Abstract
Purpose
Syndesmotic screw removal following acute syndesmotic injury is a commonly performed procedure. However, recent studies suggest that the removal does not result in improved patient reported outcome, while the procedure has proved not to be without complications. The aim of this study was to present a health-economic evaluation of on-demand removal (ODR) compared to routine removal (RR) of the syndesmotic screw.
Methods
Data were collected from the RODEO trial, a randomized controlled non-inferiority trial comparing functional outcome of ODR with RR. Economic evaluation resulted in total costs, costs (in Euro) per quality adjusted life year (QALY) and costs per point improvement on the Olerud Molander Ankle Score (OMAS). This included both direct and indirect costs.
Results
Total costs for ODR were significantly lower with a mean difference of 3160 euro compared to RR (p < 0.001). The difference in QALY was not significant. The difference in OMAS at 12 months was 1.79 with an incremental cost-effectiveness ratio (ICER) of €-1763 (p = 0.512). The ICER was well below the willingness to pay. Although unit costs might vary between hospitals and countries, these results provide relevant data of cost-effectiveness.
Conclusion
The clinical effectiveness of both ODR and RR can be considered equal. The costs are lower for patients treated with ODR, which leads to the conclusion that ODR is cost-effective.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00068-022-02158-9.
Keywords: Ankle fractures surgery; Cost–Benefit analysis; Fracture fixation, internal/economics; Fracture fixation, internal/instrumentation; Implant removal; Quality of life
Introduction
Syndesmotic screw removal is a commonly performed procedure within the field of orthopaedic trauma surgery. Syndesmotic screws are placed in order to fixate syndesmotic injuries in unstable ankle injuries, either with or without a fracture [1–3]. Although other fixation methods for syndesmotic injury (e.g. suture-buttons, bioabsorbable screws) are being used increasingly, the metallic syndesmotic screw thus far remains the most commonly used device [1–4]. The syndesmotic screw is a rigid fixation method, inhibiting motion of the distal tibiofibular joint. Combined with the risk of breakage, the assumed limitation in range of motion is why the screw is often removed after the syndesmosis has healed (8–12 weeks) [5, 6]. However, recent studies have suggested that the removal of this screw does not necessarily result in improved patient reported outcome [7–9]. Moreover, removing syndesmotic screws has proved not to be without complications, such as surgical site infections (SSI) [10].
Surgical site infections (SSI) occur frequently following implant removal [11]. SSIs are not only limiting functional recovery but are also associated with an increase in health care costs of up to €10,000 per patient [12–14]. By leaving the screw in place, these complications could be adverted, potentially resulting in improved overall outcome and in reduced health care costs. Syndesmotic screw removal may still be indicated in some cases, for example if the screw causes skin irritation, limited range of motion without screw loosening, or when there is a malposition of the fibula in the fibular notch of the tibia [8, 15]. If the syndesmotic screws were to be removed “on demand” (only in case of complaints), many procedures may be avoided. A recent randomized controlled trial (RCT) by Sanders et al. showed that on-demand removal (ODR) was non-inferior to routine removal (RR) of the syndesmotic screw when it comes to functional outcome [15]. The aim of the current study was to present a health-economic evaluation of ODR compared to RR of the syndesmotic screw in patients with acute syndesmotic injury. We hypothesize that there will be lower costs following ODR and therefore that ODR is cost-effective.
Materials and methods
Data were collected from the RODEO trial, a randomized controlled non-inferiority trial comparing on-demand removal to routine removal of the syndesmotic screw, of which the full study protocol has been previously reported [16]. In summary, all adult (> 17 y/o) patients with acute syndesmotic injury (with or without accompanying ankle fracture), fixated within 14 days of trauma using one or two syndesmotic screws, were eligible for inclusion. Excluded were patients with an ISS score > 15, insufficient physical condition (to allow for potential removal surgery), concomitant injury of the ipsi- or contralateral ankle or other medical conditions hampering rehabilitation, and insufficient comprehension of Dutch, Finnish, Swedish or English language. Patients were included from 17 centres within the Netherlands and Finland, of which three were academic and 14 were teaching hospitals. As further elaborated on in the protocol, patients randomized for routine removal underwent removal of the syndesmotic screw 8–12 weeks after fixation, whereas in the ODR group, patients retained their screw unless they had complaints warranting removal [16]. The reasons for removals in the ODR group were pain, limited ROM, stiffness, revision surgery where new syndesmotic fixation was indicated, skin reaction to implants, screw backing out or patient’s wish not otherwise described. The primary outcome of this trial was functional outcome, measured by the Olerud Molander Ankle Score (OMAS). Secondary outcomes were the AOFAS (American Orthopaedic Foot and Ankle Society Ankle-Hindfoot scale), range of motion, quality of life (EQ-5D-5L), cost-utility and cost-effectiveness. Outcomes were all measured at 3, 6 and 12 months after syndesmotic fixation.
The trial was registered in the Netherlands Trial Register (NTR5965) and Clinicaltrials.gov (NCT02896998) and sponsored by ZonMw, a Dutch governmental organization (grant number: 843002705).
Economic evaluation
The economic evaluation consisted of a cost-utility analysis (CUA) and a cost-effectiveness analysis (CEA) from a societal perspective with the costs per quality adjusted life year (QALY) and the costs per point functional outcome improvement as the primary economic outcomes. The costs were also compared to the willingness to pay. Both direct and indirect costs were used, based on average unit costs of 2018. The analyses were based on the intention-to-treat groups, using a time horizon of 12 months, since relevant differences in outcome and health care costs were expected to occur within that period.
Resource utilization
Data on resource utilization were collected through questionnaires at 3, 6 and 12 months after syndesmotic fixation. The questionnaires used to evaluate in and out of hospital resource use were the iMTA Medical Consumption Questionnaire (iMCQ) and the iMTA Productivity Cost Questionnaire (iPCQ). In addition to this, patients’ medical records were screened after follow-up completion (12 months) to check for complications and revisions procedures. Resources were classified as either direct medical, direct non-medical or indirect non-medical costs. Direct medical costs were further subdivided into (1) regular in hospital costs, related to the index admission (syndesmotic screw removal, visits to outpatient clinic), (2) additional in hospital costs, related to complications or readmissions (additional implant removal, revision surgery, surgical debridement, readmission surgical ward, emergency room visits and ambulance rides), (3) out of hospital (para-)medical costs (general practitioner, company doctor, physiotherapist, home care). Indirect non-medical costs resulting from work absence or decreased productivity were determined using the iPCQ. To estimate loss of productivity, the friction costs method was used. Total costs per patient and per group were calculated by multiplying resources by the associated unit costs.
Definition of outcomes
Quality of life was measured by the single value calculated from the EQ-5D-5L questionnaire on each time point (3, 6 and 12 months after syndesmotic fixation), using the standard Dutch tariff values[17]. Quality Adjusted Life Years (QALYs) were then calculated by multiplying the overall quality of life at each time point with the period of time, using the area under the curve method. Incremental cost-effectiveness ratios were calculated both as the difference in costs per QALY gained and as the difference in costs per additional point of improvement in functional outcome. Functional outcome was defined as the mean OMAS at 12 months, for which the difference between the two groups was calculated.
Unit costs (in euro)
Costs of the various resources were extracted from the Dutch guideline on unit costs for health care, which was based on average health care prices in 2014[18][18]. To adjust these costs to the situation during the inclusion period of this study (2017–2019), a conversion factor of 1,041, based on the Consumer Price Index, was used in order to adjust all costs to the year 2018 [19]. Costs of specific procedures were based on DBC Health care products which are data of the Dutch Health Care Authority indicating costs for procedures based on insurance billing coledes, taking the 2018 price for each procedure [20]. Costs and units for each variable, adjusted to 2018, are displayed in Table 1 of the supplementary content.
Table 1.
Baseline characteristics
| Routine Removal (N = 93) | On-Demand Removal (N = 104) | |
|---|---|---|
| Sex, men | 57 (61.3%) | 62 (59.6%) |
| Age, mean (SD) | 44.8 (1.6) | 47.1 (1.4) |
| < 60 y/o | − 76 (81.7%) | − 84 (80.8%) |
| > / = 60 y/o | − 17 (18.3%) | − 20 (19.2%) |
| BMI, mean (SD) | 28.1 (0.6) | 28.3 (0.6) |
| Missing | 3 | 5 |
| Nicotine use | 24 (27.9%) | 25 (25.5%) |
| Missing | 7 | 6 |
| Alcohol abuse (> 2units/day) | 7 (8.1%) | 11 (11.2%) |
| Missing | 7 | 6 |
| Injury | ||
| Weber B | 26 (28.3%) | 21 (20.2%) |
| Weber C | 46 (50.0%) | 54 (51.9%) |
| Maisonneuve | 16 (17.4%) | 26 (25.0%) |
| Isolated* | 3 (3.3%) | 2 (1.9%) |
| Other | 1 (1.1%) | 1 (1.0%) |
| Missing | 1 | |
| ASA classification | ||
| I | 46 (50.0%) | 42 (41.2%) |
| II | 43 (46.7%) | 49 (48.0%) |
| III | 3 (3.3%) | 11 (10.8%) |
| Missing | 1 | 2 |
| No. Screw(s): | ||
| 1 | 63 (68.5%) | 68 (66.0%) |
| 2 | 29 (31.5%) | 35 (34.0%) |
| Missing | 1 | 1 |
| Cortices: | ||
| 3 | 74 (80.4%) | 84 (81.6%) |
| 4 | 18 (19.6%) | 19 (18.4%) |
| Missing | 1 | 1 |
ASA American Society of Anesthesiologists, BMI body mass index (weight/(height2)), No number of, y/o years old
*Isolated syndesmotic injury (without fracture)
Statistical analysis
Results are reported as means and mean difference along with their 95% confidence intervals and tested using independent sample t test. Differences in costs and effectiveness between the two groups were drawn and displayed graphically with cost-effectiveness planes. Incremental cost-utility (ICUR) and cost-effectiveness (ICER) ratios were calculated by dividing the mean difference in total costs per patient between treatment groups by the mean difference in QALYs and in OMAS, respectively. Therefore, ICER is the price in euro’s per point difference on the OMAS.
Missing data were handled according to the recent paper by Brand et al. [21]. Costs, QALYs and OMAS were multiple imputed at the item per time point level. Ten imputation sets were generated using MICE with predictive mean matching and combined using Rubins rule. Costs and effectiveness were predicted by randomized group, age, sex, BMI, smoking, alcohol, diabetes, chronic obstructive pulmonary disease, American Society of Anesthesiologists (ASA) classification, type of injury, all health care costs, productivity loss, QALYs and OMAS. Dependencies over time were taken into account by including measurements at all time points.
The confidence intervals of the ICER and the cost-effectiveness plane were based on bias-corrected and accelerated non-parametric bootstrapping of 1000 bootstrap samples after combining the multiple data sets into one mean single imputation [21].
In addition to the primary CUA and CEA analyses, preplanned subgroup-analyses were performed for patients younger/older than 60 years old and for patients with/without a SSI. Sensitivity analyses were performed by varying medical costs of screw removal, outpatient clinic visits, emergency room visits and revalidation clinic admissions by 30%. Analyses were performed using R version 3.6.1 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Between January 2017 and April 2019, 197 patients were included in the RODEO trial, of which 93 randomized for RR and 104 for ODR of the syndesmotic screw. Baseline characteristics of all patients incorporated in the current economic evaluation are shown in Table 1. Overall response rates of the questionnaires were 69.5%, 68.5% and 68.5% at 3, 6 and 12 months, respectively.
Costs and resource use
Table 2 shows the difference in resource utilization and costs in total and as mean per patient for each group. There was a significant difference in total costs per patient (sum of direct and indirect costs) of − €3160 (95% CI − €4170 to − €2149, p < 0.001), in favour of ODR. This difference was made up by the difference in direct costs; 1. Costs for syndesmotic screw removal, which were significantly lower in the ODR group, as expected (− €1000, 95% CI − €1166 to − €835, p < 0.001), 2. More readmissions and surgical debridements in RR, leading to a mean difference per patient of -€1,274 (95% CI -€2,690 to €142, p = 0.077), and 3. A shorter duration of revalidation and home care in the ODR group (− €144, 95% CI − €341 to €53, p = 0.152). Also included in the difference were the indirect non-medical costs, which were €503,985 for RR and €482,891 for ODR (Table 2).
Table 2.
Resource utilization and (mean) costs, as indexed for 2018
| Routine Removal (n = 93) | On-Demand Removal (n = 104) | ||||
|---|---|---|---|---|---|
| Unit | Total units | Total costs (€) | Total units | Total costs (€) | |
| Index admission | |||||
| Syndesmotic screw removal | Procedures | 82 | 127,920 | 25 | 39,000 |
| Mean subtotal per patient (95% CI) | 1375 (1343–1408) | 375 (334–416) | |||
| Mean difference in subtotal (95% CI) | − 1000 (− 1166 to − 835, p < 0.001) | ||||
| Readmissions and reinterventions | |||||
| Removal of other material | Procedures | 4 | 6,240 | 4 | 6240 |
| Revision reconstruction /syndesmotic fixation | Procedures | 9 | 31,050 | 9 | 31,050 |
| Surgical debridement | Procedures | 4 | 13,800 | 1 | 3,450 |
| Readmission Surgical Ward | Days | 120 | 50,593 | 80 | 33,729 |
| Emergency room visits/ ambulance | Frequency | 94 | 50,395 | 79 | 42,353 |
| Revalidation | Days | 148 | 70,871 | 0 | 0 |
| Subtotal | 222,949 | 116,822 | |||
| Mean subtotal per patient (95% CI) | 2397 (1018 to 3776) | 1123 (794–1,4527) | |||
| Mean difference in subtotal (95% CI) | −1274 (− 2690 to 142, p = 0.077) | ||||
| Regular care | |||||
|
Outpatient clinic visits Dep. of surgery |
Visits | 226 | 17,174 | 190 | 14,438 |
| Physician | 138 | 4,740 | 169 | 5805 | |
| Company doctor | 198 | 19,996 | 198 | 19,996 | |
| Physiotherapist | 1393 | 47,850 | 1420 | 48,777 | |
| Home care | Days | 113 | 5316 | 87 | 2317 |
| Subtotal | 95,076 | 91,333 | |||
| Mean subtotal per patient (95% CI) | 1022 (871–1174) | 878 (750–1007) | |||
| Mean difference in subtotal (95% CI) | − 144 (− 341 to 53, p = 0.152) | ||||
| Other costs | |||||
| Out of pocket expenses | Euro | 2,508 | 2051 | ||
| Total direct medical costs | 448,453 | 249,207 | |||
| Indirect non-medical costs | 503,985 | 482,891 | |||
| Total costs | 952,438 | 732,098 | |||
| Mean total costs per patient (95% CI) | 9913 (9073–10,754) | 6753 (6190–7316) | |||
| Mean difference in total costs per patient (95% CI) | − 3,160 (− 4170 to –2149, p < 0.001) | ||||
Cost-utility
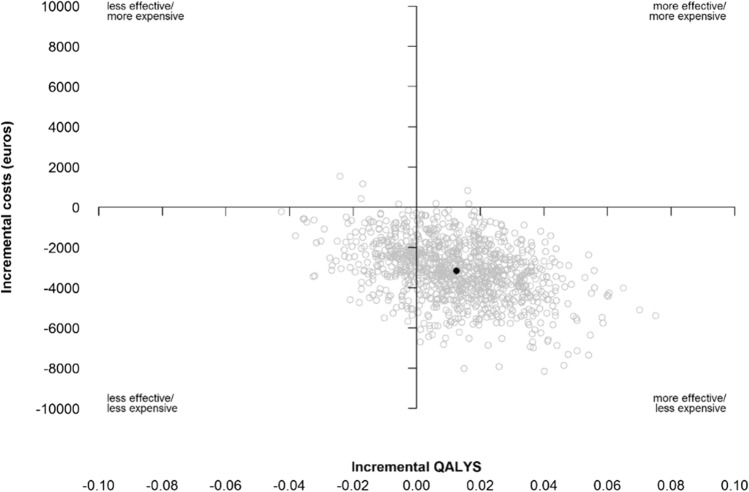
The mean QALYs in 1 year was 0.795 (95% CI 0.727–0.862) in the group with on-demand removal and 0.782 (95% CI 0.753–0.811) in the group with routine removal, which lead to a difference in QALYs of 0.013 (95% CI − 0.026 to 0.051, p = 0.474). This difference was not statistically significant, nor clinically relevant. Figure 1 shows the cost-effectiveness plane for QALYS. The incremental cost-utility ratio was -€252,673 (95% BCa CI: − €24,219,700 to €65,306).
Fig. 1.
Effectiveness plane of QALYS compared to Incremental costs in Euros
Cost-effectiveness
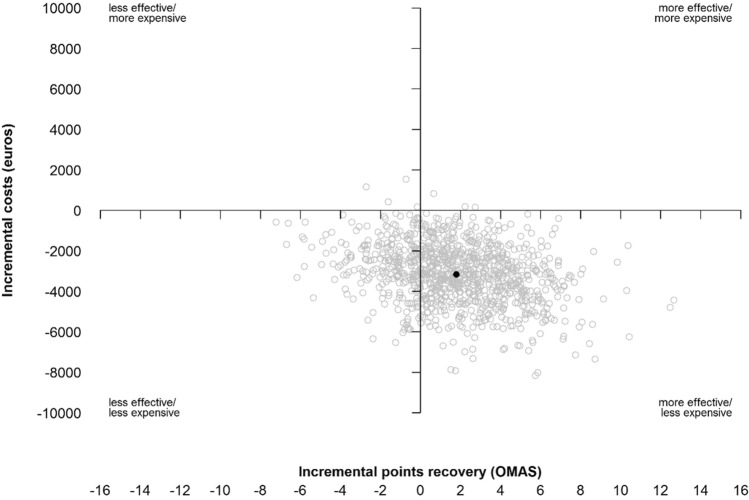
The mean difference in functional outcome, measured by the OMAS at 12 months, was 1.79 (95% CI − 4.92 to 8.50), with a mean OMAS of 78.62 (95% CI 66.90–90.34) in the ODR group and 76.83 (95% CI 71.82–81.83) in the RR group. The ICER was in favour of ODR: − €1.763 (95% CI − €564,687 to €166, p = 0.512). This is shown in Fig. 2.
Fig. 2.
Effectiveness plane of functional outcome score in OMAS compared to Incremental costs in Euros
Subgroup analyses
The subgroup analysis based on age (< 60 vs. > / = 60) showed cost-effectiveness for ODR when it comes to functional outcome for patients under 60 y/o. For every point difference on the OMAS, there was a difference of − €3,333 (− €8,253,179 to − €1,097) between ODR and RR with less expenses in the ODR group (Table 2 of Supplementary content). ODR in patients < 60 costs €1,017,572 less per QALY and a QALY costs €43,716 less in patients ≥ 60 years.
The subgroup analysis which excludes patients with a SSI is specified in the supplementary content and had a mean difference in costs of €− 3226 (− €6822 to €370), mean difference in functional recovery by OMAS at 12 months of 1.34 (− 5.35 to 8.04) and a mean difference in QALY over 12 months of 0.014 (− 0.026 to 0.054). Costs, functional recovery and QALY were more favourable in the ODR group. The ICUR was -€230,542 (€− 219.210.538 to €54.613).
Following sensitivity analyses, medical costs all showed a difference in costs between RR and ODR, in favour of ODR (Table 3).
Table 3.
Sensitivity analyses of medical costs per patient
| ODR (€) | RR (€) | Cost difference (€) | |
|---|---|---|---|
| Total medical costs (base analysis) | 2396 ( 2020–2840) | 4822 (3901–7522) | − 2426 ( − 4916 to − 1437) |
| Syndesmotic screw removal | |||
| -30% | 1967 ( 1682–2345) | 4055 ( 3224–7276) | − 2,088 ( − 5110 to − 1200) |
| + 30% | 2228 ( 1880–2649) | 4921 ( 4075 to 8092) | − 2693 ( − 5473 to − 1765) |
| Outpatient visits | |||
| -30% | 2392 ( 2025–2839) | 4804 ( 3879–7493) | − 2413 ( − 4895 to − 1432) |
| + 30% | 2507 ( 2126 to 2963) | 4948 ( 4020–7627) | -2441 ( − 4887 to − 1444) |
| ER visits | |||
| -30% | 1975 ( 1665–2353) | 4326 ( 3496–7516) | − 2350 ( − 5263 to − 1464) |
| + 30% | 2220 ( 1897–2634) | 4651 ( 3787–7827) | − 2431 ( − 5240 to − 1497) |
| Removal of revalidation | |||
| 2098 ( 1794–2508) | 3726 ( 3323–4209) | − 1628 ( − 2234 to − 1088) | |
Discussion
The mean difference in total costs was €3,160 per patient in favour of the ODR group. Even though the upper limit of the 95% confidence interval of the ICER was marginally higher than zero, it was well below the level of willingness to pay, which is 50.000 euro, which makes ODR a cost-effective intervention [22].
This is the first cost analysis study to focus solely on screw fixation for syndesmotic injury, comparing cost-effectiveness of syndesmotic screws removed routinely or on demand. Previously performed cost analyses have focussed on the cost-effectiveness of screw versus dynamic implants, such as the suture button [23–25]. Neary et al. described that when comparing a tightrope to not-routinely removed syndesmotic screws, less than 10% of screws would have to be removed in order to be cost-effective [23]. However, their study was based solely on numbers from the literature, and not on original data. Moreover, their calculations were based on a revision (removal) surgery price of $14,768, which is much higher than the €1560 ($1796 based on exchange rate of 2018) that was indexed in the Netherlands for this procedure in 2018. Weber et al. found that cost-effectiveness of screw and Suture button fixation were more dependent on the removal rate and that they would be equivalent in price when the removal rate of screws would be between 18 and 53%, assuming that the removal rate of Suture button is 0[25]. Since the removal rate in the ODR group in our trial was 23%, this would make it cost-effective or at least equivalent to use a syndesmotic screw. Although long-term complications of retaining syndesmotic screws have not been studied yet, several long-term complications of dynamic implants (e.g. infections, osteomyelitis, osteolysis, and diastasis as a result from failed stabilization) have been described, which have not been incorporated in any of the above-mentioned studies [26–29]. Combining these complications with the cost-effectiveness of ODR of syndesmotic screws makes a strong case for keeping/implementing ODR of the syndesmotic screw as standard treatment.
In this study, the direct costs were higher following RR, mainly because of the costs of higher frequency of surgery and more readmissions at the surgical ward. In addition, we expected the costs to be higher due to the higher rate of SSIs in the RR group, resulting in higher health care costs. Therefore, we also calculated the difference in costs excluding patients with SSI, which had no relevant effect on the results. Thus, the difference in costs cannot be explained solely by the amount of SSIs in the RR group.
For indirect costs, the iPCQ and the friction costs method with age-adjusted mean daily wages were used to estimate loss of productivity. Indirect costs, defined as lost hours of productivity, were higher in the RR group. Because this cohort was part of a RCT, we can assume that the hourly wage and therefore lost productivity costs were equally divided between both groups and that this does not account for the difference.
The functional outcome after 12 months, measured with OMAS, did show a difference of 1.79 with higher scores following ODR [15]. This leads to an ICER of €-1763 (the difference in costs per point at the OMAS), supporting the suggestion to opt for ODR.
In the subgroup analysis comparing patients aged < 60 years and patients ≥ 60 years, we found that the costs gained when choosing for ODR are higher in the younger group, which can be attributed to the fact that the younger group has less indirect costs following ODR because these costs include costs made by work deprivation. The results of this subgroup analysis could be taken into account in daily practice.
This study compared ODR and RR following syndesmotic injury, and the removal was performed at the operation room. Sugi et al. recently state that it is safe to remove the syndesmotic screw in a clinical setting out of the operating room based on a complication rate of 2 SSIs in 170 patients [30]. This might affect removal costs but is not likely to change OMAS and QALYs after 12 months compared to our study. Since these results are from one single study and costs may vary compared to our study, an additional RCT with clinical setting for removal might attribute to the current literature.
A limitation of our study was that unit costs might vary between hospitals due to overhead costs, which was not accounted for in the current study, leading to an estimation of the costs per patient and in total. However, due to the randomized set-up of the study, uncertainties are expected to be equally divided. Additionally, in this study, only costs made within 12 months after syndesmotic fixation were incorporated. The results thereby do not include removal of screws after this period of time, or potential late complications of retaining the syndesmotic screw. We know that if the retained syndesmotic screw breaks, the location of breakage affects the chance of cortical erosion due to the broken syndesmotic screw [31]. But to the best of our knowledge, there have not been any trials studying the long-term complications and outcome of retaining syndesmotic screws. Therefore, we are unable to say what the consequences for costs would be.
Conclusion
The clinical effectiveness of both ODR and RR can be considered equal. The costs are lower for patients treated with ODR, which leads to the conclusion that ODR is cost-effective.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
RODEO collaborator group: M.P. van den Bekerom: Department of Orthopedic Surgery, OLVG, Amsterdam, The Netherlands. Orchid: 0000-0002-1184-0529. B. van Dijkman: Department of Surgery, Flevo Hospital, Almere, The Netherlands. J.A. Halm: Trauma Unit Amsterdam UMC, location AMC, Amsterdam, the Netherlands. Orchid: 0000-0002-3649-0609. J. M. Hoogendoorn: Department of Surgery, Haaglanden MC, The Hague, The Netherlands. Orchid: 0000-0001-8445-2079. M. Parkkinen: Department of Orthopaedics and Traumatology, Helsinki University Hospital, Helsinki, Finland. R.N. van Veen: Department of Surgery, OLVG, Amsterdam, The Netherlands
Funding
This research was sponsored by ZonMw, a Dutch governmental organization (grant number: 843002705).
Data availability
The datasets analyzed during the current work are available upon reasonable request from the corresponding author.
Declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of the Amsterdam UMC, location AMC: ‘METC AMC’.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Footnotes
List of authors in RODEO collaborator group are in acknowledgements.
D. Penning and F. R. K. Sanders shared first authorship.
Contributor Information
T. Schepers, Email: t.schepers@amsterdamumc.nl
RODEO collaborator group:
M. P. van den Bekerom, B. van Dijkman, J. A. Halm, J. M. Hoogendoorn, M. Parkkinen, and R. N. van Veen
References
- 1.Schnetzke M, Vetter SY, Beisemann N, Swartman B, Grützner PA, Franke J. Management of syndesmotic injuries: What is the evidence? World J Orthopaedics. 2016 doi: 10.5312/wjo.v7.i11.718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tourné Y, Molinier F, Andrieu M, Porta J, Barbier G. Diagnosis and treatment of tibiofibular syndesmosis lesions. Orthop Traumatol Surg Res. 2019 doi: 10.1016/j.otsr.2019.09.014. [DOI] [PubMed] [Google Scholar]
- 3.Magan A, Golano P, Maffulli N, Khanduja V. Evaluation and management of injuries of the tibiofibular syndesmosis. Br Med Bull. 2014 doi: 10.1093/bmb/ldu020. [DOI] [PubMed] [Google Scholar]
- 4.Ræder BW, Stake IK, Madsen JE, Frihagen F, Jacobsen SB, Andersen MR, et al. Randomized trial comparing suture button with single 3.5 mm syndesmotic screw for ankle syndesmosis injury: similar results at 2 years. Acta Orthop. 2020; DOI: 10.1080/17453674.2020.1818175 [DOI] [PMC free article] [PubMed]
- 5.Schepers T, van Zuuren WJ, van den Bekerom MPJ, Vogels LMM, van Lieshout EMM. The management of acute distal tibio-fibular syndesmotic injuries: results of a nationwide survey. Injury. 2012;43(10):1718–1723. doi: 10.1016/j.injury.2012.06.015. [DOI] [PubMed] [Google Scholar]
- 6.Bell DP, Wong MK. Syndesmotic screw fixation in Weber C ankle injuries–should the screw be removed before weight bearing? Injury. 2006;37(9):891–898. doi: 10.1016/j.injury.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 7.Boyle MJ, Gao R, Frampton CMA, Coleman B. Removal of the syndesmotic screw after the surgical treatment of a fracture of the ankle in adult patients does not affect one-year outcomes: A randomised controlled trial. Bone Jt J. 2014 doi: 10.1302/0301-620X.96B12.34258. [DOI] [PubMed] [Google Scholar]
- 8.Walley KC, Hofmann KJ, Velasco BT, Kwon JY. Removal of hardware after syndesmotic screw fixation: a systematic literature review. Foot Ankle Spec. 2017 doi: 10.1177/1938640016685153. [DOI] [PubMed] [Google Scholar]
- 9.DIngemans SA, Rammelt S, White TO, Goslings JC, Schepers T. Should syndesmotic screws be removed after surgical fixation of unstable ankle fractures? a systematic review. Bone and Joint Journal. 2016. DOI: 10.1302/0301-620X.98B11.BJJ-2016-0202.R1 [DOI] [PubMed]
- 10.Sanders FRK, Birnie MFN, Penning D, Goslings JC, Schepers T. Surgical site infections following routine syndesmotic screw removal; a systematic review. J Orthop Trauma. 2020 doi: 10.1097/BOT.0000000000001954. [DOI] [PubMed] [Google Scholar]
- 11.Backes M, Dingemans SA, Dijkgraaf MGW, Van den Berg HR, Van Dijkman B, Hoogendoorn JM, et al. Effect of antibiotic prophylaxis on surgical site infections following removal of orthopedic implants used for treatment of foot, ankle, and lower leg fractures a randomized clinical trial. JAMA—J Am Med Assoc. 2017 doi: 10.1001/jama.2017.19343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wille, Schrieck van der, Genugten V. Wat levert surveillance van postoperatieve wondinfecties op? Sneller beter doorbraakproject wondinfecties 2004–2008. 2008;4:28–34.
- 13.Nobile M, Navone P, Orzella A, Colciago R, Auxilia F, Calori G. Developing a model for analysis the extra costs associated with surgical site infections (SSIs): an orthopaedic and traumatological study run by the Gaetano Pini Orthopaedic Institute. Antimicrob Resist Infect Control. 2015 doi: 10.1186/2047-2994-4-s1-p68. [DOI] [Google Scholar]
- 14.Alfonso JL, Pereperez SB, Canoves JM, Martinez MM, Martinez IM, Martin-Moreno JM. Are we really seeing the total costs of surgical site infections? A Spanish study Wound Repair Regen. 2007 doi: 10.1111/j.1524-475X.2007.00254.x. [DOI] [PubMed] [Google Scholar]
- 15.Sanders FRK, Birnie MF, Dingemans SA, van den Bekerom MPJ, Parkkinen M, van Veen RN, et al. Functional outcome of routine versus on-demand removal of the syndesmotic screw: a multicentre randomized controlled trial. Bone Joint J. 2021 Nov;103-B(11):1709–16. DOI: 10.1302/0301-620X.103B11.BJJ-2021-0348.R2 [DOI] [PMC free article] [PubMed]
- 16.Dingemans SA, Birnie MFN, Sanders FRK, Van Den Bekerom MPJ, Backes M, Van Beeck E, et al. Routine versus on demand removal of the syndesmotic screw; A protocol for an international randomised controlled trial (RODEO-trial). BMC Musculoskelet Disord. 2018;19(1). DOI: 10.11.86/s12891–018–1946–5. [DOI] [PMC free article] [PubMed]
- 17.Versteegh M, M. Vermeulen K, M. A. A. Evers S, de Wit GA, Prenger R, A. Stolk E. Dutch Tariff for the Five-Level Version of EQ-5D. Value Heal. 2016; DOI: 10.1016/j.jval.2016.01.003 [DOI] [PubMed]
- 18.Hakkaart-van Roijen L, van der Linden N, Bouwmans C, Kanters T, Swan Tan S. Kostenhandleiding: Methodologie van kostenonderzoek en referentieprijzen voor economische evaluaties in de gezondheidszorg. Zorginstituut Ned. 2016;Sep 8th:1–84.
- 19.Consumer Price Index 2018 [Internet]. [cited 2020 Sep 5]. https://www.cbs.nl/
- 20.DBC-Zorgproducten [Internet]. [cited 2020 Sep 5]. https://www.opendisdata.nl/msz/zorgproduct
- 21.Brand J, van Buuren S, le Cessie S, van den Hout W. Combining multiple imputation and bootstrap in the analysis of cost-effectiveness trial data. Stat Med. 2019 doi: 10.1002/sim.7956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Van Gils PF, Schoemaker CG, Polder JJ. Hoeveel mag een gewonnen levensjaar kosten? Onderzoek naar de waardering van de QALY. Ned Tijdschr Geneeskd. 2014; [PubMed]
- 23.Neary KC, Mormino MA, Wang H. Suture button fixation versus syndesmotic screws in supination-external rotation type 4 injuries. Am J Sports Med. 2017 doi: 10.1177/0363546516664713. [DOI] [PubMed] [Google Scholar]
- 24.Weber AC, Hull MG, Johnson AJ, Henn RF. Cost analysis of ankle syndesmosis internal fixation. J Clin Orthop Trauma. 2019 doi: 10.1016/j.jcot.2017.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ramsey DC, Friess DM. Cost-effectiveness analysis of syndesmotic screw versus suture button fixation in tibiofibular syndesmotic injuries. J Orthop Trauma. 2018 doi: 10.1097/BOT.0000000000001150. [DOI] [PubMed] [Google Scholar]
- 26.Willmott HJS, Singh B, David LA. Outcome and complications of treatment of ankle diastasis with tightrope fixation. Injury. 2009 doi: 10.1016/j.injury.2009.05.008. [DOI] [PubMed] [Google Scholar]
- 27.Rigby RB, Cottom JM. Does the arthrex tightrope® provide maintenance of the distal tibiofibular syndesmosis? A 2-year follow-up of 64 tightropes® in 37 patients. J Foot Ankle Surg. 2013 doi: 10.1053/j.jfas.2013.04.013. [DOI] [PubMed] [Google Scholar]
- 28.Storey P, Gadd RJ, Blundell C, Davies MB. Complications of suture button ankle syndesmosis stabilization with modifications of surgical technique. Foot Ankle Int. 2012 doi: 10.3113/FAI.2012.0717. [DOI] [PubMed] [Google Scholar]
- 29.Fantry AJ, O’Donnell SW, Born CT, Hayda RA. Deep infections after syndesmotic fixation with a suture button device. Orthopedics. 2017 doi: 10.3928/01477447-20161229-02. [DOI] [PubMed] [Google Scholar]
- 30.Sugi MT, Ortega B, Shepherd L, Zalavras C. Syndesmotic Screw Removal in a Clinic Setting Is Safe and Cost-effective. Foot Ankle Spec. 2020 doi: 10.1177/1938640019843321. [DOI] [PubMed] [Google Scholar]
- 31.Penning D, Birnie MF, Sanders FR, de Ruiter KJ, Schepers T. Syndesmotic screw: Where does it break? J Foot Ankle Surg (Asia Pacific). 2021 doi: 10.5005/jp-journals-10040-1184. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data availability
The datasets analyzed during the current work are available upon reasonable request from the corresponding author.
The datasets analyzed during the current work are available upon reasonable request from the corresponding author.