Abstract
Background:
Recreational cannabis legalization has become more prevalent over the past decade, increasing the need to understand its impact on downstream health-related outcomes. Although prior reviews have broadly summarized research on cannabis liberalization policies (including decriminalization and medical legalization), directed efforts are needed to synthesize the more recent research that focuses on recreational cannabis legalization specifically. Thus, the current review summarizes existing studies using longitudinal designs to evaluate impacts of recreational cannabis legalization on cannabis use and related outcomes.
Method:
A comprehensive bibliographic search strategy revealed 61 studies published from 2016 to 2022 that met criteria for inclusion. The studies were predominantly from the United States (66.2%) and primarily utilized self-report data (for cannabis use and attitudes) or administrative data (for health-related, driving, and crime outcomes).
Results:
Five main categories of outcomes were identified through the review: cannabis and other substance use, attitudes toward cannabis, health-care utilization, driving-related outcomes, and crime-related outcomes. The extant literature revealed mixed findings, including some evidence of negative consequences of legalization (such as increased young adult use, cannabis-related healthcare visits, and impaired driving) and some evidence for minimal impacts (such as little change in adolescent cannabis use rates, substance use rates, and mixed evidence for changes in cannabis-related attitudes).
Conclusions:
Overall, the existing literature reveals a number of negative consequences of legalization, although the findings are mixed and generally do not suggest large magnitude short-term impacts. The review highlights the need for more systematic investigation, particularly across a greater diversity of geographic regions.
Keywords: Cannabis, marijuana, legalization, attitudes, health, crime, driving
Introduction
Cannabis is one of the most widely used substances globally, with nearly 2.5% of the world population reporting past year cannabis use. 1 Cannabis use rates are particularly high in North America. In the U.S., 45% of individuals reported ever using cannabis and 18% reported using at least once annually in 2019.2,3 In Canada, approximately 21% of people reported cannabis use in the past year use in 2019. 4 In terms of cannabis use disorder (CUD), a psychiatric disorder defined by clinically significant impairment in daily life due to cannabis use, 5 ~5.1% of the U.S. population ages 12+ years met criteria in 2020, with ~13.5% of individuals ages 18 to 25 years meeting criteria. 6
Overall, rates of cannabis use have shown long-term increasing trends among several age groups in North America.7-9 Moreover, research has revealed recent cannabis use increases in at risk populations, such as individuals with depression and pregnant women.10,11 Parallel to increased cannabis use over time, rates of cannabis-related consequences have also increased across Canada and the U.S., including cannabis dependence and CUD,8,12 crime rates (eg, increased possession charges), 8 and cannabis-impaired driving (and, lower perception of impairment and risk from cannabis use).11,13,14 Further, cannabis use poses a risk for early-onset or use during adolescence as there is evidence that cannabis use in adolescence is linked with poorer cognitive performance, psychotic disorders, and increased risk of mood and addictive disorders. 15 With the rates of negative consequences from cannabis use increasing, particularly in North America where cannabis has become legal in many parts of the US and all of Canada, understanding the role of cannabis legalization in these changes is crucial to inform ongoing changes in cannabis policies worldwide.
The legal status of cannabis varies widely across countries and regions. Although cannabis is largely illegal at the global level, policies surrounding cannabis use are becoming steadily liberalized. Decriminalization (reduced penalties for self-use but not distribution) is more widespread worldwide, including in the Netherlands, Portugal, and parts of Australia. Medical legalization is also seen in Peru, Germany, New Zealand, the Netherlands and across many U.S. states. To date, Canada, Uruguay, and Malta are the only 3 countries to legalize recreational cannabis use at the national level. Further, individual U.S. states began legalizing recreational cannabis in 2012, with nearly half of U.S. states having legalized recreational cannabis by 2023. As national and subnational recreational legalization continues to gain support and take effect, understanding the consequences of such major regulatory changes is crucial to informing ongoing policy changes.
There are arguments both for and against recreational cannabis legalization (RCL). Common pro-legalization arguments involve increasing regulatory control over product distribution, weakening organized crime, reducing burden and inequality in the criminal justice system, and generating economic benefits such as tax revenues and commercial activity. 16 Furthermore, as cannabis obtained from illicit markets is of varying and unknown potency, 17 cannabis legalization may help better regulate the potency and quality of cannabis products. 18 On the other hand, there are anti-legalization arguments such as the possibility of legalization leading to increased use among youth and increased cannabis-impaired driving. 16 A nationally representative survey in the U.S. found that pro-legalization arguments were perceived to be more persuasive than public health anti-legalization arguments in a U.S. nationally representative survey, 19 suggesting policymaker concerns regarding RCL do not seem to hold as much weight in the general public. However, while research may be increasing surrounding the impacts of RCL, the general consensus of if RCL leads to more positive or negative consequences is unclear.
With RCL becoming more prevalent globally, the impacts it may have on a variety of health-related outcomes are of critical importance. Prevalence of cannabis use is of course a relevant issue, with many concerned that RCL will cause significant spikes in rates of cannabis use for a variety of groups, including youth. However, current studies have revealed mixed evidence in the U.S.,20,21 thus there is a need to synthesize the extant literature to better understand the balance of evidence and potential impacts of RCL across different samples and more diverse geographic areas. Another common question about RCL is whether it will result in changes in attitudes toward cannabis. These changes are of interest as they might forecast changes in consumption or adverse consequences. Similarly, there are concerns surrounding RCL and potential spill-over effects that may influence rates of alcohol and other substance use. 22 Thus, there remains a need to examine any changes in use of other substance use when studying effects of RCL.
Beyond changes in cannabis and other substance use and attitudes, health-related impacts of RCL are important to consider as there are links between cannabis use and adverse physical and mental health consequences (eg, respiratory and cardiovascular diseases, psychosis). 23 Additionally, emergency service utilization associated with cannabis consumption is a frequent concern associated with RCL, particularly due to the spikes in admissions following RCL in Colorado. 24 However, the rates of cannabis-related emergency service admissions more globally (eg, in legal countries like Canada and Uruguay) have not been fully integrated into summaries of the current literature. Finally, another health-related consequence of RCL is potential impacts on opioid use. While opioid-related outcomes can fall into substance use, they are considered health-related for this review as much of the discussion surrounding RCL and opioids involve cannabis substituting opioid use for medicinal reasons or using cannabis as an alternate to prescription opioids in the healthcare system. The current opioid crisis is a global public health problem with serious consequences. While there is evidence that medicinal cannabis may reduce prescription opioid use 25 and that cannabis may be a substitute for opioid use, 26 the role of recreational cannabis legalization should also be examined as the 2 forms of cannabis use are not interchangable 27 and have shown unique associations with prescription drug use. 28 Thus, there is a need to better understand how and if RCL has protective or negative consequences on opioid-related outcomes.
Due to the impairing effects of cannabis on driving abilities and the relationship with motor vehicle accidents, 29 another important question surrounding RCL is how these policy changes could result in adverse driving-related outcomes. An understanding of how RCL could influence impaired driving prevalence is needed to give insight into how much emphasis jurisdictions should put on impaired driving rates when considering RCL implementation. A final consequence of RCL that is often debated but requires a deeper understanding is how it impacts cannabis-related arrest rates. Cannabis-related arrests currently pose a significant burden on the U.S. and Canadian justice system.30,31 Theoretically, RCL may ease the strain seen on the justice system and have positive trickle-down effects on criminal-related infrastructure. However, the overall implications of RCL on arrest rates is not well understood and requires a systematic evaluation. With the large number of RCL associated outcomes there remains a need to synthesize the current evidence surrounding how RCL can impact cannabis use and other relevant outcomes
Present review
Currently, no reviews have systematically evaluated how RCL is associated with cannabis-use changes across a variety of age groups as well as implications on other person- or health-related outcomes. The present review aims to fill an important gap in the literature by summarizing the burgeoning research examining a broad range of consequences of RCL across the various jurisdictions that have implemented RCL to date. Although previous reviews have considered the implications of RCL,32,33 there has recently been a dramatic increase in studies in response to more recent changes in recreational cannabis use policies, requiring additional efforts to synthesize the latest research. Further, many reviews focus on specific outcomes (eg, parenting, 34 adolescent use 35 ). There remains a need to systematically summarize how RCL has impacted a variety of health-related outcomes to develop a more comprehensive understanding of the more negative and positive outcomes of RCL. While a few reviews have examined a broad range of outcomes such as cannabis use, related problems, and public health implications,32,33 some reviews have been limited to studies from a single country or published in a narrow time window. 32 Thus, a broader review is necessary to examine multiple types of outcomes from studies in various geographic regions. Additionally, a substantial amount of the current literature examining the impact of RCL relies on cross-sectional designs (eg, comparing across jurisdictions with vs without recreational legalization) which severely limit any conclusions about causal associations. Thus, given its breadth, the current systematic review is more methodologically selective by including only studies with more rigorous designs (such as longitudinal cohort studies), which provide stronger evidence regarding the effects of RCL. In sum, the aim of the current review was to characterize the health-related impacts of RCL, including changes in these outcomes in either a positive or negative direction.
Method
The review is compliant with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA 36 ). Full-text extraction was initiated immediately following article search, therefore the protocol was not registered with PROSPERO. Relevant articles on cannabis legalization were principally identified using the Boolean search terms (“cannabis” OR “marijuana” OR “THC” OR “marihuana”) AND “legalization” AND (“recreational” OR “non-medical” OR “nonmedical”) AND (“longitudinal” OR “pre-post” OR “prospective” OR “timeseries” OR “cohort”). The search was conducted using PubMed/MEDLINE, EMBASE, and PsycINFO through November 2022. Relevant studies identified through secondary means (eg, prior knowledge of a relevant publication, articles brought to the authors’ attention) were also included for screening. Titles and abstracts resulting from the initial search were screened in Covidence (Veritas Health Innovation Inc) by 2 reviewers for suitability for full-text review and final inclusion. Conflicts were discussed by both reviewers and a final decision was made by consensus. Following screening, reviewers read and extracted relevant data. To be included, an article was required to meet the following criteria: (i) an original empirical research article published in a peer-reviewed journal; (ii) written in (or available in) English; (iii) RCL serves as an independent variable; (iv) quantitative study design that clearly permitted the evaluation of the role of RCL with a more rigorous non-cross-sectional study design (eg, pre- vs post-legalization, longitudinal, cohort, interrupted time series, etc.); and (v) reports on health-related outcomes (ie, changes in consumption or attitudes, as opposed to changes in price or potency).
RCL related outcomes that were considered were those specifically involving the behavior, perceptions, and health of individuals. Population-level outcomes (eg, health-care utilization or impaired driving) were considered eligible for inclusion as they involve the impacts that legalization has on individual behavior. Thus, economic- or product-level outcomes that do not involve individual behavior (eg, cannabis prices over time, changes in cannabis strain potency) were considered out of scope. The outcome groups were not decided ahead of time and instead 5 main themes in outcomes emerged from our search and were organized into categories for ease of presentation due to the large number of studies included.
Studies that examined medicinal cannabis legalization or decriminalization without recreational legalization, and studies using exclusively a cross-sectional design were excluded as they were outside the scope of the current review. The study also excluded articles that classified RCL as the passing of legal sales rather than implementation of RCL itself as RCL is often distinct from introduction of legal sales, or commercialization. Thus, we excluded studies examining commercialization as they were outside the scope of the current review.
Results
Characteristics of the literature
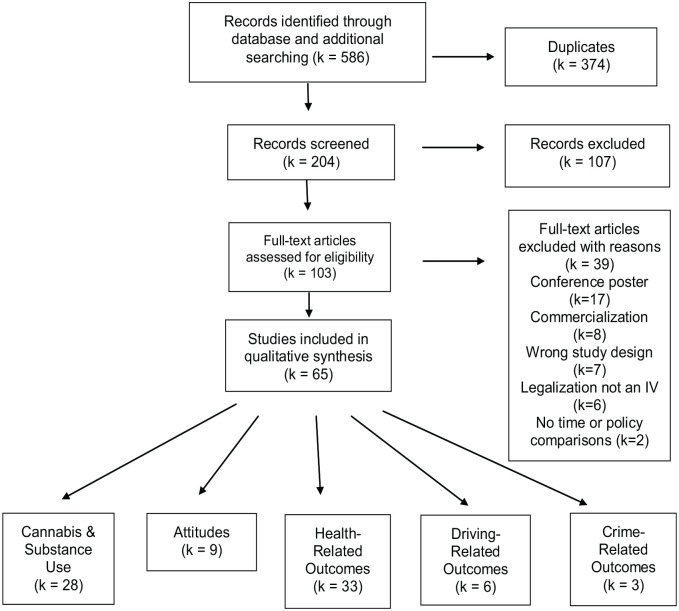
The search revealed 65 relevant articles examining RCL and related outcomes (see Figure 1). There were 5 main themes established: cannabis use and other substance use behaviors (k = 28), attitudes toward cannabis (k = 9), health-related outcomes (k = 33), driving related impacts (k = 6), and crime-related outcomes (k = 3). Studies with overlapping themes were included in all appropriate sections. Most studies (66.2%) involved a U.S. sample, 32.3% examined outcomes in Canada, and 1.5% came from Uruguay. Regarding study design, the majority (46.2%) utilized archival administrative data (ie, hospital/health information across multiple time points in one jurisdiction) followed by cohort studies (18.5%). The use of administrative data was primarily used in studies examining health-related outcomes, such as emergency department utilization. Studies examining cannabis use or attitudes over time predominantly used survey data. Finally, both driving and crime related outcome studies primarily reported findings with administrative data.
Figure 1.
Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) study flow diagram.
Changes in cannabis and other substance use
Cannabis and other substance use changes represented the second largest number of studies, with 28 articles identified. Studies examining changes in cannabis use behaviors were divided by subpopulation (ie, adolescents, young adults, general population adults, clinical populations, and maternal use; see Table 1). Finally, we separately summarized studies reporting changes in concurrent use of other substances, and routes of cannabis administration.
Table 1.
Studies investigating the role of recreational cannabis legalization on cannabis and other substance consumption.
| Author | Year | Location | Date of legalization | Study design | Sample | Brief findings |
|---|---|---|---|---|---|---|
| Cannabis use in adolescents | ||||||
| Duan et al | 2022 | U.S. | Longitudinal | N = 19 503 | In states with RCL adolescents who never used cannabis but used e-cigarettes were more likely to use cannabis than those living in states without recreational cannabis legalization. | |
| Estoup et al | 2016 | Washington | 2012 | Cohort | N = 262 | Cannabis-related consequences significantly increased following RCL. There was not a significant effect of frequency of cannabis use. |
| Gunadi et al | 2022 | U.S. | 2016 | Longitudinal | N = 21 863 | Significant association between RCL and transition from non-users to cannabis users when compared to states with no medical or recreational cannabis legalization and states with no legalization combined with those with medical cannabis legalization, but not when compared to states with medical cannabis legalization only. |
| Mason et al | 2016 | Washington | 2012 | Cohort | N = 238 | RCL cohort had increased cannabis use at follow-up compared to pre-RCL, but this increase was not significant. There were positive, but not significant, cohort effects for cannabis use. |
| Paschall et al | 2022 | California | 2016 | Repeated cross-sectional | N = 3 319 329 | Adolescent alcohol and cannabis co-users had a significant increase in the frequency of past 30-day cannabis use following RCL. |
| Rusby et al | 2018 | Oregon | 2015 | Cohort | N = 444 | RCL cohort was more likely to increase their intent to use cannabis overtime, while the pre-RCL cohort was less likely to increase willingness and intent to use. RCL was not associated with initiating cannabis use. The RCL cohort did have significant increases in cannabis use compared to pre-RCL. |
| Stormshak et al | 2019 | U.S. | Cohort | N = 1438 | Post-RCL cohort had higher odds of cannabis use compared to the pre-RCL cohort over time. Use decreased over time for pre-RCL but increased post-RCL. However, patterns of use were similar in cohorts. | |
| Vignault et al | 2021 | Quebec | 2018 | Archival administrative data | N = 2615 | No significant increase in the frequency of or prevalence of cannabis use following RCL. |
| Yu et al | 2020 | U.S. | Cohort | N = 749 152 | RCL was not significantly associated with period effects for cannabis use, but medical legalization was. | |
| Zuckermann et al | 2021 | Canada | 2018 | Repeated cross-sectional | N = 102 685 | Adolescents had increased odds of ever using cannabis in the year following RCL in the cross-sectional data 28 . However, the longitudinal sample revealed no significant differences in the odds of ever use, current use, and regular use of cannabis post-RCL. |
| Cannabis use in young adults | ||||||
| Bailey et al | 2020 | Washington | 2012 | Longitudinal | N = 281 | RCL predicted a higher likelihood of past-year cannabis use. |
| Barker & Moreno | 2021 | Washington & Wisconsin | 2012 | Longitudinal cohort | N = 338 | Significant association between RCL and increased cannabis use. The rate of students ever using cannabis did not change, however, in those who had used cannabis prior to RCL, the proportion of students using in the past 28-days increased faster following RCL in Washington (legal-state) when compared with the rate of increase in Wisconsin (non-legal state). |
| Han & Seo | 2022 | U.S. | Longitudinal cohort | N = 6155 | In a sample of young adults who had never vaped cannabis at the time of recruitment results revealed that cannabis use in the past year did not differ in states with or without RCL, although, those living in states with RCL did show a larger increase in rates of cannabis vaping across time, compared to those in non-RCL states. | |
| Kerr et al | 2017 | Oregon | 2015 | Repeated cross-sectional | N = 10 924 | Rates of cannabis use significantly increased following RCL but use also increased over time in non-legal states. Oregon students with heavy alcohol use had greater increases in recent use. Among heavy drinker’s RCL had a greater impact on cannabis use for minors. No support that first year students experience a greater effect of RCL on use. RCL was not associated with changes in cigarette and alcohol use. |
| Cannabis use in adults | ||||||
| Gali et al | 2021 | California | 2016 | Longitudinal cohort | N = 429 | Past 30-day cannabis use increased significantly 1-month post-RCL and remained elevated 6-months post-RCL. |
| Gunadi et al | 2022 | U.S. | 2016 | Longitudinal cohort | N = 21, 863 | In adults, there was an association between legalization and transition from non-users to cannabis users and non-users to weekly users when compared to states with no medical or recreational cannabis legalization and states with no legalization combined with those with medical cannabis legalization. |
| Kerr et al | 2018 | U.S. | 2018 | Repeated cross-sectional | N = 37 359 | There was a non-significant increase in cannabis use post-RCL. Rates of simultaneous cannabis and alcohol use did not increase with RCL. Comparison studies found evidence of some increase in cannabis use 12 months after RCL. Past year cannabis use rates started increasing prior to RCL. |
| Turna et al | 2021 | Ontario | 2018 | Longitudinal | N = 1502 | For non-users prior to RCL, there were significant increases in cannabis use frequency, quantity of cannabis used, and severity of cannabis misuse following RCL. The opposite pattern was seen for those reporting cannabis use prior to RCL, with significant decreases in frequency of use, quantity, and misuse. |
| Vignault et al | 2021 | Quebec | 2018 | Archival administrative data | N = 2615 | No significant increase in the frequency of or prevalence of cannabis use following RCL. |
| Cannabis use in clinical populations | ||||||
| Geoffrion et al | 2021 | British Columbia | 2018 | Archival administrative data | N = 3705 | Cannabis use rates increased from pre- to post-RCL for women with pelvic pain. |
| Grigorian et al | 2019 | California | 2016 | Archival administrative data | N = 21 173 | The rate of adult positive THC screens increased post-RCL. Pediatric positive THC screens were non-significant. |
| Hawke & Henderson | 2021 | Ontario | 2018 | Cohort | N = 269 | In a sample of youth in an outpatient addictions treatment program, there was no change in the rate of cannabis use following RCL. |
| Hawley et al | 2019 | British Columbia | 2018 | Repeated cross-sectional | N = 1673 | There was a significant increase in the prevalence of current cannabis use after RCL among cancer patients. |
| Pusateri et al | 2022 | Colorado & Washington | 2012 | Archival administrative data | N = 18 545 | There was a significant increase of irritable bowel disease patients reporting cannabis use post-RCL. |
| Rosic et al | 2021 | Ontario | 2018 | Repeated cross-sectional | N = 1390 | In individuals receiving treatment for opioid use disorder, cannabis use was compared for those recruited 6 months before or after RCL with no significant changes in the prevalence or frequency of self-reported or urine screen-detected cannabis use following RCL. |
| Maternal cannabis use | ||||||
| Grant et al | 2018 | Washington | 2012 | Cohort | N = 1359 | Increases in cannabis use in mothers who used substances during pregnancy at treatment exit post-RCL. Post-RCL cohort more likely to report cannabis use 30 days following exit compared to pre-RCL-cohort. Post-RCL cohort also less likely to quit cannabis use and more likely to have used from enrollment to exit. Post-RCL cohort who initiated use during treatment used about 3x more than Pre-RCL cohort. |
| Lee et al | 2022 | California | 2016 | Cohort | N = 466 | Urine screen-detected cannabis use during pregnancy increased from 6% to 11% following RCL. |
| Yee et al | 2021 | U.S. | Cohort | N = 2926 | No significant difference in cannabis or alcohol use associated with RCL in women living with HIV during pregnancy or the postpartum period. | |
| Other substance use | ||||||
| Bailey et al | 2020 | Washington | 2012 | Longitudinal | N = 281 | RCL predicted a higher likelihood of alcohol use. RCL was not significantly associated with past-year cigarette use. |
| Grigorian et al | 2019 | California | 2016 | Archival administrative data | N = 21 173 | There was no difference for alcohol and other drug screens in adults post-RCL. Post-RCL there was increased rate of benzodiazepine and barbiturate screens for pediatrics. |
| Hawke & Henderson | 2021 | Ontario | 2018 | Cohort | N = 269 | No significant effect of RCL on rates of alcohol or illicit drug use. |
| Kerr et al | 2017 | Oregon | 2015 | Repeated cross-sectional | N = 10 924 | Among heavy drinker’s RCL had a greater impact on cannabis use for minors. RCL was not associated with changes in cigarette and alcohol use. |
| Mason et al | 2016 | Washington | 2012 | Cohort | N = 238 | The pre-RCL cohort had higher past month cigarette use at follow-up compared to the RCL cohort. Alcohol use was also greater for the pre-RCL cohort but not significantly. There were negative and significant cohort effects for alcohol and cigarette use. |
| Paschall et al | 2022 | California | 2016 | Repeated cross-sectional | N = 3 319 329 | Among 7th, 9th, and 11th grade students in the U.S., RCL was associated with a 6% increase in the odds of past 30-day alcohol and cannabis co-use. The association was even stronger in students with past 30-day alcohol use and heavy drinking. However, among past 30-day cannabis users, RCL was associated with a 24% reduction in co-use. |
| Route of administration | ||||||
| Gali et al | 2021 | California | 2016 | Longitudinal cohort | N = 429 | Smoking, vaping, and edibles (in that order) were the most frequent modes of cannabis use pre- and post-RCL. The least common mode of cannabis use was blunts, which declined following RCL. |
| Zuckerman et al | 2021 | Canada | 2018 | Cohort | N = 2953 | Changes in the number of different modes of cannabis use reported by high school students showed that 31.3% of students maintained a single mode of use, 14.3% maintained multiple modes of use, 42.3% expanded and 12.1% reduced their modes of use pre- and post-RCL. |
Author, author of article; Year, publication year of article; Location, jurisdiction article data was collected in; Date of Legalization, year legalization was enacted in jurisdiction; Sample, total N of article sample; RCL, Recreational Cannabis Legalization.
Cannabis use changes in adolescents (~12-17)
Ten studies examined changes in cannabis use among adolescents and found that changes in the rates of use were inconsistent following RCL. Gunadi et al 37 found an association between RCL and more pronounced transition from non-use to cannabis use when compared to states with no legalization and those with medical cannabis legalization (P ⩽ .001) combined, but not when compared to states with medical cannabis legalization only. Another study found that in states with RCL adolescents who never used cannabis but used e-cigarettes were more likely to use cannabis at follow-up than those living in states without RCL (aOR = 18.39, 95% CI: 4.25-79.68vs aOR = 5.09, 95% CI: 2.86-9.07, respectively) suggesting a risk of cannabis initiation among legal states. 38 Among adolescents reporting recent alcohol and cannabis co-use, one study found a significant increase in the frequency of past 30-day cannabis use following RCL (b = 0.36, SE = 0.07, P ⩽ .001). 39 In a Canadian study using a repeated cross-sectional design as well as a longitudinal design to examine changes in cannabis use, results revealed that adolescents had increased odds of ever using cannabis in the year following RCL in the cross-sectional data (P = .009). 40 However, the longitudinal sample revealed no significant differences in the odds of ever use, current use, and regular use of cannabis post-legalization. There is also evidence of RCL impacts on adolescent cannabis use consequences, as a Washington study found a significant indirect effect of RCL on cannabis consequences through perceived risk as a mediator (B = 0.37, P ⩽ .001). 41
On top of the above evidence, there were multiple studies examining cannabis use changes over time among adolescents in Washington and Oregon that found higher rates of cannabis use associated with cohorts examined during RCL compared to non-legal cohorts,42-44 although the differences across legal cohorts were not significant in all cases. 42 Furthermore, in another study, RCL did not impact initiation of use, but for current users the RCL group had significantly greater increased rates of cannabis use compared to the pre-RCL group (RR = 1.26, 95% CI = 1.10, 1.45). 43 For the final study, cannabis use increased in the post-RCL group but patterns of use (frequency; daily vs weekly use) were similar across groups. 44 Overall, the preceding 8 studies reveal some evidence that RCL was associated with increasing rates of cannabis use in adolescent. However, 5 studies point to some inconsistent associations of RCL and cannabis use and suggest that overall relationship of RCL and adolescent cannabis as mixed.
Three studies add to these inconsistent findings and point to lack of an association between RCL and changes in cannabis use among adolescents. Two studies found no significant increase in the frequency of or prevalence of cannabis use following RCL.41,45 Finally, a study examining trends of adolescent cannabis use and associations with period effects (ie, external world events that could influence use) suggests laws and regulations associated with RCL were not associated with cannabis use changes. 46 The current research reveals conflicting evidence about the role of RCL on adolescent cannabis use.
Cannabis use changes in young adults (~18-25)
Young adulthood, typically defined as ages 18 to 25 and also known as emerging adulthood, is commonly associated with decreased parental supervision, increased availability of substances, and greater substance experimentation making it a key developmental period for the onset of cannabis use. 47 Four studies examined the impact of RCL on cannabis use among young adults, 2 of which found significant associations between RCL and increased cannabis use in college students.47,48 Barker and Moreno 48 found the rate of students ever using cannabis did not change. However, in those who had used cannabis prior to RCL, the proportion of students using in the past 28-days increased faster following RCL in Washington (legal-state) when compared with the rate of increase in Wisconsin (non-legal state; P ⩽ .001). 48 Further, in college students from Oregon, rates of cannabis use increased significantly from before to after RCL (P = .0002). 47 Another study looked at changes in cannabis use in a sample of young adults from the U.S. who had never vaped cannabis at the time of recruitment. 49 Results revealed that cannabis use in the past year did not differ in states with or without RCL, although, those living in states with RCL did show a larger increase in rates of cannabis vaping across time, compared to those in non-RCL states. Finally, in a sample of youth from Oregon and Washington, RCL predicted a higher likelihood of past-year cannabis use (P = .001). 50 In contrast to the adolescent literature, studies examining cannabis use in young adult samples fairly consistently point to an association between RCL and increasing rates of cannabis use.
Cannabis use changes in general population adults
Five studies examined changes in cannabis use in adults (without further age subclassification) associated with RCL. Four of these studies suggested higher rates of cannabis use in adults for RCL jurisdictions compared to non-legal states post-RCL, or increased use following RCL.37,45,51,52 Past 30-day cannabis use increased significantly 1-month post-RCL and remained elevated 6-months post-RCL (ps = 0.01) in a sample of adults from California. 51 Another study found an association between RCL and transition from non-users to cannabis users and non-users to weekly users when compared to states with no medical legalization or RCL (P ⩽ .001) and states with no legalization combined with those with medical cannabis legalization (P ⩽ .001). 37 Meanwhile, in Canada, a significant increase in prevalence of cannabis use was observed following RCL. 45 Additionally, in those reporting no cannabis use prior to RCL in Canada, there were significant increases in cannabis use frequency, quantity of cannabis used, and severity of cannabis misuse following RCL. 52 The opposite pattern was seen for those reporting cannabis use prior to RCL, with significant decreases in frequency of use, quantity, and misuse. 52 However, not all studies found RCL was associated with increased cannabis use. For instance, a repeated cross-sectional study of adult in the U.S. found no association between RCL and frequency of cannabis use. 53
A benefit of the extant literature examining general population cannabis use is that it covers a variety of jurisdictions and study designs, albeit with some heterogeneity and mixed findings. On balance, the evidence within the current literature, generally suggests an increase in cannabis use for adults in the general population following RCL with 80% of the reviewed studies supporting this conclusion.
Maternal use
Three studies examined whether rates of cannabis use during pregnancy have increased following RCL. Two studies suggested increased cannabis use during pregnancy associated with RCL. In one study urine screen-detected cannabis use during pregnancy increased from 6% to 11% following RCL in California (P = .05). 54 Another study in a sample of women participating in an intensive case management program for heavy alcohol and/or drug use during pregnancy, examined cannabis use among those exiting from the program before versus after RCL. Findings revealed women exiting after RCL were more likely to report using cannabis in the 30 days prior to exit compared to those pre-RCL (OR = 2.1, P ⩽ .0001). 55 One study revealed no significant difference in cannabis or alcohol use associated with RCL in women living with HIV during pregnancy or the postpartum period. 56 Overall, the evidence from these three studies suggests there may be increases in perinatal cannabis use following RCL, but the small number of studies and unique features of the samples suggests a need for more research.
Clinical populations use
Six studies examined cannabis use in clinical populations. One study investigated use and trauma admissions for adults and pediatric patients in California. 57 Results showed an increase in adult trauma patients with THC+ urine tests from pre- to post-RCL (9.4% to 11.0%; P = .001), but no difference for pediatric trauma patients. A study based in Colorado and Washington, found that cannabis use rates in inflammatory bowel disease patients significantly increased from 107 users to 413 (P ⩽ .001) pre to post-RCL. 58 A Canada-based study of women with moderate-to-severe pelvic pain found an increase in the prevalence of current cannabis use following RCL (13.3% to 21.5%; P ⩽ .001). 59 Another Canadian study showed an increase in the prevalence of current cannabis use after RCL among cancer patients (23.1% to 29.1%; P ⩽ .01). 60 Finally, two studies examined changes in cannabis use among individuals receiving treatment for a substance use disorder. In a sample of Canadian youth in an outpatient addictions treatment program, there was no change in the rate of cannabis use following RCL. 61 Further, in a sample of individuals receiving treatment for opioid use disorder, cannabis use was compared for those recruited 6 months before or after RCL with no significant changes in the prevalence or frequency of self-reported (P = .348 and P = .896, respectively) or urine screen-detected (P = .087 and P = .638, respectively) cannabis use following RCL. 62 Although these studies only represent a small number of observations, their findings do reveal associations between RCL and increasing cannabis use within some clinical samples.
Changes in polysubstance and other substance use
One study examined simultaneous cannabis and alcohol use among 7th, 9th, and 11th grade students in the U.S. 39 This study found that RCL was associated with a 6% increase in the odds of past 30-day alcohol and cannabis co-use. The association was even stronger in students with past 30-day alcohol use and heavy drinking. However, among past 30-day cannabis users, RCL was associated with a 24% reduction in co-use. This study suggests at least a modest association between RCL and concurrent cannabis and alcohol use among adolescents.
Numerous studies examined changes of alcohol and other substance use pre to post RCL. With regard to alcohol, one study from Colorado and Washington found a decrease in alcohol consumption among adolescents following RCL, 42 whereas another Washington study found RCL predicted a higher likelihood of alcohol use among youth. 50 A Canadian study also found no significant effect of RCL on rates of alcohol or illicit drug use among youth. 61 Finally, in a sample of trauma patients in California the findings around changes in substance use were mixed. 57 In adult patients, the rates of positive screens for alcohol, opiates, methamphetamine, benzodiazepine/barbiturate, and MDMA did not change following RCL, but there was an increase in positive screens for cocaine. In pediatric patients, increases were seen in positive screens for benzodiazepine/barbiturate, but positive screens for alcohol, opiates, methamphetamine, and cocaine did not change. 57 The current evidence is divided on whether RCL is associated with increased alcohol and other substance use, with 40% of studies finding an association and 60% not observing one or finding mixed results.
In the case of cigarettes, Mason et al 42 did find significant cohort effects, where the post-RCL cohort was less likely to consume cigarettes compared to the pre-RCL one (Coefficient: − 2.16, P ⩽ .01). However, these findings were not echoed in more recent studies. Lack of an effect for cigarette use is supported by an Oregon study that found RCL was not associated with college student’s cigarette use. 47 Similarly, RCL was not significantly associated with past-year cigarette use in a sample of young adults from Oregon and Washington. 50 On balance, there is little evidence that RCL is linked with changes in cigarette smoking.
Route of administration
The increase in smoke-free alternative routes of cannabis administration (eg, vaping and oral ingestion of edibles)63,64 make method of cannabis consumption an important topic to understand in the context of RCL. Two studies examined differences in route of cannabis consumption as a function of cannabis policy. One study examined changes in the number of different modes of cannabis use reported by high school students in Canada. 65 Results showed that from pre-to-post RCL 31.3% of students maintained a single mode of use, 14.3% continued to use cannabis in multiple forms, while 42.3% expanded from a single mode to multiple modes of administration and 12.1% reduced the number of modes they used. Another study found that smoking, vaping, and edibles (in that order) were the most frequent modes of cannabis use pre- and post-RCL in California, suggesting minimal impact of RCL on mode of cannabis use. 51 However, the least common mode of cannabis use was blunts, which did decline following RCL (13.5%-4.3%). 51 Overall, the evidence suggests RCL may be associated with changes in modes of cannabis consumption, but as the evidence is only from two studies there still remains a need for more studies examining RCL and cannabis route of administration.
Attitudes
Nine studies examined RCL and cannabis attitudes (see Table 2). Regarding cannabis use intentions, one U.S. study found that for both a non-RCL state and a state that underwent RCL, intention to use in young adults significantly increased post-RCL, suggesting a lack of RCL specific effect, 48 and that aside from the very first time point, there were no significant differences between the states in intention to use. Further, attitudes and willingness to use cannabis, between the RCL and non-RCL state remained similar overtime (Ps ⩾ .05), although both states reported significantly more positive attitudes toward cannabis following RCL (P ⩽ .001). 48 However, another study U.S. from found differences in adolescent use intentions across RCL, whereby those in the RCL cohort in jurisdictions that allowed sales were less likely to increase intent to use cannabis (P = .04), but the RCL cohort without sales were more likely to increase intent to use (P = .02). 43 The pre-RCL cohort in communities that opted out of sales were also less likely to increase willingness to use compared to the cohort with legal sales (P = .02). 43 Both studies reveal contrasting findings surrounding RCL’s relationship with cannabis use intentions and willingness to use.
Table 2.
Studies examining recreational cannabis legalization and attitudes surrounding cannabis.
| Author | Year | Location | Date of legalization | Study design | Sample | Brief findings |
|---|---|---|---|---|---|---|
| AminiLari et al | 2022 | Ontario | 2018 | Longitudinal | N = 254 | Pre-RCL 25% of adults reported having medical cannabis authorization. Post-RCL the biggest shift in motivations for use was from solely medical to medical and recreational reasons. About ¼ of medicinal only users shifted to both medicinal and recreational reasons for use, and ¼ of participants reporting both reasons shifted to exclusively recreational reasons for use. |
| Bailey et al | 2020 | Washington | 2012 | Longitudinal | N = 281 | RCL was not associated with perceived harm from cannabis use among youth. |
| Barker & Moreno | 2021 | Washington & Wisconsin | 2012 | Longitudinal cohort | N = 338 | Attitudes toward cannabis were similar across states over time. However, post RCL attitudes toward cannabis became more positive for both states. Intentions to use cannabis also increased post RCL for both states. |
| Estoup et al | 2016 | Washington | 2012 | Cohort | N = 262 | There was a significant indirect effect of RCL to cannabis-related consequences through lower perceived risk of use, but not frequency of use. |
| Gali et al | 2021 | California | 2016 | Longitudinal cohort | N = 429 | Exposure to others cannabis use did not change post-RCL. Mental health perceptions from cannabis increased from slightly harmful to slightly beneficial. Physical health perceptions decreased 1-month post-RCL but increased 6-months post-RCL. Well-being perceptions remained similar 1-month post-RCL and increased 6-moths post-RCL. |
| Hawke & Henderson | 2021 | Ontario | 2018 | Cohort | N = 269 | Reports of using cannabis alone, using with friends, and concealing cannabis use did not differ between the cohorts. Ease of cannabis access and reported safety of cannabis did not differ between cohorts. |
| Hawley et al | 2019 | British Columbia | 2018 | Repeated cross-sectional | N = 1673 | The percent of cancer patients reporting some recreational reasons for cannabis increased post-RCL. Percent of pure medicinal users did decrease, non-significantly, post-RCL. Post-RCL cannabis users reported more problems accessing cannabis, with greatest barriers being lack of dispensaries and preferred products. |
| Rosic et al | 2021 | Ontario | 2018 | Repeated cross-sectional | N = 1390 | The perceptions of how RCL would impact cannabis use did not change post- RCL. Most participants reported RCL would not/has no impact on use. |
| Rusby et al | 2018 | Oregon | 2015 | Cohort | N = 444 | RCL cohort was more likely to increase cannabis intentions overtime, while the pre-RCL cohort was less likely to increase willingness and intent to use. RCL was not associated with initiating cannabis use. |
Author, author of article; Year, publication year of article; Location, jurisdiction article data was collected in; Date of Legalization, year legalization was enacted in jurisdiction; Sample, total N of article sample; RCL, Recreational Cannabis Legalization.
Looking at cannabis use motives, one study found a non-significant increase in recreational motives for cannabis use post-RCL. 60 Similarly following RCL in Canada, 24% of individuals previously reporting cannabis use exclusively for medical purposes declared using for both medical and non-medical purposes following RCL, and 24% declared use for non-medical purposes only, 66 suggesting RCL can influence recreational/nonmedicinal motivations for cannabis use among those who previously only used for medical reasons.
In studies examining perceived risk and perceptions of cannabis use, one U.S. study found an indirect effect between RCL and increased consequences of use in adolescents through higher perceived risk (P ⩽ .001), but no association with frequency of use. 41 Another U.S. study revealed mixed results and found that RCL was not associated with perceived harm of use in youth. 50 Further, youth in one study did not report differences in perceptions of safety of cannabis, ease of accessing cannabis use or on concealing their use from authority, 61 which contrasts with another study finding increased reports of problems accessing cannabis post-RCL (P ⩽ .01). 60 Regarding health perceptions, a California study found that cannabis use was perceived as more beneficial for mental health, physical health, and wellbeing in adults at 6 months post-RCL compared to pre-RCL and 1-month post-RCL (P = .02). 51 Mental health perceptions of cannabis use increased from being perceived as “slightly harmful” pre-RCL to perceived as “slightly beneficial” at 6 months post-RCL. 51 However, in a sample of treatment seeking individuals with an opioid use disorder, the vast majority of participants reported beliefs that RCL would not impact their cannabis use, with no difference in beliefs pre- to post-RCL (85.9% reported belief it would have no impact pre-RCL and 85.7%, post-RCL). 62 The combined results of the studies suggest potential associations of RCL with risk and benefit perceptions of cannabis use, however as 55% of studies suggest a lack of or inconsistent association with RCL, on balance the literature on RCL’s impact on cannabis attitudes is mixed.
Health-related outcomes
We identified 33 articles that examined various health-related outcomes associated with RCL (see Table 3). The largest number involved hospital utilization (ie, seeking emergency services for cannabis-related problems such as unintentional exposure, CUD, and other harms). Other health-care outcomes included opioid-related harms, mental health variables, and adverse birth outcomes.
Table 3.
Studies investigating the relationship of recreational cannabis legalization and health-related outcomes.
| Author | Year | Location | Date of legalization | Study design | Sample | Brief findings |
|---|---|---|---|---|---|---|
| Emergency service utilization | ||||||
| Baraniecki et al | 2021 | Ontario | 2018 | Retrospective chart review | N = 173 | There was no difference in rate of cannabis intoxication related visits pre to post RCL. RCL was associated with an increase in patients 18 to 29. Post-RCL, the patients needing only observation increased, and the number of patients ordered for bloodwork or imaging decreased. |
| Calcaterra et al | 2019 | Colorado | 2012 | Archival administrative data | N = 38 406 | Rates of cannabis related emergency visits significantly increased from 2009 to 2015. Alcohol related visits also increased, but to less of an extent than cannabis. Cannabis related emergency visits did show an abrupt increase following RCL. |
| Callaghan et al | 2022 | Alberta & Ontario | 2018 | Archival administrative data | N = 230 206 | The rate of emergency department visits with cannabis-induced psychosis did not change pre- to post-RCL. Further, there was no change in admissions with amphetamine or alcohol induces psychosis. |
| Delling et al | 2019 | Colorado, New York, & Oklahoma | 2012 | Archival administrative data | Colorado: N = 2 088 909, New York: N = 11 726 283, Oklahoma: N = 2 334 988 | The rate of change for cannabis diagnoses was greater in Colorado than New York and Oklahoma post-RCL. There were decreased admissions for cannabis abuse in Colorado compared to Oklahoma post-RCL. Healthcare costs and length of patient stay showed no significant difference across state. Colorado also had increased motor vehicle accidents, alcohol abuse, injection overdose injuries, and decreased chronic pain admissions post-RCL compared to both states. |
| Grigorian et al | 2019 | California | 2016 | Archival administrative data | N = 21 173 | Post-RCL also had significantly higher adult trauma activation. Both adults and pediatrics had increased mortality rates post-RCL. |
| Kim et al | 2022 | Ontario | 2018 | Interrupted time series | N = 14 900 820 | Cannabis-related emergency department visits increased for individuals under 65 post-RCL. RCL was associated with immediate visits for men 45 to 64, women 25 to 44, and women 45 to 65. However, RCL was not associated with trend level increases in emergency visits. |
| Masonbrink et al | 2021 | U.S. | Cohort | N = 1 898 432 | RCL was associated with increased adolescent cannabis-related admissions from 2008 to 2019. While there was an increasing trend pre-RCL, the rate of increase in admissions accelerated post-RCL. | |
| Mennis & Stahler | 2020 | Colorado & Washington | 2012 | Archival administrative data | N = 653 232 | Adolescent cannabis treatment admissions rates decreased in both states over time, with steep declines post-RCL. The decrease in admissions for both states was greater than non-legal states but not significantly. |
| Myran et al | 2022 | Ontario | 2018 | Repeated cross-sectional | N = 13 853 396 | Cannabis-related emergency visits in youth and young adults were increasing pre-RCL, but RCL was associated with an immediate spike followed by a monthly attenuation in rate of visits. |
| Myran et al | 2022 | Ontario | 2018 | Repeated cross-sectional | N = 14 375 697 | Rates of cannabis hyperemesis related emergency visits were increasing pre-RCL. Post-RCL there was no significant change in rates of emergency visits, but the increasing trend continued. |
| Myran et al | 2022 | Canada | 2018 | Archival administrative data | N-581 | Children hospital admissions for cannabis poisonings increased 2.6x post-RCL for all provinces examined (British Columbia, Alberta, Ontario, Quebec). |
| Pusateri et al | 2022 | Colorado & Washington | 2012 | Archival administrative data | N = 18 545 | Rates of steroid use and need for total parenteral nutrition in irritable bowel disease patients decreased post-RCL. Total hospital costs in patients also dropped post-RCL. In cannabis users specifically, there was less patients needing total parenteral nutrition and lower hospital costs post-RCL. |
| Roth et al | 2022 | California | 2016 | Archival administrative data | N = 12 108 | Post-RCL monthly cannabis-exposure poisons control calls significant increased. By age, exposures in youth under 13 significant increase post-RCL, but there was no change for those 13+. |
| Sokoya et al | 2018 | Colorado | 2012 | Archival administrative data | N = 2164 | There was no change in number of facial fractures pre to post RCL. Maxillary and skull base fractures were the only type to significantly increase post-RCL. |
| Thomas et al | 2019 | Washington | 2012 | Archival administrative data | N = 161 | The number of unintentional pediatric cannabis exposures per month increased post-RCL. |
| Wang et al | 2018 | Colorado | 2012 | Archival administrative data | N = 4202 | Overall, 67% of adolescent patients had THC positive urine drug screens. The rate of annual cannabis-related visits to emergency care significantly increased over time. Behavioral health evaluations from visits also increased over time. |
| Wang et al | 2022 | Colorado | 2012 | Archival administrative data | N = 262 699 | Cannabis-related pregnancy admissions significantly increased from 2011 to 2018, with spikes in 2012 and 2014. |
| Wang et al | 2017 | Colorado | 2012 | Archival administrative data | N = 7 440 392 | Cannabis related hospitalizations increased over time, with the greatest increases in 2009 and 2014. Visits associated with mental illness were more common in cannabis related visits. Poison control calls remained stable but there were significant increases in 2010. There were increases in calls for those under 17 and over 25 after 2014. Unintentional cannabis exposure increased for those 0 to 8 from 2008 to 2014 and for 9+ year old’s from 2013 to 2015. |
| Wang et al | 2016 | Colorado | 2012 | Archival administrative data | N = 244 | Unintentional cannabis exposure in children increased 2 years post-RCL compared to 2 years pre-RCL. There was also a significant increase in poison control cases over time. This increase was significantly greater compared to the rest of the U.S. |
| Yeung et al | 2021 | Alberta | 2018 | Archival administrative data | N = 1920 | Overall pediatric cannabis-related emergency department visits did not change pre- to post-RCL. For specific age groups rate and proportion of visits for children under 12 increased post-RCL. Emergency visit rates for cannabis and other substances decreased in adolescents 15 to 17. For cannabis co-diagnoses, the proportion of cannabis hyperemesis presentations increased post-RCL in adolescents 15 to 17. Unintentional cannabis ingestion rates did increase post-RCL for children and older adolescents, but not for younger adolescents. |
| Yeung et al | 2020 | Alberta | 2018 | Archival administrative data | N = 14 732 | The volume of cannabis-related emergency department visits and poison control calls increased post-RCL. Cannabis and other substance admissions and co-diagnoses decreased post-RCL. |
| Opioid use | ||||||
| Dranitsaris et al | 2021 | Canada | 2018 | Archival administrative data | Public and private prescription claims | There was a steady decline in volume of opioids prescribed for public and private drug plans. Post-RCL there was a significant spike in the rate of declines (5.4x greater than pre-RCL). |
| Geoffrion et al | 2021 | British Columbia | 2018 | Archival administrative data | N = 3705 | Post-RCL women were less likely to consume opioids and other narcotics. |
| Livingston et al | 2017 | Colorado | 2012 | Interrupted time series | CDC and Prevention WONDER from 2000 to 2015 | There was a significant decrease in opioid-related deaths post-RCL. Even after controlling for trends in comparison states there was still a significant reduction. |
| Lopez et al | 2021 | U.S. | Archival administrative data | N = 144 000 | There was no significant association between RCL and opioid prescriptions by an orthopedic surgeon. RCL states had non-significant increases in daily doses of opioid and hydrocodone prescriptions respectively. | |
| Shi et al | 2019 | U.S. | Archival administrative data | Medicaid State Drug Utilization Data | RCL states had slightly greater, not significantly, Schedule II and III opioid prescriptions compared to medical only states. States with RCL in 2015 to 2017 had reduced Schedule III prescriptions while states with RCL to 2012 had increases. RCL was not associated with number of prescriptions, total doses, or spending of Schedule II opioids. However, RCL in 2015 was associated with the former two and Schedule III spending. | |
| Adverse birth outcomes | ||||||
| Siega-Riz et al | 2020 | Colorado & Washington | 2012 | Archival administrative data | N = 1 347 916 | The rate of small for gestational age births did not change pre to post RCL in both Washington and Colorado. Pre-term births did increase post-RCL but only in Colorado. Congenital anomalies significantly increased for both states pre to post-RCL. |
| Straub et al | 2021 | Washington | 2012 | Archival administrative data | N = 5343 | The prevalence of positive THC screens in women giving birth did not change over time. The prevalence of low-birth-weight births did increase from pre to post-RCL. However, RCL was not associated with small for gestational age births. |
| Mental health outcomes | ||||||
| Callaghan et al | 2022 | Alberta & Ontario | 2018 | Archival administrative data | N = 230 206 | Emergency visits with schizophrenia and related conditions codes did not change pre- to post-RCL. |
| Geoffrion et al | 2021 | British Columbia | 2018 | Archival administrative data | N = 3705 | Post-RCL, women had higher anxiety scores than pre-RCL. |
| Hawke & Henderson | 2021 | Ontario | 2018 | Cohort | N = 269 | There were no significant differences for the pre and post-RCL cohorts for internalizing or externalizing disorders or crime/violence screenings. |
| Rusby et al | 2019 | Oregon | 2014 | Ecological momentary assessment | N = 466 | Cannabis users had higher mood lability scores compared to non-users. RCL had no impact on the association of anxious mood and cannabis use. |
| Vignault et al | 2021 | Quebec | 2018 | Archival administrative data | N = 2615 | Prevalence of psychotic disorders did not differ pre- to post-RCL, but personality disorders and other psychiatric disorders were more prevalent post-RCL. |
| Yeung et al | 2021 | Alberta | 2018 | Archival administrative data | N = 1920 | Personality and mood related co-diagnosis decreased post-RCL for adolescents 15 to 17. |
| Miscellaneous health outcomes | ||||||
| Fedorova et al | 2022 | California | 2016 | Longitudinal | N = 668 | Approximately half of medical cannabis patients remained so from pre- to post-RCL. The most common transition group pre- to post-RCL was out of medical cannabis patient status, followed by never been issued a medical cannabis recommendation, with into medical cannabis patient at the smallest transition group. RCL was the most common reason reported for transitioning out if medical cannabis patient status. |
| Geoffrion et al | 2021 | British Columbia | 2018 | Archival administrative data | N = 3705 | Post-RCL, women had higher pain catastrophizing scores than pre-RCL. Post-RCL women were less likely to consume anti-inflammatories, and nerve medications to treat pelvic pain, but more likely to use herbal pain medication. |
| Jordan et al | 2022 | New Brunswick | 2018 | Retrospective chart review | N = 3060 | The proportion of post-mortem positive cannabis screens did increase from pre- to post-RCL but was not significant following Benjamini-Hochberg correction. The only age group with a significant increase in proportion of positive screens post-RCL was 25-44-year-olds. Those who died post-RCL did have higher odds of cannabis present post-mortem. Tests for cannabinoid detection, did find an increase in positive detection over time, with the steepest increases occurring pre-RCL. There was no change in detection of other drugs. |
Author, Author of article; Year, Publication year of article; Location, Jurisdiction article data was collected in; Date of Legalization, Year legalization was enacted in jurisdiction; Sample, Total N of article sample; CDC, Center for Disease Prevention; WONDER, Wide-Ranging Online Data for Epidemiologic Research; RCL, Recreational Cannabis Legalization.
Emergency service utilization
Seventeen studies examined the association between RCL and use of emergency services related to cannabis (eg, hospital visits, calls to regional poison centers). Regarding emergency service rates in youth, a Colorado study found the rate of pediatric cannabis-related emergency visits increased pre- to post-RCL (P ⩽ .0001). 67 Similarly, cannabis-related visits requiring further evaluation in youth also increased. 67 This increasing need for emergency service related to cannabis exposure in youth following RCL was supported in 4 other U.S. studies.68-71 A Canadian study supported the U.S. studies, finding a 2.6 increase in children admissions for cannabis poisonings post-RCL. 72 In contrast, overall pediatric emergency department visits did not change from pre- to post-RCL in Alberta, Canada, 73 but there was a non-significant increase of the rate and proportion of children under 12 presenting to the emergency department. However, unintentional cannabis ingestion did increase post-RCL for children under 12 (95% CI: 1.05-1.47) and older adolescents (1.48, 95% CI: 1.21-1.81). 74 Taken together, these studies do suggest a risk for increasing cannabis-related emergency visits in youth following RCL, with 75% of studies finding an association between RCL and increasing emergency service rates in youth.
There is also evidence of increased hospital utilization in adults following RCL. Five studies found evidence of increased emergency service utilization or poison control calls from cannabis exposure associated with RCL in the U.S. and Canada.24,69,74-76 Finally, a Colorado study saw an increase in cannabis involved pregnancy-related hospital admissions from 2011 to 2018, with notable spikes after 2012 and 2014, timeframes associated with state RCL. 77
However, some evidence points to a lack of association between RCL and emergency service utilization. A chart review in Ontario, Canada found no difference in number of overall cannabis emergency room visits pre- versus post-RCL (P = .27). 78 When broken down by age group, visits only increased for those 18 to 29 (P = .03). This study also found increases in patients only needing observation (P = .002) and fewer needing bloodwork or imaging services (both Ps ⩽.05). 78 Further in a California study that found overall cannabis exposure rates were increasing, when breaking these rates down by age there was no significant change in calls for those aged 13 and up, only for those 12 and under. 69 An additional Canadian study found that rates of cannabis related visits were already increasing pre-RCL. 79 Following RCL, although there was a non-significant immediate increase in in cannabis-related emergency visits post-RCL this was followed a significant drop off in the increasing monthly rates seen prior to RCL. 79 Another Canadian study that examined cannabis hyperemesis syndrome emergency visits found that rates of admissions were increasing prior to RCL and the enactment of RCL was not associated with any changes in rates of emergency admissions. 80 As this attenuation occurred in Canada prior to commercialization where strict purchasing policy was in place, it may suggest that having proper regulations in place can prevent the uptick in cannabis-related emergency visits seen in U.S. studies.
Other hospital-related outcomes examined included admissions for cannabis misuse and other substance use exposure. One study found decreasing CUD admission rates over time (95% CI: −4.84, −1.91), with an accelerated, but not significant, decrease in Washington and Colorado (following RCL) compared to the rest of the U.S. 81 In contrast, another study found increased rates of healthcare utilization related to cannabis misuse in Colorado compared to New York and Oklahoma (Ps ⩽.0005). 82 With respect to other substance use, findings revealed post-RCL increases in healthcare utilization in Colorado for alcohol use disorder and overdose injuries but a decrease in chronic pain admissions compared to both controls (P ⩽ .05). 82 However, two Canadian studies found the rate of emergency department visits with co-ingestant exposure of alcohol, opioid, cocaine, and unclassified substances in older adolescents and adults decreased post-RCL.73,77 Another Canadian study found no change in cannabis-induced psychosis admissions nor in alcohol- or amphetamine-induced admissions. 83
Finally, three studies examined miscellaneous hospital-related outcomes. A study examining hospital records in Colorado to investigate facial fractures (of significance as substance impairment can increase the risk of accidents) showed a modest but not significant influence of RCL. 84 The only significant increases of facial trauma cases were maxillary and skull base fracture cases (Ps ⩽ .001) suggesting a partial influence of RCL on select trauma fractures. The second study found increased trauma activation (need for additional clinical care in hospital) post-RCL in California (P = .01). 57 Moreover, both adult and pediatric trauma patients had increased mortality after RCL (P = .03; P = .02, respectively). 57 The final study examining inflammatory bowel disease (IBD) outcomes in the U.S. found more cannabis users on total parenteral nutrition post-RCL (95% CI: 0.02, 0.89) and lower total hospital costs in users post-RCL (95% CI: −15 717, −1119). 58 No other IBD outcomes differed pre- to post-RCL (eg, mortality, length of stay, need for surgery, abscess incision and drainage).
Overall, these studies point to increased cannabis-related health-care utilization following RCL for youth and pediatrics (75% finding an increase). However, the impact of legalization on adult rates of cannabis-related emergency visits is mixed (44% finding lack of an association with RCL). As findings also varied across different countries (ie, Canada vs the U.S.), it suggests the importance of continually monitoring the role of RCL across different jurisdictions which may have different cannabis regulations in place. These studies also suggest there may be other health consequences associated with RCL. Further research should be done to examine trends of other emergency service use that could be influenced by RCL.
Opioid use
Two studies reported a weak or non-existent effect of RCL on opioid related outcomes.85,86 First, a U.S. administrative study found no association of RCL and opioid prescriptions from orthopedic surgeons. 85 The second study found that, of U.S. states that passed RCL, those that passed policies before 2015 had fewer Schedule III opioid prescriptions (P = .003) and fewer total doses prescribed (P = .027), 86 but when compared to states with medicinal cannabis legislation, there were no significant differences. However, 3 studies suggested a potential protective effect of RCL, with one study finding a significant decrease for monthly opioid-related deaths following RCL (95% CI: –1.34, –0.03), compared to medical cannabis legalization and prohibition. 87 A Canadian study examining opioid prescription claims also found an accelerated decline in claims for public payers post-RCL compared to declines seen pre-RCL (P ⩽ .05). 88 Next a study examining women with pelvic pain found that post-RCL patients were less likely to report daily opioid use, including use for pain (P = .026). 59 These studies indicate some inconsistencies in relationships between RCL, opioid prescriptions and use indicators in the current literature, while the literature on balance points to a potential relationship with RCL (60%), the overall evidence is still mixed as 40% of studies support a weak association with RCL.
Adverse birth outcomes
Changes in adverse birth outcomes including small for gestational age (SGA) births, low birth weight, and congenital anomalies were examined in two studies. The first study, which examined birth outcomes in both Colorado and Washington, found that RCL was associated with an increase in congenital anomaly births for both states (P ⩽ .001, P = .01 respectively). 89 Preterm births also significantly increased post-RCL, but only in Colorado (P ⩽ .001). Regarding SGA outcomes, there was no association with RCL for either state. 89 Similarly, the second study did find an increase in the prevalence of low birth weight and SGA over time, but RCL was not directly associated with these changes. 90 Although the current literature is small and limited to studies in Washington and Colorado, the evidence suggests minimal changes in adverse birth outcomes following RCL.
Mental health outcomes
Six studies examined mental health related outcomes. A Canadian study examining psychiatric patients did not see a difference in rates of psychotic disorders pre- to post-RCL. 45 Similarly, another Canadian study did not see a difference in hospital admissions with schizophrenia or related codes post-RCL. 83 However, the prevalence of personality disorders and “other” diagnoses was higher post-RCL (P = .038). 45 In contrast, another Canadian study found that rates of pediatric cannabis-related emergency visits with co-occurring personality and mood-related co-diagnoses decreased post-RCL among older adolescents. 73 A U.S. study examining the relationship between cannabis use and anxious mood fluctuations in adolescents found RCL had no impact on the association. 91 Similarly, another Canadian study found no difference in mental health symptomology pre- to post-RCL. 61 In contrast, anxiety scores in women with pelvic pain were higher post-RCL compared to pre-RCL (P = .036). 59 The small number and mixed findings of these studies, 66.7% finding no association or mixed findings and 33.3% finding an association but in opposite directions, identify a need for further examination of mental health outcomes post-RCL.
Miscellaneous health outcomes
Three studies examined additional health-related outcomes. First, a California study examined changes in medical cannabis status across RCL. Post-RCL, 47.5% of medical cannabis patients remained medical cannabis patients, while 73.8% of non-patients remained so. 92 The transition into medical cannabis patient status post-RCL represented the smallest group (10%). Cannabis legalization was the most reported reason for transition out of medical cannabis patient status (36.2%). 92 Next, a study examining pelvic pain in women found that post-RCL patients reported greater pain catastrophizing (P ⩽ .001), less anti-inflammatory (P ⩽ .001) and nerve medication use (P = .027), but more herbal pain medication use (P = .010). 59 Finally, a Canadian study that examined cannabinoids in post-mortem blood samples reported that post-RCL deaths had higher odds of positive cannabis post-mortem screens compared to pre-RCL (95% CI: 1.09-1.73). 93 However, the majority of growth for positive cannabinoid screens took place in the two years prior to RCL implementation. In sub-group analyses, only 25- to 44-year-olds had a significant increase in positive cannabinoid screens (95% CI: 0.05-0.19). Additional post-mortem drug screens found an increase in positive screens for amphetamines (P ⩽ .001) and cocaine (P = .042) post-RCL. These additional health outcomes demonstrate the wide-ranging health impacts that may be associated with RCL and indicate a continued need to examine the role of RCL on a variety of outcomes.
Driving-related outcomes
Six studies examined rates of motor vehicle accidents and fatalities (see Table 4). Two U.S. studies found no statistical difference in fatal motor vehicle collisions associated with RCL.94,95 Further, a California-based study examining THC toxicology screens in motor vehicle accident patients, did find a significant increase in positive screens, but this increase was not associated with implementation of RCL. 96 However, three studies suggest a negative impact of RCL, as one U.S. study found both RCL states and their neighboring states had an increase in motor vehicle fatalities immediately following RCL. 97 Additionally, a Canadian study did find a significant increase in moderately injured drivers with cannabis positive blood screens post-RCL. 98 Finally, a study in Uruguay found RCL was associated with increased immediate fatal crashes for cars, but not motorcycles; further investigation suggested this effect was noticeable in urban areas, but not rural areas. 99 While the overall evidence was inconsistent, current evidence does suggest a modest increase, seen in two studies, in motor vehicle accidents associated with RCL. Further longitudinal research in more jurisdictions is needed to understand the long-term consequences of RCL on motor vehicle accidents.
Table 4.
Studies looking at recreational cannabis legalization and driving related outcomes.
| Author | Year | Location | Date of legalization | Study design | Sample | Brief findings |
|---|---|---|---|---|---|---|
| Aydelotte et al | 2017 | Colorado & Washington | 2012 | Archival administrative data | N = 60 737 | Rates of fatal car crashes did not differ between both states pre-RCL and controls. Post-RCL, there were no significant changes in fatality rates. |
| Aydelotte et al | 2019 | Colorado & Washington | 2012 | Archival administrative data | N = 25 561 | Rates of fatal accidents were non-significantly higher in both states post-RCL than control states. |
| Borst et al | 2021 | California | 2016 | Archival administrative data | N = 11 491 | The rate of drivers testing positive for cannabis over time did increase. However, there was not a significant association with RCL, suggesting that the increasing rates were not driven by RCL. |
| Brubacher et al | 2022 | British Columbia | 2018 | Archival administrative data | N = 4339 | There was a significant increase in moderately injured drivers testing positive for THC with a THC level of 2 ng/ml and 5 ng/ml post-RCL. |
| Lane & Hall | 2018 | Colorado, Washington & Oregon | 2012 | Interrupted time series | CDC and Prevention WONDER | There was significant increase in traffic fatalities post-RCL. Neighboring states of Colorado also had significant increases in followed significant trend reductions, suggesting RCL creates a temporary increase in fatalities. |
| Nazif-Munoz et al | 2020 | Uruguay | 2013 | Interrupted time series | National Road Safety Agency of Uruguay and the Ministry of Transport and Public Work | RCL was associated with an immediate increase in light motor vehicle driver fatality rate in larger cities. However, there was no change in light motor vehicle driver fatality rates in rural areas. There was no significant change associated with RCL for motorcyclist fatality rates. |
Author, Author of article; Year, Publication year of article; Location, Jurisdiction article data was collected in; Date of Legalization, Year legalization was enacted in jurisdiction; Sample, Total N of article sample; CDC, Center for Disease Prevention; WONDER, Wide-Ranging Online Data for Epidemiologic Research; RCL, Recreational Cannabis Legalization.
Crime-related outcomes
Three studies explored crime-related outcomes associated with RCL (see Table 5). A Washington study examining cannabis-related arrest rates in adults did find significant drops in cannabis-related arrests post-RCL for both 21+ year olds (87% drop; P ⩽ .001) and 18 to 20-year-olds (46% drop; P ⩽ .001). 100 However, in another study examining Oregon youth this post-RCL decline for arrests was not seen; cannabis-related allegations in youth actually increased following RCL (28%; 95% CI = 1.14, 1.44). 101 Further, declines in youth allegations prior to RCL ceased after RCL was implemented. In contrast, a Canadian study did find significant decreases in cannabis-related offenses in youth post RCL (P ⩽ .001), but rates of property and violent crime did not change across RCL. 102 These studies highlight the diverse effects of RCL across different age groups. However, there remains a need for a more comprehensive evaluation on the role of RCL on cannabis-related arrests.
Table 5.
Studies investigating recreational cannabis legalization and crime related outcomes.
| Author | Year | Location | Date of legalization | Study design | Sample | Brief findings |
|---|---|---|---|---|---|---|
| Callaghan et al | 2021 | Canada | 2018 | Archival administrative data | N = 32 178 | RCL was associated with a significant decrease in daily cannabis-related offenses in youth overall and when broken down by sex. There was no evidence of an RCL association for property or violent crime rates in youth. |
| Firth et al | 2020 | Oregon | 2014 | Interrupted time series | N = 18 779 | Overall rate of cannabis-related allegations increased post-RCL. American Indian/Alaskan Native more likely than White youth to have an allegation pre-and post-RCL but was stable over time. Black youth also more likely than White youth pre-RCL with the disparity decreasing post-RCL. |
| Firth et al | 2019 | Washington | 2012 | Archival administrative data | National Incident Based Reporting System 2012-2015 | Arrest rates dropped in those 21+ after post-RCL. Arrest rates for 18 to 20 decreased post-RCL. Rates for Black individuals 21+ dropped post-RCL but relative disparities from White individuals increased. Rates for Black individuals 18 to 20 also dropped post-RCL but there was no significant increase in relative disparities to White counterparts. Arrest rates for selling cannabis did drop more for White individuals compared to Black individuals. |
Author, Author of article; Year, Publication year of article; Location, Jurisdiction article data was collected in; Date of Legalization, Year legalization was enacted in jurisdiction; Sample, Total N of article sample; RCL, Recreational Cannabis Legalization.
Notably, two studies also examined race disparities in cannabis-related arrests. For individuals 21+ relative arrest disparities between Black and White individuals grew post-RCL. 100 When looking at 18 to 20-year-olds, cannabis-related arrest rates for Black individuals did slightly decrease, albeit non-significantly, but there was no change in racial disparities. 100 In youth ages 10 to 17, Indigenous and Alaska Native youth were more likely than White youth to receive a cannabis allegation before RCL (95% CI: 2.31, 3.01), with no change in disparity following RCL (95% CI: 2.10, 2.81). 101 On the other hand, Black youth were more likely to receive a cannabis allegation than White youth prior to RCL (95% CI: 1.66, 2.13), but the disparity decreased following RCL (95% CI: 1.06, 1.43). 101 These studies suggest improvements in racial disparities for cannabis-related arrests following RCL, although there ware only two studies and they are limited to the U.S.
Discussion
The aim of this systematic review was to examine the existing literature on the impacts of RCL on a broad range of behavioral and health-related outcomes. The focus on more rigorous study designs permits greater confidence in the conclusions that can be drawn. The literature revealed five main outcomes that have been examined: cannabis use behaviors, cannabis attitudes, health-related outcomes, driving-related outcomes, and crime-related outcomes. The overall synthesizing of the literature revealed heterogenous and complex effects associated with RCL implementation. The varied findings across behavioral and health related outcomes does not give a clear or categorical answer as to whether RCL is a negative or positive policy change overall. Rather, the review reveals that while a great deal of research is accumulating, there remains a need for more definitive findings on the causal role of RCL on a large variety of substance use, health, attitude-related, driving, and crime-related outcomes.
Overall, studies examining cannabis use behavior revealed evidence for cannabis use increases following RCL, particularly for young adults (100%), peri-natal users (66%), and certain clinical populations (66%).47,54,59 While general adult samples had some mixed findings, the majority of studies (80%) suggested increasing rates of use associated with RCL. 51 Of note, the increasing cannabis use rates found in peri-natal and clinical populations are particularly concerning as they do suggest increasing rates in more vulnerable samples where potential adverse consequences of cannabis use are more pressing. 103 However, for both groups the overall literature revealed only a few studies and thus requires further examination. Further, a reason to caution current conclusions surround RCL impacts on substance use, is that there is research suggesting cannabis use rates were increasing prior to RCL in Canada. 104 Thus, there still remains a need to better disentangle causal consequences of RCL on cannabis use rates.
In contrast to studies of adults, studies of adolescents pointed to inconsistent evidence of RCL’s influence on cannabis use rates,38,45 with 60% of studies finding no change or inconsistent evidence surrounding adolescent use following RCL. Thus, a key conclusion of the cannabis use literature is that there is not overwhelming evidence that RCL is associated with increasing rates of cannabis among adolescents, which is notable as potential increases in adolescent use is a concern often voiced by critics of RCL. 16 This might suggest that current RCL policies that limit access to minors may be effective. However, a methodological explanation for the discrepancy between findings for adolescents and adults is that adults may be more willing to report their use of cannabis following RCL as it is now legal for them to use. However, for adolescents’ cannabis use remained illicit, which may lead to biased reporting from adolescents. Thus, additional research using methods to overcome limitations of self-reports may be required.
With regard to other substance use, primarily alcohol and cigarettes, there is little evidence that RCL is associated with increased use rates and may even be associated with decreased rates of cigarette use.42,61 The lack of a relationship with RCL and increasing alcohol and other substance use, seen in 60% of studies, is relevant due to concerns of RCL causing “spill-over” effects to substances other than cannabis. However, the decreasing rates on cigarette use associated with RCL seen in 33% of studies may also suggest a substitution effect of cannabis. 105 It is possible that RCL encourages a substitution effect where cannabis is used to replace use other substances such as cigarettes, but 66% of studies found no association of RCL and cigarette use so further research examining a potential substitution effect is needed. In sum, the literature points to a heterogenous impact of RCL on cannabis and other substance use rates, suggesting complex effects of RCL on use rates that may vary across age and population. However, the review also highlights that there are still limited studies examining RCL and other substance use, particularly a lack of multiple studies examining the same age group.
The current evidence for the impact of RCL on attitudes surrounding cannabis revealed mixed or limited results, with 44% studies finding some sort of relationship with attitudes and RCL and 55% studies suggest a lack of or inconsistent relationship. Studies examining cannabis use attitudes or willingness to use revealed conflicting evidence whereas some studies pointed to increased willingness to use associated with RCL, 43 and others found no change or that changes were not specific to regions that implemented RCL. 48 For attitude-related studies that did reveal consistent findings (eg, use motivation changes, perceptions of lower risk and greater benefits of use), the literature was limited in the number of studies or involved heterogenous samples, making it difficult to make conclusive statements surrounding the effect of RCL. As cannabis-related attitudes (eg, perceived risk, intentions to use) can have implications for cannabis use and consequences106,107 it is interesting that current literature does not reveal clear associations of cannabis-related attitudes and RCL. Rather, this review reveals a need for more research examining changes in cannabis-attitudes over time and potential impacts of RCL.
In terms of health outcomes, the empirical literature suggests RCL is associated with increased cannabis-related emergency visits24,67,70,76 and other health consequences (eg, trauma-related cases 57 ). The literature also suggests there may be other potential negative health consequences associated with RCL, such as increasing adverse birth outcomes and post-mortem cannabis screens.45,89 Synthesizing of the literature points to a well-established relationship of RCL and increasing cannabis-related emergency visits. While some extant literature was mixed, on balance most studies included in the review (70.6%) found consistent evidence of increased emergency service use (eg, emergency department admissions and poison control calls) for both adolescents and adults with only 31% of studies finding mixed or no association with RCL. This points to a need for stricter RCL policies to prevent unintentional consumption or hyperemesis such as promoting safe or lower risk use of cannabis (eg, using lower THC products, avoiding deep inhales while smoking), clearer packaging for cannabis products, and safe storage procedures.
However, the literature on health outcomes outside of emergency service utilization is limited and requires more in-depth evaluations to be fully understood. Additionally, not all health-outcomes indicated negative consequences associated with RCL. There is emerging evidence of the potential of RCL to help decrease CUD and multiple substance hospital admissions74,82 Furthermore, while some findings were mixed and the number of studies limited, 60% of studies found potential for RCL to have protective effects for opioid-related negative consequences.87,88 However, opioid-related findings should be considered in the context of population-level changes in opioid prescriptions and shifting opioid policy influence. 108 Thus, findings may be a result of changes driven by the response to the opioid epidemic rather than RCL, and there remains a need to better disentangle RCL impacts on opioid-related consequences. It is also worth noting that some opioid and cannabis studies are underwritten by the cannabis industry, so the findings should be interpreted with caution due to potential for conflicts of interest. 88 In sum, the overall literature suggests that RCL is associated with both negative and positive health-related consequences and reveals a need to examine the role of RCL across a wide range of health outcomes.
The findings from the driving-related literature do suggest RCL is associated with increased motor vehicle accidents (50% of studies) although the literature was quite evenly split as higher accident rates were not seen across all studies (50% studies). These results point to potential negative consequence associated with RCL and may indicate a need for better measures to prevent driving while under the influence of cannabis in legalized jurisdictions. However, as the evidence was split and predominately in the U.S. additional studies spanning diverse geographical jurisdictions are still needed.
On the other hand, the findings from crime-related outcomes showed some inconsistencies. While one study did suggest minimal decreases for substance-use related arrests in adults, the findings were not consistent across the two studies examining arrest-rates in youth.100-102 These potential decreases in arrest rates for adults can have important implications as cannabis-related crime rates make up a large amount of overall crime statistics and drug-specific arrests.30,31 This discrepancy in youth findings between a U.S. and Canadian study are notable as Canadian RCL policies do include stipulations to allow small scale regulations in youth. Thus, it suggests RCL policies that maintain prohibition of use among underage youth do not address issues related to arrests and crime among youth. In fact, the current literature suggests that cannabis-related charges are still being enforced for youth under the legal age of consumption in the U.S. Another important outcome revealed is racial disparities in cannabis-related arrests. Previous evidence has shown there are racial disparities, particularly between Black, Indigenous, and Hispanic individuals compared to White counterparts, in cannabis-related charges and arrests.109,110 Regarding racial disparities and RCL, there was very little evidence of decreases in disparities for cannabis-related arrests following RCL.100,101 This racialized arresting is significant as it can be associated with additional public health concerns such as physical and mental health outcomes, harm to families involved, and to communities. 111 This finding is particularly concerning as it suggests racialized arrests for cannabis are still occurring despite the intentions of liberalization of cannabis policies to help reduce racial disparities in the criminal justice system. However, it is important to note that there were only 2 studies of racial disparities in cannabis-related arrests and both were conducted in the U.S. Thus, additional research is required before drawing any firm conclusions about the ability of RCL to address systemic issues in the justice system.
Limitations
The findings should be considered within context of the following limitations. The research was predominately from North America (U.S. and Canada). While both countries have either federal or state RCL, findings only from two countries that are geographically connected may not reflect the influence of RCL across different cultures and countries globally. The majority of studies also relied on self-report data for cannabis-related outcomes. Thus, there is a risk that any increases in use or other cannabis-related outcomes may be due to an increased comfort in disclosing cannabis use due to RCL.
Given the large number of studies on multiple outcomes, we chose to focus on implementation of RCL exclusively, rather than related policy changes such as commercialization (ie, the advent of legal sales), to allow for clearer conclusions about the specific impacts on RCL. However, a limitation is that the review does not address the impact of commercialization or changes in product availability. While outside the scope of the current review, it does limit the conclusions that can be drawn about RCL overall as some jurisdictions implemented features of commercialization separately from legalization. For example, in Ontario, Canada, storefronts and edible products became legal a year after initial RCL (when online purchase was the exclusive modality), which may have had an additional impact on behavioral and health-related outcomes. Additionally, the scope of the review was limited to recreational legalization and did not consider other forms of policy changes such as medicinal legalization or decriminalization, as these have been summarized more comprehensively in prior reviews.112-114 Further, this review focused on behavioral and health outcomes; other important outcomes to examine in the future include economic aspects such as cannabis pricing and purchasing behaviors, and product features such as potency. Finally, as this review considered a broad range of outcomes, we did not conduct a meta-analysis which limits conclusions that can be drawn regarding the magnitude of the associations.
Conclusions
The topic of RCL is a contentious and timely issue. With nationwide legalization in multiple countries and liberalizing policies across the U.S., empirical research on the impacts of RCL has dramatically expanded in recent years. This systematic review comprehensively evaluated a variety of outcomes associated with RCL, focusing on longitudinal study designs and revealing a wide variety of findings in terms of substance use, health, cannabis attitudes, crime, and driving outcomes examined thus far. However, the current review highlights that the findings regarding the effects of RCL are highly heterogenous, often inconsistent, and disproportionately focused on certain jurisdictions. With polarizing views surrounding whether RCL is a positive or negative policy change, it is noteworthy that the extant literature does not point to one clear answer at the current time. In general, the collective results do not suggest dramatic changes or negative consequences, but instead suggest that meaningful tectonic shifts are happening for several outcomes that may or may not presage substantive changes in personal and public health risk. Furthermore, it is clear that a more in-depth examinations of negative (eg, frequent use, CUD prevalence, ‘gateway’ relationships with other substance use), or positive consequences (eg, therapeutic benefits for mental health and/or medical conditions, use of safer products and routes of administration), are needed using both quantitative and qualitative approaches.
Acknowledgments
None.
Footnotes
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Funding support from the Peter Boris Chair in Addictions Research and a Canada Research Chair in Translational Addiction Research (JM). Funders had no role in the design or execution of the review.
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: James MacKillop discloses he is a principal and senior scientist in Beam Diagnostics, Inc, and a consultant to ClairvoyantRx. No other authors have disclosures.
Author Contributions: The author’s contribution is as follows: study conceptualization and design: KF, JW, JT, JM; data collection and interpretation: KF, EM, MS; manuscript writing and preparation: KF, EM, MS, PN; manuscript reviewing and editing: JW, JT, JM. All authors have reviewed and approved the final manuscript.
References
- 1.World Health Organization. Alcohol Drugs and Addictive Behaviours Unit. Cannabis. World Health Organization. 2021. Accessed September 24, 2021. https://www.who.int/teams/mental-health-and-substance-use/alcohol-drugs-and-addictive-behaviours/drugs-psychoactive/cannabis. [Google Scholar]
- 2.Centers for Disease Control and Prevention. Data and Statistics. CDC. June8, 2021. Accessed September 24, 2021. https://www.cdc.gov/marijuana/data-statistics.htm [Google Scholar]
- 3.National Center for Drug Abuse Statistics. Marijuana Addiction: Rates and Usage Statistics. Drug Abuse Statistics. 2019. Accessed September 24, 2021. https://drugabusestatistics.org/marijuana-addiction/ [Google Scholar]
- 4.Government of Canada. Candian alcohol and drugs survey (CADS): Summary of results for 2019. December20, 2021. Accessed December 28, 2022. https://www.canada.ca/en/health-canada/services/canadian-alcohol-drugs-survey/2019-summary.htm
- 5.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed.American Psychiatric Publishing; 2013. [Google Scholar]
- 6.Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the 2019 National Survey on Drug Use and Health. October, 2021. Accessed December 28, 2022. https://www.samhsa.gov/data/sites/default/files/reports/rpt35319/2020NSDUHFFR102121.htm
- 7.Han BH, Palamar JJ. Trends in cannabis use among older adults in the United States, 2015-2018. JAMA Intern Med. 2020;180:609-611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Azofeifa A, Mattson ME, Schauer G, McAfee T, Grant A, Lyerla R. National estimates of marijuana use and related indicators - National Survey on Drug Use and Health, United States, 2002-2014. MMWR Surveill Summ. 2016;65:1-28. [DOI] [PubMed] [Google Scholar]
- 9.Rotermann M, Macdonald R. Analysis of trends in the prevalence of cannabis use in Canada, 1985 to 2015. Health Rep. 2018;29:10-20. [PubMed] [Google Scholar]
- 10.Corsi DJ, Hsu H, Weiss D, Fell DB, Walker M. Trends and correlates of cannabis use in pregnancy: A population-based study in Ontario, Canada from 2012 to 2017. Can J Public Health. 2019;110:76-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pacek LR, Weinberger AH, Zhu J, Goodwin RD. Rapid increase in the prevalence of cannabis use among people with depression in the United States, 2005-17: the role of differentially changing risk perceptions. Addiction. 2020;115: 935-943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bonn-Miller MO, Harris AHS, Trafton JA. Prevalence of cannabis use disorder diagnoses among veterans in 2002, 2008, and 2009. Psychol Serv. 2012;9:404-416. [DOI] [PubMed] [Google Scholar]
- 13.Johnson MB, Kelley-Baker T, Voas RB, Lacey JH. The prevalence of cannabis-involved driving in California. Drug Alcohol Depend. 2012;123:105-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Salloum NC, Krauss MJ, Agrawal A, Bierut LJ, Grucza RA. A reciprocal effects analysis of cannabis use and perceptions of risk. Addiction. 2018;113:1077-1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hammond CJ, Chaney A, Hendrickson B, Sharma P. Cannabis use among US adolescents in the era of marijuana legalization: A review of changing use patterns, comorbidity, and health correlates. Int Rev Psychiatry. 2020;32:221-234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McGinty EE, Samples H, Bandara SN, Saloner B, Bachhuber MA, Barry CL. The emerging public discourse on state legalization of marijuana for recreational use in the US: analysis of news media coverage, 2010-2014. Prev Med. 2016;90: 114-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McLaren J, Swift W, Dillon P, Allsop S. Cannabis potency and contamination: A review of the literature. Addiction. 2008;103:1100-1109. [DOI] [PubMed] [Google Scholar]
- 18.American Public Health Association. Regulating Commercially Legalized Marijuana as a Public Health Policy. APHA. November18, 2014. Accessed September 24, 2021. https://www.apha.org/policies-and-advocacy/public-health-policy-statements/policy-database/2015/01/23/10/17/regulating-commercially-legalized-marijuana-as-a-public-health-priority [Google Scholar]
- 19.McGinty EE, Niederdeppe J, Heley K, Barry CL. Public perceptions of arguments supporting and opposing recreational marijuana legalization. Prev Med. 2017;99:80-86. [DOI] [PubMed] [Google Scholar]
- 20.Cerdá M, Mauro C, Hamilton A, et al. Association between recreational marijuana legalization in the United States and changes in marijuana use and cannabis use disorder from 2008 to 2016. JAMA Psychiatr. 2020;77:165-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dilley JA, Richardson SM, Kilmer B, Pacula RL, Segawa MB, Cerdá M. Prevalence of cannabis use in youths after legalization in Washington state. JAMA Pediatr. 2019;173:192-193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guttmannova K, Lee CM, Kilmer JR, et al. Impacts of changing marijuana policies on alcohol use in the United States. Alcohol Clin Exp Res. 2016;40:33-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hall W. The adverse health effects of cannabis use: what are they, and what are their implications for policy? Int J Drug Policy. 2009;20:458-466. [DOI] [PubMed] [Google Scholar]
- 24.Wang GS, Hall K, Vigil D, Banerji S, Monte A, VanDyke M. Marijuana and acute health care contacts in Colorado. Prev Med. 2017;104:24-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vyas MB, LeBaron VT, Gilson AM. The use of cannabis in response to the opioid crisis: A review of the literature. Nurs Outlook. 2018;66:56-65. [DOI] [PubMed] [Google Scholar]
- 26.Lucas P, Boyd S, Milloy MJ, Walsh Z. Cannabis significantly reduces the use of prescription opioids and improves quality of life in authorized patients: results of a large prospective study. Pain Med. 2021;22:727-739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Metrik J, Bassett SS, Aston ER, Jackson KM, Borsari B. Medicinal versus recreational cannabis use among returning veterans. Transl Issues Psychol Sci. 2018;4:6-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wardell JD. Correlates of self-reported medicinal cannabis use for physical health, mental health, and sleep-related conditions in a population-based survey of Canadian youth. J Stud Alcohol Drugs. 2022;83:528-536. [PubMed] [Google Scholar]
- 29.Hartman RL, Huestis MA. Cannabis effects on driving skills. Clin Chem. 2013; 59:478-492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Federal Bureau of Investigations. Persons Arrested. FBI UCR. 2018. Accessed September 24, 2021. https://ucr.fbi.gov/crime-in-the-u.s/2018/crime-in-the-u.s.-2018/topic-pages/persons-arrested [Google Scholar]
- 31.Government of Canada. Cannabis Crime Statistics in Canada, 2016. Department of Justice. February, 14, 2018. Accessed September 24, 2021. https://www.justice.gc.ca/eng/rp-pr/jr/jf-pf/2017/july01.html [Google Scholar]
- 32.Bahji A, Stephenson C. International perspectives on the implications of cannabis legalization: A systematic review & thematic analysis. Int J Environ Res Public Health. 2019;16:3095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hasin DS. US epidemiology of cannabis use and associated problems. Neuropsychopharmacology. 2018;43:195-212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wilson S, Rhee SH. Causal effects of cannabis legalization on parents, parenting, and children: A systematic review. Prev Med. 2022;156:106956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.O’Grady MA, Iverson MG, Suleiman AO, Rhee TG. Is legalization of recreational cannabis associated with levels of use and cannabis use disorder among youth in the United States? A rapid systematic review. Eur Child Adolesc Psychiatry. 2022;31:1-23. doi:10.1007/s00787-022-01994-9 [DOI] [PubMed] [Google Scholar]
- 36.Page MJ, Moher D, Bossuyt PM, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gunadi C, Zhu B, Shi Y. Recreational cannabis legalization and transitions in cannabis use: findings from a nationally representative longitudinal cohort in the United States. Addiction. 2022;117:2651-2659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Duan Z, Wang Y, Weaver SR, et al. Effect modification of legalizing recreational cannabis use on the association between e-cigarette use and future cannabis use among US adolescents. Drug Alcohol Depend. 2022;233:109260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Paschall MJ, García-Ramírez G, Grube JW. Recreational marijuana legalization and co-use with alcohol among adolescents. Am J Prev Med. 2022;62:57-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zuckermann AME, Battista KV, Bélanger RE, et al. Trends in youth cannabis use across cannabis legalization: data from the COMPASS prospective cohort study. Prev Med Rep. 2021;22:101351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Estoup AC, Moise-Campbell C, Varma M, Stewart DG. The impact of marijuana legalization on adolescent use, consequences, and perceived risk. Subst Use Misuse. 2016;51:1881-1887. [DOI] [PubMed] [Google Scholar]
- 42.Mason WA, Fleming CB, Ringle JL, Hanson K, Gross TJ, Haggerty KP. Prevalence of marijuana and other substance use before and after Washington State’s change from legal medical marijuana to legal medical and nonmedical marijuana: Cohort comparisons in a sample of adolescents. Subst Abuse. 2016;37: 330-335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rusby JC, Westling E, Crowley R, Light JM. Legalization of recreational marijuana and community sales policy in Oregon: Impact on adolescent willingness and intent to use, parent use, and adolescent use. Psychol Addict Behav. 2018;32: 84-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stormshak EA, Caruthers AS, Gau JM, Winter C. The impact of recreational marijuana legalization on rates of use and behavior: A 10-year comparison of two cohorts from high school to young adulthood. Psychol Addict Behav. 2019;33: 595-602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vignault C, Massé A, Gouron D, Quintin J, Asli KD, Semaan W. The potential impact of recreational cannabis legalization on the prevalence of cannabis use disorder and psychotic disorders: A retrospective observational study. Can J Psychiatry. 2021;66:1069-1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yu B, Chen X, Chen X, Yan H. Marijuana legalization and historical trends in marijuana use among US residents aged 12-25: Results from the 1979-2016 National Survey on drug use and health. BMC Public Health. 2020;20:156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kerr DCR, Bae H, Phibbs S, Kern AC. Changes in undergraduates’ marijuana, heavy alcohol and cigarette use following legalization of recreational marijuana use in Oregon. Addiction. 2017;112:1992-2001. [DOI] [PubMed] [Google Scholar]
- 48.Barker AK, Moreno MA. Effects of recreational marijuana legalization on college students: A longitudinal study of attitudes, intentions, and use behaviors. J Adolesc Health. 2020;68:110-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Han DH, Seo DC. Identifying risk profiles for marijuana vaping among US young adults by recreational marijuana legalization status: A machine learning approach. Drug Alcohol Depend. 2022;232:109330. [DOI] [PubMed] [Google Scholar]
- 50.Bailey JA, Epstein M, Roscoe JN, Oesterle S, Kosterman R, Hill KG. Marijuana legalization and youth marijuana, alcohol, and cigarette use and norms. Am J Prev Med. 2020;59:309-316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gali K, Winter SJ, Ahuja NJ, Frank E, Prochaska JJ. Changes in cannabis use, exposure, and health perceptions following legalization of adult recreational cannabis use in California: A prospective observational study. Subst Abuse Treat Prev Policy. 2021;16:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Turna J, Belisario K, Balodis I, Van Ameringen M, Busse J, MacKillop J. Cannabis use and misuse in the year following recreational cannabis legalization in Canada: A longitudinal observational cohort study of community adults in Ontario. Drug Alcohol Depend. 2021;225:108781. [DOI] [PubMed] [Google Scholar]
- 53.Kerr WC, Lui C, Ye Y. Trends and age, period and cohort effects for marijuana use prevalence in the 1984-2015 US National Alcohol Surveys. Addiction. 2018; 113:473-481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lee E, Pluym ID, Wong D, Kwan L, Varma V, Rao R. The impact of state legalization on rates of marijuana use in pregnancy in a universal drug screening population. J Matern Fetal Neonatal Med. 2022;35:1660-1667. [DOI] [PubMed] [Google Scholar]
- 55.Grant TM, Graham JC, Carlini BH, Ernst CC, Brown NN. Use of marijuana and other substances among pregnant and parenting women with substance use disorders: Changes in washington state after marijuana legalization. J Stud Alcohol Drugs. 2018;79:88-95. [PubMed] [Google Scholar]
- 56.Yee LM, Kacanek D, Brightwell C, et al. Marijuana, opioid, and alcohol use among pregnant and postpartum individuals living with HIV in the US. JAMA Netw Open. 2021;4:e2137162-e2137162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Grigorian A, Lester E, Lekawa M, et al. Marijuana use and outcomes in adult and pediatric trauma patients after legalization in California. Am J Surg. 2019; 218:1189-1194. [DOI] [PubMed] [Google Scholar]
- 58.Pusateri A, Anaizi A, Nemer L, Hinton A, Lara L, Afzali A. Impact of cannabis use on inpatient inflammatory bowel disease outcomes in 2 states legalizing recreational cannabis. Crohns Colitis 360. 2022;4(2):otac015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Geoffrion R, Yang EC, Koenig NA, et al. Recreational cannabis use before and after legalization in women with pelvic pain. Obstet Gynecol. 2021;137:91-99. [DOI] [PubMed] [Google Scholar]
- 60.Hawley P, Gobbo M, Afghari N. The impact of legalization of access to recreational cannabis on Canadian medical users with cancer. BMC Health Serv Res. 2020;20:977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hawke LD, Henderson J. Legalization of cannabis use in Canada: Impacts on the cannabis use profiles of youth seeking services for substance use. J Subst Abuse Treat. 2021;126:108340. [DOI] [PubMed] [Google Scholar]
- 62.Rosic T, Sanger N, Panesar B, et al. Cannabis use in patients treated for opioid use disorder pre- and post-recreational cannabis legalization in Canada. Subst Abuse Treat Prev Policy. 2021;16:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Knapp AA, Lee DC, Borodovsky JT, Auty SG, Gabrielli J, Budney AJ. Emerging trends in cannabis administration among adolescent cannabis users. J Adolesc Health. 2019;64:487-493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Reboussin BA, Wagoner KG, Sutfin EL, et al. Trends in marijuana edible consumption and perceptions of harm in a cohort of young adults. Drug Alcohol Depend. 2019;205:107660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zuckermann AME, Gohari MR, Romano I, Leatherdale ST. Changes in cannabis use modes among Canadian youth across recreational cannabis legalization: data from the COMPASS prospective cohort study. Addict Behav. 2021;122:107025. [DOI] [PubMed] [Google Scholar]
- 66.AminiLari M, Busse JW, Turna J, MacKillop J. Declared rationale for cannabis use before and after legalization for nonmedical use: A longitudinal study of community adults in Ontario. Cannabis Cannabinoid Res. Published online March 23, 2022 doi: 10.1089/can.2021.0128 [DOI] [PubMed] [Google Scholar]
- 67.Wang GS, Davies SD, Halmo LS, Sass A, Mistry RD. Impact of marijuana legalization in Colorado on adolescent emergency and urgent care visits. J Adolesc Health. 2018;63:239-241. [DOI] [PubMed] [Google Scholar]
- 68.Masonbrink AR, Richardson T, Hall M, Catley D, Wilson K. Trends in adolescent cannabis-related hospitalizations by state legalization laws, 2008-2019. J Adolesc Health. 2021;69:999-1005. [DOI] [PubMed] [Google Scholar]
- 69.Roth W, Tam M, Bi C, et al. Changes in California cannabis exposures following recreational legalization and the COVID-19 pandemic. Clin Toxicol. 2022; 60:632-638. [DOI] [PubMed] [Google Scholar]
- 70.Thomas AA, Von Derau K, Bradford MC, Moser E, Garrard A, Mazor S. Unintentional pediatric marijuana exposures prior to and after legalization and commercial availability of recreational marijuana in Washington state. J Emerg Med. 2019;56:398-404. [DOI] [PubMed] [Google Scholar]
- 71.Wang GS, Le Lait MC, Deakyne SJ, Bronstein AC, Bajaj L, Roosevelt G. Unintentional pediatric exposures to marijuana in Colorado, 2009-2015. JAMA Pediatr. 2016;170:e160971-e160971. [DOI] [PubMed] [Google Scholar]
- 72.Myran DT, Tanuseputro P, Auger N, Konikoff L, Talarico R, Finkelstein Y. Edible cannabis legalization and unintentional poisonings in children. N Engl J Med. 2022;387:757-759. [DOI] [PubMed] [Google Scholar]
- 73.Yeung MEM, Weaver CG, Hartmann R, Haines-Saah R, Lang E. Emergency department pediatric visits in Alberta for cannabis after legalization. Pediatrics. 2021;148:e2020045922. [DOI] [PubMed] [Google Scholar]
- 74.Yeung MEM, Weaver CG, Janz K, Haines-Saah R, Lang E. Clearing the air: A study of cannabis-related presentations to urban Alberta emergency departments following legalization. Can J Emerg Med. 2020;22:776-783. [DOI] [PubMed] [Google Scholar]
- 75.Calcaterra SL, Hopfer CJ, Keniston A, Hull ML. Changes in healthcare encounter rates possibly related to cannabis or alcohol following legalization of recreational marijuana in a safety-net hospital: an interrupted time series analysis. J Addict Med. 2019;13:201-208. [DOI] [PubMed] [Google Scholar]
- 76.Kim C, Chum A, Nielsen A, et al. Associations between recreational cannabis legalization and cannabis-related emergency department visits by age, gender, and geographic status in Ontario, Canada: an interrupted time series study. PLoS One. 2022;17:e0268718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Wang GS, Buttorff C, Wilks A, et al. Cannabis legalization and cannabis-involved pregnancy hospitalizations in Colorado. Prev Med. 2022;156:106993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Baraniecki R, Panchal P, Malhotra DD, Aliferis A, Zia Z. Acute cannabis intoxication in the emergency department: the effect of legalization. BMC Emerg Med. 2021;21:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Myran DT, Pugliese M, Tanuseputro P, Cantor N, Rhodes E, Taljaard M. The association between recreational cannabis legalization, commercialization and cannabis-attributable emergency department visits in Ontario, Canada: an interrupted time–series analysis. Addiction. 2022;117:1952-1960. [DOI] [PubMed] [Google Scholar]
- 80.Myran DT, Roberts R, Pugliese M, Taljaard M, Tanuseputro P, Pacula RL. Changes in emergency department visits for cannabis hyperemesis syndrome following recreational cannabis legalization and subsequent commercialization in Ontario, Canada. JAMA Netw Open. 2022;5:e2231937-e2231937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Mennis J, Stahler GJ. Adolescent treatment admissions for marijuana following recreational legalization in Colorado and Washington. Drug Alcohol Depend. 2022;210:107960. [DOI] [PubMed] [Google Scholar]
- 82.Delling FN, Vittinghoff E, Dewland TA, et al. Does cannabis legalisation change healthcare utilisation? A population-based study using the healthcare cost and utilisation project in Colorado, USA. BMJ Open. 2019;9:e027432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Callaghan RC, Sanches M, Murray RM, Konefal S, Maloney-Hall B, Kish SJ. Associations between Canada’s cannabis legalization and emergency department presentations for transient cannabis-induced psychosis and schizophrenia conditions: Ontario and Alberta, 2015–2019. Can J Psychiatry. 2022;67:616-625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Sokoya M, Eagles J, Okland T, et al. Patterns of facial trauma before and after legalization of marijuana in Denver, Colorado: A joint study between two Denver hospitals. Am J Emerg Med. 2018;36:780-783. [DOI] [PubMed] [Google Scholar]
- 85.Lopez CD, Boddapati V, Jobin CM, Hickernell TR. State medical cannabis laws associated with reduction in opioid prescriptions by orthopaedic surgeons in Medicare Part D cohort. J Am Acad Orthop Surg. 2021;29:e188-e197. [DOI] [PubMed] [Google Scholar]
- 86.Shi Y, Liang D, Bao Y, An R, Wallace MS, Grant I. Recreational marijuana legalization and prescription opioids received by Medicaid enrollees. Drug Alcohol Depend. 2019;194:13-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Livingston MD, Barnett TE, Delcher C, Wagenaar AC. Recreational cannabis legalization and opioid-related deaths in Colorado, 2000-2015. Am J Public Health. 2017;107:1827-1829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Dranitsaris G, DeAngelis C, Pearson B, McDermott L, Pohlmann-Eden B. Opioid prescribing in Canada following the legalization of cannabis: A clinical and economic time-series analysis. Appl Health Econ Health Policy. 2021;19:537-544. [DOI] [PubMed] [Google Scholar]
- 89.Siega-Riz AM, Keim-Malpass J, Lyons GR, Alhusen J. The association between legalization of recreational marijuana use and birth outcomes in Colorado and Washington state. Birth Defects Res. 2020;112:660-669. [DOI] [PubMed] [Google Scholar]
- 90.Straub HL, Mou J, Drennan KJ, Pflugeisen BM. Maternal marijuana exposure and birth weight: an observational study surrounding recreational marijuana legalization. Am J Perinatol. 2021;38:65-75. [DOI] [PubMed] [Google Scholar]
- 91.Rusby JC, Westling E, Crowley R, Mills KL, Light JM. Associations between marijuana use and anxious mood lability during adolescence. Addict Behav. 2019;92:89-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Fedorova EV, Ataiants J, Wong CF, Iverson E, Lankenau SE. Changes in medical cannabis patient status before and after cannabis legalization in California: Associations with cannabis and other drug use. J Psychoactive Drugs. 2022;54:129-139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Jordan A, Sherazi A, Flewelling AJ, Northrup V, Naseemuddin A, Shea JL. Identification of cannabinoids in post-mortem blood samples from the province of New Brunswick before and after recreational cannabis legalization. Int J Drug Policy. 2022;103:103629. [DOI] [PubMed] [Google Scholar]
- 94.Aydelotte JD, Brown LH, Luftman KM, et al. Crash fatality rates after recreational marijuana legalization in Washington and Colorado. Am J Public Health. 2017;107:1329-1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Aydelotte JD, Mardock AL, Mancheski CA, et al. Fatal crashes in the 5 years after recreational marijuana legalization in Colorado and Washington. Accid Anal Prev. 2019;132:105284. [DOI] [PubMed] [Google Scholar]
- 96.Borst JM, Costantini TW, Reilly L, et al. Driving under the influence: A multi-center evaluation of vehicular crashes in the era of cannabis legalization. Trauma Surg Acute Care Open. 2021;6(1):e000736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Lane TJ, Hall W. Traffic fatalities within US states that have legalized recreational cannabis sales and their neighbours. Addiction. 2019;114:847-856. [DOI] [PubMed] [Google Scholar]
- 98.Brubacher JR, Chan H, Erdelyi S, Staples JA, Asbridge M, Mann RE. Cannabis legalization and detection of tetrahydrocannabinol in injured drivers. N Engl J Med. 2022;386:148-156. [DOI] [PubMed] [Google Scholar]
- 99.Nazif-Munoz JI, Oulhote Y, Ouimet MC. The association between legalization of cannabis use and traffic deaths in Uruguay. Addiction. 2020;115:1697-1706. [DOI] [PubMed] [Google Scholar]
- 100.Firth CL, Maher JE, Dilley JA, Darnell A, Lovrich NP. Did marijuana legalization in Washington state reduce racial disparities in adult marijuana arrests? Subst Use Misuse. 2019;54:1582-1587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Firth CL, Hajat A, Dilley JA, Braun M, Maher JE. Implications of cannabis legalization on juvenile justice outcomes and racial disparities. Am J Prev Med. 2020;58:562-569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Callaghan RC, Vander Heiden J, Sanches M, Asbridge M, Hathaway A, Kish SJ. Impacts of Canada’s cannabis legalization on police-reported crime among youth: Early evidence. Addiction. 2021;116:3454-3462. [DOI] [PubMed] [Google Scholar]
- 103.El Marroun H, Brown QL, Lund IO, et al. An epidemiological, developmental and clinical overview of cannabis use during pregnancy. Prev Med. 2018; 116:1-5. [DOI] [PubMed] [Google Scholar]
- 104.Rotermann M. Analysis of trends in the prevalence of cannabis use and related metrics in Canada. Health Rep. 2019;30:3-13. [DOI] [PubMed] [Google Scholar]
- 105.Lemyre A, Poliakova N, Bélanger RE. The relationship between tobacco and cannabis use: A review. Subst Use Misuse. 2019;54:130-145. [DOI] [PubMed] [Google Scholar]
- 106.Parker MA, Anthony JC. Population-level predictions from cannabis risk perceptions to active cannabis use prevalence in the United States, 1991-2014. Addict Behav. 2018;82:101-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Burdzovic Andreas J, Sivertsen B, Lønning KJ, Skogen JC. Cannabis use among Norwegian university students: Gender differences, legalization support and use intentions, risk perceptions, and use disorder. Addict Behav Rep. 2021;13:100339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Strickler GK, Kreiner PW, Halpin JF, Doyle E, Paulozzi LJ. Opioid prescribing behaviors — prescription behavior surveillance system, 11 states, 2010–2016. MMWR Surveill Summ. 2020;69:1-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Golub A, Johnson BD, Dunlap E. The race/ethnicity disparity in misdemeanor marijuana arrests in New York City. Criminol Public Policy. 2007;6:131-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Owusu-Bempah A, Luscombe A. Race, cannabis and the Canadian war on drugs: an examination of cannabis arrest data by race in five cities. Int J Drug Policy. 2021;91:102937. [DOI] [PubMed] [Google Scholar]
- 111.Wildeman C, Wang EA. Mass incarceration, public health, and widening inequality in the USA. Lancet. 2017;389:1464-1474. [DOI] [PubMed] [Google Scholar]
- 112.Ng JY, Homayouni P, Usman S, Gomes Z. The medical cannabis regulatory framework in Canada: A narrative review. Eur J Integr Med. 2022;50:102104. [Google Scholar]
- 113.Scheim AI, Maghsoudi N, Marshall Z, Churchill S, Ziegler C, Werb D. Impact evaluations of drug decriminalisation and legal regulation on drug use, health and social harms: A systematic review. BMJ Open. 2020;10:e035148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Williams J, Bretteville-Jensen AL. Does liberalizing cannabis laws increase cannabis use? J Health Econ. 2014;36:20-32. [DOI] [PubMed] [Google Scholar]