Abstract
Purpose
First time examination of the physical and psychological long-term outcome following traumatic hemipelvectomy.
Methodology
In this study, all patients suffering from traumatic hemipelvectomy that were treated in a level-A trauma center since 1988 were retrospectively evaluated. The authors aimed to compare the physical and psychological outcome following primary amputation (A) vs. limb-preservation (LP) procedures. The patients were examined with a focus on pain, function, mobility and general health. As part of this examination, various scores were recorded, i.e., Majeed Score, Time up & Go or SF-36.
Results
The following work showed 13 patients who had suffered a traumatic hemipelvectomy, 8 of whom survived. Five of these were available for subsequent clinical re-examination; of these, three patients underwent an amputation, while limb preservation was performed on two patients. Mean follow-up of the amputee group was after 12 years compared to 6.5 years following limb preservation. After limb preservation, both patients reported phantom limb pain at the affected leg, despite pain medication. The general state of health was assessed as 82/100 (A) and 45/100 (LP). The Majeed score was 61 (A) vs. 45 (LP). In the clinical examination, three out of five patients (2 LP, 1 A) showed peroneal palsy (PP). In the quality-of-life analysis based on the SF12/36 and the NHP, amputees scored higher than the patients who underwent limb preservation surgery.
Conclusion
In our small patient cohort, satisfaction, pain and mobility tend to be better following primary amputation compared to limb preserving surgery.
Keywords: Traumatic hemipelvectomy, Amputation, Pelvic ring fracture, Quality of life
Introduction
Traumatic hemipelvectomy (THP) is a rare injury to the pelvis, accounting for only 0.6% of all pelvic fractures [9, 32, 34, 42]. The first case of traumatic hemipelvectomy was reported by Turnbull in 1978 [4, 6, 21, 30]. This specific injury is defined as the combination of an anterior pelvic ring fracture/transsymphyseal disruption and an iliosacral fracture on one or both sides, with avulsion of the external iliac vessels and severe stretch injury or disruption of the femoral and sciatic nerves [17, 32, 34, 42]. There were a few authors who subdivided this injury as complete or partial THP dependent on if the lower extremity was still attached to the trunk or not [16, 43]. In this study, both complete and partial THP were included. The most common accidental mechanisms causing traumatic hemipelvectomy include trauma from car and motorcycle crashes, as well as falls from great heights [6, 10]. Most patients with THP sustain multiple injuries [26, 28, 32]. The fatality rate of THP is approximately 60% with lethal hemorrhage being the main reason [15, 16, 19, 26, 35, 42, 44, 46].
In 1989, Beal et al. described THP in a larger patient cohort for the first time. During a three-year period, eight patients sustained a traumatic hemipelvectomy, of whom three survived [1]. Current literature -to our knowledge- reports additional 140 cases, of which a few have been analyzed in larger collectives with sample sizes maximum high as 21 patients [9, 16, 32, 44, 45]. None of these studies reported long-term Quality of Life (QoL) and functional outcomes. Table 1 summarizes the results of studies reporting cohorts > 3 patients. As there is still a lack of information about the functional long-term outcomes and the overall QoL following THP [1, 9, 16, 32, 45].
Table 1.
Published case series that include more than 3 patients
| Author/year | N | Sex | Outcome | Age | Side | QoL |
|---|---|---|---|---|---|---|
| Beal et al. [1] | 8 | N/A | 3 survived | N/A | N/A | N/A |
| Pohlemann et al. [32, 34] | 11 | 11 M | 4 survived | 21.2 | 6L,5R | N/A |
| Wu et al. [45] | 4 | 3F 1 M | 4 survived | 32 | 2L,2R | N/A |
| D’Alleyrand et al. [9] | 13 | 13 M | 12 survived | 25 | 6L,7R | N/A |
| Yu He [16] | 21 | 8 F 13 M | 17 survived | 31.3 | N/A | N/A |
M male, F female, L left, R right, N/A not available
Materials and methods
A retrospective analysis of all patients with pelvic fractures, that were treated in a level-one trauma center since 1988, was performed. All patients that met the definition of a traumatic hemipelvectomy were selected for evaluation.
The analysis includes demographic data, mechanism of the injury, vital parameters, the Glasgow Coma Scale (GCS) and laboratory parameters at arrival in emergency room, microbiological contamination of the wound and the clinical course.
At a follow-up visit of patients that had survived the long-term functional outcomes, current intake of pain medication and QoL were analyzed.
Functional outcome at follow-up
To evaluate the functional long-term outcome, follow-up examinations were organized, including standardized scores, as: Timed Up and Go Test (TUG-T), Majeed Score, Merle D’Aubigne Score (MDA Score) and Harris Hip Score (HHS).
The range of motion of the large lower joints was examined using the neutral-zero method. Muscle strength was examined according to Janda [8, 14, 20, 29, 40].
Quality of Life at follow-up
The health-related quality of life and the psychosocial conditions were analyzed using the 36/12-Item Short-Form Health Survey (SF-36/SF-12) measuring with following eight scales: physical functioning (PF), role physical (RP), bodily pain (BP), general health (GH), vitality (VT), social functioning (SF), role emotional (RE), and mental health (MH) a physical dimension, represented by the Physical Component Summary (PCS), and a mental dimension, represented by the Mental Component Summary (MCS) [5, 24]. The Nottingham Health Profile (NHP) measured six further dimensions, such as energy, sleep, pain, emotional reactions, social isolation, and physical mobility [1, 24]. Data were evaluated according to the instructions given by Bullinger and Kirchberger [5].
Statistical analysis
Collected data were managed with Microsoft Excel for Mac 2011 (version 14.1.0, Microsoft, Redmond, Washington, US), and, after further processing, analyzed with the statistics program IBM SPSS® Statistics® (version 21, IBM, Armonk, New York, US). However, no statistical analysis was included into this manuscript due to the small patient sample.
Results
From the pelvic ring fractures treated in a level-A trauma center between 1988 and 2019, 13 patients suffered from THP of whom eight patients survived and five patients died. Detailed medical information of patients are summarized in Table 2. Main reasons for THP were motorcycle accidents (5/13).
Table 2.
Detailed patient information
| Patient | Year of accident | Age | Sex | Side | Outcome | Hip stabilization | GCS | Accident mechanism | Vital parameters (HF + RR) | LA | T(°C) | Hb (mg/dl) | Aptt (sec.) | pH | PBC |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 1988 | 50 | M | R | Died | Hemipelvectomy | 3 | Overrolling |
100 bpm 60/40 |
N/A | N/A | 3.9 | N/A | 7 | 60 |
| 2 | 1991 | 3 | M | R | Survived | Hemipelvectomy | N/A | Overrolling |
90 bpm 100/75 |
1.4 | 37 | 6.6 | 52 | 7.53 | 20 |
| 3 | 1992 | 6 | M | R | Survived | Hemipelvectomy | 14 | Overrolling |
90 bpm 80/50 |
N/A | 36,6 | 12 | 53 | 7.46 | 60 |
| 4 | 1997 | 39 | M | R | Died | External fixator + Plate osteosynthesis | N/A | Trapped |
110 bpm 80/60 |
86 | 36,6 | 12,8 | 30,5 | 7.12 | 84 |
| 5 | 1997 | 47 | M | L | Died | Plate osteosynthesis | 6 | Burial |
120 bpm 60/40 |
18.7 | 36,7 | 15 | N/A | 7.23 | 72 |
| 6 | 1998 | 35 | M | L | Died | External fixator | 3 | Suicide |
120 bpm 85/65 |
N/A | 37 | 10.6 | 200 | 7.34 | 32 |
| 7 | 2000 | 25 | M | L | Died | Plate osteosynthesis | 14 | Motorcycle accident |
90 bpm 75/35 |
3.9 | 37 | 8.7 | N/A | 7.3 | 120 |
| 8 | 1988 | 38 | M | L | Survived | Plate osteosynthesis | 3 | Motorcycle accident |
100 bpm 100/70 |
N/A | 37.1 | 10.7 | 51 | 7.24 | 115 |
| 9 | 1995 | 44 | M | R | Survived | Plate osteosynthesis | 14 | Traffic accident |
120 bpm 60/35 |
7.2 | 37 | 3.1 | N/A | 7.3 | 80 |
| 10 | 2007 | 18 | M | R | Survived | Plate osteosynthesis | 15 | Motorcycle accident |
90 bpm 90/60 |
0,7 | 36.5 | 6,5 | 49 | 7.3 | 50 |
| 11 | 2012 | 21 | M | R | Survived | Hemipelvectomy | 15 | Motorcycle accident |
135 bpm 75/45 |
3.3 | 35,9 | 12,4 | 30 | 7.15 | 64 |
| 12 | 2013 | 56 | M | R | Survived | Hemipelvectomy | 5 | Explosionstrauma |
90 bpm 80/50 |
6.1 | 37 | 5,7 | 97 | 7.2 | 68 |
| 13 | 2013 | 50 | W | R | Survived | External fixator | 5 | Motorcycle accident |
100 bpm 60/40 |
10.1 | 37 | 4,6 | 128 | 7.14 | 79 |
Vital parameters and blood sample results are the first values at the emergency room
Time the values were all determined from the venous blood by means of blood gas analysis (BGA) in the emergency room
m male, f female, R right, L left, GCS Glasgow coma scale, LA lactat, T temperature, Hb Hemoglobin, apt activated Partial Thromboplastin, PBC packed blood cells, N/A not available
In five of thirteen patients’ treatment included surgically completion of the traumatic hemipelvectomy resulting in amputation of the affected leg for primary life rescue. Three patients were treated with external fixator; five patients received a plate osteosynthesis. In three cases, control of bleeding was the main reason for amputation. Two patients received a hemipelvectomy because of septical complications.
The most common accompanying injuries were anorectal and urogenital injuries (11/13). Microbiological swabs of the wounds detected gastrointestinal pathogens such as enterococci and enterobacteriacae. Ten patients suffered from septic complications during the following clinical course.
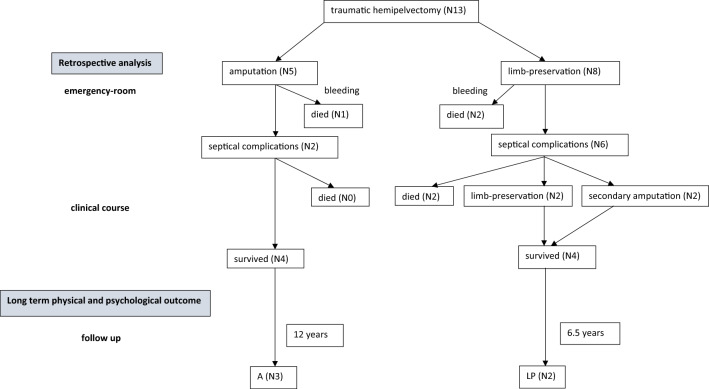
After primary hemipelvectomy all patients suffered septic complications (Table 3). Due to septic complications, a secondary hemipelvectomy had to be performed on two patients following initial limb salvage, both survived. In the group of the limb-preservation four patients had septic complications, two of them died following septic shock (Fig. 1).
Table 3.
List of secondary injuries, the pathogenic germ, septical complications and outcome
| Patient | Secondary injuries | Pathogen spectrum | Reason for THP | Complications | Outcome |
|---|---|---|---|---|---|
| 1 | Amputation of the testicle, haematothorax | Enterococcus, Enterobacter, Xanthomonas | Bleedingcontroll | Septical | Died |
| 2 | Rupture of the bladder and the anal channel | N/A | Bleedingcontroll | Septical | Survived |
| 3 | Perineum- rupture, fracture of the femur | N/A | Bleedingcontroll | Septical | Survived |
| 4 | Disruption of the ureter and the rectum, fracture of the femur | Enterobacter, Enterococcus | Septical | Died | |
| 5 | Rupture of the bladder, hämatothorax | N/A | N/A | Died | |
| 6 | Rupture of the rectum, hämatothorax, fracture of the femur | N/A | Septical | Died | |
| 7 | Rupture of the rectum, disruption of the ureter | N/A | Septical | Died | |
| 8 | Disruption of the rectum and bladder | Bacillus cereus, Enterococcus faecalis | Septical | Survived | |
| 9 | Fracture of the femur, trauma of the liver vena cava disruption | E. coli, Enterococcus faecalis, Pseudomonas | Septical | Survived | |
| 10 | Disruption of the small intestine, rupture of the bladder | Enterococcus faecalis, Enterobacter, E. coli, Morganella morganii | N/A | Survived | |
| 11 | Disruption of the ureter, psoas-Abscess, disruption of the plexus iliosacralis, laceration of the liver and the kidney | Enterobacter faecalis, Staph aureus, Achromobacter, Candida albicans | Septical complications | Septical | Survived |
| 12 | Rupture of vena and arteria iliaca, fracture of the radius | Enterococcus faecalis | Septical complications | Septical | Survived |
| 13 | Rupture of the bladder, arterial bleeding of the arteria iliaca interna, morel-Lavallée-Lesion | E. coli, Enterococcus, Candida albicans | Survived | N/A | Survived |
N/A not available
Fig. 1.
Identified patients suffering from traumatic hemipelvectomy; A amputated, LP limb-preservation
Long-term functional outcome
Five out of 13 patients were available for the follow-up visit on average 11.8 years after the accident. Two patients were treated without amputation (LP) whereas three patient’s emergency surgery included amputation of the affected leg (A). Mean follow-up in the group A was 12 years, in the group LP 6.5 years after traumatic hemipelvectomy.
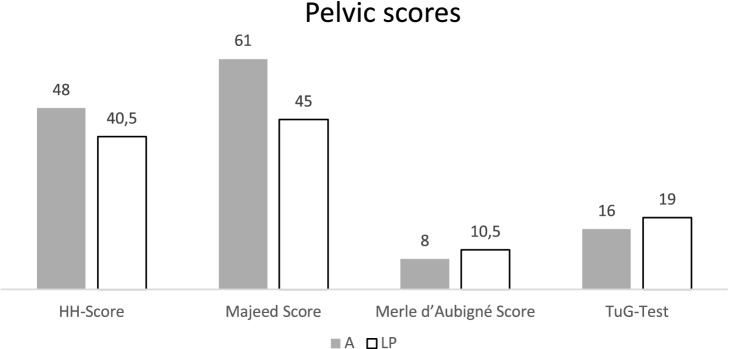
Pelvic scores
The evaluation of the collected data showed with (A: 48; LP: 40) on average poor results in the Harris Hip Score for both groups [14]. Evaluation of the Merle d'Aubigne score showed a moderate result for group LP (10.5) and a poor result for group A (8) [8]. The Majeed score was unsatisfactory for group LP (45) and satisfactory for group A (60) [29]. The results of the Timed Up and Go Test (TUG-T) are, on average, 16 s (A) and 19 s (LP), which should be rated as a minor mobility restriction without relevance for daily living in both groups [40]. The results of the pelvic scores were balanced in both groups. The Results are shown in Fig. 2.
Fig. 2.
Results of the Pelvic scores; A amputated, LP limb-preservation
The daily pain medication intake and their substance class (opioids/non-opioids) were also analyzed. No patient in group A was taking opioids. In group LP, both patients took opioid analgesics daily.
Non-opioid analgesics were taken as concomitant medication in both patients in group LP. In group A, one patient regularly took nonsteroidal anti-inflammatory drugs (NSAID) for pre-existing headaches. Two amputated patients frequently used a wheelchair. One limp preservation and the third amputated patient were able to walk with crutches. One patient after limp preservation needed an ankle foot orthosis (AFO) to walk (Table 4).
Table 4.
Medical devices
| Medical device | Wheelchair | Crutches | Ankle foot orthosis |
|---|---|---|---|
| A (N3) | 2 | 1 | |
| LP (N2) | 1 | 1 |
A amputated, LP limb-preservation
Clinical examination
Muscle strength at the big muscle groups in hip and knee joint and in the upper ankle joint (UAJ) was balanced in both groups, the different values are summarized in Table 5.
Table 5.
Muscle strength according to Janda of the knee joint, hip joint, upper ankle joint (UAJ), lower ankle joint (LAJ)
| Hip joint | Flexion | Extension | Internal rotation | External rotation |
|---|---|---|---|---|
| A (N3) | 5/5 | 5/5 | 5/5 | 5/5 |
| LP (N2) | 5/5 | 4/5 | 4/5 | 5/5 |
| Knee joint | ||||
| A (N3) | 5/5 | 5/5 | 5/5 | 5/5 |
| LP(N2) | 4.5/5 | 4.5/5 | 4.5/5 | 4.5/5 |
| LPa | 4.5/5 | 5/5 | ||
| UAJ | Dorsalextension | Plantarflexion | LAJ | Supination | Pronation |
|---|---|---|---|---|---|
| A (N3) | 3/5 | 4/5 | 4/5 | 3.5/5 | |
| LP (N2) | 1/5 | 2/5 | 3/5 | 1/5 | |
| LPa | 1/5 | 2/5 | 3/5 | 1/5 |
A amputated, LP limb-preservation
aContralateral side
Range of motion (neutral-zero-method) of neighbored joints
See Table 6.
Table 6.
Range of Motion indicated by the neutral zero of the upper ankle joint (UAJ), lower ankle joint (LAJ)
| Hip joint (°) | Flexion | Extension | Internal rotation | External rotation |
|---|---|---|---|---|
| A (N3) | 133.3 | 8.33 | 35 | 38.33 |
| LP (N2) | 125 | 5 | 40 | 45 |
| Knee joint (°) | ||||
| A (N3) | 120 | 3.33 | 16.67 | 20 |
| LP (N2) | 120 | 5 | 10 | 20 |
| LPa | 120 | 7.50 | 5 | 20 |
| UAJ (°) | Dorsalextension | Plantarflexion | LAJ (°) | Supination | Pronation |
|---|---|---|---|---|---|
| A (N3) | 10 | 40 | 40 | 3.33 | |
| LP (N2) | 0 | 45 | 35 | 0 | |
| LPa | 5 | 45 | 35 | 0 |
A amputated, LP limb-preservation
aContralateral side
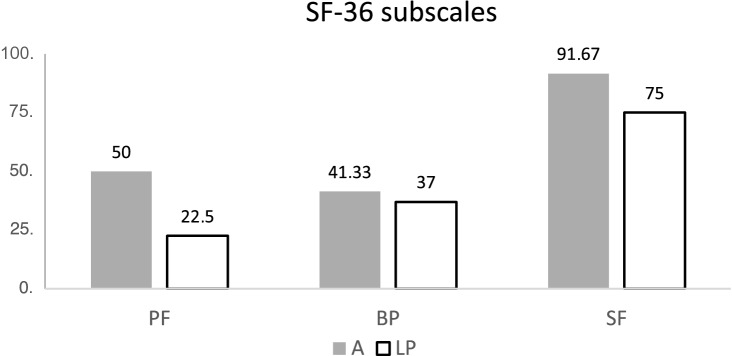
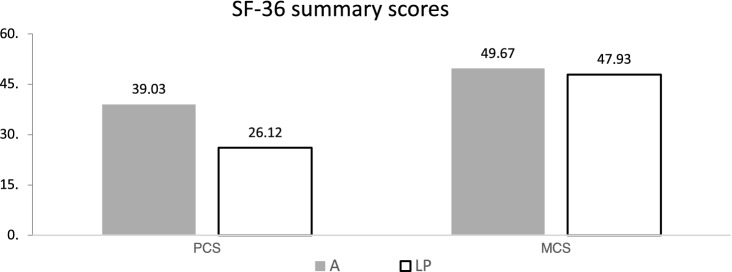
Long-term outcome of QoL
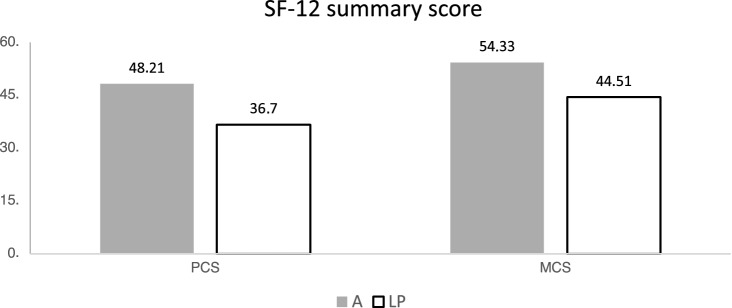
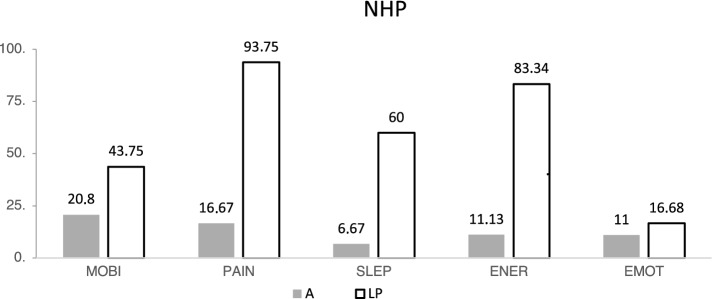
The analysis of the SF-12/36 demonstrated that the patients who underwent amputation were able to achieve higher values in all recorded sub-areas. Not only did they rate their physical resilience or their social functioning higher, at the same, time they also reported less pain and greater emotional satisfaction. Accordingly, the aggregated total scores (KSK and PSK) of group A were higher than in the LP group (Figs. 3, 4, 5).
Fig. 3.
Results of the SF 36 subscales physical functioning (PF), bodily pain (BP) and social functioning (SF); A amputated, LP limb-preservation
Fig. 4.
Results of the SF 36 summary scores Mental Component Summary (MCS), Physical Component Summary (PCS); A amputated, LP limb-preservation
Fig. 5.
Results of the SF 12 summary scores Mental (MCS) and Physical Component Summary scores (PCS); A amputated, LP limb-preservation
The analysis of the NHP- results revealed differences (Fig. 6), for less pain, a higher sleep quality and general energy level after amputation in the context of a THP.
Fig. 6.
NHP: Results of mobility (MOBI); pain (PAIN); sleep (SLEP); Energy (ENER); Emotion (EMOT) A amputated, LP limb-preservation
Discussion
The existing literature reports the results of case reports and small patient cohorts primarily targeting the survival-rate after traumatic hemipelvectomy, wound healing and related pain following traumatic hemipelvectomy [31, 46]. Here in total, the authors were able to examine long-term outcomes on functional outcome and QoL of five out of 13 patients after traumatic hemipelvectomy and following limb salvage (N2) or amputation (N3).
Functional outcome
The results of specific hip and pelvic scores were comparable in both groups. The mean Merle d’Aubigne score was better within the LP group. With 10.5 points, the value can nevertheless be assessed as “moderate” [8]. The Majeed Score, Harris Hip Score and the Timed Up and Go Test (TUG-T) results of group A were better than in the LP group [2, 14, 29].
The range of motion and muscle strength measurements for the hip and knee joints and the upper ankle joint revealed no differences in either group. Within the LP and A group abnormal results for ROM of the ankle joint can be related to co-existing peroneal palsy of the contralateral leg (A) and the affected leg (LP) (Table 5) [20, 41]. In the LP group, both patients suffered drop foot due to accident-related peroneal palsy.
Furthermore, the follow-up examination demonstrated that after amputation, the daily mobility seems less restricted according to the results of TUG test [2]. In comparison, the achieved mobility following amputation is satisfactory when comparing these results on functional outcomes to hemipelvectomy outcomes for tumor resection [3, 36]. Even though more nerves and vessels injuries at the pelvis following traumatic hemipelvectomy compared to tumor resections.
Despite daily intake of opioid medication, the reported pain at the pelvic area and the foot could not be controlled sufficiently for the LP subjects. Surprisingly, expecting phantom limb pain, none of the amputees take daily pain medication.
QoL
Reference groups from the manual by Bullinger and Kirchberger can be used to compare the quality of life of the analyzed two groups to each other and to further musculoskeletal diseases and degenerative diseases as arthritis [5]. In the majority of the analyzed sub-areas of the SF-36 test, the values of the A group were better. The social function (SF) after traumatic hemipelvectomy were higher (91) than patients with musculoskeletal diseases (61) and patients with arthritis (75). In contrast, group LP lags far behind the comparison populations in all categories (75). The group A had less pain (41) compared to the LP (37) and the patients with musculoskeletal diseases (30).
The results for physical function (PF) of group A (50) were superior to the group LP (22) and were similar to the control group of musculoskeletal diseases (51).
Like the SF-36, the results in the SF-12 on both the physical and psychological total scales for group LP are inferior compared to group A and the control groups. The NHP was used and evaluated as an additional screening tool. The Nottingham Health Profile (NHP), together with the SF-36, is one of the standard international instruments for recording quality-of-life [1, 24].
SF-12 results are in concordance with the prior assessed a higher quality of life in the SF-36 for the A group. The individual analysis revealed differences between the two groups in three dimensions. The sleep quality, the general energy level and the level of pain were also better after amputation.
Of clinical interest is the question of post-THP pain [19]. The study found less pain after primary amputation following THP. Despite taking pain medication containing opioids, the LP group reported more frequent and more severe pain than the A group. Pain as long-term sequelae was more common in the group of non-amputee patients, even though a daily intake of opioids. All herein performed statements need to be critically reviewed due to the small cohort. However, in this patient, cohort QoL was better after amputation compared to limb preservation following traumatic hemipelvectomy. Especially the assessment of the patient's subjective QoL will continue to be a very important parameter when assessing the overall outcome [11, 13, 32] and revealed interesting results in this study.
Furthermore, developments in modern prosthetics, socket technologies and assistive devices might allow wider possibilities for those patients regarding pain free mobility and related QoL even in very proximal amputation levels than in the past [18, 37].
The decision on whether to perform a (delayed) primary amputation following THP or not is a very difficult one to make. In contrast to open fractures of the legs there are no scores. But the scores available can possibly help in the decision-making process in traumatic hemipelvectomies. Reconstruction is always the primary aim in trauma surgery, with amputation reserved for exceptional cases as traumatic hemipelvectomy might belong to as nerve and vessels in the pelvis are major injured. In severe open fractures of the leg, there is no difference in outcome between primary and delayed primary amputation, but the prognosis is noticeably worse for secondary than for primary amputations especially regarding development of chronic pain and social consequences related to the high number of revision surgeries during limb salvage and chronification of pain [12].
Once a traumatic hemipelvectomy has been diagnosed, surgical completion could ensure the survival of patients and could presumably cause fewer septic complications. Long-term quality of life after amputation also appears to be good [22, 25, 27, 35, 38]. In conclusion to this study, the authors share this approach to traumatic hemipelvectomies and rely on the presented results pointing out a tendency to a superior functional and mental situation after amputation compared to limb preservation. However, as to the small patient cohort only, deriving any recommendations for treatment of course is difficult. A multicentric study or a metaanalytical view of the work of recent decades could improve validity, power and thus the basis for decision-making.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Declarations
Conflict of interest
The authors declare that they do not have any conflict of interest.
Ethical approval
The questionnaires and methodology for this study was approved by the local ethic committee (10039_B0_K_2021).
Consent to participate and consent to publish
Informed consent was obtained from all individual participants included in the study. The participants has consented to the submission of the study to the journal.
References
- 1.Beal SL, Blaisdell FW. Traumatic hemipelvectomy: a catastrophic injury. J Trauma. 1989;29:1346–1351. [PubMed] [Google Scholar]
- 2.Beauchet O, et al. Timed Up and Go test and risk of falls in older adults: a systematic review. J Nutr Health Aging. 2011;15:933–938. doi: 10.1007/s12603-011-0062-0. [DOI] [PubMed] [Google Scholar]
- 3.Beck LA, Einertson MJ, Winemiller MH, DePompolo RW, Hoppe KM. Functional outcomes and quality of life after tumor-related hemipelvectomy. Sim FF Phys Ther. 2008;88(8):916–927. doi: 10.2522/ptj.20070184. [DOI] [PubMed] [Google Scholar]
- 4.Bosch U, Pohlemann T, Tscherne H. Strategie bei der Versorgung von Beckenverletzungen. Orthopäde. 1992;21:385–392. [PubMed] [Google Scholar]
- 5.Bullinger M, Kirchbergerger I. SF-36 Fragebogen zum Gesundheitszustand Handanweisung 2. ergänzte und überarbeitete. Göttingen: Hogrefe Verlag; 2011. [Google Scholar]
- 6.Burgess A, Eastridge B, Young J, Ellison T, Ellison P, Poka A. Pelvic ring disruption: effective classification systems and treatment protocols. J Trauma. 1990;30(7):848–856. [PubMed] [Google Scholar]
- 7.Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 8.Coste F, Merle D, Aubigne R, Postel M. Functional Results of hip arthroplasty with acrylic prosthesis. Presse Med. 1965;73:263–267. [Google Scholar]
- 9.D’Alleyrand JC, Lewandowski LR, Forsberg JA, Gordon WT, Fleming ME, Mullis BH, Andersen RC, Potter BK. Combat-related hemipelvectomy: 14 cases, a review of the literature and lesson learned. J Orthop Trauma. 2015;29(12):e493–e498. doi: 10.1097/BOT.0000000000000398. [DOI] [PubMed] [Google Scholar]
- 10.Danisi FJ, Stromberg BV. Traumatic hemipelvectomy. Plast Reconstr Surg. 1985;76:945–947. doi: 10.1097/00006534-198512000-00030. [DOI] [PubMed] [Google Scholar]
- 11.Ebrahimzadeh MH, Kachooei AR, Soroush MR, Hasankhani EG, Razi S, Birjandinejad A. Long-term clinical outcomes of war-related hip disarticulation and trans- pelvic amputation. J Bone Joint Surg Am. 2013;95(16):e114(1-6). doi: 10.2106/JBJS.L.01160. [DOI] [PubMed] [Google Scholar]
- 12.Farina D, Vujaklija I, Brånemark R, Bull AM, Dietl H, Graimann B, Aszmann OC. Toward higher-performance bionic limbs for wider clinical use. Nat Biomed Eng. 2021 doi: 10.1038/s41551-021-00732-x. [DOI] [PubMed] [Google Scholar]
- 13.Findler M, Cantor J, Haddad L, Gordon W, Ashman T. The reliability and validity of the SF-36 health survey questionnaire for use with individuals with traumatic brain injury. Brain Inj. 2001;15(8):715–723. doi: 10.1080/02699050010013941. [DOI] [PubMed] [Google Scholar]
- 14.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fracture: treatment by mold arthroplasty. J Bone Jt Surg. 1969;51:737–755. [PubMed] [Google Scholar]
- 15.Hauschild O, Strohm PC, Culemann U, et al. Mortality in patients with pelvic fractures: results from the German pelvic injury register. J Trauma. 2008;64:449–455. doi: 10.1097/TA.0b013e31815982b1. [DOI] [PubMed] [Google Scholar]
- 16.He Y, Qiu D, Zhou D, Li L, Wang B, Wang L. Treatment of partial traumatic hemipelvectomy a study of 21 Cases. J Bone Jt Surg Am. 2019;101(9):e36. doi: 10.2106/JBJS.18.00877. [DOI] [PubMed] [Google Scholar]
- 17.Hofmann GO, Gonschorek O, Bühren V. Indikationen zur primären Amputation bei Unterschenkelfraktur. Trauma und Berufskrankheit. 2001;3(2):S110–S116. [Google Scholar]
- 18.Houdek MT, Andrews K, Kralovec ME, Kotajarvi B, Smither FC, Shives T, Sim FH. Functional outcome measures of patients following hemipelvectomy. Prosthet Orthot Int. 2016;40(5):566–572. doi: 10.1177/0309364615574164. [DOI] [PubMed] [Google Scholar]
- 19.Jahn R, Heinrich P. Die traumatische Hemipelvektomie. Zentralbl Chir. 1990;115:631–634. [PubMed] [Google Scholar]
- 20.Janda V (2000) Manuelle Muskelfunktionsdiagnostik. München: Urban & Fischer. 4., überarb. und erw. Aufl
- 21.Kayalar M, Gurbuz Y, Sugun TS, Kaplan I. Traumatic hemipelvectomy: case presentation. Acta Orthop Traumatol Turc. 2014;48:226–230. doi: 10.3944/AOTT.2014.2629. [DOI] [PubMed] [Google Scholar]
- 22.Klevsgård R, et al. Nottingham Health Profile and Short-Form 36 Health Survey questionnaires in patients with chronic lower limb ischemia: before and after revascularization. J Vasc Surg. 2002;36(2):310–317. doi: 10.1067/mva.2002.125747. [DOI] [PubMed] [Google Scholar]
- 23.Klingman RR, Smith P, Stromberg B, Valentine J, Goebel M. Traumatic hemipelvectomy. Ann Plast Surg. 1991;27(2):156–163. doi: 10.1097/00000637-199108000-00011. [DOI] [PubMed] [Google Scholar]
- 24.Kohlmann T, Bullinger M, Kirchberger-Blumstein I. Die deutsche Version des Nottingham Health Profile (NHP): Übersetzungsmethodik und psychometrische Validierung. Soz Präventivmed. 1997;42:175–185. doi: 10.1007/BF01300568. [DOI] [PubMed] [Google Scholar]
- 25.Kurth BM, Ellert U. The SF-36 questionnaire and its usefulness in population studies: results of the German Health Interview and Examination Survey 1998. Soz-Präventivmed. 2002;47:266–277. doi: 10.1007/BF01326408. [DOI] [PubMed] [Google Scholar]
- 26.Labler L, Trentz O, Keel M. Traumatic hemipelvectomy. Eur J Trauma. 2005;31:543–550. [Google Scholar]
- 27.Lier H, et al. Coagulation management in multiple trauma: a systematic review. Intensive Care Med. 2011;37(4):572–582. doi: 10.1007/s00134-011-2139-y. [DOI] [PubMed] [Google Scholar]
- 28.Losch A, Stankovicˇ P, Stürmer KM. Traumatic hemipelvectomy and quality of life—report on 2 cases 18 years after the accident. Die Unfallchirurgie. 2001;104(1):91–94. doi: 10.1007/s001130050695. [DOI] [PubMed] [Google Scholar]
- 29.Majeed SA. Grading the outcome of pelvic fractures. J Bone Joint Surg Br. 1989;71(2):304–306. doi: 10.1302/0301-620X.71B2.2925751. [DOI] [PubMed] [Google Scholar]
- 30.Moore WM, Brown JJ, Haynes J-L, et al. Traumatic hemipelvectomy. J Trauma. 1987;27(5):570–572. doi: 10.1097/00005373-198705000-00020. [DOI] [PubMed] [Google Scholar]
- 31.Olivares PR, Gusi N, Prieto J, Hernandez-Mocholi M. Fitness and health-related quality of life dimensions in community-dwelling middle aged and older adults. Health Qual Life Outcomes. 2011;22(9):117. doi: 10.1186/1477-7525-9-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pohlemann T, Paul Ch, Gänsslen A, Regel G, Tscherne H. Die traumatische Hemipelvektomie. Unfallchirurg. 1996;99:304–313. [PubMed] [Google Scholar]
- 33.Radoschewski M. Gesundheitsbezogene Lebensqualität – Konzepte und Maße. Entwicklungen und Stand im Überblick. Bundesgesundheitsbl - Gesundheitsforsch - Gesundheitsschutz. 2000;43:165–189. [Google Scholar]
- 34.Rieger H, Dietl K. Traumatic Hemipelvectomy: an update. J Trauma. 1998;45(2):422–426. doi: 10.1097/00005373-199808000-00045. [DOI] [PubMed] [Google Scholar]
- 35.Rommens PM, Hofmann A, Hessmann MH. Management of acute hemorrhage in pelvic trauma: an overview. Eur J Trauma Emerg Surg. 2010;36(2):91–99. doi: 10.1007/s00068-010-1061-x. [DOI] [PubMed] [Google Scholar]
- 36.Salunke AA, et al. Surgical management of pelvic bone sarcoma with internal hemipelvectomy: oncological and functional outcomes. J Clin Orthop Trauma. 2017;8(3):249–253. doi: 10.1016/j.jcot.2017.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sham AR, Spencer RF. Traumatic hemipelvectomy: a case report. South Afr J Surg. 1988;26(2):79–81. [PubMed] [Google Scholar]
- 38.Singh A, Gnanalingham K, Casey A, Crockard A. Quality of life assessment using the Short Form-12 (SF-12) questionnaire in patients with cervical spondylotic myelopathy: comparison with SF-36. Phila Pa 1976) 2006;31(6):639–643. doi: 10.1097/01.brs.0000202744.48633.44. [DOI] [PubMed] [Google Scholar]
- 39.Smith AC, et al. Traumatic hemipelvectomy with a contralateral unstable pelvis and acetabular fracture. JBJS Case Connector. 2017;7(3):e52. doi: 10.2106/JBJS.CC.16.00211. [DOI] [PubMed] [Google Scholar]
- 40.Steffen TM, Hacker TA, Mollinger L. Age- and gender-related test performance in community-dwelling elderly people: Six-Minute Walk Test, Berg Balance Scale, Timed Up & Go Test, and gait speeds. Phys Ther. 2002;82:128–137. doi: 10.1093/ptj/82.2.128. [DOI] [PubMed] [Google Scholar]
- 41.Stuby FM, Schäffler A, Hass T, König B, Stöckle U, Freude T. Insuffizienzfrakturen des Beckenrings. Unfallchirurg. 2013;116:351–366. doi: 10.1007/s00113-012-2349-y. [DOI] [PubMed] [Google Scholar]
- 42.Tscherne H, Pohlemann T, Gänsslen A. Classification, staging, urgency and indications in pelvic injuries. Zentralbl Chir. 2000;125:717–724. doi: 10.1055/s-2000-10662. [DOI] [PubMed] [Google Scholar]
- 43.Walcher F, Lustenberger T, Schmandra T, Byhahn C, Laurer H, Bingold T, Schweigkofler U, Winckler B, Walter G, Marzi I. First successful complete replantation of a traumatic hemipelvectomy: follow-up after 30 months. Injury. 2013;44(9):1252–1256. doi: 10.1016/j.injury.2012.09.025. [DOI] [PubMed] [Google Scholar]
- 44.Wang G, Zhou D, Shen WJ, Xin M, He J, Li Q, et al. Management of partial traumatic hemipelvectomy. Orthopedics. 2013;36:e1340–1345. doi: 10.3928/01477447-20131021-12. [DOI] [PubMed] [Google Scholar]
- 45.Wu, et al. Management of traumatic hemipelvectomy: an institutional experience on four consecutive cases. Scandinavian J Trauma Resuscit Emerg Med. 2013;21:64. doi: 10.1186/1757-7241-21-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yalniz E, Ciftdemir M, Durukan T. Traumatic hemipelvectomy: a case report and a review of the literature. Eur J Trauma Emerg Surg. 2007;33(3):306–309. doi: 10.1007/s00068-007-6063-3. [DOI] [PubMed] [Google Scholar]