Abstract
Multicentric reticulohistiocytosis, also called as lipoid dermato-arthritis is a rare form of non-Langerhans cell histiocytosis characterised by nodular and papular skin lesions containing characteristic bizarre multinucleate giant cells with ground glass cytoplasm. The disease commonly involves the skin, mucosa, synovium, and internal organs with cutaneous nodules and progressive erosive arthritis being the most common presenting features. We report a case of a 61-year-old male presenting with multiple swellings over distal part of fingers for 6 years without involvement of joints. A diagnosis of multicentric histiocytosis was made based on typical histopathological features of sheets of histiocytes and multinucleate giant cells with ground glass eosinophilic cytoplasm. The disease has a low incidence and about 300 cases have been reported so far in literature. The present case is being reported as it is uncommon for the disease to present in absence of arthritis.
Keywords: Arthritis, Reticulohistocytosis, Multinucleate giant cells
Introduction
Multicentric reticulohistiocytosis is a rare systemic disorder classified as type of non-Langerhans histiocytosis. The condition is characterised by papulonodular lesions on the skin and mucous membranes along with destructive arthritis.1 On histopathology, the lesions show characteristic proliferation of histiocytes and multinucleate giant cells with eosinophilic “ground-glass like” cytoplasm. Systemic involvement, although rare, has been reported with pulmonary, cardiac and muscular system being the common systems involved.2 An underlying malignancy has been associated in up to 25% cases and association with autoimmune conditions is seen in 5–20% cases.3 The peak age of occurrence is between 40 and 50 years. The disorder has a female preponderance with female: male ratio of 2–3: 1. Caucasians are most commonly affected (80%) as compared with other races which might be due to increased number of cases being reported from developed countries.4 We present this case due to its rare nature and uncommon presentation of cutaneous manifestation of 6 years duration in absence of joint involvement.
Case report
A 61-year-old male patient presented with complaints of multiple swellings over distal parts of fingers of both hands for past 6 years. The lesions had initially developed over the distal phalangeal area of left middle finger and had gradually increased in size and number to involve all the fingers. There was no history of any febrile episode, joint pains, morning stiffness, mucosal involvement, or anorexia. Patient was a known diabetic and hypertensive, on regular medications.
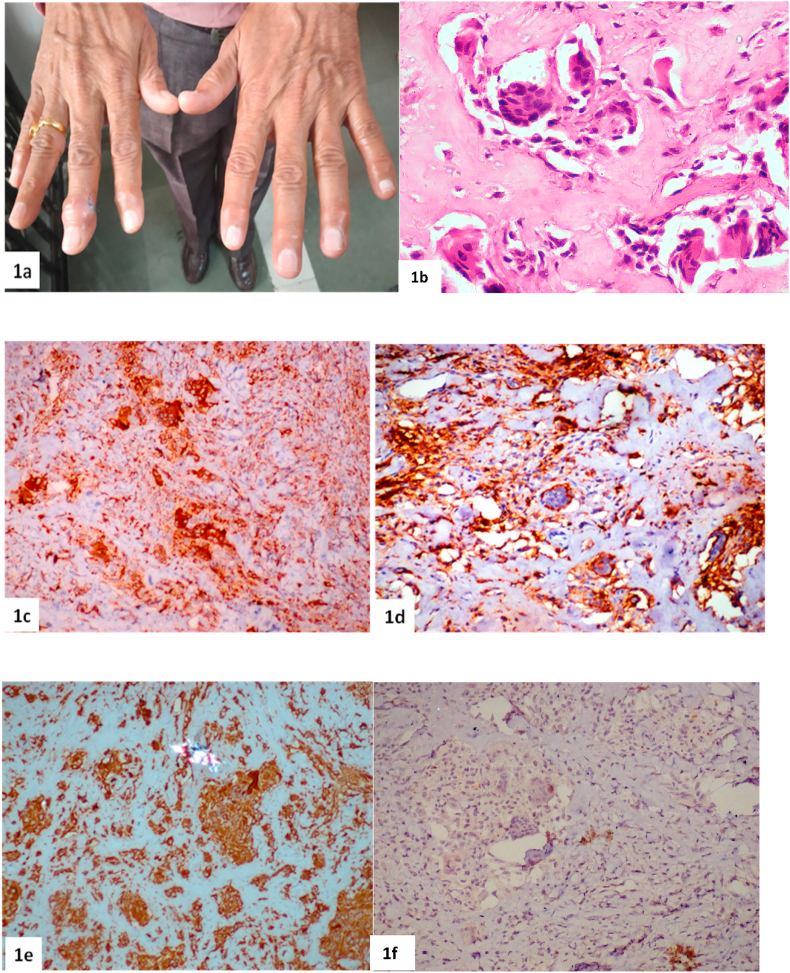
Dermatological examination revealed multiple well-defined discrete to confluent skin coloured nodules over the distal interphalangeal joints of right middle and index finger and left ring and index fingers. The nodules were arranged in string of pearl pattern around the base of the nail. The swellings were nontender, nonmobile and firm in consistency (Fig. 1a). Skin over the swellings was normal. Systemic examination was within normal limits. No visible deformity or restrictions in joint mobility was noted.
Fig. 1.
a. Multiple well-defined skin coloured nodules over the distal interphalangeal joints of right middle and index finger and left ring and index fingers in a “string of pearl” like arrangement. b. Skin biopsy showing presence of numerous multinucleate giant cells with eosinophilic finely granular cytoplasm with a characteristic “ground glass” appearance along with histiocytes, plasma cells and lymphocytes (H&E stain, 400x). These giant cells were positive for CD 68, CD 45 and vimentin, respectively (Fig. 1c–e, 200x). CD1a was negative (Fig. 1f and 200x).
Histopathological examination of skin biopsy revealed a mildly acanthotic epidermis. The dermis showed presence of numerous multinucleate giant cells with eosinophilic finely granular cytoplasm with a characteristic “ground glass” appearance with fair number of histiocytes, plasma cells and lymphocytes (Fig. 1b). On immunohistochemistry the giant cells were positive for CD68, CD45 and vimentin while were negative for CD1a (Fig. 1c–f). In addition, CD 15, CD 34, S100 and desmin were also negative. Radiograph and magnetic resonance imaging of hand showed soft tissue swelling with unremarkable joint involvement. Serum uric acid, rheumatoid arthritis factor, anti-CCP antibodies, thyroid function test, antinuclear antibodies were within normal limits. With the help of classical clinical features and histopathology with immunohistochemistry, a diagnosis of multicentric reticulohistiocytosis was made. A further workup for underlying malignancy including screening ultrasound abdomen, radiograph of chest, tumour markers (PSA, CEA, CA19.9) and serum protein electrophoresis was done and found to be within normal limits. Patient is kept under regular follow-up and plan to start disease modifying antirheumatic drugs in case patient develop any joint symptoms. Patient consent was obtained for images and inclusion in the study.
Discussion
Multicentric reticulohistiocytosis (MRH) is a rare disorder of unknown aetiology characterised by papulonodular eruptions of the skin and mucosa and progressive development of erosive arthritis.5 Weber et al, were the first to identify the disorder as a distinct clinical entity in 1937 while it was in 1954 that the term MRH was coined.6,7 MRH has been known by varying names through history such as lipoid dermatoarthritis, lipoid rheumatism, giant cell histiocytosis and reticulohistiocytic granuloma.4
The peak age of presentation of the disease is 40–50 years. The disease has a global presence, more in caucasians (80%) and almost three times commoner in females.4 Skin involvement and arthritis form the predominant clinical features of MRH. Arthritis is the earliest manifestation in majority (40%) of the cases. Patients usually present with symmetric, progressive and destructive polyarthritis with predilection for distal interphalangeal joints. Simultaneous involvement of skin and joints is seen in about 30% cases whereas skin involvement precedes joint involvement in about 30% cases.8 Cutaneous lesions of MRH are typically papulonodular, reddish brown lesions, distributed symmetrically over face, neck, chest arm and hands.5 Dorsal surface and nail folds are commonly involved sites in hands as in our case. A concurrent autoimmune disorder such as systemic lupus erythematosus, rheumatoid arthritis, primary biliary cirrhosis, systemic sclerosis, celiac disease etc. is seen in approximately 5–20% of the cases. An underlying malignancy is seen in up to 15–30% of cases. The most common malignancies associated with the condition include carcinoma ovary, breast, stomach and lung.3 Systemic involvement is varied with pulmonary system being the most commonly involved (up to 20% cases) in form of pleural effusion, pleural thickening, airway infiltrates, mottling of lungs, as well as hilar and mediastinal lymphadenopathy.9 Cardiac involvement is less common and usually manifests as fibrinous pericarditis leading to constrictive pericarditis, cardiomegaly and pericardial effusion.10 Other systemic manifestations include muscle weakness and dermatomyositis.
Diagnosis is based on classical histopathological findings on biopsy of the skin lesions. A typical infiltrate of mononuclear histiocytes and multinucleate giant cells is seen. The giant cells have a granular cytoplasm and an eosinophilic “ground glass” like cytoplasm. On immunohistochemistry the cells are positive for CD68, CD45 and vimentin while are negative for S100, CD34 and factor XIIIa.11 In our case the histiocytes and giant cells were positive for CD68, CD45 and vimentin while were negative for CD1a. Laboratory investigations were noncontributory in our case.
No clear-cut guidelines for treatments exist for MRH. Various lines of therapy such as NSAIDS, immunomodulators and immunosuppressive agents have been used. Our patient is on regular follow-up for any joint or systemic involvement.
After extensive PubMed and Scopus search, we found approximately 300 case reports of MRH, mostly as single case study. Two of the recent large studies by Tariq et al who in their meta-analysis over 24 years have found only 14% reported cases of MRH without joint involvement (7/50).9 While the long study spread over 37 years from Mayo Clinic, USA, by Sanchez-Alaverez et al had only 8% of their cases who did not have joint involvement (2/24).12 This rarity of joint erosion in MRH patients is what makes our case unique.
Conclusion
Multicentric reticulohistiocytosis is a rare disorder and is often misdiagnosed due to its close resemblance to other forms of arthritis and skin conditions. A high index of suspicion is required to prevent misdiagnosis and wrong treatment. An early treatment if instituted can prevent the progression of the disease which otherwise has a debilitating and aggressive course.
Disclosure of competing interest
The authors have none to declare.
References
- 1.Kuntoji V., Kudligi C., Bhagwat P.V., Krishna S., Rathod R.M., Bansal A. Multicentric reticulohistiocytosis: a case report with review. Our Dermatol Online. 2017;8(3):302–305. [Google Scholar]
- 2.Sinha A., Dhungana S., De Dipankar, Prakash M., Sharma S.K., Das A. Multicentric reticulohistiocytosis: a clinicoradiological review. Indian J Rheumatol. 2018;13:195–201. [Google Scholar]
- 3.Trotta F., Castellino G., Lo Monaco A. Multicentric reticulohistiocytosis. Best Pract Res Clin Rheumatol. 2004;18(5 SPEC. ISS.):759–772. doi: 10.1016/j.berh.2004.06.002. [DOI] [PubMed] [Google Scholar]
- 4.Barrow M.V., Holubar K. Multicentric reticulohistiocytosis. A review of 33 patients. Medicine (Baltim) 1969;48:287–305. [PubMed] [Google Scholar]
- 5.Sinha A., Dhungana S., De Dipankar, Prakash M., Sharma S.K., Das A. Multicentric reticulohistiocytosis: a clinicoradiological review. Indian J Rheumatol. 2018;13:195–201. [Google Scholar]
- 6.Weber F.P., Freudenthal W. Nodular non-diabetic cutaneous xanthomatosis with hypercholesterolæmia and atypical histological features. Proc Roy Soc Med. 1937;30:522–526. [PMC free article] [PubMed] [Google Scholar]
- 7.Goltz R.W., Laymon C.W. Multicentric reticulohistiocytosis of the skin and synovia; reticulohistiocytoma or ganglioneuroma. AMA Arch Derm Syphilol. 1954;69:717–731. doi: 10.1001/archderm.1954.01540180067010. [DOI] [PubMed] [Google Scholar]
- 8.Luz F.B., Gaspar T.A., Kalil-Gaspar N., Ramos-e-Silva M. Multicentric reticulohistiocytosis. J Eur Acad Dermatol Venereol. 2001;15:524–531. doi: 10.1046/j.1468-3083.2001.00362.x. [DOI] [PubMed] [Google Scholar]
- 9.Tariq S., Hugenberg S.T., Hirano-Ali S.A., Tariq H. Multicentric reticulohistiocytosis (MRH): case report with review of literature between 1991 and 2014 with in depth analysis of various treatment regimens and outcomes. Springerplus. 2016;5:180. doi: 10.1186/s40064-016-1874-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yee K.C., Bowker C.M., Tan C.Y., Palmer R.G. Cardiac and systemic complications in multicentric reticulohistiocytosis. Clin Exp Dermatol. 1993;18:555–558. doi: 10.1111/j.1365-2230.1993.tb01030.x. [DOI] [PubMed] [Google Scholar]
- 11.Luz F.B., Gaspar A.P., Ramos-e-Silva M., et al. Immunohistochemical profile of multicentric reticulohistiocytosis. Skinmed. 2005;4:71–77. doi: 10.1111/j.1540-9740.2005.03415.x. [DOI] [PubMed] [Google Scholar]
- 12.Sanchez-Alvarez C., Sandhu A.S., Crowson C.S., et al. Multicentric reticulohistiocytosis: the Mayo clinic experience (1980-2017) Rheumatology (Oxford) 2020;59(8):1898–1905. doi: 10.1093/rheumatology/kez555. [DOI] [PubMed] [Google Scholar]