Abstract
Study Design
Systematic review.
Objectives
Spinal orthoses are frequently used to non-operatively treat osteoporotic vertebral fractures (OVF), despite the available evidence is rare. Previously systematic reviews were carried out, presenting controversial recommendations. The present study aimed to systematic review the recent and current literature on available evidence for the use of orthoses in OVF.
Methods
A systematic review was conducted using PubMed, Medline, EMBASE and CENTRAL databases. Identified articles including previous systematic reviews were screened and selected by three authors. The results of retrieved articles were presented in a narrative form, quality assessment was performed by two authors using scores according to the study type.
Results
Thirteen studies (n = 5 randomized controlled trials, n = 3 non- randomized controlled trials and n = 5 prospective studies without control group) and eight systematic reviews were analyzed. Studies without comparison group reported improvements in pain, function and quality of life during the follow-up. Studies comparing different types of orthoses favor non-rigid orthoses. In comparison to patients not wearing an orthosis three studies were unable to detect beneficial effects and two studies reported about a significant improvement using an orthosis. In the obtained quality assessment, three studies yielded good to excellent results. Previous reviews detected the low evidence for spinal orthoses but recommended them.
Conclusion
Based on the study quality and the affection of included studies in previous systematic reviews a general recommendation for the use of a spinal orthosis when treating OVF is not possible. Currently, no superiority for spinal orthoses in OVF treatment was found.
Keywords: osteoporosis, vertebral fracture, spine fracture, orthosis, conservative treatment
Introduction
Spinal orthoses are traditionally applied treating thoracolumbar fractures, but their mechanism is currently not completely understood.1,2 Nevertheless, over 60% of spine surgeons prescribe an orthosis for the treatment of fractures, degenerative diseases or use them after surgical treatment. 3 Most recently a systematic review found no evidence treating traumatic spinal fractures conservatively with an orthosis. 4 However, for osteoporotic vertebral fractures (OVF), spinal orthosis are recommended and previous systematic reviews highlight their benefits though the evidence of included studies is limited.5-11 But methodical aspects of the included studies were not fully evaluated possibly resulting in controversial recommendations.5-12 Additionally, several aspects like the type of diagnostics used, fracture region, number of fractures, orthosis treatment (daily treatment and duration) were sparsely reported. Although several reviews highlight the low quality of included studies, their recommendations are based on them. Besides a risk of bias (RoB) assessment, quality examinations are rare. We aimed to report on the evidence for spinal orthosis treating OVF and describe the treated population, fracture morphology and orthotic treatment. Secondarily, the investigated publications were graded using quantitative quality scores. Thirdly, previous systematic reviews were analyzed and qualitatively graded.
Materials and Methods
The present study was registered on the International Prospective Register of Systematic Reviews (PROSPERO) network (CRD42020177426) before starting the review process and performed accordingly to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
The first authors searched within PubMed, Medline, EMBASE and Cochrane Central Register of Controlled Trials (CENTRAL) without a limitation of the publication date but limited to English and German publications until April 2020 and updated the studies using PubMed messenger. According to the PI (CO) scheme the following question was formulated: Does spinal orthoses improve the outcome of patients suffering from thoracolumbar spinal fragility fractures and related deformities?
An example for the search strategy is outlined for PubMed:
(((((Orthotic devices [Mesh] OR Spinal orthos*) AND ((Spinal Fractures [Mesh] OR Spinal fracture) OR (Spinal Curvatures [Mesh] OR (Adult spinal deformity)) OR ((Fractures, Stress [Mesh] AND Spine) OR (Fracture, Spontaneous [Mesh] AND Spine)) OR (Osteoporosis [Mesh] AND Spine) OR (Osteoporotic Fractures [Mesh] AND Spine))) AND (“german" [Language] OR “english" [Language])) NOT (“case reports" [All Fields] OR “comment" [All Fields] OR “letter" [All Fields])) NOT cervical). Case reports, comments and narrative reviews were excluded. An exclusion based on the level of evidence or study type was not done. The remaining manuscripts were considered for inclusion. Retrieved titles of studies, abstracts and full texts were screened in triplicate by PP, UJS, CEH. At each step controversy was discussed until consensus was achieved. The screening process and extracted data included in tables and figures are presented in Figure 1. Data extraction and qualitative assessment were done by PP and UJS using a predefined Research electronic data capture (REDCap) form. 13 The Coleman Methodology Score (CMS) was assessed for all studies. 14 Higher scores indicate a less risk for bias and confounding factors. The CMS was graded as followed: excellent (85-100 points), good (70-84 points), fair (50-69 points), and poor (<50 points). 15 For non- randomized trials the Newcastle-Ottawa Scale (NOS) was assessed. 16 In addition, the total score was presented in percentage of the maximum available score, low risk of bias was considered if the score achieved ≥50% in the three categories. 17 Randomized controlled trials (RCT) were examined using the modified RoB tool. 18 Based on the 10 questions a score of 10 points is possible; a point is given for each question. A score >8 points indicate low risk of bias. In addition, the Detsky Score was used, a score ≥15 (75%) indicate high quality.18,19
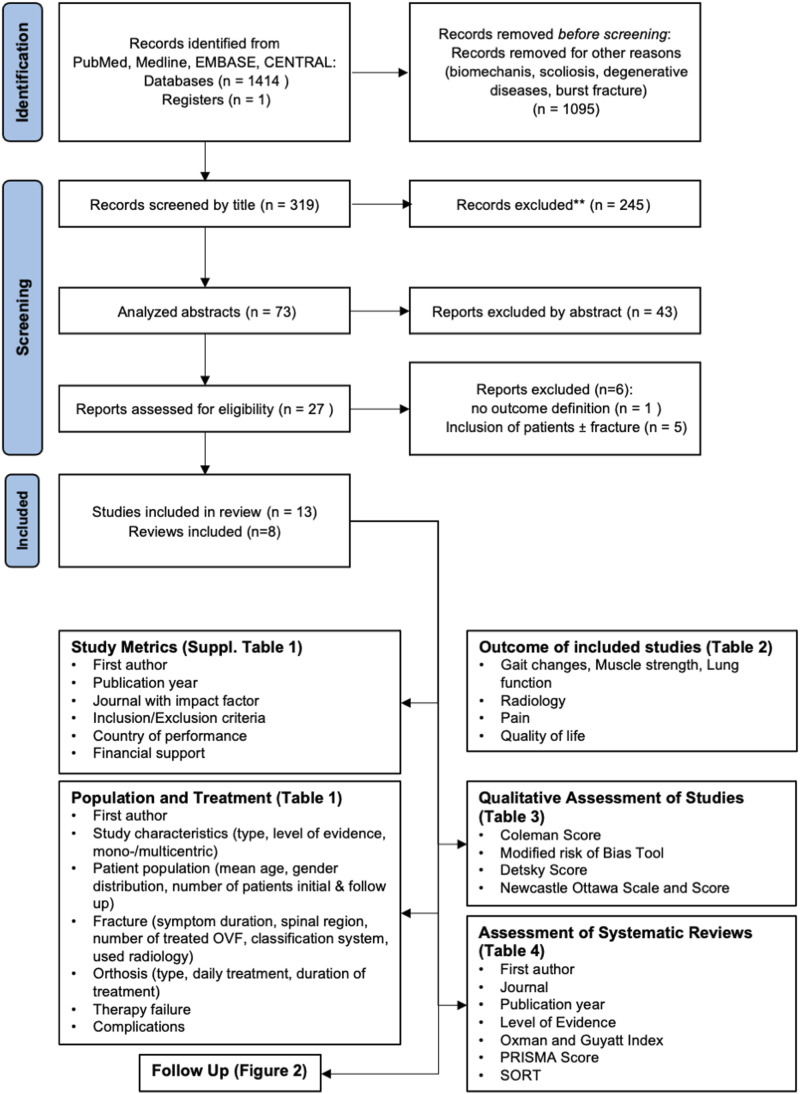
Figure 1.
Scheme according to PRISMA criteria and retrieved data. ** Manuscripts were excluded due to wrong treatment indication or comparison to surgery (scoliosis, comparison of non-operative to operative treatment, missing relevant outcome). Retrieved studies were additionally excluded due to missing outcome definition (n = 1), 37 inclusion of patients ± fracture (n = 5).38,41,55-57
Results extracted from analyzed studies were summarized in a narrative preformatted form after review of each author and approved by PP, UJS, CEH. The primary outcome were gait changes, radiological changes, pain, functional outcome, and quality of life (QoL). If two studies seemed to share data, these studies were summarized.
Studies were categorized as followed: report of only one orthosis without comparison, comparison of orthoses types, comparison of orthosis to no orthosis.
Previous systematic reviews were assessed regarding the following parameters: research question, similar articles included, reason for repetition of the review mentioned, recommendation of spinal orthosis, Oxman and Guyatt Index and PRISMA Score and Strength of Recommendation Taxonomy (SORT). The Oxman and Guyatt Index was categorized as followed: strong weakness 1-2 points, severe 3-4 points, moderate 5-6 points, minimal >7 points.20,21
The PRIMSA score was graded as followed: <19 low quality, 19-22.5 moderate quality, >22.5 high quality.22,23
A meta-analysis was not performed due to the heterogeneity of data.
Results
Thirteen studies and eight systematic reviews were analyzed. Seven studies were performed in Asia (four in Japan24-27 and each one from China, 28 South Korea, 29 Taiwan 30 ) and six from Europe (two from Germany31,32 summarized to one due to an assumed shared patient cohort and one from Netherlands, 33 Denmark, 34 Greece, 35 and Italy 36 each; Supplemental Table 1). Seven studies defined a precise inclusion time frame.24,26,27,29,33,34,36 All studies were unblinded. Three studies had a financial support,29,31,32 two were funded by an orthosis manufacturer.31,32
The level of evidence was 4 in three studies,24,33,34 2 in eight studies25,27,28,30-32,35,36 and 1 in two studies26,29 (Table 1). Ten studies24,27,29,33,34 were monocentric and three multicentric.25,26,36 The mean age of the included patients was more than 65 years in all studies. Exclusively female patients were included in seven studies.26,28,31-35 Symptom duration of patients ranged from days (four studies),25,27-29 weeks (two studies)26,33 to months (two studies)32,34 or were not defined (five studies).24,30,31,35,36 The fracture was located in the thoracic and lumbar spine in seven studies,24,25,27-29,35,36 thoracolumbar junction in two studies26,33 and not defined in four studies.30-32,34 The number of treated fractures ranged from 1 (six studies24-27,29,36), 2 (four studies31-34) to >3 in one study 28 and was not defined in two studies.30,35 Three studies used a fracture classification system (AO, Genant, Sugita).25,27,36
Table 1.
Population and Treatment. Study Characteristics, Investigated Patient Cohort and Fracture Related Parameters as Well Orthotic Treatment, Therapy Failure and Complications are Presented.
| Mei-Yun Liaw | Eva Jacobs | Tetsuya Abe | Kenji Murata | Gitte Hoff Valentin | Tsuyoshi Kato | Meng Li | Luigi Meccariello | Ho-Joong Kim | Yannis Dionyssiotis | Masatoshi Hoshino | Michael Pfeifer 2004 | Michael Pfeifer 2011 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study Characteristics | Type | PoS | PoS | PoS | PoS | PoS | RCT | RCT | Non-RCT | RCT | Non-RCT | Non-RCT | RCT | RCT |
| Level of Evidence | 2c | 4 | 4 | 2c | 4 | 1b | 2b | 2b | 1b | 2c | 2c | 2c | 2c | |
| Mo/Mult | mo | Mo | mo | mo | mo | mu | mo | mu | Mo | mo | mu | mo | mo | |
| Patient population | Mean age | 68.2 | 69 | 81.2 | 75.3 | 70.8 | Soft brace 75.5 Hard brace: 76.0 | Spinomed: 82 Soft lumbar orthosis: 81 | 3-PO: 81.9 Spinomed 82.8 | No brace: 72.3 soft brace: 66.8 rigid 71.8 | No orthosis: 61 Spinomed: 72.3; p=0.014 | No brace: 77 Brace: 76.2 | Control: 72.3 Spinomed: 72.8 | Control: 69.7 Spinomed: 72.8 Spinomed active: 72.3 |
| Gender Distribution (f:m) | 37:10 | 15:0 | 106:18 | 39:14 | 13:0 | 284:0 | 51:0 | 100:40 | 41:19 | 20:0 | 303:59 | 62:0 | 108:0 | |
| Number of patients | 108 | |||||||||||||
| intial | 47 | 15 | 124 | 55 | 13 | 284 | 51 | 140 | 60 | 20 | 362 | 62 | 108 | |
| Follow-up | - | 15 | 124 | 53 | 13 | 228 | 51 | 140 | 49 | 20 | 362 | 62 | 108 | |
| Fracture | Symptom duration | Nd | <3 we | Nd | <1 we | <3 we | ||||||||
| Spinal Region | Nd | TLJ (TH11-L4) | TH+L (TH4-L5) | TH+L (TH1-L5) | nd | TLJ (TH12-L2) | TH+L (TH4-L5) | TH+L (TH6-L3) | TH+L (TH7-L3) | TH+L | TH+L (TH5-L5) | nd | <6 mo | |
| Number of treated OVF | Nd | 1-2 | 1 | 1 | nd | 1 | 2 | 2 | ||||||
| Classification System | none | none | none | AO classification | none | none | none | Genant’s classification | none | Sugita et al. | None | None | ||
| Radiology | ||||||||||||||
| X-ray | x | x | x | x | x | x | x | x | x | x | x | x | x | |
| CT | x | — | — | — | x | — | — | x | - | — | — | — | — | |
| MRI | — | x | — | x | — | — | ||||||||
| Orthoses | Type | TLSO Knight-Taylor brace | TLSO Osteolind Plus | 3-po Jewett brace | Plastic rigid TLSO | Spinomed III | Rigid TLSO (n=141) | 1 we TLSO 2-3 we Spinomed+lumbar orthosis (n=27) | 3-PO (n=72) | No brace (n = 20) | No orthosis (n = 10) | No orthosis (n=35) | No orthosis (n=31) | After 6 mon start with Spinomed (n=36) |
| Soft TLSO (n = 143) | 2-3 we soft lumbar orthosis (n = 24) | Spinomed (n = 68) | Rigid brace (n = 20) | Spinomed (n=10) | Tailor-made hard brace (n = 71) | Spinomed (n=31) | Spinomed for 12 months (n= 36) | |||||||
| Soft brace (n = 20) | Tailor-made elastic braces (n = 190) | Spinomed active for 12 months (n=36) | ||||||||||||
| Ready-made elastic braces (n = 66) | ||||||||||||||
| Daily Treatment | Nd | 24 h/d 6 we | nd | except for shower | 15 min/d for 14 d increasing 2-4h/d in the next 10 we | 24 h/d | 24 h/d 3 h/d Spinomed soft lumbar orthosis rest | sitting and standing | 24 h/d except during lying | 2 h/d | n/d | 2 h/d | 2 h/d | |
| Duration of Treatment | nd | 6 mon | 3-6 mon | min. 2 mon | 3 mon | 3mon | 3 we | 2.5 mon | 2mon | - | 4.1 + 1.9 mon | 6-12 mon | 6-12 mon | |
| Therapy failure | nr | nr | 10 (surgical intervention) | non-union: n=6 | nr | nr | nr | Non-union: 3-PO n = 5, Spinomed n = 4 | nr | nr | nr | nr | nr | |
| Complications | nr | No complications | Urinary tract infection (n = 10) | Decubitus (n = 3) | — | New OVF (n=16) | nr | Gastric ulcer (each n = 6 3-PO, Spinomed) | — | nr | nr | nr | nr | |
| Pneumonia (n = 5) | Pneumonia (n = 1) | Subjected to surgery (n=2) | Decubitus (n = 8 3-PO) | |||||||||||
| Ileus (n=1) | Inguinal hernia (n = 4 3-PO) | |||||||||||||
| Pulmonary disease (n = 4 3-PO) | ||||||||||||||
| Re-fracture (n = 4 3-PO, n = 2 Spinomed) | ||||||||||||||
PoS - Prospective observational study without comparison group; RCT – randomized controlled trial; Mo- monocentric; Mu- multicentric, national; 3-PO- 3-point orthosis; we- weeks; mon- months; d – days; nd – not defined; th- thoracic; TLJ- thorcolumbar junction; l- lumbar; TLSO- thoracolumbar orthosis; nr – not reported.
Six studies used solely radiographs28,30-32,34,35 and five studies radiographs and magnetic resonance imaging (MRI).25-27,29,33 Each one study combined X-rays, CT scan and MRI 24 or X-rays and CT. 36
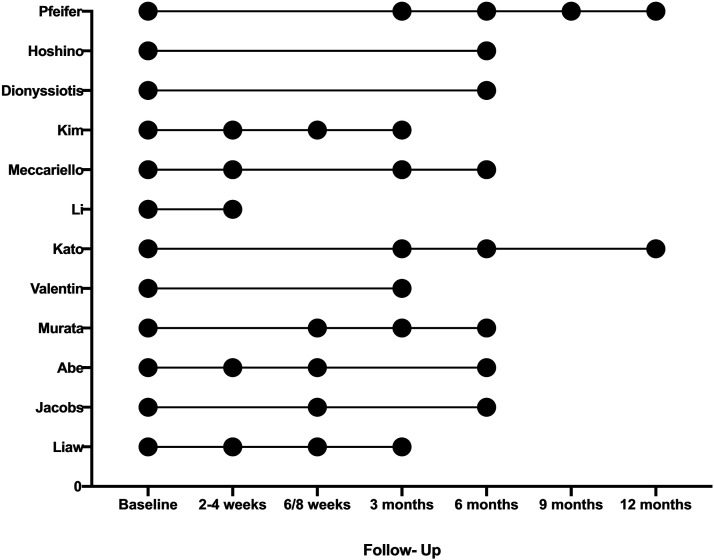
Daily treatment ranged from 15 minutes/day (one study 34 ) at the beginning, 2-3 hours/day (four studies28,31,32,35) to the whole day (four studies26,27,29,33) or only during sitting and standing. 36 Three studies did not define the daily duration.24,25,30 The duration of treatment ranged from 2.5 months to 1 year (Table 1). The different follow- up times are shown in Figure 2.
Figure 2.
Presentation of the different follow-up visits of the included studies.
Spinal Orthosis Without Comparison (n=5)
By applying an orthosis an immediate and partial persistent improvements on gait stability resulting in an decrease of falls as well as an increase of back extensor muscle strength was observed.30,33,34 Initially observed changes in alignment were not persistent during the follow-up though the wedge angle increased until 6 months. 33 Jacobs et al 33 observed a significant pain reduction Tables 1 and 2. 33
Table 2.
Summarized Outcomes of Included Studies Separated According to the Paragraphs.
| First Author | Gait changes, Muscle strength, Lung function | Radiology | Pain | Quality of Life | |||
|---|---|---|---|---|---|---|---|
| Score | Domain | Different Time Points | |||||
| Spinal orthosis without comparison | Mei-Yun Liaw | Greater average stability (MD 4.7%, p < .001) | — | — | — | ||
| Frequency of falls closed eyes (MD 12, p = .008) | |||||||
| Eva Jacobs | Decreased trunk motion (decline 51%, p = .006) | Wedge angle 6 weeks (MD 3.94, p < .001) | VAS (MD 3 po, p < .001) | QUALEFFO 41 | + pain, physical function and social function, p < .001 | — | |
| Increased walking speed (MD 0.21 m/s, p < .001) | |||||||
| Increased stride length (0.05 m, p = 0.007) | |||||||
| Decreased stride time (0.06 s, p = .003) | Global sagittal alignment (MD 2.04, p > .05) | ± mental and general health | |||||
| Decreased cadence (5.62 steps/min, p = .003) | |||||||
| Decreased step width (0.02, p = .041) | |||||||
| Tetsuya Abe | — | Delayed union (n = 16, 14%) | — | ||||
| Kenji Murata | — | Bony union (3 mon 79.2%; 6 mon 88.7%) | — | JOABPEQ | Low back pain (MD 36.5 po, p < .05) | — | |
| Lumbar function (MD 37.7 po, p < .05) | |||||||
| Walking ability (MD 33.2 po, p < .05) | |||||||
| Social life function (MD 26.2 po, p < .05) | |||||||
| Mental health (MD 18.6 po, p < .05) | |||||||
| Gitte Hoff Valentin | Increase of back extensor strength (MD 40N, p < .01) | — | VAS (MD 1 point, p = .06) | SF-36 | PCS (MD 6.5 po, p = .07) | — | |
| MCS (MD 0.3 po, p = .70) | |||||||
| Comparison of different types of spinal orthoses | Tsuyoshi Kato | — | AVBCP (12 we MD 3.9; p = .04002; 24 we MD 3.9; p = .07; 48 we MD 2.5, p = .2) | VAS (12 we MD 0.2 points, p = .095; 48 we MD -1.9, p = .43) | EQ-5D-3L | 12 we MD 0.02 po, p = .58 | |
| 48 we MD 0.01 po, p = .67 | |||||||
| JOABPEQ | Pain related disorder | 12 we MD 3.6 po, p = .38 | |||||
| 48 we MD 3.3 po, p = .43 | |||||||
| Lumbar function | 12 we MD 4.2 po, p = .29 | ||||||
| 48 we MD -1.6 po, p = .91 | |||||||
| Walking ability | 12 we MD 0.3 po, p = .92 | ||||||
| 48 we MD 0.4 po, p = .82 | |||||||
| Social life function | 12 we MD 2.7 po, p = .36 | ||||||
| 48 we MD 5.7 po, p = .12 | |||||||
| Mental health | 12 we MD 2.4 po, p = .14 | ||||||
| 48 we MD -0.3 po, p = .96 | |||||||
| Meng Li | — | — | VAS (MD SP 2.7 po, MD SOL 1.8 po, p for time < .05) | FIM- motor score (MD SP 11.8 po, MD SOL 9.6 po, p for time < .05) | — | ||
| Elderly Mobility Score (MD SP 5.1 po, MD SOL 5.2 po, p for time<0.05) | |||||||
| Luigi Meccariello | FEV1 (MD 3 mon 2.3%, MD 6 mon 11.5, p < .05) | DI (MD 6 mon 1.1°, p > .05) | VAS (MD 3 mon 1.3 po, MD 6 mon 1.7 po, p < .05) | OLBPDQ | 3 mon MD 6.3 po, p < .05 | ||
| CA (MD 6 mon 0.2°, p > .05) | 6 mon MD 13.7po, p < .05 | ||||||
| RKA (MD 3 mon 0.3°, 6 mon 0°, p > .05) | |||||||
| Spinal orthosis to no orthosis | Ho-Joong Kim | — | BCR (p = .237) | VAS (p = .292) | |||
| Opioid use (MAXD 6.1%, p=0.912) | |||||||
| Yannis Dionyssiotis | Abdominal strength (MD 21.3N, p = .8) | — | VAS (MD 4 po, p = .67) | Baseline adjusted ODI (MD 1.88 to 2.49, p > .05) | — | ||
| ODI (p = .26) | PCS (p = .716) | ||||||
| Back extensor strength (MD 28.3N, p = .6) | SF- 36 | MCS (p = .889) | |||||
| Masatoshi Hoshino | — | Vertebral collapse (MAXD 0.57) | Prolonged back pain (MAXD OR 0.51) | SF- 36 | PCS ≤ 40 (MAXD OR 0.39) | ||
| MCS ≤ 40 (MAXD OR 0.11) | — | ||||||
| Reduced ADL (MAXD OR 0.68) | |||||||
| Pfeifer | Abdominal strength (MD 71N, p < .01) | Kyphosis angle (MD 6.3°, p < .01) | Miltner’s rating scale (MD 1.6po, p < .01) | Begerow well-being scale (MD 12.7po, p < .05) | — | ||
| Back extensor strength (MD 182N, p < .01) | Leidig-Bruckner scale | PCS ≤ 40 (MAXD OR 0.39) | |||||
| FEV1 (MD 6.7%, p < .01) | MCS ≤ 40 (MAXD OR 0.11) | ||||||
MD- mean difference, EQ-5D-3L- European Quality of Life-5 Dimensions, 3-Level questionnaire, SP- Spinomed, SOL- soft lumbar orthosis, po - points, FIM- Functional Independence Measure, OLBPDQ- Oswestry Low Back Pain Disability Questionnaire Score, FEV1- forced expiratory volume in the first second, DI- Delmas Index, CA- Cobb´s angle, RKA- regional kyphosis angle, VH- vertebral body height, BCR- Body compressions ratio, OR- Odd´s ratio, MAXD maximum difference, ADL- activities of daily living.
Several aspects of QoL improved but Jacobs et al were not able to detect changes for general and mental health.27,33 In contrast, Valentin et al. did not observed significant improvements in pain and QoL. 34 The effects were predominantly found during the first 6-12 weeks.27,33 Using an orthosis resulted in a success rate of >80% analysing dynamic X-ray examination regarding persistent instability24,27 but high intensity on T2-weightened MRI and vertebral instability >5° at 3-week follow were identified as risk factors for treatment failure. 24
Comparison of Different Types of Spinal Orthoses (n = 3)
The Spinomed orthosis led to a significant higher forced expiratory volume in the first second compared to a 3-point orthosis (3-PO) Tables 1 and 2. 36
The anterior vertebral body compression percentage (AVBCP) differed between soft and rigid brace after 12 weeks but not after 24 and 48 weeks. A higher decrease was found in the rigid brace group (MD 3 points) compared to the soft brace group (MD 1.6 points) during the follow-up. 26 Other radiological parameters like the Cobb´s angle did not differ comparing a Spinomed to a 3-PO. 36
A significant improvement in pain, QoL for the Spinomed orthosis at 3- and 6 months follow-up but not after 1-week or 1-month was detected in comparison to a 3-PO. 36 Pain decreased significantly over time independent of the orthoses type. 28 In contrast to the study of Meccariello et al., QoL did not differ comparing orthoses types in two studies.26,28 No association between QoL and AVBCP was determined. 26
Spinal Orthosis to No Orthosis (n = 5)
Wearing an orthosis – independent of the type- did not lead to a significant improvement in QoL, pain, decelerated increase of radiological compression or minimized opioid use compared to patients who do not wear an orthosis.29,35 Pain and QoL improved over time independent of the orthotic treatment.25,29,35 In the study of Dionyssiotis et al, 35 the significantly younger control group refused to wear an orthosis. The two studies of Pfeifer et al31,32 were summarized because the difference of cohorts could not be ensured (please see Table 1, 31 and Group A 32 regarding age and consecutive variables). In their planned crossover study, patients refused after 6 months to discard the orthosis. In contrast to the above-mentioned studies, Pfeifer er al.31,32 observed a significant decrease for kyphosis angle using three-dimensional photomorphometry, improved body sway path length, body sway velocity, pain, QoL and abdominal and back extensor muscle strength. Noteworthy, Pfeifer et al31,32 determined similar changes starting to wear the orthosis after 6 months Tables 1 and 2.
Quality Assessment
According to the CMS 4 studies were graded as poor28,30,33,35 six studies as fair,24,25,27,31,32,34 two studies as good26,36 and one as excellent. 29 The overall NOS of non-randomized trials ranged from 22-78%, but only one study 36 achieved points in comparability and has therefore a low risk of bias. Of the RCTs, according to the RoB score two studies reached 8 points.26,29 Thus, at all no study was considered with low risk of bias. Using the Detsky score two studies were graded as high quality Table 3.26,29
Table 3.
Qualitative Assessment of the Included Studies.
| PoS/non-RCT | RCT | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PoS/non-RCT | Tetsuya Abe | Yannis Dionyssiotis | Masatoshi Hoshino | Eva Jacobs | Mei-Yun Liaw | Luigi Meccariello | Kenji Murata | Gitte Hoff Valentin | Tsuyoshi Kato | Ho-Joong Kim | Meng Li | Michael Pfeifer | Michael Pfeifer | RCT |
| Coleman Score | 61 | 33 | 51 | 44 | 39 | 72 | 69 | 51 | 84 | 89 | 46 | 67 | 64 | Coleman Score |
| Newcastle Ottawa Scale | 16 | 17 | 12 | 11 | 11 | Detsky Score | ||||||||
| Selection | ** | *** | **** | ** | * | ** | *** | ** | 8 | 8 | 2 | 3 | 3 | Risk of Bias Tool |
| Comparability | — | — | — | — | ** | — | — | low | low | high | unclear | unclear | randomization | |
| Outcome | ** | ** | ** | * | * | *** | ** | * | low | low | unclear | unclear | unclear | allocation concealment |
| Total (%) | 46% | 56% | 67% | 33% | 22% | 78% | 56% | 33% | high | unclear | unclear | unclear | unclear | surgeon or treatment provider blinding |
| low | low | unclear | unclear | unclear | assessor blinding | |||||||||
| high | unclear | unclear | high | high | patient blinding | |||||||||
| low | low | unclear | low | low | patient follow-up | |||||||||
| low | low | unclear | high | high | selective outcome reporting | |||||||||
| low | low | low | high | high | objectivity of outcomes | |||||||||
| low | low | low | low | low | surgeon experience with treatment | |||||||||
| low | low | unclear | low | low | adequate sample size | |||||||||
Studies were categorized according to the study type and parameters.
Comparison to Other Systematic Reviews (n = 8)
Two studies included a research question formulated according to the PICO scheme.5,8 Ameis et al. solely analyzed previous systematic reviews and included the review of Rzewuska et al. who aimed to determine the efficacy of conservative treatment.5,11 Both based their recommendations mainly on the studies of Pfeifer et al. Table 4.31,32
Table 4.
Assessment of the Included Systematic Reviews Including Quality Assessment and Strength of Recommendation Taxonomy (SORT).
| First Author | Journal | Publication Year | Level Of Evidence | IS/ISH/EX | Oxman & Guyatt Score | PRISMA Score | SORT |
|---|---|---|---|---|---|---|---|
| Arthur Ameis | European Spine Journal | 2018 | 3a | 6/1/5 | 5 | 11 | B |
| Victora A Goodwin | BMJ Open | 2016 | 3a | 9/7/2 | 7 | 17 | B |
| Ryan C. Hofler | WORLD NEUROSURGERY | 2020 | 3a | 16/10/6 | 5 | 16 | B |
| Yuan Zhe Jin | Journal of Korean Medical Science | 2016 | 3a | 10/8/2 | 6 | 20 | B |
| Barry Ting Sheen Kweh | Global Spine Journal | 2020 | 3a | 7/0/0 | 5 | 17 | B |
| Meredith Newman | Archives of Physical Medicine and Rehabilitation | 2016 | 2a | 12/6/6 | 7 | 16 | B |
| Michael Pfeifer | Zeitschrift für Rheumatologie | 2017 | 2a | 12/5/7 | 1 | 3 | C |
| Magdalena Rzewuska | European Spine Journal | 2015 | 1b | 5/3/2 | 8 | 25 | B |
IS- included studies, ISH- included studies in the present review, EX- excluded studies in the present review but analyzed in the respective review.
Three studies analyzed the effects of orthoses independent of their type on biomechanics, pain, QoL.7-10 Besides of bracing Goodwin et al investigated the effects of taping and Hofler and Jones included studies with a crossover design and operatively treated patients.6,12 Included articles in previous reviews, in the present review and excluded articles are summarized for each review in Table 4. The following articles were included in previous reviews and excluded here as follows: included in six6-10,12 and excluded here due to no outcome definition, 37 included in two9,10 and excluded due to language availability, included in three7,9,10 and excluded due to missing fracture status (with/without/healed) (n = 5),38−42 included in one 6 excluded because the intervention was taping, 43 included in one 11 and were excluded because primary intervention was medication, 44 included in one 12 and excluded here due to a crossover design to surgery,45,46 comparison to kyphoplasty, 47 primary comparison regarding bed rest and inclusion of traumatic fractures, 48 orthosis not primary intervention and solely report of reduction over time, 49 orthosis not primary intervention. 50
Despite five5,7-10 reviews detected the low evidence for the use of orthoses in the treatment of OVF, their use was recommended. Two studies determined inconclusive evidence for orthotic use and therefore no recommendation was given.6,11 Hofler and Jones neglected the standard use of orthosis. 12
Five studies did not mention the reason for the repetition of the systematic review.5,9-12 Three authors repeated the review because they detected missing clear recommendations, included further studies or performed statistical analyses.6-8 Six previous reviews used RoB,5-9,12 two the GRADE approach,7,11 and two a meta-analysis7,11 and one study did not perform a qualitative analysis. 9 Meta-analyses7,11 based mainly on the Pfeifer studies.31,32
According to the Oxman and Guyatt index: three reviews had minimal,6,9,11 three some5,7,12 and one with severe weakness. 10 According to the PRISMA Score six reviews were graded low,5,6,8-10,12 each one moderate 7 and high. 11 Except of one review 10 the remaining reviews had SORT grade B.
Discussion
Studies reporting on one orthosis described benefits over time and biomechanically immediately after application.
Liaw et al 30 and Jacob et al 33 showed benefits for gait parameters, decrease of falls and their persistence during follow-up but effects on function, pain and QoL remains unclear because no comparison groups are included. In addition, the orthosis showed a failure rate <25% in terms of bony union.24,27 However, there is no mandatory relation of bony union to the function and QoL.24,27 Most beneficial effects occurred in the first time after applying a spinal orthosis whereas effects after 3 months were rare 27 contradicting observations of other studies.31,32
In terms of the type of orthosis, the data favor soft orthosis or active orthosis like the Spinomed orthosis more than rigid braces based on a determined non-inferiority. Despite spinal orthosis led to a reproducible increase of trunk muscle strength, 34 previous reported improvements on pain and function were not reproducible.31,32 The observed superiority of spinal orthosis was only reported in two studies of the same author.31,32 The comparison of the here applied scores for pain, function and QoL are limited due to the missing use in the remaining studies.31,32 In addition, the authors reported these beneficial effects after delayed treatment (6 months) after inclusion.31,32 Considering the fracture union of >80% after 6 months24,27 may lead to the assumption that spinal orthosis improved osteoporotic related pain but not mandatory fracture related pain.
Here, the used diagnostics in relation to fracture age and thereby fracture related pain of the different studies should be considered. 51 The MRI was only used in six studies and was shown as appropriate diagnostic for OVF. 51 All of them comparing orthosis to no orthosis (n = 225,29) found no significant improvement by the orthosis. In addition, solely three studies25,27,36 used fracture classification systems although they are required guiding therapy and may be used to for the outcome prognosis. 52 Apart from other classification systems, for example the OF classification seems to be an appropriate classification due to the inclusion of the MRI. 53 Considering the performed quality assessment and the thereby identified higher quality studies led to the following conclusions: Comparing orthosis types, a preference for soft or active orthosis compared to rigid braces was found. Nonetheless, the highest quality study 29 showed no inferiority of patients treated without an orthosis compared to patients treated with orthosis though the patient number is limited. A larger study, 25 though with limited quality, supported these findings. Thus, spinal orthoses seem to not significantly improve the outcome of patients suffering from thoracolumbar OVF. Despite previous systematic reviews underline the limited evidence for the application of spinal orthosis and the high risk of bias of the included studies, at least weak recommendations for the application of spinal orthosis were given. At least three of them had only minimal weakness according to the Oxman and Guyatt Index. Thus, the contradicting recommendations given by us might be challenged. Compared to previous systematic reviews we performed a quality assessment and used the obtained results for our recommendations. In contrast, previously the recommendations and meta-analysis are based on two studies31,32 which were here graded with low quality and a high risk of bias. Furthermore, it was not possible to detect if these studies31,32 shared patients’ cohorts as outlined above and a previous review assumed a potential conflict of interest. 11 Therefore, though the reviews were conducted with high quality, their recommendation and analyses were affected by the included studies and the overestimation of two studies caused by their initially planned study design. 54 Currently the evidence regarding the application of spinal orthosis is limited and based on small sample size and/or low-quality studies. Therefore, large multicenter studies considering appropriate diagnostics, the use of therapy guiding classification systems and with power should be carried out. Analyzing the inclusion and exclusion criteria highlight additionally the selective reporting because especially patients with cognitive impairment or neurodegenerative diseases as well as spinal degenerative diseases were excluded but in clinical practice a relevant patient cohort.
Conclusion
After the application of a spinal orthosis pain decreases and QoL improves over time. This is not different to the outcomes of patients treated without an orthosis. Thus, a clear recommendation for the application of spinal orthosis cannot be given. Indeed, this recommendation is predominately based on non-high-quality studies but is based on the grading of the different available studies and caused by the results of a meticulous quality assessment.
Supplemental Material
Supplemental Material for Spinal Orthoses in the Treatment of Osteoporotic Thoracolumbar Vertebral Fractures in the Elderly: A Systematic Review With Quantitative Quality Assessment by Philipp Pieroh, Ulrich J.A. Spiegl, Anna Völker, Sven Märdian, Nicolas H. von der Höh, Georg Osterhoff, Christoph-E. Heyde; Spine Section of the German Society for Orthopaedics and Trauma in Global Spine Journal
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was organized and financially supported by Deutsche Gesellschaft für Orthopädie und Unfallchirurgie e.V. (DGOU).
Supplemental Material: Supplemental material for this article is available online.
ORCID iDs
Philipp Pieroh https://orcid.org/0000-0003-0906-5479
Nicolas H. von der Höh https://orcid.org/0000-0003-1928-5686
Georg Osterhoff https://orcid.org/0000-0001-5051-0998
References
- 1.Agabegi SS, Asghar FA, Herkowitz HN. Spinal orthoses. J Am Acad Orthop Surg. 2010;18(11):657-667. doi: 10.5435/00124635-201011000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Zarghooni K, Beyer F, Siewe J, Eysel P. The orthotic treatment of acute and chronic disease of the cervical and lumbar spine. Dtsch Arztebl Int. 2013;110(44):737-742. doi: 10.3238/arztebl.2013.0737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Spiegl UJ, Götz A, Grüninger S, et al. Stellenwert der orthetik für die wirbelsäule des erwachsenen – ergebnisse einer umfrage und diskussion der literatur. Die Wirbelsäule. 2020;4(3):174-181. doi: 10.1055/a-0968-9210. [DOI] [Google Scholar]
- 4.Spiegl UJ, Fischer K, Schmidt J, et al. The conservative treatment of traumatic thoracolumbar vertebral fractures. Dtsch Arztebl Int. 2018;115(42):697-704. doi: 10.3238/arztebl.2018.0697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ameis A, Randhawa K, Yu H, et al. The global Spine care initiative: A review of reviews and recommendations for the non-invasive management of acute osteoporotic vertebral compression fracture pain in low- and middle-income communities. Eur Spine J. 2018;27(suppl 6):861-869. doi: 10.1007/s00586-017-5273-6. [DOI] [PubMed] [Google Scholar]
- 6.Goodwin VA, Hall AJ, Rogers E, Bethel A. Orthotics and taping in the management of vertebral fractures in people with osteoporosis: A systematic review. BMJ Open. 2016;6(5):e010657. doi: 10.1136/bmjopen-2015-010657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jin YZ, Lee JH. Effect of brace to osteoporotic vertebral fracture: A meta-analysis. J Kor Med Sci. 2016;31(10):1641-1649. doi: 10.3346/jkms.2016.31.10.1641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kweh BTS, Lee HQ, Tan T, et al. The role of spinal Orthoses in osteoporotic vertebral fractures of the elderly population (age 60 years or older): Systematic review. Global Spine J. 2021;11(6):975-987. doi: 10.1177/2192568220948036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Newman M, Minns Lowe C, Barker K. Spinal orthoses for vertebral osteoporosis and osteoporotic vertebral fracture: A systematic review. Arch Phys Med Rehabil. 2016;97(6):1013-1025. doi: 10.1016/j.apmr.2015.10.108. [DOI] [PubMed] [Google Scholar]
- 10.Pfeifer M, Gehlen M, Hinz C. Rückenorthesen in der behandlung von wirbelkörperfrakturen bei osteoporose: Eine systematische ubersichtsarbeit. Z Rheumatol. 2017;76(10):860-868. doi: 10.1007/s00393-017-0404-3. [DOI] [PubMed] [Google Scholar]
- 11.Rzewuska M, Ferreira M, McLachlan AJ, Machado GC, Maher CG. The efficacy of conservative treatment of osteoporotic compression fractures on acute pain relief: A systematic review with meta-analysis. Eur Spine J. 2015;24(4):702-714. doi: 10.1007/s00586-015-3821-5. [DOI] [PubMed] [Google Scholar]
- 12.Hofler RC, Jones GA. Bracing for acute and subacute osteoporotic compression fractures: A systematic review of the literature. World Neurosurg. 2020;141:e453-e460. doi: 10.1016/j.wneu.2020.05.199. [DOI] [PubMed] [Google Scholar]
- 13.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Coleman BD, Khan KM, Maffulli N, Cook JL, Wark JD. Studies of surgical outcome after patellar tendinopathy: Clinical significance of methodological deficiencies and guidelines for future studies. Victorian institute of sport tendon study group. Scand J Med Sci Sports. 2000;10(1):2-11. doi: 10.1034/j.1600-0838.2000.010001002.x. [DOI] [PubMed] [Google Scholar]
- 15.Messner J, Papakostidis C, Giannoudis PV, Kanakaris NK. Duration of administration of antibiotic agents for open fractures: Meta-analysis of the existing evidence. Surg Infect. 2017;18(8):854-867. doi: 10.1089/sur.2017.108. [DOI] [PubMed] [Google Scholar]
- 16.Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. The newcastle-ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses.
- 17.Ochtman AEA, Kruyt MC, Jacobs WCH, et al. Surgical restoration of sagittal alignment of the Spine: Correlation with improved patient-reported outcomes: A systematic review and meta-analysis. JBJS Rev. 2020;8(8):e1900100. doi: 10.2106/JBJS.RVW.19.00100. [DOI] [PubMed] [Google Scholar]
- 18.Smith CS, Mollon B, Vannabouathong C, et al. An assessment of randomized controlled trial quality in the journal of bone & joint surgery: Update from 2001 to 2013. J Bone Joint Surg Am. 2020;102(20):e116. doi: 10.2106/JBJS.18.00653. [DOI] [PubMed] [Google Scholar]
- 19.Detsky AS, Naylor CD, O’Rourke K, McGeer AJ, L’Abbé KA. Incorporating variations in the quality of individual randomized trials into meta-analysis. J Clin Epidemiol. 1992;45(3):255-265. doi: 10.1016/0895-4356(92)90085-2. [DOI] [PubMed] [Google Scholar]
- 20.Oxman AD, Guyatt GH. Validation of an index of the quality of review articles. J Clin Epidemiol. 1991;44(11):1271-1278. doi: 10.1016/0895-4356(91)90160-b. [DOI] [PubMed] [Google Scholar]
- 21.Dijkman BG, Abouali JAK, Kooistra BW, et al. Twenty years of meta-analyses in orthopaedic surgery: Has quality kept up with quantity? J Bone Joint Surg Am. 2010;92(1):48-57. doi: 10.2106/JBJS.I.00251. [DOI] [PubMed] [Google Scholar]
- 22.Tian J, Zhang J, Ge L, Yang K, Song F. The methodological and reporting quality of systematic reviews from China and the USA are similar. J Clin Epidemiol. 2017;85:50-58. doi: 10.1016/j.jclinepi.2016.12.004. [DOI] [PubMed] [Google Scholar]
- 23.Zhang J, Han L, Shields L, Tian J, Wang J. A PRISMA assessment of the reporting quality of systematic reviews of nursing published in the cochrane library and paper-based journals. Medicine (Baltim). 2019;98(49):e18099. doi: 10.1097/MD.0000000000018099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Abe T, Shibao Y, Takeuchi Y, et al. Initial hospitalization with rigorous bed rest followed by bracing and rehabilitation as an option of conservative treatment for osteoporotic vertebral fractures in elderly patients: A pilot one arm safety and feasibility study. Arch Osteoporos. 2018;13(1):134. doi: 10.1007/s11657-018-0547-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hoshino M, Tsujio T, Terai H, et al. Impact of initial conservative treatment interventions on the outcomes of patients with osteoporotic vertebral fractures. Spine Phila Pa. 1976;38(11):E641-E648. doi: 10.1097/BRS.0b013e31828ced9d. [DOI] [PubMed] [Google Scholar]
- 26.Kato T, Inose H, Ichimura S, et al. Comparison of rigid and soft-brace treatments for acute osteoporotic vertebral compression fracture: A prospective, randomized, multicenter study. J Clin Med. 2019;8(2):198. doi: 10.3390/jcm8020198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Murata K, Watanabe G, Kawaguchi S, et al. Union rates and prognostic variables of osteoporotic vertebral fractures treated with a rigid external support. J Neurosurg Spine. 2012;17(5):469-475. doi: 10.3171/2012.7.SPINE122. [DOI] [PubMed] [Google Scholar]
- 28.Li M, Law S, Cheng J, Kee H, Wong MS. A comparison study on the efficacy of SpinoMed® and soft lumbar orthosis for osteoporotic vertebral fracture. Prosthet Orthot Int. 2015;39(4):270-276. doi: 10.1177/0309364614528204. [DOI] [PubMed] [Google Scholar]
- 29.Kim HJ, Yi JM, Cho HG, et al. Comparative study of the treatment outcomes of osteoporotic compression fractures without neurologic injury using a rigid brace, a soft brace, and no brace: A prospective randomized controlled non-inferiority trial. J Bone Joint Surg Am. 2014;96(23):1959-1966. doi: 10.2106/JBJS.N.00187. [DOI] [PubMed] [Google Scholar]
- 30.Liaw MY, Chen CL, Chen JF, Tang FT, Wong AMK, Ho HH. Effects of Knight-Taylor brace on balance performance in osteoporotic patients with vertebral compression fracture. J Back Musculoskelet Rehabil. 2009;22(2):75-81. doi: 10.3233/BMR-2009-0218. [DOI] [PubMed] [Google Scholar]
- 31.Pfeifer M, Begerow B, Minne HW. Effects of a new spinal orthosis on posture, trunk strength, and quality of life in women with postmenopausal osteoporosis: A randomized trial. Am J Phys Med Rehabil. 2004;83(3):177-186. doi: 10.1097/01.phm.0000113403.16617.93. [DOI] [PubMed] [Google Scholar]
- 32.Pfeifer M, Kohlwey L, Begerow B, Minne HW. Effects of two newly developed spinal orthoses on trunk muscle strength, posture, and quality-of-life in women with postmenopausal osteoporosis: A randomized trial. Am J Phys Med Rehabil. 2011;90(10):805-815. doi: 10.1097/PHM.0b013e31821f6df3. [DOI] [PubMed] [Google Scholar]
- 33.Jacobs E, Senden R, McCrum C, van Rhijn LW, Meijer K, Willems PC. Effect of a semirigid thoracolumbar orthosis on gait and sagittal alignment in patients with an osteoporotic vertebral compression fracture. Clin Interv Aging. 2019;14:671-680. doi: 10.2147/CIA.S199853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Valentin GH, Pedersen LN, Maribo T. Wearing an active spinal orthosis improves back extensor strength in women with osteoporotic vertebral fractures. Prosthet Orthot Int. 2014;38(3):232-238. doi: 10.1177/0309364613497393. [DOI] [PubMed] [Google Scholar]
- 35.Dionyssiotis Y, Trovas G, Thoma S, Lyritis G, Papaioannou N. Prospective study of spinal orthoses in women. Prosthet Orthot Int. 2015;39(6):487-495. doi: 10.1177/0309364614545416. [DOI] [PubMed] [Google Scholar]
- 36.Meccariello L, Muzii VF, Falzarano G, et al. Dynamic corset versus three-point brace in the treatment of osteoporotic compression fractures of the thoracic and lumbar spine: A prospective, comparative study. Aging Clin Exp Res. 2017;29(3):443-449. doi: 10.1007/s40520-016-0602-x. [DOI] [PubMed] [Google Scholar]
- 37.Talic A, Kapetanovic J, Dizdar A. Effects of conservative treatment for osteoporotic thoracolumbal spine fractures. Mater Sociomed. 2012;24(1):16-20. doi: 10.5455/msm.2012.24.16-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hübscher M, Schmidt K, Fink M, Vogt L, Banzer W. Prospektive evaluation funktions- und lebensqualitätsbezogener effekte einer wirbelsäulenorthese bei frauen mit osteoporose. Z Orthop Unfall. 2010;148(4):443-447. doi: 10.1055/s-0029-1240820. [DOI] [PubMed] [Google Scholar]
- 39.Raeissadat SA, Sedighipour L, Pournajaf S, Vahab Kashani R, Sadeghi S. Effect of posture training with weighted kypho-orthosis (WKO) on improving balance in women with osteoporosis. J Aging Res. 2014;2014:427903. doi: 10.1155/2014/427903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kaplan RS, Sinaki M, Hameister MD. Effect of back supports on back strength in patients with osteoporosis: A pilot study. Mayo Clin Proc. 1996;71(3):235-241. doi: 10.4065/71.3.235. [DOI] [PubMed] [Google Scholar]
- 41.Schmidt K, Hübscher M, Vogt L, et al. Einflüsse einer wirbelsäulenorthese auf gangparameter und alltagsfunktion bei postmenopausaler osteoporose. Orthopä. 2012;41(3):200-205. doi: 10.1007/s00132-011-1867-6. [DOI] [PubMed] [Google Scholar]
- 42.Sinaki M, Lynn SG. Reducing the risk of falls through proprioceptive dynamic posture training in osteoporotic women with kyphotic posturing: A randomized pilot study. Am J Phys Med Rehabil. 2002;81(4):241-246. doi: 10.1097/00002060-200204000-00001. [DOI] [PubMed] [Google Scholar]
- 43.Greig AM, Bennell KL, Briggs AM, Hodges PW. Postural taping decreases thoracic kyphosis but does not influence trunk muscle electromyographic activity or balance in women with osteoporosis. Man Ther. 2008;13(3):249-257. doi: 10.1016/j.math.2007.01.011. [DOI] [PubMed] [Google Scholar]
- 44.Vorsanger GJ, Farrell J, Xiang J, Chow W, Moskovitz BL, Rosenthal NR. Tapentadol, oxycodone or placebo for acute pain of vertebral compression fractures: A randomized Phase IIIb study. Pain Manag. 2013;3(2):109-118. doi: 10.2217/pmt.13.5. [DOI] [PubMed] [Google Scholar]
- 45.Bornemann R, Hanna M, Kabir K, Goost H, Wirtz DC, Pflugmacher R. Continuing conservative care versus crossover to radiofrequency kyphoplasty: A comparative effectiveness study on the treatment of vertebral body fractures. Eur Spine J. 2012;21(5):930-936. doi: 10.1007/s00586-012-2148-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lee HM, Park SY, Lee SH, Suh SW, Hong JY. Comparative analysis of clinical outcomes in patients with osteoporotic vertebral compression fractures (OVCFs): Conservative treatment versus balloon kyphoplasty. Spine J. 2012;12(11):998-1005. doi: 10.1016/j.spinee.2012.08.024. [DOI] [PubMed] [Google Scholar]
- 47.Colangelo D, Nasto LA, Genitiempo M, et al. Kyphoplasty vs conservative treatment: A case-control study in 110 post-menopausal women population. Is kyphoplasty better than conservative treatment? Eur Rev Med Pharmacol Sci. 2015;19(21):3998-4003. [PubMed] [Google Scholar]
- 48.Kishikawa Y. Initial non-weight-bearing therapy is important for preventing vertebral body collapse in elderly patients with clinical vertebral fractures. Int J Gen Med. 2012;5:373-380. doi: 10.2147/IJGM.S25972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Piazzolla A, Solarino G, Lamartina C, et al. Vertebral bone marrow edema (VBME) in conservatively treated acute vertebral compression fractures (VCFs): Evolution and clinical correlations. Spine Phila Pa. 2015;40(14):E842-E848. doi: 10.1097/BRS.0000000000000973. [DOI] [PubMed] [Google Scholar]
- 50.Shah S, Goregaonkar AB. Conservative management of osteoporotic vertebral fractures: A prospective study of thirty patients. Cureus. 2016;8(3):e542. doi: 10.7759/cureus.542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Spiegl U, Bork H, Grüninger S, et al. Osteoporotic fractures of the thoracic and lumbar vertebrae: Diagnosis and conservative treatment. Dtsch Arztebl Int. 2021;118(40):670-677. doi: 10.3238/arztebl.m2021.0295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Burstein AH. Fracture classification systems: Do they work and are they useful? J Bone Joint Surg Am. 1993;75(12):1743-1744. [PubMed] [Google Scholar]
- 53.Schnake KJ, Blattert TR, Hahn P, et al. Classification of osteoporotic thoracolumbar Spine fractures: Recommendations of the Spine section of the German society for orthopaedics and trauma (DGOU). Global Spine J. 2018;8(2 suppl l):46S-49S. doi: 10.1177/2192568217717972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Simunovic N, Sprague S, Bhandari M. Methodological issues in systematic reviews and meta-analyses of observational studies in orthopaedic research. J Bone Joint Surg Am. 2009;91(suppl 3):87-94. doi: 10.2106/JBJS.H.01576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kaijser Alin C, Uzunel E, Grahn Kronhed AC, Alinaghizadeh H, Salminen H. Effect of treatment on back pain and back extensor strength with a spinal orthosis in older women with osteoporosis: A randomized controlled trial. Arch Osteoporos. 2019;14(1):5. doi: 10.1007/s11657-018-0555-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hosseinabadi M, Kamyab M, Azadinia F, Sarrafzadeh J. Effect of a spinomed orthosis on balance performance, spinal alignment, joint position sense and back muscle endurance in elderly people with hyperkyphotic posture: A randomized controlled trial. Prosthet Orthot Int. 2020;44(4):234-244. doi: 10.1177/0309364620923816. [DOI] [PubMed] [Google Scholar]
- 57.Vogt L, Hübscher M, Brettmann K, Banzer W, Fink M. Postural correction by osteoporosis orthosis (Osteo-med): A randomized, placebo-controlled trial. Prosthet Orthot Int. 2008;32(1):103-110. doi: 10.1080/03093640701838265. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for Spinal Orthoses in the Treatment of Osteoporotic Thoracolumbar Vertebral Fractures in the Elderly: A Systematic Review With Quantitative Quality Assessment by Philipp Pieroh, Ulrich J.A. Spiegl, Anna Völker, Sven Märdian, Nicolas H. von der Höh, Georg Osterhoff, Christoph-E. Heyde; Spine Section of the German Society for Orthopaedics and Trauma in Global Spine Journal