Abstract
Sepsis affects millions of people worldwide and is associated with multiorgan dysfunction that is a major cause of increased morbidity and mortality. Sepsis is associated with several morbidities, such as lung, liver, and central nervous system (CNS) dysfunction. Sepsis-associated CNS dysfunction usually leads to several mental problems including depression. IL-17A is one of the crucial cytokines that is expressed and secreted by Th17 cells. Th17 cells are reported to be involved in the pathogenesis of depression and anxiety in humans and animals. One of the protein tyrosine kinases that plays a key role in controlling the development/differentiation of Th17 cells is ITK. However, the role of ITK in sepsis-associated neuroinflammation and depression-like symptoms in mice has not been investigated earlier. Therefore, this study investigated the efficacy of the ITK inhibitor, BMS 509744, in sepsis-linked neuroinflammation (ITK, IL-17A, NFkB, iNOS, MPO, lipid peroxides, IL-6, MCP-1, IL-17A) and a battery of depression-like behavioral tests, such as sucrose preference, tail suspension, and the marble burying test. Further, the effect of the ITK inhibitor on anti-inflammatory signaling (Foxp3, IL-10, Nrf2, HO-1, SOD-2) was assessed in the CNS. Our data show that sepsis causes increased ITK protein expression, IL-17A signaling, and neuroinflammatory mediators in the CNS that are associated with a depression-like state in mice. ITK inhibitor-treated mice with sepsis show attenuated IL-17A signaling, which is associated with the upregulation of IL-10/Nrf2 signaling and the amelioration of depression-like symptoms in mice. Our data show, for the first time, that the ITK inhibition strategy may counteract sepsis-mediated depression through a reduction in IL-17A signaling in the CNS.
Keywords: sepsis, ITK, neuroinflammation, IL-17A, depression
1. Introduction
Sepsis is associated with multiorgan dysfunction that may lead to increased morbidity and mortality. The prevalence of sepsis is reported to be 300–500 cases/100,000 people in the world. It is one of the leading causes of death in intensive care units with as many as 11 million sepsis-associated deaths worldwide per year [1,2,3,4]. Sepsis is associated with several morbidities, such as kidney, liver, cardiac, and central nervous system (CNS) dysfunction. Sepsis-associated encephalopathy causes a variety of mental problems, such as depression, delirium, and dementia. As many as 70% of critically ill patients are associated with sepsis-associated encephalopathy, which is a major cause of increased mortality and hospital costs for survivors especially in elderly people [4,5,6,7]. Therefore, there is a need for early intervention that may block the inflammatory pathways leading to neuroinflammation.
ITK is a member of the Tec kinase family and plays a quintessential function in T lymphocyte development and differentiation, i.e., CD4+ T cells, CD8 + T cells, NKT cells, and γδ T cells. ITK becomes activated through cell surface receptors on T cells, i.e., TCR and causes the activation of downstream signaling leading to the modulation of transcriptional machinery [8,9]. Transcriptional factors such as NFATc1 and STAT3 are regulated by ITK in naïve CD4+ T cells (Th0), which convert these cells into Th17 cells [8,10,11]. ITK signaling is also known to negatively regulate the development of Foxp3 expressing regulatory T cells (Treg) [12,13]. Hence, ITK has been shown to be overactivated in a variety of disease states, such as autoimmune neuroinflammatory disorders, acute lung/kidney injury, and psoriatic inflammation in animals [14,15,16]. Based on these observations, several ITK inhibitors have been shown to cause the downregulation of inflammatory pathways in immune-mediated autoimmune/inflammatory diseases, such as psoriasis, asthma, multiple sclerosis, and ulcerative colitis in both humans and animals [10,17,18]. However, sepsis-associated neuroinflammation remains uninvestigated with respect to ITK signaling.
It has been reported in the past that there is bidirectional communication between immune cells and CNS. T cells may contribute towards neuroinflammation via the expression of pro-inflammatory mediators. These inflammatory signals may include costimulatory signals or pro-inflammatory cytokines [7,19,20]. Other immune cells, such as neutrophils, which express iNOS and MPO, may also promote neuroinflammation through the induction of BBB dysfunction [21,22,23]. This may allow a greater infiltration and accumulation of other immune cells such as monocytes/T cells/B cells from systemic circulation into the CNS during sepsis. Infiltrated immune cells further amplify neuroinflammation by activating microglial cells, which release different pro-inflammatory chemokines, cytokines, and oxidants [24,25]. However, how ITK signaling affects oxidative inflammation in the CNS remains unexplored with respect to sepsis.
Therefore, this study attempted to explore the role of ITK signaling in causing systemic inflammation and neuroinflammation associated with sepsis. Further, the ITK inhibition approach was utilized to affirm whether ITK signaling was associated with depression-like effects in sepsis survivor mice. Our data reveal increased p-ITK protein levels in circulating CD4+ T cells and ITK protein levels in the cerebral cortex, which are associated with sepsis-mediated neuroinflammation and depression-like symptoms. The ITK inhibitor, BMS 509744, causes significant attenuation in sepsis-associated neuroinflammation and depression-like behavior through the downregulation of Th17-related mediators and oxidative stress in peripheral immune cells and the CNS.
2. Results
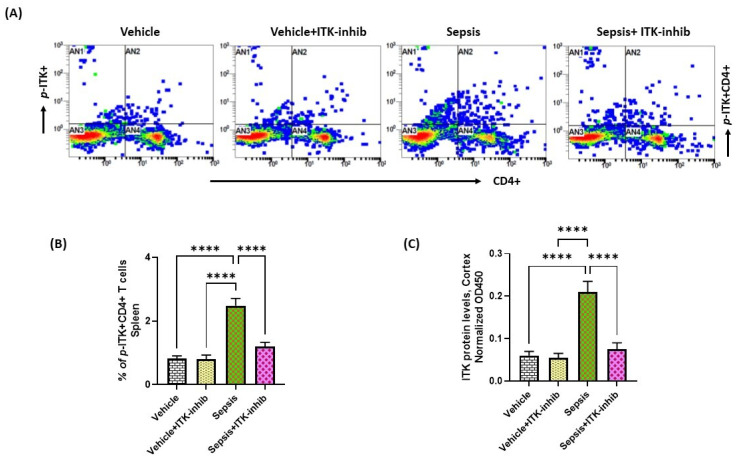
2.1. Sepsis Causes Upregulation of ITK in the Periphery and CNS
Sepsis is known to be associated with systemic inflammation and neuroinflammation in which ITK signaling may be involved; therefore, the modulation of ITK signaling in these phenomena was examined in this study. Our study showed an increased activation of ITK in CD4+ T cells as reflected by an increased % of p-ITK+ CD4+ T cells in the periphery of sepsis survivor mice (Figure 1A,B). Further, the ITK protein levels were also elevated in the cerebral cortex of sepsis survivor mice (Figure 1C). Treatment with the ITK inhibitor caused a downregulation in the p-ITK+ CD4+ T cells and ITK levels in the CNS of sepsis survivor mice (Figure 1). These data highlight that ITK signaling becomes activated in the CD4+ T cells and CNS of sepsis survivor mice.
Figure 1.
Elevation of ITK signaling in the periphery and CNS of sepsis survivor mice. (A) Representative flow plot for p-ITK+ CD4+ T cells’ immunostaining; (B) % of p-ITK+ CD4+ T cells; and (C) ITK protein levels in the cerebral cortex. Values are depicted as the mean ± SEM, n = 6–8/group. **** p < 0.0001.
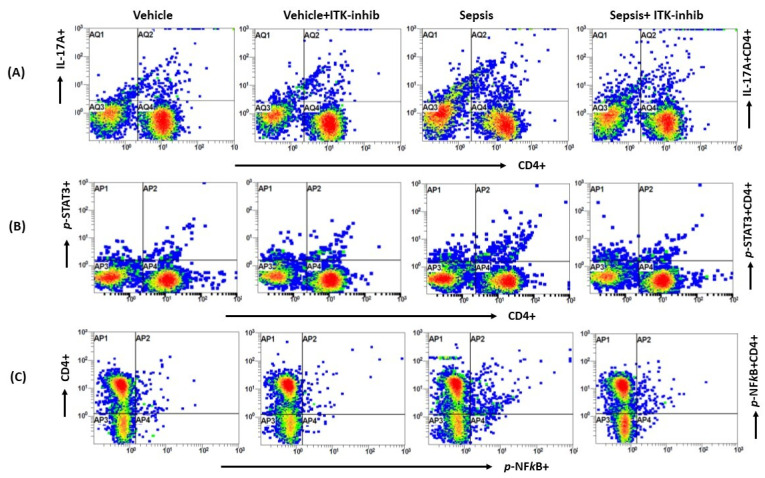
2.2. Sepsis-Induced Elevation in Th17 Cell-Related Signaling Is Attenuated by ITK Inhibition
Next, we wanted to explore whether Th17-related immune responses are controlled by ITK signaling in periphery and the CNS, and whether the BMS compound is able to attenuate them. Our data show that IL-17A, p-STAT3, and p-NFkB are elevated in CD4+ T cells in the periphery as depicted by the % of IL-17A+ CD4+ T cells, p-STAT3+ CD4+ T cells, and p-NFkB+ CD4+ T cells (Figure 2). Sepsis-induced elevation in the Th17-related parameters were attenuated by the ITK inhibitor in the periphery (Figure 2).
Figure 2.
The ITK inhibitor downregulated Th17-related signaling in the periphery of sepsis survivor mice. (A) Representative flow plot for IL-17A+ CD4+ T cells’ immunostaining; (B) Representative flow plot for p-STAT3+ CD4+ T cells’ immunostaining; (C) Representative flow plot for p-NFkB+ CD4+ T cells; (D) % of IL-17A+ CD4+ T cells; (E) % of p-STAT3+ CD4+ T cells; (F) % of p-NFkB+ CD4+ T cells; and (G) IL-17A protein levels in serum. The values are depicted as the mean ± SEM, n = 6/group. *** p < 0.001; **** p < 0.0001.
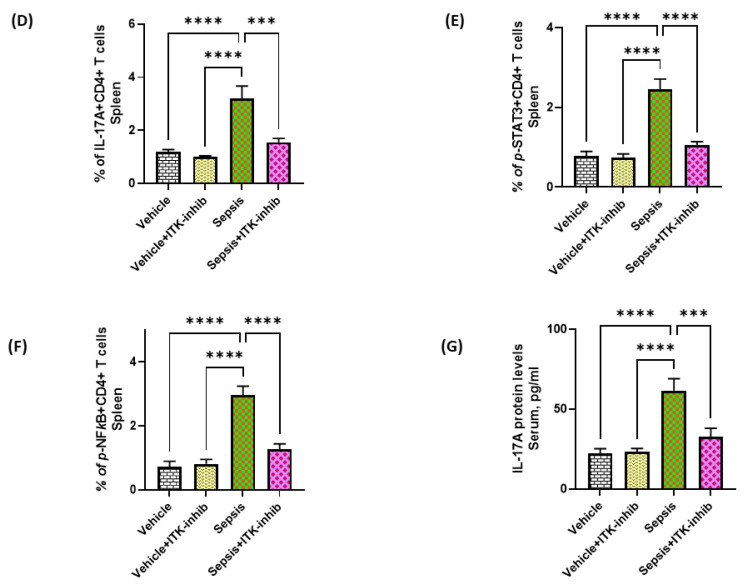
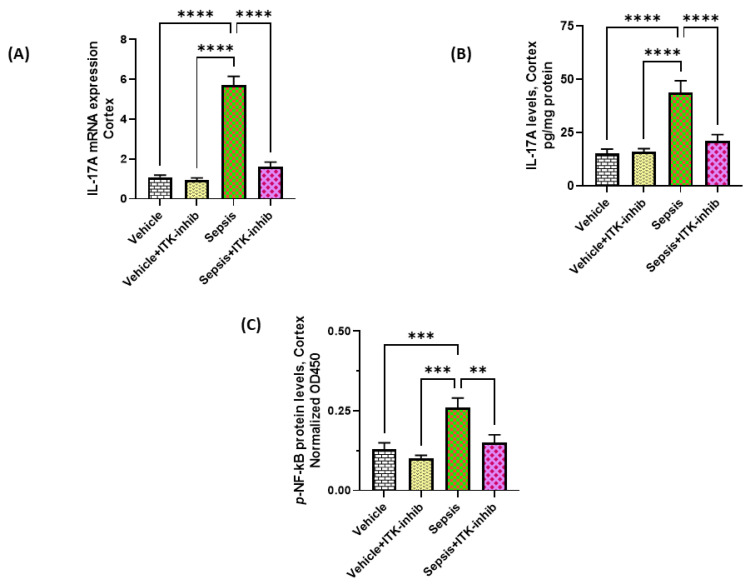
2.3. Sepsis-Induced Elevation in IL-17A Signaling Is Attenuated by ITK Inhibition
Further, IL-17A-mediated signaling in the cerebral cortex was also explored. Our data show elevated IL-17A levels in the cerebral cortex, which were associated with elevated p- NFkB protein levels (Figure 3A–C). Sepsis-induced IL-17A signaling was greatly reduced by the ITK inhibitor (Figure 3). p-STAT3 protein levels in the cerebral cortex were also significantly increased in the sepsis group (0.183 ± 0.02, mean ± SEM, n = 8) as compared to the vehicle (0.097 ± 0.01, mean ± SEM, n = 6; p < 0.01) and the vehicle + ITK-inhib (0.103 ± 0.012, mean ± SEM, n = 6; p < 0.01) groups; however, the sepsis + ITK-inhib group (0.155 ± 0.015, mean ± SEM, n = 8; p > 0.05) did not have any significant difference in the p-STAT3 levels as compared to the sepsis group (0.183 ± 0.02, mean ± SEM, n = 8). These data show that ITK activation is involved in the elevation of IL-17A levels both in the periphery and the CNS, which can be controlled by ITK inhibition.
Figure 3.
ITK inhibitor caused a reduction in IL-17A-related signaling in the CNS of sepsis survivor mice. (A) IL-17A mRNA expression; (B) IL-17A protein levels; and (C) p-NFkB protein levels. The values are depicted as the mean ± SEM, n = 6–8/group. ** p < 0.01; *** p < 0.001; **** p < 0.0001.
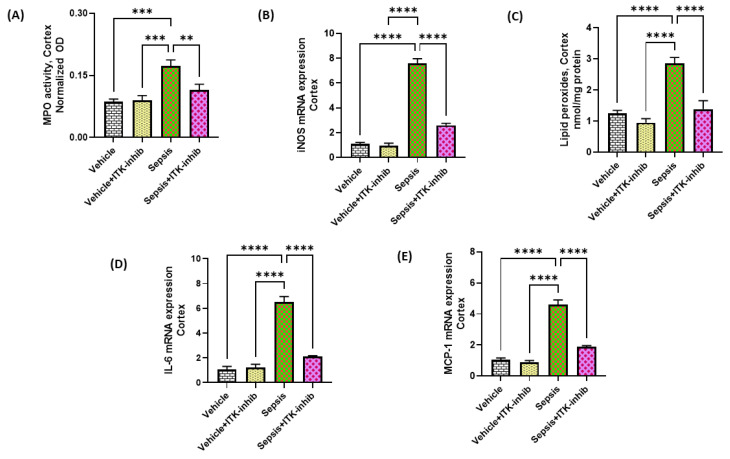
2.4. Sepsis-Induced Oxidative Neuroinflammation Is Attenuated by ITK Inhibition
Oxidative inflammation is a major contributor in neuroinflammatory pathways associated with sepsis; therefore, we next explored whether ITK inhibition would lead to a modulation of the oxidative neuroinflammation. Our data show that the MPO activity, iNOS, and lipid peroxides were elevated in the cerebral cortex of mice with sepsis (Figure 4A–C). Treatment with BMS 509744 caused a significant downregulation of the oxidative markers in the cerebral cortex of sepsis survivor mice (Figure 4A–C). Further, it was evaluated whether the ITK inhibitor also caused the downregulation of neuroinflammatory mediators in sepsis survivor mice. Our data reveal that IL-6 and MCP-1 mRNA were elevated in the cerebral cortex of sepsis survivor mice (Figure 4D,E). The sepsis-associated elevation in neuroinflammatory mediators, such as IL-6 and MCP-1, were greatly reduced in the CNS by the ITK inhibitor (Figure 4D,E). These data show that the ITK inhibition approach has the potential to attenuate sepsis-induced oxidative and neuroinflammatory mediators.
Figure 4.
ITK inhibitor caused a reduction in oxidative and inflammatory mediators in the CNS of sepsis survivor mice. (A) MPO activity; (B) iNOS mRNA expression; (C) Lipid peroxides; (D) IL-6 mRNA expression; and (E) MCP-1 mRNA expression. The values are depicted as the mean ± SEM, n = 6–8/group. ** p < 0.01; *** p < 0.001; **** p < 0.0001.
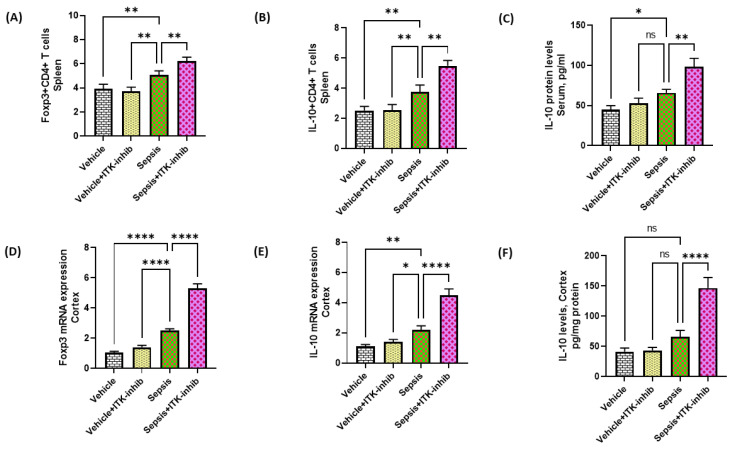
2.5. Treg Cell-Related Signaling Is Further Elevated by ITK Inhibition in Sepsis Survivor Mice
ITK is also known to regulate the development of Treg cells. Therefore, the effect of the ITK inhibitor was investigated on Treg-related parameters in the periphery and CNS. Our data show that IL-10 and Foxp3 are elevated in CD4+ T cells in the periphery of sepsis survivor mice as depicted by the % of IL-10+ CD4+ T cells and Foxp3+ CD4+ T cells (Figure 5A–C). Treg cells were further elevated by the ITK inhibitor in sepsis survivor mice (Figure 5A–C). Further, IL-10 and Foxp3 mRNA levels were also elevated in the cerebral cortex of sepsis survivor mice by the ITK inhibitor (Figure 5D–F). These data show that ITK inhibition upregulates Treg-related signaling in the periphery and CNS, which may attenuate sepsis-induced neuroinflammation.
Figure 5.
The ITK inhibitor caused an elevation in Treg-related signaling in the periphery and CNS of sepsis survivor mice. (A) % of Foxp3 + CD4+ T cells; (B) % of IL-10+ CD4+ T cells; (C) IL-10 protein levels in serum; (D) Foxp3 mRNA expression; (E) IL-10 mRNA expression; and (F) IL-10 protein levels in the cortex. The values are depicted as the mean ± SEM, n = 6–8/group. * p < 0.05; ** p < 0.01; **** p < 0.0001; ns = not significant.
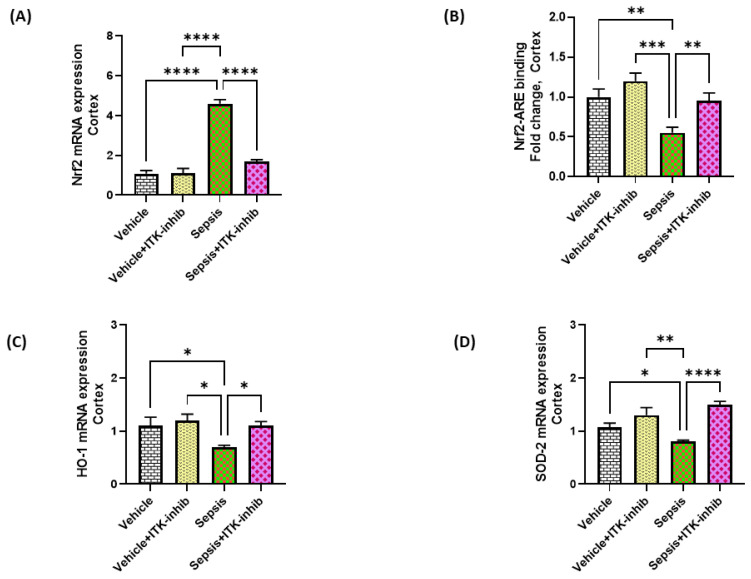
2.6. Sepsis-Mediated Decrease in Antioxidant Transcription Factor Nrf2 Is Restored by ITK Inhibition in the CNS
Further, the effect of BMS 509744 was assessed on the Nrf2 antioxidant system. Nrf2/HO-1 signaling was dysregulated in the cerebral cortex as depicted by the decreased nuclear translocation of Nrf2 in mice with sepsis, although the Nrf2 mRNA levels were increased in the same group (Figure 6A,B). Consequently, Nrf2-induced antioxidant enzymes were dysregulated in the cortex as depicted by the decreased HO-1 and SOD-2 mRNA levels in the sepsis survivor mice (Figure 6C,D). Sepsis-induced derangements in Nrf2 signaling were corrected by the ITK inhibitor as reflected by the restoration of Nrf2 nuclear translocation in the cerebral cortex (Figure 6).
Figure 6.
The ITK inhibitor caused a restoration of the Nrf2 signaling in the CNS of sepsis survivor mice. (A) Nrf2 mRNA expression; (B) Nrf2–ARE binding in the cortex; (C) HO-1 mRNA expression; and (D) SOD2 mRNA expression. The values are depicted as the mean ± SEM, n = 6–8/group. * p < 0.05; ** p < 0.01; *** p < 0.001; **** p < 0.0001.
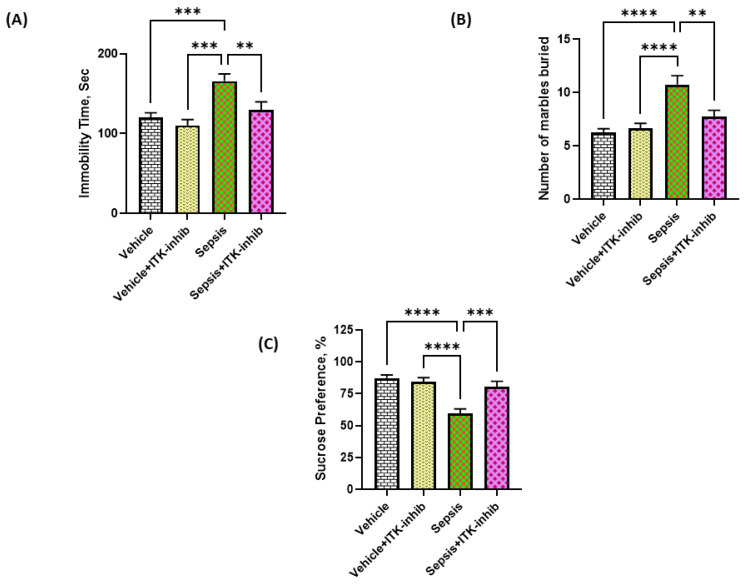
2.7. Sepsis-Induced Depression-like Behavior Is Ameliorated by ITK Inhibition
Sepsis is known to induce depression-like behavior after the recovery period. Therefore, we finally investigated whether ITK inhibition has the potential to modulate depression-like behavior in sepsis survivor mice. Our data display that mice with sepsis survival had depression-like behavior. Mice that recovered from sepsis had an increased immobility time in the tail suspension test, an increased marble burying character, and a decreased sucrose preference indicative of depression-like behavior (Figure 7A–C). BMS 509744 caused a reversal of sepsis-induced depression-like behavior as displayed by a decrease in immobility time and a decrease in the number of marbles buried (Figure 7A,B). Further, BMS 509744 caused a reversal of the sepsis-induced reduction in sucrose preference (Figure 7C). These data show that the sepsis-induced depression-like state is ameliorated by the ITK inhibition strategy.
Figure 7.
The ITK inhibitor caused an amelioration of the sepsis-induced depression-like state in mice. (A) Immobility time in TST; (B) Marble burying behavior; and (C) Sucrose preference test. The values are depicted as the mean ± SEM, n = 6–8/group. ** p < 0.01; *** p < 0.001; **** p < 0.0001.
3. Discussion
Immune dysfunction in sepsis is characterized by dysregulated immune responses, which are orchestrated by both arms of the immune system, i.e., the innate (neutrophils/DCs) and adaptive (T cells/B cells) arms. The innate immune system is initially activated by different microbial agents in sepsis, which causes the release of a variety of mediators that include oxidants, chemokines, prostaglandins, and cytokines [7,26,27,28]. This systemic inflammatory soup causes an activation of the adaptive immune system as well as other structural cells ultimately leading to a hyperinflammatory state that causes neuroinflammation and behavioral derangements [8,29,30]. Our study shows that ITK plays an important role in sepsis-associated neuroinflammation through the modification of Th17-related signaling in the periphery and CNS.
The Tec kinase family consists of several members that include TEC, BTK, TXK, BMX, and ITK. ITK is favorably expressed in T cells where ITK expression is the highest [14,15,16]. Apart from T cells, ITK is also expressed in natural killer T cells, γδ T cells, and mast cells. Based on ITK expression, it has been shown to have a predominant role in T cell function through T cell receptor signaling (TCR) [14,15].
Phosphorylated ITK activates several downstream targets, such as PLCγ1, leading to the formation of secondary messengers, such as IP3 and DAG, which further activate other signaling pathways, such as NFkB, NFATc1 and STAT3 [9,16,18]. These transcription factors translocate to the T cell nucleus and are involved in the differentiation of Th0 into Th17 cells. Th17 cells, after polarization, release several inflammatory cytokines, with IL-17A being the most predominant one [10,31]. To investigate the contribution of ITK in sepsis-mediated neuroinflammation, its expression in CD4+ T cells and the CNS was determined. Our data showed an increased expression of p-ITK and its downstream targets in CD4+ T cells and the CNS in mice with sepsis.
Immune cells in the systemic compartment are known to communicate with the CNS through the bidirectional trafficking of mediators. Peripheral immune cells have the potential to modulate the BBB and communicate with the CNS through various mechanisms following sepsis [7,19,32,33]. Sepsis can disturb the BBB, which may create an environment for the extravasation of leukocytes such as Th17 cells from the peripheral blood into the CNS. ITK signaling is required for the trafficking of Th17 cells across the BBB, which is a critical step in the induction of neuroinflammation [17]. Infiltrated Th17 cells may further activate resident CNS immune cells, such as microglia, causing them to produce a neuroinflammatory cocktail of mediators, such as cytokines, oxidants, proteases, and chemokines. These mediators further facilitate the influx of other immune cells into the brain, which aggravates the sepsis-linked neuroinflammatory state [23,34,35,36]. Consistently, Th17 cells and IL-17A protein levels along with other inflammatory mediators were increased in the periphery and the cerebral cortex of septic mice. BMS 509744-treated mice had a significant attenuation of IL-17A levels in the periphery and the CNS in sepsis survivor mice.
It is well-known that IL-17A can cause neuroinflammation through the activation of IL-17R, STAT3 and NF-kB [37,38]. IL-17A can cause the activation of resident brain immune cells such as microglial cells/astrocytes, which can promote the neuroinflammatory response through the production of pro-inflammatory cytokines, such as MCP-1, IL-6, and TNF-alpha from microglial cells, further worsening CNS dysfunction [39,40,41]. Overactivation of the microglia is involved in the progression of brain dysfunction, which could be responsible for a depression-like state and worse survival in septic patients. IL-17A has been shown to cause a depression-like state in animal models and human beings by causing neuroinflammation [35,40,41,42,43]. A recent study in rats has shown that Th17 cell recruitment into the CNS is required for the induction of a depression-like state [44]. The reduction in neuroinflammatory markers via a blockade of Th17/IL-17A signaling leads to cognitive improvements and anti-depressant effects in mice/rats [37,40,44]. Our study shows a reduction in IL-17A levels with a concurrent abatement of neuroinflammation by the ITK inhibitor, which may be responsible for the amelioration in sepsis-associated depression-like behavior.
Neutrophils are active participants in the innate immune response and are regarded as one of the major immune cells in sepsis-induced immune dysfunction [23]. Increased MPO activity (considered to be a marker of neutrophilic presence) in the cerebral cortex of sepsis survivor mice could be due to increased IL-17A levels. IL-17A has been shown to be a major chemoattract cytokine for neutrophilic transmigration across the BBB [35,43,45]. IL-17A-mediated neutrophil infiltration in the CNS may endanger neuronal cells by releasing oxidants through the activity of iNOS and MPO, thus promoting sepsis-associated CNS dysfunction [23,33,37]. Oxidative neuroinflammation was confirmed by the increased MPO activity, which is a hallmark of neutrophil infiltration in the brain. It has also been shown, earlier, during sepsis-induced neuroinflammation [24,43]. The ITK inhibitor mediated the downregulation of IL-17A, and subsequent oxidative stress in the CNS may protect neuronal cells from oxidative injury, which can partly mitigate sepsis-mediated behavioral problems.
ITK activity and Treg cell development have been shown to have a negative correlation. ITK plays a gatekeeper role in the development of Treg cells. Foxp3-expressing regulatory T cells (Treg) and Th17 cells share common requirements for their development such as the presence TGF-β [14,31]. Moreover, Th0 (naïve CD4+ T cells) deficient in ITK preferentially differentiate into Treg cells under the influence of Th17-differentiating cytokines in vitro [13,46]. Treg cells cause anti-inflammatory actions through multiple mechanisms such as the inhibition of DC maturation and the production of suppressive cytokines such as IL-10 [47]. A reduction in the Treg-related immune response in the CNS has been shown to cause a depression-like state in mice [39]. Our study showed elevated Foxp3/IL-10 levels and Treg cells in the CNS/periphery by the ITK inhibitor, which may counter the sepsis-mediated depression-like state in mice.
NFkB and Nrf2 signaling have been reported to have reciprocal relationships. Nrf2 is a ubiquitous transcription factor, which is heavily involved in the regulation of the antioxidant defense mechanism. Nrf2, by binding to its ARE in the nucleus, is responsible for the transcription of multiple antioxidant genes, such as hemoxygenase-1, superoxide dismutase-2, and thioredoxin [48]. Excessive activation of the NFkB pathway and ROS production can diminish Nrf2–ARE signaling in the nucleus leading to impaired antioxidant defense [41,49,50,51]. ITK inhibition caused the restoration of Nrf2 signaling in the cerebral cortex, which could lead to an amelioration of a depression-like state. Enhancing Nrf2 levels via genetic/pharmacological manipulation in mice has shown improved outcomes in sepsis [49,52].
This study has some limitations. Firstly, the CD4+ T cells were not isolated from the brain, which would have provided direct confirmation of ITK expression within these immune cells. Secondly, other types of T cells, which also express ITK as well as IL-17A, have not been analyzed in this study. Thirdly, sepsis-induced changes have been measured only in the cerebral cortex. Other brain areas, such as the hippocampus, amygdala, and hypothalamus, which may be affected by sepsis and play an important role in depression-like behavior, also need to be investigated in future studies. Moreover, the direct administration of the ITK inhibitor to the CNS through the intracerebroventricular route should also be investigated as it will show whether targeting ITK in CNS T cells has any effect on sepsis-induced depression-like behavior.
Sepsis in ICUs is one of the leading causes of deaths and morbidity throughout the world. The interaction between peripheral immune cells such as Th17 cells and the CNS during sepsis may cause multiple neurological outcomes. Sepsis survivors are linked to behavioral/mental derangements, such as depression, anxiety, delirium, loss of consciousness, and cognitive impairments in almost 70% of critically ill patients [5,7,36]. Our study shows for the first time that early intervention using the ITK inhibitor strategy may limit sepsis-induced neuroinflammation and depression via the regulation of the Th17/Treg balance, which may improve the long-term survival and better the prognosis of septic patients.
4. Materials and Methods
4.1. Animals
This investigation utilized male C57BL/6 mice following approval from the Animal Care and Research Committee of the College of Pharmacy, King Saud University. All experimental protocols were followed as per the recommended guidelines of the NIH for the utilization of animals. The mice used for the experiments were 48–50 weeks old (40–42 gm) and bred in-house at our college animal care facility. The mice were provided specific pathogen-free conditions with ventilated cages and a controlled environment (standard conditions of temperature and humidity with a 12 h light-dark cycle) for proper growth. The mice had access to food and water ad libitum.
4.2. Induction of Sepsis and Drug Administration
To investigate the effect of ITK signaling on sepsis-induced neuroinflammation as well as depression-like symptoms, the aged mice were administered BMS 509744 (Tocris, Bristol, UK) at a dose of 10 mg/kg, i.p., at the time of the LPS injection. Thereafter, BMS 509744 was administered at the same dose once every day for 10 days. For the induction of sepsis, the mice were given an i.p. injection of LPS (derived from E. coli, O111:B4) at a dose of 2.5 mg/kg. There were four groups of mice, which were as follows: (1) Vehicle: mice treated with the vehicle (n = 6); (2) Vehicle + ITK-inhib (n = 6): mice treated with the vehicle and ITK inhibitor (10 mg/kg); (3) LPS (n = 8): mice administered at the set dose of 2.5 mg/kg as described above; and (4) LPS + ITK-inhib (n = 8): mice administered a dose of LPS (2.5 mg/kg) and treated with the ITK inhibitor (10 mg/kg). On days 8–10, the mice were utilized for different behavioral experiments followed by the sacrifice of the mice using a deep inhalational anesthesia of isoflurane. The organs (spleen/brain) were dissected out on day 10 for different molecular and biochemical assays as described below.
4.3. Tail Suspension Method
The tail suspension method is one of the most-well known methods to assess depression-like behavior in mice, as described previously [53]. This test utilizes the paradigm of putting the animal in an unavoidable and uncomfortable situation via the tail suspension method. The mouse was suspended 25 cm above the ground by its tail using adhesive tape and the immobility time was recorded by a blinded observer for a period of 6 min. Immobility of the mouse was characterized by motionless hanging without active kicking and struggling.
4.4. Sucrose Preference Test
The mice were provided access to two liquid bottles ad libitum. One bottle contained normal tap water and the other contained 2% sucrose in tap water. On the day of the experiment, the mice were provided with both water bottles for a period of 24 h. After that, the mice were returned to the home cage and the amount of water consumed from each bottle (sucrose/tap water bottle) was calculated. The mice were habituated to a consumption of 2% sucrose solution and normal tap water before the actual testing. The sucrose preference (%) was calculated as follows = (sucrose intake/total fluid intake) × 100.
4.5. Marble Bury Behavior
The marble burying experiment was carried out to evaluate the depression-like behavior of mice [39]. In summary, each mouse was given a task to explore burying behavior for 30 min in a cage that had 20 marbles (placed in a pattern of 4 × 5 with a diameter of 15 mm for each marble) on top of 3–4 cm deep unperfumed bedding. A scientist blinded to the experimental groups counted the number of marbles that were buried by each mouse. If a marble was buried >50% in the bedding, then it was counted as a buried marble.
4.6. Measurement of Myeloperoxidase Activity in CNS
Myeloperoxidase (MPO) activity was measured in the cortex of different experimental groups as an indicator of neutrophilic inflammation, as described earlier [54,55]. Briefly, an MPO substrate buffer containing H2O2 (0.0005%) and O-dianisidine (0.167 mg/mL) in 50 mM potassium phosphate was incubated with the sample and allowed to stand for 20 min at 25 °C. The MPO activity was recorded by measuring the OD at 450 nm. The OD was normalized by the protein content of the respective sample.
4.7. Nrf2 Trans-Activation ELISA Assay in the CNS
The Nrf2 trans-activation binding activity of the nuclear extracts of cortex was assessed utilizing a commercial Trans-AM Nrf2 kit (Active Motif, Carlsbad, CA, USA). Nuclear extract from the brain cortex of each mouse was prepared using a Nuclear Extract kit according to the protocol of the supplier (Active Motif, Carlsbad, CA, USA). In summary, this ELISA kit utilizes the coupling of Nrf2 present in the brain sample to its ARE, i.e., 5′-GTCACAGTACTCAGCAGAATCTG-3′. Nrf2/ARE binding activity in the nuclear extracts of cortex is directly proportional to the color development. The data were expressed in fold difference.
4.8. Real-Time PCR
The cortex was isolated in a RNAlater® (Thermo Fisher Scientific, Waltham, MA, USA) solution and used within a month after its isolation. The total RNA was isolated using the TRIzol method followed by checking its purity (OD:260/280 > 2) and concentration. The total RNA (1 µg) was then converted into cDNA via the reverse transcription method using a high-Capacity cDNA archive kit (Applied Biosystems, Waltham, MA, USA) as written before [45,54,55]. mRNA expression was conducted on the ABI PRISM 7500 sequence detection system (Applied Biosystems, Waltham, MA, USA) using the primers (GenScript, Piscataway, NJ, USA) for the following genes, i.e., iNOS, HO-1, Nrf2, IL-6, MCP-1, IL-17A, SOD2, and GAPDH (endogenous control). The relative mRNA expression in different brain samples was measured using the well-known ddCt method.
4.9. Preparation of Samples for Biochemical Measurements
The brain cortex from each mouse was homogenized in an ice-cold cell lysis buffer with a protease inhibitor cocktail (Thermo Fisher Scientific, Waltham, MA, USA) followed by centrifugation at 12,000 rpm for 20 min. The supernatant was then collected from each sample and used in the different assays mentioned below. Blood was collected via cardiac puncture in non-heparinized tubes after terminal anesthesia, and the serum was separated and stored at −80 °C for the IL-17A/IL-10 measurement.
4.10. Estimation of ITK, p-NFkB, and p-STAT3 Levels in the Cortex
Levels of the ITK and phospho-NFkB proteins in the cerebral cortex of different groups were measured using ITK (Aviva Systems Biology, San Diego, CA, USA), CST’s PathScan® Phospho-NFkBp65 (Ser536), and CST’s PathScan® Phospho-STAT3 (Tyr705) (Cell Signaling Tech, Danvers, MA, USA) ELISA kits, respectively. ITK, p-NFkB, and p-STAT3 levels were measured in terms of the OD and later normalized with protein content with the respective samples. The results are expressed as the OD450/mg protein.
4.11. Estimation of Lipid Peroxides in Cortex
An assessment of the lipid peroxides in the cortex was performed as described before [56]. The data were expressed as nmol/mg protein.
4.12. Estimation of Cytokines in Cortex/Serum
An assessment of IL-17A/IL-10 in the cortex/serum was carried out using commercially available ELISA kits (Biolegend, San Diego, CA, USA). The data were expressed as pg/mg protein (cortex) and pg/mL (serum).
4.13. Flow Cytometry
The spleen was made into a single cell suspension for flow cytometry, as described earlier [45,55]. Briefly, the spleen was collected immediately after sacrifice and placed in a 70 μm stainless steel strainer, which was kept on top of a 50 mL conical tube containing RMPI-1640 medium. The spleen was then dilacerated with the piston of a syringe to collect a single cell suspension. Immune cells (1 million cells) in the splenic cell suspension were immunostained with monoclonal antibodies against cell surface receptors, i.e., CD4 coupled to APC-Cy7/FITC/APC (Biolegend, San Diego, CA, USA; Santa Cruz Biotech, Dallas, TX, USA). Immune cells were then permeabilized/fixed and processed for intracellular staining. Immune cells were then immunostained with monoclonal antibodies against intracellular proteins such as IL-10, p-ITK, p-NFkB, Foxp3, p-STAT3 and IL-17A coupled to APC/PE/FITC (Biolegend, San Diego, CA, USA; Cell Signaling Tech, Danvers, MA, USA). Immune cells were then acquired (10,000 events) on a flow cytometer and analyzed with Cytomics FC500 software (Beckman Coulter, Brea, CA, USA), as described earlier [45,55]. CD4+ T cells and their intracellular markers were analyzed in a lymphocytic gate on a forward and side scatter plot.
4.14. Statistical Analysis
The data were shown as the Mean ± SE and the significance level was set at p < 0.05 for statistical analyses. Molecular/biochemical data were analyzed with one-way ANOVA followed by Tukey’s post-hoc test for multiple comparisons. Brown–Forsythe is used automatically by GraphPad Prism 9 software for testing the homogeneity of variances; this test showed p > 0.05 for the analyzed parameters. All statistical calculations were analyzed using GraphPad Prism 9 (GraphPad Software, San Diego, CA, USA).
5. Conclusions
Sepsis in ICUs is one of leading causes of deaths and morbidity throughout the world. The interaction between peripheral immune cells such Th17 cells and CNS during sepsis may cause multiple neurological outcomes. Sepsis survivors are linked to behavioral/mental derangements such as depression, anxiety, delirium, loss of consciousness, and cognitive impairments in almost 70% of critically ill patients [5,7,30]. Our study shows for the first time that early intervention by ITK inhibitor strategy may limit sepsis-induced neuroinflammation and depression by regulation of Th17/Treg balance which may improve the long-term survival and better the prognosis of septic patients.
Acknowledgments
The authors extend their appreciation to the Deputyship for Research and Innovation, Ministry of Education in Saudi Arabia for funding this research work through the project no. (IFKSURG-2-1303).
Author Contributions
Conceptualization, A.N.; Data curation, S.F.A., K.E.I. and A.N.; Formal analysis, S.A., S.S.A., S.F.A., A.S.A., S.M.A. and A.N.; Investigation, M.M.A., S.F.A., S.A.A., A.S.A., K.E.I., S.M.A. and A.N.; Methodology, M.M.A., S.A., S.F.A., S.A.A., A.S.A., K.E.I., S.M.A. and A.N.; Project administration, N.O.A.-H. and A.N.; Resources, M.M.A., S.A., S.S.A. and N.O.A.-H.; Software, S.S.A. and S.A.A.; Supervision, N.O.A.-H.; Validation, K.E.I., S.M.A. and A.N.; Writing—original draft, S.F.A., N.O.A.-H., S.A.A., A.S.A., K.E.I., S.M.A. and A.N.; Writing—review and editing, M.M.A., S.A., S.S.A. and A.N. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The animal study protocol was approved by the Ethical Committee of the College of Pharmacy, King Saud University (Ethical Reference No: KSU-SE-19-45).
Informed Consent Statement
Not applicable.
Data Availability Statement
All data presented in this study are available on reasonable request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
Deputyship for Research and Innovation, Ministry of Education in Saudi Arabia: (IFKSURG-2-1303).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Dellinger R.P., Levy M.M., Rhodes A., Annane D., Gerlach H., Opal S.M., Sevransky J.E., Sprung C.L., Douglas I.S., Jaeschke R., et al. Surviving sepsis campaign: International guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med. 2013;41:580–637. doi: 10.1007/s00134-012-2769-8. [DOI] [PubMed] [Google Scholar]
- 2.Levy M.M., Artigas A., Phillips G.S., Rhodes A., Beale R., Osborn T., Vincent J.-L., Townsend S., Lemeshow S., Dellinger R.P. Outcomes of the Surviving Sepsis Campaign in intensive care units in the USA and Europe: A prospective cohort study. Lancet Infect. Dis. 2012;12:919–924. doi: 10.1016/S1473-3099(12)70239-6. [DOI] [PubMed] [Google Scholar]
- 3.Rudd K.E., Johnson S.C., Agesa K.M., Shackelford K.A., Tsoi D., Kievlan D.R., Colombara D.V., Ikuta K.S., Kissoon N., Finfer S., et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: Analysis for the Global Burden of Disease Study. Lancet. 2020;395:200–211. doi: 10.1016/S0140-6736(19)32989-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.De La Rica A.S., Gilsanz F., Maseda E. Epidemiologic trends of sepsis in western countries. Ann. Transl. Med. 2016;4:325. doi: 10.21037/atm.2016.08.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huang Y., Chen R., Jiang L., Li S., Xue Y. Basic research and clinical progress of sepsis-associated encephalopathy. J. Intensiv. Med. 2021;1:90–95. doi: 10.1016/j.jointm.2021.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kaukonen K.M., Bailey M., Suzuki S., Pilcher D., Bellomo R. Mortality related to severe sepsis and septic shock among critically ill patients in Australia and New Zealand, 2000–2012. JAMA. 2014;311:1308–1316. doi: 10.1001/jama.2014.2637. [DOI] [PubMed] [Google Scholar]
- 7.Ren C., Yao R.-Q., Zhang H., Feng Y.-W., Yao Y.-M. Sepsis-associated encephalopathy: A vicious cycle of immunosuppression. J. Neuroinflammation. 2020;17:14. doi: 10.1186/s12974-020-1701-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Adam N., Kandelman S., Mantz J., Chrétien F., Sharshar T. Sepsis-induced brain dysfunction. Expert Rev. Anti-infective Ther. 2013;11:211–221. doi: 10.1586/eri.12.159. [DOI] [PubMed] [Google Scholar]
- 9.Gallagher M.P., Conley J.M., Vangala P., Garber M., Reboldi A., Berg L.J. Hierarchy of signaling thresholds downstream of the T cell receptor and the Tec kinase ITK. Proc. Natl. Acad. Sci. USA. 2021;118:e2025825118. doi: 10.1073/pnas.2025825118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lechner K.S., Neurath M.F., Weigmann B. Role of the IL-2 inducible tyrosine kinase ITK and its inhibitors in disease pathogenesis. J. Mol. Med. 2020;98:1385–1395. doi: 10.1007/s00109-020-01958-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mammadli M., Harris R., Suo L., May A., Gentile T., Waickman A.T., Bah A., August A., Nurmemmedov E., Karimi M. Interleu-kin-2-inducible T-cell kinase (Itk) signaling regulates potent noncanonical regulatory T cells. Clin. Transl. Med. 2021;11:e625. doi: 10.1002/ctm2.625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huang W., Jeong A.-R., Kannan A.K., Huang L., August A. IL-2–Inducible T Cell Kinase Tunes T Regulatory Cell Development and Is Required for Suppressive Function. J. Immunol. 2014;193:2267–2272. doi: 10.4049/jimmunol.1400968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weeks S., Harris R., Karimi M. Targeting ITK signaling for T cell-mediated diseases. iScience. 2021;24:102842. doi: 10.1016/j.isci.2021.102842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Andreotti A.H., Schwartzberg P.L., Joseph R.E., Berg L.J. T-Cell Signaling Regulated by the Tec Family Kinase, Itk. Cold Spring Harb. Perspect. Biol. 2010;2:a002287. doi: 10.1101/cshperspect.a002287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Berg L.J., Finkelstein L.D., Lucas J.A., Schwartzberg P.L., Smith-Garvin J.E., Koretzky G.A., Jordan M.S., Thomas S.M., Brugge J.S., Veillette A., et al. Tec family kinases in t lymphocyte development and function. Annu. Rev. Immunol. 2005;23:549–600. doi: 10.1146/annurev.immunol.22.012703.104743. [DOI] [PubMed] [Google Scholar]
- 16.Gomez-Rodriguez J., Kraus Z.J., Schwartzberg P.L. Tec family kinases Itk and Rlk / Txk in T lymphocytes: Cross-regulation of cytokine production and T-cell fates. FEBS J. 2011;278:1980–1989. doi: 10.1111/j.1742-4658.2011.08072.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kannan A.K., Kim D.-G., August A., Bynoe M.S. Itk Signals Promote Neuroinflammation by Regulating CD4+T-Cell Activation and Trafficking. J. Neurosci. 2015;35:221–233. doi: 10.1523/JNEUROSCI.1957-14.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nadeem A., Ahmad S.F., Al-Harbi N.O., Ibrahim K.E., Alqahtani F., Sobeai H.M.A., Alotaibi M.R. Inhibition of interleukin-2-inducible T-cell kinase causes reduction in imiquimod-induced psoriasiform inflammation through reduction of Th17 cells and en-hancement of Treg cells in mice. Biochimie. 2020;179:146–156. doi: 10.1016/j.biochi.2020.09.023. [DOI] [PubMed] [Google Scholar]
- 19.Galea I. The blood–brain barrier in systemic infection and inflammation. Cell. Mol. Immunol. 2021;18:2489–2501. doi: 10.1038/s41423-021-00757-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reyes M., Filbin M.R., Bhattacharyya R.P., Billman K., Eisenhaure T., Hung D.T., Levy B.D., Baron R.M., Blainey P.C., Goldberg M.B., et al. An immune-cell signature of bacterial sepsis. Nat. Med. 2020;26:333–340. doi: 10.1038/s41591-020-0752-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Anderson S.T., Commins S., Moynagh P.N., Coogan A.N. Lipopolysaccharide-induced sepsis induces long-lasting affective changes in the mouse. Brain Behav. Immun. 2015;43:98–109. doi: 10.1016/j.bbi.2014.07.007. [DOI] [PubMed] [Google Scholar]
- 22.Sankowski R., Mader S., Valdés-Ferrer S.I. Systemic inflammation and the brain: Novel roles of genetic, molecular, and envi-ronmental cues as drivers of neurodegeneration. Front. Cell. Neurosci. 2015;9:28. doi: 10.3389/fncel.2015.00028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shen X.-F., Cao K., Jiang J.-P., Guan W.-X., Du J.-F. Neutrophil dysregulation during sepsis: An overview and update. J. Cell. Mol. Med. 2017;21:1687–1697. doi: 10.1111/jcmm.13112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Comim C.M., Vilela M.C., Constantino L., Petronilho F., Vuolo F., Lacerda-Queiroz N., Rodrigues D.H., Da Rocha J.L., Teixeira A.L., de Quevedo J.L., et al. Traffic of leukocytes and cytokine up-regulation in the central nervous system in sepsis. Intensiv. Care Med. 2011;37:711–718. doi: 10.1007/s00134-011-2151-2. [DOI] [PubMed] [Google Scholar]
- 25.Gu M., Mei X.-L., Zhao Y.-N. Sepsis and Cerebral Dysfunction: BBB Damage, Neuroinflammation, Oxidative Stress, Apoptosis and Autophagy as Key Mediators and the Potential Therapeutic Approaches. Neurotox. Res. 2021;39:489–503. doi: 10.1007/s12640-020-00270-5. [DOI] [PubMed] [Google Scholar]
- 26.Andrades M., Morina A., Spasić S., Spasojević I. Bench-to-bedside review: Sepsis—From the redox point of view. Crit. Care. 2011;15:230. doi: 10.1186/cc10334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Delano M.J., Ward P.A. Sepsis-induced immune dysfunction: Can immune therapies reduce mortality? J. Clin. Invest. 2016;126:23–31. doi: 10.1172/JCI82224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kim K.S., Jekarl D.W., Yoo J., Lee S., Kim M., Kim Y. Immune gene expression networks in sepsis: A network biology approach. PLoS ONE. 2021;16:e0247669. doi: 10.1371/journal.pone.0247669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Catorce M.N., Gevorkian G. Evaluation of Anti-inflammatory Nutraceuticals in LPS-induced Mouse Neuroinflammation Model: An Update. Curr. Neuropharmacol. 2020;18:636–654. doi: 10.2174/1570159X18666200114125628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Xu X.-E., Liu L., Wang Y.-C., Wang C.-T., Zheng Q., Liu Q.-X., Li Z.-F., Bai X.-J., Liu X.-H. Caspase-1 inhibitor exerts brain-protective effects against sepsis-associated encephalopathy and cognitive impairments in a mouse model of sepsis. Brain Behav. Immun. 2019;80:859–870. doi: 10.1016/j.bbi.2019.05.038. [DOI] [PubMed] [Google Scholar]
- 31.Elmore J.P., McGee M.C., Nidetz N.F., Anannya O., Huang W., August A. Tuning T helper cell differentiation by ITK. Biochem. Soc. Trans. 2020;48:179–185. doi: 10.1042/BST20190486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Neuroimmune communication. Nat. Neurosci. 2017;20:127. doi: 10.1038/nn.4496. [DOI] [PubMed] [Google Scholar]
- 33.Zarbato G.F., de Souza Goldim M.P., Giustina A.D., Danielski L.G., Mathias K., Florentino D., de Oliveira Junior A.N., da Rosa N., Laurentino A.O., Trombetta T., et al. Dimethyl Fumarate Limits Neu-roinflammation and Oxidative Stress and Improves Cognitive Impairment After Polymicrobial Sepsis. Neurotox. Res. 2018;34:418–430. doi: 10.1007/s12640-018-9900-8. [DOI] [PubMed] [Google Scholar]
- 34.Hasegawa-Ishii S., Inaba M., Umegaki H., Unno K., Wakabayashi K., Shimada A. Endotoxemia-induced cytokine-mediated re-sponses of hippocampal astrocytes transmitted by cells of the brain-immune interface. Sci. Rep. 2016;6:25457. doi: 10.1038/srep25457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shi Y., Wei B., Li L., Wang B., Sun M. Th17 cells and inflammation in neurological disorders: Possible mechanisms of action. Front. Immunol. 2022;13:932152. doi: 10.3389/fimmu.2022.932152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shimada A., Hasegawa-Ishii S. Histological Architecture Underlying Brain–Immune Cell–Cell Interactions and the Cerebral Response to Systemic Inflammation. Front. Immunol. 2017;8:17. doi: 10.3389/fimmu.2017.00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nadeem A., Ahmad S.F., Al-Harbi N.O., Fardan A.S., El-Sherbeeny A.M., Ibrahim K.E., Attia S.M. IL-17A causes depression-like symptoms via NFκB and p38MAPK signaling pathways in mice: Implications for psoriasis associated depression. Cytokine. 2017;97:14–24. doi: 10.1016/j.cyto.2017.05.018. [DOI] [PubMed] [Google Scholar]
- 38.Guo K., Zhang X. Cytokines that Modulate the Differentiation of Th17 Cells in Autoimmune Uveitis. J. Immunol. Res. 2021;2021:6693542. doi: 10.1155/2021/6693542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Saito M., Fujinami Y., Ono Y., Ohyama S., Fujioka K., Yamashita K., Inoue S., Kotani J. Infiltrated regulatory T cells and Th2 cells in the brain contribute to attenuation of sepsis-associated encephalopathy and alleviation of mental impairments in mice with polymicrobial sepsis. Brain Behav. Immun. 2021;92:25–38. doi: 10.1016/j.bbi.2020.11.010. [DOI] [PubMed] [Google Scholar]
- 40.Ye B., Tao T., Zhao A., Wen L., He X., Liu Y., Fu Q., Mi W., Lou J. Blockade of IL-17A/IL-17R Pathway Protected Mice from Sep-sis-Associated Encephalopathy by Inhibition of Microglia Activation. Mediat. Inflamm. 2019;2019:8461725. doi: 10.1155/2019/8461725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nadeem A., Ahmad S.F., Al-Harbi N.O., Sarawi W., Attia S.M., Alanazi W.A., Ibrahim K.E., Alsanea S., Alqarni S.A. Acetyl-11-keto-β-boswellic acid improves clinical symptoms through modulation of Nrf2 and NF-κB pathways in SJL/J mouse model of experimental autoimmune encephalomyelitis. Int. Immunopharmacol. 2022;107:108703. doi: 10.1016/j.intimp.2022.108703. [DOI] [PubMed] [Google Scholar]
- 42.Beurel E., Lowell J.A. Th17 cells in depression. Brain Behav. Immun. 2018;69:28–34. doi: 10.1016/j.bbi.2017.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Andonegui G., Zelinski E.L., Schubert C.L., Knight D., Craig L.A., Winston B.W., Spanswick S.C., Petri B., Jenne C.N., Sutherland J.C., et al. Targeting inflammatory monocytes in sep-sis-associated encephalopathy and long-term cognitive impairment. JCI Insight. 2018;3:99364. doi: 10.1172/jci.insight.99364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Peng Z., Peng S., Lin K., Bin Zhao B., Wei L., Tuo Q., Liao D., Yuan T., Shi Z. Chronic stress-induced depression requires the recruitment of peripheral Th17 cells into the brain. J. Neuroinflammation. 2022;19:186. doi: 10.1186/s12974-022-02543-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Alhazzani K., Ahmad S.F., Al-Harbi N.O., Attia S.M., Bakheet S.A., Sarawi W., Alqarni S.A., Algahtani M., Nadeem A. Pharmacological Inhibition of STAT3 by Stattic Ameliorates Clinical Symptoms and Reduces Autoinflammation in Myeloid, Lymphoid, and Neuronal Tissue Compartments in Relapsing-Remitting Model of Experimental Autoimmune Encephalomyelitis in SJL/J Mice. Pharmaceutics. 2021;13:925. doi: 10.3390/pharmaceutics13070925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gomez-Rodriguez J., Wohlfert E.A., Handon R., Meylan F., Wu J.Z., Anderson S.M., Kirby M.R., Belkaid Y., Schwartzberg P.L. Itk-mediated integration of T cell receptor and cytokine signaling regulates the balance between Th17 and regulatory T cells. J. Exp. Med. 2014;211:529–543. doi: 10.1084/jem.20131459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jiang Q., Yang G., Liu Q., Wang S., Cui D. Function and Role of Regulatory T Cells in Rheumatoid Arthritis. Front. Immunol. 2021;12:626193. doi: 10.3389/fimmu.2021.626193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ahmed S.M.U., Luo L., Namani A., Wang X.J., Tang X. Nrf2 signaling pathway: Pivotal roles in inflammation. Biochim. Biophys. Acta Mol. Basis Dis. 2017;1863:585–597. doi: 10.1016/j.bbadis.2016.11.005. [DOI] [PubMed] [Google Scholar]
- 49.Li Y., Feng Y.-F., Liu X.-T., Li Y.-C., Zhu H.-M., Sun M.-R., Li P., Liu B., Yang H. Songorine promotes cardiac mitochondrial biogenesis via Nrf2 induction during sepsis. Redox Biol. 2021;38:101771. doi: 10.1016/j.redox.2020.101771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yu M., Li H., Liu Q., Liu F., Tang L., Li C., Yuan Y., Zhan Y., Xu W., Li W., et al. Nuclear factor p65 interacts with Keap1 to repress the Nrf2-ARE pathway. Cell. Signal. 2011;23:883–892. doi: 10.1016/j.cellsig.2011.01.014. [DOI] [PubMed] [Google Scholar]
- 51.Wardyn J.D., Ponsford A.H., Sanderson C.M. Dissecting molecular cross-talk between Nrf2 and NF-κB response pathways. Bio-Chem. Soc. Trans. 2015;43:621–626. doi: 10.1042/BST20150014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kong X., Thimmulappa R., Craciun F., Harvey C., Singh A., Kombairaju P., Reddy S.P., Remick D., Biswal S. Enhancing Nrf2 Pathway by Disruption of Keap1 in Myeloid Leukocytes Protects against Sepsis. Am. J. Respir. Crit. Care Med. 2011;184:928–938. doi: 10.1164/rccm.201102-0271OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kinsey S.G., Bailey M.T., Sheridan J.F., Padgett D.A., Avitsur R. Repeated social defeat causes increased anxiety-like behavior and alters splenocyte function in C57BL/6 and CD-1 mice. Brain Behav. Immun. 2007;21:458–466. doi: 10.1016/j.bbi.2006.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Al-Harbi N.O., Nadeem A., Ansari M.A., Al-Harbi M.M., Alotaibi M.R., AlSaad A.M., Ahmad S.F. Psoriasis-like inflammation leads to renal dysfunction via upregulation of NADPH oxidases and inducible nitric oxide synthase. Int. Immunopharmacol. 2017;46:1–8. doi: 10.1016/j.intimp.2017.02.018. [DOI] [PubMed] [Google Scholar]
- 55.Nadeem A., Al-Harbi N.O., Al-Harbi M.M., El-Sherbeeny A.M., Ahmad S.F., Siddiqui N., Ansari M.A., Zoheir K.M., Attia S.M., Al-Hosaini K.A., et al. Imiquimod-induced psoriasis-like skin inflammation is suppressed by BET bromodomain inhibitor in mice through RORC/IL-17A pathway modulation. Pharmacol. Res. 2015;99:248–257. doi: 10.1016/j.phrs.2015.06.001. [DOI] [PubMed] [Google Scholar]
- 56.Nadeem A., Chhabra S.K., Masood A., Raj H.G. Increased oxidative stress and altered levels of antioxidants in asthma. J. Allergy Clin. Immunol. 2003;111:72–78. doi: 10.1067/mai.2003.17. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data presented in this study are available on reasonable request from the corresponding author.