Background:
Persons living with diagnosed HIV (PLWDH) have higher COVID-19 diagnoses rates and poorer COVID-19–related outcomes than persons living without diagnosed HIV. The intersection of COVID-19 vaccination status and likelihood of severe COVID-19 outcomes has not been fully investigated for PLWDH.
Setting:
New York State (NYS).
Methods:
We matched HIV surveillance, immunization, and hospitalization databases to compare COVID-19 vaccination and COVID-19–related hospitalizations among PLWDH during B.1.617.2 (Delta) and B.1.1.529 (Omicron) predominance.
Results:
Through March 4, 2022, 69,137 of the 101,205 (68%) PLWDH were fully vaccinated or boosted for COVID-19. PLWDH who were virally suppressed or in care were more often to be fully vaccinated or boosted compared with PLWDH who were not virally suppressed (77% vs. 44%) or without evidence of care (74% vs. 33%). Overall hospitalization rates were lower among virally suppressed PLWDH. During Delta predominance, PLWDH with any vaccination history who were in care had lower hospitalization rates compared with those not in care; during Omicron predominance, this was the case only for boosted PLWDH.
Conclusions:
Approximately 28% (28,255) of PLWDH in NYS remained unvaccinated for COVID-19, a rate roughly double of that observed in the overall adult NYS population. PLWDH of color were more often than non-Hispanic White persons to be unvaccinated, as were the virally unsuppressed and those without evidence of HIV-related care, threatening to expand existing disparities in COVID-19–related outcomes. Vaccination was protective against COVID-19–related hospitalizations for PLWDH; however, differences in hospitalization rates between fully vaccinated and unvaccinated PLWDH were smaller than those among all New Yorkers.
Key Words: HIV, COVID-19, COVID-19 vaccines, vaccination coverage, hospitalization
INTRODUCTION
As of August 18, 2022, there have been more than 5.8 million cases of COVID-19 and more than 73,000 COVID-19–associated deaths in New York State (NYS).1 NYS ranks fourth in the United States in the number of cases of COVID-19 (as of January 6, 2023)2 and, at the end of 2020, ranked second in the number of persons living with diagnosed HIV (PLWDH) and first in the rate of HIV per 100,000 population, placing the state as an epicenter of both the US COVID-19 and HIV/AIDS epidemics.3 Approximately 83% of adults residing in NYS completed their COVID-19 vaccine series, and 45% were boosted as of March 7, 2022, though completion varied by demographics and region.4 Previous research has shown that COVID-19 vaccines remain effective against symptomatic infection and hospitalization across periods where the predominant SARS-CoV-2 variants included B.1.617.2 (Delta) and B.1.1.529 (Omicron) variants in NYS.5,6
There continues to be increasing evidence that COVID-19 vaccines are effective against severe outcomes. A multisite case–control study found that people who were hospitalized for COVID-19 were less likely to be vaccinated for COVID-19 (aOR 0.15, 95% CI: 0.13–0.18).7 Unvaccinated patients accounted for 94% of disease progression to death or invasive mechanical ventilation and 91% of deaths among patients with COVID-19. Recent studies found that hospitalization rates increased during Omicron circulation compared with those during Delta (38.4 vs. 15.5 per 100,000)8; however, COVID-19–related outcomes among hospitalized patients may have been worse during Delta circulation.9
Research suggests PLWDH may be at risk for more severe clinical outcomes of COVID-19 compared with persons who do not have HIV.10–16 PLWDH in NYS who were diagnosed with COVID-19 during March–June 2020 were more likely to be hospitalized compared with persons without diagnosed HIV.13 However, once hospitalized, mortality did not differ significantly between PLWDH and persons without diagnosed HIV.13,17 Nationally and in NYS, PLWDH were prioritized early for initial vaccine, booster, and additional doses; vaccines were available at no cost in NYS.18 However, our previous study demonstrates that early vaccination coverage among PLWDH through October 24, 2021 was lower than that of the general adult NYS population during the same time frame.19 Coverage was particularly low among PLWDH who were not virally suppressed or not in HIV care compared with PLWDH overall.
Many studies of COVID-19 breakthrough infections have focused on the general population,5–7,20 though a few have compared outcomes among patients with immunocompromised conditions, including HIV, before Omicron variant predominance. Immunocompromised patients had increased odds of COVID-19 breakthrough infections, severe COVID-19 breakthrough illness, and hospitalization.21–24 Two large cohort studies observed higher breakthrough infection rates among PLWDH compared with those among persons living without HIV and persons without immune dysfunction.23,25 In addition, a multisite case–control study found a weaker association between COVID-19 vaccination and a decreased risk of COVID-19 hospitalization in immunocompromised patients compared with that in immunocompetent patients, indicating potentially reduced vaccine effectiveness among immunocompromised persons generally.7 As new SARS-CoV-2 variants emerge, it is important to continue to assess the impact of the COVID-19 vaccination and different variants on immunocompromised persons and particularly, PLWDH. The purpose of this study was to update early vaccination coverage estimates19 among PLWDH in NYS and compare coverage with that of the adult NYS population to determine whether this coverage increased over time. In addition, we compared COVID-19–associated hospitalizations among PLWDH by vaccination status during periods of B.1.617.2 (Delta) and B.1.1.529 (Omicron) variant predominance in NYS.
METHODS
Data Sources
This is a retrospective cohort study of PLWDH aged 18 years or older who reside in NYS. This cohort was constructed based on matches of 4 surveillance databases: (1) NYS HIV surveillance registry, which is composed of name-based reports for all HIV-related laboratory tests among persons who reside or receive HIV-related care in NYS; (2) New York City (NYC) Citywide Immunization Registry (CIR), which collects data on COVID-19 vaccinations for persons who reside in NYC; (3) New York State Immunization Information System (NYSIIS), which collects vaccination data for persons residing in the rest of the state (ROS) with the exception of vaccinations reported directly to a federal system, such as for veterans, military personnel, or American Indian Health Program enrollees; and (4) Health Electronic Response Data System, which includes data on new hospital admissions of persons with laboratory-confirmed COVID-19 diagnoses through an electronic survey of all inpatient facilities in NYS.
The CIR and NYSIIS COVID-19 vaccination data were combined and deduplicated by first name, last name, date of birth, and zip code following previously reported methodology.20 The combined vaccination data (vaccinations through February 22, 2022) were matched with the NYS HIV surveillance registry (PLWDH through December 31, 2020) using a deterministic matching algorithm (matched on first name, last name, date of birth, and zip code) in SAS DataFlux. Data were matched to Health Electronic Response Data System using first and last initials, sex, date of birth, and zip code.
HIV surveillance registry data were used to compare demographic and HIV-related characteristics of PLWDH by vaccination status. Demographic characteristics included age at the end of 2020 (persons aged 18–49 years, 50–64 years, and 65 years or older), current gender (women, men, or nonconforming or nonbinary persons), race/ethnicity (non-Hispanic Black, non-Hispanic White, Asian/Pacific Islander, Hispanic, Multiracial, Native American, or unknown), and residence reported by the end of 2020 (NYC or ROS). HIV-related characteristics included viral suppression of <200 copies/mL at last test in 2020 and evidence of HIV care in 2020 (any CD4, viral load or genotype test reported to the NYS HIV surveillance registry in 2020). Consultation with the NYS Department of Health Institutional Review Board indicated that this work constitutes public health surveillance. We followed STROBE reporting guidelines.26
Study Cohorts
NYS implemented a phased approach to COVID-19 vaccination eligibility, prioritizing residents based on age, occupation, setting, and comorbidity, beginning in December 2020. On February 15, 2021,27 HIV became a qualifying condition for prioritized vaccination. PLWDH were categorized into 4 mutually exclusive closed exposure cohorts based on vaccination status during the period of interest: (1) an additional or booster dose beyond full vaccination of the Food and Drug Administration–authorized or approved Ad.26.COV2.S (Janssen [Johnson & Johnson]), BNT162b2 (Pfizer-BioNTech), or mRNA-1273 (Moderna); (2) full vaccination; (3) partial vaccination; or (4) having no matching vaccine record during the period of interest (unvaccinated). Booster dose was defined as ≥14 days since receipt of a dose of Pfizer-BioNTech or Moderna after prior full vaccination. Full vaccination was defined as ≥14 days since receipt of either a single dose of Johnson & Johnson or 2 doses of Pfizer-BioNTech or Moderna. Partial vaccination was defined as ≥14 days since receipt of only the first of a 2-dose series vaccine (Pfizer-BioNTech or Moderna) or <14 days since receipt of either a single dose of Johnson & Johnson or second dose of Pfizer-BioNTech or Moderna. Analyses did not differentiate between the type of vaccine received. However, there was a 99% agreement between the first and second vaccine types, and among PLWDH who received an additional or booster dose beyond full vaccination, there was an 88% agreement between the primary series type and additional booster type. PLWDH who were possible but not confirmed matches to the vaccination registries were excluded from analyses (n = 478).
To assess characteristics of PLWDH by COVID-19 vaccination status, cohorts included vaccination status for the entire study population as of March 4, 2022. To assess the outcome of COVID-19 hospitalizations among PLWDH during the period in which Delta variant prevalence was >50% (June 26, 2021–December 17, 2021 in Region 2), cohorts included vaccination status as of June 25, 2021.2 To assess COVID-19 hospitalizations among PLWDH during the period in which Omicron variant prevalence was >50% (December 18, 2021–February 24, 2022 in Region 2), cohorts included vaccination status as of December 17, 2021.
Statistical Analysis
The 4 vaccination status cohorts were analyzed by demographic groups for the entire study population, and separated into the 2 hospitalization time periods (Delta and Omicron) by calculating frequencies of the number of people in each vaccine cohort divided by the entire study population. Hospitalization rates were expressed as rates per 10,000 individuals by dividing the number of people with a hospitalization by the vaccine cohort population and multiplying by 10,000. All analyses were conducted using SAS software, version 9.4 (SAS Institute).
RESULTS
Vaccination Coverage
As of March 4, 2022, 39,655 (39%) of the 101,205 PLWDH included in the study received a booster dose, 29,482 (29%) were fully vaccinated without additional doses, 3813 (4%) received partial vaccination, and 28,255 (28%) were unvaccinated (Table 1).
TABLE 1.
Characteristics of Persons Living With Diagnosed HIV Infection in 2020 and COVID-19 Vaccination Status, New York, as of March 4, 2022*
| Received 1 Dose of Janssen Vaccine or 2 Doses of Pfizer-BioNTech or Moderna Vaccine, Additional Dose or Booster Dose | Received 1 Dose of Janssen Vaccine or 2 Doses of Pfizer-BioNTech or Moderna Vaccine | Received Only 1 Dose of Pfizer-BioNTech or Moderna Vaccine | Not Vaccinated | Total | |
| N (%) | No. (%) | No. (%) | No. (%) | No. | |
| Total | 39,655 (39) | 29,482 (29) | 3813 (4) | 28,255 (28) | 101,205 |
| Age† | |||||
| 18–49 yrs | 11,471 (27) | 14,138 (33) | 2109 (5) | 14,996 (35) | 42,714 |
| 50–64 yrs | 20,096 (46) | 11,945 (28) | 1314 (3) | 10,073 (23) | 43,428 |
| 65+ yr | 8088 (54) | 3399 (23) | 390 (3) | 3186 (21) | 15,063 |
| Current gender‡ | |||||
| Men | 29,408 (42) | 19,391 (27) | 2550 (4) | 19,287 (27) | 70,636 |
| NCNB | 29 (31) | 31 (33) | 1 (1) | 32 (34) | 93 |
| Women | 10,218 (34) | 10,060 (33) | 1262 (4) | 8936 (29) | 30,476 |
| Race/ethnicity | |||||
| Hispanic | 11,202 (39) | 8813 (30) | 1046 (4) | 8014 (28) | 29,075 |
| Non-Hispanic Black | 15,065 (33) | 14,672 (32) | 2083 (5) | 13,714 (30) | 45,534 |
| Asian/Pacific Islander | 1155 (46) | 646 (26) | 52 (2) | 666 (26) | 2519 |
| Multirace | 212 (36) | 167 (28) | 25 (4) | 186 (32) | 590 |
| Native American | 75 (39) | 54 (28) | 4 (2) | 57 (30) | 190 |
| Non-Hispanic White | 11,894 (51) | 5116 (22) | 599 (3) | 5599 (24) | 23,208 |
| Unknown | 52 (58) | 14 (16) | 4 (4) | 19 (21) | 89 |
| Residence in 2020§ | |||||
| New York City | 30,557 (38) | 23,401 (29) | 3117 (4) | 22,358 (28) | 79,433 |
| ROS | 9098 (42) | 6081 (28) | 696 (3) | 5897 (27) | 21,772 |
| Virally suppressed in 2020¦ | |||||
| No | 4799 (19) | 6263 (25) | 1326 (5) | 12,919 (51) | 25,307 |
| Yes | 34,856 (46) | 23,219 (31) | 2487 (3) | 15,336 (20) | 75,898 |
| In care in 2020¶ | |||||
| No | 2092 (15) | 2648 (18) | 489 (3) | 9186 (64) | 14,415 |
| Yes | 37,563 (43) | 26,834 (31) | 3324 (4) | 19,069 (22) | 86,790 |
Vaccination status determined based on status ≥14 days since receipt of most recent dose.
Age was determined as of the end of 2020.
Current gender was determined as of the end of 2020 based on gender reported to the New York State HIV surveillance registry.
Residency was determined as last known residence in 2020.
Viral suppression is defined as <200 HIV RNA copies/mL at the last viral load test reported to the New York State HIV surveillance registry in 2020.
HIV care was defined as any CD4, viral load, or genotype test reported to the New York State HIV surveillance registry in 2020.
NCNB, nonconforming or nonbinary.
Receipt of at least full vaccination (full vaccination with or without booster dose) increased with age, including 60% of PLWDH aged 18–49 years, 74% of PLWDH aged 50–64 years, and 76% of PLWDH aged 65 years or older (Table 1). Receipt of a booster dose varied even more, ranging from 27% of PLWDH aged 18–49 years to 54% of PLWDH aged 65 years or older. While the receipt of vaccine short of booster doses varied slightly by current gender, it varied more in the receipt of a booster dose, including 42% of male individuals, 34% of women, and 31% of nonconforming or nonbinary persons. Among persons with known race/ethnicity, the percent of PLWDH who received at least full vaccination was highest among non-Hispanic White (73%) and Asian/Pacific Islander (71%) and lowest among multiracial (64%) and non-Hispanic Black PLWDH (65%). Racial and ethnic differences were more pronounced in the receipt of a booster dose. Significantly more non-Hispanic White PLWDH received booster doses (51%) compared with all other racial and ethnic groups, with the largest disparities observed for multiracial (36%) and non-Hispanic Black PLWDH (33%). Full vaccination coverage (with or without booster dose) and booster dose coverage were slightly higher among residents in ROS (70% and 42%, respectively) compared with that among residents of NYC (68% and 38%, respectively).
Receipt of at least full vaccination and receipt of a booster dose were both substantially higher among PLWDH who were virally suppressed at the end of 2020 (77% and 46%, respectively) compared with PLWDH who were not virally suppressed (44% and 19%, respectively) (Table 1). Similarly, PLWDH who were in care at the end of 2020 were more often to be at least fully vaccinated (74%) and to have received a booster dose (43%) compared with PLWDH without evidence of care (33% at least fully vaccinated and 15% received a booster dose).
Hospitalizations During Delta Predominance (June 26, 2021–December 17, 2021)
Table 2 summarizes hospitalization rates among PLWDH by vaccination status during Delta predominance. There were a total of 162 COVID-19 hospitalizations among PLWDH between June 26, 2021 and December 17, 2021. Unvaccinated PLWDH had greater hospitalization rates (24/10,000) compared with those with partial (15/10,000) and full vaccination (10/10,000). Older PLWDH were more often to be hospitalized, with total hospitalization rates of 28/10,000 among PLWDH aged 65 years or older compared with 9/10,000 among PLWDH aged 18–49 years. The direct relationship between increasing age group and higher hospitalization rates was realized within each vaccination status.
TABLE 2.
COVID-19 Hospitalizations Among Persons Living With Diagnosed HIV Infection During Delta Predominance Period (June 26, 2021–December 17, 2021) by Vaccination Status*
| Received 1 Dose of Janssen Vaccine or 2 Doses of Pfizer-BioNTech or Moderna Vaccine | Received Only 1 Dose of Pfizer-BioNTech or Moderna Vaccine | Not Vaccinated | Total | |||||||||
| Persons | Hospitalizations | Persons | Hospitalizations | Persons | Hospitalizations | Persons | Hospitalizations | |||||
| No. | Rate per 10,000 | No. | Rate per 10,000 | No. | Rate per 10,000 | No. | Rate per 10,000 | |||||
| Total | 53,509 | 53 | 10 | 6088 | 9 | 15 | 41,608 | 100 | 24 | 101,205 | 162 | 16 |
| Age† | ||||||||||||
| 18–49 yrs | 17,524 | 6 | 3 | 2776 | 2 | 7 | 22,414 | 30 | 13 | 42,714 | 38 | 9 |
| 50–64 yrs | 25,927 | 31 | 12 | 2569 | 5 | 19 | 14,932 | 46 | 31 | 43,428 | 82 | 19 |
| 65+ yr | 10,058 | 16 | 16 | 743 | 2 | 27 | 4262 | 24 | 56 | 15,063 | 42 | 28 |
| Current gender‡ | ||||||||||||
| Men | 39,437 | 41 | 10 | 4025 | 4 | 10 | 27,174 | 44 | 16 | 70,636 | 89 | 13 |
| NCNB | 43 | 0 | 0 | 4 | 0 | 0 | 46 | 0 | 0 | 93 | 0 | 0 |
| Women | 14,029 | 12 | 9 | 2059 | 5 | 24 | 14,388 | 56 | 39 | 30,476 | 73 | 24 |
| Race/Ethnicity | ||||||||||||
| Hispanic | 15,755 | 16 | 10 | 1888 | 5 | 26 | 11,432 | 23 | 20 | 29,075 | 44 | 15 |
| Non-Hispanic Black | 20,694 | 22 | 11 | 2967 | 3 | 10 | 21,873 | 63 | 29 | 45,534 | 88 | 19 |
| Asian/Pacific Islander | 1530 | 1 | 7 | 131 | 0 | 0 | 858 | 0 | 0 | 2519 | 1 | 4 |
| Multirace | 300 | 2 | 67 | 39 | 1 | 256 | 251 | 1 | 40 | 590 | 4 | 68 |
| Native American | 102 | 0 | 0 | 10 | 0 | 0 | 78 | 0 | 0 | 190 | 0 | 0 |
| Non-Hispanic White | 15,069 | 12 | 8 | 1051 | 0 | 0 | 7088 | 13 | 18 | 23,208 | 25 | 11 |
| Unknown | 59 | 0 | 0 | 2 | 0 | 0 | 28 | 0 | 0 | 89 | 0 | 0 |
| Residence in 2020§ | ||||||||||||
| New York City | 41,102 | 31 | 8 | 4912 | 7 | 14 | 33,419 | 61 | 18 | 79,433 | 99 | 12 |
| ROS | 12,407 | 22 | 18 | 1176 | 2 | 17 | 8189 | 39 | 48 | 21,772 | 63 | 29 |
| Virally suppressed in 2020¦ | ||||||||||||
| No | 7160 | 15 | 21 | 1372 | 9 | 66 | 16,775 | 27 | 16 | 25,307 | 46 | 18 |
| Yes | 46,349 | 38 | 8 | 4716 | 0 | 0 | 24,833 | 73 | 29 | 75,898 | 116 | 15 |
| In care in 2020¶ | ||||||||||||
| No | 3142 | 7 | 22 | 511 | 1 | 20 | 10,762 | 10 | 9 | 14,415 | 18 | 12 |
| Yes | 50,367 | 46 | 9 | 5577 | 8 | 14 | 30,846 | 90 | 29 | 86,790 | 144 | 17 |
Vaccination status determined as of June 25, 2021, based on status ≥14 days since receipt of most recent dose.
Age was determined as of the end of 2020.
Current gender was determined as of the end of 2020 based on gender reported to the New York State HIV surveillance registry.
Residency was determined as last known residence in 2020.
Viral suppression is defined as <200 HIV RNA copies/mL at the last viral load test reported to the New York State HIV surveillance registry in 2020.
HIV care was defined as any CD4, viral load, or genotype test reported to the New York State HIV surveillance registry in 2020.
NCNB, nonconforming or nonbinary.
The overall hospitalization rate was nearly twice as high among women (24/10,000) than among men (13/10,000) (Table 2). This trend was contingent on vaccination status, occurring among PLWDH with either no or partial vaccination, but not among PLWDH achieving full vaccination. More than 80% of hospitalizations were among Hispanic (n = 44) and non-Hispanic Black (n = 88) PLWDH. Persons in these groups also exhibited higher hospitalization rates relative to non-Hispanic White PLWDH. The hospitalization rate varied by region and was significantly greater among PLWDH residing outside NYC (29/10,000) compared with those residing within NYC (12/10,000). This difference persisted within each category of vaccination status.
Those who were virally suppressed at the end of 2020 had lower hospitalization rates compared with PLWDH who were not virally suppressed, overall, and among those with any vaccination history. (Table 2). However, among unvaccinated PLWDH, those who were virally suppressed had higher hospitalization rates (29/10,000) compared with unsuppressed and unvaccinated PLWDH (16/10,000).
PLWDH who were in care at the end of 2020 had higher hospitalization rates (17/10,000) compared with PLWDH who were not in care at the end of 2020 (12/10,000) (Table 2). This overall trend was driven among the unvaccinated PLWDH, where the hospitalization rates among those in care (29/10,000) and not in care (9/10,000) differed the greatest. Fully vaccinated and partially vaccinated PLWDH who were in care had lower hospitalization rates (9/10,000 and 14/10,000, respectively) compared with those not in care (22/10,000 among fully vaccinated and 20/10,000 among partially vaccinated).
Hospitalizations During Omicron Predominance (December 18, 2021–February 24, 2022)
Table 3 summarizes hospitalization rates among PLWDH by vaccination status during Omicron predominance. Between December 18, 2021, and February 24, 2022, there were a total of 425 hospitalizations among PLWDH, for an overall hospitalization rate of 42/10,000. This rate was nearly 3 times that observed during Delta predominance (16/10,000). The lowest overall rates were among boosted PLWDH (25/10,000); however, the highest were observed among partially vaccinated PLWDH (77/10,000) rather than the unvaccinated (52/10,000) (Fig. 1). There were similar trends in hospitalizations by age, gender, and race/ethnicity in both Delta and Omicron predominance periods. One exception was that among partially vaccinated PLWDH, the highest hospitalization rates during Omicron predominance were among PLWDH aged 50–64 years (124/10,000). Hospitalization rates were more similar between PLWDH outside NYC (45/10,000) and PLWDH in NYC (41/10,000) during Omicron than Delta predominance period.
TABLE 3.
COVID-19 Hospitalizations Among Persons Living With Diagnosed HIV Infection During Omicron Predominance Period (December 18, 2021–February 24, 2022) by Vaccination Status*
| Received 1 Dose of Janssen Vaccine or 2 Doses of Pfizer-BioNTech or Moderna Vaccine, Additional Dose or Booster Dose | Received 1 Dose of Janssen Vaccine or 2 Doses of Pfizer-BioNTech or Moderna Vaccine | Received Only 1 Dose of Pfizer-BioNTech or Moderna Vaccine | Not Vaccinated | Total | |||||||||||
| Persons | Hospitalizations | Persons | Hospitalizations | Persons | Hospitalizations | Persons | Hospitalizations | Persons | Hospitalizations | ||||||
| n | Rate per 10,000 | N | Rate per 10,000 | n | Rate per 10,000 | n | Rate per 10,000 | n | Rate per 10,000 | ||||||
| Total | 27,285 | 69 | 25 | 39,516 | 167 | 42 | 4432 | 34 | 77 | 29,972 | 155 | 52 | 101,205 | 425 | 42 |
| Age, yr† | |||||||||||||||
| 18–49 | 6794 | 14 | 21 | 17,460 | 24 | 14 | 2441 | 11 | 45 | 16,019 | 51 | 32 | 42,714 | 100 | 23 |
| 50–64 | 14,045 | 30 | 21 | 17,178 | 95 | 55 | 1538 | 19 | 124 | 10,667 | 75 | 70 | 43,428 | 219 | 50 |
| 65+ | 6446 | 25 | 39 | 4878 | 48 | 98 | 453 | 4 | 88 | 3286 | 29 | 88 | 15,063 | 106 | 70 |
| Current gender‡ | |||||||||||||||
| Men | 21,108 | 53 | 25 | 26,302 | 88 | 33 | 2920 | 22 | 75 | 20,306 | 89 | 44 | 70,636 | 252 | 36 |
| NCNB | 17 | 0 | 0 | 36 | 0 | 0 | 5 | 0 | 0 | 35 | 0 | 0 | 93 | 0 | 0 |
| Women | 6160 | 16 | 26 | 13,178 | 79 | 60 | 1507 | 12 | 80 | 9631 | 66 | 69 | 30,476 | 173 | 57 |
| Race/Ethnicity | |||||||||||||||
| Hispanic | 7404 | 22 | 30 | 12,057 | 42 | 35 | 1171 | 10 | 85 | 8443 | 35 | 41 | 29,075 | 109 | 37 |
| Non-Hispanic Black | 9434 | 36 | 38 | 18,873 | 93 | 49 | 2437 | 17 | 70 | 14,790 | 92 | 62 | 45,534 | 238 | 52 |
| Asian/Pacific Islander | 783 | 3 | 38 | 979 | 1 | 10 | 68 | 1 | 147 | 689 | 0 | 0 | 2519 | 5 | 20 |
| Multirace | 137 | 0 | 0 | 229 | 1 | 44 | 27 | 0 | 0 | 197 | 3 | 152 | 590 | 4 | 68 |
| Native American | 50 | 0 | 0 | 72 | 2 | 278 | 5 | 0 | 0 | 63 | 0 | 0 | 190 | 2 | 105 |
| Non-Hispanic White | 9435 | 8 | 8 | 7284 | 28 | 38 | 719 | 6 | 83 | 5770 | 25 | 43 | 23,208 | 67 | 29 |
| Unknown | 42 | 0 | 0 | 22 | 0 | 0 | 5 | 0 | 0 | 20 | 0 | 0 | 89 | 0 | 0 |
| Residence in 2020§ | |||||||||||||||
| New York City | 21,029 | 57 | 27 | 31,035 | 130 | 42 | 3611 | 23 | 64 | 23,758 | 116 | 49 | 79,433 | 326 | 41 |
| ROS | 6256 | 12 | 19 | 8481 | 37 | 44 | 821 | 11 | 134 | 6214 | 39 | 63 | 21,772 | 99 | 45 |
| Virally suppressed in 2020¦ | |||||||||||||||
| No | 3014 | 13 | 43 | 7369 | 46 | 62 | 1459 | 16 | 110 | 13,465 | 61 | 45 | 25,307 | 136 | 54 |
| Yes | 24,271 | 56 | 23 | 32,147 | 121 | 38 | 2973 | 18 | 61 | 16,507 | 94 | 57 | 75,898 | 289 | 38 |
| In care¶ | |||||||||||||||
| No | 1341 | 4 | 30 | 3109 | 7 | 23 | 546 | 3 | 55 | 9419 | 13 | 14 | 14,415 | 27 | 19 |
| Yes | 25,944 | 65 | 25 | 36,407 | 160 | 44 | 3886 | 31 | 80 | 20,553 | 142 | 69 | 86,790 | 398 | 46 |
Vaccination status determined as of December 17, 2021, based on status ≥14 days since receipt of most recent dose.
Age was determined as of the end of 2020.
Current gender was determined as of the end of 2020 based on gender reported to the New York State HIV surveillance registry.
Residency was determined as last known residence in 2020.
Viral suppression is defined as <200 HIV RNA copies/mL at the last viral load test reported to the New York State HIV surveillance registry in 2020.
HIV care was defined as any CD4, viral load, or genotype test reported to the New York State HIV surveillance registry in 2020.
NCNB, nonconforming or nonbinary.
FIGURE 1.
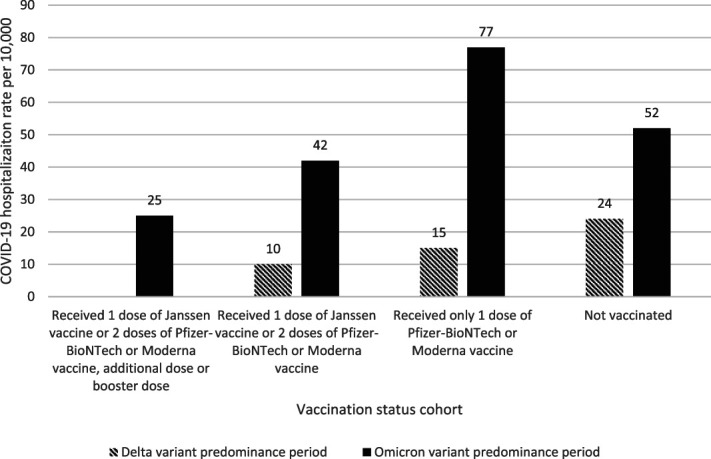
COVID-19 hospitalization rates among infection during Deltaa and Omicronb predominance periods by vaccination status. aDelta variant predominance period (June 26, 2021–December 17, 2021). bOmicron variant predominance period (December 18, 2021–February 24, 2022). cVaccination status cohorts varied based on COVID-19 variant predominance period. Vaccination status cohorts during Delta variant predominance period was defined by vaccination status determined as of June 25, 2021, based on status ≥14 days since receipt of most recent dose. Vaccination status cohorts during Omicron variant predominance period was defined by vaccination status determined as of December 17, 2021, based on status ≥14 days since receipt of most recent dose.
PLWDH who were virally suppressed had lower hospitalization rates (38/10,000) compared with PLWDH who were not virally suppressed (54/10,000) (Table 3). Similarly, PLWDH who were boosted, fully vaccinated, and partially vaccinated had lower hospitalization rates if they were virally suppressed. Unvaccinated PLWDH who were virally suppressed had higher hospitalization rates (57/10,000) compared with unvaccinated PLWDH who were not virally suppressed (45/10,000). Overall and among nonboosted cohorts, PLWDH who were in care had higher hospitalization rates compared with PLWDH who were not in care. However, boosted PLWDH who were in care had slightly lower hospitalization rates (25/10,000) compared with PLWDH who were not in care (30/10,000).
DISCUSSION
COVID-19 vaccination coverage among PLWDH in NYS increased only 5 percentage points since October 24, 2021.19 Although there were modest declines in the percentage of PLWDH who were unvaccinated in every race/ethnicity category, previously reported disparities still exist and at similar levels. One exception was a slightly greater improvement (6%) in vaccination coverage among non-Hispanic Black PLWDH compared with non-Hispanic White (2%) and Hispanic (2%) PLWDH. More than 25% of PLWDH remain unvaccinated, and PLWDH still had lower full vaccination coverage (68%) compared with the general adult population (83%) as of March 7, 2022.1 Differences in the demographic composition of PLWDH compared with the general NYS population might account for some of this lower coverage; however, coverage was lower than 83% across all PLWDH categories, as listed in Table 1. Socioeconomic status and other unmeasured variables might help to further explain coverage differences between PLWDH and the overall NYS population.
In both the Delta and Omicron predominance periods, the hospitalization rates among PLWDH increased by age and were also higher for women and persons of color, excepting Asian/Pacific Islander adults during Delta predominance period. These age and racial/ethnic disparities are consistent with higher hospitalizations among older adults and persons of color in the general population.8,28 Disparities may be explained by uncontrolled variables such as social determinants. As expected, hospitalization rates in both periods were lowest among fully vaccinated PLWDH. Hospitalization rates increased between Delta and Omicron for all groups except multiracial PLWDH.
One important finding from this study concerns the much smaller difference in hospitalization rates between fully vaccinated (with or without booster dose) and unvaccinated PLWDH compared with those in all New Yorkers. In the overall NYS population, unvaccinated persons had hospitalization rates approximately 10 times higher than fully vaccinated persons in both the Delta (10.9) and Omicron (9.6) predominance periods.1 Among PLWDH in our study, unvaccinated persons had hospitalization rates approximately 2 times higher than those fully vaccinated during Delta (2.4) and Omicron (1.5) predominance periods. Of importance, this difference is being driven by higher hospitalization rates among vaccinated PLWDH. For example, during Omicron predominance period, hospitalization rates among unvaccinated PLWDH (52/10,000) were somewhat higher than those among all unvaccinated New Yorkers (29/10,000); however, rates among fully vaccinated PLWDH (35/10,000) were more than 10 times greater than rates among all fully vaccinated New Yorkers (3/10,000). Time since vaccination between PLWDH and all New Yorkers may differ; however, results support previous findings of greater COVID-19 hospitalizations among PLWDH,13,21–23 and vaccination may have reduced protective effects against hospitalization among immunocompromised populations compared with the general population.7
During Delta predominance, PLWDH with at least some vaccination history who were in care had lower hospitalization rates compared with those not in care. However, during Omicron predominance, only boosted PLWDH in care had lower hospitalization rates compared with those out of care. PLWDH who are in care may be more engaged in healthcare services and may be more likely to access the hospital than those not in care. In addition, PLWDH have a high prevalence of comorbidities that increase the risk of severe COVID-19 infection,29–33 so it is plausible that PLWDH with comorbidities may be more engaged in the healthcare system in general and thus more likely to have access to hospitalization. This study did not assess COVID-19 diagnoses among all PLWDH, so we are unable to determine the extent to which SARS-CoV-2 infection varied by vaccination status. However, it is likely that COVID-19 diagnoses among PLWDH were greater during the Omicron predominance period, similar to reports of increased COVID-19 incidence nationally,34 which contributed to increased hospitalization rates during this period.
Addressing the expansive gap in vaccination coverage by HIV care and viral suppression status is critical, given the increased risk and/or prevalence of severe COVID-19 outcomes among immunocompromised persons, including PLWDH,10–16,21–23,25 and CDC recommendations for these persons to stay up to date with COVID-19 vaccines.35 However, there is limited research on effective interventions to increase vaccination coverage among PLWDH or members of the general population who remain unvaccinated. Reminder notifications can address scheduling-related barriers, resulting in increased appointment and vaccination rates.36 Disparities in COVID-19 vaccination coverage among PLWDH may be reduced by incorporating COVID-19 vaccination into existing HIV programming and services.19 For example, HIV providers can be leveraged to promote vaccination and subsequent booster and additional shots, as relevant, and promoting vaccination could be incorporated into existing HIV and STI partner services activities, such as Data to Care.37
LIMITATIONS
Vaccination status was limited to reports to NYSIIS and CIR during this study. PLWDH were categorized as unvaccinated when there was an absence of a matching vaccination record during matching. This may include PLWDH who were vaccinated outside of NYS and not reported to NYSIIS or CIR, PLWDH who were unmatched during matching, or PLWDH who died after December 31, 2020. Death data were available only through December 2020; thus, deaths reported in previous years in NYS, including 2020, were used to estimate the number of PLWDH aged 18 years or older who were alive as of March 4, 2022. This analysis likely includes 2000 PLWDH who died during 2021 and early 2022; these decedents may have died before they were able to begin or complete vaccination, which may have resulted in a slight misclassification of vaccination status.
CONCLUSIONS
Fifteen months after vaccines became available, more than 25% of PLWDH in NYS remained unvaccinated for COVID-19. Differences in vaccination status were most pronounced within categories of race/ethnicity, viral suppression, and HIV care status. Lower vaccination rates among non-Hispanic Black and Hispanic PLWDH could magnify already higher diagnosis rates and more severe COVID-19 outcomes experienced in these communities.28,38 More research is needed to understand why PLWDH are less likely to be vaccinated for COVID-19, and why PLWDH, particularly vaccinated PLWDH, have significantly higher hospitalizations rates compared with those in New Yorkers overall.
Footnotes
N.A. is supported by the Fogarty International Center and the National Institute of Alcohol Abuse and Alcoholism of the National Institutes of Health under Award Number D43 TW011532.
The authors have no conflicts of interest to disclose.
Contributor Information
Wendy Patterson, Email: wendy.patterson@health.ny.gov.
Joyce Chicoine, Email: joyce.chicoine@health.ny.gov.
Vajeera Dorabawila, Email: Vajeera.Dorabawila@health.ny.gov.
Natalia Adamashvili, Email: natalia.adamashvili@gmail.com.
Deepa T. Rajulu, Email: deepa.rajulu@health.ny.gov.
Eli S. Rosenberg, Email: eli.rosenberg@health.ny.gov.
James M. Tesoriero, Email: james.tesoriero@health.ny.gov.
REFERENCES
- 1.New York State Department of Health. COVID-19 data in New York. https://coronavirus.health.ny.gov/covid-19-data-new-york. Accessed April 28, 2022.
- 2.Centers for Disease Control and Prevention. COVID data tracker. US department of health and human services, CDC. https://covid.cdc.gov/covid-data-tracker. Accessed January 6, 2023.
- 3.Centers for Disease Control and Prevention. HIV surveillance report, 2020. Vol 33; 2022. https://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Accessed January 6, 2023. [Google Scholar]
- 4.New York State Department of Health. Vaccination progress to date. https://coronavirus.health.ny.gov/vaccination-progress-date. Accessed August 4, 2022.
- 5.Leon TM, Dorabawila V, Nelson L, et al. COVID-19 cases and hospitalizations by COVID-19 vaccination status and previous COVID-19 diagnosis - California and New York, May-November 2021. MMWR Morb Mortal Wkly Rep. 2022;71:125–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rosenberg ES, Holtgrave DR, Dorabawila V, et al. New COVID-19 cases and hospitalizations among adults, by vaccination status - New York, May 3-July 25, 2021. MMWR Morb Mortal Wkly Rep. 2021;70:1306–1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tenforde MW, Self WH, Adams K, et al. Association between mRNA vaccination and COVID-19 hospitalization and disease severity. JAMA 2021;23326:2043–2054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Taylor CA, Whitaker M, Anglin O, et al. COVID-19-Associated hospitalizations among adults during SARS-CoV-2 Delta and Omicron variant predominance, by race/ethnicity and vaccination status - COVID-NET, 14 states, July 2021-January 2022. MMWR Morb Mortal Wkly Rep. 2022;71:466–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Modes ME, Directo MP, Melgar M, et al. Clinical characteristics and outcomes among adults hospitalized with laboratory-confirmed SARS-CoV-2 infection during periods of B.1.617.2 (Delta) and B.1.1.529 (Omicron) variant predominance - one hospital, California, July 15-September 23, 2021, and December 21, 2021-January 27, 2022. MMWR Morb Mortal Wkly Rep. 2022;71:217–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bhaskaran K, Rentsch CT, MacKenna B, et al. HIV infection and COVID-19 death: a population-based cohort analysis of UK primary care data and linked national death registrations within the OpenSAFELY platform. Lancet HIV 2021;8:e24–e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Braunstein SL, Lazar R, Wahnich A, et al. . Coronavirus disease 2019 (COVID-19) infection among people with human immunodeficiency virus in New York city: a population-level analysis of linked surveillance data. Clin Infect Dis. 2020;72:e1021–e1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Geretti AM, Stockdale AJ, Kelly SH, et al. Outcomes of coronavirus disease 2019 (COVID-19) related hospitalization among people with human immunodeficiency virus (HIV) in the ISARIC world health organization (WHO) clinical characterization protocol (UK): a prospective observational study. Clin Infect Dis. 2020;73:e2095–e2106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tesoriero JM, Swain CAE, Pierce JL, et al. COVID-19 outcomes among persons living with or without diagnosed HIV infection in New York state. JAMA Netw Open 2021;4:e2037069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Boulle A, Davies MA, Hussey H, et al. Risk factors for coronavirus disease 2019 (COVID-19) death in a population cohort study from the western cape province, South Africa. Clin Infect Dis. 2021;73:e2005–e2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Health Organization. Clinical Features and Prognostic Factors of COVID-19 in People Living with HIV Hospitalized with Suspected or Confirmed SARS-CoV-2 Infection; 2021:2021. https://www.who.int/publications/i/item/WHO-2019-nCoV-Clinical-HIV-2021.1 [Google Scholar]
- 16.Yang X, Sun J, Patel RC, et al. Associations between HIV infection and clinical spectrum of COVID-19: a population level analysis based on US National COVID Cohort Collaborative (N3C) data. Lancet HIV 2021;8:e690–e700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rosenthal EM, Rosenberg ES, Patterson W, et al. Factors associated with SARS-CoV-2-related hospital outcomes among and between persons living with and without diagnosed HIV infection in New York State. PLoS One 2022;17:e0268978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.New York State Department of Health. Covid-19 vaccine: frequently asked questions. https://covid19vaccine.health.ny.gov/frequently-asked-questions-0. Accessed January 6, 2023.
- 19.Tesoriero JM, Patterson W, Daskalakis D, et al. Notes from the field: COVID-19 vaccination among persons living with diagnosed HIV infection - New York, October 2021. MMWR Morb Mortal Wkly Rep. 2022;71:182–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rosenberg ES, Dorabawila V, Easton D, et al. Covid-19 vaccine effectiveness in New York state. N Engl J Med. 2022;386:116–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Di Fusco M, Moran MM, Cane A, et al. Evaluation of COVID-19 vaccine breakthrough infections among immunocompromised patients fully vaccinated with BNT162b2. J Med Econ. 2021;24:1248–1260. [DOI] [PubMed] [Google Scholar]
- 22.Suleyman G, Fadel R, Brar I, et al. Risk factors associated with hospitalization and death in COVID-19 breakthrough infections. Open Forum Infect Dis. 2022;9:ofac116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Coburn SB, Humes E, Lang R, et al. Analysis of postvaccination breakthrough COVID-19 infections among adults with HIV in the United States. JAMA Netw Open 2022;5:e2215934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lang R, Humes E, Coburn SB, et al. Analysis of severe illness after postvaccination COVID-19 breakthrough among adults with and without HIV in the US. JAMA Netw Open 2022;5:e2236397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sun J, Zheng Q, Madhira V, et al. Association between immune dysfunction and COVID-19 breakthrough infection after SARS-CoV-2 vaccination in the US. JAMA Intern Med. 2022;182:153–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147:573–577. [DOI] [PubMed] [Google Scholar]
- 27.gov NY. Governor Cuomo Announces List of Comorbidities and Underlying Conditions Eligible for COVID-19 Vaccine Starting February 15. Updated February 5, 2021.https://www.governor.ny.gov/news/governor-cuomo-announces-list-comorbidities-and-underlying-conditions-eligible-covid-19-vaccine. Accessed May 25, 2022. [Google Scholar]
- 28.Price-Haywood EG, Burton J, Fort D, Seoane L. Hospitalization and mortality among Black patients and white patients with covid-19. N Engl J Med. 2020;382:2534–2543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sigel K, Swartz T, Golden E, et al. Coronavirus 2019 and people living with human immunodeficiency virus: outcomes for hospitalized patients in New York city. Clin Infect Dis. 2020;1271:2933–2938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Meyerowitz EA, Kim AY, Ard KL, et al. Disproportionate burden of coronavirus disease 2019 among racial minorities and those in congregate settings among a large cohort of people with HIV. AIDS 2020;1034:1781–1787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kamis KF, Barbera L, Abdo M, et al. Risk factors for hospitalization in people with HIV and COVID-19. JAIDS 2021;88:e22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kalichman SC, Eaton LA, Berman M, et al. Intersecting pandemics: impact of SARS-CoV-2 (COVID-19) protective behaviors on people living with HIV, Atlanta, Georgia. JAIDS 2020;85:66–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ambrosioni J, Blanco JL, Reyes-Urueña JM, et al. Overview of SARS-CoV-2 infection in adults living with HIV. Lancet HIV 2021;8:e294–e305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Johnson AG, Amin AB, Ali AR, et al. COVID-19 incidence and death rates among unvaccinated and fully vaccinated adults with and without booster doses during periods of Delta and Omicron variant emergence - 25 U.S. Jurisdictions, April 4-december 25, 2021. MMWR Morb Mortal Wkly Rep 2022;71:132–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Centers for Disease Control and Prevention. People with Certain Medical Conditions. Updated May 2, 2022.https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. Accessed May 25, 2022. [Google Scholar]
- 36.Dai H, Saccardo S, Han MA, et al. Behavioural nudges increase COVID-19 vaccinations. Nature 2021;597:404–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Centers for Disease Control and Prevention. Data to care. https://www.cdc.gov/hiv/effective-interventions/treat/data-to-care/index.html?Sort=Title%3A%3Aasc&Intervention%20Name=Data%20to%20CareName%3DData%20to%20Care. Accessed July 22, 2022.
- 38.Holtgrave DR, Barranco MA, Tesoriero JM, et al. . Assessing racial and ethnic disparities using a COVID-19 outcomes continuum for New York State. Ann Epidemiol. 2020;48:9–14. [DOI] [PMC free article] [PubMed] [Google Scholar]


