Abstract
Background
Polypharmacy, using five or more medications, may increase the risk of nonadherence to prescribed treatment. We aimed to identify the interrelationship between trajectories of adherence to antiretroviral therapy (ART) and polypharmacy.
Methods
We included women with HIV (aged ≥ 18) enrolled in the Women’s Interagency HIV Study in the United States from 2014 to 2019. We used group-based trajectory modeling (GBTM) to identify trajectories of adherence to ART and polypharmacy and the dual GBTM to identify the interrelationship between adherence and polypharmacy.
Results
Overall, 1,538 were eligible (median age of 49 years). GBTM analysis revealed five latent trajectories of adherence with 42% of women grouped in the consistently moderate trajectory. GBTM identified four polypharmacy trajectories with 45% categorized in the consistently low group.
Conclusions
The joint model did not reveal any interrelationship between ART adherence and polypharmacy trajectories. Future research should consider examining the interrelationship between both variables using objective measures of adherence.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12981-023-00520-4.
Introduction
In the United States, women constitute a significant minority of the HIV epidemic. According to the Centers for Disease Control and Prevention (CDC) statistics, in 2020, women constituted 18% of the new cases diagnosed with HIV in the United States [1].
Adherence to antiretroviral therapy (ART) is a key component of successful treatment, yet women’s ART adherence is suboptimal. For example, in a recent analysis of 2,601 women enrolled in the Women’s Interagency HIV Study (WIHS) in the United States, 18% of participants reported taking ART less than 75% of the time, and only 52% were virally suppressed [2]. Substantial advances have been made in developing potent antiretroviral drugs with lower toxicity and improved pharmacokinetic profiles [3].
Concurrent with challenges in adherence are challenges that arise with increasing rates of premature comorbid conditions that commonly arise as people with HIV (PWH) age. Women followed in the WIHS were found to have a significantly higher mean number of non-AIDS-related comorbidities compared to HIV seronegative women (3.6 vs. 3.0, respectively) [4]. An increase in comorbidities typically leads to polypharmacy, defined as the concomitant use of five or more non-HIV medications with ART [5]. Polypharmacy can be associated with negative consequences such as nonadherence to treatment due to pill burden, increased medication side effects, and drug-drug interactions [6]. Among women with HIV (WHIV) and without HIV enrolled in WIHS both polypharmacy and the use of neurocognitive adverse effects medications were found to be strong determinants of falls [7]. Another study among elderly WHIV (> 50 years) in WIHS revealed a strong association between polypharmacy and poor executive function and processing speed [8]. In addition, polypharmacy can cause physical decline, hospitalization, and death [6]. Furthermore, polypharmacy can have a negative impact on the health-related quality of life outcomes of PWH [9].
A few studies have examined the impact of polypharmacy on adherence to ART therapy [10, 11]. For example, Zheng et al. [10] found that the high medication burden caused by polypharmacy, as measured by the Living with Medicines Questionnaire (LMQ), had a negative impact on ART self-reported adherence scores in a cross-sectional study of 185 Chinese PWH aged 50 years and above.
Static measures are commonly used to explore both adherence and polypharmacy (e.g., cross-sectional assessments of the proportion of days covered to measure adherence and pill count); however, these approaches fall short of capturing the dynamic nature of long-term behaviors and phenomena given the changing nature of many influencing factors [12]. Group-based trajectory modeling (GBTM) is a novel statistical data-driven approach used for analyzing developmental trajectories (i.e., the evolution of an outcome over age or time) [13]. In most studies, GBTM defines four to six trajectory groups that describe the dynamic behavior of longitudinal adherence [13]. Identifying individuals with suboptimal adherence trajectories is valuable because it informs the design of tailored interventions based on the group’s specific characteristics [14]. The identification of multiple characteristics defining the group may be more relevant for screening purposes when compared to single risk factors. Moreover, compared to the conventional method of determining the level of adherence based on dichotomized cut-offs and specific time points, GMBT can predict treatment outcomes with trends over time, both from initiation and during chronic care [15]”.
To the best of our knowledge, no other study has used dual GBTM to delineate the evolution of adherence and polypharmacy over time and characterize the interrelationships between them. We hypothesized that GBTM analysis would delineate different latent trajectories of ART adherence and of polypharmacy with variation in the predictors of group membership among trajectories of both variables; we specifically anticipated that a high polypharmacy trajectory would be associated with low ART adherence among WHIV enrolled in WIHS.
Methods
Study design
We conducted a retrospective analysis of longitudinal data of WHIV enrolled in WIHS between April 2014 to September 2019. WIHS is the oldest and largest prospective cohort of women living with or at risk for HIV [16, 17], which has now been combined with the Multicenter AIDS Cohort Study (MACS) to form the MACS/WIHS Combined Cohort Study (MWCCS). The main goal of WIHS is to investigate the natural history of HIV treatment and prevention in women in the United States. WIHS was founded in 1993, and women were recruited in four waves (1994-95, 2001–2002, 2011–2012, and 2013–2015). During the first three waves, participants were enrolled from the Bronx and Brooklyn, New York; Washington, DC; Los Angeles and San Francisco, California; and Chicago, Illinois. During the fourth wave, more participants were recruited from other research sites in Atlanta, Georgia; Chapel Hill, North Carolina; Miami, Florida; Birmingham, Alabama; and Jackson, Mississippi [18]. The Institutional Review Board approved this study at each of the study sites.
WIHS data
At semi-annual study visits, data collection involved clinical exams, blood sample collection, and interviewer-administered questionnaires to collect basic sociodemographic, behavioral, and clinical data. This analysis included data on age (years), geographical region (Midwest, South, West, and Northeast), race (non-Hispanic white, non-Hispanic African American, and Hispanic of any race), educational level (below secondary, completed secondary, some college/completed college), household income (categorized here as <$24,000 vs. ≥$24,000), employment status (employed vs., unemployed), time since diagnosis with HIV (years), smoking status (women who never smoked, women who smoke, women who previously smoked), alcohol intake (abstainer, > 0–7 drinks/week, > 7–12 drinks/week, > 12 drinks/week), substance use at baseline (marijuana or hash, crack, cocaine, heroin, illicit methadone, methamphetamines, amphetamines, narcotics, hallucinogens, other drugs), and depression status (measured by the Center for Epidemiological Studies Depression (CES-D) Scale with a score of ≥ 16 indicating the presence of depressive symptoms and < 16 indicating no depression) [19]. It also included self-reported non-HIV and HIV medication use and adherence to ART. Self-reported ART adherence over the past month is categorized as “100% of the time”, “95–99% of the time”, “75–94% of the time”, “<75% of the time,” and “I have not taken any of my prescribed medications.”
Study participants
We included WHIV enrolled in WIHS between April 2014 to September 2019 aged ≥ 18 years on ART, who had at least three self-reported adherence measurements and three visits with recorded data on non-HIV medications. Women with less than three adherence measurements and less than three visits with non-HIV medications recorded data were excluded due to the prerequisites for fitting GBTM. The first adherence visit between the above dates was designated as the “baseline” visit.
Data analysis
Polypharmacy
To assess polypharmacy, we determined the number of non-HIV medications being taken at the time of each visit, including all reported prescribed and over-the-counter medications, herbal supplements, topical and ophthalmic, and as-needed medications. If a medication contained two or more pharmacologically active agents, each substance was counted individually in the analysis. Multivitamins that have multiple ingredients were counted as one. Herbals were counted as one regardless of the mixture. At each visit, polypharmacy was defined as the concomitant use of five or more non-HIV medications [6], and no polypharmacy was defined as zero to four non-HIV medications. Prescription-only polypharmacy was defined as five or more prescription-only medications, and no prescription polypharmacy was defined as zero to four non-HIV medications, excluding over-the-counter medications, herbal supplements, and as-needed medications. We defined polypharmacy as 5 or more medications because this threshold has been associated with poor treatment outcomes (e.g., disability, falls, frailty, and death) [20]. Furthermore, the definition has been used in most studies conducted among PWHIV to assess polypharmacy [21]. We assessed the pharmacologically active ingredients rather than the number of pills because the former is more comprehensive and can capture whether nonadherence to ART is due to pill burden or drug unintended effects.
Group-based trajectory modeling
We used GBTM to identify latent adherence and polypharmacy groups using a censored normal model and a logit model, respectively [22]. Each of the following steps was performed to identify the number and shape of trajectory groups for adherence and polypharmacy separately. Initially, the analysis procedure involved fitting several models sequentially to determine the appropriate number of trajectory groups. The second step entailed visual inspections and determining trajectory shapes considering constant, linear, quadratic, and cubic specifications. A set of criteria was considered to determine model fit namely, (1) Bayesian Information Criteria (BIC) with smaller values indicating better model fit, (2) the mean posterior probability of membership within each group (entropy) with values > 0.70 generally indicating acceptable classification, (3) the smallest group with at least 5% of the sample, (4) a tight confidence interval around estimated group membership probabilities and statistically significant groups (P < 0.05), and (5) parsimony in the model with few classes and parameters probabilities [13]. In addition, the model selection process was based on subject matter knowledge about the patterns of both variables and the interpretability of the model. The final step involved estimating a dual trajectory model using the univariate models that had been identified. We tested several models by varying the number of groups in each variable to ensure that the groups identified in univariate GBTM analysis in both adherence and polypharmacy were the best models for the joint analysis. The joint model summarized the interrelationships between adherence and polypharmacy trajectories as conditional probabilities of each variable on the other and their joint probabilities as well [13]. We assumed that the missingness was fully random, in which case GBTM would account for the missingness by fitting the model with maximum likelihood estimation and giving asymptotically unbiased parameter estimates [13].
Descriptive and comparative analysis
For each trajectory within adherence and polypharmacy, categorical variables were presented as numbers, and percentages and continuous variables were summarized as median and interquartile ranges (IQR). Comparisons were made across trajectories of adherence using the Chi-square test. We measured the association between the percentage of women who reported adherence at a level of ≥ 95% and the percentage of women on polypharmacy during the study period using the Pearson correlation method.
Predictors for membership in adherence trajectories
We fitted multinomial logistic regression analysis to identify predictors of the group membership of adherence, namely, age (years), race, educational level, annual income, alcohol intake, history of smoking, cumulative years in ART, depression, and substance use. We planned to use the group with the highest level of adherence probability as a reference group in the model. As an initial step, we performed univariable analyses, and covariates with P-values < 0.25 were selected to be included in the final model.
Sensitivity analyses
In a sensitivity analysis, we used the above-mentioned definition of prescription-only polypharmacy to classify women as having polypharmacy or not at every study visit. We assumed that the state of polypharmacy using prescription-only medications potentially affects ART adherence more than polypharmacy of a combination of prescription-only, over-the-counter, as-needed medications, and herbal supplements. We used GBTM to identify polypharmacy trajectories using the logit model, following the same statistical steps and criteria for identifying group numbers and trajectory shapes described above. Furthermore, we used GBTM to conduct another sensitivity analysis in which we considered the number of non-HIV medications as a continuous variable. We included all prescription-only, over-the-counter, as-needed medications, and herbal supplements in this analysis. We assumed that using a large number of non-HIV medications concurrently with ART at any given time would create a burden and, as a result, influence adherence. Using the same statistical procedure described above, we used the censored normal model to identify the number and shapes of trajectories.
Data analysis was conducted using Stata version 16, and the Stata Plugin was used to estimate GBTM parameters.
Results
Participants’ baseline characteristics
Overall, 1,678 women were followed during the study period, of whom 1,538 (91.7%) were eligible for this analysis, contributing to 14,080 participant -visits. Self-reported ART adherence was recorded in 13,692 (97.2%) participant-visits and use of non-HIV medications in 13,987 (99.0%) participant-visits. The participants’ median age was 49 (interquartile range [IQR] 42–54) years and the majority (1,117; 72.6%) were non-Hispanic African Americans.
Group-based trajectory modeling
Average trend and association of adherence and polypharmacy over the study period
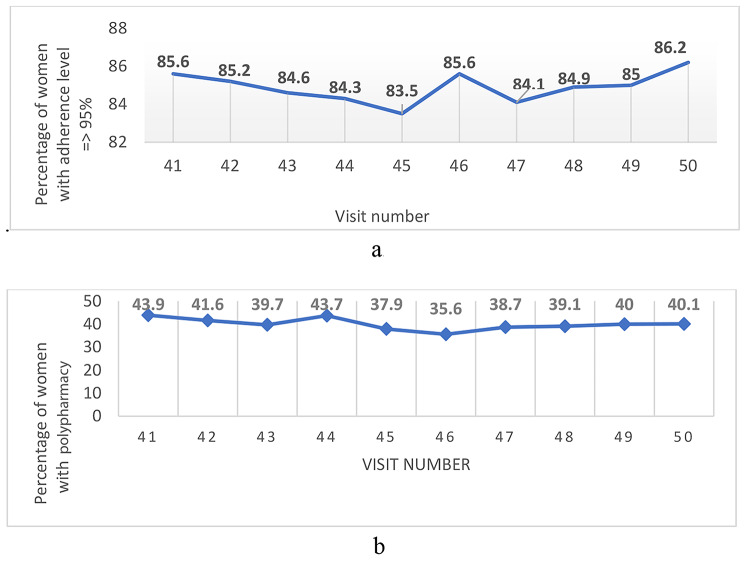
Figure 1a and b show the trends in the percentages of women with adherence levels ≥ 95% and the percentages of women with polypharmacy at each study visit. There were no linear trends in adherence or polypharmacy over the study period, with only small fluctuations in percentages between study visits in both variables. The overall correlation between adherence and polypharmacy during the study period was 0.11; (P = 0.75).
Fig. 1.
a Trends of > 95% self-report adherence to ART over the study period. b Trends of polypharmacy (5 + medications) over the study period
Trajectories of ART adherence
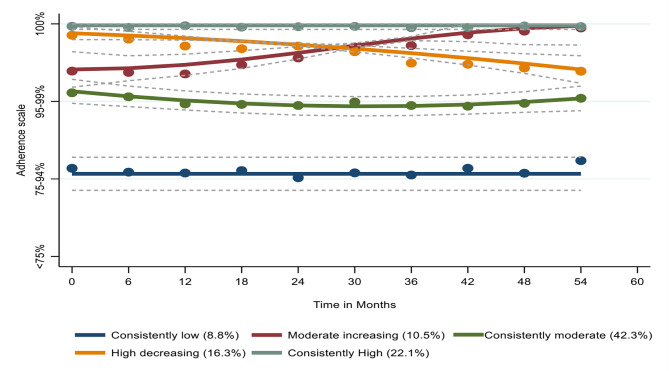
We identified five latent trajectories of adherence, namely ‘consistently low’ (N = 136; 8.8%), ‘consistently moderate’ (N = 650; 42.3%), ‘moderate increasing’ (N = 162; 10.5%) ‘high decreasing’ (N = 250; 16.3%), and ‘consistently high’ (N = 340; 22.1%), as depicted in Fig. 2. Women who belonged to the consistently low adherence group were more likely to be younger, recruited from study sites in western U.S, African American, highly educated (had Some college or completed college), used alcohol in different quantities, women who smoke, and experience depression symptoms at baseline compared to women in other groups. Table 1 shows women’s characteristics at the start of the current study by adherence trajectories. We compared the baseline characteristics of the women in the high decreasing and moderate increasing groups because their adherence patterns changed over time while the other three groups remained relatively stable. The women who followed the high decreasing trajectory were more likely to consume high quantities of alcohol compared to women who were members of the moderate increasing group, as shown in Table 2.
Fig. 2.
Trajectories of adherence to antiretroviral therapy
Table 1.
Women’s characteristics at the start of the current study by adherence trajectories in the WIHS cohort
| Characteristic | Adherence trajectories | ||||||
|---|---|---|---|---|---|---|---|
| Consistently high (n = 340) |
High decreasing (n = 250) |
Consistently moderate (n = 650) |
Moderate increasing (n = 162) |
Consistently low (n = 136) |
Total (n = 1538) |
P-value | |
| Geographical region | |||||||
|
Midwest West South Northeast |
33 (17.6) 25 (13.4) 143 (25.1) 139 (23.3) |
21(11.2) 21(11.3) 86 (15.1) 122 (20.5) |
100 (53.5) 87 (46.8) 238 (41.8) 225 (37.7) |
20(10.7) 27(14.5) 54 (9.4) 61(10.2) |
13(7.0) 26 (14.0) 48(8.4) 49(9.2) |
187 (12.2) 186 (12.1) 569 (37.0) 596 (38.7) |
< 0.001 |
| Age groups | |||||||
|
< 50 years ≥ 50 years |
166 (48.8) 174 (51.2) |
134 (53.6) 116 (46.4) |
358 (55.1) 292 (44.9) |
79 (48.8) 83 (51.2) |
93 (68.4) 43 (31.6) |
830 (54.0) 708 (46.0) |
0.002 |
| Race | |||||||
|
White African American Hispanic Others |
35 (10.3) 244 (71.8) 54 (15.8) 7 (2.1) |
31 (12.4) 176 (70.4) 36 (14.4) 7 (2.8) |
72 (11.1) 483 (74.3) 74 (11.4) 21 (3.2) |
13 (8.0) 107 (66.0) 37 (22.8) 5 (3.1) |
10 (7.4) 107 (78.7) 14 (10.3) 5 (3.6) |
161(10.5) 1117 (72.6) 215 (14.0) 45 (2.9) |
0.04 |
| Education | |||||||
|
Below secondary school Completed secondary school Some /completed college |
127 (37.4) 118 (34.7) 95 (27.9) |
83 (33.3) 78 (31.3) 88 (35.3) |
186 (28.7) 215 (33.1) 248 (38.2) |
60 (37.0) 48 (29.6) 54 (33.3) |
48 (35.5) 34 (25.2) 53 (39.3) |
504 (32.8) 493 (32.1) 538 (35.1) |
0.024 |
| Employment status | |||||||
|
No Yes |
225 (66.2) 115 (33.8) |
172 (68.8) 78 (31.2) |
416 (64.1) 233 (35.9) |
108 (67.1) 53 (32.9) |
84 (62.2) 51 (37.8) |
1005 (65.5) 530 (34.5) |
0.61 |
| Annual income | |||||||
|
≤ $24,000 >$24,000 |
270 (79.4) 70 (20.6) |
197 (78.8) 53 (21.2) |
478 (73.8) 170 (26.2) |
123 (75.9) 39 (24.1) |
106 (77.9) 30 (22.1) |
1174 (76.4) 362 (23.6) |
0.26 |
| Alcohol categories (%) | |||||||
|
0 drinks/week >0–7 drinks/week >7–12 drinks/week >12 drinks/week |
224 (65.9) 89 (26.2) 13 (3.8) 14 (4.1) |
125 (50.4) 98 (39.5) 8 (3.2) 17 (6.8) |
340 (52.3) 233 (35.8) 32 (4.9) 45 (6.9) |
105 (64.8) 49 (30.2) 3 (1.8) 5 (3.1) |
50 (36.8) 55 (40.4) 13 (9.6) 18 (13.2) |
844 (54.9) 524 (34.1) 69 (4.5) 99 (6.4) |
< 0.001 |
| History of smoking status (%) | |||||||
|
Women who never smoked Women who smoke Women who previously smoked |
130 (38.2) 113 (33.2) 97 (28.5) |
78 (31.2) 98 (39.2) 74 (29.6) |
235 (36.1) 239 (36.8) 176 (27.1) |
51 (31.5) 61 (37.7) 50 (30.7) |
38 (27.9) 69 (50.7) 29 (21.3) |
532 (34.6) 580 (37.7) 426 (27.7) |
0.04 |
| Substance use | |||||||
|
Yes No |
122 (35.9) 218 (64.1) |
70 (28) 180 (72) |
190 (29.4) 456 (70.6) |
47 (29.0) 115 (71.0) |
34 (25.2) 101 (74.8) |
463 (30.2) 1070 (69.8) |
0.1 |
| Depression symptoms (%) | |||||||
|
No Yes |
273 (80.3) 67 (19.7) |
183 (73.2) 67 (26.8) |
418 (64.3) 232 (35.7) |
114 (70.4) 48 (29.6) |
73 (53.7) 63 (46.3) |
1061(69.0) 477 (31.0) |
< 0.001 |
Table 2.
Characteristics of women in moderate increasing and high decreasing adherence groups at baseline
| Characteristic | Adherence trajectory | Total n (%) N = 412 |
P-value | |
|---|---|---|---|---|
| Moderate increasing n (%) N = 162 |
High decreasing n (%) N = 250 |
|||
| Age groups | ||||
|
< 50 years ≥ 50 years |
79 (48.8) 83 (51.2) |
134 (53.6) 116 (46.4) |
213 (51.7) 199 (48.3) |
0.33 |
| Race | ||||
|
White African American Hispanic Others |
13 (8.0) 107 (66.0) 37 (22.8) 5 (3.1) |
31 (12.4) 176 (70.4) 36 (14.4) 7 (2.8) |
44 (10.7) 283 (68.7) 73 (17.7) 12 (2.9) |
0.11 |
| Education | ||||
|
Below secondary Completed secondary Some college/ completed college |
60 (37.0) 48 (29.6) 54 (33.3) |
83 (33.3) 78 (31.3) 88 (35.3 |
143 (34.8) 126 (30.7) 142 (34.5) |
0.74 |
| Employment | ||||
|
No Yes |
108 (67.1) 53 (32.9) |
172 (68.8) 78 (31.2) |
280 (68.1) 131(31.9) |
0.71 |
| Annual income | ||||
|
= < $ 24,000 >$ 24,000 |
123 (75.9) 39 (24.1) |
197 (78.8) 53 (21.2) |
320 (77.7) 92 (22.3) |
0.49 |
| Alcohol categories | ||||
|
0 drinks/week >0–7 drinks/week >7–12 drinks/week >12 drinks/week |
105 (64.8) 49 (30.2) 3 (1.9) 5 (3.1) |
125 (50.4) 98 (39.5) 8 (3.2) 17 (6.9) |
230 (56.1) 147 (35.8) 11(2.7) 22 (5.4) |
0.02 |
| History of smoking status | ||||
|
Women who never smoked Women who smoke Women who previously smoked |
51 (31.4) 61 (37.7) 50 (30.9) |
78 (31.2) 98 (39.2) 74 (29.6) |
129 (31.3) 159 (38.6) 124 (30.1) |
0.94 |
| Depression symptoms | ||||
|
No Yes |
114 (70.4) 48 (29.6) |
183 (73.2) 67 (26.8) |
297 (72.1) 115 (27.9) |
0.53 |
| Substance use | ||||
|
No Yes |
47 (29.0) 115 (71.0) |
70 (28.0) 180 (72.0) |
117 (28.4) 295 (71.6) |
0.82 |
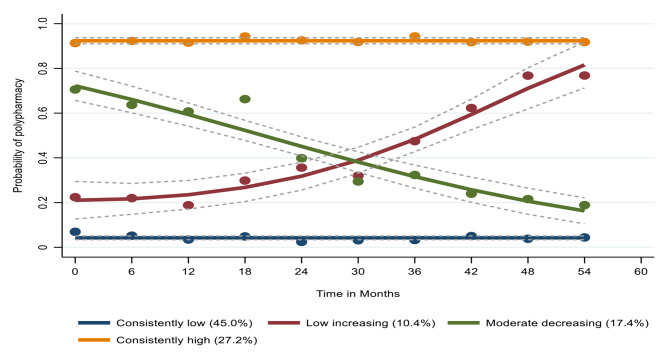
Trajectories of polypharmacy (considering all medications)
When considering all prescribed, over-the-counter, and as-needed medications and herbal supplements, GBTM identified four latent trajectories of polypharmacy, namely ‘consistently high’ (N = 418; 27.2%), ‘moderate decreasing’ (N = 268; 17.4%), ‘low increasing’ (N = 160; 10.4%), and ‘consistently low’ (N = 692; 45.0%), as shown in Fig. 3. The low increasing and moderate decreasing groups’ polypharmacy patterns altered over time, while the other groups remained largely steady. In comparing the baseline characteristics of the women who were members of those groups, we found that 11 (6.9%) of White women were in the low increasing group, while 31 (11.6%) were in the moderate decreasing group. In contrast, 125 (78.1%) African Americans were in the low increasing group, while 188 (70.1%) were in the moderate decreasing group, (P = 0.07), as shown in supplemental Table 1.
Fig. 3.
Trajectories of polypharmacy (considering all medications)
Dual trajectory model
For the joint model, the number of groups identified in the univariate analysis for each variable was found to be optimal (Supplemental Table 2). The results showed small changes in the probabilities of group membership when comparing the univariate and joint models except in the consistently low and consistently moderate, as presented in Supplemental Table 3.
Interrelationships across the trajectory groups of adherence and polypharmacy (considering all medications)
Table 3a shows the probability of trajectory group membership in polypharmacy conditional on ART adherence. The results showed that half of the women in the moderate increasing adherence group were members of the consistently low polypharmacy group compared to 46%, 44%, and 41% of the women in the consistently moderate, consistently low, and consistently high adherence groups, respectively. Table 3b shows the probability of trajectory group membership in ART adherence conditional on polypharmacy groups. The analysis showed that across all polypharmacy groups, the consistently moderate adherence group constituted the largest component as follows: 42% of the consistently low, 40% of the consistently high, 35% of the moderate decreasing, and 34% of the low increasing polypharmacy groups. Table 3c reports the joint probability of the ART adherence and polypharmacy groups, which all sum to 1. As shown in Table 3c the joint probability for women to be members of both the high decreasing adherence group and low polypharmacy group was 18%, 11.0% for women who belonged to both the high decreasing adherence group and consistently high polypharmacy group, and 8% for women grouped in both the consistently high adherence and low polypharmacy group.
Table 3.
Dual group-based trajectory modeling of polypharmacy and adherence to antiretroviral therapy
| 3a. Probability of polypharmacy group conditional on adherence group /all medications | ||||||||
| Adherence trajectory group | Polypharmacy trajectory group | |||||||
| Consistently high | Moderate decreasing | Low increasing |
Consistently low |
Total | ||||
| Consistently high | 0.31 | 0.14 | 0.14 | 0.41* | 1 | |||
| High decreasing | 0.3 | 0.22 | 0.15 | 0.33 | 1 | |||
| Moderate increasing | 0.33 | 0.15 | 0.02 | 0.5* | 1 | |||
| Consistently moderate | 0.28 | 0.16 | 0.10 | 0.46* | 1 | |||
| Consistently low | 0.13 | 0.28 | 0.15 | 0.44* | 1 | |||
| 3b. Probability of adherence conditional on polypharmacy/ all medications | ||||||||
| Adherence trajectory group | Polypharmacy trajectory group | |||||||
| Consistently high | Moderate decreasing | Low increasing |
Consistently low |
|||||
| Consistently high | 0.22 | 0.15 | 0.23 | 0.19 | ||||
| High decreasing | 0.19 | 0.21 | 0.23 | 0.14 | ||||
| Moderate increasing | 0.12 | 0.08 | 0.02 | 0.11 | ||||
| Consistently moderate | 0.40* | 0.35* | 0.34* | 0.42* | ||||
| Consistently low | 0.07 | 0.21 | 0.18 | 0.14 | ||||
| Total | 1 | 1 | 1 | 1 | ||||
| 3c. Joint probability of adherence and polypharmacy / all medications | ||||||||
| Adherence trajectory group | Polypharmacy trajectory group | |||||||
| Consistently high | Moderate decreasing | Low increasing | Low | |||||
| Consistently high | 0.06 | 0.03 | 0.03 | 0.08 | ||||
| High decreasing | 0.11* | 0.06 | 0.04 | 0.18* | ||||
| Moderate increasing | 0.05 | 0.04 | 0.03 | 0.06 | ||||
| Consistently moderate | 0.03 | 0.01 | 0.00 | 0.05 | ||||
| Consistently low | 0.02 | 0.04 | 0.02 | 0.06 | ||||
*Indicate high probability
Predictors of group membership in ART adherence trajectories
Table 4 shows the predictors of group membership for each ART adherence trajectory compared to the consistently high adherence group in the multivariable multinomial model. The results showed that significant predictors of being a member of the consistently low trajectory were younger age < 50 years, recruited from study sites in the western U.S, being non-Hispanic African American, higher education, any alcohol intake, being on ART for six or more years, and presence of depression symptoms at baseline.
Table 4.
Predictors of group membership in ART adherence trajectories compared to the reference group consistently high adherence
| Covariates | Consistently low (N = 136) aOR (95% CI) |
Consistently moderate (N = 650) aOR (95% CI) |
Moderate increasing (N = 162) aOR (95% CI) |
High decreasing (N = 250) aOR (95% CI) |
|---|---|---|---|---|
| Geographical region | ||||
|
Midwest West South Northeast |
1.0 2.6 (1.1–6.3) * 0.8 (0.4–1.9) 1.1(0.5–2.3) |
1.0 1.1(0.6- 2.0) 0.5 (0.3–0.9) * 0.6 (0.4-1.0) * |
1.0 1.7 (0.8–3.7) 0.8 (0.4–1.7) 0.7 (0.4–1.3) |
1.0 1.2 (0.5–2.7) 0.8 (0.4–1.6) 1.6 (0.9–2.9) |
| Age groups | ||||
|
≥50 years < 50 years |
1.0 2.8 (1.8–4.4) * |
1.0 1.4 (1.1–1.9) * |
1.0 1.2 (0.8–1.8) |
1.0 1.4 (0.9-2.0) |
| Race | ||||
|
White (Non-Hispanic) African American (Non-Hispanic) Hispanic Others |
1.0 2.4 (1.1–5.5) * 1.6 (0.6–4.5) 2.7(0.7–11.1) |
1.0 1.4 (0.8–2.3) 1.1 (0.6-2.0) 1.7 (0.7–4.7) |
1.0 1.7 (0.9–3.5) 2.6 (1.2–5.9) * 2.1 (0.6-8.0) |
1.0 0.9 (0.5–1.6) 0.9 (0.5–1.8) 1.1 (0.3–3.6) |
| Education | ||||
|
Below secondary Completed secondary Some college/ completed college |
1.0 1.1 (0.6–1.8) 2.1 (1.2–3.4) * |
1.0 1.4 (0.9–1.9) 1.9 (1.3–2.7) * |
1.0 1.0 (0.6–1.5) 1.4 (0.8–2.3) |
1.0 1.1 (0.7–1.7) 1.6 (1.0-2.4) * |
| Annual income | ||||
|
≤ $24,000 >$24,000 |
1.0 1.1 (0.6–1.8) |
1.0 1.3 (0.9–1.8) |
1.0 1.3 (0.8–2.1) |
1.0 0.9 (0.6–1.4) |
| Alcohol categories | ||||
|
0 drinks/week >0–7 drinks/week >7–12 drinks/week >12 drinks/week |
1.0 2.5 (1.5-4.0) * 3.5 (1.4–8.4) * 4.6 (2.0-10.6) * |
1.0 1.5 (1.1–2.1) * 1.4 (0.7–2.8) 2.0 (1.03–3.8) * |
1.0 1.1 (0.7–1.8) 0.4 (0.1–1.6) 0.7 (0.2–2.1) |
1.0 1.9 (1.3–2.8) * 1.0 (0.4–2.5) 2.1 (0.9–4.5) |
| History of smoking | ||||
|
Women who never smoked Women who smoke Women who previously smoked |
1.0 1.7 (0.9–3.2) 1.0 (0.5–1.9) |
1.0 1.1 (0.7–1.6) 0.9 (0.6–1.4) |
1.0 1.4 (0.8–2.4) 1.1 (0.6-2.0) |
1.0 1.3 (0.8-2.0) 1.1 (0.6–1.8) |
| Cumulative years on ART | ||||
|
< 6 years ≥ 6 years |
1.0 2.0 (1.13.6) * |
1.0 1.2 (0.8–1.8) |
1.0 1.5 (0.9–2.5) |
1.0 0.9 (0.6–1.4) |
|
Depression symptoms No |
1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 3.8 (2.3–6.1) * | 2.5 (1.9–3.6) * | 1.8 (1.2–2.9) * | 1.6 (1.1–2.4) * |
| Substance use at baseline | ||||
|
No Yes |
1.0 1.2 (0.7-2.0) |
1.0 1.3 (0.9–1.9) |
1.0 1.3 (0.8–2.1) |
1.0 1.2 (0.8–1.9) |
*P-value < 0.05
Abbreviation: aOR-adjusted odds ratio
Sensitivity analysis
The results of the sensitivity analysis are presented in the Supplemental file. Similar to the findings of the primary analysis, GBTM using prescription-only drugs and non-HIV drugs as a continuous variable identified four trajectory groups. As with the primary analysis, the joint model analysis in both cases revealed no interrelationship between adherence groups and polypharmacy considering prescription-only medication or non-HIV medications trajectory groups as a continuous variable.
Discussion
Our analysis revealed five latent trajectories of adherence to ART, with the consistently moderate group accounting for the largest proportion of women (42%). Considering all non-ARV drugs, GBTM identified four polypharmacy categories, with 45% of the women following a low polypharmacy trajectory. The joint model did not reveal any apparent relationship between ART adherence and polypharmacy trajectories. Likewise, the sensitivity analyses that assessed (1) prescription-only medications and (2) non-HIV as a continuous variable did not identify any evidence of an interrelationship between both variables.
In the current analysis, GBTM provided a unique perspective on the evolving nature of WHIV adherence behavior, distinguishing five categories of adherence across time. Prior studies generally utilized a traditional method of categorizing adherence into two or, at most, three categories, which miss changes in adherence over time [23]. The experiences of women who followed the moderate increasing trajectory may seem to indicate minor changes in adherence (i.e., 95–99–100%); however, such a change may be clinically meaningful. That is, social desirability bias often results in over-reporting of adherence [24]. Any reported non-adherence is therefore likely accurate and the change to complete adherence may reflect significant improvement in pill taking and the corresponding clinical benefits. Additional qualitative research is needed to identify the factors that motivated and/or facilitated their improved adherence. These findings may help in designing interventions to improve adherence among similar women. In general, the findings revealed that most predictors of membership in the continuously low and consistently moderate adherence trajectories (i.e., younger age, being non-Hispanic African American, higher education, any alcohol intake, being on ART for six or more years, and depression) have been described in the literature [25]. However, classifying women based on their adherence trajectories may shed new light on the design of a focused intervention to target these factors to improve adherence. These results revealed that women who were members of the high decreasing trajectory were more likely to consume high quantities of alcohol compared to women who were members of the moderate increasing. In addition to having a direct impact on medication-taking behavior, alcohol consumption has a negative impact on the immune system, which could result in HIV progression [26]. In another study of nearly one thousand WHIV, excessive alcohol consumption was found to be a predictor of poor adherence to ART [27]. Women in the high decreasing may benefit from combined behavioral interventions that address both adherence and alcohol consumption, as such interventions have been shown to reduce alcohol consumption and improve treatment outcomes [28].
The use of GBTM as a novel statistical approach proved to be beneficial in the analysis of polypharmacy data. The model revealed four trajectories, with 45% of all women classified in the consistently low group, which means they never used more than five medications concurrently with ART. In comparison, Ware et al. [29] used GBTM to examine polypharmacy among men participating in the Multicenter AIDS Cohort Study (MACS); four groups were identified with 48% of participants falling into a non-polypharmacy group (less than five medications with ART). A notable difference was observed in the percentage of women who consistently remain in the high polypharmacy group compared to men in the MACS study (27.2% vs. 14.2%, respectively). A population-based study in Spain analyzed a large database (23,000 PWHIV) and found polypharmacy was more common among women than among men (45% vs. 30%, respectively) [30]. High polypharmacy among women may be associated with higher rates of chronic illnesses than their male counterparts [31]. Our results showed that 17.5% of the women with polypharmacy started at a moderate level at the beginning of the study and then decreased gradually during the follow-up period. The women in this group may have stopped the use of drugs for acute illnesses or perhaps vitamins and/or herbal supplements. On the contrary, nearly 10% began with a low level of polypharmacy and gradually increased during the study. The gradual increase could be attributed to the development of chronic comorbidities over time.
Contrary to our hypothesis, neither the primary nor sensitivity analyses revealed any interrelationship between adherence groups and polypharmacy groups. Cantudo-Cuenca et al. [32] examined the impact of polypharmacy on adherence to ART, as measured by pharmacy dispensing records and the Morisky Medication Adherence Scale (MMAS), in a cross-sectional study in Spain (n = 594) and found that polypharmacy reduced adherence to ART. The difference between the two studies could be attributed to the difference in the data analysis methods, the short duration of follow-up (12 months), the smaller sample size, and the methods used to measure adherence. A possible explanation for our results is that there may be a presence of an effect modifier/s between adherence and polypharmacy, for example, depression or age. This assumption will be thoroughly investigated in further research.
The findings of this analysis have the following clinical recommendations. Firstly, adherence to ART is dynamic, so healthcare providers should counsel women about the need for a lifelong commitment to ART, check to what extent each woman adheres to her medication, explore barriers if any, and provide the necessary education and support at every clinical encounter. Healthcare providers should pay particular attention to women who have the characteristics of those belonging to low, moderate, and moderate decreasing adherence trajectories. Secondly, although we did not observe an interrelationship between polypharmacy and ART adherence, further study is needed to explore potential associations using objective adherence measures. Moreover, polypharmacy is associated with inappropriate prescribing and has known negative effects, including drug-drug interactions and drug-disease interactions [33, 34]. Rational drug use is therefore critical for all patients.
Strengths of this analysis include the robust and rich data collected on a large sample size of women who were followed for an extended period, which allows the model to identify the trajectories of both variables. In addition, non-HIV medication data was well organized and mapped, making it easy to determine the number of non-HIV medications for each woman at each visit. This study was not without limitations. Firstly, adherence to ART was measured by self-report, which may have been affected by social desirability and recall biases [35]. Secondly, although women were recruited in WIHS from different parts of the country, the obtained results may not be generalizable to all women with HIV. Finally, we cannot rule out the possibility of unmeasured residual confounding.
In conclusion, dual GBTM did not identify an interrelationship between adherence to ART and polypharmacy. Future studies should consider examining the interrelationship between the trajectories of both adherence and polypharmacy using objective measures of adherence to ART.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Author contributions
AE, Study design, data analysis, conclusions of the manuscript,
MG: data analysis, conclusions of the manuscript,
DP, DJ, SC, AA, MS, MC, BT, MP, TW, AA, JH, and DJ Study design, conclusions of the manuscript
All authors have read and acknowledged the final manuscript. All authors read and approved the final manuscript.
Funding
This publication was made possible by Grant Number T32AI007433 from the National Institute of Allergy and Infectious Diseases and the grant R25MH11985 from the National Institutes of Health. JEH was supported by grant K24MH114732. MWCCS (Principal Investigators): MG and DJ were supported by grants from the Harvard University Center for AIDS Research (HU CFAR NIH/NAIDS P30-AI 060354) and the Ragon Institute of MGH, MIT and Harvard. Atlanta CRS (Ighovwerha Ofotokun, Anandi Sheth, and Gina Wingood), U01-HL146241; Bronx CRS (Kathryn Anastos, David Hanna, and Anjali Sharma), U01-HL146204; Brooklyn CRS (Deborah Gustafson and Tracey Wilson), U01-HL146202; Data Analysis and Coordination Center (Gypsyamber D’Souza, Stephen Gange and Elizabeth Topper), U01-HL146193; Chicago-Cook County CRS (Mardge Cohen and Audrey French), U01-HL146245; Northern California CRS (Bradley Aouizerat, Jennifer Price, and Phyllis Tien), U01-HL146242; Metropolitan Washington CRS (Seble Kassaye and Daniel Merenstein), U01-HL146205; Miami CRS (Maria Alcaide, Margaret Fischl, and Deborah Jones), U01-HL146203; UAB-MS CRS (Mirjam-Colette Kempf, Jodie Dionne-Odom, and Deborah Konkle-Parker), U01-HL146192; UNC CRS (Adaora Adimora and Michelle Floris-Moore), U01-HL146194. The MWCCS is funded primarily by the National Heart, Lung, and Blood Institute (NHLBI), with additional co-funding from the Eunice Kennedy Shriver National Institute Of Child Health & Human Development (NICHD), National Institute On Aging (NIA), National Institute Of Dental & Craniofacial Research (NIDCR), National Institute Of Allergy And Infectious Diseases (NIAID), National Institute Of Neurological Disorders And Stroke (NINDS), National Institute Of Mental Health (NIMH), National Institute On Drug Abuse (NIDA), National Institute Of Nursing Research (NINR), National Cancer Institute (NCI), National Institute on Alcohol Abuse and Alcoholism (NIAAA), National Institute on Deafness and Other Communication Disorders (NIDCD), National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), National Institute on Minority Health and Health Disparities (NIMHD), and in coordination and alignment with the research priorities of the National Institutes of Health, Office of AIDS Research (OAR). MWCCS data collection is also supported by UL1-TR000004 (UCSF CTSA), UL1-TR003098 (JHU ICTR), UL1-TR001881 (UCLA CTSI), P30-AI-050409 (Atlanta CFAR), P30-AI-073961 (Miami CFAR), P30-AI-050410 (UNC CFAR), P30-AI-027767 (UAB CFAR), and P30-MH-116867 (Miami CHARM). The authors gratefully acknowledge the contributions of the study participants and the dedication of the staff at the MWCCS sites.
Data availability
The data for this analysis were provided by the MACS/WIHS combined cohort study’s Data Analysis and Coordination Center (DACC) with permission. Data will be shared on request to the corresponding author with the permission from the DACC.
Declarations
Disclaimer
The contents of this publication are solely the responsibility of the authors and do not represent the official views of the National Institutes of Health (NIH).
Ethical approval
Not applicable.
Competing interests
No relevant financial or non-financial competing interests to report.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Abubaker Ibrahim Elbur, Email: bakarelbu@yahoo.co.uk.
Musie Ghebremichael, Email: musie_ghebremichael@dfci.harvard.edu.
Deborah Konkle-Parker, Email: dkparker@umc.edu.
Deborah L Jones, Email: d.jones3@med.miami.edu.
Shelby Collins, Email: shelby.collins@emory.edu.
Adaora A. Adimora, Email: adimora@med.unc.edu
Michael F. Schneider, Email: mschnei4@jhu.edu
Mardge H. Cohen, Email: mardge.cohen@gmail.com
Bani Tamraz, Email: bani.tamraz@ucsf.edu.
Michael Plankey, Email: mwp23@georgetown.edu.
Tracey Wilson, Email: tracey.wilson@downstate.edu.
Adebola Adedimeji, Email: adebola.adedimeji@einsteinmed.edu.
Jessica E. Haberer, Email: jhaberer@partners.org
Denise L. Jacobson, Email: jacobson@sdac.harvard.edu
References
- 1.Centers for Disease Control and Prevention, Surveillance Report HIV. 2020; vol. 33. http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Published May 2022. Accessed October, 17, 2022.
- 2.Benning L, Mantsios A, Kerrigan D, et al. Examining adherence barriers among women with HIV to tailor outreach for long-acting injectable antiretroviral therapy. BMC Womens Health. 2020;20:152. doi: 10.1186/s12905-020-01011-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Menéndez-Arias L, Delgado R. Update and latest advances in antiretroviral therapy. Trends Pharmacol Sci. 2022;43:16–29. doi: 10.1016/j.tips.2021.10.004. [DOI] [PubMed] [Google Scholar]
- 4.Collins LF, Sheth AN, Mehta CC, et al. The prevalence and burden of non-AIDS comorbidities among women living with or at risk for human immunodeficiency virus infection in the United States. Clin Infect Dis. 2021;72:1301–11. doi: 10.1093/cid/ciaa204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Edelman EJ, Gordon KS, Glover J, et al. The next therapeutic challenge in HIV: polypharmacy. Drugs Aging. 2013;30:613–28. doi: 10.1007/s40266-013-0093-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Back D, Marzolini C. The challenge of HIV treatment in an era of polypharmacy. J Int AIDS Soc. 2020 doi: 10.1002/jia2.25449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Psomas CK, Hoover DR, Shi Q, Brown TT, et al. Polypharmacy is associated with falls in women with and without HIV. J Acquir Immune Defic Syndr. 2022;90:351–9. doi: 10.1097/QAI.0000000000002955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rubin LH, Neijna AG, Shi Q, et al. Degree of polypharmacy and cognitive function in older women with HIV. AIDS Res Hum Retroviruses. 2022;38:571–9. doi: 10.1089/aid.2021.0231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Okoli C, de Los Rios P, Eremin A, et al. Relationship between polypharmacy and quality of life among people in 24 countries living with HIV. Prev Chronic Dis. 2020 doi: 10.5888/pcd17.190359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zheng C, Meng J, Xiao X, et al. Polypharmacy, medication-related burden and antiretroviral therapy adherence in people living with HIV aged 50 and above: a cross-sectional study in Hunan, China. Patient Prefer Adherence. 2022 doi: 10.2147/PPA.S340621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cantudo-Cuenca MR, Jiménez-Galán R, Almeida-Gonzalez CV, et al. Concurrent use of comedications reduces adherence to antiretroviral therapy among HIV-infected patients. J Manag Care Spec Pharm. 2014;20:844–50. doi: 10.18553/jmcp.2014.20.8.844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alhazami M, Pontinha VM, Patterson JA, et al. Medication adherence trajectories: a systematic literature review. J Manag Care Spec Pharm. 2020;26:1138–52. doi: 10.18553/jmcp.2020.26.9.1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nagin DS, Odgers CL. Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol. 2010;6:109–38. doi: 10.1146/annurev.clinpsy.121208.131413. [DOI] [PubMed] [Google Scholar]
- 14.Walsh CA, Mucherino S, Orlando V, Bennett KE, Menditto E, Cahir C. Mapping the use of Group-Based Trajectory Modelling in medication adherence research: A scoping review protocol. HRB Open Res 2020 Aug 5; 3:25. doi: 10.12688/hrbopenres.13056.2. [DOI] [PMC free article] [PubMed]
- 15.Lo-Ciganic WH, Donohue JM, Jones BL, Perera S, Thorpe JM, Thorpe CT, Marcum ZA, Gellad WF. Trajectories of diabetes medication adherence and hospitalization risk: a retrospective cohort study in a large state Medicaid Program. J Gen Intern Med. 2016 Sep;31(9):1052–60. [DOI] [PMC free article] [PubMed]
- 16.Bacon MC, von Wyl V, Alden C, et al. The women’s interagency HIV Study: an observational cohort brings clinical sciences to the bench. Clin Diagn Lab Immunol. 2005;12:1013–9. doi: 10.1128/CDLI.12.9.1013-1019.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Barkan SE, Melnick SL, Preston-Martin S, et al. WIHS Collaborative Study Group. The women’s interagency HIV Study. Epidemiology. 1998;9:117–25. doi: 10.1097/00001648-199803000-00004. [DOI] [PubMed] [Google Scholar]
- 18.Adimora AA, Ramirez C, Benning L, et al. Cohort Profile: the Women’s Interagency HIV Study (WIHS) Int J Epidemiol. 2018;47:393–394i. doi: 10.1093/ije/dyy021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Radloff LS, The CES-D, Scale A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- 20.Gnjidic D, Hilmer SN, Blyth FM, et al. Polypharmacy cutoff and outcomes: five or more medicines were used to identify community-dwelling older men at risk of different adverse outcomes. J Clin Epidemiol. 2012 Sep;65(9):989–95. [DOI] [PubMed]
- 21.Danjuma MIM, Khan S, Wahbeh F, et al. What is polypharmacy in people living with HIV/AIDS? A systematic review. AIDS Res Ther. 2022;19:37. doi: 10.1186/s12981-022-00461-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jones BL, Nagin DS. A note on a Stata plugin for estimating group-based trajectory models. Sociol Methods Res. 2013;42:608–13. doi: 10.1177/0049124113503141. [DOI] [Google Scholar]
- 23.Sok P, Mgbere O, Pompeii L et al. Evaluation of the sociodemographic, behavioral, and clinical influences on complete antiretroviral therapy adherence among HIV-infected adults receiving medical care in Houston, Texas. HIV AIDS (Auckl). 2021; doi: 10.2147/HIV.S303791. [DOI] [PMC free article] [PubMed]
- 24.Wilson IB, Tie Y, Padilla M et al. Performance of a short, self-report adherence scale in a probability sample of persons using HIV antiretroviral therapy in the United States. AIDS. 2020 Dec 1;34(15):2239–2247. [DOI] [PMC free article] [PubMed]
- 25.Lambert CC, Mugavero MJ, Najjar YS, et al. The state of adherence to HIV care in black women. J Assoc Nurses AIDS Care. 2018;29:487–503. doi: 10.1016/j.jana.2018.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shuper PA, Neuman M, Kanteres F, et al. Causal considerations on alcohol and HIV/AIDS–a systematic review. Alcohol Alcohol. 2010;45:159–66. doi: 10.1093/alcalc/agp091. [DOI] [PubMed] [Google Scholar]
- 27.Frazier EL, Esser MB, McKnight-Eily LR, et al. Alcohol use among HIV-positive women of childbearing age, United States, 2013–2014. AIDS Care. 2021;33:1024–36. doi: 10.1080/09540121.2020.1808161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Scott-Sheldon LAJ, Carey KB, Johnson BT, et al. Behavioral interventions targeting alcohol use among people living with HIV/AIDS: a systematic review and meta-analysis. AIDS Behav. 2017;21:126–43. doi: 10.1007/s10461-017-1886-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ware D, Palella FJ, Jr, Chew KW, et al. Examination of polypharmacy trajectories among HIV-positive and HIV-negative, men in an ongoing longitudinal cohort from 2004 to 2016. AIDS Patient Care STDS. 2019;33:354–65. doi: 10.1089/apc.2019.0057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.López-Centeno B, Badenes-Olmedo C, Mataix-Sanjuan Á, Khoo A, Calvo-Alcántara S, Berenguer MJ, et al. Polypharmacy and drug-drug interactions in people living with human immunodeficiency virus in the region of Madrid, Spain: a population-based study. Clin Infect Dis. 2020;71:353–62. doi: 10.1093/cid/ciz811. [DOI] [PubMed] [Google Scholar]
- 31.Pond RA, Collins LF, Lahiri CD. Sex differences in non-AIDS comorbidities among people with human immunodeficiency virus. Open Forum Infect Dis. 2021 doi: 10.1093/ofid/ofab558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cantudo-Cuenca MR, Jiménez-Galán R, Almeida-Gonzalez CV, Morillo-Verdugo R. Concurrent use of comedications reduces adherence to antiretroviral therapy among HIV-infected patients. J Manag Care Spec Pharm. 2014 Aug;20(8):844–50. [DOI] [PMC free article] [PubMed]
- 33.McNicholl IR, Gandhi M, Hare CB, et al. A pharmacist-led program to evaluate and reduce polypharmacy and potentially inappropriate prescribing in older HIV-positive patients. Pharmacotherapy. 2017;37(12):1498–506. doi: 10.1002/phar.2043. [DOI] [PubMed] [Google Scholar]
- 34.Siefried KJ, Mao L, Cysique LA et al. Concomitant medication polypharmacy, interactions and imperfect adherence are common in Australian adults on suppressive antiretroviral therapy. AIDS 2018 Jan 2;32(1):35–48. [DOI] [PMC free article] [PubMed]
- 35.Simoni JM, Kurth AE, Pearson CR, et al. Self-report measures of antiretroviral therapy adherence: a review with recommendations for HIV research and clinical management. AIDS Behav. 2006;10:227–45. doi: 10.1007/s10461-006-9078-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data for this analysis were provided by the MACS/WIHS combined cohort study’s Data Analysis and Coordination Center (DACC) with permission. Data will be shared on request to the corresponding author with the permission from the DACC.