included the concept of beliefs and negative self‐statements, building a positive belief system, applying assertion to clinical settings and developing group and self‐reinforcement support systems. 2) Control: Traditional in‐service programme about computer applications in nursing. | |
| Outcomes | Perceived Stress Scale, Rathus Assertiveness Schedule | |
| Identification | ||
| Notes | PSS included in analysis 1.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Subjects were randomly assigned to one of two treatments: assertiveness training (AT) or alternate treatment control (ATC), which served as a control and contained updated knowledge of new computer technology for in patient settings." (p. 419) |
| Allocation concealment (selection bias) | Unclear risk | "Subjects admitted to the study agreed to random treatment assignment and a 2‐month commitment to the study. However, the subjects did not know whether they would receive treatment or control procedures during that time." (p. 425) Difficult to judge whether participants and/or investigators could possibly foresee assignment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "Of the respondents who initially chose to participate, three did not complete the study and were not included in the data analysis due to their failure to attend all sessions, failure to complete the questionnaire, or decision to leave hospital employment." (p. 425) Loss to follow‐up is below our review pre‐defined cut‐off point (three of the 60 (0.05%)) |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | We did not find any indications of other sources of bias. |
Lee 2020.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Psychotherapy
Control (no intervention)
Overall
Included criteria: the participant must be a practising physician of the primary healthcare system in Almaty (Kazakhstan), he/she should have at least one year of work experience; he/she must provide signed informed consent. Excluded criteria: incomplete filling out of questionnaires, refusal to participate in the study, lack of informed consent, dismissal from work. Pretreatment: according to the results, there was no statistically significant difference between age, gender, marital status and speciality of doctors in the two groups. Type of healthcare worker: exclusively doctors involved in primary healthcare Response rate: 93% Compliance rate: 23% |
|
| Interventions |
Intervention characteristics Psychotherapy
Control (no intervention)
|
|
| Outcomes |
Maslach Burnout Inventory ‐ Emotional Exhaustion
Maslach Burnout Inventory ‐ Depersonalisation
Maslach Burnout Inventory ‐ Personal accomplishment (lack of)
|
|
| Identification |
Sponsorship source: NR Country: Republic of Kazakhstan Setting: Two out‐patient‐clinics Comments: NR Authors name: Sergey Lee Institution: S.D. Asfendiyarov Kazakh National Medical University Email: lee.s.kaznmu@mail.ru Address: Tole Bi Street 94, Almaty, 050000, Kazakhstan Time period: 2019 |
|
| Notes | MBI‐EE included in analysis 1.2 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were assigned with an individual number, after which they were randomized using online random tools (experimental and control groups into two groups): |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to understand whether intervention allocations could have been foreseen in advance of, during, enrolment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 112 of the 243 randomised participants included in the analyses. Not reported whether lost to follow‐up was at random. |
| Selective reporting (reporting bias) | Unclear risk | No trial protocol reported, nor did we find one online. |
| Other bias | Low risk | No indication of other bias. |
Lee 2021.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Auricular acupressure (experimental)
Control (placebo acupressure)
Overall
Included criteria: Outpatient nurses who were over 20 years of age and working in a medical institution with no experience of receiving auricular acupressure. Excluded criteria: Those who were receiving complementary or alternative therapies; those taking antidepressants, anticonvulsants, or sleeping pills; and those with skin integrity problems were excluded from the study. Pretreatment: No statistically significant differences emerged between the two groups on stress, anxiety, depression, and physiological index Type of healthcare worker: Exclusively outpatient nurses Response rate: 100% Compliance rate: 90% |
|
| Interventions |
Intervention characteristics Auricular acupressure (experimental)
Control (placebo acupressure)
|
|
| Outcomes |
Perceived Stress Scale (PSS)
Beck Depression Inventory‐II (BDI‐II)
State‐Trait Anxiety Inventory (STAI)
|
|
| Identification |
Sponsorship source: NR Country: South Korea Setting: A medical institution Comments: NR Authors name: Hyojung Park Institution: College of Nursing, Ewha Womans University Email: hyojungp@ewha.ac.kr Address: 52, Ewhayeodae‐gil, Seodaemun‐gu, Seoul 03760, South Korea Time period: June 2018 to August 2018 |
|
| Notes | PSS included in analysis 2.1 Beck Depression Inventory‐II (BDI‐II) included in analysis 2.3 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Participants for the experimental group and the control group were selected through randomization. |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to understand whether intervention allocations could have been foreseen in advance of, during, enrolment. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants were blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants were blinded and outcomes are self‐reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 54 of the 60 randomised participants included in the analyses. |
| Selective reporting (reporting bias) | Unclear risk | No trial registration, nor did we find one online. |
| Other bias | Low risk | No indication of other risk of bias. |
Lin 2015.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Yoga
Control (no intervention)
Overall
Included criteria: the inclusion criteria consisted of mental health professionals who were not involved in a formal exercise program and who were willing to participate in this study. Excluded criteria: exclusion criteria included pain due to injuries to shoulders, waist, or lower back, and musculoskeletal diseases such as muscle strains, that made participants unsuitable to participate in this study. Pretreatment: the demographic characteristics of the two groups, including gender, marital status, religious reference, educational status, job title, and age, showed no significant differences. The total scores of pretest stress adaptation between yoga and control groups did not reach statistical significance. The total scores of pretest work‐related stress between the two groups reached statistical significance. Thus, we took the total scores of pretest work‐related stress as a covariate to control for possible confounding. Type of healthcare worker: mental health professionals in a teaching hospital, but 38% non‐medical nor nursing staff Response rate: 80% Compliance rate: 100% |
|
| Interventions |
Intervention characteristics Yoga
Control (no intervention)
|
|
| Outcomes |
Work‐related stress scale
Stress adaptation scale
|
|
| Identification |
Sponsorship source: Funding for this study was provided by a grant RA12042 from Changhua Show Chwan Memorial Hospital and a grant MOST‐103‐2314‐B‐166‐003 from the Minister of Science in Taiwan Country: Taiwan Setting: A teaching hospital Comments: NR Authors name: Shu‐Hui Yeh Institution: Central Taiwan University of Science and Technology–Nursing Email: yehshuhui@gmail.com ; 107514@ctust.edu.tw Address: No.666 Buzih Road, Beitun District, Taichung City 40601, Taiwan Time period: NR |
|
| Notes | Stress adaptation scale (higher is better) included in analysis 2.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | This study was a single‐blind, parallel‐arm randomized controlled trial in which the analyzer was unaware of which group was the experimental or control group. The intervention consisted of a series of weekly, 60‐minute yoga classes over a 12‐week period (Figure 1). Those who were assigned to the control group participated in a free tea time during which they watched television and did not exercise. The participants each signed an informed consent prior to enroling in the study. Then, the participants signed the informed consent form and were randomly assigned to yoga or control groups by drawing lots. There were 30 participants each in the yoga and control groups. It was expected that the two groups were homogeneous through drawing lots of random allocation. |
| Allocation concealment (selection bias) | High risk | Then, the participants signed the informed consent form and were randomly assigned to yoga or control groups by drawing lots. There were 30 participants each in the yoga and control groups. It was expected that the two groups were homogeneous through drawing lots of random allocation. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | No trial registration, nor did we find one online. |
| Other bias | Unclear risk | Statistically significant baseline differences on stress. |
Lin 2019.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Mindfulness‐based group intervention
Control (wait list)
Overall
Included criteria: being employed as a full‐time nurse Excluded criteria: (a) being a student nurse, (b) suffering from serious somatic disease, (c) taking mood‐regulating drugs, (d) having suffered a major traumatic event in the past 6 months, and (e) having participated in mindfulness training previously. Pretreatment: no significant differences were observed between the two groups for any of the demographic characteristics. Type of healthcare worker: exclusively nurses Response rate: NR Compliance rate: 82% |
|
| Interventions |
Intervention characteristics Mindfulness‐based group intervention
Control (wait list)
|
|
| Outcomes |
Perceived Stress Scale (PSS)
|
|
| Identification |
Sponsorship source: This study was supported by a grant from the General Program of Science and Technology Plan for Health Care in Dongguan City of Guangdong Province. The funder played no role in the study design, data collection, data analysis, manuscript preparation, or decision to publish the report. Country: China Setting: Two general hospitals Comments: NR Authors name: Guoping He Institution: Xiangya Nursing School of Central South University Email: lily453125836@126.com Address: No. 172, Tongzipo Road, Yuelu District, Changsha, Hunan 410013, China Time period: 2017 |
|
| Notes | PSS included in analysis 1.1 and 1.2 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "utilized a randomized controlled design.Eligible participants were randomized 1:1 using a computer‐generated random number table to the intervention group or the wait‐list control group." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to understand whether intervention allocations could have been foreseen in advance of, during, enrolment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | No trial registration, nor did we find one online. |
| Other bias | Unclear risk | Response rate not reported. |
Luthar 2017.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Authentic Connections Groups
Control (no intervention)
Overall
Included criteria: inclusion required at least one child 18 years of age or younger. Excluded criteria: NR Pretreatment: other than the difference in proportion of NP/PAs and physicians, the intervention and control groups did not differ in demographics, baseline adjustment or cortisol levels. Type of healthcare worker: female (physicians, PhD’s in clinical practice, NPs, and PAs) Response rate: NR Compliance rate: 100% |
|
| Interventions |
Intervention characteristics Authentic Connections Groups
Control (no intervention)
|
|
| Outcomes |
Maslach Burnout Inventory ‐ Emotional Exhaustion
Maslach Burnout Inventory ‐ Depersonalisation
Maslach Burnout Inventory ‐ Personal accomplishment
Beck Depression Inventory
|
|
| Identification |
Sponsorship source: This study was supported by a Seed fund from Arizona State University to Luthar. Mayo Clinic funded and supported medical‐care professionals’ time to participate in study activities Country: United States Setting: Mayo Clinic Comments: NR Authors name: Suniya S. Luthar Institution: Department of Psychology, Arizona State University, Tempe, Arizona Email: Suniya.Luthar@asu.edu Address: 950 S. McAllister Drive, Tempe, AZ85281 Time period: February to November 2015 |
|
| Notes | MBI‐EE included in analysis 4.1 Beck Depression scale included in analysis 4.4 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Participants were assigned randomly to the ACG intervention group (n ¼ 21) or to the control group (n ¼ 19)" |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "With blinded random assignment," |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants were blinded and outcomes self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "On psychological measures, one participant was missing data on parenting stress at follow‐up. On biological measures, pregnancies and maternity leaves precluded draws from one woman throughout, and from two at the follow‐up. An additional two could not schedule times to provide samples at follow‐up, and two were statistical outliers and removed from the analysis (> 2 SD from the mean)." |
| Selective reporting (reporting bias) | Unclear risk | No trial registration nor did we find one online. |
| Other bias | Unclear risk | Response rate not reported. |
Mache 2015.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Psychosocial Resiliency Training
Control (no intervention)
Overall
Included criteria: inclusion criteria were (1) employment as a hospital doctor, (2) working at least full time, (3) work‐ing experience of less than a year, (4) being able and willing to participate, and (5) agreement to complete a survey at least two times. Excluded criteria: NR Pretreatment: baseline data on gender, age, and perceived health indicate only small, insignificant differences between the control and the intervention group. Type of healthcare worker: exclusively junior physicians Response rate: NR Compliance rate: 89% |
|
| Interventions |
Intervention characteristics Psychosocial Resiliency Training
Control (no intervention)
|
|
| Outcomes |
Perceived Stress Questionnaire (PSQ)
|
|
| Identification |
Sponsorship source: NR Country: Germany Setting: Hospital: several clinic departments specialising in different medical specialities (e.g., internal medicine, paediatrics, neurology, and gynaecology). Comments: NR Authors name: Stefanie Mache Institution: Institute for Occupational and Maritime Medicine (ZfAM), University Medical Center Hamburg‐Eppendorf Email: s.mache@uke.de Address: Seewartenstrasse 10, 20459 Hamburg, Germany Time period: February to August 2014 |
|
| Notes | PSQ included in analysis 1.1, 1.2 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "physicians were randomized into an intervention and control group. Of" |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | No trial registration, nor did we find one online. |
| Other bias | Unclear risk | Response rate not reported. |
Mache 2016.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Self‐care health intervention programme
Control (no intervention)
Overall
Included criteria: study participation requires positive inclusion criteria: (1) employment as a psychiatrist in a psychiatric department, (2) working full time, (3) being able and willing to take part in the study, (4) agreement to complete a survey at least three times. Excluded criteria: NR Pretreatment: only small, insignificant differences between intervention and control group have been found in baseline data on gender, age and working experience. Statistically significant positive advance was found for perceived stress, resilience and self‐efficacy in the intervention group. Type of healthcare worker: exclusively physicians Response rate: 51% Compliance rate: 95% |
|
| Interventions |
Intervention characteristics Self‐care health intervention programme
Control (no intervention)
|
|
| Outcomes |
Perceived Stress Questionnaire (PSQ)
|
|
| Identification |
Sponsorship source: NR Country: Germany Setting: Twelve hospital departments in the North of Germany specialising in Psychiatry Medicine Comments: NR Authors name: Stefanie Mache Institution: Institute for Occupational and Maritime Medicine (ZfAM), University Medical Center Hamburg‐Eppendorf Email: s.mache@uke.de Address: Seewartenstrasse 10, 20459 Hamburg, Germany Time period: NR |
|
| Notes | PSQ included in analysis 1.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "study. These physicians were randomised into two groups through a computer‐generated algorithm." |
| Allocation concealment (selection bias) | Unclear risk | Quote: "The surveys were conducted by using a secure web‐based survey sys tem, via links within e‐mail messages." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "76 participants; four needed to be excluded due to health reasons (sickness absence)." Loss to follow‐up below our review's pre‐defined cut‐off value. |
| Selective reporting (reporting bias) | Unclear risk | No trial registration, nor did we find one online. |
| Other bias | Low risk | No indication of other bias. |
Mache 2017.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Psychosocial competency training program
Control (wait list)
Overall
Included criteria: (1) regular access to the Internet, (2) working full time in the hospital, and (3) working experience of max. Two years (4) being able and willing to participate for the next 36 weeks, (5) agreement to complete the questionnaires, (6) no prior knowledge of or experience with a mental health promotion training. Excluded criteria: NR Pretreatment: baseline data on socio‐demographic differences indicated only small, insignificant differences between IG and CG (P > 0.05). Type of healthcare worker: junior physicians working in clinic departments of oncology and haematology medicine Response rate: 66% Compliance rate: 100% |
|
| Interventions |
Intervention characteristics Psychosocial competency training program
Control (wait list)
|
|
| Outcomes |
Perceived Stress Questionnaire (PSQ)
Maslach Burnout Inventory ‐ Emotional Exhaustion
|
|
| Identification |
Sponsorship source: NR Country: Germany Setting: Oncology and hematology hospital departments Comments: NR Authors name: Stefanie Mache Institution: Institute for Occupational and Maritime Medicine (ZfAM), University Medical Center Hamburg‐Eppendorf Email: s.mache@uke.de Address: NR Time period: NR |
|
| Notes | MBI‐EE included in analysis 1.1, 1.2 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "participants were randomized with the ratio 50%:50% to the 2 study groups (IG or CG). The randomization was performed with a computer‐generated list of numbers." |
| Allocation concealment (selection bias) | Low risk | Quote: "This list was created by an independent assistant; the other assistant was blinded to the list, securing covered distribution to research conditions." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "There was a total dropout rate (from randomization to analyses) of 10%. Eleven participants decided not to finish the study (reasons included illness and participants did not show up) and did not answer the questionnaires. Overall, 4% (3 of 80) of participants at T1, 6% (5 of 80) of partici‐ pants at T2, and 5% (4 of 80) of participants at T3 did not provide all follow‐up data for the outcomes. Participants who did not provide all follow‐up data did not differ in a meaningful way from those who provided data, neither on the primary outcome or any other baseline outcomes (P > .05)" |
| Selective reporting (reporting bias) | Unclear risk | No trial registration, nor did we find one online. |
| Other bias | Low risk | No indication of other bias. |
Mache 2018.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Mental health promotion program
Control (wait list)
Overall
Included criteria: inclusion criteria were as follows: (a) employment in emergency medicine, (b) working full‐time in the hospital, (c) working experience of less than 3 years, (d) being able and willing to participate, (e) agreement to complete the questionnaires, and (f) e‐mail access, availability of a computer, tablet, or a smartphone, and access to the Internet. Excluded criteria: exclusion criteria were as follows: (a) having any psychiatric illness, (b) taking any psychiatric drugs, (c) engaging any counselling service, and (d) parallel use of psychosocial counselling. Pretreatment: baseline data on socio‐demographic differences indicated only small, insignificant differences between the intervention and the comparison group. Type of healthcare worker: exclusively junior physicians Response rate: NR Compliance rate: 100% |
|
| Interventions |
Intervention characteristics Mental health promotion program
Control (wait list)
|
|
| Outcomes |
Perceived Stress Questionnaire (PSQ)
Maslach Burnout Inventory ‐ Emotional Exhaustion
|
|
| Identification |
Sponsorship source: NR Country: Germany Setting: Six hospitals: clinic departments of emergency medicine Comments: NR Authors name: Stefanie Mache Institution: Institute for Occupational and Maritime Medicine (ZfAM), University Medical Center Hamburg‐Eppendorf Email: s.mache@uke.de Address: Seewartenstrasse 10, 20459 Hamburg, Germany Time period: NR |
|
| Notes | MBi‐EE included in analysis 1.1, 1.2 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "participants were randomized at a ratio of 1: 1 to the two study arms (intervention or control group). The randomization was performed with a computer‐generated list of numbers." |
| Allocation concealment (selection bias) | Low risk | Quote: "This list was generated by an independent research assistant; the other researcher was blinded to the list, ensuring concealed allocation to research conditions." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 63 of the 70 randomised participants included in the analysis. |
| Selective reporting (reporting bias) | Unclear risk | No trial registration, nor did we find on online |
| Other bias | Unclear risk | Response rate not reported. |
Mackenzie 2006.
| Study characteristics | ||
| Methods | Randomised controlled trial, Canada | |
| Participants | 30 nurses and nurse aides working in a large urban geriatric teaching hospital | |
| Interventions | 1) Experimental: mindfulness‐based stress reduction programme: four 30‐minute group sessions including didactic section and experiential exercises. Participants also received a CD or audiocassette of guided exercises and a manual with the help of which they were instructed to practise for at least 10 minutes per day five days per week. 2) Control: no intervention | |
| Outcomes | MBI, Smith Relaxation Dispositions Inventory | |
| Identification | ||
| Notes | MBI‐EE included in analysis 1.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "Nurses and nurse aides were recruited from long‐term and complex continuing care units in a large urban geriatric teaching hospital and randomly assigned to intervention or wait‐list control groups. Because the study was conducted during the summer, however, several exceptions were made to accommodate participants' vacation schedules and additional control participants were recruited." (p. 106) |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | It is unclear if any participants dropped out. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Low risk | We did not find any indications of other sources of bias. |
Mandal 2021.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Structured Yoga Program
Control (wait list)
Overall
Included criteria: Working at the hospital for at least 1 year. Excluded criteria: We excluded those who were already under pharmacological treatment for any psychiatric disorder at the time of enrolment; having service left for less than a year (from the date of enrolment); any clinical condition that would affect the ability to practice yoga. Pretreatment: the baseline characteristics were comparable in both the groups except sex, where a higher proportion of males were present in the wait‐list group. The main outcome parameters were similar in both groups. As per the per‐protocol analysis the baseline parameters also showed the similar findings. Type of healthcare worker: exclusively in‐service nursing staff working at the hospital Response rate: 97% Compliance rate: 42% |
|
| Interventions |
Intervention characteristics Structured Yoga Program
Control (wait list)
|
|
| Outcomes |
Perceived Stress Scale (PSS)
|
|
| Identification |
Sponsorship source: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: All the lab investigations were done free of cost for the participants. The necessary requirements were provided from the institution where I work. Country: India Setting: A tertiary care hospital Comments: NR Authors name: Puneet Misra Institution: Centre for Community Medicine, Room No. 30, Centre for Community Medicine, Old OT Block, All India Institute of Medical Sciences Email: doctormisra@gmail.com Address: Ansarinagar East, 110029, Delhi, India Time period: 2018 |
|
| Notes | Included in analysis 2.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The investigation team collected unpredictable allocation sequence [using computer software and permuted block randomization] generated by a third party not involved in the study. The block size was multiple of 2 and variable in size." |
| Allocation concealment (selection bias) | Unclear risk | Quote: "After the baseline assessment was over, the sealed opaque envelop at her/his respective enrolment number was opened in front of the participants to maintain the allocation concealment. The participants were allocated in either of the 2 groups; intervention i.e. yoga group or the wait‐listed group." Difficult to judge whether participants and/or investigators could possibly foresee assignment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "Masking of the allocated group was not feasible in the study." |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "Of the 52 participants joining the class, 25 participants discontinued in the first month, 5 participants in the second month and 3 participants in the third month. Therefore, the remaining 19 participants completed the minimum required 20 yoga sessions. At the end of the 12 weeks of follow up, 19 participants of intervention group and 32 participants of wait‐list control group was included in the analysis." Judgement Comment: > 20% loss to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | No trial registration, nor did we find one online. |
| Other bias | Low risk | No indication of other sources of bias. |
Mao 2021.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Emotional intelligence training
Control (daily training)
Overall
Included criteria: the inclusion criterion was the possession of Chinese nurses' practice qualification certificates. Excluded criteria: the exclusion criteria were as follows: (a) suffering from serious physical or mental illness; (b) taking psychotropic drugs; (c) nursing staff who took maternity leave, sick leave, retirement, or further study in the study period; (d) had participated in systematic EI training before; and (e) had worked in a psychiatric ward. If participants in the intervention group were absent twice, they were excluded from the study. Pretreatment: there were no statistically significant differences in demographic characteristics between the two groups at baseline. Type of healthcare worker: exclusively nurses Response rate: 76% Compliance rate: 81% |
|
| Interventions |
Intervention characteristics Emotional intelligence training
Control (received daily briefings in meetings between head nurses, which were held regularly to discuss specific problems. There was no emotional intelligence training conducted with the control group.)
|
|
| Outcomes |
Perceived Stress Scale (PSS)
|
|
| Identification |
Sponsorship source: This study was supported by the Nursing Research Project of The Second Xiangya Hospital, Central South University (2017‐YHL‐15). Country: China Setting: NR Comments: NR Authors name: LingZhi Huang, QiongNi Chen Institution: The Second Xiangya Hospital, Central South University Email: huanglingzhi@csu.edu.cn, chenqiongni@csu.edu.cn Address: 139 Renmin Middle Road, The Second Xiangya Hospital, Central South University, Changsha, Hunan 410011, China. Time period: January 2019 ‐ January 2020 |
|
| Notes | PSS included in analysis 1.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Ten wards were randomly assigned to the intervention group and ten to the control group." |
| Allocation concealment (selection bias) | Unclear risk | Difficult to judge whether participants and/or investigators could possibly foresee assignment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Overall, the intervention and control groups lost 10 and 5 participants, respectively." 15 of the 103 randomised participants lost to follow‐up, which is below our pre‐defined cut‐off value. |
| Selective reporting (reporting bias) | Unclear risk | No trial registration, nor did we find one online. |
| Other bias | Low risk | No indication of other bias. |
Martins 2011.
| Study characteristics | ||
| Methods | Randomised controlled trial, Argentina | |
| Participants | 74 hospital paediatric resident physicians. " A total of 81% were female; the mean age was 27.3 ± 1.4 years; 57% were working in inpatient areas, 35% in the outpatient clinic, and 8% in the intensive care unit." " A comparison of the characteristics of both groups (experimental and control) revealed no significant differences." (p. 494) | |
| Interventions | 1) Experimental: self‐care workshop intervention (n = 37). quote: "The experimental group received a brief intervention consisting of two 2.5‐hour workshops directed by mental health professionals, which covered repercussions of burnout syndrome on professional activity, recognition of risk indicators for burnout syndrome, and tools to cope (identification of strengths, coping behaviors, preventive and self‐care behaviors)." (p. 494) 2) Control: (n = 37) No intervention |
|
| Outcomes | MBI | |
| Identification | ||
| Notes | It is unclear why 43 (37%) out of the available 117 resident physicians did not participate in the study. Not able to include in analysis due to missing data. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "After administration of the questionnaire, subjects were randomly assigned to one of the two study groups." (p. 494) |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Apparently no participants were lost to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | The authors do not report standard deviations with the mean MBI subscale scores. |
| Other bias | Unclear risk | It is unclear if these 74 were all the participants or only those that could be followed up. |
McConachie 2014.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Acceptance and mindfulness workshop
Control (wait list)
Overall
Included criteria: inclusion criteria were that participants were over 18 years, able to provide informed consent, and had at least six months experience of working within ID services. Excluded criteria: NR Pretreatment: no significant differences were found between the intervention and control groups in relation to age, experience of working in ID services, hours worked per week, gender, professional qualifications or education. Type of healthcare worker: Support staff involved in the direct care of individuals with ID. Response rate: 100% Compliance rate: 85% |
|
| Interventions |
Intervention characteristics Acceptance and mindfulness workshop
Control (wait list)
|
|
| Outcomes |
Staff Stressor Questionnaire (SSQ)
General Health Questionnaire (GHQ‐12)
|
|
| Identification |
Sponsorship source: NR Country: NR Setting: Independent care organisations working with individuals with ID Comments: NR Authors name: Douglas AlexanderJames McConachie Institution: University of Edinburgh, Department of Clinical Psychology, School of Health in Social Science Email: Douglas.mcconachie@nhslothian.scot.nhs.uk Address: University of Edinburgh, Teviot Place, Edinburgh, Scotland EH8 9AG, UK Time period: NR |
|
| Notes | GHQ included in analysis 1.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Permuted block randomisation was used to generate quasi‐random numbers (www.jerrydallal.com/random/ random_block_size.htm) to allocate the 120 participants to the intervention or control conditions (see Fig. 1)." |
| Allocation concealment (selection bias) | High risk | Quote: "there was no allocation concealment, and the allocation of staff to the two conditions was not fully adhered to by line managers." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "The latter factor is a particular source of potential bias, as the reason the participants changed conditions is unknown. They may have either been particularly motivated to attend the workshop, or the line manager may have been keen for them to attend or not attend." |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants not blinded whereas outcomes are self‐reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "There were similar levels of attrition from both the intervention and control group (see Fig. 1). The data was found to be missing completely at random (MCAR) (Schlomer, Bauman, & Card, 2010) considering all cases and outcome measures MCAR (P > 0.05) (X 2 = 30.686, df = 27, p = .284). The" 27.5 % lost to follow‐up ‐> MCAR |
| Selective reporting (reporting bias) | Low risk | No trial registration, no indication of selective reporting. |
| Other bias | Low risk | No indication of other bias. |
McGonagle 2020.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Positive psychology‐based coaching intervention
Control (wait list)
Overall
Included criteria: inclusion criteria were currently working at least part‐time as a PCP (0.5 FTE clinical practice), having 25 years or less of experience as a PCP, and not planning to retire within two years. Excluded criteria: potential participants were screened for psychological distress using the SCL‐10 (Nguyen et al.,1983). We used the cut‐off score determined by Müller et al. (2010) of 4.0 to indicate those with high levels of psychological distress and a licenced mental health professional was retained to speak with those who reported a level of distress ≥ 4.0. All participants attained scores < 4.0 Pretreatment: no demographic variables were significantly different between the primary and wait‐listed groups. Type of healthcare worker: exclusively Primary Care Physician Response rate: 100% Compliance rate: 97% |
|
| Interventions |
Intervention characteristics Positive psychology‐based coaching intervention
Control (wait list)
|
|
| Outcomes |
Stress in General Scale
Maslach Burnout Index
|
|
| Identification |
Sponsorship source: This project was supported by the Institute of Coaching at McLean Hospital, Harvard Medical School affiliate. Country: United States Setting: Four medical practices in a large city (both community and hospital‐based settings). Comments: NR Authors name: Alyssa McGonagle Institution: University of North Carolina at Charlotte Email: amcgonag@uncc.edu Address: 9201 University City Boulevard, Charlotte, NC 28223‐0001 Time period: NR |
|
| Notes | MBI ‐ one combined scale included in analysis 1.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "and received a participant code. Eligible participants then completed an initial survey assessing all outcome measures, and were randomized using a coin flip into either an immediate start coaching group (primary) or wait‐listed control group with a six‐month delay. |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up. |
| Selective reporting (reporting bias) | Low risk | No trial registration, no indication of selective reporting. |
| Other bias | Unclear risk | Judgement Comment: The authors combined the MBI into one scale, which is not according to the MBI handbook. |
Mealer 2014.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Multimodal resilience training program
Control (no intervention)
Overall
Included criteria: nurses were eligible to participate if they (1) were currently working 20 hours per week at the ICU bedside, (2) had no underlying medical condition that would be a contraindication to exercise, and (3) scored 82 or less on the Connor‐Davidson Resilience Scale (CD‐RISC). Excluded criteria: nurses were excluded from participating if they (1) were unable to participate in a two‐day educational workshop or (2) had a medical condition that would limit exercise. Pretreatment: measures of PTSD, burnout syndrome, resiliency, and symptoms of anxiety or depression did not differ significantly between the 2 groups. Type of healthcare worker: exclusively ICU nurses Response rate: NR Compliance rate: 93% |
|
| Interventions |
Intervention characteristics Multimodal resilience training program
Control (no intervention)
|
|
| Outcomes |
Maslach Burnout Inventory ‐ Emotional exhaustion
Maslach Burnout Inventory ‐ Depersonalization
Maslach Burnout Inventory ‐ Personal accomplishment (lack of)
The Hospital Anxiety and Depression Scale (HADS)
|
|
| Identification |
Sponsorship source: This study was funded by a grant from the National Institutes of Health (grant number K24 HL‐089223‐07). Country: United States Setting: An academic institution Comments: NR Authors name: Meredith Mealer Institution: Pulmonary Sciences and Critical Care Medicine, University of Colorado Email: Meredith.Mealer@ucdenver.edu Address: Anschutz Medical Center, 12700 E 19th Ave, C‐272, Aurora, CO 80045 Time period: 2012‐2013 |
|
| Notes | MBI‐EE included in analysis 4.1 HADS included in analysis 4.4 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "An honest broker was used to ensure that participants’ responses remained anonymous. The honest broker was not part of the study team, assigned unique identification numbers to participants, and then linked individual participants’ information with those identification numbers. |
| Allocation concealment (selection bias) | Unclear risk | See above Difficult to judge whether participants could possibly foresee assignment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "All data were entered into the REDCap data management system 30 by using unique study identfication numbers so that study personnel remained blinded to the identity of the participants. Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "randomized to the control arm. Two participants withdrew from the study before the start of the 12‐week training period: 1 from the intervention arm and 1 from the control arm. Therefore, 27 participants participated" |
| Selective reporting (reporting bias) | Unclear risk | No trial registration, nor did we find one online. |
| Other bias | Unclear risk | Response rate not reported. |
Medisauskaite 2019.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline Characteristics Interventions about the psychology of burnout, stress, coping with patient death, and managing distress
Control (no intervention)
Overall
Included criteria: doctors who currently practice medicine, have regular contact with patients Excluded criteria: NR Pretreatment: there were no significant differences between the two trial groups at baseline Type of healthcare worker: exclusively doctors Response rate: 89% Compliance rate: 78% |
|
| Interventions |
Intervention characteristics Interventions about the psychology of burnout, stress, coping with patient death, and managing distress
Control (no intervention)
|
|
| Outcomes |
Maslach Burnout Inventory ‐ Emotional exhaustion
Maslach Burnout Inventory ‐ Depersonalisation
Maslach Burnout Inventory ‐ Personal accomplishment
General Anxiety Disorder
|
|
| Identification |
Sponsorship source: The RCT was not funded or determined by Focus Games or any organization involved with the app/board game. Country: United Kingdom Setting: Among nine randomly selected NHS trusts, 9 royal colleges of medicine, and the British Medical Association (BMA) Comments: NR Authors name: Asta Medisauskaite Institution: Research Department of Medical Education Email: a.medisauskaite@ucl.ac.uk Address: UCL Medical School Room GF/644, Royal Free Hospital, NW3 2PF. Time period: From July to November 2016 |
|
| Notes | MBI‐EE included in analysis 1.1. GAD included in analysis 1.4. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Qualtrics software randomly assigned doctors to one of 5 trial groups:" |
| Allocation concealment (selection bias) | Low risk | Quote: "Blindly to the researchers, Qualtrics software randomly assigned doctors to one of 5 trial groups:" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "doctors were randomly and blindly assigned to one of 5 trial groups." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The trial group was manipulated between‐subjects such that doctors were randomly and blindly assigned to one of 5 trial groups." Outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "2.2.4. Sample" Loss to follow‐up: 25% intervention; 27% control |
| Selective reporting (reporting bias) | Unclear risk | No trial registration, nor did we find one online. |
| Other bias | Low risk | No indication of other bias. |
Melchior 1996.
| Study characteristics | ||
| Methods | RCT, the Netherlands | |
| Participants | 161 psychiatric nurses in long‐stay settings | |
| Interventions | 1) Experimental: support and advice given by nurse managers or quality care co‐ordinators: Participants were assigned to patients as primary nurses and given advice by nurse managers or quality care co‐ordinators and they followed a training programme about communication skills over a year. 2) Control: no intervention | |
| Outcomes | MBI | |
| Identification | ||
| Notes | MBI‐EE included in analysis 3.3. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Random sampling was used to select 492 nurses to complete the questionnaires." (p. 696) |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "Two main problems were encountered in this study, namely a high drop‐out rate largely due to job turnover among nurses, and the imitation of the intervention by the control group." (p. 697) A total of 51.6% of the participants dropped out during the study |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | We did not find any indications of other sources of bias. |
Moench 2021.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Self‐Care Traumatic Episode Protocol
Control (wait list)
Overall
Included criteria: participants were considered suitable for study inclusion if they met the following criteria: they were willing to participate voluntarily in treatment; they provided written consent; and were licenced mental health clinicians who had taken basic EMDR training. Excluded criteria: participants were excluded if they disclosed severe levels of clinical distress, if they were concurrently receiving psychological treatment during the study period, or if they endorsed suicidal intent. Pretreatment: NR Compliance rate: 94% Response rate: NR Type of healthcare worker: 34 participants included master’s level clinical social workers (n = 8), Canadian Certified Counsellors (n = 4), master’s or PhD‐level registered psychologists (n = 21), and psychiatrists (n = 1). |
|
| Interventions |
Intervention characteristics Self‐Care Traumatic Episode Protocol
Control (wait list)
|
|
| Outcomes |
Depression Anxiety Stress Scale (DASS‐21)
|
|
| Identification |
Sponsorship source: the authors received no specific grant or financial support for the research, authorship, and/or publication of this article. Country: Canada Setting: NR Comments: NR Authors name: Judy Moench Institution: Judy Moench Psychological Services Ltd. Email: jmoench@telusplanet.net Address: #260, 10230 142 Street, NW Edmonton, AB, T5N 3Y6, Canada. Time period: June 2020 |
|
| Notes | Included in analysis 4.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Using a randomisation sequence based on a random number table. |
| Allocation concealment (selection bias) | Unclear risk | Participants were randomized by a research assistant. Insufficient information to understand whether intervention allocations could have been foreseen by participants in advance of, during, enrolment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 5% lost to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | No trial registration, nor did we find one online. |
| Other bias | Unclear risk | Response rate was not reported. |
Montaner 2021.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Acceptance and Commitment Therapy (ACT)
Control (wait list)
Overall
Included criteria: the inclusion criteria were to be over 18 years old and have at least 6 months of experience in the ce Excluded criteria: NR Pretreatment: no significant group differences were found at baseline for demographics, neither for outcome measures. Compliance rate: 86% Response rate: 43% Type of healthcare worker: various |
|
| Interventions |
Intervention characteristics Acceptance and Commitment Therapy (ACT)
Control (wait list)
|
|
| Outcomes |
Maslach Burnout Inventory ‐ Emotional Exhaustion
Maslach Burnout Inventory ‐ Depersonalisation
Maslach Burnout Inventory ‐ Personal accomplishment
State‐Trait Anxiety Inventory (STAI) ‐ Anxiety‐Trait
|
|
| Identification |
Sponsorship source: Country: NR Setting: CSSV Ricard Fortuny Hospital: a center made up of 6 long‐term hospitalization units, two nursing home units, a day center and a palliative unit. Comments: NR Authors name: Xavier Montaner Institution: Consorci Sociosanitari Ricard Fortuny Email: xavier.casino@gmail.com Address: Avinguda Garraf 3, 08720, Vilafranca del Penedés (Barcelona), Spain Time period: The study was carried out between May 2017 and September 2018 |
|
| Notes | MBI‐EE included in analysis 4.1 and 4.2 STAI included in analysis 4.4 and 4.5 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomly assigned" |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "The drop‐out rate at the end of the intervention in the sample as a whole was 15.5%, 17.3% at 3 months of follow‐up, and 20% at 12 months of follow‐up. Although the attrition effect was higher in the IG, there were no statistically significant differences between groups drop‐out rates (Table 2)." |
| Selective reporting (reporting bias) | Unclear risk | No trial registration, nor did we find one online. |
| Other bias | Low risk | No indication of other bias. |
Montibeler 2018.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Massage with aromatherapy
Control (no intervention)
Overall
Included criteria: under employment bond and working in the surgical centre for at least one year; acceptance to participate in the study, including the stages of the study protocol; score of at least 12 points on the List of Stress Symptoms (LSS); and olfactory acceptance of the Lavandula angustifolia and Pelargonium graveolens aromas. Excluded criteria: all workers on vacation or on leave during the data collection period, as well as pregnant women. Pretreatment: except for the variable of time in the institution, there were no differences with statistical significance, confirming homogeneity among the study groups. Type of healthcare worker: nursing staff workers (nurses and nursing technicians) Response rate: 81% Compliance rate: 100% |
|
| Interventions |
Intervention characteristics Massage with aromatherapy
Control (no intervention)
|
|
| Outcomes |
The List of Stress Symptoms (LSS)
Work stress scale (WSS)
|
|
| Identification |
Sponsorship source: NR Country: Brazil Setting: A surgical center of a teaching hospital Comments: NR Authors name: Juliana Montibeler Institution: Universidade Estadual Paulista, Faculdade de Medicina de Botucatu, Departamento de Enfermagem Email: ju.montibeller.jm@gmail.com Address: Rua Dr. José Barbosa de Barros, 1540 – Bloco 2 – Apto 106CEP 18610‐307 – Botucatu, SP, Brazil Time period: 2016 |
|
| Notes | LSS included in analysis 2.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "A draw was made to randomize participants into two groups:" |
| Allocation concealment (selection bias) | High risk | Quote: "Esc Enferm USP · 2018;52:03348 A draw was made to randomize participants into two groups. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | No trial registration, nor did we find on online. |
| Other bias | Low risk | No indication of other bias. |
Moody 2013a.
| Study characteristics | ||
| Methods | RCT with individual participants, USA | |
| Participants | Paediatric oncology staff (50% nurses, 20% physicians); Experimental 23 Control 24; Men: Experimental 30% Control 8%; Age: not reported; stated to be equal; Experience > 10 years: Experimental 48% Control 46% | |
| Interventions | 1) Experimental: 8 weeks of didactic and experiential mindfulness education via a structured, skills‐training course delivered in a group setting at their hospital. The course included 1 initial 6‐hour session; 6 weekly 1‐hour follow‐up sessions; and a final 3‐hour wrap‐up session (15 hours total class time) 2) Control: No intervention |
|
| Outcomes | MBI; Perceived Stress Scale | |
| Identification | ||
| Notes | Authors provided additional data: SDs of MBI at follow‐up: Experimental: EE: 7.67; DP: 3.54; PA 3.69 Control: EE: 6.39; DP: 4.59; PA: 5.27 MBI‐EE included in analysis 1.1 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Using a computer‐generated random numbers schema in blocks of ten |
| Allocation concealment (selection bias) | Unclear risk | Participants were stratified according to their respective professions and randomised to a mindfulness‐based course (intervention) or no intervention (control) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants reported outcomes |
| Selective reporting (reporting bias) | Low risk | All outcomes stated in the 'Methods' section reported. |
| Other bias | Low risk | We did not find any indications of other sources of bias. |
Norvell 1987.
| Study characteristics | ||
| Methods | RCT, USA | |
| Participants | 12 respiratory therapists | |
| Interventions | 1) Experimental: stress management programme: 8 weekly group sessions on average 60 minutes and a manual containing homework assignments to be completed between sessions. Topics covered were deep muscle relaxation, cognitive‐behavioural exercises to identify and examine stressful situations, replacing negative thoughts and emotions with adaptive rational cognitions, effective communication skills, social support networks and problem‐solving skills, physical fitness, nutrition and weight management and maintenance of behaviour change. 2) Control: no intervention | |
| Outcomes | MBI, C‐H Inventory of Phys Symptoms, The Hassles Scale, The Uplifts Scale | |
| Identification | ||
| Notes | MBI included in analysis 4.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The 12 participating employees were randomly assigned to one of two conditions: 6 to an 8‐week stress management programme and 6 to a wait‐list control group." (p. 120) |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There were no dropouts because of small sample size. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | We did not find any indications of other sources of bias. |
Novoa 2014.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Reiki treatment
Placebo condition
Control (no intervention)
Overall
Included criteria: inclusion criteria included identification of a moderate to high risk of STS as determined by the Professional Quality of Life scale: Compassion Satisfaction, Burnout, and Compassion Fatigue/Secondary Trauma subscales (ProQOL R‐V; Stamm, 2009) Excluded criteria: respondents who were not at moderate to high risk for STS were not included in the study sample. Additional exclusion criteria included having received a Reiki treatment or other energy modality in the past month and pregnancy. Pretreatment: the dependent variables did not differ at baseline among the three groups (Reiki, placebo, and control). Compliance rate: NR Response rate: 85% Type of healthcare worker: 51% social work professionals,42% social work student interns, 5% licenced professional counsellors (LPCs). |
|
| Interventions |
Intervention characteristics Reiki treatment
Placebo condition
Control (no intervention)
|
|
| Outcomes |
Professional Quality of Life ‐ Compassion Fatigue/Secondary Trauma
Symptom Questionnaire (SQ)
|
|
| Identification |
Sponsorship source: NR Country: United States Setting: One state in the Deep South Comments: NR Authors name: Martha P. Novoa Institution: energy practitioner at the White Horse Email: NR Address: Baton Rouge, LA Time period: Recruitment for the study started in January 2010 and ended in May 2011. |
|
| Notes | Not able to include in analysis due to missing data. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The researchers randomly assigned treatment conditions using three differ‐ently colored pebbles: orange corresponded to Reiki treatment, white corre‐sponded to the placebo condition, and blue corresponded to the control group. Thirty‐three pebbles of each color were put in a paper bag and mixed." |
| Allocation concealment (selection bias) | High risk | Quote: "The researcher pulled a random pebble from the bag and the participant was assigned to treatment according to the colour of the pebble. Once the pebble had been selected it was discarded." At the end of the randomisation the researcher could possibly foresee assignment as not many pebbles were left. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants were blinded to treatment condition. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants were blinded to treatment condition and outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not recorded. |
| Selective reporting (reporting bias) | Unclear risk | No trial registration, no indication of selective reporting. |
| Other bias | Unclear risk | Compliance rate was not reported. |
OBrien 2019.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Acceptance and Commitment Therapy
Control (wait list)
Overall
Included criteria: NR Excluded criteria: NR Pretreatment: there were also no significant between‐group differences on any demographic measure at baseline or follow‐up (all P‐values > 0.20) Compliance rate: 87% Response rate: NR Type of healthcare worker: Nurses and nurse aides |
|
| Interventions |
Intervention characteristics Acceptance and Commitment Therapy
Control (wait list)
|
|
| Outcomes |
General Health Questionnaire (GHQ‐12)
|
|
| Identification |
Sponsorship source: This project was supported by a research grant provided by the Ohio Bureau Workers Compensation Ohio Occupational Safety and Health Research Program. Country: United States Setting: Nursing homes and assisted living facilities Comments: NR Authors name: William H. O’Brien Institution: Department of Psychology, Bowling Green State University Email: wobrien@bgsu.edu Address: Bowling Green, OH 43403 Time period: NR |
|
| Notes | GHQ included in analysis 4.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Interested participants were randomly assigned to the treatment or control group and then contacted by the project coordinators. An assessment session was then scheduled. Randomisation sequence generation process not described |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to understand whether intervention allocations could have been foreseen in advance of, during, enrolment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "participants were informed that they were either in the treatment group or wait‐list control group." |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote: "This was described to them as the immediate treatment group or the delayed treatment group." Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "There were no significant differences in dropout rates between the ACT and control groups (Fisher’s exact test p = 0.36)." |
| Selective reporting (reporting bias) | Unclear risk | No trial registration, nor did we find one online. |
| Other bias | Unclear risk | Response rate was not reported. |
Oman 2006.
| Study characteristics | ||
| Methods | RCT, USA | |
| Participants | 58 staff members (64% nurses, 12% physicians and 24% other) of a large hospital | |
| Interventions | 1) Experimental: Eight‐Point Program Spiritual Skills Training: 8 weekly 2‐hour training sessions about meditation skills (passage meditation, mantram repetition, slowing down, focused attention, training the senses, putting others first, spiritual association and inspirational reading). 2) Control: no intervention | |
| Outcomes | Perceived Stress Scale, MBI, Medical Outcomes Study | |
| Identification | ||
| Notes | Included in analysis 2.2 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Details of randomisation were provided in a separate supplement to the article: "While participants were completing pretests, individuals were randomly assigned to treatment (n = 30) or wait‐list control (n = 31). Computer pre‐generated 1:1 random assignment tables had been prepared by the lead investigator for each potential number of registering participants, up to 60, for each session (precise number of registrants could not be anticipated). At each session, as participants completed pretests, their consent forms were rapidly assembled in an arbitrary order and given sequential numbers by the lead investigator or the main instructor. The total number of received consent forms dictated the appropriate random assignment table, which dictated how to separate the numbered consent forms into two groups." (p. S4) |
| Allocation concealment (selection bias) | Unclear risk | "Immediately following pretest, participants were informed of their group assignment. One or two weeks later, those in the treatment condition began the eight‐week training, meeting together in one large group." (p. S4) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "Selected characteristics of the 58 final participants included in the intention‐to‐treat analysis are displayed in Table 1" (p. 715) |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Unclear risk | We did not find any indications of other sources of bias. |
Ozbas 2016.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Psychological empowerment program
Control (no intervention)
Overall
Included criteria: scored less than 17 on the Beck Depression Inventory and did not have any diagnosed physical or mental disease. Excluded criteria: NR Pretreatment: NR Type of healthcare worker: exclusively nurses Response rate: 86% Compliance rate: 83% |
|
| Interventions |
Intervention characteristics Psychological empowerment program
Control (no intervention)
|
|
| Outcomes |
Maslach Burnout Inventory ‐ Emotional exhaustion
Maslach Burnout Inventory ‐ Desensitization
Maslach Burnout Inventory ‐ Personal achievement
|
|
| Identification |
Sponsorship source: NR Country: Turkey Setting: Adult inpatient oncology clinics Comments: NR Authors name: Azize AtliO ¨zbas Institution: Hacettepe University Nursing Faculty, Psychiatric Nursing Department, Hacettepe Universitesi Hems ¸irelik Faku ¨ ltesi Email: azeozbas@gmail.com Address: 06100 Sıhhiye, Ankara, Turkey. Time period: NR |
|
| Notes | MBI‐EE included in analysis 4.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Using a computerized black‐box randomization assignment program," |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to understand whether intervention allocations could have been foreseen in advance of, during, enrolment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Some 8 nurses dropped out of the intervention group and 1 dropped of the control group," Nine of 82 randomised (11%) nurses were lost to follow‐up. This is below our pre‐defined cut‐off value. |
| Selective reporting (reporting bias) | Unclear risk | No trial registration, nor did we find one online. |
| Other bias | Low risk | No indication of other bias. |
Ozgundondu 2019.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Progressive muscle relaxation combined with music
Control (no intervention)
Overall
Included criteria: the eligible nurses included those who (a) were 18 years old, (b) had an experience of at least three months in ICUs, and (c) had no documented history of chronic obstructive pulmonary disease, heart failure and asthma. Excluded criteria: the exclusion criteria were as follows: (a) history of severe psychiatric disorder, (b) ICU experience of less than three months, and (c) not currently using any complementary therapy modalities such as acupuncture, massage therapy, relaxation techniques, and yoga that can be influential on perceived stress and fatigue or coping styles. Pretreatment: the study groups were homogeneous in terms of age, gender, marital status, educational level, income status, living with either their family or friends, comorbid conditions, experience in ICU, working hours per week and satisfaction levels with ICUs (P > 0.05). Compliance rate: 90% Response rate: 89% Type of healthcare worker: exclusively nurses |
|
| Interventions |
Intervention characteristics Progressive muscle relaxation combined with music
Control (no intervention)
|
|
| Outcomes |
Perceived Stress Scale (PSS)
|
|
| Identification |
Sponsorship source: The author(s) received no financial support for the research, authorship, and/or publication of this article Country: Turkey Setting: University of Health Sciences, Ankara Gulhane Training and Research Hospital Comments: NR Authors name: Zehra Gok Metin Institution: Hacettepe University Email: zehragok85@hotmail.com Address: Hacettepe University, Faculty of Nursing, 06000 Sihhiye, Ankara, Turkey. Time period: were recruited from 1 July 2018 to 15 January 2019. |
|
| Notes | We kindly received the mean and SD from the author. PSS included in analysis 2.1 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "were assigned randomly into two groups (Group A: 31; Group B: 32) through lottery method (A: Control; B: Intervention)" |
| Allocation concealment (selection bias) | Low risk | Quote: "by the second author of the present report who was not involved in the intervention procedures, and the PI informed the nurses about the randomisation results." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "All the sessions comprising PMR combined with music were also conducted by the PI who was not blinded to the study groups due to the nature of PMR. ," |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | No trial registration, nor did we find one online. |
| Other bias | Low risk | No indication of other bias. |
Palumbo 2012.
| Study characteristics | ||
| Methods | RCT, USA | |
| Participants | 14 registered or licenced practical female nurses aged 49 years and older who were currently employed at an academic medical centre full‐time or part‐time in a staff nurse position that involved lifting patients. | |
| Interventions | 1) Experimental: Tai Chi: onsite Tai Chi classes once a week and to practise on their own for 10 minutes each day at least four days per week for 15 weeks. Each Tai Chi class lasted 45 minutes, with 10 minutes of breathing exercises, followed by 30 minutes of Tai Chi practice, and ended with 5 minutes of visualisation and cool‐down exercises. 2) Control: o intervention | |
| Outcomes | Nursing Stress Scale, Perceived Stress Scale | |
| Identification | Not able to include in analysis due to missing data. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported. |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 3/14 participants dropped out. No imputation of data. |
| Selective reporting (reporting bias) | Unclear risk | Only change values were reported. |
| Other bias | Low risk | We did not find any indications of other sources of bias. |
Pehlivan 2020.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Compassion fatigue resiliency I
Compassion fatigue resiliency II
Control (no intervention)
Overall
Included criteria: nurses working in inpatient oncology–haematology, outpatient chemotherapy, or BMT unit Excluded criteria: providing care for paediatric oncology patients, being a nurse manager, not providing direct patient care Pretreatment: there was a statistically significant difference between the groups regarding age, total work hours per week, total years of professional experience, total years of oncology experience, level of received social support, and marital status (P < 0.05). The comparison of the mean scores for nurses’ compassion satisfaction P = 0.036 Compliance rate: 100% Response rate: NR Type of healthcare worker: nurses |
|
| Interventions |
Intervention characteristics Compassion fatigue resiliency I
Compassion fatigue resiliency II
Control (no intervention)
|
|
| Outcomes |
Professional quality of life scale‐IV ‐ Compassion fatigue
Professional quality of life scale‐IV ‐ Burnout
Professional quality of life scale‐IV ‐ Compassion satisfaction
Perceived Stress Scale (PSS)
|
|
| Identification |
Sponsorship source: This research received no specific grant from any funding agency in the public, commercial, or not‐for‐profit sectors Country: Turkey Setting: Oncology–haematology inpatient services, outpatient chemotherapy units, and bone marrow transplant (BMT) units of three private hospitals in Istanbul Comments: NR Authors name: Tuğba Pehlivan Institution: Koç University Hospital Email: tpehlivan14@ku.edu.tr Address: Istanbul, Turkey. Time period: January 2017 January 2019 |
|
| Notes | We kindly got the mean and SD for the primary outcome from author T. Pehlivan. PSS included in analysis 1.1, 1.2 and 1.3. Intervention groups combined to create a single pair‐wise comparison |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Nurses were randomly assigned to the Experimental I, Experimental II, or control group" Sequence generation process insufficiently described. |
| Allocation concealment (selection bias) | Unclear risk | Difficult to judge whether participants and/or investigators could possible foresee assignment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Low number of participants that filled in the one‐year follow‐up questionnaire. Lost to follow‐up 57/125 (45%). Reasons provided. Not sure whether loss to follow‐up was at random. |
| Selective reporting (reporting bias) | Low risk | Outcomes reported according to trial registration. |
| Other bias | Unclear risk | Not able to assess response rate. |
PelitAksu 2020.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Progressive muscle relaxation exercise (PMRE)
Control (no intervention)
Overall
Included criteria: sample inclusion criteria were as follows: Not having a disease that prevents students from doing PMR, such as metabolic diseases, cancer, heart disease, and diabetes, and not receiving antidepressant treatment, not doing any other mind–body exercises and using a smartphone Excluded criteria: NR Pretreatment: there were no statistically significant differences between the groups’ age and gender (P > 0.05) Compliance rate: 16 of the 100 less than 4 days (16%) Response rate: 100% Type of healthcare worker: exclusively student nurse interns |
|
| Interventions |
Intervention characteristics Progressive muscle relaxation exercise (PMRE)
Control (no intervention)
|
|
| Outcomes |
Burnout Measure Short Version
|
|
| Identification |
Sponsorship source: This study did not receive any specific grant from funding agencies in the public, commercial, or not‐for‐profit sectors Country: Turkey Setting: Gynecology and obstetrics clinics Comments: NR Authors name: Sıdıka Pelit‐Aksu Institution: Department of Nursing, Faculty of HealthSciences, Gazi University, Ankara, Turkey Email: sidikapelit@hotmail.com Address: Sıdıka Pelit‐Aksu, MSN, RN, Department ofNursing, Faculty of Health Sciences, GaziUniversity, Emek mah. Bişkek Cad. 6. Cad.(eski 81. sokak) No:2 06490 Çankaya, Ankara, Turkey Time period: 2018–2019 |
|
| Notes | Burnout Measure Short Version included in analysis 2.1. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "All of the students who met the inclusion criterias were grouped randomly using simple randomization method. Students names were selected from course attendance sheet of the internship and they were assigned simultaneously and sequentially to experimental group (EG = 100) and control group (CG = 100)." Sequence generation process insufficiently described |
| Allocation concealment (selection bias) | Low risk | Quote: "Students names were selected from course attendance sheet of the internship and they were assigned simultaneously and sequentially to experimental group (EG = 100) and control group (CG = 100)." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 55 of the 200 randomised participants were lost to follow‐up (28%). Not mentioned whether loss to follow‐up was at random. |
| Selective reporting (reporting bias) | Unclear risk | No trial registration or no study protocol reported, nor did we find one online. |
| Other bias | Unclear risk | Quote: "and the information leakage from experimental groups to the control groups may have affected the results of the study." |
Peterson 2008.
| Study characteristics | ||
| Methods | RCT, Sweden | |
| Participants | 131 healthcare workers who scored above the 75th percentile on the exhaustion dimension of the Oldenburg Burnout Inventory | |
| Interventions | 1) Experimental: reflecting peer‐support group: Ten 2‐hour weekly sessions where participants discussed and reflected with colleagues about work‐related stress and burnout, provided mutual support for each other, compared experiences and set individual goals to find out alternative ways to handle perceived stressful situations. The sessions started with a short 10‐minute guided relaxation. 2) Control: no intervention | |
| Outcomes | The General Nordic Questionnaire for Psychological and Social Factors at Work (QPS Nordic), Oldenburg Burnout Inventory, The Hospital Anxiety and Depression Scale, The Short Form Health Survey (SF‐36) | |
| Identification | ||
| Notes | OBI included in analysis 3.2 and the HADS in analysis 3.4 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The randomization procedure was performed by a statistician using the Statistical Analysis Software, version 8.2." (p. 508) |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Altogether 27% of participants dropped out during follow‐up and the reasons for the control group participants leaving were not known |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | We did not find any indications of other sources of bias. |
Prado 2018.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Auriculotherapy
Placebo
Control (wait list)
Overall
Included criteria: The sample consisted of 168 nurses who presented a stress score between 40 and 110 points on the List of Stress Symptoms (LSS). Since few people presented very high stress level, the level was limited to medium and high in order to obtain homogeneous samples. Other inclusion criteria were voluntary participation and availability for the auriculotherapy sessions Excluded criteria: NR Pretreatment: No socio‐demographic NR for primary outcomes. Compliance rate: NR Response rate: NR appears to be 100% Type of healthcare worker: exclusively nurses |
|
| Interventions |
Intervention characteristics Auriculotherapy
Placebo
Control (wait list)
|
|
| Outcomes |
The List of Stress Symptoms (LSS)
|
|
| Identification |
Sponsorship source: NR Country: Brazil Setting: Hospital Comments: NR Authors name: Juliana Miyuki do Prado Institution: Universidade de São Paulo, Escola de Enfermagem, São Paulo, SP, Brazil Email: fumieibez@gmail.com Address: Leonice Fumiko Sato Kurebayashi Rua Vieira Fazenda, 80, Vila MarianaCEP 04117‐030 – São Paulo, SP, Brazil Time period: 2014 |
|
| Notes | LSS included in analysis 2.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "From the inclusion criteria, the participants were randomized to the three groups by the Random Allocation Software, each group receiving 56 participants. Thirty‐five people left the study. " |
| Allocation concealment (selection bias) | Unclear risk | Quote: "From the inclusion criteria, the participants were randomized to the three groups by the Random Allocation Software, each group receiving 56 participants. Thirty‐five people left the study. " Difficult to judge whether participants and/or investigators could possibly foresee assignment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "This is a randomized, single‐blind, controlled trial with three groups: experimental auriculotherapy (with points indicated for stress), sham auriculotherapy (with sham points), and control group (without any treatment). The study was conducted with nurses of the Hospital Beneficência Portuguesa in São Paulo, São Joaquim Unit, in 2014. The control group without intervention was a waiting list, and the participants of this group later received the auriculotherapy intervention for the same time and number of sessions." Participants were blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants were blinded and outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Judgement Comment: 35 of the 168 randomised participants were lost to follow‐up (21%). Not reported whether lost to follow‐up was at random. Reasons for lost to follow‐up provided. |
| Selective reporting (reporting bias) | Unclear risk | No trial registration or study protocol reported, nor did we find one online. |
| Other bias | Unclear risk | Compliance rate and response rate difficult to assess. |
Redhead 2011.
| Study characteristics | ||
| Methods | RCT, UK | |
| Participants | 42 nurses working in a low‐secure mental health unit (LSU). Inclusion criteria: working on the LSU for a minimum of 35 hours and having direct contact with service users. Exclusion criteria: having been previously trained in Psychosocial Intervention. Quote: "A total of 79 nursing staff worked on the LSU. Forty‐two (58%) volunteered to participate in the study and provided informed consent. Of the remaining 37 staff, none actively refused, but eight were on sick leave, 23 were unable to be released by their managers to attend the training and six were excluded as they had previously been trained in PSI." (p. 61) Quote"There were no significant differences at baseline between the experimental and control groups in terms of age, gender, clinical area or qualification." (p. 62) |
|
| Interventions | 1) Experimental: psychosocial intervention training (12 qualified and 10 unqualified nurses). Quote: "Nurses allocated to the experimental group attended a PSI [Psychosocial Intervention] training programme which was delivered in a meeting room within the LSU. As the learning outcomes for qualified and unqualified staff were different, they were trained on separate courses. The training programme for qualified staff consisted of 16 half‐day sessions delivered over 8 months. The content covered a broad range of PSI including cognitive behavioural approaches for managing symptoms..." " The training for unqualified staff was delivered in 8 half‐day sessions and focused on understanding symptom related behaviours, relationship formation and helping services users to cope with symptoms..." "Teaching sessions were supplemented by small group supervision..." (p. 61) 2) Control: no intervention control (9 qualified and 11 unqualified nurses) |
|
| Outcomes | The MBI | |
| Identification | ||
| Notes | From reference list: Doyle 2007 ‐ check for inclusion MBI‐EE included in analysis 3.2 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "A randomized controlled design was adopted with nurses who volunteered to participate being allocated to either the experimental PSI training group or a waiting list control group." (p. 60) Random sequence generation process insufficiently described. |
| Allocation concealment (selection bias) | Unclear risk | Not reported if group allocation was concealed |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Apparently no participants were lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | The authors report all results for outcome measures listed in the Methods section |
| Other bias | Unclear risk | We did not find any indications of other sources of bias |
Reynolds 1993.
| Study characteristics | ||
| Methods | RCT, UK | |
| Participants | 62 health service workers | |
| Interventions | 1) Experimental: Stress Management Training (SMT): 6 weekly 2‐hour sessions of didactic learning, practice of techniques, group exercises and discussion. Topics covered were: nature, signs, causes and symptoms of stress, progressive muscular relaxation, relationship difficulties at home and work, assertiveness techniques, cognitive appraisal and reappraisal, time‐management and goal‐setting skills and emotions and seeking social support. 2) Control: no intervention | |
| Outcomes | General Health Questionnaire (GHQ‐12) used to obtain a score labelled psychological distress | |
| Identification | ||
| Notes | GHQ included in analysis 4.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The main features of the overall study design include random allocation of groups to receive SMT either immediately or after a waiting period." (p. 329) |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Only the data for those participants (62/92) who had completed the full set of assessment questionnaires were used in the analyses |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Low risk | We did not find any indications of other sources of bias |
Riley 2017.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline Characteristics Cognitive Behavioral Stress Management (CBSM)
Yoga‐Based Stress Management (YBSM)
Overall
Included criteria: to determine eligibility, potential participants completed the Physical Activity Readiness Questionnaire (PAR‐Q; Canadian Society for Exercise Physiology, 2002), a 7‐item questionnaire assessing individuals’ ability to engage in exercise without risk. Only potential participants who answered No to all of the PAR‐Q items were eligible to participate in this study. Employees who attested to meeting all eligibility requirements underwent an informed consent process. Excluded criteria: NR Pretreatment: The two intervention groups were statistically similar to each other on most demographic baseline variables. However, the sample of mental health care providers was, on average, significantly less stressed than national norms (Table 2; Crawford & Henry, 2003). Compliance rate: YBSM participants attended an average of 6.43 sessions (SD = 1.78), and CBSM participants attended an average of 6.13 sessions (SD = 1.86), a difference that was not statistically significantly different. Response rate: not able to assess Type of healthcare worker: exclusively frontline mental health care providers. |
|
| Interventions |
Intervention characteristics Cognitive Behavioural Stress Management (CBSM)
Yoga‐Based Stress Management (YBSM)
|
|
| Outcomes |
DASS‐stress
DASS anxiety
DASS depression
ProQOL ‐ Compassion satisfaction
ProQOL ‐ Burnout
ProQOL ‐ Secondary Trauma
PHQ‐9‐ Patient Health Questionnaire.
|
|
| Identification |
Sponsorship source: NR Country: USA Setting: Department of Psychiatry at a large regional hospital in New England. Comments: NR Authors name: Kristen E. Riley Institution: Department of Psychology, University of Connecticut Email: kristen.e@gmail.com Address: 486 Babbidge Rd., Unit 1020, Storrs, CT 06269, USA Time period: NR |
|
| Notes | DASS‐stress included in analysis 5.1 and 5.2. PHQ included in analysis 5.4 and 5.5. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Participants were directed to an online, secure website (Qualtrics) to complete the online survey assessments at each of the four study time points. Baseline survey assessments were completed within 3 days after completing informed consent. After completing baseline measures, participants were e‐mailed their randomized group assignment (CBSM or YBSM) and information on the meeting time and place of the assigned group." Random sequence generation process insufficiently described. |
| Allocation concealment (selection bias) | Unclear risk | Difficult to judge whether participants and/or investigators could possibly foresee assignment, however it is assumed that it affects outcomes is small. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "After completing baseline measures, participants were e‐mailed their randomized group assignment (CBSM or YBSM) and information on the meeting time and place of the assigned group. Two 8‐week" Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Thirty‐eight participants completed baseline questionnaires (YBSM = 19, CBSM = 19), 28 participants completed postintervention Time 2 questionnaires, 25 participants completed Time 3 2‐month follow‐up questionnaires, and 19 completed 6‐month post‐follow‐up questionnaires. Based on t tests and chi‐squared tests, drop‐out participants did not differ significantly on any baseline variable from those who remained in the study." |
| Selective reporting (reporting bias) | Unclear risk | No trial registration or study protocol reported, nor did we find one online |
| Other bias | Unclear risk | Response rate not reported. |
Saganha 2012.
| Study characteristics | ||
| Methods | RCT with individual participants, Portugal | |
| Participants | Physiotherapists scoring more than 26 on Emotional Exhaustion subscale of MBI out of 106 screened with MBI, and not familiar with Qigong; Experimental n = 8 Control n = 8 | |
| Interventions | 1) Experimental: Qigong exercise: posture, breathing and mind focus; classes 20 min/day 1 week; self‐treatment 2X / day 2 weeks, total 3 weeks 2) Control: waiting list for 3 weeks; after that they got the treatment as well |
|
| Outcomes | MBI | |
| Identification | ||
| Notes | MBI‐EE included in analysis 2.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "the design was a prospective randomized controlled study" |
| Allocation concealment (selection bias) | Unclear risk | Quote: "the design was a prospective randomized controlled study" |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcomes for all participants reported |
| Selective reporting (reporting bias) | Unclear risk | Baseline data not reported for the RCT group only |
| Other bias | Low risk | We did not find any indications of other sources of bias |
Sampson 2019.
| Study characteristics | ||
| Methods |
Study design:‐cluster randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics MINDBODYSTRONG
Control (no intervention)
Overall
Included criteria: inclusion criteria included all NLRNs hired during the study period who signed consent for the study. Excluded criteria: exclusion criteria included any NLRN who did not consent to participate in the study. Pretreatment: A MANOVA was used to determine group differences at baseline. No significant differences were noted in mean variable scores between the control group and the intervention group for any of the study variables Compliance rate: 96% Response rate: 85% (89 out of 105) Type of healthcare worker: exclusively newly licenced nurses |
|
| Interventions |
Intervention characteristics MINDBODYSTRONG
Control (no intervention)
|
|
| Outcomes |
Perceived Stress Scale (PSS)
Generalized Anxiety Disorder Scale (GAD‐7)
Personal Health Questionnaire
|
|
| Identification |
Sponsorship source: NR Country: USA Setting: a large, Midwestern academic medical center with an accredited nurse residency program. Comments: NR Authors name: Dr Sampson Institution: The Ohio State University Wexner Medical Center Email: marlene.sampson@osumc.edu Address: 600 Ackerman Rd, Suite 2017E, Columbus, OH 43202 Time period: 2018‐2019 |
|
| Notes | We kindly received the mean and SD of the PSS for both groups from author M. Sampson PSS included in analysis 1.1 and 1.2. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Participants were NLRNs hired between July 1, 2018, and September 30, 2018, and placed in 1 of 4 cohorts based on hire date. Two cohorts were randomly assigned to the control group, and 2 cohorts were randomly assigned to the MINDBODYSTRONG intervention group." Sequence generation process insufficiently described |
| Allocation concealment (selection bias) | Unclear risk | Difficult to judge whether participants and/or investigators could possibly foresee assignment. However, it is assumed that randomization was performed in one go and that participants and/or investigators could not foresee assignment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 89 of the 93 (96%) randomised participants included in the analyses. Not reported whether loss to follow‐up was at random. |
| Selective reporting (reporting bias) | Unclear risk | No trial registration or no study protocol reported, nor did we find one online |
| Other bias | Low risk | No indication of other sources of bias |
Sawyer 2021.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Resilience, insight, self‐compassion, and empowerment (RISE)
Control (no intervention)
Overall
Included criteria: inclusion criteria for participants were age 18 years or older; licenced as a registered nurse; employed by the health care system in a hospital‐based setting; able to speak, read, and understand English fluently; able to provide informed consent; and willing and able to comply with all study procedures and requirements for the duration of the study. Excluded criteria: exclusion criteria were employed by the health care system as an advanced registered nurse practitioner, employed in a role that completes another registered nurse’s annual evaluations, or at imminent risk of harm to themselves or others. Pretreatment: NR Compliance rate: many nurses in both the intervention group and the control group withdrew from the study before starting the intervention because they had scheduling conflicts, employment changes, or personal obligations that affected their ability to attend. Response rate: NR Type of healthcare worker: exclusively nurses |
|
| Interventions |
Intervention characteristics Resilience, insight, self‐compassion, and empowerment (RISE)
Control (no intervention)
|
|
| Outcomes |
Perceived Stress Scale (PSS)
Maslach Burnout Inventory ‐ Emotional Exhaustion
Maslach Burnout Inventory ‐ Depersonalisation
Maslach Burnout Inventory ‐ Personal accomplishment (lack of)
|
|
| Identification |
Sponsorship source: The authors received no financial support for the research, authorship, and/or publication of this article. Country: USA Setting: Hospital‐based setting Comments: NR Authors name: Amanda T. Sawyer, Institution: Research Institute, Advent Health Email: amanda.sawyer@adventhealth.com Address: Orlando, 301 East Princeton Street, Orlando, FL 32804, USA. Time period: NR |
|
| Notes | We kindly received the mean and SD for the primary outcome from author A. Swayer PSS included in analysis 1.2 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "This study was a parallel randomized controlled trial with an allocation ratio of 1:1. Participants were randomized into the intervention or wait‐list control group by a computer‐generated randomized number concealed from the recruitment team member in an opaque envelope until it was time to assign a participant to a group." |
| Allocation concealment (selection bias) | Low risk | Quote: "This study was a parallel randomized controlled trial with an allocation ratio of 1:1. Participants were randomized into the intervention or wait‐list control group by a computer‐ generated randomized number concealed from the recruitment team member in an opaque envelope until it was time to assign a participant to a group. " |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "Many nurses in both the intervention group and the control group withdrew from the study before starting the intervention because they had scheduling conflicts, employment changes, or personal obligations that affected their ability to attend. At the 1‐month, 3‐month, and 6‐month follow‐up timepoints, there were 75, 63, and 49 participants in the study, respectively." 26 of the 75 randomised participants were lost to follow‐up (35%). Not reported whether loss to follow‐up was at random. |
| Selective reporting (reporting bias) | Low risk | Quote: "The study was approved by the institutional review board and registered on ClinicalTrials.gov." The authors did not provide a registration number. Using Google we found registration information for a pilot study ‐> https://clinicaltrials.gov/ct2/show/NCT03645707. No indication of selective reporting |
| Other bias | Unclear risk | Quote: "Many nurses in both the intervention group and the control group withdrew from the study before starting the intervention because they had scheduling conflicts, employment changes, or personal obligations that affected their ability to attend. At the 1‐month, 3‐month, and 6‐month follow‐up timepoints, there were 75, 63, and 49 participants in the study, respectively." Compliance rate could not be assessed. Baseline differences not reported. |
Schrijnemaekers 2003.
| Study characteristics | ||
| Methods | Cluster‐randomised trial, the Netherlands | |
| Participants | 300 professional caregivers in homes for elderly persons | |
| Interventions | 1) Experimental: emotion‐oriented care training, clinical lessons and supervision meetings: 1‐hour clinical lesson, 6‐day training programme with 4 days at a 2‐week interval and last 2 days at a 4‐week interval. The participants were taught about the dementia syndrome and various care models for communicating with elderly people with dementia (e.g. reality orientation, validation and reminiscence), inequality of the resident‐caregiver relation, understanding the residents' perception of the environment and the attitude and (non‐)verbal communication of staff towards the resident. Intervention homes also received 3 half‐day supervision meetings to support the implementation of emotion‐oriented care. 2) Control: no intervention | |
| Outcomes | MBI, Job satisfaction | |
| Identification | Not able to include in analysis due to missing data. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Randomization was performed on the level of homes. ...within each pair, one home was randomly assigned to the intervention or control group, and the home was assigned to the alternate state." (p. S51) |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Missing values on items that were part of a scale or subscale were replaced according to the "mean value of valid subtests" principle (i.e. replacement by the mean value calculated from the valid item scores of the [sub‐] scale obtained for the same subject at the same time point). This replacement strategy was only used if less than 25% of the items of a scale or subscale had missing values." (p. S52) |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Low risk | We did not find any indications of other sources of bias |
Schroeder 2018.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Mindful Medicine Curriculum (MMC)
Control (waitlist)
Overall
Included criteria: inclusion criteria were (a) employed as a primary care physician by Providence Medical Group (PMG), (b) working at least 30% time in direct patient care, (c) aged between 25 and 75 years, (d) willing to be randomised to the intervention or wait list control group, and (e) no prior participation in the same MBI offered at PMG. Excluded criteria: NR Pretreatment: there were no significant differences between the intervention (n = 17) and wait list control (n = 16) group on any demographic variables (all P > 0.05). Compliance rate: 1/15 (6.7%) did not receive the intervention Response rate: NR Type of healthcare worker: exclusively primary care physicians |
|
| Interventions |
Intervention characteristics Mindful Medicine Curriculum (MMC)
Control (waitlist)
|
|
| Outcomes |
Perceived Stress Scale
Maslach Burnout Inventory ‐ Emotional Exhaustion
Maslach Burnout Inventory ‐ Depersonalisation
Maslach Burnout Inventory ‐ Personal accomplishment (lack of)
|
|
| Identification |
Sponsorship source: The author(s) received no financial support for the research, authorship, and/or publication of this article. Country: USA Setting: family medicine and internal medicine departments Comments: NA Authors name: David A. Schroeder Institution: Providence Heart Clinic, Portland, OR (DAS); Endocrinology–Medical Education, Providence Medical Center, Portland, OR (ES); Department of Internal Medicine, Oregon Health and Sciences University, Email: mchristopher@pacificu.edu. Address: Michael S. Christopher, PhD, School of Professional Psychology, Pacific University, 190 SE 8th Avenue, Suite 260, Hillsboro, OR 97123; e‐mail: mchristopher@pacificu.edu Time period: December 2014 and May 2015 |
|
| Notes | PSS included in analysis 1.1. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "After completing the baseline measures, participants were randomized 1:1 into the intervention or a waitlist control." Sequence generation process insufficiently described. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "After completing the baseline measures, participants were randomized 1:1 into the intervention or a waitlist control." Difficult to judge whether participants and/or investigators could possibly foresee assignment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 4 of the 33 (12%) randomised participants included in the analyses. Not reported whether loss to follow‐up was at random. However loss to follow‐up is below our pre‐defined cut‐off point. |
| Selective reporting (reporting bias) | Low risk | Quote: "Trial Registration Not applicable, because this article does not contain any clinical trials." No trial registration or no study protocol reported. No indication of selective reporting. |
| Other bias | Unclear risk | Quote: "Potential participants were recruited via email for 3 weeks prior to the first MBI group (January 2015). Participants responded to the recruitment email by directing their browser to the study website, which was housed on Qualtrics, a secure web‐based survey system." Not able to assess response rate. |
Seidel 2021.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Mindfulness Curriculum
Control (wait list)
Overall
Included criteria: NR Excluded criteria: NR Pretreatment: NR Compliance rate: NR Response rate: NR Type of healthcare worker: quote: "Physicians, nurses, physician assistants, nurse practitioners, clinical nurse specialists, social workers, physical therapists, occupational therapists, pharmacists, psychologists, and chaplains" |
|
| Interventions |
Intervention characteristics Mindfulness Curriculum
Control (wait list)
|
|
| Outcomes |
Maslach Burnout Inventory ‐ Emotional Exhaustion
Maslach Burnout Inventory ‐ Depersonalisation
Maslach Burnout Inventory ‐ Personal accomplishment (lack of)
|
|
| Identification |
Sponsorship source: "Portions of the project were funded by a Research AccelerationProgram grant from Carilion Clinic." Country: USA Setting: Academic medical centre Comments: The publication discusses two studies: 1 a quasi‐experimental study and another an RCT. The RCT details are abstracted here. Authors name: Laurie Walker Seidel Institution: Virginia Tech Email: wseidel@vt.edu Address: Roanoke City Public Schools Central Office, 40 Douglass Ave, Roanoke, VA 24012, USA Time period: 2016‐2017 |
|
| Notes | MBI‐EE included in analysis 2.1 and 2.2 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were randomly assigned to either the intervention group or a waitlist control group. Sequence generation process insufficiently described. |
| Allocation concealment (selection bias) | Unclear risk | Unable to judge whether participants and/or investigators could possible foresee assignment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not possible |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Of the 103 healthcare professionals who enroled, 83 completed the study (81%). Reasons not provide, nor whether missing was at random. Lost to follow‐up just below our pre‐defined cut‐off value. |
| Selective reporting (reporting bias) | Low risk | No trial registration or no study protocol reported. No indication of selective reporting. |
| Other bias | Unclear risk | No information on baseline differences. Contamination between groups ‐> There was a low attrition rate, supporting the effectiveness of offering each class multiple times within the week to expand choice and flexibility with the typical scheduling of a healthcare environment. The pattern of results may indicate that participants' knowing they were eventually to receive mindfulness training motivated members of the control group to improve their outlook. Although one cannot be certain about any post hoc explanation, it seems more likely that intervention participants shared what they learnt with those in the control group during the training period. It was observed during study 2 enrolment, for example, that several groupings of friends were assigned randomly to different conditions. Sharing information may explain why control participants increased mindful awareness during the intervention but did not continue that increase to the 6‐month posttest |
Shapiro 2005.
| Study characteristics | ||
| Methods | RCT, USA | |
| Participants | 38 healthcare professionals including physicians, nurses, social workers, physical therapists and psychologists | |
| Interventions | 1) Experimental: Mindfulness‐Based Stress Reduction programme: 8 weekly 2‐hour training sessions about employing the techniques involved in sitting meditation, body scan, Hatha yoga, 3‐minute breathing space (a "minimeditation") and a "loving kindness" meditation. 2) Control: no intervention | |
| Outcomes | MBI, Perceived Stress Scale, Brief Symptom Inventory | |
| Identification | ||
| Notes | PSS included in analysis 2.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Participants were randomly assigned to an 8‐week MBSR group or a wait‐list control group." (p. 167) |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "Owing to the pilot nature of this study and the small sample size, we did not perform intention‐to‐treat analyses but compared only those participants who did not drop out" (p. 169) |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Low risk | We did not find any indications of other sources of bias |
Sharif 2013.
| Study characteristics | ||
| Methods |
Study design: cluster‐randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline Characteristics Emotional intelligence training
Control (no intervention)
Overall
Included criteria: NR Excluded criteria: NR Pretreatment: the two study arms were not significantly different in terms of age, working experience, and working hours (Table 1); the distribution of employment status, shift working, and number of night shifts per week, were also not different between the two groups (Table 2). No significant difference was observed between the two groups in terms of emotional intelligence and mental health mean scores before the intervention (Tables 3 and 4). Compliance rate: 25 of the 28 randomised participants did not receive the intervention for being busy. Response rate: 84 of the 140 eligible participants did not participate (60%) Type of healthcare worker: various healthcare professionals including nurses 44 (75%), head nurses 10 (17%) and supervisors 5 (9%) |
|
| Interventions |
Intervention characteristics Cognitive‐behavioral therapy + relaxation
Control (no intervention)
|
|
| Outcomes |
28‐item Goldberg's general health questionnaires (GHQ‐20)
|
|
| Identification |
Sponsorship source: The authors would like to thank the Vice‐Chancellor for Research, Shiraz University of Medical Sciences, for financially supporting this study. Country: Iran Setting: Hospital Comments: NR Authors name: Farkhondeh Sharif, PhD Institution: Faculty of Nursing, Department of Mental Health Nursing, Shiraz University of Medical Science. Email: fsharif@sums.ac.ir Address: NR Time period: NR |
|
| Notes | GHQ included in analysis 1.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Of 200 ICU nurses, 28 were working in Shahid Faghihi hospital and selected as the control group; 28 nurses who were working in Namazi hospital were allocated to the intervention group. Selection of the hospitals for the control and the intervention group was random. |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 52 of the 56 randomised participants included in the analysis. Not reported whether missing was at random. |
| Selective reporting (reporting bias) | Unclear risk | Inaccessible trial registration. No indication of selective reporting. |
| Other bias | Unclear risk | Low participation rate (40%). Did not incorporate unit of analysis error. |
Shin 2020.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Patchouli
Control (placebo)
Overall
Included criteria: participants were included if they (1) understood the purpose of this study and agreed to participate voluntarily, (2) had been a nurse in the emergency room for at least 6 months, (3) did not have any disease and were not being treated for illness, (4) were not pregnant, (5) did not have an abnormality in olfactory function, (6) did not have asthma or an allergic reaction to patchouli oil, (7) were not receiving stress management such as an exercise or massage program, (8) had never received aromatherapy, and (9) were not regularly taking any medication that was likely to affect mental health status. Excluded criteria: NR Pretreatment: There were no significant differences between the groups in age, gender, body mass index, marital status, education, religion, duration of nursing career, duration of serving as emergency nurses, and experience of traumatic events. Compliance rate: 83% Response rate: 100% Type of healthcare worker: exclusively emergency nurses |
|
| Interventions |
Intervention characteristics Patchouli
Control (placebo)
|
|
| Outcomes |
ProQOL ‐ Compassion satisfaction
Professional quality of life scale‐IV ‐ Compassion fatigue
ProQOL ‐ Burnout
Stress (VAS)
|
|
| Identification |
Sponsorship source: This work was supported by a grant from the Basic Science Research Program through the National ResearchFoundation of Korea (NRF‐2018R1D1A1B07050048) and the Institute of Nursing Research, Korea University Grant. Country: Korea Setting: University hospital Comments: NR Authors name: You Kyoung Shin Institution: Department of Basic Nursing Science, College of Nursing, Korea University, Seoul, Republic of Korea Email: NR Address: NR Time period: May to August 2018 |
|
| Notes | VAS Stress Included in analysis 2.1 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Therefore, 60 subjects were recruited and randomly assigned to the two groups by an investigator using a random number table." |
| Allocation concealment (selection bias) | Low risk | Quote: "To conceal the allocation sequence, generation of the random allocation sequence and recruitment of participants were conducted by independent investigators." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Participants were blinded to the type of essential oil they inhaled to avoid any placebo effect and were not informed of the study group to which they were allocated." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants were blinded and outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "Of the 60 subjects recruited to this study, 10 discontinued interventions and were therefore excluded. Thus, 50 subjects were included, 25 in 5% patchouli oil (patchouli) group and 25 in sweet almond oil (control) group (Fig. 1)." No intention‐to‐treat analysis. |
| Selective reporting (reporting bias) | Low risk | Trial registration KCT0004615. No indication of selective reporting |
| Other bias | Low risk | No indication of other source of bias |
Sood 2011.
| Study characteristics | ||
| Methods | RCT, USA | |
| Participants | 40 physicians working at Mayo Clinic Rochester Quote: "Inclusion criteria were: (1) being a faculty member of the DOM and (2) being able and willing to participate. Exclusion criteria were: (1) recent (within the past 6 months) psychotic episode or (2) clinically significant acute unstable neurological, psychiatric, hepatic, renal, cardiovascular, or respiratory disease that prevented participation in the study." (p. 859) Quote: "Mean age of the participants in the active arm (46.8 ± 8.3 years) was comparable to the control arm (50.2 ± 5.7 years). Gender distribution was comparable across the two arms (55% vs 50% males in the active and control arm, respectively)." (p. 859) |
|
| Interventions | 1) Experimental: Stress Management and Resiliency Training (SMART) programme (n = 20). Quote: "The study intervention was a single 90‐min session training in the SMART program. The SMART program has been adapted from Attention and Interpretation Therapy (AIT). AIT is a structured therapy developed at the Mayo Clinic to decrease stress and enhance resilience. AIT addresses two aspects of human experience, attention and interpretation." "AIT guides learners to delay judgement and pay greater attention to the novelty of the world. Complementing attention training is instruction to help participants direct their interpretations away from fixed prejudices towards a more flexible disposition while cultivating skills such as gratitude, compassion, acceptance, forgiveness, and higher meaning." " Participants were also offered an optional 30–60‐min follow‐up session depending on individual needs. (p. 859) 2) Control: No intervention control (n = 20) |
|
| Outcomes | Perceived Stress Scale, Smith Anxiety Scale | |
| Identification | PSS included in analysis 4.1 and the Smith Anxiety Scale in 4.4 | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "After obtaining the informed consent, physicians were randomly assigned to one of two groups ‐ an active arm or a wait‐list control arm." (p. 859) |
| Allocation concealment (selection bias) | Unclear risk | The authors do not report if they concealed allocation |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Apparently there were no dropouts |
| Selective reporting (reporting bias) | Unclear risk | The authors report all results for outcome measures listed in the 'Methods' section. |
| Other bias | Unclear risk | Quote:"Eight participants (all in the control arm) declined to participate after randomization and prior to filling out any assessments because of scheduling issues" (p. 860) |
Stanton 1988.
| Study characteristics | ||
| Methods | RCT, Australia | |
| Participants | 40 trained hospital nurses who complained being overstressed | |
| Interventions | 1) Experimental: Ego‐enhancement training: One 50‐minute session and three 20‐minute sessions 1 week as part of training in the techniques of: physical relaxation, mental calmness, disposing of "rubbish", removal of a barrier and enjoyment of a special place. 2) Control: no intervention | |
| Outcomes | Stress Profile | |
| Identification | ||
| Notes | Stress profile included in analysis 2.2. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote:"In the first stage of the experiment the nurses were matched on their Profile scores, one member of each pair being allocated at random to either a non‐treatment control group or an experimental group experiencing four treatment sessions" (p. 318) |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | It is unclear if any participants dropped out |
| Selective reporting (reporting bias) | Low risk | Only 1 outcome measure used and reported |
| Other bias | Low risk | We did not find any indications of other sources of bias |
Tonarelli 2018.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Experimental group: expressive writing
Control group: neutral writing instruction
Overall
Included criteria: professionals that work in the Palliative Care field, speak and write Italian Excluded criteria: NR Pretreatment: NR Compliance rate: NR Response rate: NR Type of healthcare worker: palliative healthcare workers |
|
| Interventions |
Intervention characteristics Experimental group: expressive writing
Control group: neutral writing instruction
|
|
| Outcomes |
Maslach Burnout Inventory ‐ Emotional Exhaustion
Maslach Burnout Inventory ‐ Depersonalisation
Maslach Burnout Inventory ‐ Personal accomplishment (lack of)
|
|
| Identification |
Sponsorship source: NR Country: Italy Setting: Palliative care and hospice Comments: NR Authors name: Annalisa Tonarelli Institution: Department of Medicine and Surgery, University of Parma, Italy; Email: annalisa.tonarelli@unipr.it Address: Annalisa TonarelliDepartment of Medicine and Surgery, University of Parma, ItalyVia Gramsci 14 ‐ 43126, Parma, Italy Time period: NR |
|
| Notes | Not able to include in analysis due to missing data. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Participants who expressed the desire to partici‐ pate in the study, after signing the informed consent, were assigned by randomization" No details on how randomisation sequence was generated. |
| Allocation concealment (selection bias) | Unclear risk | Not described well enough |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not described |
| Selective reporting (reporting bias) | Unclear risk | No registration protocol nor did we find one online |
| Other bias | Unclear risk | Did not report reponse rate, compliance rate, differences between the groups at baseline |
Tsai 1993.
| Study characteristics | ||
| Methods | RCT, Taiwan | |
| Participants | 137 nurses | |
| Interventions | 1) Experimental: Training about stress at work, relaxation, breathing, imagery and meditation: One 90‐minute session in each of 2 weeks and 1 follow‐up session in the 5th week. Training covered: sources of stress at work, relaxation as a coping method and meditation including breathing exercise and imagery that emphasised the underlying cognitive process of meditation. 2) Control: traditional in‐service education about theory analysis | |
| Outcomes | Nurse Stress Checklist, Chinese General Health Questionnaire | |
| Identification | ||
| Notes | GHQ included in analysis 2.1. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "For each unit, a coin was thrown to select which nurse from this unit would be assigned to either the experimental or control group." (p. 56) |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | It is unclear if any participants dropped out |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Low risk | We did not find any indications of other sources of bias |
Verdes Montenegro Atalaya 2021.
| Study characteristics | ||
| Methods |
Study design: cluster‐randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Experimental group 1: MRBS 4 weeks
Experimental group 1: MRBS 8 weeks
Control: no intervention
Overall
Included criteria: NR Excluded criteria: NR Pretreatment: At baseline, statistically significant differences were found between the three groups in age, professional type, and work experience. Compliance rate: NR Response rate: NR Type of healthcare worker: various types of healthcare workers |
|
| Interventions |
Intervention characteristics Experimental group 1: MRBS 4 weeks
Experimental group 1: MRBS 8 weeks
Control: no intervention
|
|
| Outcomes | PSQ
|
|
| Identification |
Sponsorship source: NR Country: Spain Setting: Spanish National Health System teaching units Comments: NR Authors name: Juan Carlos Verdes‐Montenegro‐Atalaya Institution: Family and Community Medicine Teaching Department of Burgos, 0 Email: juancarlosverdesm@yahoo.es Address: Family and Community Medicine Teaching Department of Burgos, 09006 Burgos, Spain Time period: NR |
|
| Notes | PHQ included in analysis 1.1. Intervention groups combined to create a single pair‐wise comparison | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Each TU was considered as a different and independent cluster, randomly assigned to the CG (2 TUs) or one of the two EGs (4 TUs)." Insufficiently described. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "EG1 participants were included in a standard training program of mindfulness and self‐compassion; while EG2, in an abbreviated one. Furthermore, the participants from each TU were stratified according to the type of professional (66 tutors versus 66 resident intern specialists)." Insufficient information to understand whether intervention allocations could have been foreseen in advance of, during, enrolment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 53 of the 165 (32%) randomised participants lost to follow‐up. Reasons provided. The baseline characteristics of participants who dropped out of the study were similar to those who completed it, so systematic selectionbias is unlikely. |
| Selective reporting (reporting bias) | Unclear risk | No trial registration or no study protocol reported nor did we find one online |
| Other bias | Unclear risk | Statistically significant differences were observed between the three groups in age, type of professional, and time working in the Spanish National Health System |
Wei 2017.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Experimental group: active intervention and regular management.
Control (no intervention)
Overall
Included criteria: NR Excluded criteria: NR Pretreatment: there were no significant differences between the control group and intervention group nurses in the job burnout scales before the intervention Compliance rate: NR Response rate: NR Type of healthcare worker: exclusively nurses |
|
| Interventions |
Intervention characteristics Experimental group: active intervention and regular management.
Control (no intervention)
|
|
| Outcomes |
Maslach Burnout Inventory ‐ Emotional Exhaustion
Maslach Burnout Inventory ‐ Depersonalisation
Maslach Burnout Inventory ‐ Personal accomplishment (lack of)
|
|
| Identification |
Sponsorship source: NR Country: China Setting: Hospital Comments: NA Authors name: Rong Wei Institution: Department of Clinical Nursing, Qianfoshan Hospital, Jinan, Shandong, China. Email: lijianxin0531@126.com Address: Jianxin Li, Department of Clinical Nursing, Qianfoshan Hospital, NO. 16766, Jingshi Road, Jinan, Shandong, China; Time period: NR |
|
| Notes | MBI‐EE included in analysis 1.1. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "total of 112 registered nurses were randomly selected from 3 of 8 comprehensive high‐level hospitals in Jinan, China." Only mentioned that nurses where randomly selected. |
| Allocation concealment (selection bias) | Unclear risk | Unable to judge whether participants and/or investigators could possible foresee assignment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | No trial registration or no study protocol reported, nor did we find one online |
| Other bias | Unclear risk | Compliance rate and response rate not reported. |
West 1984.
| Study characteristics | ||
| Methods | RCT, USA | |
| Participants | 60 acute care hospital nurses | |
| Interventions | 1) Experimental: four weeks of Stress Inoculation (SI) training divided as: i) Education‐only group (Ed) weekly 30‐minute sessions of information about anxiety, stress and coping skills and practice of self‐monitoring of stress producing events (n = 12) ii) Education + coping skills group (CS), 4 weekly 60‐minute sessions including education plus CS. CS: relaxation training, assertive skill training, cognitive restructuring and time‐management instruction (n = 12) iii) Education + exposure group (Ex) 4 weekly 60‐minute including education plus simulated stress‐producing situations via role play (n = 12) iv) Education + coping skills + exposure group (SI) 60‐minute sessions twice a week during 4 weeks including all the above (n = 12) 2) Control: No intervention (n = 12) |
|
| Outcomes | MBI (used frequency and intensity separately for each subscale); we used Emotional Exhaustion intensity scores. Job‐Related Tension Index, Life Satisfaction Index, STAI, Rathus Assertiveness Schedule, systolic and diastolic blood pressure | |
| Identification | ||
| Notes | Results are only presented for the group including CS (n = 24) versus education plus no‐intervention (n = 24). MBI‐EE included in analysis 1.1 and STAI included in analysis 1.4. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "...60 registered nurses... were stratified on the basis of work shift and randomly assigned to 1 of 6 counselors and one of five treatment conditions." (p. 212) |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "No subject attrition occurred at posttesting." (p. 213) |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Other bias | Low risk | We did not find any indications of other sources of bias |
West 2014.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Protected time with facilitated small group curriculum
Control (protected time unstructured)
Overall
Included criteria: practising physicians in the Mayo Clinic Department of Medicine Excluded criteria: not specified Pretreatment: baseline characteristics were similar for both groups with no statistically significant differences observed. However, the intervention group had "slightly higher rates of high emotional exhaustion and overall burnout." P values for statistical significance are not provided in the paper. Compliance rate: NR Response rate: 13% Type of healthcare worker: physicians |
|
| Interventions |
Intervention characteristics Protected time with facilitated small group curriculum
Control (protected time unstructured)
|
|
| Outcomes |
Maslach Burnout Inventory ‐ Emotional Exhaustion
Maslach Burnout Inventory ‐ Depersonalisation
Perceived Stress Scale (PSS)
|
|
| Identification |
Sponsorship source: Mayo Clinic Program on Professionalism and Ethics and the Department of Medicine at Mayo Clinic, Rochester, USA. Country: USA Setting: One medical centre Comments: NR Authors name: Colin P. West Institution: Division of General Internal Medicine, Department of Medicine, Mayo Clinic Email: west.colin@mayo.edu Address: Division of General Internal Medicine, Department of Medicine, Mayo Clinic, 200 First St, Rochester, MN 55905, USA. Time period: 2010‐2012 |
|
| Notes | We kindly receivede the mean and SD for the primary outcome from author C. West. PSS included in analysis 4.1 and 4.2. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants were randomized in a concealed fashion into 2 groups via a computer‐generated algorithm." |
| Allocation concealment (selection bias) | Low risk | Participants were randomized in a concealed fashion into 2 groups via a computer generated algorithm |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low response rate. 74 of the 565 eligible physicians participated (13%) |
| Selective reporting (reporting bias) | Low risk | Data we kindly received match trial registration: NCT01159977 |
| Other bias | Low risk | No indication of other source of bias. |
West 2021.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline Characteristics Experimental group: topic focused discussion
Control (no intervention)
Overall
Included criteria: NR Excluded criteria: NR Pretreatment: NR Compliance rate: NR Response rate: 21% Type of healthcare worker: physicians |
|
| Interventions |
Intervention characteristics Experimental group: topic focused discussion
Control (no intervention)
|
|
| Outcomes |
Maslach Burnout Inventory ‐ Emotional Exhaustion
Maslach Burnout Inventory ‐ Depersonalisation
Maslach Burnout Inventory ‐ Personal accomplishment (lack of)
|
|
| Identification |
Sponsorship source: NR Country: United States of America Setting: Hospital Comments: NR Authors name: Colin West Institution: Department of Quantitative Health Sciences Mayo Clinic, Rochester, MN; and the Division of Hematology, Email: west.colin@mayo.edu Address: Department of Medicine, Stanford University, Palo Alto, CA Time period: 2013‐2014 |
|
| Notes | We kindly receivede the mean and SD for the primary outcome from author C. West MBI‐EE included in analysis 1.1 and 1.2. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants were randomized in concealed fashion into two arms via a computer‐ generated algorithm." |
| Allocation concealment (selection bias) | Low risk | Participants were randomized in concealed fashion into two arms via a computer‐ generated algorithm. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 107 of the 123 randomized participants (87%) complete follow‐up data. |
| Selective reporting (reporting bias) | Low risk | Registation trial checked: NCT04466423. No indication of selective outcome reporting. |
| Other bias | Unclear risk | Compliance not reported. |
Xie 2020.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Educational group
Mindfulness‐based intervention
Overall
Included criteria: a) they had obtained professional certification; (b) they were independently responsible for clinical work; (c) they were willing to participate and available to attend sessions; and (d) they were suffering from“moderate or above” occupational burnout Excluded criteria: (a) they had been in work for less than one year; (b) they were on vacation or on study leave; (c) they had taken a mindfulness program such as MBSR or MBCT and had been practising mindfulness in the last six months. Pretreatment: reported socio demographic baseline characteristics of participants randomised to the intervention group were similar to socio demographic baseline characteristics of participants randomised to the control group Compliance rate: EB (46/53 87%). MBIB (45/53 85%) Response rate: 63% Type of healthcare worker: exclusively nurses |
|
| Interventions |
Intervention characteristics Educational group
Mindfulness‐based intervention
|
|
| Outcomes |
Maslach Burnout Inventory ‐ Emotional Exhaustion
Maslach Burnout Inventory ‐ Depersonalisation
Maslach Burnout Inventory ‐ Personal accomplishment (lack of)
|
|
| Identification |
Sponsorship source: NR Country: China Setting: Hospital Comments: NR Authors name: Caixia Xie Institution: Nursing School, West China School of Medicine/West China Hospital, Sichuan University Email: huxiuying@scu.edu.cn xiuying_hu@163.com Address: Chengdu 610041, Sichuan, China Time period: 2017‐2018 |
|
| Notes | MBI‐EE included in analysis 5.1. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Participants were assigned to the EB or the MBIB group. This" Sequence generation process insufficiently described. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Participants in the EB group were randomly divided into three subgroups, consisting of 18, 17, and 17 individuals, respectively." Insufficient information to understand whether intervention allocations could have been foreseen in advance of, during, enrolment. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss at follow‐up |
| Selective reporting (reporting bias) | Low risk | Trial registration in Chinese. No indication of selective reporting. |
| Other bias | Low risk | No indication of other sources of bias |
Yazdani 2010.
| Study characteristics | ||
| Methods | RCT, Iran | |
| Participants | 76 nursing students Quote: "The study population included all male and female nursing students who were studying in Isfahan Nursing and Midwifery university in 2010‐2011, in the second and third years (third, fourth, fifth and sixth semesters). 72 [sic] students were randomly assigned to two groups using the list of students studying in the second and third year in 2010‐2011 and based on the odd and even numbers." (p. 210) "The groups were heterogeneous in terms of gender..." (p. 210) |
|
| Interventions | 1) Experimental: Stress management training (n = 38). Quote: "[First group (n=38) trained stress management training program (8 two hours sessions, twice a week). And second group (n = 38) did not received [sic] training." (p. 210) The stress management program consisted of: information about stress, gradual muscle relaxation and its implementation with mental imagery, consequences and physical symptoms of stress, relaxation and imagery and training and diaphragm breathing practices, linking thoughts and emotions and familiarity with cognitive errors, discussion about relaxation exercises and replacement of logical thoughts and personal stress management program. 2) Control: no intervention (n = 38) |
|
| Outcomes | DASS‐42: Depression, Anxiety and Stress Scale | |
| Identification | ||
| Notes | DASS‐stress included in analysis 2.1 and DASS‐depression in analysis 2.3. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "...students were randomly assigned to two groups using the list of students studying in the second and third year in 2010‐2011 and based on the odd and even numbers." (p. 210) |
| Allocation concealment (selection bias) | Unclear risk | Not reported if group allocation was concealed |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | It is difficult to tell if some participants were lost to follow‐up or not as the authors give three separate numbers for the amount of participants. Quote: "This study was a parallel ‐group randomized quasi‐experimental trial...on 68 BSc nursing students.", " 72 students were randomly assigned..." and "Finally seventy‐six subjects elected among them." (p. 210) |
| Selective reporting (reporting bias) | Low risk | The study had only one outcome and its results are all reported |
| Other bias | Low risk | We did not find any indications of other sources of bias |
Yung 2004.
| Study characteristics | ||
| Methods | RCT, China | |
| Participants | 65 nurse managers | |
| Interventions | 1) Experimental 1: cognitive relaxation: participants were asked to imagine the relaxation of different muscle groups. 2) Experimental 2: stretch‐release relaxation: training guided by the model of Stretch Relaxation developed by Carlson and Collins (1990) which focused on the stretching and relaxation of muscle groups. Unlike the popular progressive relaxation exercise which involves the tensing and relaxing of muscle groups, stretch‐release relaxation is less strenuous. Muscle relaxation exercise, based upon the stretching of muscle groups, incorporates the beneficial effects of muscle sensation contrast with accompanied reductions in muscle activity from the stretch procedure resulting in relaxation. 3) Control: No intervention | |
| Outcomes | C‐STAI, C‐GHQ | |
| Identification | ||
| Notes | GHQ included in analysis 2.1 and C‐STAI in analysis 2.3. Intervention groups combined to create a single pair‐wise comparison. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Of the 65 participants, 35 were randomly assigned to the experimental condition and the remaining 30 were put to the control condition. Subsequently, the 35 subjects assigned to the experimental condition were randomly allocated to the stretch‐release relaxation (n = 17) and cognitive relaxation (n = 18) groups." (p. 256) |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Quote: "All participants including the TC [test control] group were assessed again in a follow‐up session after 1 month." (p. 258). Insufficiently recorded to judge attrition bias |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | We did not find any indications of other sources of bias |
Zarvijani 2021.
| Study characteristics | ||
| Methods |
Study design: randomised controlled trial Study grouping: parallel group |
|
| Participants |
Baseline characteristics Acceptance and Commitment Therapy (ACT)
Control (no intervention ‐ routine support)
Overall
Included criteria: ‐ having a bachelor’s or higher degree in nursing, ‐ at least 2 years of work experience in psychiatric wards, ‐ attending intervention sessions based on ACT for the first time, and ‐ no history of taking psychiatric drugs in the past and present. Excluded criteria: ‐ not completing the questionnaires, ‐ absenteeism in more than one intervention session, and ‐ the occurrence of stressful events during the study. Pretreatment: statistical difference not reported. Only numbers and proportions were reported which were similar on most variables but no statistical reporting. Compliance rate: 94%. two out of 35 participants in the intervention group were excluded since they missed more than one session out of eight, i.e. 33 of the participants attended 6 or more sessions. Response rate: NR. 84 psychiatric nurses from all 23 wards in the hospital were randomly selected and screened for eligibility proportional to the required sample size for the study. However, the total number of nurses in the facility is not reported. Type of healthcare worker: psychiatric nurses |
|
| Interventions |
Intervention characteristics Acceptance and Commitment Therapy (ACT)
Control (no intervention ‐ routine support)
|
|
| Outcomes |
Perceived Stress Scale (PSS)
|
|
| Identification |
Sponsorship source: Islamic Azad University, Tehran. Country: Iran Setting: One large psychiatric hospital Comments: NR Authors name: Ladan Fattah Moghaddam Institution: Tehran University of Medical Sciences, Islamic Azad University, Tehran, Iran Email: lfatah@iautmu.ac.ir Address: Department of Psychiatric Nursing, Faculty of Nursing and Midwifery, Tehran University of Medical Sciences, Islamic Azad University, Tehran, Iran Time period: 2018 |
|
| Notes | PSS included in analysis 1.1. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Of the 84 nurses selected, fourteen were excluded due to lack of inclusion criteria, and 70 remaining nurses were each assigned a number and were randomly divided into experimental and control groups, each consisting of 35 participants. (Fig. 1). Sequence generation process insufficiently described. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not recorded. Difficult to judge whether participants and/or investigators could possibly foresee assignment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants were not blinded whereas outcomes are self‐reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rate was less than 20% and a priori outcomes were reported. |
| Selective reporting (reporting bias) | Low risk | Trial registration IRCT20180506039557N1. No indication of selective reporting |
| Other bias | Unclear risk | Response rate could not be calculated since total number of nurses was not provided. Statistical differences if any on baseline parameters not reported. |
ACT: Acceptance and Commitment Therapy; BP: blood pressure; BSI: Brief Symptom Inventory; DCWs: Direct Care Workers' ERT: Emotion regulation training; ESRT‐1: Enhanced stress resilience training‐1; GHQ: General Health Questionnaire; HCW: healthcare worker; HR: heart rate; ICU: intensive care unit; MBI: Maslach Burnout Inventory; MBSR: Mindfulness‐based stress reduction; NLGNs: newly incensed graduate nurses; PSQ: Perceived Stress Questionnaire; PSS: Perceived Stress Scale; SD: standard deviation; SMI: Stress Management Intervention; TTI: Transfer Technique Intervention; PTSD: Post‐traumatic stress disorder; STAI: State‐Trait Anxiety Inventory; WCG: waitist control group
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Adair 2020 | Wrong population: not only healthcare workers |
| Akyurek 2020 | Wrong comparison (intervention type 2 vs intervention type 2) |
| Ali 2011 | Wrong intervention: organisational intervention |
| Alkhawaldeh 2020 | Wrong outcome (stressor) ‐ trial protocol checked. |
| Ameli 2020 | Wrong population: not only healthcare workers |
| Anonymous 2021 | Not an article, wrong population: consisted of not only healthcare workers (original study considered) . |
| Aronson 2022 | Wrong intervention (organisational intervention). |
| Barbosa 2016 | Wrong population: caregivers of family not officially employed |
| Barrett 2021 | Wrong comparison (intervention type 1 vs intervention type 1) |
| Beck 2018 | Wrong population: students |
| Behzadi 2021 | Wrong outcome (stressor) |
| Bielderman 2021 | Wrong intervention: organisational intervention |
| Bittman 2003 | Wrong study design |
| Boehm 2017 | Thesis (not an article in a peer‐reviewed scientific journal) |
| BorgesSouza 2019 | Not an article |
| Bourbonnais 2011 | Wrong intervention:organisational intervention |
| Braun 2020 | Wrong population: students |
| Buruck 2016 | Wrong study design |
| Butow 2015 | Wrong intervention |
| Carneiro 2020 | Wrong population: not only healthcare workers |
| Carson 1999 | Wrong intervention: organisational intervention |
| Cascales Perez 2021 | Wrong population: not only healthcare workers |
| Cayir 2021 | Wrong intervention: organisational intervention. |
| Chaabane 2021 | Wrong population: also volunteers |
| Chen 2017 | Wrong intervention |
| Cheung 2020 | Wrong comparison (intervention type 2 vs intervention type 2) |
| Clemow 2018 | Wrong population: not only healthcare workers |
| Coelhoso 2019 | Wrong population: not only healthcare workers |
| Cordoza 2018 | Wrong intervention |
| Cosentino 2021 | Wrong study design |
| Daigle 2018 | Wrong outcome assessment: use of unvalidated questionnaire |
| Davidson 2017 | Wrong study design |
| DeKock 2022 | Wrong outcomes. Trial protocol checked. |
| Delvaux 2004 | Wrong outcome (stressor) |
| Deneckere 2013 | Wrong intervention: organisational intervention |
| Doran 2018 | Wrong population: not only healthcare workers |
| Fadaei 2020 | Wrong outcome assessment: use of unvalidated questionnaire |
| Fang 2015 | Wrong outcome (stressor) |
| Farsi 2021 | Wrong outcome (stressor) |
| Feldman 2017 | Wrong study design |
| Fiore 2021 | Wrong comparison (intervention type 2 vs intervention type 2) |
| Frogeli 2016 | Wrong comparison (intervention type 1 vs intervention type 1) |
| Gaggioli 2014 | Wrong population: not only healthcare workers |
| Gardner 2005 | Wrong population: not only healthcare workers |
| Gartner 2013 | Duplicate |
| Gauthier 2015 | Wrong study design |
| Ghafarzadegan 2014 | Wrong intervention |
| Ghazavi 2010 | Use of unvalidated questionnaire. |
| Grahn 2020 | Not an article |
| Greeson 2015 | Wrong study design |
| Griffith 2008 | Wrong population: not only healtcare workers |
| Grigorescu 2020 | Wrong study design |
| Gross 2018 | Not an article |
| Guerrier 2021 | Wrong study design |
| Gupta 2021 | Wrong population: not only healthcare workers |
| Gutman 2020 | Wrong population: students |
| Hansen 2006 | Wrong outcome. Stressor only outcome. |
| Havermans 2018 | Wrong intervention: Organisational intervention |
| Heaney 1995 | Wrong intervention:organisational intervention |
| HemmatiMaslakpak 2016 | Wrong study design |
| Hill 2016 | Wrong study design |
| Hofer 2018 | Wrong population: no healthcare workers |
| Hu 2015 | Wrong study design |
| Johnson 2015 | Wrong population: caregivers with symptoms |
| Jones 2000a | Wrong population: student nurses |
| KarbakhshRavari 2020 | Wrong outcome (stressor) |
| Karpaviciute 2016 | Wrong study design |
| Kesselheim 2018 | Not an article |
| Khaghanizadeh 2008 | Wrong intervention: organisational intervention |
| Khalsa 2021 | Not an article |
| Kiley 2018 | Wrong population: not only healthcare workers |
| Kloos 2019 | Wrong population: not only healthcare workers |
| Kon 2019 | Not an article |
| Kubota 2016 | Wrong intervention |
| Kwok 2012 | Abstract of a PhD‐thesis (not an article in a peer‐reviewed scientific journal) |
| Lahn 2015 | Abstract of a PhD‐thesis, not an article in a peer‐review scientific journal |
| Lai 2011 | Wrong comparison (intervention type 2 vs intervention type 2) |
| Lambert 2019 | Not an article |
| Le Blanc 2007 | Wrong intervention:organisational intervention |
| Lebares 2019 | Wrong comparison (intervention type 1 vs intervention type 1) |
| Leiter 2011 | Wrong intervention: organisational intervention |
| Lemaire 2011 | wrong comparison (intervention type 1 vs intervention type 1) |
| Li 2011 | Wrong intervention: organisational intervention |
| Lilly 2019 | Wrong population: no healthcare workers |
| Linzer 2015 | Wrong intervention ‐ organisational intervention |
| Loiselle 2018 | Thesis (not an article in a peer‐reviewed scientific journal) |
| Low 2015 | Wrong intervention |
| Lucas 2012 | Wrong intervention: organisational intervention. |
| Lui 2019 | Thesis (not an article in a peer‐reviewed scientific journal) |
| Luoma 2013 | Wrong comparison (intervention type 1 vs intervention type 1) |
| Lökk 2000 | Use of unvalidated questionnaire |
| Mahdizadeh 2019 | Wrong outcome (stressor). Trial registration checked. |
| Manotas 2013 | Thesis (not an article in a peer‐reviewed scientific journal) |
| McConville 2017 | Wrong study design |
| McElligott 2003 | Wrong outcome |
| Mellis 2019 | Not an article |
| Meng 2018 | Wrong population: students |
| Meyer Lamp 2020 | Wrong intervention: organisational intervention |
| Millspaugh 2021 | Wrong study design |
| Mistretta 2018 | Not an article |
| Miyoshi 2019 | Wrong study design |
| Mohebbi 2019 | Wrong outcome (stressor) |
| Moll 2018 | Wrong intervention. |
| Moody 2013 | Duplicate |
| Moyle 2013 | Wrong outcomes |
| Muller 2016 | Wrong outcomes |
| Navidian 2019 | Wrong outcome (stressor) |
| Nazari 2015 | Wrong outcome (stressor) |
| NeCamp 2020 | Wrong outcomes |
| Niva 2021 | Wrong outcomes |
| Nourian 2021 | Wrong outcomes |
| Ozturk 2021 | Wrong population: students |
| Pehlivan 2019 | Not an article |
| Penprase 2015 | Wrong study design |
| Perula deTorres 2021 | Wrong outcomes |
| Pich 2018 | Not an article |
| Ploukou 2018 | Wrong outcomes |
| Poulsen 2015 | Wrong outcomes |
| Prasad 2018 | Not an article |
| Procaccia 2021 | Wrong outcomes |
| Proctor 1998 | Wrong intervention:organisational intervention |
| Profit 2021 | Wrong population: not only healthcare workers |
| Raglio 2020 | Wrong outcome (stressor) |
| Rajeswari 2019 | Wrong intervention |
| Razavi 1993 | Wrong outcome |
| Riello 2021 | Wrong outcome assessment: no use of validated questionnaire |
| Ripp 2019 | Not an article |
| Rollins 2016 | Wrong population: not only healthcare workers |
| Romig 2012 | Wrong intervention: organisational intervention |
| Rosada 2015 | Wrong study design |
| Rowe 2006 | Wromg population:not only healthcare workers |
| Ruehl 2014 | Thesis (not an article in a peer‐reviewed scientific journal) |
| Ruotsalainen 2014 | Review |
| Ruotsalainen 2015 | Review |
| Ruotsalainen 2016 | Review |
| Safarzei 2016 | Wrong outcomes |
| Saffari 2021 | Wrong intervention |
| Salles 2013 | Wrong outcome |
| Salyers 2019 | Wrong outcome assessment: no use of validated questionnaire |
| Sampson 2020a | Thesis (not an article in a peer‐reviewed scientific journal) |
| Sargazi 2018 | Wrong outcomes |
| Seo 2014 | Wrong study design |
| Shaw 2021 | Wrong population: not only healthcare workers |
| Siedsma 2015 | Wrong publication type |
| Silva Junior 2016 | Wrong study design |
| Smith 2019 | Not an article |
| Smith 2021 | Wrong population: students |
| Smoktunowicz 2021 | We kindly got the mean and SD for the primary outcome from author E. Smoktunowicz. However, we retrospectively excluded this study as it includes wrong comparison (intervention type 1 vs intervention type 1) |
| Son 2019 | Wrong population: students |
| Steinberg 2017 | Wrong population: not only healthcare workers |
| Strauss 2021 | Wrong population: not only healthcare workers |
| Taylor 2020 | Wrong comparison (intervention type 2 vs intervention type 2) |
| Tung 2021 | Thesis (not an article in a peer‐reviewed scientific journal) |
| Uchiyama 2013 | Wrong outcomes. Trial protocol checked. |
| Uchiyama 2013b | Wrong intervention: organisational intervention |
| Valley 2017 | Wrong outcomes |
| Valley 2017a | Wrong outcomes |
| van Duinen‐van den IJssel 2019 | Wrong intervention:organisational intervention |
| vanDorssen Boog 2021 | Wrong outcomes |
| vanLeeuwen 2021 | Wrong outcomes. Study protocol checked. |
| Villani 2013 | Wrong outcomes |
| Von Baeyer 1983 | Wroing outcome use of unvalidated questionnaire |
| Watanabe 2018 | Wrong intervention: pharmacological intervention |
| Watanabe 2019 | Wrong comparison (intervention type 1 vs intervention type 1) |
| Watanabe 2019a | Not an article |
| Weitzman 2021 | Wrong study design |
| Wilczek Ruzyczka 2021 | Wrong intervention |
| Wild 2020 | Wrong outcomes |
| Xu 2021 | Wrong outcomes |
| Yamagishi 2008 | Wrong intervention |
| Yang 2018 | Wrong outcome (stressor) |
| Yang 2018a | Wrong population: students |
| Yong 2020 | Wrong study design: not randomised |
| Zwijsen 2015 | Wrong intervention: organisational intervention |
Characteristics of studies awaiting classification [ordered by study ID]
Ahmadi 2019.
| Methods | ? |
| Participants | Nurses |
| Interventions | Resilience education |
| Outcomes | Quality of working life |
| Notes | in Persian awaiting translation |
Akyurek 2022.
| Methods | Randomised control trial |
| Participants | Nurses |
| Interventions | Workplace Health Promotion Program |
| Outcomes | ProQol |
| Notes | Selected with the updated search on the 26th of September 2022. |
Bo, 2022.
| Methods | Randomised controlled trial |
| Participants | Nurses |
| Interventions | Mindfulness |
| Outcomes | MBI |
| Notes | In Chines awaiting translation. Selected with the updated search on the 26th of September 2022. |
Fainstad 2022.
| Methods | Randomised controlled trial |
| Participants | physicians |
| Interventions | Novel Online Group‐Coaching Program |
| Outcomes | MBI |
| Notes | Selected with the updated search on the 26th of September 2022. |
Fei 2019.
| Methods | Randomised controlled trial |
| Participants | Nurses |
| Interventions | Psychological resilience training |
| Outcomes | The Perceived Stress Scale, the Positive and Negative Affect Schedule & the Pittsburgh Sleep Quality Index Scale |
| Notes | No full text available |
Ferreres‐Galan 2022.
| Methods | Randomised controlled trial |
| Participants | Nurses |
| Interventions | Unified Protocol (UP) prevention program to provide emotional regulation skills to cope with stressful situations. |
| Outcomes | Emotional symptomatology, emotional regulation, burnout, |
| Notes | Selected with the updated search on the 26th of September 2022. |
Fraiman 2022.
| Methods | Randomised controlled trial |
| Participants | Paediatric Interns |
| Interventions | Mindfulness |
| Outcomes | Maslach Burnout Inventory (MBI) |
| Notes | Selected with the updated search on the 26th of September 2022. |
Ghods 2017.
| Methods | Randomised controlled trial? |
| Participants | Nurses |
| Interventions | Lavender essential oil |
| Outcomes | Taft Anderson job stress questionnaire |
| Notes | Article in Persian awaiting translation |
Goktas 2022.
| Methods | Randomised controlled trial |
| Participants | Nurses |
| Interventions | Motivational Messages Sent to Emergency Nurses During the COVID‐19 Pandemic |
| Outcomes | The Job Satisfaction Scale, Compassion Fatigue Scale, and Communication Skills Scale |
| Notes | Selected with the updated search on the 26th of September 2022. |
Hata 2022.
| Methods | Randomised controlled trial |
| Participants | physicians, nurse practitioners, and certified nurse midwives. |
| Interventions | three monthly self‐facilitated groups for faculty |
| Outcomes | Burnout & work stress |
| Notes | Selected with the updated search on the 26th of September 2022. |
Hsieh 2022.
| Methods | Randomised controlled trial |
| Participants | Nurses |
| Interventions | Gong medication |
| Outcomes | Stress & burnout |
| Notes | Selected with the updated search on the 26th of September 2022. |
Imamura 2019.
| Methods | Randomised controlled trial |
| Participants | Nurses |
| Interventions | Internet cognitive behavioural therapy (iCBT) |
| Outcomes | depressive and anxiety symptoms, measured by using the Depression Anxiety and Stress Scales (DASS) |
| Notes |
Joshi 2022.
| Methods | Randomised controlled trial |
| Participants | Various healthcare workers |
| Interventions | Transcendental Meditation (TM) is a mantra meditation practice with potential efficacy in reducing stress. |
| Outcomes | Psychological distress measured by the Global Severity Index. Secondary outcomes included changes in burnout (measured by the Maslach Burnout Inventory), insomnia (measured by the Insomnia Severity Index), and anxiety (measured by the Generalized Anxiety Disorder‐7 scale). |
| Notes | Selected with the updated search on the 26th of September 2022. |
Klatt 2012.
| Methods | Randomised controlled trial |
| Participants | Surgical Intensive Care Unit (SICU) personnel |
| Interventions | Mindfulness‐based worksite intervention |
| Outcomes | Depression, Anxiety and Stress Scale (DASS‐21) |
| Notes | No full text available. |
Klatt 2022.
| Methods | Randomised controlled trial |
| Participants | Healthcare workers (not specified) |
| Interventions | Mindfulness Based Intervention (MBI), Mindfulness in Motion (MIM), |
| Outcomes | Burnout & perceived stress |
| Notes | Selected with the updated search on the 26th of September 2022. |
Lu 2020.
| Methods | Randomised controlled trial |
| Participants | pediatric nurses |
| Interventions | Balint group |
| Outcomes | MBI |
| Notes | Article in Chinese awaiting translation |
Montaner 2022.
| Methods | Randomised controlled trial |
| Participants | Dementia healthcare workers |
| Interventions | Acceptance and Commitment Therapy (ACT) |
| Outcomes | MBI |
| Notes | Selected with the updated search on the 26th of September 2022. |
Moss 2022.
| Methods | Randomised controlled trial |
| Participants | Healthcare Professionals |
| Interventions | Creative Arts Therapy |
| Outcomes | Burnout |
| Notes | Selected with the updated search on the 26th of September 2022. |
Perez 2022.
| Methods | Randomised controlled trial |
| Participants | Nurses |
| Interventions | Mindfulness‐Based Intervention |
| Outcomes | ProQol |
| Notes | Selected with the updated search on the 26th of September 2022. |
Purdie 2022.
| Methods | Randomised controlled trial |
| Participants | Resident Physicians |
| Interventions | Hybrid Mindful Awareness Practices ( |
| Outcomes | MBI |
| Notes | Selected with the updated search on the 26th of September 2022. |
Rogala 2016.
| Methods | Randomised controlled trial |
| Participants | Professionals working with trauma survivors |
| Interventions | web‐based intervention, “The Helpers’ Stress” |
| Outcomes | MBI |
| Notes | In Polish awaiting translaten |
Sasaki 2021.
| Methods | Randomised controlled trial |
| Participants | Nurses |
| Interventions | cognitive behavioral therapy |
| Outcomes | Utrecht Work Engagement Scale–9 item (UWES‐9) |
| Notes | Trial protocol checked bmjopen‐2018‐025138. In the trial protocol DASS stress is one of the outcomes but not reported in this article. |
Spilg 2022.
| Methods | Randomised controlled trial |
| Participants | Physicians |
| Interventions | The Stress Management and Resilience Training (SMART) program is an evidence‐based intervention designed to build resilience. |
| Outcomes | Stress |
| Notes | Selected with the updated search on the 26th of September 2022. |
Taft 2021.
| Methods | Randomised controlled trial |
| Participants | Cardiac surgery nurses |
| Interventions | Educational intervention |
| Outcomes | Nursing Stress Scale (NSS) |
| Notes | Article in Persian awaiting translation |
Taylor 2022.
| Methods | Randomised controlled trial |
| Participants | Healthcare workers |
| Interventions | Unguided, digital, mindfulness‐based self‐help (MBSH) |
| Outcomes | MBI |
| Notes | Selected with the updated search on the 26th of September 2022. |
Vajpeyee 2022.
| Methods | Randomised controlled trial |
| Participants | Healthcare workers |
| Interventions | Yoga and music intervention |
| Outcomes | Stress |
| Notes | Selected with the updated search on the 26th of September 2022. |
Valipour 2020.
| Methods | Randomised controlled trial |
| Participants | Nurses |
| Interventions | stress management training |
| Outcomes | The Job Stress Questionnaire |
| Notes | No full text available |
Xiao Yan 2019.
| Methods | ? |
| Participants | Psychiatric nurses |
| Interventions | drum circle activity combined with the psychological diary technique |
| Outcomes | stress |
| Notes | Article in Chinese awaiting translation |
Characteristics of ongoing studies [ordered by study ID]
Al‐Hammouri 2022.
| Study name | Al‐Hammouri |
| Methods | Randomised controlled trial |
| Participants | Inclusion criteria: 1) Jordanian nurses 2) at least one‐year experience in the workplace setting 3) don’t have previous experience with mindfulness meditation |
| Interventions | The intervention protocol is similar to the brief mindfulness‐based stress reduction program designed by Mackenzie (2006). He synthesises its main elements from Kabat‐Zinn's (1990) traditional mindfulness‐based stress reduction program. The participants will be recruited from nurses inside the hospital for the two intervention groups so that the 65 nurses will receive the mindfulness meditation session inside one of the hospital rooms equipped to deliver the intervention, and the second group of the 65 nurses who will receive the intervention in a natural setting outside the hospital (i.e. park or recreation centre, that will be decided based on the funding to be determined after getting the IRB approval). Intervention groups will practice mindfulness meditation once weekly for 4 weeks as a group (i.e. 4 sessions for each of the two interventional groups). There are no recommendations about group size in the literature, but we will use small group sizes between 10 and 20 participants in each session for convenience. Mindfulness‐based intervention trainers will guide the mindfulness meditation sessions, and each session is 30 minutes long. The intervention comprises four 30‐minute training sessions that cover the following topics: an introduction to mindfulness, typical barriers to practice, the repercussions of attachment and aversion to judging events, and methods for bringing mindfulness into one's daily life. The body scan, sitting meditation, and a brief three‐minute breathing exercise for use in times of acute stress were all experienced components of the sessions (Mackenzie et al., 2006; Poulin et al. 2008). In addition, the participants in the intervention groups will be instructed to practice mindfulness mediation individually at home for at least 10 minutes |
| Outcomes | Stress Overload Scale Depression will be measured using the Center for Epidemiologic Studies Depression Scale‐Revised (CESD‐R). |
| Starting date | 31/05/2022 |
| Contact information | Jordan University of Science & Technology P.O.Box 3030, Irbid 22110, Jordan Jordan mmalhammouri@just.edu.jo |
| Notes |
Baker 2015.
| Study name | NR |
| Methods | Randomised controlled trial |
| Participants | Healthcare workers of care homes |
| Interventions | Mindfulness‐based stress reduction (MBSR) |
| Outcomes | The Work Stress Inventory The Karasek Job Content Questionnaire |
| Starting date | ? |
| Contact information | |
| Notes |
Bateman 2020.
| Study name | STOPTHEBURN |
| Methods | Randomised controlled Trial |
| Participants | ICU clinicians & non‐physicians (nurses, pharmacists, therapists). |
| Interventions | debriefing |
| Outcomes | Maslach Burnout Inventory (MBI) Score. Patient Health Questionnaire 8 (PHQ‐8) and Generalized Anxiety Disorder 7‐item scale (GAD‐7). |
| Starting date | ? |
| Contact information | |
| Notes |
Bratt 2022.
| Study name | NR |
| Methods | Randomised controlled trial |
| Participants | Healthcare professionals |
| Interventions | Compassion course A cognitive behavioural stress management course |
| Outcomes | COPSOQ / PROQOL |
| Starting date | February 2021 |
| Contact information | Anna Bratt, Linnaeus University anna.bratt@lnu.se |
| Notes |
Jeffers 2017.
| Study name | Jeffers |
| Methods | Randomised controlled trial |
| Participants | Nurse currently rostered to work in the RBWH DEM Able to attend program |
| Interventions | A face‐to‐face self‐care intervention program designed and supervised by an accredited clinical psychologist with over 10 years of experience. Participants will be offered one of two weekly hospital based sessions of approximately 1 hour duration for 5 weeks (10 participants should be in each of the sessions) with a home program. |
| Outcomes | Stress will be measured using the Depression, Anxiety and Stress Scale‐21 Professional Quality of Life will be measured using the Professional Quality of Life Scale, version 5 (Pro‐QOL‐5) |
| Starting date | 23/10/2017 |
| Contact information | Ms Carol Jeffers
Butter field Street
Royal Brisbane and Women's Hospital
Herston QLD 4029 James.Hughes@health.qld.gov.au |
| Notes |
Kuribayashi 2019.
| Study name | NR |
| Methods | Randomised controlled trial |
| Participants | Nurses |
| Interventions | Internet‐based Cognitive Behavioral Therapy (iCBT) |
| Outcomes | Psychological distress |
| Starting date | ? |
| Contact information | kkuribayashi‐jans@umin.ac.jp |
| Notes |
Ng 2019.
| Study name | Brief Daily Body‐Mind‐Spirit Practice |
| Methods | Multi‐site randomised controlled trial |
| Participants | Community Mental Health Workers |
| Interventions | Brief Daily Body‐Mind‐Spirit Practice |
| Outcomes | Copenhagen Burnout Inventory |
| Starting date | ? |
| Contact information | SM Ng Department of Social Work and Social Administration, The University of Hong Kong, Pokfulam, Hong Kong |
| Notes |
Pérula‐de Torres 2019.
| Study name | MINDUUDD |
| Methods | Multicentre cluster‐randomised controlled trial |
| Participants | Community medicine physicians and nurses |
| Interventions | Mindfulness and self‐compassion 4‐session programme versus an 8‐session programme |
| Outcomes | |
| Starting date | June 2019 |
| Contact information | luisangel.perula@gmail.com |
| Notes |
Rees 2018.
| Study name | Mindful Self‐Care and Resiliency (MSCR) |
| Methods | Randomised controlled trial |
| Participants | Rural general practitioners |
| Interventions | Mindful Self‐Care and Resiliency (MSCR) |
| Outcomes | Compassion fatigue? |
| Starting date | ? |
| Contact information | C.Rees@curtin.edu.au |
| Notes |
Weiner 2020.
| Study name | REST |
| Methods | Randomised controlled trial |
| Participants | Healthcare workers during the COVID‐19 pandemic |
| Interventions | Online cognitive behavioural therapy program |
| Outcomes | Perceived Stress Scale (PSS) |
| Starting date | September 2021 |
| Contact information | weiner.l@gmail.com |
| Notes |
PSQ: Perceived Stress Questionnaire
Differences between protocol and review
In the previous version of this review titled "Preventing occupational stress in healthcare workers" (Ruotsalainen 2015) interventions were categorised into cognitive‐behavioural, mental and physical relaxation and organisational‐level interventions. We excluded interventions solely targeting organisational‐level stressors, such as work‐demands, variation at work, because they are covered by the Giga 2018 review. We think the new categorisation into focusing on the experience of stress, focusing away from the experience of stress, focusing on individual work‐related risk factors and any combination of these is more informative.
In the previous version of this review (Ruotsalainen 2015) stressors were pooled with stress symptoms. For example, a stressor such as the reward imbalance questionnaire or the Nursing Stress Scale was pooled with stress symptom questionnaires such as the Perceived Stress Scale (PSS)or the Maslach Burnout Inventory (MBI). We are of the opinion, that stressors and stress symptoms cannot be pooled in one meta‐analysis because these are two different constructs (van der Molen 2020). Stressor questionnaires measure organisational‐level risk factors such as, job demands, jobs control, workplace social support, whereas stress symptoms questionnaires such as the PSS focus on the individual's experience of stress (e.g. have you been angered because of things that were outside your control?) (Cohen 1983). Since we have excluded organisational‐level interventions, stressor questionnaires were also excluded.
In the previous version of this review (Ruotsalainen 2015) the review authors reported secondary outcomes of physiological parameters such as hair cortisol. We excluded these secondary outcomes as we think that these parameters cannot be interpreted, because there is no consensus on the validation of stress‐related physiological parameters (Schaafsma 2021).
In the previous version of this review (Ruotsalainen 2015) subgroup analyses were performed for type of healthcare worker. Since interventions targeting organisational‐level interventions were excluded because they are covered by the Giga 2018 review, we did not perform subgroup analysis by type of healthcare worker. We think that the individual‐level interventions work the same way for various healthcare workers (e.g. physicians, nurses), which makes this type of subgroup analysis redundant. We discussed the proposed subgroup analyses based on the duration and intensity of the intervention as stated in the original protocol (Marine 2000). However, no definitions were formulated a priori, and we discussed what a proper grouping would be. We concluded that dividing the studies in shorter or longer and intense or less intense interventions would be an arbitrary ‐ and possibly data driven ‐ approach. Moreover, such a grouping would ideally be based on a mixture of the duration and intensity of the intervention (e.g. number of sessions, the length of the sessions, homework assignments) and the compliance with the intervention. However, we explored whether the arbitrary cut‐off for duration of the intervention of 12 weeks shows an effect in effect size.
De Wijn (de Wijn 2022) found that stress management interventions for nurses in which the sample was exposed to the majority of the planned sessions reached greater effect sizes compared to interventions in which the compliance to the intervention/attendance to the planned sessions was lower. Although this finding should be interpreted with caution due to a lot of missing data, we explored if the effect sizes based on studies in which participants attended 80% or more of the scheduled sessions would differ from the studies were participants attended less than 80% of the scheduled sessions de Wijn 2022.
In the previous version of this review (Ruotsalainen 2015), the objective was formulated as: 'to evaluate the effectiveness of work‐ and person‐directed interventions compared to no intervention or alternative interventions in preventing stress at work in healthcare workers.' Since, healthcare workers have higher levels of stress compared to the general population we think that 'reduce stress' better describes what we want to study than 'preventing stress at work'. In our opinion, this is not really a difference between protocol and review, rather a semantic difference.
In the previous version of this review (Ruotsalainen 2015), the most intensive intervention was included in the analyses in the case of multiple arms. As recommended by the Cochrane Handbook, we have now combined groups to create a single pair‐wise comparison.
In the previous version of this review (Ruotsalainen 2015), the time frames of the measurement of outcomes were: (i) up to one month (ii) from one month to six months (iii) over six months. We have changed these time frames into short‐term defined as up to and including three months after the intervention has been completed, medium term defined as more than three months up to 12 months, and long term defined as 12 months or longer. The rationale here was to focus more on the long‐term effects.
In the previous version of this review (Ruotsalainen 2015), one missing standard deviation (SD) was imputed. We have now excluded studies from the meta‐analyses if missing SDs could not be provided by study authors or when they could not be calculated from the available data.
Contributions of authors
This update, 2023:
ST, LE, AL, AT, KN and HM screened the systematic search results for potential new studies to include.
ST, LE and AL extracted data from included studies.
ST and JB rebuilt the comparisons and ran the analyses.
The following review authors wrote parts of the first draft of the updated review text: ST (methods, results), LE (introduction), JB (abstract, plain language summary, summary of findings), RS (discussion ‐ overall completeness and applicability of evidence), KN (discussion ‐ agreements and disagreements with other studies or reviews) and HM (discussion ‐ quality of evidence and potential biases in the review process). All review authors commented on the draft.
2015 version of the review:
JR, AM, JV and CS screened the systematic search results for potential new studies to include.
JR, AM, CS and JV extracted data from new included studies and also assessed the risk of bias of the previously included studies.
JR and JV rebuilt the comparisons and ran the analyses.
JV and JR wrote the first draft of the updated review text.
All authors commented on the draft.
JR is the guarantor of the review.
Sources of support
Internal sources
-
Amsterdam UMC location University of Amsterdam, Public and Occupational Health, Meibergdreef 9, Amsterdam, The Netherlands, Netherlands
Personnel
External sources
-
National Institute for Health Research (NIHR), UK
An incentive grant to support the production of this review was distributed between the authors and the Cochrane review group.
Declarations of interest
ST: has declared no conflict of interest.
LE: has declared no conflict of interest.
JB: employed as Managing Editor for Cochrane Work up to July 2022. JB was not involved in the editorial process from that moment on.
AL: has declared no conflict of interest.
AT: has declared no conflict of interest.
JR: has declared no conflict of interest.
RS: has declared no conflict of interest.
KN: reports to be involved in a study eligible for inclusion (Gärtner 2013). KN was not involved in assessing this study for eligibility, it's data extraction or bias assessment.
HM: has declared no conflict of interest.
Cochrane Work managed the editorial process for this review. The author team had no influence on how the editorial team managed this review.
These authors contributed equally to this work.
Edited (no change to conclusions)
References
References to studies included in this review
Alexander 2015 {published data only}
- Alexander GA, Rollins K, Walker D, Wong L, Pennings J. Yoga for self-care and burnout prevention among nurses. Workplace Health & Safety 2015;63(10):462-70. [DOI: doi: 10.1177/2165079915596102.] [DOI] [PubMed] [Google Scholar]
Amutio 2015 {published data only}
- Amutio A, Martinez-Taboada C, Delgado LC, Hermosilla Dl, Mozaz MJ. Acceptability and effectiveness of a long-term educational intervention to reduce physicians' stress-related conditions. Journal of Continuing Education in the Health Professions 2015;35(4):255-60. [DOI: ] [DOI] [PubMed] [Google Scholar]
Aranda Ausern 2016 {published data only}
- Aranda Auserón G, Elcuaz Viscarret MR, Fuertes Goñi C, Güeto Rubio V, Pascual Pascual P, Sainz de Murieta García de Galdeano E. Evaluation of the effectiveness of a Mindfulness and Self-Compassion program to reduce stress and prevent burnout in Primary Care health professionals [Evaluación de la efectividad de un programa de mindfulness y autocompasión para reducir el estrés y prevenir el burnout en profesionales sanitarios de atención primaria]. Atencion Primaria 2018;50(3):141-50. [DOI: 10.1016/j.aprim.2017.03.009] [DOI] [PMC free article] [PubMed] [Google Scholar]
Axisa 2019 {published data only}
- Axisa C, Nash L, Kelly P, Willcock S. Burnout and distress in Australian physician trainees: Evaluation of a wellbeing workshop. Australasian Psychiatry: Bulletin of Royal Australian and New Zealand College of Psychiatrists 2019;27(3):255-61. [DOI: ] [DOI] [PubMed] [Google Scholar]
Bagheri 2019 {published data only}
- Bagheri T, Fatemi MJ, Payandan H, Skandari A, Momeni M. The effects of stress-coping strategies and group cognitive-behavioral therapy on nurse burnout. Annals of Burns and Fire Disasters 2019;32(3):184-9. [PMC free article] [PubMed] [Google Scholar]
Barattucci 2019 {published data only}
- Barattucci M, Padovan AM, Vitale E, Rapisarda V, Ramaci T, De Giorgio A. Mindfulness-based IARA model R proves effective to reduce stress and anxiety in health care professionals. A six-month follow-up study. International Journal of Environmental Research and Public Health 2019;16(22):4421. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Barbosa 2015 {published data only}
- Barbosa A, Nolan M, Sousa L, Figueiredo D. Supporting direct care workers in dementia care: effects of a psychoeducational intervention. American Journal of Alzheimer's Disease & Other Dementias 2015;30 (2):130-8. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbosa A, Nolan M, Sousa L, Marques A, Figueiredo D. Effects of a psychoeducational intervention for direct care workers caring for people with dementia: results from a 6-month follow-up study. American Journal of Alzheimer's Disease & Other Dementias 2015;31(2):144-55. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Behnammoghadam 2019 {published data only}
- Behnammoghadam M, Kheramine S, Zoladl M, Cooper RZ, Shahini S. Effect of eye movement desensitization and reprocessing (EMDR) on severity of stress in emergency medical technicians. Psychology Research and Behavior Management 2019;12:289-96. [DOI: 10.2147/PRBM.S190428] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bernburg 2019 {published data only}
- Bernburg M, Groneberg DA, Mache S. Mental health promotion intervention for nurses working in German psychiatric hospital departments: a pilot study. Issues in Mental Health Nursing 2019;40(8):706-11. [DOI: 10.1080/01612840.2019.1565878] [DOI] [PubMed] [Google Scholar]
Bernburg 2020 {published data only}
- Bernburg M, Groneberg D, Mache. Professional training in mental health self-care for nurses starting work in hospital departments. Work (Reading, Mass.) 2020;67(3):583-90. [DOI: ] [DOI] [PubMed] [Google Scholar]
Brazier 2022 {published data only}
- Brazier A, Larson E, Xu Y, Judah G, Egan M, Burd H, et al. 'Dear Doctor': a randomised controlled trial of a text message intervention to reduce burnout in trainee anaesthetists. Anaesthesia 2022;77(4):405-15. [DOI: ] [DOI] [PubMed] [Google Scholar]
Brennan 2006 {published data only}
- Brennan MK, DeBate RD. The effect of chair massage on stress perception of hospital bedside. Journal of Bodywork and Movement Therapies 2006;10(4):335-42. [Google Scholar]
CezardaCosta 2019 {published data only}
- Cezar da Costa MV, da Silva Filho JN, Lírio Gurgel J, Porto F. Stretching exercises in perception of stress in nursing professionals: randomised clinical trial. Brazilian Journal of Occupational Therapy / Cadernos Brasileiros de Terapia Ocupacional 2019;27(2):357-66. [DOI: 10.4322/2526-8910.ctoAO1696] [DOI] [Google Scholar]
Chen 2015 {published data only}
- Chen MC, Fang SH, Fang L. The effects of aromatherapy in relieving symptoms related to job stress among nurses. International Journal of Nursing Practice 2015;21(1):87-93. [DOI: ] [DOI] [PubMed] [Google Scholar]
Cheng 2015 {published data only}
- Cheng ST, Tsui PK, Lam JH. Improving mental health in health care practitioners: randomized controlled trial of a gratitude intervention. Journal of Consulting and Clinical Psychology 2015;83(1):177-86. [DOI: 10.1037/a0037895] [DOI] [PubMed] [Google Scholar]
Chesak 2020 {published data only}
- Chesak SS, Bhagra A, Cutshall S, Ingram A, Benoit R, Medina-Inojosa JR, et al. Authentic connections groups: a pilot test of an intervention aimed at enhancing resilience among nurse leader mothers. Worldviews on Evidence-Based Nursing 2020;17(1):39-48. [DOI: ] [DOI] [PubMed] [Google Scholar]
Cho 2021 {published data only}
- Cho Y, Joo, JM, Kim S, Sok S. Effects of meridian acupressure on stress, fatigue, anxiety, and self-efficacy of shiftwork nurses in south korea. International Journal of Environmental Research and Public Health 2021;18(8):4199. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cohen‐Katz 2005 {unpublished data only}
- Cohen-Katz J, Wiley SD, Capuano T, Baker DM, Kimmel S, Shapiro S. The effects of mindfulness-based stress reduction on nurse stress and burnout, Part II: a quantitative and qualitative study. Holistic Nursing Practice 2005;19(1):26-35. [DOI] [PubMed] [Google Scholar]
Concilio 2021 {published data only}
- Concilio L, Lockhart JS, Kronk R, Oermann M, Brannan J, Schreiber JB. Impact of a digital intervention on perceived stress, resiliency, social support, and intention to leave among newly licensed graduate nurses: a randomized controlled trial. Journal of Continuing Education in Nursing 2021;52(8):367-74. [DOI: 10.3928/00220124-20210714-06] [DOI] [PubMed] [Google Scholar]
Copeland 2021 {published data only}
- Copeland D. Brief workplace interventions addressing burnout, compassion fatigue, and teamwork: a pilot study. Western Journal of Nursing Research 2021;43(2):130-7. [DOI: 10.1177/0193945920938048] [DOI] [PubMed] [Google Scholar]
Dahlgren 2022 {published data only}
- Dahlgren A, Tucker P, Epstein M, Gustavsson P, Soderstrom M. Randomised control trial of a proactive intervention supporting recovery in relation to stress and irregular work hours: effects on sleep, burn-out, fatigue and somatic symptoms. Occupational and Environmental Medicine 2022;79:460-8. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
deSouza 2021 {published data only}
- Souza TP, Kurebayashi LF, Souza-Talarico JN, Turrini RN. The effectiveness of chair massage on stress and pain in oncology. International Journal of Therapeutic Massage & Bodywork 2021;14(3):27-38. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dincer 2021 {published data only}
- Dincer B, Inangil D. The effect of Emotional Freedom Techniques on nurses' stress, anxiety, and burnout levels during the COVID-19 pandemic: a randomized controlled trial. Explore 2021;17(2):109-14. [DOI: 10.1016/j.explore.2020.11.012] [DOI] [PMC free article] [PubMed] [Google Scholar]
Duchemin 2015 {published data only}
- Duchemin AM, Steinberg BA, Marks DR, Vanover K, Klatt M. A small randomized pilot study of a workplace mindfulness-based intervention for surgical intensive care unit personnel: effects on salivary α-amylase levels. Journal of Occupational and Environmental Medicine 2015;57(4):393-9. [DOI: 10.1097/JOM.0000000000000371] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dunne 2019 {published and unpublished data}
- Dunne PJ, Lynch J, Prihodova L, O'Leary C, Ghoreyshi A, Basdeo SA. Burnout in the emergency department: Randomized controlled trial of an attention-based training program. Journal of Integrative Medicine 2019;17(3):173-80. [DOI: 10.1016/j.joim.2019.03.009] [DOI] [PubMed] [Google Scholar]
Dyrbye 2016 {published data only}
- Dyrbye LN, West CP, Richards ML, Ross HJ, Satele D, Shanafelt TD. A randomized, controlled study of an online intervention to promote job satisfaction and well-being among physicians. Burnout Research 2016;3(3):69-75. [DOI: ] [Google Scholar]
Dyrbye 2019 {published and unpublished data}
- Dyrbye LN, Shanafelt TD, Gill PR, Satele DV, West CP. Effect of a professional coaching intervention on the well-being and distress of physicians: a pilot randomized clinical trial. JAMA Internal Medicine 2019;179(10):1406-14. [DOI: 10.1001/jamainternmed.2019.2425] [DOI] [PMC free article] [PubMed] [Google Scholar]
ElKhamali 2018 {published data only}
- El Khamali R, Mouaci A, Valera S, Cano-Chervel M, Pinglis C, Sanz C. Effects of a multimodal program including simulation on job strain among nurses working in intensive care units: a randomized clinical trial. JAMA 2018;320(19):1988-97. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Emani 2020 {published data only}
- Emani R, Ghavami H, Radfar M, Reza Khalkhali H. Impact of chromotherapy on professional quality of life in intensive care unit nurses: a randomized controlled trial. Fatigue: Biomedicine, Health and Behavior 2020;8(3):121-9. [DOI: 10.1080/21641846.2020.1782058] [DOI] [Google Scholar]
Errazuriz 2022 {published and unpublished data}
- Errazuriz A, Schmidt K, Undurraga EA, Medeiros S, Baudrand R, Cussen D, et al. Effects of mindfulness-based stress reduction on psychological distress in health workers: a three-arm parallel randomized controlled trial. Journal of Psychiatric Research 2022;145:284-93. [DOI: 10.1016/j.jpsychires.2020.11.011] [DOI] [PubMed] [Google Scholar]
Ewers 2002 {published data only}
- Ewers P, Bradshaw T, McGovern J, Ewers B. Does training in psychosocial interventions reduce burnout rates in forensic nurses? Journal of Advanced Nursing 2002;37(5):470-6. [DOI] [PubMed] [Google Scholar]
Fendel 2021 {published data only}
- Fendel JC, Aeschbach VM, Schmidt S, Göritz AS. The impact of a tailored mindfulness-based program for resident physicians on distress and the quality of care: A randomised controlled trial. Journal of Internal Medicine 2021;290(6):1233-48. [DOI: 10.1111/joim.13374] [DOI] [PubMed] [Google Scholar]
Finnema 2005 {published data only}
- Finnema E, Droes RM, Ettema T, Ooms M, Ader H, Ribbe M, et al. The effect of integrated emotion-oriented care versus usual care on elderly persons with dementia in the nursing home and on nursing assistants: a randomized clinical trial. International Journal of Geriatric Psychiatry 2005;20(4):330-43. [DOI] [PubMed] [Google Scholar]
Fiol DeRoque 2021 {published data only}
- Fiol-DeRoque MA, Serrano-Ripoll MJ, Jiménez R, Zamanillo-Campos R, Yáñez-Juan AM, Bennasar-Veny M, et al. A mobile phone-based intervention to reduce mental health problems in health care workers during the COVID-19 pandemic (PsyCovidApp): randomized controlled trial. JMIR mHealth and uHealth 2021;9(5):- . [DOI: 10.2196/27039] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serrano-Ripoll MJ, Ricci-Cabello I, Jiménez R, Zamanillo-Campos R, Yañez-Juan AM, Bennasar-Veny M, et al. Effect of a mobile-based intervention on mental health in frontline healthcare workers against COVID-19: Protocol for a randomized controlled trial. Journal of Advanced Nursing 2021;77(6):2898-907. [DOI] [PMC free article] [PubMed] [Google Scholar]
Foji 2020 {published data only}
- Foji S, Vejdani M, Salehiniya H, Khosrorad R. The effect of emotional intelligence training on general health promotion among nurse. Journal of Education and Health Promotion 2020;9:4. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Frogeli 2020 {published data only}
- Frogeli E, Rudman A, Ljotsson B, Gustavsson P. Preventing stress-related ill health among new registered nurses by supporting engagement in proactive behaviors - a randomized controlled trial. Worldviews on Evidence-Based Nursing 2020;17(3):202-12. [DOI: ] [DOI] [PubMed] [Google Scholar]
Gärtner 2013 {published and unpublished data}
- Bolier L, Ketelaar SM, Nieuwenhuijsen K, Smeets O, Gartner FR, Sluiter JK. Workplace mental health promotion online to enhance well-being of nurses and allied health professionals: a cluster-randomized controlled trial. Internet Interventions 2014;1(4):196-204. [DOI: 10.1016/j.invent.2014.10.002] [DOI] [Google Scholar]
- Gärtner FR, Nieuwenhuijsen K, Ketelaar SM, Van Dijk FJ, Sluiter JK. The Mental Vitality @ Work Study: effectiveness of a mental module for workers E-health surveillance for nurses and allied health care professionals on their help-seeking behavior. Journal of Occupational and Environmental Medicine 2013;55(10):1219-29. [DOI] [PubMed] [Google Scholar]
- Ketelaar SM, Gärtner FR, Bolier L, Smeets O, Nieuwenhuijsen K, Sluiter JK. Mental Vitality @ Work--a workers' health surveillance mental module for nurses and allied health care professionals: process evaluation of a randomized controlled trial. Journal of Occupational and Environmental Medicine 2013;55(5):563-71. [DOI] [PubMed] [Google Scholar]
- Ketelaar SM, Nieuwenhuijsen K, Gärtner FR, Bolier L, Smeets O, Sluiter JK. Effect of an E-mental health approach to workers' health surveillance versus control group on work functioning of hospital employees: a cluster-RCT. PLoS ONE 2013;8(9):- . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noben C, Smit F, Nieuwenhuijsen K, Ketelaar S, Gartner F, Boon B, et al. Comparative cost-effectiveness of two interventions to promote work functioning by targeting mental health complaints among nurses: pragmatic cluster randomised trial. International Journal of Nursing Studies 2014;51(10):1321-31. [DOI: ] [DOI] [PubMed] [Google Scholar]
Ghawadra 2020 {published data only}
- Ghawadra SF, Lim Abdullah K, Choo WY, Danaee M, Phang CK. The effect of mindfulness-based training on stress, anxiety, depression and job satisfaction among ward nurses: a randomized control trial. Journal of Nursing Management 2020;28(5):1088-97. [DOI: 10.1111/jonm.13049] [DOI] [PubMed] [Google Scholar]
Gollwitzer 2018 {published data only}
- Gollwitzer PM, Mayer D, Frick C, Oettingen G. Promoting the self-regulation of stress in health care providers: an internet-based intervention. Frontiers in Psychology 2018;9:838. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Grabbe 2020 {published data only}
- Grabbe L, Higgins MK, Baird M, Craven PA, San Fratello S. The Community Resiliency Model R to promote nurse well-being. Nursing Outlook 2020;68(3):324-36. [DOI: ] [DOI] [PubMed] [Google Scholar]
Gunasingam 2015 {published data only}
- Gunasingam N, Burns K, Edwards J, Dinh M, Walton M. Reducing stress and burnout in junior doctors: the impact of debriefing sessions. Postgraduate Medical Journal 2015;91(1074):182-7. [DOI: 10.1136/postgradmedj-2014-132847] [DOI] [PubMed] [Google Scholar]
Günüsen 2010 {published data only}
- Gunusen N, Ustun B. Support groups to reduce burnout among nurses [An RCT of coping and support groups to reduce burnout among nurses]. International Nursing Review 2010 2010;57(4):485-92. [DOI] [PubMed] [Google Scholar]
Hersch 2016 {published data only}
- Hersch RK, Cook RF, Deitz DK, Kaplan S, Hughes D, Friesen MA, et al. Reducing nurses' stress: a randomized controlled trial of a web-based stress management program for nurses. Applied Nursing Research 2016;32:18-25. [DOI: 10.1016/j.apnr.2016.04.003] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hilcove 2021 {published data only}
- Hilcove K, Marceau C, Thekdi P, Larkey L, Brewer MA, Jones K. Holistic nursing in practice: mindfulness-based yoga as an intervention to manage stress and burnout. Journal of Holistic Nursing 2021;39(1):29-42. [DOI: 10.1177/0898010120921587] [DOI] [PubMed] [Google Scholar]
Ho 2021 {published data only}
- Ho AHY, Tan-Ho G, Ngo TA, Ong G, Chong PH, Dignadice D, et al. A novel mindful-compassion art therapy (MCAT) for reducing burnout and promoting resilience for end-of-life care professionals: a waitlist RCT protocol. Trials 2019;20(1):406. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho AHY, Tan-Ho G, Ngo TA, Ong G, Chong PH, Dignadice D, et al. A novel mindful-compassion art-based therapy for reducing burnout and promoting resilience among healthcare workers: findings from a waitlist randomized control trial. Frontiers in Psychology 2021;12:744443. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Huang 2020 {published data only}
- Huang H, Zhang H, Xie Y, Wang SB, Cui H, Li L, et al. Effect of Balint group training on burnout and quality of work life among intensive care nurses: a randomized controlled trial. Neurology Psychiatry and Brain Research 2020;35:16-21. [DOI: 10.1016/j.npbr.2019.12.002] [DOI] [Google Scholar]
Huang 2020a {published data only}
- Huang, L, Harsh, J, Cui, H, Wu, J, Thai, J, Zhang, X, et al. A randomized controlled trial of Balint groups to prevent burnout among residents in China. Frontiers in Psychiatry 2020;10:- . [DOI: 10.3389/fpsyt.2019.00957] [DOI] [PMC free article] [PubMed] [Google Scholar]
Janzarik 2022 {published data only}
- Janzarik G, Wollschlager D, Wessa M, Lieb K. A group intervention to promote resilience in nursing professionals: a randomised controlled trial. International Journal of Environmental Research and Public Health 2022;19(2):649. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Jensen 2006 {published and unpublished data}
- Jensen LD, Gonge H, Jors E, Ryom P, Foldspang A, Christensen MA, et al. Prevention of low back pain in female eldercare workers: randomized controlled work site trial. Spine 2006;31(16):1761-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Kavurmaci 2022 {published data only}
- Kavurmaci M, Tan M, Bahcecioglu Turan G. Determining the effect of yoga on job satisfaction and burnout of nurse academicians. Perspectives in Psychiatric Care 2022;58(1):404-10. [DOI: ] [DOI] [PubMed] [Google Scholar]
Kesselheim 2020 {published data only}
- Kesselheim J, Baker JN, Kersun L, Lee-Miller C, Moerdler S, Snaman JM, et al. Humanism and professionalism training for pediatric hematology-oncology fellows: results of a multicenter randomized trial. Pediatric Blood & Cancer 2020;67(11):e28308. [DOI: 10.1002/pbc.28308] [DOI] [PubMed] [Google Scholar]
Kharatzadeh 2020 {published data only}
- Kharatzadeh H, Alavi M, Mohammadi A, Visentin D, Cleary M. Emotional regulation training for intensive and critical care nurses. Nursing and Health Sciences 2020;22(2):445-53. [DOI: 10.1111/nhs.12679] [DOI] [PubMed] [Google Scholar]
Kim 2016 {published data only}
- Kim YI, Kim SM, Kim H, Han DH. The effect of high-frequency repetitive transcranial magnetic stimulation on occupational stress among health care workers: a pilot study. Psychiatry Investigation 2016;13(6):622-9. [DOI: 10.4306/pi.2016.13.6.622] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kline 2020 {published and unpublished data}
- Kline JA, VanRyzin K, Davis JC, Parra JA, Todd ML, Shaw LL, et al. Randomized trial of therapy dogs versus deliberative coloring (art therapy) to reduce stress in emergency medicine providers. Academic Emergency Medicine 2020;27(4):266-75. [DOI: 10.1111/acem.13939] [DOI] [PubMed] [Google Scholar]
Kurebayashi 2012 {published data only}
Kurebayashi 2014 {published data only}
- Kurebayashi LF, Silva MJ. Efficacy of Chinese auriculotherapy for stress in nursing staff: a randomized clinical trial. Revista Latino-Americana de Enfermagem 2014;22(3):371-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurebayashi LF, da Silva MJ. Chinese auriculotherapy to improve quality of life of nursing team. Revista Brasileira de Enfermagem 2015;68(1):109-15, 117-23. [DOI: 10.1590/0034-7167.2015680116p] [DOI] [PubMed] [Google Scholar]
Leao 2017 {published data only}
- Leao ER, Dal Fabbro DR, Oliveira RB, Santos IR, Victor ED, Aquarone RL, et al. Stress, self-esteem and well-being among female health professionals: A randomized clinical trial on the impact of a self-care intervention mediated by the senses. PLOS One 2017;12(2):e0172455. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lebares 2021 {published data only}
- Lebares CC, Coaston TN, Delucchi KL, Guvva EV, Shen WT, Staffaroni AM, et al. Enhanced stress resilience training in surgeons: iterative adaptation and biopsychosocial effects in 2 small randomized trials. Annals of Surgery 2021;273(3):424-32. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lee 1994 {published data only}
- Lee S, Crockett MS. Effect of assertiveness training on levels of stress and assertiveness experienced by nurses in Taiwan, Republic of China. Issues in Mental Health Nursing 1994;15(4):419-32. [DOI] [PubMed] [Google Scholar]
Lee 2020 {published data only}
- Lee S, Rozybakieva Z, Asimov M, Bagiyarova F, Tazhiyeva A, Ussebayeva N, et al. Coping strategy as a way to prevent emotional burnout in primary care doctors: a randomized controlled trial. Archives of the Balkan Medical Union 2020;55(3):398-409. [DOI: 10.31688/ABMU.2020.55.3.05] [DOI] [Google Scholar]
Lee 2021 {published data only}
- Lee SN, Kim B, Park H. The effects of auricular acupressure on stress, anxiety, and depression of outpatient nurses in South Korea. Complementary Therapies in Clinical Practice 2021;44:101797. [DOI: 10.1016/j.ctcp.2021.101447] [DOI] [PubMed] [Google Scholar]
Lin 2015 {published data only}
- Lin Shu-Ling, Huang CY, Shiu SP, Yeh SH. Effects of yoga on stress, stress adaption, and heart rate variability among mental health professionals - a randomized controlled trial. Worldviews on Evidence-Based Nursing 2015;12(4):236-45. [DOI: ] [DOI] [PubMed] [Google Scholar]
Lin 2019 {published data only}
- Lin L, He G, Yan J, Gu C, Xie J. The effects of a modified mindfulness-based stress reduction program for nurses: a randomized controlled trial. Workplace Health & Safety 2019;67(3):111-22. [DOI: ] [DOI] [PubMed] [Google Scholar]
Luthar 2017 {published data only}
- Luthar SS, Curlee A, Tye SJ, Engelman JC, Stonnington CM. Fostering resilience among mothers under stress: “Authentic Connections Groups” for Medical Professionals. Women's Health Issues 2017;27(3):382-90. [DOI: 10.1016/j.whi.2017.02.007] [DOI] [PubMed] [Google Scholar]
Mache 2015 {published data only}
- Mache S, Vitzthum K, Klapp BF, Groneberg DA. Evaluation of a multicomponent psychosocial skill training program for junior physicians in their first year at work: a pilot study. Family Medicine 2015;47(9):693-8. [PubMed] [Google Scholar]
Mache 2016 {published data only}
- Mache S, Bernburg M, Baresi L, Groneberg DA, Bamberger B, Bradshaw B, et al. Evaluation of self-care skills training and solution-focused counselling for health professionals in psychiatric medicine: A pilot study. International Journal of Psychiatry in Clinical Practice 2016;20(4):239-44. [DOI: ] [DOI] [PubMed] [Google Scholar]
Mache 2017 {published data only}
- Mache S, Vitzthum K, Hauschild I, Groneberg D. A pilot study evaluation of psychosocial competency training for junior physicians working in oncology and hematology. Psycho-oncology 2017;26:1894– 900. [DOI: 10.1002/pon.4403] [DOI] [PubMed] [Google Scholar]
Mache 2018 {published data only}
- Mache S, Bernburg M, Baresi L, Groneberg D. Mental health promotion for junior physicians working in emergency medicine: evaluation of a pilot study. European Journal of Emergency Medicine: Official Journal of the European Society for Emergency Medicine 2018;25(3):191-8. [DOI: ] [DOI] [PubMed] [Google Scholar]
Mackenzie 2006 {published data only}
- Mackenzie CS, Poulin PA, Seidman-Carlson R. A brief mindfulness-based stress reduction intervention for nurses and nurse aides. Applied Nursing Research 2006;19(2):105-9. [DOI] [PubMed] [Google Scholar]
Mandal 2021 {published data only}
- Mandal S, Misra P, Sharma G, Sagar R, Kant S, Dwivedi SN, et al. Effect of structured yoga program on stress and professional quality of life among nursing ataff in a tertiary care hospital of Delhi—a small scale phase-II trial. Journal of Evidence-Based Integrative Medicine 2021;26:1-10. [DOI: 10.1177/2515690X21991998] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mao 2021 {published data only}
- Mao L, Huang L, Chen Q. Promoting resilience and lower stress in nurses and improving inpatient experience through emotional intelligence training in China: a randomized controlled trial. Nurse Education Today 2021;107:Epub. [DOI: 10.1016/j.nedt.2021.105130] [DOI] [PubMed] [Google Scholar]
Martins 2011 {published data only}
- Martins AE, Davenport MC, Del Valle MD, Di Lalla S, Dominguez P, Ormando L, et al. Impact of a brief intervention on the burnout levels of pediatric residents. Jornal de Pediatria 2011;87(6):493-8. [DOI] [PubMed] [Google Scholar]
McConachie 2014 {published data only}
- McConachie DA, McKenzie K, Morris PG, Walley RM. Acceptance and mindfulness-based stress management for support staff caring for individuals with intellectual disabilities. Research in Developmental Disabilities 2014;35(6):1216-27. [DOI: 10.1016/j.ridd.2014.03.005] [DOI] [PubMed] [Google Scholar]
McGonagle 2020 {published data only}
- McGonagle AK, Schwab L, Yahanda N, Duskey H, Gertz N, Prior L, et al. Coaching for primary care physician well-being: A randomized trial and follow-up analysis. Journal of Occupational Health Psychology 2020;25(5):297-314. [DOI: ] [DOI] [PubMed] [Google Scholar]
Mealer 2014 {published data only}
- Mealer M, Conrad D, Evans J, Jooste K, Solyntjes J, Rothbaum B, et al. Feasibility and acceptability of a resilience training program for intensive care unit nurses. American Journal of Critical Care 2014;23(6):e97-105. [DOI: 10.4037/ajcc2014747] [DOI] [PubMed] [Google Scholar]
Medisauskaite 2019 {published data only}
- Medisauskaite A, Kamau C. Reducing burnout and anxiety among doctors: randomized controlled trial. Psychiatry Research 2019;274:383-90. [DOI: 10.1016/j.psychres.2019.02.075] [DOI] [PubMed] [Google Scholar]
Melchior 1996 {published data only}
- Melchior ME, Philipsen H, Abu-Saad HH, Halfens RJ, Van De Berg AA, Gassman P. The effectiveness of primary nursing on burnout among psychiatric nurses in long-stay settings. Journal of Advanced Nursing 1996;24(4):694-702. [DOI] [PubMed] [Google Scholar]
Moench 2021 {published data only}
- Moench J, Billsten O. Randomized controlled trial: self-care Traumatic episode protocol, computerized EMDR treatment of COVID-19-related stress. Journal of EMDR Practice and Research 2021;15(2):99-113. [DOI: 10.1891/EMDR-D-20-00047] [DOI] [Google Scholar]
Montaner 2021 {published data only}
- Montaner X, Tarrega S, Pulgarin M, Moix J. Effectiveness of acceptance and commitment therapy (ACT) in professional dementia caregivers burnout. Clinical Gerontologist 2021;45:1-12. [DOI: ] [DOI] [PubMed] [Google Scholar]
Montibeler 2018 {published data only}
- Montibeler J, Domingos TS, Braga EM, Gnatta JR, Kurebayashi LFS, Kurebayashi AK. Effectiveness of aromatherapy massage on the stress of the surgical center nursing team: a pilot study. Efetividade da massagem com aromaterapia no estresse da equipe de enfermagem do centro cirurgico: estudo-piloto 2018;52:03348. [DOI: ] [DOI] [PubMed] [Google Scholar]
Moody 2013a {published and unpublished data}
- Moody K, Kramer D, Santizo RO, Magro L, Wyshogrod D, Ambrosio J, et al. Helping the helpers: mindfulness training for burnout in pediatric oncology--a pilot program. Journal of Pediatric Oncology Nursing 2013;30(5):275-84. [DOI] [PubMed] [Google Scholar]
Norvell 1987 {published data only}
- Norvell N, Belles D, Brody S, Freund A. Worksite stress management for medical care personnel: results from a pilot program. Journal for Specialists in Group Work 1987;57:118-26. [Google Scholar]
Novoa 2014 {published data only}
- Novoa MP, Cain DS. The effects of reiki treatment on mental health professionals at risk for secondary traumatic stress: a placebo control study. Best Practices in Mental Health: An International Journal 2014;10(1):31-46. [Google Scholar]
OBrien 2019 {published data only}
- O'Brien WH, Singh WS, Horan K, Moeller MT, Wasson R, Jex SM. Group-based acceptance and commitment therapy for nurses and nurse aides working in long-term care residential settings. Journal of Alternative and Complementary Medicine (New York, N.Y.) 2019;25(7):753-61. [DOI: ] [DOI] [PubMed] [Google Scholar]
Oman 2006 {published data only}
- Oman D, Hedberg J, Thoresen CE. Passage meditation reduces perceived stress in health professionals: A randomized, controlled trial. Journal of Consulting and Clinical Psychology 2006;74(4):714-9. [DOI] [PubMed] [Google Scholar]
Ozbas 2016 {published data only}
- Ozbas AA, Tel H. The effect of a psychological empowerment program based on psychodrama on empowerment perception and burnout levels in oncology nurses: Psychological empowerment in oncology nurses. Palliative & Supportive Care 2016;14(4):393-401. [DOI: ] [DOI] [PubMed] [Google Scholar]
Ozgundondu 2019 {published data only}
- Ozgundondu B, Gok MZ. Effects of progressive muscle relaxation combined with music on stress, fatigue, and coping styles among intensive care nurses. Intensive & Critical Care Nursing 2019;54:54-63. [DOI: 10.1016/j.iccn.2019.07.007] [DOI] [PubMed] [Google Scholar]
Palumbo 2012 {published data only}
- Palumbo MV, Wu G, Shaner-McRae H, Rambur B, McIntosh B. Tai Chi for older nurses: a workplace wellness pilot study. Applied Nursing Research 2012;25(1):54-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pehlivan 2020 {published and unpublished data}
- Pehlivan T, Güner P. Effect of a compassion fatigue resiliency program on nurses’ professional quality of life, perceived stress, resilience: a randomized controlled trial. Journal of Advanced Nursing 2020;76(12):3584-96. [DOI: 10.1111/jan.14568] [DOI] [PubMed] [Google Scholar]
PelitAksu 2020 {published data only}
- Pelit‐Aksu S, Özkan‐Şat S, Yaman‐Sözbi̇r S, Şentürk‐Erenel A. Effect of progressive muscle relaxation exercise on clinical stress and burnout in student nurse interns. Perspectives in Psychiatric Care 2020;57 ((3)):1095-102. [DOI: 10.1111/ppc.12662] [DOI] [PubMed] [Google Scholar]
Peterson 2008 {published data only}
- Peterson U, Bergstrom G, Samuelsson M, Asberg M, Nygren A. Reflecting peer-support groups in the prevention of stress and burnout: randomized controlled trial. Journal of Advanced Nursing 2008;63(5):506-16. [DOI] [PubMed] [Google Scholar]
Prado 2018 {published data only}
- Prado JM, Kurebayashi LF, Silva MJ. Experimental and placebo auriculotherapy for stressed nurses: randomized controlled trial. Auriculoterapia verdadeira e placebo para enfermeiros estressados: ensaio clinico randomizado 2018;52:e03334. [DOI: ] [DOI] [PubMed] [Google Scholar]
Redhead 2011 {published data only}
- Redhead K, Bradshaw T, Braynion P, Doyle M. An evaluation of the outcomes of psychosocial intervention training for qualified and unqualified nursing staff working in a low-secure mental health unit. Journal of Psychiatric and Mental Health Nursing 2011;18(1):59-66. [DOI] [PubMed] [Google Scholar]
Reynolds 1993 {published data only}
- Reynolds S, Taylor E, Shapiro D. Session impact and outcome in stress management-training. Journal of Community & Applied Social Psychology 1993;3(4):325-37. [Google Scholar]
Riley 2017 {published data only}
- Riley KE, Park CL, Wilson A, Sabo AN, Antoni MH, Braun TD, et al. Improving physical and mental health in frontline mental health care providers: yoga-based stress management versus cognitive behavioral stress management. Journal of Workplace Behavioral Health 2017;32(1):26-48. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Saganha 2012 {published data only}
- Saganha JP, Doenitz C, Greten T, Efferth T, Greten HJ. Qigong therapy for physiotherapists suffering from burnout: a preliminary study. Journal of Chinese Integrative Medicine 2012;10(11):1233-9. [DOI] [PubMed] [Google Scholar]
Sampson 2019 {published data only}
- Sampson M, Melnyk BM, Hoying J. Intervention effects of the MINDBODYSTRONG cognitive behavioral skills building program on newly licensed registered nurses' mental health, healthy lifestyle behaviors, and job satisfaction. Journal of Nursing Administration 2019;49(10):487-95. [DOI: ] [DOI] [PubMed] [Google Scholar]
- Sampson M, Melnyk BM, Hoying J. The MINDBODYSTRONG intervention for new nurse residents: 6-month effects on mental health outcomes, healthy lifestyle behaviors, and job satisfaction. Worldviews on Evidence-Based Nursing 2020;17(1):16-23. [DOI: ] [DOI] [PubMed] [Google Scholar]
Sawyer 2021 {published and unpublished data}
- Sawyer AT, Bailey AK, Green JF, Sun J, Robinson PS. Resilience, insight, self-compassion, and empowerment (RISE): a randomized controlled trial of a psychoeducational group program for nurses. Journal of the American Psychiatric Nurses Association 2021;Epub ahead of print(-):10783903211033338. [DOI: ] [DOI] [PubMed] [Google Scholar]
Schrijnemaekers 2003 {published data only}
- Schrijnemaekers VJ, Van Rossum E, Candel MJ, Frederiks CM, Derix MM, Sielhorst H, et al. Effects of emotion-oriented care on work-related outcomes of professional caregivers in homes for elderly persons. Journals of Gerontology Series B-Psychological Sciences & Social Sciences 2003;58(1):S50-7. [DOI] [PubMed] [Google Scholar]
Schroeder 2018 {published data only}
- Schroeder DA, Stephens E, Colgan D, Hunsinger M, Rubin D, Christopher MS. A brief mindfulness-based intervention for primary care physicians: a pilot randomized controlled trial. American Journal of Lifestyle Medicine 2018;12(1):83-91. [DOI: 10.1177/1559827616629121] [DOI] [PMC free article] [PubMed] [Google Scholar]
Seidel 2021 {published data only}
- Seidel LW, Dane FC, Carter KF. Brief mindfulness practice course for healthcare providers. Journal of Nursing Administration 2021;51(7-8):395-400. [DOI: ] [DOI] [PubMed] [Google Scholar]
Shapiro 2005 {published data only}
- Shapiro SL, Astin JA, Bishop SR, Cordova M. Mindfulness-based stress reduction for health care professionals: results from a randomized trial. International Journal of Stress Management 2005;12(2):164-76. [Google Scholar]
Sharif 2013 {published data only}
- Sharif F, Rezaie S, Keshavarzi S, Mansoori P, Ghadakpoor S. Teaching emotional intelligence to intensive care unit nurses and their general health: a randomized clinical trial. International Journal of Occupational and Environmental Medicine 2013;4(3):141-8. [PubMed] [Google Scholar]
Shin 2020 {published data only}
- Shin YK, Lee SY, Lee JM, Kang P, Seol GH. Effects of short-term inhalation of patchouli oil on professional quality of life and stress levels in emergency nurses: randomized controlled trial. Journal of Alternative and Complementary Medicine (New York, N.Y.) 2020;26(11):1032-8. [DOI: ] [DOI] [PubMed] [Google Scholar]
Sood 2011 {published data only}
- Sood A, Prasad K, Schroeder D, Varkey P. Stress management and resilience training among department of medicine faculty: a pilot randomized clinical trial. Journal of General Internal Medicine 2011;26(8):858-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stanton 1988 {published data only}
- Stanton HE. Relaxation, deepening, and ego-enhancement: a stress reduction "package". Australian Psychologist 1988;23:315-22. [Google Scholar]
Tonarelli 2018 {published data only}
- Tonarelli A, Cosentino C, Tomasoni C, Nelli L, Damiani I, Goisis S, et al. Expressive writing. A tool to help health workers of palliative care. Acta Bio-Medica: Atenei Parmensis 2018;89(6-S):35-42. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tsai 1993 {published data only}
- Tsai SL, Crockett MS. Effects of relaxation training, combining imagery, and meditation on the stress level of Chinese nurses working in modern hospitals in Taiwan. Issues in Mental Health Nursing 1993;14(1):51-66. [DOI] [PubMed] [Google Scholar]
Verdes Montenegro Atalaya 2021 {published data only}
- Verdes-Montenegro-Atalaya JC, Perula-de Torres LA, Lietor-Villajos N, Bartolome-Moreno C, Moreno-Martos H, Rodriguez L, et al. Effectiveness of a mindfulness and self-compassion standard training Program versus an abbreviated Ttraining program on stress in tutors and resident Intern Ssecialists of family and community Medicine and nursing in Spain. International Journal of Environmental Research and Public Health 2021;18(19):10230. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wei 2017 {published data only}
- Wei R, Ji H, Li J, Zhang L. Active intervention can decrease burnout In Ed nurses. Journal of emergency nursing: JEN : official publication of the Emergency Department Nurses Association 2017;43(2):145-9. [DOI: ] [DOI] [PubMed] [Google Scholar]
West 1984 {published data only}
- West DJ Jr, Horan JJ, Games PA. Component analysis of occupational stress inoculation applied to registered nurses in an acute care hospital setting. Journal of Counseling Psychology 1984;31(2):209-18. [Google Scholar]
West 2014 {published and unpublished data}
- West CP, Dyrbye LN, Rabatin JT, Call TG, Davidson JH, Multari A, et al. Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. JAMA Internal Medicine 2014;174(4):527-33. [DOI: 10.1001/jamainternmed.2013.14387] [DOI] [PubMed] [Google Scholar]
West 2021 {published and unpublished data}
- West CP, Dyrbye LN, Satele DV, Shanafelt TD. Colleagues Meeting to Promote and Sustain Satisfaction (COMPASS) groups for physician well-being: a randomized clinical trial. Mayo Clinic Proceedings 2021;96(10):2606-14. [DOI: ] [DOI] [PubMed] [Google Scholar]
Xie 2020 {published data only}
- Xie C, Zeng Y, Lv Y, Li X, Xiao J, Hu X. Educational intervention versus mindfulness-based intervention for ICU nurses with occupational burnout: a parallel, controlled trial. Complementary Therapies in Medicine 2020;52(Aug):102485.. [DOI: 10.1016/j.ctim.2020.102485] [DOI] [PubMed] [Google Scholar]
Yazdani 2010 {published data only}
- Yazdani M, Rezaei S, Pahlavanzadeh S. The effectiveness of stress management training program on depression, anxiety and stress of the nursing students. Iranian Journal of Nursing and Midwifery Research 2010;15(4):208-15. [PMC free article] [PubMed] [Google Scholar]
Yung 2004 {published data only}
- Yung PM, Fung MY, Chan TM, Lau BW. Relaxation training methods for nurse managers in Hong Kong: a controlled study. International Journal of Mental Health Nursing 2004;13(4):255-61. [DOI] [PubMed] [Google Scholar]
Zarvijani 2021 {published data only}
- Zarvijani SAH, Moghaddam LF, Parchebafieh S. Acceptance and commitment therapy on perceived stress and psychological flexibility of psychiatric nurses: a randomized control trial. BMC Nursing 2021;20(1):239 . [DOI: 10.1186/s12912-021-00763-4] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Adair 2020 {published data only}
- Adair KC, Rodriguez-Homs, LG, Masoud S, Mosca PaulJ, Sexton, JB. Gratitude at work: prospective cohort study of a web-based, single-exposure well-being intervention for health care workers. Journal of Medical Internet Research 2020;22(5):e15562. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Akyurek 2020 {published data only}
- Akyurek G, Avci N, Ekici G. The effects of “Workplace Health Promotion Program” in nurses: A randomized controlled trial and one-year follow-up. Health Care for Women International 2020;-:-. [DOI: 10.1080/07399332.2020.1800013] [DOI] [PubMed] [Google Scholar]
Ali 2011 {published data only}
- Ali NA, Hammersley J, Hoffmann SP, O'Brien JM Jr, Phillips GS, Rashkin M, et al. Continuity of care in intensive care units: a cluster-randomized trial of intensivist staffing. American Journal of Respiratory and Critical Care Medicine 2011;184(7):803-8. [DOI] [PubMed] [Google Scholar]
Alkhawaldeh 2020 {published data only}
- Alkhawaldeh JF, Soh KL, Mukhtar F, Peng OC, Alkhawaldeh HM, Al-Amer R, et al. Stress management training program for stress reduction and coping improvement in public health nurses: a randomized controlled trial. Journal of Advanced Nursing 2020;76(11):3123-35. [DOI: ] [DOI] [PubMed] [Google Scholar]
Ameli 2020 {published data only}
- Ameli R, Sinaii N, West CP, Luna MJ, Panahi S, Zoosman M, et al. Effect of a brief mindfulness-based program on stress in health care professionals at a US biomedical research hospital: a randomized clinical trial. JAMA Network Open 2020;3(8):e2013424. [DOI: 10.1001/jamanetworkopen.2020.13424] [DOI] [PMC free article] [PubMed] [Google Scholar]
Anonymous 2021 {published data only}
- Anonymous. Effects of acupuncture and acupressure on burnout in health care workers: a randomized trial. Journal of Trauma Nursing: the official journal of the Society of Trauma Nurses 2021;28(6):E12. [DOI: ] [DOI] [PubMed] [Google Scholar]
Aronson 2022 {published data only}
- Aronson M, Henderson T, Dodd KW, Cirone M, Putman M, Salzman D, et al. Effects of brief mental skills training on emergency medicine residents’ stress response during a simulated resuscitation: a prospective randomized trial. Western Journal of Emergency Medicine: Integrating Emergency Care with Population Health 2022;23(1):79-85. [DOI: 10.5811/westjem.2021.10.53892] [DOI] [PMC free article] [PubMed] [Google Scholar]
Barbosa 2016 {published data only}
- Barbosa A, Marques A, Sousa L, Nolan M, Figueiredo D. Effects of a psycho-educational intervention on direct care workers’ communicative behaviors with residents with dementia. Health Communication 2016;31(4):45359. [DOI: 10.1080/10410236.2014.965382] [DOI] [PubMed] [Google Scholar]
Barrett 2021 {published data only}
- Barrett K, Stewart I. A preliminary comparison of the efficacy of online Acceptance and Commitment Therapy (ACT) and Cognitive Behavioural Therapy (CBT) stress management interventions for social and healthcare workers. Health & Social Care in the Community 2021;29(1):113-26. [DOI: ] [DOI] [PubMed] [Google Scholar]
Beck 2018 {published data only}
- Beck AR, Verticchio H. Effectiveness of a method for teaching self-compassion to Communication Sciences and Disorders graduate students. American Journal of Speech-Language Pathology 2018;27(1):192‐206. [DOI: 10.1044/2017_AJSLP-17-0060] [DOI] [PubMed] [Google Scholar]
Behzadi 2021 {published data only}
- Behzadi S, Alizadeh Z, Samani NK, Ghasemi A, Fereidouni Z, Kargar L, et al. Effect of stress management on job stress of intensive care unit nurses in hospitals affiliated to the University of Medical Sciences. Archivos Venezolanos de Farmacologia y Terapeutica 2021;40(8):824-7. [DOI: 10.5281/zenodo.5791329] [DOI] [Google Scholar]
Bielderman 2021 {published data only}
- Bielderman A Nieuwenhuis A, Hazelhof TJ, Gaal BG, Schoonhoven L, Akkermans RP, et al. Effects on staff outcomes and process evaluation of the educating nursing staff effectively (TENSE) program for managing challenging behavior in nursing home residents with dementia: A cluster-randomized controlled trial. International Journal of Nursing Studies 2021;120:103982. [DOI: ] [DOI] [PubMed] [Google Scholar]
Bittman 2003 {published data only}
- Bittman B, Bruhn KT, Stevens C, Westengard J, Umbach PO. Recreational music-making: a cost-effective group interdisciplinary strategy for reducing burnout and improving mood states in long-term care workers. Advances in Mind-Body Medicine 2003;19(3-4):4-15. [PubMed] [Google Scholar]
Boehm 2017 {published data only}
- Boehm, LB. Guided imagery for stress reduction in graduate nurses transitioning into practice. Dissertation abstracts international: section B: the sciences and engineering 2017;77(8-B(E)):No-Specified. [Google Scholar]
BorgesSouza 2019 {published data only}
- Borges Souza TP, Souza-Talarico JN, Kuba G, Turrini R. Awakening cortisol response and perceived stress decrease after quick massage intervention in nursing professionals. Psychoneuroendocrinology 2019;107:38‐. [DOI: 10.1016/j.psyneuen.2019.07.107] [DOI] [Google Scholar]
Bourbonnais 2011 {published data only}
- Bourbonnais R, Brisson C, Vinet A, Vézina M, Abdous B, Gaudet M. Effectiveness of a participative intervention on psychosocial work factors to prevent mental health problems in a hospital setting. Occupational and Environmental Medicine 2006;63(5):335-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourbonnais R, Brisson C, Vinet A, Vézina M, Lower A. Development and implementation of a participative intervention to improve the psychosocial work environment and mental health in an acute care hospital. Occupational and Environmental Medicine 2006;63(5):326-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourbonnais R, Brisson C, Vézina M. Long-term effects of an intervention on psychosocial work factors among healthcare professionals in a hospital setting. Occupational and Environmental Medicine 2011;68(7):479-86. [DOI] [PubMed] [Google Scholar]
Braun 2020 {published data only}
- Braun SE, Dow A, Loughan A, Mladen S, Crawford M, Rybarczyk, B, et al. Mindfulness training for healthcare professional students:a waitlist controlled pilot study on psychological and work-relevant outcomes. Complementary Therapies in Medicine 2020;51:102405. [DOI: ] [DOI] [PubMed] [Google Scholar]
Buruck 2016 {published data only}
- Buruck G, Dörfel D, Kugler J, Brom SS. Enhancing well-being at work: the role of emotion regulation skills as personal resources. Journal of oOcupational Health Psychology 2016;21(4):480-93. [DOI: 10.1037/ocp0000023] [DOI] [PubMed] [Google Scholar]
Butow 2015 {published data only}
- Butow P, Brown R, Aldridge J, Juraskova I, Zoller P, Boyle F, et al. Can consultation skills training change doctors' behaviour to increase involvement of patients in making decisions about standard treatment and clinical trials: A randomized controlled trial. Health Expectations: an International Journal of Public Participation in Health Care & Health Policy 2015;18(6):2570-83. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Carneiro 2020 {published data only}
- Carneiro EM, Oliveira LF, da Silva DA, Sousa JB, Timoteo RP, Neto OB, Silva AP, et al. Effects of the laying on of hands on anxiety, stress and autonomic response of employees in a hospital: a double-blind randomized controlled trial. Complementary Therapies in medicine 2020;52:102475. [DOI: ] [DOI] [PubMed] [Google Scholar]
Carson 1999 {published data only}
- Carson J, Cavagin J, Bunclark J, Maal S, Gournay K, Kuipers E, et al. Effective communication in mental health nurses: did social support save the psychiatric nurse? NT Research 1999;4:31-42. [Google Scholar]
Cascales Perez 2021 {published data only}
- Cascales-Perez, ML, Ferrer-Cascales R, ernandez-Alcantara M, Cabanero-Martinez MJ. Effects of a mindfulness-based programme on the health- and work-related quality of life of healthcare professionals. Scandinavian Journal of Caring Sciences 2021;35(3):881-91. [DOI: ] [DOI] [PubMed] [Google Scholar]
Cayir 2021 {published data only}
- Cayir E, Cunningham T, Ackard R, Haizlip J, Logan J, Yan G. The effects of the medical pause on physiological stress markers among health care providers: a pilot randomized controlled trial. Western Journal of Nursing Research 2021;44(11):1036-46. [DOI: 10.1177/01939459211027657] [DOI] [PubMed] [Google Scholar]
Chaabane 2021 {published data only}
- Chaabane, S, Etienne, AM, Schyns, M, Wagener, A. The impact of virtual reality exposure on stress level and sense of competence in ambulance workers. Journal of Traumatic Stress 2021;35(1):120-7. [DOI: ] [DOI] [PubMed] [Google Scholar]
Chen 2017 {published data only}
- Chen SH, Chen SC, Lee SC, Chang YL, Yeh KY. Impact of interactive situated and simulated teaching program on novice nursing practitioners' clinical competence, confidence, and stress. Nurse Education Today 2017;55:11-6. [DOI: 10.1016/j.nedt.2017.04.025] [DOI] [PubMed] [Google Scholar]
Cheung 2020 {published data only}
- Cheung EO, Barsuk JH, Mitra D, Gannotta RJ, Horowitz B, Didwania AK, et al. Preliminary efficacy of a brief mindfulness intervention for procedural stress in medical intern simulated performance: a randomized controlled pilot trial. Journal of Alternative and Complementary Medicine (New York, N.Y.) 2020;26(4):282-90. [DOI: ] [DOI] [PubMed] [Google Scholar]
Clemow 2018 {published data only}
- Clemow LP, Pickering TG, Davidson KW, Schwartz JE, Williams VP, Shaffer JA, et al. Stress management in the workplace for employees with hypertension: a randomized controlled trial. Translational Behavioral Medicine 2018;8(5):761-70. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Coelhoso 2019 {published data only}
- Coelhoso CC, Tobo PR, Lacerda SS, Lima AH, Barrichello CR, Amaro E Jr, et al. A new mental health mobile app for well-being and stress reduction in working women: randomized controlled trial. Journal of Medical Internet Research 2019;21(11):e14269. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cordoza 2018 {published data only}
- Cordoza M, Ulrich RS, Manulik BJ, Gardiner SK, Fitzpatrick PS, Hazen TM, et al . Impact of nurses taking daily work breaks in a hospital garden on burnout. American Journal of Critical Care : an official publication, American Association of Critical-Care Nurses 2018;27(6):508-12. [DOI: ] [DOI] [PubMed] [Google Scholar]
Cosentino 2021 {published data only}
- Cosentino C, D'apice C, Del Gaudio M, Bertoletti C, Bini M, Liotti MC, et al. Effectiveness of expressive writing protocol in palliative care healthworkers: a quantitative study. Acta Bio-Medica : Atenei Parmensis 2021;92(S2):e2021010. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Daigle 2018 {published data only}
- Daigle S, Talbot F, French DJ. Mindfulness‐based stress reduction training yields improvements in well‐being and rates of perceived nursing errors among hospital nurses. Journal of Advanced Nursing (John Wiley & Sons, Inc.) 2018;74(10):2427-230. [DOI: 10.1111/jan.13729] [DOI] [PubMed] [Google Scholar]
Davidson 2017 {published data only}
- Davidson JE, Graham P, Montross-Thomas L, Norcross W, Zerb, G. Code Lavender: cultivating intentional acts of kindness in response to stressful work situations. Explore: the Journal of Science and Healing 2017;13(3):181-5. [DOI: 10.1016/j.explore.2017.02.005] [DOI] [PubMed] [Google Scholar]
DeKock 2022 {published data only}
- De Kock JH, Latham HA, Cowden RG, Cullen B, Narzisi K, Jerdan S, et al. Brief digital interventions to support the psychological well-being of NHS staff during the COVID-19 pandemic: a three-arm pilot randomised controlled trial. JMIR Mental Health 2022;9(4):e34002. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Delvaux 2004 {published data only}
- Delvaux N, Razavi D, Marchal S, Bredart A, Farvacques C, Slachmuylder JL. Effects of a 105 hours psychological training program on attitudes, communication skills and occupational stress in oncology: a randomised study. British Journal of Cancer 2004;90(1):106-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Deneckere 2013 {published data only}
- Deneckere S, Euwema M, Lodewijckx C, Panella M, Mutsvari T, Sermeus W, et al. Better interprofessional teamwork, higher level of organized care, and lower risk of burnout in acute health care teams using care pathways: a cluster randomized controlled trial. Medical Care 2013;51(1):99-107. [DOI: ] [DOI] [PubMed] [Google Scholar]
Doran 2018 {published data only}
- Doran K, Resnick B, Alghzawi H, Zhu S. The worksite heart health improvement project's impact on behavioral risk factors for cardiovascular disease in long-term care: a randomized control trial. International Journal of Nursing Studies 2018;86:107-14. [DOI: ] [DOI] [PubMed] [Google Scholar]
Fadaei 2020 {published data only}
- Fadaei MH, Torkaman M, Heydari N Kamali M, Ghodsbin F. Cognitivebehavioral therapy for occupational stress among the intensive care unit nurses. Indian Journal of Occupational and Environmental Medicine 2020;24(3):178-82. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Fang 2015 {published data only}
- Fang R, Li X. A regular yoga intervention for staff nurse sleep quality and work stress: a randomised controlled trial. Journal of Clinical Nursing 2015;24(23-4):3374-3379. [DOI: 10.1111/jocn.12983] [DOI] [PubMed] [Google Scholar]
Farsi 2021 {published data only}
- Farsi Z, Rajai N, Teymouri F, Gholami M. Effect ofaromatherapy with rosa damascena essential oil on nurses' occupational stress in the emergency department: a randomized controlled trial. Nursing & Midwifery Care Journal 2021;11(3):46-54. [Google Scholar]
Feldman 2017 {published data only}
- Feldman E. Caring for providers: mindfulness for healthcare practitioners. Integrative Medicine Alert 2017;20(10):113-6. [Google Scholar]
Fiore 2021 {published data only}
- Fiore J. Randomized pilot study exploring an online pre-composed receptive music experience and a mindfulness-based intervention for hospice workers’ stress and professional quality of life. Arts in Psychotherapy 2021;74:-. [DOI: 10.1016/j.aip.2021.101797] [DOI] [Google Scholar]
Frogeli 2016 {published data only}
- Frogeli E, Djordjevic A, Rudman A, Livheim F, Gustavsson P, Biglan, et al. A randomized controlled pilot trial of acceptance and commitment training (ACT) for preventing stress-related ill health among future nurses. Anxiety, Stress & Coping: An International Journal 2016;29(2):202-18. [DOI: ] [DOI] [PubMed] [Google Scholar]
- Frögéli E, Rudman A, Gustavsson P. Preventing stress-related ill health among future nurses: effects over 3 years. International Journal of Stress Management 2019;26(3):272-86. [DOI: 10.1037/str0000110] [DOI] [Google Scholar]
Gaggioli 2014 {published data only}
- Gaggioli A, Pallavicini F, Morganti L, Serino, S, Scaratti C, Briguglio M, et al. Experiential virtual scenarios with real-time monitoring (interreality) for the management of psychological stress: a block randomized controlled trial. Journal of Medical Internet Research 2014;16(7):e167. [DOI: 10.2196/jmir.3235] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gardner 2005 {published data only}
- Gardner B, Rose J, Mason O, Tyler P, Cushway D. Cognitive therapy and behavioural coping in the management of work-related stress: an intervention study. Work and Stress 2005;19(2):137-52. [Google Scholar]
Gartner 2013 {published data only}
- Gartner FR, Nieuwenhuijsen K, Ketelaar SM, Dijk FJ, Sluiter JK. The Mental Vitality @ Work Study: effectiveness of a Mental Module for Workers E Health Surveillance for nurses and allied health care professionals on their help-seeking behavior. Journal of Occupational and Environmental Medicine 2013;55(10):1219-29. [DOI: 10.1097/JOM.0b013e31829f310a] [DOI] [PubMed] [Google Scholar]
Gauthier 2015 {published data only}
- Gauthier T, Meyer RM, Dagmar G, Jeffrey I. An on-the-job mindfulness-based intervention for pediatric ICU nurses: a pilot. Journal of Pediatric Nursing 2015;30(2):402-9. [DOI: ] [DOI] [PubMed] [Google Scholar]
Ghafarzadegan 2014 {published data only}
- Ghafarzadegan, R, Saeedi M, Malekhosseini A, Hekmatpou D, Ghafarzadegan R, Hajiaghaee R. The effect of Ginkgo on stress level of nurses. Journal of Medicinal Plants 2014;13(50):64-72. [Google Scholar]
Ghazavi 2010 {published data only}
- Ghazavi Z, Lohrasbi F, Mehrabi T. Effect of communication skill training using group psycho-education method on the stress level of psychiatry ward nurses. Iranian Journal of Nursing and Midwifery Research 2010;15(Suppl 1):395-400. [PMC free article] [PubMed] [Google Scholar]
Grahn 2020 {published data only}
- Grahn P, Bonaventura K, Wippert PM. Stress levels in cardiac catherization laboratory – can an MBSR intervention reduce stress of medical practitioners in a cardiac catherization laboratory? Psychoneuroendocrinology 2020;119(-):-. [DOI: 10.1016/j.psyneuen.2020.104925] [DOI] [Google Scholar]
Greeson 2015 {published data only}
- Greeson JM, Toohey MJ, Pearce MJ. An adapted, four-week mind-body skills group for medical students: reducing stress, increasing mindfulness, and enhancing self-care. Explore (new york, N.Y.) 2015;11(3):186-92. [DOI: ] [DOI] [PubMed] [Google Scholar]
Griffith 2008 {published data only}
- Griffith JM, Hasley JP, Liu H, Severn DG, Conner LH, Adler LE. Qigong stress reduction in hospital staff. Journal of Alternative and Complementary Medicine 2008;14(8):939-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
Grigorescu 2020 {published data only}
- Grigorescu S, Cazan AM, Rogozea L, Grigorescu DO. Original targeted therapy for the management of the burnout syndrome in nurses: an innovative approach and a new opportunity in the context of predictive, preventive and personalized medicine. The EPMA journal 2020;11(2):161-76. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gross 2018 {published data only}
- Gross ME. The impact of text messages on anxiety and health-promoting behaviors among baccalaureate nursing students: a mixed methods approach. Dissertation 2018;79:-.
Guerrier 2021 {published data only}
- Guerrier G, MargetisD, Agostini C, Machroub Z, Di Maria S. Improving wellness of operating Rroom personnel: a light-based intervention on perceived nursing-related stress. Frontiers in Psychiatry 2021;12:718194. [DOI: 10.3389/fpsyt.2021.718194] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gupta 2021 {published data only}
- Gupta S, Kumar M, Rozatkar AR, Basera D, Purwar S, Gautam S, et al. Feasibility and effectiveness of telecounseling on the psychological problems of frontline healthcare workers amidst COVID-19: a randomized controlled trial from central India. Indian journal of Psychological Medicine 2021;43(4):343-50. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gutman 2020 {published data only}
- Gutman SA, Sliwinski M, Laird J, Nguyen J. Effectiveness of a Multimodal Mindfulness Program for student health care professionals: a randomized controlled trial. Open Journal of Occupational Therapy (OJOT) 2020;8(2):1-18. [DOI: 10.15453/2168-6408.1662] [DOI] [Google Scholar]
Hansen 2006 {published data only}
- Hansen TM, Hansen B, Ringdal GI. Does aromatherapy massage reduce job-related stress? Results from a randomised, controlled trial. International Journal of Aromatherapy 2006;16:89-94. [Google Scholar]
Havermans 2018 {published data only}
- Havermans BM, Boot CR, Brouwers EP, Houtman IL, Heerkens YF, Zijlstra-Vlasveld MC, et al. Effectiveness of a digital platform-based implementation strategy to prevent work stress in a healthcare organization: a 12-month follow-up controlled trial. Scandinavian Journal of Work, Environment & Health 2018;44(6):613-21. [DOI: ] [DOI] [PubMed] [Google Scholar]
Heaney 1995 {published data only}
- Heaney CA, Price RH, Rafferty J. Increasing coping resources at work: a field experiment to increase social support, improve work team functioning, and enhance employee mental health. Journal of Organizational Behavior 1995;16:335-52. [Google Scholar]
HemmatiMaslakpak 2016 {published data only}
- HemmatiMaslakpak M, Farhadi M, Fereidoni J. The effect of neuro-linguistic programming on occupational stress in critical care nurses. Iranian Journal of Nursing and Midwifery Research 2016;21(1):38-44. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hill 2016 {published data only}
- Hill RC, Dempster M, Donnelly M, McCorry NK, , Asai B. Improving the wellbeing of staff who work in palliative care settings: A systematic review of psychosocial interventions. Palliative medicine 2016;30(9):825833. [DOI: ] [DOI] [PubMed] [Google Scholar]
Hofer 2018 {published data only}
- Hofer PD, Waadt M, Aschwanden R, Milidou M, Acker J, Meyer AH, et al. Self-help for stress and burnout without therapist contact: An online randomised controlled trial. Work & Stress 2018;32(2):189-208. [DOI: 10.1080/02678373.2017.1402389] [DOI] [Google Scholar]
Hu 2015 {published data only}
- Hu YC, Chen SR, Chen IH, Shen HC, Lin YK, Chang WY. Evaluation of work stress, turnover intention, work experience, and satisfaction with preceptors of new graduate nurses using a 10-minute preceptor model. Journal of Continuing Education in Nursing 2015;46(6):261271. [DOI: 10.3928/00220124-20150518-02] [DOI] [PubMed] [Google Scholar]
Johnson 2015 {published data only}
- Johnson JR, Emmons HC, Rivard RL, Griffin KH, Dusek JA. Resilience TTaining: a Pilot SSudy of a Mindfulness-Based Program with Depressed Healthcare Professionals. Explore (new york, N.Y.) 2015;11(6):433-44. [DOI: 10.1016/j.explore.2015.08.002] [DOI] [PubMed] [Google Scholar]
Jones 2000a {published data only}
- Jones MC, Johnston DW. Evaluating the impact of a worksite stress management programme for distressed students: a randomised controlled trial. Psychology and Health 2000;15:689-706. [Google Scholar]
KarbakhshRavari 2020 {published data only}
- Karbakhsh Ravari A, Farokhzadian J, Nematollahi M, Miri, S, Foroughameri G. The effectiveness of a time management workshop on job stress of nurses working in emergency departments: an experimental study. Journal of Emergency Nursing 2020;46(4):548.e1-548.e11. [DOI: ] [DOI] [PubMed] [Google Scholar]
Karpaviciute 2016 {published data only}
- Karpaviciute S, Macijauskiene J. The impact of arts activity on nursing staff well-being: an intervention in the workplace. International Journal of Environmental Research and Public Health 2016;13(4):435. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kesselheim 2018 {published data only}
- Kesselheim J, Weng S, Allen V. Humanism and professionalism training in pediatric hematologyoncology fellowship: results of a multi-center randomized trial. Pediatric Blood & Cancer 2018;65:S182‐. [DOI: 10.1002/pbc.27057] [DOI] [Google Scholar]
Khaghanizadeh 2008 {published data only}
- Khaghanizadeh M, Vafadar Z, Salari M, Ebadi A. Effects of suggestions' system on decreasing job burn out among the staff . Journal of Psychology 2008;12((46)):213-26. [Google Scholar]
Khalsa 2021 {published data only}
- Khalsa SB, Dyer N, Loewenthal J, Lipsyc-Sharf M, Mehta D, Dusek J. A pilot study of a six week yoga and mindfulness-based program in resident physicians. European Journal of Integrative Medicine 2021;48:-. [DOI: 10.1016/j.eujim.2021.102080] [DOI] [Google Scholar]
Kiley 2018 {published data only}
- Kiley KA, Sehgal AR, Neth S, Dolata J, Pike E, Spilsbury JC, et al. The effectiveness of guided imagery in treating compassion fatigue and anxiety of mental health workers. Social Work Research 2018;42(1):33-43. [DOI: 10.1093/swr/svx026] [DOI] [Google Scholar]
Kloos 2019 {published data only}
- Kloos N, Drossaert CH, Bohlmeijer ET, Westerhof GJ. Online positive psychology intervention for nursing home staff: A cluster-randomized controlled feasibility trial of effectiveness and acceptability. International Journal of Nursing Studies 2019;98:48-56. [DOI: ] [DOI] [PubMed] [Google Scholar]
Kon 2019 {published data only}
- Kon RH, Flickinger TE, Schorling J, May N, Owens JE, Harrison M, et al. Flourishing in the clerkship year: a longitudinal curriculum introducing skills to reduce burnout and foster resilience in medical students. Journal of General Internal Medicine 2019;34(2):S809‐. [DOI: 10.1007/11606.1525-1497] [DOI] [Google Scholar]
Kubota 2016 {published data only}
- Kubota Y, Okuyama T, Uchida M, Umezawa S, Nakaguchi T, Sugano K, et al. Effectiveness of a psycho-oncology training program for oncology nurses: A randomized controlled trial. Psycho-oncology 2016;25(6):712-8. [DOI: ] [DOI] [PubMed] [Google Scholar]
Kwok 2012 {published data only}
- Kwok WO. The effects of an intervention program (medi) on reducing occupational stress in emergency department nurses. Dissertation Abstracts International: Section B: The Sciences and Engineering 2012;72(7-B):3963.
Lahn 2015 {published data only}
- Lahn, MJ. Indices of heart rate variability and compassion in healthcare professionals following stress resilience training. Dissertation abstracts international: section B: the sciences and engineering 2015;75(11-B(E)):Not Specified. [Google Scholar]
Lai 2011 {published data only}
- Lai HL, Li YM. The effect of music on biochemical markers and self-perceived stress among first-line nurses: a randomized controlled crossover trial. Journal of Advanced Nursing 2011;67(11):2414-24. [DOI] [PubMed] [Google Scholar]
Lambert 2019 {published data only}
- Lambert KG, Aufricht WR, Mudie D, Brown LH. 279 Does a phone-based meditation application improve mental wellness among emergency medicine personnel. Annals of Emergency Medicine 2019;74(4):S110‐. [DOI: 10.1016/j.annemergmed.2019.08.237] [DOI] [PubMed] [Google Scholar]
Lebares 2019 {published data only}
- Lebares CC, Guvva EV, Olaru, M, Sugrue LP, Staffaroni AM, Delucchi KL, et al. Efficacy of mindfulness-based cognitive training in surgery: additional analysis of the mindful surgeon pilot randomized clinical trial? JAMA Network Open 2019;2(5):e194108. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Le Blanc 2007 {published data only}
- Le Blanc PM, Hox JJ, Schaufeli WB, Taris TW, Peeters MC. Take care! The evaluation of a team-based burnout intervention program for oncology care providers. Journal of Appled Psychology 2007;92(1):213-27. [DOI] [PubMed] [Google Scholar]
Leiter 2011 {published data only}
- Leiter MP, Laschinger HK, Day A, Oore DG. The impact of civility interventions on employee social behavior, distress, and attitudes. Journal of Applied Psychology 2011;96(6):1258-74. [DOI] [PubMed] [Google Scholar]
Lemaire 2011 {published data only}
- Lemaire JB, Wallace JE, Lewin AM, De Grood J, Schaefer JP. The effect of a biofeedback-based stress management tool on physician stress: a randomized controlled clinical trial. Open Medicine 2011;5(4):e154-65. [PMC free article] [PubMed] [Google Scholar]
Li 2011 {published data only}
- Li HC, Wang LS, Lin YH, Lee I. The effect of a peer-mentoring strategy on student nurse stress reduction in clinical practice. International Nursing Review 2011;58(2):203-10. [DOI] [PubMed] [Google Scholar]
Lilly 2019 {published data only}
- Lilly M, Calhoun R, Painter I, Beaton R, Stangenes S, Revere D, et al. Destress 9-1-1-an online mindfulness-based intervention in reducing stress among emergency medical dispatchers: a randomised controlled trial. Occupational and Environmental Medicine 2019;76(10):705-11. [DOI: ] [DOI] [PubMed] [Google Scholar]
Linzer 2015 {published data only}
- Linzer M, Poplau S, Grossman E, Varkey A, Yale S, Williams E, et al. A cluster randomized trial of interventions to improve work conditions and clinician burnout in primary care: results from the Healthy Work Place (HWP) Study. Journal of General Internal Medicine 2015;30(8):1105-11. [DOI: 10.1007/s11606-015-3235-4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Loiselle 2018 {published data only}
Lökk 2000 {published data only}
- Lökk J, Arnetz B. Impact of management change and an intervention program on health care personnel. Psychotherapy and Psychosomatics 2000;69(2):79-85. [DOI] [PubMed] [Google Scholar]
- Lökk J, Arnetz B. Psychophysiological concomitants of organizational change in health care personnel: effects of a controlled intervention study. Psychotherapy and Psychosomatics 1997;66(2):74-7. [DOI] [PubMed] [Google Scholar]
Low 2015 {published data only}
- Low V, Gebhart B, Reich C. Effects of a worksite program to improve the cardiovascular health of female health care workers. Journal of Cardiopulmonary Rehabilitation and Prevention 2015;35(5):342-7. [DOI: 10.1097/HCR.0000000000000116] [DOI] [PubMed] [Google Scholar]
Lucas 2012 {published data only}
- Lucas B, Trick W, Evans A, Weinstein R, Varkey A, Smith J, et al. Emotional exhaustion, life stress, and perceived control among medicine ward attending physicians: A randomized trial of 2-versus 4-week ward rotations. Journal of Hospital Medicine 2011;6(4):S43-4. [Google Scholar]
- Lucas BP, Trick WE, Evans AT, Mba B, Smith J, Das K, et al. Effects of 2- vs 4-week attending physician inpatient rotations on unplanned patient revisits, evaluations by trainees, and attending physician burnout: a randomized trial. JAMA 2012;308(21):2199-207. [DOI] [PubMed] [Google Scholar]
Lui 2019 {published data only}
- Lui, WS. A randomized controlled trial study to alleviate healthcare workers' burnout and perceived stress by mindful practice program. Dissertation of thesis 2019;80:-.
Luoma 2013 {published data only}
- Luoma JB, , Vilardaga JP. Improving therapist psychological flexibility while training acceptance and commitment therapy: a pilot study. Cognitive Behaviour Therapy 2013;42(1):1-8. [DOI: ] [DOI] [PubMed] [Google Scholar]
Mahdizadeh 2019 {published data only}
- Mahdizadeh M, Jaberi AA, Bonabi TN. Massage therapy in management of occupational stress in emergency medical services staffs: a randomized controlled trial. InternationalJjournal of Therapeutic Massage & Bodywork 2019;12(1):16-22. [PMC free article] [PubMed] [Google Scholar]
Manotas 2013 {published data only}
- Manotas MA. Brief mindfulness training to improve mental health with colombian healthcare professionals. Dissertation abstracts international: section B: the sciences and engineering 2013;74(4-B(E)):Not-Specified. [Google Scholar]
McConville 2017 {published data only}
- McConville J, McAleer R, Hahne A. Mindfulness training for health profession students-the effect of mindfulness training on psychological well-being, learning and clinical performance of health professional students: a systematic review of randomized and non-randomized controlled trials. Explore (new york, N.Y.) 2017;13(1):26-45. [DOI: ] [DOI] [PubMed] [Google Scholar]
McElligott 2003 {published data only}
- McElligott D, Holz MB, Carollo L, Somerville S, Baggett M, Kuzniewski S, et al. A pilot feasibility study of the effects of touch therapy on nurses. Journal of the New York State Nurses Association 2003;34(1):16-24. [PubMed] [Google Scholar]
Mellis 2019 {published data only}
- Mellis, C. Reducing work stress in intensive care unit nurses. Journal of Paediatrics & Child Health 2019;55(3):373-373. [DOI: 10.1111/jpc.14361] [DOI] [Google Scholar]
Meng 2018 {published data only}
- Meng L, Qi J. The effect of an emotional intelligence intervention on reducing stress and improving communication skills of nursing students. NeuroQuantology 2018;16(1):37-42. [DOI: 10.14704/nq.2018.16.1.1175] [DOI] [Google Scholar]
Meyer Lamp 2020 {published data only}
- Meyer-Lamp I, Boos M, Schugmann LS, Leitsmann C, Trojan L, Friedrich MG. Silent operating theatre optimisation system for positive impact on surgical staff-members' stress, exhaustion, activity and concentration in urological da Vinci surgeries. BMJ innovations 202;7:175-84. [DOI: 10.1136/bmjinnov-2019-000413] [DOI] [Google Scholar]
Millspaugh 2021 {published data only}
- Millspaugh J, Errico C, Mortimer S, Kowalski MO, Chiu S, Reifsnyder C. Jin Shin Jyutsu® self-help reduces nurse stress: a randomized controlled study. Journal of Holistic Nursing 2021;39(1):4-15. [DOI: 10.1177/0898010120938922] [DOI] [PubMed] [Google Scholar]
Mistretta 2018 {published data only}
- [No authors listed]. Erratum: resilience Training for Work-Related Stress Among Health Care Workers: results of a Randomized Clinical Trial Comparing In-Person and Smartphone-Delivered Interventions: erratum (Journal of occupational and environmental medicine (2018) 60 6 (559. Journal of Occupational and Environmental Medicine 2018;60(8):e436‐. [DOI: 10.1097/JOM.0000000000001414] [DOI] [PubMed] [Google Scholar]
Miyoshi 2019 {published data only}
- Miyoshi Y. Restorative yoga for occupational stress among Japanese female nurses working night shift: Randomized crossover trial. Journal of Occupational Health 2019;61(6):508-16. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mohebbi 2019 {published data only}
- Mohebbi Z, Dehkordi S, Fazel S, Farkhondeh B. Theeffect of aerobic exercise on occupational stress of female nurses: a controlled clinical trial. Investigacion y Educacion en Enfermeria 2019;37(2):-. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Moll 2018 {published data only}
- Moll SE, Patten S, Stuart H, MacDermid JC, Kirsh B. Beyond silence: a randomized, parallel-group trial exploring the impact of workplace mental health literacy training with healthcare employees. Canadian Journal of Psychiatry. Revue cCanadienne de Psychiatrie 2018;63(12):826‐33. [DOI: 10.1177/0706743718766051] [DOI] [PMC free article] [PubMed] [Google Scholar]
Moody 2013 {published data only}
- Moody K, Kramer D, Santizo RO, Magro L, Wyshogrod D, Ambrosio J, et al. Helping the helpers: mindfulness training for burnout in pediatric oncology--a pilot program. Journal of Pediatric Oncology Nursing 2013;30(5):275-84. [DOI: 10.1177/1043454213504497] [DOI] [PubMed] [Google Scholar]
Moyle 2013 {published data only}
- Moyle W, Cooke M, O'Dwyer ST, Murfield J, Johnston A, Sung B. The effect of foot massage on long-term care staff working with older people with dementia: a pilot, parallel group, randomized controlled trial. BMC Nursing 2013;12(1):-. [DOI: 10.1186/1472-6955-12-5] [DOI] [PMC free article] [PubMed] [Google Scholar]
Muller 2016 {published data only}
- Muller A, Heiden B, Herbig B, Poppe F, Angerer P. Improving well-being at work: a randomized controlled intervention based on selection, optimization, and compensation. Journal of Occupational Health Psychology 2016;21(2):169-81. [DOI: 10.1037/a0039676] [DOI] [PubMed] [Google Scholar]
Navidian 2019 {published data only}
- Navidian A, Navaee M, Kaykha H. Effectiveness of stress inoculation training on occupational stress of midwives in healthcare centers of Zahedan in Health Transformation Plan in 2017. Journal of Education and Health Promotion 2019;8:66. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Nazari 2015 {published data only}
- Nazari F, Mirzamohamadi M, Yousefi H. The effect of massage therapy on occupational stress of Intensive Care Unit nurses. Iranian Journal of Nursing and Midwifery Research 2015;20(4):508-15. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
NeCamp 2020 {published data only}
- NeCamp T, Sen S, Frank E, Walton MA, Ionides EL, Fang Y, et al. Assessing real-time moderation for developing adaptive mobile health interventions for medical interns: micro-randomized triall. Journal of Medical Internet Research 2020;22(3):e15033. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Niva 2021 {published data only}
- Niva WJ, Lavanya S, Manikandan A, MaheshKumar K, Ganesan T, Vanishree S, et al. Mahamantra chanting as an effective intervention for stress reduction among nursing professionals—a randomized controlled study. Advances in Integrative Medicine 2021;8(1):27-32. [DOI: 10.1016/j.aimed.2020.05.007] [DOI] [Google Scholar]
Nourian 2021 {published data only}
- Nourian M, Nikfarid L, Khavari AM, Barati M, Allahgholipour AR. The impact of an online mindfulness-based stress reduction program on sleep quality of nurses working in covid-19 care units: a clinical trial. Holistic Nursing Practice 2021;35(5):257-63. [DOI: 10.1097/HNP.0000000000000466] [DOI] [PubMed] [Google Scholar]
Ozturk 2021 {published data only}
- Ozturk, FO, Tezel, A. Effect of laughter yoga on mental symptoms and salivary cortisol levels in first‐year nursing students: a randomized controlled trial. International Journal of Nursing Practice (John Wiley & Sons, Inc.) 2021;27(2):1-10. [DOI: 10.1111/ijn.12924] [DOI] [PubMed] [Google Scholar]
Pehlivan 2019 {published data only}
- Pehlivan T, Guner P. The effect of the short-term and long-term compassion fatigue resiliency program on the quality of life, perceived stress and psychological resilience of oncology-haematology nurses. Annals of Oncology 2019;30:v847‐. [DOI: 10.1093/annonc/mdz277.006] [DOI] [Google Scholar]
Penprase 2015 {published data only}
- Penprase B, Johnson A, Pittiglio L, Pittiglio B. Does mindfulness-based stress reduction training improve nurse satisfaction? Nursing Management 2015;46(12):38-45. [DOI: ] [DOI] [PubMed] [Google Scholar]
Perula deTorres 2021 {published data only}
- Perula-de Torres LA, Verdes-Montenegro-Atalaya JC, Melus-Palazon E, Garcia-de Vinuesa L, Valverde FJ, Rodriguez LA, et al. Comparison of the effectiveness of an abbreviated program versus a standard program in mindfulness, self-compassion and self-perceived empathy in tutors and resident intern specialists of family and community medicine and nursing in Spain. International Journal of Environmental Research and Public Health 2021;18(8):-. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pich 2018 {published data only}
- Pich, J. Preventing occupational stress in healthcare workers. Research in Nursing & Health 2018;41(4):408-9. [DOI: 10.1002/nur.21899] [DOI] [Google Scholar]
Ploukou 2018 {published data only}
- Ploukou S, , Panagopoulou E. Playing Music improves well-being of oncology nurses. Applied Nursing Research 2018;39:77-80. [DOI: 10.1016/j.apnr.2017.11.007] [DOI] [PubMed] [Google Scholar]
Poulsen 2015 {published data only}
- Poulsen AA, Sharpley CF, Baumann KC, Henderson J, Poulsen MG. Evaluation of the effect of a 1-day interventional workshop on recovery from job stress for radiation therapists and oncology nurses: a randomised trial. Journal of Medical Imaging and Radiation Oncology 2015;59(4):491-8. [DOI: 10.1111/1754-9485.12322] [DOI] [PubMed] [Google Scholar]
Prasad 2018 {published data only}
- Prasad K, Poplau S, Brown R, Yale SH, GrossmanE, Varkey AB, et al . Time pressure, clinician stress and medical errors: results from the healthy work place trial. Journal ofGeneral Internal Medicine 2018;33(2):374‐. [Google Scholar]
Procaccia 2021 {published data only}
- Procaccia R, Segre G, Tamanza G, Manzoni GM. Benefits of expressive writing on healthcare workers' psychological adjustment during the COVID-19 Pandemic. Frontiers in Psychology 2021;12:624176. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Proctor 1998 {published data only}
- Proctor R, Stratton-Powell H, Tarrier N, Burns A. The impact of training and support on stress among care staff in nursing and residential homes for the elderly. Journal of Mental Health 1998;7(1):59-71. [Google Scholar]
Profit 2021 {published data only}
- Profit J, Adair KC, Cui X, Mitchell B, Brandon D, Tawfik DS, et al. Randomized controlled trial of the "WISER" intervention to reduce healthcare worker burnout. Journal of Perinatology : official journal of the California Perinatal Association 2021;41(9):2225-34. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Raglio 2020 {published data only}
- Raglio A, Bellandi D, Gianotti M, Zanacchi E, Gnesi M, Monti MC, et al. Daily music listening to reduce work-related stress: a randomized controlled pilot trial. Journal of Public Health (Oxford, England) 2020;42(1):e81-e87. [DOI: ] [DOI] [PubMed] [Google Scholar]
Rajeswari 2019 {published data only}
- Rajeswari H Sreelekha BK, Nappinai S Subrahmanyam, U Rajeswari V. Outcome of accelerated recovery programme on occupational stress among nurses. Indian Journal of Public Health Research and Development 2019;10(12):127-32. [DOI: 10.37506/v10/i12/2019/ijphrd/192207] [DOI] [Google Scholar]
Razavi 1993 {published data only (unpublished sought but not used)}
- Razavi D, Delvaux N, Marchal S, Bredart A, Farvacques C, Paesmans M. The effects of a 24-h psychological training program on attitudes, communication skills and occupational stress in oncology: a randomised study. European Journal of Cancer 1993;29A(13):1858-63. [DOI] [PubMed] [Google Scholar]
Riello 2021 {published data only}
- Riello M, Purgato M, Bove C, Tedeschi F, MacTaggart D, Barbu C, et al. Effectiveness of self-help plus (SH+) in reducing anxiety and post-traumatic symptomatology among care home workers during the COVID-19 pandemic: a randomized controlled trial. Royal Society Open Science 2021;8(11):210219. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ripp 2019 {published data only}
- Ripp J, Lau, CS, Prochno KW. A randomized controlled trial to reduce job burnout using an inter-professional facilitated discussion group intervention. Journal of General internal Medicine 2019;34(2):S116‐S117. [DOI: 10.1007/11606.1525-1497] [DOI] [Google Scholar]
Rollins 2016 {published data only}
- Rollins AL, Kukla M, Morse G, Davis L, Leiter, M, Monroe-DeVita M, et al. Comparative effectiveness of a burnout reduction intervention for behavioral health providers. Psychiatric Services 2016;67(8):920-3. [DOI: ] [DOI] [PubMed] [Google Scholar]
Romig 2012 {published data only}
- Romig MC, Latif A, Gill RS, Pronovost PJ, Sapirstein A. Perceived benefit of a telemedicine consultative service in a highly staffed intensive care unit. Journal of Critical Care 2012;27(4):426.e9-16. [DOI] [PubMed] [Google Scholar]
Rosada 2015 {published data only}
- Rosada RM, Rubik, B, Mainguy B, Plummer J, Mehl-Madrona L. Reiki reduces burnout among community mental health clinicians. Journal of Alternative and Complementary Medicine (New York, N.Y.) 2015;21(8):489-95. [DOI: 10.1089/acm.2014.0403] [DOI] [PubMed] [Google Scholar]
Rowe 2006 {published data only}
- Rowe MM. Four-year longitudinal study of behavioral changes in coping with stress. American Journal of Health Behavior 2006;30(6):602-12. [DOI] [PubMed] [Google Scholar]
- Rowe MM. Teaching health-care providers coping: results of a two-year study. Journal of Behavioral Medicine 1999;22(5):511-27. [DOI] [PubMed] [Google Scholar]
Ruehl 2014 {published data only}
- Ruehl, Brooke D. The psychological and physical heatlh effects of written emotional expression in pediatric hematology/oncology, intensive care, and neonatal intensive care nursing staff. Dissertation abstracts international: section B: the sciences and engineering 2014;74(9-B(E)):Not-Specified. [Google Scholar]
Ruotsalainen 2014 {published data only}
- Ruotsalainen JH, Verbeek JH, Marine, Serra C. Preventing occupational stress in healthcare workers. Cochrane Database of Systematic Reviews 2014, Issue 12. Art. No: CD002892. [DOI: ] [DOI] [PubMed] [Google Scholar]
Ruotsalainen 2015 {published data only}
- Ruotsalainen JH, Verbeek JH, Marine A, Serra C. Preventing occupational stress in healthcare workers. Cochrane Database of Systematic Reviews 2015, Issue 4. Art. No: CD002892. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ruotsalainen 2016 {published data only}
- Ruotsalainen JH, VerbeekJH, Mariné A Serra C. Preventing occupational stress in healthcare workers. Sao Paulo Medical Journal 2016;134(1):92. [DOI: 10.1590/1516-3180.20161341T1] [DOI] [PMC free article] [PubMed] [Google Scholar]
Safarzei 2016 {published data only}
- Safarzei E, Darban F, Mazloum SR. Effect of stress on the nurses’ work life quality in psychiatric ward. IIOAB Journal 2016;7(10):16-21. [Google Scholar]
Saffari 2021 {published data only}
- Saffari M, Bashar FR, Vahedian-Azimi A, Pourhoseingholi MA, Karimi L, Shamsizadeh M, et al. Effect of a multistage educational skill-based program on nurse's stress and anxiety in the intensive care setting: a randomized controlled trial. Behavioural Neurology 2021;2021:8811347. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Salles 2013 {published data only}
- Salles A, Nandagopal K, Walton G. Belonging: a simple, brief intervention decreases burnout. Journal of the American College of Surgeons 2013;217(3):S116. [Google Scholar]
Salyers 2019 {published data only}
- Salyers MP, Garabrant JM, Luther L, Henry N, Fukui S, Shimp D, et al. A comparative effectiveness trial to reduce burnout and improve quality of care. Administration and Policy in Mental Health 2019;46(2):238‐54. [DOI: 10.1007/s10488-018-0908-4] [DOI] [PubMed] [Google Scholar]
Sampson 2020a {published data only}
Sargazi 2018 {published data only}
- Sargazi O, Foroughameri G, Miri S, Farokhzadian J. Improving the professional competency of psychiatric nurses: Results of a stress inoculation training program. Psychiatry Research 2018;270:682-7. [DOI: ] [DOI] [PubMed] [Google Scholar]
Seo 2014 {published data only}
- Seo I, Yong J, Park J, Kim J. Spiritual and psychosocial effects of the spirituality promotion program on clinical nurses. Journal of Korean Academy of Nursing 2014;44(6):726-34. [DOI: 10.4040/jkan.2014.44.6.726] [DOI] [PubMed] [Google Scholar]
Shaw 2021 {published data only}
- Shaw WS, McLellan RK, Besen E, Namazi S, Nicholas K, Dugan AG, et al. A worksite self-management program for workers with chronic health conditions improves worker engagement and retention, but not workplace function. Journal of OccupationalRehabilitation 2021;Mar;32(1):77-86. [DOI: 10.1007/s10926-021-09983-6] [DOI] [PMC free article] [PubMed] [Google Scholar]
Siedsma 2015 {published data only}
- Siedsma M, Emlet L. Physician burnout: can we make a difference together? Critical Care (London, England) 2015;19(1):-. [DOI: 10.1186/s13054-015-0990-x] [DOI] [PMC free article] [PubMed] [Google Scholar]
Silva Junior 2016 {published data only}
- Silva-Junior, JS. Preventing occupational stress in healthcare workers. Sao Paulo medical journal = Revista paulista de medicina 2016;134(1):92. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Smith 2019 {published data only}
- Smith O, Faulkner K, Skiffington A, McShane J, Wan C, Krock M. A randomized controlled trial of an intervention to enhance resilience in acute care nurses (ARISE). Critical Care Medicine 2019;47(1):-. [Google Scholar]
Smith 2021 {published data only}
- Smith, JL, Allen JW, Haack CI, Wehrmeyer KL, Alden KG, Lund MB, et al. Impact of App-delivered mindfulness meditation on functional connectivity, mental health, and sleep disturbances among physician assistant students: randomized, wait-list controlled pilot study. JMIRFformative Research 2021;5(10):e24208. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Smoktunowicz 2021 {published and unpublished data}
- Smoktunowicz, E, Lesnierowska M, Carlbring P, Andersson G, Cieslak R. Resource-based internet intervention (med-stress) to improve well-being among medical professionals: randomized controlled trial. Journal of Medical Internet Research 2021;23(1):e21445. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smoktunowicz, Lesnierowska M, Cieslak R, Carlbring P, Gerhard A. Efficacy of an Internet-based intervention for job stress and burnout among medical professionals: study protocol for a randomized controlled trial. Trials 2019;Jun 10;20(1):338. [DOI] [PMC free article] [PubMed] [Google Scholar]
Son 2019 {published data only}
- Son HK, So WY, Kim M. Effects of aromatherapy combined with music therapy on anxiety, stress, and fundamental nursing skills in nursing students: a randomized controlled trial. International Journal of Environmental Research and Public Health 2019;16(21):4185. [DOI: 10.3390/ijerph16214185] [DOI] [PMC free article] [PubMed] [Google Scholar]
Steinberg 2017 {published data only}
- Steinberg BA, Klatt, M, Duchemin AM, Adriaenssens BB, Chang C, Cohen-Katz D, et al. Feasibility of a mindfiilness-based intervention for surgical intensive care unit personnel. American Journal of Critical Care 2017;26(1):10-18. [DOI: ] [DOI] [PubMed] [Google Scholar]
Strauss 2021 {published data only}
- Strauss C, Gu J, Montero-Marin J, Whittington S, Chapman C Kuyken W. Reducing stress and promoting well-being in healthcare workers using mindfulness-based cognitive therapy for life. InternationalJjournal of Clinical and Health Psychology : IJCHP 2021;21(2):100227. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Taylor 2020 {published data only}
- Taylor J, McLean L, Richards B, Glozier N. Personalised yoga for burnout and traumatic stress in junior doctors. Postgraduate Medical Journal 2020;96(1136):349-57. [DOI: ] [DOI] [PubMed] [Google Scholar]
Tung 2021 {published data only}
- Tung, LN. Using mindful self-compassion (MSC) as a strategy to reduce stress and develop self-compassion in nursing students. Dissertation of a thesis 2021;82.
Uchiyama 2013 {published data only}
- Uchiyama A, Odagiri Y, Ohya Y, Takamiya T, Inoue S, Shimomitsu T. Effect on mental health of a participatory intervention to improve psychosocial work environment: A cluster andomized controlled trial among nurses. Journal of Occupational Health 2013;55(3):173-83. [DOI] [PubMed] [Google Scholar]
Uchiyama 2013b {published data only}
- Uchiyama A, Odagiri Y, Ohya Y, Takamiya T, Inoue S, Shimomitsu T. Effect on mental health of a participatory intervention to improve psychosocial work environment: a cluster randomized controlled trial among nurses. Journal of Occupational Health 2013;55(3):173-83. [DOI] [PubMed] [Google Scholar]
Valley 2017 {published data only}
- Valley MA. Feasibility of a mindfulness-based stress reduction intervention on health care safety. Dissertation abstracts international: section B: the sciences and engineering 2017;78(3-B(E)):Not-Specified. [Google Scholar]
Valley 2017a {published data only}
- Valley MA, Stallones L. Effect of mindfulness-based stress reduction training on health care worker safety: a randomized waitlist controlled trial. Journal of Occupational and Environmental Medicine 2017;Oct;59(10):935-41. [DOI: 10.1097/JOM.0000000000001090] [DOI] [PubMed] [Google Scholar]
vanDorssen Boog 2021 {published data only}
- Dorssen-Boog P, Vuuren T, Jong JP, Veld M. Facilitating health care workers' self-determination: The impact of a self-leadership intervention on work engagement, health, and performance. Journal ofOoccupational and Organizational Psychology 2021;94(2):259-81. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
van Duinen‐van den IJssel 2019 {published data only}
- Duinen-van den Ijssel JC, Bakker C, Smalbrugge M, Zwijsen SA, Appelhof B, Teerenstra S, et al. Effects on staff outcomes from an intervention for management of neuropsychiatric symptoms in residents of young-onset dementia care units: A cluster randomised controlled trial. International Journal of Nursing Studies 2019;96:35-43. [DOI: ] [DOI] [PubMed] [Google Scholar]
vanLeeuwen 2021 {published data only}
- Leeuwen EH, Taris TW, den Heuvel M, Knies E, Rensen EL, Lammers JW. A career crafting training program: results of an intervention study. Frontiers in Psychology 2021;12:664453. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Villani 2013 {published data only}
- Villani D, Grassi A, Cognetta C, Toniolo D, Cipresso P, Riva G. Self-help stress management training through mobile phones: an experience with oncology nurses. Psychological Services 2013;10(3):315-22. [DOI: ] [DOI] [PubMed] [Google Scholar]
Von Baeyer 1983 {published data only}
- Von Baeyer C, Krause L. Effectiveness of stress management training for nurses working in a burn treatment unit. International Journal of Psychiatry in Medicine 1983;13(2):113-26. [DOI] [PubMed] [Google Scholar]
Watanabe 2018 {published data only}
- Watanabe N, Matsuoka Y, Kumachi M, Hamazaki K, Horikosh M, Furukawa TA. Omega-3 fatty acids for a better mental state in working populations - Happy Nurse Project: a 52-week randomized controlled trial. Journal of Psychiatric Research 2018;102:72-80. [DOI: ] [DOI] [PubMed] [Google Scholar]
Watanabe 2019 {published data only}
- Watanabe N, Horikoshi M, Shinmei I, Oe Y, Narisawa T, Kumachi M, et al. Brief mindfulness-based stress management program for a better mental state in working populations - Happy Nurse Project: A randomized controlled trial ✰✰. Journal of Affective Disorders 2019;251:186-194. [DOI: 10.1016/j.jad.2019.03.067] [DOI] [PubMed] [Google Scholar]
Watanabe 2019a {published data only}
- Watanabe N. Brief mindfulness-based stress management program for a better mental state in working populations-happy nurse project: a randomized controlled trials. Psychosomatic Medicine 2019;81(4):A136‐. [DOI: 10.1097/PSY.0000000000000699] [DOI] [PubMed] [Google Scholar]
Weitzman 2021 {published data only}
- Weitzman RE, Wong K, Worrall DM, Park C, McKee S, Tufts RE, et al. Incorporating virtual reality to improve otolaryngology resident wellness: one institution's experience. Laryngoscope 2021;131(9):1972-6. [DOI: ] [DOI] [PubMed] [Google Scholar]
Wilczek Ruzyczka 2021 {published data only}
- Wilczek-Ruzyczka E, Gawronska A, Goral-Polrola, J. An evaluation of transcranial direct current stimulation (Tdcs) in the reduction of occupational burnout syndrome in nurses. Acta Neuropsychologica 2021;19(2):169‐85. [Google Scholar]
Wild 2020 {published data only}
- Wild J, El-Salahi S, Degli Esposti M, Thew GR. Evaluating the effectiveness of a group-based resilience intervention versus psychoeducation for emergency responders in England: a randomised controlled trial. PLOS One 2020;15(11):e0241704. [DOI: 10.1371/journal.pone.0241704] [DOI] [PMC free article] [PubMed] [Google Scholar]
Xu 2021 {published data only}
- Xu B, Li S, Bian W, Wang M, Lin Z, Wang, X. Effects of group psychological counseling on transition shock in newly graduated nurses: a quasi-experimental study. Journal of Nursing Management 2021;30:455–62. [DOI: 10.1111/jonm.13506] [DOI] [PMC free article] [PubMed] [Google Scholar]
Yamagishi 2008 {published data only}
- Yamagishi M, Kobayashi T, Nakamura Y. Effects of web-based career identity training for stress management among Japanese nurses: a randomized control trial. Journal of Occupational Health 2008;50(2):191-3. [DOI] [PubMed] [Google Scholar]
Yang 2018 {published data only}
- Yang J, Tang S, Zhou W. Effect ofmindfulness-based stress reduction therapy on work stress and mental health of psychiatric nurses. Psychiatria Danubina 2018;30(2):189-96. [DOI: ] [DOI] [PubMed] [Google Scholar]
Yang 2018a {published data only}
- Yang E, Schamber E, Meyer RM, Gold JL. Happier healers: randomized controlled trial of mobile mindfulness for stress management. Journal of Alternative and Complementary Medicine 2018;24(5):505-13. [DOI: 10.1089/acm.2015.0301] [DOI] [PubMed] [Google Scholar]
Yong 2020 {published data only}
- Yong JS, Park JF, Park Y, Lee H, Lee G, Rim S. Effects of Holy Name Meditation on the quality of life of hospital middle manager nurses in korea: a 6-month follow-up. Journal of Continuing Education in Nursing 2020;51(5):215224. [DOI: 10.3928/00220124-20200415-06] [DOI] [PubMed] [Google Scholar]
Zwijsen 2015 {published data only}
- Zwijsen SA, Smalbrugge M, Eefsting JA, Twisk JW, Gerritsen DL, Pot AM, et al . Coming to grips with challenging behaviour: a cluster randomised controlled trial on the effects of a new care programme for challenging behaviour on burnout, job satisfaction and job demands of care staff on dementia special care units. International Journal of Nursing Studies 2015;52(1):68-74. [DOI: ] [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Ahmadi 2019 {published data only}
- Ahmadi B, Mosadeghrad AM, Karami B. Effectiveness of resilience education on quality of working life among nursing personnel: a randomized controlled study. Payesh Health Monitor 2019;18(3):279-89. [Google Scholar]
Akyurek 2022 {published data only}
- Akyurek G, Avci N, Ekici G. The effects of "Workplace Health Promotion Program" in nurses: a randomized controlled trial and one-year follow-up. Health Care for Women International 2022;43(9):980-96. [DOI] [PubMed] [Google Scholar]
Bo, 2022 {published data only}
- Bo Y, Wu Q, Hu C, Peng W, Xie X, Zhang QX. Effect of mindfulness self-compassion training on job burnout of psychiatric nurses. ? ?;?:?. [Google Scholar]
Fainstad 2022 {published data only}
- Fainstad T, Mann A, Suresh K, Shah P, Dieujuste N, Thurmon K, et al. Effect of a novel online group-coaching program to reduce burnout in female resident physicians: a randomized clinical trial. JAMA Network Open 2022;5(5):e2210752. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fei 2019 {published data only}
- Fei Y. Effects of emotional resilience training on nurses' perceived stress, positive and negative emotions and sleep quality. Revista Argentina de Clínica Psicológica 2019;28(2):199-209. [Google Scholar]
Ferreres‐Galan 2022 {published data only}
- Ferreres-Galán V, Navarro-Haro MV, Peris-Baquero Ó, Guillén-Marín S, Luna-Hermoso J, Osma J. Assessment of acceptability and initial effectiveness of a unified protocol prevention program to train emotional regulation skills in female nursing professionals during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health 2022;19(9):5715. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fraiman 2022 {published data only}
- Fraiman YS, Cheston CC, Cabral HJ, Allen C, Asnes AG, Barrett JT, et al. Effect of a novel mindfulness curriculum on burnout during pediatric internship: a cluster randomized clinical trial. JAMA Pediatrtrics 2022;176(4):365-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ghods 2017 {published data only}
- Ghods AA, Sotodehasl N, Khalaf ME, Mirmohamadkhani M. Effects of lavender essential oil inhalation on nurses' job stress. Koomesh 2017;19(2):421-8. [Google Scholar]
Goktas 2022 {published data only}
- Goktas S, Gezginci E, Kartal H. The Effects of motivational messages sent to emergency nurses during the COVID-19 pandemic on job satisfaction, compassion fatigue, and communication skills: a randomized controlled trial. Journal of Emergency Nursing 2022;48(5):547-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hata 2022 {published data only}
- Hata SR, Berkowitz LR, James K, Simpkin AL. An interprofessional group intervention to promote faculty well-being: a randomized clinical trial. Journal of Continuing Education in the Health Professions 2022;42(1):e75-e82. [DOI] [PubMed] [Google Scholar]
Hsieh 2022 {published data only}
- Hsieh HF, Huang YT, Ma SC, Wang YW. Occupational burnout and stress of nurses in Taiwan regarding COVID-19: an intervention with gong medication. Journal of Nursing Management 2022;-:13653. [DOI] [PMC free article] [PubMed] [Google Scholar]
Imamura 2019 {published data only}
- Imamura K, Tran TT, Nguyen HT, Kuribayashi K, Sakuraya A, Nguyen AQ, et al. Effects of two types of smartphone-based stress management programmes on depressive and anxiety symptoms among hospital nurses in Vietnam: a protocol for three-arm randomised controlled trial. BMJ Open 2019;9(4):e025138. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Joshi 2022 {published data only}
- Joshi SP, Wong AI, Brucker A, Ardito TA, Chow SC, Vaishnavi S, et al. Efficacy of transcendental meditation to reduce stress among health care workers: a randomized clinical trial. JAMA Network Open 2022;5(9):e2231917. [DOI] [PMC free article] [PubMed] [Google Scholar]
Klatt 2012 {published data only}
- Klatt M, Steinberg B, Marks D, Duchemin A. Changes in physiological and psychological markers of stress in hospital personnel after a low-dose mindfulness-based worksite intervention. BMC Complementary and Alternative Medicine 2012;12(Suppl 1):O16. [Google Scholar]
Klatt 2022 {published data only}
- Klatt M, Westrick A, Bawa R, Gabram O, Blake A, Emerson B. Sustained resiliency building and burnout reduction for healthcare professionals via organizational sponsored mindfulness programming. Explore (NY) 2022;18(2):179-86. [DOI] [PubMed] [Google Scholar]
Lu 2020 {published data only}
- Lu D, Lan M, Zhang N. [Intervention of Balint group on the emotional labor and job burnout of nurses in cardiology]. Zhonghua lao dong wei sheng zhi ye bing za zhi = Zhonghua laodong weisheng zhiyebing zazhi = Chinese Journal of Industrial Hygiene and Occupational Diseases 2020;38(3):203-6. [DOI: ] [DOI] [PubMed] [Google Scholar]
Montaner 2022 {published data only}
- Montaner X, Tarrega S, Pulgarin M, Moix J. Effectiveness of Acceptance and Commitment Therapy (ACT) in professional dementia caregivers burnout. Clinical Gerontology 2022;45(4):915-26. [DOI] [PubMed] [Google Scholar]
Moss 2022 {published data only}
- Moss M, Edelblute A, Sinn H, Torres K, Forster J, Adams T, et al. The effect of creative arts therapy on psychological distress in health care professionals. American Journal of Medicine 2022;135(10):1255-62 e5. [DOI] [PubMed] [Google Scholar]
Perez 2022 {published data only}
- Perez V, Menendez-Crispin EJ, Sarabia-Cobo C, Lorena P, Fernandez-Rodriguez A, Gonzalez-Vaca J. Mindfulness-based intervention for the reduction of compassion fatigue and burnout in nurse caregivers of institutionalized older persons with dementia: a randomized controlled trial. International Journal of Environmental Research and Public Health 2022;19(18):11441. [DOI] [PMC free article] [PubMed] [Google Scholar]
Purdie 2022 {published data only}
- Purdie DR, Federman M, Chin A, Winston D, Bursch B, Olmstead R, et al. Hybrid delivery of mindfulness meditation and perceived stress in pediatric resident physicians. J ournal ofClinical Psychology in Medical Settings 2022;Epub ahead of print:-. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rogala 2016 {published data only}
- Rogala A, Smoktunowicz E, Zukowska K, Kowalska M, Cieslak R. [The helpers' stress: effectiveness of a web-based intervention for professionals working with trauma survivors in reducing job burnout and improving work engagement]. Stres pomagajacych - efektywnosc interwencji internetowej dla osob pracujacych z ofiarami traumy w obnizaniu wypalenia zawodowego i wzmacnianiu zaangazowania w prace 2016;67(2):223-37. [DOI: ] [DOI] [PubMed] [Google Scholar]
Sasaki 2021 {published data only}
- Sasaki N, Imamura K, Tran TT, Nguyen HT, Kuribayashi K, Sakuraya A, et al. Effects of smartphone-based stress management on improving work engagement among nurses in Vietnam: secondary analysis of a three-arm randomized controlled trial: a randomized clinical trial of in-person and digital mindfulness meditation. Journal of Medical Internet Research 2021;23(2):e20445. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Spilg 2022 {published data only}
- Spilg EG, Kuk H, Ananny L, McNeill K, LeBlanc V, Bauer BA, et al. The impact of Stress Management and Resailience Training (SMART) on academic physicians during the implementation of a new Health Information System: an exploratory randomized controlled trial. PLOS One 2022;17(4):e0267240. [DOI] [PMC free article] [PubMed] [Google Scholar]
Taft 2021 {published data only}
- Taft TS, Keshmiri F, Dehabadi SJ, Jambarsang S, Aghaei F, Sadeghian HA. The effect of educational intervention on stress management in cardiac surgery nurses. Journal of Military Medicine 2021;22(12):1280-7. [DOI: 10.30491/JMM.22.12.1280] [DOI] [Google Scholar]
Taylor 2022 {published data only}
- Taylor H, Cavanagh K, Field AP, Strauss C. Health care workers' need for headspace: findings from a multisite definitive randomized controlled trial of an unguided digital mindfulness-based self-help app to reduce healthcare worker stress. JMIR Mhealth and Uhealth 2022;10(8):e31744. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vajpeyee 2022 {published data only}
- Vajpeyee M, Tiwari S, Jain K, Modi P, Bhandari P, Monga G, et al. Yoga and music intervention to reduce depression, anxiety, and stress during COVID-19 outbreak on healthcare workers. International Journal of Social Psychiatry 2022;68(4):798-807. [DOI] [PubMed] [Google Scholar]
Valipour 2020 {published data only}
- Valipour S, Aazami S, Mozafari M. The effect of training intervention on the level of stress management skills in novice nurses working at educational hospitals in Ilam Province. Journal of Cardiovascular Disease Research 2020;11(4):98-104. [DOI: 10.31838/jcdr.2020.11.04.17] [DOI] [Google Scholar]
Xiao Yan 2019 {published data only}
- Xiao Y, Feng C, MS, Wang H, Liu N. Application of drum circle music therapy combined with psychological diary in relieving work pressure of psychiatric nurses [鼓圈音乐治疗联合心理日记在缓解 精神科护士工作压力中的应用]. Nursing of Integrated Traditional Chinese & Western Medicine 2019;5(10):156-8. [Google Scholar]
References to ongoing studies
Al‐Hammouri 2022 {published data only}
- Al-Hammouri et a l. The effect of mindfulness-based intervention on behavioral and psychological variables among Jordanian nurses: a randomized controlled trial study. International Clinical Trials Registery Platform. https://trialsearch.who.int/Trial2.aspx?TrialID=ACTRN12622000389707 07/03/2022.
Baker 2015 {published data only}
- Baker C, Huxley P, Dennis M, Islam S, Russell I. Alleviating staff stress in care homes for people with dementia: protocol for stepped-wedge cluster randomised trial to evaluate a web-based Mindfulness- Stress Reduction course. BMC Psychiatry 2015;15:317. [DOI: 10.1186/s12888-015-0703-7] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bateman 2020 {published data only}
- Bateman ME, Hammer R, Byrne A, Ravindran N, Chiurco J, Lasky S, et al. Death Cafés for prevention of burnout in intensive care unit employees: study protocol for a randomized controlled trial (STOPTHEBURN). Trials 2020;21(1):1019. [DOI: 10.1186/s13063-020-04929-4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bratt 2022 {published data only}
- Bratt AS, Johansson M, Holmberg M, Fagerstrom C, Elmqvist C, Rusner M, et al. An internet-based compassion course for healthcare professionals: rationale and protocol for a randomised controlled trial. Internet Interventions 2022;28:100463. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jeffers 2017 {published data only}
- Jeffers C . Caring for HEalthy Engaged Resilient staff: effect of a wellness training program on stress in emergency department nurses. International Clinical Trials Registery Platform https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?ACTRN=12617000798369 2017.
Kuribayashi 2019 {published data only}
- Kuribayashi K, Imamura K, Watanabe K, Miyamoto Y, Takano A, Sawada U, et al. Effects of an internet-based cognitive behavioral therapy (iCBT) intervention on improving depressive symptoms and work-related outcomes among nurses in Japan: a protocol for a randomized controlled trial. BMC Psychiatry 2019;19(1):245. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ng 2019 {published data only}
- Ng SM, Lo HH, Yeung A, Young D, Fung MH, Wang AM. Study protocol of brief daily body-mind-spirit practice for sustainable emotional capacity and work engagement for community mental health workers: a multi-site randomized controlled trial. Frontiers in Psychology 2020 ;11:1482. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pérula‐de Torres 2019 {published data only}
- Pérula-de Torres L-A, Verdes-Montenegro Atalaya JC, García-Campayo J, Roldán-Villalobos A, Magallón-Botaya R, Bartolomé-Moreno C, et al. Controlled clinical trial comparing the effectiveness of a mindfulness and self-compassion 4-session programme versus an 8-session programme to reduce work stress and burnout in family and community medicine physicians and nurses: MINDUUDD study protocol. BMC Family Practice 2019 ;20(1):24. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rees 2018 {published data only}
- Rees C, Craigie M, Slatyer S, Heritage B, Harvey C, Brough P, et al. Mindful self-care and resiliency (MSCR): protocol for a pilot trial of a brief mindfulness intervention to promote occupational resilience in rural general practitioners. BMJ Open 2018;8(6):e021027. [DOI] [PMC free article] [PubMed] [Google Scholar]
Weiner 2020 {published data only}
- Weiner L, Berna F, Nourry N, Severac F, Vidailhet P, Mengin AC. Efficacy of an online cognitive behavioral therapy program developed for healthcare workers during the COVID-19 pandemic: the REduction of STress (REST) study protocol for a randomized controlled trial. Trials 2020;21(1):870. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Alberdi 2016
- Alberdi A, Aztiria A, Basarab A. Towards an automatic early stress recognition system for office environments based on multimodal measurements: a review. Journal of Biomedical Informatics 2016;59:49-75. [DOI] [PubMed] [Google Scholar]
Arrigoni 2015
- Arrigoni C, Caruso R, Campanella F, Berzolari FG, Miazza D, Pelissero G. Investigating burnout situations, nurses' stress perception and effect of a post-graduate education program in health care organizations of northern Italy: a multicenter study. Giornale Italiano di Medicina del Lavoro ed Ergonomia 2015;37(1):39-45. [PubMed] [Google Scholar]
Aryankhesal 2019
- Aryankhesal A, Mohammadibakhsh R, Hamidi Y, Alidoost S, Behzadifar M, Sohrabi R, Farhadi Z. Interventions on reducing burnout in physicians and nurses: a systematic review. Medical Journal of the Islamic Republic of Iran 2019;33:77. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bamber 2006
- Bamber MR. CBT for Occupational Stress in Health Professionals. Introducing a Schema-Focused Approach. London: Routledge, 2006. [DOI: ] [Google Scholar]
Beck 1961
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry 1961;4:561-71. [DOI] [PubMed] [Google Scholar]
Beck 2005
- Beck AT. The current state of cognitive therapy: a 40-year retrospective. Archives of General Psychiatry 2005;62(9):953-9. [DOI] [PubMed] [Google Scholar]
Beehr 1987
- Beehr TA and O'Hara K. Methodological designs for the evaluation of occupational stress interventions. Journal of Occupational Psychology 1987;53:187-94. [Google Scholar]
Blake 2020
- Blake H, Bermingham F, Johnson G, Tabner A. Mitigating the psychological impact of COVID-19 on healthcare workers: a Digital Learning Package. International Journal of Environmental Resesrch and Public Health 2020;17(9):-. [DOI] [PMC free article] [PubMed] [Google Scholar]
Borges 2021
- Borges de Souza TP, Fumiko Sato Kurebayashi PhD Leonice, Nery de Souza-Talarico PhD Juliana, Natalia Teresa Turrini PhD Ruth. The effectiveness of chair massage on stress and pain in oncology. International Journal of Therapeutic Massage & Bodywork: Research, Education, & Practice 2021;14(3):27-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bridgeman 2018
- Bridgeman PJ, Bridgeman MB, Barone J. Burnout syndrome among healthcare professionals. American Journal of Health System Pharmacy 2018;75(3):147-52. [DOI] [PubMed] [Google Scholar]
Burton 2010
- Joan Burton. WHO hHealthy Workplace Framework and Model: Background and Supporting Literature and Practices. World Health Organization. . WHO, 2010. [WEBSITE: https://apps.who.int/iris/handle/10665/113144] [Google Scholar]
Busireddy 2016
- Busireddy K, Jonathan M, Ellison KE, Ren V, Panda M, Qayyum R. Efficacy of interventions to reduce resident physician burnout: A systematic review. Journal of General Internal Medicine 2016;31(2):S209. [DOI] [PMC free article] [PubMed] [Google Scholar]
Campbell 2001
- Campbell MK, Mollison J, Grimshaw JM. Cluster trials in implementation research: estimation of intracluster correlation coefficients and sample size. Statistics in Medicine 2001;20(3):391-9. [DOI] [PubMed] [Google Scholar]
Clough 2017
- Clough BA, March S, Chan RJ, Casey LM, Phillips R, Ireland MJ. Psychosocial interventions for managing occupational stress and burnout among medical doctors: a systematic review. Systematic Reviews 2017; 6(1):144 . [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
CMA Prediction Intervals [Computer program]
- CMA Prediction Intervals. https://www.meta-analysis.com, unknown.
Cohen 1983
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior 1983;24(4):385-96. [PubMed] [Google Scholar]
Costello 2016
- Costello EJ. Early detection and prevention of mental health problems: developmental epidemiology and systems of support. Journal of Clinical Child andAdolescent Psychology 2016;45(6):710-7. [DOI] [PubMed] [Google Scholar]
Covidence 2022 [Computer program]
- Covidence. Version accessed 1 March 2022. Melbourne, Australia: Ventas Health Innovation, 2022. Available at covidence.org.
Creswell 2014
- Creswell JDavid, Lindsay Emily K. How does mindfulness training affect Health? A mindfulness stress buffering account. Current Directions in Psychological Science 2014;23(6):401-7. [Google Scholar]
De Hert 2020
- De Hert S. Burnout in healthcare workers: prevalence, impact and preventative strategies. Local andRegional Anesthesia 2020;13:171-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
de Wijn 2022
- Wijn AN and Van der Doef MP. A meta-analysis on the effectiveness of stress management interventions for nurses: capturing 14 years of research. International Journal of Stress Management 2022;29(2):113-29. [Google Scholar]
Demerouti 2003
- Demerouti E, Bakker AB, Vardakou I, Kantas A. The convergent validity of two burnout instruments: A multitrait-multimethod analysis. European Journal of Psychological Assessment 2003;19:12-23. [Google Scholar]
Faltinsen 2022
- Faltinsen E, Todorovac A, Staxen Bruun L, Hróbjartsson A, Gluud C, Kongerslev MT, et al. Control interventions in randomised trials among people with mental health disorders. Cochrane Database of Systematic Reviews 2022, Issue 4. Art. No: MR000050. [DOI: 10.1002/14651858.MR000050.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Fang 2015
- Fang R, Li X. A regular yoga intervention for staff nurse sleep quality and work stress: a randomised controlled trial. Journal of Clinical Nursing 2015;24(23-24):3374-9. [DOI] [PubMed] [Google Scholar]
Faul 2017
- Faul F, Erdfelder E, Lang A, Buchner A. Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods 2007;39.2:175-91. [DOI] [PubMed] [Google Scholar]
Fendel 2021
- Fendel JC, Bürkle JJ, Göritz AS. Mindfulness-based interventions to reduce burnout and stress in physicians: a systematic review and meta-analysis. Academic Medicine 2021;96(5):751-64. [DOI] [PubMed] [Google Scholar]
Giga 2018
- Giga SI, Fletcher IJ, Sgourakis G, Mulvaney CA, Vrkljan BH. Organisational level interventions for reducing occupational stress in healthcare workers. Cochrane Database of Systematic Reviews 2018, Issue 4. Art. No: CD013014. [DOI: 10.1002/14651858.CD013014] [DOI] [Google Scholar]
Goldberg 1991
- Goldberg D, Williams P. A User's Guide to the General Health Questionnaire. London: NFER–Nelson, 1991. [Google Scholar]
Guyatt 2011
- Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction—GRADE evidence profiles and summary of findings tables. Journal of Clinical Epidemiology 2011;64(4):383-94. [DOI] [PubMed] [Google Scholar]
Hassard 2018
- Hassard J, Teoh KR, Visockaite G, Dewe P, Cox T. The cost of work-related stress to society: a systematic review. Journal of Occupational Health Psychology 2018;23(1):1-17. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane-handbook.org.
Higgins 2022
- Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). www.training.cochrane.org/handbook 2022;6.3.
Hofmann 2017
- Hofmann SG, Gómez AF. Mindfulness-based interventions for anxiety and depression. Psychiatric Clinics of North America 2017;40(4):739-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jung 2021
- Jung SE, Ha DJ, Park JH, Lee B, Kim MS, Sim KL, et al. The effectiveness and safety of mind-body modalities for mental health of nurses in hospital setting: a systematic review. InternationalJournal of Environmental Research and Public Health 2021;18(16):8855. [DOI] [PMC free article] [PubMed] [Google Scholar]
Knapp 1988
- Knapp TR. Stress versus strain: a methodological critique. Nursing Research 1988;37:181-4. [PubMed] [Google Scholar]
Kristensen 2005
- Kristensen TS, Borritz M, Villadsen E, Christensen KB. The Copenhagen Burnout Inventory: a new tool for the assessment of burnout. Work & Stress 2005;19(3):192-207. [Google Scholar]
Kunzler 2020
- Kunzler AM, Helmreich I, Chmitorz A, König J, Binder H, Wessa M, et al. Psychological interventions to foster resilience in healthcare professionals. Cochrane Database of Systematic Reviews 2020, Issue 7. Art. No: CD012527. [DOI: 10.1002/14651858.CD012527.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lovibond 1995
- Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research andTherapy 1995;33(3):335-43. [DOI] [PubMed] [Google Scholar]
Mahdizadeh 2019
- Mahdizadeh M, Jaberi AA, Bonabi TN. Massage therapy in management of occupational stress in emergency medical services Ssaffs: a randomized controlled trial. International Journal of Therapeutic Massage & Bodywork 2019;12(1):16-22. [PMC free article] [PubMed] [Google Scholar]
Marine 2000
- Marine A, Serra C. Effectiveness of occupational stress management programmes. Cochrane Database of Systematic Reviews 2000, Issue 2. Art. No: CD002892. [DOI: 10.1002/14651858.CD002892.pub2] [DOI] [Google Scholar]
Maslach 1982
- Maslach C. Burnout: the Cost of Caring. New York, NY: Prentice-Hall, 1982. [Google Scholar]
Maslach 1996
- Maslach C, Jackson SE, Leiter SP. Maslach Burnout Inventory Manual. 3rd edition. Palo Alto, CA: Consulting Psychologists Press, 1996. [Google Scholar]
Maunder 2006
- Maunder RG, Lancee WJ, Balderson KE, Bennett JP, Borgundvaag B, Evans S, et al. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerging Infectious Diseases 2006;12(12):1924-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nielsen 2010
- Nielsen K, Taris T, Cox T. The future of organizational interventions: addressing the challenges of today's organizations. Work and Stress 2010;24(3): 219–33. [DOI: ] [Google Scholar]
Patel 2019
- Patel RS, Sekhri S, Bhimanadham NN, Imran S, Hossain S. A review on strategies to manage physician burnout. Cureus 2019;11(6):e4805. [DOI] [PMC free article] [PubMed] [Google Scholar]
Richardson 2008
- Richardson KM, Rothstein HR. Effects of occupational stress management intervention programs: a meta-analysis. Journal of Occupational Health Psychology 2008 ;13(1):69. [DOI] [PubMed] [Google Scholar]
Rohatgi, 2022 [Computer program]
- WebPlotDigitizer. Rohatgi, A. California: https://automeris.io/WebPlotDigitizer, September 2022.
Sanfilippo 2017
- Sanfilippo F, Noto A, Foresta G, Santonocito C, Palumbo GJ, Arcadipane A, et al. Incidence and factors associated with burnout in anesthesiology: a systematic review. Biomed Research International 2017;2017:8648925. [DOI] [PMC free article] [PubMed] [Google Scholar]
Santesso 2020
- Santesso N, Glenton C, Dahm P, Garner P, Akl EA, Alper B, et al. GRADE guidelines 26: informative statements to communicate the findings of systematic reviews of interventions. Journal of Clinical Epidemiology 2020;119:126-35. [PMID: ] [DOI] [PubMed] [Google Scholar]
Schaafsma 2021
- Schaafsma FG, Hulsegge G, Jong MA, Overvliet J, Rossum EF, Nieuwenhuijsen K. The potential of using hair cortisol to measure chronic stress in occupational healthcare; a scoping review. Journal of Occupational Health 2021;63(1):e12189. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schünemann 2013
- Schünemann H, Brożek J, Guyatt G, Oxman A, editors. GRADE handbook for grading quality of evidence and strength of recommendations. Updated October 2013. The GRADE Working Group, 2013. [Google Scholar]
Shanafelt 2010
- Shanafelt TD, Balch CM, Bechamps G, Russell T, Dyrbye L, Satele D, et al. Burnout and medical errors among American surgeons. Annals of Surgery 2010;251(6):995-1000. [DOI] [PubMed] [Google Scholar]
Shoman 2021
- Shoman Y, Marca SC, Bianchi R, Godderis L, Molen HF, Guseva Canu I. Psychometric properties of burnout measures: a systematic review. Epidemiology and Psychiatric Sciences 2021;Jan 13(30):e8. [DOI: doi: 10.1017/S2045796020001134] [DOI] [PMC free article] [PubMed] [Google Scholar]
Simmons 2018
- Simmons J, Nelson L, Simonsohn, U. False-Positive Citations. Perspectives on Psychological Science 2018;13(2):255–9. [DOI: ] [DOI] [PubMed] [Google Scholar]
Spielberger 1970
- Spielberger CD, Gorsuch RL, Lushene RE. Manual for the State-Trait Anxiety Inventory (Self-Evaluation Questionnaire). Palo Alto, CA: Mind Garden, 1970. [Google Scholar]
Spinelli 2019
- Spinelli C, Wisener M, Khoury B. Mindfulness training for healthcare professionals and trainees: a meta-analysis of randomized controlled trials. Journal of Psychosomatic Research 2019;120:29-38. [DOI] [PubMed] [Google Scholar]
STATA 2022 [Computer program]
- STATA/BE 17.0. by StataCorp LLC, College Station, Tx USA, , 2022.
Tang 2015
- Tang Yi-Yuan, Hölzel Britta K, Posner Michael I. The neuroscience of mindfulness meditation. Nature Reviews. Neuroscience 2015;16(4):213-25. [DOI] [PubMed] [Google Scholar]
Tawfik 2019
- Tawfik DS, Scheid A, Profit J, Shanafelt T, Trockel M, Adair KC, et al. Evidence relating health care Provider burnout and Quality of care: a systematic review and meta-analysis. Annls of Internal Medicine 2019;171(8):555-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
van Dam 2021
- van Dam Ar. A clinical perspective on burnout: diagnosis, classification, and treatment of clinical burnout. European Journal of Work and Organizational Psychology 2021;30(5):732-41. [Google Scholar]
van der Molen 2020
- Molen HF, Nieuwenhuijsen K, Frings-Dresen MH, Groene G. Work-related psychosocial risk factors for stress-related mental disorders: an updated systematic review and meta-analysis. BMJ Open 2020;10(7):e034849. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wiederhold 2018
- Wiederhold BK, Cipresso P, Pizzioli D, Wiederhold M, Riva G. Intervention for physician burnout: a systematic review. Open Medicine 2018;13(1):253-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zhang 2020
- Zhang XJ, Song Y, Jiang T, Ding N, Shi TY. Interventions to reduce burnout of physicians and nurses: An overview of systematic reviews and meta-analyses. Medicine (Baltimore) 2020;99(26):e20992. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zhang 2021
- Zhang M, Murphy B, Cabanilla A, Yidi C. Physical relaxation for occupational stress in healthcare workers: a systematic review and network meta-analysis of randomized controlled trials.. J Occupational Health 2021;63(1):e12243. [DOI: doi: 10.1002/1348-9585.12243] [DOI] [PMC free article] [PubMed] [Google Scholar]
Zigmond 1983
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica 1983;67(6):361-70. [DOI] [PubMed] [Google Scholar]
Zwetsloot 2017
- Zwetsloot P, Naald M, Sena ES, Howells DW, IntHout J, AH de Groot J, et al. Standardized mean differences cause funnel plot distortion in publication bias assessments. Elife 2017;Sep 8(6):e24260. [DOI: 10.7554/eLife.24260.] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Marine 2006
- Marine A, Ruotsalainen Jani H, Serra C, Verbeek Jos H. Preventing occupational stress in healthcare workers. Cochrane Database of Systematic Reviews 2006, Issue 4. Art. No: CD002892. [DOI: 10.1002/14651858.CD002892.pub2] [DOI] [PubMed] [Google Scholar]
Ruotsalainen 2014
- Ruotsalainen JH, Verbeek JH, Mariné A, Serra C. Preventing occupational stress in healthcare workers. Cochrane Database of Systematic Reviews 2014, Issue 12. Art. No: CD002892. [DOI: 10.1002/14651858.CD002892.pub3] [DOI] [PubMed] [Google Scholar]
Ruotsalainen 2015
- Ruotsalainen JH, Verbeek JH, Mariné A, Serra C. Preventing occupational stress in healthcare workers . Cochrane Database of Systematic Reviews 2015, Issue 4. Art. No: CD002892. [DOI: 10.1002/14651858.CD002892.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Serra 2000
- Serra C . Occupational health programmes for psychological stress in health care professionals. Cochrane Database of Systematic Reviews 2000, Issue 1,. Art. No: CD002892. [DOI: 10.1002/14651858.CD002892] [DOI] [Google Scholar]


