Abstract
Bone and cartilage disorders are the leading causes of musculoskeletal disability. There is no absolute cure for all bone and cartilage disorders. The exploration of natural compounds for the potential therapeutic use against bone and cartilage disorders is proving promising. Among these natural chemicals, naringin, a flavanone glycoside, is a potential candidate due to its multifaceted pharmacological activities in bone and cartilage tissues. Emerging studies indicate that naringin may promote osteogenic differentiation, inhibit osteoclast formation, and exhibit protective effects against osteoporosis in vivo and in vitro. Many signaling pathways, such as BMP-2, Wnt/β-catenin, and VEGF/VEGFR, participate in the biological actions of naringin in mediating the pathological development of osteoporosis. In addition, the anti-inflammatory, anti-oxidative stress, and anti-apoptosis abilities of naringin also demonstrate its beneficial effects against bone and cartilage disorders, including intervertebral disc degeneration, osteoarthritis, rheumatoid arthritis, bone and cartilage tumors, and tibial dyschondroplasia. Naringin exhibits protective effects against bone and cartilage disorders. However, more efforts are still needed due to, at least in part, the uncertainty of drug targets. Further biological and pharmacological evaluations of naringin and its applications in bone tissue engineering, particularly its therapeutic effects against osteoporosis, might result in developing potential drug candidates.
Keywords: naringin, osteoporosis, intervertebral disc degeneration, osteoarthritis, rheumatoid arthritis, osteogenic differentiation, bone tissue engineering
1. Introduction
Bone and cartilage disorders, the leading causes of musculoskeletal disability, are characterized by the destruction of bone and cartilage, as manifested by imbalanced homeostasis, increased inflammatory responses, and dysregulated osteoimmunology [1]. The prevalence of bone and cartilage disorders has increased significantly due to the aging population. This situation has posed a challenge to the economy and society worldwide. In particular, bone infection, a difficult-to-treat disease, may enhance the ratio of treatment failure by up to 20–30% [2]. Although promising experimental research and the exploration of clinical diagnosis and therapeutic management techniques are currently underway, there is no absolute cure for all bone and cartilage disorders. An effective clinical treatment strategy for bone and cartilage disorders is essential.
Researchers are interested in the potential efficacy of synthetic and/or natural compounds against bone and cartilage disorders [3,4]. Tofacitinib, a Janus kinase inhibitor, is a disease-modifying anti-rheumatic drug (DMARDs) and shows therapeutic effects against rheumatoid arthritis (RA). A recent study shows that tofacitinib (5 mg and 10 mg BID) exhibits a consistent safety profile and sustained efficacy for patients with RA [5]. Tocilizumab, a non-tumor necrosis factor inhibitor (TNFi) biologic agent, has a satisfactory efficacy against RA, with a low risk of cardiovascular events [6]. The chicken embryo tissue hydrolysate (CETH) dose-dependently reverses the morphological changes of RA induced by Freund’s full adjuvant in rats [7]. Several natural chemicals and synthetic nanoparticular compounds have been reviewed for their therapeutic effects against osteoarthritis (OA) [8].
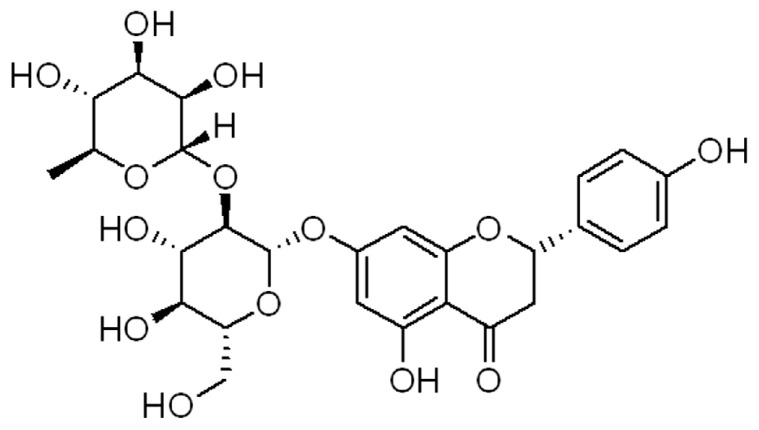
Flavonoids are polyphenolic compounds and a source of effective chemicals in plants and nutraceuticals consumed by humans. Studies have reported that these effective compounds exhibit various pharmacological activities by modulating certain enzymes. For example, genistein may exhibit estrogen-like effects to protect against many diseases, such as cancers, osteoporosis (OP), and OA [9]. Icariin shows promising characteristics in biomedicine and bone/cartilage tissue engineering [10]. Naringin (4′, 5,7-trihydroxy flavanone-7-rhamnoglucoside, Figure 1) is a flavonoid glycoside that is found in the extract of citrus fruits [11] and rhizoma drynariae [12]. Naringin possesses several pharmacological effects, including anti-inflammation, anti-oxidation, anti-cancer, anti-bacteria, liver protection, and bone/cartilage protection [13,14].
Figure 1.
The chemical structure of naringin.
The pharmacokinetic profiles and bioavailability of naringin have been comprehensively discussed recently [15,16]. Briefly, naringin can be poorly absorbed in the gastrointestinal tract and converted to its aglycone form, naringenin, by gut microorganisms [17]. The bioavailability of naringin by oral administration is about 5–9% [18], and the Cmax value is about 5.5 h [19]. The distribution of naringin includes the trachea, gastrointestinal tract, lungs, liver, and kidneys. After administration, naringin undergoes oxidation, demethylation, glucuronidation, and sulfation [20]. Naringin is a nontoxic bioactive natural compound. It has been reported that the oral administration of naringin at a dose of 200 mg/kg in humans exhibits no obvious side effects [21].
Naringin has been used in traditional Chinese medical regimens to treat osteoporosis [22]. Naringin may mediate the intracellular signaling pathways that are important for the development of bone and cartilage. Currently, the applications of naringin in bone are particularly strongly associated with the therapeutic management of OP and the pro-osteogenic differentiation of mesenchymal stromal stem cells (MSCs). The beneficial effects of naringin are also seen in its contribution to the field of tissue engineering [23]. The potential therapeutic effects of naringin might be associated with its biological actions on intracellular targets. In this review article, we describe the protective effects of naringin against bone and cartilage disorders, including OP, OA, intervertebral disc degeneration (IDD), RA, femoral head (FH) diseases, bone and cartilage tumors, and tibial dyschondroplasia (TD).
2. The Protective Activities of Naringin against Osteoporosis
OP is characterized by a reduction in bone mineral density (BMD), a deterioration of the bone microstructure, and the degradation of matrix protein. These pathological changes may lead to an increase in bone fragility and fracture risk. OP causes a reduction in quality of life and places a financial burden on patients and society [24]. The causes of OP might be associated with the hypofunction of osteoblasts and the hyperfunction of osteoclasts. Therefore, improving osteoblast biofunctions and attenuating osteoclast activity can be an effective therapeutic strategy for OP treatment. The clinically approved drugs regulate the remodeling of bone in ways that increase BMD, strengthen bones, and decrease fracture risks. Anti-resorptive drugs, such as bisphosphonates, calcitonin, and denosumab, improve BMD and restore bone strength; as a result, they reduce fracture risk by inhibiting bone resorption [25]. Osteoanabolic drugs, such as teriparatide, stimulate new bone formation and improve bone strength and bone microarchitecture (the parathyroid hormone restores bone quality to levels equal to the control group, at least in a rodent model) [26]. Both blocking bone resorption and stimulating new bone formation are effective strategies for OP treatment.
The current OP drug therapies have been reviewed in detail by Reid et al. [27]. Anti-resorptives, including bisphosphonates, are the first line of treatment against osteoporosis. Denosumab, another first-line anti-osteoporotic drug, is a monoclonal antibody against RANKL and acts as an anti-resorptive, similar to bisphosphonates. The osteoanabolic drugs teriparatide and abaloparatide, two different synthetic peptide analogs of human PTH, bind and activate the parathyroid hormone-1 receptor (PTH1R), stimulating bone formation [28]. Statins, the inhibitors of hepatic hydroxy-methylglutaryl coenzyme A (HMG-CoA) reductase, have been reported to stimulate the expression of bone morphogenetic protein-2 (BMP-2), which is a regulator of osteogenic differentiation. Statins may produce anabolic effects on bone. However, the administration of statins can induce several side effects, such as weakness, headache, and muscle problems [29]. Thus, the therapeutic inhibition of HMG-CoA reductase expression can be a potential strategy for developing bone-inductive agents.
Naringin acts as an inhibitor of HMG-CoA reductase. In addition, naringin may increase bone formation, as shown by increased cell viability and enhanced ALP activity in UMR-106 cells [30]. The positive effects of naringin on bone in rodents, particularly in females in most research, have been demonstrated. Naringin or hesperidin, and a combination of both, have been linked to the accrual and maintenance of BMD and the structure and strength of bone [31,32]. A recent study indicates that the maternal consumption of naringin and hesperidin during pregnancy and lactation shows transient effects on the BMD in trabecula and the structure of bone at the proximal tibia in female CD-1 mice offspring after weaning. However, these biological effects cannot influence the skeletal integrity and strength of the tibia, femur, and LV in adulthood [33].
2.1. Osteogenic Differentiation Induction
Naringin can effectively enhance the proliferative activity of MC3T3-E1 cells and promote the differentiation of osteoblasts, as shown by the increased activity of ALP [34]. In human bone marrow mesenchymal stem cells (BMSCs), naringin has been demonstrated to promote proliferation and osteogenic differentiation, as indicated by an increased expression of ALP, OPN, OCN, and COL1A2 [35]. Another study shows that naringin may promote osteoblast differentiation and suppress adipocyte formation by mediating miR-20a/PPARγ signaling in BMSCs. Specifically, the naringin-increased expression of miR-20a targets the degradation of PPARγ, which may induce BMSCs to differentiate into adipocytes [36]. Fish-derived collagen films fabricated with genistein, icariin, and naringin may improve the proliferation and differentiation of human MSCs by upregulating the expression of RUNX-2, Collagen I, c-Fos, and TGFβ1/Smad3. In addition, the mechanical properties, solubility, and in vitro biodegradation of the fabricated collagen films were also improved [37].
Human periodontal ligament stem cells (hPDLSCs) may differentiate into osteoblasts, osteoclasts, fibroblasts, and cementum cells. Naringin, at a dose of 1 μM, can promote the proliferation and differentiation of hPDLSCs into osteoblasts, as indicated by upregulating bone-related factors, such as RUNX2, COL1A2, OPN, and OCN [38]. However, the limited lifespan of hPDLSCs restricts their application [39]. The knock-in of Bmil may enhance the cell cycle, cell replication, and stemness of hPDLSCs. Interestingly, naringin induces the osteogenic differentiation of hPDLSC-Bmil cells by stimulating the expression of the ERK1/2 signaling pathway [40].
Similarly, naringin ameliorates the H2O2-induced inhibition of osteogenic differentiation by activating the Wnt/β-catenin signaling pathways in human adipose-derived stromal cells (ADSCs) [41]. Consistently, naringin rescues H2O2-inhibited β-catenin and cyclin D1 expression, stimulates ALP activity, increases RUNX2 and OSX expression, and promotes osteogenic differentiation by inhibiting oxidative stress in human adipose-derived mesenchymal stem cells (hADMSCs) [42]. Similarly, human amniotic fluid-derived stem cells (hAFSCs) can also produce osteogenic cells, increase the expression of RUNX2, OPG, OPN, and Collagen I, and decrease the expression of RANKL by upregulating the activity of the BMP4 and Wnt/β-catenin signaling pathways [43].
The directional migration of the MSCs and osteogenesis contribute to bone fracture healing. In addition, MSCs may produce a series of cytokines, growth factors, and chemokines by autocrine and paracrine, affecting bone fracture healing. Naringin can stimulate MSC migration and induce differential chemokine secretion of the C-X-C motif chemokine-5 (CXCL-5), CXCL-6, and the C-C motif chemokine-20 (CCL-20) by activating the Ras signaling pathway [44]. Another study demonstrated that naringin might promote the osteogenic differentiation of human BMSCs by increasing the phosphorylation of ERK, as indicated by the upregulated expression of RUNX-2, OCN, COL1, and osterix (Osx). The inductive effect of naringin may be abolished by U0126, which is a specific inhibitor of ERK [45].
2.2. Osteoclast Formation Inhibition
Increased osteoclast formation and bone resorption contribute to the development of osteolytic bone diseases, such as OP. The receptor activator of the nuclear factor-κB (NF-κB) ligand (RANKL) contributes to the formation and activation of osteoclasts. The association of RANKL with RANK triggers the intracellular signaling pathways, such as NF-κB, AKT, MAPKs, and Ca2+/calmodulin (CaM)-dependent kinase [46]. Naringin can suppress RANKL-induced NF-κB signaling by inhibiting RANKL-regulated IκBα degradation, perturbing osteoclast formation and bone resorption. Specifically, naringin downregulates the expression of the osteoclast gene biomarkers, such as cathepsin k, calcitonin receptor, and TRACP, in a dose-dependent manner [47].
In lipopolysaccharide (LPS)-induced rat alveolar bone resorption models, naringin may increase the BMD value, decrease the osteoclast number, and increase the production of the non-calcified bone-like matrix, demonstrating osteogenic effects [48]. Retinoic acid (ReA) is used to treat psoriasis and nodular acne. The adverse reactions of ReA include OP. In ReA-induced rat OP, naringin can reduce the serum levels of alkaline phosphatase (ALP) and improve the bone weight coefficient, the length, and diameter of the bone, the content of bone ash, calcium, and phosphorus, and promote new bone formation [49]. Naringin consistently increases the number of trabeculae, improves trabecular bone structure, and increases the bone mineral density of the femur neck in ReA-induced rat OP. The possible mechanism of naringin in protecting against OP might be associated with the upregulation of ALP and PTH1R expression and the downregulation of bone resorption-related proteins, such as TRAP, RANKL, and RANK [50] (Table 1).
Table 1.
The protective activities of naringin in bone and cartilage disorders.
| Models/Cells | Doses/Concentrations | Biological Actions | Ref. |
|---|---|---|---|
| ReA-induced rat OP | 50 mg/kg | Increases BMD of femur shaft, increases BV/TV and Tb.Sp, increases ALP activity, decreases SOST, TRAP, and RANKL expression, and increases PTH1R expression. | [50] |
| IDG-SW3 cells | 50 μM | Decreases SOST and RANKL expression. | [50] |
| OVX-induced rat OP | 40, 100, 200 mg/kg | Improves BMD, bone indices, and pathological changes. Increases the average maximum fracture load. Increases the serum OC and decreases the serum CTX-1. | [51] |
| Osteoclasts | 20 ng/mL | Reduces the number of TRAP-positive osteoclasts; promotes cell apoptosis. | [51] |
| OVX-induced rat OP | 300 mg/kg + treadmill exercise | Increases bone indices, BMD, and mechanical strength; increases OCN expression and decreases CTX-1 expression. | [52] |
| GC-treated IBD rats | 100 and 200 mg/kg | Decreases the serum TNFα and increases the serum P1NP; improves the bone indices; decreases MDA, CAT, and SOD activity; increases ALP, OC, and RUNX-2 expression. | [53] |
| NP cells from patients with IDD | 20 μg/mL | Increases cell proliferation, increases BMP2, Sox6, and aggrecan expression, and decreases MMP-3 expression. | [54] |
| IL-1β-treated human NP cells | 0.4, 0.8, 1.2, and 1.6 μM | Decreases MMP-3, MMP-13, ADAMTS4, and ADMATS5 expression, increases collagen II and aggrecan production; attenuates p65 and IκBα phosphorylation; decreases p65 and p53 expression. | [55] |
| TNFα-treated NP cells | 10 μg/mL | Decreases COX-2, cleaved caspase-3, Bax, MMP-3, ADAMTS4, and p63 expression; enhances SOD, Bcl-2, collagen II, aggrecan, Sox9, LC3-II/I ratio, AMPK, and Sirt1 expression; improves mitochondrial functions. | [56] |
| H2O2-treated NP-derived MSCs | 10 μM | Inhibits apoptosis; improves mitochondrial functions; decreases Bax, caspase-3, and p53 expression; increases Bcl-2, PI3K, and AKT expression | [57] |
| TNFα-treated mouse chondrocytes | 5 μM | Decreases IL-1β, iNOS, COX-2, MMP-13, ADAMTS5, p-IκBα, and NF-κB2 expression. | [58] |
| ACLT-induced mouse OA | 100 mg/kg | Decreases IL-1β, iNOS, COX-2, MMP-13, ADAMTS5, p-IκBα, and NF-κB2 expression. | [58] |
| MIA-induced rat OA | 5 and 10 mg/kg | Decreases the serum levels of PGE2, IL-6, IL-1β, and TNFα; improves histopathological changes. | [59] |
| LPS-treated RAW 264.7 cells | 5 and 10 μg/mL | Decreases the production of PGE2, NO, IL-6, and TNFα. | [59] |
| Cartilage defects in New Zealand rabbits | 84 mg/kg + ADM | Improves the repair morphology of defect cartilages and enhances the expression of TGFβ2, TGFβ3, and SOX9. | [60] |
| TNFα-treated RA FLSs | 20, 40, 60, and 80 μg/mL | Decreases cell viability, increases apoptosis, downregulates the expression of IL-1, IL-6, IL-8, MMP-1, MMP-2, and MMP-13, and suppresses the MAPK/ERK and PI3K/AKT signaling pathways. | [61] |
| MPS-induced rat SANFH | 5, 10, and 20 mg/kg | Increases the serum OC levels, decreases the total cholesterol, the LDL/HDL ratio, and caspase-3 expression; promotes osteogenic differentiation by increasing the expression of PPARγ, Notch, β-catenin, and p-AKT. | [62] |
| Dex-treated MLO-Y4, MC3T3-E1, and RAW 264.7 cells | 100 μM | Attenuates cell apoptosis and decreases Bax and cleaved caspase-3 expression; increases Bcl-2 expression; promotes osteogenic differentiation and inhibits osteoclast formation by activating the PI3K/AKT signaling pathway. | [63] |
| MPS-induced rat GIONFH | 300 mg/kg | Improves histopathological changes and enhances the expression of OC and AKT | [63] |
| MG63 cells | 10 and 20 μmol/L | Decreases the expression of Cyclin D1, MMP2, and Bcl-2 and inhibits cell proliferation, migration, and invasion. | [64] |
| JJ012 and SW1353 cells | 3, 10, and 30 μM | Decreases VCAM-1 expression, increases miR-126 expression, and suppresses cell migration and invasion. | [65] |
| Thiram-induced TD broiler chickens | 30 mg/kg | Restores the tibia weight and length, inhibits the reduction in blood vessels, and increases the expression of Ihh and PTHrP. | [66] |
Osteoclast-associated bone resorption plays a critical role in aseptic loosening after joint arthroplasty. The regulation of osteoclast maturation is associated with the balance of RANKL and OPG. Naringin effectively suppresses osteoclastogenesis and wear-particle-stimulated osteolysis by increasing Wnt/β-catenin signaling-mediated OPG expression. However, naringin does not affect RANKL expression in fibroblasts [67]. Consistently, naringin, administered by intraperitoneal injection for 7 days at doses of 50 μg/kg and 100 μg/kg, respectively, may significantly suppress polymethyl methacrylate (PMMA)-induced osteolysis and aseptic loosening, which is promoted by wear-particle-induced inflammatory cytokines. In an in vitro study, naringin effectively inhibited osteoclastogenesis and osteoclast maturity functions [68]. Another study indicated that, at a dose of 10–100 μg/mL, naringin might decrease PMMA-induced TRAP activity, inflammatory responses, osteoclastogenesis, and bone resorption. Administered at a dose of 300 mg/kg by oral gavage for 30 days, naringin may ameliorate periprosthetic bone resorption [69].
2.3. The Underlying Mechanisms of Naringin in Protecting against Osteoporosis
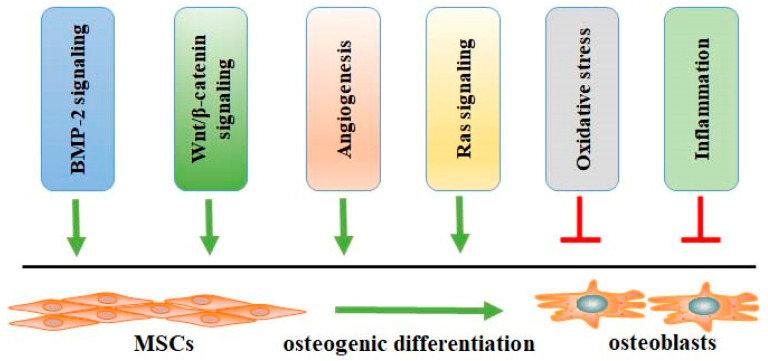
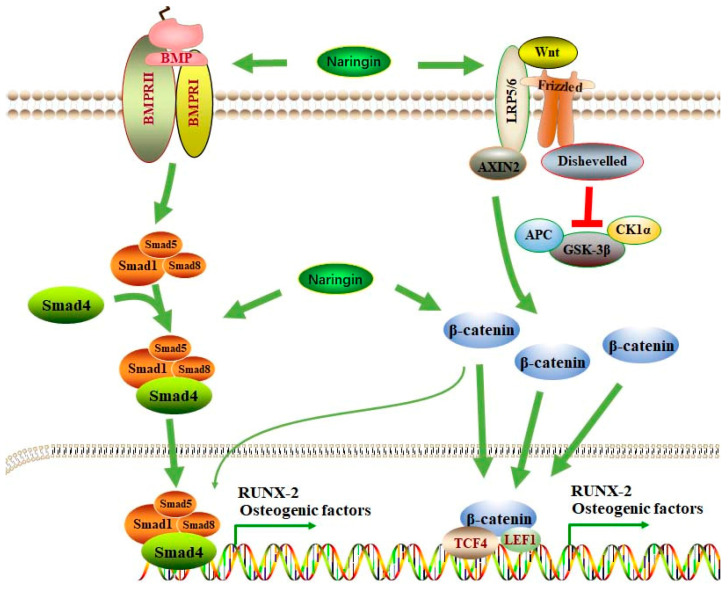
Emerging evidence has reported that many factors, such as BMP-2, Wnt/β-catenin, angiogenesis, and oxidative stress, may affect the biological processes of osteogenic differentiation (Figure 2), which is the potential target for the therapeutic management of OP. Naringin promotes osteogenic differentiation, as shown by the increased expression of ALP, bone sialoprotein (BSP), and RUNX-2, as well as increased calcium deposits and a decreased expression of PPARγ2 in rat BMSCs [70]. BMP-2 mediates cell proliferation and differentiation by binding with BMP receptors (BMPRs) (Figure 3), such as BMPR-1A and BMPR-1B, and activating the BMPR signaling pathway. The activation of BMP-2/BMPR-1A may initiate the differentiation of BMSC into adipocytes. In contrast, BMP-2/BMPR-1B signaling activation may result in osteogenesis and bone formation [71]. Naringin and naringin-containing Drynaria fortunei (Gusuibu) may block the interaction between BMP-2 and BMPR-1A and enhance the binding of BMP-2 to BMPR-1B, promoting osteoblast differentiation [72]. However, some studies indicate that BMPR-1A is essential for osteogenesis and chondrogenesis, and BMPR-1B inhibits hypertrophic differentiation. BMPR-1B activation facilitates chondrogenesis over hypertrophy [73]. These findings suggest that differentiating the competitive interaction of BMP-2 with their receptors may govern the differentiation of BMSCs.
Figure 2.
The factors affecting the processes of osteogenic differentiation of MSCs to osteoblasts. Many factors, such as BMP-2 signaling, Wnt/β-catenin signaling, angiogenesis, Ras signaling, oxidative stress, and inflammation, may affect osteogenic differentiation. Abbreviations: BMP-2, bone morphogenetic protein-2; MSCs, mesenchymal stromal stem cells.
Figure 3.
BMP-2 and Wnt/β-catenin signaling pathways participate in the pharmacological activity of naringin in mediating osteogenic differentiation. BMP-2 may interact with its receptors, such as BMPRII and BMPRI; this is followed by the activation of Smad1/5/8, which recruits Smad4, forming a complex and entering the nucleus for the transcriptional mediation of osteogenic factors, such as RUNX-2. After being activated by Wnt, β-catenin is stabilized and translocated to the nucleus for the transcriptional mediation of osteogenic factors. Activated β-catenin may also stimulate the BMP-2/Smad signaling pathway to induce osteogenic differentiation. Naringin can stimulate the BMP-2/Smad and Wnt/β-catenin signaling pathways to promote osteogenic differentiation. Abbreviations: BMP, bone morphogenetic protein; BMPRs, BMP receptors; SMAD: suppressor of mothers against decapentaplegic; Runx-2, Runt-related transcription factor-2; LRP, LDL receptor-related protein; Axin2, axis inhibition protein 2; APC, adenomatous polyposis coli; CK1α, casein kinase 1α; TCF-4, transcription factor 4; LEF1, lymphoid enhancer-binding factor 1.
The BMP-2 signaling pathway in the demineralized bone matrix (DBM) is also involved in osteogenic differentiation during the repairing of bone fractures. Naringin may act as an activator of the BMP-2 promoter and increase bone formation. In rabbits with bone/collagen matrix grafts, naringin in the collagen matrix increases new bone by 284% and 490% more than the autogenous endochondral bone grafts alone and a collagen matrix alone, respectively [30,74]. The inductive activity of BMP-2 in osteogenic differentiation is also regulated by the PI3K/AKT, c-Fos/c-Jun, and AP-1 signaling pathways. Mutations of p85, Akt, c-Fos, and c-Jun may block the potentiating actions of naringin on the expression of BMP-2 in osteoblasts [75]. The notch signaling pathway regulates cell functions, such as proliferation, differentiation, and cell-fate decisions. Notch reception activation may produce γ-secretase-cleaved NICD, which is translocated into the nucleus for the transcriptional regulation of target genes, such as HES [76]. The importance of notch signaling in bone formation has been demonstrated [77]. It is reported that notch signaling is activated and regulates BMP-2/DLX3-mediated osteogenic differentiation in dental follicle cells [78].
Wnt/β-catenin signaling has been associated with osteogenesis [79] (Figure 3). Naringin may promote the phosphorylation of the Ser552 residue on β-catenin, leading to the stabilization and nuclear translocation of β-catenin and the upregulation of ALP, RUNX-2, and COL1 expression in rat osteoblast-like UMR-106 cells. However, treatment with AKTi (an AKT inhibitor) or Dorsomorphin (an AMPK inhibitor) may significantly reduce the effects of naringin on β-catenin. In OVX-induced mouse OP, the osteoprotective effects of naringin are also abolished by AKTi or Dorsomorphin [80]. Sclerostin, an antagonist of Wnt/β-catenin signaling, plays an important role in the development of OP. Periostin, an upstream regulator of sclerostin, negatively regulates sclerostin expression in response to mechanotransduction by upregulating Sost expression [81]. Semaphorin 3A (Sema3A), an axonal guidance chemorepellent in the nerve system, plays a critical role in the maintenance of bone mass. Sema3A can be produced by osteoblasts and osteocytes, promoting bone formation by stimulating osteoblast differentiation through the upregulation of the Wnt/β-catenin signaling pathway and downregulation of osteoclast differentiation [82]. In unilateral sciatic neurectomy (USN)-induced rat disuse OP, naringin may increase bone formation and suppress bone resorption by activating the Wnt/β-catenin signaling pathway and increasing Sema3A expression [83].
Forkhead box C2 (Foxc2), a member of the family of forkhead transcriptional factors, has been shown to promote the osteogenic differentiation of MSCs by activating Wnt/β-catenin signaling. Indian hedgehog (IHH) is a member of the hedgehog family, and it regulates the actions of tissue patterning, skeletogenesis, and cell proliferation. A deficiency of IHH may inhibit osteoblast development [84]. Naringin can upregulate the expression of Foxc2 and promote osteogenic differentiation in BMSCs. However, the inhibition of the IHH signaling pathway may block the potentiated effects of naringin on Foxc2 expression and osteogenic differentiation [85]. It has been reported that sciatic neurectomy can decrease periostin expression, increase sclerostin, and inactivate Wnt/β-catenin signaling, leading to the deterioration of the trabecular microstructure and bone loss. Naringin may exhibit osteoprotective effects against sciatic-neurectomy-induced bone loss by suppressing sclerostin expression and activating Wnt/β-catenin signaling [86].
Estrogen and selective estrogen receptor modulators (SERMS) act primarily as anti-resorptive candidates. Phytoestrogens, such as flavonoids, have been investigated as new strategies for managing estrogen-deficient diseases, such as OP. Naringin has estrogenic agonist activity at low concentrations, as it selectively interacts with estrogen receptor β (ERβ), preventing OP development. However, at high concentrations, naringin exhibits anti-estrogenic effects [87]. Another study reports that naringin, at doses of 0.2 and 0.4 mg/g/day, can enhance the value of BMD at the distal femur, proximal tibia, and lumber spine in ovariectomized (OVX) mice. The protective activity of naringin may be abolished by ER antagonist ICI-182780 in rat osteoblast-like UMR-106 cells [88]. One study demonstrated that naringin could enhance cell viability and proliferation by increasing the translocation of ERα to the nucleus for transcriptional regulation in MC3T3-E1 cells. In addition, the Erα-specific inhibitor, methylpiperidinopyrazole, can abrogate the naringin-stimulated expression of ERα and ALP, suppressing bone healing and mass in ICR mice [89]. A meta-analysis of the protective effects of naringin against postmenopausal OP in OVX rats found that naringin may promote bone formation [90]. Naringin exhibits protective activity against OVX-induced rat OP by promoting mitochondria-mediated apoptosis in osteoclasts. Specifically, naringin can decrease the expression of Bcl-2 and increase the expression of Bax, caspase-3, and cytochrome C in osteoclasts, reducing bone resorption [51] (Table 1). When combined with treadmill exercise, naringin may protect against OVX-induced rat OP, as indicated by an increased BMD, improved morphological bone indices, the upregulation of osteocalcin (OCN) expression, and the downregulation of the C-terminal telopeptides of type I collagen (CTX-1) [52] (Table 1).
Blood vessels and angiogenesis may play an essential role in orchestrating the balance between bone regeneration and resorption (Figure 3). Postmenopausal OP is associated with reduced sinusoidal and arterial capillaries in the bone marrow and decreased bone perfusion. Vascular endothelial growth factor (VEGF) can improve fracture repair by stimulating angiogenesis, ossification, and bone metabolism [91]. Thus, increased angiogenesis can be an effective strategy for the therapeutic management of OP. Recently, the effects of naringin on vascular endothelial cells (VECs) in OVX-induced rat OP have been explored. Naringin may suppress the expression of GRP78, CHOP, caspase-12, caspase-3, and caspase-9, increase the production of NO, inhibit cell apoptosis, and improve the values of BMD, leading to the amelioration of OP by promoting angiogenesis [92]. Similarly, it is shown that naringin may induce angiogenesis in OVX-induced rat OP by activating the expression of VEGF and VEGFR-2. Specifically, naringin can increase the vessel number and larger vessel area and improve bone repair [93].
Oxidative stress is associated with a decline in tissue and organ functions (Figure 3). The redox homeostasis in cells is orchestrated by ROS generation and scavenging. Excessive ROS production may induce biological damage to the DNA, proteins, and lipids. The antioxidants include superoxide dismutase (SOD), glutathione (GSH), catalase (CAT), and glutathione peroxidase (GPX) [94]. Oxidative stress is involved in diabetes-associated bone diseases. Moreover, 60Co γ-radiation induces acentric fragments, chromatid and chromosome breaks, dicentrics, and exchanges. These aberrations in mouse bone marrow cells can be significantly suppressed by naringin (2 mg/kg) by scavenging free radicals [95]. Naringin may also reduce chromosome aberrations and reduce the frequency of micronucleated polychromatic (MPCE) and normochromatic (MNCE) in mouse bone marrow [96]. Both glucocorticoid (GC) and inflammatory bowel disease (IBD) can induce bone loss. Clinically, OP and bone fractures can occur at high rates in patients with IBD. Naringin exhibits osteoprotective effects against bone loss in GC-treated IBD rats by reducing oxidative stress and promoting bone formation [53] (Table 1). In addition, naringin promotes the proliferation and differentiation of osteoblasts by upregulating the PI3K/AKT/mTOR signaling pathway and activating autophagy. In GC-induced rat OP, naringin can increase BMD, improve bone morphology parameters, and upregulate the expression of autophagy-related factors [34]. In streptozotocin (STZ)-induced rat diabetes, naringin exhibits anti-oxidative effects in the bone marrow of the femur, increases the BMD and bone mineral content (BMC) of the distal femur and proximal tibia, decreases the number of adipocytes and TRAP-positive cells, and upregulates the expression of OCN. These findings indicate that naringin exhibits protective effects against diabetes-associated OP by increasing osteoblastogenesis and decreasing osteoclastogenesis and adipogenesis by inhibiting oxidative stress [97]. In addition, diabetes may worsen the bone indices, leading to decreased values for new bone formation, calvaria thickness, bone volume, the midline suture area, and the OCN concentration in streptozotocin (STZ)-treated mice. Naringin exhibits osteoanabolic activity and improves bone indices, promoting new bone formation [98].
The Janus-activated kinase 2 (JAK2)/signal transducer and the activator of transcription 3 (STAT3) signaling play a critical role in the pathogenesis and progression of OP. The activation of the JAK2/STAT3 signaling may stimulate the expression of RANKL and promote the differentiation of osteoclasts [99]. Another study also supports the idea that RANKL promotes osteoclastogenesis by inactivating the Akt and JAK2/STAT3 signaling pathways [100]. Naringin may significantly improve BMSC viability and osteogenic differentiation by suppressing JAK2/STAT3 signaling. In OVX-induced rat postmenopausal OP, naringin exhibits similar effects to AG490 (an inhibitor of JAK2/STAT3 signaling) to improve the bone parameters from dual-energy X-ray absorptiometry and micro-CT and suppresses the development of OP [101]. These results consistently support the finding that naringin ameliorates OVX-induced rat bone loss, increases the expression of osteocalcin, and promotes the osteogenic differentiation of BMSCs [102].
2.4. Potential Applications of Naringin in Bone Tissue Engineering
Titanium (Ti) and its alloys have demonstrated good biocompatibility and mechanical characteristics in clinical settings. However, Ti-implant-associated infection and tumor recurrence have challenged their application in osteosarcoma resection [103]. Zinc oxide nanoparticles (ZnO NPs), 3-carboxyphenylboronic acid (PBA), and naringin (NG) are modified to be ZnO-PBA-NG NPs, which are then immobilized on Ti substrates. This functional Ti substrate has pH-responsive characteristics and triggers the release of naringin due to the presence of bacterial infections and an acidic environment. In addition, this Ti substrate may induce oxidative stress to damage the bacterial biofilm and membrane, promote osteosarcoma cell apoptosis by stimulating the ERK signaling pathway, and stimulate osteoblast proliferation and differentiation [104].
At overly high concentrations, naringin may exhibit harmful effects on cells, while very low concentrations may be ineffective. The prevention of burst release and the facilitation of the controlled release of naringin may benefit cells. A hybrid depot of a naringin-loaded microsphere/sucrose acetate isobutyrate was prepared to control the release of naringin and prevent burst release, promoting the new bone formation rate [105]. A multifunctional mineralized collagen (Col) coating on Ti through metal–organic framework (MOF) nanocrystals was designed to control the release of naringin (NG). This substrate of Col/MOF/NG may induce osteogenic differentiation by stimulating the expression of BMP-2 and Sema3A in MSCs, as indicated by the upregulation of Collagen I and RUNX2 [106]. Another study reported that micro-Ti is covered with naringin (NA), chitosan, and gelatin multilayers, forming LBL(NA)-coated Ti. In an in vitro study, LBL(NA)-coated Ti exhibited a sustained release of naringin. In addition, LBL(NA)-coated Ti may promote the expression of ALP, RUNX-2, OCN, OPN, OPG, and COL I and suppress the expression of CTSK, NFAT, TRAP, and VATP, indicating the induction of osteoblastogenesis and the inhibition of osteoclastogenesis [107].
Additionally, researchers have explored the possibility of incorporating naringin into the electrospun nano-scaffold containing poly(ε-caprolactone) (PCL) and poly(ethylene glycol)-block-poly(ε-caprolactone) (PEG-b-PCL). Significantly, the burst release of naringin is reduced [108]. The electrospinning of the PLGA, PLLA, and PDLLA solutions with naringin, producing a naringin-loaded fiber mesh, may increase osteogenic differentiation and cellular proliferation and decrease the burst release of naringin [109]. A nanocomposite hydrogel, comprising the liposomal building blocks of naringin-loaded salmon-derived lecithin and the embedding of gelatin methacryloyl macro-sized hydrogels, was synthesized, and it may control the release of naringin and improve the characteristics of the hydrogel matrix [110].
One study reported the preparation of naringin (NG)/gelatin microspheres (GMs)/nanohydroxyapatite (nHA)/silk fibroin (SF) scaffolds. NG/GMs/nHA/SF scaffolds demonstrated good biocompatibility and biomechanical strength, enhanced the adhesion and proliferation of BMSCs, and increased the formation of calcium nodules, promoting osteogenic differentiation [111]. An NG/SF/HA scaffold was fabricated to repair bone defects, and it exhibits osteogenic and angiogenic properties. Specifically, naringin may facilitate the growth of human umbilical-cord-derived mesenchymal stem cells (hUCMSCs) in the SF/HA scaffold by enhancing the PI3K/AKT signaling pathway [112]. Naringin poly lactic-co-glycolic acid (PLGA) microspheres adhering to the SF/HA scaffold may sustain the release of naringin. The NG/PLGA/SF/HA scaffold has been demonstrated to promote the osteogenic differentiation of BMSCs by activating the Notch signaling pathway, as shown by the increased expressions of ALP, RUNX-2, BMP2, and OCN and increased calcium deposition [113]. Another study indicates that nHA/collagen (COL)/NG also exhibits desirable biocompatibility and promotes the osteogenic differentiation of BMSCs, as shown by the increased expressions of ALP, BMP2, OCN, and OPN and the increased number of calcium nodules. In an in vivo study, the nHA/COL/NG scaffold effectively repaired skull defects and exhibited great potential in bone tissue engineering [114].
Inflammatory responses affect the outcome of bone biomaterial implantation. Specifically, inflammation may induce the formation of a fibrous envelope, inhibiting the interaction of bone cells with the implant materials and promoting implantation failure. Ideally, the bone materials will induce osteogenic proliferation and differentiation and attenuate the inflammatory responses [115]. It has been reported that loading naringin into β-cyclodextrin-modified mesoporous bioactive glass nanoparticles (NG@CD-MBG) may promote macrophages to induce M2 polarization, inhibit inflammatory responses, induce osteogenesis, and suppress osteoclastogenesis. However, the over-transition of M1 to M2 may inhibit the activity of osteoclasts, leading to the delayed resorption of implant materials and old bone. Thus, pathological fibrosis and delayed bone healing may arise. NG@CD-MBG may effectively control the release of naringin, benefiting tissue regeneration [116]. A further study shows that naringin can rescue the TNFα-stimulated expression of p-IκBα and nuclear p65 and enhance the levels of RUNX-2 and Osx in BMSCs, inhibiting the NF-κB signaling pathway and promoting osteogenic differentiation [117].
3. The Protective Activities of Naringin against Intervertebral Disc Degeneration (IDD)
Lower back pain, a common and complicated disease, is closely associated with disability. Intervertebral disc degeneration (IDD) contributes to the development of lower back pain. More than 10% of 50-year-old and 60% of 70-year-old people have severe IDD [118]. Various factors, such as aging, immune dysregulation, inflammation, metabolic disorders, excessive mechanical loads, and insufficient nutritional supply, may promote the pathological development of IDD [119]. However, the potential molecular mechanism of IDD-associated lower back pain remains unclear. The intervertebral disc (IVD), an avascular connective tissue, is constituted by a central nucleus pulposus (NP), a peripheral annulus fibrosus (AF), and a cartilage endplate (CEP). ECM acts as the microenvironment for IVD cells, and it mediates the metabolism and functions of IVD cells. The pathological changes in IDD may involve a decreased supply of nutrition, the alterations of ECM components, and the apoptosis of IVD cells [120].
Natural compounds may be effective against IDD and low back pain. At a dose of 20 μg/mL, naringin may increase the proliferative activity of NP cells. In addition, naringin may suppress the production of TNFα, enhance the expression of BMP-2, collagen II, aggrecan, and SOX6, and inhibit the expression of MMP-3 in NP cells [54] (Table 1). It has been shown that inflammation plays a critical role in the development of IDD [121]. Pro-inflammatory cytokines, such as IL-1β and IL-6, may promote the expression of MMPs and ADAMTSs, which can induce the degradation of collagen II and aggrecan and contribute to the pathological development of IDD [122]. In IL-1β-treated human NP cells, naringin may decrease the expression of MMP-3, MMP-13, ADAMTS4, ADMATS5, IL-6, and TNFα and increase the production of collagen II and aggrecan by suppressing the NF-κB and p53 signaling pathways [55] (Table 1).
TNFα can also trigger an inflammatory cascade, which promotes mitochondrial dysfunctions and ROS generation in NP cells. Autophagy, an evolutionarily conserved stress-responsive process, can dispose of the damaged cytoplasmic organelles and transport them for their degradation in lysosomes. Autophagy contributes to the recycling of these damaged organelles for cell metabolism. The over-activation of autophagy may promote cell survival. The AMP-activated protein kinase (AMPK)/Sirt1 signaling pathway facilitates mitochondrial homeostasis by producing an autophagic effect [123]. Naringin may increase Beclin-1, the LC3-II/LC3-I ratio, and collagen II expression, decrease p62 and MMP-3 expression, and inhibit cell apoptosis by activating AMPK/Sirt1 signaling in TNFα-treated NP cells [56] (Table 1).
Additionally, naringin can enhance autophagy and suppress oxidative-stress-associated apoptosis by upregulating the AMPK signaling in NP cells. In an in vivo study, naringin was shown to ameliorate the pathological development of IDD in puncture-treated rats [124]. In cyclic stretch-treated rat AF cells, naringin consistently decreased cell apoptosis by suppressing oxidative stress and the NF-κB signaling pathway, delaying the pathological development of IDD [125]. Increased apoptosis of NP cells is one of the main pathological changes of IDD. In H2O2-treated NP-derived MSCs, naringin has exhibited protective activities against H2O2-induced oxidative stress, mitochondrial dysfunction, MMP expression, and cell apoptosis by activating the PI3K/AKT signaling pathway [57] (Table 1).
4. The Protective Activities of Naringin against Osteoarthritis (OA)
OA is associated with chronic inflammation, osteophyte formation, cartilage degeneration, and subchondral bone sclerosis. The global prevalence of OA has been estimated to be 23% among middle- to old-aged individuals [126]. Currently, no effective drugs are available to cure OA. Clinically, symptom relief becomes the effective strategy to treat OA. TNFα and IL-1βplay a central role in the pathological development of OA [127]. The inhibition of inflammatory responses is an effective therapeutic strategy for managing OA. Naringin can suppress the TNFα-induced inflammatory responses and ECM degradation in mouse chondrocytes by downregulating the NF-κB signaling pathway, as indicated by the decreased expression of IL-1β, iNOS, COX-2, MMP-13, and ADAMTS5. In ACLT-induced mouse OA models, naringin may significantly improve the OARSI scores and pathohistological changes and decrease the expression of catabolic factors [58] (Table 1).
The anti-inflammatory activity of naringin in LPS-treated RAW 264.7 cells and monosodium iodoacetate (MIA)-induced rat OA shows that naringin can reduce the generation of PGE2, NO, IL-6, and TNFα, protecting against OA development [59] (Table 1). Articular cartilage is an avascular tissue with limited self-repair abilities. MSCs demonstrate an ability to differentiate into cartilage cells [128]. A combination of naringin with rabbit BMSCs is effective in the repair of cartilage defects in rabbit knee joint cartilage. Mechanically, naringin/BMSCs significantly enhance the expression of TGFβ3 and SOX9, promoting chondrocyte differentiation and displaying satisfactory therapeutic effects [129]. The TGFβ/Smad signaling pathway is closely associated with the process of repairing cartilage injury. Combined with the acellular dermal matrix (ADM), naringin may significantly improve the pathological changes in the defect structures of cartilage in New Zealand rabbits by upregulating the expression of TGFβ2, TGFβ3, and SOX9 [60] (Table 1).
5. The Protective Activities of Naringin against Rheumatoid Arthritis (RA)
Rheumatoid arthritis (RA) is an autoimmune disease characterized by the progressive destruction of bone and cartilage due to chronic inflammation and T-cell and macrophage infiltration. No specific drugs are available to treat RA. The global prevalence of RA is estimated to be 0.5–1.0% [130]. Persistent inflammatory responses may result in synovial hyperplasia, joint deformity, and disability. Clinically, nonsteroidal anti-inflammatory drugs (NSAIDs), Janus kinase inhibitors, and disease-modifying anti-rheumatic drugs are used to improve the symptoms [131]. The pathogenesis of RA is complicated. Infection, genetics, and environmental factors contribute to RA development [132]. However, the potential molecular mechanisms that mediate the pathological development of RA remain unclear.
Naringin has demonstrated anti-inflammatory and pro-apoptotic activities in RA fibroblast-like synoviocytes (FLSs), as indicated by the decreased expression of IL-1, IL-6, and IL-8, the increased expression of caspase-3 and an increased Bax/Bcl-2 ratio, and attenuated expression of MMP-1, MMP-2, and MMP-13; it achieves this by downregulating the MAPK/ERK and PI3K/AKT signaling pathways [61] (Table 1). A combinational therapy against inflammation and arthritis has become a promising strategy. Naringin-containing combination liposomal formulations (CLFs) can significantly improve both paw edema and the arthritic score in FCA-induced rat RA models [133].
6. The Protective Activities of Naringin against Femoral Head (FH) Diseases
Femoral head (FH) disease, a refractory disease in bone, can be separated into invasive and non-invasive clinical groups. Skeletal trauma, such as femoral neck fracture and hip dislocation, can be included in the invasive group. Steroid- and alcohol-induced FH diseases are non-invasive [134]. The incidence of osteonecrosis of the FH (ONFH) is 2.91 cases per 100,000 person-years in Japan [135]. In Korea, the estimated yearly prevalence was 37.96/100,000 in 2006 [136]. In China, there were approximately 8.12 million cases among Chinese people aged ≥15 in 2010 [137]. Clinically, FH diseases are considered complications of glucocorticoid therapy. However, the underlying molecular mechanisms of glucocorticoid-induced FH diseases are still unelucidated. Fat embolism, vascular thrombosis, osteocyte apoptosis, and oxidative stress contribute to steroid-induced osteonecrosis in the femoral head [138]. The protective effects of naringin on steroid-induced avascular necrosis of the femoral head (SANFH) have been investigated. Naringin can protect against methylprednisolone (MPS)-induced increases in the total cholesterol and LDL/HDL ratio, decreases in the serum levels of osteocalcin, the downregulation of caspase-3 expression, and the inhibition of osteoblast differentiation by enhancing the protein expression of PPARγ, Notch, β-catenin, and p-AKT [62] (Table 1). Naringin stimulates osteogenesis and osteocyte proliferation and suppresses osteoclastogenesis and osteocyte apoptosis by activating the AKT/Bad signaling pathway. Specifically, naringin promotes Bcl-2 expression and decreases Bax and cleaved caspase-3 expression, inhibiting apoptosis in Dex-treated MLO-Y4 cells. In addition, naringin upregulates the expression of RUNX2, OPG, and collagen I and downregulates the expression of RANKL, promoting osteogenesis and inhibiting osteoclast formation [63] (Table 1).
7. The Protective Activities of Naringin against Bone and Cartilage Tumors
The multiple pharmacological properties of naringin suggest its beneficial effects on the therapeutic management of cancers. The preventive activities of naringin against tumor development in humans have been reported in detail [139]. The potential molecular mechanisms of naringin in counteracting tumor development may include, at least in part, the MAPK/NF-κB, TGFβ/Smad, Wnt/β-catenin, and JAK2/STAT3 signaling pathways [140]. Osteosarcoma is one of the most common types of bone cancer. The annual incidence of osteosarcoma is 3.1 per million [141]. Treatment for osteosarcoma involves surgical resection, chemotherapy, and interventional therapy. Recently, adjuvant chemotherapy has increased the survival rate, and the development of multidrug resistance has posed challenges to the therapeutic management of osteosarcoma [142]. Naringin inhibits proliferative and invasive activities and promotes apoptosis in human osteosarcoma cells by suppressing the expression of Zeb1, which is a transcriptional factor involved in tumor metastasis. In an in vivo study, naringin reduced the formation of tumor nodules in a liver injected with MG63 cells [64] (Table 1). Vascular cell adhesion molecule-1 (VCAM-1) is also associated with tumor metastasis. Naringin also suppresses the migration and invasion of malignant cartilaginous neoplasms, as evidenced in the human chondrosarcoma JJ012 and SW1353 cells by increasing the expression of miR-126 and decreasing the expression of VCAM-1. However, naringin does not affect the cell death of human chondrosarcoma, which is the second most malignant bone tumor and accounts for 10–15% of all primary bone tumors [65,143] (Table 1). There is not a great deal of information on the protective activity of naringin against bone and cartilage tumors. More efforts are still needed to elucidate the potential mechanism of naringin in regulating the biological actions of tumor cells.
8. The Protective Activities of Naringin against Tibial Dyschondroplasia
Tibial dyschondroplasia (TD) is characterized by ambulation dysfunction, growth retardation, tibial bone deformation, and avascular nonmineralized growth plates. Ihh increases the maturation and proliferation of chondrocytes, while PTHrP suppresses chondrocyte maturation and proliferation in endochondral ossification. The dysregulation of the Ihh/PTHrP axis is closely associated with various bone diseases [144]. In thiram-induced TD broiler chickens, naringin, at a dose of 30 mg/kg, can effectively improve the thiram-induced pathological changes by decreasing Ihh expression and increasing PTHrP expression. Specifically, naringin can increase growth performance, recuperate growth plate width, improve functions, and enhance the levels of antioxidant enzymes [66] (Table 1).
9. Conclusions and Future Directions
Naringin exhibits promising therapeutic effects against bone and cartilage disorders, including OP, OA, IDD, RA, and FH diseases, bone and cartilage tumors, and TD. Naringin exhibits osteoprotective effects against OP both in vivo and in vitro by inducing osteogenic differentiation and inhibiting osteoclast formation. The potential molecular mechanisms of naringin in the bone system might be associated with the upregulation of BMP-2 and Wnt/β-catenin as well as the angiogenesis and downregulation of oxidative stress and inflammation. Numerous studies on the potential biomaterial-based applications of naringin have been explored, aiming to decrease its degradation and sustain its release. In addition, naringin also exhibits protective activities against IDD, OA, and RA by ameliorating inflammatory responses and oxidative stress and suppressing cell apoptosis and ECM degradation.
Naringin can be beneficial as a medication for bone and cartilage disorders due to its ability to mediate several signaling pathways. However, naringin has yet to obtain approval as a single or combinational agent for therapeutic use in treating bone and cartilage disorders in the clinic. The potential drug targets of naringin should be demonstrated. Most studies on naringin are investigated in vitro or in animals. Continued efforts to improve bioavailability, pharmacokinetic profiles, and bone/cartilage-target drug delivery systems are still needed. It is essential to elucidate the potential biological functions of naringin in clinical practice.
Abbreviations
OP, osteoporosis; OA, osteoarthritis; IDD, intervertebral disc degeneration; RA, rheumatoid arthritis; FH, femoral head; TD, tibial dyschondroplasia; MSCs; mesenchymal stromal stem cells; BMD, bone mineral density; NF-κB, nuclear factor-κB; RANKL, receptor activator of nuclear factor kappa-B ligand; PTH1R, parathyroid hormone-1 receptor; HMG-CoA, hydroxy-methylglutaryl coenzyme A; BMP-2, bone morphogenetic protein-2; BMSCs, bone mesenchymal stem cells; PPARγ, peroxisome proliferators-activated receptor γ; Sost, sclerosteosis; RUNX2, Runt-related transcription factor-2; TGFβ1, transforming growth factor β1; Smad: suppressor of mothers against decapentaplegic; CXCL-5, C-X-C motif chemokine-5; Osx, osterix; LPS, lipopolysaccharide; BMPRs, BMP receptors; Foxc2, Forkhead box C2; IHH, Indian hedgehog; SERMS, estrogen and selective estrogen receptor modulators; OC/OCN, osteocalcin; CTX-1, C-terminal telopeptides of type I collagen; VEGF, vascular endothelial growth factor; SOD, superoxide dismutase; GSH, glutathione; CAT, catalase; GPX, glutathione peroxidase; JAK2, Janus-activated kinase 2; STAT3, signal transducer and the activator of transcription 3; MMPs, matrix metalloproteinases; ADAMTSs, a disintegrin and metalloproteinase with thrombospondins; COX-2, cyclooxygenase; AMPK, adenosine 5′-monophosphate (AMP)-activated protein kinase; PGE2, Prostaglandin E2; SOX9, SRY-Box transcription factor 9; VCAM-1, vascular cell adhesion molecule 1.
Author Contributions
Conceptualization, X.L.; methodology, X.L.; validation, X.L., J.G. and X.D.; writing—original draft preparation, J.G., X.D., Y.L., J.L. and X.L.; writing—review and editing, J.G., X.D., Y.L., J.L. and X.L. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data used to support the findings of this study are included within the article.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was funded by the Ganzhou United Science and Technology Program, grant number 2022—YB1495.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Wen J., Cai D., Gao W., He R., Li Y., Zhou Y., Klein T., Xiao L., Xiao Y. Osteoimmunomodulatory Nanoparticles for Bone Regeneration. Nanomaterials. 2023;13:692. doi: 10.3390/nano13040692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zan P., Wang H., Cai Z., Shen J., Sun W. Revision surgeries for tumor endoprostheses around the knee joint: A mid-long-term follow-up of 20 cases. World J. Surg. Oncol. 2022;20:76. doi: 10.1186/s12957-022-02542-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li Y., Li L., Li X., Luo B., Ye Q., Wang H., Yang L., Zhu X., Han L., Zhang R., et al. A mechanistic review of chinese medicine polyphenols on bone formation and resorption. Front. Pharm. 2022;13:1017538. doi: 10.3389/fphar.2022.1017538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Koushik T.M., Miller C.M., Antunes E. Bone Tissue Engineering Scaffolds: Function of Multi-Material Hierarchically Structured Scaffolds. Adv. Health Mater. 2022;12:e2202766. doi: 10.1002/adhm.202202766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wollenhaupt J., Lee E.B., Curtis J.R., Silverfield J., Terry K., Soma K., Mojcik C., DeMasi R., Strengholt S., Kwok K., et al. Safety and efficacy of tofacitinib for up to 9.5 years in the treatment of rheumatoid arthritis: Final results of a global, open-label, long-term extension study. Arthritis Res. Ther. 2019;21:89. doi: 10.1186/s13075-019-1866-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Singh S., Fumery M., Singh A.G., Singh N., Prokop L.J., Dulai P.S., Sandborn W.J., Curtis J.R. Comparative Risk of Cardiovascular Events With Biologic and Synthetic Disease-Modifying Antirheumatic Drugs in Patients With Rheumatoid Arthritis: A Systematic Review and Meta-Analysis. Arthritis Care Res. 2020;72:561–576. doi: 10.1002/acr.23875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rzhepakovsky I., Anusha Siddiqui S., Avanesyan S., Benlidayi M., Dhingra K., Dolgalev A., Enukashvily N., Fritsch T., Heinz V., Kochergin S., et al. Anti-arthritic effect of chicken embryo tissue hydrolyzate against adjuvant arthritis in rats (X-ray microtomographic and histopathological analysis) Food Sci. Nutr. 2021;9:5648–5669. doi: 10.1002/fsn3.2529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schulze-Tanzil G. Experimental Therapeutics for the Treatment of Osteoarthritis. J. Exp. Pharmacol. 2021;13:101–125. doi: 10.2147/JEP.S237479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rasheed S., Rehman K., Shahid M., Suhail S., Akash M.S.H. Therapeutic potentials of genistein: New insights and perspectives. J. Food Biochem. 2022;46:e14228. doi: 10.1111/jfbc.14228. [DOI] [PubMed] [Google Scholar]
- 10.Seyedi Z., Amiri M.S., Mohammadzadeh V., Hashemzadeh A., Haddad-Mashadrizeh A., Mashreghi M., Qayoomian M., Hashemzadeh M.R., Simal-Gandara J., Taghavizadeh Yazdi M.E. Icariin: A Promising Natural Product in Biomedicine and Tissue Engineering. J. Funct. Biomater. 2023;14:44. doi: 10.3390/jfb14010044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ravetti S., Garro A.G., Gaitán A., Murature M., Galiano M., Brignone S.G., Palma S.D. Naringin: Nanotechnological Strategies for Potential Pharmaceutical Applications. Pharmaceutics. 2023;15:863. doi: 10.3390/pharmaceutics15030863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang Y., Lei X., Xu H., Liu G., Wang Y., Sun H., Geng F., Zhang N. Tissue Distribution of Total Flavonoids Extracts of Drynariae Rhizoma in Young and Old Rats by UPLC-MS/MS Determination. J. Anal. Methods Chem. 2022;2022:2447945. doi: 10.1155/2022/2447945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stabrauskiene J., Kopustinskiene D.M., Lazauskas R., Bernatoniene J. Naringin and Naringenin: Their Mechanisms of Action and the Potential Anticancer Activities. Biomedicines. 2022;10:1686. doi: 10.3390/biomedicines10071686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen R., Qi Q.L., Wang M.T., Li Q.Y. Therapeutic potential of naringin: An overview. Pharm. Biol. 2016;54:3203–3210. doi: 10.1080/13880209.2016.1216131. [DOI] [PubMed] [Google Scholar]
- 15.Yang Y., Trevethan M., Wang S., Zhao L. Beneficial effects of citrus flavanones naringin and naringenin and their food sources on lipid metabolism: An update on bioavailability, pharmacokinetics, and mechanisms. J. Nutr. Biochem. 2022;104:108967. doi: 10.1016/j.jnutbio.2022.108967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Memariani Z., Abbas S.Q., Ul Hassan S.S., Ahmadi A., Chabra A. Naringin and naringenin as anticancer agents and adjuvants in cancer combination therapy: Efficacy and molecular mechanisms of action, a comprehensive narrative review. Pharm. Res. 2021;171:105264. doi: 10.1016/j.phrs.2020.105264. [DOI] [PubMed] [Google Scholar]
- 17.Li S.Q., Dong S., Su Z.H., Zhang H.W., Peng J.B., Yu C.Y., Zou Z.M. Comparative pharmacokinetics of naringin in rat after oral administration of chaihu-shu-gan-san aqueous extract and naringin alone. Metabolites. 2013;3:867–880. doi: 10.3390/metabo3040867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zeng X., Yao H., Zheng Y., He Y., He Y., Rao H., Li P., Su W. Tissue distribution of naringin and derived metabolites in rats after a single oral administration. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2020;1136:121846. doi: 10.1016/j.jchromb.2019.121846. [DOI] [PubMed] [Google Scholar]
- 19.Manach C., Williamson G., Morand C., Scalbert A., Rémésy C. Bioavailability and bioefficacy of polyphenols in humans. I. Review of 97 bioavailability studies. Am. J. Clin. Nutr. 2005;81:230s–242s. doi: 10.1093/ajcn/81.1.230S. [DOI] [PubMed] [Google Scholar]
- 20.Zeng X., Su W., Zheng Y., He Y., He Y., Rao H., Peng W., Yao H. Pharmacokinetics, Tissue Distribution, Metabolism, and Excretion of Naringin in Aged Rats. Front. Pharm. 2019;10:34. doi: 10.3389/fphar.2019.00034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li P., Wang S., Guan X., Liu B., Wang Y., Xu K., Peng W., Su W., Zhang K. Acute and 13 weeks subchronic toxicological evaluation of naringin in Sprague-Dawley rats. Food Chem. Toxicol. Int. J. Publ. Br. Ind. Biol. Res. Assoc. 2013;60:1–9. doi: 10.1016/j.fct.2013.07.019. [DOI] [PubMed] [Google Scholar]
- 22.Yu K.E., Alder K.D., Morris M.T., Munger A.M., Lee I., Cahill S.V., Kwon H.K., Back J., Lee F.Y. Re-appraising the potential of naringin for natural, novel orthopedic biotherapies. Ther. Adv. Musculoskelet. Dis. 2020;12:1759720x20966135. doi: 10.1177/1759720X20966135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Meng D., Song J., Yi Y., Li J., Zhang T., Shu Y., Wu X. Controlled released naringin-loaded liposome/sucrose acetate isobutyrate hybrid depot for osteogenesis in vitro and in vivo. Front. Bioeng. Biotechnol. 2022;10:1097178. doi: 10.3389/fbioe.2022.1097178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xiao P.L., Cui A.Y., Hsu C.J., Peng R., Jiang N., Xu X.H., Ma Y.G., Liu D., Lu H.D. Global, regional prevalence, and risk factors of osteoporosis according to the World Health Organization diagnostic criteria: A systematic review and meta-analysis. Osteoporos. Int. J. Establ. Result Coop. Eur. Found. Osteoporos. Natl. Osteoporos. Found. USA. 2022;33:2137–2153. doi: 10.1007/s00198-022-06454-3. [DOI] [PubMed] [Google Scholar]
- 25.van den Blink Q.U., Garcez K., Henson C.C., Davidson S.E., Higham C.E. Pharmacological interventions for the prevention of insufficiency fractures and avascular necrosis associated with pelvic radiotherapy in adults. Cochrane Database Syst. Rev. 2018;4:Cd010604. doi: 10.1002/14651858.CD010604.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Keaveny T.M., Crittenden D.B., Bolognese M.A., Genant H.K., Engelke K., Oliveri B., Brown J.P., Langdahl B.L., Yan C., Grauer A., et al. Greater Gains in Spine and Hip Strength for Romosozumab Compared With Teriparatide in Postmenopausal Women With Low Bone Mass. J. Bone Miner. Res. 2017;32:1956–1962. doi: 10.1002/jbmr.3176. [DOI] [PubMed] [Google Scholar]
- 27.Reid I.R., Billington E.O. Drug therapy for osteoporosis in older adults. Lancet. 2022;399:1080–1092. doi: 10.1016/S0140-6736(21)02646-5. [DOI] [PubMed] [Google Scholar]
- 28.Chandran M. The why and how of sequential and combination therapy in osteoporosis. A review of the current evidence. Arch. Endocrinol. Metab. 2022;66:724–738. doi: 10.20945/2359-3997000000564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sharpton S.R., Loomba R. Emerging role of statin therapy in the prevention and management of cirrhosis, portal hypertension, and HCC. Hepatology. 2023 doi: 10.1097/HEP.0000000000000278. [DOI] [PubMed] [Google Scholar]
- 30.Wong R.W., Rabie A.B. Effect of naringin on bone cells. J. Orthop. Res. 2006;24:2045–2050. doi: 10.1002/jor.20279. [DOI] [PubMed] [Google Scholar]
- 31.Chiba H., Kim H., Matsumoto A., Akiyama S., Ishimi Y., Suzuki K., Uehara M. Hesperidin prevents androgen deficiency-induced bone loss in male mice. Phytother. Res. PTR. 2014;28:289–295. doi: 10.1002/ptr.5001. [DOI] [PubMed] [Google Scholar]
- 32.Habauzit V., Sacco S.M., Gil-Izquierdo A., Trzeciakiewicz A., Morand C., Barron D., Pinaud S., Offord E., Horcajada M.N. Differential effects of two citrus flavanones on bone quality in senescent male rats in relation to their bioavailability and metabolism. Bone. 2011;49:1108–1116. doi: 10.1016/j.bone.2011.07.030. [DOI] [PubMed] [Google Scholar]
- 33.Sacco S.M., Saint C., LeBlanc P.J., Ward W.E. Maternal Consumption of Hesperidin and Naringin Flavanones Exerts Transient Effects to Tibia Bone Structure in Female CD-1 Offspring. Nutrients. 2017;9:250. doi: 10.3390/nu9030250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ge X., Zhou G. Protective effects of naringin on glucocorticoid-induced osteoporosis through regulating the PI3K/Akt/mTOR signaling pathway. Am. J. Transl. Res. 2021;13:6330–6341. [PMC free article] [PubMed] [Google Scholar]
- 35.Zhang P., Dai K.R., Yan S.G., Yan W.Q., Zhang C., Chen D.Q., Xu B., Xu Z.W. Effects of naringin on the proliferation and osteogenic differentiation of human bone mesenchymal stem cell. Eur. J. Pharm. 2009;607:1–5. doi: 10.1016/j.ejphar.2009.01.035. [DOI] [PubMed] [Google Scholar]
- 36.Fan J., Li J., Fan Q. Naringin promotes differentiation of bone marrow stem cells into osteoblasts by upregulating the expression levels of microRNA-20a and downregulating the expression levels of PPARγ. Mol. Med. Rep. 2015;12:4759–4765. doi: 10.3892/mmr.2015.3996. [DOI] [PubMed] [Google Scholar]
- 37.Wang R., Bao B., Wang S., Elango J., Wu W. Fabrication of Chinese Traditional Medicines incorporated collagen biomaterials for human bone marrow mesenchymal stem cells. Biomed. Pharmacother. Biomed. Pharmacother. 2021;139:111659. doi: 10.1016/j.biopha.2021.111659. [DOI] [PubMed] [Google Scholar]
- 38.Yin L., Cheng W., Qin Z., Yu H., Yu Z., Zhong M., Sun K., Zhang W. Effects of Naringin on Proliferation and Osteogenic Differentiation of Human Periodontal Ligament Stem Cells In Vitro and In Vivo. Stem Cells Int. 2015;2015:758706. doi: 10.1155/2015/758706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Suwittayarak R., Klincumhom N., Ngaokrajang U., Namangkalakul W., Ferreira J.N., Pavasant P., Osathanon T. Shear Stress Enhances the Paracrine-Mediated Immunoregulatory Function of Human Periodontal Ligament Stem Cells via the ERK Signalling Pathway. Int. J. Mol. Sci. 2022;23:7119. doi: 10.3390/ijms23137119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wei K., Xie Y., Chen T., Fu B., Cui S., Wang Y., Cai G., Chen X. ERK1/2 signaling mediated naringin-induced osteogenic differentiation of immortalized human periodontal ligament stem cells. Biochem. Biophys. Res. Commun. 2017;489:319–325. doi: 10.1016/j.bbrc.2017.05.130. [DOI] [PubMed] [Google Scholar]
- 41.Yang X., Dong J., Hao Y., Qi Y., Liang J., Yan L., Wang W. Naringin Alleviates H2O2-Inhibited Osteogenic Differentiation of Human Adipose-Derived Stromal Cells via Wnt/β-Catenin Signaling. Evid.-Based Complement. Altern. Med. ECAM. 2022;2022:3126094. doi: 10.1155/2022/3126094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wang L., Zhang Y.G., Wang X.M., Ma L.F., Zhang Y.M. Naringin protects human adipose-derived mesenchymal stem cells against hydrogen peroxide-induced inhibition of osteogenic differentiation. Chem. Biol. Interact. 2015;242:255–261. doi: 10.1016/j.cbi.2015.10.010. [DOI] [PubMed] [Google Scholar]
- 43.Liu M., Li Y., Yang S.T. Effects of naringin on the proliferation and osteogenic differentiation of human amniotic fluid-derived stem cells. J. Tissue Eng. Regen. Med. 2017;11:276–284. doi: 10.1002/term.1911. [DOI] [PubMed] [Google Scholar]
- 44.Lin F., Zhu Y., Hu G. Naringin promotes cellular chemokine synthesis and potentiates mesenchymal stromal cell migration via the Ras signaling pathway. Exp. Ther. Med. 2018;16:3504–3510. doi: 10.3892/etm.2018.6634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wang H., Li C., Li J., Zhu Y., Jia Y., Zhang Y., Zhang X., Li W., Cui L., Li W., et al. Naringin enhances osteogenic differentiation through the activation of ERK signaling in human bone marrow mesenchymal stem cells. Iran. J. Basic Med. Sci. 2017;20:408–414. doi: 10.22038/ijbms.2017.8582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Li L., Li J., Li S., Chen H., Wu Y., Qiu Y. IL-37 alleviates alveolar bone resorption and inflammatory response through the NF-κB/NLRP3 signaling pathway in male mice with periodontitis. Arch. Oral Biol. 2023;147:105629. doi: 10.1016/j.archoralbio.2023.105629. [DOI] [PubMed] [Google Scholar]
- 47.Ang E.S., Yang X., Chen H., Liu Q., Zheng M.H., Xu J. Naringin abrogates osteoclastogenesis and bone resorption via the inhibition of RANKL-induced NF-κB and ERK activation. FEBS Lett. 2011;585:2755–2762. doi: 10.1016/j.febslet.2011.07.046. [DOI] [PubMed] [Google Scholar]
- 48.Chen L.L., Lei L.H., Ding P.H., Tang Q., Wu Y.M. Osteogenic effect of Drynariae rhizoma extracts and Naringin on MC3T3-E1 cells and an induced rat alveolar bone resorption model. Arch. Oral Biol. 2011;56:1655–1662. doi: 10.1016/j.archoralbio.2011.06.008. [DOI] [PubMed] [Google Scholar]
- 49.Wei M., Yang Z., Li P., Zhang Y., Sse W.C. Anti-osteoporosis activity of naringin in the retinoic acid-induced osteoporosis model. Am. J. Chin. Med. 2007;35:663–667. doi: 10.1142/S0192415X07005156. [DOI] [PubMed] [Google Scholar]
- 50.Jin H., Jiang N., Xu W., Zhang Z., Yang Y., Zhang J., Xu H. Effect of flavonoids from Rhizoma Drynariae on osteoporosis rats and osteocytes. Biomed. Pharmacother. Biomed. Pharmacother. 2022;153:113379. doi: 10.1016/j.biopha.2022.113379. [DOI] [PubMed] [Google Scholar]
- 51.Li F., Sun X., Ma J., Ma X., Zhao B., Zhang Y., Tian P., Li Y., Han Z. Naringin prevents ovariectomy-induced osteoporosis and promotes osteoclasts apoptosis through the mitochondria-mediated apoptosis pathway. Biochem. Biophys. Res. Commun. 2014;452:629–635. doi: 10.1016/j.bbrc.2014.08.117. [DOI] [PubMed] [Google Scholar]
- 52.Sun X., Li F., Ma X., Ma J., Zhao B., Zhang Y., Li Y., Lv J., Meng X. The Effects of Combined Treatment with Naringin and Treadmill Exercise on Osteoporosis in Ovariectomized Rats. Sci. Rep. 2015;5:13009. doi: 10.1038/srep13009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Li C., Zhang J., Lv F., Ge X., Li G. Naringin protects against bone loss in steroid-treated inflammatory bowel disease in a rat model. Arch. Biochem. Biophys. 2018;650:22–29. doi: 10.1016/j.abb.2018.05.011. [DOI] [PubMed] [Google Scholar]
- 54.Li N., Whitaker C., Xu Z., Heggeness M., Yang S.Y. Therapeutic effects of naringin on degenerative human nucleus pulposus cells for discogenic low back pain. Spine J. 2016;16:1231–1237. doi: 10.1016/j.spinee.2016.05.007. [DOI] [PubMed] [Google Scholar]
- 55.Gao G., Chang F., Zhang T., Huang X., Yu C., Hu Z., Ji M., Duan Y. Naringin Protects Against Interleukin 1β (IL-1β)-Induced Human Nucleus Pulposus Cells Degeneration via Downregulation Nuclear Factor kappa B (NF-κB) Pathway and p53 Expression. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2019;25:9963–9972. doi: 10.12659/MSM.918597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chen R., Gao S., Guan H., Zhang X., Gao Y., Su Y., Song Y., Jiang Y., Li N. Naringin protects human nucleus pulposus cells against TNF-α-induced inflammation, oxidative stress, and loss of cellular homeostasis by enhancing autophagic flux via AMPK/SIRT1 activation. Oxid Med. Cell Longev. 2022;2022:7655142. doi: 10.1155/2022/7655142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Nan L.P., Wang F., Ran D., Zhou S.F., Liu Y., Zhang Z., Huang Z.N., Wang Z.Y., Wang J.C., Feng X.M., et al. Naringin alleviates H2O2-induced apoptosis via the PI3K/Akt pathway in rat nucleus pulposus-derived mesenchymal stem cells. Connect. Tissue Res. 2020;61:554–567. doi: 10.1080/03008207.2019.1631299. [DOI] [PubMed] [Google Scholar]
- 58.Zhao Y., Li Z., Wang W., Zhang H., Chen J., Su P., Liu L., Li W. Naringin Protects Against Cartilage Destruction in Osteoarthritis Through Repression of NF-κB Signaling Pathway. Inflammation. 2016;39:385–392. doi: 10.1007/s10753-015-0260-8. [DOI] [PubMed] [Google Scholar]
- 59.Xu Q., Zhang Z.F., Sun W.X. Effect of Naringin on Monosodium Iodoacetate-Induced Osteoarthritis Pain in Rats. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2017;23:3746–3751. doi: 10.12659/MSM.902396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ye C., Chen J., Qu Y., Qi H., Wang Q., Yang Z., Wu A., Wang F., Li P. Naringin in the repair of knee cartilage injury via the TGF-β/ALK5/Smad2/3 signal transduction pathway combined with an acellular dermal matrix. J. Orthop. Transl. 2022;32:1–11. doi: 10.1016/j.jot.2021.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Aihaiti Y., Song Cai Y., Tuerhong X., Ni Yang Y., Ma Y., Shi Zheng H., Xu K., Xu P. Therapeutic Effects of Naringin in Rheumatoid Arthritis: Network Pharmacology and Experimental Validation. Front. Pharm. 2021;12:672054. doi: 10.3389/fphar.2021.672054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Huang D., Li Z., Chen B., Fang G., Sun X., Li F., Xu H., Chen Y., Ding W. Naringin protects against steroid-induced avascular necrosis of the femoral head through upregulation of PPARγ and activation of the Notch signaling pathway. Mol. Med. Rep. 2018;17:3328–3335. doi: 10.3892/mmr.2017.8247. [DOI] [PubMed] [Google Scholar]
- 63.Kuang M.J., Zhang W.H., He W.W., Sun L., Ma J.X., Wang D., Ma X.L. Naringin regulates bone metabolism in glucocorticoid-induced osteonecrosis of the femoral head via the Akt/Bad signal cascades. Chem. Biol. Interact. 2019;304:97–105. doi: 10.1016/j.cbi.2019.03.008. [DOI] [PubMed] [Google Scholar]
- 64.Ming H., Chuang Q., Jiashi W., Bin L., Guangbin W., Xianglu J. Naringin targets Zeb1 to suppress osteosarcoma cell proliferation and metastasis. Aging. 2018;10:4141–4151. doi: 10.18632/aging.101710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Tan T.W., Chou Y.E., Yang W.H., Hsu C.J., Fong Y.C., Tang C.H. Naringin suppress chondrosarcoma migration through inhibition vascular adhesion molecule-1 expression by modulating miR-126. Int. Immunopharmacol. 2014;22:107–114. doi: 10.1016/j.intimp.2014.06.029. [DOI] [PubMed] [Google Scholar]
- 66.Jiang X., Li A., Wang Y., Iqbal M., Waqas M., Yang H., Li Z., Mehmood K., Qamar H., Li J. Ameliorative effect of naringin against thiram-induced tibial dyschondroplasia in broiler chicken. Environ. Sci. Pollut Res. Int. 2020;27:11337–11348. doi: 10.1007/s11356-020-07732-5. [DOI] [PubMed] [Google Scholar]
- 67.Yang C., Liu W., Zhang X., Zeng B., Qian Y. Naringin increases osteoprotegerin expression in fibroblasts from periprosthetic membrane by the Wnt/β-catenin signaling pathway. J. Orthop. Surg. Res. 2020;15:600. doi: 10.1186/s13018-020-02145-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Yu X., Zhao X., Wu T., Zhou Z., Gao Y., Wang X., Zhang C.Q. Inhibiting wear particles-induced osteolysis with naringin. Int. Orthop. 2013;37:137–143. doi: 10.1007/s00264-012-1668-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Li N., Xu Z., Wooley P.H., Zhang J., Yang S.Y. Therapeutic potentials of naringin on polymethylmethacrylate induced osteoclastogenesis and osteolysis, in vitro and in vivo assessments. Drug Des. Dev. Ther. 2014;8:1–11. doi: 10.2147/dddt.S52714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Yu G.Y., Zheng G.Z., Chang B., Hu Q.X., Lin F.X., Liu D.Z., Wu C.C., Du S.X., Li X.D. Naringin Stimulates Osteogenic Differentiation of Rat Bone Marrow Stromal Cells via Activation of the Notch Signaling Pathway. Stem Cells Int. 2016;2016:7130653. doi: 10.1155/2016/7130653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Sun C., Chen X., Yang S., Jin C., Ding K., Chen C. LBP1C-2 from Lycium barbarum alleviated age-related bone loss by targeting BMPRIA/BMPRII/Noggin. Carbohydr. Polym. 2023;310:120725. doi: 10.1016/j.carbpol.2023.120725. [DOI] [PubMed] [Google Scholar]
- 72.Dong G.C., Ma T.Y., Li C.H., Chi C.Y., Su C.M., Huang C.L., Wang Y.H., Lee T.M. A study of Drynaria fortunei in modulation of BMP–2 signalling by bone tissue engineering. Turk. J. Med. Sci. 2020;50:1444–1453. doi: 10.3906/sag-2001-148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mang T., Kleinschmidt-Doerr K., Ploeger F., Schoenemann A., Lindemann S., Gigout A. BMPR1A is necessary for chondrogenesis and osteogenesis, whereas BMPR1B prevents hypertrophic differentiation. J. Cell Sci. 2020;133:jcs246934. doi: 10.1242/jcs.246934. [DOI] [PubMed] [Google Scholar]
- 74.Wong R.W., Rabie A.B. Effect of naringin collagen graft on bone formation. Biomaterials. 2006;27:1824–1831. doi: 10.1016/j.biomaterials.2005.11.009. [DOI] [PubMed] [Google Scholar]
- 75.Wu J.B., Fong Y.C., Tsai H.Y., Chen Y.F., Tsuzuki M., Tang C.H. Naringin-induced bone morphogenetic protein-2 expression via PI3K, Akt, c-Fos/c-Jun and AP-1 pathway in osteoblasts. Eur. J. Pharm. 2008;588:333–341. doi: 10.1016/j.ejphar.2008.04.030. [DOI] [PubMed] [Google Scholar]
- 76.Liu K., Ge H., Liu C., Jiang Y., Yu Y., Zhou Z. Notch-RBPJ Pathway for the Differentiation of Bone Marrow Mesenchymal Stem Cells in Femoral Head Necrosis. Int. J. Mol. Sci. 2023;24:6295. doi: 10.3390/ijms24076295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Souza P.G., Adolpho L.F., Lopes H.B., Weffort D., Souza A.T.P., Oliveira F.S., Rosa A.L., Beloti M.M. Effects of Modulation of the Hedgehog and Notch Signaling Pathways on Osteoblast Differentiation Induced by Titanium with Nanotopography. J. Funct. Biomater. 2023;14:79. doi: 10.3390/jfb14020079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Viale-Bouroncle S., Gosau M., Morsczeck C. NOTCH1 signaling regulates the BMP2/DLX-3 directed osteogenic differentiation of dental follicle cells. Biochem. Biophys. Res. Commun. 2014;443:500–504. doi: 10.1016/j.bbrc.2013.11.120. [DOI] [PubMed] [Google Scholar]
- 79.Ge J., Yu Y.J., Li J.Y., Li M.Y., Xia S.M., Xue K., Wang S.Y., Yang C. Activating Wnt/β-catenin signaling by autophagic degradation of APC contributes to the osteoblast differentiation effect of soy isoflavone on osteoporotic mesenchymal stem cells. Acta Pharm. Sin. 2023 doi: 10.1038/s41401-023-01066-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wang D., Ma W., Wang F., Dong J., Wang D., Sun B., Wang B. Stimulation of Wnt/β-Catenin Signaling to Improve Bone Development by Naringin via Interacting with AMPK and Akt. Cell. Physiol. Biochem. Int. J. Exp. Cell. Physiol. Biochem. Pharmacol. 2015;36:1563–1576. doi: 10.1159/000430319. [DOI] [PubMed] [Google Scholar]
- 81.Gerbaix M., Vico L., Ferrari S.L., Bonnet N. Periostin expression contributes to cortical bone loss during unloading. Bone. 2015;71:94–100. doi: 10.1016/j.bone.2014.10.011. [DOI] [PubMed] [Google Scholar]
- 82.Hayashi M., Nakashima T., Taniguchi M., Kodama T., Kumanogoh A., Takayanagi H. Osteoprotection by semaphorin 3A. Nature. 2012;485:69–74. doi: 10.1038/nature11000. [DOI] [PubMed] [Google Scholar]
- 83.Ma X., Lv J., Sun X., Ma J., Xing G., Wang Y., Sun L., Wang J., Li F., Li Y., et al. Naringin ameliorates bone loss induced by sciatic neurectomy and increases Semaphorin 3A expression in denervated bone. Sci. Rep. 2016;6:24562. doi: 10.1038/srep24562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Wang Y., Dong Z., Yang R., Zong S., Wei X., Wang C., Guo L., Sun J., Li H., Li P. Inactivation of Ihh in Sp7-Expressing Cells Inhibits Osteoblast Proliferation, Differentiation, and Bone Formation, Resulting in a Dwarfism Phenotype with Severe Skeletal Dysplasia in Mice. Calcif. Tissue Int. 2022;111:519–534. doi: 10.1007/s00223-022-00999-5. [DOI] [PubMed] [Google Scholar]
- 85.Lin F.X., Du S.X., Liu D.Z., Hu Q.X., Yu G.Y., Wu C.C., Zheng G.Z., Xie D., Li X.D., Chang B. Naringin promotes osteogenic differentiation of bone marrow stromal cells by up-regulating Foxc2 expression via the IHH signaling pathway. Am. J. Transl. Res. 2016;8:5098–5107. [PMC free article] [PubMed] [Google Scholar]
- 86.Lv J., Sun X., Ma J., Ma X., Xing G., Wang Y., Sun L., Wang J., Li F., Li Y. Involvement of periostin-sclerostin-Wnt/β-catenin signaling pathway in the prevention of neurectomy-induced bone loss by naringin. Biochem. Biophys. Res. Commun. 2015;468:587–593. doi: 10.1016/j.bbrc.2015.10.152. [DOI] [PubMed] [Google Scholar]
- 87.Guo D., Wang J., Wang X., Luo H., Zhang H., Cao D., Chen L., Huang N. Double directional adjusting estrogenic effect of naringin from Rhizoma drynariae (Gusuibu) J. Ethnopharmacol. 2011;138:451–457. doi: 10.1016/j.jep.2011.09.034. [DOI] [PubMed] [Google Scholar]
- 88.Pang W.Y., Wang X.L., Mok S.K., Lai W.P., Chow H.K., Leung P.C., Yao X.S., Wong M.S. Naringin improves bone properties in ovariectomized mice and exerts oestrogen-like activities in rat osteoblast-like (UMR-106) cells. Br. J. Pharm. 2010;159:1693–1703. doi: 10.1111/j.1476-5381.2010.00664.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Wu G.J., Chen K.Y., Yang J.D., Liu S.H., Chen R.M. Naringin Improves Osteoblast Mineralization and Bone Healing and Strength through Regulating Estrogen Receptor Alpha-Dependent Alkaline Phosphatase Gene Expression. J. Agric. Food Chem. 2021;69:13020–13033. doi: 10.1021/acs.jafc.1c04353. [DOI] [PubMed] [Google Scholar]
- 90.Zhu Z., Xie W., Li Y., Zhu Z., Zhang W. Effect of Naringin Treatment on Postmenopausal Osteoporosis in Ovariectomized Rats: A Meta-Analysis and Systematic Review. Evid.-Based Complement. Altern. Med. ECAM. 2021;2021:6016874. doi: 10.1155/2021/6016874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Wang Y., Zhao L., Zhou L., Chen C., Chen G. Sequential release of vascular endothelial growth factor-A and bone morphogenetic protein-2 from osteogenic scaffolds assembled by PLGA microcapsules: A preliminary study in vitro. Int. J. Biol. Macromol. 2023;232:123330. doi: 10.1016/j.ijbiomac.2023.123330. [DOI] [PubMed] [Google Scholar]
- 92.Shangguan W.J., Zhang Y.H., Li Z.C., Tang L.M., Shao J., Li H. Naringin inhibits vascular endothelial cell apoptosis via endoplasmic reticulum stress- and mitochondrial-mediated pathways and promotes intraosseous angiogenesis in ovariectomized rats. Int. J. Mol. Med. 2017;40:1741–1749. doi: 10.3892/ijmm.2017.3160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Song N., Zhao Z., Ma X., Sun X., Ma J., Li F., Sun L., Lv J. Naringin promotes fracture healing through stimulation of angiogenesis by regulating the VEGF/VEGFR-2 signaling pathway in osteoporotic rats. Chem. Biol. Interact. 2017;261:11–17. doi: 10.1016/j.cbi.2016.10.020. [DOI] [PubMed] [Google Scholar]
- 94.Davalli P., Mitic T., Caporali A., Lauriola A., D’Arca D. ROS, Cell Senescence, and Novel Molecular Mechanisms in Aging and Age-Related Diseases. Oxid Med. Cell Longev. 2016;2016:3565127. doi: 10.1155/2016/3565127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Jagetia G.C., Venkatesha V.A., Reddy T.K. Naringin, a citrus flavonone, protects against radiation-induced chromosome damage in mouse bone marrow. Mutagenesis. 2003;18:337–343. doi: 10.1093/mutage/geg001. [DOI] [PubMed] [Google Scholar]
- 96.Jagetia G.C., Reddy T.K. The grapefruit flavanone naringin protects against the radiation-induced genomic instability in the mice bone marrow: A micronucleus study. Mutat. Res. 2002;519:37–48. doi: 10.1016/S1383-5718(02)00111-0. [DOI] [PubMed] [Google Scholar]
- 97.Rivoira M., Rodríguez V., Picotto G., Battaglino R., Tolosa de Talamoni N. Naringin prevents bone loss in a rat model of type 1 Diabetes mellitus. Arch. Biochem. Biophys. 2018;637:56–63. doi: 10.1016/j.abb.2017.12.001. [DOI] [PubMed] [Google Scholar]
- 98.Zhou X., Zhang P., Zhang C., Zhu Z. Promotion of bone formation by naringin in a titanium particle-induced diabetic murine calvarial osteolysis model. J. Orthop. Res. 2010;28:451–456. doi: 10.1002/jor.21002. [DOI] [PubMed] [Google Scholar]
- 99.Zhu J., Tang Y., Wu Q., Ji Y.C., Feng Z.F., Kang F.W. HIF-1α facilitates osteocyte-mediated osteoclastogenesis by activating JAK2/STAT3 pathway in vitro. J. Cell Physiol. 2019;234:21182–21192. doi: 10.1002/jcp.28721. [DOI] [PubMed] [Google Scholar]
- 100.Li C., Zhao J., Sun L., Yao Z., Liu R., Huang J., Liu X. RANKL downregulates cell surface CXCR6 expression through JAK2/STAT3 signaling pathway during osteoclastogenesis. Biochem. Biophys. Res. Commun. 2012;429:156–162. doi: 10.1016/j.bbrc.2012.10.122. [DOI] [PubMed] [Google Scholar]
- 101.Wang W., Mao J., Chen Y., Zuo J., Chen L., Li Y., Gao Y., Lu Q. Naringin promotes osteogenesis and ameliorates osteoporosis development by targeting JAK2/STAT3 signalling. Clin. Exp. Pharmacol. Physiol. 2022;49:113–121. doi: 10.1111/1440-1681.13591. [DOI] [PubMed] [Google Scholar]
- 102.Li N., Jiang Y., Wooley P.H., Xu Z., Yang S.Y. Naringin promotes osteoblast differentiation and effectively reverses ovariectomy-associated osteoporosis. J. Orthop. Sci. 2013;18:478–485. doi: 10.1007/s00776-013-0362-9. [DOI] [PubMed] [Google Scholar]
- 103.Zhang Y., Shen X., Ma P., Peng Z., Cai K. Composite coatings of Mg-MOF74 and Sr-substituted hydroxyapatite on titanium substrates for local antibacterial, anti-osteosarcoma and pro-osteogenesis applications. Mater. Lett. 2019;241:18–22. doi: 10.1016/j.matlet.2019.01.033. [DOI] [Google Scholar]
- 104.Yang Y., Tao B., Gong Y., Chen R., Yang W., Lin C., Chen M., Qin L., Jia Y., Cai K. Functionalization of Ti substrate with pH-responsive naringin-ZnO nanoparticles for the reconstruction of large bony after osteosarcoma resection. J. Biomed. Mater. Res. Part A. 2020;108:2190–2205. doi: 10.1002/jbm.a.36977. [DOI] [PubMed] [Google Scholar]
- 105.Yang X., Almassri H.N.S., Zhang Q., Ma Y., Zhang D., Chen M., Wu X. Electrosprayed naringin-loaded microsphere/SAIB hybrid depots enhance bone formation in a mouse calvarial defect model. Drug Deliv. 2019;26:137–146. doi: 10.1080/10717544.2019.1568620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Yu M., You D., Zhuang J., Lin S., Dong L., Weng S., Zhang B., Cheng K., Weng W., Wang H. Controlled Release of Naringin in Metal-Organic Framework-Loaded Mineralized Collagen Coating to Simultaneously Enhance Osseointegration and Antibacterial Activity. ACS Appl. Mater. Interfaces. 2017;9:19698–19705. doi: 10.1021/acsami.7b05296. [DOI] [PubMed] [Google Scholar]
- 107.Shen K., Zhang X., Tang Q., Fang X., Zhang C., Zhu Z., Hou Y., Lai M. Microstructured titanium functionalized by naringin inserted multilayers for promoting osteogenesis and inhibiting osteoclastogenesis. J. Biomater. Sci. Polym. Ed. 2021;32:1865–1881. doi: 10.1080/09205063.2021.1949098. [DOI] [PubMed] [Google Scholar]
- 108.Ji Y., Wang L., Watts D.C., Qiu H., You T., Deng F., Wu X. Controlled-release naringin nanoscaffold for osteoporotic bone healing. Dent. Mater. 2014;30:1263–1273. doi: 10.1016/j.dental.2014.08.381. [DOI] [PubMed] [Google Scholar]
- 109.Guo Z., Wu S., Li H., Li Q., Wu G., Zhou C. In vitro evaluation of electrospun PLGA/PLLA/PDLLA blend fibers loaded with naringin for guided bone regeneration. Dent. Mater. J. 2018;37:317–324. doi: 10.4012/dmj.2016-220. [DOI] [PubMed] [Google Scholar]
- 110.Elkhoury K., Sanchez-Gonzalez L., Lavrador P., Almeida R., Gaspar V., Kahn C., Cleymand F., Arab-Tehrany E., Mano J.F. Gelatin Methacryloyl (GelMA) Nanocomposite Hydrogels Embedding Bioactive Naringin Liposomes. Polymers. 2020;12:2944. doi: 10.3390/polym12122944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Yu X., Shen G., Shang Q., Zhang Z., Zhao W., Zhang P., Liang D., Ren H., Jiang X. A Naringin-loaded gelatin-microsphere/nano-hydroxyapatite/silk fibroin composite scaffold promoted healing of critical-size vertebral defects in ovariectomised rat. Int. J. Biol. Macromol. 2021;193:510–518. doi: 10.1016/j.ijbiomac.2021.10.036. [DOI] [PubMed] [Google Scholar]
- 112.Zhao Z.H., Ma X.L., Zhao B., Tian P., Ma J.X., Kang J.Y., Zhang Y., Guo Y., Sun L. Naringin-inlaid silk fibroin/hydroxyapatite scaffold enhances human umbilical cord-derived mesenchymal stem cell-based bone regeneration. Cell Prolif. 2021;54:e13043. doi: 10.1111/cpr.13043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Zhao Z.H., Ma X.L., Ma J.X., Kang J.Y., Zhang Y., Guo Y. Sustained release of naringin from silk-fibroin-nanohydroxyapatite scaffold for the enhancement of bone regeneration. Mater. Today Bio. 2022;13:100206. doi: 10.1016/j.mtbio.2022.100206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Zuo Y., Li Q., Xiong Q., Li J., Tang C., Zhang Y., Wang D. Naringin Release from a Nano-Hydroxyapatite/Collagen Scaffold Promotes Osteogenesis and Bone Tissue Reconstruction. Polymers. 2022;14:3260. doi: 10.3390/polym14163260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Spiller K.L., Koh T.J. Macrophage-based therapeutic strategies in regenerative medicine. Adv. Drug Deliv. Rev. 2017;122:74–83. doi: 10.1016/j.addr.2017.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Mo Y., Zhao F., Lin Z., Cao X., Chen D., Chen X. Local delivery of naringin in beta-cyclodextrin modified mesoporous bioactive glass promotes bone regeneration: From anti-inflammatory to synergistic osteogenesis and osteoclastogenesis. Biomater. Sci. 2022;10:1697–1712. doi: 10.1039/D1BM01842F. [DOI] [PubMed] [Google Scholar]
- 117.Cao X., Lin W., Liang C., Zhang D., Yang F., Zhang Y., Zhang X., Feng J., Chen C. Naringin rescued the TNF-α-induced inhibition of osteogenesis of bone marrow-derived mesenchymal stem cells by depressing the activation of NF-кB signaling pathway. Immunol. Res. 2015;62:357–367. doi: 10.1007/s12026-015-8665-x. [DOI] [PubMed] [Google Scholar]
- 118.Raj P.P. Intervertebral disc: Anatomy-physiology-pathophysiology-treatment. Pain Pract. 2008;8:18–44. doi: 10.1111/j.1533-2500.2007.00171.x. [DOI] [PubMed] [Google Scholar]
- 119.Huang J., Zhou Q., Ren Q., Luo L., Ji G., Zheng T. Endoplasmic reticulum stress associates with the development of intervertebral disc degeneration. Front. Endocrinol. 2022;13:1094394. doi: 10.3389/fendo.2022.1094394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Zhu L., Xie Z.Y., Jiang Z.L., Wang X.H., Shi H., Chen L., Wu X.T. Unfolded protein response alleviates acid-induced premature senescence by promoting autophagy in nucleus pulposus cells. Cell Biol. Int. 2022;46:568–578. doi: 10.1002/cbin.11751. [DOI] [PubMed] [Google Scholar]
- 121.Yang B., Yang X. Mesenchymal stem cell-derived exosomes are beneficial to suppressing inflammation and promoting autophagy in intervertebral disc degeneration. Folia Morphol. 2023 doi: 10.5603/FM.a2023.0021. [DOI] [PubMed] [Google Scholar]
- 122.Liu Z., Zhu J., Liu H., Fu C. Natural products can modulate inflammation in intervertebral disc degeneration. Front. Pharm. 2023;14:1150835. doi: 10.3389/fphar.2023.1150835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Song S., Bao S., Zhang C., Zhang J., Lv J., Li X., Chudhary M., Ren X., Kong L. Stimulation of AMPK Prevents Diabetes-Induced Photoreceptor Cell Degeneration. Oxid Med. Cell Longev. 2021;2021:5587340. doi: 10.1155/2021/5587340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Zhang Z., Wang C., Lin J., Jin H., Wang K., Yan Y., Wang J., Wu C., Nisar M., Tian N., et al. Therapeutic Potential of Naringin for Intervertebral Disc Degeneration: Involvement of Autophagy Against Oxidative Stress-Induced Apoptosis in Nucleus Pulposus Cells. Am. J. Chin. Med. 2018;46:1561–1580. doi: 10.1142/S0192415X18500805. [DOI] [PubMed] [Google Scholar]
- 125.Zhang Y.H., Shangguan W.J., Zhao Z.J., Zhou F.C., Liu H.T., Liang Z.H., Song J., Shao J. Naringin Inhibits Apoptosis Induced by Cyclic Stretch in Rat Annular Cells and Partially Attenuates Disc Degeneration by Inhibiting the ROS/NF-κB Pathway. Oxid Med. Cell Longev. 2022;2022:6179444. doi: 10.1155/2022/6179444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Cui A., Li H., Wang D., Zhong J., Chen Y., Lu H. Global, regional prevalence, incidence and risk factors of knee osteoarthritis in population-based studies. EClinicalMedicine. 2020;29–30:100587. doi: 10.1016/j.eclinm.2020.100587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Wu Z., Liu L. The protective activity of genistein against bone and cartilage diseases. Front. Pharm. 2022;13:1016981. doi: 10.3389/fphar.2022.1016981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Sun Y., Xue C., Wu H., Li C., Li S., Luo J., Liu T., Ding Y. Genetically Modified Mesenchymal Stromal Cells in Cartilage Regeneration. Stem Cells Dev. 2023 doi: 10.1089/scd.2022.0242. online ahead of print . [DOI] [PubMed] [Google Scholar]
- 129.Ye C., Chen J., Qu Y., Liu H., Yan J., Lu Y., Yang Z., Wang F., Li P. Naringin and bone marrow mesenchymal stem cells repair articular cartilage defects in rabbit knees through the transforming growth factor-β superfamily signaling pathway. Exp. Ther. Med. 2020;20:59. doi: 10.3892/etm.2020.9187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Firestein G.S., McInnes I.B. Immunopathogenesis of Rheumatoid Arthritis. Immunity. 2017;46:183–196. doi: 10.1016/j.immuni.2017.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Pelechas E., Voulgari P.V., Drosos A.A. Recent advances in the opioid mu receptor based pharmacotherapy for rheumatoid arthritis. Expert Opin. Pharm. 2020;21:2153–2160. doi: 10.1080/14656566.2020.1796969. [DOI] [PubMed] [Google Scholar]
- 132.Khan S., Mohan K., Muzammil S., Alam M.A., Khayyam K.U. Current Prospects in Rheumatoid Arthritis: Pathophysiology, Genetics, and Treatments. Recent Adv. Anti-Infect. Drug Discov. 2023 doi: 10.2174/2772434418666230406083149. [DOI] [PubMed] [Google Scholar]
- 133.Mohanty S., Sahoo A.K., Konkimalla V.B., Pal A., Si S.C. Naringin in Combination with Isothiocyanates as Liposomal Formulations Potentiates the Anti-inflammatory Activity in Different Acute and Chronic Animal Models of Rheumatoid Arthritis. ACS Omega. 2020;5:28319–28332. doi: 10.1021/acsomega.0c04300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Ma Y., Wang T., Liao J., Gu H., Lin X., Jiang Q., Bulsara M.K., Zheng M., Zheng Q. Efficacy of autologous bone marrow buffy coat grafting combined with core decompression in patients with avascular necrosis of femoral head: A prospective, double-blinded, randomized, controlled study. Stem Cell Res. Ther. 2014;5:115. doi: 10.1186/scrt505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Ikeuchi K., Hasegawa Y., Seki T., Takegami Y., Amano T., Ishiguro N. Epidemiology of nontraumatic osteonecrosis of the femoral head in Japan. Mod. Rheumatol. 2015;25:278–281. doi: 10.3109/14397595.2014.932038. [DOI] [PubMed] [Google Scholar]
- 136.Kang J.S., Park S., Song J.H., Jung Y.Y., Cho M.R., Rhyu K.H. Prevalence of osteonecrosis of the femoral head: A nationwide epidemiologic analysis in Korea. J. Arthroplast. 2009;24:1178–1183. doi: 10.1016/j.arth.2009.05.022. [DOI] [PubMed] [Google Scholar]
- 137.Zhao D.W., Yu M., Hu K., Wang W., Yang L., Wang B.J., Gao X.H., Guo Y.M., Xu Y.Q., Wei Y.S., et al. Prevalence of Nontraumatic Osteonecrosis of the Femoral Head and its Associated Risk Factors in the Chinese Population: Results from a Nationally Representative Survey. Chin. Med. J. 2015;128:2843–2850. doi: 10.4103/0366-6999.168017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Li Z., Shao W., Lv X., Wang B., Han L., Gong S., Wang P., Feng Y. Advances in experimental models of osteonecrosis of the femoral head. J. Orthop. Transl. 2023;39:88–99. doi: 10.1016/j.jot.2023.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Ghanbari-Movahed M., Jackson G., Farzaei M.H., Bishayee A. A Systematic Review of the Preventive and Therapeutic Effects of Naringin Against Human Malignancies. Front. Pharm. 2021;12:639840. doi: 10.3389/fphar.2021.639840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Rauf A., Shariati M.A., Imran M., Bashir K., Khan S.A., Mitra S., Emran T.B., Badalova K., Uddin M.S., Mubarak M.S., et al. Comprehensive review on naringenin and naringin polyphenols as a potent anticancer agent. Environ. Sci. Pollut. Res. Int. 2022;29:31025–31041. doi: 10.1007/s11356-022-18754-6. [DOI] [PubMed] [Google Scholar]
- 141.Yuan X., Ma C., Li J., Li J., Yu R., Cai F., Qu G., Yu B., Liu L., Zeng D., et al. Indirect bilirubin impairs invasion of osteosarcoma cells via inhibiting the PI3K/AKT/MMP-2 signaling pathway by suppressing intracellular ROS. J. Bone Oncol. 2023;39:100472. doi: 10.1016/j.jbo.2023.100472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Degnan A.J., Chung C.Y., Shah A.J. Quantitative diffusion-weighted magnetic resonance imaging assessment of chemotherapy treatment response of pediatric osteosarcoma and Ewing sarcoma malignant bone tumors. Clin. Imaging. 2018;47:9–13. doi: 10.1016/j.clinimag.2017.08.003. [DOI] [PubMed] [Google Scholar]
- 143.Hua K.C., Hu Y.C. Treatment method and prognostic factors of chondrosarcoma: Based on Surveillance, Epidemiology, and End Results (SEER) database. Transl. Cancer Res. 2020;9:4250–4266. doi: 10.21037/tcr-20-357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Peng G., Sun H., Jiang H., Wang Q., Gan L., Tian Y., Sun J., Wen D., Deng J. Exogenous growth hormone functionally alleviates glucocorticoid-induced longitudinal bone growth retardation in male rats by activating the Ihh/PTHrP signaling pathway. Mol. Cell Endocrinol. 2022;545:111571. doi: 10.1016/j.mce.2022.111571. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study are included within the article.