Abstract
Background
Periprosthetic infections are a debilitating complication of alloplastic breast reconstruction. Local antibiotic delivery for prophylaxis and infection clearance has been used by other surgical specialties but rarely in breast reconstruction. Because local delivery can maintain high antibiotic concentrations with lower toxicity risk, it may be valuable for infection prophylaxis or salvage in breast reconstruction.
Methods
A systematic search of the Embase, PubMed, and Cochrane databases was performed in January 2022. Primary literature studies examining local antibiotic delivery systems for either prophylaxis or salvage of periprosthetic infections were included. Study quality and bias were assessed using the validated MINORS criteria.
Results
Of 355 publications reviewed, 8 met the predetermined inclusion criteria; 5 papers investigated local antibiotic delivery for salvage, and 3 investigated infection prophylaxis. Implantable antibiotic delivery devices included polymethylmethacrylate, calcium sulfate, and collagen sponges impregnated with antibiotics. Non-implantable antibiotic delivery methods used irrigation with antibiotic solution into the breast pocket. All studies indicated that local antibiotic delivery was either comparable or superior to conventional methods in both the salvage and prophylaxis settings.
Conclusions
Despite varied sample sizes and methodologies, all papers endorsed local antibiotic delivery as a safe, effective method of preventing or treating periprosthetic infections in breast reconstruction.
Keywords: Implant-Based Breast, Reconstruction, Local Antibiotic Delivery, Infection Prophylaxis, Implant Salvage, Periprosthetic Infection
Introduction
Implant-based methods remain the most commonly performed type of postmastectomy breast reconstruction,1 accounting for approximately 80% of reconstructions.2 While autologous breast reconstruction is often rated higher than alloplastic reconstruction in terms of patient satisfaction,3,6 increased surgical complexity, donor site morbidity, and requirement for microsurgical expertise remain limiting factors for many patients.7 Despite their popularity, tissue expander and implant-based surgeries carry a higher risk of infection compared with that of autologous reconstruction,2 which can lead to additional surgeries, significant patient morbidity, and even loss of the reconstructed breast pocket. The literature discussing infections in implant-based breast reconstructions (IBBRs) report infection rates ranging widely from 1% to 43%,8 highlighting the importance of both effective infection prophylaxis and implant salvage protocols.
In an effort to mitigate this risk, antibiotics are a common tool used to prevent and treat surgical site infections. While there is currently no consensus regarding the prophylactic use of antibiotics,9 their administration has been demonstrated to have some benefit10 and is recommended for clean breast surgeries.11 However, there is a lack of consistent evidence in support of antibiotic prophylaxis for other breast surgeries,12 and adherence to guidelines among breast surgeons is poor.13 Postoperative antibiotic use is another source of debate. Postoperative antibiotics are commonly prescribed following many surgical procedures, and some studies have identified a benefit from their use in prosthetic breast reconstruction.14 However, on aggregate, there is limited evidence illustrating a benefit from postoperative antibiotic use15; in fact, the World Health Organization recommends against this practice.16
Once established, periprosthetic infections can be highly morbid and difficult to treat. Traditional methods for managing infected breast implants have previously included a trial of intravenous (IV) antibiotics, breast pocket washout with removal of the device, and consideration of delayed reconstruction several months later.17,18 Reconstruction following infection and explantation is often abandoned by patients, especially when the primary reason for mastectomy is oncologic rather than prophylactic.19,20 As a result of the morbidity posed by an infection following alloplastic breast reconstruction, many recent studies have investigated new modalities for preventing infection and salvaging infected implants. Local antibiotic delivery systems are of significant interest as they can greatly increase the concentration of antibiotics in the breast pocket without the same risk of complications that result from high systemic doses.
The use of local antibiotic delivery systems has been popularized in other surgical fields, such as orthopedic surgery, but their use within plastic surgery remains scarce. Antibiotic-infused bone cement has been used by orthopedic surgeons since the 1970s for the treatment and prevention of infections following joint arthroplasty.21,22 More recently, the use of antibiotic-eluting devices like nonabsorbable polymethylmethacrylate (PMMA) or absorbable calcium sulfate have begun to appear in soft tissue surgeries, such as vascular surgeries23,26 and hernia repair,27,28 but their use is far from routine. Other proposed methods for local antibiotic delivery to surgical sites include continuous antibiotic infusion via catheterization29 and antibiotic lavage.30,32 Some authors even propose using materials like antibiotic-loaded collagen matrix33,34 or antibiotic-infused surgical meshes35,37 as a means of providing both local antibiotic delivery and soft tissue support; however, few publications have explored their efficacy in reconstructive surgery.
With breast cancer being the most common cancer among women worldwide, even a low incidence of surgical infection has the potential to affect a large number of patients.38 Though novel, the use of local antibiotic delivery methods for infection prophylaxis and implant salvage may potentially offer better infection control than standard methods. Thus, the focus of this systematic review is to identify studies that use local antibiotic delivery as either a method of prophylaxis or salvage for IBBR and provide an evidence-based summary of their results.
Methods
Search strategy
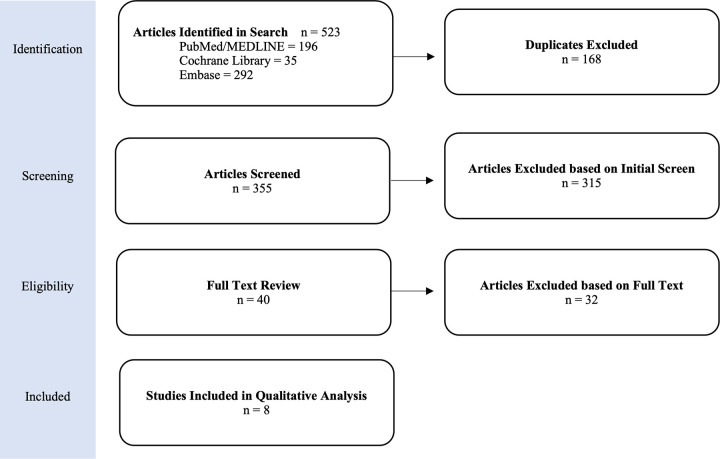
A systematic review was performed using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement guidelines (Figure 1). The search included the following bibliographic databases: PubMed, Cochrane Library, and Embase. The following search terms were used for PubMed and were adapted as necessary for the additional databases to identify all possible papers that may meet this study's inclusion criteria: (breast reconstruction [TW] OR mammaplasty [TW] OR mammoplasty [TW] OR mastoplasty [TW] OR alloplastic breast reconstruction [TW] OR implant-based breast reconstruction [TW] OR breast implant [TW] OR breast implants [TW] OR IBBR [TW] OR periprosthetic infection [TW] OR prosthesis-related infection [TW] OR tissue expander [TW] OR tissue expander infection [TW] OR reconstruction, breast [TW]) AND (antibiotic [TW] OR local antibiotic [TW] OR local antibiotic delivery [TW] OR antibiotic cement [TW] OR antibiotic bone cement [TW] OR antibiotic-eluting [TW] OR antibiotic PMMA [TW] OR antibiotic plate [TW] OR antibiotic polymethylmethacrylate [TW] OR PMMA [TW] OR antibiotic bead [TW] OR STIMULAN [TW] OR antibiotic lavage [TW]) AND (antibiotic prophylaxis [TW] OR prophylaxis, antibiotic [TW] OR antibiotic premedication [TW] OR salvage [TW] OR implant salvage [TW] OR infection clearance [TW]).
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram. Diagram illustrates the process of identifying, evaluating, and excluding or including publications identified in the literature according to the PRISMA guidelines. This flow chart describes the number of initial publications identified from each database and how many were excluded at each screening step until only articles meeting inclusion criteria remained (8 publications total).
Inclusion and exclusion criteria
Criteria for eligibility and exclusion were decided before the review was performed. Patients undergoing IBBR following either oncologic or prophylactic mastectomy were included. Only studies that examined local delivery of antibiotics to the breast pocket were included. Papers involving both prophylactic local antibiotic delivery in immediate reconstruction and local antibiotic delivery for implant salvage were included in this review; surgical procedures at either the tissue expander or implant stage were eligible. Studies investigating the use of systemic antibiotics, application or topical antibiotics, or use of antibiotic wound dressings were excluded, but no exclusions were made based on the type of device used for local antibiotic delivery. Papers based solely on animal or in vitro models were excluded, as were papers published in a language other than English. Bibliographies of all included articles were screened to identify additional articles not obtained in the preliminary search. Two independent reviewers repeated the review process.
Table 1.
Profile of Included Studies
| Study | Title | PMID | Study Type | Sample Size | Intervention | Important Findings |
|---|---|---|---|---|---|---|
| Xue et al, 2020 | Follow-Up Study: One-Step Salvage of Infected Prosthetic Breast Reconstructions Using Antibiotic-Impregnated Polymethylmethacrylate Plates and Concurrent Tissue Expander Exchange | 31985610 | Retrospective cohort study | 58 patients, 62 breasts | Salvage, antibiotic-loaded PMMA plate | The rate of infection clearance was similar between the intervention and explantation groups (82.2% vs 92.1%, p = 0.42). Compared with the conventional group, significantly fewer salvage patients abandoned reconstruction after infection clearance (2.2% vs 58.8%; P < .001) and more completed final reconstruction (84.4% vs 35.3%; P < .001). The mean number of operations performed was higher in the salvage group compared with explantation (2.9 vs 2.5; P = .002). |
| Kim et al, 2020 | Minimally Invasive Salvage of Infected Breast Tissue Expanders: A Continuous Closed Irrigation Technique Based on Surface Biofilm Disruption. | 31515192 | Retrospective case-control | 21 breasts | Salvage, continuous antibiotic irrigation (11 days) | Both the expander irrigation group and explantation group had 100% infection clearance. There was a tendency for more patients to complete their reconstruction in the irrigation group compared with the explantation group (80% vs 31%; P = .1). The mean cost of treatment in the irrigation group was lower. |
| Sherif et al, 2017 | Use of Antibiotic Beads to Salvage Infected Breast Implants | 28651885 | Retrospective cohort study | 12 patients | Salvage, absorbable antibiotic beadsa | Infection clearance was 75% using this method (9 of 12 patients). The salvage rate is higher than most other conventional methods reported in the literature. |
| Albright et al, 2016 | One-Step Salvage of Infected Prosthetic Breast Reconstructions Using Antibiotic-Impregnated Polymethylmethacrylate Plates and Concurrent Tissue Expander Exchange | 25774968 | Retrospective cohort study | 14 patients | Salvage, antibiotic-loaded PMMA plate OR beads | Infection clearance was 100% using this method (14 of 14 patients). The salvage rate higher than most other conservative methods reported in the literature. No patients required reoperation for capsular contracture. |
| Lapid, 2011 | Use of Gentamicin Collagen Sponges for the Treatment of Periprosthetic Breast Implant Infection | 21798834 | Case series | 4 cases | Salvage, antibiotic-infused collagen sponge | All 4 cases resulted in successful implant salvage and infection clearance with minimal complications and no notable capsular contracture. |
| Kenna et al, 2018 | Absorbable Antibiotic Beads Prophylaxis in Immediate Breast Reconstruction | 29240639 | Retrospective cohort study | 74 patients, 127 breasts | Prophylaxis, absorbable antibiotic beadsa | The rate of tissue expander loss due to infection was significantly lower in the intervention group compared with the conventional group (1.5% vs 11.9%; P = .024). |
| Hunsicker et al, 2017 | Efficacy of Vancomycin-based Continuous Triple Antibiotic Irrigation in Immediate, Implant-based Breast Reconstruction | 29632794 | Retrospective case-control | 276 patients | Prophylaxis, continuous antibiotic irrigation (96 hours) | The irrigation group had a lower infection rate compared with the historical control group (1.9% vs 6.4%; P = .007) but a higher rate of seroma formation (P = .033). The rate of other surgical complications did not differ between groups. |
| Tutela et al, 2015 | Continuous Postoperative Antibiotic Irrigation via Catheter System Following Immediate Breast Reconstruction | 26664672 | Prospective cohort study | 79 patients | Prophylaxis, continuous antibiotic irrigation (24 hours) | The irrigation group had a lower incidence of premature explantation (2.9% vs 20.0%; P = 0.037), and the infection rate tended to be lower (5.8% vs 22.2%; P = .060). There were no differences in seroma or hematoma formation between groups. |
STIMULAN antibiotic-eluting calcium sulfate beads (Biocomposites; Wilmington, NC). Abbreviation: PMMA, polymethylmethacrylate.
Table 2.
Details of Local Delivery Intervention
| Study | Intervention Type and Group Sizes | Antibiotics and Dosages | Treatment Course | Primary Outcome Measures | Study Weaknesses |
|---|---|---|---|---|---|
| Xue et al, 2020 | Salvage, antibiotic-loaded PMMA plate (45 breasts) OR explantation (17 breasts) | Vancomycin (3 g) and tobramycin (2.2 g) | Periprosthetic infections unresponsive to IV antibiotics underwent either explantation or device exchange with placement of antibiotic impregnated PMMA plate. | Rate of infection clearance (defined by a negative drain culture), abandonment of reconstruction, and successful TE to implant exchange | Variable demographics between groups (comparison group had a worse comorbidity profile), lack of randomization (potential for selection bias), lack of tailored antibiotic regimen to match culture data, retrospective study |
| Kim et al, 2020 | Salvage, continuous vancomycin irrigation to infected breast pocket for a mean time of 11 days (5 breasts) OR explantation (16 breasts) | Vancomycin (1 g/L) irrigation at 250 mL/h for a mean duration of 11 days | Periprosthetic infections unresponsive to IV antibiotics underwent either explantation or antibiotic irrigation of infected pocket with placement of percutaneous catheters in the periexpander cavity under local anesthesia. | Rate of infection clearance and completion of reconstruction, mean cost of treatment | Small sample size, lack of comprehensive outcome measures, lack of tailored antibiotic regimen to match culture data, uneven distribution of adjuvant therapy rates across the study groups, retrospective study design |
| Sherif et al, 2017 | Salvage, absorbable antibiotic beads (12 patients) | Vancomycin (1 g) and tobramycin (1.2 g) | Periprosthetic infections unresponsive to IV antibiotics underwent explantation, pocket lavage, and placement of antibiotic-infused calcium sulfate beads in the breast pocket with a new expander. | Rate of infection clearance | Small sample size, noncomparative study, lack of tailored antibiotic regimen to match culture data, short follow up period (mean, 10.6 months), retrospective study design |
| Albright et al, 2016 | Salvage, antibiotic-loaded PMMA plate OR beads (14 patients) | Vancomycin (2 g) and tobramycin (2.2 g) | Periprosthetic infections unresponsive to IV antibiotics underwent either explantation or device exchange with placement of antibiotic impregnated PMMA plate or beads. Plate and beads removed at time of TE to implant exchange. | Implant pocket sterilization (defined by 2 or more consecutive negative fluid cultures), reoperation for pain or capsular contracture, and infection recurrence (7.1%) were all recorded. | Small sample size, mixed intervention methodology (PMMA plates vs beads), noncomparative study, lack of tailored antibiotic regimen to match culture data, short follow-up period (mean, 8.2 months), retrospective study design |
| Lapid, 2011 | Salvage, implant replacement + gentamicin-infused collagen sponge AND post-op systemic antibiotics (4 patients) | Gentamicin (130 mg) | Periprosthetic infections unresponsive to IV antibiotics underwent explantation, pocket lavage, and replacement of implant with addition of gentamicin-infused collagen sponge. Patients then received a 6-week course of postoperative oral antibiotic regimen. | Infection clearance and implant salvage were primary outcome measures. The presence of capsular contracture was also recorded. | Case series, inadequate description of cases, lack of standardization between patients, use of extensive systemic antibiotic therapy, lack of tailored antibiotic regimens to match culture data |
| Kenna et al, 2018 | Prophylaxis, reconstruction with standard methods (59 patients) OR standard methods + absorbable antibiotic beads (68 breasts) | Vancomycin (0.5 g) and gentamicin (0.24 g) | All patients received immediate, submuscular TE placement. Intervention group had antibiotic-impregnated calcium sulfate beads placed in the pocket along with the expander. | Rate of tissue expander loss secondary to infection | Variable demographics between groups (intervention group had higher BMI, incidence of diabetes, smoking, chemotherapy, and radiation therapy), lack of randomization into treatment vs control groups (sequential enrollment), retrospective study design |
| Hunsicker et al, 2017 | Prophylaxis, continuous vancomycin irrigation into periexpander space for 4 days (163 patients) OR infusion of local anesthetic alone (113 patients) | Irrigation with vancomycin-based triple-antibiotic solution (1 g vancomycin, 80 mg gentamicin, 50,000 IU bacitracin per L) at 4 mL/h for 96 hours | All patients had a catheter and 2 drains placed in the breast pocket. Control group received irrigation with ropivacaine, treatment group also had an antibiotic solution infused into the breast pocket. After 96 hours of irrigation, catheters of both groups were removed. | The incidence of periprosthetic infection was the primary outcome measure. The rate of other surgical complications, such as seroma, hematoma, and skin necrosis were also recorded. | Short follow-up period (6 weeks), subdivision of the intervention group (textured vs smooth implants), uneven baseline patient metrics between study groups, retrospective study design |
| Tutela et al, 2015 | Prophylaxis, continuous irrigation with gentamicin-based triple-antibiotic solution for 24 hours after surgery (34 patients) OR standard methods (45 patients) | Irrigation with gentamicin-based triple antibiotic solution (80 mg gentamicin, 1 g cefazolin, 50,000 IU bacitracin) at 40 mL/h for 24 hours | Patients underwent immediate submuscular TE placement. Intervention group received antibiotic irrigation system in the pocket. Antibiotic irrigation continued for 24 hours after surgery then was discontinued. | Rates of infection and premature explantation were primary outcome measures. The rates of hematoma and seroma formation were also recorded. | Follow-up time not described, few patient demographics reported, few outcome measures recorded, nonrandomized, heterogeneous sample population |
Abbreviations: IV, intravenous; PMMA, polymethylmethacrylate; TE, tissue expander.
Assessment and data extraction
Outcomes of interest covered a range of complications typically associated with breast reconstruction. In studies investigating local antibiotic delivery for the purpose of infection prophylaxis, the rate ofpostoperative infection was the primary outcome of interest. For papers investigating implant salvage, the rate of infection clearance and successful salvage were the primary outcomes of interest. For eachincluded article, information regarding the study design, device used for local antibiotic delivery, metrics, and infection and salvage rates were extracted. After full-text screening as detailed in Figure 1, 8 studies met inclusion criteria. Included studies are summarized in Table 1 and Table 2. In all cases, a P value of <.05 was considered to be statistically significant.
Assessment of quality and bias
To assess the research quality and the risk of bias, Methodological Index for Non-Randomized Studies (MINORS) scores were calculated for each article included in the review. The MINORS framework is a validated scoring system for assessing the methodological quality of nonrandomized surgical studies.39 In the case of noncomparative studies, there are 8 criteria that can be scored from 0 to 2, and the global ideal score is 16. For comparative studies, there are an additional 4 criteria that are also scored between 0 and 2 and add up to a global ideal of 24. The MINORS score was calculated for each paper in this review, and the percent of the global ideal score are reported in Table 3. MINORS scores were determined separately by 2 independent reviewers, and all discrepancies were discussed.
Results
Search results
Searches of Cochrane, Pubmed, and Embase databases yielded a total of 523 articles based on our search criteria. A total of 168 articles were removed as duplicates while 315 articles were removed for irrelevance based on titles and abstracts. Of 40 remaining full-text articles that were assessed for eligibility, 8 articles were found to meet the predetermined inclusion criteria (Figure 1). All included studies were primary literature publications focused on local antibiotic delivery as a method for infection prophylaxis or salvage of periprosthetic infections in IBBR. No randomized control trials were identified in the literature. The study designs and data collection of the 8 studies identified by this review were too heterogeneous to allow for meta-analysis. Table 1 summarizes each of the included studies.
Study methods and sample sizes
Of the 8 studies included, all were retrospective in nature. Three studies examined the use of local antibiotic delivery on infection prophylaxis.40,42 Kenna et al used absorbable, antibiotic-eluting STIMULAN calcium sulfate beads (Biocomposites; Wilmington, NC) placed in the breast pocket alongside a tissue expander as a means of local antibiotic delivery.40 This intervention was compared with conventional reconstructive techniques with a tissue expander but no local antibiotics, and the outcomes were the rate of infection and expander loss. This study included a total of 74 patients; however, individual breasts were treated as data points, resulting in a sample size of n = 127 (68 intervention group, 59 comparison group). Hunsicker et al used continuous irrigation of the periprosthetic space with a triple-antibiotic solution for 96 hours after surgery as a means of infection prophylaxis.41 This group was compared with controls who received continuous infusion of local anesthetic only. A total of 276 patients were included in this study (163 intervention, 113 control), and the outcome measures were the incidence of periprosthetic infection, hematoma, seroma, and skin necrosis.
Tutela et al also used continuous irrigation of the periprosthetic space with a triple-antibiotic solution as a means of prophylaxis.42 Antibiotic irrigation occurred for 24 hours after surgery and results were compared with those in a control group that received no irrigation. Outcome measures included rates of infection, explantation, hematoma, and seroma between the groups. A total of 79 patients were studied (34 intervention, 45 control).
Five studies investigated local antibiotic delivery devices to salvage implants with an existing infection.43,47 Of these 5 studies, 3 were based on small sample sizes (n < 15) and had no intrinsic comparison group. Albright et al (n = 14) used antibiotic-impregnated PMMA (either plates or beads) that were placed in the infected breast pocket.46 Salvage was determined by 2 or more consecutive negative fluid cultures. Sherif et al (n = 12) used absorbable, antibiotic-eluting STIMULAN calcium sulfate beads placed in the infected pocket for implant salvage.45 The outcome measure reported was infection clearance without the need for continued use of IV antibiotics. Lapid used gentamicin collagen sponges placed around an infected implant as a means of local antibiotic delivery.47 In this study, a 6-week parenteral antibiotic therapy was also used concurrently with the novel salvage intervention, making differentiation of the local antibiotics from the systemic regimen difficult. The total number of patients studied was 4, and the outcome measures included infection clearance and capsular contracture.47
Of the 5 salvage studies, 2 used comparison groups and larger sample sizes. Xue et al included a total of 58 patients; however, each breast was again treated as individual data points, resulting in a sample size of n = 62 (45 intervention, 17 comparison).44 This study examined implant salvage using an antibiotic-impregnated PMMA plate with immediate reconstruction compared with conventional methods (explantation and delayed reconstruction). Outcome measures included infection clearance and the rate of completed breast reconstruction. Kim et al used continuous closed irrigation with a vancomycin solution in their intervention group (mean irrigation duration was 11 days) compared with conventional methods (explantation and delayed reconstruction) in the comparison group.43 Outcome measures included infection clearance, rate of reconstruction completion, and total cost.
Methods of local antibiotic delivery
The studies included in this review involve 2 main methods: local antibiotic delivery using an implantable antibiotic eluting material,40,44,45 or continuous irrigation of the periprosthetic space with an antibiotic solution.41,43
Most studies based on a static, implantable antibiotic-eluting device used a combination of 2 broad- spectrum antibiotics combined with a delivery vehicle. Kenna et al and Sherif et al used absorbable calcium sulfate beads while Albright et al and Xue et al used PMMA to supply antibiotics to the surgical site.40,44,46 Lapid used the gentamicin-infused collagen sponges GENTA-COLL (Resorba Medical) as a means of antibiotic delivery to the breast pocket.47 A summary of these parameters is provided in Table 2. Notably, there was substantial variability in the dosages of antibiotics given, with a significantly lower antibiotic concentration used in the prophylaxis study compared with the salvage papers. While each study concluded with an endorsement of their method's efficacy, most authors highlighted the fact that their experimental protocols did not allow them to tailor the type of antibiotic or the dosages used to the bacterial species or severity of infection.
The studies that employed an irrigation-based antibiotic delivery system also varied substantially in their methodology. Both of the studies using irrigation for prophylaxis used a triple-antibiotic solution and a shorter duration of irrigation with less total antibiotic solution when compared with the paper using irrigation for salvage. For prophylaxis, Hunsicker et al used 400 mL of antibiotic solution delivered through a 96-hour irrigation while Tutela et al irrigated for 24 hours and used a total volume of 1 L of antibiotic solution.41,42 For salvage, Kim et al irrigated the periprosthetic space for an average of 11 days at a rate of 250 mL of antibiotic solution per hour.43
While the antibiotic elution profile from delivery vehicles like PMMA or calcium sulfate is reported in other surgical fields where these materials are more commonly used,48 elution profile was only discussed in 1 paper included in this review, Albright et al.46 Surgical drains are often placed in the breast pocket following IBBR and offer an ideal method of sampling antibiotic concentration in the periprosthetic space. Albright et al compared the concentration of vancomycin in the drain fluid with serum levels.46 Their results showed a substantial increase of vancomycin concentration in the drain output compared with serum measurements. In the drain fluid, they measured vancomycin levels ranging from 355 μg/mL the day after surgery to 2.4 μg/mL up to 48 days following the procedure. Serum concentrations of patients receiving IV antibiotics during their hospital stay ranged from 28 μg/mL to 0.8 μg/mL and were not detected beyond 20 days after surgery.
Effects of local antibiotic delivery on salvage
Five of the studies in this review investigated the use of local antibiotic delivery as a method of breast implant salvage, which was defined as complete infection clearance.43,47 All of the papers were retrospective, and only 2 included a comparison group.43,44 The other 3 papers piloted a novel technique for implant salvage using either calcium sulfate beads,45 PMMA implants,46 or gentamicin- infused collagen sponges,47 with no comparison or control group. These noncomparative papers demonstrated favorable outcomes that matched or exceeded salvage rates reported in the literature using more conventional methods. Albright et al reported 100% infection clearance in their 14 patients.46 However, they also reported 1 instance of infection recurrence that resulted in the loss of the implant, which they attributed to steroid use outside of their study design. Sherif et al reported a salvage rate of 75% in their 12 patients.45 The 3 failed salvage cases were attributed to “exceptionally complicated situations,” which included 1 patient who had inadequate soft tissue coverage secondary to radiation treatment and went on to receive a superior gluteal artery perforator flap, 1 patient with antibiotic-resistant Rhodococcus species, and 1 patient who left the country immediately after surgery and was subsequently lost to follow-up. In the Lapid study, local antibiotic delivery was used in combination with extended parenteral antibiotic treatment for prosthetic salvage.47 Though the salvage rate was 100% in the 4 patients included in this series, the author's combined antibiotic approach obscures the efficacy of local antibiotic delivery method on its own.47
The salvage papers that included a comparison group used the most conservative treatment, implant removal and systemic antibiotics, as their control. Xue et al compared implant salvage using antibioticeluting PMMA plates with immediate explantation.44 The authors reported an infection clearance rate of 82.2% in their treatment group compared with 94.1% in the explantation group (P = .42). Notably, significantly more patients who received the salvage procedure went on to complete their breast reconstruction (84.4% vs 35.3%; P < .001), and far fewer abandoned reconstruction altogether (2% vs 58.8%; P < .001). Kim et al used a similar methodology, comparing salvage with continuous vancomycin irrigation of the periprosthetic space to explantation.43 Both treatment groups achieved 100% infection clearance. Though there was no significant difference between the groups in any reported outcome measure, those who underwent salvage via antibiotic irrigation tended to be less likely to abandon their reconstruction (20% vs 68.8%; P = .1).
Effects of local antibiotic delivery on prophylaxis
Three studies investigated the use of local antibiotic delivery as a means of prophylaxis against periprosthetic infections. Kenna et al compared tissue expander-based breast reconstruction using conventional methods to the same procedure with the addition of antibiotic-infused calcium sulfate beads in the implant pocket.40 Their primary outcome was the rate of tissue expander loss due to infection, which they found to be reduced by 8-fold in the group that included the beads (1.5% vs 11.9%; P = .024). Hunsicker et al used a continuous irrigation of the periexpander space with either tripleantibiotic solution (intervention group) or anesthetic solution alone for 96 hours after surgery.41 They found that irrigation with antibiotic solution significantly reduced infection rates (1.9% vs 6%; P = .007). Tutela et al compared irrigation of the periprosthetic space with triple-antibiotic solution for 24 hours following surgery to reconstruction with standard methods without irrigation.42 They found that antibiotic irrigation tended to reduce the total rate of infection (5.9% vs 22%; P = .06) and significantly reduced the total number of premature explantations (3% vs 20%; P = .03).
Table 3.
Study Quality Assessment
| Study | Intervention Type | Antibiotic Vehicle | Comparative Study (yes, no)a | Mean MINORS Scoreb | Percent of “Ideal” Scorec |
|---|---|---|---|---|---|
| Xue ct al, 2020 | Salvage | PMMA plate or beads | Ves | 14 | 58% |
| Kim et al, 2020 | Salvage | Irrigation | Ves | 16 | 67% |
| Sherif et al, 2017 | Salvage | Calcium sulfate beads | μ | 6 | 38% |
| Albright et al, 2016 | Salvage | PMAAA plate or beads | μ | 9 | 56% |
| Lapid, 2011 | Salvage | Collagen sponge | μ | 6 | 38% |
| Kenna et al, 2013 | Prophylaxis | Calcium sulfate beads | Ves | 16 | 67% |
| Hunsicker et al, 2017 | Prophylaxis | Irrigation | Ves | 17 | 71% |
| Tutela et al, 2015 | Prophylaxis | Irrigation | Ves | 9 | 38% |
Studies were either comparative (containing an internal control group) or noncomparative (lacking a control group) and were scored according to their respective guidelines.
Using the Methodological Index for Non-Randomized Studies (MINORS) scoring system, the quality and potential for bias present of each study was calculated independently by 2 reviewers and averaged.
For comparative studies, the ideal score was 24. For noncomparative studies, the ideal score was 16. Abbreviation: PMMA, polymethylmethacrylate.
Assessment of quality and bias
Table 3 summarizes the MINORS score of each study included in this review. The MINORS assessment was based on 8 criteria for noncomparative studies and 12 criteria for comparative studies. Each criterion was assigned scores of 0 (not reported), 1 (reported but inadequate), or 2 (reported and adequate). The authors of the validated instrument state the global ideal score is 16 for noncomparative studies and 24 for comparative studies.39 There were 3 noncomparative studies included in this review, with MINORS scores ranging from 6 to 9. In the noncomparative group, the mean MINORS score was 7, representing 43.75% of the ideal score. There were 5 comparative studies included in this review, with scores ranging from 14 to 17. In this group, the mean MINORs score was 14.4, representing 60% of the ideal score. On average, the 8 papers included in this review scored 53.9% of the ideal MINORs score.
Discussion
This systematic review includes a total of 8 studies that met the predetermined inclusion criteria, with 5 studies focusing on use of local antibiotic delivery as a means of implant salvage and 3 on infection prophylaxis. Of the studies identified in the literature, only 1 was prospective, and none were randomized control trials. Five studies featured comparison groups; the other 3 studies were noncomparative, proof-of-concept studies employing new methods for salvaging infected implants where the salvage rate was compared with salvage rates of more conventional approaches found in the literature. Though there is a high degree of variability among the study techniques described, all 8 articles advocate for the use of local antibiotic delivery for either implant infection salvage or prophylaxis.
The 2 comparative studies investigating implant salvage both reported similar salvage rates in the intervention and explantation groups.43,44 As a result, both papers concluded that local antibiotic delivery, either via PMMA or direct irrigation, for the purpose of implant salvage offers a successful alternative to explantation. The other studies investigating salvage of infected implants did not include a comparison group. Still, all authors concluded that the use of local antibiotic delivery either by PMMA,46 calcium sulfate beads,45 or collagen sponges47 represents a promising method for salvaging infected breast implants without the need for extended IV antibiotic use or the delayed recovery time typical of explantation. Similarly, the 3 papers examining local antibiotic delivery for infection prophylaxis all concluded that local antibiotic treatment reduced postoperative rates of infection, with some reports indicating that the infection rate was as much as 8-fold lower than that seen in control groups.40,42
When analyzing the studies that used antibiotic irrigation, the included articles differed significantly in the types of antibiotics used, the total volume of antibiotics used, and the duration of use. Kim et al investigated salvage and used a vancomycin solution (1 g/L) that was continuously infused into the periexpander cavity at a rate of 250 mL/h for an average of 11 days.43 This method used both the highest volume of solution and longest duration of irrigation, resulting in a mean use of 66 g of vancomycin for infection clearance. By contrast, the 2 papers examining irrigation as a means of prophylaxis reported that pumps were in place for only 96 hours41 and 24 hours42 following surgery, using an average of 400 mL of vancomycin-based triple-antibiotic solution and 1 L of gentamicin-based triple-antibiotic solution, respectively. In all cases, both the pumps and accompanying drains were removed from the breast without the need for additional surgical intervention, minimizing any complications that may stem from reoperation.
In the study on salvage by Kim et al, placement of the irrigation pump and drain was done under local anesthesia, enabling infection clearance without any invasive surgery.43 While the device itself may be cumbersome and poses a risk of infection due to the transdermal nature of the tubing, its ability to be inserted and removed nonsurgically is a major advantage. Another advantage that the authors mention highlights the hydrodynamic role of the irrigation itself. Even in the absence of antibiotics, continual fluid movement both removes debris from the periprosthetic space and helps disrupts biofilm formation around the implant. Though none of the papers altered the concentration or species of the antibiotics in their solutions, in theory, irrigation with an external pump would allow for this kind of highly controlled titration, even after surgery is finished.
Across the included studies, relatively little attention was given to other outcome measures or complications, such as hematoma, seroma, dehiscence, capsular contracture, patient satisfaction, or aesthetic appearance, although these undoubtedly have a bearing on overall surgical success. Two salvage studies included analysis of reconstruction completion versus abandonment. Xue et al found that implant salvage with local antibiotics (PMMA implant) significantly increased the rate of reconstruction completion (84.4% vs 35.3%; P < .001) and decreased the rate of reconstruction abandonment (2% vs 58.8%; P < .001) compared with the implant removal and delayed reconstruction, which is a more typical approach to periprosthetic infection.44 Similarly, Kim et al reported that local antibiotic delivery (irrigation) tended to increase the rate of reconstruction completion (80% vs 31%) compared with conservative treatment, although their results did not reach significance (P = .1).43
Among the comparative studies, several instances of heterogenous underlying patient populations may confound interpretation of the results. In some cases, this was due to imperfect study methodology; in other cases, however, these variations were simply a product of normal patient variability and small sample sizes. Differences in patient factors, such as obesity, radiation therapy, or diabetes, have the potential to influence study results and may be a limitation to the studies included in this review. This limitation is discussed in Table 2 and is assessed in the MINORS scores; however, these differences in patient population were generally minor and did not unilaterally favor one intervention over another. Across these studies, comorbidities were occasionally concentrated in local antibiotic group (Kenna et al; Kim et al); in others, they were less common in the local antibiotic groups (eg, Xue et al.), and in others, the distribution of these comorbidities was mixed (eg, Hunsicker et al; Tutela et al.).40,44
Kim et al was the only study to compare the costs of each intervention.43 The authors found that, on average, their method of expander irrigation was less expensive (mean, $3033) than conventional treatment with expander removal (mean, $5307), though they offered no statistics to qualify this comparison. This reduction in cost was at least partially due to the fact that salvage with antibiotic irrigation could be done under local anesthesia and did not require implant replacement. The authors also noted the tendency for the explantation group to switch to autologous reconstruction after failing implant-based methods, therefore the average difference in cost between their intervention and comparison groups was actually much starker.
The variability of antibiotic delivery vehicles used in the included studies also highlights the important decision of using absorbable versus nonabsorbable methods. For example, collagen sponges and calcium sulfate are absorbable materials that do not need to be removed from the body once implanted, allowing for more flexibility when designing a surgical protocol. PMMA, on the other hand, will remain intact in the patient until it is removed during a second operation. Thus, the only feasible use of PMMA in breast reconstruction is in 2-stage breast reconstruction, where the PMMA plate is placed alongside a tissue expander during the first stage and then removed when tissue expander is exchanged for the implant.
The papers included in this review seem to show that absorbable material can be used effectively for both prophylaxis and salvage. The authors of the papers using calcium sulfate both highlighted the advantage that an absorbable vehicle provides over PMMA, namely that there is no need to keep track of the antibiotic-eluting device once it is placed, and there is no need for reoperation to remove the device. Besides infection control and biodegradation, calcium sulfate offers the advantage of being able to carry a wider range of antibiotics, such as antibiotics that are heat-sensitive.49 During curing, PMMA produces a highly exothermic reaction that can destabilize heat-sensitive antibiotic compounds.44 Calcium sulfate does not have this same limitation and can be used with both heat-sensitive and non–heat-sensitive antibiotics without risk to the patient or antibiotic compound.50 Gentamicin collagen implants,51 on the other hand, are made already containing gentamicin, thus offering less flexibility than either calcium sulfate or PMMA in terms of antibiotic choice. As a result, this review highlights that the choice of antibiotic delivery vehicle remains nuanced and involves decision-making regarding antibiotic choice and number of future operations involved.
Limitations
The included studies in this review are not without their limitations. The noncomparative, proof-of-concept studies all had small sample sizes (n < 15) and were underpowered. In addition, most studies had limited analysis of relevant outcome measures. All studies included the outcome measure most relevant to the aim of the study, namely whether or not local antibiotic delivery reduced infection or improved salvage rates, but few reported on outcomes other than infection. Additionally, attention to the confounding role of patient comorbidities was absent in some studies.
To determine whether a new surgical protocol should be adopted, such as the addition of antibioticeluting materials in the breast pocket, a more exhaustive investigation of patient factors and surgical outcomes is needed. The impact of local antibiotic delivery systems on implant malposition, capsular contracture, hematoma, seroma, aesthetic outcome, cost, and patient satisfaction should be considered for future studies. The lack of additional outcome measures may also be a consequence of the relatively short follow-up periods used by most studies. Because many important outcomes, like capsular contracture, aesthetic appearance, rate of reoperation, and patient satisfaction are all affected by time, additional data may give more clarity on the long-term outcomes and consequences of these novel surgical methods.
Conclusions
Periprosthetic infection in the context of IBBR can be a devastating complication for patients and surgeons. Treatment of an infected breast pocket usually involves a course of antibiotics and explantation/reconstructive delay if the infection does not abate. Because local antibiotic delivery can maintain high antibiotic concentrations in a specific site of interest without the risk of toxicity that comes with similar concentrations of systemic antibiotics, its use for infection prophylaxis or salvage in IBBR may prove useful. The studies included in this review indicate that local antibiotic delivery to the breast pocket can significantly reduce infection rates when used for prophylaxis and is a viable method of implant salvage in the context of a periprosthetic infection. This is especially appealing when considering that systemic antibiotic administration for prophylaxis or salvage has inconsistent efficacy and carries a higher risk of systemic toxicity.
This systematic review offers support for both the safety and efficacy of using local antibiotic delivery in breast reconstruction. However, future studies investigating long-term outcomes and including a wider variety of outcome measures will be beneficial to determine if local antibiotic delivery to the breast pocket becomes standard of care.
Acknowledgments
Disclosures: No authors disclose financial disclosures or conflicts of interest.
References
- 1.Lohmander F, Lagergren J, Johansson H, Roy PG, Frisell J, Brandberg Y. Quality of life and patient satisfaction after implant-based breast reconstruction with or without acellular dermal matrix: randomized clinical trial. BJS Open. 2020;4(5):811–820. doi:10.1002/bjs5.50324 10.1002/bjs5.50324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ooi AS, Song DH. Reducing infection risk in implant-based breast-reconstruction surgery: challenges and solutions. Breast Cancer Dove Med Press. 2016;8:161–172. doi:10.2147/BCTT.S97764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eltahir Y, Krabbe-Timmerman IS, Sadok N, Werker PMN, de Bock GH. Outcome of quality of life for women undergoing autologous versus alloplastic breast reconstruction following mastectomy: a systematic review and meta-analysis. Plast Reconstr Surg. 2020;145(5):1109–1123. doi:10.1097/PRS.0000000000006720 10.1097/PRS.0000000000006720 [DOI] [PubMed] [Google Scholar]
- 4.Pusic AL, Matros E, Fine N, et al. Patient-reported outcomes 1 year after immediate breast reconstruction: results of the Mastectomy Reconstruction Outcomes Consortium study. J Clin Oncol Off J Am Soc Clin Oncol. 2017;35(22):2499–2506. doi:10.1200/JCO.2016.69.9561 10.1200/JCO.2016.69.9561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reinders FCJ, Young-Afat DA, Batenburg MCT, et al. Higher reconstruction failure and less patient-reported satisfaction after post mastectomy radiotherapy with immediate implant-based breast reconstruction compared to immediate autologous breast reconstruction. Breast Cancer Tokyo Jpn. 2020;27(3):435–444. doi:10.1007/s12282-019-01036-4 10.1007/s12282-019-01036-4 [DOI] [PubMed] [Google Scholar]
- 6.Tsoi B, Ziolkowski NI, Thoma A, Campbell K, O'Reilly D, Goeree R. Safety of tissue expander/implant versus autologous abdominal tissue breast reconstruction in postmastectomy breast cancer patients: a systematic review and meta-analysis. Plast Reconstr Surg. 2014;133(2):234–249. doi:10.1097/01.prs.0000436847.94408.11 10.1097/01.prs.0000436847.94408.11 [DOI] [PubMed] [Google Scholar]
- 7.Scurci S, Parecco J, De La Cruz L, Chatterjee A. Abstract P8: nationwide cost comparison of autologous vs implant-based postmastectomy reconstruction. Plast Reconstr Surg - Glob Open. 2017;5:107. doi:10.1097/01.GOX.0000516665.93739.ee 10.1097/01.GOX.0000516665.93739.ee [DOI] [Google Scholar]
- 8.Papa G, Frasca A, Renzi N, et al. Protocol for prevention and monitoring of surgical site infections in implant-based breast reconstruction: preliminary results. Med Kaunas Lith. 2021;57(2):151. doi:10.3390/medicina57020151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brahmbhatt RD, Huebner M, Scow JS, et al. National practice patterns in preoperative and postoperative antibiotic prophylaxis in breast procedures requiring drains: survey of the American Society of Breast Surgeons. Ann Surg Oncol. 2012;19(10):3205–3211. doi:10.1245/s10434-012-2477-1 10.1245/s10434-012-2477-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khan UD. Breast augmentation, antibiotic prophylaxis, and infection: comparative analysis of 1,628 primary augmentation mammoplasties assessing the role and efficacy of antibiotics prophylaxis duration. Aesthetic Plast Surg. 2010;34(1):42–47. doi:10.1007/s00266-009-9427-8 10.1007/s00266-009-9427-8 [DOI] [PubMed] [Google Scholar]
- 11.Ariyan S, Martin J, Lal A, et al. Antibiotic prophylaxis for preventing surgical-site infection in plastic surgery: an evidence-based consensus conference statement from the American Association of Plastic Surgeons. Plast Reconstr Surg. 2015;135(6):1723–1739. doi:10.1097/PRS.0000000000001265 10.1097/PRS.0000000000001265 [DOI] [PubMed] [Google Scholar]
- 12.Bratzler DW, Dellinger EP, Olsen KM, et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Am J Health Syst Pharm. 2013;70(3):195–283. doi:10.2146/ajhp120568 10.2146/ajhp120568 [DOI] [PubMed] [Google Scholar]
- 13.Mankowski P, Cherukupalli A, Slater K, Carr N. Antibiotic prophylaxis in plastic surgery correlation between practice and evidence. Plast Surg Oakv Ont. 2021;29(2):132–138. doi:10.1177/2292550321997005 10.1177/2292550321997005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Clayton JL, Bazakas A, Lee CN, Hultman CS, Halvorson EG. Once is not enough: withholding postoperative prophylactic antibiotics in prosthetic breast reconstruction is associated with an increased risk of infection. Plast Reconstr Surg. 2012;130(3):495–502. doi:10.1097/PRS.0b013e31825dbefe 10.1097/PRS.0b013e31825dbefe [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.de Jonge SW, Boldingh QJJ, Solomkin JS, et al. Effect of postoperative continuation of antibiotic prophylaxis on the incidence of surgical site infection: a systematic review and meta-analysis. Lancet Infect Dis. 2020;20(10):1182–1192. doi:10.1016/S1473-3099(20)30084-0 10.1016/S1473-3099(20)30084-0 [DOI] [PubMed] [Google Scholar]
- 16.World Health Organization. WHO recommends 29 ways to stop surgical infections and avoid superbugs. Published November 6, 2016. Accessed December 8, 2022. https://www.who.int/news/item/03-11-2016-who-recommends-29-ways-to-stop-surgical-infections-and-avoid-superbugs
- 17.Spear SL, Howard MA, Boehmler JH, Ducic I, Low M, Abbruzzesse MR. The infected or exposed breast implant: management and treatment strategies. Plast Reconstr Surg. 2004;113(6):1634–1644. doi:10.1097/01.prs.0000117194.21748.02 10.1097/01.PRS.0000117194.21748.02 [DOI] [PubMed] [Google Scholar]
- 18.Xue AS, Kania KE, Brown RH, Bullocks JM, Hollier LH, Izaddoost SA. Salvage of infected prosthetic breast reconstructions. Semin Plast Surg. 2016;30(2):55–59. doi:10.1055/s-0036-1580729 10.1055/s-0036-1580729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bennett SPH, Fitoussi AD, Berry MG, Couturaud B, Salmon RJ. Management of exposed, infected implant-based breast reconstruction and strategies for salvage. J Plast Reconstr Aesthetic Surg. 2011;64(10):1270–1277. doi:10.1016/j.bjps.2011.05.009 10.1016/j.bjps.2011.05.009 [DOI] [PubMed] [Google Scholar]
- 20.Halvorson EG, Disa JJ, Mehrara BJ, Burkey BA, Pusic AL, Cordeiro PG. Outcome following removal of infected tissue expanders in breast reconstruction: a 10-year experience. Ann Plast Surg. 2007;59(2):131–136. doi:10.1097/01.sap.0000252716.73356.68 10.1097/01.sap.0000252716.73356.68 [DOI] [PubMed] [Google Scholar]
- 21.Gardner AD, Medcraft JW. Letter: Antibiotic-bone-cement mixtures in prevention of infection following total joint replacement. Lancet Lond Engl. 1974;2(7885):891. doi:10.1016/s0140-6736(74)91217-3 10.1016/S0140-6736(74)91217-3 [DOI] [PubMed] [Google Scholar]
- 22.Elson RA, Jephcott AE, McGechie DB, Verettas D. Antibiotic-loaded acrylic cement. J Bone Joint Surg Br. 1977;59(2):200–205. doi:10.1302/0301-620X.59B2.873980 10.1302/0301-620X.59B2.873980 [DOI] [PubMed] [Google Scholar]
- 23.Gorvetzian JW, Kunkel RP, Demas CP. A single center retrospective evaluation of a surgical strategy to combat persistent soft tissue wounds utilizing absorbable antibiotic beads. Adv Wound Care. 2019;8(2):49–57. doi:10.1089/wound.2018.0795 10.1089/wound.2018.0795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Poi MJ, Pisimisis G, Barshes NR, et al. Evaluating effectiveness of antibiotic polymethylmethacrylate beads in achieving wound sterilization and graft preservation in patients with early and late vascular graft infections. Surgery. 2013;153(5):673–682. doi:10.1016/j.surg.2012.10.011 10.1016/j.surg.2012.10.011 [DOI] [PubMed] [Google Scholar]
- 25.Schade VL, Roukis TS. The role of polymethylmethacrylate antibiotic-loaded cement in addition to debridement for the treatment of soft tissue and osseous infections of the foot and ankle. J Foot Ankle Surg. 2010;49(1):55–62. doi:10.1053/j.jfas.2009.06.010 10.1053/j.jfas.2009.06.010 [DOI] [PubMed] [Google Scholar]
- 26.Stone PA, Armstrong PA, Bandyk DF, et al. Use of antibiotic-loaded polymethylmethacrylate beads for the treatment of extracavitary prosthetic vascular graft infections. J Vasc Surg. 2006;44(4):757–761. doi:10.1016/j.jvs.2006.05.056 10.1016/j.jvs.2006.05.056 [DOI] [PubMed] [Google Scholar]
- 27.Drohan A, Minor S. Prospective study of single-stage repair of contaminated hernias with the novel use of calcium sulphate antibiotic beads in conjunction with biologic porcine submucosa tissue graft. Can J Surg J Can Chir. 2020;63(6):E530–E532. 10.1503/cjs.021819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hoogerboord CM, Cwinn M, Minor SR. Conservative treatment of infected mesh by use of gentamycin impregnated calcium sulphate antibiotic beads: a report of two cases. Hernia. 2019;23(2):407–409. doi:10.1007/s10029-019-01910-2 10.1007/s10029-019-01910-2 [DOI] [PubMed] [Google Scholar]
- 29.Whiteside LA, Roy ME. One-stage revision with catheter infusion of intraarticular antibiotics successfully treats infected THA. Clin Orthop. 2017;475(2):419–429. doi:10.1007/s11999-016-4977-y 10.1007/s11999-016-4977-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Baker NF, Hart AM, Carlson GW, Losken A. A systematic review of breast irrigation in implant-based breast surgery. Ann Plast Surg. 2021;86(3):359–364. doi:10.1097/SAP.0000000000002481 10.1097/SAP.0000000000002481 [DOI] [PubMed] [Google Scholar]
- 31.Epps MT, Langsdon S, Pels TK, Lee TM, Thurston T, Brzezienski MA. Antimicrobial irrigation and technique during breast augmentation: survey of current practice. Plast Reconstr Surg Glob Open. 2019;7(8):e2310. doi:10.1097/GOX.0000000000002310 10.1097/GOX.0000000000002310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Frois AO, Harbour PO, Azimi F, et al. The role of antibiotics in breast pocket irrigation and implant immersion: a systematic review. Plast Reconstr Surg Glob Open. 2018;6(9):e1868. doi:10.1097/GOX.0000000000001868 10.1097/GOX.0000000000001868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bain MA, Koullias GJ, Morse K, Wendling S, Sabolinski ML. Type I collagen matrix plus polyhexamethylene biguanide antimicrobial for the treatment of cutaneous wounds. J Comp Elf Res. 2020;9(10):691–703. doi:10.2217/cer-2020-0058 10.2217/cer-2020-0058 [DOI] [PubMed] [Google Scholar]
- 34.Oropallo AR. Use of native type I collagen matrix plus polyhexamethylene biguanide for chronic wound treatment. Plast Reconstr Surg Glob Open. 2019;7(1):e2047. doi:10.1097/GOX.0000000000002047 10.1097/GOX.0000000000002047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Blatnik JA, Thatiparti TR, Krpata DM, Zuckerman ST, Rosen MJ, von Recum HA. Infection prevention using affinity polymer-coated, synthetic meshes in a pig hernia model. J Surg Res. 2017;219:5–10. doi:10.1016/j.jss.2017.05.003 10.1016/j.jss.2017.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Majumder A, Neupane R, Novitsky YW. Antibiotic coating of hernia meshes: the next step toward preventing mesh infection. Surg Technol Int. 2015;27:147–153. [PubMed] [Google Scholar]
- 37.Minor S, Brown CJ, Rooney PS, et al. Single-stage repair of contaminated hernias using a novel antibiotic-impregnated biologic porcine submucosa tissue matrix. BMC Surg. 2020;20(1):58. doi:10.1186/s12893-020-00715-w 10.1186/s12893-020-00715-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Negenborn VL, Smit JM, Dikmans REG, et al. Short-term cost-effectiveness of one-stage implant- based breast reconstruction with an acellular dermal matrix versus two-stage expander-implant reconstruction from a multicentre randomized clinical trial. Br J Surg. 2019;106(5):586–595. doi:10.1002/bjs.11102 10.1002/bjs.11102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. doi:10.1046/j.1445-2197.2003.02748.x 10.1046/j.1445-2197.2003.02748.x [DOI] [PubMed] [Google Scholar]
- 40.Kenna DM, Irojah BB, Mudge K, Eveler K. Absorbable antibiotic beads prophylaxis in immediate breast reconstruction. Plast Reconstr Surg. 2018;141(4):486e–492e. doi:10.1097/PRS.0000000000004203 10.1097/PRS.0000000000004203 [DOI] [PubMed] [Google Scholar]
- 41.Hunsicker LM, Chavez-Abraham V, Berry C, McEwen D. Efficacy of vancomycin-based continuous triple antibiotic irrigation in immediate, implant-based breast reconstruction. Plast Reconstr Surg Glob Open. 2017;5(12):e1624. doi:10.1097/GOX.0000000000001624 10.1097/GOX.0000000000001624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tutela JP, Duncan DP, Kelishadi SS, Chowdhry S, Boyd T, Little JA. Continuous postoperative antibiotic irrigation via catheter system following immediate breast reconstruction. Eplasty. 2015;15:e49. [PMC free article] [PubMed] [Google Scholar]
- 43.Kim A, Jung JH, Lee YJ, Park JW, Pyon JK. Minimally invasive salvage of infected breast tissue expanders: A continuous closed irrigation technique based on surface biofilm disruption. J Plast Reconstr Aesthet Surg. 2020;73(2):295–302. doi:10.1016/j.bjps.2019.07.020 10.1016/j.bjps.2019.07.020 [DOI] [PubMed] [Google Scholar]
- 44.Xue AS, Volk AS, DeGregorio VL, Jubbal KT, Bullocks JM, Izaddoost SA. Follow-up study: one-step salvage of infected prosthetic breast reconstructions using antibiotic-impregnated polymethylmethacrylate plates and concurrent tissue expander exchange. Plast Reconstr Surg. 2020;145(2):240e–250e. doi:10.1097/PRS.0000000000006501 10.1097/PRS.0000000000006501 [DOI] [PubMed] [Google Scholar]
- 45.Sherif RD, Ingargiola M, Sanati-Mehrizy P, Torina PJ, Harmaty MA. Use of antibiotic beads to salvage infected breast implants. J Plast Reconstr Aesthet Surg. 2017;70(10):1386–1390. doi:10.1016/j.bjps.2017.05.023 10.1016/j.bjps.2017.05.023 [DOI] [PubMed] [Google Scholar]
- 46.Albright SB, Xue AS, McKnight A, et al. One-step salvage of infected prosthetic breast reconstructions using antibiotic-impregnated polymethylmethacrylate plates and concurrent tissue expander exchange. Ann Plast Surg. 2016;77(3):280–285. doi:10.1097/SAP.0000000000000409 10.1097/SAP.0000000000000409 [DOI] [PubMed] [Google Scholar]
- 47.Lapid O. Use of gentamicin collagen sponges for the treatment of periprosthetic breast implant infection. J Plast Reconstr Aesthetic Surg. 2011;64(12):e313–316. doi:10.1016/j.bjps.2011.05.007 10.1016/j.bjps.2011.05.007 [DOI] [PubMed] [Google Scholar]
- 48.Metsemakers WJ, Fragomen AT, Moriarty TF, et al. Evidence-based recommendations for local antimicrobial strategies and dead space management in fracture-related infection. J Orthop Trauma. 2020;34(1):18–29. doi:10.1097/BOT.0000000000001615 10.1097/BOT.0000000000001615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jiang N, Dusane DH, Brooks JR, et al. Antibiotic loaded β-tricalcium phosphate/calcium sulfate for antimicrobial potency, prevention and killing efficacy of Pseudomonas aeruginosa and Staphylococcus aureus biofilms. Sci Rep. 2021;11(1):1446. doi:10.1038/s41598-020-80764-6 10.1038/s41598-020-80764-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Karr JC, Lauretta J, Keriazes G. In vitro antimicrobial activity of calcium sulfate and hydroxyapatite (Cerament Bone Void Filler) discs using heat-sensitive and non-heat-sensitive antibiotics against methicillin-resistant Staphylococcus aureus and Pseudomonas aeruginosa. J Am Podiatr Med Assoc. 2011;101(2):146–152. doi:10.7547/1010146 10.7547/1010146 [DOI] [PubMed] [Google Scholar]
- 51.Resorba Medical. Biosurgicals: GENTA-COLL resorb. Accessed March 5, 2023. https://resorba.com/region/row/product/biosurgicals/genta-coll-resorb/