Abstract
BACKGROUND:
Older adults with limited mobility are at an increased risk of adverse health outcomes, an outcome inadequately investigated in older Mexican Americans. We explored whether pre-admission life-space mobility predicts post-hospitalization outcomes among hospitalized Mexican American Medicare beneficiaries.
METHODS:
Life-space mobility, using the Life-Space Assessment (LSA), was analyzed using quartiles and 5-point intervals. Using the Hispanic Established Populations for the Epidemiologic Study of the Elderly (HEPESE) Waves 7 and 8 data linked to Medicare claims data, 426 older Mexican Americans with at least two months of Medicare coverage and who were hospitalized within two years of completing the LSA were included. Logistic and Cox Proportional regression analyses estimated the association of pre-admission LSA with post-hospitalization outcomes.
RESULTS:
Prior to hospitalization, 85.4% reported limited life-space mobility. Most patients (n=322, 75.6%) were hospitalized for medical reasons. About 65% were discharged to the community. Pre-admission LSA scores were not associated with community discharge (Odds Ratio [OR]=1.02, 0.95-1.10). Higher pre-admission LSA scores were associated with 30-day readmission (OR=1.11, 1.01-1.22). Patients in the highest pre-admission LSA quartile (i.e., greatest life-space mobility) were less likely to die within two years after hospital discharge (OR=0.61, 0.39-0.97) compared to those with lower pre-admission LSA scores.
CONCLUSIONS:
Among older Mexican American Medicare beneficiaries, greater pre-admission LSA scores were associated with increased risk of 30-day readmission and decreased risk of mortality within two years following hospitalization. Future work should further investigate the relationship of LSA and post-hospitalization outcomes in a larger sample of Mexican American older adults.
Keywords: Medicare, Mexican Americans, mobility, mortality risk, patient readmission
INTRODUCTION
Hispanic individuals are the largest US ethnic minority group, with Mexican American adults accounting for 62% of the Hispanic population in 2017.1 Older Hispanics are living longer with disability and comorbid conditions.2 The Hispanic Paradox or Immigrant Health Paradox suggests that, despite disparities in income, education, and access to care, Hispanic mortality is comparable to that of Non-Hispanic White (NHW) older adults.3
Life-space mobility measures how older adults move through their community, accounting for the level of assistance needed.4 Biological, cultural, cognitive, physical, environmental, and psychosocial factors are key determinants of mobility in older adults.5 Decreased levels of life-space mobility are associated with poorer physical/mental health, lower physical functioning,4,6 cognitive decline,7,8 greater depressive symptoms,4 frailty,9 and the risk of hospital and nursing home admission9–11 and of mortality.9,12 Among a population-based cohort of community-dwelling older adults with heart failure, a decrease in life-space mobility was associated with a 14% increase in emergency department use or hospitalization.13 The assessment of life-space mobility among older adults may help identify those at risk of adverse outcomes, but most studies have included only Black and NHW cohorts.14–17
Limited studies have assessed life-space mobility among Hispanic older adults.18–22 Decreased life-space mobility was associated with lower educational and income levels, greater depression, and decreased cognitive function among older Latin American adults.18 In a sample of older adults in Mexico, depression indirectly and directly mediated the relationship of chronic diseases and comorbidities with perceived health and life-space mobility.20 In a study using data from the Hispanic Established Population for the Epidemiologic Study of the Elderly survey (HEPESE), nearly 80% of the sample of Mexican American older adults reported restricted life-space, which was related to older age, female sex, stroke, high depressive symptoms, obesity, and disability in Activities of Daily Living (ADL).22 Greater life-space mobility was also a significant predictor of a slower rate of cognitive decline over 5 years in the HEPESE sample.21 In the US, an array of factors can influence mobility limitations among community-dwelling Hispanic older adults.23
In the aging literature, life-space mobility is known to decline following hospitalization10,24,25 and is associated with both increased readmission within 90 days26 and mortality;27 however, we do not know whether life-space mobility is associated with post-hospitalization outcomes among Mexican American older adults. Therefore, we aimed to explore the relationship between pre-admission life-space mobility, using the Life-Space Assessment (LSA), and community discharge, 30-day all-cause readmission, and all-cause mortality after hospitalization. We hypothesized that lower pre-admission LSA scores are associated with an increased likelihood of non-community discharge, hospital readmission, and mortality following acute hospital discharge among a cohort of community-dwelling Mexican American older adults.
METHODS
Study Design
This is a retrospective cohort study using survey data from Waves 7 (2010-11) and 8 (2012-13) of the HEPESE study. The HEPESE is an ongoing longitudinal study of community-dwelling Mexican American older adults aged ≥65 years, first interviewed in 1993/94.28 The study cohort includes English- and Spanish-speaking Mexican American older adults residing in Arizona, California, Colorado, New Mexico, and Texas. Information and data for the HEPESE are available at the National Archive of Computerized Data on Aging.29 Waves 7 and 8 included survey data from 1,078 and 743 participants or their proxies/informants, respectively. Survey data were linked with Medicare Beneficiary claims data (Part A) to identify the study cohort and determine their hospital-related outcomes. The University of Texas Medical Branch at Galveston (UTMB) Institutional Review Board approved the study.
Sample Cohort Selection
Included individuals completed Waves 7 or 8 surveys (n = 1,119), which were linked with the Medicare Beneficiary Summary File (MBSF) and the Medicare Provider Analysis and Review (MedPAR) files.30 The Centers for Medicare and Medicaid Services (CMS) used the HEPESE personal identifiers along with a Medicare beneficiary ID number to successfully match participants (n = 767, 68.5%) to the Medicare data files. Of these, 558 were hospitalized within two years of survey completion. Subjects without Medicare Advantage (MA) coverage were required to be enrolled continuously in Part A for at least two months after the index hospitalization. Beneficiaries enrolled in MA were excluded because they may have information-only claims submitted and incomplete data. Using the MedPAR, we identified acute hospitalizations. Two months of coverage (the month of discharge and the following month) was required to assess 30-day readmissions. We used the first hospitalization within two years after the HEPESE interview as the index stay. If the participant completed both Wave 7 and Wave 8 surveys and had several hospitalizations, the most recent LSA score was selected. The final sample included 426 HEPESE participants. Figure 1 depicts the cohort selection.
Figure 1.
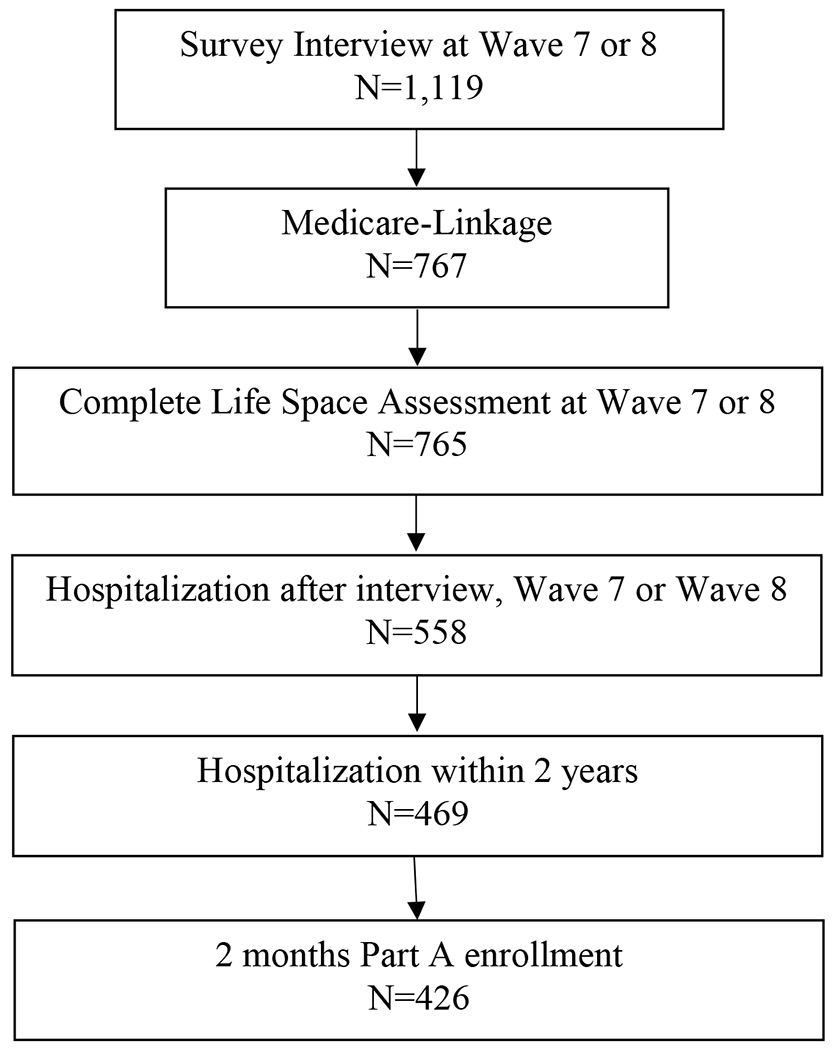
Flowchart of Cohort Selection
Measures
Reasons for hospitalization.
The Medicare Severity-Diagnosis Related Groups (MS-DRG) were recorded in the MedPAR file for each hospital stay. MS-DRG was mapped to Major Diagnostic Category (MDC) according to the CMS-released DRG table. The DRG table was downloaded from the website: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Acute-Inpatient-Files-for-Download. One of 25 MDCs was used to identify each hospitalization. Within each MDC, MS-DRGs were defined by the principal diagnosis, secondary diagnoses, procedures, sex, and discharge status. Using the MDCs, we were able to determine the reasons for medical (e.g., chest pain, stroke) or surgical (e.g., pacemaker or stent placement) hospitalizations.
Post-hospitalization outcomes.
Using the patient discharge status codes, we identified the discharge destination for each subject. A dichotomized variable was created to distinguish patients discharged to the community (e.g., home with/without services) from those transferred to another hospital/facility (e.g., inpatient rehabilitation, nursing home, other facility). Readmission was defined as an all-cause acute hospital admission within 30 days from the acute hospital discharge. Survival status was determined by cross-verifying the date of death from the National Death Index and Medicare data. The follow-up of survival status was followed from hospital discharge to December 31, 2016, and the follow-up period was up to 6.5 years (from 2010 to 2016). Date of death is included in the MBSF Base segment.
Life-space mobility.
Life-space mobility was assessed using the University of Alabama at Birmingham (UAB) LSA.4,31 The LSA measures community mobility in older adults during the prior four weeks. The composite measure accounts for specific locations where an individual goes (e.g., beyond bedroom, outside of home or town), how often (e.g., less than once per week, daily), and whether assistance from an assistive device or person is needed. Sub-scores are calculated for each of the five life-space levels (bedroom, home, neighborhood, town, beyond town) by multiplying the life-space level by frequency and level of independence. The level sub-scores are summed to obtain the composite score, which ranges from 0 to 120, where higher scores indicate greater life-space mobility. LSA mobility was analyzed as an ordinal variable with 5-point intervals and as quartiles: quartile 1 (0–15, n = 105), quartile 2 (16–28, n = 110), quartile 3 (28.5–44, n = 104), and quartile 4 (45–92, n = 107). The experiences of individuals from two different quartiles can be quite different. For example, a subject who can move freely around their home without assistance and go outside on their porch a few times a week with a cane, but not go to places in their neighborhood, would have a score of 12 (quartile 1). A subject with a score of 92 (quartile 4) is able to freely move around their home without assistance but needs a cane when leaving their home and can travel daily beyond their home, neighborhood, within their town, and outside of their town. For each subject, we selected the pre-hospitalization LSA score closest to the first hospitalization within two years after the interview. If participants completed a LSA score for both Waves 7 and 8, then the closest LSA score prior to the index hospitalization was chosen.
Covariates.
Demographic variables (i.e., age, sex, nativity, marital status, and years of education), self-reported comorbid conditions (i.e., diabetes, hypertension, acute myocardial infarction, and stroke), and hospitalization type (i.e., medical, surgical) and length of stay (days from discharge date to admission date) were included. Disability was determined using the Katz ADL scale,32 which was dichotomized to differentiate participants who required no assistance from those who needed assistance or were unable to perform one or more ADLs. Cognitive status was based on the Mini-Mental State Examination (MMSE) scores,33 where scores ≤ 21 indicated cognitive impairment.34 Lastly, high depressive symptoms was determined using the 20-item Center for Epidemiologic Studies Depression Scale (CES-D ≥ 16).35
Statistical Analyses
Descriptive statistics were used to summarize participant characteristics by baseline LSA quartiles. Logistic regression models were used to estimate the odds ratio (OR) and 95% confidence interval of discharge to the community and 30-day all-cause hospital readmission after hospital discharge as a function of LSA scores, after controlling for all covariates. Cox proportional regression analysis was used to estimate the hazard of death at 2 years of follow up as a function of LSA, after controlling for all covariates. The Cox proportional hazard regression assumption was confirmed. Survival curves were estimated according to the Kaplan Meier method and quartiles of LSA scores were compared using the log-rank test. All analyses were performed using the SAS System for Windows, version 9.4 (SAS Institute, Inc., Cary, NC).
RESULTS
Sample Characteristics
Mexican American older adults (n=426) were hospitalized within two years of completing their Wave 7 (2010 to 2011) or 8 (2012 to 2013) HEPESE interview. The study cohort includes English- (17%) and Spanish-speaking (83%) Mexican American older adults who resided in Arizona (4%), California (26%), Colorado (1%), New Mexico (3%), and Texas (66%).Table 1 presents the descriptive characteristics of the sample by pre-hospitalization LSA score in quartiles. Mexican American older adults with the greatest life-space mobility before hospitalization were younger on average, and those quartiles with the most limited life-space mobility had a greater proportion of females and those with stroke, high depressive symptoms, cognitive impairment, and ADL disability. Most were hospitalized for medical reasons (n=322, 75.6%), while the remainder were hospitalized for surgical reasons. Figure 2 shows the distribution of reasons for medical and surgical hospitalizations. The two most common types of medical hospitalizations were for circulatory or respiratory illness. Reasons for surgical hospitalization included joint replacement, pacemaker or stent placement, bowel procedures, and laparoscopic cholecystectomy.
Table 1.
Participant Pre- and Post-Hospital Characteristics by Life-Space Assessment (LSA) Quartiles
| Variables | All (N=426) | Quartile 1 (N=105) | Quartile 2 (N=110) | Quartile 3 (N=104) | Quartile 4 (N=107) | p-value |
|---|---|---|---|---|---|---|
| LSA-continuous score, mean ± SD | 31.40 ± 20.78 | 7.38 ± 4.81 | 21.67 ± 3.72 | 36.08 ± 4.71 | 60.44 ± 11.31 | <0.001* |
| LSA-continuous score, min-max | 0-92 | 0-15 | 16-28 | 28.5-44 | 45-92 | |
| Age, mean ± SD | 87.09 ± 3.96 | 87.64 ± 4.38 | 87.65 ± 3.93 | 87.38 ± 3.85 | 85.70 ± 3.32 | <0.001* |
| Sex (female) | 263 (61.7) | 79 (75.2) | 76 (69.1) | 64 (61.5) | 44 (41.1) | <0.001* |
| Interview at wave 7 | 250 (58.7) | 56 (53.3) | 67 (60.9) | 64 (61.5) | 63 (58.9) | 0.612 |
| US Born | 234 (54.9) | 59 (56.2) | 61 (55.5) | 61 (58.7) | 53 (49.5) | 0.589 |
| Married | 128 (30.0) | 32 (30.5) | 28 (25.5) | 27 (26.0) | 41 (38.3) | 0.143 |
| Diabetes | 161 (37.8) | 45 (42.9) | 38 (34.5) | 36 (34.6) | 42 (39.3) | 0.535 |
| Hypertension | 312 (73.2) | 79 (75.2) | 80 (72.7) | 82 (78.8) | 71 (66.4) | 0.214 |
| Acute Myocardial Infarction | 42 (9.9) | 12 (11.4) | N<11 | N<11 | 12 (11.2) | 0.718 |
| Stroke | 52 (12.2) | 21 (20.0) | 11 (10.0) | N<11 | N<11 | 0.048* |
| Depressive symptoms (CES-D ≥ 16)† | 113 (29.2) | 41 (50.6) | 36 (35.6) | 28 (28.0) | N<11 | <0.001* |
| Cognitive Impairment (MMSE<21)† | 191 (48.8) | 57 (71.3) | 58 (55.2) | 47 (46.5) | 29 (27.6) | <0.001* |
| ADL disability | 277 (65.0) | 96 (91.4) | 86 (78.2) | 66 (63.5) | 29 (27.1) | <0.001* |
| Length of stay, mean ± SD | 4.95 ± 3.94 | 5.24 ± 3.56 | 5.05 ± 3.83 | 5.48 ± 4.98 | 4.04 ± 3.09 | 0.041* |
| Community discharge | 275 (64.6) | 63 (60.0) | 64 (58.2) | 71 (68.3) | 77 (72.0) | 0.107 |
| 30-Day Readmission | 54 (12.7) | 12 (11.4) | 16 (14.5) | 10 (9.6) | 16 (15.0) | 0.599 |
| 2-year Mortality | 113 (26.5) | 40 (38.1) | 27 (24.5) | 27 (26.0) | 19 (17.8) | 0.009* |
Note: CES-D= Center for Epidemiologic Studies Depression Scale, MMSE= Mini Mental State Examination, ADL= Activities of Daily Living.
P<0.05 for group comparison.
There was missing data for CES-D or MMSE.
Figure 2.
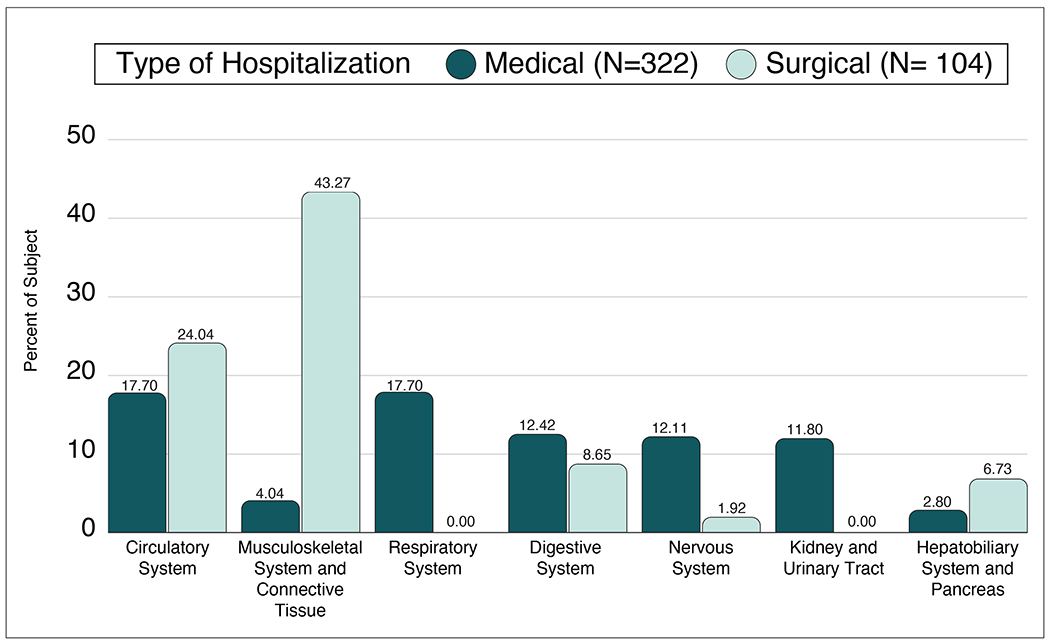
Percent Distribution of Reasons for Hospitalization
For the multivariable models, we excluded 41 individuals who had missing MMSE and CES-D scores. The final sample included 385 Mexican American older adults with Medicare Fee-for-Service who were hospitalized.
Life-space Mobility and Community Discharge
We used the full model to determine if pre-hospital LSA, as an ordinal variable with 5-point intervals, had a significant association with community discharge (Table 2). LSA was not a significant predictor of community discharge. Stroke history, length of stay, and medical hospitalization were significant predictors of community discharge. Having a history of stroke was associated with a 56% decrease in the odds of community discharge (OR: 0.44; 95% Confidence Interval [CI]: 0.20-0.96). For each day increase in stay, there was a 20% decrease in the odds of being discharged to the community (OR: 0.80; 95% CI: 0.74-0.86). Medical hospitalization, compared to surgical hospitalization, was associated with a 69% increase in community discharge (OR: 1.69; 95% CI: 1.01-2.86).
Table 2.
Effect of Life-Space Assessment (LSA) by 5-point Intervals on Community Discharge, Readmission, and Mortality (N=385)
| Variables | Discharge to community | 30-day readmission | Mortality§ |
|---|---|---|---|
| OR (95% CI) | OR (95% CI) | HR (95% CI) | |
| LSA 5-point intervals | 1.02 (0.95- 1.10) | 1.11 (1.01- 1.22)* | 0.97 (0.93- 1.01) |
| Age (years) | 0.99 (0.93- 1.05) | 0.92 (0.84- 1.02) | 1.06 (1.03- 1.11)* |
| Sex (female) | 1.21 (0.69- 2.12) | 1.42 (0.66- 3.06) | 0.86 (0.63- 1.18) |
| US Born | 1.04 (0.65- 1.68) | 1.15 (0.60- 2.23) | 1.04 (0.80- 1.37) |
| Married | 1.20 (0.67- 2.15) | 0.80 (0.36- 1.77) | 1.06 (0.77- 1.46) |
| Diabetes | 1.17 (0.71- 1.93) | 1.39 (0.71- 2.72) | 1.23 (0.92- 1.65) |
| Hypertension | 1.32 (0.77- 2.27) | 1.36 (0.60- 3.07) | 0.71 (0.52- 0.96)* |
| Acute Myocardial Infarction | 0.60 (0.27- 1.35) | 0.97 (0.32- 3.00) | 1.04 (0.64- 1.69) |
| Stroke | 0.44 (0.20- 0.96)* | 1.19 (0.45- 3.18) | 1.21 (0.77- 1.90) |
| Depressive symptoms (CES-D ≥ 16) | 0.66 (0.38- 1.14) | 0.77 (0.35- 1.71) | 1.20 (0.89- 1.62) |
| Cognitive Impairment (MMSE <21) | 1.37 (0.81- 2.32) | 1.06 (0.52- 2.16) | 0.93 (0.69- 1.25) |
| Any ADL limitations | 1.04 (0.60- 1.81) | 2.15 (0.96- 4.85) | 1.32 (0.95- 1.83) |
| Length of stay (days) | 0.81 (0.75- 0.87)* | 1.07 (0.99- 1.16) | 1.08 (1.04- 1.12)** |
| Hospitalization type (medical) | 1.69 (1.01 – 2.86)* | 1.36 (0.617-3.00) | 1.43 (1.03-2.01) ** |
| 30-day readmission | NA | NA | 2.57 (1.79- 3.70)** |
Note. OR= Odds Ratio, CI= confident interval, HR= Hazard Ratio, LSA= Life-space Assessment, ADL= Activities of Daily Living, CES-D= Center for Epidemiologic Studies Depression Scale, MMSE= Mini Mental State Examination, NA= not available.
P<0.05;
P<.001
Mortality was observed from hospital discharge to end of study (December 31st, 2016).
Life-space Mobility and 30-day Readmission
We applied the full model to determine if pre-hospital life-space mobility had a significant association with 30-day readmission using the LSA score in 5-point intervals (Table 2). Interestingly, greater LSA scores were associated with increased odds of being readmitted within 30 days from discharge, after accounting for length of stay, demographics, comorbidities, cognition, depression, disability, and hospitalization type.
Life-space Mobility and Mortality
Pre-admission LSA scores by 5-point intervals had no significant effect on mortality following hospitalization (Table 2, Hazard Ratio [HR]: 0.97; 95% CI: 0.93–1.01). Older age, history of hypertension, increased length of stay, medical hospitalization, and 30-day readmission were factors associated with increased 2-year mortality. Participants with hypertension had a decreased risk of death (HR: 0.71; 95% CI: 0.52-0.96). When we estimated mortality using LSA in quartiles, Mexican American older adults who were in the fourth quartile (i.e., greatest life-space mobility) were most likely to survive following discharge from the hospital (HR: 0.61; 95% CI: 0.39-0.97) compared to those in the first quartile. Figure 3 shows the Kaplan–Meier survival curve for each LSA quartile.
Figure 3. Kaplan-Meier Estimates for Survival Probability Stratified by Life-Space Assessment (LSA) Quartiles.
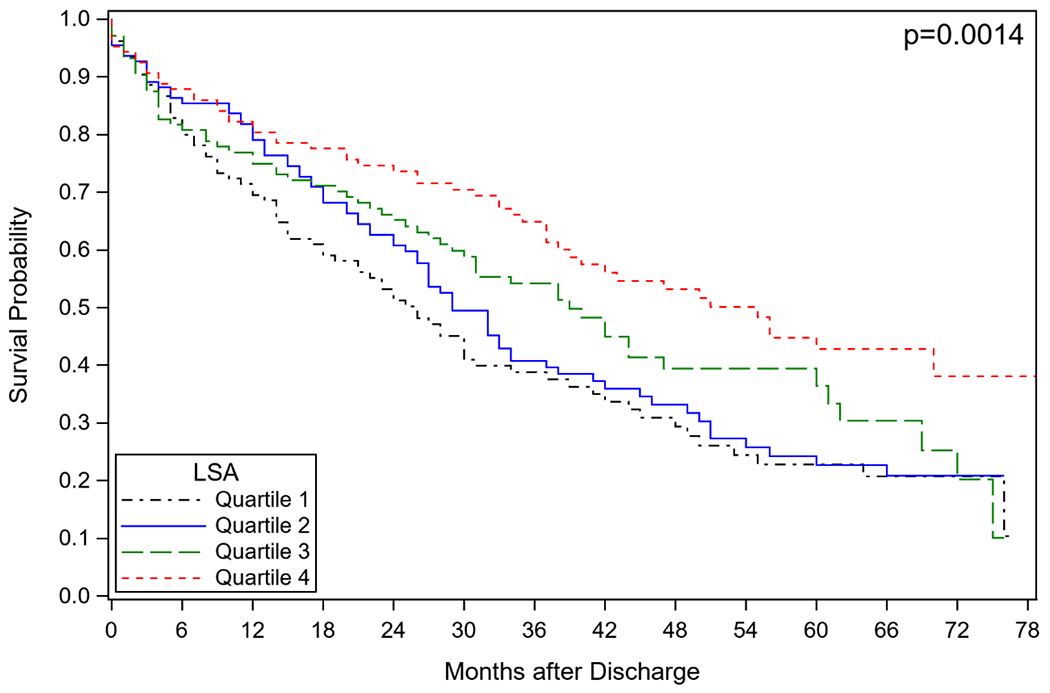
Note. LSA scores by quartiles: Quartile 1 (0–15), quartile 2 (16–28), quartile 3 (28.5–44), and quartile 4 (45–92); Greater LSA scores indicate greater life-space mobility.
DISCUSSION
This study aimed to explore the relationship between pre-admission life-space mobility using the LSA and post-hospital outcomes (i.e., community discharge, 30-day readmission, and mortality). Pre-admission LSA scores were not associated with being discharged to the community following hospitalization. However, among HEPESE participants, having a history of stroke and each additional day spent in the hospital were associated with a decreased likelihood of being discharged to the community. Hospitalization for medical reasons compared to surgical reasons was associated with an increased likelihood of community discharge. Interestingly, greater pre-admission LSA scores, as measured in 5-point intervals, were associated with an increased odds of 30-day readmission. In contrast, being in the highest pre-admission LSA quartile was associated with a decreased likelihood of mortality within two years following hospital discharge, but this association was non-significant when measured using the LSA score by 5-point intervals. As expected, older age, spending more days in the hospital, hospitalization for medical reasons, and being re-admitted within 30 days increased the participants’ odds of mortality.
Prior to hospitalization, Mexican American older adults reported significant comorbidities, such as stroke, depressive symptoms, ADL disability, and restricted life-space mobility. Of those who were hospitalized, most were hospitalized due to respiratory and circulatory medical reasons and musculoskeletal surgical reasons. Older age, female sex, stroke, high depressive symptoms, cognitive impairment, and ADL disability were associated with having the most limited life-space mobility among hospitalized Mexican American older adults. Previous studies have found similar results among community-dwelling and clinical patient populations.36
We did not find a significant relationship between pre-admission LSA and community discharge. However, its relationship was in the expected direction: those less limited in their life-space mobility were more likely to return to the community. Limited mobility could be the result of a number of health conditions and physical limitations that would place individuals at increased risk for continued care following acute hospitalization. We did find that each one-day increase in a patient’s hospital length of stay decreased the odds of community discharge by 20%, whereas stroke history was associated with a nearly 60% decrease in odds. These findings were not surprising, as length of stay is a critical factor during acute hospital discharge planning, because functional status and illness complexity can inform discharge destination choices. In addition, it is common for patients to be discharged to a post-acute setting following a stroke.37 In a previous study of Medicare beneficiaries, longer length of acute hospital stay was significantly associated with decreased odds of successful community discharge,38 results similar to those for patients hospitalized in a skilled nursing facility.39 Length of stay may also be associated with nursing home placement, because patients may have to wait an extra day or two to get nursing home clearance and a bed.
When LSA was measured by 5-point intervals, greater pre-admission life-space mobility was associated with an increased odds for readmission. These results differ from those of previous studies. In a sample of older adults with heart failure, a 10-point decrease in LSA was associated with an increased risk of an emergency room visit or admission within 6 months.13 Another study found that pre-hospital restricted life-space mobility was associated with increased odds of 90-day readmission following hospitalization for chronic obstructive pulmonary disease or congestive heart failure.26 More recently, in a study including only non-Hispanic Black and NHW older adults, a decrease in LSA was associated with increased health care utilization (i.e., emergency department visit or hospitalization) as early as one month following assessment.17 It is unclear why individuals with greater mobility were more likely to be readmitted after hospitalization. It is possible that they experienced a significant change in their health status that placed them at greater risk for readmission, while those with less mobility prior to hospitalization were at greater risk of mortality following hospitalization. The positive relationship between LSA and readmission needs to be further investigated in a larger sample to determine if indeed this relationship maintains.
We found that Mexican American older adults in the greatest life-space mobility category compared to other categories were more likely to be alive at two years following hospital discharge. In a previous study of 1,445 community-dwelling older adults without dementia, a restricted life-space mobility was associated with an increase in odds for death over an 8-year period.12 Based on data from 1,000 Medicare beneficiaries in the UAB Study of Aging, a 10-point decrease in LSA over a 6-month period was associated with a 72% increased odds of not surviving the following 6 months.27 In a sample of men aged 71-92 years, only a LSA score < 20 was significantly associated with an increased risk of death.40 Another study found that older women with LSA scores < 60 were at an increased risk of death compared to women with LSA scores 81-120, with those scoring 0-20 having the greatest risk of death.41 One study found that leaving the house daily is associated with a reduced risk of mortality in older adults.42 Therefore, our findings suggest that even pre-hospital life-space mobility may be an indicator of mortality within two years following an illness or surgery resulting in hospitalization. All the factors associated with poor health status — such as longer length of stay, medical hospitalization (versus surgical), and 30-day readmission — are significant factors increasing mortality risk. This finding suggests the importance of clinically monitoring patient mobility to identify when individuals may be at risk of death.
Among our sample, in which nearly 75% reported hypertension, hypertension was associated with a decreased risk of mortality within two years of hospital discharge. Possible reasons for the decreased mortality risk could be aggressive blood pressure management and other complex comorbidities among a population of older adults whose mean age is 85 years. A recent study found that older adults aged 85 and older with hypertension and moderate-to-severe frailty were at lower risk of mortality.43 More work is needed to explore blood pressure management and associated outcomes among Mexican American older adults.
In summary, pre-admission LSA was not a reliable indicator of potential for post-hospitalization community discharge nor could it identify individuals at an increased risk of 30-day readmission. However, it may be useful in identifying those at lower risk of mortality after hospital discharge. In other studies including mostly non-Hispanic Black and NHW older adults, the LSA has served as a proxy measure of health status and functional disability. However, this measure have underlying social and geographical components . Given that our sample of Mexican American older adults had more limited life-space mobility compared to other older adult datasets, the LSA may be not be capturing the familial, environmental, and psychosocial factors, such as multi-generational homes, environmental barriers, and structural factors, that may lower life-space mobility capacity. Further investigation is needed to examine the appropriateness of using the LSA in Mexican American older adults, identify better monitoring tools to prevent non-community discharge and 30-day readmission, and distinguish those older adults at greater risk of dying after hospital discharge.
Limitations.
There are some considerations to remember when interpreting our findings. We must acknowledge that only one pre-hospital LSA was used for our analysis, which was assessed up to two years prior to the hospitalization. Therefore, we could not capture changes in LSA that could have occurred prior to admission, nor the variability in recovery following a hospitalization that might affect post-hospitalization outcomes. Another consideration is the potentially low power of the study; therefore, this study should be replicated in a larger sample of Hispanic older adults. We are also not able to generalize our findings to other Hispanic populations in the US, as our study included only Mexican American older adults residing in one of the five southwestern states. We included only Mexican American Medicare-Fee-for-Service beneficiaries aged 65 and older with two-month continuous enrollment; therefore, our results may not be generalizable to individuals with Medicare Advantage or those who had disruptions in their Medicare coverage.
In light of these considerations, we were able to link successfully longitudinal survey data from the HEPESE with Medicare claims Part A data to study hospitalization and post-hospitalization outcomes among Mexican American older adults. This study contributes to the literature on life-space mobility and post-hospitalization outcomes among Mexican American Medicare Fee-for-Service beneficiaries, which is limited due to previous studies including only non-Hispanic Black and NHW older adult populations.
CONCLUSION
Older Mexican American Medicare Fee-for-Service beneficiaries report a restricted life-space mobility and a number of comorbidities prior to hospitalization. Pre-hospital life-space mobility was not associated with community discharge following hospitalization, but was associated with the risk of 30-day all-cause readmission. Mexican American older adults in the greatest life-space mobility quartile (i.e., 45-92) had the greatest decrease in risk of death compared to those with more restricted mobility. Continued monitoring of life-space mobility following discharge is needed to determine when to intervene following hospitalization. Future work should evaluate the impact of life-space mobility trajectories on post-hospital outcomes among older Mexican American beneficiaries.
Key Points.
Prior to hospitalization, 85.4% of older Mexican American Medicare beneficiaries reported limited life-space mobility.
Pre-admission Life-Space Assessment (LSA) scores were associated with 30-day readmission and mortality, but not community discharge, among Mexican American older adults.
Why Does this Paper Matter?
The assessment of life-space mobility may help identify older Medicare beneficiaries who are at decreased risk of mortality.
ACKNOWLEDGMENTS
The authors acknowledge Sarah Toombs Smith, PhD, ELS for editing this manuscript. The contents of this publication were developed under grants from the National Institute on Aging [NIA grant numbers K01AG065492; P30AG024832; P30AG059301; R01MD010355], the National Institute on Minority Health and Health Disparities [NIMHD grant number R01MD010355, contract number L60MD009326L] and the National Center for Advancing Translational Sciences/National Institutes of Health, Grant/Award Number [NIH grant number UL1-TR001439]. The views, opinions, and/or findings contained in this article are those of the authors and should not be construed as an official institutional position or any other federal agency, policy, or decision unless so designated by other official documentation. The contents of this publication do not necessarily represent the policy of the National Institutes of Health, and you should not assume endorsement by the Federal Government.
Funding sources:
The contents of this publication were developed under grants from the National Institute on Aging [NIA grant numbers K01AG065492; P30AG024832; P30AG059301, R01 MD010355, AG10939], the National Center for Advancing Translational Sciences/National Institutes of Health, Grant/Award Number [NIH grant number UL1-TR001439], and the National Institute on Minority Health and Health Disparities [NIMHD contract number L60MD009326L]. The views, opinions, and/or findings contained in this article are those of the authors and should not be construed as an official institutional position or any other federal agency, policy, or decision, unless so designated by other official documentation. The contents of this publication do not necessarily represent the policy of the National Institutes of Health, and you should not assume endorsement by the Federal Government.
Footnotes
Conflict of Interest: We have no conflicts of interest to disclose.
REFERENCES
- 1.Noe-Bustamante L, Flores A, Shah S. Facts on Hispanics of Mexican origin in the United States, 2017. Hispanic Trends September 16, 2019; https://www.pewresearch.org/hispanic/fact-sheet/u-s-hispanics-facts-on-mexican-origin-latinos/. Accessed July 13, 2020.
- 2.Garcia MA, Downer B, Crowe M, Markides KS, Suitor JJ. Aging and disability among Hispanics in the United States: Current knowledge and future directions. Innovation in aging. 2017;1(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Markides KS, Rote S. Immigrant health paradox. Emerging trends in the social and behavioral sciences: An interdisciplinary, searchable, and linkable resource. 2015:1–15. [Google Scholar]
- 4.Baker PS, Bodner EV, Allman RM. Measuring life-space mobility in community-dwelling older adults. J Am Geriatr Soc. 2003;51(11):1610–1614. [DOI] [PubMed] [Google Scholar]
- 5.Webber SC, Porter MM, Menec VH. Mobility in older adults: a comprehensive framework. Gerontologist. 2010;50(4):443–450. [DOI] [PubMed] [Google Scholar]
- 6.Bentley JP, Brown CJ, McGwin G Jr., Sawyer P, Allman RM, Roth DL. Functional status, life-space mobility, and quality of life: a longitudinal mediation analysis. Qual Life Res. 2013;22(7):1621–1632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Crowe M, Andel R, Wadley VG, Okonkwo OC, Sawyer P, Allman RM. Life-space and cognitive decline in a community-based sample of African American and Caucasian older adults. J Gerontol A Biol Sci Med Sci. 2008;63(11):1241–1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.James BD, Boyle PA, Buchman AS, Barnes LL, Bennett DA. Life space and risk of Alzheimer disease, mild cognitive impairment, and cognitive decline in old age. Am J Geriatr Psychiatry. 2011;19(11):961–969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xue QL, Fried LP, Glass TA, Laffan A, Chaves PH. Life-space constriction, development of frailty, and the competing risk of mortality: the Women’s Health And Aging Study I. Am J Epidemiol. 2008;167(2):240–248. [DOI] [PubMed] [Google Scholar]
- 10.Brown CJ, Roth DL, Allman RM, Sawyer P, Ritchie CS, Roseman JM. Trajectories of life-space mobility after hospitalization. Ann Intern Med. 2009;150(6):372–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sheppard KD, Sawyer P, Ritchie CS, Allman RM, Brown CJ. Life-space mobility predicts nursing home admission over 6 years. Journal of aging and health. 2013;25(6):907–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Boyle PA, Buchman AS, Barnes LL, James BD, Bennett DA. Association between life space and risk of mortality in advanced age. Journal of the American Geriatrics Society. 2010;58(10):1925–1930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lo AX, Flood KL, Kennedy RE, et al. The association between life-space and health care utilization in older adults with heart failure. Journals of Gerontology Series A: Biomedical Sciences and Medical Sciences. 2015;70(11):1442–1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McCaskill GM, Sawyer P, Burgio KL, et al. The impact of Veteran status on life-space mobility among Older Black and White men in the Deep South. Ethnicity & disease. 2015;25(3):255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Choi M, O’Connor ML, Mingo CA, Mezuk B. Gender and racial disparities in life-space constriction among older adults. The Gerontologist. 2016;56(6):1153–1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.De Silva NA, Gregory MA, Venkateshan SS, Verschoor CP, Kuspinar A. Examining the Association between Life-Space Mobility and Cognitive Function in Older Adults: A Systematic Review. J Aging Res. 2019;2019:3923574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kennedy RE, Williams CP, Sawyer P, et al. Life-Space Predicts Health Care Utilization in Community-Dwelling Older Adults. J Aging Health. 2019;31(2):280–292. [DOI] [PubMed] [Google Scholar]
- 18.Curcio CL, Alvarado BE, Gomez F, Guerra R, Guralnik J, Zunzunegui MV. Life-Space Assessment scale to assess mobility: validation in Latin American older women and men. Aging Clin Exp Res. 2013;25(5):553–560. [DOI] [PubMed] [Google Scholar]
- 19.Simoes M, Garcia IF, Costa LDC, Lunardi AC. Life-Space Assessment questionnaire: Novel measurement properties for Brazilian community-dwelling older adults. Geriatr Gerontol Int. 2018;18(5):783–789. [DOI] [PubMed] [Google Scholar]
- 20.Gonzalez BC, Delgado LH, Quevedo JE, Gallegos Cabriales EC. Life-space mobility, perceived health, and depression symptoms in a sample of Mexican older adults. Hisp Health Care Int. 2013;11(1):14–20. [DOI] [PubMed] [Google Scholar]
- 21.Silberschmidt S, Kumar A, Raji MM, Markides K, Ottenbacher KJ, Al Snih S. Life-Space Mobility and Cognitive Decline Among Mexican Americans Aged 75 Years and Older. J Am Geriatr Soc. 2017;65(7):1514–1520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Al Snih S, Peek KM, Sawyer P, Markides KS, Allman RM, Ottenbacher KJ. Life-space mobility in Mexican Americans aged 75 and older. J Am Geriatr Soc. 2012;60(3):532–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chung J, Flores-Montoya A. Correlates and Predictors of Mobility Limitation in Community-Dwelling Hispanic Older Adults in the United States: A Systematic Review. J Immigr Minor Health. 2018;20(3):729–743. [DOI] [PubMed] [Google Scholar]
- 24.Brown CJ, Kennedy RE, Lo AX, Williams CP, Sawyer P. Impact of emergency department visits and hospitalization on mobility among community-dwelling older adults. The American journal of medicine. 2016;129(10):1124. e1129–1124. e1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Loyd C, Beasley TM, Miltner RS, Clark D, King B, Brown CJ. Trajectories of community mobility recovery after hospitalization in older adults. Journal of the American Geriatrics Society. 2018;66(7):1399–1403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fathi R, Bacchetti P, Haan MN, Houston TK, Patel K, Ritchie CS. Life-Space Assessment Predicts Hospital Readmission in Home-Limited Adults. J Am Geriatr Soc. 2017;65(5):1004–1011. [DOI] [PubMed] [Google Scholar]
- 27.Kennedy RE, Sawyer P, Williams CP, et al. Life-Space Mobility Change Predicts 6-Month Mortality. J Am Geriatr Soc. 2017;65(4):833–838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Markides KS, Stroup-Benham CA, Goodwin JS, Perkowski LC, Lichtenstein M, Ray LA. The effect of medical conditions on the functional limitations of Mexican-American elderly. Ann Epidemiol. 1996;6(5):386–391. [DOI] [PubMed] [Google Scholar]
- 29.Markides KS, Chen N-W, Angel R, Palmer R. Hispanic Established Populations for the Epidemiologic Study of the Elderly (HEPESE) Wave 8, 2012-2013 [Arizona, California, Colorado, New Mexico, and Texas]. In: Inter-university Consortium for Political and Social Research [distributor]; 2016. [Google Scholar]
- 30.Downer B, Al Snih S, Chou LN, Kuo YF, Markides KS, Ottenbacher KJ. Differences in hospitalizations, emergency room admissions, and outpatient visits among Mexican-American Medicare beneficiaries. BMC Geriatr. 2019;19(1):136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Parker M, Baker PS, Allman RM. A life-space approach to functional assessment of mobility in the elderly. J Gerontological Social Work. 2002;35(4):35–55. [Google Scholar]
- 32.Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged: the index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185(12):914–919. [DOI] [PubMed] [Google Scholar]
- 33.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. [DOI] [PubMed] [Google Scholar]
- 34.Alfaro-Acha A, Al Snih S, Raji MA, Kuo YF, Markides KS, Ottenbacher KJ. Handgrip strength and cognitive decline in older Mexican Americans. J Gerontol A Biol Sci Med Sci. 2006;61(8):859–865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied psychological measurement. 1977;1(3):385–401. [Google Scholar]
- 36.Johnson J, Rodriguez MA, Al Snih S. Life-Space Mobility in the Elderly: Current Perspectives. Clin Interv Aging. 2020;15:1665–1674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Duncan PW, Bushnell C, Sissine M, et al. Comprehensive Stroke Care and Outcomes: Time for a Paradigm Shift. Stroke. 2021;52(1):385–393. [DOI] [PubMed] [Google Scholar]
- 38.Cary MP Jr., Prvu Bettger J, Jarvis JM, Ottenbacher KJ, Graham JE. Successful Community Discharge Following Postacute Rehabilitation for Medicare Beneficiaries: Analysis of a Patient-Centered Quality Measure. Health Serv Res. 2018;53(4):2470–2482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Holup AA, Gassoumis ZD, Wilber KH, Hyer K. Community Discharge of Nursing Home Residents: The Role of Facility Characteristics. Health Serv Res. 2016;51(2):645–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mackey DC, Cauley JA, Barrett-Connor E, et al. Life-space mobility and mortality in older men: a prospective cohort study. J Am Geriatr Soc. 2014;62(7):1288–1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mackey DC, Lui LY, Cawthon PM, Ensrud K, Yaffe K, Cummings SR. Life-Space Mobility and Mortality in Older Women: Prospective Results from the Study of Osteoporotic Fractures. J Am Geriatr Soc. 2016;64(11):2226–2234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jacobs JM, Hammerman-Rozenberg A, Stessman J. Frequency of Leaving the House and Mortality from Age 70 to 95. J Am Geriatr Soc. 2018;66(1):106–112. [DOI] [PubMed] [Google Scholar]
- 43.Masoli JAH, Delgado J, Pilling L, Strain D, Melzer D. Blood pressure in frail older adults: associations with cardiovascular outcomes and all-cause mortality. Age Ageing. 2020;49(5):807–813. [DOI] [PMC free article] [PubMed] [Google Scholar]


