Abstract
Objective: To investigate the effect of fine nursing with dietary intervention on the pain level and health of patients with advanced lung cancer (LC). Methods: The clinical data of 92 patients with advanced LC admitted to the Nanfang Hospital, Southern Medical University/the First School of Clinical Medicine, Southern Medical University from February 2018 to June 2020 were studied in this retrospective analysis. Among them, 48 patients who received fine nursing with dietary intervention were grouped into the research group (RG), and the other 44 who received conventional nursing were grouped into the control group (CG). The two groups were compared in terms of pain level, nutrition, quality of life, anxiety and depression, sleep quality, satisfaction with care, and complication rate. Results: The visual analogue scale (VAS), self-rating anxiety scale (SAS), self-rating depression scale (SDS), patient-Generated Subjective Global Assessment (PG-SGA), and Pittsburgh Sleep Quality Index (PSQI) scores were lower in the RG than in the CG after nursing, and the scores were higher in both groups before nursing than after nursing (P<0.05). The World Health Organization Quality of Life Brief Version (WHOQOL-BREF) scores, forced vital capacity (FVC), forced expiratory volume in 1 second (FEV1) and maximum ventilation volume (MVV) were higher in the RG than in the CG after nursing, and the scores, FVC, FEV1 and MVV were lower in both groups before nursing than after nursing (P<0.05). The complication rate of patients in the CG was higher than that of those in the RG (P<0.05). The nursing satisfaction of patients in the CG was lower than that of those in the RG (P<0.05). Age, TNM stage, smoking history, and maximum tumor diameter were risk factors affecting patient prognosis, and logistic regression analysis found that smoking history was an independent risk factor affecting patient prognosis. Conclusion: Fine nursing with dietary intervention can effectively reduce pain, regulate patients’ restlessness, reduce the incidence of complications, improve patients’ nutrition and sleep quality, and can improve their quality of life, which is worthy of application and promotion in clinical practice.
Keywords: Fine nursing, dietary intervention, advanced lung cancer, pain level
Introduction
Lung cancer, or primary bronchopulmonary cancer, originates in the trachea, bronchial mucosa or glands and is the most common primary malignant tumor of the lung [1]. Lung cancer (LC) is one of the most important diseases that endanger human health [2]. According to statistics, in 2015, the incidence of LC (57/100,000) in China accounted for the first and second place of malignancies in men and women, respectively, and the mortality rate ranked first among all malignancies [3]. In recent years, the incidence and mortality rates of LC have remained high and are on the rise. Some data show that squamous lung cancer accounts for about 30% to 40% of lung cancers; adenocarcinoma accounts for about 40% to 55% of lung cancers [4]. The main causes of LC are related to smoking, followed by air pollution, ionizing radiation, genetics, history of lung disease, and other causes [5]. Most of them are caused by smoking, and a small number of patients are exposed to some radioactive gases, which may also increase the incidence of LC. It has also been shown that implementing an effective smoking cessation program may further reduce the incidence and mortality associated with LC [6].
LC is quite difficult to diagnose and treat. Because early symptoms are not obvious or atypical, they are easily overlooked, most patients are already at an advanced stage when they are diagnosed with LC [7]. Patients who have entered the advanced stage of LC have experienced extensive metastasis and spread of cancer cells in their bodies and are therefore not suitable for surgical treatment. Currently, the treatment of advanced LC mainly adopts chemotherapy molecular targeting therapy, immunotherapy, anti-cancer drug therapy, and nutritional therapy to prolong patients’ survival time, improve their quality of life, reduce their pain, and prevent complications [8]. Therefore, nursing during the treatment process is particularly important to enhance the quality of life of patients, improve their condition and reduce psychological stress. Fine nursing is an advanced nursing model that focuses on quantification, implementation, and results, with fine operation as the basic feature and “patient-centered” nursing service concept, which is widely used in nursing quality management [9]. It has been noted that this model of care can improve negative emotion, quality of life, and reduce adverse effects during radiotherapy for patients with LC compared to conventional nursing. It has also been shown that this model of nursing is more effective in improving the ability to perform activities of daily living (ADL), quality of life, and compliance of stroke patients compared to conventional nursing. At the same time, it is equally important to provide dietary interventions for LC patients. Patients with advanced LC have poor nutrition and lack of appetite, so the development of a specialized diet plan has a positive effect on improving the appetite and improving the physical status of patients [10].
Therefore, this study will use fine nursing with dietary intervention for patients with advanced LC, in order to investigate the effect of the intervention program on patients’ pain level and health and its application in advanced LC, aiming to provide more reliable references for clinical treatment.
Materials and methods
Clinical data
The clinical data of 92 patients with advanced LC admitted to the Nanfang Hospital, Southern Medical University/the First School of Clinical Medicine, Southern Medical University from February 2018 to June 2020 were studied by this retrospective analysis. Among them, 48 patients who received fine nursing with dietary intervention were the research group (RG), and the other 44 who received conventional nursing were the control group (CG). In terms of prognosis, patients were regrouped based on whether they survive. Survival patients were included in the good prognosis group (n=70) and patients who died were included in the poor prognosis group (n=22). The study was conducted with the approval of the medical ethics committee of the Nanfang Hospital, Southern Medical University/the First School of Clinical Medicine, Southern Medical University. Ethical Lot No. 854256.
Inclusion and exclusion criteria
Inclusion criteria: patients met the diagnostic criteria related to advanced LC [11]; all of them received conservative treatment; their medical records were complete; they had no communication impairment, and all had completed all tests in this study.
Exclusion criteria: those who did not cooperate with this study; those with low compliance; those with comorbid cognitive dysfunction; those with comorbid psychiatric abnormalities; those with comorbid infectious or immune diseases; those who dropped out of the study.
Nursing programs
CG: Patients were given routine care and dietary interventions. After admission, basic disease education, adequate diet, routine nursing operations, and any abnormalities in the course of nursing were promptly notified to the doctor and dealt with.
RG: Patients were given fine nursing in conjunction with dietary interventions. (1) Health education. Targeted health education strategies are developed according to patients’ and families’ knowledge of the disease and their education level. Patients and family members were introduced to detailed knowledge about LC and pain, pain mechanism, relief methods, care precautions, etc. If a patient has a painful episode, family members who have received health education can also work with the nursing staff to provide supportive care to them, give emotional comfort, help relieve anxiety, massage the painful area to reduce pain, etc. Patients and their families can better cooperate with the treatment by establishing the correct disease perception. (2) Basic care. Ensure that the ward is neat and quiet with fresh air to create a good living environment for patients and keep them in a happy mood, which can also ensure that they get enough sleep. (3) Psychological care. Pay attention to patients’ psychological emotions in a timely manner, detect and relieve the tension and anxiety and other uneasy emotions caused by cancer to them. Different patients are given different psychological interventions, actively communicating with them, answering questions, eliminating concerns, or distracting them so that they can maintain a stable and good mood and actively cooperate with treatment. (4) Social family cooperation care. Communicate more with the family, instruct them to ease patients’ anxiety, and give them some company and support, which can also help them actively cooperate with the treatment. (5) Pain care. Strengthen the training of nursing staff on LC-related knowledge and update the nursing content of the training according to the actual situation. The medical history was carefully inquired about, and the pain grade was recorded when patients are admitted to the hospital. Patients were encouraged and guided to express the pain site, pain level, duration, and concomitant symptoms as accurately as possible, so that the impact of pain on patients, including their ability to live, psychological stress, and anxiety and tension, could be assessed, from which a fine nursing plan could be formulated. To record in detail the clinical efficacy of patients’ pain medication and to modify or update the care plan in a timely manner according to the actual situation during their treatment. (6) Dietary intervention. A detailed understanding of patients’ daily eating habits and preferences is then combined with the nutritional needs of the treatment process to develop a personalized diet plan. Diet should be light and nutritious, with no single type of diet to meet the various tastes of patients, equipped with semi-liquid food such as milk, vegetables and other high protein and high vitamin at each meal. At the same time, patients were instructed to eat less spicy and thick food, eat more fruits, no smoking and no alcohol.
Outcome measures
Main outcome measures
The visual analogue scale (VAS) was used to compare the pain level of the two groups before and after nursing, with a total of 10 points, the higher the score, the more severe the pain level [12]. The Patient-Generated Subjective Global Assessment (PG-SGA) was used to compare the nutrition of patients before and after nursing, including five dimensions such as weight change and food intake, and the higher the score, the worse the nutrition [13]. The World Health Organization Quality of Life Brief Version (WHOQOL-BREF) was used to assess the quality of life of patients before and after nursing, including four items such as physical and environmental, using a 5-point rating system, with higher scores associated with better quality of life [14].
Secondary outcome measures
The anxiety and depression of patients were assessed using the self-rating anxiety scale (SAS) and the self-rating depression scale (SDS), both with a total score of 100, with higher scores indicating a more severe anxiety [15]. The Pittsburgh Sleep Quality Index (PSQI) was used to evaluate the sleep quality of patients in both groups, with higher scores associated with poorer sleep quality [16]. Newcastle Satisfaction with Nursing Scale (NSNS) was used to assess patients’ satisfaction with nursing, with a total of 100 points, of which <60 was dissatisfied, 60-89 was basically satisfied, and ≥90 was satisfied. Satisfaction = (satisfied + basically satisfied)/total number of cases × 100%. Patients’ pulmonary function was measured using a spirometer, including forced vital capacity (FVC), forced expiratory volume in 1 second (FEV1) and maximum ventilation volume (MVV). The occurrence of complications was compared between the two groups.
Statistical analysis
The data were statistically analyzed using SPSS 21.0, and the current data were graphically plotted using GraphPad Prism 7. Comparisons between counting data were made by chi-square test, expressed as χ2; the data were analyzed by t-test, where independent samples t-test was used for comparison between groups and paired t-test for that within groups. P<0.05 represents statistical significance.
Results
Comparison of clinical data
As regard to the basic clinical data of the two groups, there were no statistical differences in age, gender, body mass index (BMI), course of disease, TNM stage, and education between the two groups (all P>0.05), as shown in Table 1.
Table 1.
Comparison of clinical data
| Factor | Control group (n=44) | Research group (n=48) | χ2 value | P value |
|---|---|---|---|---|
| Age | 0.174 | 0.676 | ||
| ≤60 years old | 21 | 25 | ||
| >60 years old | 23 | 23 | ||
| Gender | 0.075 | 0.783 | ||
| Male | 26 | 27 | ||
| Female | 18 | 21 | ||
| BMI | 0.428 | 0.512 | ||
| ≤21 kg/m2 | 19 | 24 | ||
| >21 kg/m2 | 25 | 24 | ||
| Course of disease | 0.001 | 0.970 | ||
| ≤7 months | 20 | 22 | ||
| >7 months | 24 | 26 | ||
| Education | 0.075 | 0.783 | ||
| Below college | 26 | 27 | ||
| College and above | 18 | 21 | ||
| TNM stage | 0.271 | 0.603 | ||
| Stage IIIa | 16 | 20 | ||
| Stage IIIb | 28 | 28 |
Note: χ2: chi-square test. BMI: body mass index.
Comparison of anxiety-depression mood changes
A comparison of the changes in anxiety and depression in the two groups before and after nursing revealed that there were no remarkable differences in SAS and SDS scores compared to before nursing (all P>0.05), but SAS and SDS scores in the RG were lower than those in the CG after nursing (all P<0.05). In addition, further comparison within the group revealed that SAS and SDS scores were higher in both groups before nursing than after nursing (all P<0.05, Figure 1).
Figure 1.
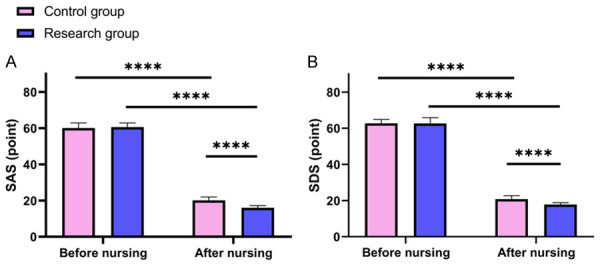
Comparison of anxiety-depression mood changes. A: Change in SAS scores of patients before and after nursing; B: Change in SDS scores of patients before and after nursing. Note: ****P<0.0001. SAS: self-rating anxiety scale; SDS: self-rating depression scale.
Comparison of patient pain scores
A comparison of the pain scores of the two groups before and after nursing revealed that before nursing, there was no marked difference in VAS scores compared with the two groups (P>0.05). after nursing, the VAS scores of the RG were lower than those of the control group (P<0.05). In addition, further comparison within the group manifested that the pre-care VAS scores were higher than post-care in both groups (P<0.05, Figure 2).
Figure 2.
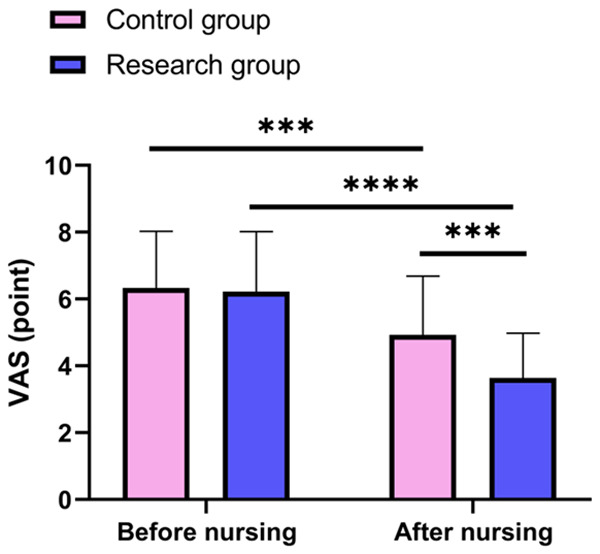
Comparison of pain scores. Note: ***P<0.001, ****P<0.0001. VAS: visual analogue scale.
Nutrition and quality of life
A comparison of the nutrition and quality of life of the two groups before and after nursing revealed that before nursing, there were no significant differences in the PG-SGA and WHOQOL-BREF scores (all P>0.05). After nursing, the PG-SGA scores of the RG were lower than those of the CG, and the WHOQOL-BREF scores of the RG were higher than those of the CG (all P<0.05). In addition, further comparison within the group revealed that the PG-SGA score was higher before nursing and the WHOQOL-BREF score was lower than after nursing in both groups (all P<0.05, Figure 3).
Figure 3.
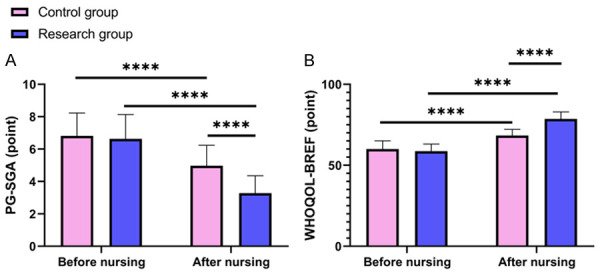
Comparison of changes in nutrition and quality of life. A: Changes in PG-SGA scores of patients before and after nursing; B: Change in WHOQOL-BREF scores of patients before and after nursing. Note: ****P<0.0001. PG-SGA: Patient-Generated Subjective Global Assessment; WHOQOL-BREF: World Health Organization Quality of Life Brief Version.
Change in sleep quality
A comparison of the sleep quality of the two groups before and after nursing revealed that before nursing, there was no marked difference in PSQI scores (P>0.05). After nursing, the PSQI scores of the RG were lower than those of the CG (P<0.05). In addition, further comparison within groups manifested that PSQI scores were higher before nursing than after nursing in both groups (P<0.05, Figure 4).
Figure 4.
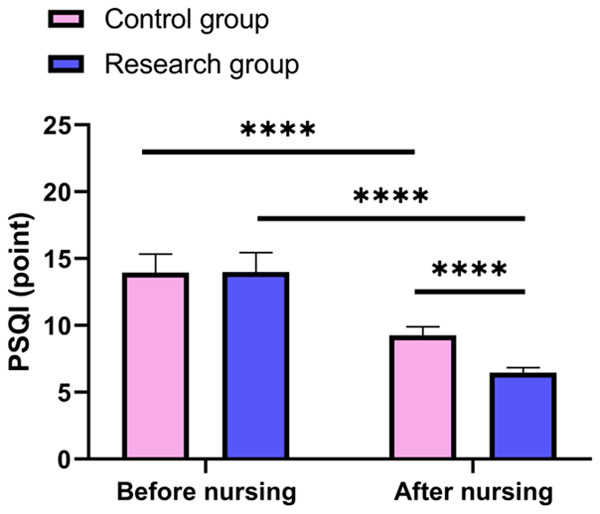
Change in sleep quality. Note: ****P<0.0001. PSQI: Pittsburgh Sleep Quality Index.
Comparison of lung function
A comparison of pulmonary function before and after nursing between the two groups revealed that there were no significant differences in FVC, FEV1, and MVV before nursing (all P>0.05), but FVC, FEV1, and MVV were significantly higher in the research group than in the control group after nursing (all P<0.05). In addition, further comparison within the group revealed that FVC, FEV1, and MVV were significantly higher in both groups after nursing than before nursing (all P<0.05), as shown in Figure 5.
Figure 5.
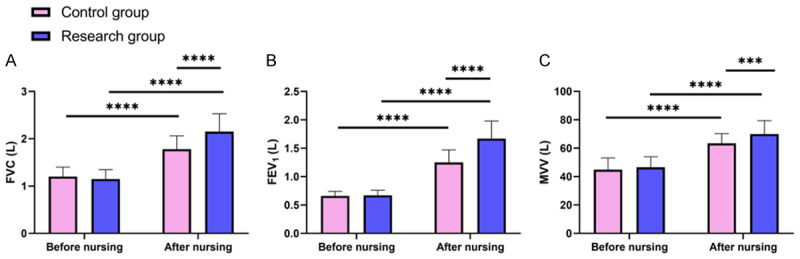
Comparison of lung function. A. Change in FVC before and after patient nursing. B. Change in FEV1 before and after patient nursing. C. Change in MVV before and after patient nursing. Note: *** indicates P<0.001, **** indicates P<0.0001. FVC: forced vital capacity; FEV1: forced expiratory volume in 1 second; MVV: maximum ventilation volume.
Comparison of nursing satisfaction
The nursing satisfaction of the two groups was compared. The results showed that the nursing satisfaction of patients in the CG was lower than that of those in the RG (P=0.028), as shown in Table 2.
Table 2.
Comparison of nursing satisfaction
| Groups | Satisfied | Basically satisfied | Dissatisfied | Satisfaction rate |
|---|---|---|---|---|
| Control group (n=44) | 11 (25.00) | 18 (40.91) | 15 (34.10) | 29 (65.91) |
| Research group (n=48) | 20 (41.67) | 21 (43.75) | 7 (14.58) | 41 (85.42) |
| χ2 | 2.854 | 0.076 | 4.801 | 4.801 |
| P | 0.091 | 0.783 | 0.028 | 0.028 |
Note: χ2: chi-square test.
Comparison of occurrence of complications
A comparison of complications between the two groups denoted those patients in the CG had a significantly higher complication rate than those in the RG (P=0.009), as shown in Table 3.
Table 3.
Comparison of occurrence of complications
| Groups | Lung infection | Hemorrhage | Atelectasis | Hydrothorax | Incidence of complications |
|---|---|---|---|---|---|
| Control group (n=44) | 2 (4.55) | 2 (4.55) | 2 (4.55) | 2 (4.55) | 8 (18.18) |
| Research group (n=48) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 1 (2.08) | 1 (2.08) |
| χ2 | 2.230 | 2.230 | 2.230 | 0.441 | 6.741 |
| P | 0.135 | 0.135 | 0.135 | 0.507 | 0.009 |
Note: χ2: chi-square test.
Analysis of impact on patient prognosis
Patients were regrouped based on whether they survive. Survival patients were included in the good prognosis group (n=70) and death patients were included in the poor prognosis group (n=22). We then compared the differences in clinical data between the two groups and found that age, TNM stage, smoking history, and maximum tumor diameter were risk factors affecting the prognosis of patients, as shown in Table 4. The indicators that differed in the above results were assigned values as a result of the univariate analysis, as shown in Table 5. Further logistic regression analysis revealed that smoking history was an independent risk factor for patient prognosis. See Table 6.
Table 4.
Univariate analysis
| Factor | Poor prognosis group (n=22) | Good prognosis group (n=70) | χ2 | P |
|---|---|---|---|---|
| Age | 11.65 | 0.001 | ||
| ≤60 years old | 5 | 45 | ||
| >60 years old | 17 | 25 | ||
| Gender | 1.164 | 0.281 | ||
| Male | 16 | 42 | ||
| Female | 6 | 28 | ||
| BMI | 1.005 | 0.316 | ||
| ≤21 kg/m2 | 14 | 36 | ||
| >21 kg/m2 | 8 | 34 | ||
| Course of disease | 0.896 | 0.344 | ||
| ≤7 months | 10 | 24 | ||
| >7 months | 12 | 46 | ||
| TNM stage | 5.948 | 0.015 | ||
| Stage IIIa | 11 | 16 | ||
| Stage IIIb | 11 | 54 | ||
| Smoking history | 4.332 | 0.037 | ||
| Yes | 20 | 48 | ||
| No | 2 | 22 | ||
| Maximum tumor diameter | 7.240 | 0.007 | ||
| >6 cm | 9 | 10 | ||
| ≤6 cm | 13 | 60 | ||
| Education | 0.741 | 0.340 | ||
| Below college | 13 | 35 | ||
| College and above | 9 | 37 |
Note: χ2: chi-square test. BMI: body mass index.
Table 5.
Assignment table
| Factor | Assignment |
|---|---|
| Age | ≤60 years old =0, >60 years old =1 |
| TNM stage | Stage IIIa =0, Stage IIIb =1 |
| Smoking history | Yes =1, No =0 |
| Maximum tumor diameter | >6 cm =1, ≤6 cm =0 |
| Prognosis | Poor prognosis =1, Good prognosis =0 |
Table 6.
Multivariate analysis
| Factor | B | S.E. | Wals | Sig. | Exp (B) | 95% C.I. of the EXP (B) | |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Lower limit | Upper limit | ||||||
| Age | 37.029 | 7965.487 | 0 | 0.996 | 1.2069E+16 | 0 | . |
| TNM stage | -16.893 | 5706.15 | 0 | 0.998 | 0 | 0 | . |
| Smoking history | 3.497 | 0.995 | 12.35 | 0 | 33 | 4.695 | 231.956 |
| Maximum tumor diameter | 18.345 | 5557.776 | 0 | 0.997 | 92666639.6 | 0 | . |
Discussion
Among respiratory malignancies, LC has the highest incidence and the highest mortality rate, and thus remains a serious threat to human life and health worldwide [17]. Since the clinical symptoms of early-stage LC are not obvious and atypical, most patients are diagnosed with advanced LC. In addition, the survival cycle of patients with advanced LC is short, and generally the natural survival time of most patients may not exceed one year, with less than 50% of patients exceeding one year and only about 15% of patients exceeding 5 years, which imposes a great psychological burden on patients and their families [18,19]. In addition, affected by cancer metastasis, treatment and other factors, patients will have different degrees of pain, and the resulting anxiety, resistance to treatment and other adverse emotions will seriously hinder the treatment of the disease, so nursing is particularly important. Currently, most clinical care is focused on purely caring for disease, so it is difficult to meet the multifaceted needs of patients for care [20]. Fine nursing refers to a patient-centered care model in which a more detailed, personalized care plan is developed based on the actual needs of patients, which supplies better care for them [21].
Patients with advanced LC may suffer from cough, dyspnea, or even metastasis to the head, causing a series of adverse reactions such as headache, and patients may experience different degrees of pain during radiotherapy treatment, which may easily lead to anxiety and tension, which will have a certain impact on patients’ treatment [22]. Therefore, pain care is also an important part of fine nursing. In this study, we analyzed and compared the changes in pain level and anxiety and depression in the two groups before and after nursing. The results manifested that the VAS, SAS, and SDS scores in the RG were lower than those in the CG after nursing, and the scores before nursing were higher than those after nursing in both groups, indicating that patients’ pain and anxiety and depression were relieved after nursing. Pain care and psychological care in fine nursing can effectively help patients reduce pain and relieve their restlessness, which is beneficial to the subsequent treatment and nursing of the disease. Hao et al. [23] found that fine nursing can effectively improve the quality of life and restlessness of elderly patients with coronary artery disease, greatly increasing their self-care motivation and expectations, which is similar to the present study. In addition, we also analyzed and compared the nutrition, sleep quality and quality of life of patients. The results manifested that the PG-SGA and PSQI scores of the RG were lower than those of the CG after nursing, and the PG-SGA and PSQI scores of both groups before nursing were higher than those after nursing, indicating that the nutrition and sleep quality of patients with advanced LC who had undergone fine nursing with dietary intervention had been improved to a great extent, which made patients’ physical fitness and immunity stronger and more conducive to fighting the disease. In addition, WHOQOL-BREF scores were higher in the RG than in the CG after nursing, and the scores were lower in both groups before nursing than after nursing, indicating that patients’ quality of life was improved, which was conducive to patients maintaining an optimistic attitude and actively cooperating with treatment, thus prolonging survival. Similarly, Ai et al. [24] found that fine nursing was effective in improving quality of life and reducing psychological stress in patients with upper gastrointestinal bleeding, which is similar to the present study. Comparison of the pulmonary function of the two groups after nursing revealed that the levels of FVC, FEV1, and MVV were significantly higher in the two groups, and the research group was higher than the control group, indicating that patients’ pulmonary function was significantly improved after fine nursing.
At the end of the study, the complications of patients before and after nursing were also analyzed and compared, and the results showed that the complication rate of patients in the CG was higher than that of those in the RG, indicating that the complication rate during the treatment of advanced LC patients who underwent fine nursing with dietary intervention was lower. The analysis of factors affecting patients’ prognosis manifested that age, TNM stage, smoking history, and maximum tumor diameter were risk factors affecting patients’ prognosis. Logistic regression analysis found that smoking history was an independent risk factor affecting patients’ prognosis. In addition, nursing satisfaction was also compared. The results revealed that the nursing satisfaction of patients in the CG was lower than that of those in the RG, indicating that fine nursing with dietary interventions was more easily accepted by patients than single conventional nursing, and that patients were more cooperative and had less difficulty to treat the disease. Fine nursing refines the quality and refinement of routine care and requires nursing staff to pay more attention to nursing details to make nursing more effective, accurate, rational, and controllable [25].
Although this study demonstrated the effectiveness of fine nursing in patients with advanced LC, there are still certain shortcomings. First of all, there were some differences in the work experience of the nursing staff, which may have had an impact on the quality of nursing for both groups. Second, the economic value to patients of the two types of care in the text was not analyzed from an economic perspective. Thus, we hope to conduct more experiments in the follow-up study to refine our findings.
In conclusion, fine nursing with dietary intervention can effectively reduce the pain of advanced LC patients, regulate patients’ restlessness, reduce the incidence of complications, improve nutrition, sleep quality and their quality of life, which is worthy of application and promotion in clinical practice.
Disclosure of conflict of interest
None.
References
- 1.Schabath MB, Cote ML. Cancer progress and priorities: lung cancer. Cancer Epidemiol Biomarkers Prev. 2019;28:1563–1579. doi: 10.1158/1055-9965.EPI-19-0221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Romaszko AM, Doboszyńska A. Multiple primary lung cancer: a literature review. Adv Clin Exp Med. 2018;27:725–730. doi: 10.17219/acem/68631. [DOI] [PubMed] [Google Scholar]
- 3.Jones GS, Baldwin DR. Recent advances in the management of lung cancer. Clin Med (Lond) 2018;18(Suppl 2):s41–s46. doi: 10.7861/clinmedicine.18-2s-s41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hirsch FR, Scagliotti GV, Mulshine JL, Kwon R, Curran WJ Jr, Wu YL, Paz-Ares L. Lung cancer: current therapies and new targeted treatments. Lancet. 2017;389:299–311. doi: 10.1016/S0140-6736(16)30958-8. [DOI] [PubMed] [Google Scholar]
- 5.Bade BC, Dela Cruz CS. Lung cancer 2020: epidemiology, etiology, and prevention. Clin Chest Med. 2020;41:1–24. doi: 10.1016/j.ccm.2019.10.001. [DOI] [PubMed] [Google Scholar]
- 6.Tammemägi MC, Berg CD, Riley TL, Cunningham CR, Taylor KL. Impact of lung cancer screening results on smoking cessation. J Natl Cancer Inst. 2014;106:dju084. doi: 10.1093/jnci/dju084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vinod SK, Hau E. Radiotherapy treatment for lung cancer: current status and future directions. Respirology. 2020;25(Suppl 2):61–71. doi: 10.1111/resp.13870. [DOI] [PubMed] [Google Scholar]
- 8.Nooreldeen R, Bach H. Current and future development in lung cancer diagnosis. Int J Mol Sci. 2021;22:8661. doi: 10.3390/ijms22168661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yuan Z, Yang S, Zhang C, Chen K, Wang M, Hao S, Dong S, Yang Y. Retrospective analysis of the clinical efficacy of early goal-directed therapy combined with meticulous nursing intervention in patients with posttraumatic sepsis. J Healthc Eng. 2021;2021:6706464. doi: 10.1155/2021/6706464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Castro-Barquero S, Ruiz-León AM, Sierra-Pérez M, Estruch R, Casas R. Dietary strategies for metabolic syndrome: a comprehensive review. Nutrients. 2020;12:2983. doi: 10.3390/nu12102983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dingemans AC, Soo RA, Jazieh AR, Rice SJ, Kim YT, Teo LLS, Warren GW, Xiao SY, Smit EF, Aerts JG, Yoon SH, Veronesi G, De Cobelli F, Ramalingam SS, Garassino MC, Wynes MW, Behera M, Haanen J, Lu S, Peters S, Ahn MJ, Scagliotti GV, Adjei AA, Belani CP. Treatment guidance for patients with lung cancer during the coronavirus 2019 pandemic. J Thorac Oncol. 2020;15:1119–1136. doi: 10.1016/j.jtho.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sung YT, Wu JS. The visual analogue scale for rating, ranking and paired-comparison (VAS-RRP): a new technique for psychological measurement. Behav Res Methods. 2018;50:1694–1715. doi: 10.3758/s13428-018-1041-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.De Groot LM, Lee G, Ackerie A, van der Meij BS. Malnutrition screening and assessment in the cancer care ambulatory setting: mortality predictability and validity of the patient-generated subjective global assessment short form (PG-SGA SF) and the GLIM criteria. Nutrients. 2020;12:2287. doi: 10.3390/nu12082287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abbasi-Ghahramanloo A, Soltani-Kermanshahi M, Mansori K, Khazaei-Pool M, Sohrabi M, Baradaran HR, Talebloo Z, Gholami A. Comparison of SF-36 and WHOQoL-BREF in measuring quality of life in patients with type 2 diabetes. Int J Gen Med. 2020;13:497–506. doi: 10.2147/IJGM.S258953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yue T, Li Q, Wang R, Liu Z, Guo M, Bai F, Zhang Z, Wang W, Cheng Y, Wang H. Comparison of hospital anxiety and depression scale (HADS) and Zung self-rating anxiety/depression scale (SAS/SDS) in evaluating anxiety and depression in patients with psoriatic arthritis. Dermatology. 2020;236:170–178. doi: 10.1159/000498848. [DOI] [PubMed] [Google Scholar]
- 16.Han Q, Liu B, Lin S, Li J, Liang P, Fu S, Zheng G, Yang S, Li B, Yang Q. Pittsburgh sleep quality index score predicts all-cause mortality in Chinese dialysis patients. Int Urol Nephrol. 2021;53:2369–2376. doi: 10.1007/s11255-021-02842-6. [DOI] [PubMed] [Google Scholar]
- 17.de Sousa VML, Carvalho L. Heterogeneity in lung cancer. Pathobiology. 2018;85:96–107. doi: 10.1159/000487440. [DOI] [PubMed] [Google Scholar]
- 18.Schwartz AG, Cote ML. Epidemiology of lung cancer. Adv Exp Med Biol. 2016;893:21–41. doi: 10.1007/978-3-319-24223-1_2. [DOI] [PubMed] [Google Scholar]
- 19.Brody H. Lung cancer. Nature. 2020;587:S7. doi: 10.1038/d41586-020-03152-0. [DOI] [PubMed] [Google Scholar]
- 20.Paterson C. Introduction: prostate cancer care - implications for nursing practice. Semin Oncol Nurs. 2020;36:151040. doi: 10.1016/j.soncn.2020.151040. [DOI] [PubMed] [Google Scholar]
- 21.Ren R, Bao S, Qian W, Zhao H. Topical ALA-photodynamic therapy combined with acne debridement and meticulous nursing for the treatment of moderate-severe acne in adolescent patients. Clin Cosmet Investig Dermatol. 2021;14:1303–1310. doi: 10.2147/CCID.S322768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Arrieta O, Lazcano E. Lung cancer. Epidemiology, diagnosis and treatment. Salud Publica Mex. 2019;61:217–218. doi: 10.21149/10660. [DOI] [PubMed] [Google Scholar]
- 23.Hao W, Ma T, Feng C. Application effect of meticulous nursing on community elderly patients with coronary heart disease under the background of medical treatment partnerships. J Healthc Eng. 2021;2021:3511985. doi: 10.1155/2021/3511985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ai H. A randomised controlled trial: effect of the meticulous nursing model on the treatment compliance and quality of life of patients with upper gastrointestinal bleeding. Ann Palliat Med. 2021;10:8737–8745. doi: 10.21037/apm-21-1283. [DOI] [PubMed] [Google Scholar]
- 25.Zhai Y, Li R, Yan Z. Research on application of meticulous nursing scheduling management based on data-driven intelligent optimization technology. Comput Intell Neurosci. 2022;2022:3293806. doi: 10.1155/2022/3293806. [DOI] [PMC free article] [PubMed] [Google Scholar]


