Abstract
Purpose
Social distancing and strict visitor restrictions at hospitals have been national policies since the onset of the coronavirus disease 2019 (COVID-19) pandemic. This has challenged the concept of a good death in comfort with the opportunity to say goodbye. Little is known about how these measures have influenced end-of-life (EOL) care among cancer patients who die in acute care hospitals. This study examined changes in the EOL care of cancer patients during the COVID-19 pandemic.
Methods
We retrospectively analyzed 1,456 adult cancer patients who died in 2019 (n=752) and 2020 (n=704) at a tertiary hospital. Data on EOL care—symptom control and comfort care in an imminently dying state, preparation for death, place of death, and aggressive care in the last month—were reviewed.
Results
The 1,456 patients had a median age of 67 years, and 62.5% were men. Patients who died in 2020 were more likely to experience agitation or delirium before death (17.2% vs. 10.9%), to use inotropes/vasopressors near death (59.2% vs. 52.3%), and to receive cardiopulmonary resuscitation in their last months (16.3% vs. 12.5%) than those who died in 2019. Additionally, the number of deaths in the emergency room doubled in 2020 compared to 2019 (from 7.1% to 14.1%).
Conclusion
This study suggests that EOL care for cancer patients who died in a tertiary hospital deteriorated during the COVID-19 pandemic. The implementation of medical care at the EOL and the preferred place of death should be discussed carefully in advance for high-quality EOL care.
Keywords: COVID-19, Pandemics, Terminal care, Neoplasms, Hospitals
INTRODUCTION
The coronavirus disease 2019 (COVID-19) pandemic has caused global excess mortality [1]. In addition to quantitative changes, social distancing and hospital policies such as visitor restrictions have left seriously ill patients isolated, even during the end of life (EOL) [2], leading to qualitative changes in EOL care. This problem is not entirely specific to the COVID-19 pandemic, as healthcare systems have been radically overwhelmed in previous epidemics and pandemics of severe acute respiratory syndrome, Ebola virus, and human influenza virus [3,4]. During these events, people face severe challenges, including difficulty in accessing care services, isolation, disrupted connectedness and dehumanization of care, and barriers to EOL care discussions [4,5]. Meanwhile, the role of high-quality palliative and EOL care has been emphasized in response to the pandemic crisis [4,6].
Cancer patients constitute a vulnerable population during a pandemic because they are both at high risk of infection and affected by the disruption of continuity of cancer care [7]. During the EOL, they often discuss their preferred place of care or death, as well as their preferences for medical care near the EOL, via advance care planning. Cancer patients can also use hospice and palliative care services when approaching their terminal state. However, most cancer patients still die in non-hospice facilities, such as acute care hospitals, as the hospice enrollment rate of cancer patients in Korea was only 23% in 2020 [8].
Recent studies have reported that during the COVID-19 pandemic, patients have tended to be admitted to the inpatient hospice ward less or with very late timing [9,10]. People also tended to die home more frequently during the pandemic than before [11]. However, limited research has investigated the impact of the COVID-19 pandemic on EOL care, especially regarding symptom management and the receipt of medical procedures at the EOL for cancer patients in hospital settings. The specific site of in-hospital death for cancer patients who die in hospitals is also of interest. Therefore, this study examined the changes in EOL care during the COVID-19 pandemic for patients with cancer who died in an acute care-based tertiary hospital.
METHODS
1. Design
We performed a single-center, retrospective cohort study to compare EOL care regarding symptom control and comfort care in an imminently dying state, preparation for death, place of death, and aggressive care in the last months between the pre-COVID-19 and during-COVID-19 periods in patients with cancer who died in an acute care-based tertiary hospital.
2. Subjects
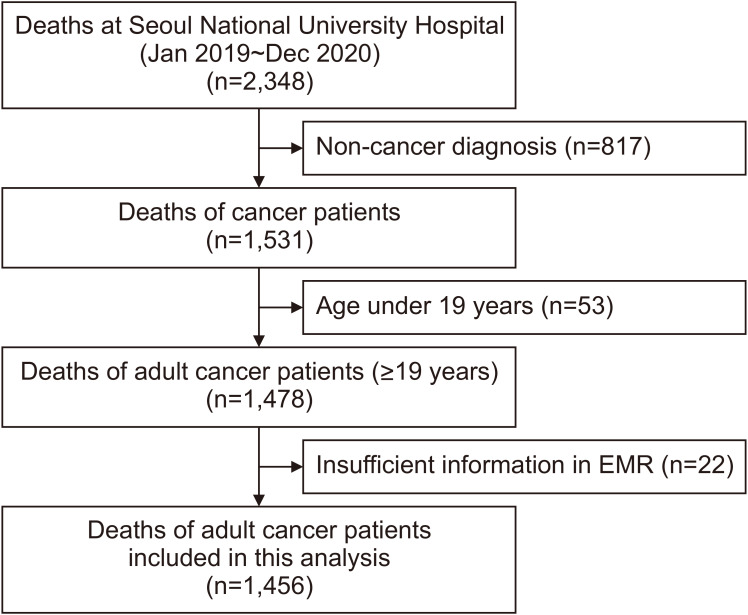
The subjects of this study were adult cancer patients who died at Seoul National University Hospital between January 1, 2019, and December 31, 2020. The palliative care services at this tertiary hospital comprise an outpatient palliative care clinic and an inpatient consultation-based palliative care team; however, there is no inpatient hospice-palliative care unit. A cancer patient was defined as a patient with a confirmed diagnosis as per the International Classification of Diseases, 10th Revision codes (C00-90, D45–D48), visited outpatient clinics three or more times, or visited the emergency room (ER), or was hospitalized more than once. Among the 1,531 cancer patients who died during these periods, 1,456 patients were finally included in the analysis after we excluded the records of 53 patients younger than 19 years of age and 22 patients with insufficient information about their cancer diagnosis and treatment in the electronic medical records: 752 (51.6%) in 2019 and 704 (48.4%) in 2020 (Figure 1).
Figure 1.
Enrollment of study participants.
3. Tools
We defined 2019 as the “pre-COVID-19 period” and 2020 as the “during-COVID-19 period.” A literature review of factors that are considered to be important at the EOL was performed [12,13]. Among the significant items (e.g., symptom management, communication, and relationships with loved ones), we chose items that could be retrospectively reviewed from medical records and organized the following four domains to assess EOL care: symptom control and comfort care in an imminently dying state, preparation for death, place of death, and aggressive care in the last month.
Symptom control and comfort care in an imminently dying state included managing the patient’s discomfort (pain [a numeric rating scale of 5 points or higher] resting dyspnea, and agitation or delirium) and medical procedures (laboratory tests, imaging tests, continuous monitoring of vital signs, inotrope or vasopressor use, and transfusion) in an imminently dying state. As the patients who die in the ER usually have shorter stays than those in the general ward (GW) or intensive care unit (ICU), we investigated the discomfort and medical procedures within 24 hours before death for the former and within 72 hours before death for the latter. Distressing symptoms were assessed as positive when they persisted for two consecutive days based on the daily medical and nursing assessment records.
The second domain, preparation for death, included consultation with the inpatient palliative care team and the presence of an advance statement. In Korea, since the enforcement of the Life-Sustaining Treatment Decisions Act in February 2018 [14], advance directives (form 6) or a life-sustaining treatment plan (form 1) can be acknowledged as a legal document for a patient’s advance statement.
The place of death included the location of death in the hospital (GW, ICU, or ER) and death in a single-patient room. Finally, regarding aggressive care in the last month of life, we assessed the receipt of cardiopulmonary resuscitation, mechanical ventilation, renal replacement therapy, ICU admission, ER visits, and the last dose of chemotherapy in the last month before death.
4. Data collection
The study protocol was reviewed and approved by the institutional review board of the Seoul National University Hospital (no. H-2010-121-1166). The study was conducted in accordance with the Principles of the Declaration of Helsinki. The requirement for informed consent was waived for all participants in the study due to its retrospective nature.
We obtained clinical data on patients’ final admission or hospital visit by reviewing the electronic medical records and using the data retrieval system of the Seoul National University Hospital. The database of the National Agency for Management of Life-Sustaining Treatment was used to identify the presence of advance directives or a life-sustaining treatment plan [14,15].
5. Data analysis
For this study, we used descriptive data, such as the median and range of values and the number of patients (expressed as a percentage) to illustrate the demographics and clinical characteristics of the patients. To compare data between 2019 and 2020, we applied the Student t-test for continuous variables and the chi-square test for categorical variables. The Mann–Whitney U test and the Fisher exact test were performed as non-parametric tests for continuous and categorical variables, respectively. A subgroup analysis of the death site was performed. Statistical significance was set at P<0.05. Statistical analyses were performed using STATA ver. 12.0 (StataCorp LP, College Station, TX, USA).
RESULTS
Table 1 shows the sociodemographic and clinical characteristics of the patients with cancer who died in 2019 and 2020. The median age was 67 years (range, 59~75 years), and 62.5% of the patients were men. The top three cancer types were hepatobiliary-pancreatic cancer (30.7%), lung and intrathoracic cancer (17.8%), and hematologic neoplasms (17.3%). Among the patients, the number of foreigners without insurance significantly decreased in 2020 compared to 2019. Most of the participants had recurrent or metastatic disease (80.4%) and were treated in the medical department (71.8%); both of these percentages decreased significantly in 2020 compared to 2019. The median length of hospital stay was 13 days (interquartile range, 4~28 days) in all patients, which remained constant between 2019 and 2020. However, the length of hospital stay in the ICU and ER was significantly longer in 2020 than in 2019 (P=0.011 and P=0.036, respectively).
Table 1.
Sociodemographic and Clinical Characteristics of Cancer Patients Who Died in 2019 and Those Who Died in 2020 (N=1,456).
| Characteristics | Total | 2019 (n=752) | 2020 (n=704) | P† | |||||
|---|---|---|---|---|---|---|---|---|---|
| n (median) | % (IQR‡) | n (median) | % (IQR) | n (median) | % (IQR) | ||||
| Age (yr) | 67 | 59~75 | 67 | 58~74 | 67 | 59~75 | 0.346 | ||
| ≥60 | 1057 | 72.6 | 534 | 71.0 | 523 | 74.3 | 0.161 | ||
| <60 | 399 | 27.4 | 218 | 29.0 | 181 | 25.7 | |||
| Sex | |||||||||
| Male | 910 | 62.5 | 468 | 62.2 | 442 | 62.8 | 0.828 | ||
| Female | 546 | 37.5 | 284 | 37.8 | 262 | 37.2 | |||
| Insurance | |||||||||
| National insurance | 1358 | 93.3 | 692 | 92.0 | 666 | 94.6 | <0.001 | ||
| Medical aid | 59 | 4.1 | 26 | 3.5 | 33 | 4.7 | |||
| Foreigner (no insurance) | 39 | 2.6 | 34 | 4.5 | 5 | 0.7 | |||
| Residence | |||||||||
| Metropolitan | 943 | 64.8 | 500 | 66.5 | 443 | 62.9 | 0.155 | ||
| Non-metropolitan | 513 | 35.2 | 252 | 33.5 | 261 | 37.1 | |||
| Cancer subtypes | |||||||||
| Lip, oral cavity, and pharynx | 31 | 2.1 | 25 | 3.3 | 6 | 0.9 | 0.016 | ||
| Gastrointestinal | 168 | 11.5 | 79 | 10.5 | 89 | 12.6 | |||
| Hepatobiliary-pancreas | 447 | 30.7 | 223 | 29.7 | 224 | 31.8 | |||
| Lung and intrathoracic | 259 | 17.8 | 140 | 18.6 | 119 | 16.9 | |||
| Bone and soft tissue | 45 | 3.1 | 23 | 3.1 | 22 | 3.1 | |||
| Breast | 77 | 5.3 | 49 | 6.5 | 28 | 4.0 | |||
| Gynecological | 51 | 3.5 | 22 | 2.9 | 29 | 4.1 | |||
| Genitourinary | 68 | 4.7 | 35 | 4.7 | 33 | 4.7 | |||
| Hematological | 252 | 17.3 | 123 | 16.4 | 129 | 18.3 | |||
| Other* | 58 | 4.0 | 33 | 4.4 | 25 | 3.6 | |||
| Disease status at death | |||||||||
| Recurrent or metastatic disease | 1170 | 80.4 | 620 | 82.5 | 550 | 78.1 | 0.038 | ||
| Non-metastatic disease | 286 | 19.7 | 132 | 17.5 | 154 | 21.9 | |||
| Medical division | |||||||||
| Medical department | 1045 | 71.8 | 566 | 75.3 | 479 | 68.5 | 0.006 | ||
| Surgical department | 135 | 9.2 | 57 | 7.6 | 78 | 11.1 | |||
| Emergency medicine | 276 | 19.0 | 129 | 17.1 | 147 | 20.9 | |||
| Length of hospital stay (last hospital visit) | |||||||||
| Overall | 13 | 4~28 | 13 | 4~27.5 | 13 | 4~28 | 0.784 | ||
| General ward | 16 | 8~31 | 15 | 7~31 | 17 | 8~31 | 0.224 | ||
| ICU | 12 | 3~28 | 10 | 2~24 | 17 | 4~35 | 0.011 | ||
| ER | 1 | 0~1 | 0 | 0~1 | 1 | 0~1 | 0.036 | ||
*“Other” includes malignant neoplasms of the skin (C43, C44), central nervous system (C69~C72), endocrine glands (C73~C75), and metastatic or unknown origin (C76~C80).
†The Student t-test was used for continuous variables and the chi-square test for categorical variables. The Mann-Whitney U test and the Fisher exact test were performed as non-parametric tests for continuous and categorical variables, respectively.
‡IQR indicates the difference between the 75th and 25th percentiles of the data (the lower quartile-the upper quartile).
IQR: interquartile range, ICU: intensive care unit, ER: emergency room.
1. Domains of EOL care
The details of the four domains of EOL care (symptom control and comfort care in an imminently dying state, preparation for death, place of death, and aggressive care in the last month) for the participants in 2019 and 2020 are described in Table 2.
Table 2.
Domains of End of Life Care (N=1,456).
| Domains and items | Total | 2019 (n=752) | 2020 (n=704) | P* | |||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||||
| Symptom control and comfort care in an imminently dying state | |||||||||
| Pain | 475 | 32.6 | 266 | 35.4 | 209 | 29.7 | 0.021 | ||
| Resting dyspnea | 558 | 38.3 | 286 | 38.0 | 272 | 38.6 | 0.813 | ||
| Agitation or delirium | 203 | 13.9 | 82 | 10.9 | 121 | 17.2 | 0.001 | ||
| Laboratory tests | 1326 | 91.1 | 687 | 91.4 | 639 | 90.8 | 0.694 | ||
| Imaging tests | 1014 | 69.6 | 538 | 71.5 | 476 | 67.6 | 0.103 | ||
| Continuous monitoring of vital signs | 1219 | 83.7 | 631 | 83.9 | 588 | 83.5 | 0.842 | ||
| Inotropes/vasopressors | 810 | 55.6 | 393 | 52.23 | 417 | 59.2 | 0.007 | ||
| Transfusion | 541 | 37.17 | 291 | 38.7 | 250 | 35.5 | 0.209 | ||
| Preparation for death | |||||||||
| Palliative care consultation | 688 | 47.3 | 335 | 44.6 | 353 | 50.1 | 0.033 | ||
| Advance statements | 536 | 36.8 | 259 | 34.4 | 277 | 39.4 | 0.052 | ||
| Place of death | |||||||||
| General ward | 949 | 65.2 | 501 | 66.6 | 448 | 63.6 | <0.001 | ||
| Single-patient room | 355 | 37.4 | 184 | 36.7 | 171 | 38.2 | 0.646 | ||
| Multiple-patient room | 594 | 62.6 | 317 | 63.3 | 277 | 61.8 | |||
| ICU | 355 | 24.4 | 198 | 26.3 | 157 | 22.3 | |||
| ER | 152 | 10.4 | 53 | 7.1 | 99 | 14.1 | |||
| Aggressive care in the last month | |||||||||
| Cardiopulmonary resuscitation | 209 | 14.4 | 94 | 12.5 | 115 | 16.3 | 0.037 | ||
| Mechanical ventilation | 371 | 25.5 | 187 | 24.9 | 184 | 26.1 | 0.579 | ||
| Renal replacement therapy | 246 | 16.9 | 139 | 18.5 | 107 | 15.2 | 0.095 | ||
| ICU admission | 491 | 33.7 | 261 | 34.7 | 230 | 32.7 | 0.411 | ||
| ER visit | 911 | 62.6 | 473 | 62.9 | 438 | 62.2 | 0.788 | ||
| Last dose of chemotherapy | 515 | 35.4 | 286 | 38.0 | 229 | 32.5 | 0.028 | ||
*The Student t-test was used for continuous variables and the chi-square test for categorical variables. The Mann-Whitney U test and the Fisher exact test were performed as non-parametric tests for continuous and categorical variables, respectively.
ICU: intensive care unit, ER: emergency room.
Regarding symptom control and comfort care in an imminently dying state, 32.6% of the patients experienced pain at the EOL, and this proportion significantly decreased from 35.4% in 2019 to 29.7% in 2020 (P=0.021). Contrastingly, the number of patients who had agitation or delirium in an imminently dying state significantly increased from 10.9% in 2019 to 17.2% in 2020 (P=0.001). Inotropes/vasopressors were utilized in 55.6% of the patients, and this proportion significantly increased in 2020 compared to 2019 (from 52.3% to 59.2%).
For the second domain, preparation for death, both palliative care consultation and documentation of an advance statement showed an increasing trend in 2020 compared to 2019 (44.6% to 50.1% for palliative care consultation; 34.4% to 39.4% for documentation of an advance statement), although statistical significance was not observed for the latter change.
The place of death changed significantly during the pandemic. While the number of patients who died either in the GW or ICU decreased, the proportion of ER deaths doubled in 2020 compared to 2019 (7.1% to 14.1%), with a statistically significant difference (P<0.001). Among the patients who died in the GW, there was no significant difference in the mortality rate between single-patient rooms and multi-patient rooms (P=0.646).
Regarding aggressive care in the last month, cardiopulmonary resuscitation was performed in 14.4% of the overall population, with an increasing trend from 2019 to 2020 (12.5% in 2019 and 16.3% in 2020; P=0.037). The proportion of patients who received chemotherapy in the last month of life decreased from 38.0% in 2019 to 32.5% in 2020 (P=0.028). The receipt of mechanical ventilation, renal replacement therapy, ICU admission, and ER visits did not differ between 2019 and 2020.
2. EOL care by the site of death
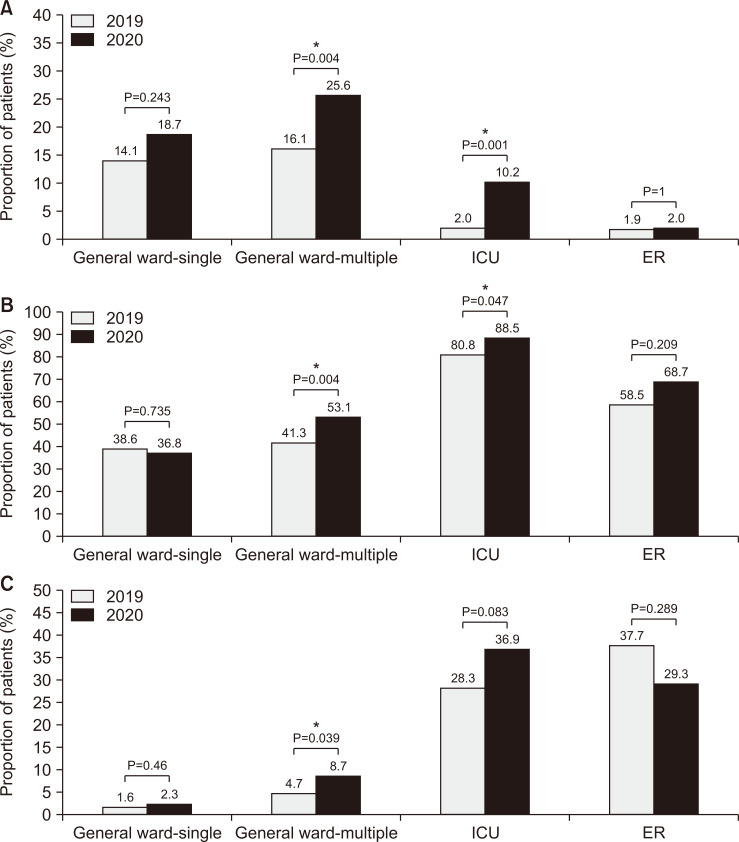
We compared the attributes of EOL care—agitation or delirium in an imminently dying state, receipt of inotropes/vasopressors in an imminently dying state, and receipt of cardiopulmonary resuscitation in the last month—that were significantly different between 2019 and 2020, by the site of death, grouped into four categories (GW-single, GW-multiple, ICU, and ER) (Figure 2). The number of patients who had agitation or delirium in an imminently dying state increased from 2019 to 2020, and the GW-multiple group (16.1% in 2019 to 25.6% in 2020; P=0.004) and ICU group (2.0% in 2019 to 10.2% in 2020; P=0.001) showed statistically significant differences that were larger than those in the other groups (Figure 2A). Similarly, the proportion of patients who received inotropes/vasopressors close to their death increased more in the GW-multiple group (41.3% in 2019 to 53.1% in 2020; P=0.004) and ICU group (80.8% in 2019 to 88.5% in 2020; P=0.047) than in the other groups (Figure 2B). The proportion of patients who received cardiopulmonary resuscitation in the month of death significantly increased in the GW-multiple group (4.7% in 2019 to 8.7% in 2020; P=0.039). In the ICU group, the cardiopulmonary resuscitation rate slightly increased in 2020 (28.3%) compared to 2019 (36.9%), although the difference was not statistically significant (P=0.083) (Figure 2C).
Figure 2.
Comparisons of end-of-life care between 2019 and 2020 by the site of death. (A) Agitation or delirium in an imminently dying state. (B) The receipt of inotropes/vasopressors in an imminently dying state. (C) The receipt of cardiopulmonary resuscitation in the last month. *P<0.05. “General ward-single” refers to single-patient rooms in the general ward, while “General ward-multiple” refers to multiple-patient rooms.
ICU: intensive care unit, ER: emergency room.
DISCUSSION
This retrospective cohort study demonstrates that cancer patients who died in a tertiary hospital experienced several problems at the EOL during the COVID-19 pandemic. We found significant increases in the proportion of patients who experienced agitation or delirium in an imminently dying state, as well as higher frequencies of aggressive care, such as the use of inotropes/vasopressors in an imminently dying state and cardiopulmonary resuscitation within the last month of life in 2020 compared to 2019. We also found that deaths of cancer patients in the ER doubled in 2020 compared to 2019.
The increase in agitation or delirium in an imminently dying state during the pandemic in our study, which may indicate terminal delirium, is in line with results from a few studies of patients with COVID-19 or critically ill patients [16-18]. The ability of the virus to penetrate the central nervous system and influence neurons may make patients with COVID-19 susceptible to delirium [16]. Furthermore, complex factors such as functional impairment, polypharmacy, dehydration, electrolyte imbalances, and immobilization are generally known to be associated with the risk of delirium in hospitalized patients regardless of COVID-19 status [19,20]. Although evidence is insufficient regarding whether restricting visitors in hospitalized patients may influence the risk of delirium, a review suggested that cognitive dysfunction and other neuropsychiatric changes may be associated with social isolation due to the COVID-19 pandemic [21]. Furthermore, hospital policies isolating patients are the opposite of family-involved reorientation interventions to prevent delirium [22]. We cautiously speculate that the absence of loved ones beside the patient may be a factor associated with terminal restlessness.
Surprisingly, we observed an increase in the use of inotropes/vasopressors and cardiopulmonary resuscitation in 2020 compared to 2019, although the proportions of patients who received other life-sustaining treatments were not elevated. The increase in these aggressive measures near death might have been due to increased clinical uncertainty and difficulty in early and detailed advance care planning, including the implementation of specific medical procedures, during the COVID-19 pandemic [23,24]. We also found that the increase in these measures was more evident in places where visitor restrictions are usually stricter, potentially making communication between the patient and family more difficult than in other places. However, further studies should confirm this possible association.
The finding of increased ER mortality among cancer patients who died in the hospital can be considered a significant contribution of our study. This result is consistent with data from another Korean study, which showed that disease-related deaths in the ER increased during the COVID-19 pandemic [25]. We cautiously hypothesize two scenarios to explain the reason for the rise in ER deaths in cancer patients during the pandemic. First, cancer patients might not want to be hospitalized and might want to avoid the hospital as much as possible [26] due to the strict visitor restrictions in the hospital setting [27]. Other studies reporting an increase in the number of people who died at home in the United Kingdom [11] or constant mortality in home hospice rather than decreased mortality in inpatient hospice care in Taiwan [10] may support this hypothesis. Similarly, an Australian study showed that an increased number of deaths was observed within 24 hours of admission to the palliative care unit during the pandemic [9]. Second, terminal cancer patients might remain in the ER much longer due to difficulties in transferring them to other hospitals, thus, eventually dying in the ER. Similar to the national data in Korea [28], we observed longer ER stays in 2020 than in 2019. In any case, the ER is not an adequate or preferred place of death for cancer patients, as care in the ER usually focuses on resuscitation without established guidelines for EOL care. Moreover, as the ER is an important and scarce resource during the pandemic, allocation issues for terminally dying cancer patients in the ER are of major concern.
We can make suggestions for high-quality EOL care based on past experiences of palliative care in response to other epidemics and pandemics. For early and detailed advance care planning, using telemedicine based on information communication technology can bridge the physical gap between patients, family members, and healthcare providers [6]. The ongoing pandemic has raised uncertainty in clinical settings in many ways. Therefore, goal-of-care discussions and communication about the implementation of medical procedures at the EOL, including suddenly deteriorating situations without the family’s presence beside the patient, may help the patient avoid unnecessary and futile procedures, such as inotrope/vasopressor use or cardiopulmonary resuscitation [2,24]. The enhancement of home-based and transitional care can also be considered as an alternative for patients who remain at home at the EOL to prevent avoidable ER visits [10].
Our study also has some limitations. First, the findings from this single-center study cannot be generalized to all dying cancer patients in other tertiary hospitals. Second, due to the nature of Seoul National University Hospital, which focuses on acute medical care and does not have an inpatient hospice ward, the issues related to EOL care identified in this study may be more prominent than those experienced by patients who prepare for dying and death in a hospice facility. Third, we only investigated agitation or delirium based on patients’ medical records, not using a systematic diagnosis of delirium; the resultant exclusion of some subtypes, such as hypoactive delirium, may have underestimated the prevalence of terminal delirium. Fourth, we included both deaths in the GW/ICU and ER, which may show different patterns of medical care utilization and having EOL discussions. Regardless, the increase in deaths in the ER during the COVID-19 pandemic is an important finding. Finally, owing to its retrospective nature based on a review of medical records, the context of the specific EOL discussions and the presence of family members could not be verified, although these factors may be crucial for assessing the quality of EOL care. Further prospective studies investigating the quality of EOL care by physicians or bereaved families are needed to obtain an in-depth understanding of the topic.
In conclusion, our study indicates that cancer patients who died in a tertiary hospital experienced various symptoms and underwent aggressive procedures during their EOL without a beloved family member by their side, even in the ER. Careful discussions of the implementation of medical care at the EOL and the preferred place of death should be held in advance in order to achieve the goal of high-quality EOL care through early and detailed advanced care planning, even in contact-restricted situations [29], thereby helping prevent the deterioration of EOL care for these patients in hospitals during the pandemic.
SUPPLEMENTARY MATERIALS
Supplementary materials can be found via https://doi.org/10.14475/jhpc.2022.25.4.150.
ACKNOWLEDGMENTS
We would like to acknowledge the research assistant JY Park at Seoul National University Hospital for her support of this project.
Funding Statement
Funding/Support This research was supported by a grant from the Patient-Centered Clinical Research Coordinating Center (PACEN) and COVID-19 Public Health Research through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI20C1995, HC20C0005).
Footnotes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
AUTHOR’S CONTRIBUTIONS
JS and SHY performed research design, data collection, the analysis and interpretation of results, and manuscript preparation and writing. YK and JAS contributed to the data collection and helped prepare the manuscript. BK designed, and interpreted the results; advised the whole research process; and acquired the funding. All authors read and approved the final manuscript.
REFERENCES
- 1.COVID-19 Excess Mortality Collaborators, author. Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020-21. Lancet. 2022;399:1513–36. doi: 10.1016/S0140-6736(21)02796-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ersek M, Smith D, Griffin H, Carpenter JG, Feder SL, Shreve ST, et al. End-of-life care in the time of COVID-19: communication matters more than ever. J Pain Symptom Manage. 2021;62:213–22. e2. doi: 10.1016/j.jpainsymman.2020.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cheng HW, Li CW, Chan KY, Sham MK. The first confirmed case of human avian influenza A(H7N9) in Hong Kong and the suspension of volunteer services: impact on palliative care. J Pain Symptom Manage. 2014;47:e5–e7. doi: 10.1016/j.jpainsymman.2013.12.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Etkind SN, Bone AE, Lovell N, Cripps RL, Harding R, Higginson IJ, et al. The role and response of palliative care and hospice services in epidemics and pandemics: a rapid review to inform practice during the COVID-19 pandemic. J Pain Symptom Manage. 2020;60:e31–e40. doi: 10.1016/j.jpainsymman.2020.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kelly M, Mitchell I, Walker I, Mears J, Scholz B. End-of-life care in natural disasters including epidemics and pandemics: a systematic review. BMJ Support Palliat Care. 2021 doi: 10.1136/bmjspcare-2021-002973. bmjspcare-2021-002973. [DOI] [PubMed] [Google Scholar]
- 6.Arya A, Buchman S, Gagnon B, Downar J. Pandemic palliative care: beyond ventilators and saving lives. CMAJ. 2020;192:E400–E404. doi: 10.1503/cmaj.200465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Malagon T, Yong JHE, Tope P, Miller WH, Jr, Franco EL. McGill Task Force on the Impact of COVID-19 on Cancer Control and Care. Predicted long-term impact of COVID-19 pandemic-related care delays on cancer mortality in Canada. Int J Cancer. 2022;150:1244–54. doi: 10.1002/ijc.33884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Hospice Center & Ministry of Health and Welfare, author. Hospice & palliative care in Korea: facts & figures 2020. National Hospice Center & Ministry of Health and Welfare; Goyang: 2020. [DOI] [Google Scholar]
- 9.Everitt R, Robinson N, Marco D, Weil J, Bryan T. Increased number of deaths within 24 h of admission during a period of social restriction related to the COVID-19 pandemic: A retrospective service evaluation in a metropolitan palliative care unit. Palliat Med. 2021;35:1508–13. doi: 10.1177/02692163211026518. [DOI] [PubMed] [Google Scholar]
- 10.Chou YC, Yen YF, Feng RC, Wu MP, Lee YL, Chu D, et al. Impact of the COVID-19 pandemic on the utilization of hospice care services: a cohort study in Taiwan. J Pain Symptom Manage. 2020;60:e1–e6. doi: 10.1016/j.jpainsymman.2020.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bone AE, Finucane AM, Leniz J, Higginson IJ, Sleeman KE. Changing patterns of mortality during the COVID-19 pandemic: population-based modelling to understand palliative care implications. Palliat Med. 2020;34:1193–201. doi: 10.1177/0269216320944810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Steinhauser KE, Christakis NA, Clipp EC, McNeilly M, McIntyre L, Tulsky JA. Factors considered important at the end of life by patients, family, physicians, and other care providers. JAMA. 2000;284:2476–82. doi: 10.1001/jama.284.19.2476. [DOI] [PubMed] [Google Scholar]
- 13.Singer PA, Martin DK, Kelner M. Quality end-of-life care: patients' perspectives. JAMA. 1999;281:163–8. doi: 10.1001/jama.281.2.163. [DOI] [PubMed] [Google Scholar]
- 14.National Law Information Center, author. Act on decisions on life-sustaining treatment for patients in hospice and palliative care or the end-of-life [Internet] Korea Ministry of Government Legislation; Sejong: 2016. [cited 2021 Feb 17]. Available from: https://law.go.kr . [Google Scholar]
- 15.Lee HY, Kim HJ, Kwon JH, Baek SK, Won YW, Kim YJ, et al. The situation of life-sustaining treatment one year after enforcement of the act on decisions on life-sustaining treatment for patients at the end-of-life in Korea: data of national agency for management of life-sustaining treatment. Cancer Res Treat. 2021;53:897–907. doi: 10.4143/crt.2021.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Helms J, Kremer S, Merdji H, Schenck M, Severac F, Clere-Jehl R, et al. Delirium and encephalopathy in severe COVID-19: a cohort analysis of ICU patients. Crit Care. 2020;24:491. doi: 10.1186/s13054-020-03200-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Persaud TV. Fetal outcome following maternal treatment with prostaglandin E2. Prostaglandins Leukot Med. 1986;24:75–8. doi: 10.1016/0262-1746(86)90209-X. [DOI] [PubMed] [Google Scholar]
- 18.Jackel M, Aicher N, Biever PM, Heine L, Bemtgen X, Rilinger J, et al. Delirium in critically Ill patients with and without COVID-19-a retrospective analysis. J Clin Med. 2021;10:4412. doi: 10.3390/jcm10194412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Maldonado JR. Delirium in the acute care setting: characteristics, diagnosis and treatment. Crit Care Clin. 2008;24:657–722. doi: 10.1016/j.ccc.2008.05.008. vii. [DOI] [PubMed] [Google Scholar]
- 20.Guo D, Lin T, Deng C, Zheng Y, Gao L, Yue J. Risk factors for delirium in the palliative care population: a systematic review and meta-analysis. Front Psychiatry. 2021;12:772387. doi: 10.3389/fpsyt.2021.772387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Manca R, De Marco M, Venneri A. The impact of COVID-19 infection and enforced prolonged social isolation on neuropsychiatric symptoms in older adults with and without dementia: a review. Front Psychiatry. 2020;11:585540. doi: 10.3389/fpsyt.2020.585540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Inouye SK. The importance of Delirium and Delirium prevention in older adults during lockdowns. JAMA. 2021;325:1779–80. doi: 10.1001/jama.2021.2211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hauk H, Bernhard J, McConnell M, Wohlfarth B. Breaking bad news to cancer patients in times of COVID-19. Support Care Cancer. 2021;29:4195–8. doi: 10.1007/s00520-021-06167-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mott FE, Bruera E, Johnson F. End-of-life and goals of care discussions with cancer patients in the coronavirus pandemic. Palliat Support Care. 2021;19:384–5. doi: 10.1017/S1478951520000668. [DOI] [PubMed] [Google Scholar]
- 25.Jung E, Ro YS, Ryu HH, Shin SD, Moon S. Interaction effects between COVID-19 outbreak and community income levels on excess mortality among patients visiting emergency departments. J Korean Med Sci. 2021;36:e100. doi: 10.3346/jkms.2021.36.e100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Harrison NE, Ehrman RR, Curtin A, Gorelick D, Hill AB, Brennan E, et al. Factors associated with voluntary refusal of emergency medical system transport for emergency care in Detroit during the early phase of the COVID-19 pandemic. JAMA Netw Open. 2021;4:e2120728. doi: 10.1001/jamanetworkopen.2021.20728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pak YS, Ro YS, Kim SH, Han SH, Ko SK, Kim T, et al. Effects of emergency care-related health policies during the COVID-19 pandemic in Korea: a Quasi-experimental study. J Korean Med Sci. 2021;36:e121. doi: 10.3346/jkms.2021.36.e121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kim SJ, Kim H, Park YH, Kang CY, Ro YS, Kim OH. Analysis of the impact of the Coronavirus disease epidemic on the emergency medical system in South Korea using the Korean triage and acuity scale. Yonsei Med J. 2021;62:631–9. doi: 10.3349/ymj.2021.62.7.631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kim Y, Yoo SH, Shin JM, Han HS, Hong J, Kim HJ, et al. Practical considerations in providing end-of-life care for dying patients and their family in the era of COVID-19. Korean J Hosp Palliat Care. 2021;24:130–4. doi: 10.14475/jhpc.2021.24.2.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.