Abstract
Blood biomarkers have been considered tools for the diagnosis, prognosis, and monitoring of Alzheimer’s disease (AD). Although amyloid-β peptide (Aβ) and tau are primarily blood biomarkers, recent studies have identified other reliable candidates that can serve as measurable indicators of pathological conditions. One such candidate is the glial fibrillary acidic protein (GFAP), an astrocytic cytoskeletal protein that can be detected in blood samples. Increasing evidence suggests that blood GFAP levels can be used to detect early-stage AD. In this systematic review and meta-analysis, we aimed to evaluate GFAP in peripheral blood as a biomarker for AD and provide an overview of the evidence regarding its utility. Our analysis revealed that the GFAP level in the blood was higher in the Aβ-positive group than in the negative groups, and in individuals with AD or mild cognitive impairment (MCI) compared to the healthy controls. Therefore, we believe that the clinical use of blood GFAP measurements has the potential to accelerate the diagnosis and improve the prognosis of AD.
Keywords: Alzheimer’s disease, cognitive impairment, glial fibrillary acidic protein, GFAP, blood biomarker
1. Introduction
Alzheimer’s disease (AD) is a progressive neurodegenerative disorder, clinically manifested by cognitive deterioration and behavioral disruptions [1]. Over the past few decades, several attempts have been made to identify accurate blood biomarkers for AD. However, differentiating AD from numerous dementia-causing neuropathologies remains difficult [2,3,4,5]. An optimal blood biomarker for AD would exhibit characteristics, such as reliability, reproducibility, non-invasiveness, ease of measurement, and cost-effectiveness [1]. Moreover, it is very important to discover potential targets for developing molecular markers and verifying their effectiveness in the early detection of AD, ultimately leading to improved treatment approaches and better results for patients [6]. AD, predicted to affect more than 152 million people by 2050, is now recognized as common senile dementia with main pathological hallmarks, such as extracellular neuritic plaques containing amyloid-β peptide (Aβ) and intracellular neurofibrillary tangles composed of hyper phosphorylated tau [7].
Some proteins related to the two biomarkers detected in the peripheral blood are attractive candidates for AD diagnosis [8,9,10,11,12] because they are contained in the amyloid cascade hypothesis, which introduces the idea that Aβ misfolding and deposition are the primary precipitants of AD [4,5]. These proteins include 1) single-type proteins such as Aβ40, Aβ42, Aβ oligomers (AβO), total tau (t-tau), tau phosphorylated at threonine 181 (p-tau 181), tau phosphorylated at threonine 217 (p-tau 217), or tau phosphorylated at threonine 231 (p-tau 231) and 2) combined types, such as the Aβ42/Aβ40 ratio, the ratio of amyloid precursor protein669-771 (APP669-771) to Aβ42 (Aβ42/APP669-771 ratio), the Aβ42/Aβ43 ratio, the t-tau/Aβ42 ratio, or the p-tau 181/Aβ42 ratio [8,9,10,11,12]. However, controversy exists regarding the plausibility of the amyloid cascade hypothesis [3,13,14]. Therefore, many researchers have suggested alternative hypotheses that place other proteins or processes, such as neuroinflammation, as the central initiating mechanisms of AD pathogenesis [5,15,16,17,18].
Apart from the Aβ and tau proteins, recent studies have identified other candidates for AD, such as the neurofilament light (NFL) protein, brain-derived neurotrophic factor (BDNF), clusterin, glial fibrillary acidic protein (GFAP), and neurogranin [9,12,19]. GFAP is an astrocytic cytoskeleton intermediate filament protein. The expression and concentrations of GFAP are higher in areas surrounding Aβ plaques and increased with tau accumulation in the brains of patients with AD [20,21]. In pathological situations, astrocytes undergo a series of morphological and functional alterations collectively referred to as reactive astrocytes and overexpress proteins, such as GFAP [22]. Reactive astrocytes contribute to neuroinflammatory changes in AD by releasing cytokines, inflammatory mediators, nitric oxide, and reactive oxygen species and promoting redox status imbalance [23]. Previous studies have shown that reactive astrocytes can precede early pathological hallmarks of AD, such as Aβ and tau, during disease progression [24,25,26,27,28,29,30].
GFAP has recently attracted attention because of preliminary evidence indicating a better performance of the plasma biomarker than its CSF counterpart in detecting AD pathology [31]. Plasma GFAP more accurately discriminated Aβ-positive from Aβ-negative individuals than CSF GFAP (area under the curve for plasma GFAP, 0.69–0.86; area under the curve for CSF GFAP, 0.59–0.76) [32]. Serum GFAP levels were increased in AD and correlated with the Mini-Mental State Examination (MMSE) score [33]. Therefore, GFAP may be a sensitive blood biomarker for detecting and tracking reactive astrogliosis and Aβ pathology [32]. For this reason, we focused on the relationship between blood GFAP and AD and aimed to evaluate GFAP in the peripheral blood as a biomarker for AD by conducting a systematic review and meta-analysis and discussing the possibility of GFAP as an AD blood biomarker.
2. Materials and Methods
2.1. Literature Search and Selection Criteria
A literature search was performed on PubMed, Embase, Web of Science, and the Cochrane Library on 19 September 2022. All previous papers written in English were included in this study. This study was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [34]. For PubMed, we used the following search terms: (AD [MeSH] or Alzheimer* or “mild cognitive impairment”) and (glial fibrillary acidic protein [MeSH] or GFAP) and (blood, plasma, or serum). The following terms were used for the other databases: Alzheimer* or “mild cognitive impairment” and “glial fibrillary acidic protein” or GFAP, and blood, plasma, or serum. The inclusion criterion was a clinical study using human blood samples to assess the GFAP levels between AD and normal controls, or Aβ-positive and Aβ-negative groups. The human blood GFAP level was measured with single-molecule arrays in most studies. In our study, both the AD and normal control groups, as well as the Aβ-positive and Aβ-negative groups, were classified based on each original study. The Aβ status was determined through Aβ PET imaging. The exclusion criteria were (1) studies with disease groups other than AD; (2) studies that did not include the GFAP level in the analysis group; (3) studies that used cell, tissue, or animal models; and (4) commentaries, letters, editorials, conference abstracts, or reviews.
2.2. Data Extraction and Analysis
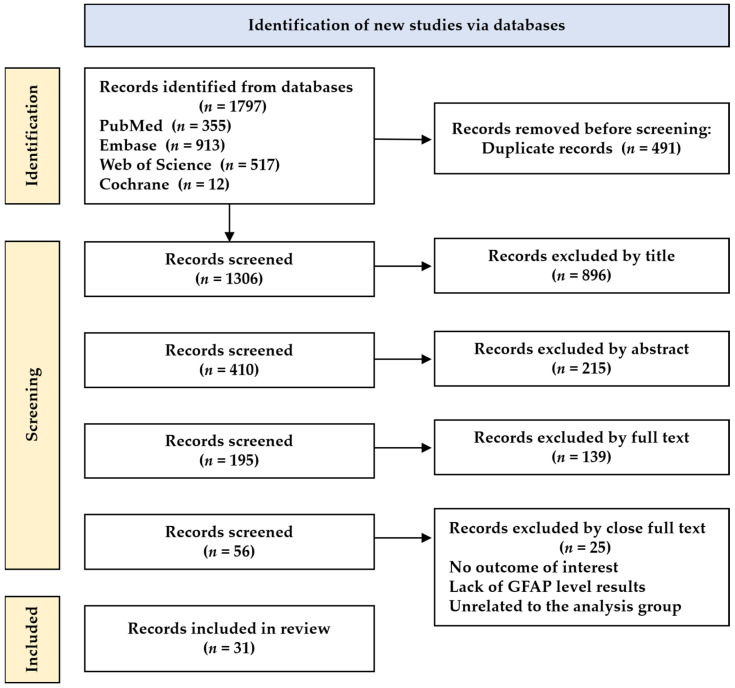
Two authors (K.Y. Kim and K.-A. Chang) independently reviewed the articles, and disagreements were resolved via a discussion by all authors. Among the 1797 studies, 31 were selected based on the title, abstract, and full text. The following data were extracted from the selected studies: first author’s last name, year, country of participants, analyzed group, total sample size by dividing female and male, mean age, blood sample type, and GFAP level in the analyzed group. For the meta-analysis, the standardized mean difference (SMD) of the GFAP level was analyzed between the AD and normal control groups or the Aβ-positive and Aβ-negative groups using comprehensive meta-analysis software version 3 (Biostats Inc., Englewood, NJ, USA). After analyzing the Q statistic and I2 method to assess the heterogeneity, a random-effects model was used. Publication bias was evaluated using funnel plots and Egger’s intercept test. Statistical significance was defined as p < 0.05.
3. Results
3.1. Characteristics of the Selected Studies
Figure 1 illustrates the literature search and selection process. A total of 1797 studies were screened, including 355 from PubMed, 913 from Embase, 517 from Web of Science, and 12 from the Cochrane databases. After removing duplicates and irrelevant studies, 31 articles were finally subjected to data extraction. Table 1 presents the articles evaluating the blood GFAP levels in patients with AD. In total, 87.5% of the selected articles were published in the last two years, 2021–2022. The participants were from various countries, including the USA, Canada, Spain, France, Italy, Germany, Australia, the UK, Sweden, the Netherlands, Finland, Greece, and Poland. The groups used in the analysis were controls (healthy controls, cognitively unimpaired individuals, etc.), and AD, and Aβ-negative and Aβ-positive groups. The sample sizes of the case and control groups ranged from 8 to 1439. The patients’ sexes and mean ages for each included study are illustrated in Table 1. The GFAP plasma or serum levels were presented in pg/mL in the control and case groups.
Figure 1.
Flowchart of the literature search.
Table 1.
Characteristics of selected studies.
| Author, Year | Country (Cohort) | Analyzed Group | N (M/F or Female, %) |
Age (Mean (SD or Range or IQR)) |
Blood | GFAP (Mean (SD or IQR)) |
|||
|---|---|---|---|---|---|---|---|---|---|
| Control | Case | Control | Case | Control | Case | ||||
| Asken, 2021 [35] | USA | CN/MCI (Cohort1) | 39 (78%) | 11 (22%) | 72.7 (6.3) | 70.7 (8.6) | Plasma | 183 (140, 242), | 213 (168, 254) |
| CN/MCI/AD (Cohort2) | 32 (45%) | MCI: 18 (25%)/ AD: 21 (30%) |
75.4 (4.6) | MCI: 70.4 (11.2)/AD: 68.9 (11.2) | Plasma | 110 (75, 184) | MCI: 172 (151, 233)/AD: 167 (137, 265) | ||
| Benedet, 2021 [32] | Canada (TRIAD) | CU Aβ−/CU+ Aβ+/MCI Aβ+/AD | CU Aβ−: 114 (41/73)/CU Aβ+: 42 (13/29) | MCI Aβ+: 39 (18/21)/AD: 45 (24/21) | CU Aβ−: 69.9 (9.4)/CU Aβ+: 4.1 (7.7) | MCI Aβ+: 71.2 (7.7)/AD: 66.1 (9.7) | Plasma | CU Aβ−: 185.1 (93.5)/CU Aβ+: 285.0 (142.6) | MCI Aβ+: 332.5 (153.6)/AD: 388.1 (152.8) |
| Aβ− Aβ+ | Aβ−: 185.1 (95.5) | Aβ+: 285.0 (142.6) | |||||||
| Spain (ALFA) | CU−/CU+ | CU−: 249 (96/153)/CU+: 135 (54/81) | CU−: 60.5 (4.50)/ CU+: 62.2 (4.9) |
Plasma | CU−: 121.9 (42.4)/CU+: 169.9 (78.5) | ||||
| France (BioCogBank) |
CU Aβ−/MCI Aβ+/AD | 21 (7/14) | MCI Aβ+: 42 (16/26)/AD: 76 (39/47) | 64.4 (9.5) | MCI Aβ+: 72.4 (7.9)/AD: 72.2 (8.4) | Plasma | 161.2 (67.1) | MCI Aβ+: 368.6 (158.5)/AD: 376.4 (179.6) | |
| Benedet, 2022 [36] | USA/Canada (ADNI) | Aβ−/Aβ+ | 58 (34/24) | 60 (34/26) | 70.8 (66.5, 75.7) | 73.8 (69.9, 77.4) | Plasma | 113 (80.7, 154) | 164 (125, 223) |
| Benussi, 2020 [37] | Italy | HC/AD | 61 (20.6%) | 63 (31.7%) | 65.5 (12.3) | 75.5 (8.1) | Serum | 183.1 (93.7) | 394.8 (176.2) |
| Bettcher, 2022 [38] | USA | Asymptomatic/Symptomatic (MCI/AD) | 69 (21/48) | 45 (23/22) | 69.5 (6.4) | 71.7 (7.5) | Plasma | 148.1 (72.7) | 265.9 (125.6) |
| Beyer, 2022 [39] | Germany (ESTHER) | Con/AD (within 17 y) | 240 (114/126) | 68 (25/43) | 66.1 (4.6) | 68.8 (4.3) | Plasma | 99.6 (46.7) | 159.0 (111.1) |
| Chatterjee, 2021a [40] | Australia (KARVIAH) | Aβ−/Aβ+ | 63 (18/45) | 33 (13/20) | 77.41 (5.45) | 79.64 (5.20) | Plasma | 151.42 (58.49) | 240.12 (124.88) |
| Non-SMC Aβ−/Non-SMC Aβ+/SMC Aβ-/SMC Aβ+ | Non-SMC Aβ−: 14/Non-SMC Aβ+: 8 | SMC Aβ−: 49/SMC Aβ+: 25 | Non-SMC Aβ−: 146.83 (61.58)/Non-SMC Aβ+: 202.28 (63.81) | SMC Aβ−: 152.73 (58.18)/SMC Aβ+: 252.22 (137.75) | |||||
| Chatterjee, 2021b [41] | Australia (KARVIAH) | Aβ−/Aβ+ | 67 (19/48) | 33 (13/20) | 77.78 (5.56) | 79.00 (5.44) | 146.96 (49.48) | 211.39 (86.04) | |
| Chatterjee, 2022 [42] | Australia (AIBL) | SMCs Aβ−/SMCs Aβ+ | SMCs Aβ−: 52 (77.61%) | SMCs Aβ+: 24 (72.72%) | SMCs Aβ−: 147.85 (47.07) | SMCs Aβ+: 229.50 (93.49) | |||
| Chouliaras, 2022 [43] | UK (NIMROD/AMPLE/MIDAS/MILOS) | Con/MCI + AD | 73 (43/30) | 63 (43/20) | 70.2 (7.79) | 73.9 (7.80) | Plasma | 154 (96.5) | 243 (99.9) |
| LBD Aβ−/LBD Aβ+ | 30 (25/5) | 29 (23/6) | 73.9 (6.25) | 75.2 (6.75) | 179 (62.0) | 219 (85.9) | |||
| Cicognola, 2021 [44] | Sweden | Stable MCI Aβ−/Stable MCI Aβ+/MCI-AD Aβ+/MCI-other Aβ−/MCI-other Aβ+ | Stable MCI Aβ−: 58 (55%)/MCI-other Aβ-: 25 (44%) | Stable MCI Aβ+: 21 (48%)/MCI-AD Aβ+: 47 (75%)/MCI-other Aβ+: 9 (33%) | Stable MCI Aβ−: 69 (8)/MCI-other Aβ−: 73 (7) | Stable MCI Aβ+: 69 (6)/MCI-AD Aβ+: 76 (7)/MCI-other Aβ+: 74 (6) | Plasma | Stable MCI Aβ−: 36 (17)/MCI-other Aβ−: 42 (16) | Stable MCI Aβ+: 46 (25)/MCI-AD Aβ+: 67 (24)/MCI-other Aβ+: 52 (11) |
| Ebenau, 2022 [45] | Netherlands (ADC) | Stable/Progression | 337 (196/141), | 64 (38/26) | Serum | 190.8 (124.9) | 281.1 (128.6) | ||
| Frontera, 2021 [46] | USA (ADRC) | Normal/MCI/AD (COVID-19 patients) | 54 (19/35) | MCI: 54 (11/43)/AD: 53 (21/32) | 71 (65–76) | MCI: 77 (70–86)/AD: 82 (72–88) | Plasma | 111.4 | MCI: 152.5/AD: 257.1 |
| Gonzales, 2021 [47] | USA (TARCC) | CU/MCI/Dementia (Hispanic) | 711 (196/515) | MCI: 325(102/223)/Dementia: 157 (55/102) | 63 (8) | MCI: 70 (9)/Dementia: 75 (8) | Serum | 134 (98, 186) | MCI: 174 (120, 249)/Dementia: 279 (182, 432) |
| CU/MCI/Dementia (Non-Hispanic) | 184 (67/117) | MCI: 115 (62/52)/Dementia: 351 (162/189) | 72 (8) | MCI: 73 (9)/Dementia: 75 (9) | Serum | 206 (145, 367) | MCI: 253 (175, 380)/Dementia: 429 (308, 591) | ||
| Gonzales, 2022 [48] | USA (TARCC) | CU/MCI/Dementia | 479 (125/354) | MCI: 207 (67/140)/Dementia: 59 (20/39) | 63 (7) | MCI: 71 (8)/Dementia: 74 (8) | Serum | 136 (102, 189) | MCI: 179 (123, 261)/Dementia: 223 (160, 391) |
| Mila-Aloma, 2022 [49] | Spain (ALFA+) | Aβ−/Aβ+ | 262 (61.8) | 135 (60) | 60.6 (4.45) | 62.2 (4.91) | Plasma | 122 (42.8) | 170 (78.5) |
| Oeckl, 2022 [50] | Portugal/Netherlands/Germany | Con/MCI-AD/AD | 129 (66/63) | MCI-AD: 111 (47/64)/AD: 230 (91/139) | Con: 63 (57–69) | MCI-AD: 71 (64–74)/AD: 69 (62–76) | Serum | 167 (108–234) | MCI-AD: 300 (232–433)/AD: 375 (276–505) |
| Oeckl, 2019 [33] | Germany | Con/AD | 34 (25/9) | 28 (9/19) | 66 (57–74) | 71 (67–78) | Serum | 157 (126–218) | 376 (294–537) |
| Palmqvist, 2022 [51] | Germany (Panel A+ study) | Aβ−/Aβ+ | 117 (65/52) | 110 (48/62) | 63.6 (10.8) | 69.5 (7.9) | Plasma | 98.9 (86.3) | 155 (94) |
| Sweden (Swedish BioFINDER) |
Aβ−/Aβ+ | 403 (187/216) | 290 (137/153) | 71.9 (5.6) | 73.0 (5.3) | 89.6 (59) | 130 (67) | ||
| Parvizi, 2022 [52] | Austria | HC/MCI | 44 (20/24) | 63 (34/29) | 61.2 (55.8, 69.5) |
69.9 (59.3, 77.8) | Plasma | 79 (53.7, 120.6) | 167.5 (93.8, 256.3) |
| HC/AD | 60 (24/36) | 69 (61.3, 75) | 181.9 (129.6, 269.6) | ||||||
| Pereira, 2021 [53] | Sweden (Swedish BioFINDER-2) | CU Aβ−/CU Aβ+/CI Aβ+/CI Aβ− | CU Aβ−: 217 (98/119)/ | CI Aβ−: 63 (36/27) |
63.8 (41.2–87.9) | 67.9 (45.2–83.4) | Plasma | 179.6 (31.1–534.9) | 166.9 (24.5–476.0) |
| CU Aβ+: 71 (35/36) | CI Aβ+: 78 (34/44) | 72.1 (51.0–88.7) | 73.0 (53.7–93.3) | 252.1 (86.1–672.9) | 262.6 (94.0–650.7) | ||||
| Pichet Binette, 2022 [54] | Sweden | Non-progression to AD/Progression to AD | 84 (46/38) | 26 (12/14) | 71.52 (8.20) | 74.77 (8.12) | Plasma | 164.69 (117.31) | 251.30 (115.21) |
| Prins, 2022 [55] | Netherlands | Aβ−/Aβ+ | 50 (29/21) | 50 (33/17) | 71.88 (4.45) | 73.4 (4.72) | Plasma | 134.0 (50.71) | 195.1 (87.13) |
| Salvadó, 2022 [56] | Spain (ALFA+) | Aβ−Tau−/Aβ+Tau−/Aβ+Tau+ | Aβ−Tau−: 202 (72/130) | Aβ+Tau−: 88 (39/49)/Aβ+Tau−: 24 (7/17) | Aβ−Tau−: 60.5 (4.3) | Aβ+Tau−: 61.7 (5.1)/Aβ+Tau−: 64.3 (4.7) | Plasma | Aβ−Tau−:121 (42) | Aβ+Tau−: 153 (66)/Aβ+Tau+: 201 (53) |
| Shir, 2022 [57] | USA | Aβ−/Aβ+ | 99 (57/42) | 101 (44/57) | 75 (9) | 81 (8) | Plasma | 134 (65) | 197 (83) |
| Simrén, 2021 [58] | Finland/Italy/Greece/UK/Poland/France (Add NeuroMed) |
CU/MCI/AD | CU: 99 (46/53) | MCI: 107 (51/56)/AD: 103 (40/63) | CU:73 (6.14) | MCI: 74.47 (5.89)/AD: 76.35 (5.76) | Plasma | CU:125.23 (73.76) | MCI: 147.81 (81.14)/AD: 219.04 (136.1) |
| Simrén, 2022 [59] | Sweden | Aβ−/Aβ+ | 28 (17/11) | 21 (9/12) | 73.5 (62.8–76.3) | 73 (67.0–76.0) | Serum | 160 (115–282) | 231 (167–283) |
| Stevenson-Hoare, 2022 [60] | UK (ADCC) | Con/AD | 508 (221/287) | 1439 (748/691) | 82.2 (6.72) | 68.1 (8.03) | Plasma | 196 (85.3) | 215 (103) |
| Stocker, 2022 [61] | Germany (ESTHER) | Con/AD (0–17 y) | 507 (229/278) | 145 (56/89) | 61.2 (6.5) | 66.7 (5.2) | Plasma | 87.0 (46.7) | 133.3 (86.0) |
| Thijssen, 2022 [62] | Netherlands (Amsterdam Dementia) | Con/AD (Cohort1) | 40 (20/20) | 40 (20/20) | 56 (53–59) | 58 (55–59) | Plasma | 534 (342–693) | 1580 (1091–1970) |
| Con/AD (Cohort2) | 38 (18/20) | 38 (18/20) | 63 (59–66) | 63 (59–67) | 66.6 (47.1–85.9) | 119 (99.4–178) | |||
| Verberk, 2020 [63] | Netherlands (Amsterdam Dementia) | Aβ−/Aβ+ | 76 (49/27) | 176 (89/87) | 61 (9) | 63 (7) | Plasma | 96 (53) | 168 (77) |
Healthy controls (HC), subjective memory complainers (SMC), compressed subjective memory complainers (SMCs), semantic variant primary progressive aphasia (svPPA), clinically normal (CN), mild cognitive impairment (MCI), Alzheimer’s disease (AD), cognitively unimpaired (CU), glial fibrillary acidic protein (GFAP), Aβ-negative cognitively unimpaired (CU−), Aβ-positive cognitively unimpaired (CU+), Aβ-positive mild cognitive impairment (MCI+), control (Con), age: years, GFAP: pg/mL.
3.2. Association between GFAP and AD or Aβ-Positive Group
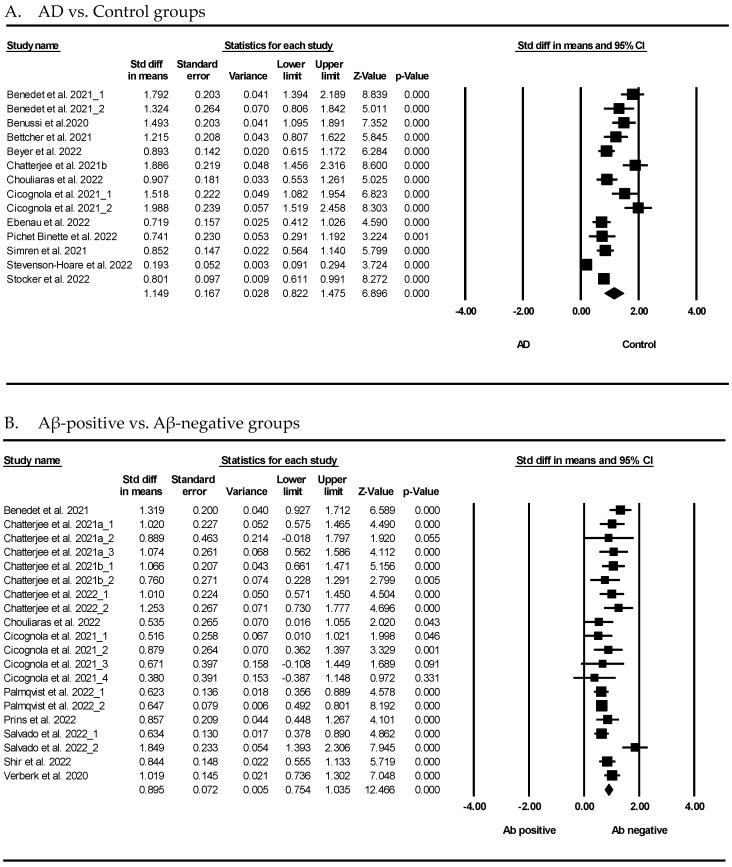
Figure 2 presents the results of the meta-analysis, demonstrating the association between GFAP and AD. As shown in Figure 2A, the GFAP levels showed that patients with AD had a significant difference compared to the normal controls (SMD = 1.149, 95% confidence interval (CI) = 0.822 to 1.475, p < 0.001). The random-effects model was used because the heterogeneity was significant (I2 = 94.32%, p < 0.001). Furthermore, GFAP showed that the Aβ-positive group had a significant difference compared to the Aβ-negative group in Figure 2B (SMD = 0.895, 95% CI = 0.754 to 1.035, p < 0.001). Considering the heterogeneity, a random-effects model was used (I2 = 59.76%, p < 0.001).
Figure 2.
Forest plots of the GFAP levels in the blood of subjects with Alzheimer’s disease (AD) and those who tested positive for Aβ. (A) GFAP levels in AD and control, (B) GFAP levels in Aβ-positive and Aβ-negative subjects. The forest plots describe the statistical parameters and effect size of each comparison, and quantitatively synthesized results. Black square represents the odds ratio, as calculated for each study and horizontal bars show the 95% CI of each study. The black rhombus represents the confidence limits. GFAP: pg/mL, Std diff: standard difference, CI: confidence interval.
3.3. Association between GFAP and Mild Cognitive Impairment (MCI)
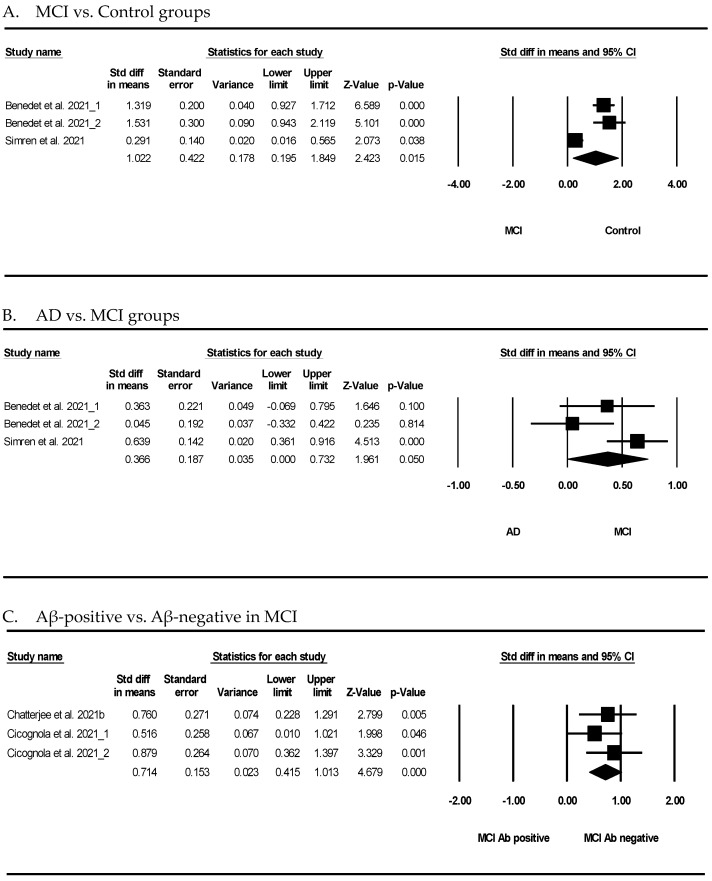
Figure 3 shows the results of the meta-analysis for the potential association between GFAP and MCI. As shown in Figure 3A, the meta-analysis of GFAP showed that the participants with MCI had a significant difference compared to the normal controls (SMD = 1.022, 95% CI = 0.195 to 1.849, p = 0.015). GFAP showed that AD was not significantly different compared to MCI (SMD = 0.366, 95% CI = 0.000 to 0.732, p = 0.050) (Figure 3B). Furthermore, GFAP showed that the Aβ-positive subjects had a significant difference compared to the Aβ-negative subjects in MCI (SMD = 0.714, 95% CI = 0.415 to 1.013, p < 0.001) (Figure 3C).
Figure 3.
Forest plots of the GFAP levels in the blood of subjects with mild cognitive impairment (MCI). (A) GFAP levels in MCI and control, (B) GFAP levels in AD and MCI, and (C) GFAP levels in Aβ-positive and Aβ-negative subjects. The forest plots describe the statistical parameters and effect size of each comparison, and quantitatively synthesized results. Black square represents the odds ratio, as calculated for each study and horizontal bars show the 95% CI of each study. The black rhombus represents the confidence limits. Std diff: standard difference, CI: confidence interval.
4. Discussion
Blood biomarkers can be used as diagnostic, prognostic, and disease-monitoring tools for AD [14,64,65]. The utilization of biomarkers from peripheral blood presents several benefits for AD diagnosis, including minimal invasiveness, ease of sampling, cost-effectiveness, time-efficiency, and widespread adoption [14,64,65]. Although developing blood diagnostic assays for AD remains challenging owing to the lack of specific biomarkers, methodological inconsistencies, and insufficient standardization of assays, it is an interesting field where many theoretical and clinical screening approaches can be realized [66,67,68,69].
GFAP is a blood biomarker that has recently gained attention in AD research. GFAP is primarily found in astrocytes, a type of glial cell in the brain. GFAP is expressed at a low level in healthy people but is markedly elevated in the brains of patients with AD. Several studies have investigated the potential of GFAP as a biomarker for AD, with promising results. A systematic review and meta-analysis demonstrated that GFAP might be a potential blood biomarker for AD. As shown in Figure 2, the blood GFAP levels in the AD group were significantly higher than those in the control group. GFAP was not only detectable in the blood of AD patients but also discriminated between the AD and control groups. There are several advantages to GFAP as a useful biomarker for AD. First, the use of blood GFAP as an AD biomarker has increased because the possibility of more sensitive assays has made it available for measurement in the blood. As detection techniques, such as the state-of-the-art single-molecule array (Simoa), have advanced quickly, accumulated results have verified that GFAP can diagnose AD patients. Interestingly, many studies have reported that plasma GFAP distinguished between patients with AD and cognitively normal individuals during the last three years (Table 1). It has been revealed that plasma GFAP concentrations correlate strongly with cerebral Aβ pathology [5,40,63]. The rate of change in GFAP concentrations was significantly higher among individuals who developed clinical AD than those with no cognitive impairment [70]. In our meta-analysis, the GFAP levels in patients with AD were also significantly higher than those in normal individuals. This evidence was confirmed in various nations, such as the United States, Italy, Germany, Sweden, Austria, and England (Table 1).
Second, GFAP is a highly brain-specific protein. The blood of healthy individuals has a very low level of GFAP protein [71,72]. In the brain of patients with AD, gliosis is marked by an increase in activated microglia and reactive astrocytes near the sites of Aβ plaques [73,74], and astrocyte disruption results in the easy release of GFAP from the tissue into the blood [75]. This is also supported by a plethora of evidence highlighting that the integrity of the blood–brain barrier is abnormal in AD, resulting in the microvascular leakage of proteins into the blood [76]. To determine the accuracy of blood GFAP in discriminating between individuals who are PET positive and those who are PET negative using specific Aβ, the area under the curve (AUC) was calculated and ranged from 0.69 to 0.86, indicating GFAP’s greater discriminatory power [32,42,53]. Therefore, it is possible to detect elevated blood GFAP levels as a useful diagnostic indicator of AD [77,78].
Third, a detection system including GFAP may become a tracking tool for the disease progression course and the prognosis and diagnosis of AD. In other words, this biomarker could track the therapeutic effect of developed AD therapeutic agents or the severity of AD in patients. Because inflammation occurs in pathologically vulnerable AD regions, it is possible to develop anti-inflammatory therapeutics for AD or delay the progression and onset of this ruinous disorder [79]. Therefore, blood GFAP may be a good candidate for AD diagnosis and prognosis.
Fourth, blood GFAP levels can be useful in detecting MCI and AD. In a clinical study, the increase in serum GFAP levels correlated with the MMSE score, extensively used to measure cognitive impariment [33,73]. Plasma GFAP can predict the subsequent conversion of MCI to AD [5,44]. Plasma GFAP concentrations have been shown to correlate strongly with decreased cognitive function [5,33,80]. Another review mentioned that blood GFAP was useful as an additional marker for the early detection and prediction of the time course of AD [81] and as a biomarker to predict MCI-to-dementia conversion [50].
This review found a meaningful trend in the blood GFAP concentrations between the controls and patients with MCI and AD though the result was not statistically significant (p = 0.050) (Figure 3). It may be demonstrated that blood GFAP should be considered for a more robust determination of the Aβ burden in cognitively unimpaired people [36].
Nevertheless, the challenges of using GFAP as an AD blood biomarker should be considered. GFAP is a commonly used marker of astroglial activation because of its markedly increased expression in most pathological conditions, including neurodegeneration and injuries [82,83]. Elevated blood GFAP concentrations have been observed not only in AD but also in various other neurodegenerative and non-neurodegenerative neurological conditions [84,85,86]. Blood GFAP levels are correlated with the clinical severity and extent of intracranial pathology in spinal cord disorders, acute CNS trauma, ischemia, neurodegenerative diseases, malignant brain tumors, and cerebrovascular events [49,82,87,88]. Therefore, it is important to determine the specificity of GFAP-related AD pathology.
In addition, we cannot assert that GFAP is more attractive than other well-known candidates such as Aβ, tau, APP, NFL, or BDNF, because research comparing their effectiveness as biomarkers is scarce. Some researchers have enumerated the effects of various proteins rather than suggesting their superiority [55,89]. A solution to this dilemma is as follows: the present trend is a mix of some candidates for AD diagnosis with or without GFAP. A few mixtures might be useful to discriminate AD: a combination of plasma p-tau181, NFL, and GFAP [62], and a combination of Aβ misfolding and GFAP [39]. Furthermore, co-detecting Aβ42/Aβ40, p-tau181, and ApoE4 improved the areas under the curve significantly (0.90 to 0.93; p < 0.01) in Aβ-positive versus Aβ-negative participants [51].
This study had some limitations. First, we obtained limited results because we only used data from the papers in this study. Second, our results included the control and AD groups regardless of AD stage. Therefore, further research is required to analyze the stages of AD and MCI. Third, this study included overlapping authors and cohort data among the selected articles; therefore, it needs to be considered in the interpretation of the results. Nevertheless, our study demonstrated that the levels of GFAP were remarkably changed in the blood of patients with AD. Therefore, GFAP could be a potential biomarker for diagnosis, prognosis prediction, and progression evaluation of AD, especially in relation to brain damage and cognitive impairment. As research advances, using GFAP as a blood biomarker for AD may become a valuable tool for diagnosing this devastating disease.
Author Contributions
Conceptualization, K.-A.C. and K.Y.K.; formal analysis, K.-A.C. and K.Y.K.; investigation, K.Y.S.; writing—original draft, K.Y.S. and K.Y.K.; writing—review and editing, K.Y.S. and K.-A.C.; supervision, K.-A.C.; project administration, K.-A.C.; funding acquisition, K.-A.C. All authors have read and agreed to the published version of the manuscript.
Data Availability Statement
The data supporting the findings of this study are available from the corresponding authors upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was supported by a National Research Foundation of Korea (NRF) grant funded by the Ministry of Education (No. 2022R1A2C1092597) and by the Basic Science Research Program through the NRF of Korea funded by the Ministry of Education (2020R1I1A1A01070793). The funders had no role in the study design, data collection and analysis, decision to publish, or manuscript preparation.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Molinuevo J.L., Ayton S., Batrla R., Bednar M.M., Bittner T., Cummings J., Fagan A.M., Hampel H., Mielke M.M., Mikulskis A., et al. Current state of Alzheimer’s fluid biomarkers. Acta Neuropathol. 2018;136:821–853. doi: 10.1007/s00401-018-1932-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hane F.T., Robinson M., Lee B.Y., Bai O., Leonenko Z., Albert M.S. Recent Progress in Alzheimer’s Disease Research, Part 3: Diagnosis and Treatment. J. Alzheimers Dis. 2017;57:645–665. doi: 10.3233/JAD-160907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang J., Gu B.J., Masters C.L., Wang Y.J. A systemic view of Alzheimer disease—Insights from amyloid-beta metabolism beyond the brain. Nat. Rev. Neurol. 2017;13:612–623. doi: 10.1038/nrneurol.2017.111. [DOI] [PubMed] [Google Scholar]
- 4.Hardy J.A., Higgins G.A. Alzheimer’s disease: The amyloid cascade hypothesis. Science. 1992;256:184–185. doi: 10.1126/science.1566067. [DOI] [PubMed] [Google Scholar]
- 5.Alawode D.O.T., Fox N.C., Zetterberg H., Heslegrave A.J. Alzheimer’s Disease Biomarkers Revisited From the Amyloid Cascade Hypothesis Standpoint. Front. Neurosci. 2022;16:837390. doi: 10.3389/fnins.2022.837390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guzman-Martinez L., Maccioni R.B., Farias G.A., Fuentes P., Navarrete L.P. Biomarkers for Alzheimer’s Disease. Curr. Alzheimer Res. 2019;16:518–528. doi: 10.2174/1567205016666190517121140. [DOI] [PubMed] [Google Scholar]
- 7.O’Brien R.J., Wong P.C. Amyloid precursor protein processing and Alzheimer’s disease. Annu. Rev. Neurosci. 2011;34:185–204. doi: 10.1146/annurev-neuro-061010-113613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zou K., Abdullah M., Michikawa M. Current Biomarkers for Alzheimer’s Disease: From CSF to Blood. J. Pers. Med. 2020;10:85. doi: 10.3390/jpm10030085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Auso E., Gomez-Vicente V., Esquiva G. Biomarkers for Alzheimer’s Disease Early Diagnosis. J. Pers. Med. 2020;10:114. doi: 10.3390/jpm10030114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Verde F. Tau proteins in blood as biomarkers of Alzheimer’s disease and other proteinopathies. J. Neural Transm. 2022;129:239–259. doi: 10.1007/s00702-022-02471-y. [DOI] [PubMed] [Google Scholar]
- 11.Kulichikhin K.Y., Fedotov S.A., Rubel M.S., Zalutskaya N.M., Zobnina A.E., Malikova O.A., Neznanov N.G., Chernoff Y.O., Rubel A.A. Development of molecular tools for diagnosis of Alzheimer’s disease that are based on detection of amyloidogenic proteins. Prion. 2021;15:56–69. doi: 10.1080/19336896.2021.1917289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mankhong S., Kim S., Lee S., Kwak H.B., Park D.H., Joa K.L., Kang J.H. Development of Alzheimer’s Disease Biomarkers: From CSF- to Blood-Based Biomarkers. Biomedicines. 2022;10:850. doi: 10.3390/biomedicines10040850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Morris G.P., Clark I.A., Vissel B. Inconsistencies and controversies surrounding the amyloid hypothesis of Alzheimer’s disease. Acta Neuropathol. Commun. 2014;2:135. doi: 10.1186/s40478-014-0135-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim K.Y., Shin K.Y., Chang K.A. Brain-Derived Exosomal Proteins as Effective Biomarkers for Alzheimer’s Disease: A Systematic Review and Meta-Analysis. Biomolecules. 2021;11:980. doi: 10.3390/biom11070980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alvarez A., Toro R., Caceres A., Maccioni R.B. Inhibition of tau phosphorylating protein kinase cdk5 prevents beta-amyloid-induced neuronal death. FEBS Lett. 1999;459:421–426. doi: 10.1016/S0014-5793(99)01279-X. [DOI] [PubMed] [Google Scholar]
- 16.Alvarez R., Alvarez V., Lahoz C.H., Martinez C., Pena J., Sanchez J.M., Guisasola L.M., Salas-Puig J., Moris G., Vidal J.A., et al. Angiotensin converting enzyme and endothelial nitric oxide synthase DNA polymorphisms and late onset Alzheimer’s disease. J. Neurol. Neurosurg. Psychiatry. 1999;67:733–736. doi: 10.1136/jnnp.67.6.733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ittner L.M., Gotz J. Amyloid-beta and tau--a toxic pas de deux in Alzheimer’s disease. Nat. Rev. Neurosci. 2011;12:65–72. doi: 10.1038/nrn2967. [DOI] [PubMed] [Google Scholar]
- 18.Guzman-Martinez L., Maccioni R.B., Andrade V., Navarrete L.P., Pastor M.G., Ramos-Escobar N. Neuroinflammation as a Common Feature of Neurodegenerative Disorders. Front. Pharmacol. 2019;10:1008. doi: 10.3389/fphar.2019.01008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Blennow K. A Review of Fluid Biomarkers for Alzheimer’s Disease: Moving from CSF to Blood. Neurol. Ther. 2017;6:15–24. doi: 10.1007/s40120-017-0073-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Simpson J.E., Ince P.G., Lace G., Forster G., Shaw P.J., Matthews F., Savva G., Brayne C., Wharton S.B., Function M.R.C.C., et al. Astrocyte phenotype in relation to Alzheimer-type pathology in the ageing brain. Neurobiol. Aging. 2010;31:578–590. doi: 10.1016/j.neurobiolaging.2008.05.015. [DOI] [PubMed] [Google Scholar]
- 21.Teunissen C.E., Verberk I.M.W., Thijssen E.H., Vermunt L., Hansson O., Zetterberg H., van der Flier W.M., Mielke M.M., Del Campo M. Blood-based biomarkers for Alzheimer’s disease: Towards clinical implementation. Lancet Neurol. 2022;21:66–77. doi: 10.1016/S1474-4422(21)00361-6. [DOI] [PubMed] [Google Scholar]
- 22.Wilhelmsson U., Bushongt E.A., Price D.L., Smarr B.L., Phung V., Terada M., Ellisman M.H., Pekny M. Redefining the concept of reactive astrocytes as cells that remain within their unique domains upon reaction to injury. Proc. Natl. Acad. Sci. USA. 2006;103:17513–17518. doi: 10.1073/pnas.0602841103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Heneka M.T., Rodriguez J.J., Verkhratsky A. Neuroglia in neurodegeneration. Brain Res. Rev. 2010;63:189–211. doi: 10.1016/j.brainresrev.2009.11.004. [DOI] [PubMed] [Google Scholar]
- 24.Carter S.F., Scholl M., Almkvist O., Wall A., Engler H., Langstrom B., Nordberg A. Evidence for astrocytosis in prodromal Alzheimer disease provided by 11C-deuterium-L-deprenyl: A multitracer PET paradigm combining 11C-Pittsburgh compound B and 18F-FDG. J. Nucl. Med. 2012;53:37–46. doi: 10.2967/jnumed.110.087031. [DOI] [PubMed] [Google Scholar]
- 25.Carter S.F., Herholz K., Rosa-Neto P., Pellerin L., Nordberg A., Zimmer E.R. Astrocyte Biomarkers in Alzheimer’s Disease. Trends Mol. Med. 2019;25:77–95. doi: 10.1016/j.molmed.2018.11.006. [DOI] [PubMed] [Google Scholar]
- 26.Marutle A., Gillberg P.G., Bergfors A., Yu W., Ni R., Nennesmo I., Voytenko L., Nordberg A. (3)H-deprenyl and (3)H-PIB autoradiography show different laminar distributions of astroglia and fibrillar beta-amyloid in Alzheimer brain. J. Neuroinflamm. 2013;10:90. doi: 10.1186/1742-2094-10-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rodriguez-Vieitez E., Ni R., Gulyas B., Toth M., Haggkvist J., Halldin C., Voytenko L., Marutle A., Nordberg A. Astrocytosis precedes amyloid plaque deposition in Alzheimer APPswe transgenic mouse brain: A correlative positron emission tomography and in vitro imaging study. Eur. J. Nucl. Med. Mol. Imaging. 2015;42:1119–1132. doi: 10.1007/s00259-015-3047-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rodriguez-Vieitez E., Saint-Aubert L., Carter S.F., Almkvist O., Farid K., Scholl M., Chiotis K., Thordardottir S., Graff C., Wall A., et al. Diverging longitudinal changes in astrocytosis and amyloid PET in autosomal dominant Alzheimer’s disease. Brain. 2016;139:922–936. doi: 10.1093/brain/awv404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Scholl M., Carter S.F., Westman E., Rodriguez-Vieitez E., Almkvist O., Thordardottir S., Wall A., Graff C., Langstrom B., Nordberg A. Early astrocytosis in autosomal dominant Alzheimer’s disease measured in vivo by multi-tracer positron emission tomography. Sci. Rep. 2015;5:16404. doi: 10.1038/srep16404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kumar A., Fontana I.C., Nordberg A. Reactive astrogliosis: A friend or foe in the pathogenesis of Alzheimer’s disease. J. Neurochem. 2021;164:309–324. doi: 10.1111/jnc.15565. [DOI] [PubMed] [Google Scholar]
- 31.Baiardi S., Quadalti C., Mammana A., Dellavalle S., Zenesini C., Sambati L., Pantieri R., Polischi B., Romano L., Suffritti M., et al. Diagnostic value of plasma p-tau181, NfL, and GFAP in a clinical setting cohort of prevalent neurodegenerative dementias. Alzheimers Res. Ther. 2022;14:153. doi: 10.1186/s13195-022-01093-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Benedet A.L., Milà-Alomà M., Vrillon A., Ashton N.J., Pascoal T.A., Lussier F., Karikari T.K., Hourregue C., Cognat E., Dumurgier J., et al. Differences between Plasma and Cerebrospinal Fluid Glial Fibrillary Acidic Protein Levels across the Alzheimer Disease Continuum. JAMA Neurol. 2021;78:1471–1483. doi: 10.1001/jamaneurol.2021.3671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Oeckl P., Halbgebauer S., Anderl-Straub S., Steinacker P., Huss A.M., Neugebauer H., von Arnim C.A.F., Diehl-Schmid J., Grimmer T., Kornhuber J., et al. Glial Fibrillary Acidic Protein in Serum is Increased in Alzheimer’s Disease and Correlates with Cognitive Impairment. J. Alzheimers Dis. 2019;67:481–488. doi: 10.3233/JAD-180325. [DOI] [PubMed] [Google Scholar]
- 34.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviewsDeclaracion PRISMA 2020: Una guia actualizada para la publicacion de revisiones sistematicas. Rev. Panam. Salud Publica. 2022;46:e112. doi: 10.26633/RPSP.2022.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Asken B.M., Elahi F.M., La Joie R., Strom A., Staffaroni A.M., Lindbergh C.A., Apple A.C., You M., Weiner-Light S., Brathaban N., et al. Plasma Glial Fibrillary Acidic Protein Levels Differ Along the Spectra of Amyloid Burden and Clinical Disease Stage (vol 78, pg 265, 2020) J. Alzheimers Dis. 2021;80:471–474. doi: 10.3233/JAD-219001. [DOI] [PubMed] [Google Scholar]
- 36.Benedet A.L., Brum W.S., Hansson O., Initiative A.D.N., Karikari T.K., Zimmer E.R., Zetterberg H., Blennow K., Ashton N.J. The accuracy and robustness of plasma biomarker models for amyloid PET positivity. Alzheimers Res. Ther. 2022;14:26. doi: 10.1186/s13195-021-00942-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Benussi A., Ashton N.J., Karikari T.K., Gazzina S., Premi E., Benussi L., Ghidoni R., Rodriguez J.L., Emeršič A., Binetti G., et al. Serum Glial Fibrillary Acidic Protein (GFAP) Is a Marker of Disease Severity in Frontotemporal Lobar Degeneration. J. Alzheimer’s Dis. 2020;77:1129–1141. doi: 10.3233/JAD-200608. [DOI] [PubMed] [Google Scholar]
- 38.Bettcher B.M., Olson K.E., Carlson N.E., McConnell B.V., Boyd T., Adame V., Solano D.A., Anton P., Markham N., Thaker A.A., et al. Astrogliosis and episodic memory in late life: Higher GFAP is related to worse memory and white matter microstructure in healthy aging and Alzheimer’s disease. Neurobiol. Aging. 2021;103:68–77. doi: 10.1016/j.neurobiolaging.2021.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Beyer L., Stocker H., Rujescu D., Holleczek B., Stockmann J., Nabers A., Brenner H., Gerwert K. Amyloid-beta misfolding and GFAP predict risk of clinical Alzheimer’s disease diagnosis within 17 years. Alzheimer’s Dement. 2022;19:1020–1028. doi: 10.1002/alz.12745. [DOI] [PubMed] [Google Scholar]
- 40.Chatterjee P., Pedrini S., Stoops E., Goozee K., Villemagne V.L., Asih P.R., Verberk I.M.W., Dave P., Taddei K., Sohrabi H.R., et al. Plasma glial fibrillary acidic protein is elevated in cognitively normal older adults at risk of Alzheimer’s disease. Transl. Psychiatry. 2021;11:27. doi: 10.1038/s41398-020-01137-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chatterjee P., Pedrini S., Ashton N.J., Tegg M., Goozee K., Singh A.K., Karikari T.K., Simrén J., Vanmechelen E., Armstrong N.J., et al. Diagnostic and prognostic plasma biomarkers for preclinical Alzheimer’s disease. Alzheimer’s Dement. 2021;18:1141–1154. doi: 10.1002/alz.12447. [DOI] [PubMed] [Google Scholar]
- 42.Chatterjee P., Pedrini S., Doecke J.D., Thota R., Villemagne V.L., Doré V., Singh A.K., Wang P., Rainey-Smith S., Fowler C., et al. Plasma Aβ42/40 ratio, p-tau181, GFAP, and NfL across the Alzheimer’s disease continuum: A cross-sectional and longitudinal study in the AIBL cohort. Alzheimer’s Dement. 2022;19:1117–1134. doi: 10.1002/alz.12724. [DOI] [PubMed] [Google Scholar]
- 43.Chouliaras L., Thomas A., Malpetti M., Donaghy P., Kane J., Mak E., Savulich G., Prats-Sedano M.A., Heslegrave A.J., Zetterberg H., et al. Differential levels of plasma biomarkers of neurodegeneration in Lewy body dementia, Alzheimer’s disease, frontotemporal dementia and progressive supranuclear palsy. J. Neurol. Neurosurg. Psychiatry. 2022;93:651–658. doi: 10.1136/jnnp-2021-327788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cicognola C., Janelidze S., Hertze J., Zetterberg H., Blennow K., Mattsson-Carlgren N., Hansson O. Plasma glial fibrillary acidic protein detects Alzheimer pathology and predicts future conversion to Alzheimer dementia in patients with mild cognitive impairment. Alzheimer’s Res. Ther. 2021;13:68. doi: 10.1186/s13195-021-00804-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ebenau J.L., Pelkmans W., Verberk I.M.W., Verfaillie S.C.J., Van Den Bosch K.A., Van Leeuwenstijn M., Collij L.E., Scheltens P., Prins N.D., Barkhof F., et al. Association of CSF, Plasma, and Imaging Markers of Neurodegeneration with Clinical Progression in People with Subjective Cognitive Decline. Neurology. 2022;98:E1315–E1326. doi: 10.1212/WNL.0000000000200035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Frontera J.A., Boutajangout A., Masurkar A.V., Betensky R.A., Ge Y., Vedvyas A., Debure L., Moreira A., Lewis A., Huang J., et al. Comparison of serum neurodegenerative biomarkers among hospitalized COVID-19 patients versus non-COVID subjects with normal cognition, mild cognitive impairment, or Alzheimer’s dementia. Alzheimer’s Dement. 2022;18:899–910. doi: 10.1002/alz.12556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gonzales M.M., Short M.I., Satizabal C.L., O’ Bryant S., Tracy R.P., Zare H., Seshadri S. Blood biomarkers for dementia in Hispanic and non-Hispanic White adults. Alzheimer’s Dement. Transl. Res. Clin. Interv. 2021;7:e12164. doi: 10.1002/trc2.12164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gonzales M.M., Wang C.P., Short M.I., Parent D.M., Kautz T., MacCarthy D., Satizabal C.L., González D.A., Royall D.R., Zare H., et al. Blood biomarkers for cognitive decline and clinical progression in a Mexican American cohort. Alzheimers Dement. 2022;14:e12298. doi: 10.1002/dad2.12298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Abdelhak A., Foschi M., Abu-Rumeileh S., Yue J.K., D’Anna L., Huss A., Oeckl P., Ludolph A.C., Kuhle J., Petzold A., et al. Blood GFAP as an emerging biomarker in brain and spinal cord disorders. Nat. Rev. Neurol. 2022;18:158–172. doi: 10.1038/s41582-021-00616-3. [DOI] [PubMed] [Google Scholar]
- 50.Oeckl P., Anderl-Straub S., Von Arnim C.A.F., Baldeiras I., Diehl-Schmid J., Grimmer T., Halbgebauer S., Kort A.M., Lima M., Marques T.M., et al. Serum GFAP differentiates Alzheimer’s disease from frontotemporal dementia and predicts MCI-to-dementia conversion. J. Neurol. Neurosurg. Psychiatry. 2022;93:659–667. doi: 10.1136/jnnp-2021-328547. [DOI] [PubMed] [Google Scholar]
- 51.Palmqvist S., Stomrud E., Cullen N., Janelidze S., Manuilova E., Jethwa A., Bittner T., Eichenlaub U., Suridjan I., Kollmorgen G., et al. An accurate fully automated panel of plasma biomarkers for Alzheimer’s disease. Alzheimers Dement. 2022;19:1204–1215. doi: 10.1002/alz.12751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Parvizi T., Konig T., Wurm R., Silvaieh S., Altmann P., Klotz S., Rommer P.S., Furtner J., Regelsberger G., Lehrner J., et al. Real-world applicability of glial fibrillary acidic protein and neurofilament light chain in Alzheimer’s disease. Front. Aging Neurosci. 2022;14:887498. doi: 10.3389/fnagi.2022.887498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pereira J.B., Janelidze S., Smith R., Mattsson-Carlgren N., Palmqvist S., Teunissen C.E., Zetterberg H., Stomrud E., Ashton N.J., Blennow K., et al. Plasma GFAP is an early marker of amyloid-beta but not tau pathology in Alzheimer’s disease. Brain. 2021;144:3505–3516. doi: 10.1093/brain/awab223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pichet Binette A., Palmqvist S., Bali D., Farrar G., Buckley C.J., Wolk D.A., Zetterberg H., Blennow K., Janelidze S., Hansson O. Combining plasma phospho-tau and accessible measures to evaluate progression to Alzheimer’s dementia in mild cognitive impairment patients. Alzheimers Res. Ther. 2022;14:46. doi: 10.1186/s13195-022-00990-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Prins S., de Kam M.L., Teunissen C.E., Groeneveld G.J. Inflammatory plasma biomarkers in subjects with preclinical Alzheimer’s disease. Alzheimers Res. Ther. 2022;14:106. doi: 10.1186/s13195-022-01051-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Salvado G., Mila-Aloma M., Shekari M., Ashton N.J., Operto G., Falcon C., Cacciaglia R., Minguillon C., Fauria K., Ninerola-Baizan A., et al. Reactive astrogliosis is associated with higher cerebral glucose consumption in the early Alzheimer’s continuum. Eur. J. Nucl. Med. Mol. Imaging. 2022;49:4567–4579. doi: 10.1007/s00259-022-05897-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Shir D., Graff-Radford J., Hofrenning E.I., Lesnick T.G., Przybelski S.A., Lowe V.J., Knopman D.S., Petersen R.C., Jack C.R., Jr., Vemuri P., et al. Association of plasma glial fibrillary acidic protein (GFAP) with neuroimaging of Alzheimer’s disease and vascular pathology. Alzheimers Dement. 2022;14:e12291. doi: 10.1002/dad2.12291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Simren J., Leuzy A., Karikari T.K., Hye A., Benedet A.L., Lantero-Rodriguez J., Mattsson-Carlgren N., Scholl M., Mecocci P., Vellas B., et al. The diagnostic and prognostic capabilities of plasma biomarkers in Alzheimer’s disease. Alzheimers Dement. 2021;17:1145–1156. doi: 10.1002/alz.12283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Simren J., Weninger H., Brum W.S., Khalil S., Benedet A.L., Blennow K., Zetterberg H., Ashton N.J. Differences between blood and cerebrospinal fluid glial fibrillary Acidic protein levels: The effect of sample stability. Alzheimers Dement. 2022;18:1988–1992. doi: 10.1002/alz.12806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Stevenson-Hoare J., Heslegrave A., Leonenko G., Fathalla D., Bellou E., Luckcuck L., Marshall R., Sims R., Morgan B.P., Hardy J., et al. Plasma biomarkers and genetics in the diagnosis and prediction of Alzheimer’s disease. Brain. 2023;146:690–699. doi: 10.1093/brain/awac128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Stocker H., Beyer L., Perna L., Rujescu D., Holleczek B., Beyreuther K., Stockmann J., Schottker B., Gerwert K., Brenner H. Association of plasma biomarkers, p-tau181, glial fibrillary acidic protein, and neurofilament light, with intermediate and long-term clinical Alzheimer’s disease risk: Results from a prospective cohort followed over 17 years. Alzheimers Dement. 2023;19:25–35. doi: 10.1002/alz.12614. [DOI] [PubMed] [Google Scholar]
- 62.Thijssen E.H., Verberk I.M.W., Kindermans J., Abramian A., Vanbrabant J., Ball A.J., Pijnenburg Y., Lemstra A.W., van der Flier W.M., Stoops E., et al. Differential diagnostic performance of a panel of plasma biomarkers for different types of dementia. Alzheimers Dement. 2022;14:e12285. doi: 10.1002/dad2.12285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Verberk I.M.W., Thijssen E., Koelewijn J., Mauroo K., Vanbrabant J., de Wilde A., Zwan M.D., Verfaillie S.C.J., Ossenkoppele R., Barkhof F., et al. Combination of plasma amyloid beta((1-42/1-40)) and glial fibrillary acidic protein strongly associates with cerebral amyloid pathology. Alzheimers Res. Ther. 2020;12:118. doi: 10.1186/s13195-020-00682-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Balasa A.F., Chircov C., Grumezescu A.M. Body Fluid Biomarkers for Alzheimer’s Disease-An Up-To-Date Overview. Biomedicines. 2020;8:421. doi: 10.3390/biomedicines8100421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Paraskevaidi M., Allsop D., Karim S., Martin F.L., Crean S. Diagnostic Biomarkers for Alzheimer’s Disease Using Non-Invasive Specimens. J. Clin. Med. 2020;9:1673. doi: 10.3390/jcm9061673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Omar S.H., Preddy J. Advantages and Pitfalls in Fluid Biomarkers for Diagnosis of Alzheimer’s Disease. J. Pers. Med. 2020;10:63. doi: 10.3390/jpm10030063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Khan S., Barve K.H., Kumar M.S. Recent Advancements in Pathogenesis, Diagnostics and Treatment of Alzheimer’s Disease. Curr. Neuropharmacol. 2020;18:1106–1125. doi: 10.2174/1570159X18666200528142429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Mantzavinos V., Alexiou A. Biomarkers for Alzheimer’s Disease Diagnosis. Curr. Alzheimer Res. 2017;14:1149–1154. doi: 10.2174/1567205014666170203125942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Frisoni G.B., Boccardi M., Barkhof F., Blennow K., Cappa S., Chiotis K., Demonet J.F., Garibotto V., Giannakopoulos P., Gietl A., et al. Strategic roadmap for an early diagnosis of Alzheimer’s disease based on biomarkers. Lancet Neurol. 2017;16:661–676. doi: 10.1016/S1474-4422(17)30159-X. [DOI] [PubMed] [Google Scholar]
- 70.Rajan K., McAninch E.A., Aggarwal N., Barnes L.L., Wilson R., Weuve J., DeCarli C.S., Evans D. Longitudinal Changes in Blood Biomarkers of Clinical Alzheimer Disease in a Biracial Population Sample. Neurology. 2022;100:e874–e883. doi: 10.1212/WNL.0000000000201289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Foerch C., Niessner M., Back T., Bauerle M., De Marchis G.M., Ferbert A., Grehl H., Hamann G.F., Jacobs A., Kastrup A., et al. Diagnostic accuracy of plasma glial fibrillary acidic protein for differentiating intracerebral hemorrhage and cerebral ischemia in patients with symptoms of acute stroke. Clin. Chem. 2012;58:237–245. doi: 10.1373/clinchem.2011.172676. [DOI] [PubMed] [Google Scholar]
- 72.Missler U., Wiesmann M., Wittmann G., Magerkurth O., Hagenstrom H. Measurement of glial fibrillary acidic protein in human blood: Analytical method and preliminary clinical results. Clin. Chem. 1999;45:138–141. doi: 10.1093/clinchem/45.1.138. [DOI] [PubMed] [Google Scholar]
- 73.Qin T., Prins S., Groeneveld G.J., Van Westen G., de Vries H.E., Wong Y.C., Bischoff L.J.M., de Lange E.C.M. Utility of Animal Models to Understand Human Alzheimer’s Disease, Using the Mastermind Research Approach to Avoid Unnecessary Further Sacrifices of Animals. Int. J. Mol. Sci. 2020;21:3158. doi: 10.3390/ijms21093158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Frost G.R., Li Y.M. The role of astrocytes in amyloid production and Alzheimer’s disease. Open. Biol. 2017;7:170228. doi: 10.1098/rsob.170228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Chmielewska N., Szyndler J., Makowska K., Wojtyna D., Maciejak P., Plaznik A. Looking for novel, brain-derived, peripheral biomarkers of neurological disorders. Neurol. Neurochir. Pol. 2018;52:318–325. doi: 10.1016/j.pjnns.2018.02.002. [DOI] [PubMed] [Google Scholar]
- 76.Banks W.A. Drug delivery to the brain in Alzheimer’s disease: Consideration of the blood-brain barrier. Adv. Drug. Deliv. Rev. 2012;64:629–639. doi: 10.1016/j.addr.2011.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Mouser P.E., Head E., Ha K.H., Rohn T.T. Caspase-mediated cleavage of glial fibrillary acidic protein within degenerating astrocytes of the Alzheimer’s disease brain. Am. J. Pathol. 2006;168:936–946. doi: 10.2353/ajpath.2006.050798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Heimfarth L., Passos F.R.S., Monteiro B.S., Araujo A.A.D., Quintans J.L., Quintans J.D.S. Serum glial fibrillary acidic protein is a body fluid biomarker: A valuable prognostic for neurological disease—A systematic review. Int. Immunopharmacol. 2022;107:108624. doi: 10.1016/j.intimp.2022.108624. [DOI] [PubMed] [Google Scholar]
- 79.Akiyama H., Barger S., Barnum S., Bradt B., Bauer J., Cole G.M., Cooper N.R., Eikelenboom P., Emmerling M., Fiebich B.L., et al. Inflammation and Alzheimer’s disease. Neurobiol. Aging. 2000;21:383–421. doi: 10.1016/S0197-4580(00)00124-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Rajan K.B., Aggarwal N.T., McAninch E.A., Weuve J., Barnes L.L., Wilson R.S., DeCarli C., Evans D.A. Remote Blood Biomarkers of Longitudinal Cognitive Outcomes in a Population Study. Ann. Neurol. 2020;88:1065–1076. doi: 10.1002/ana.25874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hansen N., Rauter C., Wiltfang J. Blood Based Biomarker for Optimization of Early and Differential Diagnosis of Alzheimer’s Dementia. Fortschr. Neurol. Psyc. 2022;90:326–335. doi: 10.1055/a-1839-6237. [DOI] [PubMed] [Google Scholar]
- 82.Hol E.M., Pekny M. Glial fibrillary acidic protein (GFAP) and the astrocyte intermediate filament system in diseases of the central nervous system. Curr. Opin. Cell. Biol. 2015;32:121–130. doi: 10.1016/j.ceb.2015.02.004. [DOI] [PubMed] [Google Scholar]
- 83.Jurga A.M., Paleczna M., Kadluczka J., Kuter K.Z. Beyond the GFAP-Astrocyte Protein Markers in the Brain. Biomolecules. 2021;11:1361. doi: 10.3390/biom11091361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Heller C., Foiani M.S., Moore K., Convery R., Bocchetta M., Neason M., Cash D.M., Thomas D., Greaves C.V., Woollacott I.O.C., et al. Plasma glial fibrillary acidic protein is raised in progranulin-associated frontotemporal dementia. J. Neurol. Neurosurg. Psychiatry. 2020;91:263–270. doi: 10.1136/jnnp-2019-321954. [DOI] [PubMed] [Google Scholar]
- 85.Mayer C.A., Brunkhorst R., Niessner M., Pfeilschifter W., Steinmetz H., Foerch C. Blood levels of glial fibrillary acidic protein (GFAP) in patients with neurological diseases. PLoS ONE. 2013;8:e62101. doi: 10.1371/journal.pone.0062101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.van Ballegoij W.J.C., van de Stadt S.I.W., Huffnagel I.C., Kemp S., Willemse E.A.J., Teunissen C.E., Engelen M. Plasma NfL and GFAP as biomarkers of spinal cord degeneration in adrenoleukodystrophy. Ann. Clin. Transl. Neur. 2020;7:2127–2136. doi: 10.1002/acn3.51188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Lange R.P., Everett A., Dulloor P., Korley F.K., Bettegowda C., Blair C., Grossman S.A., Holdhoff M. Evaluation of eight plasma proteins as candidate blood-based biomarkers for malignant gliomas. Cancer Investig. 2014;32:423–429. doi: 10.3109/07357907.2014.933237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Dvorak F., Haberer I., Sitzer M., Foerch C. Characterisation of the diagnostic window of serum glial fibrillary acidic protein for the differentiation of intracerebral haemorrhage and ischaemic stroke. Cerebrovasc. Dis. 2009;27:37–41. doi: 10.1159/000172632. [DOI] [PubMed] [Google Scholar]
- 89.McGrath E.R., Beiser A.S., O’Donnell A., Yang Q., Ghosh S., Gonzales M.M., Himali J.J., Satizabal C.L., Johnson K.A., Tracy R.P., et al. Blood Phosphorylated Tau 181 as a Biomarker for Amyloid Burden on Brain PET in Cognitively Healthy Adults. J. Alzheimers Dis. 2022;87:1517–1526. doi: 10.3233/JAD-215639. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data supporting the findings of this study are available from the corresponding authors upon reasonable request.