Abstract
Systemic and mucosal antibody responses against both the major subunit of colonization factor antigen I (CFA/I) of enterotoxigenic Escherichia coli (ETEC) and the somatic lipopolysaccharide expressed by recombinant bivalent Salmonella vaccine strains were significantly enhanced by coadministration of a detoxified derivative with preserved adjuvant effects of the ETEC heat-labile toxin, LT(R192G). The results further support the adjuvant effects of LT(R192G) and represent a simple alternative to improve responses against passenger antigens expressed by orally delivered Salmonella vaccine strains.
Oral vaccines based on bivalent or multivalent attenuated Salmonella strains represent one of the most dynamic and promising areas of mucosal vaccine development (8). Such strains are effective delivery systems of heterologous antigens to the mammalian immune system due to their ability to colonize the gut-associated lymphoid tissue (GALT) and invade deeper tissues and organs, leading to serum and secreted antibody responses without inflicting significant damage to the host (2, 8, 18). However, the low immunogenicity of the carried antigen, unstable or reduced gene expression, and deficient gut colonization impair the ability of Salmonella vaccine strains to induce significant antigen-specific immune responses against somatic and passenger antigens, thus decreasing the potential usefulness of such a vaccine approach for humans as well as other mammalian hosts.
The immunogenicity of orally administered antigens can be improved by bacterial products with known adjuvant properties. Among the most studied orally delivered adjuvants are the cholera toxin (CT) (10, 22–24), produced by Vibrio cholerae, and the heat-labile toxin (LT) (4, 7, 14, 32, 34), produced by some enterotoxigenic Escherichia coli (ETEC) strains. Both LT and CT are A/B-type toxins, which increase secretion of water and electrolytes by enterocytes through adenylate cyclase activation (10, 22, 34). The B subunits bind to host cell membrane ganglioside receptors and promote internalization of the enzymatically active A subunit, which is cleaved in a trypsin-sensitive site into two portions, A2 and A1 (10, 14, 21, 34). LT seems to be particularly interesting as an adjuvant for human use since it has an inherent lower toxicity than CT (4, 24, 32, 34); it activates both Th1- and Th2-type CD4+ cells (32) and, unlike CT, it does not evoke allergic sensitization after oral administration (31, 32, 34). The mucosal and systemic adjuvant properties of LT have been repeatedly demonstrated in mice given soluble antigens orally, such as ovalbumin and keyhole limpet hemocyanin (4, 7, 9, 14, 32, 34), or inactivated microorganisms, such as viruses and bacterial cells (3, 5, 17, 20, 25). In order to explore the use of LT as an adjuvant for humans, several LT variants with reduced toxicity but preserved adjuvant functions have been described (3, 5–7, 9, 17, 28). Dickinson and Clements (6–7) designed a nontoxic LT derivative, LT(R192G), containing an amino acid exchange (R192→G) at the A subunit trypsin-sensitive site. The resulting molecule lacked detectable ADP-ribosylating activity but retained the LT adjuvant effects following oral coadministration with soluble antigens (6–7) or inactivated Salmonella (3) or attenuated Shigella (17) cells.
In this study we propose a new orally delivered vaccine formulation consisting of the combined use of a live bivalent Salmonella enterica serovar Typhimurium aroA strain expressing the major subunit of the colonization factor antigen I (CFA/I), a fimbrial antigen involved with the colonization of the human gut epithelium by ETEC (1, 10), and LT(R192G). The hybrid ETEC-Salmonella vaccine strain (HG3) has previously been shown to elicit weak systemic and mucosal antibody responses against the heterologous antigen after repeated oral dosing to mice (15).
The bacterial strain used in this work is a derivative of the aromatic-dependent (aroA) histidine-requiring serovar Typhimurium SL3261 strain (18) transformed with pCFA-1 which encodes the major subunit of the CFA/I fimbriae. pCFA-1 is a derivative of pKK223-3 (Pharmacia, Uppsala, Sweden) containing the PCR-amplified cfaB gene cloned into the vector polylinker region under control of the tac promoter. The cloned cfaB gene contained the complete sequence of the mature fimbrial subunit (herein referred as the CFA/I subunit), which is composed of 143 amino acids (Mr 15,057) and a signal peptide of 23 amino acids (11, 19). To avoid overexpression of the CFA/I subunit under noninducing conditions, an F′ plasmid carrying the lacIq gene was also introduced into the vaccine strain (15). The HG3 strain could only express the CFA/I subunit in the presence of inducer (isopropyl-β-d-thiogalactopyranoside [IPTG]) during in vitro growth, a feature probably associated with the inherently low immunogenicity of this construction following oral delivery to BALB/c mice (15). ETEC strains 258909-3 (CFA/I, O128:H?, and ST/LT) and 258909-3M, a CFA/I-negative derivative (13), were used in inhibition of hemagglutination assays (IHA). The HG3 strain was grown aerobically in Luria broth supplemented with 1 μg of 2,3-dihydroxybenzoic acid (Sigma Chemical Co., St. Louis, Mo.) per ml, ampicillin (100 μg/ml), and streptomycin (70 μg/ml) at 37°C. ETEC strains were grown overnight on Casamino Acids-yeast extract agar plates at 37°C, as previously described (11). The HG3 strain was grown to exponential phase (optical density = 30 Klett units), incubated with 0.5 mM IPTG for 4 h at 37°C under aeration, harvested by centrifugation, and washed with phosphate-buffered saline (PBS). Cells (2 × 1010 CFU/ml) were suspended in PBS, and 0.5-ml aliquots were orally delivered using a blunt-tipped feeding needle (Popper & Sons, Inc., New Hide Park, N.Y.) to 4- to 5-week-old female BALB/c mice. Groups of five animals were inoculated weekly with three doses of either live HG3 cells (grown under inducing or noninducing conditions) or purified CFA/I fimbriae (5 μg in PBS); groups were denominated as HG3 and CFA/I, respectively. LT(R192G) (25 μg) was admixed to CFA/I-expressing HG3 cells (HG3/LT group) or purified CFA/I fimbriae (CFA/I+LT group) immediately before oral delivery. The vaccination experiments, based on the same immunization schedule, were independently repeated three times during the course of 1 year using different mice batches and vaccine preparations. Serum samples collected from the retroorbital plexus before immunization and by cardiac puncture 1 week after the last inoculation were kept at −20°C. Intestine homogenates for mucosal immunoglobulin A (IgA) assays were obtained as previously described (2, 15) and stored at −70°C until assayed. Serum IgG and intestinal IgA specific for CFA/I, lipopolysaccharide (LPS), and LT were detected in MaxiSorp plates (Nalge Nunc International, Naperville, Ill.) previously coated with either 0.1 μg of heat-dissociated CFA/I subunits, 0.2 μg of serovar Typhimurium LPS (Sigma), or 0.2 μg of LT(R192G) per well, respectively. After overnight blocking with 1% skim milk in PBS (pH 7.4) at 4°C, serum or intestine homogenates serially diluted in PBS–0.05% Tween 20 were added to the wells and incubated at room temperature for 90 min. Bound antibodies were detected with rabbit anti-mouse IgG or IgA antibodies conjugated to peroxidase (Sigma) diluted in PBS-Tween and developed with o-phenylenediamine (Sigma) and H2O2. Quantification of IgG and IgA levels was performed using standard curves obtained with purified mouse myeloma proteins MOPC 21 (IgG1) and MOPC 315 (IgA) (The Binding Site, Inc., San Diego, Calif.), respectively. IgG subclasses were determined with rabbit anti-mouse IgG1 and IgG2a peroxidase-conjugated antibodies (Southern Biotechnology, Birmingham, Ala.). Endpoint titers of IgG1 and IgG2a antibodies were expressed as the reciprocal of the last dilution giving an absorbance of ≥0.1 above that of samples collected from nonimmunized mice. The ability to block the adhesive properties of intact CFA/I fimbriae expressed by live ETEC cells was determined by IHA carried out with sera collected from vaccinated mice diluted 1:3 in PBS containing 1% d-mannose and ETEC strains 258909-3 and 258909-3M, as previously described (1, 21).
Following cultivation of the HG3 strains in the presence of IPTG, the CFA/I subunit accumulated intracellularly; no homologous protein was detected in the growth medium or in the acellular fraction collected from intact cells submitted to a shearing treatment. On the other hand, sonic disruption followed by differential centrifugation of IPTG-induced HG3 showed that the CFA/I subunit accumulates mainly in the soluble fraction (cytoplasm and periplasm), as revealed in polyacrylamide gels and Western blots developed with CFA/I subunit-specific antibodies (data not shown).
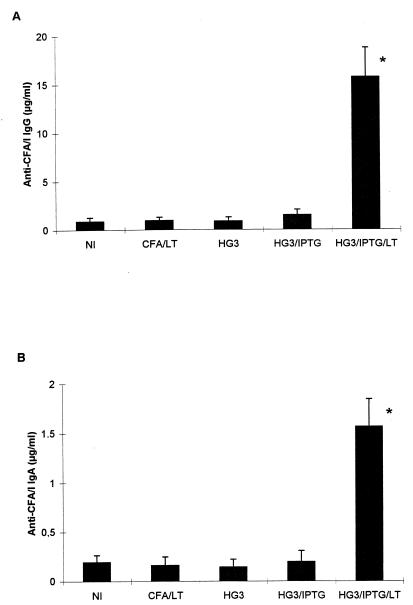
The HG3 groups (three doses of 1010 live cells) showed low CFA/I-specific serum IgG levels (<5 μg/ml) in only 20 to 40% of the vaccinated mice, leading to nonsignificant CFA/I-specific IgG levels in this group serum pools (Fig. 1). On the other hand, HG3/LT groups had positive CFA/I-specific serum IgG antibody responses in all mice (average value of 15 ± 3 μg/ml) (Fig. 1A). The CFA/I+LT group did not elicit significant CFA/I subunit-specific IgG responses, which probably reflects the great lability of the purified antigen in the gastric and intestinal environments (Fig. 2A). Serum pools collected from the HG3/LT groups, but not those harvested from the HG3 groups, were able to inhibit the adhesive properties of intact CFA/I fimbriae expressed by live ETEC cells, as evaluated in IHA tests (data not shown). These results suggest that antibodies raised in mice orally immunized with the HG3 strain expressing the CFA/I subunit in the presence of LT(R192G) were able to properly recognize CFA/I epitopes involved in the receptor binding of intact fimbriae.
FIG. 1.
CFA/I-specific serum IgG (A) and mucosal IgA (B) responses of orally immunized BALB/c mice. Sera and gut homogenates were collected from nonimmunized mice (NI) or mice immunized with three doses of purified CFA/I plus LT(R192G) (CFA/LT), noninduced HG3 cells (HG3), CFA/I-expressing HG3 cells (HG3/IPTG), or CFA/I-expressing HG3 cells plus LT(R192G) (HG3/IPTG/LT). Samples were collected 1 week following the last immunization. Results are reported as the mean ± 1 standard error. The statistical significance (P < 0.05) was determined using the Student's t test and is indicated by an asterisk.
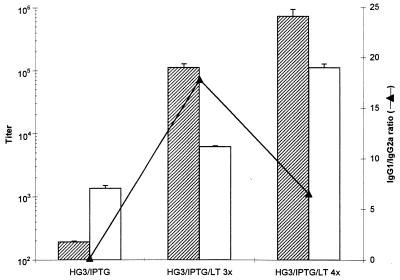
FIG. 2.
CFA/I-specific IgG subclass responses of BALB/c mice orally immunized with the HG3 strain. Dashed bars indicate IgG1 titers, and open bars indicate the IgG2a titers. Determined IgG1/IgG2a ratios are indicated by filled triangles. Mice were immunized with three doses of CFA/I-expressing HG3 cells (HG3/IPTG), three doses of CFA/I-expressing HG3 cells plus LT(R192G) (HG3/IPTG/LT 3×), or four doses of CFA/I-expressing HG3 cells plus LT(R192G) (HG3/IPTG/LT 4×). Results based on immunization carried out with orally administered CFA/I-expressing HG3 cells were based only on mice with a positive response in the IgG-ELISA analyses. Other results were based on pools of serum harvested from the different groups of vaccinated mice. Titers are reported as the means of two independent measurements.
The adjuvant effects of LT(R192G) were also observed in the secreted antibody (IgA) responses elicited by orally delivered CFA/I subunit-expressing HG3 cells. Fewer than 20% of mice from the HG3 groups showed a low CFA/I-specific IgA level in intestine homogenates and nonsignificant values in serum pools (Fig. 1B). In contrast, all mice from the HG3/LT groups exhibited a positive CFA/I-specific IgA response, and serum pool values of 1.6 ± 0.2 μg/ml were detected (Fig. 1B). Similar adjuvant effects promoted by LT(R192G) on the mucosal immune system were observed when the tests were carried out using fecal extracts (data not shown). No significant CFA/I subunit-specific IgA response was detected in three independent experiments using mice orally vaccinated with purified CFA/I fimbriae, irrespective of LT(R192G) addition (Fig. 1B). Therefore, our data demonstrate that purified LT(R192G) can significantly improve the low immunogenicity of the CFA/I subunit expressed by HG3 cells.
Analysis of CFA/I subunit-specific IgG responses showed that IgG1 represented the predominant subclass (IgG1/IgG2a ratios of 18 and 6 in mice immunized with three or four oral doses, respectively) in sera from the HG3/LT group of mice. On the other hand, sera from the HG3 groups (only those with a positive serum response) showed that IgG2a represented the predominant subclass (IgG1/IgG2a ratio of 0.14) (Fig. 2). These results suggest that oral administration of live recombinant Salmonella cells in the presence of LT(R192G) resulted in a Th2-biased immune response, although enhanced levels of both IgG1 and IgG2a subclasses were detected in all vaccinated mice (Fig. 2).
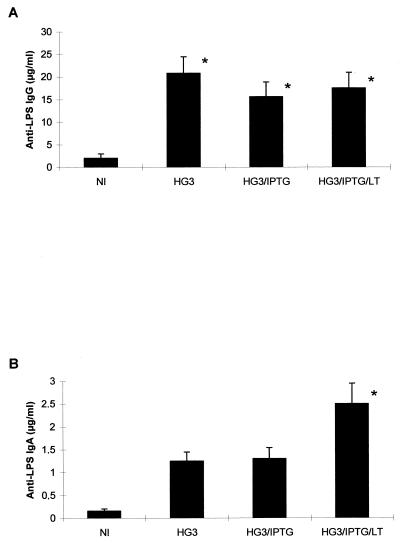
In contrast to the immune responses against the heterologous antigen, coadministration of LT(R192G) did not significantly enhance the serum LPS-specific IgG responses in mice vaccinated with HG3 cells (Fig. 3). On the other hand, coadministration of LT(R192G) enhanced by at least twofold the average anti-LPS IgA response in intestine homogenates of mice orally inoculated with CFA/I-expressing HG3 cells (Fig. 3). These results indicate that orally administered LT(R192G) also enhances the local antibody response against the LPS component of the host Salmonella strain. Finally, all mice orally immunized with LT(R192G)-added vaccine formulations (either live HG3 cells or purified CFA/I) developed LT-specific IgA (intestine homogenates) and IgG (serum) responses (data not shown). These results confirm that, besides the systemic and secreted adjuvant effects toward the heterologous antigen expressed by a live recombinant Salmonella vaccine strain, LT(R192G) behaves as an orally active antigen which can potentially contribute to the generation of a more effective ETEC vaccine.
FIG. 3.
LPS-specific serum IgG (A) and mucosal IgA (B) antibody responses of orally immunized BALB/c mice. Sera and gut homogenates were collected from nonimmunized mice (NI) or mice immunized with three doses of noninduced HG3 cells (HG3), CFA/I-expressing HG3 cells (HG3/IPTG), or CFA/I-expressing HG3 cells plus LT(R192G) (HG3/IPTG/LT). Samples were collected 1 week following the last immunization. Results are reported as mean ± the standard error. Statistical significance (P < 0.05), indicated by an asterisk, was determined using the Student's t test.
In this work we have shown that serum and mucosal antibody responses against a heterologous antigen carried by a recombinant Salmonella strain can be significantly improved by the coadministration of a nontoxic mucosal adjuvant derived from LT. These results show that, besides the reported adjuvant effects toward purified soluble proteins (6, 7, 32, 34), inactivated viruses (20), and killed (3, 25, 34) or attenuated (5, 17, 28) bacterial cells, LT also can be used as an oral adjuvant for passenger antigens expressed by bivalent Salmonella vaccine strains. Although our model system, based on the expression of the CFA/I subunit, was clearly unable to elicit efficient systemic and mucosal antibody responses against the heterologous antigen, the incorporation of the adjuvant to the vaccine formulation resulted in enhanced production of CFA/I subunit-specific antibodies both in the systemic compartment (IgG) and in the intestinal environment (IgA). We believe that the same approach can be applied to other bivalent Salmonella-based vaccine (or any other oral vaccine based on attenuated bacterial cells), thus contributing to the generation of more efficient bivalent vaccine formulations.
The lack of significant anti-CFA/I subunit serum IgG or secreted IgA responses following oral delivery of purified fimbriae coadministered with LT(R192G) probably reflects the lability of the soluble antigens during passage through the gastric and/or intestinal environment, as previously reported (12, 30). Thus, intracellular expression of the CFA/I subunit by live attenuated Salmonella cells seems to reduce antigen degradation and promotes better targeting to GALT inductive sites. The combined use of nontoxic mucosal adjuvants derived from LT and more efficient bivalent Salmonella vaccines, such as those based on in vivo-activated promoters, may also contribute to decreasing the number of doses, the amount of administered cells, and/or induction of tolerance following repeated use. These are possibilities to be tested in the near future.
The precise mechanism operating behind the systemic and mucosal adjuvant effects of LT, as well as CT, is still a matter of debate (4, 6–7, 14, 22–24, 32, 34). Preserved receptor binding function of B subunit and ADP-ribosylating activity of the A1 subunit are important functions to target and activate host cells leading to the immunological properties of both CT and LT (14, 22, 34). The systemic and mucosal adjuvanticity of LT(R192G) toward soluble or particulate antigens, including living Salmonella cells as shown here, indicates that the trypsin-sensitive site of the A subunit represents one of the most interesting targets to reduce toxicity without affecting the immune modulating properties of LT, at least in the murine model. The unique properties of LT(R192G) in regard to other in vitro-engineered LT derivatives represents, therefore, a relevant step toward the development of a safe and efficient oral adjuvant for human use.
Several approaches aimed at the combination of the adjuvant properties of LT or CT and the shuttle functions of attenuated bacterial strains for orally delivered antigens have been previously reported (5, 16–17, 28). For example, attempts to use attenuated Salmonella strains able to express in vivo hybrid CT derivatives, which had the A1 subunit replaced by heterologous peptides, elicited reduced antibody responses against the passenger antigen in vaccinated mice (16). Recently, Ryan and colleagues (28) evaluated the ability of orally delivered attenuated V. cholerae strains transformed with the LT(R192G)-encoding plasmid to act as immunoadjuvant for systemic and secreted antibody responses against coexpressed antigens (28), but the observed enhancement of the antibody responses against the heterologous antigens was meager (28). Compared with these previous experiences, admixing LT(R192G) to the recombinant bacterial strains represents a simpler approach to considerably improve antibody responses both at systemic and at mucosal compartments.
The intracellular expression of the major CFA/I subunit by recombinant serovar Typhimurium cells has some potential advantages, both in quantitative and qualitative aspects, compared to bacterial strains expressing intact fimbriae at the cell surface. First, in contrast to the complex natural regulation of the cfa/I operon, tac-regulated CFA/I expression could be easily standardized. Second, expression of nonpolymerized CFA/I subunits discloses continuous epitopes, not available in intact fimbriae, which give rise to cross-reactive antibodies against several ETEC colonization factors, as PCFO166, CS1, CS4, and CS17 (26–27). A recent report indicates that a minor fimbrial component, the cfaE gene product, is essential for adherence of the CFA/I fimbria (29). It is possible that antibodies raised against specific epitopes located on the major fimbrial subunit inhibit the binding properties of CFA/I by steric hindrance of the fimbrial adhesin residue (1, 26–27). The finding that sera from mice of the HG3/LT group inhibit the heamagglutination promoted by ETEC cells further supports the importance of using the CFA/I subunit (CfaB protein) as a component of an anticolonization ETEC vaccine.
Determination of CFA/I-specific serum IgG subclass responses in mice orally immunized with the Salmonella vaccine strain and LT(R192G) revealed a mixed Th1-Th2 immune response, with a predominance of the Th2 type, as evaluated by the induced IgG1/IgG2a ratios. On the other hand, the HG3 group yielded a predominant Th1-type pattern, supporting previous observations based on the pattern of produced cytokines (33). These results suggest that LT(R192G) may quantitatively and qualitatively affect the induced antibody responses against an heterologous antigen carried by a live bivalent Salmonella strain, favoring a Th2-type response which leads to enhanced production of IgG1 and IgA. A clear definition of the immune modulation activities of LT(R192G) on heterologous antigens expressed by live Salmonella cells will require the determination of the specific cytokine profile produced by lymphocytes specifically stimulated by the passenger antigen.
Acknowledgments
We are grateful to Maria Friberg, Celeste Chong, Eduardo Camacho, and Celso Pereira for invaluable suggestions and/or technical assistance and Marcio O. Lásaro for the preparation of figures.
This work was supported by FINEP, FAPERJ, and PADCT grants (Brazil) and an Office of Naval Research grant (United States).
REFERENCES
- 1.Bühler T, Hoschützky H, Jann K. Analysis of colonization factor antigen I, an adhesin of enterotoxigenic Escherichia coli O78:H11: fimbrial morphology and location of the receptor-binding site. Infect Immun. 1991;59:3876–3882. doi: 10.1128/iai.59.11.3876-3882.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cárdenas L, Dasgupta U, Clements J D. Influence of strain viability and antigen dose on the use of attenuated mutants of Salmonella as vaccine carriers. Vaccine. 1994;12:833–840. doi: 10.1016/0264-410x(94)90293-3. [DOI] [PubMed] [Google Scholar]
- 3.Chong C, Friberg M, Clements J D. LT(R192G), a non-toxic mutant of the heat-labile enterotoxin of Escherichia coli, elicits enhanced humoral and cellular immune responses associated with protection against lethal oral challenge with Salmonella spp. Vaccine. 1998;16:732–740. doi: 10.1016/s0264-410x(97)00255-7. [DOI] [PubMed] [Google Scholar]
- 4.Clements J D, Hartzog N M, Lyon F L. Adjuvant activity of Escherichia coli heat-labile enterotoxin and effect on the induction of oral tolerance in mice to unrelated protein antigens. Vaccine. 1988;6:269–277. doi: 10.1016/0264-410x(88)90223-x. [DOI] [PubMed] [Google Scholar]
- 5.Covone M G, Brocchi M, Palla E, da Silveira W D, Rappuoli R, Galeotti C L. Levels of expression and immunogenicity of attenuated Salmonella enterica serovar Typhimurium strains expressing Escherichia coli heat-labile enterotoxin. Infect Immun. 1998;66:224–231. doi: 10.1128/iai.66.1.224-231.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dickinson B L, Clements J D. Dissociation of Escherichia coli heat-labile enterotoxin adjuvanticity from ADP-ribosyltransferase activity. Infect Immun. 1995;63:1617–1623. doi: 10.1128/iai.63.5.1617-1623.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dickinson B L, Clements J D. Use of Escherichia coli heat-labile enterotoxin as an oral adjuvant. In: Kiyono H, Ogra P L, McGhee J R, editors. Mucosal vaccines. San Diego, Calif: Academic Press; 1996. pp. 73–87. [Google Scholar]
- 8.Doggett T A, Brown P K. Attenuated Salmonella as vector for oral immunization. In: Kiyono H, Ogra P L, McGhee J R, editors. Mucosal vaccines. San Diego, Calif: Academic Press; 1996. pp. 105–118. [Google Scholar]
- 9.Douce G, Turcotte C, Cropley I, Roberts M, Pizza M, Domenghini M, Rapuoli R, Dougan G. Mutants of Escherichia coli heat-labile toxin lacking ADP-ribosyltransferase activity act as nontoxic, mucosal adjuvants. Proc Natl Acad Sci USA. 1995;92:1644–1648. doi: 10.1073/pnas.92.5.1644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Elson C O. Cholera toxin and its subunits as potential oral adjuvants. Immunol Today. 1989;146:29–33. doi: 10.1007/978-3-642-74529-4_3. [DOI] [PubMed] [Google Scholar]
- 11.Evans D G, Evans D J, Jr, Clegg S, Pauley J A. Purification and characterization of the CFA/I antigen of enterotoxigenic Escherichia coli. Infect Immun. 1979;25:738–748. doi: 10.1128/iai.25.2.738-748.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Evans D G, Graham D Y, Evans D J, Jr, Opekun A. Administration of purified colonization factor antigens (CFA/I, CFA/II) of enterotoxigenic Escherichia coli to volunteers. Gastroenterology. 1984;87:934–940. [PubMed] [Google Scholar]
- 13.Gothefors L, Åhren C, Stoll B, Barua D K, Ørskov F, Salek M A, Svennerholm A-M. Presence of colonization factor antigens on fresh isolates of fecal Escherichia coli: a prospective study. J Infect Dis. 1995;152:1128–1133. doi: 10.1093/infdis/152.6.1128. [DOI] [PubMed] [Google Scholar]
- 14.Guidry J J, Cárdenas L, Cheng E, Clements J D. Role of receptor binding in toxicity, immunogenicity, and adjuvanticity of Escherichia coli heat-labile enterotoxin. Infect Immun. 1997;65:4943–4950. doi: 10.1128/iai.65.12.4943-4950.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guillobel H C R, Luna M G, Camacho E F, de Almeida D F, Ferreira L C S. Immunization against the colonization factor antigen I of enterotoxigenic Escherichia coli by administration of a bivalent Salmonella typhimurium aroA strain. Braz J Med Biol Res. 1998;31:545–555. doi: 10.1590/s0100-879x1998000400012. [DOI] [PubMed] [Google Scholar]
- 16.Harokopakis E, Hajishengallis G, Greenway T E, Russel M W, Michalek S M. Mucosal immunogenicity of a recombinant Salmonella typhimurium cloned heterologous antigen in the absence or presence of coexpressed cholera toxin A2 and B subunits. Infect Immun. 1997;65:1445–1454. doi: 10.1128/iai.65.4.1445-1454.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hartman A B, van de Verg L L, Venkatesan M M. Native and mutant forms of cholera toxin and heat-labile enterotoxin effectively enhance protective efficacy of live attenuated and heat-killed Shigella vaccines. Infect Immun. 1999;67:5841–5847. doi: 10.1128/iai.67.11.5841-5847.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hoiseth S D, Stocker B A D. Aromatic-dependent Salmonella typhimurium are non-virulent and effective as live vaccines. Nature. 1981;291:238–239. doi: 10.1038/291238a0. [DOI] [PubMed] [Google Scholar]
- 19.Karjalainen T K, Evans D G, So M, Lee C H. Molecular cloning and nucleotide sequence of the colonization factor antigen I gene of Escherichia coli. Infect Immun. 1989;57:1126–1130. doi: 10.1128/iai.57.4.1126-1130.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Katz J M, Lu X, Young S A, Galphin J C. Adjuvant activity of the heat-labile enterotoxin from enterotoxigenic Escherichia coli for oral administration of inactivated influenza virus vaccine. J Infect Dis. 1997;175:352–363. doi: 10.1093/infdis/175.2.352. [DOI] [PubMed] [Google Scholar]
- 21.Luna M G, Martins M M, Newton S M C, Costa S O P, de Almeida D F, Ferreira L C S. Cloning and expression of colonization factor antigen I (CFA/I) epitopes of enterotoxigenic Escherichia coli (ETEC) in Salmonella flagellin. Res Microbiol. 1997;148:217–228. doi: 10.1016/S0923-2508(97)85242-4. [DOI] [PubMed] [Google Scholar]
- 22.Lycke N. The mechanism of cholera toxin adjuvanticity. Res Immunol. 1997;148:504–520. doi: 10.1016/s0923-2494(98)80144-2. [DOI] [PubMed] [Google Scholar]
- 23.Lycke N, Karlsson U, Sjolander A, Magnusson K E. The adjuvant action of cholera toxin is associated with an increased intestinal permeability for luminal antigens. Scand J Immunol. 1991;33:691–698. doi: 10.1111/j.1365-3083.1991.tb02542.x. [DOI] [PubMed] [Google Scholar]
- 24.Lycke N, Tsuji T, Holmgren J. The adjuvant effect of Vibrio cholerae and Escherichia coli heat-labile enterotoxins is linked to their ADP-ribosyltransferase activity. Eur J Immunol. 1992;22:2277–2281. doi: 10.1002/eji.1830220915. [DOI] [PubMed] [Google Scholar]
- 25.Rollwagen F M, Pacheco N D, Clements J D, Pavlovskis O, Rollins D M, Walker R I. Killed Campylobacter elicits immune response and protection when administered with an oral adjuvant. Vaccine. 1993;11:1316–1320. doi: 10.1016/0264-410x(93)90101-3. [DOI] [PubMed] [Google Scholar]
- 26.Rudin A, Olbe L, Svennerholm A-M. Monoclonal antibodies against fimbrial subunits of colonization factor antigen I (CFA/I) inhibit binding to human enterocytes and protect against enterotoxigenic Escherichia coli expressing heterologous colonization factors. Microb Pathog. 1996;20:35–45. doi: 10.1006/mpat.1996.0040. [DOI] [PubMed] [Google Scholar]
- 27.Rudin A, Svennerholm A-M. Identification of a cross-reactive continuous B-cell epitope in enterotoxigenic Escherichia coli colonization factor antigen I. Infect Immun. 1996;64:4508–4513. doi: 10.1128/iai.64.11.4508-4513.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ryan E T, Crean T I, John M, Butterton J R, Clements J D, Calderwood S B. In vivo expression and immunoadjuvancy of a mutant of heat-labile enterotoxin of Escherichia coli in vaccine and vector strains of Vibrio cholerae. Infect Immun. 1999;67:1694–1701. doi: 10.1128/iai.67.4.1694-1701.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sakellaris H, Murson G P, Scott J R. A conserved residue in the tip proteins of CS1 and CFA/I pili of enterotoxigenic Escherichia coli that is essential for adherence. Proc Natl Acad Sci USA. 1999;96:12828–12832. doi: 10.1073/pnas.96.22.12828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schmidt M, Kelley E P, Tseng L Y, Boedecker E C. Towards an oral E. coli pilus vaccine for traveller's diarrhea: susceptibility to proteolytic digestion. Gastroenterology. 1985;82:1575. [Google Scholar]
- 31.Snider D P, Marshall J S, Pardue M H, Liang H. Production of IgE antibody and allergic sensitization of intestinal and peripheral tissues after oral immunization with protein Ag and cholera toxin. J Immunol. 1994;153:647–653. [PubMed] [Google Scholar]
- 32.Takahashi M, Marinaro M, Kiyono H, Jackson R J, Nakagawa I, Fijihashi K, Hamada S, Clements J D, Bost K L, McGhee J R. Mechanisms for mucosal immunogenicity and adjuvancy of Escherichia coli labile enterotoxin. J Infect Dis. 1996;173:627–635. doi: 10.1093/infdis/173.3.627. [DOI] [PubMed] [Google Scholar]
- 33.VanCott J L, Staats H F, Pascual D W, Roberts M, Chatfield S N, Yamamoto M, Coste M, Carter P B, Kiyono H, McGhee J R. Regulation of mucosal and systemic antibody responses by T helper cell subsets, macrophages, and derived cytokines following oral immunization with live recombinant Salmonella. J Immunol. 1996;156:1504–1514. [PubMed] [Google Scholar]
- 34.Walker R, Clements J D. Use of heat-labile toxin of enterotoxigenic Escherichia coli to facilitate mucosal immunization. Vaccine Res. 1993;2:1–10. [Google Scholar]