Abstract
Objective: This research was designed to probe into the effect of butylphthalide injection combined with gastrodin on sTRAIL and inflammatory factors in elderly patients with cerebral infarction (CI). Methods: Elderly CI patients admitted to the Strategic Support Force Characteristic Medical Center from June 2019 to September 2021 were collected for this retrospective analysis, and then divided into Group A and B. Patients in group A were given gastrodin injection by intravenous drip, and those in group B were treated with butylphthalide injection additionally. The general data, efficacy and adverse reactions of patients were observed and compared. The neurological impairment (NIHSS) score before and after treatment was analyzed. The activities of daily living and Barthel index (BI) after treatment were tested. The levels of sTRAIL and inflammatory factors were assessed before and after treatment. Their quality of life (SF-36 score) was observed before and after treatment. Logistic regression was used to analyze the risk factors affecting patient prognosis. Results: There was no difference in general data between the two groups (P>0.05). Compared with group A, group B showed higher total effective rate (P<0.05), lower total incidence of adverse reactions (P<0.05), and lower NIHSS scores after treatment (P<0.05). Besides, after treatment, the levels of sTRAIL and inflammatory factors were lower (P<0.05), BI was higher (P<0.05), and the quality of life was better (P<0.05) in group B than in group A. Age and NIHSS score were risk factors for poor prognosis (P<0.05). Conclusion: Butylphthalide injection combined with gastrodin is better than gastrodin alone in the treatment of senile CI. This combination can improve the neurological function and activities of daily living and reduce the levels of serum sTRAIL and inflammatory factors in patients.
Keywords: Butylphthalide, gastrodin, cerebral infarction, inflammatory factors
Introduction
Cerebral infarction (CI) is an acute cerebrovascular disease, which occurs because of cerebral vascular obstruction resulting from atherosclerosis or arteriosclerosis and fat accumulation [1,2]. Due to high mortality, it is has been called the “No. 1 killer” of health, and it seriously affects the quality of life of patients [3,4]. Previously, it has been shown that CI can cause brain tissue damage, including hemorrhagic and ischemic stroke. sTRAIL is the receptor 2 of an apoptosis-inducing ligand related to soluble tumor necrosis factor, which is a sign of plaque apoptosis and cardiovascular events [5]. sTRAIL levels can predict cardiovascular events in the general population. In addition, a high level of plasma sTRAIL is associated with higher risk of severe cerebral atherosclerosis, while a high level of plasma TRAIL is related to lower risk [6]. Due to a strict treatment time window and bleeding complications after treatment, the intravenous thrombolysis rate after CI is not high [7]. Thus, it is particularly important to find new drug targets and choose a better treatment scheme for CI to provide a reliable basis for improved therapy.
Gastrodin is extracted from Gastrodia elata Blume. Natural phenolic compounds have been used to improve stroke, epilepsy, dizziness and dementia for a long time [8]. Gastrodin reduces the levels of neurotoxic proinflammatory mediators and cytokines. This discovery implies that gastrodin may have beneficial effects on central nervous system diseases [9]. However, the potential mechanism is still unknown. Butylphthalide sodium chloride injection has certain efficacy in CI patients [10]. Although several drug mechanisms have been proposed, the effects of butylphthalide injection combined with gastrodin on inflammatory cytokines in the immune system of elderly CI patients have not been reported. This experiment studied the effect of butylphthalide injection combined with gastrodin on sTRAIL and inflammatory factors in elderly CI patients.
Methods
General data
Elderly CI patients admitted to the Strategic Support Force Characteristic Medical Center from June 2019 to September 2021 were collected for this retrospective analysis, and then divided into Group A and B. Patients in group A were given gastrodin injection by intravenous drip, and those in group B were additionally treated with butylphthalide injection. There were 35 males and 22 females in group B, with an average age of (72.02±2.47) years. In group A, there were 34 males and 19 females, with an average age of (71.33±2.70) years. This study was approved by the Ethics Committee of the Strategic Support Force Characteristic Medical Center.
Inclusion and exclusion criteria
Inclusion criteria: Patients met the diagnostic criteria established by the Fourth National Conference on Cerebrovascular Diseases [11]; patients admitted within 48 h of onset of illness; patients were diagnosed with CI and hemorrhage by imaging; patients was able to take care of themselves before the onset of the disease. Exclusion criteria: patients with severe infections, cancer, multisystem dysfunction or bleeding tendencies; patients who had been treated with other drugs prior to admission or were not first-episode patients; women during pregnancy; patients aged younger than 18 years.
Patient treatment options
Group A was given asparagine injection (produced by Shaanxi Bosen Biological Pharmaceutical Group Co., Ltd., SFDA Approval No. H20059312, 2 mL: 0.2 g) 0.6 g in 5% glucose injection, 250 mL intravenously once daily for 2 weeks. Group B was given the same treatment of asparagine injection with additional intravenous butylphthalein sodium chloride injection (100 mL: 25 mg, produced by CSPC Enbipu Pharmaceutical Co. Ltd. SFDA Approval No. H20100041) 100 mL, twice daily for 2 weeks.
Outcome measures
Swallowing function was evaluated by the Standardized Swallowing Assessment (SSA) [12], and the scores were negatively correlated with swallowing function. Patients’ depression and anxiety were evaluated through the Hamilton Depression Scale (HAMD) [13] and Hamilton Anxiety Scale (HAMA) [14], respectively, and the scores were positively correlated with the levels of depression and anxiety. The recovery of patients’ neurological function was analyzed via the National Institutes of Health Stroke Scale (NIHSS) [15], and the scores were positively correlated with the recovery of neurological function. The recovery of limb movement was tested via Barthel index (BI), and the scores were positively correlated with the recovery of limb function. The quality of life (cognitive function, emotional function, overall function and social function) were evaluated by SF-36 scale [16], with a total score of 100 points, and the higher the score, the higher the quality of life. sTRAIL (ml025375), OPG (ml063551), TNF-α (ml077385) and IL-8 (ml028580) were tested via ELISA (All kits are from Mlbio, shanghai, Beijing). The postoperative complications, including epilepsy, gastrointestinal bleeding, pulmonary infection and arrhythmia, were recorded. The efficacy of patients was assessed [17]. According to NIHSS score, the efficacy was reflected in the change of neurological deficit scores, as follows: decreased 91%-100% (markedly effective), decreased 18%-91% (effective), decreased less than 18% (ineffective) and increased more than 18% (aggravated). The overall efficacy was calculated: overall efficacy = (number of patients with markedly effective response + number of those with effective response)/total number of patients × 100%. The patients with markedly effective and effective response were further put into an improvement group, and the patients with ineffective and aggravated response were put into a non-improvement group. Then, the risk factors affecting patients’ prognosis were analyzed using logistic regression.
Statistical methods
Data were statistically analyzed via SPSS 19.0 (Asia Analytics Formerly SPSS China). The counting data were analyzed via χ2 test. The measurement data were represented as (mean ± SD) and processed via t test. The risk factors affecting patient prognosis were assessed through Logistic regression-based analysis. P<0.05 denoted that the difference was statistically significant.
Results
General data
No obvious difference was shown in the general data such as sex, age, body mass index, history of smoking and drinking and obesity between the two groups (P>0.05) (Table 1).
Table 1.
General data of both groups of patients
| Classification | Group A (n=53) | Group B (n=57) | t/X2 | P |
|---|---|---|---|---|
| Sex | 0.089 | 0.766 | ||
| Male | 34 (64.15) | 35 (61.40) | ||
| Female | 19 (36.85) | 22 (38.60) | ||
| Age (years) | 71.33±2.70 | 72.02±2.47 | 1.400 | 0.165 |
| BMI (kg/m2) | 22.05±1.46 | 22.38±1.10 | 1.345 | 0.182 |
| Smoking | 0.104 | 0.747 | ||
| Yes | 35 (67.31) | 40 (70.18) | ||
| No | 17 (32.69) | 17 (29.82) | ||
| Drinking | 0.967 | 0.325 | ||
| Yes | 39 (73.58) | 37 (64.91) | ||
| No | 14 (26.42) | 20 (35.09) | ||
| Hyperlipidemia | 0.015 | 0.901 | ||
| Yes | 35 (66.04) | 37 (64.91) | ||
| No | 18 (33.96) | 20 (35.09) | ||
| Hypertension | 0.002 | 0.967 | ||
| Yes | 37 (69.81) | 40 (70.18) | ||
| No | 16 (30.19) | 17 (29.82) | ||
| Diabetes | 0.055 | 0.815 | ||
| Yes | 15 (28.30) | 15 (26.32) | ||
| No | 38 (71.70) | 42 (73.68) |
Note: Body Mass Index (BMI).
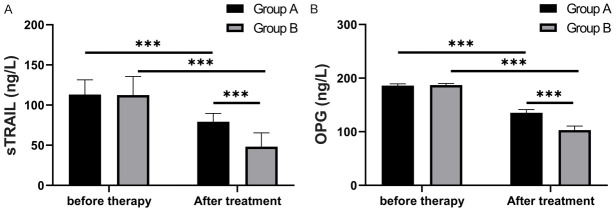
Swallowing function
With regard to the SSA scores before and after treatment between in the two groups, there was no statistical difference in the SSA scores between the two groups before treatment (P>0.05). After treatment, the SSA scores in both groups were lower compared with those before treatment (P<0.05), and the scores of patients in group B were lower than those in group A (P<0.05) (Figure 1).
Figure 1.
SSA scores in both groups: The SSA scores decreased in both groups after treatment, and the score of group B after treatment was lower than that of group A (P<0.001). Note: *** means P<0.001; Standardized Swallowing Assessment (SSA).
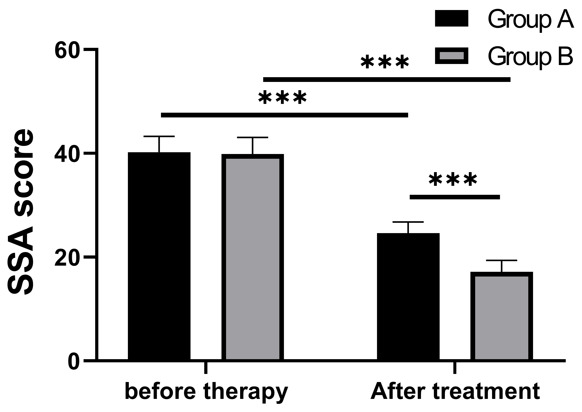
Comparison of quality of life
In terms of quality of life (cognitive function, emotional function, overall function, and social function), there was no statistical difference in the quality of life between the two groups before treatment (P>0.05). After treatment, the quality of life of patients in both groups increased compared with those before treatment (P<0.05), and the quality of life of patients in group B was better than that in group A (P<0.001) (Figure 2).
Figure 2.
Quality of life: After treatment, the scores of quality of life (cognitive function, emotional function, holistic function and social function) in group B were better than those in group A (P<0.001). Note: *** means P<0.001, short form 36 questionnaire.
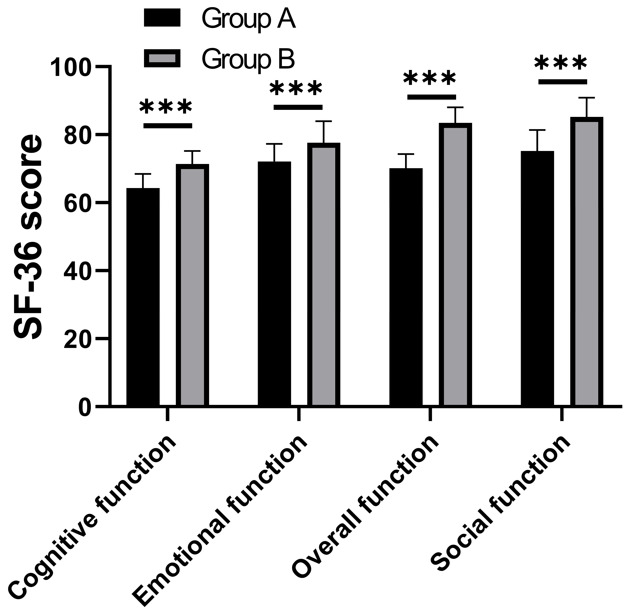
Recovery of anxiety and depression
It was revealed that there was no statistical difference between HAMD and HAMA scores before treatment (P>0.05). After treatment, HAMD and HAMA scores were lower in both groups compared with those before treatment (P<0.05), and the two scores were lower in group B than in group A after treatment (P<0.001) (Figure 3).
Figure 3.
HAMD, HAMA scores in two groups: There was no significant difference in HAMD (A) and HAMA (B) scores before treatment (P>0.05), but after treatment, the scores of patients in group B were obviously lower than those in group A (P<0.001). Note: *** means P<0.001; Hamilton Depression Scale (HAMD); Hamilton Anxiety Scale (HAMA).
Nerve function and limb function
There was no statistical difference between NIHSS and BI scores before treatment between the two groups (P>0.05). After treatment, the NIHSS scores were lower, while the BI scores were higher in both groups compared with those before treatment (P<0.05). Also, the post-treatment NIHSS score in group B was lower than that in group A, while the post-treatment BI score in group B was higher than that in group A (P<0.001) (Figures 4, 5).
Figure 4.
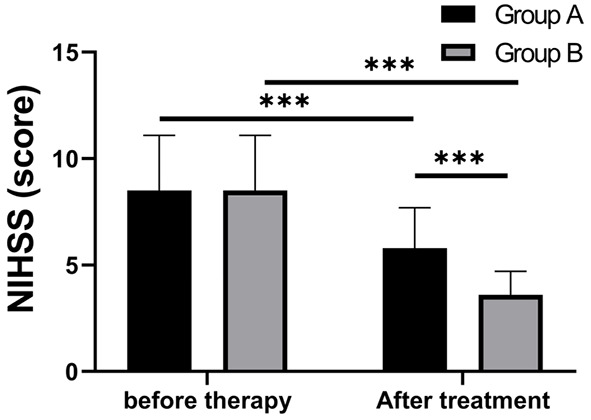
NIHSS scores in both groups: the NIHSS scores decreased in both groups after treatment, and the score of group B after treatment was lower than that of group A (P<0.001). Note: *** means P<0.001; National Institutes of Health Stroke Scale (NIHSS).
Figure 5.
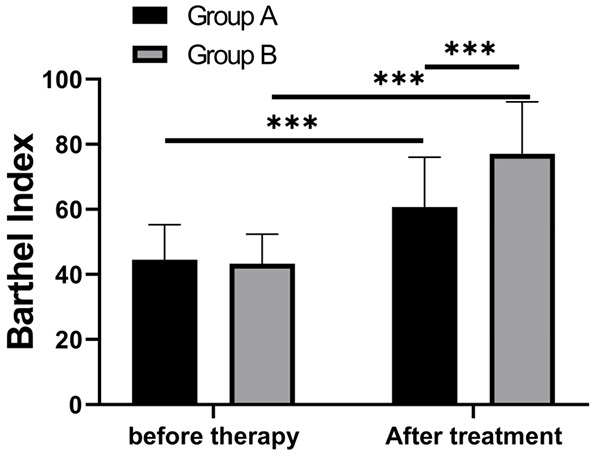
Barthel index of both groups. There was no difference in Barthel index between the two groups before treatment (P>0.05), but after treatment, the score of patients in group B was higher than that in group A (P<0.001). Note: *** means P<0.001.
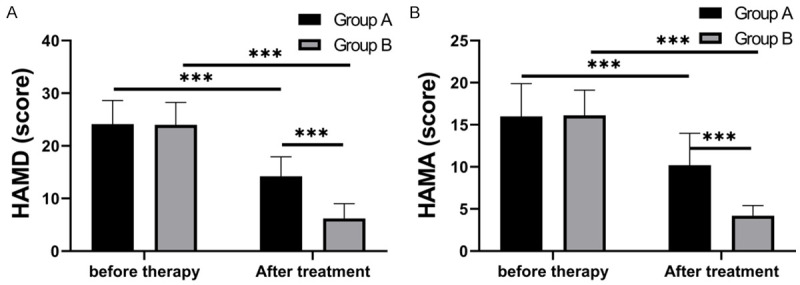
sTRAIL, OPG and inflammatory factors
Comparisons of sTRAIL, OPG, TNF-α and IL-8 before and after treatment between the two groups revealed that there was no statistical difference in sTRAIL, OPG, TNF-α and IL-8 between the two groups before treatment (P>0.05). After treatment, sTRAIL, OPG, TNF-α and IL-8 were lower in both groups compared with those before treatment (P<0.05), and the four were lower in group B than those in group A (P<0.001) (Figures 6, 7).
Figure 6.
Levels of sTRAIL and OPG. The levels of serum sTRAIL (A) and OPG (B) decreased in both groups after treatment (P<0.001), and there was no difference between them before treatment (P>0.05), but the levels in group B were lower than those in group A after treatment (P<0.001). Note: *** means P<0.001, Soluble tumor necrosis factor related apoptosis inducing ligand (sTRAIL), Osteoprotectin (OPG).
Figure 7.
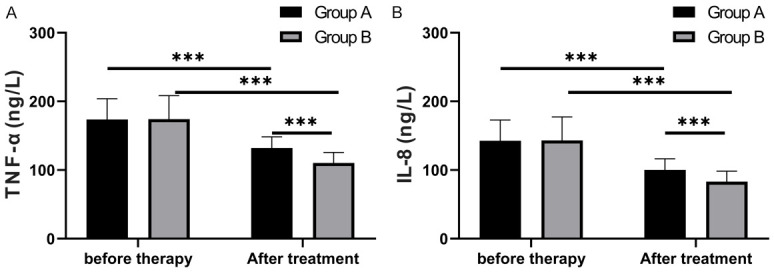
Levels of inflammatory factors. The levels of serum TNF-α (A) and IL-8 (B) decreased in both groups after treatment (P<0.001), and there was no difference between them before treatment (P>0.05), but the levels in group B were lower than those in group A after treatment (P<0.001). Note: *** means P<0.001, tumor necrosis factor-α (TNF-α), Interleukin 8 (IL-8).
Adverse reactions
Compared with that in group A, the incidence of epilepsy, gastrointestinal bleeding, pulmonary infection and arrhythmia in group B was lower (P<0.05) (Table 2).
Table 2.
Incidence of adverse reactions in both groups
| Classification | Group A (n=53) | Group B (n=57) | X2 | P |
|---|---|---|---|---|
| Epilepsy | 2 (3.77) | 1 (1.75) | - | - |
| Gastrointestinal bleeding | 1 (1.89) | 1 (1.75) | - | - |
| Pulmonary infection | 2 (3.77) | 0 (0.00) | - | - |
| Arrhythmia | 2 (3.77) | 1 (1.75) | - | - |
| Total incidence of adverse reactions | 13.21% | 5.26% | 1.341 | 0.247 |
Clinical efficacy
Compared with that in group A, the total effective treatment rate was higher in group B (P>0.05) (Table 3).
Table 3.
Total effective rate of two groups of patients
| Classification | Group A (n=53) | Group B (n=57) | X2 | P |
|---|---|---|---|---|
| Markedly effective | 25 (47.17) | 27 (47.37) | - | - |
| Effective | 20 (37.74) | 27 (47.37) | - | - |
| Ineffective | 4 (7.55) | 2 (3.51) | - | - |
| Aggravated | 4 (7.55) | 1 (1.75) | - | - |
| Total effective rate | 84.91% | 94.74% | 2.949 | 0.086 |
Analysis of prognostic factors
Patients were divided into an improvement group (n=99) and a non-improvement group (n=11) based on their conditions after treatment. The clinical data of patients were collected to analyze the risk factors affecting their prognosis by logistic regression. In our results, age and NIHSS score were found to be risk factors affecting the prognosis of patients (Table 4, P<0.05).
Table 4.
Analysis of prognostic factors
| Factor | Single-factor analysis | Multi-factor analysis | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| P value | OR value | 95% CI | P value | OR value | 95% CI | |
| Sex | 0.978 | 0.972 | 0.134-7.053 | |||
| Age | 0.013 | 11.466 | 1.675-78.494 | 0.008 | 10.638 | 1.835-61.66 |
| BMI | 0.696 | 0.845 | 0.363-1.968 | |||
| History of smoking | 0.703 | 1.443 | 0.219-9.524 | |||
| History of alcoholism | 0.851 | 0.844 | 0.142-4.995 | |||
| Hyperlipidemia | 0.380 | 0.448 | 0.074-2.695 | |||
| Hypertension | 0.350 | 2.570 | 0.356-18.574 | |||
| Diabetes | 0.555 | 1.673 | 0.303-9.234 | |||
| NIHSS | 0.009 | 2.486 | 1.259-4.906 | 0.002 | 2.343 | 1.366-4.02 |
Note: Body Mass Index (BMI); National Institutes of Health Stroke Scale (NIHSS).
Discussion
CI is a cardiovascular disease with high morbidity and mortality. At the moment, many studies have reported upon traditional Chinese medicine in treating CI. Gastrodin is a major traditional Chinese medicine [18]. Nevertheless, the effect and mechanism of gastrodin on CI are still unclear. An important cause of CI is the serious neurological deficit in patients with brain injury [19]. OPG, a member of TNF receptor superfamily, is involved in the development of atherosclerosis. It affects the relationship between the severity of neurological deficit and vascular stenosis in patients with brain injury [20]. The plasma OPG level increases with the increase of the number of cerebral arteries in atherosclerosis, which is considered as a biomarker of cerebral atherosclerosis [21]. In various acute and chronic central nervous system diseases, the inflammatory process leads to brain cell damage and disease progression [22]. sTRAIL, together with other regulatory cytokines, is involved in pathological process of various types of encephalitis, stroke and Alzheimer’s disease. Based on various beneficial and harmful effects in the immune and nervous systems, sTRAIL has marked neuroprotective potential for limiting acute granulocyte-driven inflammation [23]. Related studies have shown that after stimulation with TNF-α and IL-1β, the release of sTRAIL in cultured monocytes increases, and plaque sTRAIL plays a vital role in inflammatory activation and erythrocytosis. The association between sTRAIL and inflammatory cytokines may also reflect the ongoing macrophage phenotype transfer [24]. The levels of sTRAIL and inflammatory factors can reflect the recovery of the body after patients receive treatment for CI. This experiment proved that the levels of sTRAIL, OPG and inflammatory factors in the two groups decreased after treatment, and those in group B were lower than those in group A. The TNF-α and IL-8 levels in serum decreased obviously after treatment, but deceases in group B were more significant than those in group A.
This study also compared the neurological function and mental health scores of all patients. With the decrease of the number of brain cells in the elderly, their memory function declines, and some corresponding reactions or execution also declines [25]. Thus, brain damage in the elderly mainly refers to the decline of cognition. There is a great correlation between neurological function and depression. When the neurological function becomes worse, the depression of patients becomes more serious, and the improvement of neurological function indicates that their depression is alleviated [26]. Our experimental results showed that patients treated with butylphthalide injection combined with gastrodin had better mental health. In terms of BI, the score of patients receiving butylphthalide injection combined with gastrodin was higher, which indicated that the limb function of these patients recovered better.
In the case of acute CI, hormone secretion increases rapidly. Intravenous instillation of butylphthalide and sodium chloride can regulate human immunity and reduce complications such as infection, so it is an effective brain protection therapy [1]. The quality of life in group B was better than that in group A after treatment, and the incidence of adverse reactions such as epilepsy, gastrointestinal bleeding, pulmonary infection and arrhythmia was also lower in group B than that in group A. Dysphagia is relevant to CI, especially for elderly CI patients, and can easily lead to pulmonary infection [27]. According to the recovery of swallowing function and limb function in this research, butylphthalide injection combined with gastrodin were more effective in improving limb neurological function in elderly CI patients, and the combined use of the two drugs alleviated dysphagia. With the improvement of swallowing function, the incidence of epilepsy, gastrointestinal bleeding, pulmonary infection and arrhythmia adverse reactions of patients was greatly reduced, which improved their quality of life.
At the end of the study, we analyzed the factors affecting the prognosis of patients and found that age and NIHSS score were risk factors affecting their prognosis. It was discovered that the risk of poor prognosis increased significantly with age, which is related to the decreased physical function and weakened immunity in elderly patients. Besides, elderly patients are commonly combined with various underlying diseases and thereby have a poorer prognosis [28]. The NIHSS score not only reflects stroke severity, but is also an important factor in determining stroke regression. Higher NIHSS scores suggest more severe neurological damage in patients with AIS and often predispose them to early neurological deterioration [29]. Therefore, treatment for stroke patients should be targeted by paying attention to their age and the NIHSS score at the time of admission.
Nevertheless, there are still some shortcomings in this study. For example, we have not investigated patients’ cooperation during operation and their satisfaction with the treatment. In future clinical studies, we will improve these shortcomings, making the treatment and prognosis plans more suitable for patients and more conducive to their recovery.
In general, butylphthalide injection combined with gastrodin has a better down-regulation effect on expression of sTRAIL and its related inflammatory regulators in elderly CI patients than conventional gastrodin treatment. The combination improves neurological damage and limb function, thus improving the quality of life of patients, so it is worthy of clinical promotion.
Disclosure of conflict of interest
None.
References
- 1.Matsumoto K, Sato S, Okumura M, Niwa H, Hida Y, Kaga K, Date H, Nakajima J, Usuda J, Suzuki M, Souma T, Tsuchida M, Miyata Y, Takeshi N Committee for Patient Safety, Quality Management of Japanese Association for Chest Surgery. Left upper lobectomy is a risk factor for cerebral infarction after pulmonary resection: a multicentre, retrospective, case-control study in Japan. Surg Today. 2020;50:1383–1392. doi: 10.1007/s00595-020-02032-4. [DOI] [PubMed] [Google Scholar]
- 2.Bao L, Zhang S, Gong X, Cui G. Trousseau syndrome related cerebral infarction: clinical manifestations, laboratory findings and radiological features. J Stroke Cerebrovasc Dis. 2020;29:104891. doi: 10.1016/j.jstrokecerebrovasdis.2020.104891. [DOI] [PubMed] [Google Scholar]
- 3.Xin Y, Shi S, Yuan G, Miao Z, Liu Y, Gu Y. Application of CT imaging in the diagnosis of cerebral hemorrhage and cerebral infarction nerve damage. World Neurosurg. 2020;138:714–722. doi: 10.1016/j.wneu.2020.02.007. [DOI] [PubMed] [Google Scholar]
- 4.Wang D, Bo Z, Lan T, Pan J, Cui D. Application of magnetic resonance imaging molecular probe in the study of pluripotent stem cell-derived neural stem cells for the treatment of posttraumatic paralysis of cerebral infarction. World Neurosurg. 2020;138:637–644. doi: 10.1016/j.wneu.2020.01.146. [DOI] [PubMed] [Google Scholar]
- 5.Goncalves I, Singh P, Tengryd C, Cavalera M, Yao Mattisson I, Nitulescu M, Flor Persson A, Volkov P, Engstrom G, Orho-Melander M, Nilsson J, Edsfeldt A. sTRAIL-R2 (soluble TNF [tumor necrosis factor]-related apoptosis-inducing ligand receptor 2) a marker of plaque cell apoptosis and cardiovascular events. Stroke. 2019;50:1989–1996. doi: 10.1161/STROKEAHA.119.024379. [DOI] [PubMed] [Google Scholar]
- 6.Mielczarek-Palacz A, Sikora J, Kondera-Anasz Z. Assessment of concentrations of sTRAIL ligand and its receptors sTRAIL-R1 and sTRAIL-R2 - markers monitoring the course of the extrinsic pathway of apoptosis induction: potential application in ovarian cancer diagnostics. Arch Med Sci. 2017;13:624–628. doi: 10.5114/aoms.2015.53144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baena Alvarez B, Garcia-Madrona S, Sainz Amo R, Rodriguez Jorge F, Gomez Corral J, Vera Lechuga R, Matute Lozano MC, Sanchez Sanchez A, De Felipe Mimbrera A, Cruz Culebras A, Masjuan Vallejo J. Intravenous thrombolysis for acute ischemic stroke in centenarians. Eur Geriatr Med. 2021;12:893–897. doi: 10.1007/s41999-021-00494-4. [DOI] [PubMed] [Google Scholar]
- 8.Liu XC, Wu CZ, Hu XF, Wang TL, Jin XP, Ke SF, Wang E, Wu G. Gastrodin attenuates neuronal apoptosis and neurological deficits after experimental intracerebral hemorrhage. J Stroke Cerebrovasc Dis. 2020;29:104483. doi: 10.1016/j.jstrokecerebrovasdis.2019.104483. [DOI] [PubMed] [Google Scholar]
- 9.Zhang HS, Liu MF, Ji XY, Jiang CR, Li ZL, OuYang B. Gastrodin combined with rhynchophylline inhibits cerebral ischaemia-induced inflammasome activation via upregulating miR-21-5p and miR-331-5p. Life Sci. 2019;239:116935. doi: 10.1016/j.lfs.2019.116935. [DOI] [PubMed] [Google Scholar]
- 10.Yang G, Zeng X, Li J, Leung CK, Zhang D, Hong S, He Y, Huang J, Li L, Li Z. Protective effect of gastrodin against methamphetamine-induced autophagy in human dopaminergic neuroblastoma SH-SY5Y cells via the AKT/mTOR signaling pathway. Neurosci Lett. 2019;707:134287. doi: 10.1016/j.neulet.2019.134287. [DOI] [PubMed] [Google Scholar]
- 11.Li Y, Teng D, Shi X, Qin G, Qin Y, Quan H, Shi B, Sun H, Ba J, Chen B, Du J, He L, Lai X, Li Y, Chi H, Liao E, Liu C, Liu L, Tang X, Tong N, Wang G, Zhang JA, Wang Y, Xue Y, Yan L, Yang J, Yang L, Yao Y, Ye Z, Zhang Q, Zhang L, Zhu J, Zhu M, Ning G, Mu Y, Zhao J, Teng W, Shan Z. Prevalence of diabetes recorded in mainland China using 2018 diagnostic criteria from the American Diabetes Association: national cross sectional study. BMJ. 2020;369:m997. doi: 10.1136/bmj.m997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Feng XG, Hao WJ, Ding Z, Sui Q, Guo H, Fu J. Clinical study on tongyan spray for post-stroke dysphagia patients: a randomized controlled trial. Chin J Integr Med. 2012;18:345–349. doi: 10.1007/s11655-012-1140-9. [DOI] [PubMed] [Google Scholar]
- 13.An JX, Williams JP, Fang QW, Wang Y, Liu H, Shi L, Zhang WH. Feasibility of patient-controlled sleep with dexmedetomidine in treating chronic intractable insomnia. Nat Sci Sleep. 2020;12:1033–1042. doi: 10.2147/NSS.S262991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Erratum: epigenetic alterations of the promoter region of the pomc gene in adolescent depressive disorder patients with nonsuicidal self-injury behaviors [Erratum] Psychol Res Behav Manag. 2021;14:27–30. doi: 10.2147/PRBM.S298795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Amalia L, Dalimonthe NZ. Clinical significance of platelet-to-white blood cell ratio (PWR) and national institute of health stroke scale (NIHSS) in acute ischemic stroke. Heliyon. 2020;6:e05033. doi: 10.1016/j.heliyon.2020.e05033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wartenberg KE, Henkner J, Brandt S, Zierz S, Muller TJ. Effect of recanalization on cerebral edema, long-term outcome, and quality of life in patients with large hemispheric infarctions. J Stroke Cerebrovasc Dis. 2020;29:105358. doi: 10.1016/j.jstrokecerebrovasdis.2020.105358. [DOI] [PubMed] [Google Scholar]
- 17.Chen Q, Cao C, Gong L, Zhang Y. Health related quality of life in stroke patients and risk factors associated with patients for return to work. Medicine (Baltimore) 2019;98:e15130. doi: 10.1097/MD.0000000000015130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li L, Ren S, Hao X, Zhen Z, Ji H. Efficacy of minimally invasive intervention in patients with acute cerebral infarction. J Cardiovasc Pharmacol. 2019;73:22–26. doi: 10.1097/FJC.0000000000000625. [DOI] [PubMed] [Google Scholar]
- 19.Lv Y, Cao H, Chu L, Peng H, Shen X, Yang H. Effects of gastrodin on BV2 cells under oxygen-glucose deprivation and its mechanism. Gene. 2021;766:145152. doi: 10.1016/j.gene.2020.145152. [DOI] [PubMed] [Google Scholar]
- 20.Deligiorgi MV, Panayiotidis MI, Griniatsos J, Trafalis DT. Harnessing the versatile role of OPG in bone oncology: counterbalancing RANKL and TRAIL signaling and beyond. Clin Exp Metastasis. 2020;37:13–30. doi: 10.1007/s10585-019-09997-8. [DOI] [PubMed] [Google Scholar]
- 21.Akhtar Ali S, Kang H, Olney R, Ramos-Platt L, Ryabets-Lienhard A, Cheung C, Georgia S, Pitukcheewanont P. Evaluating RANKL and OPG levels in patients with Duchenne muscular dystrophy. Osteoporos Int. 2019;30:2283–2288. doi: 10.1007/s00198-019-05077-5. [DOI] [PubMed] [Google Scholar]
- 22.Sun J, Sun WJ, Li ZY, Li L, Wang Y, Zhao Y, Wang C, Yu LR, Li LZ, Zhang YL. Daidzein increases OPG/RANKL ratio and suppresses IL-6 in MG-63 osteoblast cells. Int Immunopharmacol. 2016;40:32–40. doi: 10.1016/j.intimp.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 23.Luz A, Santos M, Magalhaes R, Oliveira JC, Pacheco A, Silveira J, Cabral S, Torres S, Leite-Moreira AF, Carvalho H. Soluble TNF-related apoptosis induced ligand (sTRAIL) is augmented by Post-Conditioning and correlates to infarct size and left ventricle dysfunction in STEMI patients: a substudy from a randomized clinical trial. Heart Vessels. 2017;32:117–125. doi: 10.1007/s00380-016-0851-9. [DOI] [PubMed] [Google Scholar]
- 24.Huang Y, Li X, Sha H, Zhang L, Bian X, Han X, Liu B. sTRAIL-iRGD is a promising therapeutic agent for gastric cancer treatment. Sci Rep. 2017;7:579. doi: 10.1038/s41598-017-00688-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Guo YB, Ji TF, Zhou HW, Yu JL. Effects of microRNA-21 on nerve cell regeneration and neural function recovery in diabetes mellitus combined with cerebral infarction rats by targeting PDCD4. Mol Neurobiol. 2018;55:2494–2505. doi: 10.1007/s12035-017-0484-8. [DOI] [PubMed] [Google Scholar]
- 26.Pan L, Jin J, Huang R, Wang W, Chen Q. Application of transcranial Doppler in prognosis assessment of nerve function in patients with acute cerebral infarction after intracranial mechanical thrombectomy. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2020;32:835–839. doi: 10.3760/cma.j.cn121430-20200410-00281. [DOI] [PubMed] [Google Scholar]
- 27.Zeng Y, Yip J, Cui H, Guan L, Zhu H, Zhang W, Du H, Geng X. Efficacy of neuromuscular electrical stimulation in improving the negative psychological state in patients with cerebral infarction and dysphagia. Neurol Res. 2018;40:473–479. doi: 10.1080/01616412.2018.1451015. [DOI] [PubMed] [Google Scholar]
- 28.van Alebeek ME, Arntz RM, Ekker MS, Synhaeve NE, Maaijwee NA, Schoonderwaldt H, van der Vlugt MJ, van Dijk EJ, Rutten-Jacobs LC, de Leeuw FE. Risk factors and mechanisms of stroke in young adults: the FUTURE study. J Cereb Blood Flow Metab. 2018;38:1631–1641. doi: 10.1177/0271678X17707138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Knight-Greenfield A, Nario JJQ, Gupta A. Causes of acute stroke: a patterned approach. Radiol Clin North Am. 2019;57:1093–1108. doi: 10.1016/j.rcl.2019.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]