Abstract
After intranasal inoculation, Brucella melitensis chronically infects the mononuclear phagocyte system in BALB/c mice, but it causes no apparent illness. Adaptive immunity, which can be transferred by either T cells or antibody from immune to naive animals, confers resistance to challenge infection. The role of innate, non-B-, non-T-cell-mediated immunity in control of murine brucellosis, however, is unknown. In the present study, we documented that BALB/c and C57BL/6 mice had a similar course of infection after intranasal administration of 16M, validating the usefulness of the model in the latter mouse strain. We then compared the course of infection in Rag1 knockout mice (C57BL/6 background) (referred to here as RAG-1 mice) which have no B or T cells as a consequence of deletion of Rag1 (recombination-activating gene 1), with infection in normal C57BL/6 animals after intranasal administration of B. melitensis 16M. C57BL/6 mice cleared brucellae from their lungs by 8 to 12 weeks and controlled infection in the liver and spleen at a low level. In contrast, RAG-1 mice failed to reduce the number of bacteria in any of these organs. From 1 to 4 weeks after inoculation, the number of splenic bacteria increased from 2 to 4.5 logs and remained at that level. In contrast to the consistently high numbers of brucellae observed in the spleens, the number of bacteria rose in the livers sampled for up to 20 weeks. Immunohistologic examination at 8 weeks after infection disclosed foci of persistent pneumonia and large amounts of Brucella antigen in macrophages in lung, liver, and spleen in RAG-1, but not C57BL/6, mice. These studies indicate that T- and B-cell-independent immunity can control Brucella infection at a high level in the murine spleen, but not in the liver. Immunity mediated by T and/or B cells is required for clearance of bacteria from spleen and lung and for control of bacterial replication in the liver.
Brucellosis, a zoonosis that affects several species of domestic animals, manifests itself in humans as a systemic, febrile illness. Most human disease is caused by Brucella melitensis, but B. abortus and B. suis are also highly pathogenic. The disease is recognized in more than 100 countries, with an estimated one million new cases per year. Most cases occur as a result of occupational exposure to animals or ingestion of nonpasteurized dairy products (6). Laboratory workers exposed to the agent are also at high risk of infection. Brucellosis can be acquired through ingestion and through breaks in the skin; aerosol transmission also occurs (6). There are no suitably attenuated, well-characterized human vaccines available.
To simulate infection by a mucosal or aerosol route of infection, we have recently established a murine model of brucellosis in which BALB/c mice are inoculated intranasally with B. melitensis 16M (14, 17). In this model, the organism infects the lung and disseminates to the blood, liver, and spleen. Both antibody and cellular immune effectors mediate control of dissemination and replication of brucellae in laboratory animal models of infection (1, 2, 10, 20, 25, 32, 37). Animals deficient in T cells (7) or CD8 cells (23) have increased intensity of Brucella infection but do not die. Elimination of natural killer (NK) cells (13), however, does not enhance infection. Paradoxically, scid mice show increased resistance to infection with B. abortus 2308 (22). The importance of a Th1-type response modulated by T-cell-derived cytokines, including gamma interferon (IFN-γ [37]) and a counterregulator of IFN-γ, interleukin-10 (IL-10 [12]), has recently been demonstrated. The pivotal role of IFN-γ in mediating an effective response is demonstrated by the fatal course of infection in IFN-γ knockout mice challenged with B. abortus 2308 (C. Baldwin, personal communication).
Rag1 knockout mice (referred to here as RAG-1 mice) lack recombination-activating gene 1 (Rag1) (19), which controls V(D)J recombination of immunoglobulin and T-cell receptor genes. As a consequence of this defect, they have no mature T or B cells (18, 19). RAG-1 NK cells can be activated for cytotoxicity in vitro by activation stimuli, including IL-12 and heat-killed Listeria monocytogenes plus IL-2 (9). In the studies described here, we administered B. melitensis 16M intranasally to C57BL/6 and RAG-1 mice and monitored the course of infection for up to 20 weeks. The results demonstrate the importance of T and B cells in the control of brucellosis but suggest that additional, non-T- and/or non-B-cell processes, i.e., natural immune processes, must also have a regulatory role in limiting the intensity of infection, especially in the spleen.
MATERIALS AND METHODS
Animals.
Six- to eight-week-old RAG-1 (C57BL/6J-Rag1tm1mom), C57BL/6, and BALB/c mice were purchased from The Jackson Laboratory (Bar Harbor, Maine) and used for studies 1 week later. Since our previous studies of murine brucellosis had used BALB/c mice but RAG-1 mice were only available on a C57BL/6 background, we performed a preliminary experiment to exclude a large contribution of strain background to the final interpretations of our data. At the time the comparative experiments between RAG-1 and C57BL/6 mice were performed, only male RAG-1 mice were available. Thus, the studies comparing BALB/c with C57BL/6 mice used females; in subsequent work, male RAG-1 and C57BL/6 animals were compared. Animals were housed in biosafety level 3 facilities and provided sterile food and water.
Growth of bacteria and infection of mice.
B. melitensis 16M was obtained from Gerhardt Schurig (Virginia Polytechnic Institute, Blacksburg), passaged once through mice and grown overnight in shaker flasks in brucella broth at 37°C. This primary stock was frozen at −70°C in aliquots in 50% glycerol in brucella broth. A secondary stock was made by growing a vial of primary stock overnight in shaker flasks in brucella broth, which was then frozen at −70°C in aliquots in 50% glycerol in brucella broth. Before injection into animals, secondary stock was grown overnight as described above. Cells were then pelleted, washed twice with saline, and diluted to a bacterial concentration of 3.3 × 105 bacteria/ml of saline based on the optical density (OD). Thirty microliters of this suspension, containing 104 bacteria, was administered dropwise into the external nares with a micropipette to mice that were anesthetized with xylazine and ketamine (14). For the study comparing female BALB/c with female C57BL/6 mice and one study comparing male RAG-1 mice with male C57BL/6 mice, 18 mice per group were used. In a second study comparing male RAG-1 mice with male C57BL/6 mice, 21 mice of each strain received 16M and 3 mice of each strain received saline intranasally; 3 mice from each group were euthanized 8 weeks later for histopathological examination.
Quantitation of brucellae in the lung, liver, and spleen.
At different time points, three mice from each group of animals inoculated with 16M intranasally were euthanized by CO2 narcosis, weighed, and bled by cardiac puncture for collection of serum, which was stored at −80°C. The spleen, lungs, and livers were removed and weighed. Organs were suspended individually in 1 ml of 0.9% NaCl and homogenized in tissue grinders. Then, 0.5 ml of neat homogenates and 10 μl of serial 10-fold saline dilutions of spleen homogenates were cultured on brucella agar. For culture of liver and lung homogenates, agar was supplemented with 25 U of bacitracin and 5 U of polymyxin B (16, 29) per ml to prevent overgrowth by more rapidly growing contaminants in these organs. After incubation for 4 days at 37°C, colonies were visualized and the CFU per organ were determined. In preliminary experiments, to ensure that inclusion of antibiotics did not reduce recovery of brucellae, we compared antibiotic-containing and antibiotic-free plates for culture of spleens of mice infected with brucellae. Spleens from these mice are not colonized with organisms other than brucellae. Recovery was identical using either antibiotic-containing or antibiotic-free plates (data not shown), indicating that these plates were suitable for culture of contaminated sites such as liver and lung.
Histology and immunohistochemistry.
Spleens, lungs, and livers were harvested from three male RAG-1 and C57BL/6 mice that had been inoculated intranasally 8 weeks previously with saline or 104 16M organisms. Organs collected at the time of necropsy were removed entirely and fixed in 10% formalin in phosphate-buffered saline (PBS), pH 7.4, for 3 days. For light microscopic examination, tissue sections that were approximately 2 mm thick were embedded in paraffin, and 4- to 5-μm-thick serial sections were processed in an automatic tissue processor (Tissue-tek VIP; Miles Scientific, Mishawake, Ind.). Sections were stained with hematoxylin and eosin (H&E) according to standard protocols. For immunohistochemical studies, 4- to 5-μm-thick paraffin-embedded tissue sections were mounted on Esco Superfrost Plus slides (Erie Scientific, Portsmouth, N.H.), deparaffinized, and rehydrated. Slides were processed using Biogenex reagents (Biogenex, San Ramon, Calif.), and an Optimax Plus Automated Cell Stainer (Biogenex, San Ramon, Calif.). Tissue sections were rinsed between reagent incubations using a phosphate-buffered saline wash at room temperature. Endogenous peroxidase activity was blocked by incubation with peroxide block for 30 min at room temperature. Antiserum used as a source for primary antibody was prepared from a rabbit immunized with B. melitensis lipopolysaccharide (LPS). LPS was prepared by phenol/water extraction and treatment with DNase, RNase, and proteinase K as previously described (31). Immunoglobulin G (IgG) was prepared from immune or control (preimmune) rabbit serum by affinity chromatography on protein G-Sepharose. The B. melitensis LPS-specific IgG was further purified by passing immune rabbit IgG through an affinity column made of purified B. melitensis LPS linked to Sepharose 4B (Pharmacia-LKB Biotechnology, Piscataway, N.J.) by a method described previously (3). Enzyme-linked immunosorbent assay of these reagents, performed as previously described (14), gave titers of 3,360 OD U/ml for B. melitensis LPS-specific IgG and 2 OD U/ml for preimmune rabbit IgG. Tissue sections were incubated with the primary antibody overnight at 4°C at a 1:5,000 dilution using common antibody diluent. The secondary antibody (biotinylated goat anti-rabbit link) was applied for 20 min. The slides were then incubated with peroxidase-conjugated streptavidin label for 20 min, followed by incubation with AEC substrate for 5 min and a 1-min hematoxylin counterstain. An aqueous mounting media was used for the final preparation.
Morphometry.
Prior to paraffin embedding, sections of spleen were transected longitudinally along the median plane, providing at least one longitudinal section from each animal for morphometric analysis of splenic compartment areas. H&E-stained sections of spleen from three mice within each group were examined using a Zeiss Axiophot microscope (Carl Zeiss) and a Sony 3CCD color video camera (DXC 960 MD; Sony Corp.) and analyzed using Zeiss Image version 3.0 image analysis software. The area (the number of pixels on a captured image) of white pulp, including both the white pulp and the marginal zone, and red pulp on each slide was determined for each mouse within each group. The marginal zone was defined as the zone of macrophages and some lymphocytes that surround the periarteriolar lymphoid sheath.
Statistical analysis.
Culture data from each time point were expressed as mean log CFU ± the standard deviation (SD) for each group. Data from spleen morphometry were expressed as mean ratios of white pulp areas/red pulp areas ± the SD for each group. The significance of differences between groups was analyzed by Student's t test. A P value of ≤0.05 was regarded as significant.
RESULTS
Course of infection in BALB/c versus C57BL/6 mice.
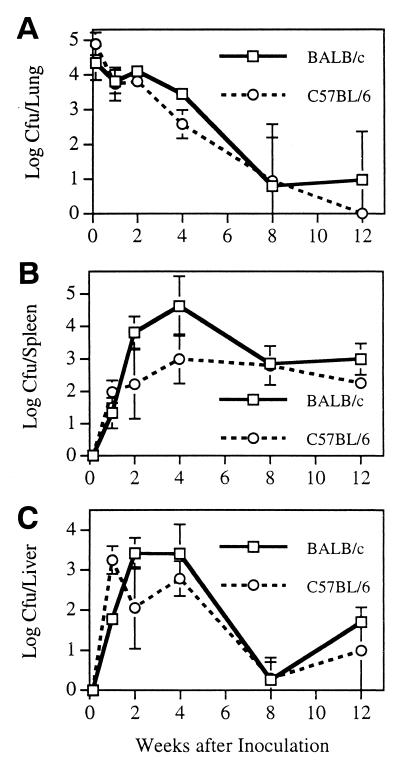
To determine whether the course of B. melitensis infection was similar in BALB/c and C57BL/6 mice, we administered 16M intranasally to female mice of both strains as a preliminary experiment. C57BL/6 and BALB/c animals had similar patterns of susceptibility to infection and dissemination, although there was a trend toward more rapid clearance of infection in C57BL/6 animals (Fig. 1). Both mouse strains nearly eliminated bacteria from the lungs by 8 weeks (Fig. 1A); at that time, only one of three animals of each strain had lung cultures positive for 16M. At 12 weeks, the lungs remained infected in only one of the three BALB/c animals, and in none of the three C57BL/6 animals were the lungs still infected. Although trends for increased spleen infection in BALB/c mice compared to C57BL/6 mice were noted at 2 and 4 weeks (Fig. 1B), these differences did not reach statistical significance (P = 0.08 for both time periods). The spleens of all animals remained infected through 12 weeks. Liver infection (Fig. 1C) in the two mouse strains was also similar except at 1 week postchallenge, when C57BL/6 animals had approximately 40-fold more CFU/liver than the BALB/c animals (P < 0.003).
FIG. 1.
Bacteriologic course of infection in BALB/c versus C57BL/6 mice. Mice were inoculated intranasally with 104 16M organisms. Animals were euthanized, and the lungs (A), spleen (B), and liver (C) were harvested and homogenized at various times after infection. The numbers of CFU per organ were determined by serial dilution and plating of homogenates on brucella agar. Limit of detection, 2 CFU/organ.
Course of infection in RAG-1 versus C57BL/6 mice.
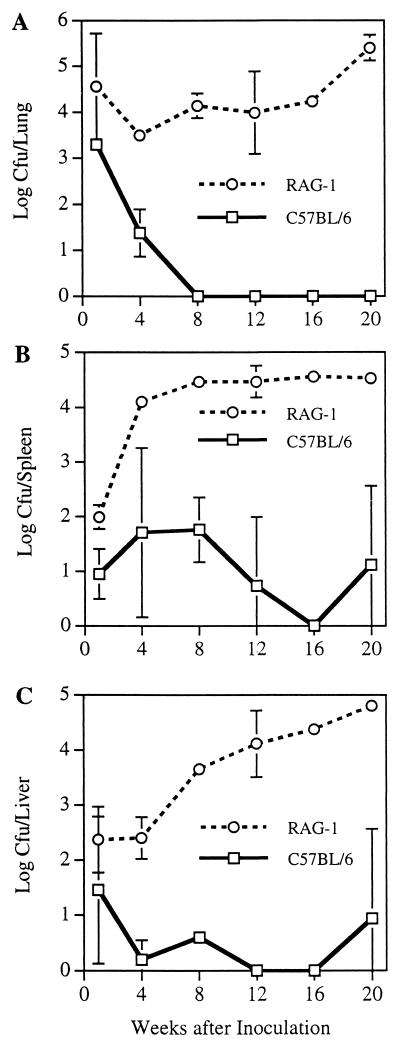
In two additional experiments in which male C57BL/6 and male RAG-1 mice were compared, the course of infection in C57BL/6 mice was similar to that depicted in Fig. 1. In contrast to their normal parent strain, however, RAG-1 mice were profoundly deficient in their ability to control infection with virulent B. melitensis. While C57BL/6 animals eliminated 16M from their lungs within 8 weeks of intranasal challenge, RAG-1 mice did not reduce the number of bacteria in their lungs (Fig. 2A) over the entire study period of 20 weeks. Indeed, at 20 weeks, the number of 16M organisms in the lungs of RAG-1 mice was higher than the number observed at 4 to 12 weeks. This difference in the control of brucellae was not due to different intensities of infection immediately postchallenge since in the first of these two experiments the number of CFU/lung at 1 day postchallenge was identical in both strains of mice (data not shown). This failure to control local infection extended to the control of systemic infection. C57BL/6 mice permitted growth of 16M to approximately 1.8-log CFU in the spleen, while RAG-1 mice permitted bacteria to reach approximately 4.5-log CFU by 8 weeks postchallenge (Fig. 2B). This level of spleen infection was maintained in spleens harvested for up to 20 weeks. In the liver, the number of 16M organisms was reduced by C57BL/6 mice to less than 1-log CFU after the first week (Fig. 2C). In contrast, the number of 16M organisms was higher at each successive harvest point in RAG-1 mouse livers, finally reaching nearly 5-log CFU/liver when the experiment was terminated at 20 weeks. The results for the first 12 weeks shown in Fig. 2 were essentially identical to those of the other experiment, in which animals were monitored for only 12 weeks (data not shown).
FIG. 2.
Bacteriologic course of infection in C57BL/6 versus RAG-1 mice. Mice were inoculated intranasally with 104 16M organisms. Animals were euthanized, and the lungs (A), spleen (B), and liver (C) were harvested and homogenized at various times after infection. The numbers of CFU per organ were determined by serial dilution and plating of homogenates on brucella agar. Limit of detection, 2 CFU/organ.
The failure of RAG-1 mice to control infection was associated with impaired weight gain. RAG-1 and C57BL/6 mice had similar weights through 4 weeks postchallenge. By 8 weeks postchallenge, when the numbers of brucellae in their livers and spleens were high, RAG-1 animals were no longer gaining weight. In contrast, infected C57BL/6 mice gained approximately 30% in body weight over the 20-week period (data not shown).
Pathology of infected RAG-1 and C57BL/6 mice.
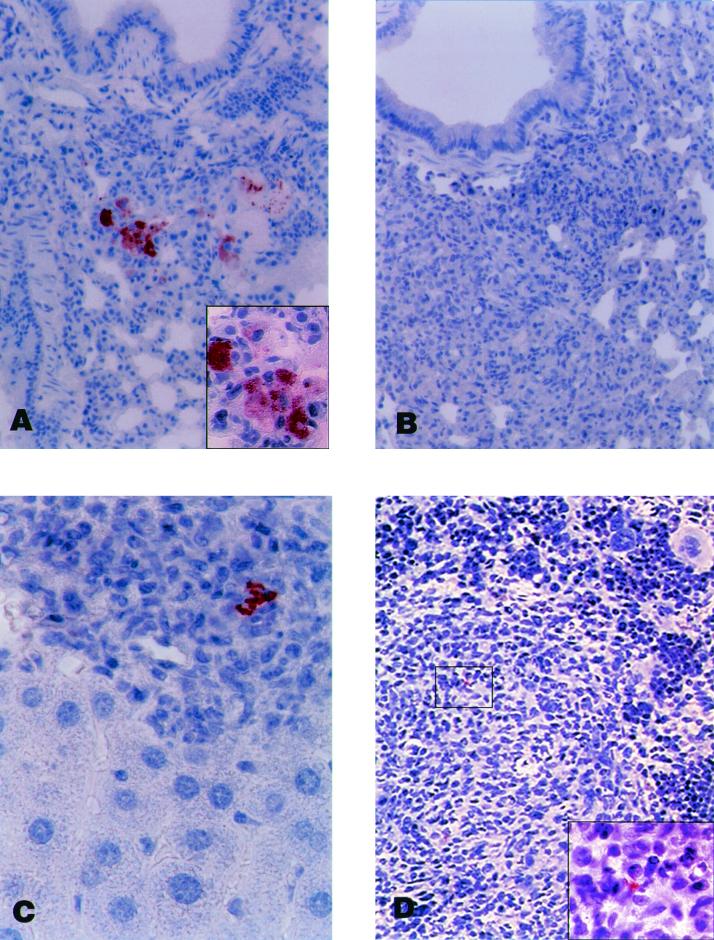
Lungs from RAG-1 mice inoculated with 16M had multifocal areas of red discoloration interspersed with patches of red to gray discoloration. Grossly, these areas were interpreted as hyperemia and consolidation, respectively. Microscopically, they corresponded to foci of peribronchial pneumonia with intra-alveolar accumulation of proteinaceous fluid and inflammatory cells. The inflammatory cells were predominantly polymorphonuclear leukocytes and macrophages. The proportion of polymorphonuclear leukocytes varied between the affected areas of lung tissue. This finding suggests that some of the changes observed were due to a secondary acute bacteremia in addition to persistent inflammation established by the initial intranasal challenge. These foci of inflammation were frequently characterized by a central area containing polymorphonuclear leukocytes surrounded by alveoli filled with a mixture of eosinophilic proteinaceous fluid, necrotic cellular debris, and foamy macrophages. Some foci had a granulomatous appearance, with a few alveoli filled with mostly distended macrophages, that after immunohistochemical staining with anti-B. melitensis LPS demonstrated abundant accumulation of Brucella antigen (Fig. 3A). The staining pattern within individual macrophages ranged from particulate, suggestive of individual bacteria, to diffuse or globular, reflecting staining of large amounts of bacterial antigen (Fig. 3A, inset). No bacteria were seen when sections of the same or similar pneumonic foci were stained using preimmune rabbit serum IgG (Fig. 3B). Lungs of RAG-1 mice inoculated with saline appeared normal. Lungs of C57BL/6 mice inoculated with 16M occasionally contained low numbers of peribronchial or perivascular lymphoid cells. Similar accumulations, however, were also detected in sections of lungs examined light microscopically from C57BL/6 mice inoculated with saline, suggesting that these lesions represented an inflammatory response to a nonspecific environmental agent rather than a response to Brucella infection.
FIG. 3.
Tissue response of RAG-1 mice to infection with 16M. Mice were inoculated intranasally with 104 16M organisms. Organs were harvested at 8 weeks and stained using an immunoperoxidase technique, which stains Brucella LPS red. Slides were counterstained with hematoxylin. (A) Peribronchial pneumonic focus; original magnification, ×200 (inset detail of central field; original magnification, ×600). Numerous discrete and coalescent accumulations of Brucella antigen are present in macrophage cytoplasm. (B) Similar focus stained with control antibody; original magnification, ×200. (C) Periportal inflammation in liver with presence of Brucella antigen in macrophages; original magnification, ×600. (D) Response to Brucella infection in spleen. A hypoplastic, periarteriolar lymphoid sheath and the border of atrophic follicle with red pulp can be seen. A large amount of antigen is present in the macrophages. Original magnification, ×200; inset original magnification, ×600.
Livers removed from RAG-1 mice appeared smaller than livers from C57BL/6 animals, but both they and the livers from C57BL/6 mice inoculated with 16M or saline were a normal color and texture. Light microscopically, the livers from all animals given saline were within normal limits, except that a single spontaneous lymphoid-macrophage granuloma was noted in one C57BL/6 mouse. In contrast, the livers from RAG-1 mice infected with 16M contained numerous, multifocal, intralobular and/or periportal accumulations of predominantly polymorphonuclear leukocytes and macrophages. Immunohistochemical analysis revealed Brucella antigen accumulation in patterns similar to those observed in the lungs but which was less abundant in the liver (Fig. 3C). Brucella-infected C57BL/6 mouse livers also had multifocal intralobular and/or periportal accumulations of cells, but these consisted primarily of lymphoid cells and macrophages, with few polymorphonuclear leukocytes. A thorough review of immunohistochemically stained sections demonstrated occasional punctate accumulations of Brucella antigen, a finding consistent with the presence of individual brucellae or residual antigen in macrophages. Many macrophages within affected areas had distinctive light microscopic characteristics consistent with epithelioid cells.
Macroscopically, the spleens from RAG-1 mice inoculated with saline were much smaller than those from C57BL/6 mice. By light microscopy, they were characterized by decreased amounts of white pulp, consisting of atrophic T-cell-specific periarteriolar lymphoid sheath areas and B-cell-specific lymphoid follicles. There was also a decrease in the amount of splenic red pulp. The ratio of white to red pulp in noninfected RAG-1 mice was 0.12 ± 0.07, compared to 0.45 ± 0.06 in noninfected C57BL/6 animals (P < 0.001). The remaining red pulp in RAG-1 mice consisted of reticular stromal and dendritic cells, small numbers of macrophages, lymphoid cells, and myeloid cells. Immunohistochemical analysis of infected mice showed both punctate and coalescent accumulations of Brucella antigen in macrophages in the affected areas, particularly at the marginal zones as well as in the red pulp proper (Fig. 3D). While there was a trend toward a decreased ratio of white pulp to red pulp in the spleens of infected (0.07 ± 0.04) compared to noninfected (0.12 ± 0.07) RAG-1 animals, this difference was not statistically significant (P = 0.314).
In distinct contrast to these findings, spleens of infected C57BL/6 mice had pronounced expansion of both white and red pulp compared to noninfected animals, with relatively decreased expansion of white pulp. The ratio of white pulp to red pulp was 0.45 ± 0.06 in infected versus 0.65 ± 0.05 in noninfected C57BL/6 animals (P = 0.013). Cells morphologically consistent with macrophages were particularly prominent at the marginal zones between the lymphoid follicles or periarteriolar lymphoid sheaths and the red pulp. However, as noted for the liver, only a few, discrete, punctate accumulations of Brucella antigen consistent with individual Brucella organisms were occasionally found in macrophages. Despite these extensive histologic changes and systemic and bacteriologic evidence of increased infection, RAG-1 mice appeared healthy throughout the course of infection.
DISCUSSION
Our bacteriologic and histopathologic results for 16M infection in C57BL/6 mice are similar to those of studies with other immunocompetent mouse strains infected with virulent strains of B. abortus (7, 11, 24, 26, 28, 30). They are also consistent with the course of infection previously demonstrated in BALB/c mice after intraperitoneal (8) or intravenous (27) injection of 16M, although the intensity of infection in liver and spleen was lower in the present study, presumably reflecting both the lower dose and the different route of inoculation. These results differ substantially from those of Young et al. (36), who infected C3H mice intraperitoneally with 5 × 108 CFU of B. melitensis EP, which was isolated from a patient with brucellosis, and examined murine tissue response and clearance of bacteria. In those studies, EP was cleared from spleens and livers within 30 days in association with the development of poorly formed hepatic and splenic granulomas composed of polymorphonuclear leukocytes, lymphocytes, and macrophages. In our studies, animals remained infected for up to 20 weeks and robust granulomas persisted in the spleen and liver for at least 8 weeks after intranasal challenge of C57BL/6 animals with 16M. The inflammatory infiltrate was composed of macrophages, with some having characteristics of epithelioid cells, and lymphocytes, along with variable, but low, numbers of polymorphonuclear leukocytes. It is likely that the differences between the findings of Young et al. and our own are attributable to differences in the challenge strains (strain EP versus 16M). The clearance of EP from liver and spleen in the earlier study was similar to the clearance of B. melitensis Rev1, suggesting that EP may be less virulent than 16M. This suggestion is reinforced by the observation that EP expresses small amounts of O polysaccharide on its surface (5), thus rendering it potentially less virulent than 16M, which expresses large amounts of surface O polysaccharide. The absence of pneumonia in these normal mice, despite the intranasal route of challenge and the documentation of bacteria in the lungs, is notable and is consistent with observations made with BALB/c mice (17).
In contrast to this benign course of infection in normal mice, B. melitensis caused severe pneumonia in RAG-1 mice and was present in large numbers in alveolar, liver, and spleen macrophages at 8 weeks. These studies provide a unique perspective by documenting the course of brucellosis in animals with no known specific immune effector cells. Any antibrucella activity they mount must depend on natural immunity, i.e., mucosal barriers, complement, other soluble antibacterial factors, phagocytes, and NK cells. In immunologically intact animals infected with virulent brucellae, a phase of bacterial replication is followed by a plateau phase, in which bacteria persist in spleen at a relatively constant level for several weeks. Organisms are then gradually cleared. The intensity of liver infection in normal animals is consistently lower than that of spleen when sampled at more than a week postchallenge (8, 37). Our data on liver infection in normal animals (Fig. 1 and 2) are consistent with these published reports. In contrast, however, we observed a plateau phase in the spleens of RAG-1 mice several weeks after challenge: brucellae persisted but did not sharply increase after the first 4 weeks of infection. The number of CFU/spleen during the plateau phase, however, was substantially higher in immunocompromised animals than in normal animals, and no clearance phase occurred during the course of these studies. It is unlikely that clearance would have eventually taken place, since infected, immunocompromised animals were losing weight and developing increased intensity of liver infection at the time of necropsy 20 weeks after challenge. In contrast to the apparent control of infection in the spleen, the numbers of liver CFU gradually increased throughout the course of infection in RAG-1 animals. The numbers of lung CFU remained relatively constant until 20 weeks, when they increased. It is possible that the increase in the lung reflects systemic dissemination of bacteria multiplying in the liver.
These findings suggest that control of bacteria in the spleen, as manifested by the high but constant number of bacteria at 12 to 20 weeks after infection, does not depend on B and/or T cells. Which of the remaining host defenses are responsible for this effect is unknown. NK cells are attractive candidates as nonspecific guardians against brucellosis: whole brucellae or their extracts induce NK-cell-mediated cytotoxicity (13, 34). Moreover, NK cells are a potent source of IFN-γ, which plays an important role in antibrucella defense (37), perhaps by activating macrophages to kill intracellular brucellae (15). In animals with functional B and T cells, however, elimination of NK cells does not affect the intensity of infection with 2308 (13). On the other hand, it is possible that in RAG-1 mice, which lack T and B cells, NK cells contribute to the control of infection. We are planning to test this hypothesis in subsequent experiments.
The pathologic findings in RAG-1 mice 8 weeks after challenge, with a prominence of polymorphonuclear leukocytes, minimal infiltration with lymphocytes, and large numbers of macrophages in lung, liver, and spleen lesions of infected animals are consistent with the persistence of a natural immune response. In the absence of specific, T- or B-cell-mediated immunity, chemotactic bacterial and host factors attract phagocytes that are unable to kill the organisms effectively. The inability of polymorphonuclear leukocytes to kill B. melitensis has been well documented (35). Moreover, IFN-γ and other cytokines provided by NK cells in the absence of a contribution from specifically sensitized T cells may not be sufficient to activate macrophages for effective killing. The failure of robust hepatic granuloma development in RAG-1 mice and the prominence of polymorphonuclear leukocytes in tissue reactions are similar to changes described by Cheville et al. (7) in nude mice infected with B. abortus 2308. Nude mice, which have severely reduced or absent T cells, maintain persistent liver infection with Brucella spp., albeit at much lower levels than we have found in this study in RAG-1 animals infected with 16M. It is possible that the difference in intensity of liver infection between our studies is attributable to differences in the bacterial species used, but the complete absence of antibody in RAG-1 mice may also play a role. Nude mice make both IgG and IgM in response to brucella LPS (21). Antibody of both classes is important for defense against the smooth B. abortus strain 2308 (10) and may play a role in protection against 16M (33), which is also smooth. Both the present study and that of Cheville et al. (7) suggest that the liver may be an important site of control of Brucella spp. by T- and B-cell-mediated defenses. Our data are in marked contrast to those of Morfitt et al. (22), who studied the course of infection over 72 days in scid and control mice inoculated intraperitoneally with 2308. scid mice controlled infection better than controls. Notably, liver granulomas regressed faster in the immunodeficient animals, and bacterial infection failed to establish in spleens of scid mice to the same degree as the controls. In contrast, RAG-1 mice had much higher numbers of bacteria in both the spleen and the liver compared to C57BL/6 animals (Fig. 2). Differences between these two studies may be explained by choice of bacterial species and strains (2308 versus 16M) route of inoculation (intraperitoneal versus intranasal) or genetic background of strains used (presumably C.B-17 versus C57BL/6) but may also reflect a defensive contribution by B and T cells in mice with the “leaky” scid mutation (4). RAG-1 mice should provide an excellent model to determine the site of action of humoral immune components that mediate recovery from infection or limit systemic spread of infection after mucosal challenge. They should also permit analysis of mechanisms by which T cells contribute to elimination of brucellae from their intracellular niche.
ACKNOWLEDGMENTS
We are grateful to Joseph Thompson, Adrien Ravizee, Brett Wood, and James Hart for technical assistance.
REFERENCES
- 1.Araya L N, Elzer P H, Rowe G E, Enright F M, Winter A J. Temporal development of protective cell-mediated and humoral immunity in BALB/c mice infected with Brucella abortus. J Immunol. 1989;143:3330–3337. [PubMed] [Google Scholar]
- 2.Bascoul S, Cannat A, Huguet M F, Serre A. Studies on the immune protection to murine experimental brucellosis conferred by Brucella fractions. I. Positive role of immune serum. Immunology. 1978;35:213–221. [PMC free article] [PubMed] [Google Scholar]
- 3.Bhattacharjee A K, Opal S M, Palardy J E, Drabick J J, Collins H, Taylor R, Cotton A, Cross A S. Affinity-purified Escherichia coli J5 lipopolysaccharide-specific IgG protects neutropenic rats against gram-negative bacterial sepsis. J Infect Dis. 1994;170:622–629. doi: 10.1093/infdis/170.3.622. [DOI] [PubMed] [Google Scholar]
- 4.Bosma M J, Carroll A M. The SCID mouse mutant: definition, characterization, and potential uses. Annu Rev Immunol. 1991;9:323–350. doi: 10.1146/annurev.iy.09.040191.001543. [DOI] [PubMed] [Google Scholar]
- 5.Bowden R A, Verger J M, Grayon M, Limet J N, Dubray G. Simultaneous expression of smooth and rough phase properties related to lipopolysaccharide in a strain of Brucella melitensis. J Med Microbiol. 1993;39:363–370. doi: 10.1099/00222615-39-5-363. [DOI] [PubMed] [Google Scholar]
- 6.Buchanan T M, Hendricks S L, Patton C M, Feldman R A. Brucellosis in the United States, 1960–1972: an abattoir-associated disease. Part III. Epidemiology and evidence for acquired immunity. Medicine (Baltimore) 1974;53:427–439. [PubMed] [Google Scholar]
- 7.Cheville N F, Kunkle R A, Jensen A E, Palmer M V. Persistence of Brucella abortus in the livers of T-cell-deficient nude mice. Lab Investig. 1995;73:96–102. [PubMed] [Google Scholar]
- 8.Crawford R M, Van De Verg L, Yuan L, Hadfield T L, Warren R L, Drazek E S, Houng H H, Hammack C, Sasala K, Polsinelli T, Thompson J, Hoover D L. Deletion of purE attenuates Brucella melitensis infection in mice. Infect Immun. 1996;64:2188–2192. doi: 10.1128/iai.64.6.2188-2192.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Daugelat S, Ladel C H, Flesch I E, Kaufmann S H. Activation of natural killer cells by heat-killed Listeria monocytogenes requires additional signals from lymphoid cells. Immunol Lett. 1996;50:81–85. doi: 10.1016/0165-2478(96)02523-0. [DOI] [PubMed] [Google Scholar]
- 10.Elzer P H, Jacobson R H, Jones S M, Nielsen K H, Douglas J T, Winter A J. Antibody-mediated protection against Brucella abortus in BALB/c mice at successive periods after infection: variation between virulent strain 2308 and attenuated vaccine strain 19. Immunology. 1994;82:651–658. [PMC free article] [PubMed] [Google Scholar]
- 11.Enright F M, Araya L N, Elzer P H, Rowe G E, Winter A J. Comparative histopathology in BALB/c mice infected with virulent and attenuated strains of Brucella abortus. Vet Immunol Immunopathol. 1990;26:171–182. doi: 10.1016/0165-2427(90)90065-z. [DOI] [PubMed] [Google Scholar]
- 12.Fernandes D M, Baldwin C L. Interleukin-10 downregulates protective immunity to Brucella abortus. Infect Immun. 1995;63:1130–1133. doi: 10.1128/iai.63.3.1130-1133.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fernandes D M, Benson R, Baldwin C L. Lack of a role for natural killer cells in early control of Brucella abortus 2308 infections in mice. Infect Immun. 1995;63:4029–4033. doi: 10.1128/iai.63.10.4029-4033.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hoover D L, Crawford R M, Van De Verg L L, Izadjoo M J, Bhattacharjee A K, Paranavitana C M, Warren R L, Nikolich M J, Hadfield T L. Protection of mice against brucellosis by vaccination with Brucella melitensis WR201 (ΔpurEK) Infect Immun. 1999;67:5877–5884. doi: 10.1128/iai.67.11.5877-5884.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jones S M, Winter A J. Survival of virulent and attenuated strains of Brucella abortus in normal and gamma interferon-activated murine peritoneal macrophages. Infect Immun. 1992;60:3011–3014. doi: 10.1128/iai.60.7.3011-3014.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marin C M, Jimenez de Bagues M, Barberan M, Blasco J M. Comparison of two selective media for the isolation of Brucella melitensis from naturally infected sheep and goats. Vet Rec. 1996;138:409–411. doi: 10.1136/vr.138.17.409. [DOI] [PubMed] [Google Scholar]
- 17.Mense, M. G., L. L. Van De Verg, A. K. Bhattacharjee, J. L. Garrett, J. A. Hart, L. E. Lindler, T. L. Hadfield, and D. L. Hoover. Bacteriological and histopathological features of a murine model for intranasal Brucella melitensis infection. Am. J. Vet. Res., in press. [DOI] [PubMed]
- 18.Mombaerts P. Lymphocyte development and function in T-cell receptor and RAG-1 mutant mice. Int Rev Immunol. 1995;13:43–63. doi: 10.3109/08830189509061737. [DOI] [PubMed] [Google Scholar]
- 19.Mombaerts P, Iacomini J, Johnson R S, Herrup K, Tonegawa S, Papaioannou V E. RAG-1-deficient mice have no mature B and T lymphocytes. Cell. 1992;68:869–877. doi: 10.1016/0092-8674(92)90030-g. [DOI] [PubMed] [Google Scholar]
- 20.Montaraz J A, Winter A J. Comparison of living and nonliving vaccines for Brucella abortus in BALB/c mice. Infect Immun. 1986;53:245–251. doi: 10.1128/iai.53.2.245-251.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moreno E, Kurtz R S, Berman D T. Induction of immune and adjuvant immunoglobulin G responses in mice by Brucella lipopolysaccharide. Infect Immun. 1984;46:74–80. doi: 10.1128/iai.46.1.74-80.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morfitt D C, Cheville N F, Jensen A E. Diminution of virulence of B. abortus for severe combined immunodeficient mice. Proc Conf Res Workers Anim Dis. 1991;72:2. [Google Scholar]
- 23.Oliveira S C, Splitter G A. CD8+ type 1 CD44hi CD45 RBlo T lymphocytes control intracellular Brucella abortus infection as demonstrated in major histocompatibility complex class I- and class II-deficient mice. Eur J Immunol. 1995;25:2551–2557. doi: 10.1002/eji.1830250922. [DOI] [PubMed] [Google Scholar]
- 24.Palmer M V, Cheville N F, Tatum F M. Morphometric and histopathologic analysis of lymphoid depletion in murine spleens following infection with Brucella abortus strains 2308 or RB51 or an htrA deletion mutant. Vet Pathol. 1996;33:282–289. doi: 10.1177/030098589603300304. [DOI] [PubMed] [Google Scholar]
- 25.Pavlov H, Hogarth M, McKenzie I F, Cheers C. In vivo and in vitro effects of monoclonal antibody to Ly antigens on immunity to infection. Cell Immunol. 1982;71:127–138. doi: 10.1016/0008-8749(82)90502-0. [DOI] [PubMed] [Google Scholar]
- 26.Phillips M, Pugh G J, Deyoe B L. Duration of strain 2308 infection and immunogenicity of Brucella abortus lipopolysaccharide in five strains of mice. Am J Vet Res. 1989;50:318–322. [PubMed] [Google Scholar]
- 27.Phillips R W, Elzer P H, Roop R I. A Brucella melitensis high-temperature requirement A (htrA) deletion mutant demonstrates a stress response defective phenotype in vitro and transient attenuation in the BALB/c mouse model. Microb Pathog. 1995;19:227–284. [PubMed] [Google Scholar]
- 28.Pugh G J, Zehr E S, Meador V P, Phillips M, McDonald T J, Deyoe B L. Immunologic, histopathologic, and bacteriologic responses of five strains of mice to Brucella abortus strain 2308. Am J Vet Res. 1989;50:323–328. [PubMed] [Google Scholar]
- 29.Robertson L, Farrell I D, Hinchliffe P M. The isolation of brucellae from contaminated sources. A review. Br Vet J. 1977;133:193–200. doi: 10.1016/s0007-1935(17)34142-8. [DOI] [PubMed] [Google Scholar]
- 30.Stevens M G, Olsen S C, Pugh G J, Palmer M V. Immune and pathologic responses in mice infected with Brucella abortus 19, RB51, or 2308. Infect Immun. 1994;62:3206–3212. doi: 10.1128/iai.62.8.3206-3212.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Van De Verg L L, Hartman A B, Bhattacharjee A K, Tall B D, Yuan L, Sasala K, Hadfield T L, Zollinger W D, Hoover D L, Warren R L. Outer membrane protein of Neisseria meningitidis as a mucosal adjuvant for lipopolysaccharide of Brucella melitensis in mouse and guinea pig intranasal immunization models. Infect Immun. 1996;64:5263–5268. doi: 10.1128/iai.64.12.5263-5268.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Winter A J, Duncan J R, Santisteban C G, Douglas J T, Adams L G. Capacity of passively administered antibody to prevent establishment of Brucella abortus infection in mice. Infect Immun. 1989;57:3438–3444. doi: 10.1128/iai.57.11.3438-3444.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Winter A J, Schurig G G, Boyle S M, Sriranganathan N, Bevins J S, Enright F M, Elzer P H, Kopec J D. Protection of BALB/c mice against homologous and heterologous species of Brucella by rough strain vaccines derived from Brucella melitensis and Brucella suis biovar 4. Am J Vet Res. 1996;57:677–683. [PubMed] [Google Scholar]
- 34.Yabu K, Youngner J S, Feingold D S, Keleti G, Gorelik E. Augmentation of natural killer cell activity in mice by Bru-Pel. J Immunother. 1991;10:307–312. doi: 10.1097/00002371-199110000-00002. [DOI] [PubMed] [Google Scholar]
- 35.Young E J, Borchert M, Kretzer F L, Musher D M. Phagocytosis and killing of Brucella by human polymorphonuclear leukocytes. J Infect Dis. 1985;151:682–690. doi: 10.1093/infdis/151.4.682. [DOI] [PubMed] [Google Scholar]
- 36.Young E J, Gomez C I, Yawn D H, Musher D M. Comparison of Brucella abortus and Brucella melitensis infections of mice and their effect on acquired cellular resistance. Infect Immun. 1979;26:680–685. doi: 10.1128/iai.26.2.680-685.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhan Y, Cheers C. Endogenous gamma interferon mediates resistance to Brucella abortus infection. Infect Immun. 1993;61:4899–4901. doi: 10.1128/iai.61.11.4899-4901.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]