Abstract
Study Design
Systematic review/expert consensus.
Objectives
Fractures of the axis represent the most frequent injury of the spine in elderly patients. Both, operative and non-operative treatment are associated with a high rate of complications and mortality. The aim of this article was to summarize the current literature on the management of odontoid fractures in geriatric patients and to weigh it based on an expert consensus process.
Methods
In a joint consensus process, members of the Spine Section of the German Orthopaedic and Trauma Society (DGOU) aimed to formulate recommendations for the diagnostic workup and treatment of odontoid fractures in geriatric patients. Based on the previously published recommendations, this article is an updated version with incorporating a systematic review of the recent literature.
Results
Based on the new data available, the recommendations established in the initial consensus process were adapted.
Conclusions
Computed tomography represents the diagnostic standard for patients with suspected injuries of the upper cervical spine. Anderson/D’Alonzo odontoid fractures type 1, non-displaced type 2, and type 3 can be treated conservatively. Even non-unions do not necessarily result in poor clinical outcome. In Anderson/D’Alonzo type 2 fractures, surgical therapy offers the advantage of relatively safe osseous healing with no increased complication rate even in elderly patients and can thus be recommended. In very high aged patients, however, a case-by-case decision should be made. When surgical stabilization of osteoporotic odontoid fractures is indicated, posterior techniques are biomechanically advantageous and can be considered the standard.
Keywords: cervical, odontoid fracture, treatment, guidelines
Introduction
Fractures of the dens axis are the most common type of injury of the cervical spine in patients over 65 years of age.1,2 In view of the demographic development of the last decades, a significant incidence increase has been observed. 3 Especially in geriatric patients, fractures of the dens axis present a particular challenge. Usually, patients present with poor bone quality based on characteristic local degenerative changes. Due to unfavorable biomechanics, small fracture surface, and poor blood supply to the dens base, odontoid fractures poorly heal in elderly patients.
One-year mortality rates of 18%-45% have been described for odontoid fractures in geriatric populations.4-6 The most important factor for the increased mortality is the high number of comorbidities in elderly patients, evenly increasing the risk of perioperative complications. On the other hand, non-union rates of up to 80% have been reported with conservative therapy.7-9 There has been ongoing debate whether to treat these fractures operatively or non-operatively. 10
This paper summarizes the current state of the literature on odontoid fractures in the elderly patients and provides recommendations for their management based on expert consensus and a systematic review.
Methods
Consensus Process
A joint consensus process involving the members of the Spine Section of the German Society for Orthopaedics and Trauma Surgery (DGOU) had been performed resulting in recommendations on the diagnosis and treatment of odontoid fractures published previously in 2020. 11 Based on these previously published recommendations, this article is an updated version with systematically incorporating the recent literature.
For this, a systematic review of the literature was conducted according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) checklist and algorithm, 6 with the goal of finding all articles describing the diagnostic workup and treatment odontoid fractures during the last 5 years.
Search Strategy
Investigations between 08/2017 and 08/2022 were included. Prospective and retrospective observational investigations were considered for analysis. The authors performed a systematic an initial search of PubMed/Medline databases for eligible investigations. The search terms were (odontoid) AND (fracture*). Studies were selected according the following inclusion criteria: a) case series, cohort studies, clinical trials, or registry studies regarding the epidemiology, the diagnostic workup or the treatment of odontoid fractures in patients older than 60 years, b) articles published in English or German language. Exclusion criteria were: a) cadaver studies, biomechanical studies, anatomical studies, systematic or narrative reviews, meta-analyses, case reports, uncontrolled case series, case series reporting only descriptive outcome data of a single treatment arm, case series with fewer than 100 patients or fewer than 20 patients in one treatment arm, studies reporting on only radiographic measures, recommendations and guidelines, surveys, and technical notes, b) studies investigating atypical fractures of C2, combined fractures of C1 and C2, non-unions, or metastatic fractures.
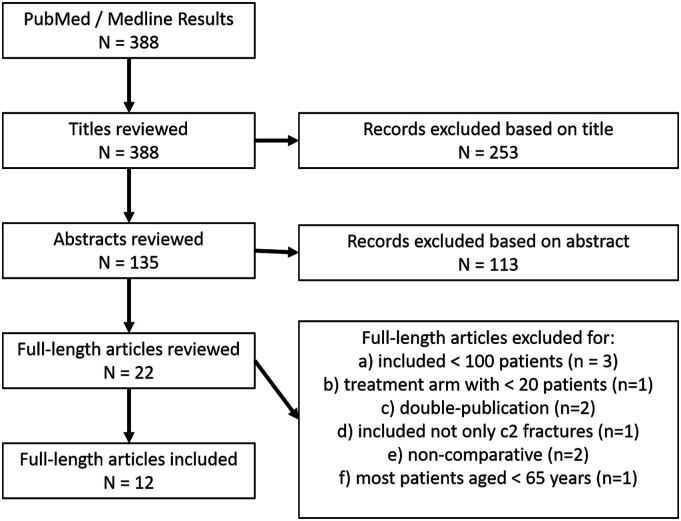
Titles and abstracts were reviewed. Duplicates were removed and full texts were checked for suitability. The remaining full-length articles were then screened by all authors and disagreement was resolved by consensus. The final decision was made based on the analysis of the full text. In doubt, articles were included into the next stage. A flowchart of the filtering stages (titles, abstracts, full-length texts) is shown in Figure 1.
Figure 1.
Literature research flow chart.
Synthesis of Results
We extracted data concerning study characteristics including authors’ names, title, year of publication, journal of publication, number of patients, time of follow-up and type of study. For the description of the study population, the number of patients and their age were collected. Outcome parameters were analyzed according to the inclusion criteria. For all included studies we used the Oxford Centre for Evidence-Based Medicine 2011 for defining the level of evidence. 7
Results
Systematic Review
Twelve articles met the inclusion criteria (Figure 1), among these 5 were retrospective case series and seven were studies using data from national databases (Table 1). Publication dates ranged from 2017 to 2022 and data from totally 48,316 patients with an odontoid fracture were reported. Nine studies compared some operative vs non-operative treatment, while three studies compared different operative techniques. The results of the analyzed studies were therefore incorporated into the following chapters on Operative versus non-operative management and Operative therapy.
Table 1.
Studies Included into the Systematic Review.
| 1st Author | Year | Design | N | Patient Age | Treatment | Main Outcome |
|---|---|---|---|---|---|---|
| Patterson | 2017 | Retrospective, national database | 141 | 78 | Operative: Anterior (34%) vs posterior (66%) | Anterior odontoid fracture stabilization associated with shorter operative times, greater risk of unplanned readmissions and revision operations within 30 days of surgery |
| Robinson | 2018 | Retrospective, national database | 3375 | 83 | Operative (22%) vs non-operative (78%) | Adjusted for age, gender, comorbidity, and year of injury, surgically treated patients had greater survival than non-surgically treated patients. Among those >88 years, surgical treatment lost its effect on survival |
| Bhimani | 2018 | Retrospective, national database | 165 | 70 | Operative: C1-C2 vs C0-cervical | Higher risk of reoperation for occiputo-cervical (9%) vs C1-C2 fixation (2%) |
| De Bonis | 2019 | Retrospective, multicenter | 147 | ≥65 | Operative (54%) vs non-operative (46%) | Modified Rankin scale and Charlson comorbidity Index are independent predictors for functional outcome and posttreatment disability. No significant differences between patients of 65 to 79 years and ≥80 years |
| Gembruch | 2019 | Retrospective, monocentric | 125 | 86 | Operative (78%) vs non-operative (22%) | Fracture union in 91% after surgery and 70% after conservative treatment. 3-month mortality 28% in the surgical group and 20% in the non-op group |
| Shousha | 2019 | Retrospective, monocentric | 133 | 74 anterior 78 posterior |
Operative: Anterior (35%) vs posterior (65%) | Less blood loss and shorter hospital stay with anterior fixation but higher rates for non-union and revision surgery compared to posterior fixation |
| Honda | 2020 | Retrospective, national database | 3167 | 70 | Operative (22%)2 vs non-operative (78%) | No significant difference in in-hospital mortality between conservative treatment (4.6%) vs surgery (3.0%), also in patients aged ≥80 years (7.2% vs 5.4%) |
| Lukins | 2020 | Retrospective, monocentric | 141 | ≥65 | Operative (28%) vs non-operative (72%) | Age, male gender, and injury severity are predictors of 12-month mortality, choice of treatment is not |
| Rizvi | 2020 | Retrospective, monocentric | 282 | 77 | Operative (68%) vs non-operative (32%) | Secondary surgery in 14.4% after initial non-op treatment and 9.5% after initial operative treatment. Higher fusion rates with surgery |
| Alluri | 2021 | Retrospective, national database | 32,419 | 77 | Operative (67%) vs non-operative (32%) | Operative treatment associated with higher odds of complications (pulmonary, gastrointestinal, renal). Inpatient mortality 3.6% for operative and 5.9% for nonoperative treatment, but more preexisting comorbidities in non-operative patients |
| von Glinski | 2021 | Retrospective, national database | 2921 | 77 non-op 70 operative |
Operative (19%) vs non-operative (81%) | Higher overall 90-day readmission rate of after nonoperative (29.4%) vs operative (16.4%) treatment |
| Smith | 2022 | Retrospective, national database | 5300 | 77 | Operative (8%) vs non-operative (92%) | Surgery was associated with decreased one-year mortality in all patients, patients between the ages of 65 and 74, and patients over the age of 75 |
Imaging
In elderly patients, odontoid fractures usually occur as a result of low-energy trauma. Patients often present after a fall from standing height including some kind of head impact and clinical sings of head or face injury. Patients report with neck pain and limited motion of the head and cervical spine. Neurologic deficits are rare but may be fatal, because of the localization at the level of the cervical medulla. Clinical examination is therefore an inaccurate measure for detecting odontoid fractures.
In accordance with the C-spine rules, radiologic imaging including CT-scan of the cervical spine is always recommended in patients over 65 years of age with traumatically induced neck pain or after head impact. 12
Conventional radiographs of the cervical spine in antero-posterior and lateral projection as well as a transoral odontoid radiographs continue to be part of basic diagnostics because of their availability, low cost, and low radiation exposure.
However, because computed tomography (CT) is clearly superior to conventional radiographs in the cervical spine in terms of sensitivity and specificity,13,14 it is considered the gold standard, especially in cases of suspected upper cervical spine injury.
Magnetic resonance imaging (MRI) is used only in cases of neurologic deficits, suspected disco-ligamentous injury, or to differentiate between fresh and old fractures. 13
Native CT should be supplemented by CT/MRI angiography to exclude lesions of the vertebral artery and to detect an irregular course of the vessels preoperatively. This is recommended especially if CT shows fracture extensions into the vertebral canal or if surgical anterior or posterior C1/2 fusion is planned.15,16
Angulation (>11°) and displacement (>5 mm) on CT scans are strong predictors for fracture instability. 17 Dynamic fluoroscopic examination can be performed in borderline cases or to detect disco-ligamentous C1/2 instability or to differentiate between stable or unstable non-union. The examination should be performed by a physician and with the patient awake in guided passive flexion and extension.
Classifications
Odontoid fractures are usually classified according to the system described by Anderson and D'Alonzo 18 (Figure 2). The classification distinguishes three morphological types: Type 1 is a fracture of the odontoid tip in terms of a bony avulsion of the ala ligaments, type 2 is a fracture in the odontoid base region, and type 3 is a fracture in the odontoid base region extending into the body of the axis.
Figure 2.
Classification of odontoid fractures by Anderson and D’Alonzo. 18
According to Eysel and Roosen, type 2 can be further divided into three subtypes (Figure 3): 19 type 2A has a horizontal fracture course, in type 2B the fracture proceeds from antero-superior to postero-inferior, and in type 2C the fracture proceeds from antero-inferior to postero-superior. The fracture course in type 2A and 2B allows anterior screw osteosynthesis, whereas this is not possible in type 2C. A nearly similar subclassification was described by Grauer et al in 2005. 20
Figure 3.
Sub-Classification of type 2 fractures by Eysel and Roosen. 19
The Upper Cervical Spine Injury Classification System of the AOSpine summarizes odontoid fractures under type A (“bony injury only without significant ligamentous, tension band, discal injury”; www.aospine.org/classification).
Treatment
Operative Versus Non-Operative Management
The decision for or against a surgical procedure in odontoid fractures of elderly patients is influenced by several factors. In addition to fracture morphology and concomitant injuries in the cervical spine, the patient’s age and comorbidities must be considered.
There is consensus for conservative therapy for Anderson and D’Alonzo type 1 and type 3 fractures - if there is no gross dislocation or concomitant ligamentous instability.21,22
In contrast, the treatment of type 2 fractures has been subject of controversial debates in the literature. Type 2 fractures are localized at the base of the dens, where the shear forces of the articulating atlas ring are particularly strong. Stress shielding by limited degenerative C1/2 motion of the dens base leads to a localized osteopenic situation. In combination with the weak blood supply to the dens base and a frequently existing anklyosis of the anterior arch of the atlas with the odontoid tip in older individuals, this leads to non-union rates of up to 80% under conservative therapy. 9 In contrast, very high osseous union rates were reported with surgical therapy.23,24 Meta-analyses show significantly higher fracture healing in surgically treated patients, especially for fractures with a displacement of more than 4 mm.22,25 However, odontoid non-unions do not necessarily lead to a worse functional outcome.26,27 Cases of secondary myelopathy in odontoid non-union have mostly been described for younger and more active individuals but rarely occur in elderly patients.28,29 A recent systematic review concluded that it is safe to forgo surgery for carefully selected patients with non-united odontoid fractures when near-anatomic alignment is present, dynamic instability is lacking on imaging studies, the neurologic examination findings are normal, and the risk of neck injury is low. 30
The complication rates in geriatric patients under 85 years of age treated operatively or conservatively do not differ in terms of frequency - but they do in terms of complication patterns.26,31 The overall 90-day readmission rate after non-operative treatment is almost twice as high as after operative treatment. 32 Surgically treated patients over 80 years of age suffer from an increased incidence of internal complications,22,33 while 10% of patients who are treated conservatively with a cervical orthosis develop pressure ulcers.34,35
In elderly patients, odontoid fractures are associated with high mortality regardless of the therapy chosen.4-6,36,37 For non-operative treatment, 1-year mortalities of up to 45% have been described.36,38 Similar mortality rates have been described for operative therapy, even in patients over 80 years of age.33,39 A retrospective multicenter study of the AOSpine North America reported significantly lower mortality in surgically vs non-operatively treated patients (7% vs 22%). This difference was still evident at 2-year follow-up. 4 Improved 1-year survival after surgical management was also reported in a recent national database study analyzing data of 5300 patients with an odontoid fracture. 40 In contrast a single center study reported an increased mortality with surgery, 41 However, systematic meta-analyses of numerous studies have so far failed to detect significant differences in mortality between conservatively and surgically treated elderly patients with odontoid fractures. 22 Most recent studies with large cohorts report that age, gender and comorbidities are the most relevant risk factors for mortality and that choice of treatment is not.31,37,42,43 A recent retrospective national database analysis of 3375 patients reported that - when adjusted for age, gender, comorbidity, and year of injury - surgically treated patients had greater survival than non-surgically treated patients. 44 Among those aged over 88 years, surgical treatment lost its effect on survival, though. 44
No significant differences in mortality can be found between conservatively and surgically treated patients over 80 years of age.22,45,46A problem with all studies on geriatric odontoid fractures, however, is the age-related high drop-out rate, which is likely to lead to a relevant selection bias, especially when comparing surgically vs non-operatively treated patients. Patients with more comorbidities are more likely to be treated non-operatively.31,40
However, the data published so far indicate that the general frailty and the comorbidities of the patients responsible for it probably play a greater role in morbidity and mortality than age.32,46,47 It can be assumed, though, that patients older than 88 years are very likely to be frail. Therefore, most authors agree that in very old patients, surgical therapy is only rarely indicated in selected cases.32,47
Non-Operative Therapy
The non-surgical treatment of odontoid fractures in geriatric patients includes medicinal pain therapy according to WHO and immobilization in a semi-rigid cervical orthosis for six weeks. There is no advantage of wearing hard cervical orthoses in terms of achieving fracture union and these should be worn for a maximum of 24 hours as they otherwise may cause pressure ulcers.35,48 Even with semi-rigid orthoses the fit should be checked regularly. In patients who are impaired or in need of care, the use of an orthosis should be questioned to avoid dysphagia and aspiration.
Especially in the beginning, clinical and radiological follow-up should be frequently performed over the first 6 weeks to detect secondary displacement. In case of doubt, a CT scan or a dynamic examination should be ordered at a low level.
Right from the beginning of conservative therapy, isometric exercises assisted by physiotherapists should be started. Active physiotherapeutic exercise for mobility should only be started after radiological confirmation of fracture healing or if there is no indication of secondary dislocation in the conventional radiographs 6 weeks after trauma.
Treatment with halo fixation is associated with significantly increased morbidity and mortality in geriatric patients and should be avoided, 49 but may serve as an alternative in individual cases in patients with unstable, highly displaced odontoid fractures whose general condition does not permit general anesthesia. 50
Operative Therapy
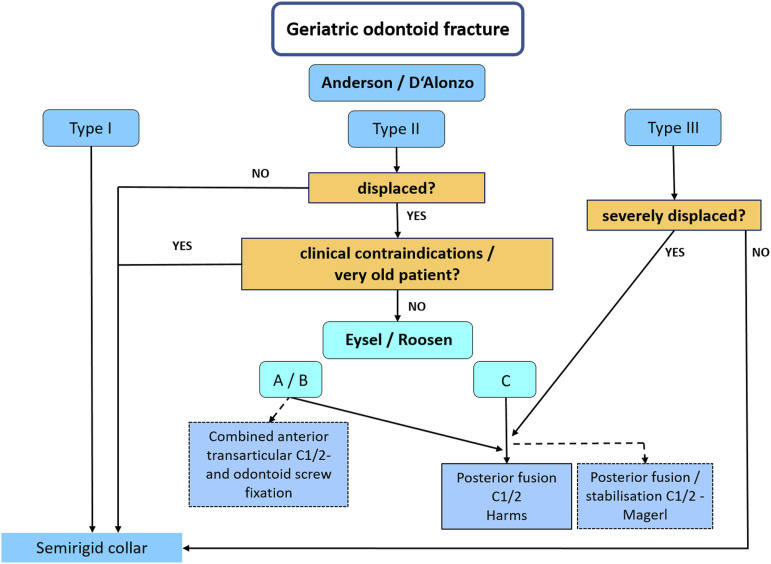
Biomechanical studies have shown that posterior instrumentation of C1/2 using a posterior internal fixator according to Goel/Harms is the most biomechanically stable method for treating odontoid fractures.51,52 In addition, it allows for direct open reduction and true osseous fusion of the C1/2 segment. For this technique, screws are placed bilaterally into the lateral masses of C1 and either into the pedicles or the pars of C2 and connected with rods. Hence, it can be considered the work horse for most geriatric odontoid fractures (Figure 4).
Figure 4.
Recommended treatment algorithm.
An alternative of almost similar initial biomechanical strength is posterior transarticular screw fixation of C1/2 as described by Magerl in combination with a Gallie cerclage and bone graft fusion through an open approach. 53 However, the true advantage of the posterior transarticular screw fixation is that it can be applied percutaneously, even though the stability achieved is not the same as with posterior Goel/Harms fixation. 51 It can also not be used in patients with a high-riding vertebral artery.15,16 It is only in these cases that a posterior occipito-cervical fixation may be used as this techniques has a higher risk for reoperation compared to posterior C1/2 fixation. 54
In patients with healthy bone and fractures according to Eysel/Roosen type 2A and 2B, anterior screw fixation of odontoid fractures represents a less-invasive alternative that – in contrast to posterior procedures – theoretically maintains mobility in the segment C1/2. In osteoporotic bone, stand-alone anterior Odontoid screw fixation has been shown to be associated with high failure and revision rates compared to posterior fixaton.55,56 However, a combination of anterior odontoid screw fixation with an anterior transarticular screw fixation of C1/2 can achieve similar stability as posterior transarticular screw fixation. 57 Therefore, this type of combined anterior odontoid/transarticular screw fixation appears to offer an alternative that is particularly suitable for patients in whom surgery in the prone position would be associated with increased perioperative risk.
Conclusion
Odontoid fractures in elderly patients are increasing in incidence and relevance. A high degree of suspicion is key and the threshold for advanced imaging diagnostics should be low. CT is the gold standard for primary diagnosis of suspected upper cervical spine injuries and should be combined with an angiography when operative treatment is considered.
Anderson/D'Alonzo type 1 and type 3 odontoid fractures and non-displaced type 2 fractures can be treated conservatively. Even non-unions do not necessarily result in poor clinical outcome. In Anderson/D'Alonzo type 2 fractures, surgical therapy offers the advantage of relatively safe osseous healing with no increased complication rate even in elderly patients and can thus be recommended. In very high aged patients, though, a case-by-case decision should be made.
When surgical stabilization of osteoporotic odontoid fractures is indicated, posterior procedures are biomechanically advantageous and can be considered the standard.
Anterior combined odontoid/transarticular screw fixation are a less invasive alternative when strictly indicated and technically well executed. However, anterior procedures are associated with an increased risk of dysphagia. 58
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was organized and financially supported by Deutsche Gesellschaft für Orthopädie und Unfallchirurgie e.V. (DGOU).
ORCID iDs
Georg Osterhoff https://orcid.org/0000-0001-5051-0998
Alexander C. Disch https://orcid.org/0000-0001-8414-4041
Max J. Scheyerer https://orcid.org/0000-0003-1392-3990
References
- 1.Ryan MD, Henderson JJ. The epidemiology of fractures and fracture-dislocations of the cervical spine. Injury. 1992;23:38-40. [DOI] [PubMed] [Google Scholar]
- 2.Asemota AO, Ahmed AK, Purvis TE, Passias PG, Goodwin CR, Sciubba DM. Analysis of cervical spine injuries in elderly patients from 2001 to 2010 using a nationwide database: Increasing incidence, overall mortality, and inpatient hospital charges. World Neurosurg. 2018;120:e114-e130. doi: 10.1016/j.wneu.2018.07.228 [DOI] [PubMed] [Google Scholar]
- 3.Hasler RM, Exadaktylos AK, Bouamra O, et al. Epidemiology and predictors of cervical spine injury in adult major trauma patients. A multicenter cohort study. J Trauma Acute Care Surg. 2012;72:975-981. doi: 10.1097/TA.0b013e31823f5e8e [DOI] [PubMed] [Google Scholar]
- 4.Chapman J, Smith JS, Kopjar B, et al. The AOSpine North America Geriatric Odontoid fracture mortality study: A retrospective review of mortality outcomes for operative versus nonoperative treatment of 322 patients with long-term follow-up. Spine. 2013;38:1098-1104. doi: 10.1097/BRS.0b013e318286f0cf [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vaccaro AR, Kepler CK, Kopjar B, et al. Functional and quality-of-life outcomes in geriatric patients with type-II dens fracture. J Bone Joint Surg Am. 2013;95:729-735. doi: 10.2106/JBJS.K.01636 [DOI] [PubMed] [Google Scholar]
- 6.Venkatesan M, Northover JR, Wild JB, et al. Survival analysis of elderly patients with a fracture of the odontoid peg. Bone Joint Lett J. 2014;96-B:88-93. doi: 10.1302/0301-620X.96B1.32024 [DOI] [PubMed] [Google Scholar]
- 7.Pal D, Sell P, Grevitt M. Type II odontoid fractures in the elderly: An evidence-based narrative review of management. Eur Spine J. 2011;20:195-204. doi: 10.1007/s00586-010-1507-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lewkonia P, Dipaola C, Schouten R, Noonan V, Dvorak M, Fisher C. An evidence-based medicine process to determine outcomes after cervical spine trauma. What surgeons should be telling their patients. Spine. 2012;37:E1140-E1147. doi: 10.1097/BRS.0b013e31825b2c10 [DOI] [PubMed] [Google Scholar]
- 9.Sasso RC. C2 dens fractures: Treatment options. J Spinal Disord. 2001;14:455-463. [DOI] [PubMed] [Google Scholar]
- 10.Watts A, Athanassacopoulos M, Breakwell L, et al. Management of C2 odontoid peg fragility fractures - A UK survey of spinal surgeons. Injury. 2022;53:1057-1061. doi: 10.1016/j.injury.2021.09.057 [DOI] [PubMed] [Google Scholar]
- 11.Osterhoff G, Schnake K, Scheyerer MJ, et al. Empfehlungen zu Diagnostik und Behandlung von Frakturen des Dens axis bei geriatrischen Patienten. Z Orthop Unfall. 2020;158:647-656. doi: 10.1055/a-0989-2791 [DOI] [PubMed] [Google Scholar]
- 12.Stiell IG, Wells GA, Vandemheen KL, et al. The Canadian C-spine rule for radiography in alert and stable trauma patients. JAMA, J Am Med Assoc. 2001;286:1841-1848. [DOI] [PubMed] [Google Scholar]
- 13.Leidel BA, Kanz K-G, Mutschler W. Evidenzbasiertes diagnostisches Vorgehen bei Verdacht auf stumpfes HWS-Trauma. Entwicklung eines Algorithmus. Unfallchirurg. 2005;108:905908-906619. doi: 10.1007/s00113-005-0968-2 [DOI] [PubMed] [Google Scholar]
- 14.Inaba K, Byerly S, Bush LD, et al. Cervical spinal clearance: A prospective Western Trauma Association Multi-institutional Trial. J Trauma Acute Care Surg. 2016;81:1122-1130. doi: 10.1097/TA.0000000000001194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ulm AJ, Quiroga M, Russo A, et al. Normal anatomical variations of the V- segment of the vertebral artery: Surgical implications. J Neurosurg Spine. 2010;13:451-460. doi: 10.3171/2010.4.SPINE09824 [DOI] [PubMed] [Google Scholar]
- 16.Wakao N, Takeuchi M, Nishimura M, et al. Risks for vascular injury during anterior cervical spine surgery. Prevalence of a medial loop of vertebral artery and internal carotid artery. Spine. 2016;41:293-298. doi: 10.1097/BRS.0000000000001241 [DOI] [PubMed] [Google Scholar]
- 17.Deluca A, Wichlas F, Deininger C, Traweger A, Mueller EJ. Reevaluation of a classification system: Stable and unstable odontoid fractures in geriatric patients-a radiological outcome measurement. Eur J Trauma Emerg Surg. 2022;48:2967-2976. doi: 10.1007/s00068-022-01985-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Anderson LD, D'Alonzo RT. Fractures of the odontoid process of the axis. The Journal of bone and joint surgery. J Bone Joint Surg Am. 1974;56:1663-1674. [PubMed] [Google Scholar]
- 19.Eysel P, Roosen K. Ventrale oder dorsale Spondylodese der Densbasisfraktur--eine neue Klassifikation zur Wahl des chirurgischen Zuganges. Zentralbl Neurochir. 1993;54:159-165. [PubMed] [Google Scholar]
- 20.Grauer JN, Shafi B, Hilibrand AS, et al. Proposal of a modified, treatment-oriented classification of odontoid fractures. Spine J. 2005;5:123-129. doi: 10.1016/j.spinee.2004.09.014 [DOI] [PubMed] [Google Scholar]
- 21.Robinson A-L, Möller A, Robinson Y, Olerud C. C2 fracture subtypes, incidence, and treatment allocation change with age: A retrospective cohort study of 233 consecutive cases. BioMed Res Int. 2017;2017:8321680. doi: 10.1155/2017/8321680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Deng H, Yue JK, Upadhyayula PS, et al. Odontoid fractures in the octogenarian: A systematic review and meta-analysis. J Neurosurg Sci. 2016;60:543-555. [PubMed] [Google Scholar]
- 23.FAure A, Graillon T, PeSenti S, FAure A, Blondel B, FuenteS S. Trends in the surgical management of odontoid fractures in patients above 75 years of age: Retrospective study of 70 cases. Orthop Traumatol Surg Res. 2017;103:1221-1228. doi: 10.1016/j.otsr.2017.07.008 [DOI] [PubMed] [Google Scholar]
- 24.Rizvi SAM, Helseth E, Rønning P, et al. Odontoid fractures: Impact of age and comorbidities on surgical decision making. BMC Surg. 2020;20:236. doi: 10.1186/s12893-020-00893-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nourbakhsh A, Shi R, Vannemreddy P, Nanda A. Operative versus nonoperative management of acute odontoid Type II fractures: A meta-analysis. J Neurosurg Spine. 2009;11:651-658. doi: 10.3171/2009.7.SPINE0991 [DOI] [PubMed] [Google Scholar]
- 26.Robinson Y, Robinson A-L, Olerud C. Systematic review on surgical and nonsurgical treatment of type II odontoid fractures in the elderly. BioMed Res Int. 2014;2014:231948. doi: 10.1155/2014/231948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chibbaro S, Mallereau C-H, Ganau M, et al. Odontoid Type II fractures in elderly: What are the real management goals and how to best achieve them? A multicenter European study on functional outcome. Neurosurg Rev. 2022;45:709-718. doi: 10.1007/s10143-021-01594-2 [DOI] [PubMed] [Google Scholar]
- 28.Hart R, Saterbak A, Rapp T. Nonoperative management of dens fracture nonunion in elderly patients without myelopathy. Spine. 2000;25:1339-1343. doi: 10.1097/00007632-200006010-00004 [DOI] [PubMed] [Google Scholar]
- 29.Crockard HA, Heilman AE, Stevens JM. Progressive myelopathy secondary to odontoid fractures: Clinical, radiological, and surgical features. J Neurosurg. 1993;78:579-586. doi: 10.3171/jns.1993.78.4.0579 [DOI] [PubMed] [Google Scholar]
- 30.Florman JE, Gerstl JVE, Kilgallon JL, Riesenburger RI. Fibrous nonunion of odontoid fractures: Is it safe to accept nonoperative management? A systematic review. World Neurosurg. 2022;164:298-304. doi: 10.1016/j.wneu.2022.05.116 [DOI] [PubMed] [Google Scholar]
- 31.Alluri R, Bouz G, Solaru S, Kang H, Wang J, Hah RJ. A nationwide analysis of geriatric odontoid fracture incidence, complications, mortality, and cost. Spine. 2021;46:131-137. doi: 10.1097/BRS.0000000000003734 [DOI] [PubMed] [Google Scholar]
- 32.von Glinski A, Frieler S, Elia C, et al. Risk factors associated with 90-day readmissions following odontoid fractures: A nationwide readmissions database study. Spine. 2021;46:1039-1047. doi: 10.1097/BRS.0000000000004010 [DOI] [PubMed] [Google Scholar]
- 33.Dhall SS, Yue JK, Winkler EA, Mummaneni PV, Manley GT, Tarapore PE. Morbidity and mortality associated with surgery of traumatic C2 fractures in octogenarians. Neurosurgery. 2017;80:854-862. doi: 10.1093/neuros/nyw168 [DOI] [PubMed] [Google Scholar]
- 34.Koech F, Ackland HM, Varma DK, Williamson OD, Malham GM. Nonoperative management of type II odontoid fractures in the elderly. Spine. 2008;33:2881-2886. doi: 10.1097/BRS.0b013e31818d5407 [DOI] [PubMed] [Google Scholar]
- 35.Ajani AE, Cooper DJ, Scheinkestel CD, Laidlaw J, Tuxen DV. Optimal assessment of cervical spine trauma in critically ill patients: A prospective evaluation. Anaesth Intensive Care. 1998;26:487-491. [DOI] [PubMed] [Google Scholar]
- 36.Stein G, Meyer C, Marlow L, et al. Typ-II-Densfrakturen des alten Menschen und therapiebedingte Mortalität: Konservative oder operative Behandlung. Unfallchirurg. 2017;120:122-128. doi: 10.1007/s00113-015-0057-0 [DOI] [PubMed] [Google Scholar]
- 37.De Bonis P, Iaccarino C, Musio A, et al. Functional outcome of elderly patients treated for odontoid fracture: A multicenter study. Spine. 2019;44:951-958. doi: 10.1097/BRS.0000000000002982 [DOI] [PubMed] [Google Scholar]
- 38.Müller EJ, Wick M, Russe O, Muhr G. Management of odontoid fractures in the elderly. Eur Spine J. 1999;8:360-365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Graffeo CS, Perry A, Puffer RC, et al. Deadly falls: Operative versus nonoperative management of Type II odontoid process fracture in octogenarians. J Neurosurg Spine. 2017;26:4-9. doi: 10.3171/2016.3.SPINE151202 [DOI] [PubMed] [Google Scholar]
- 40.Smith S, Somogyi R, Lin C, Yoo JU. Surgical management of Type II displaced dens fractures improves one-year mortality in elderly patients. Spine. 2022;47:1157-1164. doi: 10.1097/BRS.0000000000004383 [DOI] [PubMed] [Google Scholar]
- 41.Gembruch O, Lemonas E, Ahmadipour Y, et al. Treatment of odontoid Type II fractures in octogenarians: Balancing two different treatment strategies. Neurospine. 2019;16:360-367. doi: 10.14245/ns.1836250.125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Honda A, Michihata N, Iizuka Y, et al. Clinical features and early post-operative complications of isolated C2 odontoid fractures: A retrospective analysis using a national inpatient database in Japan. Eur Spine J. 2021;30:3631-3638. doi: 10.1007/s00586-021-06862-9 [DOI] [PubMed] [Google Scholar]
- 43.Lukins T, Nguyen L, Hansen MA, Ferch RD. Identifying factors influencing mortality in patients aged over 65 following an acute type II odontoid process fracture. A retrospective cohort study. Eur Spine J. 2021;30:1551-1555. doi: 10.1007/s00586-020-06694-z [DOI] [PubMed] [Google Scholar]
- 44.Robinson A-L, Olerud C, Robinson Y. Surgical treatment improves survival of elderly with axis fracture-a national population-based multiregistry cohort study. Spine J. 2018;18:1853-1860. doi: 10.1016/j.spinee.2018.03.021 [DOI] [PubMed] [Google Scholar]
- 45.Borsotti F, Starnoni D, Ecker T, Coll JB. One-year follow-up for type II odontoid process fractures in octogenarians: Is there a place for surgical management? Surg Neurol Int. 2020;11:285. doi: 10.25259/SNI_376_2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Carlstrom LP, Helal A, Perry A, Lakomkin N, Graffeo CS, Clarke MJ. Too frail is to fail: Frailty portends poor outcomes in the elderly with type II odontoid fractures independent of management strategy. J Clin Neurosci. 2021;93:48-53. doi: 10.1016/j.jocn.2021.08.027 [DOI] [PubMed] [Google Scholar]
- 47.Shafafy R, Valsamis EM, Luck J, et al. Predictors of mortality in the elderly patient with a fracture of the odontoid process. Bone Joint Lett J. 2019;101-B:253-259. doi: 10.1302/0301-620X.101B3.BJJ-2018-1004.R1 [DOI] [PubMed] [Google Scholar]
- 48.Coleman N, Chan H-YH, Gibbons V, Baker JF. Comparison of hard and soft cervical collars for the management of odontoid peg fractures in the elderly. Geriatr Orthop Surg Rehabil. 2022;13:21514593211070263. doi: 10.1177/21514593211070263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Delcourt T, Begue T, Saintyves G, Mebtouche N, Cottin P. Management of upper cervical spine fractures in elderly patients. Current trends and outcomes. Injury. 2015;46(suppl 1):S24-S27. doi: 10.1016/S0020-1383(15)70007-0 [DOI] [PubMed] [Google Scholar]
- 50.Kurucan E, Sulovari A, Thirukumaran C, Greenstein A, Molinari R, Mesfin A. Volume-outcome relationship in halo vest utilization for C2 fractures. Spine J. 2020;20:1676-1684. doi: 10.1016/j.spinee.2020.05.543 [DOI] [PubMed] [Google Scholar]
- 51.Vergara P, Bal JS, Hickman Casey AT, Crockard HA, Choi D. C1-C2 posterior fixation: Are 4 screws better than 2? Neurosurgery. 2012;71:86-95. doi: 10.1227/NEU.0b013e318243180a [DOI] [PubMed] [Google Scholar]
- 52.Claybrooks R, Kayanja M, Milks R, Benzel E. Atlantoaxial fusion: A biomechanical analysis of two C1-C2 fusion techniques. Spine J. 2007;7:682-688. doi: 10.1016/j.spinee.2006.08.010 [DOI] [PubMed] [Google Scholar]
- 53.Magerl F, Seemann P-S. Stable posterior fusion of the atlas and axis by transarticular screw fixation. In: Kehr P, Weidner AH, eds Cervical Spine I. Vienna: Springer Vienna; 1986:322-327. doi: 10.1007/978-3-7091-8882-8_59 [DOI] [Google Scholar]
- 54.Bhimani AD, Chiu RG, Esfahani DR, et al. C1-C2 fusion versus occipito-cervical fusion for high cervical fractures: A multi-institutional database analysis and review of the literature. World Neurosurg. 2018;119:e459-e466. doi: 10.1016/j.wneu.2018.07.182 [DOI] [PubMed] [Google Scholar]
- 55.Patterson JT, Theologis AA, Sing D, Tay B. Anterior versus posterior approaches for odontoid fracture stabilization in patients older than 65 years: 30-day morbidity and mortality in a national database. Clin Spine Surg. 2017;30:E1033-E1038. doi: 10.1097/BSD.0000000000000494 [DOI] [PubMed] [Google Scholar]
- 56.Shousha M, Mosafer A, Boehm H. Infection rate after transoral approach for the upper cervical spine. Spine. 2014;39:1578-1583. doi: 10.1097/BRS.0000000000000475 [DOI] [PubMed] [Google Scholar]
- 57.Sen MK, Steffen T, Beckman L, Tsantrizos A, Reindl R, Aebi M. Atlantoaxial fusion using anterior transarticular screw fixation of C1-C2: Technical innovation and biomechanical study. Eur Spine J. 2005;14:512-518. doi: 10.1007/s00586-004-0823-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Marciano RD3, Seaman B, Sharma S, Wood T, Karas C, Narayan K. Incidence of dysphagia after odontoid screw fixation of type II odontoid fracture in the elderly. Surg Neurol Int. 2018;9:84. doi: 10.4103/sni.sni_231_17 [DOI] [PMC free article] [PubMed] [Google Scholar]