Abstract
Angiogenesis, the formation of new blood vessels, is a complex and dynamic process regulated by various pro- and anti-angiogenic molecules, which plays a crucial role in tumor growth, invasion, and metastasis. With the advances in molecular and cellular biology, various biomolecules such as growth factors, chemokines, and adhesion factors involved in tumor angiogenesis has gradually been elucidated. Targeted therapeutic research based on these molecules has driven anti-angiogenic treatment to become a promising strategy in anti-tumor therapy. The most widely used anti-angiogenic agents include monoclonal antibodies and tyrosine kinase inhibitors (TKIs) targeting vascular endothelial growth factor (VEGF) pathway. However, the clinical benefit of this modality has still been limited due to several defects such as adverse events, acquired drug resistance, tumor recurrence, and lack of validated biomarkers, which impel further research on mechanisms of tumor angiogenesis, the development of multiple drugs and the combination therapy to figure out how to improve the therapeutic efficacy. Here, we broadly summarize various signaling pathways in tumor angiogenesis and discuss the development and current challenges of anti-angiogenic therapy. We also propose several new promising approaches to improve anti-angiogenic efficacy and provide a perspective for the development and research of anti-angiogenic therapy.
Subject terms: Tumour angiogenesis, Drug discovery
Introduction
Angiogenesis is a process in which new blood vessels develop from existing capillaries and eventually create a complete, regular, and mature vascular network. This process includes degradation of the basement membrane and activation, proliferation, and migration of the endothelial cells (ECs), which is regulated by various pro-angiogenic and anti-angiogenic factors.1 Under normal physiological conditions of healthy adults, endothelial cells are almost quiescent, and the frequency of mitosis is only 0.5%.2 Angiogenesis mainly occurs in embryonic development, tissue repair, the menstrual cycle, muscle growth, and organ lining regeneration through a regular (strictly controlled by the body), scope-limited (occurs locally), and short-lived (days, weeks, or months) mode.3,4 Nevertheless, angiogenesis will be disordered and excessive through the over-expression of pro-angiogenic factors and the inactivation of anti-angiogenic factors in several non-neoplastic angiogenic diseases like immune diseases (such as rheumatoid arthritis,5 psoriases,6 and Crohn’s disease),7 diabetic retinopathy (DR),8 age-related macular degeneration (AMD) and atherosclerosis.4,9 Angiogenesis also contributes to the progression of various malignant tumors such as melanoma, breast cancer (BC),10 colorectal cancer (CRC),11 non-small cell lung cancer (NSCLC),12 and renal cell carcinoma (RCC).13
The tumor is a biological tissue with rapid proliferation, vigorous metabolism, and tenacious vitality, which needs oxygen and nutrients far more than normal tissue cells. The initial stage of tumor growth is an avascular state, in which the tumor has not acquired aggressiveness and absorbs oxygen and nutrients through the diffusion of surrounding tissue.14 Therefore, tumor angiogenesis is locked or limited to a quiescent status owing to the low levels of pro-angiogenic factors and vascular inhibitory signals in the extracellular matrix, so intratumoral vascularization rarely occurs (Fig. 1).15 When the solid tumor grows to a volume of more than 1–2 mm3, the resources in the surrounding tissue are hard to maintain the tumor growth.16 A microenvironment with hypoxia, ischemia, acidosis, and high interstitial pressure is gradually developed in tumor tissue, which releases abundant growth factors and cytokines, stimulating angiogenesis and lymphangiogenesis to meet the needs of tumor growth and metabolism.16,17 Due to the rapid proliferation of tumor cells, a microenvironment with more severe hypoxia, acidosis, and high interstitial pressure originated in organizations far from the blood vessels in tumor tissue, promoting the enlargement and canceration of tumor tissue (Fig. 1). Afterwards it gradually evolves into a carcinoma, which acquires aggressiveness to induce the stromal response, including intratumoral angiogenesis, leukocyte infiltration, fibroblast proliferation, and extracellular matrix deposition, especially in cancerous tumors.18–20 Various pro-angiogenic factors are persistently released or up-regulated by tumor cells to activate endothelial cells, pericytes (PCs), tumor-associated fibroblasts (CAFs), endothelial progenitor cells (EPCs), and immune cells (ICs),21–23 subsequently causing telangiectasia, basement membrane destruction, extracellular matrix remodeling, pericytes shedding, endothelial cell differentiation to maintain a highly active stage of angiogenesis, eventually inducing tumor proliferation, diffusion, and metastasis.24 This phenomenon indirectly explains that tumors are called non-healing wounds.25 Furthermore, metabolic stress in tumors can also be aroused by immune stimulation, inflammatory response, oncogene mutation, and drug treatment to aggravate tumor angiogenesis and further promote tumor invasion and metastasis.26
Fig. 1.
The progression of the canceration through angiogenesis. The rapid expansion of tumor results in a reduction in the oxygen supply. The consequent hypoxic tumor microenvironment stimulates excessive angiogenesis via increasing various angiogenic pro-factors including VEGF, PDGF, FGF, and angiopoietin. Later, new blood vessels facilitate the transportation of oxygen and nutrients to further support the survival, growth and proliferation of tumor cells. When tumor cells develop a more aggressive phenotype, they continue to proliferate, spread and induce angiogenesis, with the invasion and metastasis of tumor cells into distant tissues through blood circulation
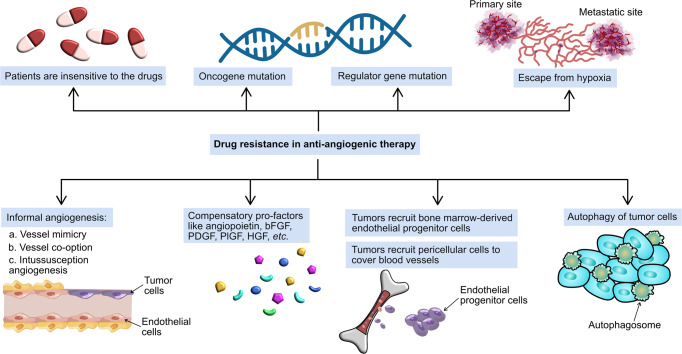
Up to now, although a significant number of research has been devoted to anti-cancer therapy to overcome this incurable and lethal disease, none of them has achieved persistent clinical efficacy.27,28 For example, chemotherapy is a form of systemic treatment, which has been utilized for the treatment of cancer for over 70 years and remains a cornerstone in the treatment of many types of cancers including BC, CRC, and NSCLC by directly killing or inhibiting the growth and reproduction of tumor cells under the administration of various cytotoxic agents such as cis-platinum, 5-fluorouracil, cyclophosphamide, methotrexate and doxorubicin.29,30 These cytotoxic chemotherapeutics have indiscriminating cell lethality, poor tissue selectivity, and severe systemic adverse effects, resulting in poor tolerance and prognosis of patients. Even so, tumor cells are not entirely killed, drug resistance rises unavoidably.31,32 Prior works have demonstrated that congenital and acquired drug resistance can be derived from tumor genetic and phenotypic mutations.33–36 Furthermore, cancerous tumors can escape into remote normal organizations through blood and lymphatic circulation to invalidate the drugs and worsen the condition of patients.37–40 As an emerging treatment, anti-angiogenic therapy fights cancer by normalizing tumor blood vessels, alleviating hypoxia of microenvironment, increasing tissue concentration of drugs, and limiting distant invasion and metastasis of tumors.41,42 Despite the ever-growing list of FDA-approved drugs, the clinical benefits of anti-angiogenic monotherapies are not long-lasting. Some limitations in chemotherapy like acquired drug resistance and tumor recurrence have also been found in anti-angiogenic therapy.43–46 The limited efficacy may be caused by compensatory angiogenesis induced by alternative pro-factors, vessel co-option and other abnormal modes. Hence, great efforts have been devoted to further improving the therapeutic efficacy and mitigating drug resistance. For example, a number of multi-targeted angiogenic inhibitors have been developed for cancer treatment. Additionally, the combination of angiogenic inhibitors with other conventional cancer treatment including chemotherapy, radiotherapy, immune therapy, adoptive cell therapy, and cancer vaccines has been evidently demonstrated through many pivotal clinical trials among patients with different types of cancer.47 With the in-depth exploration of the tumor angiogenesis and drug resistance, great progress has been made in anti-tumor therapy in recent years.
In the present review, we highlight the potent effects of angiogenesis in tumor growth, proliferation, carcinogenesis, invasion and metastasis, summarize multiple signaling pathways in tumor angiogenesis and outline the development of anti-angiogenic therapies, as well as classic anti-angiogenic drugs and some potential clinical candidates. Moreover, we discuss the challenges of anti-angiogenic treatment and some emerging therapeutic strategies to exploit the great advantages of anti-angiogenic therapy.
Pathophysiology
Blood circulation is a basis of cell metabolism, which flows in a closed circuit from the heart to arteries, capillaries, veins, and finally back to the heart. In normal tissue, tight pericyte coverage and vascular endothelial cell junction ensure regular blood circulation, forming a mature vascular structure.48 However, in tumor tissue, more mechanical stress from the hypertrophic tumor tissue results in an uneven thickness and deformed architecture of tumor vessels, which exhibit intensive sprouting orchestrated in an irregular convoluted manner that tends to hinder blood flow.49–51 Mechanical stress also disrupts lymphatic channels and prevents lymphatic drainage of excess interstitial fluid. Besides, fragile and highly permeable tumor vessels, which have an irregular arrangement of endothelial cells and thinly covered pericytes, lead to blood leakage and incoherent perfusion.52–54 This spatially anomalous structure is manifested in low blood flow, which decreases the supply of oxygen and nutrient, causing subsequent acidosis and hypoxia within tumor microenvironment and high interstitial hypertension.55 Highly permeable tumor blood vessels facilitate plasma and proteins into the surrounding interstitium, increasing blood viscosity and interstitial pressure in tumor microenvironment, further impeding blood flow.56–58 All these factors result in chaotic function and abnormal architecture of tumor blood vessels, further aggravating acid and hypoxic tumor microenvironment, which contributes to tumor angiogenesis, invasion, and metastasis.59,60
Studies have shown that 50–60% of solid tumors are hypoxic, which disrupts the expression of multiple tumor genes profiles and causes tumor necrosis, stimulating the spread and metastasis of tumor.61 Since tumor growth and reproduction require substantial energy, the tumor cells in a hypoxic environment are forced to release energy through glycolysis and secrete considerable acidic substances, aggravating the acidity of the microenvironment (pH is usually between 6.5–7.2, or even lower).62,63 Furthermore, the interstitial pressure in normal tissues is only 0–3 mmHg.64 In tumor tissue, high interstitial pressure (5–40 mmHg, even 75–130 mmHg in some cases) hinders the transport of blood and drugs,65 which is caused by blood leakage of tumor vessels and the increase of interstitial fluid, thus the tumor cannot obtain sufficient oxygen and nutrients.66,67 These factors affect the drug treatment and benefit tumor proliferation, adhesion, invasion, and metastasis, eventually leading to tumor resistance and malignant lesions.68,69 Because of the tenacious viability, various pro-angiogenic factors are secreted by tumor cells to stimulate endothelial cells proliferation and migration, promote vessel formation, increase blood circulation to meet the requirements of the tumor, and mitigate metabolic stress.
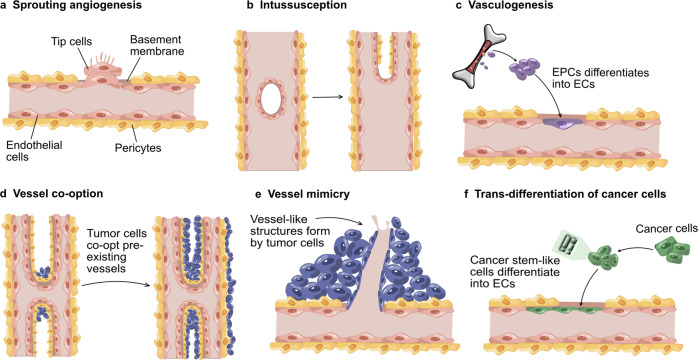
Tumor angiogenesis occurs mainly through any of the following modes described in Fig. 2. Among them, sprouting angiogenesis is the most typical process in physiological and pathological angiogenesis. The patterns of vessel co-option and vessel mimicry are significantly related to tumor invasion, metastasis, and therapeutic resistance in conventional anti-angiogenic therapy. Sprouting angiogenesis is so-called angiogenesis, in which new vascular branches form in existing blood vessels and finally infiltrate into tumor tissue through the migration of tip cells and the proliferation of stem cells (Fig. 2a).70,71 Intussusceptive angiogenesis involves the formation of a double lumen, which splits into two vessels, infiltrating into tumor tissue (Fig. 2b).72,73 Vasculogenesis refers to recruiting bone marrow-derived or vessel wall resident endothelial progenitor cells, which differentiate into endothelial cells to form new blood vessels (Fig. 2c).71,74 In addition to the above three models, tumors can achieve angiogenesis through vessel co-option, vessel mimicry, lymphangiogenesis, and rare stromal-sharing modes.3,24,75 Vessel co-option, in which tumor cells migrate around pre-existing blood vessels or infiltrate into surrounding tissue space, eventually wrapping the blood vessels and leading them into tumor tissue to supply nutrients for tumor cells (Fig. 2d).76 Vessel mimicry is a process that tumor cells extend to form a simulated vascular lumen and then insert into the pre-existing blood vessels, transporting the erythrocyte and oxygen into tumor tissue (Fig. 2e).77 Researchers believe that vessel mimicry is closely connected with hypoxia, which stimulates the secretion of matrix metalloproteinases (MMPs) and periodic acid Schiff-positive substances to irritate the formation of vascular mimicry.77 Another mode is that trans-differentiation of cancer stem-like cells (which obtain the endothelial phenotype) into endothelial-like cells via epithelial-endothelial transformation (Fig. 2f).
Fig. 2.
Most common modes in tumor angiogenesis. a Sprouting angiogenesis: main way in both physiological and pathological angiogenesis, which is induce by proliferation and migration of endothelial tip cells. b Intussusception: the existing blood vessel is divided into two vessels under mediation of cell reorganization. c Vasculogenesis: bone-marrow-derived endothelial progenitor cells differentiate into endothelial cells, participating in the formation of new vascular lumen. d Vessel co-option: tumor cells approach and hijack the existing blood vessels. e Vessel mimicry: tumor cells form a vessel-like channel around normal blood vessels to direct the transport of oxygen and nutrients into tumor tissue. f Trans-differentiation of cancer cells: cancer stem-like cells differentiate into endothelial cells, which participate in the formation of new blood vessels. (Modified from Carmeliet, P. & Jain, R. K. Molecular mechanisms and clinical applications of angiogenesis. Nature 473, 298–307 (2011).)
Key molecules and signaling pathways in tumor angiogenesis
Various biomolecules that promote or inhibit angiogenesis constitute a complex and dynamic angiogenic system, including growth factors (such as vascular endothelial growth factor, fibroblast growth factor, transforming growth factor, hepatocyte growth factor), adhesion factors (integrin, cadherin), proteases (such as matrix metalloproteinase), extracellular matrix proteins (fibronectin, collagen), transcription factors (hypoxia-inducible factor, nuclear factor), signaling molecule mechanistic target of rapamycin (mTOR), protein kinase B (AKT), p38 mitogen-activated protein kinases (p38 MAPK), nitric oxide (NO), angiopoietin, thrombospondin-1, angiostatin, endostatin, and interleukin (IL).78 The vascular endothelial growth factor (VEGF) is the most typical regulator in tumor angiogenesis, which can mediate vascular permeability and tube formation.79 Platelet-derived growth factor (PDGF) promotes vascular maturation by recruiting parietal cells.80 Notch signal guides vascular sprouting and stretching and matrix metalloproteinases activate angiogenesis by distinctly degrading the basement membrane.81 All of them initiate the downstream signaling pathway transduction through transmembrane receptors to activate gene expression and induce endothelial cells proliferation, survival, and angiogenesis (Fig. 3).
Fig. 3.
Schematic diagram showing crosstalk of multiple signaling pathways during tumor angiogenesis. Pointed arrows indicate activation whereas flat arrows indicate inhibition
Growth factors and growth factor receptors
VEGF/VEGFRs
In the 1989s, Ferrara and his colleagues found a 45 kDa permeable substance through multiple layers of amino acid sequences, named vascular endothelial growth factor, a family of soluble secreted homodimeric glycoproteins.82 VEGF regulates vascular permeability, angiogenesis, and lymphogenesis.83
VEGF family consists of seven members, including VEGF-A, VEGF-B, VEGF-C, VEGF-D, placental growth factor (PlGF), and non-human genome encoded VEGF-E and svVEGF.82 VEGF-A (known as VEGF) is a crucial secretory factor that maintains human endothelial function and promotes cell mitosis and vascular permeability.84 Meanwhile, it involves in cell homeostasis, hematopoietic stem cells survival, tumor cells survival, and invasion through autocrine or paracrine.85,86 Moreover, VEGF-A is the most important regulator of angiogenesis that plays an irreplaceable role in tumor growth, proliferation, invasion, metastasis, angiogenesis, and drug resistance.87,88 In specific body parts, such as the heart, VEGF-B promotes neuronal survival and cardiovascular growth through angiogenesis.89 VEGF-C and VEGF-D encourage tumor growth and metastasis through lymphangiogenesis and lymphatic metastasis, which is mediated by VEGFR-3. Blocking this pathway leads to apoptosis of lymphatic endothelial cells and disruption of the lymphatic network.90,91 PlGF (isoforms 1–4) is a member of the cysteine-knot superfamily of growth factors,92,93 which is widely expressed in various tumor or non-tumor cells, like endothelial cells,94,95 vascular smooth muscle cells,94 neurons,96 inflammatory cells,94 bone marrow cells,95 brain cancer cells,97 and melanoma cells.98 Mediated by VEGFR-1, pro-angiogenic PlGF contributes to activation and proliferation of stromal cells including fibroblasts, macrophages, smooth muscle cells and endothelial cells.45 With both pro- and anti-angiogenic effects, the role of PlGF has remained increasingly debatable.99
The tyrosine kinase receptor VEGFRs consist of a transmembrane domain, an extracellular ligand-binding domain with an Ig-like domain, and a tyrosine kinase with an intracellular domain.86 VEGFR-1 (known as FLT-1) is the first identified dual-function VEGF receptor, a 180–185 kDa glycoprotein, acting as a co-receptor for VEGF-A, VEGF-B, and PlGF.100 VEGFR-1 is mainly active in various endothelial cells and non-endothelial cells (monocytes,101 macrophages,102 hematopoietic stem cells,103 smooth muscle cells,104 and leukocytes103), which regulates monocytes migration, endothelial progenitor cells recruitment, hematopoietic stem cells survival, and liver epithelial cells growth.103 As a negative regulator, VEGFR-1 competitively inhibits the activation of redundant VEGF-A/VEGFR-2, regulates levels of VEGF-A in serum, and controls excessive vascular formation. However, as a promoter, over-expressed VEGFR-1 facilitates the development and metastasis of breast cancer,105 leukemia,106 prostate cancer,107 ovarian cancer (OC) and malignant melanoma.106
VEGFR-2 (known as KDR or FLK-1) is a 210–230 kDa transmembrane glycoprotein, generally expressed by vascular endothelial cells, lymphatic endothelial cells, endothelial progenitor cells, megakaryocytes, and hematopoietic stem cells.100 Under the mediation of VEGF-A, VEGFR-2 undergoes autophosphorylation and signal transduction, which potently activates typical downstream signaling pathways such as PI3K/AKT/mTOR, p38 MAPK, Ras/Raf/MEK/ERK that are related to the growth and survival of ECs and angiogenesis (Fig. 3).83,108 The most crucial signaling pathway in physiological and pathological angiogenesis is VEGF-A/VEGFR-2, which stimulates mitosis, chemotaxis, and morphogenesis of ECs, and induces the proliferation, migration, invasion, and angiogenesis in solid tumors.103 Studies have shown that over-expressed VEGFR-2 has been detected in melanoma,109 OC,110 thyroid cancer (TC),111 and other solid tumors.112,113 VEGF-A/VEGFR-2 is a popular therapeutic target occupies the major research of angiogenic inhibitors (Table 1).
Table 1.
Anti-angiogenic drugs approved by FDA for clinical treatment
| Drugs | Targets | Indications | Companies | Adverse effects |
|---|---|---|---|---|
| Monoclonal antibodies | ||||
| Bevacizumab (Avastin®) | VEGF-A |
CRC in 2004, NSCLC in 2006, RCC in 2009, GBM in 2009, CC in 2014 |
Genentech/Roche | Arterial or venous, back pain, dry skin, exfoliative dermatitis gastrointestinal perforation, headache, hemorrhage, hypertension, lacrimation disorder, poor wound healing, proteinuria, rhinitis, and taste alteration, thrombosis |
| Ranibizumab (Lucentis®, RG-6321) | VEGF-A |
wAMD in 2006, DME in 2015, DR in 2017, Myopic choroidal neovascularization in 2017 |
Genentech/Roche | Conjunctival hemorrhage, endophthalmitis, eye infection, eye pain, floaters, increased intraocular pressure, rhegmatogenous retinal detachment, and retinal hemorrhage |
| Ramucirumab (Cyramza®) | VEGFR-2 | NSCLC in 2014, Advanced GC in 2014, GEJ adenocarcinoma in 2014, metastatic CRC in 2015 | Genentech and Eli Lilly | Abdominal pain, thrombocytopenia, anorexia, arthralgia, constipation, cough, diarrhea, dyspnea, epistaxis, fatigue, headache, hypertension, leucopenia, nausea, neutropenia, peripheral edema, proteinuria, upper respiratory tract infection, and vomiting |
| Olaratumab (Lartruvo®) | PDGFR-α | STS in 2016 | ImClone/Eli Lilly | Appetite, abdominal pain, alopecia, diarrhea, decreased fatigue, headache, neuropathy, musculoskeletal pain, mucositis, nausea, and vomiting |
| Bevacizumab-awwb (Mvasi®) | VEGF | CRC, NSCLC, RCC, GBM, and CC in 2017 | Amgen | Altered taste, arterial and venous thromboembolic events, bleeding, dry skin, epistaxis, exfoliative dermatitis, headache, hypertension, hypertension, infusion-related reactions, lacrimation disorders, ovarian failure, perforation or fistula, post-reversible encephalopathy syndrome, proteinuria, proteinuria, and rhinitis |
| Oligonucleotide aptamers | ||||
| Pegaptanib (Macugen®) | VEGF-A165 | wAMD in 2004 | Eyetech/Pfizer | Endophthalmitis and retinal detachment |
| Recombinant fusion proteins | ||||
| Aflibercept (Eylea®) | VEGF-A, VEGF-B, PlGF |
wAMD in 2011 CRC in 2012 DME in 2015 DR in 2019 |
Regeneron | Cataracts, conjunctival hemorrhage, decreased vision, eye pain, floaters, increased intraocular pressure, and vitreous detachment |
| ziv-Aflibercept (Zaltrap®) | VEGF-A, VEGF-B, PlGF | CRC in 2012 | Sanofi and Regeneron | Abdominal pain, bleeding, decreased appetite, decreased ejection fraction, diarrhea, dyspnea, epigastric pain, fatigue, fatigue, gastrointestinal perforation, headache, heart failure, hypertension, impaired wound healing, infection, leukopenia, nephrotic syndrome, neutropenia, osteonecrosis of the lower jaw, proteinuria, severe diarrhea, stomatitis, thrombocytopenia, and weight loss |
| mTOR inhibitors | ||||
| Temsirolimus (Torisel®) | mTOR | RCC in 2007 | Wyeth | Acute renal failure, asthenia, edema, elevated aspartate aminotransferases, hyperlipidemia, hypersensitivity, interstitial pneumonia, intestinal perforation, lymphopenia, mucositis, nausea, rash, thrombocytopenia |
| Everolimus (RAD001, Afinitor®) | mTOR |
RCC in 2009 SEGA in 2010 pNET in 2011 HER2- BC |
Novartis | Canker sores, increased heart rate, paronychia, rash, swollen and painful gums, tiredness, and tongue ulcers |
| Immunomodulatory agents | ||||
|
Thalidomide (Thalomid®)
|
VEGF-A, TNF, NF-κB | MM in 2006 | Celgene | Abdominal pain, constipation, dizziness, drowsiness, dry oral mucosa, facial puffiness, nausea, rash, teratogenic, and tiredness |
|
Lenalidomide (Revlimid®)
|
VEGF-A, TNF, NF-κB |
MM in 2006 MCL in 2013 |
Celgene | Anemia, diarrhea, fatigue, headache, loss of appetite, low back pain, neo-malignant neoplasms, neutropenia, rash, renal insufficiency, thrombocytopenia, and thrombotic complications |
| Tyrosine kinase inhibitors | ||||
|
Sorafenib (Nexavar®, BAY-439006)
|
VEGFR-1/-2/-3, c-Kit, Flt-3, PDGFR-β, Raf, Ret |
RCC in 2005 HCC in 2007 DTC in 2013 TC in 2014 |
Bayer and Onyx/Amgen |
Abdominal pain, alopecia, decreased appetite, diarrhea, fatigue, hand-foot skin reaction, hypertension, nausea, rash, and weight loss |
|
Sunitinib (Sutent®, SU11248)
|
VEGFR-1/-2/-3, Flt-3, c-Kit, Ret, PDGFR-α/-β, CSF-1R |
RCC in 2006 GIST in 2006 pNET in 2011 |
Sugen/Pfizer | Abdominal pain, anorexia, asthenia, diarrhea, dysgeusia, dyspepsia, fatigue, hypertension, mucositis, nausea, skin discoloration, stomatitis, and thrombocytopenia |
|
Pazopanib (Votrient®, GW-786034)
|
VEGFR-1/-2/3, c-Kit, PDGFR-α/-β, |
RCC in 2009 STS in 2012 |
GlaxoSmithKline | Anorexia, diarrhea, fatigue, fatigue, hair color changes, nausea, vomiting, and weight loss |
|
Vandetanib (Caprelsa®, ZD6474)
|
VEGFR-2, VEGFR-3, EGFR, Ret | MTC in 2011 | AstraZeneca | Diarrhea, headache, rash, hypertension, nausea, and QTc prolongation |
|
Regorafenib (Stivarga®)
|
VEGFR-1/-2/-3, c-Kit, PDGFR-β, Ret, Raf-1, bRaf, FGFR-1, Tie-2 |
CRC in 2012 GIST in 2013 HCC in 2017 |
Bayer | Anorexia, diarrhea, fatigue, hand-foot skin reaction, hypertension, and oral mucositis |
|
Axitinib (Inlyta®, AG013736)
|
VEGFR-1/-2/3, c-Kit, PDGFR-α, PDGFR-β | RCC in 2012 | Pfizer | Asthenia, constipation, decreased appetite, diarrhea, dysphonia, fatigue, hand-foot syndrome, hypertension, nausea, vomiting, and weight decreased |
|
Ponatinib (Iclusig®)
|
VEGFRs, PDGFRs, EPHs, FGFRs, ABL, Src, Ret, LYN, LCK, c-Kit, HCK, FYN, FRK, c-FMS, FGR, BLK |
CML in 2012 Ph+ AML in 2012 |
Ariad/Takeda | Abdominal pain, arthralgia, dermatitis, dry skin, fatigue, increased lipase, nausea, rash, and thrombocytopenia |
|
Cabozantinib (Cometriq®, BMS-907351)
|
VEGFR-2, c-Met, c-Kit, Ret, Flt-3, Tie-2, AXL, RON |
MTC in 2013 RCC in 2016 HCC in 2019 |
Exelixis | Abdominal pain, constipation, decreased appetite, decreased weight, diarrhea, dysgeusia, fatigue, hair color changes, hypertension, nausea, oral pain, palmar-plantar erythrodysesthesia syndrome, and stomatitis |
|
Apatinib (Aitan®)
|
VEGFR-2, Src, c-Kit | GC in 2014 | Hengrui Medicine | Fatigue, gastrointestinal bleeding, granulocytopenia, hand-foot syndrome, hoarseness, hypertension, leukopenia, proteinuria, and thrombocytopenia |
|
Nintedanib (Ofev®, BIBF1120)
|
VEGFRs, FGFRs, PDGFRs, Flt-3, LCK, LYN, Src | NSCLC in 2015 |
Boehringer and Ingelheim |
Bleeding, decreased appetite, diarrhea, electrolyte imbalance, mucositis, nausea, neutropenia, peripheral neuropathy, rash, and vomiting |
|
Lenvatinib (Lenvima®, E7080)
|
VEGFRs, PDGFRs, Ret, c-Kit, FGFRs |
DTC and TC in 2015 RCC in 2016 HCC in 2018 Endometrial Carcinoma in 2019 |
Eisai | Abdominal pain, arthralgia, decreased appetite, decreased weight, diarrhea, dysphonia, fatigue, headache, hypertension, myalgia, nausea, proteinuria, stomatitis, and vomiting |
ALL acute lymphoblastic leukemia, BC breast cancer, BTC biliary tract cancer, CC cervical cancer, CML chronic myeloid leukemia, CRC colorectal cancer, CSF colony-stimulating factor, DME diabetic macular edema, DR diabetic retinopathy, DTC differentiated thyroid cancer, EC esophageal cancer, GEJ gastroesophageal junction, GBM glioblastoma, GC gastric cancer, GIST gastrointestinal stromal tumor, HCC hepatocellular carcinoma, HER2 human epidermal growth factor receptor 2, HNSCC head and neck squamous cell carcinoma, MCL mantle cell lymphoma, MM multiple myeloma, MTC medullary thyroid cancer, mTOR mammalian target of rapamycin, NSCLC non-small cell lung cancer, Ph+ AML Philadelphia chromosome-positive acute myeloid leukemia, pNET pancreas neuroendocrine tumor, RCC renal cell carcinoma, SEGA subependymal giant cell astrocytoma, STS soft tissue sarcoma, TC thyroid cancer, TNBC triple-negative breast cancer, wAMD wet age-related macular degeneration
VEGFR-3 (FLT-4) is a precursor protein with a molecular weight of 195 kDa, mainly expressed in lymphatic endothelial cells and mediates the activation of VEGF-C and VEGF-D, impelling lymphoid proliferation and metastasis of tumor.86 VEGFR-3 is frequently over-expressed in metastatic CRC,114 BC,115 lung cancer,116 gastric cancer (GC),117 cervical cancer (CC),118 and other malignant tumors.118,119 Both angiogenesis and lymphangiogenesis are essential to metastatic tumors.39,49 VEGF-C,-D/VEGFR-3 is the primary signal pathway mediates lymphangiogenesis.120 Blocking VEGF-C,-D/VEGFR-3 pathway has potential in preventing tumor metastasis.
PDGF/PDGFRs
A factor secreted by platelets and some stromal cells, which participates in coagulation or angiogenesis, is known as platelet-derived growth factor (PDGF). As the main mitogen of mesenchymal cells such as fibroblasts, smooth muscle cells, and glial cells, PDGF involves in cell growth and differentiation, wound healing, angiogenesis, recruitment, and differentiation of pericytes and smooth muscle cells through paracrine or autocrine.121–123
PDGFs have four soluble inactive polypeptide chains, including PDGF-A, PDGF-B, PDGF-C, and PDGF-D, which perform biological functions after being translated into active homodimers or heterodimers such as PDGF-AA, PDGF-AB, PDGF-BB, PDGF-CC, PDGF-DD.123,124 Among them, PDGF-AA drives cell proliferation, differentiation, metastasis, invasion and angiogenesis, which acts as a cancer promotor mediated by PDGFR-α. For example, phosphorylation of STAT3 (Y705) and the inactivation of tumor suppressor Rb1 can be motivated by PDGF-AA/PDGFR-α, accelerating the deterioration and angiogenesis of glioma stem cells.125 Additionally, tumorigenic effects of PDGF-AB, PDGF-CC, and PDGF-DD are manifested through different forms. PDGF-AB promotes mitosis and chemotaxis.126 PDGF-CC induces tumor growth and angiogenesis mediated by CAFs. PDGF-DD/PDGFR-β can irritate the proliferation and metastasis of carcinomas.127,128 PDGF-BB is one of the most studied factors in the PDGF family with potent cancer-driving efficacy through various downstream signaling pathways (such as MAPK/ERK,129 PI3K/AKT,130 and JNK pathway), which regulates the proliferation and migration of PDGF-dependent cells.131,132 Over-expressed PDGF signals not only enhance tissue fibrosis but also excite angiogenesis and drug resistance in tumor progression and anti-VEGF therapy.121,133
PDGFRs (including PDGFR-α and PDGFR-β) are membrane-bound proteins consisting of a transmembrane domain, a juxtamembrane domain, a kinase insertion domain, an intracellular domain, and five extracellular Ig-like domains.134 PDGF/PDGFR-β signaling pathway is a dominant commander of pericyte recruitment that can initiate revascularization and stromal cell activation required for wound healing.135,136 Moreover, it participates in the growth and reproduction of endothelial cells, angiogenesis, and vascular maturation.137,138 Studies have shown that PDGFs and PDGFR-α/β are commonly over-activated in numerous malignant tumors and tissues, including NSCLC,139 BC,139 OC,140,141 hepatocellular carcinoma (HCC),142,143 and GIST.144 The proliferation, metastasis, invasion and angiogenesis of carcinomas can be obstructed by inhibition or neutralization of PDGFRs,132 some PDGFR inhibitors and dual-targeted VEGFR/PDGFR inhibitors are being developed.
EGF/EGFRs
Epidermal growth factor (EGF) is a single-chain small molecule polypeptide composed of 53 amino acid residues.145 The EGF receptors consist of four proteins, EGFR (ErbB1), HER2 (ErbB2), HER3 (ErbB3), and HER4 (ErbB4),146,147 which have an extramembrane binding domain, a single-chain transmembrane domain that contains a single hydrophobic anchor sequence, and an intramembrane tyrosine kinase binding domain that generates and mediates intracellular signals.148,149
EGF is a mediator widely participates in cell growth, proliferation, differentiation, migration, adhesion, apoptosis, and tumor angiogenesis through EGFR.150 As a promoter, EGF involves in endothelial cell proliferation and differentiation through activating downstream signaling pathways (MAPK, PI3K/AKT/PKB, STAT, and PLCγ/PKC), which is mediated by EGFR (Fig. 3).147 Besides, it encourages mitosis and up-regulates the synthesis, expression, and secretion of various angiogenic factors, such as VEGF through the Ang-2 ligand, prompting tumor angiogenesis indirectly.41 Some research proposed that HIF-1α induced the expression of EGF and EGFR, while EGFR up-regulated the expression of HIF-1α and enhanced the oxygen tolerance of cells under a hypoxic microenvironment, consequently aggravating angiogenesis and progression of the tumor.151,152 The expression level of EGFR is usually up-regulated in various malignant tumors, including BC, OC, NSCLC, GBM, bladder cancer and pancreatic cancer, which directly promotes tumor growth by mediating gene expression and mediates tumor invasion and metastasis through angiogenesis.149,153 Several studies have shown that EGFR T790M gene mutation is the leading cause of drug resistance to EGFR kinase inhibitors (gefitinib and erlotinib) in the early treatment of lung cancer.154 But drug resistance from EGFR self-mutation is far less than that caused by signals crosstalk between EGFR and others (such as c-Met).155
FGF/FGFRs
As a critical factor in promoting wound healing, the fibroblast growth factor (FGF) family is one of the potent mitogens and drivers of endothelial cells and is the earliest discovered growth factor related to angiogenesis,156 which consists of 23 proteins with different structures.157,158 Secreted by vascular endothelial cells, stem cells, and damaged cardiomyocytes, FGF regulates embryonic development, wound healing, tissue homeostasis, cancer progression, and angiogenesis through synergistic FGFRs, heparan sulfate polysaccharide, and αvβ integrins.159–161 FGF-1 is an acidic fibroblast growth factor that stimulates the proliferation and differentiation of parietal vessel cells.157 The most influential pro-angiogenic factor in the FGF family is FGF-2 (known as bFGF), which regulates the functional differentiation of cardiac non-myocytes through paracrine and stimulates angiogenesis-related processes such as migration and invasion of ECs and production of plasminogen activators.158,162 bFGF is often over-expressed in BC, lung cancer, bladder cancer, and leukemia, and is related to cancer metastasis and poor prognosis in patients.160,162,163 Besides, the up-regulation of bFGF is closely related to poor outcomes of CRC patients after treatment with combined regimens (bevacizumab plus fluorouracil and irinotecan),164 and GBM patients who are treated with cediranib (AZD-2171, a potent VEGFR inhibitor).165
FGFR is a transmembrane receptor family with five members of FGFR1–5 (only FGFR5 lacks an intracellular kinase domain),163 whose genes are proto-oncogenes with tumorigenic potential after gene amplification, chromosomal translocation or point mutation.166–168 FGFR mediates the survival, multiplication, and migration, angiogenesis, and drug resistance in target cells through autophosphorylation and activating downstream Src family kinases,169 PLCγ/DAG/PKC,157,163 Ras/Raf-MAPK, and PI3K/AKT pathways activated by bFGF, playing a pro-angiogenic role in the human body (Fig. 3).159,170,171 In tumor angiogenesis, FGF/FGFR signaling plays a key role in stimulating the secretion of MMPs and regulates the proliferation, differentiation, migration, morphological changes, and vascular maturation of endothelial cells.171 Aberrant activations of bFGF/FGFR are essential alternative angiogenic pathways that induce drug resistance in anti-VEGFR therapy.133,172
HGF/c-Met
The hepatocyte growth factor (known as the scattering factor) is a multi-effect precursor protein and a mitogen of mature rat hepatocytes,173 mainly derived from mesenchymal cells and activated by extracellular protease cleavage.174 As a soluble heterodimer, HGF can be cleaved into α chain and β chain. α chain is responsible for binding receptors while β chain can trigger receptors and transduce signals.175 Transmembrane helical receptor c-Met is a 170 kDa cell-stroma-epithelium transition factor usually expressed on endothelial cells, epithelial cells, and melanocytes in the pathological liver, kidney, lung and other organs.155,173,176 c-Met was firstly discovered as a proto-oncogene in 1984 and later identified as a specific receptor for HGF in 1991.177,178 Owing to instinctively actuate cell growth, differentiation, morphogenesis and suppress apoptosis, HGF/c-Met is a crucial signaling pathway in wound healing, tissue regeneration and embryogenesis.155,173,175 Inhibition of this pathway will seriously affect the self-repair of patients with myocardial ischemia,179 diabetic retinopathy,180 liver damage,181 and arthritis.182 Nevertheless, abnormal HGF/c-Met signals such as amplification or secondary mutation of c-Met genes, transcription dysregulation, and abnormally autocrine or paracrine of HGF caused by over-expression of c-Met, encourages the spread, invasion and angiogenesis of cancerous tissues,183–185 drug resistance, and poor prognoses of patients.175,186–188 It has been demonstrated that the exon 14 mutation of c-Met promotes the metastasis of advanced cancer, like lung adenocarcinoma, RCC, and brain glioma.189 Besides, drug resistance in treatment with EGFR kinase inhibitors is partly attributed to signaling crosstalk between similar EGFR and c-Met.155,190 All of these functions above are achieved through activation of downstream signaling pathways including JAK/STAT,191 Ras/MAPK,192 PI3K/AKT,192 Wnt/β-catenin, or others (Fig. 3).193,194 As the role of the HGF/c-Met system in pathological and physiological angiogenesis and drug resistance continues to be revealed, HGF/c-Met axis becomes an attractive target for anti-tumor therapy.
IGF/IGFRs
Insulin-like growth factor (IGF) is a peptide growth factor that regulates human growth, development, and energy metabolism, which participates in physiological circulation through autocrine, paracrine, and endocrine.195 IGF modulates the survival, proliferation, and differentiation of multiplicate cells and the physiological process of the blood system under different physiological conditions.196 IGF1 and IGF2 are the two main subtypes mediated by insulin receptors IGF1R, IGF2R and IGFBPs.197,198 Highly expressed IGF1 and IGF2 induces VEGF synthesis and up-regulates the expression of HIF-1α and VEGF to promote angiogenesis. Besides, autocrine IGF2 induces drug resistance in anti-tumor therapy.195 Moreover, studies have shown that over-expression of IGF fosters the progression of diabetic retinopathy (DR),199,200 retinopathy of prematurity,201–203 atherosclerosis, and cancer.204–207
IGFBPs are high-affinity receptors of IGF, with six subtypes of IGFBP1–6, secreted by endothelial cells living in macro-vessels and capillaries.198 Pro-angiogenic IGFBP2 induces chemotaxis and migration of ECs by increasing VEGF transcription and IGF levels.208,209 IGFBP3 up-regulates the expression of VEGF, MMP2, and MMP9 and promotes tube formation.210 IGFBP4, IGFBP5, and IGFBP6 appear to inhibit angiogenesis indirectly.196 More studies are expected to dissect the roles and mechanisms of IGF family in tumor angiogenesis.
TGF-β
In 1978, a signaling protein with multiple biological effects, named transforming growth factor-β (TGF-β), was discovered by scientists in mouse fibroblasts. TGF-β is a secreted cytokine that is concerned with body homeostasis, tissue repair, inflammation, and immune responses,211 which is also involved in cell growth, differentiation, proliferation, autophagy, apoptosis, and tumor angiogenesis.212 There are three types of single-pass transmembrane receptors specifically interact with TGF-β, named type I (TβRI), type II (TβRII) and type III (TβRIII). Under the co-transduction of these receptors, the downstream Smad-dependent pathways, and non-Smad pathways (involves classical MAPK, JNK/p38 MAPK, PI3K/AKT, TAK1, and ERKs) are alternately activated to exert the physiological and pathological effects of TGF-β.213–215 Apart from various physiological processes, TGF-β involves in multiple atherosclerosis and fibrotic diseases like cirrhosis and pulmonary fibrosis and affects cancer progression.216,217 During the initial stage of tumorigenesis, TGF-β acts as a suppressor that induces apoptosis and confines pre-cancerous cells.216,218 But in mature tumor tissue, the aggressiveness of the tumor is awakened by TGF-β, which encourages various pro-cancer activities, including epithelial-mesenchymal transition (EMT), metastasis, invasion, fibrosis, angiogenesis, and immune suppression of carcinomas.219–221
The tumorigenic effects of TGF can be manifested in various modes. Firstly, TGF-β induces the migration of endothelial cells to impel vessel sprouting.222,223 Secondly, TGF-β encourages infiltration and invasion of the tumor through EMT.224 Thirdly, TGF-β up-regulates the expression of MMP-2 and MMP-9 to mobilize tumor invasiveness and angiogenesis.224–226 Last but not least, TGF-β induces the expression of connective tissue growth factor (CTGF),227 VEGF, bFGF, and interleukin-1, which are essential for tumor angiogenesis.228,229 Many studies have demonstrated that TGF-β is closely related to the tumorigenesis and poor prognosis of patients in multifarious human organizations. For example, high tissue concentrations of TGF-β have been detected in human pancreatic cancer,230–233 NSCLC,234 HCC,235–237 and BC,238 which motivates tumor progression and angiogenesis, leading to unsatisfactory clinical outcomes. Accordingly, TGF-β simultaneously promotes tumorigenesis and induces angiogenesis to nourish tumors. Perhaps TGF-β is the next breakthrough to fight against tumor angiogenesis and drug resistance.
Transcription factors
Hypoxia-inducible factor-1
Hypoxia is the most typical feature of the tumor microenvironment and is always associated with drug resistance, tumor angiogenesis, aggressiveness, and recurrence.239 The hypoxia-inducible factor-1 (HIF-1) is a heterodimeric transcription factor that regulates cell adaptation to hypoxia, energy metabolism, erythropoiesis, and tissue perfusion balance and involves in cell survival, proliferation, migration, adhesion, apoptosis, erythropoiesis, and glucose metabolism.240,241 HIF-1 is composed of the constitutive nuclear protein HIF-1β and environment-dependent isomer HIF-1α,151 which is an oxygen regulator that increases oxygen delivery, reduces oxygen consumption and maintains oxygen balance.240–242 HIF-2α and HIF-3α are the analogs of HIF-1α which are not well understood.241,243
Under normoxic conditions, the proline residues in HIF-1α are hydroxylated by the proline hydroxylase domain (PHD), which can stabilize HIF-1α. Subsequently, HIF-1α is degraded by proteasomes after ubiquitination mediated by E3 ubiquitin ligase and ρVHL. Besides, hydroxylation of asparagine residues, which regulates HIF-1α transcriptional activity and specificity, disrupts the interaction between HIF-1α and co-activation factor p300 to inhibit the transcriptional activity of HIF-1α, consequently inhibiting the expression of VEGF and angiogenesis (Fig. 4).151,239 However, since the hydroxylation under hypoxic conditions can be limited by oxygen concentration, HIF-1α constitutes a dimerized complex with HIF-1β through nuclear translocation. This complex binds the hypoxia response element (HRE) (located on the HIF target) after interacting with the coactivator p300, subsequently activating the transcription of the downstream target genes that encode VEGF, MMPs, angiopoietin, and PDGF (Fig. 4). The complicated process enhances the affinity and invasiveness of tumor cells, induces apoptosis of epithelial cells, inhibits apoptosis of tumor cells, and promotes tumor angiogenesis.244–246
Fig. 4.
The transduction of HIF-1α in normal and hypoxic conditions. Under normal conditions, HIF-1α is degraded by protease and loses transcription function. In hypoxic environment, lack of enzyme degradation leads to efficient transcription of HIF-1α, resulting in over-expression of pro-angiogenic factors including VEGF, PDGF, and MMPs
The unfavorable effects of the hypoxic microenvironment in tumor tissue are mainly realized by HIF-1α, which induces pro-oncogenic gene expression to disrupt the “homeostasis” of TME. In tumor progression, the expression of related genes of all VEGF isoforms, PlGF, FGF, PDGF, and Ang-1 can be up-regulated by HIF-1α to promote tumor angiogenesis or induce drug resistance. HIF-1α also up-regulates TGF-β, PDGF, and CXCL2 secreted by tumor cells and macrophages, which prompt the reconstruction of extracellular matrix and impel the invasion and metastasis of tumors induced by tumor-associated fibroblasts (TAFs).243,247 Various model experiments and clinical trials have demonstrated that over-expression of HIF-1α is significantly related to the progression of BC,248,249 CC,250 NSCLC,251,252 and HCC,253,254 especially some advanced metastatic cancers.151,255 Furthermore, cell cycle arrest and compensatory angiogenesis initiated by hypoxia are among the pivotal causes of drug resistance in chemotherapy and anti-angiogenic treatment, respectively.256,257 HIF-1α is a crucial target for anti-tumor therapy, while some progress has been made in developing novel small-molecule inhibitors that target HIF-1α (Table 3).
Table 3.
Selected small molecules with excellent kinase inhibition activity
| Compounds | Chemical Structures | Targets | IC50 | References |
|---|---|---|---|---|
| 1 |  |
VEGFR-2 | 0.19 nM | 471 |
| 2 |  |
VEGFR-2 | 2.6 nM | 472 |
| 3 |  |
VEGFR-2 | 3.2 nM | 473 |
| 4 |  |
VEGFR-2 | 3.2 nM | 474 |
| 5 |  |
VEGFR-2 | 27 nM | 475 |
| 6 |  |
VEGFR-2 | 66 nM | 476 |
| 7 |  |
VEGFR-2 | 0.12 μM | 477 |
| 8 |  |
VEGFR-2 | 0.12 μM | 478 |
| 9 |  |
VEGFR-2 | 0.23 μM | 479 |
| 10 |  |
VEGFR-2 | 0.29 μM | 480 |
| 11 |  |
VEGFR-2 | 0.31 μM | 481 |
| 12 |  |
VEGFR-2 PDGFR-β |
24.7 nM 16.1 nM |
481 |
| 13 |  |
VEGFR-2 FGFR-1 PDGFR-β |
7 nM 69 nM 31 nM |
482 |
| 14 |  |
VEGFR-2 FGFR-1 PDGFR-β |
0.18 μM 0.23 μM 0.1 μM |
481 |
| 15 |  |
VEGFR-2 c-Met PDGFR-β |
435 nM 654 nM 371 nM |
481,483 |
| 16 |  |
VEGFR-2 Tie-2 EphB4 |
1.05 nM 2.47 nM 0.27 nM |
484,485 |
| 17 |  |
VEGFR-2 Tie-2 EphB4 |
1.85 nM 0.73 nM 2.99 nM |
486 |
| 18 |  |
VEGFR-2 Tie-2 EphB4 |
2.35 nM 5.63 nM 3.87 nM |
487 |
| 19 |  |
VEGFR-2 HDAC4 |
5 μM 0.36 μM |
488 |
| 20 |  |
FGFR-4 | 5.4 nM | 489 |
| 21 |  |
FGFR-1 FGFR-2 VEGFR-2 |
1.0 nM 4.5 nM 2.9 nM |
490 |
| 22 |  |
FGFR-1 FGFR-2 FGFR-3 |
0.6 μM 1.3 μM 4.1 μM |
491 |
| 23 |  |
HIF-1α | 0.6 μM | 492 |
| 24 |  |
HIF-1α | 0.32 μM | 493 |
| 25 |  |
HIF-1α | 0.6 μM | 494 |
NF-κB
Being discovered in 1986, the nuclear factor κB (NF-κB) is an important transcription factor in the human body, and is involved in cell survival, oxidative damage, inflammation, immune responses, and angiogenesis.258,259 As an indirect mediator, NF-κB regulates the development of various carcinomas (such as CRC, BC, and melanoma) by modulating the expression levels of angiogenic factors, especially VEGF.260 Blocking NF-κB signals in vitro and in vivo significantly decreased tumor angiogenesis induced by VEGF, IL-8, and MMP-9.261 Targeting NF-κB may be a prospective strategy for anti-angiogenesis.
Maturation, morphogenic, and guidance molecules
Angiopoietins/Tie
A coiled-coil amino-terminal domain and a carboxy-terminal fibrinogen-like domain constitute the angiopoietin,262 which maintains quiescent endothelial cells homeostasis and blood vessels morphology and involves in new blood vessels formation, embryonic development, and tumor angiogenesis. Angiopoietins consist of four ligands, Ang-1, Ang-2, Ang-3, and Ang-4.263 Ang-1 and Ang-2 are the main factors involved in vascular homeostasis. The transmembrane protein Tie is a specific receptor family of Ang with high affinity. Tie-2 (known as TEK) is a commonly studied receptor that mediates the functions of angiopoietin.264 Tie-1 is an orphan receptor which can modulate the activity of Tie-2 receptor.263,264
Ang-1 is a bifunctional protein and is mainly secreted by pericytes,265 smooth muscle cells, tumor cells,266 and others around endothelial cells to mediate vessel remodeling and vascular stabilization.266 Ang-1 activates the signaling pathway through receptor Tie-2 on macrophages to down-regulate the expression of PHD-2, reducing the leakage and interstitial pressure of tumor vessels and preventing tumor metastasis.267 It also stimulates tumor growth by promoting endothelial cell survival and vascular maturation, inhibits tumor cell extravasation, increases pericyte coverage and matrix deposition, and maintains the integrity of healthy blood vessels outside the tumor.266,268 Over-expressed Ang-1 strengthens the malignancy of NSCLC,269 BC,270,271 OC,272 and gliomas,273,274 and impels angiogenesis in brain tumors as well, which is dominated by bone marrow-derived endothelial progenitor cells.275
Ang-2 may exert pro- or anti-angiogenic activities in different environments based on dynamic concentrations of VEGF-A. Stimulated by VEGF-A, Ang-2 promotes angiogenesis and pericyte shedding to disturb vascular stability through competitively binding Tie-2 and integrin receptors.276,277 The over-expression of Ang-2 promotes vascular proliferation and the growth of carcinomas. However, under a low concentration of VEGF-A, Ang-2 induces apoptosis and vascular degeneration to inhibit tumor growth.268 In a peptide-antibody fusion trial, tumor growth, angiogenesis, and endothelial cells proliferation were inhibited by neutralizing Ang-2.267 With advanced research on Ang-1/-2, some antibodies targeted angiopoietin (like trebananib, faricimab, nesvacumab and vanucizumab) are undergoing clinical trials to testify their anti-tumor efficacy through inhibiting tumor angiogenesis.24 More functions of the Ang/Tie pathway in tumor angiogenesis will be proven in the near further.
Notch-Delta/Jagged
Notch receptors are a kind of particular non-RTK proteins that engage in numerous cellular processes, like morphogenesis, proliferation, migration, differentiation, apoptosis, adhesion, EMT, and angiogenesis (Fig. 3).278 Notch is initially verified in Drosophila melanogaster in the mid-1980s and is a highly evolutionarily conserved local signaling pathway.278 In mammals, the Notch receptors can be divided into four subunits named Notch-1, Notch-2, Notch-3 and Notch-4, and five ligands have been discovered, including Delta-like ligand-1 (Dll-1), Dll-3, Dll-4, Jagged ligand-1 (Jag-1), and Jag-2.279 This pathway is of great significance in adult tissue homeostasis, inflammation, embryonic development, vascular maintenance, and vascular remodeling.280
Among the Notch family, Dll-4 and Jag-1 are the most representative ligands in tumor angiogenesis.281,282 Highly expressed in the vasculature, Dll-4 is secreted by tip cells (differentiated from ECs) to induce excessive sprouting and increase microvessel density. Additionally, hypoxia is one of the causes of cancer metastasis, and the interaction between Dll-4 and HIF-1α significantly upregulates the expression of Dll-4 and aggravates hypoxia, promoting the aggressiveness of cancer cells.283–285 Studies in vitro have shown that blocking Dll-4 could simultaneously decrease tumor growth and stimulate vascular sprouting and branching to increase tumor angiogenesis, although these new blood vessels formed with inferior morphology and function.286 Jag-1 is mainly expressed by stem cells that antagonizes Notch signal induced by Dll-4 within sprout and promotes the growth of new vessels. The progression of various malignant tumors such as leukemia, BC,287 HCC,288 CC,289 and cholangiocarcinoma290 is highly linked to the over-expression of Jag-1.291 Up-regulation of Jag-1 in breast cancer increases the level of IL-6 and TGF-β to induce bone metastasis of cancer cells, which Jag-1 inhibitors can neutralize.292 Furthermore, aberrant Notch-Dll/Jag transductions contribute to survival and growth of cancer stem cells, metastasis, and drug resistance.279 Activated Notch signal has been reported to promote the progression of RCC, while inhibition of Notch signal limits the tumor growth in vivo and in vitro.293 Excessive Notch-1 has also been detected in other various human cancers like cervical, lung, and hematologic carcinomas.294 In tumor models, EMT and invasion induced by hypoxia could be offset after suppressing the Notch signaling pathway.295 Notch-Dll/Jag is an indispensable pathway in the initial stage of physiological and pathological angiogenesis with visible advantages in anti-tumor therapy, but its complex mechanisms and its relationships with other factors are not well illustrated.
Ephrins/EphR
Ephrins/EphR is a unique kinase family in regulating the interaction between adjacent cells through typical bidirectional signal transduction (Fig. 3).296 Ligands ephrins (Eph receptor-interacting proteins) are divided into five glycosylphosphatidylinisotol (GPI) anchored A subunits and three B subunits that contain a transmembrane domain and a short cytoplasmic region.297 Eph (erythropoietin-producing hepatocellular carcinoma) receptors are the largest transmembrane RTK family, which consists of nine members of type A and four members of type B.296,298 In human body, Ephrins/EphR signaling pathway plays a vital role in cell morphogenesis, arteriovenous formation, nervous system development, tissue formation, tissue homeostasis, and various angiogenic processes.299–301 Among them, the most critical pathway is EphrinB2/EphB4, which potently promotes sprouting, vascular maturation, and revascularization in tumor angiogenesis, and also acts as an essential member of the VEGF-Dll4/Notch-EphrinB2/EphB4 cascade in angiogenesis.302 A study in 2020 demonstrated that EphrinB2 could involve angiogenesis and lymphangiogenesis through regulating internalization and activation of VEGFR-2 and endocytosis of VEGFR-3.302 In vitro over-expression of EphrinB2 increased the secretion of VEGF and tube formation in hypoxia conditions, resulting in excessive angiogenesis in HUVECs.303 EphB4 plays a role in regulating vessel sprouting and branching,304 and inhibition of EphB4 can effectively control micro-vessel density and cancer cell proliferation.305 Nevertheless, excessive inhibition of this receptor may aggravate hypoxia within TME, further stimulating the expression of VEGF and tumor aggressiveness.306 All these evidences indicate that regulation of this pathway is of great significance to anti-angiogenic therapy. And it much remains to be understood about the mechanisms and signaling processes of EphrinB2/EphB4 due to its complex nature, abilities for bidirectional signaling and numerous unknown functions.302 Other components in Ephrins/EphR family should also be concerned, in which various abnormal Ephrins/EphR signals have been detected in many cancerous tissues. For example, EphrinB2 is over-expressed in ovarian cancer, kidney cancer and melanoma, whereas EphrinA3 is up-regulated in squamous cell lung carcinoma (SCLC) and colon cancer.296 As for receptor subunits, EphB3, EphB4 and EphB6 are excessively activated in colon cancer, but EphA2, EphA3, EphA4, EphA6, and EphA7 are expressed at a high level in lung cancer.296
Adhesion molecules
Integrins
Integrins are major adhesion factors in the extracellular matrix, which engage in various cellular processes in the human body by regulating signaling transduction between cells and of these cells with the surrounding matrix (Fig. 3).307,308 Up to now, about 24 unique integrin heterodimers have been uncovered, which consist of 18 α subunits and 8 β subunits through non-covalent binding.309,310 Each integrin subunit includes a single transmembrane domain, an extracellular region, and a cytoplasmic region with a short chain.307 Unlike tyrosine kinase receptors, integrins without intrinsic kinase or enzymic activities rely on focal adhesion complexes to activate cellular signaling pathways. Under the mediation of soluble ligands, extracellular matrix (ECM), or cell surface bound ligands including growth factors, proteases, cytokines, structural constituents of the ECM (like collagen and fibronectin), plasma proteins, microbial pathogens, or receptors specific to immune cells, integrin plays a pivotal role in cell homeostasis, immunity, inflammation, infection, thrombosis, lymphangiogenesis, angiogenesis, and tumorigenesis within the complex human internal environment.311,312
In tumor angiogenesis, over-expressed αv integrins can be exploited by carcinomas to fight for vascular and stromal resources to encourage tumor progression and canceration. αvβ6 integrin is the first adhesion factor among αv integrins shown to have angiogenic effects and is widely expressed on activated vascular ECs within remodeling and pathological tissues. αvβ3 is an indispensable factor in angiogenesis initiated by bFGF and TNF-α signaling pathways, while αvβ5 is required for angiogenesis mediated by TGF-α and VEGF.307 Besides, αvβ5 modulates the role of VEGF in promoting vascular permeability and tumor metastasis.263 In some early preclinical studies, antibodies target αvβ3 and αvβ5 integrins prevented tumor angiogenesis and metastatic spread, supporting both of them serve as targets for anti-angiogenic therapy in cancer.313–316 In addition to αvβ3 and αvβ5 integrins, α1β1, α2β1, α4β1, α5β1, α9β1, α6β1, and α6β4 mediate tumor angiogenesis in different manners. For example, α4β1 maintains the stability of endothelial cells and pericytes under the mediation of pro-angiogenic factors VEGF, bFGF, and TNF-α to support tumor angiogenesis.317 Integrin α5β1 and its ligand fibronectin can be up-regulated in angiogenesis mediated by bFGF and IL-8.318 Integrin α9β1 promotes tumor angiogenesis in a VEGF-dependent way and regulates lymphangiogenesis by interacting with VEGF-C and VEGF-D.319 Although the biological functions and mechanisms of integrins are such complex, the future of anti-integrin in anti-angiogenic therapy is promising owing to crucial and fundamental roles in tumor angiogenesis and lymphangiogenesis.
Proteinases
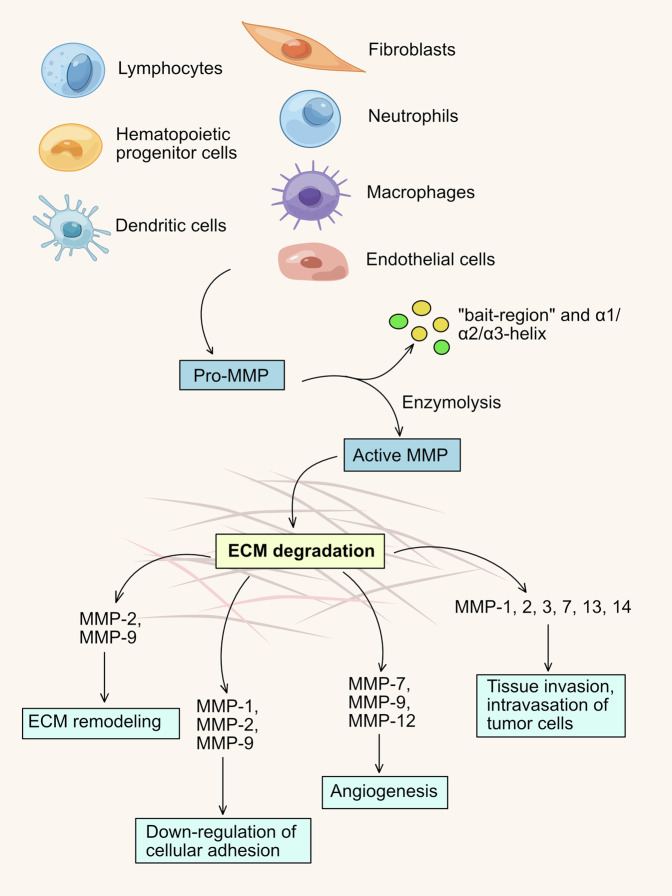
MMPs
Matrix metalloproteinases (MMPs) are a family of zinc- and calcium-dependent endopeptidases secreted by connective tissue and stromal cells, like fibroblast, ECs, macrophages, osteoblasts, lymphocytes and neutrophils (Fig. 5).320 In various angiogenesis, MMPs are dominant mediators in destroying ECM and remodeling the basement membrane, which enzymatically degrades the peptide bonds of collagen, elastin, laminin, and fibronectin.321 MMPs are attractive targets in anti-angiogenic and anti-tumor therapy. All members within the MMPs family are precursor enzymes that require proteolysis to be effective, including collagenases, gelatinases, stromelysins, matrilysins, and MMP membrane-type (MT)-MMPs.322 The major subunits involved in tumor angiogenesis are MMP-2, MMP-9 and MMP-14.323 MMP-2 is a 72 kDa gelatinase A or type IV collagenase that degrades types I and IV collagen. MMP-9 is a 92 kDa gelatinase B or type IV collagenase and MMP-14 is a type 1 membrane matrix metalloproteinase (MT1-MMP) that can degrade multiplicate extracellular matrix components.81,321 MMP-9 is the central protease for extracellular matrix degradation, which increases the bioavailability of VEGF and recruits pericytes to maintain homeostasis in tumor microenvironment.324,325 The essential component type IV collagen and other matrix proteins are degraded by MMP-9, which induces basement membrane remodeling, triggers morphogenesis and sprouting of ECs to stimulate tumor angiogenesis.326 The importance of MMP-2 is that the deletion of MMP-2 controls the angiogenesis and growth of tumor in vivo.327 MMP-14 promotes vascular lumen formation and induces ECs to infiltrate tumor tissue.328,329 Besides, MMP-1 and MMP-7 play unique roles in tumor angiogenesis. MMP-1 is an interstitial or fibroblast-type collagenase that degrades interstitial types I-III collagen, whereas MMP-7 is a matrilysin. MMP-1 releases bFGF by degrading the basement membrane to induce tumor angiogenesis, while MMP-7 mediates ECs proliferation and up-regulates the expression of MMP-1 and MMP-2 to encourage tumor angiogenesis.330,331 In addition to regulating angiogenesis, MMPs contribute to the malignant progression of tumors based on EMT, which plays an irreplaceable role in tumor vasculogenesis, invasion and metastasis.332 EMT is a process in which the transition of epithelial cells to mesenchymal migratory phenotypes,333 involves the degradation of ECM and basement membrane and the destruction of adhesion in cell-cell or cell-matrix.322
Fig. 5.
MMP-expressing stromal cells and functions of MMPs in tumor microenvironment. MMP precursors which are secreted by endothelial cells, fibroblasts, and lymphocytes et al. converted into active MMPs through enzymolysis. Subsequently, active MMPs participate in different biological processes including angiogenesis and tissue invasion by degrading specific extracellular matrix components
Actually, the expression level of MMPs is maintained in a dynamic balance under the antagonism of endogenous tissue inhibitors of matrix metalloproteinases (TIMP), a family of multifunctional proteins. In addition to stabilizing MMPs, TIMPs are involved in erythrocyte proliferation and cell growth, including soluble TIMP-1, TIMP-2, TIMP-4, and insoluble TIMP-3.334 These inhibitory components have unique physiological roles in regulating endothelial cell growth and proliferation through MMP-independent pathways and inhibiting tumor angiogenesis.334–336 Moreover, as a cathepsin to promote angiogenesis, MMP has some anti-angiogenic potential. As a potent inhibitor of endogenous angiogenesis, angiostatin is a partial fragment of plasminogen that potently inhibits ECs proliferation.337 Coincidentally, before the 2000s, scientists found that MMP-7 could hydrolyze the Pro (466)-Val (467) peptides bond, and MMP-9 could hydrolyze the Pro (465)-Pro (466) bond between cyclic domains 4 and 5 of human plasminogen, finally producing angiostatin fragments with potential anti-angiogenic effects.81 Later, in 2002, studies reported that MMP-2/-3/-12 could cleave plasminogen to create angiostatin fragments, and MMP-3/-9/-13/-20 were related to the production of endostatin.338 The physiological and pathological functions of the MMPs family are significantly specific to different internal environments and a comprehensive study of their processes will be long-term research.
In an intricate angiogenic system, almost all biomolecules act in interrelated manners to activate the proliferation, survival, migration, and morphogenesis of target cells to excite tumor angiogenesis. Apart from the factors above and downstream pathways shown in Fig. 3, Apelin/APLNR family,339 Slit/Robo family,340 adrenomedullin,341,342 COX-2,343,344 CXC chemokines,345,346 interleukins,347 interferons,348–350 nitric oxide synthase (NOS),351 pleiotrophin (PTN),352 steroid hormones,353 thrombospondin (TSP),354,355 and many other molecules also involve tumor angiogenesis to encourage tumor progression. The specific roles and mechanisms of these biomolecules in angiogenesis and tumorigenesis will gradually be explored by researchers.
Anti-angiogenic therapy: a valuable strategy for cancer treatment
The concept of angiogenesis has been proposed for more than 50 years, and the initial understanding is only “angiogenesis in tumor”: the growth, survival and proliferation of tumor rely on angiogenesis after the tumor beyond a certain volume. At present, this theory has been extended to various non-neoplastic diseases such as cardiovascular disease, rheumatoid arthritis (RA), and diabetic retinopathy.
The formation of new blood vessels has been observed since the earliest time, especially wound healing. But this process has only ever been regarded as a simple pathological or physiological process unrelated to malignancies. In the 1860s, some researchers have observed the development of blood vessels presents as a scattered pattern of branches,356,357 and pathologist Virchow also described a rich vascular network in tumors in his Die Krankhaften Greschwulste.358 Then in the 1960s, Greenblatt et al. used the “tumor angiogenesis” firstly and proposed that tumors could produce soluble angiogenic substances.359 Professor Folkman carried out related research in the following years based on previous achievements of others, and in 1971 proposed that “tumor growth depends on angiogenesis, and anti-angiogenic substances can treat tumors”. Although this hypothesis attracted little scientific interest, Folkman persisted research and successfully cultured ECs in capillaries, which facilitated multiple classical angiogenic models, such as chick chorioallantoic membrane (CAM) and corneal transplantation models.360,361
Among the 1980s, people gradually realized indeed angiogenesis in tumors, but did not believe that it could be a therapeutic target, and most people still insisted that “it is an inflammatory response from tumor necrosis”, “it is the defense response of host to tumors”, and “new blood vessels in tumor will gradually mature like normal blood vessels”. Until 1983, Senger et al. discovered that vascular permeability could be enhanced by a substance derived from tumors named vascular permeability factor (VPF), which was shown to have a strong angiogenic effect in subsequent scientific research, and was re-named as vascular endothelial growth factor (VEGF).362 In 1984, the first tumor-derived pro-angiogenic factor from chondrosarcoma was successfully isolated by Shing et al. and named as basic fibroblast growth factor (bFGF).363 Then in the following years, tumor-dependent angiogenesis was testified by a large number of experiments, anti-angiogenic therapy was more possible, and Folkman’s theory was recognized by some researchers. Followed by some major events in the field of angiogenesis: discovery to withdrawal of drugs such as TNP-470, the discovery of the anti-angiogenic effect of thalidomide,364 and the development of angiostatin and endostatin, the theory of tumor angiogenesis was generally accepted, and more researchers devoted to anti-angiogenic therapy.
In earlier studies, scientists believed that serious toxic effects and drug resistance would not develop in anti-angiogenic therapy because angiogenic inhibitors targeted genetically stable vascular ECs rather than tumor cells.358,365 Traditional anti-angiogenic therapy on the basis of “starving tumors”, which obstructed the energy supply for tumor tissue by blocking angiogenesis to guide the death of tumor cells.366 In 2004, the first anti-angiogenic drug bevacizumab (Table 1) approved by FDA significantly prolonged the PFS rates of RCC patients in combination with chemotherapy, and in the following years, other anti-angiogenic drugs were launched. Although some positive results were achieved, the clinical benefits did not meet expectations, the PFS rates of patients improved modestly, the improvement of OS rates were minimal, and even in some failed cases, it was observed that the toxicity suffered by the patients far more than the treatment effects. For example, in November 2010, the FDA withdrew the approval of bevacizumab (Avastin®) for the treatment of HER2 negative metastatic BC based on four disappointing clinical trials: serious adverse events (like hypertension and organ failure) and minimal treatment benefits among BC patients treated with bevacizumab.
Although numerous perspectives and reflections rose in anti-angiogenic therapy,367,368 proponents continued anti-angiogenic research and found that excessive limitation of angiogenesis not only affects the transportation of drugs but also exacerbates pathological manifestations of TME, inducing stronger hypoxic responses and aggressiveness of tumor, and eventually causing drug resistance or even cancer metastasis.369 Because of the high-permeability and distortion of tumor vessels, complexity and unpredictable changes of tumor tissue, these shortcomings are understandable for an emerging treatment method, which have also motivated more in-depth research. In the 2000s, Rakesh K. Jain twi-proposed “tumor vascular normalization to improve the delivery of drugs and oxygen” based on previous research to impel anti-angiogenic therapy (Fig. 6).370,371 Vascular normalization means that the disordered condition of tumor angiogenesis can be back to the normal state through measurable anti-angiogenic agents. As a result, the functional and morphological characterizations of the vessels are restored to a more normal condition, and the TME is more stable, finally improving drug transportation and delaying drug resistance and aggressiveness.372 According to clinical and preclinical research, the effects of vascular normalization are closely related to the “time window”.50 It indicates the period during which the blood vessels exhibit a normal phenotype after proper drug administration. During the “time window”, anti-tumor drugs might be more easily transported to tumor tissue through blood circulation, which may be quite beneficial to tissue concentration and efficacy of drugs.373 Despite several conventional angiogenic inhibitors that have been demonstrated effective in remodeling the tumor blood vessels, vascular normalization is still hard to maintain for a long time.374,375 Almost two decades, considerable efforts to optimize angiogenic inhibitors, administration regimens and medical detection methods, in order to prolong the “time window” of vascular normalization, and maximize the benefits of anti-angiogenic drugs and the efficacy of tumors to chemotherapy, radiotherapy and immunotherapy. Li et al. comprehensively evaluated imaging methods that commonly used to detect vascular changes in tumor tissue.376 Viallard et al.,26 R. Zheng et al.,377 and Luo et al. suggested some promising strategies to optimize vascular normalization.378 Anti-angiogenic therapy is a promising therapeutic method mixed with benefits and challenges. The timeline of milestones regarding the research on tumor angiogenesis are shown in Fig. 7.
Fig. 6.
Diagramatic illustrations of the relationship between tumor blood vessels, pro-angiogenic and anti-angiogenic factors. a Blood vessels with regularity and completeness depend on dynamic balance of pro-factors and anti- factors in normal tissues. b Abnormal vessels with chaos, leakage and feeble blood circulation are caused by imbalance of mediators in tumor tissue. c Blood vessels are repaired through neutralizing abundant pro-factors or increasing anti-factors under the guidance of angiogenic inhibitors. d Blood vessels in tumor tissue are destroyed by excessive inhibitors, which aggravates hypoxia within tumor tissue and hinders drug transportation
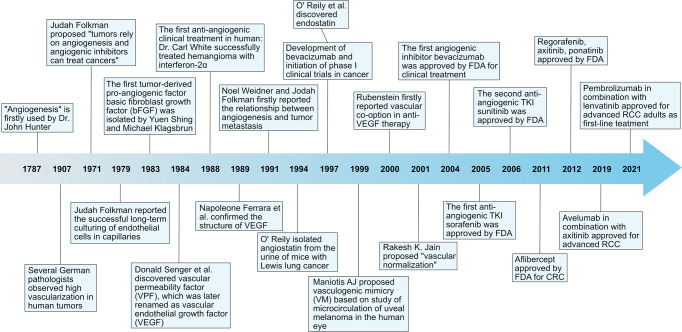
Fig. 7.
Timeline of the milestones regarding the research on tumor angiogenesis
The development of angiogenic inhibitors for anti-tumor therapy
Anti-angiogenic therapy is achieved by inhibiting tumor growth and metastasis through anti-angiogenic drugs to limit the blood supply to tumor tissue. Although molecular and mechanistic studies have indicated that numerous regulators engaged in tumor angiogenesis, research on angiogenic inhibitors still focuses on VEGF/VEGFR signaling pathway due to its dominance in the angiogenic system. Among them, recombinant monoclonal antibodies and small molecule tyrosine kinase inhibitors are the mainstream drugs used in anti-angiogenic treatment. Inhibitors approved for anti-angiogenic therapy are summarized in Table 1, and potential agents evaluated in clinical trials are described in Table 2.
Table 2.
Current status of potential angiogenic inhibitors in clinical development
| Agents | Targets | Phase | Status | Conditions or diseases | Trial ID |
|---|---|---|---|---|---|
| Antibodies | |||||
| Bemarituzumab (FPA144) | FGFR-2 | I | Not yet recruiting | Solid tumors (unspecified) | NCT05325866 |
| III | Recruiting | GC or CEJ adenocarcinoma | NCT05052801 | ||
| JY-025 | VEGFR-2 | II/III | Not yet recruiting | NSCLC with EGFR 19 exon deletion or 21 exon mutation | NCT04874844 |
| BAT-5906 | VEGFR | III | Not yet recruiting | wAMD | NCT05439629 |
| II | Completed | wAMD | NCT05141994 | ||
| I/II | Recruiting | DME | NCT04772105 | ||
| Olinvacimab | VEGFR-2 | II | Recruiting | Metastatic TNBC | NCT04986852 |
| I/II | Not yet recruiting | Metastatic CRC who failed two prior standard chemotherapies | NCT04751955 | ||
| Ak109 | VEGFR-2 | I/II | Recruiting | Advanced solid tumor | NCT05142423 |
| I/II | Recruiting | Advanced gastric adenocarcinoma or GEJ adenocarcinoma | NCT04982276 | ||
| I | Unknown | Advanced solid tumors | NCT04547205 | ||
| CTX-009 (ABL001) | VEGF-A, Dll-4 | I/II | Recruiting | Advanced or metastatic solid tumors; unresectable advanced, metastatic or recurrent BTC | NCT04492033 |
| NOV-1105 (YYB-101) | HGFR | I/II | Recruiting | Metastatic or recurrent CRC | NCT04368507 |
| MCLA-129 | c-Met, EGFR | I/II | Recruiting | Advanced NSCLC or other solid tumors | NCT04930432 |
| I/II | Recruiting | Metastatic or advanced NSCLC, HNSCC or other solid tumors | NCT04868877 | ||
| SYD-3521 (BYON3521) | c-Met | I | Recruiting | Locally advanced or metastatic solid tumors | NCT05323045 |
| VRDN-001 | IGF-1 | I/II | Recruiting | TED | NCT05176639 |
| Oligonucleotide agents | |||||
| IGV-001 | – | II | Not yet recruiting | GBM or GBM multiforme | NCT04485949 |
| Anti-angiogenic fusion proteins | |||||
| 9MW-0813 | VEGFR | III | Recruiting | DME | NCT05324774 |
| I | Completed | DME | NCT05324592 | ||
| Tyrosine kinase inhibitors | |||||
|
Surufatinib
|
VEGFR-1/-2/-3, CSF1R, FGFR-1 | II | Recruiting | Advanced CRC who failed front-line anti-angiogenic TKI therapy | NCT05372198 |
| II | Recruiting | Advanced HCC | NCT05171439 | ||
| II | Recruiting | HR+ unresectable metastatic BC refractory to endocrine therapy | NCT05186545 | ||
| II | Recruiting | High-grade advanced-neuroendocrine neoplasm | NCT05165407 | ||
| II | Not yet recruiting | Inoperable or metastatic advanced intrahepatic cholangiocarcinoma (ICC) | NCT05236699 | ||
| II | Not yet recruiting | OC with platinum-resistance and received prior PARP inhibitors | NCT05494580 | ||
| II | Not yet recruiting | Advanced gastric adenocarcinoma or GEJ adenocarcinoma | NCT05235906 | ||
|
Avapritinib (BLU-285)
|
PDGFR-α, c-Kit | - | Approved | Locally advanced unresectable or metastatic GIST | NCT03862885 |
| IV | Active, not recruiting | GIST | NCT04825574 | ||
| II | Recruiting | Locally advanced or metastatic malignant solid tumors with c-Kit or PDGFR-α mutation-positive | NCT04771520 | ||
| II | Recruiting | Chinese patients with GIST | NCT05381753 | ||
| II | Active, not recruiting | Indolent systemic mastocytosis | NCT03731260 | ||
| I/II | Recruiting | Solid tumors with mutations in c-Kit or PDGFR-α, or gliomas with the H3K27M mutation | NCT04773782 | ||
| I/II | Active, not recruiting | Chinese subjects with unresectable or metastatic GIST | NCT04254939 | ||
| I | Recruiting | Metastatic or unresectable GIST, recurrent gliomas, or other c-Kit mutant tumors | NCT04908176 | ||
|
Olverembatinib (GZD824)
|
Bcr-Abl, c-Kit | III | Recruiting | CML in chronic phase who are resistant and/or intolerant to at least two second-generation tyrosine kinase inhibitors | NCT05311943 |
| II | Recruiting | Myeloproliferative neoplasms, ALL or AML with FGFR1 rearrangement | NCT05521204 | ||
| II | Recruiting | Advanced CML | NCT05376852 | ||
| II | Not yet recruiting | Ph+ ALL | NCT05466175 | ||
| I | Not yet recruiting | Relapsed or refractory Ph+ ALL | NCT05495035 | ||
|
Pemigatinib
|
FGFR-1/-2/-3 | III | Recruiting | Unresectable or metastatic cholangiocarcinoma with FGFR2 rearrangement | NCT03656536 |
| II | Completed | Advanced/Metastatic or surgically unresectable cholangiocarcinoma with FGFR2 translocations who failed previous therapy | NCT02924376 | ||
| II | Recruiting | Previously treated GBM or other primary central nervous system tumors with FGFR1–3 alterations | NCT05267106 | ||
| II | Recruiting | GBM, or other primary CNS tumors, or adult-type diffuse gliomas with FGFR mutation | NCT05267106 | ||
| II | Recruiting | Advanced NSCLC with FGFR alterations who have failed standard therapy | NCT05287386 | ||
| II | Recruiting | Advanced GC or CRC with FGFR alterations who have failed standard therapy | NCT05202236 | ||
| II | Recruiting | HER2 negative advanced BC with FGFR 1–3 alterations who have failed standard therapy | NCT05560334 | ||
| II | Recruiting | Advanced gastrointestinal cancer (excluding BTC) with FGFR 1–3 alterations who have failed standard therapy | NCT05559775 | ||
| II | Recruiting | Relapsed or refractory advanced NSCLC with FGFR mutation | NCT05253807 | ||
| II | Active, not recruiting | Advanced or unresectable CRC with FGFR mutation | NCT04096417 | ||
| II | Active, not recruiting | Advanced, metastatic or unresectable cholangiocarcinoma | NCT04256980 | ||
|
Futibatinib
|
FGFR-1/-2/-3/-4 | III | Recruiting | Advanced, metastatic, or recurrent unresectable cholangiocarcinoma harboring FGFR2 gene rearrangements | NCT04093362 |
| III | Recruiting | Advanced or metastatic STS | NCT03784014 | ||
| II | Recruiting | Advanced or metastatic HCC with FGF19 positive | NCT04828486 | ||
| II | Recruiting | Advanced/metastatic GC or GEJ cancer, myeloid or lymphoid neoplasm, or other solid tumors with FGFR1 mutation | NCT04189445 | ||
| I/II | Recruiting | Advanced NSCLC, or other advanced or metastatic solid tumors with KRas mutation | NCT04965818 | ||
| I/II | Recruiting | HER2 mutated NSCLC or other advanced solid tumors | NCT05532696 | ||
|
Rogaratinib
|
FGFR-1/-2/-3/-4 | II/III | Completed | Locally advanced or metastatic urothelial carcinoma with FGFR-positive | NCT03410693 |
| II | Completed | Cancer (unspecified) | NCT04125693 | ||
| II | Recruiting | Advanced GIST, STS | NCT04595747 | ||
| II | Active, not recruiting | Pretreated advanced SQCLC | NCT03762122 | ||
| I | Completed | FGFR positive refractory, locally advanced or metastatic solid tumors | NCT03788603 | ||
| I | Recruiting | Metastatic FGFR1/2/3 positive, hormone receptor positive BC | NCT04483505 | ||
|
Erdafitinib
|
FGFR-1/-2/-3/-4 | IV | Recruiting | Bladder cancer with FGFR mutation | NCT05052372 |
| II | Recruiting | Recurrent non-invasive bladder cancer with FGFR3 mutation | NCT04917809 | ||
| II | Recruiting | NSCLC with FGFR genetic alterations | NCT03827850 | ||
| II | Recruiting | Advanced solid tumors with FGFR alterations | NCT04083976 | ||
| II | Active, not recruiting | Advanced urothelial cancer with selected FGFR aberrations | NCT05564416 | ||
| I/II | Recruiting | Relapsed refractory multiple myeloma | NCT03732703 | ||
| I | Recruiting | Bladder cancer with FGFR genetic alterations | NCT05316155 | ||
| I | Recruiting | Metastatic urothelial carcinoma with alterations in FGFR 2/3 genes | NCT04963153 | ||
|
Telatinib
|
PDGFR-β, c-Kit, VEGFR |
II | Unknown | Advanced HER2 negative advanced gastric or GEJ adenocarcinoma | NCT03817411 |
| II | Recruiting | Advanced GC, GEJ adenocarcinoma, or HCC | NCT04798781 | ||
|
Tepotinib
|
c-Met | II | Recruiting | Solid tumors with Met amplification or Met exon 14 skipping mutation | NCT04647838 |
| II | Recruiting | Advanced or metastatic NSCLC with Met amplifications | NCT03940703 | ||
| I/II | Recruiting | Advanced NSCLC with Met mutation | NCT04739358 | ||
| I/II | Recruiting | advanced GC, GEJ cancer with Met amplified or Met exon 14 alternated | NCT05439993 | ||
| I | Completed | Patients with hepatic impairment | NCT03546608 | ||
| I | Not yet recruiting | Brain tumors with Met alternations | NCT05120960 | ||
ALL acute lymphoblastic leukemia, AML acute myeloid leukemia, BC breast cancer, BTC biliary tract cancer, CML chronic myeloid leukemia, CRC colorectal cancer, DME diabetic macular edema, GEJ gastroesophageal junction, GBM glioblastoma, GC gastric cancer, GIST gastrointestinal stromal tumor, HCC hepatocellular carcinoma, HER2 human epidermal growth factor receptor 2, HNSCC head and neck squamous cell carcinoma, NSCLC non-small cell lung cancer, PARP poly ADP-ribose polymerase, Ph+ AML Philadelphia chromosome-positive acute myeloid leukemia, RCC renal cell carcinoma, SQCLC squamous-cell non-small cell lung cancer, STS soft tissue sarcoma, TNBC triple-negative breast cancer, TED thyroid eye disease, wAMD wet age-related macular degeneration
Angiogenic inhibitors approved by FDA for clinical treatment
Anti-angiogenic monoclonal antibodies
Monoclonal antibodies are derived from artificially prepared hybridoma cells, which have the advantages of high purity, high sensitivity, strong specificity, and less cross-reactivity. When compared with kinase inhibitors, these immanent unique advantages in clinical treatment are comparatively beneficial to patients. The most representative antibody is bevacizumab (Avastin®) (Table 1). In 1993, anti-VEGF monoclonal antibody trials demonstrated that inhibitors targeting VEGF could decrease tumor growth, provoking scientists to investigate the clinical efficacy of bevacizumab. Known as the first formal angiogenic inhibitor, bevacizumab is a macro-molecular recombinant human monoclonal antibody that obstructs the transduction of VEGF pathway by neutralizing all VEGF isoforms to inhibit tumor angiogenesis.379 In a phase III clinical trials with IFL treatment (combination of irinotecan, fluorouracil (5-FU), and leucovorin), the PFS rate of previously untreated metastatic CRC patients increased from a median of 6.2 months to 10.6 months, the OS rate increased from 34.8% to 44.8%, and the median duration of response increased 3.3 months owing to the addition of bevacizumab.380 Hence, bevacizumab was approved by FDA for patients with CRC in 2004. In addition to the first indication, bevacizumab has been approved for a variety of other cancers as monotherapy, as a surgical adjuvant, or in combination with chemotherapy, and more potential in anti-angiogenic therapy is being tested through clinical trials.381 Moreover, because of excellent anti-angiogenic activity, bevacizumab has achieved satisfactory results in several clinical trials by combining multiple chemotherapy drugs to treat recurrent or metastatic malignant tumors. For example, the combination of bevacizumab, carboplatin, and paclitaxel (or gemcitabine) was approved by FDA for later treatment after bevacizumab monotherapy in platinum-sensitive recurrent epithelial ovarian cancer in 2016.44,75 Then in 2020, bevacizumab was approved for untreated locally advanced or metastatic RCC in combination with monoclonal antibody atezolizumab, an immune checkpoint inhibitor of PD-L1.75 Bevacizumab is an anti-angiogenic drug with excellent research and application value, which has great potential for emerging combination therapies to synergy chemotherapeutic drugs and immune checkpoint inhibitors.
Ramucirumab (Cyramza®) is a fully humanized IgG1 antibody with a weight of 147 kDa, which targets the extracellular binding domain of VEGFR-2 to disturb the potent VEGF signal in tumor angiogenesis (Table 1).382,383 As the first antibody targeted VEGFR-2, ramucirumab significantly improved the median OS (5.2 months vs. placebo 3.8 months) and PFS (2.1 months vs. placebo 1.3 months) rates of patients (adults with advanced or unresectable gastric and gastroesophageal junction adenocarcinoma) in a prospective, double-blind and placebo-controlled a phase III REGARD clinical trial. Furthermore, it prolonged the median OS (9.6 months vs. 7.4 months) and PFS (4.4 months vs. 2.86 months) rates of homogeneous patients in a randomized, double-blind and placebo-controlled a phase III RAINBOW trial through a combination with paclitaxel.382 In 2014, ramucirumab was approved by FDA for previously treated advanced gastric or gastroesophageal junction (GEJ) adenocarcinoma. Additionally, the first-line therapy for metastatic CRC is a combination of ramucirumab and a modified FOLFOX-6 regimen (mFOLFOX-6), which demonstrated gratifying safety and efficacy in a phase II clinical trial (NCT00862784).384
Olaratumab (Lartruvo®) is a 154 kDa fully recombinant human IgG1 monoclonal antibody with high affinity to PDGFRα, which is the first-line drug approved by FDA for soft tissue sarcoma (STS) (Table 1).385 STS is a relatively rare malignancy that occurs in connective tissue. In a randomized ANNOUNCE clinical trial among 509 patients, the addition of olaratumab did not significantly improve the OS rate (doxorubicin plus olaratumab 20.4 months vs. doxorubicin plus placebo 19.7 months) of advanced STS patients.386,387
Bevacizumab-awwb (Mvasi®) is the first anti-tumor biosimilar of bevacizumab approved by FDA.388,389 Ranibizumab (Lucentis®) is a 48 kDa humanized anti-VEGF monoclonal antibody fragment, which can bind all VEGF-A isoforms, including VEGF110, VEGF121, and VEGF165 (Table 1). Ranibizumab is a prevalent anti-angiogenic agent in treating oculopathy (Table 1).
Anti-angiogenic oligonucleotide derivatives
Oligonucleotides are nucleic acid polymers that regulates gene expression and have specially designed sequences, including antisense oligonucleotides (ASOs), siRNA (small interfering RNA), microRNA and aptamers. Pegaptanib (Macugen®) is a 50 kDa VEGF-A targeted RNA aptamer, which has been approved for angiogenic age-related macular degeneration in December 2004, leading to good tolerability and negligible local adverse effects of AMD patients through intravitreous injections (Table 1).390
Anti-angiogenic recombinant fusion proteins
Fusion proteins are complexes from binding the Fc segment of immunoglobulin to a biologically active functional protein molecule through genetic engineering technology. Aflibercept (Eylea®) is a recombinant decoy receptor targeted VEGF, which is combined of the extracellular VEGFR domain (VEGFR-1 Ig2 region and VEGFR-2 Ig3 region) and the Fc segment of human immunoglobulin G1 (IgG1) and has long half-life in anti-angiogenesis (Table 1). Aflibercept inhibits the binding and activation of the VEGF family and natural VEGFR by specifically blocking VEGF-A and most proangiogenic cytokines, thereby inhibiting division and proliferation of ECs, reducing vascular permeability, and is commonly used in non-neoplastic angiogenic disease like AMD, DR, and DME.380,391 Ziv-aflibercept is an adaptive variant of aflibercept, which has lower pH and higher osmolality (Table 1). It has been approved by FDA for the treatment of metastatic CRC patients who are resistant to or have progressed following an oxaliplatin-containing regimen.392–394
Anti-angiogenic mTOR inhibitor
Everolimus (RAD001) is an oral analog of rapamycin that inhibits proliferation and induces apoptosis and autophagy of tumor cells through indirectly blocked mTOR (Table 1). mTOR is a serine/threonine (Ser/Thr) kinase, which plays a pivotal role in tumor cell proliferation and angiogenesis through cooperating with PI3K/AKT signaling pathway.395 Everolimus forms a complex with cyclophilin FKBP-12 to specifically bind mTOR, and then inhibits downstream signals through composing the mTORC1 with raptor and mLST8.396 In a phase II clinical trial in predominantly clear cell RCC patients who had received pre-treatment or less, and had progressive measurable metastatic disease, everolimus achieved some surprising results with a median PFS of 11.2 months and a median OS of 22.1 months.397 In a randomized, double-blind, and placebo-controlled phase III trial (NCT00410124), everolimus prolonged PFS rate of metastatic CRC patients whose disease had deteriorated after being treated with VEGFR-2 inhibitors sorafenib or sunitinib, contributing to the launch of everolimus.397
Temsirolimus (Table 1) is the other small molecule inhibitors of mTOR, and part of the PI3K/AKT pathway involved in tumor cell proliferation and angiogenesis approved by FDA for advanced RCC. And it also approved for relapsed or refractory mantle cell lymphoma/non-Hodgkins lymphoma by European Union.
Anti-angiogenic immunosuppressants
Thalidomide (Thalomid®) was synthesized by the CIBA pharmaceutical company in 1954 and was initially used for mitigating morning sickness as a non-addictive and non-barbiturate tranquilizer (Table 1).398 However, it was withdrawn by FDA due to serious teratogenic events (fundamentally attributed to chiral isomers) reported in the early 1960s. But the research on thalidomide was not terminated, in 1998, thalidomide was approved for erythema nodosum leprosum (ENL) after a series of pharmacological studies.399 Concurrently, the metabolite of thalidomide was shown to have anti-microvessel formation activity both in human and rabbit models.400 And it was not until 2006 that thalidomide received approval from FDA for multiple myeloma (MM) based on a phase III clinical trial combined with dexamethasone.401 Another unexpected harvest is that thalidomide sensitizes icotinib to increase apoptosis and prevent migration in humanized NSCLC cell lines PC9 and A549, indicating that it has the potential to treat lung cancer.402
Lenalidomide (Revlimid®) was invented to reduce toxicity and enhance efficiency of thalidomide, which can specifically inhibit the growth of mature B cell lymphomas (like MM) and induce IL-2 release from T cells (Table 1).403,404 In addition to anti-MM treatment, lenalidomide has been approved by FDA for mantle cell lymphoma (MCL) in 2013, because it demonstrated consistent efficacy and safety of heavily pretreated patients with advanced-stage relapsed/refractory MCL in multiple phase II trials.405
Angiogenic small molecule TKIs
Since the first kinase inhibitor imatinib significantly reduced adverse events and improved the prognosis of patients with chronic myeloid leukemia (CML) in 2001,381 the importance of kinases in tumorigenesis has attracted wide attention. In the early years, tyrosine kinase inhibitors approved for anti-angiogenesis were developed with different spectrums of tyrosine kinases (Table 1), which block receptors phosphorylation and suppress transduction of downstream signaling pathways (PI3K/AKT/mTOR, Ras/Raf/MEK/ERK, p38 MAPK, and JAK/STAT, shown in Fig. 4) by specifically blocking transmembrane receptors, inhibiting angiogenesis and progression of the tumor.
Originally defined as a Raf inhibitor, sorafenib was obtained from a long period of high-throughput screening (HTS) and four-step structural modification.406,407 Sorafenib (Table 1) is an orally available type II multi-targeted angiogenic inhibitor with pyridine carboxamide (Raf1 IC50 = 6 nM, bRaf IC50 = 22 nM, bRafV600E IC50 = 38 nM, VEGFR-1/-2/-3 IC50 = 26/90/20 nM, PDGFR-β IC50 = 57 nM), which deactivates downstream Ras/Raf/MEK/ERK pathway by blocking Raf and the autophosphorylation of kinase receptors including VEGFR, PDGFR, c-Kit, and RET, subsequently inhibiting proliferation, invasion, metastasis, and angiogenesis of the tumor.408,409 In December 2005, sorafenib was approved by FDA for patients with advanced RCC according to a phase II TARGET clinical trial, in which sorafenib improved PFS rate (5.5 months) of advanced clear-cell RCC patients compared with a placebo (2.8 months) alone (NCT00073307).410 However, the toxicity increased a lot due to the pan-inhibition of multiple kinases. As the first anti-angiogenic small molecule tyrosine kinase inhibitor, sorafenib remarkably promoted the subsequent development and clinical research of anti-angiogenic small molecule agents, in order to enhance the selectivity and efficacy of the drugs and reduce toxicity.
Sunitinib is an indole-2-one multi-targeted kinase inhibitor from HTS that targets VEGFR-1/-2/-3 (VEGFR-2 IC50 = 80 nM), Flt-3, c-Kit, RET, PDGFR-α/-β (PDGFR-β IC50 = 2 nM) (Table 1), and it was the first TKI approved for treating patients with advanced pancreatic neuroendocrine tumors (pNET) based on a randomized phase III trial (NCT00428597).411 Besides, sunitinib became the first and only adjuvant treatment approved by FDA in 2017 for adult patients with high-risk recurrent RCC after nephrectomy because the median disease-free survival (DFS) was increased by 1.2 years in a double-blind phase III clinical trial (NCT00375674).412
Pazopanib (Table 1) is an oral angiogenic inhibitor that primarily inhibits VEGFR-1 (IC50 = 10 nM), VEGFR-2 (IC50 = 30 nM), VEGFR-3 (IC50 = 47 nM), PDGFR-α (IC50 = 71 nM), PDGFR-β (IC50 = 84 nM), and the stem-cell factor receptor c-Kit (IC50 = 74 nM).413,414 Pazopanib was firstly enrolled in clinical treatment by FDA for patients with advanced RCC on a basis of a randomized and double-blind phase III trial (NCT00334282), in which PFS rate was increased five months compared with placebo.415 However, the advantage of pazopanib was not shown in patients with advanced NSCLC in a phase III clinical trial (NCT01208064).416 The OS and PFS rates of patients who had received standard first-line platinum-based chemotherapy were not conspicuously improved, but several serious adverse events were increased obviously like hypertension.
Vandetanib (Table 1), a derivative of 4-anilinoquinazoline, which is an orally active angiogenic inhibitor with potent inhibitory efficacy against VEGFR-2 (IC50 = 40 nM), VEGFR-3 (IC50 = 10 nM), EGFR (IC50 = 0.5 μM), and Ret (IC50 = 0.1 μM) and other tyrosine kinases.417,418 However, vandetanib was initially marketed for NSCLC, which was withdrawn by the FDA due to disappointing phase III clinical trial results in 2009.419–421 Fortunately, vandetanib was approved for patients with unresectable locally advanced or metastatic MTC in 2011 based on moderate clinical results of enhancive median rates of OS and PFS (NCT00410761).422
Regorafenib is a potent VEGFR-2 inhibitor with pyridine carboxamide derived from sorafenib structural modifications (Table 1).423,424 In the kinase inhibition assay, regorafenib exhibits multiple kinase inhibition capabilities (VEGFR-1 IC50 = 13 nM, VEGFR-2 IC50 = 4.2 nM, VEGFR-3 IC50 = 46 nM, PDGFR-β IC50 = 22 nM, FGFR-1 IC50 = 202 nM, c-Kit IC50 = 7 nM, Ret IC50 = 1.5 nM, Raf1 IC50 = 2.5 nM).425 Regorafenib was firstly marketed in 2012 and approved by FDA for patients with metastatic CRC because it dramatically stabilized the disease of 207 patients (41%) in a crucial phase III clinical trial (NCT01103323).426 In 2017, the FDA expanded another indication of regorafenib for the treatment of HCC patients who had been treated with sorafenib (NCT01774344).427 In a latest study, the researcher reported that regorafenib could regulate macrophage polarization through the p38 kinase/Creb1/Klf4 pathway, enhancing anti-tumor immunity independent of the angiogenic process.428
Cabozantinib is a selective angiogenic inhibitor with a high affinity to VEGFR-2 (IC50 = 0.035 nM), c-Met (IC50 = 1.3 nM), c-Kit (IC50 = 4.6 nM), Tie-2 (IC50 = 14.3 nM), Flt-3 (IC50 = 11.3 nM), and Ret (IC50 = 5.2 nM), which is a bismethoxyquinoline analog (Table 1).429,430 Because of the ability to inhibit autophosphorylation of VEGFR-2 and c-Met, cabozantinib exhibited decent anti-tumor, anti-metastatic, and anti-angiogenic activities in preclinical models. Up to now, cabozantinib has been ratified for several most common angiogenic carcinomas (NCT01908426, NCT01865747).431,432 A randomized and open-label phase III clinical trial has shown that combination of immune checkpoint inhibitors with cabozantinib significantly improved the OS and PFS rates of patients with clear-cell and advanced RCC rather than sunitinib (NCT03141177).433
Lenvatinib, an oral quinoline multi-targeted kinase inhibitor against VEGFRs (VEGFR-2, IC50 = 4.0 nM and VEGFR-3, IC50 = 5.2 nM), PDGFRs, c-Kit (IC50 = 0.1 μM), RET, and FGFRs, inhibits angiogenesis induced by Ret mutation and lymphogenesis mediated by VEGFR-3 (Table 1).434,435 In 2016, the combination of lenvatinib with mTOR inhibitor everolimus (Table 1) was approved for advanced RCC (NCT01136733).436,437 In 2021, the combination of lenvatinib with pembrolizumab (PD-1 antibody) became the first-line treatment for adult patients with advanced RCC due to the significantly enhanced PFS and OS rates compared to sunitinib in a randomized phase III clinical trial with 1069 patients (NCT02811861).438 Whether the combination of lenvatinib and other immune checkpoint inhibitors can be used for HCC is in evaluation through several phases III clinical trials (NCT03713593, NCT04039607).439
Axitinib (Table 1) is a novel selective angiogenic inhibitor targeted VEGFR-1 (IC50 = 0.1 nM), VEGFR-2 (IC50 = 0.2 nM), VEGFR-3 (IC50 = 0.2 nM), PDGFR-α (IC50 = 5 nM), PDGFR-β (IC50 = 1.6 nM), and c-Kit (IC50 = 1.7 nM), which is currently only approved for RCC, and other indications are still in a exploratory stage.440 Ponatinib (Table 1) was originally designed as an ABL inhibitor targeted ALL and CML patients with T315I mutation (ABL, IC50 = 0.37 nM; ABLT315I, IC50 = 2 nM).441,442 It also potently inhibits angiogenesis-related kinases, such as VEGFR-1 (IC50 = 3.7 nM), VEGFR-2 (IC50 = 1.5 nM), VEGFR-3 (IC50 = 2.3 nM), PDGFR-α (IC50 = 1.1 nM), PDGFR-β (IC50 = 7.7 nM), FGFR-1 (IC50 = 2 nM), FGFR-2 (IC50 = 2 nM), FGFR-4 (IC50 = 8 nM), and others.443,444 Relevant research of ponatinib for other angiogenic cancers have not reported.445 Apatinib and nintedanib (VEGFR-2, IC50 = 13 nM) are potent angiogenic inhibitors with encouraging preclinical and clinical data in the treatment of various solid tumors through a high kinase inhibitory level (Table 1).446–450
Other inhibitors with anti-angiogenesis approved by FDA including: Interferon α (Intron® A and Roferon®), TAS-102 (Lonsurf®) and rhEndostatin (Endostar®/Endu-available only in China) from https://angio.org/.
Potential anti-angiogenic agents in the clinical evaluation in the latest three years
In recent years, research on highly selective targeted drugs has also made considerable progress in anti-angiogenic therapy (Table 2). Individual drugs have successfully passed preliminary clinical trials about the safety, tolerability and effectiveness of drugs, and entered into phase III or even phase IV clinical evaluation, such as bemarituzumab (FPA144), avapritinib and erdafitinib. (All of the drug information is from https://clinicaltrials.gov.)
Bemarituzumab (FPA144) is the first recombinant humanized IgG1 monoclonal antibody (Table 2), which obstructs ligand binding and downstream signaling activation by blocking the IgG III region of the FGFR-2b isoform.451 As a glycosylated derivative, bemarituzumab has a higher affinity for Fc γ receptor IIIa (FcγRIIIa), which is commonly expressed on immune cells like natural killer cells (NK cells) and macrophages. Owing to this natural property of lacking the FUT8 gene, bemarituzumab can enhance antibody-independent cell-mediated cytotoxicity (ADCC) against tumor models with FGFR-2b over-expression. In the early phase I clinical trials (NCT02318329, NCT03343301), the desirable safety, tolerance and pharmacokinetic characterization of bemarituzumab was demonstrated in gastrointestinal adenocarcinoma (GEA) and GC patients with FGFR-2b over-expression, leading to phase II clinical trial of bemarituzumab.452,453 In a randomized, double-blind, and placebo-controlled phase II trial (NCT03694522), the overall efficacy of bemarituzumab is satisfactory, although the median PFS rate only prolonged 2.1 months in patients with FGFR2b-selected GC or GEJ adenocarcinoma compared with the placebo group.454 The statistical significance of bemarituzumab will be testified in the randomized and double-blind phase III clinical trial in GC and GEJ patients with untreated advanced diseases (NCT05052801).
Avapritinib (BLU-285) is a selective and oral kinase inhibitor that targets PDGFR-α and c-Kit (Table 2), which has been approved by FDA for GIST, systemic mastocytosis, and solid tumors, especially for adult patients with metastatic or unresectable GIST carrying PDGFR-α 18 exon mutations.455 In xenograft models of GIST, the anti-tumor effects of avapritinib were significantly better than imatinib or regorafenib because avapritinib could potently obstruct the autophosphorylation of Kit D816V and PDGFR-α D842V, and activation of downstream signals like AKT and STAT3.456 In a two-part and open-label NAVIGATOR clinical trial (NCT02508532), avapritinib exhibited excellent anti-tumor efficacy, safety, and tolerance in unresectable GIST patients with PDGFR-α D842V mutation. The launch of avapritinib resulted in an unprecedented, durable clinical benefit to GIST patients with PDGFRA D842V-mutation.457–459 However, the overall effects of avapritinib were not superior to regorafenib in patients with locally advanced unresectable or metastatic GIST in a randomized VOYAGER phase III study (NCT02508532).460 The phase IV clinical trial has been planned to assess the effect of avapritinib on a larger group of participants. The most common adverse events include nausea, vomiting, decreased appetite, diarrhea, fatigue, cognitive impairment, hair color changes, lacrimation, abdominal pain, constipation, rash, and dizziness.
Erdafitinib (JNJ-42756493) (Table 2), a selective angiogenic TKI with high affinity to FGFR-1 (IC50 = 1.2 nM), FGFR-2 (IC50 = 2.5 nM), FGFR-3 (IC50 = 3.0 nM), and FGFR-4 (IC50 = 5.7 nM).461,462 As an FDA-accelerated drug, erdafitinib primarily aims to adult patients with locally advanced or metastatic urothelial cancer who carrying FGFR-2 or FGFR-3 gene mutations after platinum chemotherapy.463 Up to now, several phase II and phase III clinical trials in patients with bladder cancer are still ongoing (NCT03390504, NCT04172675, NCT02365597, NCT02465060, NCT03473743). The clinical potency of erdafitinib in NSCLC, lymphoma, cholangiocarcinoma, liver cancer, prostate cancer, esophageal cancer, or other carcinomas is undergoing investigation. Common adverse events include hyponatremia, oral mucosal disease, and weakness, but no treatment-related deaths.461,464 Similar to erdafitinib, pemigatinib, futibatinib and rogaratinib are also pan-FGFR tyrosine kinase inhibitors, which play a role in angiogenesis inhibition (Table 2). Moreover, these FGFR inhibitors inhibits cell proliferation in FGFR-addicted cancer cells with FGFR aberrations such as gene amplification, activating mutations and chromosomal translocations.465
Potential anti-angiogenic small molecules reported in the latest three years
In addition to the marketed and clinically evaluated anti-angiogenic drugs described previously, some novel TKIs have shown potent biological activity in the initial evaluation in kinase assay, which may be promising to become clinical candidates. Like compounds 23, 24, and 25, are selective inhibitors with good inhibitory activity targeted HIF-α. TME is a highly complex ecosystem of cellular and noncellular components, which is broadly related to tumor invasion and recurrence.466,467 In recent years, research on tumor microenvironment and targeted therapy has indicated that limiting tumor deterioration and angiogenesis by inhibiting HIF expression to downregulate the level of some angiogenic factors may be a valuable strategy.468–470 Table 3 summarizes the structures of reported molecules and related references, which could be beneficial to the research on angiogenic inhibitors.
Limitations and challenges of anti-angiogenic therapy
Angiogenic inhibitors used in cancer therapy by affecting the formation of new blood vessels in tumors, which have expended a new field for the treatment of a wide range of solid tumors. However, there are still some shortcomings in anti-angiogenic therapy due to the complex mechanisms of tumor angiogenesis and limited research, including tumor relapse,495 drug resistance,496,497 lack of bio-markers,496 short-acting efficacy,27,28 and several serious adverse events.498,499
Limited therapeutic efficacy
It was initially assumed that anti-angiogenic therapy might not be toxic compared with other chemotherapeutic agents owing to genetic stability and quiescence of ECs under normal physiological conditions and the selectivity of targeted drugs. However, this was proved to be a miscalculation. Common serious adverse events such as hypertension, proteinuria, lymphopenia, thrombocytopenia, leukopenia, neutropenia, and some physical abnormalities caused by different drugs have appeared in a number of different clinical treatments (Table 1), which may affect the tolerance of patients and even lead to treatment termination.45,54,500 This requires further optimization of the structures of angiogenic inhibitors to better target selectivity, or other techniques to increase drug delivery to tumor tissue while bypassing normal tissue, such as nano-preparations.
In addition, angiogenic inhibitors have a result on controlling growth and spread of tumor in the short term by blocking the blood supply (which is manifested in clinical treatment as increased PFS), but the long-term result is an increased risk of tumor local invasion and distant metastasis induced by hypoxia, as well as the probability of revascularization and tumor resurgence after discontinuation of sustained treatment (which manifests as an insignificant or even unchanged increase in OS).501,502 Some molecular events understood by researchers within the past few decades could be the activation of alternative pro-angiogenic molecules, the development of other angiogenic modalities, genetic or phenotypic mutations, stromal autophagy and induction of EMT.
Drug resistance
Drug resistance is a dominant difficulty that consistently limits the clinical outcomes in targeted anti-angiogenic therapy, which can be divided into congenital resistance and acquired resistance (Fig. 8).503 Congenital drug resistance is defined as the inherent insensitivity to drugs of patients, which may be related to the genes of patients and tumors. Acquired drug resistance has been comprehensively analyzed by researchers through cytological and molecular studies. These unique mechanisms include: (a) upregulation of compensatory pro-angiogenic signaling pathways in tumor tissue (HGF, bFGF, VEGF-C, PlGF, angiopoietins, and Dll-4 have been widely testified that upregulated in various tumors with drug resistance);133,504,505 (b) recruiting bone marrow-derived endothelial progenitor cells,506 pericyte progenitor cells,507 tumor-associated macrophages,508 and immature monocytic cells, which can maintain the formation of blood vessels; (c) recruitment of perivascular cells (like pericytes), which can cover immature tumor blood vessels to prevent destruction by anti-angiogenic drugs;509 (d) unconventional angiogenic processes like vessel co-option,510–513 vessel mimicry and intussusceptive angiogenesis.77,514,515 Additionally, drug resistance also involves high heterogeneity of tumor tissue and TME, endothelial heterogeneity,516 autophagy of tumor cells, differentiation of cancer stem cells,517 infiltration of stromal cells,518 tumor types, gene mutations of tumors or targets, development stage of the tumor, medication history of patients, and other factors, all of which can affect the response and tolerance of patients to anti-tumor therapy.
Fig. 8.
Mechanisms of drug resistance in anti-angiogenic therapy. Some patients are intrinsically non-responsive to anti-angiogenic therapy while other patients who are initially responsive acquire adaptive resistance. The mechanisms that manifest acquired resistance to anti-angiogenic therapy include: compensatory upregulation of alternative pro-angiogenic factors such as bFGF, PDGF, and PlGF within the tumor; recruitment of bone marrow-derived endothelial progenitor cells to facilitate neovascularization; increased pericyte coverage protects tumor blood vessels; autophagy helps tumor cells thrive in a hypoxic environment; increased invasiveness of the tumor promotes the distant metastasis and invasion of tumor cells through blood and lymphatic circulation. In addition, genetic mutations, vessel mimicry, vessel co-option, and intussusception angiogenesis also contribute to drug resistance
Lack of valid biomarkers
The application of biomarkers is a powerful adjuvant means which are essential for disease identification, early diagnosis and prevention, and drug treatment monitoring. Biomarkers refer to biochemical indicators of normal physiological or pathogenic processes to furnish the structural or functional changes of systems, organs, tissues, cells and subcells, and can also be used for disease diagnosis, disease stage, or evaluating the safety and efficacy of a drug or regimen among targeted population.519 In clinical practice, there are at least six categories of biomarkers including diagnostic, predictive, prognostic, pharmacodynamic, safety and monitoring biomarkers owing to different bio-functions. For example, HER2 is a diagnostic indicator for breast cancer typing, and levels of PD-L1 is used to predict the efficacy of immune checkpoint inhibitors (ICIs). Despite considerable efforts, there are few biomarkers responding to angiogenesis approved for clinical application.172,519,520 Given the variable results from anti-angiogenic treatments in the clinic, there is a need to characterize changes in the blood vessels and tumor microenvironment to detect and prevent tumor escape, and to monitor the patients’ response to drugs and the advances in treatment.521,522 It is an inevitable trend to explore effective cancer-specific biomarkers responding to angiogenic system to enhance the efficacy of anti-angiogenic regime and anti-cancer therapy. With the advancement in bio-analytical technology and clinical bio-chemistry, tissue and cell concentrations of some angiogenic mediators, circulating ECs, circulating progenitor cells, CT imaging of blood flow and blood volume have been shown to have potential as biomarkers, but more clinical trials are needed to validate their prospective. Developing efficient biomarkers for diagnosing the progression and stage of cancer and identifying mechanisms of tumor angiogenesis and drug resistance, in order to benefit drug selection, balance efficacy and toxicity, and simplify anti-cancer therapy. Actually, due to numerous factors such as the complexity of tumor angiogenesis, heterogeneity and variability of tumors, the unpredictability of response or toxicity, and limitations of preclinical and clinical trials, the development of biomarkers will be a great challenge.
Emerging approches to further improve anti-angiogenic therapy
Combination therapy
Since the first angiogenic inhibitor bevacizumab approved for treatment, combination therapy based on anti-angiogenic agents has infiltrated anti-tumor field.523 Combination therapy is a modality aiming to enhance anti-tumor efficacy through combining two or more therapeutic agents, including anti-angiogenic therapy combined with surgery, immunotherapy, chemotherapy, radiotherapy, genetherapy or (and) other targeted anti-tumor agents.524 Compared with monotherapy, the combination of anti-tumor drugs improves the therapeutic efficacy in a characteristically synergistic or an additive manner targeting important signaling pathway. Diversified methods in anti-cancer therapy provide more options for clinical treatment and make strong alliances possible.
In recent several years, one of the prevalent research direction is the combination of angiogenic inhibitors and immune checkpoint inhibitors, in which better clinical benefits from HCC and RCC patients treated with programmed cell death 1 (PD-1) and VEGFR-2 inhibitors than with monotherapy.467,525,526 Tumors can induce immune tolerance and limit proliferation and activation of T cells during growth and metastasis by using immune checkpoints (ICs) produced on T cells to accomplish immune escape. Blockade with different immune checkpoint inhibitors may activate the body’s immune system and weaken immunosuppression in TME against tumor cells by promoting the activation and proliferation of T cells, including PD-1, programmed cell death-ligand 1 (PD-L1) and cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) inhibitors.525 As mentioned before, the tumor microenvironment is composed of tumor cells, cancer stem cells, immune cells, fibroblasts and other cells and their secretions, as well as non-cellular components such as extracellular matrix. High levels of VEGF in TME are not only crucial factors in inducing abnormalization and increasing permeability of tumor vessels, but also weaken the anti-tumor effect of immune cells through multiple pathways including: a) immune-activating cells and immune effector cells can be effectively blocked by VEGF, such as inhibiting maturation of dendritic cells (DCs), and inducing the failure and apoptosis of cytotoxic T cells; b) the aggregation and activity of immunosuppressive cells including regulatory T cells (Tregs), myeloid-derived suppressor cells (MDSCs), M2-like tumor-associated macrophages (M2 TAM) can be up-regulated by intratumoral VEGF; c) by elevating the production of endothelial adhesion molecules and up-regulating immune checkpoints, VEGF can generate a selective endothelial barrier for cytotoxic T cells to prevent infiltration while facilitating the transport of immunosuppressive Tregs; d) redundant VEGF derived from tumor cells lead to disordered and leaky vascular networks, which seriously affects the blood transport of cytotoxic drugs and immunosuppressants.525,527,528 If immunotherapy is accompanied by anti-angiogenic drugs targeting VEGF pathway, it reverses these immunosuppression caused by VEGF and enhances the immune function of patients. At the same time, it can neutralize excess VEGF, reconstruct the vascular system of tumor tissue, normalize vascular network, promote the blood transport of immunosuppressant, inhibit excessive angiogenesis, reduce microvascular density, and limit tumor growth, invasion and metastasis.529 Additionally, ICIs activate intratumoral effector T cells, reshape the TME, improve immunity of host, and up-regulate expression of γ-interferon,529 all of which are conducive to vascular normalization. Some optimistic results of combination therapy have been achieved in recent years (shown in Table 4). For example, in a phase III clinical trial (NCT03434379), the combination of bevacizumab with PD-1 inhibitor atezolizumab significantly improved the OS and PFS rates of unresectable HCC patients compared to sorafenib.530 And in multiple clinical trials of combination therapy, the efficiency of PD-1 inhibitors (such as nivolumab and pembrolizumab) combined with cabozantinib, axitinib, or bevacizumab was much better than a single use of sunitinib in patients with RCC, NSCLC, CRC and GIST.526 The combination of anti-angiogenic and immune therapy has a positive significance to anti-cancer treatment according to majority of clinical trials, especially patients with advanced malignant tumors who are not sensitive, willing, or tolerant to chemotherapy.526 But some common problems like effectiveness, toxicity and tolerability of this combination modality need to be optimized through further research on therapeutic dosage, time and sequence among different patients.531–533 And mechanisms of the positive loops between angiogenic inhibitors and ICIs should be performed in a more in-depth and interconnected manner to help develop new formulation and design clinical studies, in order to encourage this promising strategy into one of the most standard cancer therapeutic modality.
Table 4.
Selected clinical trials of combination therapy
| Interventions | Cancers | Phase | Results | NCT numbers |
|---|---|---|---|---|
| Successful clinical trials | ||||
| ABI-007 plus bevacizumab vs. ABI-007 | Metastatic BC | II | Promising PFS and an acceptable safety profile with no unanticipated toxicities (combination vs. ABI-007: PFS 11.4 vs. 6.11 months, ORR 30% vs. 14%)a | NCT00394082 |
| Docetaxel plus ramucirumab vs. plus placebo | Locally advanced or metastatic urothelial carcinoma | III | This combination significantly prolongs PFS with no unexpected toxic effects; PFS 4.07 vs. 2.76 monthsa. | NCT02426125 |
| Cisplatin or carboplatin, and etoposide plus sunitinib | Extensive-stage small cell lung cancer | I/II | The addition of sunitinib prolongs PFS and OS; median OS (9.0 vs. 6.9 months) and median PFS (3.7 vs. 2.1 months)a. | NCT00453154 |
| Docetaxel plus vandetanib vs. plus placebo | Advanced NSCLC | III | This combination significantly improves PFS, median PFS 4.0 vs. 3.2 monthsa. | NCT00312377 |
| Bevacizumab, carboplatin, paclitaxel plus atezolizumab (ABCP) vs. BCP | Stage IV non-squamous NSCLC | III | The addition of atezolizumab to bevacizumab plus chemotherapy is significant: median PFS 8.3 vs. 6.8 months; median OS 19.2 vs. 14.7 monthsa. | NCT02366143 |
| Atezolizumab plus bevacizumab vs. sorafenib | Untreated locally advanced or metastatic HCC | III | Atezolizumab-bevacizumab is better than sorafenib: OS at 12 months 67.2% vs. 54.6%; median PFS 6.8 vs. 4.3 monthsa. | NCT03434379 |
| Different chemotherapies (nab-paclitaxel; paclitaxel; gemcitabine/carboplatin) plus pembrolizumab | Untreated locally recurrent inoperable or metastatic TNBC | III | The addition of pembrolizumab resulted in significantly longer PFS and OS than chemotherapy-placebo in twice interim analysisb. | NCT02819518 |
| Lenvatinib plus pembrolizumab vs. doxorubicin | Advanced endometrial cancer after failure of platinum-based chemotherapy | III | The combination has significantly longer PFS and OS: median PFS 6.6 vs. 3.8 months; median OS 17.4 vs. 12.0 monthsb. | NCT03517449 |
| Atezolizumab with or without cobimetinib vs. regorafenib | Metastatic CRC | II | Positive results in median OS: atezolizumab 7.10 months, atezolizumab plus cobimetinib 8.87 months, regorafenib 8.51 monthsa. | NCT02788279 |
| Unsuccessful or terminated clinical trials | ||||
| Irinotecan and temozolomide plus bevacizumab | Relapsed or refractory neuroblastoma | II | Expected and transient toxicities, but the addition of bevacizumab did not improve response rates compared to irinotecan plus temozolomidea. | NCT01114555 |
| FOLFOX6 plus bevacizumab | Biliary system carcinoma | II | 1/8 patient with perforation of colon; impossible to get insurance companies to cover bevacizumabc. | NCT00881504 |
| Ixabepilone plus bevacizumab | Metastatic RCC | II | Well tolerated, with modest activity in second - or later-line mRCC, not recommendeda. | NCT00923130 |
| Docetaxel plus sorafenib | Advanced non-squamous cell NSCLC | II | Preliminary efficacy data was not encouraging, 4/5 patients with serious adverse eventsc. | NCT00801801 |
| Temozolomide plus sorafenib | Recurrent GBM | II | Well tolerated, but limited activity for recurrent GBMa. | NCT00597493 |
| Paclitaxel and carboplatin plus axitinib vs. plus bevacizumab | Advanced lung cancer | II | Axitinib plus paclitaxel and carboplatin is worse than bevacizumab plus paclitaxel and carboplatin: PFS 11.0 vs. 15.9 months; OS 18.1 vs. 21.6 monthsa. | NCT00600821 |
| Modified FOLFOX6 plus axitinib and/or bevacizumab | Metastatic CRC | II | No improvements in combination with axitinib or axitinib/bevacizumab compared to bevacizumab plus FOLFOX6: PFS 11.0 vs. 12.5 vs.15.9 months; OS 18.1 vs. 19.7 vs. 21.6 monthsa. | NCT00460603 |
| Chemotherapy (capecitabine or docetaxel) vs. sunitinib | TNBC | II | No improvements of sunitinib in median OS (9.4 vs. 10.5 months), objective response rates (3% vs. 7%)a. | NCT00246571 |
| Docetaxel plus vandetanib vs. plus placebo | Transitional bladder cancer | II | The additional of vandetanib not significantly improve the outcomes: median PFS 2.56 vs. 1.58 months; OS and ORR with no differencea. | NCT00880334 |
| Azacitidine plus durvalumab vs. azacitidine | Untreated adults with higher-risk MDS or elder patients with AML | II | More toxicities and without significant improvement in clinical outcomes than azacitidinea. | NCT02775903 |
| Gemcitabine and nab-paclitaxel vs. gemcitabine, nab-paclitaxel plus durvalumab and tremelimumab | Metastatic pancreatic adenocarcinoma | II | No significant benefits from the addition of durvalumab and tremelimumabb. | NCT02879318 |
| Gemcitabine plus axitinib vs. gemcitabine | Metastatic pancreatic cancer | II | Similar safety; non-statistically significant gain in OS than gemcitabine alone: 6.9 vs. 5.6 monthsa. | NCT00219557 |
AML acute myeloid leukemia, BC breast cancer, CRC colorectal cancer, FOLFOX6 oxaliplatin, calcium folinate and 5-fluorouracil, GBM glioblastoma, MDS myelodysplastic syndromes, NSCLC non-small cell lung cancer, ORR overall response rate, OS overall survival, PFS progression-free survival, RCC renal cell carcinoma, TNBC triple-negative breast cancer
aCompleted
bOngoing
cTerminated
As mentioned before, although it has more damage to normal cells, blood vessels and immune system due to the administration with maximum tolerated dosage and poor tissue selectivity, chemotherapy is an irreplaceable method for many advanced patients with cancer metastasis to prolong the survival.534 With the advancement of medical technology, clinical medicine and pharmacy, it has been proven that the addition of anti-angiogenic therapy or (and) emerging immunotherapy to chemotherapy may win more benefits for patients. Angiogenic inhibitors normalize tumor blood vessels, reduce osmolality, alleviate local hypoxia, restore the penetration and delivery of the drugs into tumor cells, and also reduce the dose of administration and improve patient tolerance under the premise of effective chemotherapy, while ICIs improve the immune system of patients and prevent “immune escape” of tumors. Some relevant clinical trials with positive outcomes have been shown in Table 4. For example, a phase III clinical trial (NCT02366143) have shown that the addition of atezolizumab (anti-PD-L1) greatly extended the OS (19.2 vs. 14.7 months), PFS (8.3 vs. 6.8 months) and OR (63.5% vs. 48.0%) rates of NSCLC patients treated with bevacizumab, carboplatin and paclitaxel.535 Although many optimistic results have been reported, some failures cannot be neglected (shown in Table 4), which underlines suitable drugs for compatibility, suitable primary or auxiliary drugs, dosage and sequence of administration, individual differences in patients, and different stages and types of tumors.533
Another notable therapeutic method is an emerging adjuvant strategy - neoadjuvant chemotherapy (NACT), aiming to reduce the tumor and kill invisible metastatic tumor cells through systemic chemotherapy to facilitate subsequent surgery, radiotherapy, and other treatments. Up to now, various NACT regimens (SOX, XELOX, FOLFOX) have been suggested with satisfactory clinical results in primary or advanced tumors and lower risk of progression, but some discouraging clinical evidence of NACT also observed in recent years (especially breast cancer).536–539 A review from Perelmuter et al. summarized a number of potential mechanisms of chemoresistance in NACT, wherein, it is reported that NACT could stimulate cancer metastasis through inducing angiogenesis, lymphangiogenesis and inflammatory infiltration, altering immune responses and worsening TME, and these changes may induce secondary chemoresistance.540 Can addition of angiogenic inhibitors and ICIs against this resistance? Theoretically, it is promising, but massive efforts are also necessary, some clinical trials are already underway (NCT05554276, NCT04294511, NCT04606108, NCT05468242, NCT05202314).
Multi-targeted anti-angiogenic agents
Apart from the means above, exploiting novel selective multi-targeted kinase inhibitors is one of the current trendy research directions. In tumor angiogenesis, various angiogenic tyrosine kinases act synergistically to induce an array of intracellular signaling cascades instead of working individually.541,542 So, selective multi-targeted angiogenic TKIs might be used to overcome compensatory angiogenesis and cross-talk of alternative angiogenic signals.543,544 The advantages of selective multi-targeted kinase inhibitors include: (a) avoiding adverse events from broad-spectrum inhibitors; (b) exerting multiple anti-angiogenic effects; (c) avoiding drug interactions; (d) forming more stable pharmacokinetic characterization.545
Exploring endogenous biomolecules with anti-angiogenesis
In normal tissue, anti-angiogenic molecules can balance the pro-angiogenic factors to maintain the homeostasis of the internal environment. The active angiogenesis in tumor tissue is related to the over-activation of pro-angiogenic factors and the over-inhibition of anti-angiogenic mediators. Hence, endogenous anti-angiogenic components or their derivatives may be conducive to vascular normalization and therapeutic efficiency. For instance, endostatin is an enzymatic fragment of XVIII collagen with a molecular weight of about 20 kDa that was identified by O’ Reilly and his colleagues in 1997.546 Endostatin can not only regulate more than 12% of angiogenesis-related genes in the human genome but can also compete with FGFs to limit ECs proliferation and tumor development. Recombinant human endostatin is an angiogenic inhibitor with no cytotoxicity approved by the Chinese FDA for treating various cancers, including NSCLC.337,546 However, the clinical application of endostatin is not very accessible due to poor stability and solubility, short half-lives, and difficult production problems. According to current studies, other molecules also have anti-angiogenic activities like angiostatin, thrombospondin-1/-2, TIMP, tumstatin, interferon, platelet factor 4, vasohibin, interleukin, chondromodulin, chemokines, pigment epithelial-derived factor, isthmin1 (ISM1), carboxy-terminus of Hsc70 interacting protein (CHIP), multimerin-2, and G-protein coupled receptor 56 (GPR56).359,547–555
Conclusion
Angiogenesis is one of the key conditions for the proliferation, invasion, and metastasis of carcinomas and anti-angiogenic treatment has gradually become a prevalent anti-tumor strategy with a criterion of vascular optimization. But some common issues that cannot be ignored remain to be solved such as insufficient therapeutic efficacy, reproducibility and popularization of treatment modalities. These limitations encourage researchers to develop novel angiogenic inhibitor, explore the druggability of more targets, validate specific biomarkers and optimize treatment administration, in order to break the “treatment deadlock” and strive more opportunities for cancer patients.
With an in-depth understanding of tumor angiogenesis, tumor microenvironment, and drug resistance, these problems may be solved in the near future. As an emerging strategy, anti-angiogenic therapy will achieve more clinical benefits for cancer patients and anti-tumor therapy, and facilitate the clinical treatment of non-neoplastic angiogenesis-related diseases as well.
Acknowledgements
This work was supported by the National Natural Science Foundation of China (21102182), the Natural Science Foundation of Jiangsu Province (BK2012760, China), Fundamental Research Funds for the Central Universities (2632018ZD09, China), and Excellent Science and Technology Innovation Team of Jiangsu Province Universities in 2015 (China).
Author contributions
L.S. designed the review and revised the draft. Z.L.L., H.H.C., and L.L.Z. drafted the manuscript and prepared the tables and figures. L.P.S. revised the manuscript. All authors have read and approved the article.
Competing interests
The authors declare no competing interests.
Contributor Information
Li-Ping Sun, Email: chslp@cpu.edu.cn.
Lei Shi, Email: shilei@cpu.edu.cn.
References
- 1.Larionova I, Kazakova E, Gerashchenko T, Kzhyshkowska J. New angiogenic regulators produced by TAMs: perspective for pargeting tumor angiogenesis. Cancers. 2021;13:3253. doi: 10.3390/cancers13133253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Duran CL, et al. Molecular regulation of sprouting angiogenesis. Compr. Physiol. 2017;8:153–235. doi: 10.1002/cphy.c160048. [DOI] [PubMed] [Google Scholar]
- 3.Teleanu RI, Chircov C, Grumezescu AM, Teleanu DM. Tumor angiogenesis and anti-angiogenic strategies for cancer treatment. J. Clin. Med. 2019;9:84. doi: 10.3390/jcm9010084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Folkman J. Angiogenesis: an organizing principle for drug discovery? Nat. Rev. Drug Discov. 2007;6:273–286. doi: 10.1038/nrd2115. [DOI] [PubMed] [Google Scholar]
- 5.Smolen JS, Aletaha D, Koeller M, Weisman MH, Emery P. New therapies for treatment of rheumatoid arthritis. Lancet. 2007;370:1861–1874. doi: 10.1016/S0140-6736(07)60784-3. [DOI] [PubMed] [Google Scholar]
- 6.Creamer D, Jaggar R, Allen M, Bicknell R, Barker J. Overexpression of the angiogenic factor platelet-derived endothelial cell growth factor/thymidine phosphorylase in psoriatic epidermis. Br. J. Dermatol. 1997;137:851–855. doi: 10.1046/j.1365-2133.1997.19772089.x. [DOI] [PubMed] [Google Scholar]
- 7.Costa C, Incio J, Soares R. Angiogenesis and chronic inflammation: cause or consequence? Angiogenesis. 2007;10:149–166. doi: 10.1007/s10456-007-9074-0. [DOI] [PubMed] [Google Scholar]
- 8.Caldwell RB, et al. Vascular endothelial growth factor and diabetic retinopathy: pathophysiological mechanisms and treatment perspectives. Diabetes Metab. Res. Rev. 2003;19:442–455. doi: 10.1002/dmrr.415. [DOI] [PubMed] [Google Scholar]
- 9.Ng EWM, Adamis AP. Targeting angiogenesis, the underlying disorder in neovascular age-related macular degeneration. Can. J. Ophthalmol. 2005;40:352–368. doi: 10.1016/S0008-4182(05)80078-X. [DOI] [PubMed] [Google Scholar]
- 10.Khosravi Shahi P, Soria Lovelle A, Pérez Manga G. Tumoral angiogenesis and breast cancer. Clin. Transl. Oncol. 2009;11:138–142. doi: 10.1007/S12094-009-0329-7. [DOI] [PubMed] [Google Scholar]
- 11.Zhong M, et al. TIPE regulates VEGFR2 expression and promotes angiogenesis in colorectal cancer. Int. J. Biol. Sci. 2020;16:272–283. doi: 10.7150/ijbs.37906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hall RD, Le TM, Haggstrom DE, Gentzler RD. Angiogenesis inhibition as a therapeutic strategy in non-small cell lung cancer (NSCLC) Transl. Lung Cancer Res. 2015;4:515–523. doi: 10.3978/j.issn.2218-6751.2015.06.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zimna A, Kurpisz M. Hypoxia-inducible factor-1 in physiological and pathophysiological angiogenesis: applications and therapies. BioMed. Res. Int. 2015;2015:549412. doi: 10.1155/2015/549412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Conway EM, Collen D, Carmeliet P. Molecular mechanisms of blood vessel growth. Cardiovasc. Res. 2001;49:507–521. doi: 10.1016/S0008-6363(00)00281-9. [DOI] [PubMed] [Google Scholar]
- 15.Kalluri R. Basement membranes: structure, assembly and role in tumour angiogenesis. Nat. Rev. Cancer. 2003;3:422–433. doi: 10.1038/nrc1094. [DOI] [PubMed] [Google Scholar]
- 16.Gasparini G, Longo R, Toi M, Ferrara N. Angiogenic inhibitors: a new therapeutic strategy in oncology. Nat. Rev. Pract. Oncol. 2005;2:562–577. doi: 10.1038/ncponc0342. [DOI] [PubMed] [Google Scholar]
- 17.Adams RH, Alitalo K. Molecular regulation of angiogenesis and lymphangiogenesis. Nat. Rev. Mol. Cell Biol. 2007;8:464–478. doi: 10.1038/nrm2183. [DOI] [PubMed] [Google Scholar]
- 18.Jain RK. Molecular regulation of vessel maturation. Nat. Med. 2003;9:685–693. doi: 10.1038/nm0603-685. [DOI] [PubMed] [Google Scholar]
- 19.Rowley DR. What might a stromal response mean to prostate cancer progression? Cancer Metastasis Rev. 1998;17:411–419. doi: 10.1023/A:1006129420005. [DOI] [PubMed] [Google Scholar]
- 20.Liakouli V, et al. The role of extracellular matrix components in angiogenesis and fibrosis: possible implication for Systemic Sclerosis. Mod. Rheumatol. 2018;28:922–932. doi: 10.1080/14397595.2018.1431004. [DOI] [PubMed] [Google Scholar]
- 21.Shiga K, et al. Cancer-associated fibroblasts: their characteristics and their roles in tumor growth. Cancers. 2015;7:2443–2458. doi: 10.3390/cancers7040902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Roland CL, et al. Inhibition of vascular endothelial growth factor reduces angiogenesis and modulates immune cell infiltration of orthotopic breast cancer xenografts. Mol. Cancer Ther. 2009;8:1761–1771. doi: 10.1158/1535-7163.MCT-09-0280. [DOI] [PubMed] [Google Scholar]
- 23.Ribatti D, Crivellato E. Immune cells and angiogenesis. J. Cell. Mol. Med. 2009;13:2822–2833. doi: 10.1111/j.1582-4934.2009.00810.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Parmar D, Apte M. Angiopoietin inhibitors: a review on targeting tumor angiogenesis. Eur. J. Pharmacol. 2021;899:174021. doi: 10.1016/j.ejphar.2021.174021. [DOI] [PubMed] [Google Scholar]
- 25.Deyell M, Garris CS, Laughney AM. Cancer metastasis as a non-healing wound. Br. J. Cancer. 2021;124:1491–1502. doi: 10.1038/s41416-021-01309-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Viallard C, Larrivée B. Tumor angiogenesis and vascular normalization: alternative therapeutic targets. Angiogenesis. 2017;20:409–426. doi: 10.1007/s10456-017-9562-9. [DOI] [PubMed] [Google Scholar]
- 27.Bellou S, Pentheroudakis G, Murphy C, Fotsis T. Anti-angiogenesis in cancer therapy: hercules and hydra. Cancer Lett. 2013;338:219–228. doi: 10.1016/j.canlet.2013.05.015. [DOI] [PubMed] [Google Scholar]
- 28.Ebos JML, Kerbel RS. Antiangiogenic therapy: impact on invasion, disease progression, and metastasis. Nat. Rev. Clin. Oncol. 2011;8:210–221. doi: 10.1038/nrclinonc.2011.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pirker R. Chemotherapy remains a cornerstone in the treatment of nonsmall cell lung cancer. Curr. Opin. Oncol. 2020;32:63–67. doi: 10.1097/CCO.0000000000000592. [DOI] [PubMed] [Google Scholar]
- 30.Biller LH, Schrag D. Diagnosis and treatment of metastatic colorectal cancer: a review. JAMA. 2021;325:669. doi: 10.1001/jama.2021.0106. [DOI] [PubMed] [Google Scholar]
- 31.Luqmani YA. Mechanisms of drug resistance in cancer chemotherapy. Med. Princ. Pract. 2005;14:35–48. doi: 10.1159/000086183. [DOI] [PubMed] [Google Scholar]
- 32.Saeki T, Tsuruo T, Sato W, Nishikawsa K. Drug resistance in chemotherapy for breast cancer. Cancer Chemother. Pharmacol. 2005;56:84–89. doi: 10.1007/s00280-005-0106-4. [DOI] [PubMed] [Google Scholar]
- 33.Salgia R, Kulkarni P. The genetic/non-genetic duality of drug ‘resistance’ in cancer. Trends Cancer. 2018;4:110–118. doi: 10.1016/j.trecan.2018.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Turner NC, Reis-Filho JS. Genetic heterogeneity and cancer drug resistance. Lancet Oncol. 2012;13:e178–e185. doi: 10.1016/S1470-2045(11)70335-7. [DOI] [PubMed] [Google Scholar]
- 35.Duesberg P, et al. Cancer drug resistance: the central role of the karyotype. Drug Resist. Updat. 2007;10:51–58. doi: 10.1016/j.drup.2007.02.003. [DOI] [PubMed] [Google Scholar]
- 36.Lahiry P, Torkamani A, Schork NJ, Hegele RA. Kinase mutations in human disease: interpreting genotype-phenotype relationships. Nat. Rev. Genet. 2010;11:60–74. doi: 10.1038/nrg2707. [DOI] [PubMed] [Google Scholar]
- 37.Claesson-Welsh L. Vascular permeability—the essentials. Ups. J. Med. Sci. 2015;120:135–143. doi: 10.3109/03009734.2015.1064501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.De Bock K, Cauwenberghs S, Carmeliet P. Vessel abnormalization: another hallmark of cancer? Molecular mechanisms and therapeutic implications. Curr. Opin. Genet. Dev. 2011;21:73–79. doi: 10.1016/j.gde.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 39.Mortezaee K. Immune escape: a critical hallmark in solid tumors. Life Sci. 2020;258:118110. doi: 10.1016/j.lfs.2020.118110. [DOI] [PubMed] [Google Scholar]
- 40.Igney FH, Krammer PH. Immune escape of tumors: apoptosis resistance and tumor counterattack. J. Leukoc. Biol. 2002;71:907–920. doi: 10.1189/jlb.71.6.907. [DOI] [PubMed] [Google Scholar]
- 41.Majidpoor J, Mortezaee K. Angiogenesis as a hallmark of solid tumors—clinical perspectives. Cell. Oncol. 2021;44:715–737. doi: 10.1007/s13402-021-00602-3. [DOI] [PubMed] [Google Scholar]
- 42.Choi SH, Yoo SS, Lee SY, Park JY. Anti-angiogenesis revisited: reshaping the treatment landscape of advanced non-small cell lung cancer. Arch. Pharm. Res. 2022;45:263–279. doi: 10.1007/s12272-022-01382-6. [DOI] [PubMed] [Google Scholar]
- 43.Zhong L, et al. Small molecules in targeted cancer therapy: advances, challenges, and future perspectives. Signal Transduct. Target. Ther. 2021;6:201. doi: 10.1038/s41392-021-00572-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Huinen ZR, Huijbers EJM, van Beijnum JR, Nowak-Sliwinska P, Griffioen AW. Anti-angiogenic agents—overcoming tumour endothelial cell anergy and improving immunotherapy outcomes. Nat. Rev. Clin. Oncol. 2021;18:527–540. doi: 10.1038/s41571-021-00496-y. [DOI] [PubMed] [Google Scholar]
- 45.Gacche RN, Meshram RJ. Angiogenic factors as potential drug target: efficacy and limitations of anti-angiogenic therapy. Biochim. Biophys. Acta. 2014;1846:161–179. doi: 10.1016/j.bbcan.2014.05.002. [DOI] [PubMed] [Google Scholar]
- 46.Bergers G, Hanahan D. Modes of resistance to anti-angiogenic therapy. Nat. Rev. Cancer. 2008;8:592–603. doi: 10.1038/nrc2442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ansari MJ, et al. Cancer combination therapies by angiogenesis inhibitors; a comprehensive review. Cell Commun. Signal. 2022;20:49. doi: 10.1186/s12964-022-00838-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bergers G, Song S. The role of pericytes in blood-vessel formation and maintenance. Neuro Oncol. 2005;7:452–464. doi: 10.1215/S1152851705000232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Carmeliet P, Jain RK. Angiogenesis in cancer and other diseases. Nature. 2000;407:249–257. doi: 10.1038/35025220. [DOI] [PubMed] [Google Scholar]
- 50.Goel S, et al. Normalization of the vasculature for treatment of cancer and other diseases. Physiol. Rev. 2011;91:1071–1121. doi: 10.1152/physrev.00038.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kim C, et al. Vascular RhoJ is an effective and selective target for tumor angiogenesis and vascular disruption. Cancer Cell. 2014;25:102–117. doi: 10.1016/j.ccr.2013.12.010. [DOI] [PubMed] [Google Scholar]
- 52.Jain RK. Normalizing tumor microenvironment to treat cancer: bench to bedside to biomarkers. J. Clin. Oncol. 2013;31:2205–2218. doi: 10.1200/JCO.2012.46.3653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chauhan VP, et al. Normalization of tumour blood vessels improves the delivery of nanomedicines in a size-dependent manner. Nat. Nanotechnol. 2012;7:383–388. doi: 10.1038/nnano.2012.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Martin JD, Seano G, Jain RK. Normalizing function of tumor vessels: progress, opportunities, and challenges. Annu. Rev. Physiol. 2019;81:505–534. doi: 10.1146/annurev-physiol-020518-114700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yang T, et al. Vascular normalization: a new window opened for cancer therapies. Front. Oncol. 2021;11:719836. doi: 10.3389/fonc.2021.719836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Stylianopoulos T, Munn LL, Jain RK. Reengineering the physical microenvironment of tumors to improve drug delivery and efficacy: from mathematical modeling to bench to bedside. Trends Cancer. 2018;4:292–319. doi: 10.1016/j.trecan.2018.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Jain RK, Martin JD, Stylianopoulos T. The role of mechanical forces in tumor growth and therapy. Annu. Rev. Biomed. Eng. 2014;16:321–346. doi: 10.1146/annurev-bioeng-071813-105259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Stylianopoulos T, Jain RK. Combining two strategies to improve perfusion and drug delivery in solid tumors. Proc. Natl Acad. Sci. USA. 2013;110:18632–18637. doi: 10.1073/pnas.1318415110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Jain RK, Stylianopoulos T. Delivering nanomedicine to solid tumors. Nat. Rev. Clin. Oncol. 2010;7:653–664. doi: 10.1038/nrclinonc.2010.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hamzah J, et al. Vascular normalization in Rgs5-deficient tumours promotes immune destruction. Nature. 2008;453:410–414. doi: 10.1038/nature06868. [DOI] [PubMed] [Google Scholar]
- 61.Vaupel P, Mayer A. Hypoxia in cancer: significance and impact on clinical outcome. Cancer Metastasis Rev. 2007;26:225–239. doi: 10.1007/s10555-007-9055-1. [DOI] [PubMed] [Google Scholar]
- 62.Stubbs M, McSheehy PMJ, Griffiths JR, Bashford CL. Causes and consequences of tumour acidity and implications for treatment. Mol. Med. Today. 2000;6:15–19. doi: 10.1016/S1357-4310(99)01615-9. [DOI] [PubMed] [Google Scholar]
- 63.Lee ES, Oh KT, Kim D, Youn YS, Bae YH. Tumor pH-responsive flower-like micelles of poly(l-lactic acid)-b-poly(ethylene glycol)-b-poly(l-histidine) J. Control. Release. 2007;123:19–26. doi: 10.1016/j.jconrel.2007.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zhang Z, et al. Rational design of nanoparticles with deep tumor penetration for effective treatment of tumor metastasis. Adv. Funct. Mater. 2018;28:1801840. doi: 10.1002/adfm.201801840. [DOI] [Google Scholar]
- 65.Khawar IA, Kim JH, Kuh HJ. Improving drug delivery to solid tumors: Priming the tumor microenvironment. J. Control. Release. 2015;201:78–89. doi: 10.1016/j.jconrel.2014.12.018. [DOI] [PubMed] [Google Scholar]
- 66.Zhu L, et al. Angiogenesis and immune checkpoint dual blockade in combination with radiotherapy for treatment of solid cancers: opportunities and challenges. Oncogenesis. 2021;10:47. doi: 10.1038/s41389-021-00335-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Li X, et al. The immunological and metabolic landscape in primary and metastatic liver cancer. Nat. Rev. Cancer. 2021;21:541–557. doi: 10.1038/s41568-021-00383-9. [DOI] [PubMed] [Google Scholar]
- 68.Provenzano PP, et al. Enzymatic targeting of the stroma ablates physical barriers to treatment of pancreatic ductal adenocarcinoma. Cancer Cell. 2012;21:418–429. doi: 10.1016/j.ccr.2012.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Milosevic M, Fyles A, Hedley D, Hill R. The human tumor microenvironment: invasive (needle) measurement of oxygen and interstitial fluid pressure. Semin. Radiat. Oncol. 2004;14:249–258. doi: 10.1016/j.semradonc.2004.04.006. [DOI] [PubMed] [Google Scholar]
- 70.Chun, C. Z., Sood, R. & Ramchandran, R. in Vascular Tumors and Developmental Malformations (eds. North, P. E. & Sander, T.) 77–99 (Springer, 2016).
- 71.Hillen F, Griffioen AW. Tumour vascularization: sprouting angiogenesis and beyond. Cancer Metastasis Rev. 2007;26:489–502. doi: 10.1007/s10555-007-9094-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gianni-Barrera R, Bartolomeo M, Vollmar B, Djonov V, Banfi A. Split for the cure: VEGF, PDGF-BB and intussusception in therapeutic angiogenesis. Biochem. Soc. Trans. 2014;42:1637–1642. doi: 10.1042/BST20140234. [DOI] [PubMed] [Google Scholar]
- 73.Burri PH, Djonov V. Intussusceptive angiogenesis—the alternative to capillary sprouting. Mol. Asp. Med. 2002;23:1–27. doi: 10.1016/S0098-2997(02)00096-1. [DOI] [PubMed] [Google Scholar]
- 74.Ratajska A, et al. Vasculogenesis and its cellular therapeutic applications. Cells Tissues Organs. 2017;203:141–152. doi: 10.1159/000448551. [DOI] [PubMed] [Google Scholar]
- 75.Shi, L. in Burger’s Medicinal Chemistry and Drug Discovery (ed. Abraham, D. J.) 1–66 (Wiley, 2021).
- 76.Teuwen LA, et al. Tumor vessel co-option probed by single-cell analysis. Cell Rep. 2021;35:109253. doi: 10.1016/j.celrep.2021.109253. [DOI] [PubMed] [Google Scholar]
- 77.Wei X, et al. Mechanisms of vasculogenic mimicry in hypoxic tumor microenvironments. Mol. Cancer. 2021;20:7. doi: 10.1186/s12943-020-01288-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Potente M, Gerhardt H, Carmeliet P. Basic and therapeutic aspects of angiogenesis. Cell. 2011;146:873–887. doi: 10.1016/j.cell.2011.08.039. [DOI] [PubMed] [Google Scholar]
- 79.Melincovici CS, et al. Vascular endothelial growth factor (VEGF)—key factor in normal and pathological angiogenesis. Rom. J. Morphol. Embryol. 2018;59:455–467. [PubMed] [Google Scholar]
- 80.Kazlauskas A. PDGFs and their receptors. Gene. 2017;614:1–7. doi: 10.1016/j.gene.2017.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Sang QXA. Complex role of matrix metalloproteinases in angiogenesis. Cell Res. 1998;8:171–177. doi: 10.1038/cr.1998.17. [DOI] [PubMed] [Google Scholar]
- 82.Ferrara N, Hillan KJ, Gerber HP, Novotny W. Discovery and development of bevacizumab, an anti-VEGF antibody for treating cancer. Nat. Rev. Drug Discov. 2004;3:391–400. doi: 10.1038/nrd1381. [DOI] [PubMed] [Google Scholar]
- 83.Shibuya M, Claesson-Welsh L. Signal transduction by VEGF receptors in regulation of angiogenesis and lymphangiogenesis. Exp. Cell Res. 2006;312:549–560. doi: 10.1016/j.yexcr.2005.11.012. [DOI] [PubMed] [Google Scholar]
- 84.Senger DR, et al. Vascular permeability factor (VPF, VEGF) in tumor biology. Cancer Metast Rev. 1993;12:303–324. doi: 10.1007/BF00665960. [DOI] [PubMed] [Google Scholar]
- 85.Bao P, et al. The role of vascular endothelial growth factor in wound healing. J. Surg. Res. 2009;153:347–358. doi: 10.1016/j.jss.2008.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Shibuya M. Vascular endothelial growth factor (VEGF) and its receptor (VEGFR) signaling in angiogenesis: a crucial target for anti- and pro-angiogenic therapies. Genes Cancer. 2011;2:1097–1105. doi: 10.1177/1947601911423031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Carmeliet P. VEGF as a key mediator of angiogenesis in cancer. Oncology. 2005;69:4–10. doi: 10.1159/000088478. [DOI] [PubMed] [Google Scholar]
- 88.Peach CJ, et al. Molecular pharmacology of VEGF-A isoforms: binding and signalling at VEGFR2. Int. J. Mol. Sci. 2018;19:1264. doi: 10.3390/ijms19041264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Carmeliet P, Jain RK. Molecular mechanisms and clinical applications of angiogenesis. Nature. 2011;473:298–307. doi: 10.1038/nature10144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ji RC. Characteristics of lymphatic endothelial cells in physiological and pathological conditions. Histol. Histopathol. 2005;20:155–175. doi: 10.14670/HH-20.155. [DOI] [PubMed] [Google Scholar]
- 91.He Y, et al. Suppression of tumor lymphangiogenesis and lymph node metastasis by blocking vascular endothelial growth factor receptor 3 signaling. J. Natl Cancer Inst. 2002;94:819–825. doi: 10.1093/jnci/94.11.819. [DOI] [PubMed] [Google Scholar]
- 92.Luttun A, Autiero M, Tjwa M, Carmeliet P. Genetic dissection of tumor angiogenesis: are PlGF and VEGFR-1 novel anti-cancer targets? Biochim. Biophys. Acta. 2004;1654:79–94. doi: 10.1016/j.bbcan.2003.09.002. [DOI] [PubMed] [Google Scholar]
- 93.McDonald NQ, Hendrickson WA. A structural superfamily of growth factors containing a cystine knot motif. Cell. 1993;73:421–424. doi: 10.1016/0092-8674(93)90127-C. [DOI] [PubMed] [Google Scholar]
- 94.Luttun A, et al. Revascularization of ischemic tissues by PlGF treatment, and inhibition of tumor angiogenesis, arthritis and atherosclerosis by anti-Flt1. Nat. Med. 2002;8:831–840. doi: 10.1038/nm731. [DOI] [PubMed] [Google Scholar]
- 95.Iyer S, Acharya KR. Role of placenta growth factor in cardiovascular health. Trends Cardiovasc. Med. 2002;12:128–134. doi: 10.1016/S1050-1738(01)00164-5. [DOI] [PubMed] [Google Scholar]
- 96.Beck H, et al. Cell type-specific expression of neuropilins in an MCA-occlusion model in mice suggests a potential role in post-ischemic brain remodeling. J. Neuropathol. Exp. Neurol. 2002;61:339–350. doi: 10.1093/jnen/61.4.339. [DOI] [PubMed] [Google Scholar]
- 97.Donnini S, Machein MR, Plate KH, Weich HA. Expression and localization of placenta growth factor and PlGF receptors in human meningiomas. J. Pathol. 1999;189:66–71. doi: 10.1002/(SICI)1096-9896(199909)189:1<66::AID-PATH390>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 98.Lacal PM, et al. Human melanoma cells secrete and respond to placenta growth factor and vascular endothelial growth factor. J. Invest. Dermatol. 2000;115:1000–1007. doi: 10.1046/j.1523-1747.2000.00199.x. [DOI] [PubMed] [Google Scholar]
- 99.Ribatti D, Conconi MT, Nussdorfer GG. Nonclassic endogenous novel regulators of angiogenesis. Pharmacol. Rev. 2007;59:185–205. doi: 10.1124/pr.59.2.3. [DOI] [PubMed] [Google Scholar]
- 100.Byrne AM, Bouchier-Hayes DJ, Harmey JH. Angiogenic and cell survival functions of vascular endothelial growth factor (VEGF) J. Cell. Mol. Med. 2005;9:777–794. doi: 10.1111/j.1582-4934.2005.tb00379.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Barleon B, et al. Migration of human monocytes in response to vascular endothelial growth factor (VEGF) is mediated via the VEGF receptor flt-1. Blood. 1996;87:3336–3343. doi: 10.1182/blood.V87.8.3336.bloodjournal8783336. [DOI] [PubMed] [Google Scholar]
- 102.Shibuya M. Vascular endothelial growth factor receptor-1 (VEGFR-1/Flt-1): a dual regulator for angiogenesis. Angiogenesis. 2006;9:225–230. doi: 10.1007/s10456-006-9055-8. [DOI] [PubMed] [Google Scholar]
- 103.Ferrara N, Gerber HP, LeCouter J. The biology of VEGF and its receptors. Nat. Med. 2003;9:669–676. doi: 10.1038/nm0603-669. [DOI] [PubMed] [Google Scholar]
- 104.Ishida A, et al. Expression of vascular endothelial growth factor receptors in smooth muscle cells. J. Cell. Physiol. 2001;188:359–368. doi: 10.1002/jcp.1121. [DOI] [PubMed] [Google Scholar]
- 105.Ghosh S, et al. High levels of vascular endothelial growth factor and its receptors (VEGFR-1, VEGFR-2, neuropilin-1) are associated with worse outcome in breast cancer. Hum. Pathol. 2008;39:1835–1843. doi: 10.1016/j.humpath.2008.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Ceci C, Atzori MG, Lacal PM, Graziani G. Role of VEGFs/VEGFR-1 signaling and its inhibition in modulating tumor invasion: experimental evidence in different metastatic cancer models. Int. J. Mol. Sci. 2020;21:1388. doi: 10.3390/ijms21041388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Ioannidou E, et al. Angiogenesis and anti-angiogenic treatment in prostate cancer: mechanisms of action and molecular targets. Int. J. Mol. Sci. 2021;22:9926. doi: 10.3390/ijms22189926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Simons M, Gordon E, Claesson-Welsh L. Mechanisms and regulation of endothelial VEGF receptor signalling. Nat. Rev. Mol. Cell Biol. 2016;17:611–625. doi: 10.1038/nrm.2016.87. [DOI] [PubMed] [Google Scholar]
- 109.Molhoek KR, et al. VEGFR-2 expression in human melanoma: revised assessment. Int. J. Cancer. 2011;129:2807–2815. doi: 10.1002/ijc.25963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Spannuth WA, et al. Functional significance of VEGFR-2 on ovarian cancer cells. Int. J. Cancer. 2009;124:1045–1053. doi: 10.1002/ijc.24028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Capp C, et al. Increased expression of vascular endothelial growth factor and its receptors, VEGFR-1 and VEGFR-2, in medullary thyroid carcinoma. Thyroid. 2010;20:863–871. doi: 10.1089/thy.2009.0417. [DOI] [PubMed] [Google Scholar]
- 112.Modi SJ, Kulkarni VM. Vascular endothelial growth factor receptor (VEGFR-2)/KDR inhibitors: medicinal chemistry perspective. Med. Drug Discov. 2019;2:100009. doi: 10.1016/j.medidd.2019.100009. [DOI] [Google Scholar]
- 113.Padró T, et al. Overexpression of vascular endothelial growth factor (VEGF) and its cellular receptor KDR (VEGFR-2) in the bone marrow of patients with acute myeloid leukemia. Leukemia. 2002;16:1302–1310. doi: 10.1038/sj.leu.2402534. [DOI] [PubMed] [Google Scholar]
- 114.Sun W. Angiogenesis in metastatic colorectal cancer and the benefits of targeted therapy. J. Hematol. Oncol. 2012;5:63. doi: 10.1186/1756-8722-5-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Valtola R, et al. VEGFR-3 and its ligand VEGF-C are associated with angiogenesis in breast cancer. Am. J. Pathol. 1999;154:1381–1390. doi: 10.1016/S0002-9440(10)65392-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Saintigny P, et al. Vascular endothelial growth factor-C and its receptor VEGFR-3 in non-small-cell lung cancer: concurrent expression in cancer cells from primary tumour and metastatic lymph node. Lung Cancer. 2007;58:205–213. doi: 10.1016/j.lungcan.2007.06.021. [DOI] [PubMed] [Google Scholar]
- 117.Yonemura Y, et al. Lymphangiogenesis and the vascular endothelial growth factor receptor (VEGFR)-3 in gastric cancer. Eur. J. Cancer. 2001;37:918–923. doi: 10.1016/S0959-8049(01)00015-6. [DOI] [PubMed] [Google Scholar]
- 118.Su JL, et al. The role of the VEGF-C/VEGFR-3 axis in cancer progression. Br. J. Cancer. 2007;96:541–545. doi: 10.1038/sj.bjc.6603487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Simiantonaki N, et al. Hypoxia-induced epithelial VEGF-C/VEGFR-3 upregulation in carcinoma cell lines. Int. J. Oncol. 2008;32:589–592. [PubMed] [Google Scholar]
- 120.Goel HL, Mercurio AM. VEGF targets the tumour cell. Nat. Rev. Cancer. 2013;13:871–882. doi: 10.1038/nrc3627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Wang H, et al. Over-expression of PDGFR-β promotes PDGF-induced proliferation, migration, and angiogenesis of EPCs through PI3K/Akt signaling pathway. PLoS ONE. 2012;7:e30503. doi: 10.1371/journal.pone.0030503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Manzat Saplacan RM, et al. The role of PDGFs and PDGFRs in colorectal cancer. Mediators Inflamm. 2017;2017:1–9. doi: 10.1155/2017/4708076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Kalra K, Eberhard J, Farbehi N, Chong JJ, Xaymardan M. Role of PDGF-A/B ligands in cardiac repair after myocardial infarction. Front. Cell Dev. Biol. 2021;9:669188. doi: 10.3389/fcell.2021.669188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Balamurugan K, et al. Structural insights into the modulation of PDGF/PDGFR-β complexation by hyaluronan derivatives. Biol. Chem. 2021;402:1441–1452. doi: 10.1515/hsz-2021-0173. [DOI] [PubMed] [Google Scholar]
- 125.Cenciarelli C, et al. PDGFRα depletion attenuates glioblastoma stem cells features by modulation of STAT3, RB1 and multiple oncogenic signals. Oncotarget. 2016;7:53047–53063. doi: 10.18632/oncotarget.10132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Chabot V, et al. Urokinase-type plasminogen activator receptor interaction with β1 integrin is required for platelet-derived growth factor-AB-induced human mesenchymal stem/stromal cell migration. Stem Cell Res. Ther. 2015;6:188. doi: 10.1186/s13287-015-0163-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Li H, et al. Development of monoclonal anti-PDGF-CC antibodies as tools for investigating human tissue expression and for blocking PDGF-CC induced PDGFRα signalling in vivo. PLoS ONE. 2018;13:e0201089. doi: 10.1371/journal.pone.0201089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Dardik A, Yamashita A, Aziz F, Asada H, Sumpio BE. Shear stress-stimulated endothelial cells induce smooth muscle cell chemotaxis via platelet-derived growth factor-BB and interleukin-1α. J. Vasc. Surg. 2005;41:321–331. doi: 10.1016/j.jvs.2004.11.016. [DOI] [PubMed] [Google Scholar]
- 129.Muratoglu SC, Mikhailenko I, Newton C, Migliorini M, Strickland DK. Low density lipoprotein receptor-related protein 1 (LRP1) forms a signaling complex with platelet-derived growth factor receptor-β in endosomes and regulates activation of the MAPK pathway. J. Biol. Chem. 2010;285:14308–14317. doi: 10.1074/jbc.M109.046672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Wang JC, et al. Metformin inhibits metastatic breast cancer progression and improves chemosensitivity by inducing vessel normalization via PDGF-B downregulation. J. Exp. Clin. Cancer Res. 2019;38:235. doi: 10.1186/s13046-019-1211-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Li M, et al. Integrins as attractive targets for cancer therapeutics. Acta Pharm. Sin. B. 2021;11:2726–2737. doi: 10.1016/j.apsb.2021.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Zou X, et al. Targeting the PDGF/PDGFR signaling pathway for cancer therapy: a review. Int. J. Biol. Macromol. 2022;202:539–557. doi: 10.1016/j.ijbiomac.2022.01.113. [DOI] [PubMed] [Google Scholar]
- 133.Gacche RN, Assaraf YG. Redundant angiogenic signaling and tumor drug resistance. Drug Resist. Updat. 2018;36:47–76. doi: 10.1016/j.drup.2018.01.002. [DOI] [PubMed] [Google Scholar]
- 134.Lee C, Li X. Platelet-derived growth factor-C and -D in the cardiovascular system and diseases. Mol. Asp. Med. 2018;62:12–21. doi: 10.1016/j.mam.2017.09.005. [DOI] [PubMed] [Google Scholar]
- 135.Berthod F, Symes J, Tremblay N, Medin JA, Auger FA. Spontaneous fibroblast-derived pericyte recruitment in a human tissue-engineered angiogenesis model in vitro. J. Cell. Physiol. 2012;227:2130–2137. doi: 10.1002/jcp.22943. [DOI] [PubMed] [Google Scholar]
- 136.Ribatti D, Nico B, Crivellato E. The role of pericytes in angiogenesis. Int. J. Dev. Biol. 2011;55:261–268. doi: 10.1387/ijdb.103167dr. [DOI] [PubMed] [Google Scholar]
- 137.Chatterjee S, Naik UP. Pericyte-endothelial cell interaction: a survival mechanism for the tumor vasculature. Cell Adh. Migr. 2012;6:157–159. doi: 10.4161/cam.20252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Luk K, et al. Influence of morphine on pericyte-endothelial interaction: implications for antiangiogenic therapy. J. Oncol. 2012;2012:1–10. doi: 10.1155/2012/458385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Cavalcanti E, Ignazzi A, De Michele F, Caruso ML. PDGFRα expression as a novel therapeutic marker in well-differentiated neuroendocrine tumors. Cancer Biol. Ther. 2019;20:423–430. doi: 10.1080/15384047.2018.1529114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Burger RA. Overview of anti-angiogenic agents in development for ovarian cancer. Gynecol. Oncol. 2011;121:230–238. doi: 10.1016/j.ygyno.2010.11.035. [DOI] [PubMed] [Google Scholar]
- 141.Raica M, Cimpean AM. Platelet-derived growth factor (PDGF)/PDGF receptors (PDGFR) axis as target for antitumor and antiangiogenic therapy. Pharmaceuticals. 2010;3:572–599. doi: 10.3390/ph3030572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Heindryckx F. Targeting the tumor stroma in hepatocellular carcinoma. World J. Hepatol. 2015;7:165–176. doi: 10.4254/wjh.v7.i2.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Cornellà H, Alsinet C, Villanueva A. Molecular pathogenesis of hepatocellular carcinoma. Alcohol. Clin. Exp. Res. 2011;35:821–825. doi: 10.1111/j.1530-0277.2010.01406.x. [DOI] [PubMed] [Google Scholar]
- 144.Brahmi M, et al. Expression and prognostic significance of PDGF ligands and receptors across soft tissue sarcomas. ESMO Open. 2021;6:100037. doi: 10.1016/j.esmoop.2020.100037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Rao L, et al. HB-EGF-EGFR signaling in bone marrow endothelial cells mediates angiogenesis associated with multiple myeloma. Cancers. 2020;12:173. doi: 10.3390/cancers12010173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Hu L, et al. Dual target inhibitors based on EGFR: promising anticancer agents for the treatment of cancers (2017-) Eur. J. Med. Chem. 2022;227:113963. doi: 10.1016/j.ejmech.2021.113963. [DOI] [PubMed] [Google Scholar]
- 147.Larsen AK, Ouaret D, El Ouadrani K, Petitprez A. Targeting EGFR and VEGF(R) pathway cross-talk in tumor survival and angiogenesis. Pharmacol. Ther. 2011;131:80–90. doi: 10.1016/j.pharmthera.2011.03.012. [DOI] [PubMed] [Google Scholar]
- 148.Holbro T, Hynes NE. ErbB receptors: directing key signaling networks throughout life. Annu. Rev. Pharmacol. Toxicol. 2004;44:195–217. doi: 10.1146/annurev.pharmtox.44.101802.121440. [DOI] [PubMed] [Google Scholar]
- 149.Ellis LM. Epidermal growth factor receptor in tumor angiogenesis. Hematol. Oncol. Clin. North Am. 2004;18:1007–1021. doi: 10.1016/j.hoc.2004.06.002. [DOI] [PubMed] [Google Scholar]
- 150.De Luca A, et al. The role of the EGFR signaling in tumor microenvironment. J. Cell. Physiol. 2008;214:559–567. doi: 10.1002/jcp.21260. [DOI] [PubMed] [Google Scholar]
- 151.Albadari N, Deng S, Li W. The transcriptional factors HIF-1 and HIF-2 and their novel inhibitors in cancer therapy. Expert Opin. Drug Discov. 2019;14:667–682. doi: 10.1080/17460441.2019.1613370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Bos R, et al. Hypoxia-inducible factor-1α is associated with angiogenesis, and expression of bFGF, PDGF-BB, and EGFR in invasive breast cancer. Histopathology. 2005;46:31–36. doi: 10.1111/j.1365-2559.2005.02045.x. [DOI] [PubMed] [Google Scholar]
- 153.Salomon DS, Brandt R, Ciardiello F, Normanno N. Epidermal growth factor-related peptides and their receptors in human malignancies. Crit. Rev. Oncol. Hematol. 1995;19:183–232. doi: 10.1016/1040-8428(94)00144-I. [DOI] [PubMed] [Google Scholar]
- 154.Yu HA, et al. Poor response to erlotinib in patients with tumors containing baseline EGFR T790M mutations found by routine clinical molecular testing. Ann. Oncol. 2014;25:423–428. doi: 10.1093/annonc/mdt573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Raj S, et al. Molecular mechanism(s) of regulation(s) of c-MET/HGF signaling in head and neck cancer. Mol. Cancer. 2022;21:31. doi: 10.1186/s12943-022-01503-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Acevedo VD, Ittmann M, Spencer DM. Paths of FGFR-driven tumorigenesis. Cell Cycle. 2009;8:580–588. doi: 10.4161/cc.8.4.7657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Chen M, Bao L, Zhao M, Cao J, Zheng H. Progress in research on the role of FGF in the formation and treatment of corneal neovascularization. Front. Pharmacol. 2020;11:111. doi: 10.3389/fphar.2020.00111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Montesano R, Vassalli JD, Baird A, Guillemin R, Orci L. Basic fibroblast growth factor induces angiogenesis in vitro. Proc. Natl Acad. Sci. USA. 1986;83:7297–7301. doi: 10.1073/pnas.83.19.7297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Giacomini A, et al. The FGF/FGFR system in the physiopathology of the prostate gland. Physiol. Rev. 2021;101:569–610. doi: 10.1152/physrev.00005.2020. [DOI] [PubMed] [Google Scholar]
- 160.Hui Q, et al. FGF family: from drug development to clinical application. Int. J. Mol. Sci. 2018;19:1875. doi: 10.3390/ijms19071875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Presta M, et al. Fibroblast growth factor/fibroblast growth factor receptor system in angiogenesis. Cytokine Growth Factor Rev. 2005;16:159–178. doi: 10.1016/j.cytogfr.2005.01.004. [DOI] [PubMed] [Google Scholar]
- 162.Fons P, et al. Tumor vasculature is regulated by FGF/FGFR signaling-mediated angiogenesis and bone marrow-derived cell recruitment: this mechanism is inhibited by SSR128129E, the first allosteric antagonist of FGFRs. J. Cell. Physiol. 2015;230:43–51. doi: 10.1002/jcp.24656. [DOI] [PubMed] [Google Scholar]
- 163.Katoh M, Nakagama H. FGF receptors: cancer biology and therapeutics. Med. Res. Rev. 2014;34:280–300. doi: 10.1002/med.21288. [DOI] [PubMed] [Google Scholar]
- 164.Kopetz S, et al. Phase II trial of infusional fluorouracil, irinotecan, and bevacizumab for metastatic colorectal cancer: efficacy and circulating angiogenic biomarkers associated with therapeutic resistance. J. Clin. Oncol. 2010;28:453–459. doi: 10.1200/JCO.2009.24.8252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Batchelor TT, et al. AZD2171, a pan-VEGF receptor tyrosine kinase inhibitor, normalizes tumor vasculature and alleviates edema in glioblastoma patients. Cancer Cell. 2007;11:83–95. doi: 10.1016/j.ccr.2006.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Katoh M. Cancer genomics and genetics of FGFR2 (Review) Int. J. Oncol. 2008;33:233–237. [PubMed] [Google Scholar]
- 167.Turner N, Grose R. Fibroblast growth factor signalling: from development to cancer. Nat. Rev. Cancer. 2010;10:116–129. doi: 10.1038/nrc2780. [DOI] [PubMed] [Google Scholar]
- 168.Greulich H, Pollock PM. Targeting mutant fibroblast growth factor receptors in cancer. Trends Mol. Med. 2011;17:283–292. doi: 10.1016/j.molmed.2011.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Cross MJ, Claesson-Welsh L. FGF and VEGF function in angiogenesis: signalling pathways, biological responses and therapeutic inhibition. Trends Pharmacol. Sci. 2001;22:201–207. doi: 10.1016/S0165-6147(00)01676-X. [DOI] [PubMed] [Google Scholar]
- 170.García-Caballero M, et al. Angioprevention of urologic cancers by plant-derived foods. Pharmaceutics. 2022;14:256. doi: 10.3390/pharmaceutics14020256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Aviles RJ, Annex BH, Lederman RJ. Testing clinical therapeutic angiogenesis using basic fibroblast growth factor (FGF-2): Clinical angiogenesis using FGF-2. Br. J. Pharm. 2003;140:637–646. doi: 10.1038/sj.bjp.0705493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Vasudev NS, Reynolds AR. Anti-angiogenic therapy for cancer: current progress, unresolved questions and future directions. Angiogenesis. 2014;17:471–494. doi: 10.1007/s10456-014-9420-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Ding S, Merkulova-Rainon T, Han ZC, Tobelem G. HGF receptor up-regulation contributes to the angiogenic phenotype of human endothelial cells and promotes angiogenesis in vitro. Blood. 2003;101:4816–4822. doi: 10.1182/blood-2002-06-1731. [DOI] [PubMed] [Google Scholar]
- 174.Bonnans C, Chou J, Werb Z. Remodelling the extracellular matrix in development and disease. Nat. Rev. Mol. Cell Biol. 2014;15:786–801. doi: 10.1038/nrm3904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Mulcahy EQX, Colόn RR, Abounader R. HGF/MET signaling in malignant brain tumors. Int. J. Mol. Sci. 2020;21:7546. doi: 10.3390/ijms21207546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Nakamura T, Mizuno S. The discovery of hepatocyte growth factor (HGF) and its significance for cell biology, life sciences and clinical medicine. Proc. Jpn. Acad. B: Phys. Biol. Sci. 2010;86:588–610. doi: 10.2183/pjab.86.588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Bottaro DP, et al. Identification of the hepatocyte growth factor receptor as the c- met proto-oncogene product. Science. 1991;251:802–804. doi: 10.1126/science.1846706. [DOI] [PubMed] [Google Scholar]
- 178.Dean M, et al. The human met oncogene is related to the tyrosine kinase oncogenes. Nature. 1985;318:385–388. doi: 10.1038/318385a0. [DOI] [PubMed] [Google Scholar]
- 179.Ono K, Matsumori A, Shioi T, Furukawa Y, Sasayama S. Enhanced expression of hepatocyte growth factor/c-Met by myocardial ischemia and reperfusion in a rat model. Circulation. 1997;95:2552–2558. doi: 10.1161/01.CIR.95.11.2552. [DOI] [PubMed] [Google Scholar]
- 180.Cai W, Rook SL, Jiang ZY, Takahara N, Aiello LP. Mechanisms of hepatocyte growth factor–induced retinal endothelial cell migration and growth. Invest. Ophthalmol. Vis. Sci. 2000;41:1885–1893. [PubMed] [Google Scholar]
- 181.Ankoma-Sey V, et al. Coordinated induction of VEGF receptors in mesenchymal cell types during rat hepatic wound healing. Oncogene. 1998;17:115–121. doi: 10.1038/sj.onc.1201912. [DOI] [PubMed] [Google Scholar]
- 182.Nagashima M, et al. Hepatocyte growth factor (HGF), HGF activator, and c-Met in synovial tissues in rheumatoid arthritis and osteoarthritis. J. Rheumatol. 2001;28:1772–1778. [PubMed] [Google Scholar]
- 183.Hughes PE, et al. In vitro and in vivo activity of AMG 337, a potent and selective MET kinase inhibitor, in MET-dependent cancer models. Mol. Cancer Ther. 2016;15:1568–1579. doi: 10.1158/1535-7163.MCT-15-0871. [DOI] [PubMed] [Google Scholar]
- 184.Leung E, et al. Blood vessel endothelium-directed tumor cell streaming in breast tumors requires the HGF/C-Met signaling pathway. Oncogene. 2017;36:2680–2692. doi: 10.1038/onc.2016.421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Kuang W, et al. Hepatocyte growth factor induces breast cancer cell invasion via the PI3K/Akt and p38 MAPK signaling pathways to up-regulate the expression of COX2. Am. J. Transl. Res. 2017;9:3816–3826. [PMC free article] [PubMed] [Google Scholar]
- 186.Hartmann S, Bhola NE, Grandis JR. HGF/Met signaling in head and neck cancer: impact on the tumor microenvironment. Clin. Cancer Res. 2016;22:4005–4013. doi: 10.1158/1078-0432.CCR-16-0951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Demuth C, Andersen MN, Jakobsen KR, Madsen AT, Sørensen BS. Increased PD-L1 expression in erlotinib-resistant NSCLC cells with MET gene amplification is reversed upon MET-TKI treatment. Oncotarget. 2017;8:68221–68229. doi: 10.18632/oncotarget.19920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Kwon MJ, et al. Frequent hepatocyte growth factor overexpression and low frequency of c-Met gene amplification in human papillomavirus-negative tonsillar squamous cell carcinoma and their prognostic significances. Hum. Pathol. 2014;45:1327–1338. doi: 10.1016/j.humpath.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 189.Miranda O, Farooqui M, Siegfried JM. Status of agents targeting the HGF/c-Met axis in lung cancer. Cancers. 2018;10:280. doi: 10.3390/cancers10090280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Wang Q, Yang S, Wang K, Sun SY. MET inhibitors for targeted therapy of EGFR TKI-resistant lung cancer. J. Hematol. Oncol. 2019;12:63. doi: 10.1186/s13045-019-0759-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Wu JC, et al. Heteronemin is a novel c-Met/STAT3 inhibitor against advanced prostate cancer cells. Prostate. 2016;76:1469–1483. doi: 10.1002/pros.23230. [DOI] [PubMed] [Google Scholar]
- 192.Imura Y, et al. Functional and therapeutic relevance of hepatocyte growth factor/c‐MET signaling in synovial sarcoma. Cancer Sci. 2016;107:1867–1876. doi: 10.1111/cas.13092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Birchmeier C, Birchmeier W, Gherardi E, Vande Woude GF. Met, metastasis, motility and more. Nat. Rev. Mol. Cell Biol. 2003;4:915–925. doi: 10.1038/nrm1261. [DOI] [PubMed] [Google Scholar]
- 194.Zhang Y, et al. Function of the c-Met receptor tyrosine kinase in carcinogenesis and associated therapeutic opportunities. Mol. Cancer. 2018;17:45. doi: 10.1186/s12943-018-0796-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Scalia P, Giordano A, Williams SJ. The IGF-II-insulin receptor isoform-A autocrine signal in cancer: actionable perspectives. Cancers. 2020;12:366. doi: 10.3390/cancers12020366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Bach LA. Endothelial cells and the IGF system. J. Mol. Endocrinol. 2014;54:R1–R13. doi: 10.1530/JME-14-0215. [DOI] [PubMed] [Google Scholar]
- 197.Clemmons DR. Modifying IGF1 activity: an approach to treat endocrine disorders, atherosclerosis and cancer. Nat. Rev. Drug Discov. 2007;6:821–833. doi: 10.1038/nrd2359. [DOI] [PubMed] [Google Scholar]
- 198.van Beijnum JR, Pieters W, Nowak-Sliwinska P, Griffioen AW. Insulin-like growth factor axis targeting in cancer and tumour angiogenesis—the missing link: IGF signaling in tumor angiogenesis. Biol. Rev. Camb. Philos. Soc. 2017;92:1755–1768. doi: 10.1111/brv.12306. [DOI] [PubMed] [Google Scholar]
- 199.Chantelau E. Evidence that upregulation of serum IGF-1 concentration can trigger acceleration of diabetic retinopathy. Br. J. Ophthalmol. 1998;82:725–730. doi: 10.1136/bjo.82.7.725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Wilkinson-Berka JL, Wraight C, Werther G. The role of growth hormone, insulin-like growth factor and somatostatin in diabetic retinopathy. Curr. Med. Chem. 2006;13:3307–3317. doi: 10.2174/092986706778773086. [DOI] [PubMed] [Google Scholar]
- 201.Higashi Y, Sukhanov S, Anwar A, Shai SY, Delafontaine P. Aging, atherosclerosis, and IGF-1. J. Gerontol. A: Biol. Sci. Med. Sci. 2012;67:626–639. doi: 10.1093/gerona/gls102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Hellstrom A, et al. Low IGF-I suppresses VEGF-survival signaling in retinal endothelial cells: direct correlation with clinical retinopathy of prematurity. Proc. Natl Acad. Sci. USA. 2001;98:5804–5808. doi: 10.1073/pnas.101113998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Smith LEH. Pathogenesis of retinopathy of prematurity. Acta Paediatr. Suppl. 2002;91:26–28. doi: 10.1111/j.1651-2227.2002.tb00157.x. [DOI] [PubMed] [Google Scholar]
- 204.Moschos SJ, Mantzoros CS. The role of the IGF system in cancer: from basic to clinical studies and clinical applications. Oncology. 2002;63:317–332. doi: 10.1159/000066230. [DOI] [PubMed] [Google Scholar]
- 205.Sachdev D, Yee D. The IGF system and breast cancer. Endocr. Relat. Cancer. 2001;8:197–209. doi: 10.1677/erc.0.0080197. [DOI] [PubMed] [Google Scholar]
- 206.Samani AA, Yakar S, LeRoith D, Brodt P. The role of the IGF system in cancer growth and metastasis: overview and recent insights. Endocr. Rev. 2007;28:20–47. doi: 10.1210/er.2006-0001. [DOI] [PubMed] [Google Scholar]
- 207.Baserga R, Peruzzi F, Reiss K. The IGF-1 receptor in cancer biology. Int. J. Cancer. 2003;107:873–877. doi: 10.1002/ijc.11487. [DOI] [PubMed] [Google Scholar]
- 208.Azar WJ, et al. IGFBP-2 enhances VEGF gene promoter activity and consequent promotion of angiogenesis by neuroblastoma cells. Endocrinology. 2011;152:3332–3342. doi: 10.1210/en.2011-1121. [DOI] [PubMed] [Google Scholar]
- 209.Png KJ, Halberg N, Yoshida M, Tavazoie SF. A microRNA regulon that mediates endothelial recruitment and metastasis by cancer cells. Nature. 2011;481:190–194. doi: 10.1038/nature10661. [DOI] [PubMed] [Google Scholar]
- 210.Liu B, et al. Insulin-like growth factor-binding protein-3 inhibition of prostate cancer growth involves suppression of angiogenesis. Oncogene. 2007;26:1811–1819. doi: 10.1038/sj.onc.1209977. [DOI] [PubMed] [Google Scholar]
- 211.Wu MY, Hill CS. TGF-β superfamily signaling in embryonic development and homeostasis. Dev. Cell. 2009;16:329–343. doi: 10.1016/j.devcel.2009.02.012. [DOI] [PubMed] [Google Scholar]
- 212.Yang Y, et al. The role of TGF-β signaling pathways in cancer and its potential as a therapeutic target. Evid. Based Complement Altern. Med. 2021;2021:6675208. doi: 10.1155/2021/6675208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Zhang YE. Non-Smad signaling pathways of the TGF-β family. Cold Spring Harb. Perspect. Biol. 2017;9:a022129. doi: 10.1101/cshperspect.a022129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Santoro R, Carbone C, Piro G, Chiao PJ, Melisi D. TAK-ing aim at chemoresistance: the emerging role of MAP3K7 as a target for cancer therapy. Drug Resist. Updat. 2017;33–35:36–42. doi: 10.1016/j.drup.2017.10.004. [DOI] [PubMed] [Google Scholar]
- 215.Colak S, Ten Dijke P. Targeting TGF-β signaling in cancer. Trends Cancer. 2017;3:56–71. doi: 10.1016/j.trecan.2016.11.008. [DOI] [PubMed] [Google Scholar]
- 216.Platten M, Wick W, Weller M. Malignant glioma biology: Role for TGF-β in growth, motility, angiogenesis, and immune escape. Microsc. Res. Tech. 2001;52:401–410. doi: 10.1002/1097-0029(20010215)52:4<401::AID-JEMT1025>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- 217.Sabbadini F, et al. The multifaceted role of TGF-β in gastrointestinal tumors. Cancers. 2021;13:3960. doi: 10.3390/cancers13163960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Massagué J. TGFβ signalling in context. Nat. Rev. Mol. Cell Biol. 2012;13:616–630. doi: 10.1038/nrm3434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Horiguchi K, et al. Role of Ras signaling in the induction of snail by transforming growth factor-β. J. Biol. Chem. 2009;284:245–253. doi: 10.1074/jbc.M804777200. [DOI] [PubMed] [Google Scholar]
- 220.Korc M. Role of growth factors in pancreatic cancer. Surg. Oncol. Clin. N. Am. 1998;7:25–41. doi: 10.1016/S1055-3207(18)30283-7. [DOI] [PubMed] [Google Scholar]
- 221.Nolan-Stevaux O, et al. GLI1 is regulated through Smoothened-independent mechanisms in neoplastic pancreatic ducts and mediates PDAC cell survival and transformation. Genes Dev. 2009;23:24–36. doi: 10.1101/gad.1753809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Budi EH, Mamai O, Hoffman S, Akhurst RJ, Derynck R. Enhanced TGF-β signaling contributes to the insulin-induced angiogenic responses of endothelial cells. iScience. 2019;11:474–491. doi: 10.1016/j.isci.2018.12.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Darland DC, D’Amore PA. TGFβ is required for the formation of capillary-like structures in three-dimensional cocultures of 10T1/2 and endothelial cells. Angiogenesis. 2001;4:11–20. doi: 10.1023/A:1016611824696. [DOI] [PubMed] [Google Scholar]
- 224.Huynh LK, Hipolito CJ, Ten Dijke P. A perspective on the development of TGF-β inhibitors for cancer treatment. Biomolecules. 2019;9:743. doi: 10.3390/biom9110743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Katz LH, et al. TGF-β signaling in liver and gastrointestinal cancers. Cancer Lett. 2016;379:166–172. doi: 10.1016/j.canlet.2016.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Tsubakihara Y, Moustakas A. Epithelial-mesenchymal transition and metastasis under the control of transforming growth factor β. Int. J. Mol. Sci. 2018;19:3672. doi: 10.3390/ijms19113672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Fu M, Peng D, Lan T, Wei Y, Wei X. Multifunctional regulatory protein connective tissue growth factor (CTGF): a potential therapeutic target for diverse diseases. Acta Pharm. Sin. B. 2022;12:1740–1760. doi: 10.1016/j.apsb.2022.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Pepper MS. Transforming growth factor-β: vasculogenesis, angiogenesis, and vessel wall integrity. Cytokine Growth Factor Rev. 1997;8:21–43. doi: 10.1016/S1359-6101(96)00048-2. [DOI] [PubMed] [Google Scholar]
- 229.Fang L, et al. TGF-β1 induces VEGF expression in human granulosa-lutein cells: a potential mechanism for the pathogenesis of ovarian hyperstimulation syndrome. Exp. Mol. Med. 2020;52:450–460. doi: 10.1038/s12276-020-0396-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Wang H, et al. Methyl-CpG-binding protein 2 drives the Furin/TGF-β1/Smad axis to promote epithelial–mesenchymal transition in pancreatic cancer cells. Oncogenesis. 2020;9:76. doi: 10.1038/s41389-020-00258-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Melisi D, et al. Modulation of pancreatic cancer chemoresistance by inhibition of TAK1. J. Natl Cancer Inst. 2011;103:1190–1204. doi: 10.1093/jnci/djr243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Zhang H, et al. TGFβ signaling in pancreatic ductal adenocarcinoma. Tumor Biol. 2015;36:1613–1618. doi: 10.1007/s13277-014-2757-4. [DOI] [PubMed] [Google Scholar]
- 233.Santoro R, et al. Modulating TAK1 expression inhibits YAP and TAZ oncogenic functions in pancreatic cancer. Mol. Cancer Ther. 2020;19:247–257. doi: 10.1158/1535-7163.MCT-19-0270. [DOI] [PubMed] [Google Scholar]
- 234.Gladilin E, et al. TGFβ-induced cytoskeletal remodeling mediates elevation of cell stiffness and invasiveness in NSCLC. Sci. Rep. 2019;9:7667. doi: 10.1038/s41598-019-43409-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Mazzocca A, Fransvea E, Lavezzari G, Antonaci S, Giannelli G. Inhibition of transforming growth factor β receptor I kinase blocks hepatocellular carcinoma growth through neo-angiogenesis regulation. Hepatology. 2009;50:1140–1151. doi: 10.1002/hep.23118. [DOI] [PubMed] [Google Scholar]
- 236.Bhagyaraj E, et al. TGF-β induced chemoresistance in liver cancer is modulated by xenobiotic nuclear receptor PXR. Cell Cycle. 2019;18:3589–3602. doi: 10.1080/15384101.2019.1693120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Yang Y, et al. GP73 promotes epithelial–mesenchymal transition and invasion partly by activating TGF-β1/Smad2 signaling in hepatocellular carcinoma. Carcinogenesis. 2018;39:900–910. doi: 10.1093/carcin/bgy010. [DOI] [PubMed] [Google Scholar]
- 238.Chiechi A, et al. Role of TGF-β in breast cancer bone metastases. Adv. Biosci. Biotechnol. 2013;4:15–30. doi: 10.4236/abb.2013.410A4003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Masoud GN, Li W. HIF-1α pathway: role, regulation and intervention for cancer therapy. Acta Pharm. Sin. B. 2015;5:378–389. doi: 10.1016/j.apsb.2015.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Yang Y, Sun M, Wang L, Jiao B. HIFs, angiogenesis, and cancer. J. Cell. Biochem. 2013;114:967–974. doi: 10.1002/jcb.24438. [DOI] [PubMed] [Google Scholar]
- 241.Konisti S, Kiriakidis S, Paleolog EM. Hypoxia—a key regulator of angiogenesis and inflammation in rheumatoid arthritis. Nat. Rev. Rheumatol. 2012;8:153–162. doi: 10.1038/nrrheum.2011.205. [DOI] [PubMed] [Google Scholar]
- 242.Ahluwalia A, Tarnawski AS. Critical role of hypoxia sensor—HIF-1 in VEGF gene activation. Implications for angiogenesis and tissue injury healing. Curr. Med. Chem. 2012;19:90–97. doi: 10.2174/092986712803413944. [DOI] [PubMed] [Google Scholar]
- 243.Tanaka T, Nangaku M. Angiogenesis and hypoxia in the kidney. Nat. Rev. Nephrol. 2013;9:211–222. doi: 10.1038/nrneph.2013.35. [DOI] [PubMed] [Google Scholar]
- 244.Chen L, Endler A, Shibasaki F. Hypoxia and angiogenesis: regulation of hypoxia-inducible factors via novel binding factors. Exp. Mol. Med. 2009;41:849–857. doi: 10.3858/emm.2009.41.12.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Ikeda H, Kakeya H. Targeting hypoxia-inducible factor 1 (HIF-1) signaling with natural products toward cancer chemotherapy. J. Antibiot. 2021;74:687–695. doi: 10.1038/s41429-021-00451-0. [DOI] [PubMed] [Google Scholar]
- 246.Pugh CW, Ratcliffe PJ. Regulation of angiogenesis by hypoxia: role of the HIF system. Nat. Med. 2003;9:677–684. doi: 10.1038/nm0603-677. [DOI] [PubMed] [Google Scholar]
- 247.Semenza GL. Targeting hypoxia-inducible factor 1 to stimulate tissue vascularization. J. Investig. Med. 2016;64:361–363. doi: 10.1097/JIM.0000000000000206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Vleugel MM, et al. Differential prognostic impact of hypoxia induced and diffuse HIF-1 expression in invasive breast cancer. J. Clin. Pathol. 2005;58:172–177. doi: 10.1136/jcp.2004.019885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Dales JP, et al. Overexpression of hypoxia-inducible factor HIF-1α predicts early relapse in breast cancer: retrospective study in a series of 745 patients. Int. J. Cancer. 2005;116:734–739. doi: 10.1002/ijc.20984. [DOI] [PubMed] [Google Scholar]
- 250.Yatabe N, et al. HIF-1-mediated activation of telomerase in cervical cancer cells. Oncogene. 2004;23:3708–3715. doi: 10.1038/sj.onc.1207460. [DOI] [PubMed] [Google Scholar]
- 251.Pezzuto A, et al. A close relationship between HIF-1α expression and bone metastases in advanced NSCLC, a retrospective analysis. Oncotarget. 2019;10:7071–7079. doi: 10.18632/oncotarget.27378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Jackson AL, Zhou B, Kim WY. HIF, hypoxia and the role of angiogenesis in non-small cell lung cancer. Expert Opin. Ther. Targets. 2010;14:1047–1057. doi: 10.1517/14728222.2010.511617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Liu K, et al. The changes of HIF-1α and VEGF expression after TACE in patients with hepatocellular carcinoma. J. Clin. Med. Res. 2016;8:297–302. doi: 10.14740/jocmr2496w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Zheng SS, Chen XH, Yin X, Zhang BH. Prognostic significance of HIF-1α expression in hepatocellular carcinoma: a meta-analysis. PLoS ONE. 2013;8:e65753. doi: 10.1371/journal.pone.0065753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Semenza GL. Targeting HIF-1 for cancer therapy. Nat. Rev. Cancer. 2003;3:721–732. doi: 10.1038/nrc1187. [DOI] [PubMed] [Google Scholar]
- 256.Schöning JP, Monteiro M, Gu W. Drug resistance and cancer stem cells: the shared but distinct roles of hypoxia‐inducible factors HIF 1α and HIF 2α. Clin. Exp. Pharmacol. Physiol. 2017;44:153–161. doi: 10.1111/1440-1681.12693. [DOI] [PubMed] [Google Scholar]
- 257.Rohwer N, Cramer T. Hypoxia-mediated drug resistance: Novel insights on the functional interaction of HIFs and cell death pathways. Drug Resist. Updat. 2011;14:191–201. doi: 10.1016/j.drup.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 258.Zhang Q, Lenardo MJ, Baltimore D. 30 years of NF-κB: a blossoming of relevance to human pathobiology. Cell. 2017;168:37–57. doi: 10.1016/j.cell.2016.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Iosef C, et al. Inhibiting NF-κB in the developing lung disrupts angiogenesis and alveolarization. Am. J. Physiol. Lung Cell. Mol. Physiol. 2012;302:L1023–L1036. doi: 10.1152/ajplung.00230.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Sakamoto K, et al. Constitutive NF-κB activation in colorectal carcinoma plays a key role in angiogenesis, promoting tumor growth. Clin. Cancer Res. 2009;15:2248–2258. doi: 10.1158/1078-0432.CCR-08-1383. [DOI] [PubMed] [Google Scholar]
- 261.Huang S, Pettaway CA, Uehara H, Bucana CD, Fidler IJ. Blockade of NF-kappaB activity in human prostate cancer cells is associated with suppression of angiogenesis, invasion, and metastasis. Oncogene. 2001;20:4188–4197. doi: 10.1038/sj.onc.1204535. [DOI] [PubMed] [Google Scholar]
- 262.Davis S, et al. Angiopoietins have distinct modular domains essential for receptor binding, dimerization and superclustering. Nat. Struct. Biol. 2003;10:38–44. doi: 10.1038/nsb880. [DOI] [PubMed] [Google Scholar]
- 263.Saharinen P, Eklund L, Alitalo K. Therapeutic targeting of the angiopoietin-TIE pathway. Nat. Rev. Drug Discov. 2017;16:635–661. doi: 10.1038/nrd.2016.278. [DOI] [PubMed] [Google Scholar]
- 264.Partanen J, et al. A novel endothelial cell surface receptor tyrosine kinase with extracellular epidermal growth factor homology domains. Mol. Cell. Biol. 1992;12:1698–1707. doi: 10.1128/mcb.12.4.1698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Fagiani E, Christofori G. Angiopoietins in angiogenesis. Cancer Lett. 2013;328:18–26. doi: 10.1016/j.canlet.2012.08.018. [DOI] [PubMed] [Google Scholar]
- 266.Shim WSN, Ho IAW, Wong PEH. Angiopoietin: a TIE(d) balance in tumor angiogenesis. Mol. Cancer Res. 2007;5:655–665. doi: 10.1158/1541-7786.MCR-07-0072. [DOI] [PubMed] [Google Scholar]
- 267.Gillen J, Richardson DL, Moore KN. Angiopoietin-1 and angiopoietin-2 inhibitors: clinical development. Curr. Oncol. Rep. 2019;21:22. doi: 10.1007/s11912-019-0771-9. [DOI] [PubMed] [Google Scholar]
- 268.Eklund L, Kangas J, Saharinen P. Angiopoietin–Tie signalling in the cardiovascular and lymphatic systems. Cancer Sci. 2016;131:87–103. doi: 10.1042/CS20160129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Takahama M, et al. Enhanced expression of Tie2, its ligand angiopoietin-1, vascular endothelial growth factor, and CD31 in human non-small cell lung carcinomas1. Clin. Cancer Res. 1999;5:2506–2510. [PubMed] [Google Scholar]
- 270.Tangkeangsirisin W, Hayashi J, Serrero G. PC Cell-derived growth factor mediates tamoxifen resistance and promotes tumor growth of human breast cancer cells. Cancer Res. 2004;64:1737–1743. doi: 10.1158/0008-5472.CAN-03-2364. [DOI] [PubMed] [Google Scholar]
- 271.Shirakawa K, et al. Absence of endothelial cells, central necrosis, and fibrosis are associated with aggressive inflammatory breast cancer. Cancer Res. 2001;61:445–451. [PubMed] [Google Scholar]
- 272.Martoglio AM, et al. Changes in tumorigenesis- and angiogenesis-related gene transcript abundance profiles in ovarian cancer detected by tailored high density cDNA arrays. Mol. Med. 2000;6:750–765. doi: 10.1007/BF03402191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Ding H, et al. Expression and hypoxic regulation of angiopoietins in human astrocytomas. Neuro Oncol. 2001;3:1–10. doi: 10.1093/neuonc/3.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Stratmann A, Risau W, Plate KH. Cell type-specific expression of angiopoietin-1 and angiopoietin-2 suggests a role in glioblastoma angiogenesis. Am. J. Pathol. 1998;153:1459–1466. doi: 10.1016/S0002-9440(10)65733-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Udani V, et al. Differential expression of angiopoietin-1 and angiopoietin-2 may enhance recruitment of bone marrow-derived endothelial precursor cells into brain tumors. Neurol. Res. 2005;27:801–806. doi: 10.1179/016164105X49319. [DOI] [PubMed] [Google Scholar]
- 276.Thurston G, Daly C. The complex role of angiopoietin-2 in the angiopoietin-Tie signaling pathway. Cold Spring Harb. Perspect. Med. 2012;2:a006650. doi: 10.1101/cshperspect.a006650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Eklund L, Saharinen P. Angiopoietin signaling in the vasculature. Exp. Cell Res. 2013;319:1271–1280. doi: 10.1016/j.yexcr.2013.03.011. [DOI] [PubMed] [Google Scholar]
- 278.Bolós V, Grego-Bessa J, de la Pompa JL. Notch signaling in development and cancer. Endocr. Rev. 2007;28:339–363. doi: 10.1210/er.2006-0046. [DOI] [PubMed] [Google Scholar]
- 279.Ranganathan P, Weaver KL, Capobianco AJ. Notch signalling in solid tumours: a little bit of everything but not all the time. Nat. Rev. Cancer. 2011;11:338–351. doi: 10.1038/nrc3035. [DOI] [PubMed] [Google Scholar]
- 280.Takeshita K, et al. Critical role of endothelial notch1 signaling in postnatal Angiogenesis. Circ. Res. 2007;100:70–78. doi: 10.1161/01.RES.0000254788.47304.6e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Blanco R, Gerhardt H. VEGF and Notch in tip and stalk cell selection. Cold Spring Harb. Perspect. Med. 2013;3:a006569. doi: 10.1101/cshperspect.a006569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Radtke F, Raj K. The role of Notch in tumorigenesis: oncogene or tumour suppressor? Nat. Rev. Cancer. 2003;3:756–767. doi: 10.1038/nrc1186. [DOI] [PubMed] [Google Scholar]
- 283.Gustafsson MV, et al. Hypoxia requires Notch signaling to maintain the undifferentiated cell state. Dev. Cell. 2005;9:617–628. doi: 10.1016/j.devcel.2005.09.010. [DOI] [PubMed] [Google Scholar]
- 284.Sainson RC, Harris AL. Hypoxia-regulated differentiation: let’s step it up a Notch. Trends Mol. Med. 2006;12:141–143. doi: 10.1016/j.molmed.2006.02.001. [DOI] [PubMed] [Google Scholar]
- 285.Diez H, et al. Hypoxia-mediated activation of Dll4-Notch-Hey2 signaling in endothelial progenitor cells and adoption of arterial cell fate. Exp. Cell Res. 2007;313:1–9. doi: 10.1016/j.yexcr.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 286.Patel NS, et al. Up-regulation of delta-like 4 ligand in human tumor vasculature and the role of basal expression in endothelial cell function. Cancer Res. 2005;65:8690–8697. doi: 10.1158/0008-5472.CAN-05-1208. [DOI] [PubMed] [Google Scholar]
- 287.Reedijk M, et al. High-level coexpression of JAG1 and NOTCH1 is observed in human breast cancer and is associated with poor overall survival. Cancer Res. 2005;65:8530–8537. doi: 10.1158/0008-5472.CAN-05-1069. [DOI] [PubMed] [Google Scholar]
- 288.Tschaharganeh DF, et al. Yes-associated protein up-regulates Jagged-1 and activates the NOTCH pathway in human hepatocellular carcinoma. Gastroenterology. 2013;144:1530–1542. doi: 10.1053/j.gastro.2013.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Yousif NG, et al. Notch1 ligand signaling pathway activated in cervical cancer: poor prognosis with high-level JAG1/Notch1. Arch. Gynecol. Obstet. 2015;292:899–904. doi: 10.1007/s00404-015-3694-1. [DOI] [PubMed] [Google Scholar]
- 290.Che L, et al. Jagged 1 is a major Notch ligand along cholangiocarcinoma development in mice and humans. Oncogenesis. 2016;5:e274. doi: 10.1038/oncsis.2016.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Bellon M, Moles R, Chaib-Mezrag H, Pancewicz J, Nicot C. JAG1 overexpression contributes to Notch1 signaling and the migration of HTLV-1-transformed ATL cells. J. Hematol. Oncol. 2018;11:119. doi: 10.1186/s13045-018-0665-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Sethi N, Dai X, Winter CG, Kang Y. Tumor-derived JAGGED1 promotes osteolytic bone metastasis of breast cancer by engaging notch signaling in bone cells. Cancer Cell. 2011;19:192–205. doi: 10.1016/j.ccr.2010.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Sjölund J, et al. Suppression of renal cell carcinoma growth by inhibition of Notch signaling in vitro and in vivo. J. Clin. Invest. 2008;118:217–228. doi: 10.1172/JCI32086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Schneider M, et al. Inhibition of Delta-induced Notch signaling using fucose analogs. Nat. Chem. Biol. 2018;14:65–71. doi: 10.1038/nchembio.2520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Sahlgren C, Gustafsson MV, Jin S, Poellinger L, Lendahl U. Notch signaling mediates hypoxia-induced tumor cell migration and invasion. Proc. Natl Acad. Sci. USA. 2008;105:6392–6397. doi: 10.1073/pnas.0802047105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Surawska H, Ma PC, Salgia R. The role of ephrins and Eph receptors in cancer. Cytokine Growth Factor Rev. 2004;15:419–433. doi: 10.1016/j.cytogfr.2004.09.002. [DOI] [PubMed] [Google Scholar]
- 297.Zozulya SA, Udovichenko IP. Eph family receptors as therapeutic targets. Bioorg. Khim. 2012;38:267–279. doi: 10.1134/s106816201203017x. [DOI] [PubMed] [Google Scholar]
- 298.Zhang J, Hughes S. Role of the ephrin and Eph receptor tyrosine kinase families in angiogenesis and development of the cardiovascular system. J. Pathol. 2006;208:453–461. doi: 10.1002/path.1937. [DOI] [PubMed] [Google Scholar]
- 299.Batlle E, Wilkinson DG. Molecular mechanisms of cell segregation and boundary formation in development and tumorigenesis. Cold Spring Harb. Perspect. Biol. 2012;4:a008227. doi: 10.1101/cshperspect.a008227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Pasquale EB. Eph receptor signalling casts a wide net on cell behaviour. Nat. Rev. Mol. Cell Biol. 2005;6:462–475. doi: 10.1038/nrm1662. [DOI] [PubMed] [Google Scholar]
- 301.Pasquale EB. Eph-ephrin bidirectional signaling in physiology and disease. Cell. 2008;133:38–52. doi: 10.1016/j.cell.2008.03.011. [DOI] [PubMed] [Google Scholar]
- 302.Du E, Li X, He S, Li X, He S. The critical role of the interplays of EphrinB2/EphB4 and VEGF in the induction of angiogenesis. Mol. Biol. Rep. 2020;47:4681–4690. doi: 10.1007/s11033-020-05470-y. [DOI] [PubMed] [Google Scholar]
- 303.Yuan C, et al. Overexpression of ephrinB2 in stem cells from apical papilla accelerates angiogenesis. Oral. Dis. 2019;25:848–859. doi: 10.1111/odi.13042. [DOI] [PubMed] [Google Scholar]
- 304.You C, et al. EphB4 forward signalling mediates angiogenesis caused by CCM3/PDCD10-ablation. J. Cell. Mol. Med. 2017;21:1848–1858. doi: 10.1111/jcmm.13105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Yang D, et al. EphrinB2/EphB4 pathway in postnatal angiogenesis: a potential therapeutic target for ischemic cardiovascular disease. Angiogenesis. 2016;19:297–309. doi: 10.1007/s10456-016-9514-9. [DOI] [PubMed] [Google Scholar]
- 306.Pierscianek D, et al. Study of angiogenic signaling pathways in hemangioblastoma. Neuropathology. 2017;37:3–11. doi: 10.1111/neup.12316. [DOI] [PubMed] [Google Scholar]
- 307.Avraamides CJ, Garmy-Susini B, Varner JA. Integrins in angiogenesis and lymphangiogenesis. Nat. Rev. Cancer. 2008;8:604–617. doi: 10.1038/nrc2353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Bergonzini C, Kroese K, Zweemer AJM, Danen EHJ. Targeting integrins for cancer therapy - disappointments and opportunities. Front. Cell Dev. Biol. 2022;10:863850. doi: 10.3389/fcell.2022.863850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Takada Y, Ye X, Simon S. The integrins. Genome Biol. 2007;8:215. doi: 10.1186/gb-2007-8-5-215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Hynes RO. Integrins. Cell. 2002;110:673–687. doi: 10.1016/S0092-8674(02)00971-6. [DOI] [PubMed] [Google Scholar]
- 311.Mezu-Ndubuisi OJ, Maheshwari A. The role of integrins in inflammation and angiogenesis. Pediatr. Res. 2021;89:1619–1626. doi: 10.1038/s41390-020-01177-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Huveneers S, Danen EH. Adhesion signaling – crosstalk between integrins, Src and Rho. J. Cell Sci. 2009;122:1059–1069. doi: 10.1242/jcs.039446. [DOI] [PubMed] [Google Scholar]
- 313.Łasiñska I, Mackiewicz J. Integrins as a new target for cancer treatment. Anticancer Agents Med. Chem. 2019;19:580–586. doi: 10.2174/1871520618666181119103413. [DOI] [PubMed] [Google Scholar]
- 314.Trikha M, et al. CNTO 95, a fully human monoclonal antibody that inhibits? αv integrins, has antitumor and antiangiogenic activityin vivo. Int. J. Cancer. 2004;110:326–335. doi: 10.1002/ijc.20116. [DOI] [PubMed] [Google Scholar]
- 315.Mitjans F, et al. In vivo therapy of malignant melanoma by means of antagonists of αv integrins. Int. J. Cancer. 2000;87:716–723. doi: 10.1002/1097-0215(20000901)87:5<716::AID-IJC14>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 316.Khalili P, et al. A non–RGD-based integrin binding peptide (ATN-161) blocks breast cancer growth and metastasis in vivo. Mol. Cancer Ther. 2006;5:2271–2280. doi: 10.1158/1535-7163.MCT-06-0100. [DOI] [PubMed] [Google Scholar]
- 317.Garmy-Susini B, et al. Integrin α4β1–VCAM-1–mediated adhesion between endothelial and mural cells is required for blood vessel maturation. J. Clin. Invest. 2005;115:1542–1551. doi: 10.1172/JCI23445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Kim S, Bell K, Mousa SA, Varner JA. Regulation of angiogenesis in vivo by ligation of integrin α5β1 with the central cell-binding domain of fibronectin. Am. J. Pathol. 2000;156:1345–1362. doi: 10.1016/S0002-9440(10)65005-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319.Vlahakis NE, et al. Integrin α9β1 directly binds to vascular endothelial growth factor (VEGF)-A and contributes to VEGF-A-induced angiogenesis. J. Biol. Chem. 2007;282:15187–15196. doi: 10.1074/jbc.M609323200. [DOI] [PubMed] [Google Scholar]
- 320.Rooprai HK, Rucklidge GJ, Panou C, Pilkington GJ. The effects of exogenous growth factors on matrix metalloproteinase secretion by human brain tumour cells. Br. J. Cancer. 2000;82:52–55. doi: 10.1054/bjoc.1999.0876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Laronha H, Caldeira J. Structure and function of human matrix metalloproteinases. Cells. 2020;9:1076. doi: 10.3390/cells9051076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322.Quintero-Fabián S, et al. Role of matrix metalloproteinases in angiogenesis and cancer. Front. Oncol. 2019;9:1370. doi: 10.3389/fonc.2019.01370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.Kessenbrock K, Plaks V, Werb Z. Matrix metalloproteinases: regulators of the tumor microenvironment. Cell. 2010;141:52–67. doi: 10.1016/j.cell.2010.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.Chantrain CF, et al. Stromal matrix metalloproteinase-9 regulates the vascular architecture in neuroblastoma by promoting pericyte recruitment. Cancer Res. 2004;64:1675–1686. doi: 10.1158/0008-5472.CAN-03-0160. [DOI] [PubMed] [Google Scholar]
- 325.Lafleur MA, Handsley MM, Knäuper V, Murphy G, Edwards DR. Endothelial tubulogenesis within fibrin gels specifically requires the activity of membrane-type-matrix metalloproteinases (MT-MMPs) J. Cell Sci. 2002;115:3427–3438. doi: 10.1242/jcs.115.17.3427. [DOI] [PubMed] [Google Scholar]
- 326.Huang H. Matrix metalloproteinase-9 (MMP-9) as a cancer biomarker and MMP-9 biosensors: recent advances. Sensors. 2018;18:3249. doi: 10.3390/s18103249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327.Itoh T, et al. Reduced angiogenesis and tumor progression in gelatinase A-deficient mice1. Cancer Res. 1998;58:1048–1051. [PubMed] [Google Scholar]
- 328.Gálvez BG, Matías-Román S, Albar JP, Sánchez-Madrid F, Arroyo AG. Membrane type 1-matrix metalloproteinase is activated during migration of human endothelial cells and modulates endothelial motility and matrix remodeling. J. Biol. Chem. 2001;276:37491–37500. doi: 10.1074/jbc.M104094200. [DOI] [PubMed] [Google Scholar]
- 329.Hiraoka N, Allen E, Apel IJ, Gyetko MR, Weiss SJ. Matrix metalloproteinases regulate neovascularization by acting as pericellular fibrinolysins. Cell. 1998;95:365–377. doi: 10.1016/S0092-8674(00)81768-7. [DOI] [PubMed] [Google Scholar]
- 330.Huo N, et al. MMP-7 (matrilysin) accelerated growth of human umbilical vein endothelial cells. Cancer Lett. 2002;177:95–100. doi: 10.1016/S0304-3835(01)00772-8. [DOI] [PubMed] [Google Scholar]
- 331.Whitelock JM, Murdoch AD, Iozzo RV, Underwood PA. The degradation of human endothelial cell-derived perlecan and release of bound basic fibroblast growth factor by stromelysin, collagenase, plasmin, and heparanases. J. Biol. Chem. 1996;271:10079–10086. doi: 10.1074/jbc.271.17.10079. [DOI] [PubMed] [Google Scholar]
- 332.Horejs CM. Basement membrane fragments in the context of the epithelial-to-mesenchymal transition. Eur. J. Cell Biol. 2016;95:427–440. doi: 10.1016/j.ejcb.2016.06.002. [DOI] [PubMed] [Google Scholar]
- 333.Nieto MA. The ins and outs of the epithelial to mesenchymal transition in health and disease. Annu. Rev. Cell Dev. Biol. 2011;27:347–376. doi: 10.1146/annurev-cellbio-092910-154036. [DOI] [PubMed] [Google Scholar]
- 334.Seo DW, et al. TIMP-2 mediated inhibition of angiogenesis: an MMP-independent mechanism. Cell. 2003;114:171–180. doi: 10.1016/S0092-8674(03)00551-8. [DOI] [PubMed] [Google Scholar]
- 335.Schnaper HW, et al. Type IV collagenase(s) and TIMPs modulate endothelial cell morphogenesis in vitro. J. Cell. Physiol. 1993;156:235–246. doi: 10.1002/jcp.1041560204. [DOI] [PubMed] [Google Scholar]
- 336.Murphy AN, Unsworth EJ, Stetler-Stevenson WG. Tissue inhibitor of metalloproteinases-2 inhibits bFGF-induced human microvascular endothelial cell proliferation. J. Cell. Physiol. 1993;157:351–358. doi: 10.1002/jcp.1041570219. [DOI] [PubMed] [Google Scholar]
- 337.Hutzen B, et al. Treatment of medulloblastoma with oncolytic measles viruses expressing the angiogenesis inhibitors endostatin and angiostatin. BMC Cancer. 2014;14:206. doi: 10.1186/1471-2407-14-206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338.Egeblad M, Werb Z. New functions for the matrix metalloproteinases in cancer progression. Nat. Rev. Cancer. 2002;2:161–174. doi: 10.1038/nrc745. [DOI] [PubMed] [Google Scholar]
- 339.Frisch A, et al. Apelin controls angiogenesis-dependent glioblastoma growth. Int. J. Mol. Sci. 2020;21:4179. doi: 10.3390/ijms21114179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 340.Tong M, Jun T, Nie Y, Hao J, Fan D. The role of the Slit/Robo signaling pathway. J. Cancer. 2019;10:2694–2705. doi: 10.7150/jca.31877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341.Nikitenko LL, Fox SB, Kehoe S, Rees MC, Bicknell R. Adrenomedullin and tumour angiogenesis. Br. J. Cancer. 2006;94:1–7. doi: 10.1038/sj.bjc.6602832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 342.Ribatti D, Nico B, Spinazzi R, Vacca A, Nussdorfer GG. The role of adrenomedullin in angiogenesis. Peptides. 2005;26:1670–1675. doi: 10.1016/j.peptides.2005.02.017. [DOI] [PubMed] [Google Scholar]
- 343.Gately S, Li WW. Multiple roles of COX-2 in tumor angiogenesis: a target for antiangiogenic therapy. Semin. Oncol. 2004;31:2–11. doi: 10.1053/j.seminoncol.2004.03.040. [DOI] [PubMed] [Google Scholar]
- 344.Toomey DP, Murphy JF, Conlon KC. COX-2, VEGF and tumour angiogenesis. Surgeon. 2009;7:174–180. doi: 10.1016/S1479-666X(09)80042-5. [DOI] [PubMed] [Google Scholar]
- 345.Belperio JA, et al. CXC chemokines in angiogenesis. J. Leukoc. Biol. 2000;68:1–8. doi: 10.1189/jlb.68.1.1. [DOI] [PubMed] [Google Scholar]
- 346.Strieter RM, Belperio JA, Phillips RJ, Keane MP. CXC chemokines in angiogenesis of cancer. Semin. Cancer Biol. 2004;14:195–200. doi: 10.1016/j.semcancer.2003.10.006. [DOI] [PubMed] [Google Scholar]
- 347.Ribatti D. Interleukins as modulators of angiogenesis and anti-angiogenesis in tumors. Cytokine. 2019;118:3–7. doi: 10.1016/j.cyto.2018.10.022. [DOI] [PubMed] [Google Scholar]
- 348.Indraccolo, S. Interferon-α as angiogenesis inhibitor: learning from tumor models. Autoimmunity43, 244–247 (2010). [DOI] [PubMed]
- 349.Xiao HB, et al. Interferon-β efficiently inhibited endothelial progenitor cell-induced tumor angiogenesis. Gene Ther. 2012;19:1030–1034. doi: 10.1038/gt.2011.171. [DOI] [PubMed] [Google Scholar]
- 350.Takano S, Ishikawa E, Matsuda M, Yamamoto T, Matsumura A. Interferon-β inhibits glioma angiogenesis through downregulation of vascular endothelial growth factor and upregulation of interferon inducible protein 10. Int. J. Oncol. 2014;45:1837–1846. doi: 10.3892/ijo.2014.2620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351.Murohara T, et al. Nitric oxide synthase modulates angiogenesis in response to tissue ischemia. J. Clin. Invest. 1998;101:2567–2578. doi: 10.1172/JCI1560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 352.Perez-Pinera P, Berenson JR, Deuel TF. Pleiotrophin, a multifunctional angiogenic factor: mechanisms and pathways in normal and pathological angiogenesis. Curr. Opin. Hematol. 2008;15:210–214. doi: 10.1097/MOH.0b013e3282fdc69e. [DOI] [PubMed] [Google Scholar]
- 353.Albrecht ED, Pepe EJ. Steroid hormone regulation of angiogenesis in the primate endometrium. Front. Biosci. 2003;8:d416–d429. doi: 10.2741/1001. [DOI] [PubMed] [Google Scholar]
- 354.DiPietro, L. A. & Polverini, P. J. in Molecular, Cellular, and Clinical Aspects of Angiogenesis (ed. Maragoudakis, M. E.) 105–113 (Springer, 1996).
- 355.Huang T, Sun L, Yuan X, Qiu H. Thrombospondin-1 is a multifaceted player in tumor progression. Oncotarget. 2017;8:84546–84558. doi: 10.18632/oncotarget.19165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 356.Marshall E. The roadblocks to angiogenesis blockers. Science. 1998;280:997. doi: 10.1126/science.280.5366.997. [DOI] [Google Scholar]
- 357.Marshall E. The power of the front page of The New York Times. Science. 1998;280:996–997. doi: 10.1126/science.280.5366.996. [DOI] [PubMed] [Google Scholar]
- 358.Boehm T, Folkman J, Browder T, O’Reilly MS. Antiangiogenic therapy of experimental cancer does not induce acquired drug resistance. Nature. 1997;390:404–407. doi: 10.1038/37126. [DOI] [PubMed] [Google Scholar]
- 359.O’Reilly MS, et al. Endostatin: an endogenous inhibitor of angiogenesis and tumor growth. Cell. 1997;88:277–285. doi: 10.1016/S0092-8674(00)81848-6. [DOI] [PubMed] [Google Scholar]
- 360.Denekamp J. Review article: angiogenesis, neovascular proliferation and vascular pathophysiology as targets for cancer therapy. Br. J. Radiol. 1993;66:181–196. doi: 10.1259/0007-1285-66-783-181. [DOI] [PubMed] [Google Scholar]
- 361.Weidner N, Semple JP, Welch WR, Folkman J. Tumor angiogenesis and metastasis—correlation in invasive breast carcinoma. N. Engl. J. Med. 1991;324:1–8. doi: 10.1056/NEJM199101033240101. [DOI] [PubMed] [Google Scholar]
- 362.Folkman J. Successful treatment of an angiogenic disease. N. Engl. J. Med. 1989;320:1211–1212. doi: 10.1056/NEJM198905043201811. [DOI] [PubMed] [Google Scholar]
- 363.Ingber D, et al. Synthetic analogues of fumagillin that inhibit angiogenesis and suppress tumour growth. Nature. 1990;348:555–557. doi: 10.1038/348555a0. [DOI] [PubMed] [Google Scholar]
- 364.Senger DR, et al. Tumor cells secrete a vascular permeability factor that promotes accumulation of ascites fluid. Science. 1983;219:983–985. doi: 10.1126/science.6823562. [DOI] [PubMed] [Google Scholar]
- 365.Liu K, et al. Targeting the vasculature in hepatocellular carcinoma treatment: Starving versus normalizing blood supply. Clin. Transl. Gastroenterol. 2017;8:e98. doi: 10.1038/ctg.2017.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 366.Jain RK. Antiangiogenesis strategies revisited: from starving tumors to alleviating hypoxia. Cancer Cell. 2014;26:605–622. doi: 10.1016/j.ccell.2014.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 367.Gupta K, Zhang J. Angiogenesis: a curse or cure? Postgrad. Med. J. 2005;81:236–242. doi: 10.1136/pgmj.2004.023309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 368.Shchors K, Evan G. Tumor angiogenesis: cause or consequence of cancer? Cancer Res. 2007;67:7059–7061. doi: 10.1158/0008-5472.CAN-07-2053. [DOI] [PubMed] [Google Scholar]
- 369.Goel S, Wong AH, Jain RK. Vascular normalization as a therapeutic strategy for malignant and nonmalignant disease. Cold Spring Harb. Perspect. Med. 2012;2:a006486. doi: 10.1101/cshperspect.a006486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 370.Jain RK. Normalization of tumor vasculature: an emerging concept in antiangiogenic therapy. Science. 2005;307:58–62. doi: 10.1126/science.1104819. [DOI] [PubMed] [Google Scholar]
- 371.Jain RK. Normalizing tumor vasculature with anti-angiogenic therapy: a new paradigm for combination therapy. Nat. Med. 2001;7:987–989. doi: 10.1038/nm0901-987. [DOI] [PubMed] [Google Scholar]
- 372.He L, et al. Antiangiogenic effects of recombinant human endostatin in lung cancers. Mol. Med. Rep. 2018;17:79–86. doi: 10.3892/mmr.2017.7859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 373.Wang J, Zhu C. Anticoagulation in combination with antiangiogenesis and chemotherapy for cancer patients: evidence and hypothesis. Onco Targets Ther. 2016;9:4737–4746. doi: 10.2147/OTT.S103184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 374.Sato Y. Persistent vascular normalization as an alternative goal of anti-angiogenic cancer therapy. Cancer Sci. 2011;102:1253–1256. doi: 10.1111/j.1349-7006.2011.01929.x. [DOI] [PubMed] [Google Scholar]
- 375.Wong PP, Bodrug N, Hodivala-Dilke KM. Exploring novel methods for modulating tumor blood vessels in cancer treatment. Curr. Biol. 2016;26:R1161–R1166. doi: 10.1016/j.cub.2016.09.043. [DOI] [PubMed] [Google Scholar]
- 376.Li W, Quan YY, Li Y, Lu L, Cui M. Monitoring of tumor vascular normalization: the key points from basic research to clinical application. Cancer Manag. Res. 2018;10:4163–4172. doi: 10.2147/CMAR.S174712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 377.Zheng R, Li F, Li F, Gong A. Targeting tumor vascularization: promising strategies for vascular normalization. J. Cancer Res. Clin. Oncol. 2021;147:2489–2505. doi: 10.1007/s00432-021-03701-8. [DOI] [PubMed] [Google Scholar]
- 378.Luo X, et al. Inducing vascular normalization: a promising strategy for immunotherapy. Int. Immunopharmacol. 2022;112:109167. doi: 10.1016/j.intimp.2022.109167. [DOI] [PubMed] [Google Scholar]
- 379.Kerr DJ. Targeting angiogenesis in cancer: clinical development of bevacizumab. Nat. Clin. Pract. Oncol. 2004;1:39–43. doi: 10.1038/ncponc0026. [DOI] [PubMed] [Google Scholar]
- 380.Kim ES, et al. Potent VEGF blockade causes regression of coopted vessels in a model of neuroblastoma. Proc. Natl Acad. Sci. USA. 2002;99:11399–11404. doi: 10.1073/pnas.172398399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 381.Cohen P, Cross D, Jänne PA. Kinase drug discovery 20 years after imatinib: progress and future directions. Nat. Rev. Drug Discov. 2021;20:551–569. doi: 10.1038/s41573-021-00195-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 382.Oholendt AL, Zadlo JL. Ramucirumab: a new therapy for advanced gastric cancer. J. Adv. Pract. Oncol. 2015;6:71–75. doi: 10.6004/jadpro.2015.6.1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 383.Lowery CD, et al. Anti-VEGFR2 therapy delays growth of preclinical pediatric tumor models and enhances anti-tumor activity of chemotherapy. Oncotarget. 2019;10:5523–5533. doi: 10.18632/oncotarget.27148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 384.Garcia-Carbonero R, et al. An open-label phase II study evaluating the safety and efficacy of ramucirumab combined with mFOLFOX-6 as first-line therapy for metastatic colorectal cancer. Oncologist. 2014;19:350–351. doi: 10.1634/theoncologist.2014-0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 385.Shirley M. Olaratumab: first global approval. Drugs. 2017;77:107–112. doi: 10.1007/s40265-016-0680-2. [DOI] [PubMed] [Google Scholar]
- 386.Tap WD, et al. Effect of doxorubicin plus olaratumab vs doxorubicin plus placebo on survival in patients with advanced soft tissue sarcomas: the ANNOUNCE randomized clinical trial. JAMA. 2020;323:1266–1276. doi: 10.1001/jama.2020.1707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 387.Tap WD, et al. Olaratumab and doxorubicin versus doxorubicin alone for treatment of soft-tissue sarcoma: an open-label phase 1b and randomised phase 2 trial. Lancet. 2016;388:488–497. doi: 10.1016/S0140-6736(16)30587-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 388.Casak SJ, et al. FDA’s approval of the first biosimilar to bevacizumab. Clin. Cancer Res. 2018;24:4365–4370. doi: 10.1158/1078-0432.CCR-18-0566. [DOI] [PubMed] [Google Scholar]
- 389.Rhodes W, et al. Real-world use of bevacizumab-awwb, a bevacizumab biosimilar, in US patients with metastatic colorectal cancer. Future Oncol. 2021;17:5119–5127. doi: 10.2217/fon-2021-0588. [DOI] [PubMed] [Google Scholar]
- 390.Ng EW, et al. Pegaptanib, a targeted anti-VEGF aptamer for ocular vascular disease. Nat. Rev. Drug Discov. 2006;5:123–132. doi: 10.1038/nrd1955. [DOI] [PubMed] [Google Scholar]
- 391.Holash J, et al. VEGF-Trap: a VEGF blocker with potent antitumor effects. Proc. Natl Acad. Sci. USA. 2002;99:11393–11398. doi: 10.1073/pnas.172398299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 392.Mansour AM, Al-Ghadban SI, Yunis MH, El-Sabban ME. Ziv-aflibercept in macular disease. Br. J. Ophthalmol. 2015;99:1055–1059. doi: 10.1136/bjophthalmol-2014-306319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 393.Malik D, et al. Safety profiles of anti-VEGF drugs: bevacizumab, ranibizumab, aflibercept and ziv-aflibercept on human retinal pigment epithelium cells in culture. Br. J. Ophthalmol. 2014;98:i11–i16. doi: 10.1136/bjophthalmol-2014-305302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 394.de Oliveira Dias JR, de Andrade GC, Novais EA, Farah ME, Rodrigues EB. Fusion proteins for treatment of retinal diseases: aflibercept, ziv-aflibercept, and conbercept. Int. J. Retin Vitreous. 2016;2:3. doi: 10.1186/s40942-016-0026-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 395.O’Reilly T, McSheehy PM. Biomarker development for the clinical activity of the mTOR inhibitor everolimus (RAD001): processes, limitations, and further proposals. Transl. Oncol. 2010;3:65–79. doi: 10.1593/tlo.09277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 396.Kawata T, et al. Dual inhibition of the mTORC1 and mTORC2 signaling pathways is a promising therapeutic target for adult T-cell leukemia. Cancer Sci. 2018;109:103–111. doi: 10.1111/cas.13431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 397.Houghton PJ. Everolimus. Clin. Cancer Res. 2010;16:1368–1372. doi: 10.1158/1078-0432.CCR-09-1314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 398.Vargesson N. Thalidomide‐induced teratogenesis: history and mechanisms. Birth Defects Res. C: Embryo Today. 2015;105:140–156. doi: 10.1002/bdrc.21096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 399.Melchert M, List A. The thalidomide saga. Int. J. Biochem. Cell Biol. 2007;39:1489–1499. doi: 10.1016/j.biocel.2007.01.022. [DOI] [PubMed] [Google Scholar]
- 400.Bauer KS, Dixon SC, Figg WD. Inhibition of angiogenesis by thalidomide requires metabolic activation, which is species-dependent. Biochem. Pharmacol. 1998;55:1827–1834. doi: 10.1016/S0006-2952(98)00046-X. [DOI] [PubMed] [Google Scholar]
- 401.Rajkumar SV, Blood E, Vesole D, Fonseca R, Greipp PR. Phase III clinical trial of thalidomide plus dexamethasone compared with dexamethasone alone in newly diagnosed multiple myeloma: a clinical trial coordinated by the Eastern Cooperative Oncology Group. J. Clin. Oncol. 2006;24:431–436. doi: 10.1200/JCO.2005.03.0221. [DOI] [PubMed] [Google Scholar]
- 402.Sun X, et al. Synergistic inhibition of thalidomide and icotinib on human non-small cell lung carcinomas through ERK and AKT signaling. Med. Sci. Monit. 2018;24:3193–3203. doi: 10.12659/MSM.909977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 403.Krönke J, Hurst SN, Ebert BL. Lenalidomide induces degradation of IKZF1 and IKZF3. OncoImmunology. 2014;3:e941742. doi: 10.4161/21624011.2014.941742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 404.Kotla V, et al. Mechanism of action of lenalidomide in hematological malignancies. J. Hematol. Oncol. 2009;2:36. doi: 10.1186/1756-8722-2-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 405.Witzig TE, et al. Long-term analysis of phase II studies of single-agent lenalidomide in relapsed/refractory mantle cell lymphoma. Am. J. Hematol. 2017;92:E575–E583. doi: 10.1002/ajh.24854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 406.Smith RA, et al. Discovery of heterocyclic ureas as a new class of raf kinase inhibitors: identification of a second generation lead by a combinatorial chemistry approach. Bioorg. Med. Chem. Lett. 2001;11:2775–2778. doi: 10.1016/S0960-894X(01)00571-6. [DOI] [PubMed] [Google Scholar]
- 407.Lowinger TB, Riedl B, Dumas J, Smith RA. Design and discovery of small molecules targeting raf-1 kinase. Curr. Pharm. Des. 2002;8:2269–2278. doi: 10.2174/1381612023393125. [DOI] [PubMed] [Google Scholar]
- 408.Wilhelm SM, et al. BAY 43-9006 exhibits broad spectrum oral antitumor activity and targets the RAF/MEK/ERK pathway and receptor tyrosine kinases involved in tumor progression and angiogenesis. Cancer Res. 2004;64:7099–7109. doi: 10.1158/0008-5472.CAN-04-1443. [DOI] [PubMed] [Google Scholar]
- 409.Kamal MA, Mandour YM, Abd El-Aziz MK, Stein U, El Tayebi HM. Small molecule inhibitors for hepatocellular carcinoma: advances and challenges. Molecules. 2022;27:5537. doi: 10.3390/molecules27175537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 410.Escudier B, et al. Sorafenib in advanced clear-cell renal-cell carcinoma. N. Engl. J. Med. 2007;356:125–134. doi: 10.1056/NEJMoa060655. [DOI] [PubMed] [Google Scholar]
- 411.Raymond E, et al. Sunitinib malate for the treatment of pancreatic neuroendocrine tumors. N. Engl. J. Med. 2011;364:501–513. doi: 10.1056/NEJMoa1003825. [DOI] [PubMed] [Google Scholar]
- 412.Ravaud A, et al. Adjuvant sunitinib in high-risk renal-cell carcinoma after nephrectomy. N. Engl. J. Med. 2016;375:2246–2254. doi: 10.1056/NEJMoa1611406. [DOI] [PubMed] [Google Scholar]
- 413.Schutz FA, Choueiri TK, Sternberg CN. Pazopanib: clinical development of a potent anti-angiogenic drug. Crit. Rev. Oncol. Hematol. 2011;77:163–171. doi: 10.1016/j.critrevonc.2010.02.012. [DOI] [PubMed] [Google Scholar]
- 414.Miyamoto S, et al. Drug review: pazopanib. Jpn. J. Clin. Oncol. 2018;48:503–513. doi: 10.1093/jjco/hyy053. [DOI] [PubMed] [Google Scholar]
- 415.Sternberg CN, et al. Pazopanib in locally advanced or metastatic renal cell carcinoma: results of a randomized phase III trial. J. Clin. Oncol. 2010;28:1061–1068. doi: 10.1200/JCO.2009.23.9764. [DOI] [PubMed] [Google Scholar]
- 416.O’Brien ME, et al. Maintenance pazopanib versus placebo in non-small cell lung cancer patients non-progressive after first line chemotherapy: a double blind randomised phase III study of the lung cancer group, EORTC 08092 (EudraCT: 2010-018566-23, NCT01208064) Eur. J. Cancer. 2015;51:1511–1528. doi: 10.1016/j.ejca.2015.04.026. [DOI] [PubMed] [Google Scholar]
- 417.Frampton JE. Vandetanib: in medullary thyroid cancer. Drugs. 2012;72:1423–1436. doi: 10.2165/11209300-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 418.Commander H, Whiteside G, Perry C. Vandetanib: first global approval. Drugs. 2011;71:1355–1365. doi: 10.2165/11595310-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 419.de Boer RH, et al. Vandetanib plus pemetrexed for the second-line treatment of advanced non-small-cell lung cancer: a randomized, double-blind phase III trial. J. Clin. Oncol. 2011;29:1067–1074. doi: 10.1200/JCO.2010.29.5717. [DOI] [PubMed] [Google Scholar]
- 420.Natale RB, et al. Phase III trial of vandetanib compared with erlotinib in patients with previously treated advanced non-small-cell lung cancer. J. Clin. Oncol. 2011;29:1059–1066. doi: 10.1200/JCO.2010.28.5981. [DOI] [PubMed] [Google Scholar]
- 421.Lee JS, et al. Vandetanib versus placebo in patients with advanced non-small-cell lung cancer after prior therapy with an epidermal growth factor receptor tyrosine kinase inhibitor: a randomized, double-blind phase III trial (ZEPHYR) J. Clin. Oncol. 2012;30:1114–1121. doi: 10.1200/JCO.2011.36.1709. [DOI] [PubMed] [Google Scholar]
- 422.Wells SA, et al. Vandetanib in patients with locally advanced or metastatic medullary thyroid cancer: a randomized, double-blind phase III trial. J. Clin. Oncol. 2012;30:134–141. doi: 10.1200/JCO.2011.35.5040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 423.Strumberg D, Schultheis B. Regorafenib for cancer. Expert Opin. Investig. Drugs. 2012;21:879–889. doi: 10.1517/13543784.2012.684752. [DOI] [PubMed] [Google Scholar]
- 424.Ettrich TJ, Seufferlein T. Regorafenib. Recent Results Cancer Res. 2018;211:45–56. doi: 10.1007/978-3-319-91442-8_3. [DOI] [PubMed] [Google Scholar]
- 425.Wilhelm SM, et al. Regorafenib (BAY 73-4506): A new oral multikinase inhibitor of angiogenic, stromal and oncogenic receptor tyrosine kinases with potent preclinical antitumor activity. Int. J. Cancer. 2011;129:245–255. doi: 10.1002/ijc.25864. [DOI] [PubMed] [Google Scholar]
- 426.Grothey A, et al. Regorafenib monotherapy for previously treated metastatic colorectal cancer (CORRECT): an international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet. 2013;381:303–312. doi: 10.1016/S0140-6736(12)61900-X. [DOI] [PubMed] [Google Scholar]
- 427.Bruix J, et al. Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2017;389:56–66. doi: 10.1016/S0140-6736(16)32453-9. [DOI] [PubMed] [Google Scholar]
- 428.Ou DL, et al. Regorafenib enhances antitumor immunity via inhibition of p38 kinase/Creb1/Klf4 axis in tumor-associated macrophages. J. Immunother. Cancer. 2021;9:e001657. doi: 10.1136/jitc-2020-001657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 429.You WK, et al. VEGF and c-Met blockade amplify angiogenesis inhibition in pancreatic islet cancer. Cancer Res. 2011;71:4758–4768. doi: 10.1158/0008-5472.CAN-10-2527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 430.Yakes FM, et al. Cabozantinib (XL184), a novel MET and VEGFR2 inhibitor, simultaneously suppresses metastasis, angiogenesis, and tumor growth. Mol. Cancer Ther. 2011;10:2298–2308. doi: 10.1158/1535-7163.MCT-11-0264. [DOI] [PubMed] [Google Scholar]
- 431.Abou-Alfa GK, et al. Cabozantinib in patients with advanced and progressing hepatocellular carcinoma. N. Engl. J. Med. 2018;379:54–63. doi: 10.1056/NEJMoa1717002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 432.Choueiri TK, et al. Cabozantinib versus everolimus in advanced renal-cell carcinoma. N. Engl. J. Med. 2015;373:1814–1823. doi: 10.1056/NEJMoa1510016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 433.Choueiri TK, et al. Nivolumab plus cabozantinib versus sunitinib for advanced renal-cell carcinoma. N. Engl. J. Med. 2021;384:829–841. doi: 10.1056/NEJMoa2026982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 434.Suyama K, Iwase H. Lenvatinib: a promising molecular targeted agent for multiple cancers. Cancer Control. 2018;25:107327481878936. doi: 10.1177/1073274818789361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 435.Kudo M, et al. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomised phase 3 non-inferiority trial. Lancet. 2018;391:1163–1173. doi: 10.1016/S0140-6736(18)30207-1. [DOI] [PubMed] [Google Scholar]
- 436.Motzer RJ, et al. Lenvatinib, everolimus, and the combination in patients with metastatic renal cell carcinoma: a randomised, phase 2, open-label, multicentre trial. Lancet Oncol. 2015;16:1473–1482. doi: 10.1016/S1470-2045(15)00290-9. [DOI] [PubMed] [Google Scholar]
- 437.Matsuki M, et al. Targeting of tumor growth and angiogenesis underlies the enhanced antitumor activity of lenvatinib in combination with everolimus. Cancer Sci. 2017;108:763–771. doi: 10.1111/cas.13169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 438.Motzer R, et al. Lenvatinib plus pembrolizumab or everolimus for advanced renal cell carcinoma. N. Engl. J. Med. 2021;384:1289–1300. doi: 10.1056/NEJMoa2035716. [DOI] [PubMed] [Google Scholar]
- 439.Rizzo A, et al. Lenvatinib plus pembrolizumab: the next frontier for the treatment of hepatocellular carcinoma? Expert Opin. Investig. Drug. 2022;31:371–378. doi: 10.1080/13543784.2021.1948532. [DOI] [PubMed] [Google Scholar]
- 440.Hu-Lowe DD, et al. Nonclinical antiangiogenesis and antitumor activities of axitinib (AG-013736), an oral, potent, and selective inhibitor of vascular endothelial growth factor receptor tyrosine kinases 1, 2, 3. Clin. Cancer Res. 2008;14:7272–7283. doi: 10.1158/1078-0432.CCR-08-0652. [DOI] [PubMed] [Google Scholar]
- 441.Huang, W. S. et al. Discovery of 3-[2-(imidazo[1,2- b]pyridazin-3-yl)ethynyl]-4-methyl- N -{4-[(4-methylpiperazin-1-yl)methyl]-3-(trifluoromethyl)phenyl}benzamide (AP24534), a potent, orally active pan-inhibitor of breakpoint cluster region-abelson (BCR-ABL) kinase including the T315I gatekeeper mutant. J. Med. Chem.53, 4701–4719 (2010) . [DOI] [PubMed]
- 442.Miller GD, Bruno BJ, Lim CS. Resistant mutations in CML and Ph+ALL—role of ponatinib. Biologics. 2014;8:243–254. doi: 10.2147/BTT.S50734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 443.O’Hare T, et al. AP24534, a pan-BCR-ABL inhibitor for chronic myeloid leukemia, potently inhibits the T315I mutant and overcomes mutation-based resistance. Cancer Cell. 2009;16:401–412. doi: 10.1016/j.ccr.2009.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 444.Gozgit JM, et al. Ponatinib (AP24534), a multitargeted pan-FGFR inhibitor with activity in multiple FGFR-amplified or mutated cancer models. Mol. Cancer Ther. 2012;11:690–699. doi: 10.1158/1535-7163.MCT-11-0450. [DOI] [PubMed] [Google Scholar]
- 445.Gainor JF, Chabner BA. Ponatinib: accelerated disapproval. Oncologist. 2015;20:847–848. doi: 10.1634/theoncologist.2015-0253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 446.Zhang H. Apatinib for molecular targeted therapy in tumor. Drug Des. Dev. Ther. 2015;9:6075–6081. doi: 10.2147/DDDT.S97235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 447.Scott LJ. Apatinib: a review in advanced gastric cancer and other advanced cancers. Drugs. 2018;78:747–758. doi: 10.1007/s40265-018-0903-9. [DOI] [PubMed] [Google Scholar]
- 448.Roviello G, et al. Apatinib: a novel receptor tyrosine kinase inhibitor for the treatment of gastric cancer. Cancer Lett. 2016;372:187–191. doi: 10.1016/j.canlet.2016.01.014. [DOI] [PubMed] [Google Scholar]
- 449.Roth GJ, et al. Design, synthesis, and evaluation of indolinones as triple angiokinase inhibitors and the discovery of a highly specific 6-methoxycarbonyl-substituted indolinone (BIBF 1120) J. Med. Chem. 2009;52:4466–4480. doi: 10.1021/jm900431g. [DOI] [PubMed] [Google Scholar]
- 450.Hilberg F, et al. BIBF 1120: triple angiokinase inhibitor with sustained receptor blockade and good antitumor efficacy. Cancer Res. 2008;68:4774–4782. doi: 10.1158/0008-5472.CAN-07-6307. [DOI] [PubMed] [Google Scholar]
- 451.Catenacci DV, et al. Bemarituzumab with modified FOLFOX6 for advanced FGFR2-positive gastroesophageal cancer: FIGHT phase III study design. Future Oncol. 2019;15:2073–2082. doi: 10.2217/fon-2019-0141. [DOI] [PubMed] [Google Scholar]
- 452.Xiang H, et al. Population pharmacokinetic analysis of phase 1 bemarituzumab data to support phase 2 gastroesophageal adenocarcinoma FIGHT trial. Cancer Chemother. Pharmacol. 2020;86:595–606. doi: 10.1007/s00280-020-04139-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 453.Catenacci DVT, et al. Phase I escalation and expansion study of bemarituzumab (FPA144) in patients with advanced solid tumors and FGFR2b-selected gastroesophageal adenocarcinoma. J. Clin. Oncol. 2020;38:2418–2426. doi: 10.1200/JCO.19.01834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 454.Wainberg ZA, et al. Bemarituzumab in patients with FGFR2b-selected gastric or gastro-oesophageal junction adenocarcinoma (FIGHT): a randomised, double-blind, placebo-controlled, phase 2 study. Lancet Oncol. 2022;23:1430–1440. doi: 10.1016/S1470-2045(22)00603-9. [DOI] [PubMed] [Google Scholar]
- 455.Dhillon S. Avapritinib: first approval. Drugs. 2020;80:433–439. doi: 10.1007/s40265-020-01275-2. [DOI] [PubMed] [Google Scholar]
- 456.Gebreyohannes YK, et al. Robust activity of avapritinib, potent and highly selective inhibitor of mutated KIT, in patient-derived xenograft models of gastrointestinal stromal tumors. Clin. Cancer Res. 2019;25:609–618. doi: 10.1158/1078-0432.CCR-18-1858. [DOI] [PubMed] [Google Scholar]
- 457.Joseph CP, et al. Optimal avapritinib treatment strategies for patients with metastatic or unresectable gastrointestinal stromal tumors. Oncologist. 2021;26:e622–e631. doi: 10.1002/onco.13632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 458.Jones RL, et al. Avapritinib in unresectable or metastatic PDGFRA D842V-mutant gastrointestinal stromal tumours: Long-term efficacy and safety data from the NAVIGATOR phase I trial. Eur. J. Cancer. 2021;145:132–142. doi: 10.1016/j.ejca.2020.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 459.Heinrich MC, et al. Avapritinib in advanced PDGFRA D842V-mutant gastrointestinal stromal tumour (NAVIGATOR): a multicentre, open-label, phase 1 trial. Lancet Oncol. 2020;21:935–946. doi: 10.1016/S1470-2045(20)30269-2. [DOI] [PubMed] [Google Scholar]
- 460.Kang Y-K, et al. Avapritinib versus regorafenib in locally advanced unresectable or metastatic GI stromal tumor: a randomized, open-label phase III study. J. Clin. Oncol. 2021;39:3128–3139. doi: 10.1200/JCO.21.00217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 461.Markham A. Erdafitinib: first global approval. Drugs. 2019;79:1017–1021. doi: 10.1007/s40265-019-01142-9. [DOI] [PubMed] [Google Scholar]
- 462.Perera TPS, et al. Discovery and pharmacological characterization of JNJ-42756493 (Erdafitinib), a functionally selective small-molecule FGFR family inhibitor. Mol. Cancer Ther. 2017;16:1010–1020. doi: 10.1158/1535-7163.MCT-16-0589. [DOI] [PubMed] [Google Scholar]
- 463.Montazeri K, Bellmunt J. Erdafitinib for the treatment of metastatic bladder cancer. Expert Rev. Clin. Pharmacol. 2020;13:1–6. doi: 10.1080/17512433.2020.1702025. [DOI] [PubMed] [Google Scholar]
- 464.Roubal K, Myint ZW, Kolesar JM. Erdafitinib: a novel therapy for FGFR-mutated urothelial cancer. Am. J. Health Syst. Pharm. 2020;77:346–351. doi: 10.1093/ajhp/zxz329. [DOI] [PubMed] [Google Scholar]
- 465.Babina IS, Turner NC. Advances and challenges in targeting FGFR signalling in cancer. Nat. Rev. Cancer. 2017;17:318–332. doi: 10.1038/nrc.2017.8. [DOI] [PubMed] [Google Scholar]
- 466.Bhat AA, et al. Tumor microenvironment: an evil nexus promoting aggressive head and neck squamous cell carcinoma and avenue for targeted therapy. Signal Transduct. Target. Ther. 2021;6:12. doi: 10.1038/s41392-020-00419-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 467.Tang T, et al. Advantages of targeting the tumor immune microenvironment over blocking immune checkpoint in cancer immunotherapy. Signal Transduct. Target. Ther. 2021;6:72. doi: 10.1038/s41392-020-00449-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 468.Tao J, et al. Targeting hypoxic tumor microenvironment in pancreatic cancer. J. Hematol. Oncol. 2021;14:14. doi: 10.1186/s13045-020-01030-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 469.Wang B, et al. Targeting hypoxia in the tumor microenvironment: a potential strategy to improve cancer immunotherapy. J. Exp. Clin. Cancer Res. 2021;40:24. doi: 10.1186/s13046-020-01820-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 470.Li Y, Zhao L, Li XF. Hypoxia and the tumor microenvironment. Technol. Cancer Res. Treat. 2021;20:153303382110363. doi: 10.1177/15330338211036304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 471.AbdelHaleem A, Mansour AO, AbdelKader M, Arafa RK. Selective VEGFR-2 inhibitors: synthesis of pyridine derivatives, cytotoxicity and apoptosis induction profiling. Bioorg. Chem. 2020;103:104222. doi: 10.1016/j.bioorg.2020.104222. [DOI] [PubMed] [Google Scholar]
- 472.Alanazi MM, et al. Discovery of new 3-methylquinoxalines as potential anti-cancer agents and apoptosis inducers targeting VEGFR-2: design, synthesis, and in silico studies. J. Enzym. Inhib. Med. Chem. 2021;36:1732–1750. doi: 10.1080/14756366.2021.1945591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 473.Alanazi MM, et al. Design, synthesis, docking, ADMET studies, and anticancer evaluation of new 3-methylquinoxaline derivatives as VEGFR-2 inhibitors and apoptosis inducers. J. Enzym. Inhib. Med. Chem. 2021;36:1760–1782. doi: 10.1080/14756366.2021.1956488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 474.Alanazi, M. M. et al. New bis([1,2,4]triazolo)[4,3-a:3’,4’-c]quinoxaline derivatives as VEGFR-2 inhibitors and apoptosis inducers: design, synthesis, in silico studies, and anticancer evaluation. Bioorg. Chem.112, 104949 (2021). [DOI] [PubMed]
- 475.Zeidan MA, et al. Design, synthesis and docking study of novel picolinamide derivatives as anticancer agents and VEGFR-2 inhibitors. Eur. J. Med. Chem. 2019;168:315–329. doi: 10.1016/j.ejmech.2019.02.050. [DOI] [PubMed] [Google Scholar]
- 476.Jiang Z, et al. Discovery of a highly selective VEGFR2 kinase inhibitor CHMFL-VEGFR2-002 as a novel anti-angiogenesis agent. Acta Pharm. Sin. B. 2020;10:488–497. doi: 10.1016/j.apsb.2019.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 477.El‐Adl K, Sakr H, Nasser M, Alswah M, Shoman FMA. 5‐(4‐Methoxybenzylidene)thiazolidine‐2,4‐dione‐derived VEGFR‐2 inhibitors: design, synthesis, molecular docking, and anticancer evaluations. Arch. Pharm. 2020;353:e2000079. doi: 10.1002/ardp.202000079. [DOI] [PubMed] [Google Scholar]
- 478.El‐Adl K, El‐Helby AA, Sakr H, El‐Hddad SSA. Design, synthesis, molecular docking, and anticancer evaluations of 1‐benzylquinazoline‐2,4(1 H, 3 H)‐dione bearing different moieties as VEGFR‐2 inhibitors. Arch. Pharm. 2020;353:e2000068. doi: 10.1002/ardp.202000068. [DOI] [PubMed] [Google Scholar]
- 479.Sun W, Hu S, Fang S, Yan H. Design, synthesis and biological evaluation of pyrimidine-based derivatives as VEGFR-2 tyrosine kinase inhibitors. Bioorg. Chem. 2018;78:393–405. doi: 10.1016/j.bioorg.2018.04.005. [DOI] [PubMed] [Google Scholar]
- 480.El-Adl K, et al. Design, synthesis, and anti-proliferative evaluation of new quinazolin-4(3H)-ones as potential VEGFR-2 inhibitors. Bioorg. Med. Chem. 2020;29:115872. doi: 10.1016/j.bmc.2020.115872. [DOI] [PubMed] [Google Scholar]
- 481.Dhokne P, Sakla AP, Shankaraiah N. Structural insights of oxindole based kinase inhibitors as anticancer agents: Recent advances. Eur. J. Med. Chem. 2021;216:113334. doi: 10.1016/j.ejmech.2021.113334. [DOI] [PubMed] [Google Scholar]
- 482.Yao Y, et al. Design, synthesis and pharmacological evaluation of 4-(3-chloro-4-(3-cyclopropylthioureido)-2-fluorophenoxy)-7-methoxyquinoline-6-carboxamide (WXFL-152): a novel triple angiokinase inhibitor for cancer therapy. Acta Pharm. Sin. B. 2020;10:1453–1475. doi: 10.1016/j.apsb.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 483.Mohamady S, et al. Dual targeting of VEGFR2 and c-Met kinases via the design and synthesis of substituted 3-(Triazolo-thiadiazin-3-yl)indolin-2-one derivatives as angiogenesis inhibitors. ACS Omega. 2020;5:18872–18886. doi: 10.1021/acsomega.0c02038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 484.Zhang L, et al. Discovery of novel anti-angiogenesis agents. Part 6: multi-targeted RTK inhibitors. Eur. J. Med. Chem. 2017;127:275–285. doi: 10.1016/j.ejmech.2016.12.059. [DOI] [PubMed] [Google Scholar]
- 485.Sun Y, et al. Discovery of novel anti-angiogenesis agents. Part 8: diaryl thiourea bearing 1H-indazole-3-amine as multi-target RTKs inhibitors. Eur. J. Med. Chem. 2017;141:373–385. doi: 10.1016/j.ejmech.2017.10.008. [DOI] [PubMed] [Google Scholar]
- 486.Pan X, et al. Discovery of novel anti-angiogenesis agents. Part 10: multi-target inhibitors of VEGFR-2, Tie-2 and EphB4 incorporated with 1,2,3-triazol. Eur. J. Med. Chem. 2019;163:1–9. doi: 10.1016/j.ejmech.2018.11.042. [DOI] [PubMed] [Google Scholar]
- 487.Li C, et al. Discovery of novel anti-angiogenesis agents. Part 7: multitarget inhibitors of VEGFR-2, TIE-2 and EphB4. Eur. J. Med. Chem. 2017;141:506–518. doi: 10.1016/j.ejmech.2017.10.030. [DOI] [PubMed] [Google Scholar]
- 488.Upadhyay N, et al. Double-edged swords: diaryl pyrazoline thiazolidinediones synchronously targeting cancer epigenetics and angiogenesis. Bioorg. Chem. 2021;116:105350. doi: 10.1016/j.bioorg.2021.105350. [DOI] [PubMed] [Google Scholar]
- 489.Xiaomeng Zhang, et al. Discovery of 1,6-naphthyridin-2(1H)-one derivatives as novel, potent, and selective FGFR4 inhibitors for the treatment of hepatocellular carcinoma. J. Med. Chem. 2022;65:7595–7618. doi: 10.1021/acs.jmedchem.1c01977. [DOI] [PubMed] [Google Scholar]
- 490.Wei M, et al. Design, synthesis and biological evaluation of a series of novel 2-benzamide-4-(6-oxy-N-methyl-1-naphthamide)-pyridine derivatives as potent fibroblast growth factor receptor (FGFR) inhibitors. Eur. J. Med. Chem. 2018;154:9–28. doi: 10.1016/j.ejmech.2018.05.005. [DOI] [PubMed] [Google Scholar]
- 491.Brameld, K. A. et al. Discovery of the irreversible covalent FGFR inhibitor 8-(3-(4-acryloylpiperazin-1-yl)propyl)-6-(2,6-dichloro-3,5-dimethoxyphenyl)-2-(methylamino)pyrido[2,3- d]pyrimidin-7(8 H)-one (PRN1371) for the treatment of solid tumors. J. Med. Chem.60, 6516–6527 (2017). [DOI] [PubMed]
- 492.An H, et al. Novel hypoxia-inducible factor 1α (HIF-1α) inhibitors for angiogenesis-related ocular diseases: discovery of a novel scaffold via ring-truncation strategy. J. Med. Chem. 2018;61:9266–9286. doi: 10.1021/acs.jmedchem.8b00971. [DOI] [PubMed] [Google Scholar]
- 493.Liu M, et al. Discovery of novel aryl carboxamide derivatives as hypoxia-inducible factor 1α signaling inhibitors with potent activities of anticancer metastasis. J. Med. Chem. 2019;62:9299–9314. doi: 10.1021/acs.jmedchem.9b01313. [DOI] [PubMed] [Google Scholar]
- 494.Lee S, et al. Synthesis and biological evaluation of kresoxim-methyl analogues as novel inhibitors of hypoxia-inducible factor (HIF)-1 accumulation in cancer cells. Bioorg. Med. Chem. Lett. 2017;27:3026–3029. doi: 10.1016/j.bmcl.2017.05.024. [DOI] [PubMed] [Google Scholar]
- 495.Jiang YF, Yang ZH, Hu JQ. Recurrence or metastasis of HCC: predictors, early detection and experimental antiangiogenic therapy. World J. Gastroenterol. 2000;6:61–65. doi: 10.3748/wjg.v6.i1.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 496.Shojaei F. Anti-angiogenesis therapy in cancer: current challenges and future perspectives. Cancer Lett. 2012;320:130–137. doi: 10.1016/j.canlet.2012.03.008. [DOI] [PubMed] [Google Scholar]
- 497.Haibe Y, et al. Resistance mechanisms to anti-angiogenic therapies in cancer. Front. Oncol. 2020;10:221. doi: 10.3389/fonc.2020.00221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 498.Al-Husein B, Abdalla M, Trepte M, DeRemer DL, Somanath PR. Antiangiogenic therapy for cancer: an update. Pharmacotherapy. 2012;32:1095–1111. doi: 10.1002/phar.1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 499.Chen HX, Cleck JN. Adverse effects of anticancer agents that target the VEGF pathway. Nat. Rev. Clin. Oncol. 2009;6:465–477. doi: 10.1038/nrclinonc.2009.94. [DOI] [PubMed] [Google Scholar]
- 500.Lugano R, Ramachandran M, Dimberg A. Tumor angiogenesis: causes, consequences, challenges and opportunities. Cell. Mol. Life Sci. 2020;77:1745–1770. doi: 10.1007/s00018-019-03351-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 501.Ebos JM, et al. Accelerated metastasis after short-term treatment with a potent inhibitor of tumor angiogenesis. Cancer Cell. 2009;15:232–239. doi: 10.1016/j.ccr.2009.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 502.Griffioen AW, et al. Rapid angiogenesis onset after discontinuation of sunitinib treatment of renal cell carcinoma patients. Clin. Cancer Res. 2012;18:3961–3971. doi: 10.1158/1078-0432.CCR-12-0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 503.Wang X, Zhang H, Chen X. Drug resistance and combating drug resistance in cancer. Cancer Drug Resist. 2019;2:141–160. doi: 10.20517/cdr.2019.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 504.Ricci V, Ronzoni M, Fabozzi T. Aflibercept a new target therapy in cancer treatment: a review. Crit. Rev. Oncol. Hematol. 2015;96:569–576. doi: 10.1016/j.critrevonc.2015.07.001. [DOI] [PubMed] [Google Scholar]
- 505.Rey S, Schito L, Wouters BG, Eliasof S, Kerbel RS. Targeting hypoxia-inducible factors for antiangiogenic cancer therapy. Trends Cancer. 2017;3:529–541. doi: 10.1016/j.trecan.2017.05.002. [DOI] [PubMed] [Google Scholar]
- 506.Asahara T, et al. Isolation of putative progenitor endothelial cells for angiogenesis. Science. 1997;275:964–967. doi: 10.1126/science.275.5302.964. [DOI] [PubMed] [Google Scholar]
- 507.Song S, Ewald AJ, Stallcup W, Werb Z, Bergers G. PDGFRβ+ perivascular progenitor cells in tumours regulate pericyte differentiation and vascular survival. Nat. Cell Biol. 2005;7:870–879. doi: 10.1038/ncb1288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 508.Dalton HJ, et al. Macrophages facilitate resistance to Anti-VEGF therapy by altered VEGFR expression. Clin. Cancer Res. 2017;23:7034–7046. doi: 10.1158/1078-0432.CCR-17-0647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 509.Greenberg JI, et al. A role for VEGF as a negative regulator of pericyte function and vessel maturation. Nature. 2008;456:809–813. doi: 10.1038/nature07424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 510.Bridgeman VL, et al. Vessel co-option is common in human lung metastases and mediates resistance to anti-angiogenic therapy in preclinical lung metastasis models. J. Pathol. 2017;241:362–374. doi: 10.1002/path.4845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 511.Frentzas S, et al. Vessel co-option mediates resistance to anti-angiogenic therapy in liver metastases. Nat. Med. 2016;22:1294–1302. doi: 10.1038/nm.4197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 512.Kuczynski EA, Reynolds AR. Vessel co-option and resistance to anti-angiogenic therapy. Angiogenesis. 2020;23:55–74. doi: 10.1007/s10456-019-09698-6. [DOI] [PubMed] [Google Scholar]
- 513.Rada M, Lazaris A, Kapelanski-Lamoureux A, Mayer TZ, Metrakos P. Tumor microenvironment conditions that favor vessel co-option in colorectal cancer liver metastases: a theoretical model. Semin. Cancer Biol. 2020;71:52–64. doi: 10.1016/j.semcancer.2020.09.001. [DOI] [PubMed] [Google Scholar]
- 514.Ribatti D, Djonov V. Intussusceptive microvascular growth in tumors. Cancer Lett. 2012;316:126–131. doi: 10.1016/j.canlet.2011.10.040. [DOI] [PubMed] [Google Scholar]
- 515.Delgado-Bellido D, Serrano-Saenz S, Fernández-Cortés M, Oliver FJ. Vasculogenic mimicry signaling revisited: focus on non-vascular VE-cadherin. Mol. Cancer. 2017;16:65. doi: 10.1186/s12943-017-0631-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 516.Guerrouahen BS, et al. Akt-activated endothelium constitutes the niche for residual disease and resistance to bevacizumab in ovarian cancer. Mol. Cancer Ther. 2014;13:3123–3136. doi: 10.1158/1535-7163.MCT-13-1053. [DOI] [PubMed] [Google Scholar]
- 517.Eyler CE, Rich JN. Survival of the fittest: cancer stem cells in therapeutic resistance and angiogenesis. J. Clin. Oncol. 2008;26:2839–2845. doi: 10.1200/JCO.2007.15.1829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 518.McMillin DW, Negri JM, Mitsiades CS. The role of tumour–stromal interactions in modifying drug response: challenges and opportunities. Nat. Rev. Drug Discov. 2013;12:217–228. doi: 10.1038/nrd3870. [DOI] [PubMed] [Google Scholar]
- 519.Jain RK, et al. Biomarkers of response and resistance to antiangiogenic therapy. Nat. Rev. Clin. Oncol. 2009;6:327–338. doi: 10.1038/nrclinonc.2009.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 520.Pircher A, et al. Biomarkers in tumor angiogenesis and anti-angiogenic therapy. Int. J. Mol. Sci. 2011;12:7077–7099. doi: 10.3390/ijms12107077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 521.Jayson GC, Hicklin DJ, Ellis LM. Antiangiogenic therapy—evolving view based on clinical trial results. Nat. Rev. Clin. Oncol. 2012;9:297–303. doi: 10.1038/nrclinonc.2012.8. [DOI] [PubMed] [Google Scholar]
- 522.Cao Y, et al. Forty-year journey of angiogenesis translational research. Sci. Transl. Med. 2011;3:144rv3. doi: 10.1126/scitranslmed.3003149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 523.Hurwitz H, et al. Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N. Engl. J. Med. 2004;350:2335–2342. doi: 10.1056/NEJMoa032691. [DOI] [PubMed] [Google Scholar]
- 524.Mokhtari RB, et al. Combination therapy in combating cancer. Oncotarget. 2017;8:38022–38043. doi: 10.18632/oncotarget.16723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 525.Song Y, et al. Anti-angiogenic agents in combination with immune checkpoint Inhibitors: a promising strategy for cancer treatment. Front. Immunol. 2020;11:1956. doi: 10.3389/fimmu.2020.01956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 526.Ciciola P, Cascetta P, Bianco C, Formisano L, Bianco R. Combining immune checkpoint inhibitors with anti-angiogenic agents. J. Clin. Med. 2020;9:675. doi: 10.3390/jcm9030675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 527.Yasuda S, et al. Simultaneous blockade of programmed death 1 and vascular endothelial growth factor receptor 2 (VEGFR2) induces synergistic anti-tumour effect in vivo. Clin. Exp. Immunol. 2013;172:500–506. doi: 10.1111/cei.12069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 528.Majidpoor J, Mortezaee K. The efficacy of PD-1/PD-L1 blockade in cold cancers and future perspectives. Clin. Immunol. 2021;226:108707. doi: 10.1016/j.clim.2021.108707. [DOI] [PubMed] [Google Scholar]
- 529.Yi M, et al. Synergistic effect of immune checkpoint blockade and anti-angiogenesis in cancer treatment. Mol. Cancer. 2019;18:60. doi: 10.1186/s12943-019-0974-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 530.Cheng AL, et al. IMbrave150: Efficacy and safety results from a ph III study evaluating atezolizumab (atezo) + bevacizumab (bev) vs sorafenib (Sor) as first treatment (tx) for patients (pts) with unresectable hepatocellular carcinoma (HCC) Ann. Oncol. 2019;30:ix186–ix187. doi: 10.1093/annonc/mdz446.002. [DOI] [Google Scholar]
- 531.Neves KB, Montezano AC, Lang NN, Touyz RM. Vascular toxicity associated with anti-angiogenic drugs. Clin. Sci. 2020;134:2503–2520. doi: 10.1042/CS20200308. [DOI] [PubMed] [Google Scholar]
- 532.Perdrizet K, Leighl NB. The role of angiogenesis inhibitors in the era of immune checkpoint inhibitors and targeted therapy in metastatic non-small cell lung cancer. Curr. Treat. Options Oncol. 2019;20:21. doi: 10.1007/s11864-019-0617-6. [DOI] [PubMed] [Google Scholar]
- 533.Hilmi M, et al. Angiogenesis and immune checkpoint inhibitors as therapies for hepatocellular carcinoma: current knowledge and future research directions. J. Immunother. Cancer. 2019;7:333. doi: 10.1186/s40425-019-0824-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 534.Anderson TS, Wooster AL, Piersall SL, Okpalanwaka IF, Lowe DB. Disrupting cancer angiogenesis and immune checkpoint networks for improved tumor immunity. Semin. Cancer Biol. 2022;86:981–996. doi: 10.1016/j.semcancer.2022.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 535.Lee WS, Yang H, Chon HJ, Kim C. Combination of anti-angiogenic therapy and immune checkpoint blockade normalizes vascular-immune crosstalk to potentiate cancer immunity. Exp. Mol. Med. 2020;52:1475–1485. doi: 10.1038/s12276-020-00500-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 536.Wang XF, et al. Neoadjuvant chemotherapy: practice and thinking for Chinese patients with early breast cancer. Chin. Med. J. 2020;133:2368–2369. doi: 10.1097/CM9.0000000000000940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 537.Ikeda T, Jinno H, Matsui A, Masamura S, Kitajima M. The role of neoadjuvant chemotherapy for breast cancer treatment. Breast Cancer. 2002;9:8–14. doi: 10.1007/BF02967540. [DOI] [PubMed] [Google Scholar]
- 538.Middleton JD, Stover DG, Hai T. Chemotherapy-exacerbated breast cancer metastasis: a paradox explainable by dysregulated adaptive-response. Int. J. Mol. Sci. 2018;19:3333. doi: 10.3390/ijms19113333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 539.Ortolan E, et al. Blood-based genomics of triple-negative breast cancer progression in patients treated with neoadjuvant chemotherapy. ESMO Open. 2021;6:100086. doi: 10.1016/j.esmoop.2021.100086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 540.Perelmuter VM, et al. Mechanisms behind prometastatic changes induced by neoadjuvant chemotherapy in the breast cancer microenvironment. Breast Cancer. 2019;11:209–219. doi: 10.2147/BCTT.S175161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 541.Xiao L, et al. Anti-vascular endothelial growth factor treatment induces blood flow recovery through vascular remodeling in high-fat diet induced diabetic mice. Microvasc. Res. 2016;105:70–76. doi: 10.1016/j.mvr.2016.01.005. [DOI] [PubMed] [Google Scholar]
- 542.Piperigkou Z, Mohr B, Karamanos N, Götte M. Shed proteoglycans in tumor stroma. Cell Tissue Res. 2016;365:643–655. doi: 10.1007/s00441-016-2452-4. [DOI] [PubMed] [Google Scholar]
- 543.Devisscher L, et al. Targeting the angio-proteostasis network: combining the forces against cancer. Pharmacol. Ther. 2016;167:1–12. doi: 10.1016/j.pharmthera.2016.07.007. [DOI] [PubMed] [Google Scholar]
- 544.Zhao Y, Adjei AA. Targeting angiogenesis in cancer therapy: moving beyond vascular endothelial growth factor. Oncologist. 2015;20:660–673. doi: 10.1634/theoncologist.2014-0465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 545.Broekman F, Giovannetti E, Peters GJ. Tyrosine kinase inhibitors: multi-targeted or single-targeted? World J. Clin. Oncol. 2011;2:80–93. doi: 10.5306/wjco.v2.i2.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 546.Mohajeri A, et al. Cloning and expression of recombinant human endostatin in periplasm of escherichia coli expression system. Adv. Pharm. Bull. 2016;6:187–194. doi: 10.15171/apb.2016.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 547.Rao N, Lee YF, Ge R. Novel endogenous angiogenesis inhibitors and their therapeutic potential. Acta Pharmacol. Sin. 2015;36:1177–1190. doi: 10.1038/aps.2015.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 548.Hanahan D, Folkman J. Patterns and emerging mechanisms of the angiogenic switch during tumorigenesis. Cell. 1996;86:353–364. doi: 10.1016/S0092-8674(00)80108-7. [DOI] [PubMed] [Google Scholar]
- 549.Lawler J. Thrombospondin-1 as an endogenous inhibitor of angiogenesis and tumor growth. J. Cell. Mol. Med. 2002;6:1–12. doi: 10.1111/j.1582-4934.2002.tb00307.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 550.Streit M, et al. Thrombospondin-2: a potent endogenous inhibitor of tumor growth and angiogenesis. Proc. Natl Acad. Sci. USA. 1999;96:14888–14893. doi: 10.1073/pnas.96.26.14888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 551.Watanabe K, et al. Vasohibin as an endothelium-derived negative feedback regulator of angiogenesis. J. Clin. Invest. 2004;114:898–907. doi: 10.1172/JCI200421152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 552.Hiraki Y, et al. Identification of chondromodulin I as a novel endothelial cell growth inhibitor. J. Biol. Chem. 1997;272:32419–32426. doi: 10.1074/jbc.272.51.32419. [DOI] [PubMed] [Google Scholar]
- 553.Bikfalvi A, Gimenez-Gallego G. The control of angiogenesis and tumor invasion by platelet factor-4 and platelet factor-4-derived molecules. Semin. Thromb. Hemost. 2004;30:137–144. doi: 10.1055/s-2004-822978. [DOI] [PubMed] [Google Scholar]
- 554.O’Reilly MS, et al. Angiostatin: a novel angiogenesis inhibitor that mediates the suppression of metastases by a lewis lung carcinoma. Cell. 1994;79:315–328. doi: 10.1016/0092-8674(94)90200-3. [DOI] [PubMed] [Google Scholar]
- 555.Maeshima Y, et al. Distinct antitumor properties of a type IV collagen domain derived from basement membrane. J. Biol. Chem. 2000;275:21340–21348. doi: 10.1074/jbc.M001956200. [DOI] [PubMed] [Google Scholar]