Abstract
Gastric epithelial cells in vitro and in vivo are shown to constitutively express the peptide antibiotic human β-defensin type 1 (hBD-1). In contrast, hBD-2 expression is regulated in gastric epithelial cells and increases in response to infection with Helicobacter pylori or stimulation with the proinflammatory cytokine interleukin-1. These data suggest that hBD-2 is a component of the regulated host gastric epithelial cell response to H. pylori infection and proinflammatory mediators.
Defensins are antimicrobial peptide components of the innate host defense system in higher mammals (10). The β-defensin family of peptides is divided into two subfamilies: type 1 and type 2 β-defensins (1). Type 2 β-defensins differ structurally from type 1 β-defensins and also differ in the presence of the nuclear factor NF-κB consensus site in their promoter region (11, 17). The induction or upregulated expression of type 2 β-defensins, such as tracheal and lingual antimicrobial peptide, human β-defensin type 2 (hBD-2) and mouse β defensin-3, in respiratory and oral epithelia of mammalian species during infection and inflammation suggests a role for these peptide antibiotics in antimicrobial defense at mucosal sites (1, 2, 6–8, 12, 17, 18, 20–24). We recently described the constitutive expression of hBD-1 and the induced expression of hBD-2 in intestinal epithelial cells in response to infection with enteropathogenic bacteria (19). Whereas the human colon contains 400 or more strains of noninvasive commensal bacteria and the human intestine can be infected by a number of different food and waterborne enteric pathogens, Helicobacter pylori, a pathogenic but noninvasive gram-negative bacterium, appears to be unique in its adaptation to long-term survival in the acidic environment of the human stomach. cagA+ strains of H. pylori activate the transcription factor NF-κB in gastric epithelial cells (15), which results in the upregulated expression of several target genes, including interleukin-8 (IL-8), cyclooxygenase 2, and nitric oxide synthase 2, whose products (e.g., IL-8, prostaglandins, and nitric oxide, respectively) are important in host innate antimicrobial defense (9, 13, 16). However, those mediators are not effective in clearing H. pylori. Thus, infection persists despite an inflammatory host response characterized by an influx of polymorphonuclear leukocytes that are chemoattracted by IL-8 and other chemokines and an influx of T cells that produce gamma interferon (IFN-γ) and other Th1 cytokines (reviewed in reference 3).
The human gastric adenocarcinoma cell line AGS (ATCC CRL 1739) was cultured in RPMI medium supplemented with 10% heat-inactivated fetal calf serum and 2 mM l-glutamine and maintained at 37°C in 5% CO2–95% air. The human colon adenocarcinoma cell line HT-29 was maintained as described before (19). AGS cells grown in six-well tissue culture plates (Corning-Costar, Cambridge, Mass.) for 3 to 5 days were left uninfected or were infected with cagA+ vacA+ clinical isolates of H. pylori (strains SD4 or SD14) (4, 5) at a multiplicity of infection (MOI) of 10. Culture supernatants and cells were harvested at various times after infection. In parallel experiments, AGS cells were left untreated or were stimulated for 4 h with IL-1α (20 ng/ml), tumor necrosis factor alpha (TNF-α) (20 ng/ml), IFN-γ (40 ng/ml), or bacterial lipopolysaccharide (LPS) (Escherichia coli O111:B4; 2 and 10 μg/ml) or were infected at an MOI of 10 with Salmonella enterica serovar Dublin, enteroinvasive E. coli O29:NM, noninvasive E. coli DH5α, or Streptococcus bovis, as described previously (19). Total cellular RNA, extracted from agonist-stimulated or infected AGS cells by using TRIzol reagent (Life Technologies, Grand Island, N.Y.), was reverse transcribed and then amplified with 4.0 U of Taq polymerase (Life Technologies) in a 50-μl volume containing 25 pmol of primers for hBD-1, hBD-2, or β-actin as described before (14, 19). After a hot start, the amplification profile for hBD-1 and hBD-2 was 35 cycles of 1 min of denaturation at 94°C, 1 min of annealing at 66°C, and a 1.5-min extension at 72°C, after which PCR products were resolved on 1.5% agarose gels as described before (19). For quantitative reverse transcription-PCR (RT-PCR) analysis, known amounts of standard RNA transcripts for hBD-1 and hBD-2 (19) were added to constant amounts of cellular RNA as described before (14, 19). hBD-1 or hBD-2 mRNAs were regarded as not expressed when PCR amplification yielded no product or <103 transcripts/μg of cellular RNA, because the latter are not likely to be paralleled by biologically meaningful protein production (i.e., because 105 cells yield ∼1 μg of cellular RNA, 103 transcripts/μg of cellular RNA is equivalent on average to ∼1 transcript per 100 cells). To confirm hBD-1 and hBD-2 production, cationic peptides were extracted from supernatants of control AGS cells or cells stimulated with IL-1α (20 ng/ml) for 5 days by using the weak cation exchange matrix MacroPrep CM (carboxymethyl) support (Bio-Rad Laboratories, Hercules, Calif.) as described before (19). Lanes were loaded with CM extracts from 3 ml of IL-1α-stimulated or unstimulated cell culture supernatants, and peptides were resolved by acetic acid-urea-polyacrylamide gel electrophoresis (AU-PAGE) and then subjected to immunoblot analysis as described before (19, 24). Recombinant hBD-1 (rhBD-1) and rhBD-2 peptides (20 ng/lane) were loaded as peptide standards (18, 19, 23, 24). Blots were developed with a 1:1,000 dilution of polyclonal rabbit anti-hBD-1 or hBD-2 as a primary antibody, alkaline phosphatase-conjugated goat anti-rabbit immunoglobulin G as a secondary antibody, and bromochloroindolyl phosphate-nitroblue tetrazolium as a substrate as described before (19, 24).
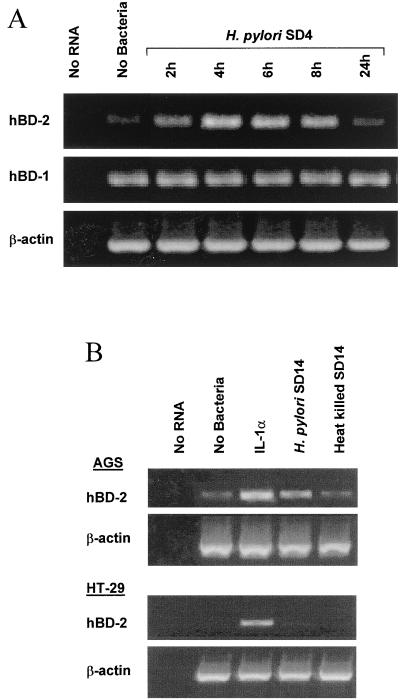
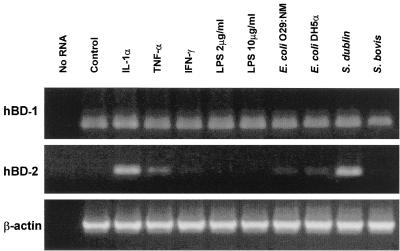
Enteroinvasive bacterial pathogens (e.g., S. enterica serovar Dublin and enteroinvasive E. coli) induce the expression of hBD-2 in human intestinal epithelial cell lines and in human intestinal xenografts (19). In the present study, we first addressed whether a noninvasive pathogen, H. pylori, upregulates human β-defensin expression in the AGS human gastric epithelial cell line. Since a prior study noted upregulated hBD-2 mRNA in MKN45 cells only following infection with cagA+ H. pylori (25), AGS cells were infected with a cagA+ strain of H. pylori, and expression of both hBD-1 and hBD-2 mRNA over time was assessed by RT-PCR. As shown in Fig. 1A, AGS cells constitutively expressed hBD-1 mRNA, and hBD-1 mRNA levels following infection with H. pylori remained unchanged, ranging from 3 × 104 to 4 × 104 transcripts/μg of cellular RNA. In contrast, hBD-2 mRNA expression was upregulated in AGS cells following H. pylori infection. Whereas the hBD-2 mRNA level in unstimulated AGS cells was 5 × 103 transcripts/μg of cellular RNA, hBD-2 mRNA levels were increased by 40-fold following H. pylori infection (2 × 105 transcripts/μg of cellular RNA). As shown in Fig. 1B, expression of hBD-2 mRNA was similarly upregulated in AGS cells infected with a second cagA+ strain of H. pylori (SD14) (1.5 × 105 transcripts/μg of cellular RNA), but not in cells cultured with heat-killed bacteria (60°C for 10 min). In contrast to AGS cells, H. pylori did not upregulate hBD-2 mRNA in HT-29 cells, although, hBD-2 mRNA was readily induced in those cells by the proinflammatory cytokine IL-1α. We next assessed the expression of gastric β-defensins in response to proinflammatory mediators or infection with other strains of noninvasive and enteroinvasive bacteria. To this end, AGS cells were stimulated with IL-1α, TNF-α, IFN-γ, and LPS or infected with S. enterica serovar Dublin, enteroinvasive E. coli O29:NM, noninvasive E. coli DH5α, or a gram-positive noninvasive bacterium, S. bovis, and mRNA levels for hBD-1 and hBD-2 were determined 4 h after infection or stimulation, a time point at which hBD-2 mRNA levels were maximal following H. pylori infection in previous experiments. Figure 2 shows that agonist stimulation or infection of AGS cells did not affect hBD-1 mRNA levels. In contrast, hBD-2 mRNA expression was markedly increased in those cells following stimulation with IL-1α (1.2 × 106 transcripts/μg of cellular RNA) and, to a lesser extent, after TNF-α stimulation. Infection with the highly invasive bacterium S. enterica serovar Dublin, at an MOI equivalent to that of H. pylori, upregulated hBD-2 mRNA expression in AGS cells to an extent similar to that of IL-1α (2 × 106 transcripts/μg of cellular RNA). Parallel infections with invasive and noninvasive strains of E. coli or with a gram-positive noninvasive bacterium, S. bovis, at the same MOI as H. pylori resulted in either little or no change in hBD-2 mRNA expression. Taken together, these findings indicate that noninvasive H. pylori can upregulate gastric epithelial hBD-2 mRNA expression and that the ability to upregulate hBD-2 mRNA in cultured gastric epithelial cells is not limited to H. pylori. Furthermore, coupled with the finding that neither heat-killed H. pylori nor high doses of soluble LPS upregulated hBD-2 mRNA levels in AGS cells, these results suggest that the upregulation of hBD-2 mRNA expression in AGS following H. pylori infection is not due to LPS.
FIG. 1.
Upregulation of hBD-2 mRNA by H. pylori in AGS cells. (A) AGS cells were cocultured with cagA+ vacA+ H. pylori strain SD4 for 2 to 24 h. Uninfected cultures were harvested at 6 h. Total cellular RNA was isolated, and hBD-1, hBD-2, and β-actin were amplified by RT-PCR. (B) AGS or HT-29 cells were cocultured with live or heat-killed H. pylori strain SD14 or were stimulated with IL-1α for 4 h. Total cellular RNA was isolated, and hBD-2 and β-actin were amplified by RT-PCR as in panel A.
FIG. 2.
Constitutive and regulated expression of human β-defensin mRNA in AGS cells in response to proinflammatory agonists. AGS cells were stimulated with IL-1α, TNF-α, IFN-γ, or LPS (2 or 10 μg/ml); infected with enteroinvasive E. coli O29:NM, E. coli DH5α, S. enterica serovar Dublin or S. bovis; or left untreated (control) as indicated. Total RNA was isolated, and hBD-1, hBD-2, and β-actin were amplified by RT-PCR.
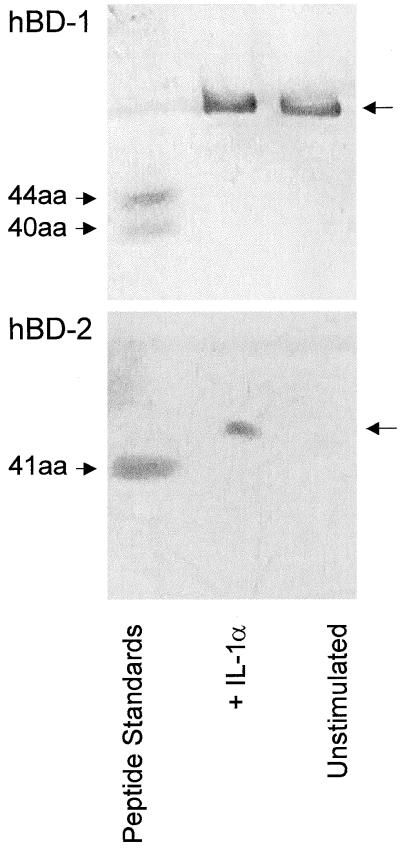
As demonstrated in Fig. 3, immunoblot analysis confirmed the production of hBD-1 and hBD-2 peptide by AGS cells. hBD-1 was present at equivalent levels (10 to 15 ng/ml) in culture supernatants from unstimulated and IL-1α-stimulated AGS cells, whereas hBD-2 peptide was detected in supernatants from IL-1α-stimulated (1.5 to 3 ng/ml), but not unstimulated cultures. In a previous study, we demonstrated two distinct isoforms of hBD-1 peptide in culture supernatants from the human colon epithelial cell line Caco-2 (19). However, only the larger of these two hBD-1 peptides was secreted by the gastric epithelial cell line AGS. This finding may reflect differences in the hBD-1 isoforms produced by these cells or, alternatively, differences in processing of the peptides in the culture medium. AGS cells, like Caco-2 cells, produced a single hBD-2 peptide that appears to be larger than the 41-amino-acid peptide identified from respiratory and oral epithelial cells (2, 19, 23).
FIG. 3.
Production of hBD-1 and hBD-2 peptides by AGS cells. Cationic peptides from unstimulated and IL-1α-stimulated AGS cells were resolved by AU-PAGE, transferred to polyvinylidene difluoride membranes, and detected with hBD-1 (top panel) or hBD-2 (bottom panel)-specific antisera. hBD-1 (20 ng of a mixture of the 44- and 40-amino-acid forms) and rhBD-2 (20 ng of the 41-amino-acid form) were loaded as peptide standards.
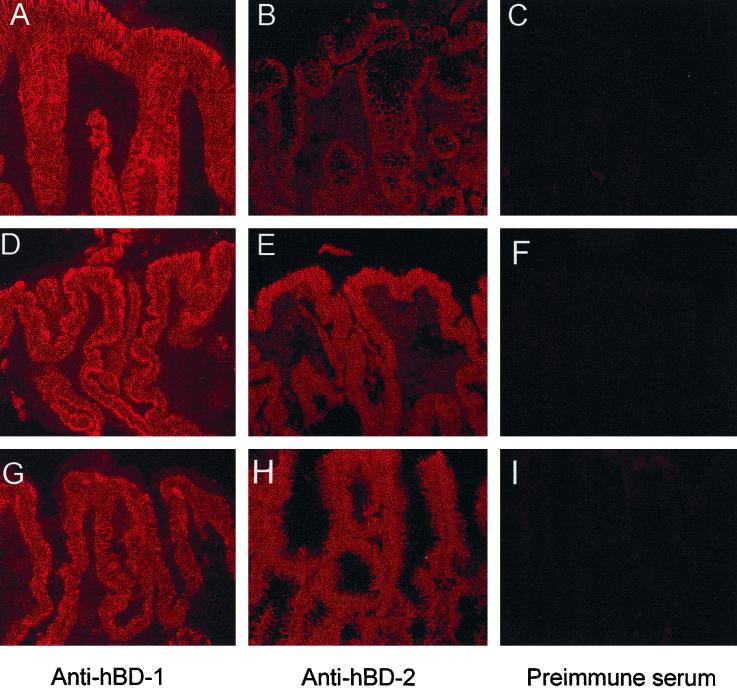
To study the constitutive and regulated production of gastric epithelial β-defensins in vivo, uninflamed gastric mucosa obtained at biopsy and inflamed mucosa from uninfected or H. pylori-infected individuals were analyzed by immunostaining for hBD-1 and hBD-2. As shown in Fig. 4, immunostaining of hBD-1 peptide was similar in the epithelium in all samples analyzed (Fig. 4A, D, and G). However, in contrast to our previous findings in normal intestinal tissue, hBD-2 appeared to be constitutively expressed, albeit at low levels, in uninflamed gastric epithelium (Fig. 4B), with expression markedly increased in epithelium from the inflamed mucosa of both H. pylori-infected (Fig. 4E) and uninfected (Fig. 4H) individuals.
FIG. 4.
Expression of hBD-1 and hBD-2 peptides in uninflamed and inflamed gastric mucosa from uninfected and H. pylori-infected individuals. Gastric mucosa was immunostained for hBD-1 (A, D, and G) and hBD-2 (B, E, and H). Adjacent sections were stained with preimmune serum corresponding to the same animal in which the hBD-2 antiserum was generated (C, F, and I). (A to C) Sections of uninflamed, H. pylori-negative gastric mucosa. (D to F) Sections of inflamed, H. pylori-positive gastric mucosa. (G to I) Sections of inflamed, H. pylori-negative gastric mucosa. The epithelium of normal and inflamed gastric mucosa contains hBD-1, whereas epithelial hBD-2 expression is most marked in inflamed gastric mucosa. Magnification, ×40. No staining was seen in sections stained with preimmune serum from the same animal in which the hBD-1 antiserum was generated (data not shown).
hBD-1 mRNA was constitutively expressed by cultured gastric epithelial cells, and its expression was not upregulated by IL-1α stimulation or infection with cagA+ vacA+ strains of H. pylori. In contrast, IL-1α stimulation or infection with cagA+ vacA+ strains of H. pylori upregulated the expression of hBD-2 mRNA in those cells. Whereas cultured gastric epithelial cells constitutively secreted detectable levels of hBD-1, but not hBD-2, hBD-2 was secreted in response to IL-1α stimulation. Upregulated production of hBD-2 during H. pylori infection in vivo, as shown herein, may result from direct contact of H. pylori with the epithelium or, alternatively, from epithelial cell stimulation with IL-1 released during the course of the mucosal inflammatory response. However, whether these peptides play a role in the host response to H. pylori infection in the stomach is not known. We note there is no information available as to whether H. pylori is susceptible to killing by concentrations of defensins that might be present at the interface between epithelial cells and the gastric lumen, or at sites more distal from the gastric epithelium; moreover, the secretion and concentration of these peptides in the gastric epithelial microenvironment are unknown. Whether hBD-1 or hBD-2 is microbicidal for H. pylori alone, together, or in combination with other antimicrobial mediators also remains to be determined. However, it is tempting to speculate that the H. pylori strains that are able to establish chronic mucosal infection may be less sensitive to innate mucosal defense mechanisms than those strains that do not induce disease. Furthermore our finding of constitutive hBD-1 and inducible hBD-2 in inflamed gastric epithelium in the absence of H. pylori also raises the possibility that β-defensins may mediate functions in addition to their putative role as antimicrobial peptides.
Acknowledgments
This work was supported by National Institutes of Health grant DK35108.
We thank John Leopard for assistance with immunostaining analysis.
REFERENCES
- 1.Bals R, Wang X, Meegalla R L, Wattler S, Weiner D J, Nehls M C, Wilson J M. Mouse β-defensin 3 is an inducible antimicrobial peptide expressed in the epithelia of multiple organs. Infect Immun. 1999;67:3542–3547. doi: 10.1128/iai.67.7.3542-3547.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bals R, Wang X, Wu Z, Freeman T, Bafna V, Zasloff M, Wilson J M. Human β-defensin 2 is a salt-sensitive peptide antibiotic expressed in human lung. J Clin Investig. 1998;102:874–880. doi: 10.1172/JCI2410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bodger K, Crabtree J E. Helicobacter pylori and gastric inflammation. Br Med Bull. 1998;54:139–150. doi: 10.1093/oxfordjournals.bmb.a011664. [DOI] [PubMed] [Google Scholar]
- 4.Cole S P, Cirillo D, Kagnoff M F, Guiney D G, Eckmann L. Coccoid and spiral Helicobacter pylori differ in their abilities to adhere to gastric epithelial cells and induce interleukin-8 secretion. Infect Immun. 1997;65:843–846. doi: 10.1128/iai.65.2.843-846.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cole S P, Kharitonov V F, Guiney D G. Effect of nitric oxide on Helicobacter pylori morphology. J Infect Dis. 1999;180:1713–1717. doi: 10.1086/315079. [DOI] [PubMed] [Google Scholar]
- 6.Diamond G, Jones D E, Bevins C L. Airway epithelial cells are the site of expression of a mammalian antimicrobial peptide gene. Proc Natl Acad Sci USA. 1993;90:4596–4600. doi: 10.1073/pnas.90.10.4596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Diamond G, Russell J P, Bevins C L. Inducible expression of an antibiotic peptide gene in lipopolysaccharide-challenged tracheal epithelial cells. Proc Natl Acad Sci USA. 1996;93:5156–5160. doi: 10.1073/pnas.93.10.5156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Diamond G, Zasloff M, Eck H, Brasseur M, Maloy W L, Bevins C L. Tracheal antimicrobial peptide, a cysteine-rich peptide from mammalian tracheal mucosa: peptide isolation and cloning of a cDNA. Proc Natl Acad Sci USA. 1991;88:3952–3956. doi: 10.1073/pnas.88.9.3952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fu S, Ramanujam K S, Wong A, Fantry G T, Drachenberg C B, James S P, Meltzer S J, Wilson K T. Increased expression and cellular localization of inducible nitric oxide synthase and cyclooxygenase 2 in Helicobacter pylori gastritis. Gastroenterology. 1999;116:1319–1329. doi: 10.1016/s0016-5085(99)70496-8. [DOI] [PubMed] [Google Scholar]
- 10.Ganz T, Lehrer R I. Antimicrobial peptides of vertebrates. Curr Opin Immunol. 1998;10:41–44. doi: 10.1016/s0952-7915(98)80029-0. [DOI] [PubMed] [Google Scholar]
- 11.Harder J. Mapping of the gene encoding human β-defensin-2 (DEFB2) to chromosome region 8p22-p23.1. Genomics. 1997;46:472–475. doi: 10.1006/geno.1997.5074. [DOI] [PubMed] [Google Scholar]
- 12.Hiratsuka T, Nakazato M, Date Y, Ashitani J, Minematsu T, Chino N, Matsukura S. Identification of human β-defensin-2 in respiratory tract and plasma and its increase in bacterial pneumonia. Biochem Biophys Res Commun. 1998;249:943–947. doi: 10.1006/bbrc.1998.9239. [DOI] [PubMed] [Google Scholar]
- 13.Huang J, O'Toole P W, Doig P, Trust T J. Stimulation of interleukin-8 production in epithelial cell lines by Helicobacter pylori. J Clin Investig. 1995;63:1732–1738. doi: 10.1128/iai.63.5.1732-1738.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jung H C, Eckmann L, Yang S-K, Morzycka-Wroblewska E, Kagnoff M F. A distinct array of proinflammatory cytokines is expressed in human colon epithelial cells in response to bacterial invasion. J Clin Investig. 1995;95:55–65. doi: 10.1172/JCI117676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Keates S, Hitti Y S, Upton M, Kelly C P. Helicobacter pylori infection activates NF-κB in gastric epithelial cells. Gastroenterology. 1997;113:1099–1109. doi: 10.1053/gast.1997.v113.pm9322504. [DOI] [PubMed] [Google Scholar]
- 16.Lindholm C, Quiding-Järbrink M, Lönroth H, Hamlet A, Svennerholm A-M. Local cytokine response in Helicobacter pylori-infected subjects. Infect Immun. 1998;66:5964–5971. doi: 10.1128/iai.66.12.5964-5971.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu L, Wang L, Jia H P, Zhao C, Heng H Q, Schutte B C, McCray P B, Jr, Ganz T. Structure and mapping of the human β-defensin HBD-2 gene and its expression at sites of inflammation. Gene. 1998;222:237–244. doi: 10.1016/s0378-1119(98)00480-6. [DOI] [PubMed] [Google Scholar]
- 18.Mathews M, Jia H P, Guthmiller J M, Losh G, Graham S, Johnson G K, Tack B F, McCray P B., Jr Production of β-defensin antimicrobial peptides by the oral mucosa and salivary glands. Infect Immun. 1999;67:2740–2745. doi: 10.1128/iai.67.6.2740-2745.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.O'Neil D A, Porter E M, Elewaut D, Anderson G M, Eckmann L, Ganz T, Kagnoff M F. Expression and regulation of the human β-defensins hBD-1 and hBD-2 in intestinal epithelium. J Immunol. 1999;163:6718–6724. [PubMed] [Google Scholar]
- 20.Russell J P, Diamond G, Tarver A P, Scanlin T F, Bevins C L. Coordinate induction of two antibiotic genes in tracheal epithelial cells exposed to the inflammatory mediators lipopolysaccharide and tumor necrosis factor alpha. Infect Immun. 1996;64:1565–1568. doi: 10.1128/iai.64.5.1565-1568.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schonwetter B S, Stolzenberg E D, Zasloff M A. Epithelial antibiotics induced at sites of inflammation. Science. 1995;267:1645–1648. doi: 10.1126/science.7886453. [DOI] [PubMed] [Google Scholar]
- 22.Schroder J M, Harder J. Human β-defensin-2. Int J Biochem Cell Biol. 1999;31:645–651. doi: 10.1016/s1357-2725(99)00013-8. [DOI] [PubMed] [Google Scholar]
- 23.Singh P K, Jia H P, Wiles K, Hesselberth J, Liu L, Conway B A, Greenberg E P, Valore E V, Welsh M J, Ganz T, Tack B F, McCray P B., Jr Production of β-defensins by human airway epithelia. Proc Natl Acad Sci USA. 1998;95:14961–14966. doi: 10.1073/pnas.95.25.14961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Valore E V, Park C H, Quayle A J, Wiles K R, McCray P B, Jr, Ganz T. Human β-defensin-1: an antimicrobial peptide of urogenital tissues. J Clin Investig. 1998;101:1633–1642. doi: 10.1172/JCI1861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wada A, Mori N, Oishi K, Hojo H, Nakahara Y, Hamanaka Y, Nagashima M, Sekine I, Ogushi K, Niidome T, Nagatake T, Moss J, Hirayama T. Induction of human β-defensin-2 mRNA expression by Helicobacter pylori in human gastric cell line MKN45 cells on cag pathogenicity island. Biochem Biophys Res Commun. 1999;263:770–774. doi: 10.1006/bbrc.1999.1452. [DOI] [PubMed] [Google Scholar]