Abstract
Objectives:
There is substantial evidence that cognitive behavioral therapy (CBT) and mindfulness-based cognitive therapy (MBCT) improve symptoms and functioning in adults with mood and psychotic disorders. There has been little work directly comparing these treatments among adolescents with early-onset mood or psychosis symptoms.
Method:
We conducted a randomized controlled trial comparing remotely administered group CBT to group MBCT for adolescents (ages 13–17) with a mood disorder or attenuated psychosis symptoms. Adolescents attended 9 sessions over 2 months; their parents attended parallel groups focused on the same skill practices. Participants were assessed for psychiatric symptoms and functioning at post-treatment and 3-months post-treatment.
Results:
Sixty-six youth (Mean age = 15.1 years, SD = 1.4; 44 females [66.7%]) initiated the trial (32 in CBT and 34 in MBCT), with 54 retained at post-treatment and 53 at the 3-month follow-up. The treatments were associated with comparable improvements in adolescents’ mood, anxiety, attenuated psychosis symptoms and psychosocial functioning over 5-months. CBT was associated with greater improvements than MBCT in emotion regulation and well-being during the post-treatment period. MBCT (compared to CBT) was associated with greater improvements in social functioning among adolescents with greater childhood adversity. Both treatments had comparable rates of retention, but youth and parents reported more satisfaction with CBT than MBCT.
Conclusions:
The beneficial effect of both treatments in a group telehealth format is encouraging. Due to our limited sample, future research should investigate whether adolescents’ history of adversity and treatment preferences replicate as treatment moderators for youth with mood or psychosis symptoms.
Keywords: MBCT, CBT, RCT, youth, depression, anxiety, psychosis, high risk, treatment
Introduction
Significant efforts have been undertaken to identify and treat youth with mood and psychosis symptoms (e.g., Birmaher et al., 2018). The uncertain prognoses of these youth has led to a push for transdiagnostic treatments that include both psychiatric groups (e.g., McGorry et al., 2018; Weintraub et al., 2020). Adverse childhood experiences such as abuse or community adversity are also common among youth with mood or attenuated psychosis symptoms (APS) and confer risk for psychiatric illness and functional impairments (LeMoult et al., 2020; Loewy et al., 2019). Thus, it is critical that adolescents with emerging mood or psychotic disorders receive early interventions that are acceptable, accessible, and help arrest illness escalation.
Mindfulness-based cognitive therapy (MBCT) and traditional cognitive behavioral therapy (CBT) have been found to reduce depressive symptoms and decrease mood episode recurrence in adolescents (Oud et al., 2019; Reangsing et al., 2021). Among youth at high risk for psychotic disorders, traditional CBT is associated with reductions in APS and psychosis onset over 12 months (Hutton & Taylor, 2014), whereas MBCT is associated with improvements in social anxiety symptoms and social functioning (Vignaud et al., 2019). There is a paucity of research that directly compares MBCT and traditional CBT in younger high-risk populations.
In this study, both CBT and MBCT were administered in group telehealth format over 9 sessions among adolescents (ages 13–17) with mood disorders or APS. Parents attended parallel groups containing the same skill-training content as their child. Over 5 months, we examined the effects of these treatments on mood symptoms, APS, psychosocial functioning and treatment satisfaction.
Method
The study was approved by the Institutional Review Board at the University of California, Los Angeles. Participants were screened for mood disorders based on the MINI International Neuropsychiatric Interview for children and adolescents, DSM-IV version (Sheehan et al., 2010). Participants were assessed for clinical high risk for psychosis (i.e., attenuated psychosis symptom syndrome) using the Structured Interview for Prodromal States (Miller et al., 2003). Adolescents were required to have a parent participate in the parent group. The entire study (consenting, study assessments, and treatment sessions) was conducted virtually on Zoom.
Study Interventions
Both CBT and MBCT treatments were administered over nine 90-minute weekly sessions in group format, with at least six participants and parents per cohort. CBT included psychoeducation, cognitive skills (e.g., cognitive reappraisal) and behavioral skills (e.g., opposite action). MBCT included psychoeducation, mindful awareness exercises, and cognitive coping strategies. Adolescents attended 75–80 minutes with their peers, while parents attended in a separate virtual room with other parents. In the final 10–15 minutes of each 90-minute session, the parents and adolescents joined together to discuss the skill(s) of the week and planned for how/when they would practice them. Greater details about treatments, randomization, and fidelity measurement are presented in the Supplemental Materials.
Study Outcomes
Assessments were conducted at baseline (i.e., within two weeks prior to the start of treatment), post-treatment (i.e., within two weeks following the final group session), and 3 months after the end of treatment. Independent evaluators assessed mood symptoms using the Children’s Depression Rating Scale, Revised (CDRS; Poznanski & Mokros, 1996) and the Young Mania Rating Scale (YMRS; Young et al., 1978). Youth made ratings of anxiety and depression using the Depression, Anxiety, and Stress Scale (DASS; Henry & Crawford, 2005), and APS on the Prodromal Questionnaire Brief (PQ-B; Loewy et al., 2011).
Psychosocial functioning was measured with the Global Functioning Scale: Social and Role Scales (Auther et al., 2006; Niendam et al., 2006), the self-rated (KINDL; Ravens-Sieberer & Bullinger, 2000), and the Difficulties with Emotion Regulation Scale (DERS; Gratz & Roemer, 2004). Youth rated adverse events at baseline using the Philadelphia Adverse Childhood Experiences Survey (PHL-ACEs; Cronholm et al., 2015).
Treatment completers were considered those who attended at least two-thirds (6 or more) of the treatment sessions. Treatment satisfaction was measured at post-treatment through youth and parent self-reports using the Client Satisfaction Questionnaire-8 (CSQ-8; Larsen et al., 1979) and a single 10-point Likert-type item, with 10 being the most satisfied.
Data Analyses
Analyses of variance (ANOVA) and chi-square tests were conducted using the Statistical Package for Social Sciences (SPSS 27) to examine differences between treatment conditions on baseline clinical and demographic variables and treatment acceptability. Intent-to-treat analyses were conducted using repeated measures mixed-effect regression models to examine the main and interactive effects of treatment condition (CBT versus MBCT) and assessment visit on outcome variables over the 5-month study. Secondarily, we examined adverse childhood experiences (measured continuously) as a moderator of treatment outcomes. More details regarding statistical analyses are found in the Supplemental Materials.
Results
A total of 69 youth met study inclusion criteria and 66 were enrolled in the trial (32 in CBT and 34 in MBCT). Youth were on average 15.1 years old (SD = 1.4), predominantly female (66.7%) and non-Hispanic White (75.8%). The majority of youth (n = 48; 72.7%) met criteria for a depressive spectrum disorder and nine (13.6%) met criteria for a bipolar spectrum disorder. Additionally, eleven youth in the sample (16.7%) met SIPS criteria for the attenuated psychosis symptom (APS) syndrome, nine of whom had a comorbid mood disorder. Among the sample, the mean attenuated psychosis symptom severity on the PQ-B was 20.1 (SD = 17.9), with 43.9% scoring ≥ 18 (the screening threshold for a psychosis-enriched sample to suggest the presence of meaningful positive symptoms and distress (Savill et al., 2018)).
There was an imbalance between treatment groups in the number of youth with the APS syndrome, as there were eight in the CBT condition and three in the MBCT condition. As shown in the Supplemental Materials (pgs. 6–7), there were no differences between youth with the APS syndrome and those without the syndrome on clinical or demographic variables, nor did the presence or absence of the APS syndrome moderate the effect of treatment or study visit on psychiatric symptoms or psychosocial functioning. There were also no differences between the two treatment conditions in youth demographic characteristics or baseline clinical variables (see Table 1).
Table 1.
Baseline demographic and clinical characteristics of study adolescents
| Demographics | MBCT (n=34) | CBT (n=32) | Total (N=66) |
|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | |
| Youth age (years) | 15.1 (1.3) | 15.1 (1.5) | 15.1 (1.4) |
| Primary parent age (years) | 50.3 (5.4) | 49.8 (5.9) | 50.3 (5.4) |
| Youth academic grade | 10th (1.4) | 10th (1.4) | 10th (1.4) |
| Household income (selected in ranges) | $100,000 – $149,000 | $100,000 – $149,000 | $100,000 – $149,000 |
| PHL-ACES total score | 3.7 (3.4) | 3.4 (2.5) | 3.6 (2.9) |
| n (%) | n (%) | n (%) | |
| Youth sex, Female | 25 (73.5) | 19 (59.4) | 44 (66.7) |
| Primary parent sex, Female | 31 (91.2) | 25 (78.1) | 56 (84.8) |
| Youth Race | |||
| White/Caucasian | 26 (76.5) | 24 (75.0) | 50 (75.8) |
| Black or African American | 2 (5.9) | 3 (9.4) | 5 (7.6) |
| Asian or Asian-American | 3 (8.8) | 3 (9.4) | 6 (9.1) |
| Mixed Race | 1 (2.9) | 1 (3.1) | 2 (3.0) |
| Other Race | 2(59 | UM) | 3145] |
| Youth Ethnicity | |||
| Non-Hispanic/Latino | 30 (88.2) | 27 (84.4) | 57 (86.4) |
| Hispanic/Latino | 4 (11.8) | 5 (15.6) | 9 (13.6) |
| Youth receiving therapy outside of trial | 11 (32.4) | 12 (37.5) | 23 (34.8) |
| Youth Baseline Illness Characteristics | |||
| n (%) | n (%) | n (%) | |
| Mood and/or psychotic spectrum diagnoses | |||
| Attenuated psychosis syndrome + mood disorder | 2 (5.9) | 7 (21.9) | 9 (13.6) |
| Attenuated psychotic syndrome only | 1 (2.9) | 1 (3.1) | 2 (3.0) |
| Bipolar spectrum disorder only | 3 (8.8) | 6 (18.8) | 9 (13.6) |
| Depressive spectrum disorder only | 26 (76.5) | 15 (46.9) | 41 (62.1) |
| No DSM-5 mood disorder or attenuated psychosis syndrome | 2 (5.9) | 4 (12.5) | 6 (9.1) |
| Additional diagnoses | |||
| Attention-deficit/hyperactivity disorder | 13 (38.2) | 12 (37.5) | 25 (37.9) |
| Generalized anxiety disorder | 12 (35.3) | 15 (46.9) | 27 (40.9) |
| Social anxiety disorder | 13 (38.2) | 6 (18.8) | 19 (28.8) |
| Obsessive compulsive disorder | 1 (2.9) | 3 (9.4) | 4 (6.1) |
| Unspecified anxiety disorder | 4 (11.8) | 2 (6.3) | 6 (9.1) |
| Post-traumatic stress disorder | 1 (2.9) | 2 (6.3) | 3 (4.5) |
| Gender dysphoria | 1 (2.9) | 2 (6.3) | 3 (4.5) |
| Trichotillomania/Excoriation disorder | 2 (5.9) | 0 (0.0) | 2 (3.0) |
| Tic Disorder | 0 (0.0) | 1 (3.1) | 1 (1.5) |
| Mean (SD) | Mean (SD) | Mean (SD) | |
| Symptom Severity Rating Scales | |||
| Child Depression Rating Scale (CDRS) | 44.6 (11.7) | 47.3 (19.9) | 45.8 (16.4) |
| Young Mania Rating Scale (YMRS) | 10.1 (6.1) | 12.9 (6.4) | 11.6 (6.4) |
| Prodromal Questionnaire Brief (PQ-B) | 22.2 (20.5) | 18.2 (15.2) | 20.1 (17.9) |
Psychiatric symptoms
Across both conditions, there were improvements in depressive symptoms over the course of the study (CDRS: F(2, 75.89) = 12.56, p < 0.001, partial η2 = 0.25; DASS depression: F(2, 63.31) = 5.49, p = 0.006, partial η2 = 0.15). The mean symptom improvement on the CDRS was 9.9 points (SE = 2.1) over the study, which indicated a move from clinically significant symptoms (≥40) to subclinical symptoms. The youth also showed improvements on manic symptoms (YMRS: F(2, 69.19) = 5.90, p = 0.003, partial η2 = 0.15), anxiety (DASS: F(2, 65.28) = 6.21, p = 0.003, partial η2 = 0.16), and APS (PQ-B: F(2, 51.12) = 14.79, p < 0.001, partial η2 = 0.37). There were no differences between treatments on these psychiatric outcomes nor did childhood adversity moderate these effects.
Psychosocial functioning
Youth across both conditions showed improvements in clinician-rated social and role (academic) functioning across the 5-month period (F(2, 68.38) = 11.47, p < 0.001, partial η2 = 0.25; F(2, 68.48) = 4.25, p = 0.02, partial η2 = 0.11, respectively). There was also an interaction of treatment and assessment visit on social functioning (F(2, 68.38) = 3.25, p < 0.05, partial η2 = 0.09). Whereas youth in the two conditions had similar improvements in social functioning from pre- to post-treatment, youth in MBCT showed greater improvements from post-treatment to the 3-month post-treatment assessment compared to youth in CBT (b = 0.60, SE = 0.25, p = 0.02). This difference was magnified for youth in MBCT with greater childhood adversity who showed significantly greater improvements in their social functioning compared to youth in CBT with greater childhood adversity (F(2, 34.78) = 4.80, p = 0.01; p = 0.004; see Figure 2).
Figure 2.
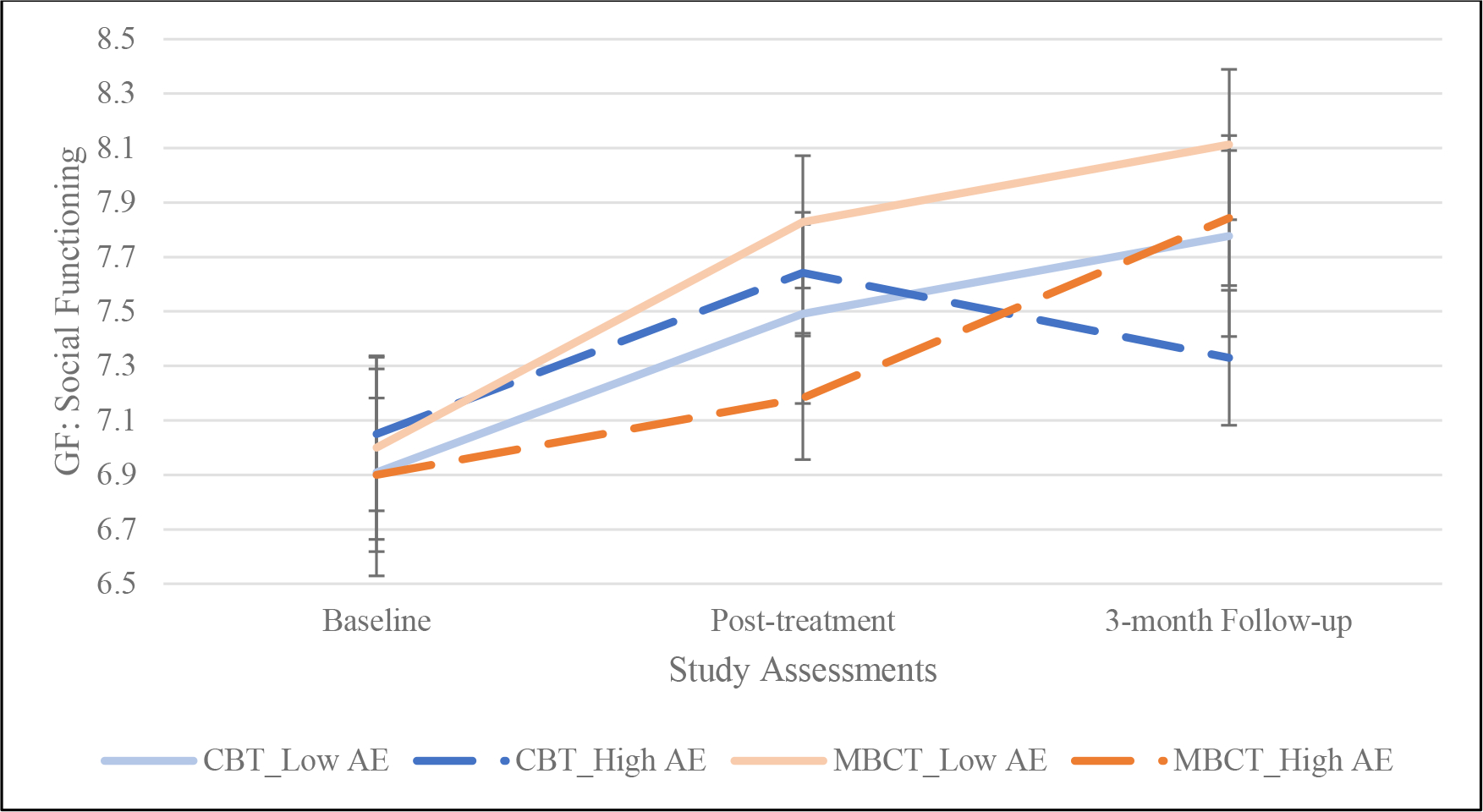
Effect of treatment conditions, moderated by childhood adverse events, on social functioning
Childhood adverse events (AE) were rated using the Philadelphia Adverse Events Scale (PHL-ACES). For ease of data visualization, a mean split was conducted on the PHL-ACES variable to identify participants with low and high childhood adversity.
There were significant improvements across both conditions in youth- and parent-reported overall KINDL global functioning scores over the 5-month study period (F(2, 56.92) = 4.59, p = 0.01, partial η2 = 0.14; F(2, 57.49) = 3.94, p = 0.03, partial η2 = 0.12, respectively). On KINDL subscales, youth and parents in both treatments reported comparable improvements in KINDL family functioning (Youth: F(2, 53.06) = 3.52, p = 0.04, partial η2 = 0.12; Parents: F(2, 57.28) = 6.21, p = 0.004, partial η2 = 0.18). Youth in both treatments reported comparable improvements in KINDL emotional functioning from pre- to post-treatment (F(2, 65.25) = 19.65, p < 0.001, partial η2 = 0.38); however, the CBT youth reporting greater improvements during the 3-month post-treatment period than their MCBT peers (F(2, 65.25) = 6.46, p = 0.003, partial η2 = 0.17; p < 0.001; Figure 3).
Figure 3.
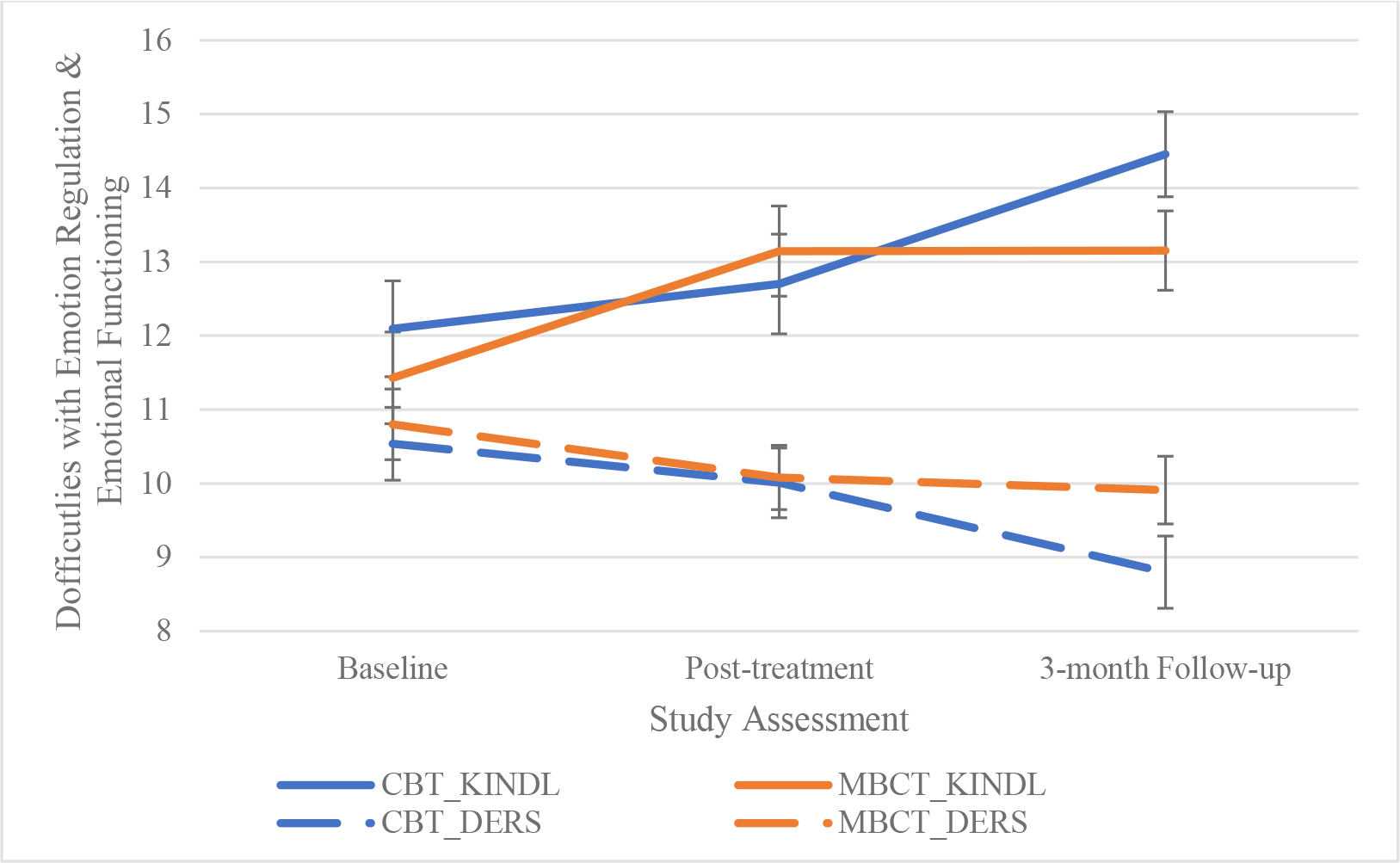
Effects of treatment condition on emotional functioning and emotion regulation
Adolescents in cognitive behavioral therapy (CBT) rated greater improvements in self-reported emotional functioning (KINDL) and emotion regulation (DERS) between the post-treatment assessment and 3-month follow-up compared to adolescents in mindfulness-based cognitive behavioral therapy (MBCT). Lower Difficulties with emotion regulation scale (DERS) indicate better emotional functioning while higher KINDL emotion functioning scores indicate better functioning. DERS scores were divided by 10 to allow for ease of graphing with the KINDL Emotion Functioning subscale.
Emotion regulation
Youth in both conditions reported fewer difficulties in emotion regulation (DERS) over the 5-month study period (F(2, 62.30) = 11.20, p < 0.001, partial η2 = 0.26), with a marginally significant treatment by assessment visit interaction (F(2, 62.30) = 2.69, p = 0.08, partial η2 = 0.08). The CBT youth showed greater improvements in emotion regulation scores between post-treatment and 3-month follow up than their MBCT peers (See Figure 4).
Figure 4.
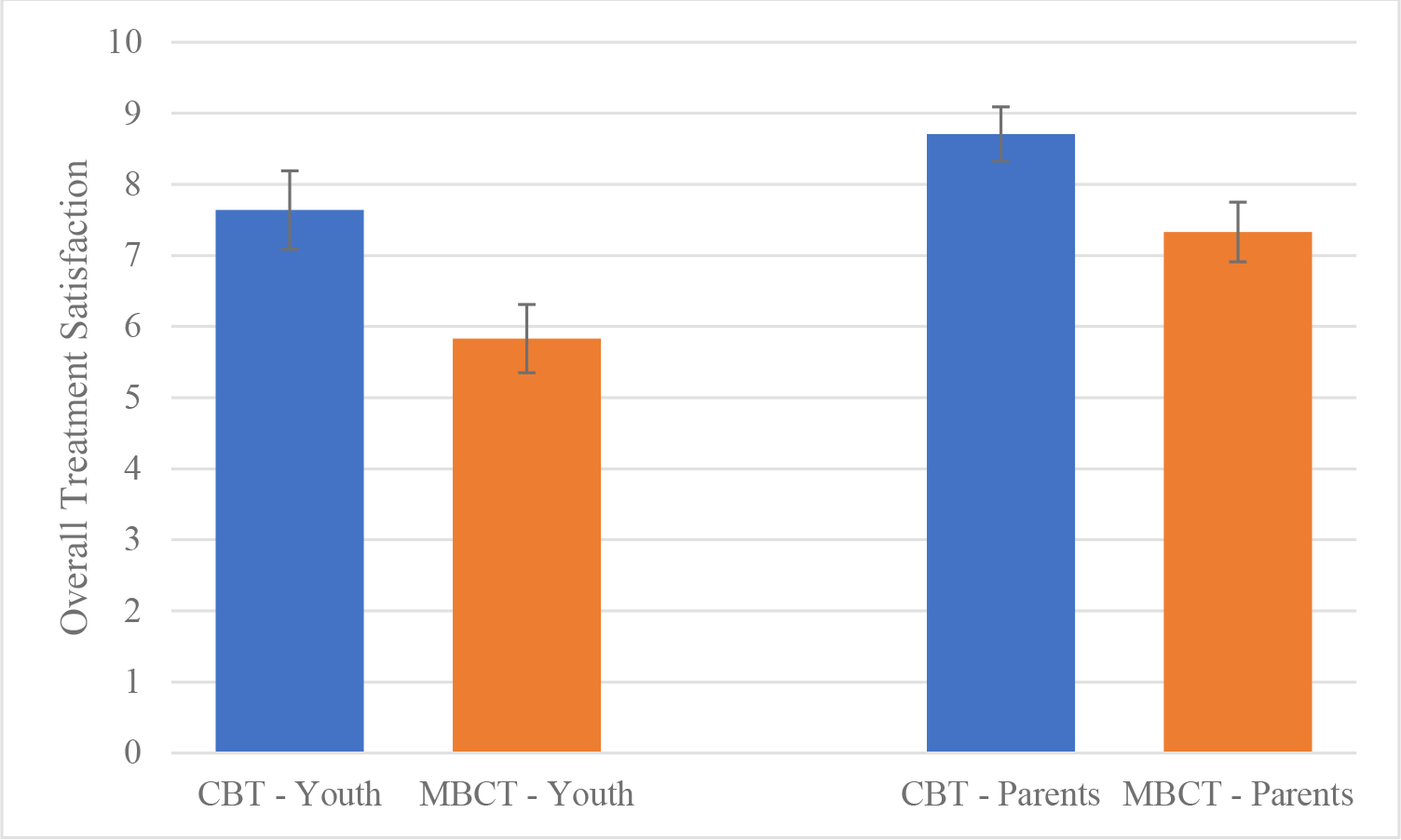
Treatment satisfaction as rated by youth and their parents
Post-treatment ratings of overall treatment satisfaction as rated by adolescents and parents who participated in cognitive behavioral therapy (CBT) and mindfulness-based cognitive behavioral therapy (MBCT) treatments, respectively.
Treatment Satisfaction
The adolescents and parents in the CBT group reported higher satisfaction scores on the single-item 10-point rating of overall satisfaction (M = 7.6, SD = 2.6, M = 8.7, SD = 1.9, respectively) as compared to the MBCT adolescents and parents (M = 5.8, SD = 2.6; M = 7.3, SD = 2.2, respectively; adolescents: F(1, 50) = 6.12, p = 0.02, partial η2 = 0.11; parents: F(1, 52) = 5.56, p = 0.02, partial η2 = 0.10). The CSQ-8 adolescents and parent satisfaction ratings were also higher for the CBT group versus MBCT group (adolescents: F(1, 50) = 11.21, p = 0.002, partial η2 = 0.18; parents: F(1, 51) = 5.47, p = 0.02, partial η2 = 0.10).
Discussion
This small-scale randomized controlled trial compared MCBT and CBT manual-based group interventions delivered via telehealth for adolescents with mood disorders and/or attenuated psychosis symptoms and their parents. Both treatments were associated with improvements in adolescents’ mood, anxiety, and attenuated psychosis symptoms, as well as psychosocial functioning over a 5-month period. These findings represented large effect sizes, which is comparable to the within-group effect size of CBT for adolescents with mood and other psychiatric disorders (Rith-Najarian et al., 2019). Findings must be considered in the context of a small sample with imbalance in youth with the APS syndrome between treatment groups. The beneficial effects of these treatments in a group telehealth format are encouraging, as these modalities can increase affordability and access to care.
MBCT (compared to CBT) was associated with greater improvements during active treatment in social functioning among adolescents with more adverse childhood experiences. This moderated effect is consistent with previous findings in adults with MDD, in which MBCT was associated with stronger effects in individuals with (as opposed to without) a history of childhood adversity (e.g., Williams et al., 2014). Certain components of MBCT, such as acceptance, self-compassion and compassion for others, and distancing from one’s emotions (e.g., watching emotions “float” by like clouds) may lead to a greater acceptance of social one’s social difficulties and/or transgressions caused by others. As a result, MBCT may be more closely associated with improvements in social functioning than CBT.
The treatment groups were associated with comparable improvements in emotion regulation from pre- to post-treatment, but only CBT was associated with continuing improvements in emotion regulation and emotional well-being during the 3-month post-treatment period. The sustained benefits of CBT on emotional regulation may translate into a greater ability to recognize early warning signs of relapse. Indeed, among adults, CBT is highly effective in preventing relapses of MDD after treatment has finished (Hollon et al., 2006).
Adolescents and their parents rated the CBT group as more satisfying and more consistent with their goals than participants in MBCT. It is possible CBT may be more consistent with traditional Western mindsets that promote one’s agency in modifying experiences or environments. In clinical settings where multiple forms of therapy are offered, obtaining patients’ preferences at the outset of treatment may predict engagement, which is known to impact degree of clinical improvement. This may be especially important for adolescents who are unmotivated for treatment.
Youths’ perceptions of family functioning and their own academic functioning improved over the 5 study months in both treatments. The skills taught in the groups (e.g., mindful acceptance, behavioral activation) may have increased teens’ engagement with school assignments, as these skills were often practiced during group discussions of school performance. The involvement of parents in both treatments may have enhanced family communication as parents and teens practiced the same skills between treatment sessions.
Although study evaluators had no investment in the outcome of this study, they were not blind to participants’ treatment conditions. This study had a small and predominantly white sample. Additionally, the sample overall had a minority of youth with the APS syndrome, with numerically more participants in CBT than in MBCT, which limits the interpretability of the treatments’ benefits for this group. The study was designed with a relatively short period of follow-up (3 months post-treatment). We are unable to draw conclusions about the endurance of treatment effects. While the 9-session treatment length was sufficient to deliver the core skills of both approaches, it is on the lower end of length for evidenced-based interventions in the literature (David-Ferdon & Kaslow, 2008). Finally, the measure of APS severity (the PQ-B) was developed as a screening tool and has only limited precedence for being used as a measure of ongoing symptom severity (Kline et al., 2016).
Future research should ascertain whether pre-treatment preferences for treatment are associated with differential treatment outcomes. Personality traits such as openness to new experiences and conscientiousness may affect treatment satisfaction as well as facilitate treatment engagement (e.g., the uptake of treatment skills). The beneficial effects of both treatments in a group telehealth format is encouraging but needs to be tested in a larger study design where format (telehealth vs. live group sessions) is randomly allocated.
Supplementary Material
Figure 1.
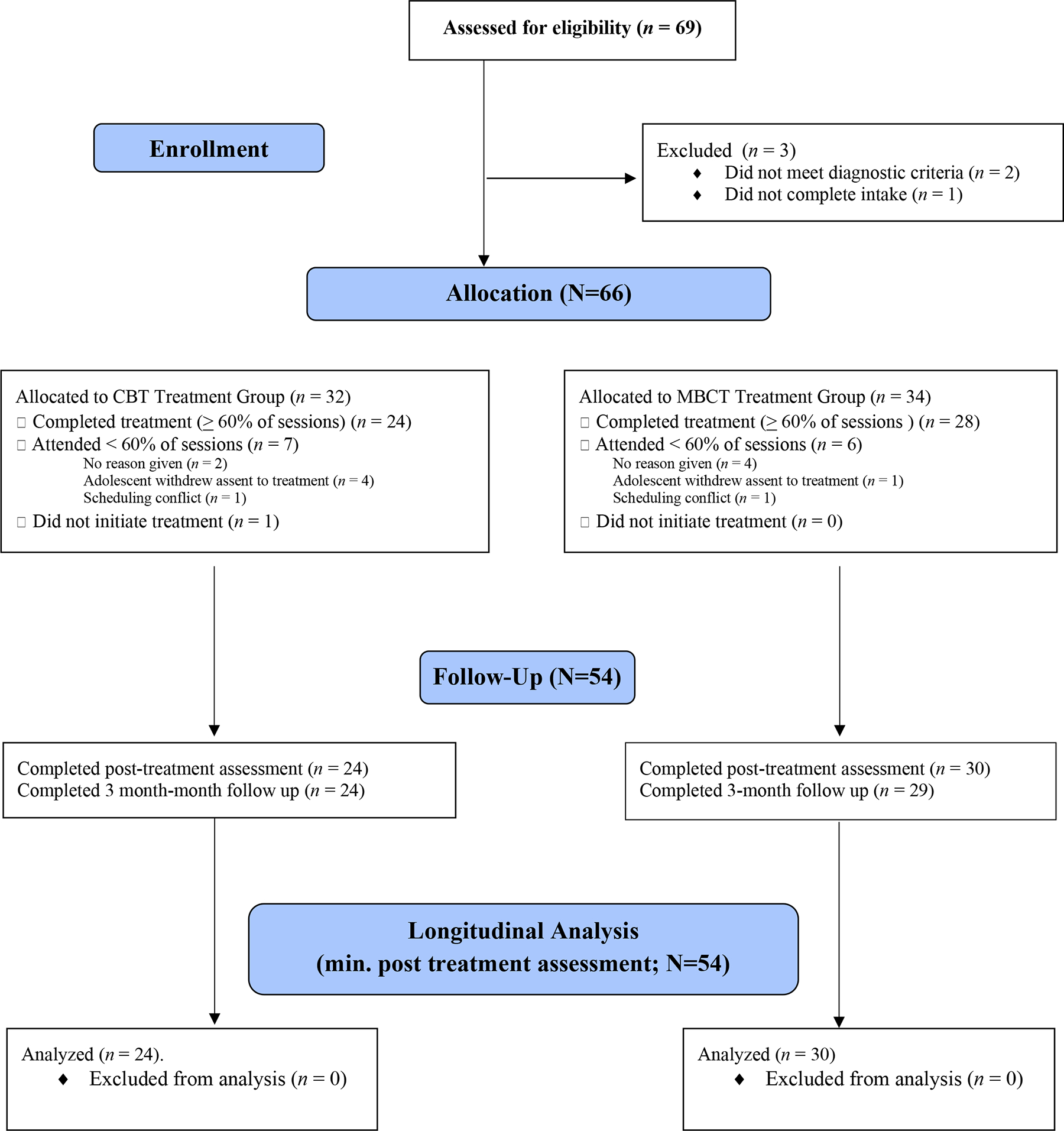
CONSORT Diagram
Public Health Significance:
This study found that remote delivery of MBCT and CBT was associated with comparable improvements in adolescents’ mood, anxiety, attenuated psychosis symptoms and psychosocial functioning over the 5-month study period. However, MBCT was associated with greater improvements than CBT in social functioning among adolescents with greater childhood adversity, while CBT was associated with greater improvements than MBCT in emotion regulation and well-being during the post-treatment period and had higher rates of treatment satisfaction. The beneficial effects of these treatments in a group telehealth format are encouraging, particularly during a period in which therapy is in high demand and community care relies extensively on remote formats.
Data Transparency:
There are no previously published or currently in press works stemming from this same data set. We collected these data to examine the comparative acceptability and efficacy of CBT and MBCT.
Acknowledgements:
We would also like to thank Linda Sepulveda, Psy.D., Ravreet Cheema, Psy.D., Alexa Connors, Psy.D., Bernalyn Ruiz, Ph.D., Roseta Patatanian, Psy.D., Hillary Shiltz, PhD, and Emily Hanna, Psy.D., for their help in facilitating the groups.
Role of funding sources: Financial support for this study was provided by National Institute of Mental Health (NIMH) grants R01MH123575, U01MH124639, R34MH117200 and K23MH124015, the Shear Family Foundation, the Levin Trust, AIM for Mental Health, and the Attias Foundation.
Footnotes
Disclosures: The authors declare no conflict of interest. Dr. Weintraub receives support from the National Institute of Mental Health (NIMH), the Shear Family Foundation, and AIM for Mental Health. Dr. Ichinose reports support from the Max Gray Fund. Dr. Bearden receives research support from the NIMH, the Foundation for the National Institutes of Health, the Shear Family Foundation, and the Don Levin Trust, and is on the scientific advisory board for Novartis neuroscience. Dr. Miklowitz receives research support from the NIMH, the Danny Alberts Foundation, Attias Family Foundation, Carl and Roberta Deutsch Foundation, Kayne Family Foundation, AIM for Mental Health, and Max Gray Fund; and book royalties from Guilford Press and John Wiley and Sons. All others authors have no declarations of interest.
The study was pre-registered on Clinicaltrials.gov (Identifier number: NCT05070052).
References
- Auther A, Smith C, & Cornblatt B (2006). Global Functioning: Social Scale (GF: Social). Glen Oaks, NY: Zucker-Hillside Hospital. [Google Scholar]
- Birmaher B, Merranko JA, Goldstein TR, Gill MK, Goldstein BI, Hower H, Yen S, Hafeman D, Strober M, & Diler RS (2018). A risk calculator to predict the individual risk of conversion from subthreshold bipolar symptoms to bipolar disorder I or II in youth. Journal of the American Academy of Child & Adolescent Psychiatry, 57(10), 755–763. e754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cronholm PF, Forke CM, Wade R, Bair-Merritt MH, Davis M, Harkins-Schwarz M, Pachter LM, & Fein JA (2015). Adverse childhood experiences: Expanding the concept of adversity. American journal of preventive medicine, 49(3), 354–361. [DOI] [PubMed] [Google Scholar]
- David-Ferdon C, & Kaslow NJ (2008). Evidence-based psychosocial treatments for child and adolescent depression. Journal of Clinical Child & Adolescent Psychology, 37(1), 62–104. [DOI] [PubMed] [Google Scholar]
- Gratz KL, & Roemer L (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment, 26(1), 41–54. [Google Scholar]
- Henry JD, & Crawford JR (2005). The short-form version of the Depression Anxiety Stress Scales (DASS-21): Construct validity and normative data in a large non-clinical sample. British Journal of Clinical Psychology, 44(2), 227–239. [DOI] [PubMed] [Google Scholar]
- Hollon SD, Stewart MO, & Strunk D (2006). Enduring effects for cognitive behavior therapy in the treatment of depression and anxiety. Annual review of psychology. [DOI] [PubMed] [Google Scholar]
- Hutton P, & Taylor PJ (2014). Cognitive behavioural therapy for psychosis prevention: a systematic review and meta-analysis. Psychological medicine, 44(3), 449–468. [DOI] [PubMed] [Google Scholar]
- Kline E, Thompson E, Demro C, Bussell K, Reeves G, & Schiffman J (2016). Self-report instruments for clinical monitoring of psychosis risk states. Psychiatric Services, 67(4), 456–459. [DOI] [PubMed] [Google Scholar]
- Larsen DL, Attkisson CC, Hargreaves WA, & Nguyen TD (1979). Client satisfaction questionnaire. Evaluation and Program Planning. [DOI] [PubMed] [Google Scholar]
- LeMoult J, Humphreys KL, Tracy A, Hoffmeister J-A, Ip E, & Gotlib IH (2020). Meta-analysis: exposure to early life stress and risk for depression in childhood and adolescence. Journal of the American Academy of Child & Adolescent Psychiatry, 59(7), 842–855. [DOI] [PubMed] [Google Scholar]
- Loewy RL, Corey S, Amirfathi F, Dabit S, Fulford D, Pearson R, Hua JP, Schlosser D, Stuart BK, & Mathalon DH (2019). Childhood trauma and clinical high risk for psychosis. Schizophrenia research, 205, 10–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loewy RL, Pearson R, Vinogradov S, Bearden CE, & Cannon TD (2011). Psychosis risk screening with the Prodromal Questionnaire—brief version (PQ-B). Schizophrenia research, 129(1), 42–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGorry PD, Hartmann JA, Spooner R, & Nelson B (2018). Beyond the “at risk mental state” concept: transitioning to transdiagnostic psychiatry. World Psychiatry, 17(2), 133–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller TJ, McGlashan TH, Rosen JL, Cadenhead K, Ventura J, McFarlane W, Perkins DO, Pearlson GD, & Woods SW (2003). Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: predictive validity, interrater reliability, and training to reliability. Schizophrenia bulletin, 29(4), 703. [DOI] [PubMed] [Google Scholar]
- Niendam T, Bearden C, Johnson J, & Cannon T (2006). Global Functioning: Role Scale (GF: Role). Los Angeles, CA: University of California, Los Angeles. [Google Scholar]
- Oud M, De Winter L, Vermeulen-Smit E, Bodden D, Nauta M, Stone L, Van Den Heuvel M, Al Taher R, De Graaf I, & Kendall T (2019). Effectiveness of CBT for children and adolescents with depression: A systematic review and meta-regression analysis. European psychiatry, 57, 33–45. [DOI] [PubMed] [Google Scholar]
- Poznanski EO, & Mokros HB (1996). Children’s depression rating scale, revised (CDRS-R). Western Psychological Services Los Angeles. [Google Scholar]
- Ravens-Sieberer U, & Bullinger M (2000). KINDL-R. Questionnaire for measuring health-related quality of life in children and adolescents, revised version. Manual. Recuperado de https://www.kindl.org/english/manual/[Links].
- Reangsing C, Punsuwun S, & Schneider JK (2021). Effects of mindfulness interventions on depressive symptoms in adolescents: A meta-analysis. International journal of nursing studies, 115, 103848. [DOI] [PubMed] [Google Scholar]
- Rith-Najarian LR, Mesri B, Park AL, Sun M, Chavira DA, & Chorpita BF (2019). Durability of cognitive behavioral therapy effects for youth and adolescents with anxiety, depression, or traumatic stress: A meta-analysis on long-term follow-ups. Behavior Therapy, 50(1), 225–240. [DOI] [PubMed] [Google Scholar]
- Savill M, D’Ambrosio J, Cannon TD, & Loewy RL (2018). Psychosis risk screening in different populations using the Prodromal Questionnaire: a systematic review. Early intervention in psychiatry, 12(1), 3–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan DV, Sheehan KH, Shytle RD, Janavs J, Bannon Y, Rogers JE, Milo KM, Stock SL, & Wilkinson B (2010). Reliability and validity of the mini international neuropsychiatric interview for children and adolescents (MINI-KID). The Journal of clinical psychiatry, 71(3), 0–0. [DOI] [PubMed] [Google Scholar]
- Vignaud P, Reilly KT, Donde C, Haesebaert F, & Brunelin J (2019). Clinical effects of mindfulness-based intervention in patients with first episode psychosis and in individuals with ultra-high risk for transition to psychosis: a review. Frontiers in psychiatry, 10, 797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weintraub MJ, Zinberg JL, Bearden CE, & Miklowitz DJ (2020). Applying a transdiagnostic unified treatment to adolescents at high risk for serious mental illness: Rationale and preliminary findings. Cognitive and Behavioral Practice, 27(2), 202–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams JMG, Crane C, Barnhofer T, Brennan K, Duggan DS, Fennell MJ, Hackmann A, Krusche A, Muse K, & Von Rohr IR (2014). Mindfulness-based cognitive therapy for preventing relapse in recurrent depression: a randomized dismantling trial. Journal of Consulting and Clinical Psychology, 82(2), 275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young R, Biggs J, Ziegler V, & Meyer D (1978). A rating scale for mania: reliability, validity and sensitivity. The British Journal of Psychiatry, 133(5), 429–435. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


